#of course i had to go an start LIKING neuropath
Explore tagged Tumblr posts
Text
Fun pathology things: spending the better part of 1.5 hours carefully sectioning and sampling an equine brain and spinal cord. I am going to get a diagnosis on this horse if it kills me (and it might)
#of course i had to go an start LIKING neuropath#like I'm excited to have a neuro case#but i did not accurately budget my time for this#pathblr#pathology#vetblr
85 notes
·
View notes
Text
Thess vs the Bank Holiday Blues
Currently doing the mental health evaluation and ... well, sometimes you just do everything you possibly can and you're still fucking struggling. Which fucking blows, thank you very much.
I've gone through the checklist. I've eaten. I've hydrated. I slept recently. Technically my "meds for neuropathic pain" are an antidepressant so I can't even say I need meds. As for therapy ... well, been there, done that, developed the coping mechanisms. But mental health-wise? I am struggling to cope at this point.
To be fair, this is largely external factors. This is the realisation that I was very much right about literally nothing changing in this country when we got a Labour government, because now they're saying, "Well, the Tories lied about the massive financial hole they left so we have to scrap all our infrastructure promises, cut the winter fuel allowance, and let the energy companies jack up their prices right at the start of autumn" and it's getting to a point where I wonder if they're just trying to kill the old people so they don't have to pay their state pension.
This is seeing some of the short-sighted bullshit going on in the US in the run-up to their own election. Because I know a whole lot about populist garbage and people making protest votes without thinking about what they're doing, okay? Our general elections here aren't the best example of it, but I have a better one - Brexit. We ended up leaving the EU for a few very simple reasons: a) populist wankers like Johnson and Farage lied through their teeth to win the racist vote; b) some people didn't really want to leave the EU but didn't like how the EU was going about things so voted leave in protest; or c) figured that Leave couldn't actually win and so didn't bother voting. Now, does any of that sound familiar?!? All you have to do is add d) third options that will never win but take the vote away from the sensible choice and you've basically got the US right now. And this country destroyed itself at least partly based on that one stupid badly-planned referendum. The US can't survive another Trump term, I can't actually do anything about the stupids that might allow Trump to take the election, and I have too many people I love in that country to be anything less than terrified. I know that my feelings are valid, I know I can't spend too much emotional energy on something I can't change, but still.
My situation is still not great. It's never going to be, and I know that, just because of circumstance. I guess it's just harder to keep from being depressed about my disability when so much else is weighing me down. I try to keep counting my blessings, because I have a lot of those. Still, no matter how hard you try, some days everything that's wrong seems so big that you're kind of stuck squished. That and probably the Bank Holiday Blues. I mean, I don't work Mondays anyway, but there's a different vibe to the world on Bank Holiday Mondays.
Right. I just need to take my mind off the blues. One of the blessings I can count is that my last therapist was basically the best. She didn't focus on the diagnosis as handed down from the psychs (which was almost definitely a standard "ADHD is often misdiagnosed as BPD in women" thing) and instead looked at my symptoms and my previous coping methods, and helped me hone them into something healthier. Some people would call what I do "avoidance" and "escapism"; I call it "therapeutic hyperfocus". I've done every healthy thing I can to improve my mood, so if the mood's still there, and hyperfocusing on, like, a video game or something keeps me grounded until it blows over, I do that.
Of course, then I have to pick which video game, but I do have a playthrough of BG3 that I am determined to complete, and nothing says "hyperfocus" like "game you've played a few times before but will still hold a couple of surprises because Dice Be Like That". And I deserve some fun after having had to spend most of Saturday in bed because migraine and exhaustion.
5 notes
·
View notes
Note
How would you go about approaching a doctor about possible chronic fatigue? I’ve struggled with very similar symptoms along with depression and most have told me it’s Because of the depression, so I don’t think they’ll be especially open to the idea.
I don't want to be a downer but you have to be prepared for the reality you'll be facing if you go to a doctor unprepared and unlucky: I'm afraid that your fears are very justified, most doctors and shrinks will insist it's ~just depression~ 😕
Doctors are usually arrogant yet ignorant lazy shitheads so patients like us have to do all the work for them but making them think THEY'RE the ones who came up with the answer, unless you luck out and run into a decent professional who bothers to test you beyond standard basic tests and believes you when you say it's something physiological. Due to that, my advice is researching yourself what the root of your chronic fatigue is before going to a doctor.
There's many disabled YouTubers who make videos about their different conditions and maybe you'll find someone whose symptoms you'll relate to a little too much. You can also seek online chronically ill communities to either ask around or lurk and learn. I've learned a lot from that. I have a tag on #chronic illness too, but I focus mostly on illnesses that I either have or suspect I might have, so you'll find few posts with detailed information of other illnesses besides mine.
To give you a headstart, I'll list you some illnesses that commonly cause chronic fatigue:
EDS: Check for it especially if your joints are very bendy and/or pop out of place often, if you bruise easily, scar abnormally, have bendy nails, velvety soft skin and dry eyes. Also, A LOT of EDS patiens (85%) are autistic or have ADHD, so if you have either of those, that's even more reason to look out for possible EDS.
Orthostatic intolerance: Most common form of it is POTS, but there's others such as orthostatic hypotension. Check it out if you feel dizzy/weak/faint when getting up too quickly, if you tend to hug your legs a lot for comfort, if you crave a lot of salt, if hot showers or hot humid weather in general exhaust you, and if you often experience heart palpitations especially after getting up or exerting yourself physically.
MCAS: Autoimmunity that expresses itself as dynamic/shifting allergies, migraines or recurrent headaches, fever-like symptoms, and food allergies. Unlike Mastocytosis (which can also cause chronic fatigue!) the problem here isn't an excess of mast-cells, but that the mast-cells are over-reactive and unpredictable, the "A" in "MCAS" stands for "activation".
ME/CFS: Check for it if your fatigue had a starting point. It's usually a post-viral illness, which means that a virus you suffered from wrecked your body in ways that threw it off either for a long time or permanently. Check if you get episodes of exacerbated fatigue after spending more energy than you usually can take (PEM), if you get flue-like symptoms out of nowhere and/or relatively regularly.
Fibromyalgia: It's more talked about regarding its neuropathic chronic pain (your nerves sending pain signals inappropriately), but it also includes chronic fatigue. Check for it if you get random numbness, if you experience chronic pain that makes it difficult for you to get proper rest and function. It also includes autoimmune symptoms (as does ME/CFS) so keep an eye out for that.
Thyroid issues: I'm not as knowledgeable on these, but I'm aware that these commonly have chronic fatigue as a symptom and these disorders are fairly common as far as chronic illnesses go.
Rheumatoid Arthritis: Another autoimmune illness in which the immune system attacks your body's tissue and causes inflammation especially in your joints. It comes with chronic joint pain that's experienced as stiffness and inflammation, and, of course, chronic fatigue.
Those are the ones I can think of right now, but there's many more. Keep in mind some of these have high comorbidity, EDS infamously gives you a 90% chance of having POTS and an 89% chance of having MCAS. MCAS and POTS also often are comorbid with ME/CFS and Fibromyalgia. EDS and ME/CFS also have comorbidity.
It's confusing as hell and that's why it's important to do thoughrough research. I hope this was helpful.
#if anyone reading this knows about more illnesses to look out for if one experiences chronic fatigue#please feel free to add them to the post
10 notes
·
View notes
Text
BROKEN TUMBLR ASKS PART ??: WHY DOES THIS WEBSITE SUCK SO BAD.
anonymous asked:
“For Buddie prompts: Eddie looking after a sick Buck?”
ooo, sorry, we actually all out of fluffy sickfics, here’s... this instead xoxo
“You’re exhausting.”
Buck hears the words ringing in his head as he clears another room, smoke swirling above him, his gear heavy on his frame. The chatter on the radio was drowned out by the roar of the flames, and it was about all he could do to keep an ear open for his name.
Kicking another door in, Buck has to grit his teeth to keep a groan of pain behind his lips, his leg throbbing—not for the first time that night. The screws had come out of his leg months ago, but that didn’t mean he was back to 100, not yet anyway; sometimes he just hurt. Neuropathic pain was something he could expect to have flair up until the wound fully healed—which could take years, according to his doctor, but...
“We all have our problems, but you don’t see us whining about it.”
But he was not about to bring it up, not about to risk... everything. His team was finally talking to him again. He was finally being brought on calls again. He could keep this to himself. He could go on without whining about it.
He had to.
Fuck, his leg hurt. Neuropathic pain was supposedly a dull, throbbing pressure, but all Buck could feel was fire, like a hot knife had torn him to the bone. Not for the first time, he only allowed himself a moment of “it isn’t fair” before he bottled all that down, gritting his teeth as he braced himself against another door, prepared to burst through the brittle, burning wood.
“Get clear, everyone. The building is getting too unstable—that means you, Buck.”
“Right, Cap.”
As if Buck would have risked disobeying another order, as long as he lived. He wasn’t about to let his problems become someone else's problems, never again.
“Somehow, we all manage to suck it up.”
“Cap, I have another resident down here!”
“Got it, Eddie. Buck, give him a hand.”
They were both on the ground floor, thankfully, and the screen on Buck’s wrist led him right to Eddie, who was trying to help an older woman up and out of her bed. It was becoming rapidly clear that she was going to need to be carried, and Buck didn’t waste any time in latching his arm with Eddies, hoisting the woman out of the apartment and bringing her out to a waiting gurney.
“Somehow, we all manage to suck it up.”
They may have been free of the inferno, but Buck’s leg was on fire. He had to make sure he was the last on the engine before they took off so no one would notice his unsteady footing, and he managed to pass off his groan of relief as a sigh when he sat down, feeling the sway of the engine as Bobby started to drive away.
They still had a good six hours left on their shift—God willing, they wouldn’t get any other major calls, and Buck could get some rest. All that he wanted was a shower and some sleep.
“Somehow, we all manage to suck it up.”
He managed to hide his pain with a smile as he de-geared with the rest of the team, always making sure that he was back far enough that his gait would be ignored, but not so far as to arouse suspicion. As much as he wanted to jump into the shower, he wasn’t sure how well he would be able to hide his pain if he had to bend over, or if, God forbid, he were to slip against the tile. He chose a bed instead—he probably still smelled of soot and sweat, but he was beyond the point of caring, and found himself obscenely thankful that the quiet room was on the first floor, and not up the stairs where the loft was. Buck was usually the last to sleep on shift, too busy being around everyone else, working out, anything he could be doing to absorb the companionship and company that came with a shared 24 hour shift, but… that was just another thing that the lawsuit had taken from him, he thought to himself, blindly propping his hurt leg with a pillow as he collapsed into the nearest cot.
“Why can’t you?”
Six more hours. He could make it six more hours.
--
Eddie was not having the best day.
Week.
Month?
He had been struggling, okay?
Part of him had hoped, maybe naively, that once the lawsuit was done, once Buck was back on the house, that… things would be back to normal. He had hoped that he and Buck could be back to normal.
Buck, obviously, hadn’t gotten the memo, because somehow, things were even worse than they were when the lawsuit was in full swing. Buck was still there, he was going through the motions, but that was it. Eddie should have known it would be too easy to hope for the easy camaraderie that there was before, but he had at least hoped they would be able to talk—even that was proving to be harder than pulling teeth.
In hindsight, of course, Eddie had realized that a good amount of the distance that had grown between them was his fault—he knew his anger had gotten the best of him when the lawsuit had started (hell, the near fatality in his little fight ring had proven that), and once it was wrapped up, it was still nearly impossible for him to look Buck in the eye.
He wasn’t proud of it, but that opinion really didn’t change until he realized what Buck had given up just to get back on the squad.
Millions of dollars. Millions. Eddie loved his job, but if someone offered him a chunk of change like that, he would have taken it and never looked back, but all Buck wanted to do was come back to his team—his family—and didn’t that just dig the knife in a little deeper?
Now, though, Eddie was determined to make it right. Even if it meant waking Buck up, dragging his ass out of the sleep room, and forcing him in to a family dinner with the rest of the squad.
“Buck, you up?”
Eddie could see the other male splayed outing a cot, his silhouette barely visible in the dimmed light. He felt bad about waking the other up—especially after how hard he had known Buck had been working—but the best time to start to apologize would have been yesterday, and today was just delaying the inevitable.
He took a few steps into the room and gently shook Buck’s leg, blinking in surprise as his hand touched dampness—was Buck sweating?
He pulled his hand up, examining it in the light from the doorway. It was… dark?
It was red.
“Buck?”
Fuck, it was red.
“Buck… oh fuck, Buck, oh fuck—“
Eddie felt his hands flying now, his voice kicking up as he spoke, throwing blanket and pillows across the room. Buck was pale, inhumanly so, and he immediately started checking for vitals as he started to shout.
“Buck, come on, wake up, Buck!”
Pulse was present, barely, thready and weak.
“Buck! Hen, Chim! Help! Buck, no, Buck!!”
--
It was a laceration. A cut, only a few inches long, along his leg, that had cut right through his PPE, and right through the first few layers of tissue in his leg. The doctor that had cleaned out the wound had pulled out shards of splintered wood, which was concerning in its own right; even though he was off blood thinners, the constant motion had kept the wound open, for… fuck, for what must have been hours.
Eddie didn’t need a doctor to get that confirmation. The blood that had pooled around the cot certainly didn’t come from a few moments—and even before then, the spatters on the floor, the soaked tear in the pant leg... it was more than enough to set Eddie on edge.
He had sent up a silent thanks to Carla, patron saint of child care, as he sat beside Eddie in the emergency room, patiently waiting for Buck to regain consciousness. No surgery required, thank God—just a dozen or so stitches, about three pints of blood, and a steady drip of pain medication.
And, okay. Maybe he was indulging himself, holding onto Buck’s hand as he started to stir once more, not bothering to hide the massive wave of relief that crashed over him when Buck started to stir again.
The pain-medication-laced smile that Buck shot him was one of the most beautiful things Eddie had ever seen.
“Hi Eddie!”
“Hey Buckaroo.”
He even sounded happy. God, Eddie missed that, seeing a shadow of his old Buck, the one who smiled and was happy and pain free, and it definitely disturbed him that he couldn’t remember the last time Buck had seemed so happy.
The moment wasn’t designed to last, though—as Buck started to take in more and more of his surroundings, his smile slipped off of his face, and it didn’t take the heart rate monitor amping up its speed to tell Eddie that Buck was starting to panic.
“Hey, hey, you’re okay, Buck. You just needed to get patched up and you’re going to be okay.”
