#respiratory assessment
Text
Comprehensive Nursing Care for Patients with Congestive Heart Failure (CHF)
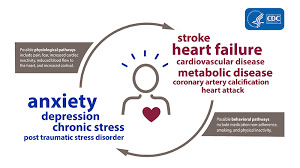
Certainly, when providing care for a patient with congestive heart failure (CHF), it’s important for nurses to be attentive to the patient’s mental status in addition to their physical condition. Here are some key aspects to consider:
Anxiety and Stress: CHF can be a chronic and debilitating condition, often causing anxiety and stress in patients. Nurses should be prepared to provide emotional…
View On WordPress
#cardiac assessment#CHF patients#congestive heart failure#dietary education#Emotional Support#exercise tolerance#fluid balance#fluid restrictions#healthcare team#heart-healthy diet#medication adherence#medication management#nursing care#oxygen therapy#patient education#respiratory assessment#self-monitoring#symptom management#vital signs
1 note
·
View note
Text




oxBk_PglA84
#doctor and patient#head to toe assessment#physical exam#stethoscope#doctor roleplay#male body#cardio exam#health assessment#heart auscultation#auscultation#male beauty#male aesthetic#pecs#big pecs#respiratory examination#respiratory exam
70 notes
·
View notes
Text
someone get me off this damn site i have an exam tomorrow at 1030am i gotta study 😭😭😭😭😭
#its health assessment w focus on respiratory and cardiovascular and supposedly the hardest of the exams in this class#there’s so much shit and i feel p good on the anatomy and normal vs abnormal signs in patients and stuff#but theres so many risk factors and symptoms we gotta know for cardiovascular diseases#and for respiratory we gotta know shit like what diseases make exactly what sounds and how people cough lmfao. so specific#but im gonna ball anyway IM NOT SETTING MY EXPECTATIONS HIGH THO IM PREPARING FOR DISAPPOINTMENT JUST INCASE U KNOW#send me good luck pleas im begging guys 🙏
9 notes
·
View notes
Text
Some days I think I probably do need an actually trained service animal for mental health crap + the occasional chronic crap affecting my mobility.
But like…I don’t really want a dog. I want a Highly Trained mainecoon or norwegian forest cat. Just. This very large very fluffy very baseline breed intelligent cat known to take on BEARS (or, home invaders and men attempting SA).
I’d be THAT Crazy Lady walking this giant fluff monster most days, but other days just have my lap full of fluff when my hips-down don’t want to cooperate, or I need the comforting weight and fluffy company to hold the brain static at bay.
And some days…look. It hurts to grasp things. Or I risk dropping things. And cats can and will open cupboards and drawers if the handles let them hook their paws Just So to make up for the lack of opposable thumbs.
(Yeah yeah I know people are more accustomed to training dogs for this, but I’ve had quite a bit of luck training my “just housecats” as adults with various things, and people post the adventures they take with their mainecoons like, all the time…so think of what I could do with socializing and training a cat if I had the chance to do so.
(…also I just get along better with cats than dogs. They’re more tolerant to my need to not have a true routine. Also they poop in a box.)
#tiger’s musings#yesterday was…ugh. think my body was fighting off a minor respiratory illness#bUT because I’m also chronically ill + have to take an immunosuppresent it…was not good#like I kinda freaked my online friends out with what my symptoms were#but…I’m just. so used to this. so used to just holding onto walls because I get so unsteady and trying to sleep through these episodes#it’s…definitely Something. not ‘jUST psYCHoSOmATiC’ like I got gaslit into believing 5+ years ago#but…with what turned out to be AS and Probably a CTD and Currently Assumed IBS (but prolly also CTD imo)#I…hadn’t really had a chance to do more than ‘okay so I also have tremors’#but hey. I have to have my annual pcp visit so I’ll make myself whine about it and the fluttery/tight/visible chest&pulse issues then#(they’re probably related. POTS…kinda can cause high bp/tachicardia and sometimes tremors too.)#(and like. high bp is kinda something so common in my family in young adulthood it’s a ‘when’ vs ‘if’)#so…yeah. sometimes I think I might need some sort of chair and service animal#in addition to custom fitted compression globes#and probably compression shorts and spats and sleeves on my knees and elbows#aaaaand prolly custom arch supports. in addition to Nicer Shoes than an Okay $50 newbalance pair#which…yeah. you can see how all this would get Very Expensive Very Fast#(aaaaaaaand… hope I don’t idk. get dropped from my medicaid? listen they’re sending me automated messages to get my risk assessment done)#(and I’ve got so much going on that I would be Screwed even if I hadn’t aged out of my dad’s insurance)#(it definitely affects me being able to work and keep a job)
2 notes
·
View notes
Text
Special Lung Health Package at HCG Hospitals Ahmedabad - Just ₹1999!

Book your lung health package at HCG Hospitals, Ahmedabad for just ₹1999 until April 30, 2024. Includes expert consultations, Spirometry, DLCO tests, and more. Prioritize your lung health and breathe easier with our comprehensive care.
#Lung health screening#Pulmonary function test#Respiratory health assessment#Lung disease detection#Bronchial health check#Lung health evaluation#Breathing capacity analysis
0 notes
Text
Airborne Risk Indoor Online Calculator (ARIA)
A team of international experts under the World Health Organization (WHO) developed an Airborne Risk Indoor Online Calculator.
ARIA is an online tool that enables users and building managers to assess the risk of SARS-COV-2 (COVID-19) airborne transmission in residential, public, and healthcare settings. The aim is to inform decisions that can significantly reduce the risk of transmission.
A 66-pages document [5.757 MB, English, archived] is available.
#clean air for all#clean air revolution#indoor air quality#COVID#COVID-19#SARS-CoV-2#COVID resources#COVID-19 resources#SARS-CoV-2 resources#online calculator#COVID tools#COVID-19 tools#SARS-CoV-2 tools#CC BY-NC-SA#Attribution-NonCommercial-ShareAlike#creative commons#respiratory aerosols and droplets#respiratory system#respiratory tract infections#risk assessment#risk reduction behavior#sneezing#disinfection#disease outbreaks#infection control#emergencies#delivery of healthcare#virion#referral and consolation#transmission
1 note
·
View note
Text
How does one manage airway and breathing in critically ill or injured patients?
Managing the airway and ensuring adequate breathing is a critical aspect of caring for critically ill or injured patients. In emergency medical services (EMS), prompt and effective airway management can significantly impact patient outcomes. This article will discuss the essential steps and considerations in managing the airway and breathing in critically ill or injured patients.
