#Amiodarone
Explore tagged Tumblr posts
Link
The Benefits and Risks of Pacerone: A Comprehensive Guide In the world of cardiology and the treatment of heart rhythm disorders, Pacerone, known by its generic name Amiodarone, shines as a vital medication. But what exactly is Pacerone, and how does it impact the cardiovascular health of those who rely on it? In this comprehensive guide, we'll delve into the nuances of Pacerone, exploring its uses, mechanisms, and both the benefits and potential risks associated with its use. [caption id="attachment_60250" align="aligncenter" width="1280"] pacer one[/caption] What is Pacerone? Pacerone, also referred to as Amiodarone is a medication that plays a crucial role in the realm of cardiology. But beyond its name, what is Pacerone? How Does Pacerone Work? The magic of Pacerone lies in its mechanism of action within the human body. Understanding how this medication operates is key to appreciating its significance in managing heart rhythm disturbances. Medical Indications Pacerone is not just another medication; it's a powerful tool in the hands of healthcare providers, primarily used for specific medical conditions and heart rhythm disturbances. Understanding its medical indications is essential: Heart Arrhythmias: Pacerone is often prescribed to individuals with various types of arrhythmias (irregular heart rhythms). These may include atrial fibrillation, ventricular tachycardia, and atrial flutter. By stabilizing heart rhythms, Pacerone helps prevent potentially life-threatening complications. Life-Saving Potential: In some cases, Pacerone can be a life-saving medication, particularly for individuals with ventricular tachycardia or ventricular fibrillation, which can lead to sudden cardiac arrest. It can be administered in emergencies to restore a normal heart rhythm. Dosage and Administration Understanding how to take Pacerone is just as important as knowing why it's prescribed: Oral Medication: Pacerone is typically administered orally in the form of tablets or capsules. The dosage and frequency are determined by the individual's specific condition and response to treatment. With or Without Food: It's important to follow the instructions provided by your healthcare provider or pharmacist regarding whether to take Pacerone with or without food. These guidelines help optimize its absorption and effectiveness. Regular Monitoring: While on Pacerone, regular check-ups and electrocardiograms (ECGs) may be required to monitor the heart's response to the medication. This ensures that the prescribed dosage remains appropriate for the individual's needs. Potential Side Effects Like any medication, Pacerone comes with potential side effects that individuals should be aware of: Common Side Effects: These may include nausea, vomiting, and fatigue. Inform your healthcare provider if these side effects become bothersome. Serious Side Effects: While uncommon, Pacerone can lead to more serious side effects, such as lung problems, liver issues, thyroid dysfunction, and skin reactions. It's crucial to promptly report any unusual symptoms to your healthcare provider. Regular Check-ups: Routine check-ups and blood tests are often recommended while taking Pacerone to monitor potential side effects and adjust treatment as needed. Precautions and Warnings While Pacerone can be highly effective, it's important to approach its use with certain precautions and awareness: Thyroid Function: Pacerone can affect thyroid function, potentially leading to hypo or hyperthyroidism. Regular thyroid function tests and monitoring are crucial while on this medication. Lung Function: In some cases, Pacerone can cause lung problems, including pulmonary fibrosis. If you experience unexplained shortness of breath, cough, or chest discomfort, seek medical attention promptly. Liver Function: Monitoring liver function is essential while taking Pacerone, as it can lead to liver abnormalities. Inform your healthcare provider if you notice symptoms such as abdominal pain, jaundice, or dark urine. Interactions with Other Medications Understanding potential drug interactions is vital when taking Pacerone: Inform Your Healthcare Provider: Always inform your healthcare provider about all medications, supplements, and herbal products you are taking. Some medications can interact with Pacerone, affecting its effectiveness or increasing the risk of side effects. Medication Adjustments: Your healthcare provider may need to adjust the dosages of other medications you are taking to ensure their compatibility with Pacerone. Patient Experiences Real-life experiences can provide valuable insights into the impact of Pacerone: Amanda's Journey: Amanda, a heart arrhythmia patient, shares her journey with Pacerone. She discusses how the medication has helped her regain a sense of normalcy and the importance of close monitoring by her healthcare team. Managing Side Effects: Mark, a Pacerone user, reflects on his experience managing potential side effects. He highlights the significance of communication with his healthcare provider in finding the right balance between benefits and side effects. FAQs About Pacerone Q: What is Pacerone used for? A: Pacerone (Amiodarone) is primarily used to treat irregular heart rhythms, including atrial fibrillation and ventricular tachycardia. Q: How does Pacerone work to control heart rhythms? A: Pacerone works by affecting the electrical signals in the heart, helping to restore and maintain normal heart rhythms. Q: What are the common brand names for Amiodarone? A: Besides Pacerone, Amiodarone is also sold under brand names like Cordarone and Nexterone. Q: Are there any dietary restrictions while taking Pacerone? A: It's important to avoid grapefruit or grapefruit juice while on Pacerone, as it can interact with the medication. Q: Can Pacerone be taken with other medications? A: Pacerone can interact with various medications, so it's essential to inform your healthcare provider about all the medications and supplements you are taking. Q: What are the potential side effects of Pacerone? A: Common side effects include nausea, fatigue, and skin changes. Serious side effects may include lung or liver problems. Q: How long does it take for Pacerone to start working? A: Pacerone's effectiveness can vary from person to person, but it may take several days to weeks to see its full effect. Q: Can Pacerone be used during pregnancy or breastfeeding? A: Pacerone use during pregnancy and breastfeeding should be discussed with a healthcare provider, as it involves complex considerations. Q: Is it safe to drink alcohol while taking Pacerone? A: Alcohol can interact with Pacerone and should be consumed in moderation, if at all. Consult your healthcare provider for specific guidance. Q: What should I do if I miss a dose of Pacerone? A: If you miss a dose, take it as soon as you remember. However, if it's close to the time for your next dose, skip the missed one and continue with your regular schedule. Conclusion: In the world of cardiac health and the management of heart rhythm disorders, Pacerone, known as Amiodarone in its generic form, stands as a formidable ally. This comprehensive guide has taken you on a journey through the intricate details of this medication, offering insights into its uses, mechanisms, benefits, and potential risks.
