#nuffield
Explore tagged Tumblr posts
Video
1951 Morris ad by totallymystified
#Morris#Minor#Oxford#Six#car#automobile#saloon#motor#motoring#Nuffield#retro#vintage#nostalgia#1950s#fifties#illustration#ad#advert#advertising#advertisement#flickr
1 note
·
View note
Text
I'VE JUST HAD TOP SURGERY! OMG! Can't believe it finally happened!
If anyone's curious, here's the timeline of my journey so far:
Referral to gender clinic sent via NHS England: April 2019
East of England gender clinic called: Jan 2022
Had 4-5 calls with clinic: Jan 2022 - May 2024
Jan 2022 = 1st call to take me off Tavistock list and onto EoE list. 2nd call week later to talk with them about myself, dysphoria, how long felt trans, where I fall on trans scale and how I see my gender, and most importantly: what I want from them, etc
Later 2022 = 3rd call that went through same things as 2nd but with a different person so they could compare notes and confirm gender dysphoria/incongruence diagnosis.
In both calls with the clinic, I expressed that my main dysphoria was with my chest and the thought of going on hormones beforehand would exacerbate feelings so I wanted to pursue top surgery (removal of breasts) first.
In both calls, I was asked if I had socially transitioned, who I'd told, how it made me feel, and experience that affirmed this was the correct path for me, etc. I had come out to my work as non-binary with a shortened version of my birth name. I knew this was temporary until I took the plunge and changed my name (ADHD procrastination is a bitch 😂)
August 2022 = I socially changed my name and confirmed the pronouns I'd like to be called. It didn't really come as a shock to anyone tbh, which was good. I think this was before my 3rd call with clinic, so I was able to tell them my new name.
Feb 2023 = I legally changed my name (big up the ADHD procrastination and finally the impulse to just DO IT!). I did this via Deedpoll and had 2 colleagues/friends sign as witnesses. I chose them as they had easy to understand jobs so would look more official than unemployed or self-owned company person.
March 2023 (I think) = I had my 4th call with the clinic, this was specifically for top surgery. They asked me about what kind I wanted, who/where I wanted to go with, if I understood the risks etc. I answered all bar who/where as I didn't have anyone bar really old names that I'd seen from YouTube. I asked them to send me a list so I could choose.
April 2023 = I chose My Andrew (Andy) Mellington at Nuffield Health in Brighton as my surgeon. I'm considered obese so I wanted a realistic BMI goal. Most wanted a BMI of 30 so I didn't even look at them (this was based off comments I'd see on social media, with some people saying a few surgeons weren't very nice), whereas his, and Mr Kneeshaw (I think) accepted a limit of 35 BMI. This was far more attainable for me. I did email them both (details on their websites to info emails can be found easily) and enquired. Mellington's team came back to me the next day asking me to send questions to a specific person, they then came back very quickly (same/next day). I'm still yet to hear back from Kneeshaw 😂 (a friend of a friend went with him which is why I considered him, but Mellington was quicker, had good reviews on social media and I was able to find someone who had my body shape, pictures, and replied to me! So that consolidated my decision.)
Aug 2023 = official referral from EoE gender clinic was sent to Nuffield requesting Mellington to take me on.
Nuffield team called me to confirm consultation date: early January 2024
At this point the team also sent a short form for me to fill in and requested pictures of my chest
Consult with Andy Mellington: late Feb 2024
I didn't expect him to talk about much of my trans experience tbh but he did ask a little (how long felt like this, how did you know etc.) before he then ran through what I requested and what I should expect
I asked for double masectomy. Due to my weight and size of breasts, this was 1 of a few options. Andy said looking at my chest pictures, it's likely my scars would be so close in the middle that to achieve a flatter chest, 1 long scar was gonna be best to avoid leaving a bulge in the middle.
I chose not to have nipples grafted. This was for a few reasons. 1. I don't like when I can see them through my shirt (big dysphoria). 2. I've watched a lot of vids of trans people's recovery and the nips are the grossest (they get removed and reattached so healing is a bit longer/itchier etc than just the main scar). 3. Someone said they were scared of scratching them off and uh...yeah that didn't help. 4. I saw vids of other people with no nips and it looked fine, there's gonna be a big ol' scar on ya chest so it's not like there's nothing to look at.
Andy did reassure that he's never had any nipples fall off of his patients, if that's what I was worried about too. But honestly, I just don't want them. And if I decide later that I want something there, then I could choose to get them tattooed on.
Nuffield team called to confirm surgery date: mid-March 2024
Date of surgery: 30th May 2024
Pre-assessment call 14th May 2024
Call from Nuffield team. Went through medical history and confirmed what needed to be done about getting bloods taken
Pre-assessment appointment: 21st May 2024
Went to my nearest Nuffield hospital (1 hour away) and had blood taken and MRSA swabs. Team were really nice and welcoming.
I got ill for a month and half so had to reschedule my surgery 😭: May 17th 2024
It was rescheduled: late Aug 24 but I asked to be kept on the list if anyone else cancelled, I was then re-rescheduled for late July 2024
And now, it's August! It's done!
In morning of July date, discharged the next morning.
2 week post-op meeting with Nuffield team will come. I will be able to take my binder off, they will check my scars. Expected to be about 30 minutes, can be in person or virtual (I was advised virtual is absolutely fine as I live far away, Andy was happy with results and no nips meant better recovery).
Then I have a gender clinic appointment expected around April 2025 to possible talk hormones.
It's been a long time to wait, and that's without all the dysphoria that comes with living in the wrong body for so long, but my god am I so relieved right now. It's (pun fully intended) such a weight off my chest!
#stark life#ftm#trans#trans uk#transgender#andrew mellington#andy mellington#nuffield health#my journey#east of england gender clinic#EoE GC#timeline#trans journey#nhs
6 notes
·
View notes
Text

