#Behavioral and Psychological Symptoms of Dementia
Explore tagged Tumblr posts
Text
Mental Health Insights: From Disorders to Treatment Strategies

Mental health is an essential aspect of overall well-being, impacting how we think, feel, and act. Understanding various mental health disorders and their treatment strategies can empower individuals and communities to foster a healthier society. In this blog, we will explore key topics including erectile dysfunction, dementia, schizophrenia, bipolar disorder, obsessive-compulsive disorder (OCD), and more, providing insights into their causes, symptoms, and effective treatment options.
Understanding Erectile Dysfunction
Erectile dysfunction (ED) is a condition that affects many men, often leading to emotional distress and relationship issues. The causes of ED can range from physical health problems, such as diabetes and heart disease, to psychological factors like stress and anxiety. Diagnostic tools, including physical exams and psychological assessments, help healthcare providers determine the underlying causes of this condition. Treatment options vary, including medication, lifestyle changes, and therapy, making it crucial for individuals to seek help when experiencing symptoms.
Dementia: Symptoms and Treatment
Dementia is a progressive condition that affects cognitive function, leading to memory loss, impaired reasoning, and changes in behavior. Common symptoms include confusion, difficulty with communication, and mood swings. Among the various types of dementia, Alzheimer’s disease is the most prevalent. Understanding the behavioral and psychological symptoms of dementia (BPSD) is vital for caregivers and healthcare professionals. Effective treatment strategies can include medication, cognitive therapy, and support from family and friends, ensuring that individuals with dementia maintain a good quality of life.
Demystifying Schizophrenia
Schizophrenia is often misunderstood, with many misconceptions surrounding its nature and treatment. This chronic mental health disorder can cause delusions, hallucinations, and disorganized thinking, severely impacting daily functioning. Dispelling myths about schizophrenia is essential for reducing stigma and promoting empathy. Treatment typically involves antipsychotic medications and psychosocial support, allowing individuals to manage their symptoms and lead fulfilling lives.
Bipolar Disorder: Navigating Mood Swings
Bipolar disorder is characterized by extreme mood swings, ranging from manic highs to depressive lows. Understanding the complexities of bipolar disorder is crucial for effective management. Early symptoms may include changes in sleep patterns, energy levels, and irritability. Treatment strategies often involve a combination of medication, therapy, and lifestyle adjustments to stabilize mood and enhance coping skills. By understanding the nature of these ups and downs, individuals can better navigate their mental health journeys.
Obsessive-Compulsive Disorder (OCD)
Obsessive-Compulsive Disorder (OCD) is a condition marked by intrusive thoughts and compulsive behaviors. Symptoms can manifest as persistent fears or worries, leading to repetitive actions aimed at reducing anxiety. In India, societal perceptions of OCD may lead to stigma, hindering individuals from seeking help. Effective treatment includes cognitive-behavioral therapy (CBT) and medication, helping individuals manage their symptoms and improve their quality of life.
The Future of Brain Stimulation for Mental Health
Innovative approaches, such as brain stimulation, are shaping the future of mental health treatment. Techniques like transcranial magnetic stimulation (TMS) and electroconvulsive therapy (ECT) have shown promise in treating conditions like depression and schizophrenia. These therapies work by modulating neural activity, offering new hope for individuals who have not responded to traditional treatments. Continued research and development in this area are essential for expanding treatment options for various mental health disorders.
Personality Disorders: Complex Behaviors
Personality disorders encompass a range of complex behaviors and emotional challenges that can impact interpersonal relationships. Conditions such as borderline personality disorder and narcissistic personality disorder can lead to difficulties in social and occupational functioning. Understanding the nuances of these disorders is vital for effective treatment, which may include therapy, medication, and support networks. By gaining insights into personality disorders, we can foster compassion and support for those affected.
Anxiety: A Natural Response to a Chronic Disorder
Anxiety is a natural response to stress; however, when it becomes chronic, it can interfere with daily life. Anxiety disorders can manifest in various forms, including generalized anxiety disorder, panic disorder, and social anxiety. Recognizing the symptoms and understanding the factors contributing to anxiety is crucial for effective management. Treatment strategies may include therapy, medication, and mindfulness practices, helping individuals regain control over their lives.
Stress, Resilience, and Health
Stress is an inevitable part of life, but how we respond to it can significantly impact our mental health. Building resilience is key to navigating life’s challenges. Stress management techniques, such as mindfulness, exercise, and social support, can enhance resilience and overall health. By understanding the relationship between stress and mental health, individuals can adopt healthier coping mechanisms and foster a supportive environment for themselves and others.
Youth Suicide: Causes and Prevention Strategies
Youth suicide is a critical issue that demands attention and action. Understanding the causes of youth suicide, including mental health disorders, bullying, and societal pressures, is vital for prevention. Implementing effective youth suicide prevention strategies involves raising awareness, providing support, and creating safe spaces for open discussions about mental health. Schools, families, and communities must work together to address this crisis and support at-risk youth.
Making Mental Health a Global Priority
Prioritizing mental health on a global scale is crucial for promoting overall well-being. Stories from individuals and communities highlight the need for accessible mental health services, education, and support systems. By sharing experiences and advocating for mental health resources, we can reduce stigma and encourage those struggling with mental health issues to seek help. Global initiatives and policies must focus on improving mental health services, ensuring that everyone has access to the care they need.
Bridging the Mental Health Gap for Indian Youth
In India, addressing the mental health needs of youth is essential for fostering a healthier future. A human-centered approach to mental health care can bridge the gap between available resources and those in need. By involving young people in the design and implementation of mental health services, we can create more effective and accessible support systems. Initiatives that focus on education, awareness, and community engagement will help empower youth to prioritize their mental well-being.
Child Mental Health Services
Investing in child mental health services is crucial for nurturing the next generation. Early intervention can help children develop healthy coping mechanisms and resilience. Understanding the signs of mental health issues in children, such as changes in behavior, academic struggles, and social withdrawal, is vital for timely support. Accessible mental health resources and trained professionals can make a significant difference in a child's life, ensuring they grow into well-adjusted adults.
Stress and Depression Among Medical Students
Stress and depression among medical students in India have become increasingly prevalent, driven by academic pressures and demanding schedules. Understanding the unique challenges faced by medical students is essential for developing effective support systems. Universities and institutions should implement mental health programs, promote work-life balance, and create environments where students feel comfortable seeking help.
Toxic Positivity and Its Impact on Mental Health
Finally, understanding toxic positivity—the belief that we should always maintain a positive attitude—can help us recognize its negative impact on mental health. This mindset can invalidate genuine feelings of sadness, anxiety, and frustration, making it difficult for individuals to express their emotions. By fostering an environment that encourages authentic emotional expression, we can promote mental well-being and support those struggling with their mental health.
Conclusion
Mental health is a multifaceted issue that requires understanding, compassion, and effective treatment strategies. From erectile dysfunction to child mental health services, each topic presents unique challenges and solutions. By fostering awareness and promoting accessible resources, we can work together to improve mental health outcomes for individuals and communities. Through education, support, and innovative approaches, we can create a future where mental health is prioritized, and everyone has the opportunity to thrive.
#Mental Health#Mental Health Disorders#Erectile Dysfunction#Dementia#Schizophrenia#Bipolar Disorder#Obsessive-Compulsive Disorder#Anxiety Disorders#Stress Management#Youth Suicide Prevention#Brain Stimulation#Personality Disorders#Child Mental Health#Toxic Positivity#Resilience#Global Mental Health#Indian Youth Mental Health#Medical Student Stress#Behavioral and Psychological Symptoms of Dementia#Mental Health Awareness
1 note
·
View note
Text
microplastics sediment in all organ systems, causing dementia-like symptoms and altered behaviour in mice.
#microplastics#plastics#organ system#dementia#symptoms#behavioural analysis unit#behavioral psychology#cognitive behavioral therapy#behavioral analysis unit#behavioral event network#behavioral health#health#ausgov#politas#auspol#tasgov#taspol#australia#neoliberal capitalism#fuck neoliberals#anthony albanese#albanese government#pollution#pollutants#polluted air#polluted water#polluters#plastic#environmentalism#environment
1 note
·
View note
Text
Chapters 1-4 of Psychosis, Trauma, and Dissociation: Historical conceptions of psychotic disorders and schizophrenia
The term 'psychosis' was first used as an alternative to terms like 'insanity' and 'lunacy.' It was coined by the Austrian physician Ernst von Feuchtersleben, taken from the Greek word 'psyche' (meaning mind or soul) and the Latin suffix '-osis' (meaning an abnormal condition). It referred to a sickness where both the body and the soul were sick, or a disease that affected 'the whole person.' The coining of this term was in response to a German psychiatry debate between mental disease located in the 'soul' and disease located in the 'body' - /Psychiker/ and /Somatiker./ Modernly, 'psychosis' is used to mean 'having psychotic symptoms.' However, psychosis is often used related to incomprehensibility. It's not new - Jaspers argued more than a century ago that 'genuine psychotic delusions' are 'not understandable.' Often, terms like "quasi-psychotic" and "psychotic-like" are used when the behavior can be made sense of in some way. The book then argues that a useful conception of the word psychosis would be one where it means that a) an alteration in the 'hierarchy of reality' has occured, and b) the person as a whole has been changed in a fundamental way.
Thomas Sydenham (1624-1689) used the term 'hysteria' to denote any mental disorder short of 'frank alienation' (outright psychosis), while Thomas Willis (1621-1675) outlined a picture in 1672 of a condition what two centuries later would be called 'dementia praecox' by Emil Kraepelin. In 1808, the term 'psychiatry' was first used by Johann Reil to refer to the treatment of the mind. Now, larger scale scientific observations could be brought to what used to be isolated accounts of individual observers. John Haslam (1766-1844) provided cases that would be consistent with what would later be called 'schizophrenia', and his 1810 book /Illustrations of madness/ detailed a single case of insanity. It was of a paranoid psychotic man, James Tilly Matthews, who believed an 'infernal machine' was controlling his life and torturing him. Haslam also recognized that in some people there were states of excitement and depression that alternated - an early recognition of bipolar disorder. In the mid-nineteenth century, the term 'psychosis' was first proposed by Ernst von Feuchtersleben to replace 'insanity' or 'lunacy.' Ironically though, he considered 'hysteria' to be a neurosis (a term proposed for any disease caused by the functioning of the nerves), and as such it was more 'biological' than psychosis… Less than a generation later, Wilhelm Griesinger helped the somaticists win the soul versus soma dispute and 'psychosis' became a term for 'organically based mental disorders.' Under Griesinger's influence, psychosis came to mean organic (caused by organic processes) and neurosis came to mean non-organic (by-products of psychological development.) Karl Ludwig Kahlbaum (1828 - 1899) labelled the disorders hebephrenia (with his student Ewald Hecker), to mean a psychosis of young adoloscents characterized by mental disorientation, and catatonia, a condition where the patient had no reactivity, was mute, and physically immobile. Emil Kraepelin (1856 - 1926), while he wrote about every major psychiatric disorder, psychosis was a major interest of his. He built upon the ideas of Griesinger and Kahlbaum, observing many patients and outlined a classification of psychosis that is still very evident in the DSM-5. Kraeplin grouped together disorders that had a poor outcome - 'catatonia', 'hebephrenia', and 'dementia paranoides.' On the sixth edition of his textbook, he outlined 'manic depressive psychosis' (bipolar disorder) and 'dementia praecox' (schizophrenic disorders.' Kraeplin claimed that on top of progressive and inevitable decline, essential features were a discrepany between thought and emotion, negativism, stereotypical behaviors, hallucinations, delusions, and disordered thought. His focus on 'inherent bodily defects' in psychiatric disorders and rapid decline led to a pessimisstic outlook on the treatment of dementia praecox. Kraepelin also described 'paranoia,' a chronic illness characterized by delusional beliefs, in the absence of personality changes. He believed paranoia was less severe and associated with partial recovery. The first use of the term 'schizophrenia' was by Eugen Bleuler (1908/1987). Over 10 years, Bleuler developed his ideas on schizophrenia in close cooperation with Carl Jung. Bleuler criticized Kraepelin's idea of dementia praecox, by saying that not all cases began early (praecox) and not all cases ended in full mental deterioration (dementia.) He proposed the term 'schizophrenia' in a Berlin psychiatry conference. The word literally means 'split mind' as he thought that /tearing apart/ ('Zerreissung') and /splitting/ ('Spaltung') were central to the disorder.
Schneider's first-rank symptoms of schizophrenia had a powerful influence on the diagnostic criteria for schizophrenia, from the 1970s onwards. They were considered sufficient but not necessary for a diagnosis of schizophrenia to be made. They were (In German, followed by their english translations): Gedankenlautwerden (audible thoughts), Stimmen in Form von Rede und Gegenrede (voices conversing or arguing), Begleitung des Tuns mit halluzinierten Bemerkungen (voices commenting on one’s behaviour), körperliche Beeinflussung (somatic influences), Gedankenentzug, Gedankeneingebung und ‐beeinflussung(thought insertion, thought withdrawal and thought influences/‘made’ thoughts), echter Wahn als Beziehungssetzung ohne Anlaß (delusional perception).
#graypost#grayrambles#psychosis#schizophrenia#psychiatry#psychology#history#nerdpost#book: psychosis trauma and dissociation
37 notes
·
View notes
Text
Psychopathology, ch 1 pt. 2
Could you describe the medical model of abnormal behavior?
- German physician Wilhelm Griesinger (1817-1868) argued that abnormal behavior was rooted in diseases of the brain.
- His views influenced another German physician named Emil Kraepelin (1856-1926), who wrote an influential textbook on psychiatry in 1883.
- According to the medical model, people behaving abnormally suffer from mental illnesses or disorders that can be classified (like physical illnesses) according to their distinctive causes and symptoms.
- Proponents of the medical model don’t necessarily believe that every mental disorder is a product of “defective” biology, but they do maintain that it’s useful to classify patterns of abnormal behavior as disorders that can be identified on the basis of their distinctive features or symptoms.
- Kraepelin specified two main groups of mental disorders:
dementia praecox (from roots meaning “precocious [premature] insanity”) which we now call schizophrenia. Kraepelin believed this was caused by a biochemical imbalance.
manic-depressive insanity, which we now call bipolar disorder. Kraepelin believed this was caused by an abnormality in the body’s metabolism.
- The medical model gained support in the late 19th century with the discovery that advanced syphilis (in which the bacterium that causes the disease directly invades the brain) led to a form of disturbed behavior called general paresis.
- General paresis is associated with physical symptoms and psychological impairment, including personality and mood changes, and with progressive deterioration of memory and judgment. Now that we have antibiotics to treat syphilis, this disorder has become extremely uncommon.
- The discovery of this connection between general paresis and syphilis inspired optimism in the scientific community, who believed that other biological causes would soon be discovered for many types of disturbed behavior. When Alzheimer’s was discovered, that lent further support to the medical model. However, an overwhelming majority of psychological disorders are more complex than scientists once thought, and we are still struggling to understand what factors are relevant, how influential they are, etc.
syndromes: clusters of symptoms that may be indicative of a particular disease or condition.
What is the major psychological model of abnormal behavior?
- Even as the medical model was gaining influence in the 19th century, some scientists argued that abnormal behavior could not have completely biological origins.
- In Paris, respected neurologist Jean-Martin Charcot (1825-1893) experimented with hypnosis as a treatment for hysteria, a condition characterized by paralysis or numbness that cannot be explained by any underlying physical cause. Hysteria was a common diagnosis in the Victorian era, but it’s quite rare today.
- Charcot’s teaching clinic was attended by a young Austrian physician named Sigmund Freud (1856-1939). Freud reasoned that if hysterical symptoms could be made to disappear or appear through hypnosis - the mere “suggestion of ideas” - then they must be psychological, not biological, in origin.
- Freud was also influenced by Viennese physician Joseph Breuer (1842-19125). He had used hypnosis to treat a 21 yr. old woman (Anna O.) for hysterical complaints which had no apparent medical basis. He encouraged her to talk about her symptoms, sometimes under hypnosis. The hysterical symptoms were taken to represent the transformation of these blocked-up emotions - forgotten but not lost - into physical complaints.
- In Anna’s case, the symptoms disappeared once the emotions were brought to the surface. Breuer labeled the therapeutic effect catharsis, or emotional discharge of feelings.
psychodynamic model: the theoretical model of Freud and his followers, in which abnormal behavior is viewed as the product of clashing forces within the personality.
What is the sociocultural perspective on abnormal behavior?
- Sociocultural theorists believe the causes of abnormal behavior may be found in the failures of society, rather than in the person. Psychological problems may be rooted in poverty, unemployment, ignorance, injustice, and lack of opportunity.
- Sociocultural theorists also focus on relationships between mental health and social factors such as gender, social class, ethnicity, and lifestyle. The social consequences of being labeled as a “mental patient” are emphasized.
- Sociocultural theorists argue that people with long-term mental health problems should have access to meaningful societal roles, rather than being stigmatized and marginalized.
What is the biopsychosocial perspective on abnormal behavior?
- Many mental health professionals take the view that abnormal behavior patterns are too complex to be understand from any single perspective, so they take into account biological, psychological, AND sociocultural causes. This is known as the biopsychosocial model or interactionist model.
What are the four major objectives of science?
Description
Explanation
Prediction
Control
theory: a formulation of the relationships underlying observed events.
What are the four major steps in the scientific method?
Formulating a research question
Framing the research question in the form of a hypothesis
Testing the hypothesis
Drawing conclusions about the hypothesis
What are the ethical principles that guide psychology research?
informed consent: research participants should receive enough information about an experiment beforehand to decide freely whether or not to participate.
confidentiality: protection of research participants by keeping records secure and not disclosing their identities.
What is the role of naturalistic research and what are its key features?
naturalistic observation method: researcher observes behavior in the field, where it happens.
- Scientists try to minimize interference with the behavior they observe, but the mere presence of an observer can cause distortion, and this must be taken into consideration.
- Naturalistic observation tells us *how* people behave, but doesn’t explain *why* people behave a certain way. Cause-and-effect is better determined through controlled experiments.
What is the role of correlational research and what are its key features?
correlational method: the use of statistical methods to examine relationships between two or more variables.
correlational coefficient: a statistical measure of the strength of the relationship between two variables expressed along a continuum that ranges between -1.00 and +1.00.
CORRELATION IS NOT CAUSALITY!
longitudinal study: a type of correlational study in which individuals are periodically tested or evaluated over lengthy periods of time.
What is the role of experimental research and what are its key features?
experimental method: allows scientists to demonstrate causal relationships by manipulating the (suspected) causal variable and measuring its effects under controlled conditions that minimize the risk of other variables explaining the results.
independent variables: factors hypothesized to play a causal role; manipulated or controlled by the investigator.
dependent variables: factors observed in order to determine the effects of manipulating the independent variable; measured but not manipulated by the experimenter.
experimental group: in an experiment, the group that receives the experimental treatment.
control group: in an experiment, a group that does not receive the experimental treatment.
random assignment: a method of assigning research subjects at random to experimental or control groups to balance the characteristics of people who comprise them.
selection factor: differences in the types of people who would select to be in one group or the other.
blind: research participants are uninformed about the treatments they are receiving in order to control for their expectations.
placebo: an inert drug that physically resembles the active drug.
- In a single-blind placebo-control study, research participants are randomly assigned to treatment conditions in which they receive either an active drug or an inert placebo, but are not told which drug they receive.
- In a double-blind placebo control design, neither the researcher nor the subject knows who is receiving the active drug or the placebo.
internal validity: the degree to which manipulation of the independent variables can be causally related to changes in the dependent variables.
external validity: the degree to which experimental results can be generalized to other settings and conditions.
construct validity: (1) in experimentation, the degree to which treatment effects can be accounted for by the theoretical mechanisms (constructs) represented in the independent variables; (2) in measurement, the degree to which a test measures the hypothetical construct that it purports to measure.
What is the role of epidemiological research and what are its key features?
epidemiological method: examines rates of occurrence of abnormal behavior in various settings or population groups.
survey method: a research method in which samples of people are questioned by means of a survey instrument such as a questionnaire or interview protocol.
incidence: the number of new cases occurring during a specific period of time.
prevalence: the overall number of cases of a disorder existing in the population during a given period of time.
random sample: a sample that is drawn in such a way that every member of a population has an equal chance of being included.
- Random sampling refers to the process of randomly choosing individuals within a target population to participate in a survey or research study.
- Random assignment refers to the process by which members of a research sample are assigned at random to different experimental conditions or treatments.
What is the role of kinship studies? What are their key features?
- Kinship studies attempt to disentangle the roles of heredity and environment in determining behavior.
genotype: set of traits specified by our genetic code.
People who possess genotypes for particular psychological disorders have a genetic predisposition that makes them more likely to develop the disorders in response to stressful life events, physical or psychological trauma, or other environmental factors.
phenotype: constellation of observable or expressed traits.
represents the interaction of genetic and environmental influences
proband, AKA index case: the case first diagnosed with a given disorder.
concordance rate: percentage of cases in which both twins have the same trait or disorder.
Researchers prefer to use monozygotic twins, but they also study dizygotic twins.
adoptee studies: studies that compare the traits and behavior patterns of adopted children to those of their biological parents and their adoptive parents.
What is the role of case studies? What are their limitations?
case studies: intensive studies of individuals.
can be based on historical material and involve subjects who passed long ago
More commonly, case studies reflect an in-depth analysis of an individual’s course of treatment. They typically include detailed histories of the subject’s background and response to treatment.
Unfortunately, they can’t be generalized, and the accuracy of the material varies.
single-case experimental design: a type of case study in which the subject is used as their own control.
reversal design: an experimental design that consists of repeated measurement of a subject’s behavior through a sequence of alternating baseline and treatment phases.
critical thinking: adoption of a questioning attitude and careful scrutiny of claims and arguments in light of evidence.
Maintain a skeptical attitude.
Consider the definitions of terms.
Weigh the assumptions or premises on which arguments are based.
Bear in mind that correlation is not causation.
Consider the kinds of evidence on which conclusions are based.
Do not oversimplify.
Do not overgeneralize.
4 notes
·
View notes
Text
Dealing with Dementia and Alzheimer's: How Tulasi Healthcare Supports Families