“Fuck, Eddie, I’m so sorry, I didn’t mean to—”
Wait, what the fuck? “Buck, it was an accident. You’re okay.” He really hoped his voice was more soothing than confused, because Buck looked dangerously close to tears.
“It was an accident, Eddie, I promise. I swear I didn’t mean to, I was trying to be careful and I didn’t mean to get hurt, you can’t let Bobby kick me off the squad again, Eddie, please.”
Eddie felt like his voice might have been as raw as Bucks, shaking off the shock at that admission, moving to gently grip Buck’s shoulders. “Woah, Buck, we know you didn’t mean to. Bobby isn’t mad, he and the rest of the squad had to bring the rig back, they’ll be here soon, they wanna see you, and—”
“I just—I didn’t want to bother anyone, I know it’s exhausting trying to put up with me sometimes, so I didn’t want to—“
“Woah woah woah, Buck, slow down, you—you’re not exhausting, who the fuck even told you that?”
There was an auditable click as Buck shut his mouth, his eyes pained and his face bright red, and Eddie had a minute to look him over before reality came crashing around his head.
“…I said that, didn’t I? Oh fuck, Buck, you have to know I was just talking out of my ass, okay? I was just angry, of course I didn’t mean it.”
“But it’s true, Eds, I have to suck it up and deal with it, it’s not fair for me to lay all of it on you guys at work, and I’m sorry, but you can’t tell Bobby—it’s hard, but I’m getting better at it! I promise, I can’t lose you all again, please, I—“
His voice dies in his throat as Eddie pulls him into his arms, crushing him in a tight hug, and Buck can’t breathe, his eyes burning with tears as Eddie buries his head in his neck. Eddie didn’t speak until Buck finally started to hug him back, arms uncertain. “You’re not going to lose us, Buck. Never again. I promise, okay? You’re basically stuck with us until the end of time, I’m not going to let you go, and neither is Chris, and neither is the 118.”
The muffled sob that Buck let out into his shoulder told Eddie all he needed to know. They had all fucked up, hard, if that had been the looming fear behind all of Buck’s decisions lately. He had been self isolating from the team, he wasn’t cracking jokes, he didn’t even come up for family dinners unless he was specifically asked to—and while Eddie thought they had all just needed some time, Buck had been suffering in silence since he returned.
Fuck.
“Buck, listen to me. We are your family. We fight sometimes, and we all make mistakes, and I’m so, so sorry that we made this mistake, okay? But no matter what, we love you. Chim, Hen, Bobby, Mads, hell, even Athena, and... and me, Buck, we love you. I love you. So please, stop beating yourself up over it and just... let us love you, okay?”
Eddie reluctantly let go as he felt Buck start to pull back, his face contorted in fear and pain, but his expression started to smooth out as he nodded, the machine next to him beeping and whirring as his heart rate started to go down. The pain medicine couldn’t have picked a better time for another dose. Eddie started to ease him back onto the bed as Buck’s eyelids started to droop, only comforted by the even rise and fall of his chest.
"Thanks, Eddie...”
Eddie let out a short, wet laugh as Buck finally relaxed against the bed, treated to another smile before Buck slipped into unconsciousness.
“...love you, too.”
And Buck was out again.
Eddie didn’t even have time to process what Buck had said, distracted by the swoosh of automatic doors, multiple voices talking at once as the 118 poured back into the emergency room, officially off shift, and Eddie gave Bucks’ hand a squeeze—just one—before he stood up and left the curtained off bed, ready to face the team with the grim reality Buck had just tossed into his lap.
They had work to do.
But Buck... Buck was worth every minute of it.
#buddie#911#fic#evan buckley#edmundo diaz#hurtfic#fixit#kinda#flospeaks#anon#ask#prompt#buddiefic#911fic#like Katya says:#things are gonna get better#but first... they gotta get a whole lot worse.
239 notes
·
View notes
Photo

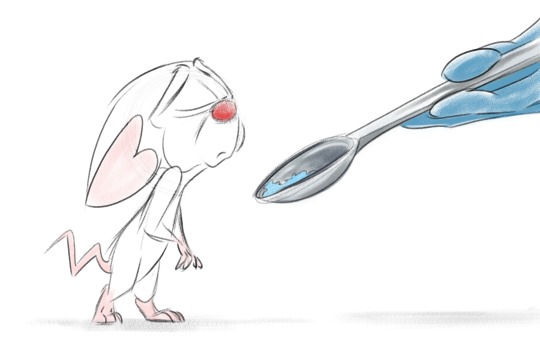
- PINKY AND THE BRAIN - EXPERIMENTS -
Below the cut is a personal project on the much more morbid side. Animal lab experimentation is always something I’ve found equal parts horrible and fascinating. Once in a blue moon, I’ll do research on the subject out of curiosity and/or for storytelling purposes. Even as a kid, I found this of interest, and when watching Pinky and the Brain I was always a bit disappointed that we never saw more of what the characters actually went through in the lab during the day. Granted, there’s a reason as to why this was never shown, as a child audience had to be kept in mind, yet still I pondered about it....
Over the last few days, I’ve been churning out compositions based on internet findings -- old and new experiments that rats and mice are put through, many of them humane, some of them very much not. It was an eye-opening journey for me artistically and otherwise, discovering what I’m comfortable drawing and what I never want to sketch again, as well as learning more about this realm of the scientific world.
WARNING: SOME GRAPHIC CONTENT BELOW THE CUT. If needles, patients dealing with the effects of cancer, and general portrayals of pain bother you, I wouldn’t bother venturing onward. I not only drew out experiments that the characters might have gone through, but also describe all of my findings in detail and provide video footage to go along with it. While I didn’t go full-on vivisection or anything, some of this might still be disturbing, so I’m taking extra precaution.
All of the images below are “color-coded” and graded. The experiments start out fairly tame, then get worse... and worse... and worse. The backgrounds reflect this, going from fairly light to quite dark.
-------------

Experiment #1 - Tail Flick Test
A fairly harmless experiment. The subject is mostly restrained, leaving only their tail exposed. An intense light beam is projected onto the exposed appendage, with the animal flicking their tail when the pain/heat becomes too much. This test is utilized in basic pain research and to measure analgesic effectiveness.
I wanted Brain to wear an expression of deep apathy -- he’s done this a million times and will probably do it a million times more. At this point, he doesn’t even care anymore.
For the background, I simply copied an environment in one of the videos I found.
Video example: https://www.youtube.com/watch?v=BzrA1tDTfkQ

Experiment #2 - Rotarod Performance Test
Another experiment that’s generally harmless. One or multiple subjects are placed on elevated rotating rods so as to measure such things as endurance, balance, grip strength, and more.
I imagine Pinky would enjoy this test, as he’s familiar with running on a wheel and actually enjoys more strenuous activities. Brain, on the other hand, would only participate via sheer force. He’d also be more prone to fall after a shorter period of time, getting tired faster than his cage mate.
Video example: https://www.youtube.com/watch?v=v56MtrmWAs0
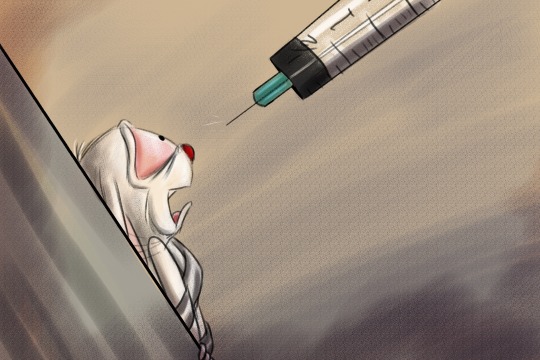
Experiment #3 - Shot (General)
Nothing special. Just Brain about to get shot.
This is all highly exaggerated, of course. A mouse would simply be held firmly, not strapped down, for a simple injection. Also, I can’t imagine why they’d be shot in the face, although Meg told me that scientists tend to draw blood samples from a mouse’s cheek. Need to look that up. I wasn’t at all going for accuracy here, but rather how it might feel -- how scary it would be.

Experiment #4 - Sciatic Nerve Constriction
An experiment in chronic neuropathic pain, due to the central or peripheral nervous system sustaining damage. Under anesthesia, the animal’s sciatic nerve is exposed via skin incision. The connective tissue between the biceps femoris muscles and the gluteus superficialis is cut. The nerve is then loosely tied with four chrome gut ligatures so to occlude, but not arrest, blood flow. The wound is sutured, the animal is given 24 hours to recover, and then both hindpaws are tested for pain sensitivity. Sounds terrible, but it’s certainly not the worst of the experiments I researched.
I have no idea what’s going on with the coloring in this. Again, going for feel more than accuracy, but the hues are way too calm.
Information link: https://www.ncbi.nlm.nih.gov/pubmed/22433911

Experiment #5 - Writhing Test
Particularly cruel test in which acetic acid is introduced into the system, inducing severe internal pain. The typical response includes writhing, abdominal retraction, and stretching of the hind limbs. Despite the test being withdrawn in 2004 for unethical reasons, it is still employed by some.
This was my favorite one to draw. Although the lighting and shading are not the greatest, it made for an interesting experiment. I did not intend for the lines to be so bold, but it kind of turned into an almost comic-style illustration. I ended up playing around with it a bit and like the result enough to post it.
I would not watch the video below if you are squeamish. It is difficult to swallow. On another note, you may find the “Empathetic Behavior: Emotional Contagion in Mice” section in the second link of interest. For cage mates in particular, if one or both mice were injected with the same acid, and allowed to observe one another, an injected mouse would writhe more if its partner was also in pain. I can’t help but imagine Brain and Pinky in this type of situation....
Information link #1: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3543562/
Information link #2: https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/writhing-test
Video example: https://www.youtube.com/watch?v=Ib63O4F856w

Experiment #6 - Transgenic K5ras Mouse / Nude Mouse (Combination)
Experiment in which cancer is induced in the system. Nude mice are bred for a number of tests, and are used for this one, as well.
My least favorite to draw, but my favorite to color. One particular experiment I found showed a tumor in every follicle on a mouse’s muzzle. Was trying to go for this look, albeit exacerbated.
Information link #1: https://www.cell.com/current-biology/fulltext/S0960-9822(98)70203-9?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0960982298702039%3Fshowall%3Dtrue
Information link #2: https://www.motherjones.com/politics/2012/08/weirdest-lab-mice/
-------
Bonus:

This is based on a test that I found absolutely hilarious. There’s a certain chemical, called W-18, that’s been on the drug market for... some years. The potency of it is supposedly insanely high, although this has never been proven. It’s basically a research chemical (created at a university in the 80s) with analgesic properties that were shown to be “painkillers or blockers of the painkilling effect of morphine in mice”. Mice, not humans. To quote a specific article:
“... when they first injected some of these chemicals into the animals at a dose similar to aspirin, the mice stood up for about a minute and fell over unconscious. They remained unconscious – for five days. But they weren’t dead. They were still breathing. And when they woke, they seemed fine, other than being really hungry and thirsty.”
They literally keeled over from the supposed potency of it. From what I recall, they don’t even know exactly what it was doing to their system, other than the fact that it knocked them out. I just find it funny that they were completely fine after awakening days later.
Although the pure smell of it wouldn’t cause such a reaction, I liked the idea of it in picture form and so depicted Brain simply taking a whiff before passing out.
Information link: https://www.forbes.com/sites/davidkroll/2016/04/30/w-18-the-high-potency-research-chemical-making-news-what-it-is-and-what-it-isnt/#2c45a5dd4757
-------------
Experiments researched, but not implemented:
- Tail dipped in ice cold water (mentioned here: cold water) - Morris water maze - Porton Down nerve agent test(s) (the worst; not even sure how I’d depict this)
The Porton Down tests sounded so indescribably cruel that I simply couldn’t bear to put Brain or Pinky through either of those, much less draw them out. It was the most horrific of the experiments I found, second only to a story about a French physiologist in the 1700s/1800s who performed, I believe, vivisection on live, six-week-old puppies. There’s a limit and that’s my limit. Even the cancer-based composition above was difficult to create. I legit felt dirty drawing it.
Researching these subjects was incredibly interesting, and I came across a few articles that touched on animal experimentation and the question of whether or not it’s ethical. Should such practices continue? It’s more complicated than a simple “yes” or no” answer. Some tests are fairly harmless, whilst others border on the inhumane, and some are downright cruel. Some people say that, without testing, there would be a lot less medicine on the shelves to assist in relieving and curing our ailments, whilst others argue that 90+% of the time the testing done is unnecessary, the results yielded by the subjects dissimilar to those that would be shown by humans and, henceforth, stating that the inaccuracies are numerous. This particular article offered up what I thought was a pretty genuine and interesting debate on the matter:
Pain in Lab Animals: How Much is Too Much?
In an interview with Dr. Jeffrey Mogil, a neuroscientist, he mentions that:
“You have complete control over everything in mice. Within limits, you can do whatever you want as long as you minimize pain and suffering of the subjects.“
Full interview: https://www.integrativepainscienceinstitute.com/latest_podcast/sex-differences-in-pain-and-pain-inhibition-with-dr-jeffrey-mogil/
While many establishments do follow the Animal Welfare Act, other laboratories still implement unethical practices. Also, the rules for what constitutes as acceptable in regards to tests that can only be performed without painkillers or anesthesia administered is... nebulous.
Thankfully, there is a number of lab testing equipment on the market specifically designed to be more humane and less stress-inducing to its subjects. These restrainers, for example, allow the animal to “walk in” without having to be physically forced backwards into a container:
Restrainers
Here is another example of testing that is relatively pain-free:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4401362/
It’s simple and inexpensive while still allowing scientists to perform tests.
Below is a video showing how a type of rotarod works, one that doesn’t place the rods too high and provides a cushion underneath in case the subjects fall:
https://www.youtube.com/watch?v=T38fDS2i13k
This tail flick analgesia meter comes installed with a cut off timer to avoid damage to the animal:
https://www.youtube.com/watch?v=JgaStZt143o
So there are options. How often are such options utilized in the field? I have no idea, although there are laws that should be followed and, from the sound of it, generally are adhered to. Not everyone in this business is cruel. Though you do have your occasional psychopath who performs very morally questionable operations behind closed doors, I believe that this is a great exception to the rule, and that there are a lot of laboratory workers who genuinely want to inflict as little pain as possible upon the animal. Just an opinion. I don’t have tons of evidence, but it seems like most people are sane. Lol.
