#pulmonary embolism
Explore tagged Tumblr posts
Text
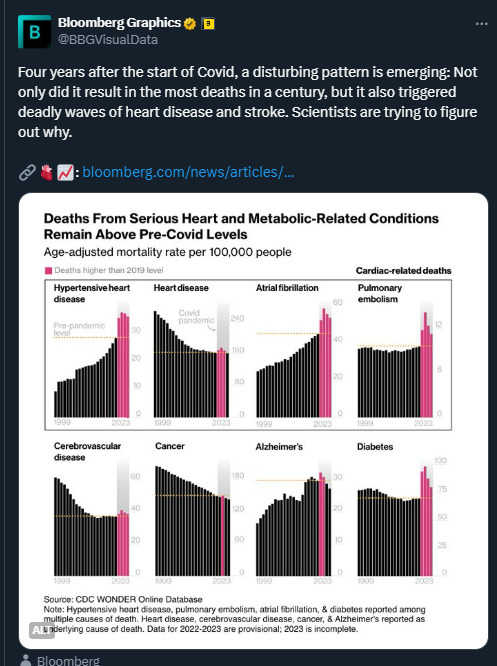
Statistics don't lie It just blows my mind that people can't see or understand that COVID is a dangerous virus that can damage your body. Getting infected multiple times will have serious consequences for many.
#covid#sars cov 2#long covid#heart issues#heart damage#diabetes#cancer#alzheimers#pulmonary embolism#atrial fibrillation#cardiovascular disease#hypertensive heart disease
253 notes
·
View notes
Text
Is it bad to feel angry at your dead mom cause she didn't listen to me when I told her to get something checked out. It was a blood clot. And it did kill her
Damn it if your family is worried about a medical thing like a blood clot listen for fucks sake. Your kid may be 19 but they still NEED you
And if you have a swollen area, especially if it's HARD, see a damn doctor IMMEDIATELY! Not six months later!
#grief#important#blood clots#pulmonary embolism#mom#mommy issues#anger#i punched the wall#grief and rage#loss of a loved one#loss of a parent#dead mom
10 notes
·
View notes
Text
Watch Out For Blood Clots in Your Lungs!
I already posted about this when my daughter died because she delayed going to the ER, thinking she had a respiratory infection. She died several hours later.
I just found out she had waited TEN DAYS.
But wait, there's more. Last Tuesday, the 3rd of September, my husband thought he had Covid and took a test. It was the first I'd heard that he had any concerning symptoms. He didn't want to worry me. (SMH...)
The test was negative. I said so wait, what symptoms are you having that you're concerned about?
It was then that he described what was going on. He would walk into another room and his chest would feel tight and he'd be out of breath and have to rest for ten minutes or more before he felt like he got his breath back. Now, my mind can go to heart problems because when I need another stent I can feel like that. I urged him to go to the ER. Now in American we often avoid the ER unless we feel like we're at death's door because it's a steeper copay. So finally I talked him into starting with Urgent Care, knowing they'd call the ambulance if the ER was the best place for him.
They did, indeed, call the ambulance. I had been waiting outside because even masked I'm avoiding exposure as a heart patient. They sent someone out to get me and I came in.
It was then I found out that he'd had symptoms for four days. Oh yes, we had a talk about that later. His blood oxygen level was in the 80s.
He turned out to have multiple clots in both lungs. (I have his permission to share this.) No sign of any clot in his legs. He's still in the hospital and will need some rehab.
When it comes to the heart they say time is muscle. There are similar admonitions to get in quickly if you're having a stroke.
THIS GOES FOR ANY ORGAN THAT HAS CLOTS. If a clot is obstructing oxygen to an organ, it's being damaged. If something as essential as breathing is obstructed, please get to a hospital.
If you're worried about copays, start with Doctors on Duty or an Urgent Care with your network. If you are completely broke, think about money vs. dying. I know; I've been uninsured too. Sometimes you can get retroactive Medicaid for that month if you end up temporarily disabled by whatever is about to kill you.
Four members of our family have had clots in their lungs. Three of four got help in time and survived. Covid has brought about an increase in clotting in various organs. Read up on symptoms.
Please just go. Your life is precious.