#amiodarone#Amiodarone_hydrochloride#Antiarrhythmic_drug#Antiarrhythmic_medication#Cardiac_arrhythmia_medication#Cordarone#Heart_rhythm_control#Heart_rhythm_stabilizer#How_does_Pacerone_work#Nexterone#Pacerone_and_alcohol_consumption#Pacerone_and_grapefruit_interaction#Pacerone_dosage_instructions#Pacerone_uses#Side_effects_of_Amiodarone
0 notes
Text
Amiodarone Drug
Medical information for Amiodarone on Pediatric Oncall including Mechanism, Indication, Contraindications, Dosing, Adverse Effect, Interaction, Hepatic Dose.
#Amiodarone#medication#medications#medicine#drug#drugs#drug information#medical information#drug index#drug center#pediatric dose#Antiarryhthmics#amiodarone mechanism#amiodarone indication#amiodarone contraindications
0 notes
Text
The energy dose depends on whether the defibrillator is biphasic or monophasic. You should know how to operate the equipment used in your facility.
If using a biphasic defibrillator, follow the manufacturer’s recommendations for the initial dose (usually between 120 and 200 J). Subsequent doses should be the same as, or higher than, the initial dose. If the manufacturer’s recommendations for the initial dose are not known, use the highest energy dose available for the first and all subsequent shocks.
If using a monophasic defibrillator, set the energy dose at 360 J. Use this energy dose for each subsequent shock.
If defibrillation is initially successful in terminating the cardiac arrest rhythm but a shockable rhythm resumes, use the energy dose that successfully terminated the rhythm for subsequent shocks.
After 2 shocks have been delivered, epinephrine (1 mg IV/IO every 3 to 5 minutes) may be administered. The vasoconstrictive and positive ionotropic effects of epinephrine help to increase cerebral and coronary perfusion. Evidence suggests that epinephrine is most effective when administered early.
After three shocks have been delivered, consider administering an antiarrhythmic agent (amiodarone or lidocaine). The initial dose of amiodarone is 300 mg administered as an IV/IO bolus. If the arrest rhythm persists, consider giving a second dose of 150 mg as an IV/IO bolus 3 to 5 minutes later. Alternatively, lidocaine may be used if amiodarone is not available. The initial dose is 1 to 1.5 mg/kg IV/IO, followed by 0.5 to 0.75 mg/kg IV/IO every 5 to 10 minutes, up to a maximum dose of 3 mg/kg.
1 note
·
View note
Text
Diagnostic Pathways for Idiopathic Neuropathy
“You have a serious illness of an undisclosed nature” says a doctor to a patient in a cartoon within Dr. Norman Latov, MD, PhD’s recent presentation on idiopathic neuropathy sponsored by the Foundation for Peripheral Neuropathy. There are many cases where people present neuropathic symptoms, but the causes are unclear. The current diagnostic pathways Dr. Latov maps out are familiar and…
View On WordPress
#AIDP#alcohol#Amiodarone#B1#B12#B6#biopsy#Cancer#Celiac#Check POint Inhibitors#chemotherapy#CIDP#diabetes#Electrodiagnostics#GBS#Hepatitis C#HIV#hypothyroidism#Idiopathic Neuropathy#INH#kidney#Lead#Lyme Disease#MAG#mercury#MMN#muscle#nerve#Nerve Conduction Velocity#Norman Latov
1 note
·
View note
Photo
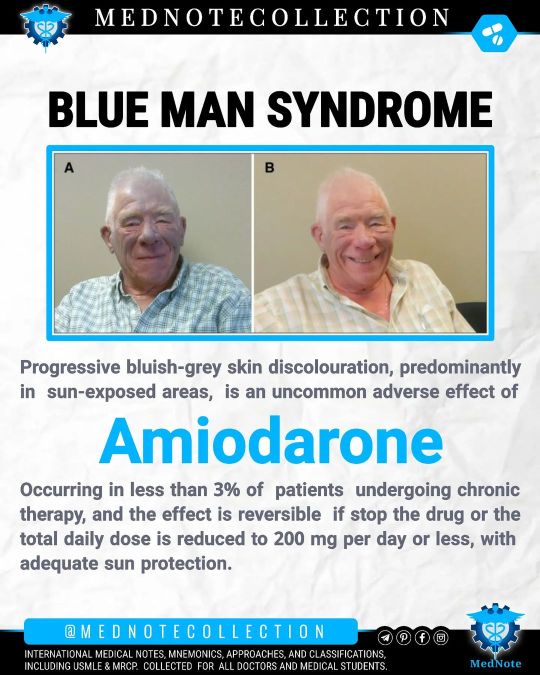
🧠 BLUE MAN SYNDROME MedNote Collection --------------------------------- instagram.com/mednotecollection t.me/MedNoteCollection pinterest.com/MedNoteCollection fb.me/MedNoteCollection --------------------------------- #medicine #medical_student #doctor #mednote_collection #MedNoteCollection #usmle #MRCP #pharmacology #amiodarone https://www.instagram.com/p/ConGiGMMKr3/?igshid=NGJjMDIxMWI=
#medicine#medical_student#doctor#mednote_collection#mednotecollection#usmle#mrcp#pharmacology#amiodarone
0 notes
Text
Looking at this new illustration from the latest chapter and...