Continue reading…

View On WordPress
#advanced airway management#airway management#bag-valve-mask ventilation#basic airway maneuvers#breathing#Collaboration#communication#continuous monitoring#critically ill#documentation#emergency medical services#endotracheal intubation#injured patients#intervention#oxygen administration#oxygen saturation#pulse oximeter#rapid assessment#recognition#respiratory distress#respiratory rate#respiratory therapists#supraglottic airway devices#ventilation
0 notes
Text
Nasal COVID-19 vaccine halts transmission - Published July 31, 2024
Study in hamsters indicates vaccines targeting nose, mouth may be key to controlling spread of respiratory infections
A nasal COVID-19 vaccine blocks transmission of the virus, according to an animal study by researchers at Washington University School of Medicine in St. Louis. The findings suggest that vaccines delivered directly to the nose or mouth could play a critical role in containing the spread of respiratory infections.
The lightning-fast development of COVID-19 vaccines just months after the virus appeared was a triumph of modern science and saved millions of lives. But for all the good they did in reducing illnesses and deaths, the shots were unable to end the pandemic because of one notable weakness: They couldn’t stop the spread of the virus.
A new study by researchers at Washington University School of Medicine in St. Louis indicates that next-generation vaccines that target the virus’s points of entry — the nose and mouth — may be able to do what traditional shots cannot: contain the spread of respiratory infections and prevent transmission. Using a nasal COVID-19 vaccine based on Washington University technology, approved for use in India and licensed to Ocugen for further development in the U.S., the researchers showed that vaccinated hamsters that developed infections did not pass the virus on to others, breaking the cycle of transmission. In contrast, an approved COVID-19 vaccine that is injected failed to prevent the spread of the virus.
The findings, published July 31 in Science Advances, provide further evidence that so-called mucosal vaccines sprayed into the nose or dropped into the mouth may be the key to controlling respiratory infections such as influenza and COVID-19 that continue to circulate and cause significant illness and death.
“To prevent transmission, you need to keep the amount of virus in the upper airways low,” said senior author Jacco Boon, PhD, a professor of medicine, of molecular microbiology and of pathology & immunology. “The less virus that is there to begin with, the less likely you are to infect someone else if you cough or sneeze or even just breathe on them. This study shows that mucosal vaccines are superior to injected vaccines in terms of limiting viral replication in the upper airways and preventing spread to the next individual. In an epidemic or pandemic situation, this is the kind of vaccine you’re going to want.”
Developing vaccines that can control virus levels in the nose has proven challenging. Viruses such as influenza virus, SARS-CoV-2 (the virus that causes COVID-19) and respiratory syncytial virus (RSV) multiply rapidly in the nose and spread from person to person within a few days of initial exposure. Traditional injectable vaccines generate immune responses that can take a week to build to full strength and are much less potent in the nose than in the bloodstream, leaving the nose relatively unprotected against a fast-multiplying, fast-spreading virus.
In principle, a vaccine sprayed or dropped directly into the nose or mouth could limit viral reproduction and thereby reduce transmission by eliciting an immune response right where it’s needed most. But gathering evidence that mucosal vaccines actually do reduce transmission has proven tricky. Animal models of transmission are not well-established, and tracking person-to-person transmission is fiendishly complicated, given the number and variety of encounters a typical person has on any given day.
For this study, Boon and colleagues developed and validated a model for community transmission using hamsters and then used it to assess the effect of mucosal vaccination on the spread of SARS-CoV-2. (Unlike mice, hamsters are naturally susceptible to infection with SARS-CoV-2, making them the ideal laboratory animals for a transmission study.)
The researchers immunized groups of hamsters with laboratory versions of approved COVID-19 vaccines: the nasal iNCOVACC used in India or the injected Pfizer vaccine. For comparison, some hamsters were not immunized. After giving the vaccinated hamsters a few weeks for their immune responses to fully mature, the researchers infected other hamsters with SARS-CoV-2 and then placed the immunized hamsters with the infected hamsters for eight hours. This first step of the experiment mimics the experience of vaccinated people who are exposed to a person with COVID-19.
After spending eight hours rubbing shoulders with infected hamsters, most of the vaccinated animals became infected. Virus was found in the noses and lungs of 12 of 14 (86%) hamsters that had received the nasal vaccine, and 15 of 16 (94%) hamsters that had received the injected vaccine. Importantly, while most animals in both groups were infected, they weren’t infected to the same degree. Hamsters that had been nasally immunized had virus levels in the airways 100 to 100,000 times lower than those that had received the shot or had not been vaccinated. The study did not assess the animals’ health, but previous studies have shown that both vaccines reduce the likelihood of severe illness and death from COVID-19.
The second step of the experiment yielded even more striking results. The researchers took vaccinated hamsters that subsequently developed infections and placed them with healthy vaccinated and unvaccinated hamsters for eight hours to model transmission of virus from a vaccinated person to others.
None of the hamsters that were exposed to nasally vaccinated hamsters became infected, regardless of whether the recipient hamster had been vaccinated or not. In contrast, roughly half of the hamsters that were exposed to hamsters vaccinated by injection became infected — again, regardless of the recipient’s immunization status. In other words, vaccination through the nose — but not by injection — broke the cycle of transmission.
These data, Boon said, could be important as the world prepares for the possibility that avian influenza, currently causing an outbreak in dairy cows, might adapt to humans and trigger a flu epidemic. An injectable vaccine for avian influenza already exists, and a team of researchers at Washington University is working toward a nasal vaccine for avian influenza. That team includes Boon and co-author Michael S. Diamond, MD, PhD, the Herbert S. Gasser Professor of Medicine and one of the inventors of the nasal vaccine technology used in this paper.
“Mucosal vaccines are the future of vaccines for respiratory infections,” Boon said. “Historically, developing such vaccines has been challenging. There’s still so much we don’t know about the kind of immune response we need and how to elicit it. I think we’re going to see a lot of very exciting research in the next few years that could lead to big improvements in vaccines for respiratory infections.”
Study linked in the first link!
#covid#mask up#pandemic#covid 19#coronavirus#wear a mask#sars cov 2#still coviding#public health#wear a respirator
218 notes
·
View notes
Text
F1 and VO2 Max Training




(x)(x)(x)(x)(x)
What is VO2 Max Training and why do drivers do it?
VO2 Max is the maximum amount of oxygen the body absorbs during exercise and can measure aerobic fitness levels. VO2 = Volume of oxygen consumed by the body per minute - it is one of the strongest predicters of heart disease and death. It is the best measure of cardiac and respiratory fitness available.
VO2 is measured in ml (of oxygen) / kg (body mass) / minute
How much oxygen the body consumes - the amount of blood the heart pumps per minute and how much oxygen was taken from it.
Now...why do F1 drivers need this?