2 notes
·
View notes
Text
A friend of mine’s friend’s sister (i know its convoluted but i know its a real person and a real gofund me is the point) needs help with medical bills
18 notes
·
View notes
Text
I’m really not okay… 😭❤️🩹 My heart is exhausted 😩 How my weekend is going…
#i feel sick#heart attack#heart been broke so many times#pulmonary embolism#overworked#heartbeat#chains of heart
7 notes
·
View notes
Text
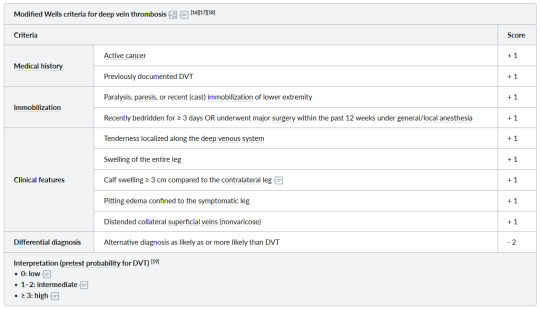
Wells Creteria for DVT and PE

2 notes
·
View notes
Text
Outline of hospitalization due to venous thromboembolism in the state of bahia between 2010 and 2020 by Wagner Ramos Borges in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
An important pathology that affects the cardiovascular system is venous thromboembolism (VTE), a disease characterized by the formation of clots in veins. VTE is divided into two clinical presentations: pulmonary thromboembolism (PT) and deep vein thrombosis (DVT). The general objective of the present work is to describe the profile of patients hospitalized for venous thromboembolism and other venous diseases, in the state of Bahia between the years 2010 and 2020. The specific objectives are the following: describe the demographic characteristics of hospitalized patients; describe the epidemiological trend of venous thromboembolism over the period. Based on data extracted from the SUS Hospital Information System (SIH/SUS), it was possible to analyze the following variables: annual frequency; race/color; sex; age range; health macro-region of the state of Bahia. Of the 21,450 hospitalizations for phlebitis, thrombophlebitis, embolism and venous thrombosis in Bahia, between 2010 and 2020, for patients from 20 years of age, it was noticed that 63.09% (13,533) are women, of which 42.14% (9,040) are self-declared as black or brown and that 43.39% (9,308) are concentrated in the East 2915 macro-region (NRS – SALVADOR). The profile of patients admitted between 2010 and 2020 was identified as being composed of brown women between 40 - 49 years old.
Keywords: Venous Thromboembolism; Pulmonary Embolism; Venous Thrombosis; Embolism and Thrombosis
Introduction
Diseases of the cardiovascular system have been seen for many years as important factors in the population's illness. According to data from the Ministry of Health, in 1999, such comorbidities led to approximately 1,100,000 hospitalizations through the Unified Health System 1. Within this scenario, Venous Thromboembolism (VTE) stands out, a pathological condition marked by the development of a clot in the veins, which leads to impairment of blood circulation.
The physiological changes that precede venous thromboembolism are grouped by Virchow's Triad, which encompasses endothelial lesions, stasis or turbulent blood flow, and blood hypercoagulability. Injury to the endothelial cell is a procoagulant factor, as it increases the expression of thrombomodulin, a thrombin modulating agent, stimulating platelet adhesion. Hemodynamic alterations, such as stasis and turbulence, by modifying normal blood flow, stimulate contact of platelets with the endothelium of vessels and reduce the elimination of coagulation factors, by decreasing flow. The state of hypercoagulability, which can have hereditary and genetic causes, also promotes an imbalance between clotting factors by activating procoagulant substances and inhibiting anticoagulants. two
VTE has two distinct clinical presentations, which are closely related: Deep Vein Thrombosis (DVT) and Pulmonary Thromboembolism (PTE) 3. DVT consists of the formation of clots in the deep veins of the lower limbs, which have the potential to reach the pulmonary circulation 3. This mechanism results in PTE, a condition marked by the migration of an embolus to the pulmonary circulation, which compromises the irrigation of this organ and is generally associated with a more serious situation 4.