Most of the experiments I inflicted upon Brain because, I think, Pinky is so pure that I have a hard time imagining him sustaining any kind of extreme pain that would genuinely hurt him. Also, he borders on being freakin’ masochistic, finding pleasure in a lot of painful situations, whereas Brain does not. Brain has been through a lot, mentally and physically. It seemed more... “appropriate” to put him in these situations, as terrible as that sounds.
All of that having been said, I never want to do this kind of exercise again. While a lot of it was interesting, and some of it even fun, parts of it were legitimately painful. The cancer one.... I felt horrible....
48 notes
·
View notes
Text
Hemp Joint And Muscle Active Relief Gel With Natural Ingredients
cannabis medicine and I've treated thousands of patients with medical cannabis in CBD over the years and this is where I share all of that knowledge with you so in this episode today we're going to be talking about CBD used for chronic pain so how can CBD help chronic pain conditions what kind of chronic pain conditions it helps with and which ones it may not be so helpful with and then we're going to talk about how to actually use CBD and the experiences I've had using high CBD types of hemp in medical cannabis with my patients with chronic pain so this is a question I get asked all of the time in facebook groups by email and of course with my patients is they really want to try to use CBD and usually in an oil forms of CBD oil for their chronic pain now there's some CBD oils that you can get over-the-counter in some countries that are from hemp and they don't have any THC in it or less than 0.2 percent THC so basically none and then there's the medical cannabis that really has high high high CBD low THC but does it a little bit of detectable THC in it let's say 1% THC so in my medical practice in Canada where medical cannabis is legal I use a lot of very high CBD very low THC oils to help patients with chronic pain now chronic pain it's a just a huge broad area of medicine because there's so many areas where pain can come from pain can come from the nervous system being injured and come from the nerves called neuropathic pain or nerve pain it can come from inflammation so if someone who has an autoimmune disease or they have arthritis from just wear and tear they can all get different types of pain and you have pain in the nerve endings and you have pain in the body and then you have pain that starts in the brain that's again something called central pain so with all of these different types of pain actually one of the most important systems in our body to manage pain is our own cannabis system in our body our endocannabinoids system so what this means is that when we are facing pain whether it's chronic pain or acute pain there's molecules in our body there's chemicals our body makes to help fight that pain and our body makes cannabis like compounds cannabis like molecules called endocannabinoids it helps to really regulate our pain perception how we kind of perceive pain and also how pain really changes the brain over time so a really common question I get is you know what should I do when I've already tried CBD from somewhere over the counter from a hemp store for example for my chronic pain and it didn't do anything does that mean that cannabis medicine in general and CBD in general it just can't help me the answer is usually no usually the answer is that it probably can be helpful somewhat but it really depends on the type of CBD the concentration of CBD it's different for every person in every pain condition and a lot of other factors like was it a full spectrum cannabis medicine product with lots of different chemicals in it besides the CBD or was a just CBD without anything else like a CBD islip what I find with a lot of chronic pain conditions is because CBD actually interacts with our own cannabis system in our own bodies called the endocannabinoid system it doesn't actually turn pain off directly like a painkiller for example what it does instead is it down regulates our perception of pain and the kind of tones our our nervous system so to speak so it can help with chronic pain over a period of time but often times it might take weeks or months to see in effect and it doesn't cure chronic pain so you have to keep taking it so what can happen with a lot of people is they start taking a very small amount of CS CBD oil and they don't really see much difference if anything oftentimes they have to use a different dose a different product or sometimes adding a tiny bit of THC so using in Canada for example where this is legal a strain of cannabis oil that has a tiny bit of THC and still very very high amount of CBD actually works better for chronic pain in many cases because it actually binds directly to some of the the pain receptors using the THC and then the CBD makes the THC work even better even at these tiny little doses so normally even at those tiny doses of THC people don't normally feel impaired or high so a lot of times people think that CBD oil is going to work directly for their chronic pain but again because CBD actually doesn't bind to either one of the cannabis like receptors in our body the cb1 or the CBT receptor like THC does it works in a more kind of overall toning capacity like a lot of herbal medicines it's all about really toning the nervous system and this is where CBD can be helpful over time there's also still so much we don't know about CBD and about the cannabis plant in general we're really only at the beginning of our scientific understanding and this is really I mean I mean when I say the beginning I mean I read the most up-to-date cutting-edge research every week on this topic and I'm still feeling like you know we're really at the beginning so that being said how can you actually use CBD if you have chronic pain well one way that you can use it is you can help use it to help decrease the anxiety that comes with chronic pain because what happens when you have chronic pain is in the back of your mind even though your brain gets used to having chronic pain it takes up so much bandwidth in your brain so much mental and brain energy to basically dampen the pain signals so you can just go about your life and not feel like you're in constant trauma that over time it can cause a lot of brain anxiety and it can cause a lot of fatigue so what I find seem to be helpful with when someone has chronic pain one of the ways there's many but one of the ways is helping to decrease the brain anxiety levels so basically it helps kind of calm their brain down which dampens the fight-or-flight response or you know the danger response system in the brain and that also dampens pain signals and it also dampens our pain perception because when you have chronic your nervous system is on edge all of the time it's like you're caught in this fight or flight running away from a saber-toothed tiger cycle all of the time and everything is heightened so your awareness of everything of sounds of smells of bright lights and of pain everything gets amplified so basically it just helps kind of calm everything down a notch and even in itself that's really helpful with chronic pain sufferers another way that can actually help chronic pain is if the chronic pain has an inflammation component so that's actually most types of chronic pain even indirectly if you have nerve pain sometimes there's an inflammation component as well so what CBD does in animal models we know and we think in humans although we need really bigger research studies to say exactly how this works but it's probably very similar to what we're seeing in animal models is that CBD actually works on inflammation through a number of different pathways in the body so it can shut down inflammation in some pathways so if pain is coming from inflammation CBD used daily over time may help reduce inflammation and that kind of pain as well another factor in many forms of chronic pain even if you didn't start out this way is the longer the pain goes on the nervous system tries to adapt to the pain and basically your own endocannabinoid system in your other pain control systems they get out of whack they just don't work as well and they kind of reach this new baseline this new kind of dysregulated baseline of I'm okay but actually the nervous system is really just regulated so this is where CBD may be able to help again because it may be able to help rebalance the endocannabinoids system when it's gotten out of whack so the last thing that I'm just gonna mention is okay what types of chronic pain do I see enjoy treat with medical cannabis and high CBD strains especially so I see quite a variety of chronic pain conditions one of the really interesting things that I've noticed in my clinical work with patients and this is not something that's really in the published literature yet is after someone's received chemotherapy for cancer in many cases they use different drugs that really affect numbness and tingling and burning sensations of burning pain the hands and the feet and this is kind of a neuropathic or nerve type of pain that specifically people get after a lot of chemo therapies especially the breast cancer chemotherapy regimens and what I've found is when patients use CBD oil after they finish their chemo and they keep using it their pain their burning pain in their hands and their tingling pain in their hands and their feet tend to tend to go away a lot quicker then I would say on average so it may be really a place specifically received II show some promise there's some animal studies on that type of pain specifically using CBD and we need more research to say exactly how it works in humans but it's really promising another type of pain that I treat is fibromyalgia I also treat arthritis pain and pain that's associated with a lot of other chronic diseases so I'm gonna talk about each of those in another video specifically but in general I think for chronic pain CBD holds a lot of promise especially when it's combined with other chemicals in the cannabis plant and potentially with other herbals and other medications so if you like this video please subscribe to our Channel and also please share this video with your friends and family who might benefit from it too and if you want more great free resources from me on CBD cannabis medicine and evidence-based natural medicine come over and join me on dr. Danny Gordon comm and sign up for our emails where you're going to get updates for me personally and exclusive content
1 note
·
View note
Text
Living With My 3 Best Friends - Fibromyalgia, Autism & Osteoarthritis
My Journey of Discovery
Written by Emma E. Threlfall

Although I was born with Autism or Aspergers (ASD-1) to be specific my journey of discovery along with that of Osteoarthritis (OA) and Fibromyalgia (FMS) didn’t really begin until my late twenties, early thirties. Around the age of 28 I began to show various and strange symptoms which I now know to all be a part of my Fibromyalgia Syndrome. At the time when they first began rearing their ugly heads they were so vast and varied I didn’t know whether I was coming or going. Let me list them for you here:
Hot flushes
Night sweats
Major fatigue
Swollen / Sore Lymph Nodes in my neck, behind my ears, armpits and even in my lower back (which is not pleasant as reminds me of the feeling when you wind yourself, if you’ve ever fallen on you’ll back you’ll know what I mean)
Headaches
Stiffness
Temperature dysregulation, once I get really cold I can’t warm up for hours and same for heat takes longer to cool my body down
Dull aches all over my body
Muscle cramps, anywhere on my body but mostly in my jaw and eyes
Skin sensitivity
Easily dehydrated - can cause headaches for days
Urinary frequency
IBS issues - constipation, diarrhea, colon cramps, back stomach aches, trapped wind
Poor short term memory
Word blindness - completely forgetting what I say as I’ve been saying it - loosing train of thought mid sentence and being completely to remember really simple words when you’re trying to say something (super annoying, and not the greatest during job interviews)
*Plus a load I’ve probably left out
It took me 5 or 6 years of various doctors visits, a hospital visit, an unnecessary laparoscopic surgery, a change of doctors surgeries, numerous blood tests, urine tests and finally going to a different doctor and bam I get a diagnosis after about 10 minutes in the consultation. The weight I felt lifting off me and just the fact that my now new doctor could just say ‘it sounds like Fibromyalgia’ (and just bare in mind there is no test for Fibromyalgia) was amazing.It then took me a few attempts but about a year or so ago my doctor put me on a medication (a controlled drug in the UK) that is actually an anti seizure drug but also has anti anxiety as well as anti neuropathic pain properties I take 100mg twice a day and I no longer have the pain I once had and it has helped so much with my fatigue which was just crippling. However this doesn’t mean I’m completely pain free I still get frequent headaches usually with my monthlys and also if I get stressed in the least little bit it can cause me to have a Fibro Flare with various symptoms of varying degrees. Fun or what?
At the same time all this was going on I was also starting with back pain, sciatic pain going down the backs of my legs a clicking in my back, and the tightest hamstrings in the world. I went for an X-ray and was told over the phone by the receptionist that I had ‘a little bit of osteoarthritis’ and that was that. I think at the time I was offered paracetamol for the pain, which of course did nothing.
So where does the Aspergers come into the fray, well like I mentioned early you are born with Autism and whilst growing up I of course I knew I was different but it wasn’t until I reached my teenage years that I really realised that I truly did have problems. I will list a few here:
Not being able to deal with change
Being a very anxious child / constantly worrying if somewhere I’m not familiar with
Can’t deal with confrontation or being told off
Prefer living in my fantasy world than living in the real world
Watching my favourite show or films on a a constant loop
Not quite comprehending what my peers were talking about
Feeling the need to copy my peers to make sure I fitted in / constantly feeling like an outsider
Being sensitive to the extreme causing me to go into meltdowns
Getting easily overwhelmed
Having depression and anxiety since being a teenager
Having few to no friends / finding it extremely difficult to make friends
Having extreme curiosity / always asking questions needing to know the how where, when and why
Not being able to ask for help at school or work
Not getting jokes / not knowing if people I don’t know well too well are using sarcasm or not
Mumbling when I talk with people I don’t know very well / laughing too loudly and not realising it until other people point it out.
Completely missing the point of homework (this may have something more to do with having a touch of dyslexia, as many people with Autism have)
Having major Social Anxiety / OCD and Agoraphobia
*Again there is probably many more things that I’ve left out.
However it wasn’t until I was 34 years of age that taking it upon myself and because the NHS was unable to (because of a postcode lottery) I paid £500 to get a private diagnosis of Autism, and having that confirmation just made everything, not easier but a hell of a lot clearer.
Why you might think am I writing about all three diagnoses here but its not just because I live with all three of them but because I believe that having Autism is the reason I now have to deal with OA and FMS, more on that to come in upcoming posts.
Just hope this blog helps shine a light on one or all three of these conditions for people. Just to note also these are things I’ve experienced so it may be slightly different for other people with these conditions as they can be as individual as the person who has them, so I’m purely writing this from my perspective, what I’ve encountered and come up against.
My journey is far from over and I’m discovering new things about my conditions all the time. For example I now also have to deal with Non-allergic Rhinitis, which believe it or not was making my Eustachian Tube in my in ear swell, that probably along with my TMJ (damaged jaw, but that’s another story), leading to me being a decibel or two deafer. I now have a steroid spray to reduce the inflammation - and it works I’m not as hard of hearing when I use that - awesome! Sorry just thought that was interesting but I digress. The point is where I am now at the moment I’m at my most equilibrium I’ve ever been at in my life, but that’s not to say a major life stressor could not really knock me off course and I am very aware of that and constantly try and find ways to keep myself calm on a day to day basis - again more of that in future posts. What I’m trying to say is getting a diagnosis is not a destination, there will never be a magic pill that gets rid of all your ills; having a conditions is like being on a continual journey of learning and discovery, educating and coping but where these type of conditions can feel like a life sentence, but they don’t have to.
#autism#asd#aspergers#fibromyalgia#fms#fm#osteoarthritis#oa#ocd#social anxiety#tmj#medication#rhinitis#outsider#depression#anxiety#diagnosis#diagnoses#deafness#muscle cramps#swollen lymph nodes#major fatigue#damaged jaw#agrophobia#noise filter#sensitivity#eustachian tube#asd1#repitition#night sweats
1 note
·
View note
Text
Rant coming up.
So some of you lovely followers, especially those of you who’ve followed me for a while, may have read that I have Complex Regional Pain Syndrome (CRPS).
The story behind this is that in 2015 I was in a psychiatric hospital, very unwell with psychosis, I believed I had bugs in my feet so I tried to cut my left foot off. Staff found me but I’d already gone through some tendons and a nerve. I had surgery to repair said injury. I returned to the psych ward, where over the next few weeks my foot got more and more painful inside the cast. The staff just said “well you tried to cut your foot off, of course it’s going to hurt”. They didn’t take me seriously. When the cast came off after four weeks there were two large, deep and smelly pressure sores from where the foot swelled up under the cast. I had to see the Tissue Viability Nurses twice weekly for dressing and cast change for 12 weeks. Eventually once they’d healed I was put in an orthopaedic boot. Two years later in 2017 I was diagnosed with CRPS.