Drivers put extreme demand on their cardiovascular, respiratory and overall physical health during races. Their bodies are subjected to enormous amounts of g-force and experience extreme heat and stress. They need a lot of energy to do this and as a result can burn a lot of calories per race.
VO2 max training is a useful measurement to assess a drivers endurance at their maximum during exercise which they are subject to during a race. The strain they're under during a race would require their bodies to be pushed to the max, requiring optimal oxygen intake and energy production.
It can ensure drivers are fit enough to endure the stress they subject their bodies to despite the environment within the car - maximum speeds/ heat. It gives drivers and their teams a greater understanding of how hard they can push their bodies and also how they can further maximise their performance during races.
Want to know a bit more about the science? Read below.
Now the (more) science-y bit - oxygen is used in respiration and as you breathe in oxygen the lungs turn it into energy called ATP (adenosine triphosphate). This powers the cells and helps release the CO2 in the body that's created during respiration when you breathe out.
The greater a persons VO2 max, the more oxygen a body can consume and the more effectively the body can use this to create the maximum amount of ATP energy and the better the body can handle aerobic/ cardio exercise.
During the test the goal is to get to maximum exercise to determine max heart rate, vo2 max and an estimated lactate threshold. The test measures oxygen consumption and CO2 production using a mask to determine values. The goal is to run at a comfortable speed but not too comfortable for around 10 minutes to max out oxygen consumption and heart rate. During the test heart rate is measured using the ECG dots you can see on the chest.
The Fick Equation is used to calculate VO2.
VO2 (mls O2/ minute) = cardiac output (stroke volume x cardiac output) x arteriovenous oxygen difference (difference in O2 content between arterial and venous blood - how much O2 is used by tissues in systemic circulation).
So in short, VO2 is how much oxygen the body consumes - how much blood the heart pumps per minute and how much oxygen was taken from it.
#f1#formula one#formula 1#carlos sainz#charles leclerc#nico hulkenberg#pierre gasly#vo2 max#science#medicine#mine
197 notes
·
View notes
Text
I’m training someone tonight, and I was like “we’re focusing on time management!!! All initial meds and assessments done by 2300!!” And then we spent 90 minutes in a patient room trying to de-escalate a deeply confused patient so they wouldn’t end up in restraints again which ended up with getting an order to discontinue the intervention that was bothering the patient the most.
That was absolutely the best use of our time, but god it really drives home the time de-escalation takes. If we were short-staffed, if any of our patients were more acute, if frankly I was much less patient—it’s so easy for physical and chemical restraints to seem like the most reasonable option there’s just no time for anything else, and all your other patients are in pain or respiratory distress or have been calling to go to the bathroom but no one came so they were incontinent in bed and now they’re furious because they feel like we made them humiliate themselves, and no one else on the floor is helping you because they also have patients in vicarious stages of crisis and we have no CNAs because why would you do this work for the money we offer, plus the thousand other factors—valid and bullshit—that motivates decision making in the hospital.
De-escalation training is important and needs to get used waaaaaaaaaaay the fuck more. And also the workplace has to make slow, patient de-escalation feasible. Also by the way the patient we de-escalated tonight and kept out of restraints is literally SUCH a sweetheart now, it’s wild. But I am gonna schedule this post for the end of shift in case saying all that jinxes it.
455 notes
·
View notes
Text
IOC Study on Transgender Athletes Severely Flawed
So, to a certain extent, the question of "should transwomen be able to compete female sports?" is an ideological question (i.e., "should identity supersede reality?").
That being said, there's a recent report [1], funded by the IOC, that is being used to "prove" that transwomen do not have a biological advantage over non-trans women. This report is severely flawed and does not actually lend support to the idea that transwomen have no biological advantage in sports over female people.
(I will mimic the language used in the report (e.g., using "ciswomen").)
Significant differences noted by the report that do NOT support transwomen's inclusion in women's sports:
Transwomen were substantially taller than ciswomen
Transwomen had more lean/fat-free mass than ciswomen
Transwomen had better lung function than ciswomen, as measured by forced vital capacity, forced expiratory volume in one second, and peak expiratory flow. (See the next section for a discussion on the ratio.)
Transwomen had greater hand grip strength (a proxy for overall strength measurement)
Transwomen had higher absolute peak power (lower extremity) compared to ciswomen. (See next section for a discussion on the relative measure.)
Transwomen had the same "absolute strength" as cismen
The data showing no significant difference between transwomen and ciswomen has substantial flaws:
The sample size was too small to reliably determine differences in bone mineral density
For lung function only the FEV1:FVC ratio was lower for transwomen, but the values are generally within the normal range for both groups. The impact of this difference is therefore questionable, as the transwomen have greater absolute values on each measurement and the ratio is not showing any abnormalities. In addition, the effect size (size of the difference) is much smaller than the effect size of the absolute differences described above. The conclusion here is simply that the participants do not have any obstructive respiratory diseases, and the transwomen have greater absolute lung function. (Although there are better tests for this.) There is also one outlier in the transwomen group that is likely driving this relationship in the ratio; unfortunately they do not perform the expected control analyses to demonstrate the retention of results without the outlier. [2]
The researchers decided to examine power in the lower extremities relative to lean/fat-free mass, which yielded a lower result for transwomen compared to ciswomen. However, this methodology make absolutely no sense. We have already established that transwomen have significantly greater lean/fat-free mass, and this paper is interested in determining equitably in sport performance. In general, sports aren't divided out by mass (and certainly not by lean mass), therefore we are interested in absolute differences, not in differences adjusted by some other factor. (Particularly not when that factor is established to be significantly different between transwomen and ciswomen!)
The same criticism applies to their analysis of cardiac function. But even more importantly, "the most crucial variable influencing VO2_max was not assessed in the present study" which is a significant oversight given the stated goals of this paper.
There are numerous other limitation and issues with this report:
This study is of "cross-sectional design, making it challenging to establish causation or examine if the performance of athletes changes as a result of undergoing GAHT"
"The athlete training intensity was self-reported. Therefore, the results may suffer from selection and recall bias." [emphasis mine] -> In other words, these results may be "comparing apples and oranges" with varying rates of fitness impacting the results.
"The athletes participating in the present study represented a variety of different sports, and this would have undoubtedly impacted the results of the study as different sports stress different training and sports modalities." [emphasis mine] -> This is a significant limitation, as comparing the strength of a ciswoman weight lifter to a transwomen distance runner (or vice versa) is meaningless. It's true that measures of fitness tend to correlate, but comparing across sport disciplines for highly competitive sports (where they are focusing on improving specific characteristics) distorts the results. (They explicitly note this: "Exercise type, intensity and duration all have an impact on physiological responses and overall laboratory performance metrics.")