Dementia and Alzheimer’s disease are among the most challenging conditions faced by both individuals and their families. As these cognitive disorders affect memory, behavior, and the ability to perform everyday tasks, families often feel overwhelmed, stressed, and unsure of how to provide the right care. At Tulasi Healthcare, we understand the complexities of dementia and Alzheimer’s and offer comprehensive support to families navigating this difficult journey. With the guidance of the best psychiatrist in East Delhi, we ensure that both patients and their families receive the care, understanding, and tools needed to cope with the emotional and practical challenges these conditions present.
Understanding Dementia and Alzheimer’s
Dementia is a general term used to describe a decline in cognitive ability severe enough to interfere with daily life. Alzheimer's disease is the most common type of dementia, characterized by memory loss, confusion, and changes in behavior. These conditions affect not only the individuals diagnosed but also their families, as they face the emotional and logistical challenges of caregiving.
At Tulasi Healthcare, we recognize the unique difficulties that come with caring for loved ones with dementia or Alzheimer's. Our services are designed to provide both direct care for patients and guidance and support for family members.
How Tulasi Healthcare Supports Families
Expert Diagnosis and Medical Management
One of the first steps in dealing with dementia and Alzheimer’s is obtaining a correct diagnosis. Often, cognitive decline is mistakenly attributed to aging, so early diagnosis is essential to plan for effective treatment. At Tulasi Healthcare, the best psychiatrist in East Delhi provides thorough evaluations, helping families understand the specific type of dementia or Alzheimer's their loved one is facing.
Through diagnostic testing, mental health assessments, and careful monitoring of symptoms, our experts create personalized care plans that address both medical needs and quality of life considerations. Medication management is also an essential aspect of the care we offer, ensuring that any underlying health conditions are treated effectively and that medications are used to alleviate symptoms.
Tailored Cognitive Therapies
Cognitive stimulation therapy (CST) and other non-pharmacological therapies are crucial for slowing the progression of dementia and improving the quality of life for individuals with Alzheimer's. At Tulasi Healthcare, we offer specialized cognitive rehabilitation programs designed to engage patients’ memory, language, and problem-solving skills. These therapies can help delay the worsening of symptoms and provide a sense of purpose and accomplishment to patients.
Our best psychiatrist in East Delhi works closely with caregivers to implement these therapies, ensuring that the treatment plan is aligned with each patient’s specific needs and cognitive abilities. By engaging in these therapies, patients can maintain their cognitive functions for longer and enjoy a better quality of life.
Emotional and Psychological Support for Families
Caring for a loved one with dementia or Alzheimer’s can be emotionally exhausting. Many caregivers experience feelings of sadness, frustration, and guilt as they witness the decline of someone they love. At Tulasi Healthcare, we provide emotional support for families to help them manage these feelings and cope with the stress of caregiving.
Our team, including the best psychiatrist in East Delhi, offers counseling and therapy sessions tailored to family members, helping them understand the nature of dementia and Alzheimer’s. These sessions provide a safe space to express emotions, share experiences, and receive coping strategies. We also provide resources on managing caregiver stress and preventing burnout, ensuring that families can maintain their own mental health while caring for their loved ones.
Family Education and Training
One of the most significant challenges faced by families of dementia and Alzheimer's patients is understanding how to care for their loved ones effectively. Tulasi Healthcare offers educational programs to help families learn about dementia, its progression, and the best caregiving practices. These training sessions empower families to provide safe and compassionate care at home.
The best psychiatrist in East Delhi plays a pivotal role in this education by guiding families through the medical aspects of dementia care, offering advice on communication strategies, and teaching techniques to manage behavioral changes. By helping families understand the disease, we ensure they feel more confident in providing care and making informed decisions for their loved one’s future.
Supportive Environment for Patients
Creating a safe and supportive environment for individuals with dementia and Alzheimer’s is crucial in maintaining their independence and dignity. At Tulasi Healthcare, we work with families to make adjustments to the home environment, ensuring that it is both safe and conducive to the needs of patients. This may involve recommending modifications to minimize hazards, such as removing tripping hazards or ensuring easy access to necessary items.
For patients who require more intensive care, we provide recommendations for day-care programs or long-term care options that align with the patient’s specific condition and needs. We also offer respite care services to give family caregivers a much-needed break while ensuring their loved one receives professional care.
Building a Support Network
Dealing with dementia or Alzheimer’s can feel isolating for families. At Tulasi Healthcare, we encourage the creation of a support network through support groups, both online and in-person. These groups offer a space for caregivers to connect with others facing similar challenges, share advice, and gain emotional support.
The best psychiatrist in East Delhi helps facilitate these support groups, ensuring that participants receive expert guidance and counseling as they navigate their caregiving journey. Building a strong support network provides families with the reassurance and strength they need to continue providing care with compassion.
Conclusion
Dealing with dementia and Alzheimer’s is a long and often challenging journey, but with the right support, families can navigate it with greater ease and confidence. At Tulasi Healthcare, we are dedicated to supporting both patients and families with expert care, educational resources, emotional support, and personalized treatment plans. With the guidance of the best psychiatrist in East Delhi, we ensure that families have the tools and understanding needed to provide the best care for their loved ones and themselves.
If you or someone you love is facing dementia or Alzheimer’s, Tulasi Healthcare is here to offer the comprehensive care and support you need. Together, we can create a better quality of life for both patients and their families, allowing them to cope with these conditions with dignity, compassion, and understanding.
0 notes
Text
هل الهياج في الدمنشيا يستدعي الحجز؟
[11/27, 10:39 AM] Ahmed Shawky M: وعليكم السلام ورحمة الله وبركاته ألف لا بأس عليه حالات الهياج في من لديه دمنشيا من نوع ألزهيمر نوعين:
إما إستمرارية لمرض ألزهيمر ويطلق عليها Behavioral and psychologic symptoms of dementia
وإما إختلاط عقلي حاد Delirium on top of dementia [11/27, 10:41 AM] Ahmed Shawky M: الإختلاط العقلي هو ما قد يستدعي الحجز للتعامل مع أسبابه
ينصح بذهاب أحد من الأسرة لعيادة طب المسنين العامة في مستشفى الشهيد المهندس أحمد شوقي لطب المسنين داخل مستشفى الباطنة
ومعه كل التحاليل والفحوصات السابقة
يتم عمل تقييم مبدئي بناءا على المتوافر من معلومات ويقدموا النصح المطلوب إما حجز أو متابعة بالعيادة الخارجية
ندعو بالشفاء والعافية للجميع [11/27, 10:42 AM] Ahmed Shawky M: طبعا يوجد أزمة في أسرة المستشفيات الجامعية محتمل يحتاج حجز ولكن أحيانا لا تتوافر سراير عادية، متاح عدد قليل سراير إقتصادية [11/27, 10:43 AM] Ahmed Shawky M: حل آخر تنسيق زايرة منزلية أو زيارة بعيادة طبيب مسنين
أنصح بالزميل د هشام البحيري [11/27, 10:44 AM] Ahmed Shawky M: وأرجو قراءة هذه الملخصات السريعة
0 notes
Link
The seven phases of Alzheimer's disease are distinguished by a variety of symptoms, which can range from forgetfulness to profound behavioral and psychological abnormalities. The most prevalent kind of dementia—a word used to describe a general deterioration in mental capacity—is Alzheimer's disease. The severity of symptoms and the course of the disease can be predicted using the three broad stages of Alzheimer's, according to the Alzheimer's Association: Mild (early stage): Mild symptoms, general forgetfulness. Moderate (middle stage): Disabling symptoms, more care needed. Severe (late stage): Significant behavioral and personality changes, lack of awareness. Alzheimer's disease can also be diagnosed by medical professionals using the seven key clinical phases identified by Dr. Barry Reisberg in his 1982 Global Deterioration Scale. Since different doctors have different preferences for staging systems, your doctor might employ the one they are most comfortable with. To find out more about the seven phases of Alzheimer's and how to get ready for what's ahead, continue reading. 1. Alzheimer's preclinical stages, or no impairment2. Extremely slight impairment or ordinary forgetfulness3. Mild impairment or decline4. Mild Alzheimer’s, or moderate decline5. Moderately severe deterioration or moderate dementia6. Moderately severe Alzheimer’s7. Severe Alzheimer’sA note on progressionTreating Alzheimer’sIs Alzheimer's preventable?Frequently requested inquiriesWhat is the timeline for Alzheimer’s to death?When do patients with Alzheimer's disease start to forget about their relatives?How long does Alzheimer's endure in its final stage?What is the typical age of an Alzheimer's patient who passes away?Conclusion 1. Alzheimer's preclinical stages, or no impairment Only if a doctor finds biomarkers that suggest your risk or based on your family history will you be aware of your Alzheimer's disease risk. A doctor will ask you about memory problems if you are at risk for Alzheimer's. During the first stage, which might extend for years or decades, there are usually no symptoms. On the other hand, evidence from study indicates that your brain is changing. Alzheimer's disease has been linked to abnormal tau protein accumulation in the fluid surrounding the brain and spinal cord. This protein can change in amounts up to 15 years before symptoms appear. 2. Extremely slight impairment or ordinary forgetfulness People over 65 are primarily affected by Alzheimer's disease. It's normal to experience mild functional impairments at this age, such forgetfulness. On the other hand, if you have stage 2 Alzheimer's, your cognitive deterioration can happen more quickly than it would for someone without the disease. For instance, you might have memory lapses where you forget the names of family members, common words, or where you put things. 3. Mild impairment or decline Mild cognitive impairment characterizes Alzheimer's disease at stage three. The Fisher Center for Alzheimer's Research Foundation states that stage 3 lasts roughly 7 years, however symptoms start to show up over a period of 2-3 years. The symptoms are probably only noticeable to those closest to you. Among the stage 3 indications and symptoms could be: decline in work quality difficulty picking up new skills becoming disoriented while taking a familiar route having trouble recalling the proper terms or names losing your memory of what you just read not remembering new names or people misplacing or losing a valuable object losing focus when taking a test To diagnose memory loss, a medical expert could question you more thoroughly than normal. 4. Mild Alzheimer’s, or moderate decline Stage 4 is when Alzheimer's disease can be diagnosed and lasts for roughly two years. At this point, you might encounter: challenges relating to more complicated daily chores, like finances more noticeable emotional swings, like denial and withdrawal decreasing emotional responses a declining consciousness of recent or present events forgetting one's own past A doctor will search for a decrease in the areas that were specified in stage 3. 5. Moderately severe deterioration or moderate dementia A person with Alzheimer's in stage 5 needs a lot of assistance, and the stage lasts for roughly 1.5 years. Anger and mistrust are common emotions experienced by those who don't have enough support. You might be able to recollect the names of your immediate family members at this point, but you might be having trouble remembering significant occasions, the state of the weather, or current addresses. You can also have trouble counting backward and feel disoriented in terms of place or time. 6. Moderately severe Alzheimer’s Over a 2.5-year period, five distinguishable traits emerge at stage 6: 6a. Clothes: Assistance with selecting and putting on clothing may be required. 6b. Hygiene: Your dental health starts to deteriorate, and you might require assistance setting the water's temperature before taking a bath. 6c, 6d, and 6e. Toilet: You can overlook the need to flush or discard the tissue paper. As the condition worsens, you may require assistance with personal hygiene and eventually lose control over your bowels and bladder. By stage 6, memory is considerably weaker, particularly in relation to recent events and the news. You may find it difficult to count backwards from ten and may mistake family members for strangers. It is feasible to encounter: personality shifts fear of being alone fidgeting frustration stuttering shame suspicions paranoia Counseling for behavioral and psychological issues must be continued. 7. Severe Alzheimer’s Stage 7 of Alzheimer's disease has substages that can last up to 2.5 years each: 7a: The interview is limited to six words or less, and the doctor may have to repeat questions. 7b: Speech reduces to a single, understandable word. 7c: The ability to speak is gone. 7d: You won't be able to sit up on your own. 7e: Smiling faces give way to somber ones. 7f: You won't be able to raise your head at all. Your body may start to move more stiffly and painfully. About 40% of Alzheimer's patients also develop contractures, or the shortening and hardening of tendons, muscles, and other tissues, according to the Alzheimer's Association. Additionally, you might acquire infantile reflexes like sucking. During this phase, some people may become immobilized. Pneumonia is the most common cause of mortality for those with stage 7 Alzheimer's disease. A note on progression The disease usually proceeds slowly, with symptoms ranging from moderate to severe. Each person will experience the condition at a different rate. According to a 2018 study, individuals in the preclinical stage (1) who were 65 years of age or older had a 92% chance of continuing to think at the same level the following year, while those who were 75 years old had a 90% chance. After 65 years of age, your chance of getting the disease also increases every five years. Treating Alzheimer’s Alzheimer's has no known cure, however medication may help delay each stage of the illness. The goal of treatment is to control behavior and mental health while delaying the onset of symptoms. Your regimen may consist of one or more of the following: medications therapy and counseling alternative treatments, like dietary and lifestyle modifications Collaborating with a medical team and a network of friends, family, and caregivers is crucial. Together, they can create the most effective treatment strategy to improve your quality of life and decrease the disease's progression. Is Alzheimer's preventable? Scientists are still working to better understand Alzheimer's and develop preventative measures. Alzheimer's disease and cognitive decline are linked to the following risk factors: diabetes depression cardiovascular disease mental inactivity poor diet physical inactivity obesity high blood pressure low education level Once symptoms appear, medications might not be able to significantly change how Alzheimer's disease progresses. On the other hand, taking certain precautions could lessen your risk of contracting the illness. Regular exercise, for instance, may help prevent Alzheimer's disease from developing or reduce its progression. Frequently requested inquiries What is the timeline for Alzheimer’s to death? Each person with Alzheimer's disease has a very different prognosis. An average person with Alzheimer's disease lives for 5.8 years after being diagnosed. Some people do, however, live longer than 20 years. When do patients with Alzheimer's disease start to forget about their relatives? During stage 2, people with Alzheimer's disease may have memory loss and forget the names of family members. It could get harder for you to remember names as the illness advances into later stages. How long does Alzheimer's endure in its final stage? Alzheimer's disease in stage 7 typically lasts 1.5–2.5 years. What is the typical age of an Alzheimer's patient who passes away? In the US, Alzheimer's disease ranks as the fifth most common cause of mortality for those 65 years of age and older (Trusted Source). The age group 85 years and older has seen the biggest increase in the death rate. Conclusion Cognitive decline is a gradual symptom of Alzheimer's disease. Depending on how severe your symptoms are, some medical practitioners divide it into seven stages. It takes a lot of work to care for someone who has Alzheimer's disease. Being a caregiver will cause you to feel a variety of emotions. You may be able to learn and share effective techniques and approaches for handling difficult circumstances via support groups. Search here
0 notes
Video
youtube