So it’s now 2019 and in the last few weeks I’ve been in more pain than ever. Yesterday morning I woke up after a restless night in absolute agony. My best friend took me to A&E. The staff were lovely to me, I can’t fault the care I received. They put me in a new orthopaedic boot, and advised that I contact my GP to increase my new pain medication (Pregabalin) because it’s not helping at all. I’ve tried most of the other neuropathic pain medications. My GP was very kind and doubled my dose so I’m at the maximum dose now. I’m still in a lot of pain and I’m sceptical about the Pregabalin because the A&E doctor said that if it was going to work it should have kicked in by now, even on the lower dose. But I’m giving it a go. I’m seeing my specialist podiatrist on the 21st of this month and seeing the pain management team on the 18th of next month. If the Pregabalin doesn’t work by then, I’m going to have to ask about next steps. I can’t carry on like this.
This brings me to my next point. I literally can’t carry on. It’s affecting my sleep, which in turn affects my mental health. I’ve just started my new job and I’m finding it increasingly hard to do my duties because I’m hobbling around on two crutches, and now a boot again. I absolutely love my job and the last thing I want is to have to give it up, because I have worked so hard to get this far in life. Now I’m in the dreaded boot of shame again, the service users at work will all ask about my foot, and I have to explain that I haven’t “done anything” to it, it’s just part of my underlying condition (CRPS), but how do I explain that to vulnerable people with severe learning disabilities. Then there’s the staff. They’re all lovely, wonderful people but they’ll ask about it too and I hate the attention being on me. Also I worry that they think I’m exaggerating or fabricating how much pain I’m in because I don’t usually complain much, I just get on with it. I’m going to have to talk to my manager. She’s amazing and supportive and great but I feel like a wimp.
A family member said to me “it’s a Syndrome, which means it’s all in your head”. I told the A&E doctor and physiotherapist this, and they told me that that is a bogus and very outdated opinion. CRPS is a very real, and very debilitating condition. And it is. It’s affecting every part of my life.
I just want to be able to go for a walk without pain. To be able to go for a stroll and hold my boyfriend’s hand. To be able to carry my shopping. To not have to rely on lifts and taxis to get everywhere. It has been mentioned that I may be eligible for a wheelchair on the NHS but I don’t want to admit defeat. The person said that I should swallow my pride and just use one when I’m having a flare but meh.
If you’ve managed to read this whole post then thank you, I hope I haven’t entirely bored you. I guess I just needed to get it all out.
Hope you’re all doing better than me at the moment, stay golden x
@finding-mollies-marbles
#mental health#mental illness#psych ward#psychiatric hospital#inpatient#schizophrenia#paranoid schizophrenia#recovery#sectioned#CRPS#chronic regional pain syndrome#complex regional pain syndrome#chronic illness#medication#amitriptyline#gabapentin#pregabalin#flare#wheelchair
41 notes
·
View notes
Note
Why do you feel the need to exaggerate and lie about your illnesses? I don't doubt you're ill, but you just pick up every single disability going around. You're not blind or deaf, and certainly not paralysed. What's the point in lying?
Hi, are you my doctors? No? Then why do you feel the need to come here and do this every couple of months? I’m assuming you’re same person who’s been stalking me on here for the last year; if you are, I’m sorry for being an abusive shit to you, but I don’t know what you’re trying to achieve by constantly sending me anon asks yelling at me for being a fake.I’m so fucking tired of this; why do you think this is okay? What the hell do you want from me? I don’t know what to tell you, anon; either you’re doing this just to be an asshole, or you won’t fuck off until I hand you a diagnosis letter on a silver fucking platter.
Also, you do realise to get hearing aids (especially fully government subsidised ones), you don’t just get tested once, right? You do realise that getting an ophthalmology referral isn’t all sunshine and daisies, right? You do realise that spine issues are often degenerative, and also accompany EDS a lot, right?I have spent years trying to be as abled as I possibly can, and I am sick of it. It is exhausting. It is painful. I am done.
Or do you think I’m saying I’m profoundly deaf and totally blind? Because that’s not what I’m saying at all; deafness is a wide range of things, as is blindness.If it’ll sate your shitty attitude, I’ll explain my experiences medically with deafness and blindness, and you can ask another Australian d/Deaf / HoH and / or blind / VI person if I’m bullshitting or not.
It’s also helpful info for other d/Deaf / HoH and / or blind / VI and / or paralysed folx to have this information, so I’ll probably copy-paste it into its own post at some point.
Here’s how getting hearing aids under the Hearing Services Program, specifically the Community Service Obligation part of it (for folx under 26); you get your hearing tested, either through Australian Hearing or another audiologist (I went to the audiology clinic run by Melb Uni on Swanston St, on recommendation of my doctor after knowing I’m deaf for my whole life but just not having a diagnosis because “my child cannot be disabled in any way”, which is something a lot of d/Deaf / HoH and disabled folx experience). They a bunch of different tests; almost all of them are relating to pure tone (beeping noise), where you press a button when you hear the sound, often with various levels of static masking in your other(?) ear. Pretty sure it’s masking in the opposite ear; never figured that part out, even after four different tests in the last year. It sounds like it’s coming from all over.Some of the tests are about word recognition; I, personally, have about 70% in my left ear (with sound magnification), I think? It’s been a while since I got the number. I do pretty well, but they’re also single-syllable words that’re really clearly enunciated, so that definitely helps.Some of them are automatic, and you cannot fake these. These are mostly used for hearing aid tuning, in my experiences; example is when I went in a couple of weeks ago to get my new earmoulds and have them turned up, they did an automatic test to check exactly what needed to be turned up (my high ranges).So, after your initial test, if you’re not with Australian Hearing, they’ll transfer you to them; if you are, they’ll chat to you about what you want out of HAs, what kind of colours you’re after, etc.; I wanted Bluetooth, telecoil (for hearing loops), and nice colours. Sadly, I only got one of those things, and my audiologist is chasing down someone to ask if we can apply for new HAs already because we’re not meeting my goals for them—unfortunately, the colour thing isn’t gonna change though. I got white to make sure they’d be visible regardless of my hair colour, though I wanted this really nice light blue.Anyways, so they order the hearing aids, you come back a few weeks later, have another hearing test; this test determines the initial programming for your HAs, though they’ll be tuned here and there over the next few weeks depending on how well they’re working (or not) for you. This stage is the worst part of it, honestly.For me, I also had to go back and get my earpieces changed a few times because I don’t have the right kind of canals for soft tips, but I also don’t have the right kinds of canals for discrete moulds (plus, they’re uncomfy, imo), but it’ll heavily depend on your needs, the shape of your ears, etc.
I have visual acuity of 6/60 (20/200) + 1 I think; I can see, I just struggle to determine what the fuck I’m looking at unless it’s A) big, or B) I’m straining my eyes (bad for you!! don’t do this!!!). This is pretty common in blind / VI folx, as not every one of us can’t see anything; legal blindness and total blindness are different. I am legally blind (in Australia and the US, at least; not sure about other countries) and also have a near-vision classification of N18, which is moderate near vision impairment. I sometimes wear glasses to read, and it makes things a little clearer, but ultimately, it’s just more hassle than it’s worth to me, so I mostly just struggle and go without.With my distance vision, glasses stopped helping me a few years ago (I’ve been wearing them since I was ten), and I’ve been seeing optometrists a lot lately to keep an eye (ha) on it because it’s been getting worse, especially with floaters and little grey dots that occasionally pop into view; I’ve seen three in the last five or six months because of it. What optometrists can do is pretty limited overall, so at the most recent visit the optometrist just went “we can’t do anything, there’s no signs of retinal detachment or anything, you need someone with better tools”, so now I’ve been referred to the Royal Eye & Ear Hospital and am waiting to hear back from them.
Deafblindness also doesn’t follow the rules of legally blind.For someone to be Deafblind, it just means they’re VI and also Deaf; it’s dual sensory impairment, and how being deaf and VI intersect when it comes to interacting with the world around us. Not every Deafblind person is profoundly deaf and totally blind; it’s a huge misconception!So, no, needing glasses and being d/Deaf doesn’t make you Deafblind, but being visually impaired (”having decreased ability to see to a degree that causes problems not fixable by usual means, such as glasses”) and also d/Deaf does. It’s more of a cultural group than anything.Most commonly (afaik), Deafblind folx have Usher’s Syndrome, but not everyone does, and deafblindness can come from various things, both genetic and acquired; genetic stuff, of course, is luck of the draw. Having a connective tissue disorder did me no favours in keeping my sight—which was better than 20/20 when I was really little, by the way, so it’s interesting now thinking back about it. I’ve been losing my vision in “chunks” since I was about ten; not great, but it is what it is. I’m okay with it; I’m not afraid of it anymore, and that’s why I’m open about it now.
Now onto paralysis:Paralysis is a pretty broad term, and it doesn’t just mean “can’t move at all”, it can mean “can’t move well”, or “struggles with fine motor movement”, or plenty of other stuff; I have paralysis caused by spinal cord damage over the course of my life, as well as repeated herniated discs and spinal cysts, which has landed me in and out of hospital a lot in the last couple of years.For me, paralysis is I have hypertonia and struggle to move my legs, especially lifting them when I’m sitting or laying down; I had to talk to a neurosurgeon about this back in February and was told “if this gets worse you’re going to need spinal surgery” and proceeded to sweep that under the rug because let’s not deal with major surgery right now, thanks. I’m also now taking Lyrica to help manage the neuropathic pain I get from this; takes the edge off a little, so that’s nice.wrt my upper body, I have a lot of issues with trunk control and getting myself back up from leaning, especially to the back, as well as II also sometimes piss and shit myself because I often have moments of “wait, is this spine pain, or do I need to shit?” and just general struggles with holding it until I get to a bathroom (especially when I’m having to chase down security guards to get them to unlock the bathroom). Thankfully, it’s not an overly common occurrence, but it still sometimes is one.A lot of this is suspected to be caused by two bike accidents and someone (a kid) falling on me from two storeys up when I was nine, because I wasn’t the most self-aware child, but the rest is just chronic illness being a chronic illness and going “hey, remember me? I brought you more stuff!” (like the cyst).
Also, in case you want proof of anything:[ID: a pair of white hearing aids with red dragon stickers on them, connected to clear skeleton moulds, and sitting on a yellow cloth, inside a grey, vaguely egg-shaped box. Sitting on the bottom half of the box are two blue Post-It tabs reading “Go Fuck Yourself,” and “Anon”, respectively, in green marker.]
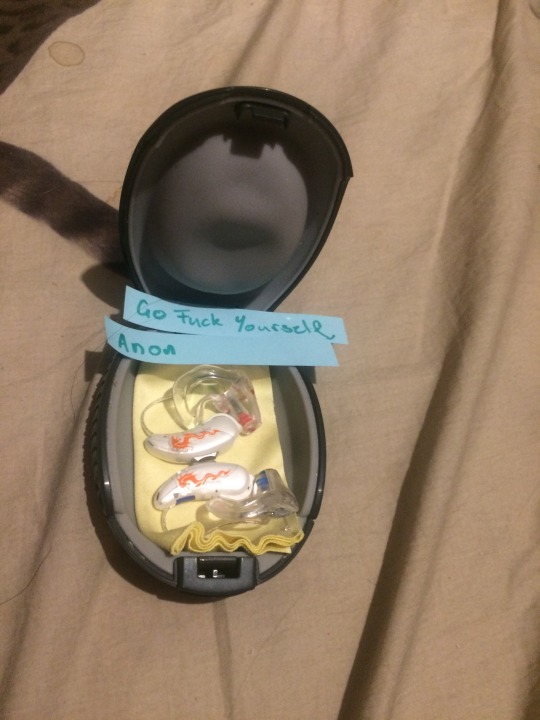
idk how you’d have me prove anything else, but this is a good starting point.
If you’d like to actually talk to me about this, I’m more than happy to, even if it’s from a throwaway blog, go ahead, I don’t mind, just please stop spreading harmful “gotcha” rhetoric; even if I was faking it, who’s the next “actually disabled” person whose disability supports get cut because of false accusations? Because it happens. People die from this sort of thing.
#answered#anonymous#anon hate tw#faking cw#gross cw#body fluids cw#ask to tag#don't reblog#//I'll make a lot of this into separate posts that can be#just not this one because good info should be shared without anon's scrutiny
10 notes
·
View notes
Text
Bad Days
Title: Bad Days
Gentle Rain Series
Author: Gumnut
8 Apr 2019
Fandom: Thunderbirds Are Go 2015/ Thunderbirds TOS
Rating: Teen
Summary: Em Harris has bad days.
Word count: 2064
Spoilers & warnings: Scott/Em
Timeline: Sometime after ‘Gentle Rain”
Author’s note: This is to celebrate Nutty injuring her back again yesterday. We all have bad days and Em more so than some. This is also an example of the fact that things are not always as rosy as they seem. I guess we’d all like a Tracy to come to our rescue sometime :D
Disclaimer: Mine? You’ve got to be kidding. Money? Don’t have any, don’t bother.
-o-o-o-
Em Harris has bad days.
There are days that start shitty and will likely end shitty. Days where she is reminded, that yes, she is paraplegic and look, now a double amputee to polish it all off. Days when the nerve pain gets her down. Days where the bare necessities of survival get ahead of her and existence just sucks.
At home, she would call in sick - her practise has back up plans for this exact reason - they’re doctors, they know the deal. She would hole up at home and just get through the day. If it got really bad, she had the visiting nurse to call. There were ways and strategies to get through the suffering and out the other side. Ways to rebuild her core, reinforce her shields and get herself back out there, usually with a smile to face the world.
It was necessary. It happened. She managed it.
But today she wasn’t at home. Today she was on a sparsely populated island in the middle of the southern Pacific.
She had woken to find Scott gone. This was nothing new. The man was a rescue operative, for crying out loud. IR had callouts around the clock. But the moment she gained consciousness, she knew it was going to be one of those days and just for once she granted herself enough selfishness to wish he was there to hold her and simply tell her it was going to be all right.
But she was Em Bloody Harris and she had been doing this alone for a long time. Get your ass out of bed and get the necessaries done, because not doing the necessaries of paraplegic existence really weren’t worth the neglect.
So she got out of bed and to the bathroom and did what she had to do. If there was a moment or two that found her cheek leaning against the coolness of the tiled wall, so be it. She had to get through this, so she would do it any way she could.
By the time she got through her routine, she was exhausted.
The irony of neuropathic pain was that while it damn hurt, it was all fake signals. There was nothing wrong with her beyond what was always wrong with her. It was just a seriously damaged nervous system doing its best to do its job when it couldn’t anymore. Pain was the result and days like today, it could get bad enough to break through her reserves and take her down.
So Doctor Harris downed some painkillers and prescribed herself a day in bed. Curling up under the covers, she closed her eyes and willed the day away.