"Social media recruitment leaves this study open to sample bias"
"The gender-affirming treatment of the transgender athletes was not controlled"
"The participants were not screened by a clinician before participation, and any medical conditions were self-reported"
The transwomen in this study all suppressed testosterone to ciswomen's levels and increased oestradiol above ciswomen's levels. This is a limitation because this degree of success in hormone suppression is uncommon, meaning that even these these poorly-supportive results are likely inapplicable to the majority of transwomen. [3]
There is a significant conflict of interest: this study was funded by the IOC after they had already changed the rules to remove the "hormone suppression" requirement [4]
All in all, this study is a classic case of researchers misrepresenting their data in the study's abstract. The data they actually collected shows that transwomen on hormone suppression maintain significant advantages over ciswomen. Further, the flaws in the study limit the applicability of their results.
---
In addition, there are other studies that contradict this result:
This review [3] discusses numerous sources describing "the inherent male physiological advantages that lead to superior athletic performance and then addresses how estrogen therapy fails to create a female-like physiology in the male"
This review [5] found "the performance gap between males and females becomes significant at puberty and often amounts to 10–50% depending on sport" and that "longitudinal studies examining the effects of testosterone suppression on muscle mass and strength in transgender women consistently show very modest changes, where the loss of lean body mass, muscle area and strength typically amounts to approximately 5% after 12 months of treatment. Thus, the muscular advantage enjoyed by transgender women is only minimally reduced when testosterone is suppressed."
This study [6] found that transwomen "generally maintained their strength level" during "gender-affirming therapy".
This study [7] found that all physical advantages were present after one year and that some are retained even after years on hormone suppression. They also specifically hypothesized that "gender dysphoria could stimulate the opposite behaviour [differences in exercise habits] in transwomen, decreasing push-up performance and explaining why transwomen performed fewer push-ups than [cismen] prior to starting oestrogen." This motivation difference likely won't apply to elite athletes, which further supports the idea that transwomen athletes should not be competing with female athletes.
As this position statement [8] indicates we know that there are substantial differences in athletic performance for male and female people.* However, there is little high-quality, definitive evidence concerning the effects of hormone suppression/replacement on people's athletic performance. The current state of evidence suggests that hormone suppression/replacement fails to bridge the physiological gap between male and female people, but we need further higher-quality evidence to definitively prove this.
(That being said, the burden of proof here is on the people attempting to initiate a change; that is equitably between transwomen and female people should be (have been) established prior to eliminating biological sex-separation.)
*Before anyone jumps on this: this is not a moral difference. There is absolutely no reason why running faster or lifting heavier things would make someone "better". The biological difference in performance exists, but it does not in anyway suggest superiority of men over women. Beyond that, it is unsurprising that men outperform women on traditional sports given that sports were designed by and for men. In sports that cater to women's physiological advantages (e.g., endurance, flexibility), women outperform men. [9]
---
So, given all this, what would we actually need to make determine transwomen's relative advantage over female people?
The "perfect" study would involve (at least) these elements:
Random selection from the desired population(s) of transwomen (e.g., top-ranked athletes in a specific sport, non-athletic, etc.) with matched (for population) non-trans female and non-trans male controls
Observation (not self-report) of activity level prior to, during, and following a standardized treatment (hormone suppression/replacement) initiation
Continual measurement of various physical and athletic performance, preferably with a range of laboratory (e.g., spirometry, body measurements) and naturalistic (e.g., actual sports competitions) tasks along with monitoring the treatment and clinical/health issues in all participants (again, not via self-report)
Large enough sample sizes to allow for sufficiently powered tests of all groups/differences of interest
A double-blinded assessment approach (or "placebo" controlled) such that both the researcher assessing the participants and the participants do not know what is being evaluated until the study is complete. For example, you may tell one half the transwomen participants that you are tracking the long term health effects of the intervention (hormone therapy), while you tell the other half that you are assessing differences in athletic performance as a result of the intervention. This will allow for the evaluation of demand characteristics like the ones impacting [7].
There are likely even more factors I have not currently thought of. Of course, completing the "perfect" study would likely be almost impossible. It would certainly be impossible to do for every population of interest (e.g., Olympic weight-lifters, adolescent track and field athletes, sedentary office workers) at the same time.
That being said, a study that fails to include all of these factors (particularly the blinded approach, matching of control participants, and sample size) is not going to meet the standard of evidence needed to make decisions of this magnitude (i.e., choosing to change the priority from biological categorization to ideological categorization). In reality, we would likely need many studies that individually evaluate each group of interest (e.g., transwomen olympic-level weight-lifters vs female olympic-level weight-lifters), each applying as many of the ideal study characteristics as possible.
In conclusion, the IOC has failed to perform their stated duty to regulate and ensure fair competition in sports. There is no current evidence suggesting that transwomen have lost their male-advantage in sports, much less any evidence suggesting they are at a disadvantage.
References below the cut:
Hamilton, B., Brown, A., Montagner-Moraes, S., Comeras-Chueca, C., Bush, P. G., Guppy, F. M., & Pitsiladis, Y. P. (2024). Strength, power and aerobic capacity of transgender athletes: a cross-sectional study. British Journal of Sports Medicine, 58(11), 586-597.
Al-Ashkar, F., Mehra, R., & Mazzone, P. J. (2003). Interpreting pulmonary function tests: recognize the pattern, and the diagnosis will follow. Cleveland Clinic journal of medicine, 70(10), 866-881.
Heather, A. K. (2022). Transwoman elite athletes: their extra percentage relative to female physiology. International Journal of Environmental Research and Public Health, 19(15), 9103.
“International Olympic Committee Issues New Guidelines on Transgender Athletes.” NBC News, 3 Jan. 2024, https://www.nbcnews.com/nbc-out/out-news/international-olympic-committee-issues-new-guidelines-transgender-athl-rcna5775.
Hilton, E. N., & Lundberg, T. R. (2021). Transgender women in the female category of sport: perspectives on testosterone suppression and performance advantage. Sports Medicine, 51, 199-214.
Wiik, A., Lundberg, T. R., Rullman, E., Andersson, D. P., Holmberg, M., Mandić, M., ... & Gustafsson, T. (2020). Muscle strength, size, and composition following 12 months of gender-affirming treatment in transgender individuals. The Journal of Clinical Endocrinology & Metabolism, 105(3), e805-e813.
Roberts, T. A., Smalley, J., & Ahrendt, D. (2021). Effect of gender affirming hormones on athletic performance in transwomen and transmen: implications for sporting organisations and legislators. British journal of sports medicine, 55(11), 577-583.