🔴🇮🇹 VECCHIAIA MAI PIÙ audio DCS di ipnosi DCS Vera e professionale unica...
DEMENZA SENILE: SOLUZIONE IPNOSI NO DEMENZA SENILE
https://www.claudiosaracino.com/prodotto/vecchiaia-mai-piu-metodo-dcs/ Il
rapporto tra ipnosi professionale e demenza senile è un campo di studio emergente che ha attirato l’attenzione della ricerca, in particolare per quanto riguarda l'uso dell'ipnosi come strumento complementare per il trattamento dei sintomi della demenza, come l’ansia, l’agitazione e alcuni deficit cognitivi. Di seguito troverai 10 ricerche scientifiche accreditate e 3 testimonianze di personaggi celebri che hanno condiviso le loro esperienze personali riguardo la demenza senile e il potenziale beneficio dell'ipnosi professionale. Ricerche Scientifiche Accreditate A Pilot Study of Hypnosis to Improve the Quality of Life in Patients with Dementia - Pubblicata su The International Journal of Clinical and Experimental Hypnosis, questa ricerca esplora l'uso dell'ipnosi per migliorare la qualità della vita dei pazienti con demenza, riducendo l'ansia e migliorando l'umore. Hypnotic Treatment of Anxiety in Dementia Patients - Uno studio pubblicato su The American Journal of Alzheimer's Disease and Other Dementias, che analizza come l'ipnosi possa ridurre significativamente i sintomi di ansia nei pazienti affetti da demenza. Hypnosis as a Therapeutic Tool for Patients with Alzheimer's and Other Forms of Dementia - Pubblicato su Psychology and Aging, questo studio esplora come l'ipnosi possa aiutare a ridurre l'agitazione e migliorare la concentrazione nei pazienti con demenza. Mind-Body Interventions for Dementia Care: Hypnosis as a Potential Option - Ricerca su Geriatric Nursing che analizza il ruolo delle terapie mente-corpo, inclusa l'ipnosi, per il trattamento dei sintomi comportamentali della demenza. Cognitive and Emotional Benefits of Hypnosis in Mild Cognitive Impairment and Dementia - Pubblicato su Clinical Gerontologist, questo studio mostra come l'ipnosi possa offrire miglioramenti nel recupero di memoria e riduzione dell’ansia nei pazienti con decadimento cognitivo lieve. Hypnotherapy for Dementia: A Review of the Literature - Una revisione sistematica pubblicata su Aging and Mental Health che valuta gli effetti dell'ipnosi sui pazienti con demenza, riscontrando miglioramenti nella qualità del sonno e nella gestione del dolore. Application of Hypnotherapy in Dementia-related Anxiety - Studio pubblicato su Dementia and Geriatric Cognitive Disorders, che esplora l'uso dell'ipnosi come metodo per ridurre l'ansia nei pazienti con demenza avanzata. Effects of Hypnotherapy on Cognitive and Behavioral Symptoms in Alzheimer’s Disease - Uno studio su The Journal of Aging Research, che mostra come l'ipnosi possa essere efficace nel ridurre comportamenti aggressivi e migliorare l'umore dei pazienti. Hypnosis and Relaxation in Dementia Treatment - Pubblicato su American Journal of Geriatric Psychiatry, lo studio analizza l'efficacia dell'ipnosi nel ridurre l'agitazione e migliorare la cooperazione dei pazienti durante i trattamenti. Therapeutic Hypnosis for Symptom Relief in Alzheimer's and Dementia - Studio su Alzheimer's and Dementia: Translational Research & Clinical Interventions che sottolinea come l'ipnosi possa contribuire a migliorare la qualità della vita dei pazienti con demenza tramite la riduzione dello stress. Testimonianze di Personaggi Celebri Glen Campbell – Il famoso musicista country Glen Campbell, diagnosticato con l'Alzheimer nel 2011, ha utilizzato tecniche di rilassamento e ipnosi per affrontare l'ansia e lo stress. La sua famiglia ha raccontato come queste pratiche abbiano migliorato la sua tranquillità durante i suoi ultimi anni. Barbara Windsor – L'attrice britannica, conosciuta per la sua partecipazione a EastEnders, ha parlato dell'importanza di trovare tecniche alternative per migliorare la qualità della vita durante la sua battaglia con l'Alzheimer. Windsor ha provato l’ipnosi per rilassarsi e gestire l'ansia associata alla perdita di memoria. Terry Pratchett – Lo scrittore britannico, affetto da demenza a corpi di Lewy, era un sostenitore di terapie alternative. Ha sperimentato diverse tecniche di rilassamento, inclusa l'ipnosi, e ha dichiarato pubblicamente il suo supporto per le pratiche che potevano contribuire a ridurre la sua ansia e migliorare la qualità della vita.
scopri di più:
NO DEMENZA SENILE
https://www.claudiosaracino.com/prodotto/vecchiaia-mai-piu-metodo-dcs/
0 notes
Text
Process Documentation - Wearable device
Wearable: some form of custom device that can be worn on the body, that either
senses something about the body or the environmental context of the wearer, or
gathers data from the internet and translates it into some form of communication/alert/action to/on the body, or
responds in some other way to the body, or the environment, or the relationship between the two
Initial Research -
What elements contributes to agitation in an elderly person with a cognition impairment.
how can we use sensors to detect biometric information in a bid to reduce the use of chemical restraints and sedatives in an Emergency Department.
DEMENTIA
This neurocognitive decline can make it difficult for people living with dementia to process and manage environmental stimuli as they become more vulnerable to social and physical stressors (Kales et al., 2015; Smith et al., 2004)
As a result, up to 90% of people living with dementia will at some stage develop Behavioural and Psychological Symptoms of Dementia (BPSD) (Lagana et al., 2022), manifesting in various verbal and nonverbal behaviours, including apathy and depression (Tible et al., 2017). More overt forms of BPSD are referred to as ‘responsive behaviours’, understanding that they often reflect an attempt to communicate or respond to a situation or environment (Yous et al., 2019). Of these responsive behaviours, agitation and aggression are often considered the most distressing form, as they may compromise the safety of the person living with dementia and those around them (Tible et al., 2017).
Behavioural and psychological symptoms of dementia often present or are exacerbated during acute hospital admission. This is in response to common physical stressors, such as temperature, light and noise levels and social stressors, such as the inability to communicate and form therapeutic relationships (Caspar et al., 2018; Lourida et al., 2020).
DEMENTIA - Sundowning
Sundowning, also known as "sundowner's syndrome," refers to a phenomenon commonly observed in individuals with dementia, particularly during the late afternoon or evening. Here’s an overview of what it involves:
Characteristics of Sundowning
Increased Agitation: Individuals may become more restless, anxious, or agitated as the day progresses. This can manifest as irritability, confusion, or aggressive behavior.
Confusion: People may experience heightened confusion or disorientation during the evening hours, leading to difficulty recognizing familiar surroundings or people.
Mood Changes: Emotional swings can become more pronounced, with individuals exhibiting sadness, anger, or frustration.
Sleep Disturbances: Sundowning can also be associated with difficulties in falling asleep or staying asleep, contributing to overall fatigue and agitation.
Causes
While the exact cause of sundowning is not fully understood, several factors may contribute to its occurrence:
Circadian Rhythm Disruption: Changes in the body’s internal clock may lead to increased confusion during evening hours.
Fatigue: Accumulated fatigue throughout the day can contribute to heightened agitation and confusion.
Reduced Lighting: Diminished natural light in the evening can create shadows and unfamiliarity, leading to anxiety.
Overstimulation: A busy day with too much activity or noise may overwhelm the individual as the day winds down.
Management Strategies
To help manage sundowning, caregivers can consider several approaches:
Establish a Routine: Maintaining a consistent daily schedule can provide a sense of security and predictability.
Create a Calm Environment: Dim lights and reduce noise in the evening to create a calming atmosphere. Soft music or familiar scents may help.
Encourage Relaxation: Activities such as gentle stretching, reading, or listening to soothing music can promote relaxation in the evening.
Limit Stimulants: Reducing caffeine or sugar intake later in the day may help decrease agitation.
Monitor Activity Levels: Ensure that the individual is engaged throughout the day but avoid overstimulation.
Provide Reassurance: Offering comfort and reassurance during episodes of confusion can help alleviate anxiety.
PITCHED - Pain, infection, Thirst, constipation, Hunger, Environment and Drugs.
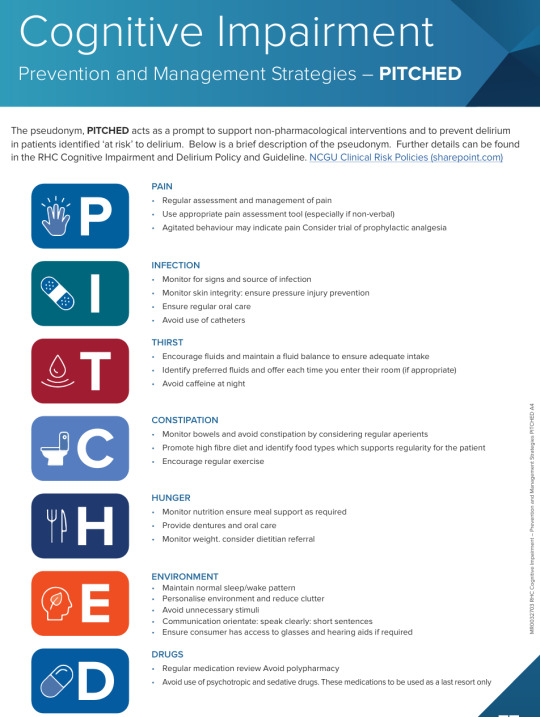
Agitation in an emergency department is common for elderly people especially with dementia and delirium.
Environment Factors
Unfamiliar Environment: The ED can be chaotic and disorienting, leading to increased anxiety and agitation.
Sensory Overload: Bright lights, loud noises, and the presence of many people can overwhelm elderly patients, causing distress.
Lack of Routine: Disruption of familiar routines can heighten feelings of insecurity and agitation.
Psychological Factors
Anxiety and Fear: Concerns about their health, treatment, or being in an unfamiliar environment can lead to heightened anxiety.
Cognitive Decline: Patients with dementia or cognitive impairment may struggle to understand their situation, leading to frustration and agitation.
Social Isolation: Feelings of loneliness or separation from caregivers or loved ones can contribute to agitation.
Social and Emotional Factors
Loss of Independence: The perception of losing control or independence can provoke agitation.
Past Trauma or Experience: Previous negative experiences in medical settings can trigger anxiety and agitation in similar situations.
Current Research
Smart Devices and Wearable Technologies to Detect and Monitor Mental Health Conditions and Stress: A Systematic Review - PMC (nih.gov)
Vital signs, neural activity (electroencephalogram ((EEG)), heart rate (electrocardiogram ((ECG)), skin temperature, and skin conductance response (electrodermal activity) can provide important information about an individual’s health status.
Devices that can sense increased agitation typically rely on various types of sensors and technology. Here are some common examples:
Wearable Devices: Smartwatches and fitness trackers often have sensors that monitor heart rate, skin temperature, and galvanic skin response, which can indicate stress or agitation.
Mobile Apps: Some apps analyze voice tone and speech patterns to detect changes in emotional states, potentially indicating agitation.
Environmental Sensors: Cameras with facial recognition software can assess changes in facial expressions that may signal agitation.
Biometric Sensors: Devices that measure physiological responses like blood pressure, heart rate variability, and respiration can indicate heightened agitation.
Smart Home Devices: Certain smart home systems can integrate multiple sensors (like cameras and environmental sensors) to monitor behavior and detect signs of agitation.
Therapeutic Robots: Some robots designed for emotional support can sense agitation through vocal and visual cues and respond accordingly.
What already currently Exists on the market
Dementia-friendly wearable devices designed to detect agitation focus on user-friendliness, comfort, and reliability. Here are some options:
Smartwatches:
Apple Watch: Features like heart rate monitoring and fall detection can help caregivers notice signs of agitation.
Fitbit: Models with heart rate and sleep tracking can alert caregivers to unusual patterns.
Fitness Trackers:
Garmin Vivosmart: This tracker monitors activity levels and can provide insights into changes in behavior or agitation through activity patterns.
Specialized Wearables:
Mindset: A device designed specifically for older adults that monitors stress levels and can alert caregivers if agitation is detected.
Seniors’ Comfort Devices: Some wearables focus on providing calming stimuli, which can help in managing agitation.
Smart Clothing:
Certain textiles integrated with sensors can monitor heart rate and stress levels, providing data to caregivers.
GPS Trackers:
While not specifically for agitation, devices like the AngelSense can help caregivers monitor location and movement patterns, which can indicate agitation or wandering.
Emotion-Sensing Wearables:
Devices like Empatica Embrace can detect physiological signs of stress and send alerts to caregivers.
When selecting a device, consider ease of use, comfort, and the specific needs of the individual with dementia to ensure it fits seamlessly
their daily life.
INTERNET OF THINGS IOT
Lots of work has been done however they are all facing the similar issues in which many of them test the prototype and get not so good feedback about the size, shape, design, and so on.
IoT-Based Wearable Devices for Patients Suffering from Alzheimer Disease - PMC (nih.gov)
Galvanic skin response (GSR) is generally considered a useful measure of physiological arousal, but its accuracy can vary based on several factors:
Sensitivity to Changes: GSR is sensitive to emotional and physiological changes, making it good for detecting arousal related to agitation, stress, or excitement.
Individual Differences: Responses can vary significantly between individuals due to factors like skin type, hydration levels, and baseline stress levels.
Context: Environmental factors, such as temperature and humidity, can influence GSR readings, affecting accuracy.
Calibration: Accurate interpretation often requires proper calibration and context-specific understanding, as GSR alone doesn’t provide insights into the specific emotions being experienced.
Supplementary Data: For improved accuracy, GSR is often used alongside other physiological measures (like heart rate or respiration) and behavioral observations.
While GSR can be a valuable tool in monitoring emotional states, it's best used as part of a broader assessment strategy rather than in isolation.
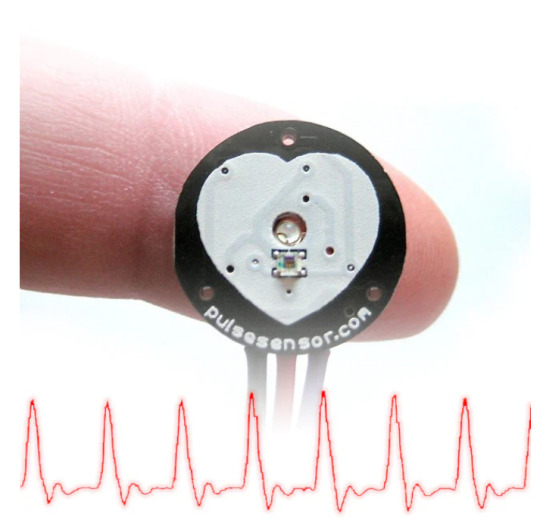
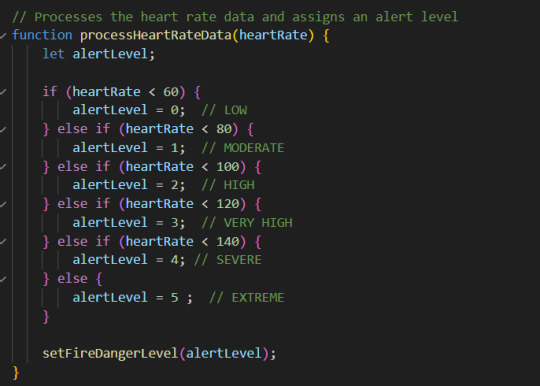
What vital sign is the biggest predictor of agitation
The heart rate is often considered the most significant predictor of agitation. Elevated heart rates can indicate increased physiological arousal, which is commonly associated with agitation, anxiety, or stress.
While other vital signs like blood pressure and respiration rate can also signal agitation, heart rate changes tend to be more immediate and responsive to emotional states. Monitoring heart rate variability can provide further insights into a person’s stress levels and overall emotional well-being.
Combining heart rate data with observations of behavior can enhance the understanding of agitation in individuals, especially in those with conditions like dementia.
heart rate data and irratic movement predictor of agitation
Heart Rate: An elevated heart rate is often a direct indicator of physiological arousal associated with stress or agitation. Sudden spikes in heart rate can signal acute agitation.
Erratic Movement: Increased physical activity, such as pacing, fidgeting, or other restless movements, often correlates with agitation. These behaviors can indicate discomfort, anxiety, or a need to escape a stressful situation.
When monitored together, these two factors can provide a clearer picture of a person's emotional state:
Correlation: A simultaneous increase in heart rate and erratic movement can reinforce the idea that the individual is experiencing significant agitation.
Timeliness: Changes in heart rate can occur quickly, allowing caregivers to respond promptly to signs of distress.
Behavioral Context: Observing erratic movements alongside heart rate data can help caregivers interpret the situation more accurately, allowing for tailored interventions.
In practice, devices that track both heart rate and movement (like smartwatches or fitness trackers) can be useful tools for monitoring agitation in real-time, especially for individuals with conditions such as dementia.
Wearable Biosensors: An Alternative and Practical Approach in Healthcare and Disease Monitoring - PMC (nih.gov)
Would using a sensory Therapy device with the monitor inside work?
Sensory therapy is a helpful way to calm and soothe without using medication. It’s an effective way to reduce anxiety, calm nerves, and provide comfort.
what are the best materials to use?? fur?
Nonpharmacological tactile activity interventions for reducing behavioural and psychological symptoms of dementia in the acute hospital setting: An integrative review - Davis - 2023 - Journal of Clinical Nursing - Wiley Online Library
Most effective - Pharmocological interventions.
There is limited evidence exploring tactile activity interventions for reducing behavioural and psychological symptoms of dementia in acute hospital settings. Individualised approaches in combination with staffing expertise appear central to implementation.
Best Textiles to use ?
5 Textile Considerations When Designing For Dementia - Materialised
The cognitive and sensory impairments people living with dementia may encounter can affect their experience of the world. This means that visual cues, surface texture and patterning are extremely important for signalling where they are, promoting independence and dignity.
One of these is clothing – finding comfortable, easy-to-wear garments that don’t exacerbate confusion or agitation can be a real pain point.
It’s important to choose soft, breathable material that won’t irritate their skin or cause discomfort.
Consideration should be given to contrast, Tactility, patterns, durability and colour.