Unfortunately she forgot to tell the Tracy family.
Sometime after no lunch there was a discreet knock on her door.
She blinked herself awake. She had finally managed some sleep, but her brain hadn’t let her fully escape, providing warped dreams where she was falling and Scott was desperately trying to catch her, but never quite fast enough. Her whole head had spun and it was only the sound of knuckles on wood that had stopped her plunge.
“Em?” Virgil’s voice. “Are you okay?”
Her head was full of cotton wool. The medication had the lovely side effect of dulling her thought processes along with her nerve pathways.
“Em?”
She opened her mouth to reply, but her body chose that exact moment to spasm and instead she found herself curled up working through a wave of pain. There may have been a whimper.
She didn’t hear the click of the door’s lock being overridden, but the voice exclaiming her name and the gentle touch to her forehead was enough to shock her brain into functioning at a bare minimum.
Virgil was crouched beside her bed, worry in every line of his face. “Em, talk to me.”
“Virgil, w-what are you doing in here?”
“Grandma was worried. It is unlike you to miss a meal, much less two. What’s going on?”
She closed her eyes and rubbed her face with a hand. “I’m fine. Juss a bad day.”
She didn’t want to look at him. Em Harris didn’t like vulnerable. Her medical status put her in that position far more often than she preferred and she put up with it, but this was new. This was her boyfriend’s brother, her boyfriend’s family, and to top it all off, Virgil was also one of her patients.
Vulnerability was not an option.
“I’m fine. I just need to get throu-“ And yes, her nervous system was the master of betrayal as it paired up the previous spasm with a lovely demonstration of exactly how bad, bad could get.
She grit her teeth and worked through the pain. Goddamnit, why did it have to hurt so much. The fog in her head wasn’t strong enough. She was due for another dose. She screwed up her face and tears leaked out of her eyes. A moment and she was gasping. Okay, okay, that one sucked. Where was her damned medication?
She opened her eyes to find a hologram of her own body floating above her.
What the hell?
“Em, what medication have you taken?”
“Wha?”
“I need to know what medication you have taken for your neuropathic pain.”
She pointed towards the bedside table and the bottle of pills. Red flannel danced in the shadows.
“I want you in the infirmary.”
“Virgil, I’m fine. I’ve got this handled.” She was so proud of actually finding her voice, she almost missed what he said next.
“Doctor Harris, the patient is in chronic pain, dehydrated and, no doubt, suffering from a low blood sugar level due to self neglect. Our infirmary has equipment that can help. I want you there and I want you there now.”
“I’m the doctor.” It was a stupid thing to say, but her reserves were shot and the thought of being paraded through the house on a stretcher sent chills up what was left of her spine. He would see her. See her injuries. See the real Em Harris. The broken mess under the facade. “No.”
“Em.” He sighed and she suddenly realised she wasn’t talking to Virgil, Scott’s brother. This was emergency responder and medic, Virgil Tracy. The man knew what he was doing. “Trust me.” The voice so many desperate people had heard in the most dire of circumstances.
As with many a rescuee, it worked. “Okay.” Her voice was so small, it was pathetic. So bloody embarrassing. She closed her eyes and hid her face behind her hands.
“C’mon, let’s get you out of that bed.” She couldn’t see him at that exact moment, but she knew he was offering her his arms.
So bloody embarrassing.
She pushed her self up, but, of course, today was a bad day so her body protested.
Loudly.
He caught her as she fumbled, scooping her up with a ridiculous lack of effort and held her close as she rode through it. She ended up gasping, her head on his shoulder, and she discovered he used the same aftershave her father had.
And then she was in tears.
Oh god. Em Bloody Harris bawling her eyes out all over his red flannel shirt. There were comforting noises, his chest rumbling with his soft voice. There was movement. She clenched her eyes shut, desperate to keep the world at bay.
And then he was laying her down on soft, cool sheets. There were beeps of medical machinery. The gentle touch of his warm hands on the skin of her back.
And the pain disappeared.
Oh god, the relief had her sagging into the bed. All her breath rushed out in a whimpered sigh.
Warm fingers brushed her hair out of her eyes. She looked up to find worried brown looking down at her. “Better?”
“Better.”
A small smile of relief flashed across his face, but then he was fiddling with an IV bag, hanging it far above. Exhaustion washed over her.
She didn’t feel the prick in her arm as sleep finally took her.
-o-o-o-
The next time she opened her eyes she encountered a pair of worried blue.
“Em?”
She swallowed. “Scott.” He was sitting beside her bed. She was in the infirmary. How?
Her brain finally decided to start functioning properly and memories lined up in all their embarrassing glory.
Shit.
“Uh, uh, uh.” His hand came down gently on her shoulder, holding her in place as she made to push herself up off the mattress. “You are staying here.”
“But I’m fine.”
A single arched eyebrow. “Tell me what happened.”
“Nothing happened. It was just a bad day.”
“That has you curled up in bed in pain.”
“It happens. I deal with it.”
His lips thinned. “Em, you’re not alone anymore.”
She opened her mouth to scoff at his words, but then their meaning sunk in and her mind jack-knifed.
Her hand was wrapped in one of his and she frowned at it. His other hand reached up and caressed her cheek. “We are not unfamiliar with the effects of injury in this family, Em. We help each other. Yes, there are bad days. We all have bad days. But those days pass better with help.” A ghost of a smile. “This family specialises in help.” He swallowed. “The thought of you hurting alone...I am so glad my brother is a stubborn ass who will chase up any member of this family hiding a damned illness. Please, Em, we’re here. There is no shame in asking for help.”
Her heart was in her throat. It had never occurred to her. She had not even thought about it. All she had seen was embarrassment and inconvenience. His fingers were so warm on her cheek. She closed her eyes and revelled in his touch.
No longer alone.
Oh god, it had been so long.
She bit her lip and was astonished to find herself holding back a sob.
Bloody hell, not again! What the hell was wrong with her today?!
His fingers brushed away a tear. His shadow fell across her eyelids and his lips touched her forehead. Whispered. “Think about it.” A smile against her skin. “I love you, Em Harris, and with me comes a large, bumbling family. You will never be alone again.”
His words had her eyes open and seeking to look at his expression, but he was too close and his lips were brushing hers, his hand in her hair. Ever, ever so gentle. Her gorgeous Scott Tracy.
She fell into the moment.
But he eventually broke it off and she missed his touch as he stepped back, sitting in the chair beside her bed, that still slightly smug smile of his knowing exactly the effect he had on her.
“Virgil says he is going to order a second TEEPS machine for you. Until then you can use Gordon’s as needed. Knowing Virgil, he’ll go and pick it up himself just for peace of mind. No doubt the second machine will be here before we have to worry about the both of you needing it at the same time.”
She blinked. “Why does Gordon need a TEEPS machine?” The thought of the cost of one, much less two, froze her brain for a moment.
“Ah, you’ll have to speak to Gordon about that. You’d be the first one to kill me if I divulged my brother’s medical information to you.”
Bloody hell, yes, she would be following up on that immediately. She had to know this stuff. What if she had to treat him? What if he needed her help? An image of the younger Tracy’s laughing face danced across her mind. Why did he need a TEEPS machine? She was almost terrified to find out.
But then she had seen Virgil’s medical records. Why wouldn’t his brothers’ medical history be any different? Her heart clenched.
“Hey, Gordon’s fine. It’s managed. And yours will be, too.” His hand tightened briefly on her arm. “Now, you focus on you.” And his hand was touching her cheek again. So distracting.
He leant in again. Another kiss.
Oh.
Perhaps he was right. Perhaps her bad days could be a little less bad. Perhaps...and her mind lost its train of thought as his tongue begged entry.
Oh god.
-o-o-o-
FIN.
#thunderbirds are go#thunderbirds#virgil tracy#thunderbirds fanfiction#scott tracy#em harris#scott/em#gentle rain#warm rain
23 notes
·
View notes
Text
Thess vs Representation
Again, I don’t really watch Critical Role anymore ... though now I’m feeling like I might at least try to start again. Again, because Taliesin Jaffe. Again, because his characters honestly make me feel represented.
Percy? TRUST ISSUES, and the lengths you’ll go to try to make it alone even when you obviously can’t, and the sheer joy of being able to trust again.
Mollymauk? Gender as a “You know, whatever” thing, trying to make someplace a little better than you found it even if it’s not the most socially acceptable thing in the world to do.
Caduceus? Asexuality mainly, but also appreciating the joys a new place has to offer, in a low-key way.
Ashton? Chronic pain, and how it’s easier to lie to yourself and everyone else about being an asshole than it is to say, “Sorry, I’m having a bad pain day and it’s harshing my mood” ... at least, for a certain type of person.
I appreciate that last when I find it. I always did, but I appreciate it even more now. When I had to get the cane, I felt better about it at least in part because Kaz Brekker. Then, of course, there’s Geralt of Rivia, and that’s good for both “I can get this done even if I hurt because it needs to get done” and “Okay, Geralt deserves a rest after a battle and so do I”.
Ashton? That’s a different kind of reassurance. Ashton is a D&D character. In a good group, where the players work together well, there’s a certain amount of ride-or-die in the found family that is a D&D party. While the other two characters I mentioned have this to greater and lesser extremes, Ashton is the best illustration of “My friends are going to love and support me even if I am something of an asshole, even if they don’t necessarily know why. Their acceptance of me is unconditional, and thus it’s probably safe, emotionally, to tell them that it’s just that I’m having a bad pain day and that I’m sorry. That is a vulnerability that I can afford”.
Ashton might not be there yet, given they only told FCG. But they did tell FCG, who’s been their companion the longest. Which means they’re getting there. And even from all the way over here, I am quietly cheering them on. Whether I watch or not, I hope Ashton feels comfortable enough to get the support they need one day.
Also ... it’s actually really nice to have a character in a RP situation that has a disability - something that can’t be magicked away without more effort than the average Cure Wounds. I mean, given Ashton’s whole appearance, I’m figuring that’s some significant neuropathic pain of the sort I deal with - a combination of the kind of trauma that sometimes triggers fibromyalgia and just ... y’know, brain damage. It’s nice to see magic with limits.
19 notes
·
View notes
Text
Medical rant ahead because the “headache department” at my hospital is an absolute headache, an essay by Me
So I’ve been getting injections for daily migraines, and they’ve had some not great side effects:
godawful neuropathy/sensory issues. If I wear certain pieces of clothing/come into contact with certain fabrics, it feels like my body is on fire/itching/just generally painful (and sometimes it even occurs when I’m not wearing anything, so that’s fun). I’ve experienced this before because of my fibromyalgia, but never this frequently (it’s daily) and never at this severity (it’s absolutely intolerable, I feel like I need to peel off my skin). So, understandably, my wardrobe has been dramatically reduced because most of my clothes (including all of my socks, except fuzzy bedtime socks, which is A Look™ in public lol) are having this effect. One way it’s impacting me is that I can’t wear any gloves, and it’s about to be winter which means it’s hella cold out already, and my hands lose a lot of mobility in the cold so I use gloves at warmer temperatures than most people (yay fibromyalgia). I’ve also become sensitive to my sheets/towels/blankets so that’s fun and not inconvenient at all *sarcasm*
I’ve also had a completely nonexistent libido. Which, like, okay theoretically isn’t the worst side effect in the world. But (without going into all the details) this is very unusual for me -- I’ve literally never lost my sex drive no matter how stressed/depressed I’ve been, and only one oral birth control has ever even dampened my libido. I’ve never had it be nonexistent. Ever since I went through puberty, it’s been sky high and super distracting (e.g. an orgasm away keeps the distraction at bay). So needless to say, I’m not feeling like myself at all, because I’ve known and dealt with my high-libido self since I was in 5th grade. At first I thought this was due to a recent breakup, but it’s persisted way longer than I would have expected and at a severity that I’ve never experienced from any kind of stressful live event ever. So it seems likely to be caused by the injections because A) the timeline matches up really well and B) it would be super unusual for my birth control to out of the blue randomly cause these symptoms, since I’ve been on this one for about a year and a half now and have never experienced this side effect.
I also get these weird stomach cramps that are worst during the first week after I get the injection, so I know it’s definitely connected. I probably wouldn’t mind if that were the only issue with the injections, because I could probably just suck it up and deal.
although the injections have reduced the severity of my daily migraines, the beneficial effects have worn off increasingly sooner with each dose. After only a handful of injections, this current dose lasted only two weeks before I was back to my baseline. So it’s not like it’s eliminating my migraines, and now it’s not even working as long as it should.
SO. I did the logical thing and messaged my neurologist explaining all of the above, with some more detail here and there. And her response to me was:
the pain/sensory stuff if probably just an allergic reaction. (That was literally the extent of her response on this. Just one single sentence. Which is concerning for a number of reasons, the foremost being that if this were indeed an allergic reaction, shouldn’t you be telling your patient how to manage it?! Like “hey take some benadryl” or “stop the injections immediately” but apparently the welfare of her patients isn’t a concern to her I guess?)
the decreased sex drive isn’t related
GI issues aren’t uncommon
Let’s maybe schedule an appointment to talk about whether or not you should continue these injections
I was a little peeved because I felt like she’d just brushed off my concerns (she didn’t even address the fact that my quality of life was being compromised but nbd I guess), and I felt like she wasn’t listening to me. But I figured she was just busy and wanted to get me an answer sooner, even if it was brusque. So this was my response:
The sensory stuff could definitely be an allergic reaction, but it seems more likely to be an amplified version of what I was already experiencing with my fibromyalgia considering that I literally already experience that symptom. Regardless, it’s causing an unsustainable way of life, so this needs to change @soon because I’m starting to get desperate, and I’m usually a pretty patient person about crappy side effects
Hi hello so I spoke on the phone with my Ob/Gyn, and based on my medical history and the evidence at hand (e.g. the timeline), we believe that this nonexistent libido is most likely caused by the injection. Just to give you an update.
(stopped talking about it because meh)
So I got a text reminder asking me to confirm the shipment of my next injection. Should I cancel it? Or should I stay on it until my next appointment?
And, kids, this is where fit hit the shan, let me tell you. Because her response. God, I can’t. The audacity. This is what she decided was an appropriate response for a CARE provider to give:
(NO acknowledgement about the quality of life/issues caused by the sensory issues. No compassion at all)
DIRECT QUOTE: “there is no evidence in all the studies that have been done, [sic] that shows [injection name] causes decreased libido”
(skipping the GI issues again)
Are the injections helping your migraines? (I LITERALLY ANSWERED THAT IN THE FIRST MESSAGE) Because my recommendation is to stay on them until our appointment in January, and at that time we can see if a change in medications would be beneficial.