Pitsiladis, Yannis MMedSci, PhD, FACSM; Harper, Joanna MS; Betancurt, Jonathan Ospina; Martinez-Patino, Maria-Jose; Parisi, Attilio MD; Wang, Guan; Pigozzi, Fabio MD, PhD. Beyond Fairness: The Biology of Inclusion for Transgender and Intersex Athletes. Current Sports Medicine Reports 15(6):p 386-388, 11/12 2016. | DOI: 10.1249/JSR.0000000000000314
Ro, Christine. The sports where women outperform men. (2024). From https://www.bbc.com/future/article/20240731-the-sports-where-women-outperform-men
85 notes
·
View notes
Note
I don’t know if the prompts can be asking for more in stories you’ve already started, but I would love to see more of the Hero of Shadow and Wild Link interacting, or more on Abel’s heart attack in the HC AU, or more interactions with Zelda and Link after they had to get married (Golden Mercy? The Imprisoning War? Not sure what that one’s called). … Or basically anything involving hurt/comfort or Hyrule, honestly. 😂
I love your writing so much, thank you for sharing it with us! < 3
Hyrule snapped his fingers in front of his friend. “Wild!”
Wild blinked, flinching and taking a step back. “S-sorry—”
“You good? Was that another—I thought the meds—”
“No,” Wild shook his head. “I—it was—sorry, I just—he—”
Wild continued to stammer, at a loss for words. What was he supposed to say? He hadn't spaced out, he'd honed in, his mind had snapped with clarity, screaming at him and wanting nothing more than to run towards the stretcher.
That man—he was—
And he was having a—
"I-I just... need to sit down for a bit," Wild finally said, walking out of the ED.
Wild had yet to fully explain everything that had happened in his past. Everyone knew he had gaps in his memory, that he'd sustained a head injury, that it made him have absence seizures, but the cause of it... the people he'd left behind because of the aftermath...
How could Wild possibly ever explain? He'd failed in his mission, and it had gotten his entire team killed. He could never face anyone from his past, let alone his—
Castle Town had promised a new life, a new beginning, especially as memories had tried to piece themselves back together and make him want to run and hide all the more. If he told everyone... then there was no more running from it.
Wild buried his face in his hands, resting on an empty stretcher in the basement. His mind screamed with anxiety as his past caught up to the present, and his heart screamed with worry over his father.
This was a nightmare.
XXX
Fable looked over her room one more time. Ambu bag? Check. Suction? Check. Defibrillator? Check. She had her maintenance IV fluid set up, the plasmolyte liter set up, the wires for the cardiac monitoring system ready to go, chest tube suction at the ready, and her little trays had all the syringes, saline flushes, blunt tips, alcohol swabs, caps, lab tubes, and everything else she could think of prepared.
She'd chart stalked the patient while he was in the OR, and she'd already gotten report from the nurse. Forty-year-old male (oh he's young, Fable thought, used to seeing far older patients) presented to the ED via EMS with chest pain and shortness of breath, STEMI confirmed with EKG, and he was sent to the cath lab. There they found multiple severe occlusions and opted for an open heart bypass surgery rather than using stents, and off to the OR he'd gone.
The surgery had gone fairly straightforward from what she could see - he'd been on bypass for about an hour, and the surgery itself had been going on for about four. He'd gotten about 500 of cell saver, 2L crystalloid, and 1 RBC, and he'd only been defibrillated once.
Just as she looked over the chart again, roll call was sent out to the unit, and she gathered her thoughts as she went to the room, awaiting the patient. He arrived a minute or so later, and the room quickly filled with Fable, the charge nurse, the tech, another nurse, the anesthesiologist, the attending surgeon, the fellow surgeon, the respiratory therapist, the ICU attending, and the nurse practitioner.
Everyone slipped into different roles and tasks fairly easily and quickly. Anesthesia handed off to the RT, who attached the ET tube to his ventilator, the tech worked on putting chest tubes to suction and getting outputs, Fable assessed her patient and looked at what drips they were on (2 of epi, 4 of levo, 0.02 of vaso, 1.5 of Dex, 1.2 of insulin), charge took the admission note while the surgeons gave report and Fable listened vaguely, her other nurse was attaching the safe set to the arterial line to collect blood for labs and an ABG, and the ICU providers listened to the report.
Vasoplegia, not too much bleeding but enough to merit product, chest tube output was a little high but not alarming, and he was cold at 35.8. Fable asked her tech to get a bear hugger, and x-ray arrived to check ET placement as the surgeons finished report. Fable stripped the chest tubes alongside the surgical fellow before they all stepped out for x-ray. ABG resulted pH 7.33, pO2 107, CO2 38, bicarb 24, and lactate 3.1. Fable opened the extra plasmolyte fluid bolus up to try and help with the lactate, which was likely indicative that the patient was dry.
The surgery team left, and Fable remained to stabilize the patient. She and her charge nurse worked on detangling the lines while the tech covered him in a warm blanket. His blood pressure was within parameters, with a mean arterial pressure greater than 65, though his systolics were in the 120s, which was right at his upper limit, so she tried weaning the levo a little, going to 3 to see what would happen, before continuing to detangle lines, get a blood sugar for the glucommander that was determining the insulin levels to give him, and obtaining cardiac output indeces. His cardiac index was 2.8, and his systemic vascular resistance indexed for his body weight was around 2600. Good CI, a little higher on the SVRI end. Perhaps she should wean the epi too, assuming his MAP tolerated it.
After about an hour, Fable felt a little less overwhelmed, and she called her charge nurse, who had left the room a good while ago alongside the rest of the team. "Have we heard anything about family?"
"He has a wife and daughter," she replied. "But they're a fair distance from here, out in Hateno. I think last we heard they were making arrangements to get here, but it wouldn't be until tomorrow morning."
Fable glanced at the clock. It was almost shift change, so night shift would have to be the ones to wake the man up, get a neuro assessment, and then hopefully extubate him.
Nodding, she went back to work. She wasn't going to wean sedation until he was warm enough, so all she had to focus on right now was stabilizing him. His labs came back and his hemoglobin was a little low, and his two mediastinal and one pleural chest tubes collectively put out about 280mL of blood. It was still a fairly high amount, mostly evenly distributed (the meds were bleeding more, but neither exceeded 100mL for the hour), but not enough to think there was an active bleed that needed surgical intervention. Not yet, at least.
Overall, he looked pretty decent.
After another hour, one blood product later, Fable finally felt like she was starting to get everything settled. Her patient's temperature was normalizing, but she was twenty minutes from shift change, so she figured it was safer to let him sleep through report and then night shift could try to figure out weaning and bathing. His lactic on his repeat ABG was improving at 2.4, so they were likely addressing all the problems.
When a transporter walked by, IV pumps in hand, she noticed him pause in front of her room. She walked over to him. "Hey. Can I help you?"
The transporter, a young man with long blonde hair tied out of his face, jumped, a little startled. "Uh, hi. Yeah. Sorry. I just..."