Wearable Textiles may be more appropriate for dementia patients because they are less bulky.
Building a platform so a caregivers and families can have up to date information about the wellbeing of the patient.
There are some already available -
1. CareSmart
A platform that provides health tracking, medication reminders, and alerts for caregivers.
Lively
Offers wearable devices and a corresponding app that tracks health metrics and sends alerts to caregivers.
3. GrandCare
A comprehensive system that combines health monitoring, communication, and reminders for seniors and their caregivers.
4. Dementia Care App by CareConnect
Designed specifically for caregivers, it includes features for tracking daily activities, medication schedules, and mood tracking.
5. LifePod
An AI-powered voice assistant that offers reminders, alerts, and companionship while keeping caregivers informed.
6. Wellness Coach
A mobile app designed to help caregivers track and manage the health and wellbeing of dementia patients.
Can I change the application or look at modifying it?
These apps more focus on a broader range of services. Like a virtual health provider.
I am looking at a more focused interface just on a couple of modalities. Heart rate and movement.... ? noise activity?
Fully Integrated, Stretchable, Wireless Skin-Conformal Bioelectronics for Continuous Stress Monitoring in Daily Life
Current Evidence for Continuous Vital Signs Monitoring by Wearable Wireless Devices in Hospitalized Adults: Systematic Review - PMC (nih.gov)
it would be really difficult to actually play someone's favourite song as we may not know them or have any previous history. There are many similar devices out there but I want it specifically to be to the ED. The ED is noisy and the nurses are really task focused and can be very busy and chaotic. It would be better for the device to display lights on an interface or a set of lights or something.
There are alot of wearable devices but not really sure that it would work in the ED due to infection control and the idea of it being disposable or how we would manage that.
Exploring the ideas of washable materials or disposable materials
How to monitor pulse rate:
Living electrodes based on green algae in hydrogels
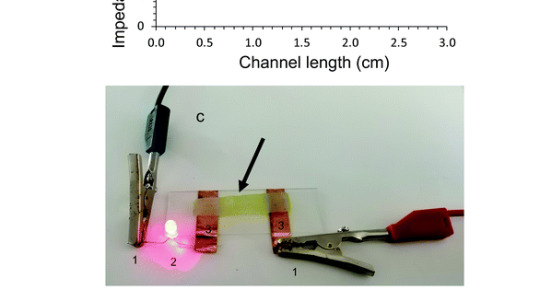
May in the future to be able to use seaweed gel to conduct a circuit - reading the biometric data.
Dorset: AI socks trial could help people with dementia and autism (bbc.com)
these socks are machine washable and detect temp, movement, heart rate and sweat. Then sends the data to AI to interpret and alert carers that the person is escalating.
The machine washable socks are paired with an app, installed on a smartphone.
A sensor embedded in one of the socks collects data from the foot and the ankle of the wearer which is sent to the AI, which estimates whether the person is distressed.
The care team would then be alerted through the app.
Dr Zeke Steer, Milbotix founder, was inspired to make the product after his grandmother began to show signs of early onset dementia.
He said partnering with the council meant the company could "hear the expert voices of people providing and receiving care".
"We are committed to building a product that genuinely help carers and improves wearers' overall wellbeing," he added.