There was a point in my life where a physician’s blatant disregard of my concerns would’ve hurt, but I’m apparently past that point. I’m just angry. Like what do you mean, “IF a change in medications would beneficial”?! Did you not read all the ways that this is impacting me? Did you not read the part where I need something to change soon because this neuropathic pain is making me lose my mind? Also, where the FORK is your compassion?? A patient is having really crappy side effects, and your best answer is “see you in January”? REALLY?! I would honestly cry if I weren’t so mad.
Also WTF was with “there’s no evidence about” your symptom that you’ve report. SO passive aggressive wtf. Like bitch do you really think my body gives a flying fuck about whether or not this symptom has been “established” as an Official Symptom of this (relatively new, btw) medication? Because the last time I checked, my body does whatever it damn well pleases and doesn’t read the literature on what it’s “supposed” to do. I’ve had side effects from medications that less than 1% of patients on those medications experience -- and if you actually bothered to read my patient file, MAYBE YOU WOULD HAVE REALIZED THAT. Also, chronically ill bodies are often complicated?? That’s not a surprise to anyone, especially for illnesses that we don’t know a lot about, like fibromyalgia, which I have??? And NEWSFLASH EINSTEIN, individuals are *gasp* individual and - guess what - can have individual reactions to things! What a WILD concept! It’s almost like everyone has a unique genetic sequence. OH WAIT.
And what really gets my goat is the fact that this is the first time she’s just blatantly ignored me/my patient history/my concerns. At the very first visit, I told her that I had chronic fatigue. We moved on to other topics and didn’t talk about the fatigue again. But what did I see in the after-visit notes? She literally wrote “fatigue appears to be from [Medication X].” Well guess what JACKASS. If you had BOTHERED to ask me if that were true/if I’d noticed a connection, I would’ve said absolutely no way in hell, because I started Medication X in May and I’ve been experiencing this bone-tired fatigue for YEARS (yes, years plural). But guess what, even if you didn’t ask me that, you could’ve easily seen it in my patient profile!! But apparently you’re an all-knowing God who is Always Right All the Time so who needs to ask patients questions or check patient histories!!
I cannot stand doctors with God complexes. I have 0% tolerance for that. I can’t handle these doctors who think that their MD somehow makes them Better Than You, and obviously they’re always the one who is correct, not you, because they’re the one with the degree so obviously your lived experiences are Just Plain Wrong.
If you are THAT arrogant and THAT uncompassioante (not a word but whatever), you should NOT be in a position where you’re dealing with patients’ wellbeing. That’s not okay. But of course, as long as we live in a society that sees becoming a doctor as prestigious/a money-maker, there are going to keep being doctors like this. And I wish someone would just take them down a notch, because, dear god, would it kill them to actually listen to and take care of their patients???
Anywho. That was LONG.
I hope to god no one read this entire thing, because if so, I apologize for that experience but also wow that’s serious dedication to this post (idk if I’d even read this whole thing lol). I just needed to rant this entire thing and this is apparently my virtual diary. And also having this all written down is going to be helpful for when my memory (inevitably) fails to remember all of these details
#tw asshole doctors#tw medical#so frustrated I could scream#like why are you even a doctor if you don't care about your patients#that shouldn't be a thing and yet here we are#growl#hiss#migraine injections#bad doctors#personal stuff#sorry for the rant
1 note
·
View note
Note
Like this is not in fact Twitch Plays Dragon's Lair, this was never your life course to direct anyway, even if I have been transcribing it in near real-time and further arcs will proceed from decisions yet to be made
Or is this the equivalent of yelling "don't go into the basement!" at the screen?
Like, back when I was originally like "oh, this is maybe displaced Issues from saving myself from choking once!" that doesn't really explain the later progression into physical symptoms or anything of that complexity in the first place and might suggest something dangerous still under the surface, okay.
But maybe I haven't been saying this clearly On Here but I'm increasingly attributing this to COVID, which would account for taking a massive hit to my nervous system in 2020.
Just at the start of the crisis, when it had first been spreading from Boston and Seattle a few weeks, when no one was wearing masks but they were disinfecting their groceries, I noticed I was feeling down for a week. I was still keeping a 3-week grocery stock so I didn't even go out, I just felt fatigued and noticed my senses of taste and smell were muted but I don't even know that was even recognized as a symptom yet, I just took it as a depressive period
Two weeks after that was when things really crashed, I didn't lose control of my self so much as my consciousness, it wasn't quite like a psychedelic trip but the experience helped. That was a month of crazy and when I pulled myself back together I noticed that individual functions I had heard of as recognizably alterable by physical (incl. chemical) means like "anxiety", "inhibition", and "emotional regulation" were also off
Also I was getting neuropathic tingling all up the length of my arms that I originally misattributed to some minor preexisting physical trauma – looking back I kind of question some of my judgment here, but then I suppose it was impressive my metacognizance held together that well at all
Then after 2 or 3 months the physical stuff degraded, I got like -3 or -4 DEX (or rather a -3 or -4 modifier, so -6 or -8) to the point of being unable to walk upright or manipulate objects with my fingers
But all of that has steadily gotten better since. With the "cigarette burn" gaps in my memory as the most obvious example, it appears that the nervous system that, you know, I run on took some widespread but scattershot damage following the passing of physical symptoms in 2020
That's something that, if not entirely explained, is at least well attested. Will it go on to hide in my nerves like herpes and recur sometimes? Who knows! Guess we'll find out! If it does, and that becomes a recognized thing, many initial "treatments" will be quack shit and even then the challenge wouldn't be paying $500 to a guy in an office who studied organic chemistry in college, but finding the right one! Doctors out there pushing ivermectin and— what was that one from 2020? Chloroquine?
In any case things have been all recovering as you would expect of someone with enough neuroplasticity remaining to patch the gaps, which like I said seem scattershot and distributed, weakening a lot but not enough concentrated damage to blow anything out of the water like you'd see with a stroke cutting off blood flow to one brain region
as a communist i should probably be okay that the guy who writes the brilliant but fashy-adjacent blog i read is refusing to seek medical attention regarding his serious neurological issues but jesus christ dude you really gotta see a doctor about this shit, its not normal and it doesn't become normal just because you're a smart dude who is analytical about your body
What exactly do you picture bringing someone who went to med school into the loop accomplishing here? It's like spraining your ankle: I might not be able to describe all the mechanics in detail but I don't need it diagnosed and there's not even really a treatment for it, I just take it easy while it heals
15 notes
·
View notes
Note
for the headcanon asks: the Master and all numbers. :3
prompts at: http://natalunasans.tumblr.com/post/163632792706/
OK so, for my version of S!M…
Something this character is truly proud of.getting along with Ten, and being trusted and needed by them.also, pretty much any cat anywhere in the universe is drawn to befriend him and he is proud of this, as anyone would be. ;)
Who they want to please the most. the doctor of course. mainly Ten. other versions… not so much (he always wants to make a good impression, though)he also eventually starts to learn to have friends… there’s Bill, there will be Donna… maybe others. he will want to make his friends happy, because that’s part of having friends.
Who depends on them. also Ten. they can’t sleep right without his dreamleading. they’re also less lost and chaotic with him there… as long as he doesn’t make things worse by hurting them. he’s slowly learning not to.Bill did depend on him while she was stuck in the Mondasian cyber-hospital, and at least he managed to keep her safe (see fix-it fic), which is more than Twelve did… she’s off on her own now, in London, but they still visit sometimes.
What they would do if they had one month to live. exactly what he’s doing now, because that could any time be true. hang out with Ten, invent stuff, eat good food, read, do music … just trying to have a life.
A cherished personal belonging.his gallifreyan tools: fob-watch (that he’s hacked to display the web of time since his time-sense is broken), his laser screwdriver that he finally got working again.his key to Ten’s TARDIS, which he wears around his neck always, it’s a symbol that the doctor finally accepts him and trusts him, as himself.
Something they lost, but would love to have backhis TARDIS. he does actually get her back, but i haven’t written that story yet, only the one after it (oops)
This character’s favorite characterzombies. he always identifies with the zombies in those shows and movies because he’s not supposed to be alive either. he likes either the stories where the zombies are the antagonists (he roots for them anyway) or those few where the zombies are protagonists like In The Flesh.
What kind of car they would drive.i know nothing about cars, but he would… and he’d choose something red and fast and expensive.
What calms them when they are upset.being sat on by purring cats, loud music, tactile stims like fidgeting with TARDIS key or his fobwatch or clothing textures. deep pressure (sometimes Ten’s hugs but could also be heavy blankets).
How they deal with pain.that could be a novel… maybe it already is.first resort is doing something to take his mind off it (music or electronics or other hobbies)if it gets bad enough, but before it gets too bad, he can ask Ten to do telepathic pain control.after he gets his TARDIS back, he can go in the zero room because his own TARDIS can help him more than Ten’s can… or is willing to.sometimes he has to take medications but he hates the side effects and it doesn’t work as well as telepathic pain control.sometimes there is nothing to be done and he just has to hide and wait it out. if his body shuts down, he may sleep it off.
This character’s favorite piece or pieces of clothing.anything soft. hoodies, scarves, worn jeans, broken-in boots… usually black, grey, red colours.
How they sleep.not much… but basically when his body shuts down he sleeps wherever and whenever.
What kind of parent they would be.TERRIBLE HORRIBLE NOGOOD VERYBAD please do not give this person a kid (to be fair, this is the same i would answer about myself too)
How they did in schoolreally really well, but never quite matching the amount of effort he put in (opposite to the doctor, who managed to goof off and still succeed)
What cologne or perfume they would usenone, now, because chemical sensitivities, but he used to in other times and other lives. he kind of misses smelling good.
Their sexualityaromantic or wtf-romantic, probably demi and bi i guess(?)
What they’d sing at karaokeanything loud. probably those songs from LotTL (voodoo child, i can’t decide, etc.) for old times’ sake… maybe something from placebo or the pogues
Special talents they havegenius-level at telepathy and engineering, good at music, pretty good at art/handcrafts. very good at organising/tidying (which gets a workout because of the doctor’s infinite chaos & hoarding)
When they feel safestcurled up in bed with the doctor behind him and the doctor does the whole-body hug thing…it kinda hurts (because neuropathic pain) but it feels very very safe
Household chore they hate the mostcooking (he’s terrible at it; he never learned)
Their fondest childhood memoryhim and the doctor running around in his father’s lands on Gallifrey, innocent and free, when the whole universe was in their future.
How they spend their money.presents & hobby supplies
What kind of alcohol they drinkwhiskey? idk much about alcohol, but he would. even though it only works on Gallifreyans if they will their body to react appropriately to it, of course sometimes he would will his body to get drunk.
What they wish they could change about themselveshe has a lot of confusions still about identity. he doesn’t like the idea of having changed his habits, even though he’s happier now that he’s not trying to hurt people (especially the doctor) all the time. he has also turned all his ambitions of control towards trying to manage chronic pain but that’s still kind of embarrassing because he still has a lot of internalised ableism to figure out. basically he misses being a normal villain because it was simpler and neater than being a person. trying to be a person is very messy. it’s not that he wants to go back, because he’s all about adapting and moving on… but this new reality is just… still a bit strange.
What other people wish they could change about themMOOD-SWINGS.probably that whole amorality thing… some people probably wish he could change his past, but that’s silly. there’s reasons we have rules about that…
#simm!master#dw headcanons#disability headcanons#neurodivergent headcanons#tenth doctor#supergranularqueer#spoonie!master#natalunasans writes stuff#ask meme#best enemies#wonder what i'd be without you
8 notes
·
View notes
Photo

New Post has been published on https://fitnesshealthyoga.com/its-a-fentanyl-crisis-stupid-national-pain-report/
It’s a Fentanyl Crisis, Stupid! – National Pain Report
By Kaatje “Gotcha” van der Gaarden, PA-C, MPAS.
Editor’s Note: This story was originally published on Dec 17, 2018 on Medium Health.
Featured Image: TEDxABQ 2018 “A Working Parachute: spinal cord injuries, ketamine & comedy” which turned into a 9 min stand-up set! Photo credit Allen Winston Photography
In 2012, life was great: I proudly wore a white coat with a stethoscope around my neck and finally felt useful to humanity. Two decades earlier, as a stuntwoman, my parachute did not quite open, and I landed on my sacrum (tailbone) at 70 mph, crushing the sacral nerves. I had lost two inches of my spine, fractured several vertabrae, and would spend a year in ICU, hospitals, and a spinal cord clinic. I was left with traumatic cauda equina syndrome,¹ suffered from residual pain, and was left with a “sitting disability.” For my atrophied lower leg and foot muscles, I used leg braces, a cane or scooter and I sat on a padded office chair. I’ve schlepped pillows and camping mats with me ever since my skydiving accident. Frequently, lying down for a few minutes was the only way to deal with my disability.
Kaatje “Gotcha” van der Gaarden
As a Physician Assistant in primary care, I loved my job and providing a true provider-patient collaboration. I had ample opportunity to prescribe opioid medications. Responsibly, of course. In my toolbox, I had excellent interview skills, the State’s Prescription Monitoring Program (PMP), and a urine test. The PMP would let me know me if patients were doctor or pharmacy shopping, although it couldn’t take into account other states. A urinalysis would tell me if the patient was taking the opioids as prescribed, or diverting, or using other, illegal drugs, or medications that were not prescribed. Heck yeah, I even had my patients sign an Opioid Use Contract.
One patient’s husband worked for the Drug Enforcement Agency (DEA), and he told me one that opioids went for about 70 cents per milligram on the street, in 2012. However, I never assumed someone was gaming the system and tried to keep an open mind. Some patients did want me to refill their emergency room (ER) hydrocodone prescription, for complaints like a mildly strained knee. At that point, I would print out knee exercises instead. I always tried to understand my patients’ emotional and physical health and encouraged exercise and healthy habits (even if most days, I couldn’t prepare food so I ate LAY’S® Limón Potato Chips and gummi worms).
Another patient had just moved from Arizona, with a history of using 30 mg of MS-Contin, a long-acting morphine tablet, three times a day, plus another opioid, Percocet 10 mg instant relief (IR), one tablet every four to six hours for breakthrough pain. The patient was full-time employed, doing fairly intense labor, and was incensed when I wanted evidence of his “bad back.” The patient did not bring any records during his first visit, but he later returned with a lengthy health record — his pain deriving from five back surgeries, three of them revisions for the original surgeries.