Manifestations in Deep Vein Thrombosis are pain, heat, redness, swelling of the affected limb, cramps and, in some cases, greater predisposition to the formation of ulcers 2-5. The edema, due to the venous obstruction, is normally of the tense type, causing a swelling, only in the calf or in the whole affected leg. The redness, heat and pain at the site are caused by inflammation of the vessel wall. The pain may be permanent or be related to orthostasis or physical exertion, such as the Hormans Sign, in which the foot is dorsiflexed to assess whether there is severe pain in the calf 6. However, certain patients may not have symptoms or only some of them 5. Pulmonary embolism is characterized by distinct manifestations, namely: chest pain, usually of a pleuritic nature, tachypnea, dyspnea on exertion and in some cases cough 5. In more serious situations, dyspnea at rest, hypotension and syncope, due to low cardiac output and hypoxemia 5. Cases of pulmonary infarction are uncommon complications and, when they exist, are associated with extensive events and previous diseases or comorbidities, such as pulmonary infections and heart failure 7.
The diagnosis of venous thrombosis is complex, as no sign or clinical manifestation presented by the patient is predictive for confirmation or exclusion of condition 8. Thus, the patient is classified according to the pre-test probability (i.e. [suspected presence of a certain disease based on anamnesis, physical examination findings and epidemiology 9]) through validated risk assessment models for deep vein thrombosis or pulmonary embolism using the Wells or Geneva diagnostic criteria, which have similar diagnostic accuracy 10. These scores are important, as they eliminated situations of intermediate probability, dichotomously characterizing patients into situations of low probability (“probable PTE”) and high probability (“unlikely PTE”) 5,10.
This predictive model can be complemented using other tests such as D-dimer. Its values can be measured in whole blood or plasma, however it should be noted that complementary tests are only performed when it is not possible to confirm the suspicion of VTE with clinical examination, which occurs in most cases 11. As it is highly sensitive ( 95%) 10, but little specific (40%) 10 for VTE, its use is related to its high negative predictive value 5 (i.e. [probability of disease absence when the test is negative])9. Thus, if the result is negative, the diagnosis of VTE can be excluded in patients with a low to moderate pre-test probability of DVT or embolism 5. However, in situations where there are strong indications of a case of VTE , treatment can be started even without the results of complementary exams 12. Treatment consists of three main categories 13: medication (use of anticoagulants paying attention to the risk of bleeding 14) thrombolysis (through an injection of a substance into the bloodstream of the patient)15,16 and vena cava filter (the insertion of devices in the inferior vena cava, indicated for patients with DVT who cannot use anticoagulation)17.
Thus, the presentation of signs and symptoms, which are often nonspecific and common to other pathologies, as well as clinical diagnoses with specificity lower than 50%, lead to underreporting of the disease 18. As a result, knowledge of the disease is significantly hampered. real incidence of venous thromboembolism.
Due to this worldwide epidemiological problem, estimating the prevalence of VTE is a challenging task, and for this reason, the numbers are variable. In the United States (USA), for example, it is estimated that the prevalence of PTE is between 3.4% and 14.8%, while in Asia, this number is around 2.0% to 4. 7% 19. In Brazil, in turn, the numbers that characterize the epidemiology of VTE are also not very precise. According to certain references, the incidence of the disease is 1 to 2 episodes per 1000 inhabitants 18, while others describe it as 0.6 per 1000 inhabitants.20
The analysis of the relationships between VTE and different health variables also allows understanding the impacts of this disease on the Brazilian population. From an epidemiological study carried out at the Hospital das Clínicas of the Federal University of Uberlândia, MG, between September and December 2005, it was concluded that the most frequent risk factors found for VTE were prolonged surgery (85.2%), anesthesia general (46.2%), age equal to or above 60 years (42.3%), prolonged restriction to bed (27.4%) and age between 40 and 59 years (24.9%) 20. age and factors that promote immobility are crucial for the development of VTE. There are also the following variables intrinsically associated with the prevalence of VTE: obesity, increasing the risk by 2 to 3 times, in cases of BMI greater than 30Kg.m2; 21 neoplasms, with an increase in risk of 5 to 7 times 22; in addition to pregnancy (increase in risk by 10 times) and the puerperium (25 times).23
Objectives
Primary objective: to describe the profile of patients hospitalized for venous thromboembolism and other venous diseases in the state of Bahia between 2010 and 2020.
Secondary objectives:
Describe the demographic characteristics of hospitalized patients;
Describe the epidemiological trend of Venous Thromboembolism over the period
Methods
The present work constitutes a descriptive observational study of secondary data, extracted from the SUS Hospital Information System (SIH/SUS), available in the DataSUS database, referring to patients hospitalized in Bahia between the years 2010 to 2020, according to the ICD chapter -10: IX. Diseases of the circulatory system, in the category Phlebitis, thrombophlebitis, embolism and venous thrombosis.