Design Concept 1 Agitation wrist band/arm strap that played music to calm the patient.
Agitation is a common problem in the Emergency Department with high stimulus for a dementia patient. The idea was to identify agitation early and use music therapy to assist with reduction in stressors.
Pros - reduction in stress and agitation. Calmer patient. Reduction in the risks of developing delirium, reduced hospital time and reduction in Medication managment.
Cons - Unaware of patients favourite songs. Would need to consider hearing impairment and disruption to other patients. Need device or sound system linked in to facilitate.
Design Concept 2
Wearable clothing that detected agitation early but was attached to an interface that could alert Nurses in the ED that the patient was getting agitated. Similar to cardiac monitoring.
Pro- Displays on stationary computer continuous monitoring interface so that the nurse could see whilst monitoring cardiac output.
Cons - The clothing may be removed. The nurse isn't always monitoring the stationary computer. So potentially elevations would be missed. Not all patients are accepting of clothing or items unless they are familiar in advanced dementia/alzheimers.
Design Concept 3
Wearable clothing that detected agitation early but was attached to a light or alert system that could alert Nurses in the ED that the patient was getting agitated. through a bright visual cue outside the patients room
Pro - easy visual cue for the nurses to establish who was escalating and provide some intervention.
Con - the wearable clothing may still be an issue....
Maybe a biopatch could be attached to the patient on their back instead so as to not agitate or aggravate them as it may not be felt. ??
In the future seaweed gel could be used as a conductor to create electronic components in wearable design instead of metal.