I had never heard of “ultra-rapid” or “slow” opioid metabolizers² which affect adequate treatment, and still believed the Center for Disease Control (CDC) had society’s best interest at heart. The opioid crisis seemed far away, and I believed that did not affect my patients, or myself. Mistakenly, I thought there hardly would have been an “opioid epidemic” had medical providers only accompanied any opioid prescription with this warning: “Use your IR (instand relief) opioid medication when you truly have breakthrough pain, a 7–8 or higher, or it will no longer be as effective.”
Perhaps. But complicating matters was that opioid medications did seem to be prescribed for relatively mild to moderate pain, or in situations where acute pain would soon resolve. For example, to my patient with that strained knee, seen in a Colorado ER. In 1991, I’d fractured my lower leg above the ankle, after a car stunt gone awry, and wasn’t prescribed any opioid medication. The ER doc in Florida who applied the hot pink cast, from my toes to my knee, pointed me to a Walgreens to buy Tylenol (acetaminophen) for the simple, uncomplicated fracture.
Although I was in tremendous pain myself from the sky diving accident and crushed sacral nerves, I denied suffering from intractable pain. Yet I was battling worsening neuropathic (nerve) pain, as well as residual musculoskeletal pain from the sacral and vertebral fractures, on a daily basis. I made it through each workday by lying down on the exam table during lunch. Work gave me great happiness, but physically I had no energy left to cook, maintain friendships or even have a hobby.
That year I recall having to do five mandatory continuing medical education credits by the State on “responsible opioid prescribing.” This seemed ludicrous since I always looked at the PMP before going into the exam room. Especially with a patient that was on medications that fell under the Controlled Substances Act.³ As a non-contract employee, I also paid my own DEA license at $780 every three years for the privilege of writing controlled substance prescriptions. I was ticked off with the cost, but also with what I perceived as government encroachment on my medical decision making.
Sure enough, over the years, after the CDC Opioid Guidelines came out (which are voluntary, and not legally binding), I began to realize that there is no true opioid epidemic. There’s an epidemic alright, of people taking opioids with multiple medications and then adding alcohol and other illegal drugs on top. What we most certainly have is an alcohol epidemic, with 88,000 deaths⁴ annually, and this epidemic is starting to effect millennials. I blame those hipster beers with ridiculously high alcohol percentages, as millennials are dying of liver cirrhosis in record-breaking numbers.
Despite the ongoing alcohol epidemic, from 2012 to 2016, using opioid medication became synonymous with being a “drug seeker.” The “opioid crisis” narrative was perpetuated and fueled by mainstream media, whose culpability lies in using labels like “opioid overdose deaths” instead of the more appropriate “mixed drug intoxication.” True opioid deaths (opioid medications alone) range around five thousand deaths annually, according to Josh Bloom, writing for the American Council on Science and Health.⁵ New York City’s medical examiner’s office is unsurpassed when it comes to accurately determining cause of death: in 2016, 71 percent of all drug-related deaths involved heroin and/or fentanyl.⁶
Looking at the numbers, most of the so-called “opioid deaths” seemed to be people who did not take their medication as instructed, if opioids were legally prescribed in the first place. Seriously, because who cooks their Fentanyl patch and injects it? Not chronic pain patients, who need slowly titrated medication to bathe, cook, work, take care of kids, or go to school. Patients were indeed dying from respiratory depression, caused by taking legal or illegal opiates. But how many of those deaths are suicides? If patients with severe pain, on a stable regimen, are denied access, they may turn to suicide, or illegal opioids like heroin, now tainted by illegal fentanyl. That is not an opioid crisis, but another iatrogenic consequence of the “guidelines.” The Law of Unintended Consequences never fails.
How was it that the CDC took advice from an anti-opioid advocacy group, Physicians for Responsible Opioid Prescribing (PROP)⁸ in constructing the Opioid Guidelines? PROP had lobbied Federal officials and the FDA for years, to change opioid labels. When they were (mostly) rebutted, PROP got involved with the CDC, behind closed doors. The Washington Legal Foundation⁷ notified the CDC in 2015, as in their opinion, the CDC broke the 1972 Federal Advisory Committee Act (FACA) law. Washington Legal Foundation states that a Core Expert Group, advising the CDC, conducted their “research” and “Draft for Opioid Guidelines” in secret, without input from pain experts, pharmocologists, or patient groups.
Dr. Jane Ballantyne (current PROP President) was part of that Core Expert Group and is notorious for her anti-opioid stance. Another Core Expert Group member is PROP executive director, and founder, Dr. Andrew Kolodny, who refers to opiate medication as “heroin” pills and proclaimed that “oxycodone and heroin have indistinguishable effects.”⁹ Yet you oughtn’t compare a 5 mg tablet of oxycodone to IV heroin, without qualifiers on potency. Dr. Kolodny, an addiction expert, doesn’t even distinguish between “plain” heroin, and heroin cut with fentanyl, which is 100 times stronger than morphine. About 80 percent of fatal overdoses are now due to illegal fentanyl. By muddying the issues of opioid dependence, opioid addiction, and heroin use with either false or incomplete statements, PROP also does a disservice to people who are addicted to heroin or illegal fentanyl.
Research has found that 75% of heroin addicts have a mental health illness, and 50% have trauma from (sexual) abuse before age 16, something that gets drowned in Dr. Ballantyne’s simplified narrative of “continuous or increasing doses of opioids [… ] can worsen a person’s ability to function and his or her quality of life. It may also lead to opioid abuse, addiction, or even death.”¹⁰ Like many others, I argue that (illegal) fentanyl, and indirectly, profound loss of hope, is the main driver behind the current “mixed use overdose” deaths.
Dr. Kolodny was Chief Medical Officer of The Phoenix House, an addiction center, at the time he helped draft the CDC Guidelines. PROP also avoids mentioning the Millennium saliva,¹¹ or other DNA tests, to identify how individual patients metabolize opiate medication and that some are “ultrafast” metabolizers. PROP fails to mention opioid blood concentration measurements, no matter how imperfect.¹² However, no one doubts the conflict of interest: PROP Board members are involved with grants from the CDC, addiction centers, medical device companies to develop an opioid tapering mechanism, and even consulted with law firms investigating lawsuits against opiate pharmaceutical companies.
PROP was originally funded by Phoenix House, one of many addiction centers that prescribes buprenorphine. PROP is currently funded by the Steve Rummler HOPE Network,¹³ another anti-opioid group that lists Dr. Ballantyne and Dr. Kolodny on the medical advisory committee. Dr. Kolodny admitted in a 2013 New York Times article titled “Addiction Treatment with a Dark Side” that as a New York City Health official, he lobbied on behalf of the buprenorphine pharmaceutical industry. He was quoted as saying, “We had New York City staff out there acting like drug reps [with $10,000 incentives -KG].”¹⁴
Buprenorphine was the supposed miracle drug after methadone, but its known side effects include serious diversion, addiction, and possibly, lifelong treatment. Dr. Kolodny publicly promoted buprenorphine in various media outlets, despite evidence of buprenorphine overprescribing, pill mills, and overdoses. The true scale is not known, as most ERs and medical examiners do not test for the presence of buprenorphine. The CDC does not track buprenorphine deaths, despite a 2013 study¹⁵ that found a tenfold increase in buprenorphine-related ED visits, according to the Federally funded Substance Abuse and Mental Health Services Administration (SAMHSA). As “bupe” availability increased, so did diversion and overdose deaths.
Interestingly, that Dr. Kolodny promotes the idea that heroin and opioid medications are the same molecular compound. Actually, buprenorphine has a molecular profile¹⁶ that more closely resembles heroin, than hydrocodone. Dr. Kolodny indirectly claims that CDC “Guidelines” are effective, when the truth is that by the time PROP advised the CDC, prescriptions had already tapered off. This is evidenced in his statement as chief medical officer from a Phoenix House Q&A,¹⁷ dated December 2015: “It will take some time, but we’re already beginning to see a plateau in opioid prescribing.” Dr. Kolodny appears to take credit for a trend that had nothing to do with PROP, and he omits the fact that prescriptions are down since 2011, and yet overdoses are up.
Mainstream media occasionally, and accidentally, reveals the truth. CNN¹⁸ in 2018: “Fentanyl-related deaths double in six months; US government takes some action.” Then again, the echo of Dr. Kolodny’s statements, as reported by CNN: “The recent rise in popularity of these synthetics has been called the third wave of the opioid epidemic; the first wave was attributed to the overprescribing of painkillers like oxycodone and hydrocodone and the second to heroin. The drugs are all chemically similar and act on the same receptors in the brain.” Again, not one word about potency.
Few realize that when the CDC issued the Opioid Guidelines in 2016, there was inadequate research done ahead of time to determine the true cause of the rise in opioid-related deaths. There are no long-term studies on the effects of chronic opiate therapy. Very few, if any, pain management experts or pharmacologists were consulted to determine potential impacts on their practice. Neither veterans nor chronic pain patients were given a true opportunity to issue public comments to the CDC or any other Federal authority prior to the implementation of these new prescribing mandates. The CDC ended up targeting one of the most vulnerable groups, patients with intractable pain.
The CDC’s Guidelines also affect patients with cancer and patients who no longer receive cancer treatment because, unfortunately, both groups report similar pain levels. The guidelines allow the use of opioids during cancer treatment, but they are confusing when it comes to equally severe, post-cancer treatment pain. I fear this “opioid” crisis is far from over, and yet, trust me, this will go down as “reefer madness” in another hundred years. It is a manufactured tragedy that does real harm to patients with intractable pain. The “opioid” crisis also hurts human beings who suffer from heroin, opioids or other addictions by siphoning money, goodwill, and energy.
Few people realize that the CDC hired a PR agency to help sell the American people myths on the “opioid epidemic.” The agency, PRR, designed graphics to “educate” primary care providers that “one in four patients on opioids will develop addiction.” Even the National Institute of Health,¹⁹ another federal entity, estimates this to be 5 percent, not 25 percent. Another research team²⁰ concluded in Pain Medicine that opioid therapy for chronic pain patients (note: in absence of prior or current drug abuse) resulted in a 0.19 percent incidence of abuse.
The language used by the media as well as PROP contributes to misunderstanding; using words like addiction, tolerance, dependence, abuse or opioid use disorder as if they mean the same, directs the casual observer to bias. It’s clear that PROP never was an independent, neutral entity advising the CDC, yet they ended up dictating federal policy, based on flawed evidence. Dr. Ballantyne, Dr. Franklin, and Dr. Kolodny in Politico.com²¹ in March 2018: “We agree with Satel that the answer is not to force millions of chronic pain patients to rapidly taper off medications they are now dependent on (Italics mine). But then, neither is the answer to absolve overprescribing for pain.”
I’m not a linguist, but in that essay, PROP uses the word “addiction/addicted” 16 times, and “dependence” twice. The CDC could have ensured that patients with severe to intractable pain (no such distinction is made) would not lose access to their medications. And yet, that is exactly what happened. Stable patients on long-term opioids were tapered against their will, as the CDC “Guidelines” state it is undesirable to titrate above or equal to 90 morphine milligram equivalent²² daily (aka MME/day). But this was meant for opioid-naive patients, not those on long-term opiate therapy. Primary care providers, who were forced to follow these “Guidelines,” either stopped prescribing opioids altogether or forced patients to rapidly taper to below 90 MME.
Dr. Ballantyne is correct in her remarks that it isn’t realistic to expect zero pain levels, especially for acute pain that is expected to resolve quickly, like a sprain or an uncomplicated fracture. But people with severe to intractable pain are condemned to a world of suffering. Recall my patient with the five back surgeries? I wonder about him. He was working full time, on 180 MME a day, but in his mid-fifties, arthritis would worsen soon. My own story did not end well; I ended up with yet another spinal cord lesion, a benign hemangioma at chest level, which causes “central neuropathic pain syndrome.” My old cauda equina syndrome morphed into “severe, chronic adhesive arachnoiditis.” This is an incurable, intractable, progressive neuroinflammatory disorder whose pain is considered on par with having terminal cancer pain. Still, I try to make the best of it, see my essay, On Being Bedbound.
The CDC and PROP came for me: after using opioids exactly as prescribed, and less than 30 MME daily, my primary care clinic was forced to stop my opioid prescription, and that of all patients. I was not accepted in any pain management clinic, in an urban area of almost one million. Pain clinics here no longer provide “medical management,” yet perform epidural steroid injections ($3000 a pop), which may have contributed to, or worsened my adhesive arachnoiditis syndrome. I’m lucky to live in an urban area, where the academic hospital’s pain team took over my prescription.
But what about elderly and impoverished patients, or those in rural areas? PROP and the CDC claim primary care providers “overprescribe” and are responsible for most of the opioid prescriptions. But they fail to publicly acknowledge that pain management clinics no longer accept patients. This epidemic of undertreated patients will become known as one of the cruelest moves by a Federal agency on an already compromised population. I do feel for teenagers and adults who become addicted. Yet there ought to be a different, more sensible approach towards legitimate, chronic pain patients who need opioid medications, as well as people who develop a substance use disorder, who deserve our help and sympathy.
It is a conundrum of extraordinary proportions. At a time when managed care and Electronic Health Records dictate the length and quality of an office visit, there is less and less time to sit down and connect with a patient. Not just with chronic pain patients. Medicine and society would benefit greatly from the extra time clinicians deserve, to encourage exercise, eat healthier, lose weight, stop smoking and assess if a patient needs other support, like therapy.
In my opinion, it is loneliness, the feeling of not being connected to humanity in a meaningful way, combined with economic hardship, that leads to unhealthy lifestyle choices, as witnessed by the Rustbelt being hit hardest. Research shows that rats who were offered spring water or water laced with heroin, choose heroin. When those same rats were given ample toys, space, and other rats to play and have sex with, they did not choose the heroin laced water. That’s right, happy rats don’t need no heroin!
It cannot be denied that in previous decades, pain was both undertreated, and opioid medications prescribed for relatively minor, self-resolving aches and pains. Forget for a moment, the narrative that places blame on overprescribing, the opioid manufacturers, or the pharmaceutical distributors that, for example, flooded impoverished communities like those in West Virginia.²³ Forget all that, and focus on what is going on. Ultimately, patients with intractable pain pay the price of ignorance by scientists, journalists, politicians, and laypeople alike.