they put his cousin on the marriage candidate wall as well? 😭😭😂 Teruaki my boy you're not beating the allegations

#Kinosaki is not on the wall because the real deal is right there#i love this manga so much#marriage toxin#marriagetoxin#official art#not my art#gero hikaru#kinosaki mei#gero teruaki#that idiot is smiling like he didn't overdose on amiodarone on purpose a few chapters ago
38 notes
·
View notes
Text
The design is still available now in our Redbubble store
RYEY22.redbubble.com

#**Medical illustration#Cardiology art#Amiodarone design#Heart anatomy#Lightning bolt art#Pharmacology design#Heart rhythm#Black and white artwork#Medical creativity#Cardiac medicine#Heart symbolism#Healthcare design#Medical art inspiration#Heart health#Medical professionals**#cnc free use#usa
2 notes
·
View notes
Text
Hyperthyroidism: Its Important Symptoms, Causes, Treatment And Lifestyle
Hyperthyroidism: Symptoms, Causes, Treatment And LifestyleIntroductionFunction Of Thyroid GlandWhat is Hyperthyroidism?Causes of HyperthyroidismSymptoms Of Hyperthyroidism Physical Manifestations Emotional RollercoasterDiagnosis Of HyperthyroidismTreatment Options: Bringing Harmony Back Medications Radioactive Iodine Therapy Surgical InterventionEmbracing a New Rhythm: Living with…
View On WordPress
#amiodarone induced thyrotoxicosis#complications of hyperthyroidism#elevated thyroid levels#factitious hyperthyroidism#goiter hyperthyroidism#graves disease hyperthyroidism#graves disease medication#graves disease tsh levels#high thyroid symptoms#hyper thyroid#hyper thyroid symptoms#hyperthyroidism#hyperthyroidism causes#hyperthyroidism hair loss#hyperthyroidism in men#hyperthyroidism medication#hyperthyroidism signs and symptoms#hyperthyroidism symptoms#hyperthyroidism symptoms in females#hyperthyroidism treatment#hyperthyroidism tsh levels#hyperthyroidism weight loss#hypo and hyperthyroidism#hypothyroidism and hyperthyroidism#i cured my hyperthyroidism#medicine for hyperthyroidism hyperthyroidism symptoms in men#over active thyroid#overactive thyroid gland#overactive thyroid medication#overactive thyroid symptoms
0 notes
Text
Drug Orders and Doses

@whumpsmith
Cool, so I think the first thing to know is how medication is ordered.
Generally speaking, it will be ordered in 5 parts, known as the "5 Rights" of medication administration:
#1 What patient is getting the medication
#2 What medication is to be given
#3 How much medication is to be given
#4 What time it is to be given (or how often)
#5 What route it is to be given
So an order might be "Give John Smith (5/13/1995) lorazepam 0.5mg IV once prior to MRI"
In this example, John Smith is the patient and 5/13/1995 is his birthday to differentiate him from all the other John Smiths. "Lorazepam" is the drug's generic name, "0.5mg" is the amount of the drug. "IV" is the route, and "once prior to MRI" is the time.
Drugs have generic and brand names. For example, acetaminophen is a generic name. Many companies make acetaminophen, and each has their own brand name for the drug. Probably the most well-known brand name for acetaminophen is Tylenol, but there are others, like Calpol and Panadol. For most people, it doesn't matter which brand of a particular drug is used, just that the active ingredient (the generic name) is the same. For some people it matters because the non-active ingredients may be different between brands, and they may be allergic to a non-active ingredient that is in one brand, but not another.
In a hospital setting, we're going to use the generic name, because the brand of the drug that is cheapest to the hospital pharmacy varies contract to contract, and there are a lot of drug shortages these days. That's why if you're in the hospital you might get an oval green pill one day and a round white one the next day. They're the same drug, just different brands.
The dose is given in milligrams, usually abbreviated "mg". Milligrams are a measure of weight. Cubic centimeter (cc), on the other hand is a measure of volume. At some point we switched from volume based to weight based measures because we had a lot of different concentrations and using volumes for everything made mistakes really common. If you're using weights, it doesn't matter if the concentration you have is 1mg/mL or 10mg/mL for a given drug, you can do the math and come up with a volume that is right instead of just hoping you picked the one the doctor was thinking about when they wrote the order.
There are many routes a drug can take into the body. There is oral (a pill or liquid), IV (injection in a vein), IM (injection in a muscle), SQ (injection into fat), rectal/PR (a suppository, gel, or liquid inserted into the rectum), SL (under the tongue), TD (a paste or patch that sends medication through the skin) and many more.
Times can be once, once every x hours, once every x hours as needed (PRN), once under a particular circumstance, daily, or pretty much any other interval you can think of. "Stat" is a term meaning "right now".
Here's a list of common medications and their dosages:
CODE DRUGS:
Epinephrine 1mg IV for cardiac arrest every 3-5 minutes, 0.3mg for anaphylaxis
Amiodarone 150-300mg IV over 10 minutes for cardiac arrest
Lidocaine 75mg for cardiac arrest initially, if that doesn't work then 37.5 10 mins later
Adenosine 6mg given very quickly for PSVT, if that doesn't work, give 12mg
Atropine 1mg every 3-5 minutes for low heart rate until heart rate is normal
OTHER DRUGS:
Albuterol 2.5mg in nebulizer for brochospasm/asthma attack
Metoprolol 5mg IV every 5 minutes up to 15mg for severe high blood pressure
Furosemide 20-80mg IV for fluid on lungs
D50 25g IV for low blood sugar
Diphenhydramine 12.5-50mg IV for allergic reaction
Morphine 2-10mg IV or IM for pain
Fentanyl 50-200mcg for sedation
Mannitol 20-150g for increased pressure inside the skull
Nitroglycerin 0.3-0.6mg every 5 minutes up to 3 times for chest pain (angina)
Naloxone 8mg nasal spray every 2-3 minutes for opioid overdose
Flumazenil 0.2mg IV for benzodiazepine poisoning, if that doesn't work give 0.3mg, if that doesn't work, give 0.5
Diazepam 15mg rectal gel for seizures that don't stop
Phenobarbital 1-1.5g IV for seizures that don't stop
Etomidate 22mg IV for anesthesia (for things like intubating someone)
Midazolam 5mg IV for sedation prior to surgery
Olanzepine 5-10mg IV for agitation (emergency sedation)
Haloperidol 0.5-10mg oral or IM for agitation (emergency sedation)
#whump reference#writing reference#drugs#whump#medical orders#sedation#anaphylaxis#cardiac arrest#pain
126 notes
·
View notes
Text



Paramedic Report
Incident Number: 2024-07-08-DK-0562 Patient Name: Darren Kozlowski Age: 31 Sex: Male Height: 6’1” Weight: Approx. 185 lbs Date of Incident: July 8, 2024 Time of Call Received: 10:12 AM
Incident Description: Emergency services were dispatched to a trail located in Riverbend Park following an alert from the patient’s smartwatch, which detected a suspected cardiac event. Bystanders reported finding the patient collapsed approximately 1.3 miles into the trail. The patient was unresponsive and pulseless upon paramedic arrival at 10:22 AM.
Initial Assessment:
Airway: Clear
Breathing: Apneic
Circulation: No palpable pulse; asystole confirmed on ECG
Skin Condition: Cool, pale, diaphoretic
Interventions (On-Site):
CPR initiated: High-quality chest compressions performed immediately upon arrival.