Process
Code to play music if the motion and heart rate exceed the threshold

couldn't get the sats prob pulse monitor to work but did have the microbit. Just keeps playing music because the heart rate monitor is not attached.
now going to change it so it lights up instead...
but there are already socks on the market that can be reappropriated - will try and recreate those and then attach it to the interface.

Another code tried where both the movement and the heartrate were visible. The movement needs to be adjusted to mimic normal body movements and then what would be outside that.
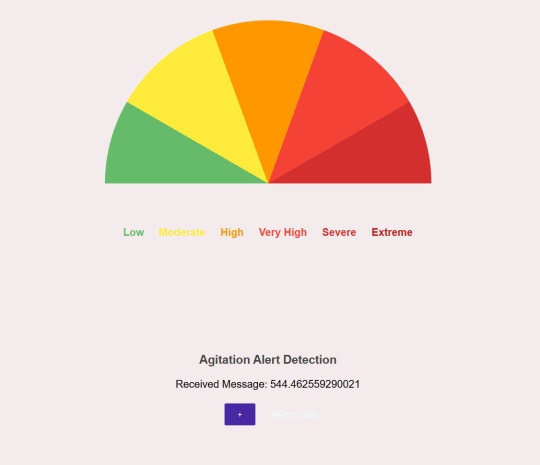
Microbit Blue tooth - Agitation Detector.
Where to place the device
Hands - pull them off or pick at them, Arms - same issues. So placing the microbit in a pair of socks would have been a great iteration and in the future may work however through the process have found that there are too many contributing factors that would actually hinder the data.
Including peripheral vascular diseases therefore limiting blood flow to the peripheral areas.
Another issue I found was the use of medication to control blood pressure and heart rate could also impede the signals putting into a pair of Socks.
In the future a wearable patch would be ideal but for the moment still a work in progress.
Initially I was looking at the best method for detecting agitation is movement and heart rate. However detecting irregular or irractic moving in a mobile patient would be extremely difficult and could be only applied to a select cohort of patients particularly those who are non ambulatory. This being the case for the purpose of task 3 I have pivoted slightly and am just going to use heart rate to indicate the changes in agigation. An acceleromotor also is not that affective unless it is used in conjunction with another piece of biometric data. Heart rate is the most responsive and will give a good indicator of agitation.
Connecting the microbit and have the styling responsive to the mobile phone/computer interface.
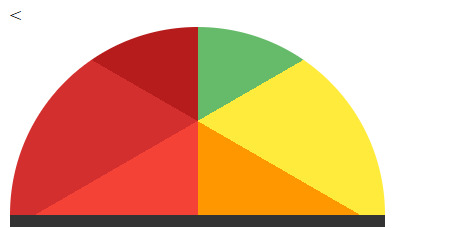
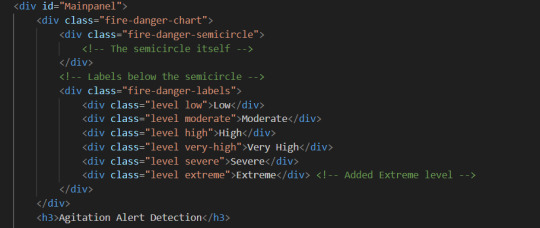
Every time I tried to create the semi circle and changed the background conic gradient in the CSS Styling I woul put the starting point of the wedges in the middle of the semicircle or it would turn it upside down.
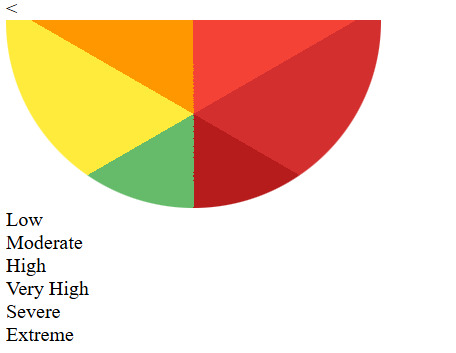
I had to change it multiple times to try and figure out how to get the gradient responding or looking the way I wanted them to look. I was definately trial and error. Eventually I was able to use the code below to visually represent the alert levels. I was many hours of trial and error to establish the right code. It was really difficult to achieve as the way I wanted it set up the coding wasn't the way you would normally do it so made it so complicated to actually achieve the results.

However I am still having difficulty converting the raw data even though I have added the parse int......
it just doesn't want to work.... But on the plus l have been able to blue tooth to my computer making it much easier to work with the interface. '
Have been using a similar code but would not work on the interface as it won't change the data or parse it properly to activate the agitation levels.

I am going to try this one and see if I am able to get it to work based on the raw and smoothed pulse rate data.
Unfortunately I lost both access to the computer and the raw data was still not being read correctly and with this code I lost the simulator as nil serial write code commands were in there. I recompleted the code.
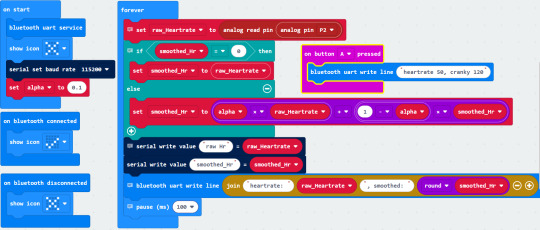
I was able to see the heart rate via the pulse monitor. But wasn't able to convert the heart rate to respond to the interface correctly. It wouldn't work and certainly wouldn't respond to the interface how I wanted it too.
So I just used simulated data to start with so I could get the corresponding styling to work appropriately on the interface.
Concept :
I wanted the heart rate to be visually represented on the interface by highlighting the wedge of the corresponding colour.
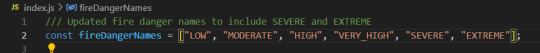
Really difficult to achieve to begin with. So I started with just having the different levels and the heading illuminate proving much harder than intended as I was trying to place the headings on the curve of the semicircle.
The names eneded up skewed and in all different positions. So I settled for placing the corresponding name under the different colours. I was able to get these to highlight easily enough and respond to the heart rate.
I added the flashing alert so as nursing staff could identify if the heart rate was at extreme and each of the levels now are visual corresponding the the heart rate.

As documented you can see that the heart rate is moderate . I may have to change the names as it is supposed to be an agitation detector....... This seems a little catastrophic when it is supposed to be referring to an agitation level.

Flashing - for severe agitation.
I was able to get the styling working based on the simulated heart rate.
However it meant that the wearable device would effectively not have worked.
After some debugging it was found that the incoming message from the microbit was too long and therefore crashing out the system.
Changing the microbit code allowed the smoothed heartrate only to come through and there was also an issues with the javascript that has also been fixed.
The new code for the microbit.
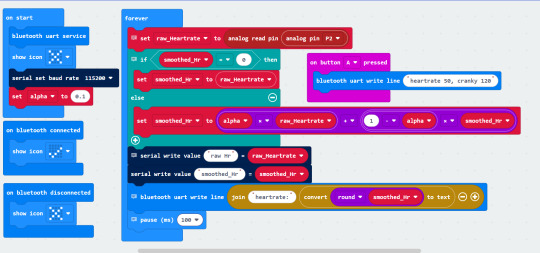
The heartrate is now displaying and am able to connect to the bluetooth on the computer.
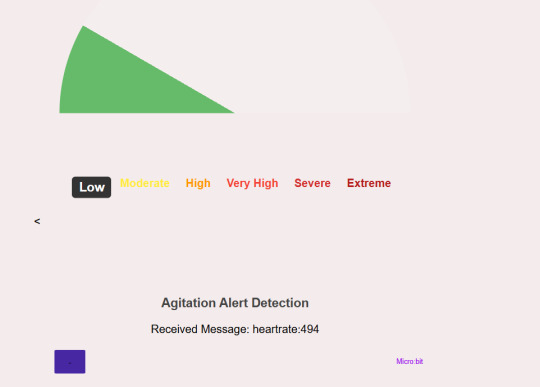
I have just realised the the very high visual doesn't actually high light the word very high?
Not sure what is happening there.
checked the CSS -

All the levels are identified there.
Will check the java :
Seems to be nominated there too!!
Will now check the html :
In each section it appears to be mentioned so I am not sure why that level is not being highlighted.
After a little bit of research I changed a few things -
HTML -
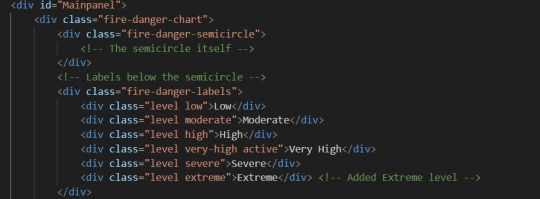
just made the level - very-high active
CSS -
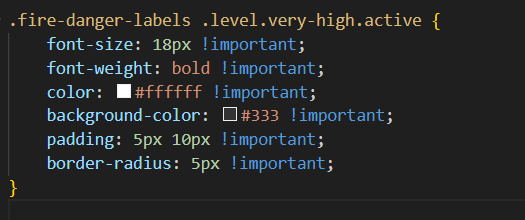
I initially tried out this to see if I could get it too work. Still not happening - Then checked the developer tools and it says :
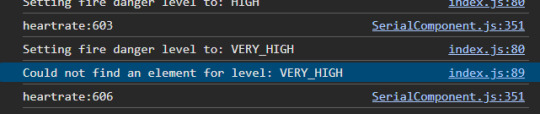
just went through all the code and found :
That in this part of the code it doesn't match to the rest of the description of very high due to the underscore between the words as all the other descriptions are very-high.
I went ahead and changed the code.

The problem is fixed. It is all now working as initially intended in the concept.
But I think it would be better to change the names of the levels - to be more indicative of escalating behaviour rather than catastrophise it all and be a cause of concern to patients, nurses and doctors in the department.
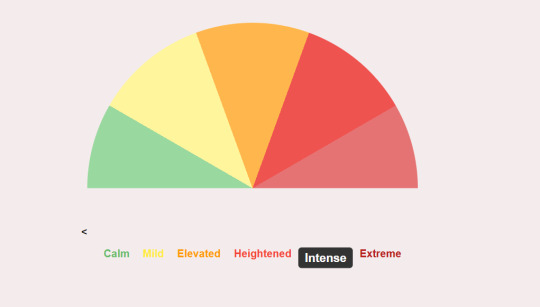
Updated the code...... the names look better.
Wearable Device
With changing from the socks I had to come up with another idea the would both be able to house the microbit, battery pack and pulse sensor. Research suggest that tactile/sensory items can have a positive effect on a patient with dementia. So I have decided to house the microbit in a material called tubi - grip common to ED in like a wrist guard fashion and add some sensory elements so the patients can fiddle with those instead.
0 notes
Text
Lewy Body Dementia: An Under-Diagnosed Yet Debilitating Form Of Dementia