For this humanitarian crisis, there are no perfect answers. For example, as Red Lawhern, Ph.D. and prominent pain advocate²⁴ recently communicated with me (12/3/2018): “there is promise in genetic testing but hasn’t yet been fully reduced to routine practice and may not be covered by insurance.” Luckily my DNA testing was covered, on the condition it tested for depression. I also discovered that ketamine infusions help me most, but will leave that topic for my upcoming book, The Queen of Ketamine. Sadly, amidst the opioid paranoia, non-invasive alternatives like ketamine infusions aren’t mentioned for neuropathic or intractable backpain, which often has a neuropathic component. Research also shows that adding an anti-seizure medication to an opiate mediation provides better neuropathic pain contral, with less morphine²⁵.
In the end, I don’t think Tai Chi, Tylenol and Cognitive Behavioral Therapy is going to cut it for meningeal inflammation or other (neuropathic) pain syndromes. I believe the tide is turning. It will take time, and in that time, patients with intractable pain will choose to end their lives. But we are not alone, and it helps to know that courageous voices, notably the Alliance for Treatment of Intractable Pain, are speaking up for us. The print and online magazine Reason²⁶ has long been a voice of, well, reason. As Red Lawhern stated in a must-listen November 2018 radio interview,²⁷ “We must address underemployment, socioeconomic despair and hopelessness which are a vector for addiction. And end the War on Pain patients.”
Love, Kaatje
Kaatje Gotcha, model and stuntwoman-turned-Physician Assistant, found comedy, writing and advocacy after developing Adhesive Arachnoiditis. This spinal cord disease causes intractable neuropathic pain and leaves her mostly bedridden. Prior to that diagnosis, she’d survived a nighttime skydiving accident, landing at 70 mph. This caused Cauda Equina Syndrome; a subsequent lumbar puncture and epidural steroidal injections may have exacerbated her previous injuries.
Kaatje’s courageous spirit led to writing “The Queen of Ketamine,” available on Kindle in February. This is a comedic yet pragmatic memoir on adhesive arachnoiditis, the opioid “epidemic,” neuropathic pain, dating with a disability, while offering hope and practical advice. Kaatje’s 2018 TEDx talk and book publication will be posted on her Facebook page, at www.kaatjegotcha.com and Instagram @kaatjegotchacomedy. Find her essays on Medium, and follow her on twitter.
Cauda Equina Syndrome https://emedicine.medscape.com/article/1148690-overview
Opioid Metabolism https://www.medscape.com/viewarticle/771480
Controlled Substance Act https://www.dea.gov/controlled-substances-act
Alcohol Epidemic https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/alcohol-facts-and-statistics
Opioid Epidemic Deception https://www.acsh.org/news/2017/10/12/opioid-epidemic-6-charts-designed-deceive-you-11935
Overdose Deaths by Heroin/Fentanyl 71percent https://www1.nyc.gov/assets/doh/downloads/pdf/epi/databrief89.pdf
Washington Legal Foundation and PROP https://www.forbes.com/sites/wlf/2015/12/15/cdc-bows-to-demands-for-transparency-and-public-input-on-draft-opioid-prescribing-guidelines/#c82eda135bc3
Physicians for Responsible Opioid Prescribing http://www.supportprop.org/
Dr Kolodny refers to “Heroin” Pills https://www.healthline.com/health-news/secondary-drug-industry-booming-amid-opioid-epidemic#2
Dr Ballantyne’s Narrative https://www.statnews.com/2015/11/30/chronic-pain-intensity-scale/
Millennium Opioid Metabolite DNA Test https://www.millenniumhealth.com/services/test-offerings/
Opioid Serum Measurements http://paindr.com/serum-opioid-monitoring-wheres-the-evidence/
Medical Advisory Committee https://steverummlerhopenetwork.org/our-team/
NYT: Addiction Treatment with a Dark Side https://www.nytimes.com/2013/11/17/health/in-demand-in-clinics-and-on-the-street-bupe-can-be-savior-or-menace.html
Sharp Rise in Buprenorphine ER Visits https://www.samhsa.gov/data/sites/default/files/DAWN106/DAWN106/sr106-buprenorphine.htm
Heroin and Buprenorphine Molecular Profile http://paindr.com/heroin-hydrocodone-buprenorphine-prop-aganda/#comment-334500]
Q&A with Dr. Kolodny, Phoenix House https://www.kolmac.com/2015/12/qa-dr-andrew-kolodny-chief-medical-officer-phoenix-house/
Fentanyl, as Reported by CNN https://www.cnn.com/2018/07/12/health/fentanyl-opioid-deaths/index.html
NIH Estimates Pain Patient “Addiction” 5 Percent https://medlineplus.gov/magazine/issues/spring11/articles/spring11pg9.html
Pain Patient “Opioid Use Disorder” without Risk Factors 0.19 percent https://academic.oup.com/painmedicine/article/9/4/444/1824073
Rebuttal by Dr. Kolodny and Dr. Ballantyne https://www.politico.com/magazine/story/2018/03/13/opioid-overprescribing-is-not-a-myth-217338
Morphine Equivalent Dosing https://www.wolterskluwercdi.com/sites/default/files/documents/ebooks/morphine-equivalent-dosing-ebook.pdf?v3
https://www.wvgazettemail.com/news/cops_and_courts/drug-firms-poured-m-painkillers-into-wv-amid-rise-of/article_99026dad-8ed5-5075-90fa-adb906a36214.html
Red Lawhern, PhD and nationally known Pain Patient Advocate http://face-facts.org/lawhern/
Combining epilepsy drug, morphine can result in less pain, lower opioid dose. https://www.sciencedaily.com/releases/2014/09/140915153613.htm
Jacob Sullum, Reason journalist and syndicated writer https://reason.com/archives/2018/03/08/americas-war-on-pain-pills-is#comment
“Unleashed” Matt Connarton Interviews Red Lawhern 11/28/18 https://www.spreaker.com/user/ipmnation/matt-connarton-unleashed-11-28-18
window.fbAsyncInit = function() FB.init( appId : 1443946719181573, autoLogAppEvents : true, xfbml : true, version : 'v3.2' ); ;
(function(d, s, id) var js, fjs = d.getElementsByTagName(s)[0]; if (d.getElementById(id)) return; js = d.createElement(s); js.id = id; js.src = "https://connect.facebook.net/en_US/sdk.js"; fjs.parentNode.insertBefore(js, fjs); (document, 'script', 'facebook-jssdk'));
Source link
0 notes
Text
Episode #12 So What's the Big Deal About Vitamin B-12?
So in the last podcast we talked about a plant-based diet and how to start that conversation and how to implement the plant based diet to achieve benefits. One of the commonly seen nutritional deficiencies in a plant-based diet is vitamin B 12 deficiency. Vitamin B-12 deficiency however, is not just common in those living in a plant-based diet.
Another cause of Vitamin B12 deficiency includes poor absorption.
Vitamin B 12 absorption is often impaired by some of the most commonly prescribed prescription medications such as Metformin, beta blockers and proton pump inhibitors. These medications can decrease the absorption of vitamin B 12, by blocking or even eliminating a protein called the intrinsic factor. The intrinsic factor is required to absorb vitamin B 12. Other medications that can block the absorption of vitamin B 12 include some of the older antiepileptics, including phenytoin, Depakote, colchicine, antibiotics and anti-inflammatories. Do you happen to prescribe any of these medications? This just adds to the fact that pharmaceuticals should be used judiciously and not used to treat side effects of medications or just because the patient insists upon having some type of medication.
So what’s the big deal? Why do we care about B12 so much? Well, because B12 is vital to neurological function and red blood cell production. I think that the nervous system and blood production are pretty important. The nervous system controls sensation, perception, energy, mood, cognition and most everything else in our body. As for the red blood cell production, we know that red blood cells carry oxygen. Without proper oxygenation, we will suffer from poor endurance, fatigue and myalgias.
When one of the most common complaints of primary care, in addition to many specialty practices is fatigue, and vitamin B 12 is a common contributor to fatigue, you should be checking Vitamin B12 in your patients.
I became fascinated with the impact of vitamin B 12 deficiency on patients during my time working as a provider in a neurology practice. We had patients referred for stroke like symptoms, neuropathy and even fatigue. The common denominator in many of these patients was a vitamin B 12 deficiency. The most significant case that I was able to observe both the effects of deficiency and the benefit of replenishment was in a gentleman that was sent for ataxia. He literally could not walk a straight line. He came down the hall with the assistance of his wife, because without her he would zigzag from wall-to-wall. He had a high steppage take gait due to a loss of perception of where his feet were. Now, many of you know that when you are evaluating a patient with neurologic dysfunction you go for patterns. Typically stroke like events occur unilaterally, neuropathic dysfunction is bilateral. And ataxia that causes you to not be able to walk a straight line is typically from something in the central nervous system, not the peripheral nervous system. So, this gentleman was very perplexing, as he did not have diabetes, he did not have a stroke on MRI and displayed conflicting presentation of neurologic processes contributing to his symptoms. There was a standard lab panel that we drew for anyone coming into the office with neurologic dysfunction and B 12 was included in the panel. His B12 level was 127. That was the only abnormality found. Of course, I was skeptical that replenishing B12 was going to return this gentleman to full function. We did, however, initiate Parenteral vitamin B 12 therapy and had him return in six weeks. His levels had increased to 700 and he had complete resolution of his symptoms, except for some decreased sensory to touch in the most distal part of the lower extremities. To say the least, I was blown away by this! He had also had improvement in his energy levels and cognitive function, which he had not realized had gotten so low until he was feeling good again.
From that point on, I have checked a vitamin B12 level on every patient that complains of numbness, tingling, fatigue or memory impairment. Some things you may find on examination, prior to such a profound presentation is decreased vibratory sensation, slow reflexes, decrease in sensation to light touch and temperature in the extremities, and abnormalities of the tongue. For vitamin B 12 deficiency’s to get to this level of extreme nature, the patient would’ve had to go through all of their vitamin B 12 stores in the liver and no longer be absorbing any type of vitamin B 12 from their diet.
A treatable vitamin B 12 level with injections, is 300 or less. Between 350 and 450, I will advise a sublingual type of B 12 that is absorbed by the oral mucosa, as opposed to the stomach. When you have lost the intrinsic factor that helps with vitamin B 12 absorption, it does not ever come back and you will not be able to absorb vitamins taken orally that need to be broken down in the stomach. If the levels continue to climb with a sublingual or a mucosal absorbable type B12 such as that in a gummy or drop, then injections aren’t necessary.
Elevated homocysteine levels can be seen in vitamin B 12 deficiency. An elevated homocysteine level indicates an increased risk of cerebrovascular disease. If vitamin B 12 is depleted and homocysteine levels are increased, be sure to use folic acid in addition to vitamin B 12 replenishment.
B12 depletion in alcoholics is quite common. The irritation to the gut and intestines from alcohol can block the absorption of nutrients. Often times, patients will not tell you the amount of alcohol they truly drink for fear of judgment. If you do observe a macrocytic anemia, associated with a B12 deficiency, discuss the causes of vitamin B deficiencies cautiously. Mention it in a way that will get them to think about it. This may help them to be more honest and upfront with you about alcoholism or more willing to take vitamin repletion.
Another consideration with B12 deficiency in alcoholism is that alcohol is a diuretic and B12 is a water-soluble vitamin. This makes excretion of vitamin B 12 occur at a higher rate in alcoholics. These vitamin B deficiency’s in alcoholics can also lead to metabolic dementia and Alzheimer’s type dementia.
On the subject of vitamin B 12 being a water-soluble vitamin, this adds security to the treatment plan. I will initially give vitamin B 12 1000 µg subcutaneously or intramuscularly once a week for four weeks followed by once per month there after to maintain vitamin B 12 levels. Some patients will continue to deplete their stores of vitamin B 12 quickly and require injections every two weeks. This is something for you to monitor. I will monitor the vitamin B12 levels every six months once B12 deficiency has been established and treatment has begun.
Sources of vitamin B 12 from your diet include primarily animal resources, such as liver and organ meats, egg yolks, tuna and salmon. For those on a plant-based diet, nutritional yeast is a valuable source of vitamin B 12. If they are not consuming enough through their diet, oral supplementation with 1000 µg daily would be fine as well. The parenteral replenishment is most often used once there is depletion, rather than as prevention.
As you know, I do have a wellness and weight management program that I offer online. Vitamin B 12 is covered in this program for considerations in weight management. That is because it is very significant for boosting metabolism and overall wellness. Once you increase your energy levels and boost your metabolism, you feel more like exercising and it enhances your motivation towards weight loss efforts. I did not speak specifically of lipotrohpic injections in that course. I will not speak of all of the vitamin Bs in this podcast either. We will save that for a future discussion. I will tell you that they are very significant due to the boost in metabolism and easy to obtain from a compounding pharmacy. My patients absolutely love the lipotrophic injections. Depending on what area of the country you are in, there are many valuable resources for compounding pharmacies. I am on the East Coast and find that some of the West Coast pharmacies charge an insane amount to ship to this area. I am currently putting together a program for the use of adjunct of therapies in wellness and weight management. This will include the supplemental resources of certain vitamins, lipotrophic injections, IV nutrition therapies and peptides. I know that seems like a lot to include into one program, but if you’re going to add one, you should add them all. They are a great ancillary source of income and they are very, very effective. if you have not already gathered this from my podcast, I do not believe in gimmicks, bad, quick fixes or anything that is going to let the patient down. I will not ruin my reputation or risk my patients health for a dollar. Anything that I promote and put into a course for you, I assure you I have researched at great length before I have offered that to my patients.
You have heard in previous podcasts, that I like to practice what I preach. That means, if I will not administer these protocols, supplements and treatment options to myself, my closest family and friends, I will not offer it to my patients or promote it to my colleagues. There are many gimmicks out there. There’s plenty of people who are trying to take advantage of you. I have lost a lot of money in the short term studying these things, but I consider it a gain in the end because I did not hurt anyone or take advantage of anyone by implementing something that is not effective.
I do hope that you’ve taken away some information on the importance of vitamin B 12 in your patients. You will make such a big difference in the lives of so many if you check that vitamin B 12 level and begin to treat them appropriately. It will boost your metabolism, boost their energy and eliminate a myriad of symptoms they may be experiencing.
If you have found this valuable to you and your practice, you might want to check out my Phytonutrient and Micronutrient module from the wellness and weight management course that I have made available as an individual course for you. You can find that at nphealthinterventions.com/phytonutrients
I would of course like you to take the entire program and get all of the information that you need to make a big difference in your patients, but I understand if you’re a little hesitant or not sure if it’s something you want to dive into. That’s why I will release some of these modules as appropriate with the topics we are currently discussing.
Have a great week! May it be filled with many Health Interventions!
Feel free to send me your feedback!!
0 notes