"What room are you looking for?" she asked helpfully. "I don't need extra channels."
"Uh, these are for 4301."
"You passed it, it's back that way."
"Right," the man nodded, looking back in the room. "Right."
Fable waited a moment, and then asked, "Can I help you with anything else?"
"Is he doing okay?" the man immediately asked.
Fable smiled. "Yeah, he's looking pretty good, I think."
"Can..." the transporter swallowed, shifting anxiously. "Can I talk to him?"
"He's pretty sedated right now," Fable answered cautiously. "Why do you want to talk to him?"
The transporter sighed in defeat. "I... he's my dad. I... haven't seen him in a long time."
His dad? Her charge nurse had said he had a daughter, not a son. Though... looking between her patient and the transporter in front of her, the family resemblance was striking.
Well, she hadn't heard of any visitor restrictions for him. "Yeah. You're not on his chart, though - can I get your name?"
The transporter sighed, putting the supplies he'd been carrying on the counter of the nurse's station. "I wouldn't be on it. My family thinks I'm dead. It's complicated."
He—uh... what?
"My name's Link," he answered her nonetheless before entering her patient's room.
Link? Huh. That was...
Wait a second.
"Hey, are you one of my brother's friends?" Fable asked as she followed him into the room.
"Your brother?"
"Link. Likes to call himself Legend to differentiate," she replied with an amused roll of her eyes.
Link gawked at her. "You're Legend's sister? He never even said he had a sister!"
"You two are alike," Fable huffed. "He doesn't particularly want a bunch of people to know he's related to me. But never mind that. Go talk to your dad."
Link stood there a moment, processing the words, before he exhaled shakily and nodded. Fable moved to the computer, working on catching up on charting to give him some privacy but also keep an eye on things. This patient's safety was her responsibility, after all.
Link seemed almost timid to approach the patient, even though he knew he was sedated. He slowly slid his hand into the older man's, shakily and quietly saying, "Hey, Papa. I... I, uh... I-I..."
Fable glanced out of the corner of her eye, seeing the young man getting tearful, and she tried to focus on her work once more.
"I missed you," Link whispered. "I'm s-sorry... about... about everything."
She heard a sniffle, and then the transporter moved quickly out of the room, offering her a brief but quick thanks before disappearing.
Fable turned towards the doorway, and then looked at her patient uncertainly. That was... odd.
Sighing, she walked up to the man, brushing hair out of his face. "Buddy, your family drama sounds almost as crazy as mine."
#you ask skye answers#lovely webhead#don't worry Abel's doing fine lol#Wild on the other hand...#writing#lu in healthcare#lu wild#abel#lu fable
84 notes
·
View notes
Text


8GP5Jf0lcpE
#doctor and patient#head to toe assessment#physical exam#stethoscope#doctor roleplay#male body#cardio exam#health assessment#heart auscultation#auscultation#respiratory exam#cardiac examination#cardiovascular examination#cardio
103 notes
·
View notes
Text



Do you have anything to spare to help pocket pets in need? We had 5 expensive vet visits on Friday totaling 724.13
Tiny Whiskers Animal Rescue is a 501c3 small mammal rescue in Minnesota. We are entirely volunteer run. We typically care for over 100 animals at a time.
Blossom, Bubbles, and Buttercup are 3 mice who were an owner surrender. Blossom has an eye infection, Bubbles has an upper respiratory infection, and Buttercup (pictured) has a skin infection. All three are getting medicated twice a day and will likely need a recheck in two weeks to assess their progress.
Gaston is a 5 year old male guinea pig who has always had a funny breathing pattern. He’s never had any other symptoms of health issues, and has been vet checked before and cleared. However his foster felt he’s been acting a little off and this time our vet recommended radiographs just to be sure. It turns out his liver is MUCH larger than it should be, so he is getting two different meds for the next few weeks as well and then a recheck in a month to assess his progress.
Pancake was a 2.5 year old sanctuary rat at the rescue whose mammary tumors grew too large to be comfortable and had to be euthanized. We miss her dearly.
If you can help us cover these costs, please! Even $5 is an immense help.
Venmo: tiny-whiskers
PayPal: [email protected]
68 notes
·
View notes
Note
Help! I think my timelord has a fever? I can't tell 100% but they don't look good. Do I need a special thermometer to check? (Where do I buy/find one?) What do I do??
Gallifreyan Pyrexia
Disclaimer: This guide is not suitable for humans. Always consult your human medical people.
🌡️ Checking Temperature
First things first, you don’t need a special thermometer to check your Time Lord’s temperature—a human one will do just fine. Here are some key points to remember:
Every Gallifreyan will have their own normal temperature baseline, somewhere between 15-19°C (59-66.2°F).
This shouldn't deviate by more than 2-3 degrees.
If their temperature rises above 19°C (66.2°F), they could be suffering from hyperthermia.
📋 Recognising Hyperthermia
Hyperthermia occurs when their body temperature exceeds 19°C (66.2°F), potentially leading to heatstroke and other serious complications. Signs and symptoms include:
Flushed Skin: The skin may appear red and feel hot to the touch.
Sweating: While not as common as in humans, excessive sweating may occur.
Weakness: A general feeling of fatigue or weakness.
Dizziness and Confusion: Disorientation and dizziness can be significant signs.
Rapid Heart Rate: Increased heart rate can accompany the rise in temperature.
Nausea and Vomiting: Digestive upset can be a symptom of severe hyperthermia.
🏡 Home Treatment for Hyperthermia
If your Time Lord shows signs of hyperthermia, here’s what you can do at home:
Move to a Cooler Environment: Get them out of the heat and into a cooler, shaded area immediately.
Hydration: Encourage them to drink cool, non-alcoholic fluids. Water is best. Avoid caffeine.
Cool Compresses: Apply cool, damp cloths to their forehead, neck, armpits, and groin.
Fan Air: Use a fan to circulate air around them or gently fan them to increase evaporative cooling.
Remove Excess Clothing: Help them remove any excess clothing to allow their body to cool down more effectively.
🚑 When to Seek Immediate Help
Temperature above 19°C (66.2°F)
Unresponsiveness or severe confusion
Severe vomiting or inability to keep fluids down
Signs of shock (rapid heartbeat, low blood pressure, clammy skin)
You suspect Sepsis (Refer to the Guide Sepsis Emergency Response (SER))
🏥 Advanced Treatment Guide
If home treatments are not effective or the patient's temperature is rising rapidly, seek medical attention immediately. If you're in a TARDIS, the medbay has an automated interface that can guide you through these next steps.
📋 Assessment
Initial Assessment: Check vital signs, including heart rate, respiratory rate, blood pressure, and oxygen saturation. For a detailed scoring system, refer to the Guide Gallifreyan Assessment Scoring System (GASS).