Defibrillation: Delivered one shock (200J) following identification of ventricular fibrillation (VF) on ECG. VF converted to sinus rhythm; ROSC (Return of Spontaneous Circulation) achieved at 10:27 AM.
Medications Administered:
1 mg Epinephrine IV every 3–5 minutes during CPR (3 doses given).
300 mg Amiodarone IV push following initial shock.
Transport to Hospital:
Time En Route: 15 minutes
Condition During Transport: Patient deteriorated en route, suffering a second cardiac arrest at 10:33 AM. Aggressive CPR was resumed with defibrillation (2 shocks, 200J each) and ROSC achieved at 10:38 AM.
Vital Signs Pre-Hospital Arrival:
Heart Rate: 48 bpm (weak, irregular)
Blood Pressure: 72/50 mmHg
SpO2: 82% (on 100% O2 via BVM)
Hospital Arrival:
Time of Arrival: 10:44 AM
Patient presented with recurrent arrhythmia, hypotension, and altered mental status. Handoff provided to ER staff for advanced resuscitation.
Autopsy Report
Patient Name: Darren Kozlowski Case Number: ME-2024-894 Age: 31 Sex: Male Date of Death: July 8, 2024 Time of Death: 11:03 AM Performed By: Dr. Laura Mendelson, MD, Forensic Pathologist Location: County Medical Examiner’s Office
External Examination:
Height: 6’1”
Weight: 185 lbs
Build: Lean and fit; well-developed musculature.
Hair: Short blonde hair and beard.
Eyes: Blue.
Distinguishing Features: None noted.
External Trauma:
Rib fractures (bilateral, 3rd–6th ribs) consistent with CPR.
Bruising along the sternum.
Minor abrasions on knees and hands from collapse.
No other injuries identified.
Internal Examination:
Heart:
Weight: 375 grams (normal range: 280–340 grams).
Severe coronary artery disease identified:
95% occlusion of the left anterior descending artery (LAD).
80% occlusion of the right coronary artery (RCA).
Evidence of acute myocardial infarction (MI) involving 40% of the left ventricle, with microscopic examination confirming recent myocardial necrosis and hemorrhage.
Mild left ventricular hypertrophy noted (wall thickness: 1.5 cm).
Lungs:
Pulmonary congestion and edema (weight: 750 grams per lung).
No evidence of pulmonary embolism.
Other Organs:
Liver: Mild steatosis.
Kidneys: Acute tubular necrosis, likely secondary to hypoperfusion during cardiac arrest events.
Brain: Mild cerebral edema, no gross signs of anoxic injury.
Toxicology Results:
Negative for alcohol, illicit drugs, and prescribed medications.
Positive for mild caffeine levels consistent with normal consumption.
Cause of Death: Acute myocardial infarction due to severe coronary artery disease, complicated by multiple cardiac arrests.
Manner of Death: Natural.
Pathologist’s Summary: The decedent, a 31-year-old male, succumbed to complications from a severe heart attack while running. Advanced resuscitation efforts successfully restored circulation twice; however, irreversible cardiac damage and circulatory collapse led to his death. Contributing factors include undiagnosed atherosclerosis and left ventricular hypertrophy, suggesting a predisposition to cardiac events under physical exertion.
16 notes
·
View notes
Text
Cytochrome P450 Inducers & Inhibitors
The main ones can be remembered using "CRAP GPs spend all day on SICKFACES.COM".
Cytochrome P450 Inducers
These induce CYP450 activity, and thus reduce the concentration of drugs which are metabolised by this system.
Carbemazepine Rifampicin Alcohol (chronic use) Phenytoin Griseofulvin Phenobarbitone Sulphonylureas, St John's Wort, Smoking
Also topiramate.
Cytochrome P450 Inhibitors
These inhibit CYP450 enzyme activity and thus increase the concentration of drugs which are metabolised by this system.
Sodium valproate Isoniazid Cimetidine Ketoconazole Fluconazole Alcohol (acute use), Amiodarone, Allopurinol Chloramphenicol Erythromycin Sulfonamides, SSRIs Ciprofloxacin Omeprazole Metronidazole
Also grapefruit, cranberry juice, diltiazem, verapamil, clarithromycin.
Common Interactions
Medications which commonly interact with CYP450 inhibitors and inducers are:
Warfarin
Phenytoin
Combined Oral Contraceptive Pill (COCP)
Theophylline
Corticosteroids
Tricyclic antidepressants
Statins
Lamotrigine
Midazolam
#medical school#pharmacology#drug interactions#mnemonic#prescribing#med student#revision#cytochrome p450#cyp450#medicine#studyblr#medblr#warfarin
9 notes
·
View notes
Text
Medwhump May- Day 5
"Stay with me."
@medwhumpmay
Tw: gore, cpr, resus and absolutely no medical accuracy or knowledge of medication, sorry! (always happy to learn something new, feel free to tell me)
Part 5 (all others here)
Everybody had their hands away from the dead body with the fibrillating heart.
Electricty jumped throughout that fragil frame of a woman.
Her head lolled to the side, the ambu bag pulling at her lips. Arms exploded in the air and fell back. The IV line jiggled, her feet also fell back with a distinct thud on the table.
The assistent had a bloody gloved hand on her shoulder a few moments after. "Come on little miss, stay with me."
The jumble on the monitor formed a single spike. And turned into an unstable sinus rhythm.
"That's it, hunny." His hand squeezed her shoulder encouraging. "We're going to get you through this."
But as if fate had her hands in it, the jumble appearing on the monitor again, begged to differ. "Shit!" The assitent yelled again and pressed his straightened arms down on her bruised sternum without hesitation.
By his third compression, a rib shifted and cracked. The sound echoing through the busy OR.
The anestesioligist had his hands on the ambu bag again and was squeezing air into her useless lungs.
After about 18 compressions, the surgeon demanded a status check again. His assitent, breathing heavily from the strain pulled his hands away from her bruised sternum. Despite, the still pumping anesthesiologist, everybody had their eyes on the equipment.
The young lady was clinically dead, but her bloody, opened body, covered in red and blue bruises from cpr, was slightly shaking from her fibrillating heart. "Still in vfib. Shocking her again." The head surgeon anounced strongly, already the paddles, handles covered in her blood, in hand.
"Clear!" Everybody had their hands visibly away from the table.