The data obtained were then treated in Microsoft Excel software, where mean and median calculations were performed. This data can be verified through the TabNet portal, at the following access link: https://datasus.saude.gov.br/.
To describe the profile of hospitalizations, Venous Thromboembolism and associated conditions in Bahia, the variables used were:
Annual frequency;
Race/Color:
the White;
or Black;
the Brown;
the Yellow;
the Brown;
the Indigenous; It is
o No information.
Gender:
the Male;
the Feminine; It is
the Ignored.
Age range:
20 to 29 years old;
30 to 39 years old;
40 to 49 years old;
50 to 59 years old;
60 to 69 years old;
70 to 79 years old; It is
80 years and over.
Health macro-region of the state of Bahia:
the North;
the Center-north;
the Northeast;
the East;
the Central-East;
the West;
the Southwest;
the South; It is
the extreme south.
System
Public services
Private services
Results
Between 2010 and 2020, 21,450 hospitalizations for Phlebitis, Thrombophlebitis, Embolism and Venous Thrombosis were recorded throughout the state of Bahia, for patients aged 20 years and over. The macro-region 2915 East (NRS – SALVADOR) had the highest number of hospitalizations, totaling 9,308 (43.39%), followed by the regions 2910 South (NBS - ILHÉUS) and 2911 Southwest (NBS - VITÓRIA DA CONQUISTA) with 2,360 (11 %) and 2303 (10.74%), respectively.
There were also 880 deaths reported throughout the period, led by 2915 EAST - (NRS – SALVADOR) with 300 (Median (M) = 27; first quartile (Q1) = 23.5; third quartile (Q3) = 32.5) , followed by 2910 SOUTH (NBS – ILHEUS) with 123 (M = 11; Q1 = 9; Q3 = 14) and 2917 CENTER-EAST (NRS – FEIRA SANTANA) with 111 (M = 12; Q1 = 6.5; Q3 = 12.5). The trend of the curve in the period suggests stability, with an annual average of 80 deaths, with a peak of 97 deaths in 2019.
The general panorama of the period demonstrates a significantly higher number of women hospitalized for phlebitis, thrombophlebitis, embolism and venous thrombosis, so that of the 21,450 hospitalized patients, 63.09% (13,533) are women and 36.91% are men (7,917) . Men had M = 717, with Q1 = 692 and Q3 = 727, and women M = 1173, with Q1 = 1145 and Q3 = 1261, demonstrating the difference in the absolute value of cases.
The central tendency values also show the density of hospitalizations over the years, which indicates that there were no alarming fluctuations between groups or between individuals of the same sex, except for the year 2019. There were 2630 hospitalizations recorded, of which 905 were men (34 .41%) and 1725 women (65.58%), absolute numbers that differ from the general average, male and female, respectively, of 1950, 719.73 and 1230.27.
When evaluating the data according to the race/color criterion, of the patients who had this information collected, the black population stands out, since in this category self-declared black and brown patients are considered, which totaled 9,040 (42.14%) in the studied period , followed by the white population with 1027 (4.79%). However, there is a greater emphasis on patients whose race/color criterion was ignored, totaling 11,669 (54.4%) between 2010 and 2020.
The regime-based analysis revealed that the sum of hospitalizations for public services (7391) significantly exceeds those for private services (3564). The numbers of hospitalizations in which the type of regime was not registered were very expressive (11089). From 2010 to 2014, there were no records of hospitalizations classified as ignored. However, between 2016 and 2020, the nature of the regime was not distinguished in any hospitalization.
During the period in which the types of regimes were considered, the median number of admissions for the public regime was 1247.5, while for the private regime it was 611.5. During the same period, the average hospitalizations by the public and private regime were, respectively, 1231.8 and 594.
Distribution by age group revealed a higher incidence among patients aged 40 to 49 years, with an annual average of 404.18 patients. Then, the ranges from 50 to 59 years old (339.64) and 30 to 39 years old (327).