Lewy Body Dementia (LBD) is the second most common type of progressive dementia after Alzheimer's disease. It occurs due to the abnormal accumulation of a protein called alpha-synuclein in the brain, which forms structures known as Lewy bodies. The presence of Lewy bodies interferes with neurotransmitter function in the brain leading to a decline in cognitive abilities along with movement and behavioral issues.
Symptoms Of LBD
The symptoms of Lewy Body Dementia can vary but commonly include problems with thinking, reasoning, and independent function. Memory loss is less prominent compared to Alzheimer's but other cognitive abilities like visualization and attentiveness are significantly impacted. Behavioral and psychological symptoms like delusions, hallucinations and paranoia are also very common. Movement symptoms mirroring Parkinson's disease like rigidity, tremors and slowed movement are seen.
Diagnosis And Diagnostic Challenges
Diagnosing Lewy Body Dementia can be challenging as the symptoms overlap with Alzheimer's and Parkinson's diseases. Brain imaging and spinal fluid tests cannot definitively diagnose LBD as Lewy bodies can only be detected by autopsy. Doctors consider medical history and evaluate symptoms to make a diagnosis based on established clinical criteria. The diagnosis is often made incorrectly or delayed as symptoms fluctuate and physicians are not well-versed with LBD.
Impact On Individuals And Caregivers
Due to a range of cognitive, behavioral and movement difficulties, individuals with LBD experience a steady decline in independence requiring progressively more assistance. Dealing with hallucinations and delusions especially impacts the quality of life. Caregivers face tremendous stress managing unpredictable behaviors and providing round-the-clock care. The demands of care often lead to increased emotional distress, worsening health and financial issues for caregivers.
Disease Progression And Management Challenges
In later stages, individuals exhibit very severe symptoms including an inability to communicate and respond. Managing symptoms like hallucinations and paranoia remains difficult even with medications which show limited effectiveness and cause undesirable side effects in this population. Non-motor and behavioral symptoms seem to progress independent of cognitive symptoms posing further clinical management challenges. Palliative care and advanced care planning are important aspects of care that are often not prioritized in a timely manner.
Need For Increased Awareness And Support
Lewy Body Dementia is still under-recognized and faces neglect in funding and research compared to other dementias. Increasing awareness about its clinical features and impact among physicians and general public is crucial. Caregivers also need education and support through dedicated community-based resources to manage the physical, psychological and financial burden of caring for LBD individuals. Further research is warranted to establish a definitive diagnosis, explore disease mechanisms and develop safe and effective treatment options. Concerted efforts are essential to address the needs of the growing number of individuals and families suffering from this little known yet debilitating form of dementia.
Lewy Body Dementia needs to be more widely recognized as a major contributor to the global dementia burden by the healthcare systems and policymakers. Improving diagnosis rates, managing symptoms better, supporting caregivers and expediting research hold the key for enhancing quality of life of individuals living with LBD and alleviating their caregivers' challenges.
Get more insights on this topic: https://www.ukwebwire.com/understanding-lewy-body-dementia/
About Author:
Priya Pandey is a dynamic and passionate editor with over three years of expertise in content editing and proofreading. Holding a bachelor's degree in biotechnology, Priya has a knack for making the content engaging. Her diverse portfolio includes editing documents across different industries, including food and beverages, information and technology, healthcare, chemical and materials, etc. Priya's meticulous attention to detail and commitment to excellence make her an invaluable asset in the world of content creation and refinement. (LinkedIn - https://www.linkedin.com/in/priya-pandey-8417a8173/)
*Note: 1. Source: Coherent Market Insights, Public sources, Desk research 2. We have leveraged AI tools to mine information and compile it
0 notes
Text
Dementia Treatment In Singapore
Dementia treatment in Singapore involves a comprehensive approach designed to manage symptoms, improve quality of life, and provide support for both patients and their families. Given the increasing prevalence of dementia, the country has developed a range of services and strategies to address this complex condition effectively.
Multidisciplinary Care
In Singapore, dementia treatment typically involves a multidisciplinary team of healthcare professionals. This team may include neurologists, geriatricians, psychiatrists, psychologists, and occupational therapists. Each specialist contributes their expertise to provide a holistic approach to managing dementia. This collaborative effort ensures that all aspects of the patient’s condition are addressed, from medical management and cognitive support to psychological and social needs.
Medical Management
Medical management of dementia in Singapore focuses on slowing disease progression and alleviating symptoms. Physicians may prescribe medications that help manage cognitive symptoms, such as memory loss and confusion, or address behavioral issues like agitation and depression. Regular follow-ups and adjustments to medication are crucial to optimizing treatment effectiveness and minimizing side effects. Additionally, ongoing research and clinical trials in Singapore offer access to emerging therapies and innovative treatments.
Cognitive and Behavioral Therapies
Cognitive and behavioral therapies play a significant role in dementia care. Cognitive stimulation therapy, for instance, involves structured activities designed to engage and stimulate cognitive function. These activities help patients maintain their abilities for as long as possible and enhance their quality of life. Behavioral therapies address challenging behaviors, providing strategies to manage issues such as aggression or wandering, and improve overall well-being.
Support Services
Support services are integral to dementia care in Singapore. These services include caregiver support programs, counseling, and educational resources to assist families and caregivers in understanding and managing the condition. Caregiver training and support groups provide essential guidance and emotional support, helping families cope with the challenges of caregiving and reducing caregiver stress.
Daycare and Residential Facilities
For patients requiring more comprehensive care, Singapore offers various daycare and residential facilities tailored to dementia care. Daycare centers provide structured activities and supervision during the day, allowing patients to remain in their homes while receiving support. Residential care facilities, including nursing homes and specialized dementia units, offer 24-hour care in a supportive environment. These facilities are designed to cater to the unique needs of individuals with dementia, providing safety, medical care, and social engagement.
Community and Home-Based Services
Community-based and home-based services are essential components of dementia care in Singapore. Home care services, including visiting nurses and personal care assistants, support patients who wish to remain at home while receiving professional care. Community programs, such as memory clinics and support groups, offer additional resources and assistance, helping patients and families navigate the challenges of dementia.
Dementia treatment in Singapore encompasses a multifaceted approach involving medical management, cognitive and behavioral therapies, and extensive support services. The country’s commitment to providing comprehensive care through multidisciplinary teams, specialized facilities, and community-based resources ensures that patients with dementia receive effective treatment and support. This holistic approach not only aims to manage the condition but also enhances the overall quality of life for both patients and their families.
0 notes
Text
Alzheimer’s Care in Sugar Land, TX: Supporting Families and Providing Compassionate Care
Caring for a loved one with Alzheimer’s disease can be an overwhelming journey, filled with emotional challenges and complex care needs. In Sugar Land, Texas, specialized Alzheimer’s care services are making a profound difference in the lives of families, offering compassionate support and expert care tailored to the unique demands of this progressive disease. This blog delves into the importance of Alzheimer’s care in Sugar Land, the types of services available, and how these services benefit both individuals with Alzheimer’s and their caregivers.
The Importance of Specialized Alzheimer’s Care
Alzheimer’s disease is a form of dementia that affects memory, thinking, and behavior, progressively worsening over time. It requires specialized care from trained professionals who understand the complexities of the disease and can provide the appropriate support. In Sugar Land, Alzheimer’s care services are designed to address these needs, ensuring that individuals with Alzheimer’s receive the best possible care while maintaining their dignity and quality of life.
Specialized care is vital for several reasons:
Safety: Alzheimer’s can lead to disorientation and confusion, making safety a significant concern. Alzheimer’s care services prioritize creating a safe environment, reducing the risk of wandering, falls, and other potential hazards.
Expert Care: Caregivers trained in Alzheimer’s care are equipped to handle the behavioral and psychological symptoms of the disease, such as agitation, anxiety, and depression. They provide support that is both compassionate and informed by the latest research and best practices in dementia care.
Tailored Support: Alzheimer’s affects each person differently, so care needs to be personalized. Professional caregivers assess the unique needs of each individual, providing care that is responsive to their cognitive and physical health.
Types of Alzheimer’s Care Services in Sugar Land
Sugar Land offers a range of Alzheimer’s care services, allowing families to choose the option that best suits their loved one’s needs. These services include:
In-Home Care: Many families prefer to keep their loved ones at home, surrounded by familiar faces and environments. In-home Alzheimer’s care provides professional caregivers who come to the home, offering assistance with daily activities, medication management, and companionship. This allows individuals with Alzheimer’s to remain in the comfort of their own home while receiving the necessary care.
Residential Memory Care Facilities: For those who require more intensive care or whose families cannot provide care at home, memory care facilities offer a structured environment specifically designed for individuals with Alzheimer’s and other forms of dementia. These facilities provide 24/7 care, specialized activities, and a secure environment to ensure safety and comfort.
Respite Care: Family caregivers often need time to rest and recharge. Respite care offers temporary relief by providing professional care for their loved ones, either at home or in a memory care facility, allowing caregivers to take a break while ensuring their loved one is in good hands.
Day Programs: Alzheimer’s day programs provide a safe, supportive environment during the day, offering structured activities, social interaction, and medical oversight. These programs allow caregivers to work or attend to other responsibilities while ensuring their loved one receives the care they need.
Conclusion
Alzheimer’s care in Sugar Land, TX, plays a crucial role in supporting individuals with Alzheimer’s and their families. By providing expert care, safe environments, and emotional support, these services help manage the challenges of Alzheimer’s while enhancing the quality of life for those affected by the disease.
0 notes
Text
Dementia Treatment by Psychiatrists in Delhi
Dementia, a progressive neurological condition affecting memory, thinking, and behavior, has become a growing concern in Delhi, India, and around the world. As the population ages, the prevalence of dementia continues to rise, making it crucial to explore the approaches taken by psychiatrists in Delhi for its treatment. In this article, we will delve into the treatment of dementia by psychiatrists in Delhi, shedding light on the challenges they face and the innovative strategies they employ.
Understanding Dementia
Dementia is a complex condition that encompasses various disorders, with Alzheimer's disease being the most common. Other forms of dementia include vascular dementia, Lewy body dementia, and frontotemporal dementia. Regardless of the type, dementia's hallmark is a decline in cognitive function, often accompanied by behavioral changes, that impairs a person's ability to perform daily activities.
The Role of Psychiatrists
Psychiatrists in Delhi play a crucial role in the diagnosis and treatment of dementia. They are specialized medical doctors who focus on mental health, making them well-equipped to address the cognitive and emotional aspects of dementia. When dealing with dementia, psychiatrists aim to provide holistic care, taking into account not only the medical aspects but also the emotional and psychological well-being of both patients and their caregivers.
Diagnosis and Assessment
The journey of dementia treatment typically begins with an accurate diagnosis. Psychiatrists in Delhi employ a variety of diagnostic tools, including cognitive assessments, brain imaging, and medical history analysis. These assessments help determine the type and stage of dementia, which is crucial for tailoring treatment plans to the individual's needs.
Medical Interventions
While there is currently no cure for dementia, there are medications that can help manage symptoms and slow down its progression. Psychiatrists in Delhi may prescribe drugs such as cholinesterase inhibitors or memantine to improve cognitive function and alleviate some of the behavioral symptoms associated with dementia. These medications are carefully monitored and adjusted as needed to ensure optimal results.
Psychosocial Support
In addition to medication, psychiatrists in Delhi place a strong emphasis on providing psychosocial support to individuals with dementia and their families. This support can take the form of counseling, support groups, and education about the condition. Such interventions are essential in helping patients and caregivers navigate the emotional and practical challenges that dementia presents.
Behavioral Interventions
Dementia often brings about behavioral changes that can be challenging for both patients and their loved ones. Psychiatrists in Delhi work closely with their patients and caregivers to develop behavioral interventions aimed at managing these symptoms. This may involve strategies to address agitation, aggression, or wandering, among other behavioral issues.
Occupational and Physical Therapy
Occupational and physical therapists are integral members of the dementia treatment team. Psychiatrists in Delhi often collaborate with these professionals to help individuals with dementia maintain their independence for as long as possible. Occupational therapy focuses on daily living skills, while physical therapy aims to improve mobility and reduce the risk of falls.
Caregiver Support
Psychiatrists in Delhi recognize the importance of supporting caregivers and may refer them to support groups or offer counseling services to help them cope with the challenges they face. A well-supported caregiver can provide better care and improve the overall quality of life for the person with dementia.
Challenges in Dementia Treatment
While psychiatrists in Delhi are making significant strides in dementia treatment, they face several challenges in providing optimal care. One of the primary challenges is the stigma associated with dementia in many Indian communities. This stigma can lead to delays in seeking medical help and isolation for individuals with dementia and their families.
Another challenge is the lack of awareness and understanding of dementia among the general public. Psychiatrists often engage in community education and outreach efforts to combat this issue, but more needs to be done to raise awareness and reduce the misconceptions surrounding the condition.
Innovative Approaches
Psychiatrists in Delhi are continually seeking innovative approaches to enhance dementia treatment. One such approach is the integration of technology into care. Mobile applications and wearable devices can assist in monitoring patients' cognitive and physical health, allowing for early intervention and personalized care plans.
Additionally, research into novel therapies, including non-pharmacological interventions like music therapy and art therapy, is gaining momentum. These therapies have shown promise in improving the well-being and quality of life for individuals with dementia.
The treatment of dementia by psychiatrists in Delhi is a multifaceted endeavor that encompasses medical, psychosocial, and behavioral interventions. While challenges such as stigma and awareness persist, psychiatrists are dedicated to providing the best possible care for individuals with dementia and their families. With a commitment to innovation and a holistic approach to care, psychiatrists in Delhi are making significant strides in improving the lives of those affected by dementia. As the prevalence of dementia continues to rise, the efforts of these dedicated professionals are more crucial than ever in navigating the journey of dementia care.
0 notes
Text
If You Notice Signs of Alzheimer’s, Professional Elderly Care Services Can Help
Alzheimer’s disease is a challenging and emotional topic for many families, affecting millions across the United States. According to the Alzheimer’s Association, approximately 1 in 9 Americans aged 65 and older suffer from Alzheimer’s, with over one-third of individuals over the age of 85 affected. This devastating disease demands careful attention and care, particularly as its progression impacts daily life.

Understanding Alzheimer’s Disease and Its Impact
Alzheimer’s disease is a progressive neurodegenerative disorder that primarily affects memory and cognitive function. This disease is the most common cause of dementia among older adults. Alzheimer’s disease slowly destroys brain cells, leading to a decline in mental capabilities severe enough to interfere with daily life. Symptoms often start subtly and worsen over time, impacting memory, thinking, and behavior. The onset of Alzheimer’s usually necessitates additional care to ensure the safety and comfort of the affected individual. At Neighborly Home Care, we understand the profound impact Alzheimer’s has on both the patient and their families. Our compassionate and skilled caregivers are here to support you through this challenging journey.
How Alzheimer’s Disease Impacts Those Afflicted
Below are common symptoms that people suffering from Alzheimer’s Disease have to endure.
Memory Loss
One of the earliest and most noticeable symptoms of Alzheimer’s is memory loss, which can manifest as difficulty remembering names, common objects, or how to perform everyday tasks. Individuals may experience confusion and frustration, struggling to recall once-familiar information. This memory loss can also lead to disorientation about time and place, making navigating their surroundings difficult.
Cognitive Decline
As Alzheimer’s progresses, various cognitive functions, including reasoning, problem-solving, and decision-making are affected. Patients may have difficulty following conversations, completing familiar tasks, or understanding visual images and spatial relationships. This cognitive decline can significantly impact their independence and quality of life.
Behavioral and Psychological Changes
Individuals with Alzheimer’s may experience significant changes in their personality and behavior, including increased agitation, anxiety, depression, and mood swings. They may become easily upset, exhibit aggressive behavior, or withdraw from social activities. These changes can be distressing for both the patient and their caregivers.
Loss of Independence
As the disease advances, individuals with Alzheimer’s often require increasing levels of care and support. Basic activities such as dressing, bathing, and eating may become challenging. Eventually, many patients will need round-the-clock care to ensure their safety and well-being.
How Alzheimer’s Disease Impacts Loved Ones
Emotional Strain
Caring for a loved one who is suffering from Alzheimer’s is challenging emotionally. Watching a family member lose their memory and cognitive abilities can be heartbreaking. Caregivers often experience feelings of grief, frustration, and helplessness as they cope with the progressive nature of the disease.
Physical and Mental Health Challenges
The demands of caregiving can have a big impact on the physical and mental health of family members, and those caregivers often experience high levels of stress, fatigue, and burnout. Balancing caregiving responsibilities with work and other family commitments can be overwhelming.
Financial Impact
The cost of care for individuals with Alzheimer’s can be significant. Families may need to cover expenses for medical treatments, home modifications, and professional caregiving services. This added financial burden can add to the challenges and stress faced by caregivers.
Seeking Help and Support
If you notice signs of Alzheimer’s in a loved one, seeking medical advice is crucial for an accurate diagnosis. Early intervention can make a substantial difference in managing the disease and planning appropriate care strategies. Once diagnosed, consider the benefits of professional elderly care services.
Neighborly Home Care is Your Partner in Alzheimer’s Disease Care
Neighborly Home Care offers specialized in-home care services for individuals with Alzheimer’s. Our in-home caregivers are experienced in managing the unique challenges posed by the disease. By providing personalized care plans, we ensure that your loved one receives the attention and support they need to maintain their quality of life.
Caring for a family member with Alzheimer’s can be overwhelming. Our services provide expert care for your loved one and respite for family caregivers. Neighborly Home Care is dedicated to making this journey as smooth as possible.
Contact Neighborly Home Care Today
Neighborly Home Care is a trusted provider of in-home care services for seniors in Pennsylvania and Delaware. Our caregivers are compassionate and dedicated to the exceptional care of seniors with dementia. For more information on Alzheimer’s disease and your care options, please contact Neighborly Home Care. We are here to help you and your loved ones navigate life with this disease.
Blog is originally published at: https://www.neighborlyhomecare.com/if-you-notice-signs-of-alzheimers-professional-elderly-care-services-can-help/
It is republished with the permission from the author.
#Professional Elderly Care Services#in-home care services#elderly care#senior care#dementia#alzheimers
0 notes
Text