Another electric shock jumped through the lifeless form. Another few thuds from extremities following gravity back to the metal surface. Her head already fallen to the side, just wiggled slightly.
No change on the monitor. A frantic line consisting out of tiny spikes lining themselves against another. Two zeros blinking at the edge of the display. The assitent was just about to get his hands down on her broken ribs.
"AGAIN!" The surgeon cried from the other side of the table. "CLEAR!"
No one had really moved. The small body jolted on the table. This time hands and feet flying even higher, just to fall back looking more lifeless. Her feet had fallen to the sides. The outstretched arm with the IV lay where it had fallen, slightly bend. The other hand had landed on her belly.
"Come on, little miss! Come on!" The assitent was looking in her pale, expressionless face as the anesthesiologist took a hold of the ambu bag again.
The surgeon, paddles still in hand, was eyeing the monitor, ready to shock her again.
Nothing. Two tense seconds passed and the sinus rhythm was back. "That's it, baby girl! I know, you could do it!" He gave the unconscious woman on his table a sympathic smile. Then his face and tone turned professional again. "Amiodarone now. We don't want to lose her again."
->Day6
My masterlist
#medwhump may#day 5#stay with me#whump#writing#whump writing#female resus#female cpr#cpr#resus#female cardiophile#female whumpee
19 notes
·
View notes
Text

TIMING: current. PARTIES: @rn-zane & @mortemoppetere SUMMARY: zane witnesses emilio 'taking care' of one of his clanmates. they're probably not going to buy friendship bracelets. CONTENT WARNINGS: none.
Rainy nights were always worse, somehow. Emilio wasn’t sure what did it. The smell, maybe, or the extra ache that the heaviness in the air added to his bad knee. His temper was always just a little shorter, his nerves just a little more frayed. Juliana would say it made him sloppy. She’d never shied away from calling him out, even when they’d been in the ‘courtship, looking to impress’ phase of their relationship. But she wasn’t here to call him out now, and the sloppiness remained.
Normally, he would have made sure there was no one else in the alley outside the hospital where he’d chased this particular vampire down to. He’d look around, sweep the perimeter, cover his bases. But the rain and the smell and the ache in his knee all served to distract, and he pounced without thinking first. The vampire turned to dust, and that feeling that made the hair stand up on the back of his neck, the one that told him there was a vampire nearby?
It stayed.
Emilio whipped his head around, eyes wild as they landed on a man in scrubs standing a few feet away. If his senses were right — which they always had been — this guy was a vampire, too. In scrubs. Working in a hospital.
Talk about recipe for disaster.
Turning to face the other fully, Emilio held up his stake in warning. “Tell me who you are,” he said, accent twisting around the words as the adrenaline pounded in his veins, “slowly.”
—
Zane had been running all night. Even though stamina wasn’t really an issue anymore, his brain was completely fried. After almost mixing up adrenaline with amiodarone, he was ushered off to take a breather and come back once he’d composed himself. It wasn’t exactly possible, composing yourself in five minutes in the bathroom with the sound of chaos still seeping in through the door but an attempt was made. A few breaths, not really bringing oxygen but centering him in a way that had always helped when he was still breathing, and a quick check at his phone. “You have time for a quick delivery? Am outside, no rush tho, buddy :D”
He really didn’t have time but this was his job with the community. A job he did well and kept him important and liked. Not that they didn’t like him for him but still. Zane couldn’t take the chance of messing up this soon and losing this precious position no one else in the community could fill. So he made the time, sneaking out of the bathroom and rushing for the emergency blood cooler. The only good thing about this ER chaos - no one questioned a bag or two missing, putting it down to a mistake in charting. Those happened a lot when people were being barreled into the ER with strange bites, weird wounds and high on some drugs no one could classify. Mixed in with the occasional hypertensive elderly woman who forget her meds this morning.
Two bags of blood in hand, covered by the ratty sweater he always brought with him, Zane traversed the less crowded hallways and down the abandoned stairwells until he reached the rarely used door to the empty alley. It used to be where they kept the organic waste dumpsters but after those kept getting broken into, the dumpsters had since been moved inside under lock and key. And there he was. Until he wasn’t.
Jack’s red eyes were visible in the dark, not quite hidden by the hulking frame of the stranger whose back was turned to Zane, until they suddenly weren’t glowing anymore. It was like he’d evaporated into thin air, if not for the thin sheen of dust now floating through the air, catching the dim street light. There was no time to think, no time to wonder if this was how he was going to die one day, just evaporating into dust, before he was being addressed. Standing, frozen with the blood still covered by his sweater, Zane’s grip tightened on the door in his hand. The wood creaked slightly in his hand.
“I work here,” was all he could muster as a response, eyes flicking to the weapon in the broad shouldered man’s hand. Had he killed Jack? Accident? No, not very likely. Was it a vampire thing or just some regular shady ass business? His feet were, on instinct, shuffling very slowly, 1/10th of an inch at a time, back towards the open doorway. “And I should get back inside…”
—
He worked here. Obvious enough, given the outfit. Emilio might not have a ton of familiarity with hospitals or doctors, but he knew enough to know that nobody dressed like that unless they were expecting to end up covered in blood. And despite the fear dancing in the vampire’s eyes, he didn’t seem outright surprised to have seen someone turn to dust in the alley outside. That probably meant he knew there was a reason for it, right? Was he in on it? Paranoia clawed at Emilio’s chest, desperate and uncertain.
“More than that, I think,” he said lowly, taking a step towards the man. “Stop moving.” He didn’t want to kill the vampire without reason — Emilio’s code of ethics made little sense to anyone outside of Emilio himself, but it did exist — but he’d do it if the only other choice was to let an unfamiliar vampire flee into a hospital full of vulnerable people. Too much damage could be done otherwise, and he could justify that risk.
Taking another step forward, Emilio wagged the stake in front of him in warning. He did his best to hide his limp as he walked, sacrificing comfort for intimidation. “You know him? This asesino I just took care of? He was a friend of yours?”
—
Zane froze in place, the low grumble of the man’s voice settling in his spine with an uneasy feeling of genuine fear. The stranger was getting closer, menacingly waving the weapon - a stake? - in his hand. Was he going to get impaled?