Discussion
Distribution by macro-regions reflects the impacts of disparities in sociodemographic factors, such as differences in income, access to health services, as well as the number of inhabitants in each region. According to the data obtained, the macro-region 2915 East (NRS – SALVADOR) stood out, in relation to the others, in terms of the number of hospitalizations, as well as the number of deaths (34%). This information is in line with results shown in the literature, which state that the Brazilian regions with the highest proportion of cases of VTE hospitalization (south and southeast) have the lowest mortality rate due to the disease 19. that, despite the disparities regarding access to health and income being important, the significantly higher number of inhabitants in the East macro-region (NRS - SALVADOR) was able to determine it as the leader in terms of the highest rates of hospitalization and death from illness.
The profile in relation to gender corroborates the literature, since women correspond to the majority of hospitalizations. Intrinsic factors may be favorable to this arrangement, such as the use of oral contraceptives, eventual pregnancy, puerperium or gynecological surgery, as well as greater search for health services by the female population compared to the male population 23, 24 . Regarding the use of oral contraceptives, although pills currently have a lower concentration of estrogen, especially ethinyl estradiol, their use increases the risk of VTE by up to six times compared to those who do not use hormonal contraceptives. The absolute risk, however, in women aged less than 35 years and without associated risk factors remains between low and moderate 25.
When analyzing the occurrence of this condition in relation to age, it is noted that the probability of involvement grows according to the patient's age, some authors consider that this growth is directly related to longevity, however the analysis showed that this pattern is not directly proportional to the age factor 19. In research carried out by other researchers, it is noted that from the age of 40 19 the occurrence rate increases considerably, with greater risk, but other authors consider that this occurs from 50 years 26. It is important to highlight that prophylactic methods are being developed with the objective of preventing the occurrence of DVT, since this is one of the causes of PE, a serious complication. Preventive diagnostic methods, especially in older patients and after surgical procedures, rely on tests such as: daily gammagraphy with fibrinogen labeled with I125 and Doppler ultrasonography, which is easier to perform, while the treatment uses anticoagulants, which have dubious efficacy. as they increase the chances of bleeding 27.
The body of evidence, including the results of this work, suggests that VTE is more frequent in the population of African ancestry 28. Epigenetic factors help justify this arrangement, such as obesity, which increases the risk two to three times, together with greater activity of the factor VIII in this ethnic group, which may favor thromboembolic events; 10% of healthy people have values above 228 IU/dl 29,30. However, the genetic basis of this increase in the population of African origin is still unknown.
During data collection, it was noticed that the studied MORB ICD-10 list does not distinguish notifications of phlebitis and thrombophlebitis from those of embolism and venous thrombosis. This bias may have compromised the analysis of the data obtained, by including phlebitis and thrombophlebitis in the analyzed variables.
Conclusion
Venous Thromboembolism is a recurrent condition in the in-hospital setting, and its complications are high-risk pathologies for the patient's health, with the associated risk factors being determinant for the patient's prognosis. The study indicates that the hospitalization profile in the Bahian population is mainly composed of brown women, aged 40 to 49 years. In the territory of the state, the Macro-region 2915 EAST - (NRS – SALVADOR) led the total number of assistances in the period. This secondary study, whose database comes from DataSUS, has limitations since it made them available from the grouping of four different pathologies into a single category, which allows data inaccuracy and impacts the epidemiological design of Venous Throboembolism in the population of Bahia .
#Venous Thromboembolism#Pulmonary Embolism#Venous Thrombosis#Embolism and ThrombosisJournal of Clinical Case Reports Medical Images and Health Sciences#jcrmhs
0 notes
Text
What Happens If You Inject Air Into Your Veins?
youtube
0 notes
Text
You were all love, nothing less. I'm struggling so hard with the loss of you. You loved me no matter what, I'll never stop missing you.
0 notes
Text
So, the blood thinners I'm on turn me into a puddle of weak ass can't do shit. I know they're currently keeping me alive and letting my body heal but I'm so damned sick of them.
And I have 4.5 months to go. Since I show no genetic predisposition for blood clotting disorders, it's very likely from having covid 3x.
There's an increased risk of blood clots having had covid once, sooooo.
But since it's idiopathic, they don't really know what caused my pulmonary embolism. So that means there's no easy answer and I may very well have to be on them for life.
I'm so exhausted all the time.