Continuous Assessment: Continuously monitor body temperature and vital signs. Use an accurate thermometer capable of reading low temperatures.
🧊 Cooling Methods
IV Fluids: Start intravenous (IV) fluids immediately to rehydrate and cool the body from the inside.
Cooling Blankets: Use cooling blankets or pads to lower body temperature. Ensure these are set to a safe temperature to avoid overcooling.
Ice Packs: Place ice packs in the axillae (armpits), groin, and neck to rapidly reduce core body temperature.
Evaporative Cooling: Use misting fans and cool water sprays to enhance evaporative cooling.
💊 Medications
If deemed appropriate by a medical professional/the TARDIS medbay computer:
Antipyretics: Administer antipyretics to help lower fever.
Anticonvulsants: Administer anticonvulsants to help reduce risk of seizures.
Sedation: In severe cases, sedation might be necessary to control agitation and allow for more effective cooling.
🖥️ Monitoring and Support
Electrolyte Monitoring: Regularly check electrolyte levels, as hyperthermia can cause imbalances.
Cardiac Monitoring: Continuous cardiac monitoring is crucial due to the risk of arrhythmias. Refer to the Guide Gallifreyan CPR for reviving a Gallifreyan in case of cardiac arrest.
Neurological Checks: Regular neurological assessments to monitor for signs of brain damage or seizures.
Mechanical Ventilation: If respiratory distress or failure occurs, mechanical ventilation may be necessary. Follow the ABCDE Assessment Guide to quickly assess and treat a sick Gallifreyan.
🚑 Post-Emergency Care
Once the immediate threat is over, following up with a specialised Gallifreyan medic is vital. Your Gallifreyan might need specific treatments to fully recover and prevent future incidents.
Remember, while these steps provide a general guide, each situation is unique. Always prioritise professional medical advice when available.
Medical Guides
These are all practical guides to assessing and treating a Gallifreyan in an emergency.
📓|⚕️Gallifreyan CPR: Guide for reviving a Gallifreyan in cardiac arrest.
📓|⚕️Gallifreyan Assessment Scoring System (GASS): Guide for assessing vital signs.
📓|⚕️ABCDE Assessment: Guide for quickly assessing and treating a sick Gallifreyan.
📓|⚕️Sepsis Emergency Response (SER): Guide for identifying and treating sepsis.
📓|⚕️Gallifreyan Pyrexia: Guide for assessment and treatment of fevers in Gallifreyans.
Hope that helped! 😃
Any purple text is educated guesswork or theoretical.
More content ...
→📫Got a question? | 📚Complete list of Q+A and factoids
→😆Jokes |🩻Biology |🗨️Language |🕰️Throwbacks |🤓Facts
→🫀Gallifreyan Anatomy and Physiology Guide (pending)
→⚕️Gallifreyan Emergency Medicine Guides
→📝Source list (WIP)
→📜Masterpost
If you're finding your happy place in this part of the internet, feel free to buy a coffee to help keep our exhausted human conscious. She works full-time in medicine and is so very tired😴
#gil#gallifrey institute for learning#dr who#dw eu#ask answered#whoniverse#doctor who#gallifreyan biology#time lord biology#gil biology
33 notes
·
View notes
Text
The One That Got Away - Chapter Fifteen

Warnings: angst, injuries, fluff, flirting.
Words: 1.7k
Pairing: Firefighter!Dean Winchester x Female Reader
A/N: I didn’t have a beta for this, so all mistakes are mine.
You can catch up here!
My Masterlist AO3 Ko-Fi

“Try to get some rest,” Y/N smiled at her patient and exited the room, heading back to the main desk to see who was next on the list. In two sweet hours, she’d finish her shift and finally get some proper time off.
Jess’ premature departure meant she and all of the nurses on her staff had banded together to cover more shifts than usual as they waited for a temporary replacement to start. It had been exhausting, and Y/N was surprised at how quickly she’d fallen out of the habit of pulling a seventy hour week, but it was finally over. The new nurse had started yesterday, and normal shift service had resumed for her and her team.
There was another reason for her excitement: her date with Dean was in fourteen hours. Not that she was counting. Y/N had been disappointed they had to postpone their date last week, even more disappointed they couldn’t fit it in last week. However, these things happened, and Dean had been right; absence made the heart grow fonder. Not that she’d tell him that. He didn’t need the extra ego boost.
“Y/N”, Dr Ellen Harvelle said as she arrived at the check-in desk, ready to take another patient. “Got an emergency four minutes out. Someone from Firehouse 3 has been injured on a job. Normally I wouldn’t ask, but everyone else is tied up.”
“I’m on it, Dr H,” Y/N replied, trying to push down the dread rising from her stomach. Throwing herself into action, she gowned up and ran to the ambulance bay. Please don’t be Dean or Bobby. Please don’t be Dean or Bobby. Was all that was running through the nurse’s head as she swallowed the bile rising in her throat.
Sirens blaring and lights flashing, the ambulance screeched to a stop in front of them, immediately followed by the firetruck. Her heart pounded painfully in her chest, but the second Dean and Bobby jumped from the engine, Y/N exhaled deeply and relaxed.
“You good?” Ellen asked, and she nodded and jumped into action.
“What have we got?” Y/N asked, stepping up to the ambulance and waiting for the paramedic’s assessment.
“Castiel Novak, thirty-five, trapped by a falling beam from the ceiling of a burning building. He was found unconscious, breathing apparatus dislodged. Suspect the collapse of both lungs and damage to the airways from smoke inhalation. Compressions have been ongoing since he crashed about thirty seconds ago,” Jack spoke as he and Jo got the gurney out of the ambulance.
“Alright, Y/N, we’re gonna need to do a ride-along,” Ellen said.
“What can we do?” Bobby asked calmly, though his widened eyes showed his concern.
“We need to keep compressions going. Jack, do everything Y/N tells you. Guys,” she directed to the firefighters surrounding her, “on my say, help me move him to trauma bay three. Y/N? Whenever you’re ready.”
Y/N climbed on the gurney and straddled Castiel’s thighs. “Alright, Jack. On the count of three, pull away, and I’ll take over, okay?” she waited until Jack met her gaze and nodded his understanding before placing one hand on top of the other and clasping her fingers together.
“One, two, three!” Seamlessly, Jack pulled his hands away, and Y/N replaced them with her own, not missing a beat as she began pumping Castiel’s chest firmly.
“Let’s move!” Ellen ordered, and Dean and Benny stepped forward and pushed Castiel and Y/N into the hospital.

Having suffered a collapse of both lungs, a concussion, and damage to his respiratory system from smoke inhalation, Castiel was in a serious but stable condition. He was responding well to treatment, but the next twenty-four hours would be critical, and Y/N knew there would be a vigil of firefighters in the waiting room until he was out of the woods.