Despite being told to stop moving, Zane dropped the sweater covered bags to the ground and raised his hands slowly. The rules of vampire versus stake were probably different than being held at gunpoint but Zane’s brain was short circuiting and he really didn’t want to die tonight. ‘This asesino I just took care of.’ It took a second to register the Spanish thrown in there and then a few more to properly swallow its meaning, not to mention the casually macabre way this man spoke about the loss of life (or unlife) that had just taken place.
“He isn’t - or wasn’t, a murderer. Or not that I… You’re the one that just impaled him and are threatening me, I haven’t hurt anyone. Ever. I wouldn’t. Not just because of the healthcare code and all that, just in general.” He was rambling, wondering what, if anything, could get this man to simply disappear. Maybe nothing would work, Zane had seen his face and the characteristic nose and beard would be burned into his retinas forever. Not to mention the icy glare in those eyes, covered by what seemed like years of stress and not too much smiling, maybe. Would Zane get killed to protect this man’s identity?
“And I won’t tell anyone. That I saw you, I mean. Or Jack. I can keep a secret, they’ll just think he ran off or got into some trouble and you won’t need to be connected to this. I just want to get back to work.”
—
The vampire dropped what he was holding, and Emilio’s eyes flickered down briefly to the ground. The sweater, which had been covering the real prize gathered in the man’s arms, shifted as it was dropped, revealing the plastic underneath. It looked like… a bag of blood? Someone more familiar with hospitals would have likely known what it was for, but to a man who’d grown up among people who’d much rather die with glory than visit any kind of real medical professional, it seemed foreign. He had no way of knowing where the blood had come from; given the way he was raised to feel about vampires, he could only assume something sinister.
“Where did you get that?” He gestured to the blood bags on the ground, suspicion clear in his expression. “You drain someone for it? Have your fill and decide to save more for later?” Was that what he was doing in the hospital? Using it as a way to troll for his next victim? It was a scary thought, the idea that a vampire was smart enough to extract blood from someone and put it into a bag to make use of later.
His eyes darted briefly to what remained of the dust on the concrete, a sharp laugh cutting through the air. “If you think that, maybe you didn’t know him.” There was every possibility that this man had just gotten wrapped up in something too big for him to understand. If that were the case, Emilio almost felt sorry for him. Almost. The blood bags on the ground were still suspicious enough to arouse Emilio’s paranoia to the extent that it was difficult to feel real empathy for the vampire.
“Tell anyone? Who would you tell?” Not his coworkers in the hospital, surely; none of them would see any sanity in the claim that he’d seen someone turn someone else to dust outside their place of employment. Other vampires, maybe? If he knew one, did he know more? Paranoia crawled in again.
—
Zane followed the stranger’s gaze to the rumbled sweater, the corner of a bag peaking out, and it took everything he had not to start cursing out loud. Stupid, impulsive brain, making him throw his literal loot to the ground for everyone to take a peek at. How nice it would be, to have a functioning head that gave a split second ‘maybe you should think about this’ before his body just did whatever the heck it wanted to. In the same vein, lying didn’t exactly come naturally to him under the most relaxed of circumstances, which this certainly wasn’t. So a truth bomb it was.
“Drain someone, what…” Eyebrows furrowed and he was almost tempted to ask a follow up question to what kind of operation this man thought the hospital was running but thankfully, the very serious air of the question stopped Zane from insulting this man and most likely getting stabbed. “No, that’s just… I stole it. Not from a person, just from the… fridge. It’s from a blood donation but just… not being donated to someone in the ER like normally.” Did that make sense? Maybe, it was hard to tell when his attention kept passing from the stake to the speckles of dust that used to be his Netflix binge watching buddy and back to watch every twitch in the man’s muscles for a glimpse of an upcoming attack.
There was no real answer to how well Zane had known the vampire-turned-dust, however. He’d known his name, how long he’d been with Alma and that he liked suspenseful shows. It had more so been the fact that there was no way he’d been living with a group of murderers, or even a single murderer, for this many months without realizing it. The whole reason for providing the blood bags was so that no one would have to get hurt and no one would have to starve… right?
Obviously, displaying the looted bags of blood hadn’t been Zane’s only slip up, evident when the interrogation about who he would tell started. “No one,” he blurted out, seeing something rise behind the other man’s eyes that made Zane’s skin crawl. “Really,” he added for pointless emphasis, wondering if he’d have time to grab the bags of blood before slamming the door shut. It locked from the inside and would at least give him a moment to think about his next steps. Maybe not, but it was worth a try.
One foot sweeped at the sweater covered bags, swooping them most of the way back into the hallway before the sweater got stuck on a stray nail. He was already trying to hurriedly close the door so when it slammed on the bags, leaving a good few inches of open door between him and the armed stranger, all he could hope was that this guy wasn’t a fast runner.
—
If it was a lie, it was a bad one. He stole the bags from a fridge? Whose fridge? Another vampire? Emilio’s head spun with the possibilities, eyes darting from the bags of blood on the concrete to the man who’d dropped them with no small amount of suspicion. What was he supposed to do here, exactly? He knew the vampire he’d killed had deserved it, but he couldn’t say the same for this one. On the surface, he seemed like a scared hospital employee who’d just witnessed something unexpected. If not for the bags of blood he was trying to make off with, Emilio might have wondered if his senses were lying to him with their claim that the man was undead. But the blood was a dead giveaway.
And so was the fact that his next statement was a much more obvious lie. Maybe that was a good thing, considering; Emilio had a baseline now, a known lie to play off of. If that was how he sounded when he was bullshitting, it seemed much more possible that he’d been telling the truth about where he’d gotten the bags. The immediate defensiveness in response to the question was enough to lead Emilio to believe there were, in fact, more vampires in this guy’s inner circle. That probably meant the blood bags weren’t just for him, then, which also made sense. It’d be a lot of blood for one man alone.
“You can be honest with me,” he said, still brandishing that stake, “or we can have a problem. And I don’t think you want to have a problem.” Threats, with vampires, tended to be the kind of thing that could go either way. Back in Mexico, when his family name had always allowed his reputation to precede him, they’d been effective more often than not. But now? Emilio hadn’t used his surname in years for fear of what it might bring to his doorstep. The only thing he had to back up his threats was him. Luckily, in this case, that seemed like it might be enough. The vampire had just seen him stake one of his buddies, after all. And he looked pretty uneasy about the whole thing. Good.