Review of The Hacking of the American Mind by Robert H. Lustig MD, MSL
Did you just get the urge for chocolate and pick up a couple of bars or maybe a cake on the way home? Do you consider yourself a chocoholic at times and laugh it off? Are you constantly on your cell phone or social media? What if these cravings for cookies, cell phones, social media, etc that have become endemic to the American culture aren't simply innocent habits but the results of years of biochemical engineering by Big Business to get people hooked? As we pursue the happiness these addictions offer they are damaging not just our minds, but our relationships, and society as a whole according to the author, pediatric endocrinologist, and professor Dr. Robert Lustig in his book The Hacking of the American Mind: The Science Behind the Corporate Takeover of Our Bodies and Brains. Lustig argues that we have been "hacked" by certain industries that intentionally "obfuscate the link between their products and disease, and to willfully confuse the concepts of pleasure and happiness with the sole motive being profit" (Lustig p 6). He supports his argument with information by delving into various areas including biochemistry, neuroscience, psychiatry, economics, etc. The past forty years of increased addiction and depression are the result of too much pleasure and not enough happiness.
The title of this book caught my attention on the library bookshelf, not having read anything by Lustig previously, but ever the student of mental and physical well-being how this can contradict the practices of our modern society. I'd first thought he might be another "expert" medical professional trying to pass his theories off as reality or serve up another dose of positive psychology, however, as an endocrinologist, Lustig does ground his argument in the underlying science of biochemistry something I found reassuring from the start of the book. "the biochemistry drives the behavior" (Lustig 27) and it is clear this is where he is comfortable as the second and third parts of the book deal exclusively with explaining the chemistry of the dopamine reward pathway and the serotonin contentment pathway. This doesn't leave much room in the book to discuss other areas such as economics and philosophy, which I would have liked to learn more about, but it did make for an engaging read.
Also, Dr. Lustig focuses on hormones in children and his previous book Fat Chance deals with obesity and metabolic syndrome in our society. I have yet to read Fat Chance, but it is apparent that this book also borrows heavily from that research as, although he touches on phones and gambling, sugar seems to be the main villain. Where sugar was a luxury at one time, it is now cheap, easy to procure, and highly addictive. Our society has become stressed and sleep-deprived leading to mental health issues like depression and addiction to processed foods loaded with sugar leading to symptoms of metabolic syndrome: weight gain, cancers, heart disease, diabetes, etc. I'm familiar with the link between sugar and metabolic syndrome, but he also argues for a link between sugar and dementia and Alzheimer's disease. This proves to be more of a correlation than a causation, but it did raise serious concerns for me. After all the medical field had claimed for a long time to not know the underlying causes of Alzheimer's. I recall during the diet fads of the past when fats were labeled the main culprit sugar was put in its place.
There are a few points where I notice when discussing politics, Lustig seems a little out of touch on the healthcare policies of the time he was writing apparently during Donald Trump's presidency claiming at one point that the Affordable Care Act had been repealed and that Trumpcare was on the way.
I appreciate how the author provides suggestions in the last part of the book to win the battle against big business, especially the food industry defined by the four c's: connection, contribute, cope, and cook. Lusting advises that we should connect with our fellow human beings in person and not just online, volunteer for a cause, cope by getting sleep and practicing mindfulness, and cook for ourselves and our family. I have seen different versions of these suggestions in other books and articles and I currently been practicing them myself and have seen great improvement in my life.
I recommend this book to those interested in learning about the biochemistry that underlies our behavior and the serious effects sugar can have on our health. I think sugar's role in keeping us eating poorly and dealing with health effects is the strongest part of The Hacking of the American Mind: The Science Behind the Corporate Takeover of Our Bodies and Brains. I agree with Lustig that the way we live needs to change and changing our diets is the main key. I can speak from experience as I have reduced sugar significantly in my diet with very positive results.
0 notes
Text
Understanding Dementia: Treatments, Care Facilities, and Advanced Approaches
Dementia is a complex and progressive condition affecting millions worldwide. This disorder leads to a decline in cognitive function, impairing memory, thinking, and the ability to perform everyday activities. In this blog, we will explore various aspects of dementia, including dementia treatment in Bangalore, the best psychiatrist in Kolkata, dementia care facilities, cognitive therapy for dementia, and advanced dementia treatment. Dr. Samyuktha, a renowned psychiatrist, will guide us through these topics.
What is Dementia?
Dementia is not a single disease but an umbrella term for several conditions characterized by cognitive decline. The most common types include Alzheimer's disease, vascular dementia, Lewy body dementia, and frontotemporal dementia. Early signs often include memory loss, difficulty concentrating, and changes in mood and behavior. Understanding these early signs is crucial for timely intervention and management.
Alzheimer's disease is the most prevalent form of dementia, accounting for 60-80% of cases. It primarily affects older adults and is characterized by the accumulation of amyloid plaques and tau tangles in the brain. Vascular dementia, the second most common type, results from reduced blood flow to the brain, often due to strokes or other vascular conditions. Lewy body dementia involves abnormal deposits of alpha-synuclein protein in the brain, leading to symptoms such as visual hallucinations and Parkinsonism. Frontotemporal dementia affects the frontal and temporal lobes, leading to changes in personality, behavior, and language.
Dementia Treatment in Bangalore
When it comes to dementia treatment in Bangalore, patients have access to a range of advanced medical facilities and specialized care. Treatment often involves a combination of medications, lifestyle changes, and supportive therapies. Medications such as cholinesterase inhibitors (donepezil, rivastigmine, galantamine) and memantine can help manage symptoms, although they cannot cure the disease. These medications work by regulating neurotransmitters, which are chemicals that transmit signals in the brain.

Lifestyle interventions are equally important in managing dementia. Physical activity, such as walking, swimming, or yoga, helps improve cardiovascular health and may delay cognitive decline. A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats supports overall brain health. Mental exercises like puzzles, reading, and learning new skills stimulate cognitive function. Additionally, social engagement and participating in group activities can help maintain mental well-being and reduce the risk of depression and anxiety.
Supportive therapies, including occupational therapy, can assist patients in maintaining their independence and performing daily activities. Speech therapy may be beneficial for those experiencing language difficulties. Music and art therapy can also provide emotional and cognitive benefits, enhancing the quality of life for individuals with dementia.
The Role of the Best Psychiatrist in Kolkata
For those seeking expert advice and treatment, consulting the best psychiatrist in Kolkata can make a significant difference. Dr. Samyuktha, a leading psychiatrist, emphasizes the importance of early diagnosis and personalized treatment plans. Her approach includes a thorough assessment of the patient's medical history, cognitive abilities, and psychological state to tailor a comprehensive treatment strategy.
Early diagnosis is crucial for effective management of dementia. It allows for timely intervention, which can slow the progression of the disease and improve the patient's quality of life. Dr. Samyuktha employs various diagnostic tools, including cognitive tests, brain imaging (MRI or CT scans), and blood tests to rule out other conditions that may mimic dementia symptoms.
Once a diagnosis is made, Dr. Samyuktha develops a personalized treatment plan that addresses the patient's specific needs. This plan may include medication management, lifestyle modifications, and supportive therapies. Regular follow-up appointments are essential to monitor the patient's progress and make necessary adjustments to the treatment plan.
Dementia Care Facilities
Dementia care facilities play a crucial role in providing specialized care and support for individuals with dementia. These facilities are designed to offer a safe and stimulating environment, with trained staff who understand the unique needs of dementia patients. Services typically include round-the-clock care, medical supervision, and various therapeutic activities aimed at enhancing quality of life.
Choosing the right dementia care facility is essential for ensuring the well-being of the patient. Factors to consider include the facility's location, staff-to-patient ratio, available medical services, and the types of activities and therapies offered. Facilities that provide personalized care plans, regular medical check-ups, and opportunities for social engagement are highly recommended.
Therapeutic activities in dementia care facilities may include physical exercise programs, cognitive stimulation activities, music and art therapy, and sensory stimulation. These activities help maintain cognitive function, improve mood, and promote social interaction. Support groups for families of dementia patients can also be beneficial, providing emotional support and practical advice on caregiving.
Cognitive Therapy for Dementia
Cognitive therapy for dementia is an essential component of managing the condition. This therapeutic approach involves structured activities and exercises that stimulate cognitive functions, such as memory, problem-solving, and attention. Cognitive therapy can slow the progression of dementia and improve the overall functioning and well-being of patients.
Cognitive therapy programs are often tailored to the individual's cognitive abilities and interests. Techniques used in cognitive therapy include reality orientation, cognitive stimulation therapy (CST), and reminiscence therapy. Reality orientation involves helping patients stay oriented to time, place, and person through the use of calendars, clocks, and structured routines. CST involves engaging patients in group activities that promote cognitive and social interaction. Reminiscence therapy encourages patients to recall and discuss past experiences, which can improve mood and cognitive function.
Additionally, assistive technologies, such as memory aids, digital reminders, and cognitive training software, can support cognitive therapy efforts. These tools help patients manage daily tasks and maintain their independence for as long as possible.
Advanced Dementia Treatment
Advanced dementia treatment involves the use of cutting-edge technologies and innovative therapies to address the complex needs of dementia patients. Techniques such as transcranial magnetic stimulation (TMS), deep brain stimulation (DBS), and stem cell therapy are being explored for their potential to improve cognitive function and delay disease progression. Dr. Samyuktha is at the forefront of these advancements, offering her patients access to the latest treatments and clinical trials.
TMS is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. It has shown promise in improving cognitive function and reducing symptoms of depression in dementia patients. DBS involves the surgical implantation of electrodes in specific brain regions, which are then stimulated with electrical impulses. This technique is primarily used for movement disorders like Parkinson's disease but is being researched for its potential benefits in dementia.
Stem cell therapy is an emerging field that involves the use of stem cells to regenerate damaged brain tissue. While still in the experimental stage, early studies suggest that stem cell therapy may hold promise for treating neurodegenerative diseases like dementia.
Conclusion
Dementia is a challenging condition, but with the right support and treatment, individuals can maintain a good quality of life. For those in Bangalore, advanced treatment options are available, and in Kolkata, the expertise of the best psychiatrists like Dr. Samyuktha can provide invaluable guidance. Dementia care facilities and cognitive therapy play vital roles in managing the condition, and ongoing advancements in treatment offer hope for better outcomes. If you or a loved one is experiencing symptoms of dementia, seek professional help to explore the best treatment options and ensure a supportive and compassionate care environment. With early diagnosis, personalized treatment plans, and access to advanced therapies, individuals with dementia can lead fulfilling lives and maintain their dignity and independence.
0 notes