0 notes
Text
Clot Management Devices: Clot Management for Improved Treatment of Thromboembolism

The Evolution of Clot Removal Technology Clot formation inside blood vessels that supply the lungs, brain or other vital organs can have life-threatening consequences if not treated promptly and effectively. For decades, pharmacological interventions involving anticoagulant and thrombolytic drugs were the primary treatment approaches. However, these systemic therapies are not always fully successful in dissolving or removing clots, and carry risks of hemorrhage. In the past two decades, medical device technologies for minimally invasive mechanical removal or dissolution of clots have rapidly advanced. These clot management devices have revolutionized the treatment of pulmonary embolism and cerebral venous thrombosis. Catheter-Based Clot Retrieval One of the earliest and most widely used clot extraction approaches involves catheter-delivered retrievable stent designs. These devices utilize a nitinol mesh cylindrical structure that can be collapsed inside a delivery catheter and expanded upon deployment within a clot. Barbera first described use of the Tulip venous filter for retrieval of acute iliofemoral deep vein thrombosis in 1994. Building upon this, devices such as the Retrieval Inferior Vena Cava Filter and Denali Filters were developed specifically for clot capture and removal from larger veins. For pulmonary embolism, retrievable expandable stent designs like the Tulip Vena Cava Filter, Recovery Filter and OptEase Filter allowed for minimally invasive extraction of clots from the pulmonary arteries. A major advancement was the introduction of stent retrievers optimized forremoving thromboembolic occlusions from intracranial blood vessels. The Merci Retriever was among the earliest such devices approved by the FDA in 2004 for mechanical thrombectomy in acute ischemic stroke. Second generation retrievable stents like the Solitaire and Trevo devices featured superior design and deliverability profiles enabling higher recanalization rates. Recent studies support use of stent retrievers as the first-line treatment for large vessel occlusions in the anterior cerebral circulation. Ongoing research aims to expand the utility of Clot Management Devices catether-deployed devices to more distal vessel occlusions. Ultrasound-Accelerated Thrombolysis While pharmacologically-assisted thrombolysis remains a mainstay for selected patients, treatment times can be prolonged. Ultrasound energy has shown promise in accelerating fibrinolysis through mechanical fracture of clot structure and increased uptake of thrombolytic drugs. Devices generating low-frequency, high-intensity ultrasound via an intravascular catheter have been evaluated. Early studies demonstrated the EKOS System's ability to rapidly dissolve pulmonary emboli when infusing alteplase, halving treatment duration versus pharmacological therapy alone. The Sonolysis Thrombolytic Infusion Catheter was developed for treating iliofemoral deep vein thrombosis, administering ultrasound plus alteplase directly within the thrombus. More recently, the EkoSonic Endovascular System received FDA clearance for use in acute massive and submassive pulmonary embolism. Its small-profile ultrasound emitter works in tandem with front-line thrombolytic drugs to rapidly recanalize blood clots. Ongoing research also investigates combining intravascular ultrasound with novel thrombolytic drug formulations like microbubbles or plasminogen activators to potentially enhance and target fibrinolysis. Get more insights on Clot Management Devices
About Author:
Ravina Pandya, Content Writer, has a strong foothold in the market research industry. She specializes in writing well-researched articles from different industries, including food and beverages, information and technology, healthcare, chemical and materials, etc. (https://www.linkedin.com/in/ravina-pandya-1a3984191)
#Clot Management Devices#Thrombectomy#Blood Clot Removal#Vascular Surgery#Thrombolysis#Endovascular Devices#Stroke Treatment#Deep Vein Thrombosis#Pulmonary Embolism
0 notes
Text
A song thanking & praising God for healing "These Lungs" from Covid pneumonia, pulmonary embolism, softball-sized lung cyst and a collapsed lung!
Praise God!! 🙏🙏🙏
"These Lungs" Mr. Weaverface T-shirt available at the Official Mr. Weaverface Merch store. Right now until May 31, 2024, use code "20OFF" for 20% off anything in the store:
https://mrweaverface.com/store
Thanks for your support!!
#foryoupage #foryou #fypage #fy #christianrock #postgrunge #christianband #alternativerock #theselungs #covidlung #covidlungs #covidlungdamage #covidpneumonia #covidpneumoniasurvivor #jesus #healing #miracles
#christianrock#christianmusic#christianrockmusic#christianrockband#christianmusician#christiansongs#christiansong#jesus#these lungs#covidpneumonia#covid 19#long covid#covid#pulmonary embolism
0 notes
Text
I’m stressed out!
#health#mentally drained#heart attack#stress#hypertension#chronic illness#pulmonary embolism#heartdoctor
5 notes
·
View notes