But… sometimes even the most well-believed threats didn’t have the effect you were hoping for. Emilio had wanted to scare the guy into talking. Instead, he ran. And that was… less than ideal. There was a time when Emilio had been far faster, able to keep up with anyone and everyone, but that time had ended in Mexico, when everything else ended with it. His bad knee screamed at the mere concept of making a break for it, but he ran anyway.
If not for the jacket catching in the door, that would have been the end of it. Emilio wasn’t fast enough to keep up and, if that door had closed, there was no way he’d have been able to get into that hospital undetected. But the door remained open just enough for him to slide his fingers through and yank it the rest of the way, sliding inside and taking off after the vampire.
—
Fuck, fuck, fuck. Zane could hear footsteps thudding down the halls after him and something told him this guy wouldn’t have any qualms about being spotted sprinting down hospital halls, seeing that he’d just casually murdered someone. A vampire, but someone nonetheless. Not that the odds of running into someone down here were very high - these halls only had traffic around shift changes and that was hours from now. Zane was well and truly alone down here. Pens and bottle caps jangled in his pockets as he ran, a few even slipping from their safety and tumbling to the ground. Escape routes, escape routes…
The sound of running still closing in behind him, Zane sped up and turned the corner, just barely avoiding the abandoned stretcher that someone had been planning to fix for months now, with a dexterity that only came about from avoiding patients on the move every day in the ER. Slippers hanging on by pure will, he tried to regain speed from the turn which was hard enough without the slippery hospital floors and ill fitting slippers. Fuck, he was going to catch up to him, he was going to drive that scary looking stake right through his heart and no one would ever know where Zane disappeared to and no one would probably even care enough to notice much anyway-
Clang.
Zane’s head whipped back around which really made it hard to run fast but it was instinct - you hear a noise, you look towards it. The stranger was clutching his knee, the stretcher now askew and clearly, not everyone was as good as dodging stretchers. Even static ones. For a second, Zane slowed and stared, the instinct to treat the wounded taking over before his brain rebooted back to the situation at hand. Imminent death. Right. Slowly but surely backing up towards the nearest access restricted door, Zane fumbled for his keycard and swiped at the reader behind his back. As it beeped, the words slipped out before he could really stop them. “Sorry.”
The door shut behind him and he sprinted until he reached the entrance to the ER, feeling like he definitely should have been panting by now. Head reeling, the first thought on his mind, and the dumbest, was that he’d just lost his favorite sweater.
—
The hall was empty. It was definitely a relief, both because Emilio wasn’t looking to explain to any concerned doctors or nurses why he was chasing one of their coworkers through the hallway and because it meant there was no one for the vampire to grab and use as leverage. Hostage situations got sticky fast, and Emilio had never been particularly good at navigating them.
Of course, even with not curious bystanders, this situation wasn’t ideal. He was at the disadvantage here and he knew it. Not only did his old injury slow him down, but the vampire also had the advantage of knowing these halls. Whatever else he’d lied about, the claim that he worked in this hospital seemed to be a true one. He navigated the twisting halls with relative ease, leaving Emilio to follow and do his best to keep up.
It was a losing battle. He knew that. He knew there was no world where he caught up, knew that it was a matter of time before this vampire found someone or something to use against him. He didn’t expect that to come in the form of a haphazardly placed gurney in the middle of the hall. So focused on following the vampire, Emilio didn’t register the obstacle until he’d barrelled straight into it. He couldn’t keep himself from toppling to the ground, bad luck ensuring that his bad knee took the brunt of it. The hunter couldn’t bite back a string of curses as he fell, clutching his knee and gritting his teeth against the pain.
Ahead of him, the vampire stopped. Emilio tensed as he turned, scrambling for his stake only to find that it had landed out of reach. And, Christ, this was it, wasn’t it? He’d taken off after a vampire through the empty halls of a hospital, and now he was going to die here, alone and forgotten. Estúpido.
Except… the vampire didn’t make a move towards him. Instead, puzzlingly, he apologized. He said sorry, and he looked like he meant it. Before Emilio could unpack that, the vampire was gone, disappearing behind a locked door with a definitive beep and leaving the slayer on the floor in an empty hallway, feeling more lost than he had in a while now.
Wicked’s Rest. Weird place.
10 notes
·
View notes
Text
Adenosine is given 0.1 mg/kg for peds pts who weigh less than 50 kg with SVT. If ther first dose of 0.1 mg/kg doesn't work, then you can give 0.2 mg/kg for the second dose.
For adults, it's 6 mg, then 12 mg. In the ED, I've seen adult pts just get 12 mg the first time.
Procainamide, amiodarone, or verapamil can be used to cardiovert peds pts who are still in SVT after failing the two doses of adenosine.
2 notes
·
View notes
Text
idk what to do anymore...
I knew that after being on my own, It’s hard to feel like I’m fully ready. I remember the first day I was by myself, my charge nurse, gave me some reassurance and even gave me their number if I needed help. I had 2 patients, one on a pressor and one who had propofol and fentanyl while being vented. From that point till now, I had days that were ups and downs. Trying to learn and not make the same mistakes. I remember every bit of what happened based on my experiences because there’s not a day that goes by where I don’t know if I gave it my all to my patients. My coworkers tell me I worry too much but it’s a unit that’s built on a critical care and I’m the type to be really cautious. I’ve had assignments that I felt where it didn’t felt right to be tripled or even appropriate for someone who just came off orientation but I still continued on. Learning from my experiences over and over again. Then go home and vent about my day to my mom who’s also a nurse because she’s someone I looked up to. I’ve had doctors who even taught me things that I haven’t learned or experienced yet. I made it to the point of almost 4 months. Just trying to survive and not kill anyone.