With her shift just about over, Y/N checked on Cas one last time and updated his chart before handing his care over to Kevin. She wanted to stay on and work a double, but when she spoke to Rowena about it, the red-head told her that she’d reached her quota of hours for the week and reminded her she’d already pulled two doubles this week and to go home before she fell down and she was the one lying in a hospital bed.
Closing her locker, Y/N threw her purse over her shoulder and let her hair loose from the uncomfortably tight and itchy bun it had been constricted for the past fifteen hours.
Making her way to the waiting room to give the firehouse her final update, she smiled slightly, seeing all the firefighters were no longer in their turnout gear. Jackets and helmets were no longer strewn all over the tables, chairs and floor. Y/N remembered from Pamela and Taylor that half of them would’ve taken the truck back, changed their clothes, and brought food back for the others before they would go back and change out of their gear.
“Y/N, what’s the latest?” Uncle Bobby asked as he saw her standing in the doorway.
“He’s responding well to treatment. His oxygen levels are coming up. There’s still a long way to go, but he’s definitely going in the right direction,” she responded.
“Thank you for everything you’ve done for him,” Uncle Bobby smiled and walked towards her. “Is your shift over, Princess?”
“Yeah, I wanted to stay, but-”
“You reached your quota again, didn’t you?” Bobby chuckled.
“Maybe…” Y/N grinned. “But, there were extenuating circumstances this week which have been resolved.”
“So, you’re telling me it’s not gonna become the norm for you to go above and beyond?” he smirked, his eyes twinkling as he teased her.
“I hope not,” Y/N smiled softly, her eyes falling on Dean, and Bobby grinned, hoping, just like his niece, that things would work out between the couple.
“You should say goodbye to him before you go,” Bobby told her softly. Y/N nodded and stepped tentatively towards where Dean stood with Benny and Charlie.
“Hey, sweetheart,” Dean smiled as she stepped beside him. “Thanks for what you did for Cas.”
“It’s nothing, just doing my job,” she lowered her gaze shyly.
“Modest much?” Charlie chuckled. “What you did was heroic!”
“Oh no, that’s not… I don’t… You guys are the real heroes here,” Y/N shifted on her feet, uncomfortable with the attention.
“Uh, can I talk to you? Outside?” Dean said, gently pushing her towards the door and she nodded gratefully at his timely rescue.
“Thanks for getting me out of there, De,” she giggled as they stepped outside.
“Well, Charlie is right about the modest thing. You’ve never done well with attention or praise,” he chuckled softly. “So, I hate to do this, but about tonight-”
“Hey, it’s fine, Dean. You’re where you need to be, and Cas is more important than our date,” Y/N said.
Dean smiled, grateful that she got it. Though he wouldn’t say Cas was more important than her, he was a higher priority right now. “Thanks for understanding, Princess. I’ll make it up to you.”
“You better,” she grinned.
“Cross my heart,” Dean smirked. “Now, your shift is over, Nurse Singer, and I think you should go home and sleep. You look dead on your feet.”
“Yeah. I feel like I could sleep until I’m back on shift!” Y/N chuckled.
“Well, if you don’t pass out for four whole days,” Dean laughed. “Call me when you’ve had some rest. Maybe we could rearrange our date?”
“I’d like that,” Y/N nodded and tried to suppress a yawn.
“Go home! Text me when you get there so I know you’re safe,” Dean said, kissing her forehead.
“Alright, I’m going! Keep me updated on Cas, please?” she responded as she stepped backwards away from Dean.
“You got it,” Dean smiled, watching her turn around and walk down the hallway.
“Hey, Y/N!” he shouted, smirking when she turned around. “Good morning, beautiful.”
“Good night, handsome,” Y/N grinned back before turning and continuing down the hallway.

Y/N spent her first day off sleeping for three to four hours, eating, watching television, doing chores for three to four hours, and then going back to sleep. During one of her awake times, she’d called Dean, and he’d happily let her know that Cas was officially “stable” and out of the woods. He’d be on his feet and heading home in no time.
They’d agreed to wait a few days before planning their date so Dean could be on hand to help Cas if he needed it. No doubt he’d be feeling the impact of the damage to his lungs and airways for a few weeks yet and would likely tire doing the most mundane of tasks.
Dean had apologised profusely and again promised to make it up to her, but Y/N convinced him there was no need, and she didn’t mind waiting a little longer for him.
“Absence makes the heart grow fonder, right?” she’d teased him.
“So they tell me,” Dean huffed lightly, suggesting just a hint of frustration.
“Come on, De. We’ve waited twelve years. What’s a few more days?” Y/N chuckled, trying to lighten his mood.
“Yeah, I know. Doesn’t mean I need to like it, Princess.”
“Aww, are you missing me?” she teased again.
“Yeah, I am,” he sighed, and Y/N’s heart ached.
“Well, I know Cas will be taking up a lot of your time the next few days, but you know where I am if you wanna come over for dinner.”
“If I can, I will, sweetheart,” he sighed again. “Just wish I could promise.”
“Then promise to give me the best second date ever,” she giggled.
“Now that I can promise,” Dean said, and Y/N could hear the grin in his voice.
“Oh, I know you will!” Y/N giggled again, and Dean chuckled softly.
“I gotta go, Princess. I’ll call you later?”
“Can’t wait! Bye, De.”
“Bye, Y/N/N.”
Next Chapter >>
Tags: @acitygrownwillow @akshi8278 @ashbatz @candy-coated-misery0731 @chriszgirl92 @deans-baby-momma @deans-spinster-witch @deansbbyx @deanwanddamons @duncanhillscoffeecups @foxyjwls007 @giggles1026 @globetrotter28 @hobby27 @hoboal87 @impala67rollingthroughtown @iprobablyshipit91 @jackles010378 @jamerlynn @jc-winchester @k-slla @kazsrm67 @kmc1989 @lacilou @ladysparkles78 @leigh70 @lyarr24 @maliburenee @michecolegate @mrsjenniferwinchester @nancymcl @negans-lucille-tblr @nelachu2423 @octoberclidan @perpetualabsurdity @roseblue373 @sandlee44 @sexyvixen7 @snackles87 @spnbaby-67 @spnwoman @stixnstripesworld @stoneyggirl2 @suckitands33 @synmorite @tristanrosspada-ackles @twinkleinadiamondsky @waters-2567 @winchestergirl1720
#the one that got away#firefighter!dean winchester x reader#au dean winchester x reader#tw: child abuse#tw: alcoholism#tw: physical abuse#tw: verbal abuse#firefighter!dean winchester#dean winchester x reader
90 notes
·
View notes