With my past, I get why it’s easy to pin the blame on me. Someone who just got off orientation 4 months prior, was given to a preceptor on the first day of orientation that didn’t really do anything and only to be taken off from work later when I wasn’t under them (i felt humble with my experience with them because they taught me what they could), had reports from nurses that say they weren’t up to their expectations even though I spent as little as a day with them, had a preceptor that didn’t work out very well which extended my time so that I can be given another chance. Through all of that to remedy the negatives, I had a wonderful time with the preceptors they’ve chosen later on, especially my night preceptor. If it wasn’t for them, I wouldn’t be where I am now. I knew I feel like I wasn’t ready when they said I was ready to be on my own. Because when do you truly feel ready when you are with no one holding your hand by your side? But as time goes by, my confidence slowly grows. Taking into account what I’ve done and take them to heart so that I could grow myself better. I had to do the self reflection on myself because no one else told me to... But I still wished they had told me what I needed to improve on. If what they’ve said was true, why did I had a patient tell me that they liked how attentive I was with them, why did I have another patient told me god bless and said they really liked how I took care of them, why did I have another patient tell me they liked me as their nurse and even praised me for my services. They were the only critics I’ve had. I’ve been there when a patient cried and held their hand, told me their story of how they weren’t shown any sympathy besides me. That’s the reason why I became a nurse. I wish they have told me what I needed to do and what to improve on, so that I can do what’s necessary. Or if there was a problem, it should’ve been brought to my attention even if it’s good or bad. It was only a matter of time before I suffered the consequences.
I would think you were supposed to be in a unit that’s built on teamwork, but the first number one advice I was given was “Don’t trust anyone.” I remember that day so vividly. I was tripled at the time and one of my patients wanted a sprite and crackers. I catered to their needs as well as the other patient with family because I wanted them to be comfortable. When I had finished giving the food, I noticed a call light with another one of my patients. I quickly came in and saw that the patient was desaturating. Immediately, I knew it was a respiratory issue and I wanted check if he was receiving the nasal cannula properly, even checked the waveform of the pulse ox. At the time, they were receiving precedex and amiodarone so I turned off the sedation to see if it would help him wake up even though it was at a low dose and not long ago he was even hanging off the bed while my Tita helped the patient get picked up to be properly place on the bed. He was mouth breathing and was barely holding on so I notified RT who was just next door to come and help me place the patient on BiPaP. I even took another pulse ox with me to check if it wasn’t picking it up properly because before that was the issue and the patient was fine. Once placed on BiPap and changing the pulse ox, I checked the saturations and it was picking up but not where it needs to be so I knew something was wrong. I checked for responsiveness and there was none so I immediately left and went to charge to tell them my findings with the interventions I’ve done while the RT was still at bedside. Since then, I didn’t know it was going to be the worst day of my life. Wasn’t it rational to escalate it to charge? I was taught since day one to notify them if there’s an emergency or situation you couldn’t handle, especially by someone who’s still learning the ropes of the ICU. When the event was over, the patient passed away. Mucus plug because of their esophageal stage 4 cancer and there was an order not to have him deep suctioned. I was numb. People try to help me and ask if I was okay, but I felt like I wasn’t. I felt like I didn’t do my best. The son understood what happened and even told me he saw what we did and he appreciated what we’ve done. I felt like it was an eye opening experience for me because it was the first time it ever happened to me... and the last. The day after, receiving report but then told to go down to meet house sup. I still didn’t feel like I was myself. Upon receiving the news I was suspended, I didn’t even have the urge to cry. I just felt like I have no emotions. It’s weird because I get emotional over things like these, but I just couldn’t get myself to do it. I just felt so... empty. A suspension without pay which was close to termination. I had no words left in me and drove home late at night close to 10. I learned afterwards and highly suspected the report was on the patient that died from a source. The report made, according to my sources, was your truly, my charge nurse. Whom I thought I was supposed to trust in situations like these. I’ve had multiple support when I asked around if what I did was right, but in their eyes, my charge’s, it wasn’t. It was so easy to blame it on me. I get it. Day after day whenever I work, I try to put a smile on my face because it helps me get through the day. I even try to ask for help if it was necessary. It’s been a few days since then, but I still feel hollow and emotionally depressed. I want to enjoy myself to ease the stress and to take my mind off of it but I can’t. I barely have an appetite and I just don’t know what to do. I hate this feeling because I wasn’t told what I was suspended for until a day later. I told my director that the assignment I was given didn’t feel right or safe, but they insisted that it was appropriate and that even PCU nurses can take it. I should’ve told them at the time that they don’t handle the meds that we have. I didn’t mention it until later on I left and got into my car. When I got home, I just feel like sleeping. I didn’t even feel happy with my mom who’s my comfort support when we went to the mall so she could cheer me up while picking up her online order. To this day, I still felt miserable. Somehow, inside me, I knew what the outcome is. If by chance this was pardoned, I don’t know if I can work in that type of environment anymore. I really really love working there. I love working with trauma. I love working ICU and the people there that I’ve met who are nice and willing to help me. What I don’t like is being backstabbed in the back. It was my second betrayal while working in that hospital. Should I even continue working in that type of unit? I just don’t even know what to do anymore...
#rant#im done#listening to numb little bug#i actually cried while writing this haha#<-- me fake laughing#currently praying#how many times have i prayed this year and last year?#idk#i feel like crap
6 notes
·
View notes
Text
Always. ALWAYS check interactions between medications and other medications, medications and food and medications and other illnesses you may have!
If you want to learn more, I've provided some examples of medicine interactions 👇
Food/medicine interactions:
alcohol and pretty much any prescription medicine.
warfarin (used to treat deep vein thrombosis (blood clot in legs) and pulmonary embolism (one or more of your arteries to your lungs become blocked) ) and leafy greens.
Grapefruit/grapefruit juice and a lot of medications such as antihistamines (allergy medications like Allegra), statin-based cholesterol medications, Buspirone (a medication used to treat anxiety), Amiodarone (used to treat irregular heart beats conditions like Arrhythmia and Arterial fibrillation), medications used to treat high blood pressure, birth control, and so many more.
Licorice can negatively interfere with medications used to treat congestive heart failure, high blood pressure, and abnormal heart rhythms
Medication/medication/supplements/other conditions interactions
St John's wart weakens the effect of medications such as some heart medications, HIV medication, Warfarin, and some statins
Vitamin E shouldn't be taken with Warfarin. It increases anti clotting activities and increases chances of bleeding
Bronchodilators ( a medication to treat bronchial asthma) and nasal decongestants ask a medical professional before you start either of these treatments, especially if you have heart disease, high blood pressure, thyroid disease or diabetes.
This list is by no means a complete list, just examples I've found interesting or have heard the interactions with since I have family members who take some of these medications
If you're not sure, please please please ask!
Don't take medicine not prescribed to you.
Don't take more than prescribed.
Finish your medicine, even if you feel better.

59K notes
·
View notes