CT scan
0 notes
Text
A Brief Look at Morris Motors in the US Market
View On WordPress
#1950&039;s#1960&039;s#Lord Nuffield#MG#Morris 10#Morris Cowley#Morris Garages#Morris Minor#Morris Motors#Morris Motors in the US Market#US Market#William Morris
1 note
·
View note
Text
My Full Experience Getting Top Surgery!
I'm officially one month post-op so it's time to post my full experience! Recovery was an absolute nightmare but I'm glad I went through it all.
I got my surgery at Nuffield Brighton Hospital, my surgeon was Mr Ian King, I LOVE my results and I highly recommend Mr King as a top surgeon to all my U.K. friends.
Before/After images and a link to the full write up of my experience under the cut! 👇
Read the full story HERE! wow i sound like a clickbait site!! you won't believe what happens !!!!!
but seriously i went through hell with some of this and have had to file two complaints to the hospital because of how bad it was. i'm shocked i didn't get some form of infection or complication.
(gonna have to censor my before pictures because this website isn't the biggest fan of trans people lmao)
before


after


#transgender#ftm#trans man#top surgery#gender affirming care#gender affirming healthcare#trans healthcare#ftm surgery#gender affirming surgery#trans#transmasc#lgbt#bishop.txt#ok to rb
304 notes
·
View notes
Text
Patients With Long-COVID Show Abnormal Lung Perfusion Despite Normal CT Scans - Published Sept 12, 2024
VIENNA — Some patients who had mild COVID-19 infection during the first wave of the pandemic and continued to experience postinfection symptoms for at least 12 months after infection present abnormal perfusion despite showing normal CT scans. Researchers at the European Respiratory Society (ERS) 2024 International Congress called for more research to be done in this space to understand the underlying mechanism of the abnormalities observed and to find possible treatment options for this cohort of patients.
Laura Price, MD, PhD, a consultant respiratory physician at Royal Brompton Hospital and an honorary clinical senior lecturer at Imperial College London, London, told Medscape Medical News that this cohort of patients shows symptoms that seem to correlate with a pulmonary microangiopathy phenotype.
"Our clinics in the UK and around the world are full of people with long-COVID, persisting breathlessness, and fatigue. But it has been hard for people to put the finger on why patients experience these symptoms still," Timothy Hinks, associate professor and Wellcome Trust Career Development fellow at the Nuffield Department of Medicine, NIHR Oxford Biomedical Research Centre senior research fellow, and honorary consultant at Oxford Special Airway Service at Oxford University Hospitals, England, who was not involved in the study, told Medscape Medical News.
The Study Researchers at Imperial College London recruited 41 patients who experienced persistent post-COVID-19 infection symptoms, such as breathlessness and fatigue, but normal CT scans after a mild COVID-19 infection that did not require hospitalization. Those with pulmonary emboli or interstitial lung disease were excluded. The cohort was predominantly female (87.8%) and nonsmokers (85%), with a mean age of 44.7 years. They were assessed over 1 year after the initial infection.
Exercise intolerance was the predominant symptom, affecting 95.1% of the group. A significant proportion (46.3%) presented with myopericarditis, while a smaller subset (n = 5) exhibited dysautonomia. Echocardiography did not reveal pulmonary hypertension. Laboratory findings showed elevated angiotensin-converting enzyme and antiphospholipid antibodies. "These patients are young, female, nonsmokers, and previously healthy. This is not what you would expect to see," Price said. Baseline pulmonary function tests showed preserved spirometry with forced expiratory volume in 1 second and forced vital capacity above 100% predicted. However, diffusion capacity was impaired, with a mean diffusing capacity of the lungs for carbon monoxide (DLCO) of 74.7%. The carbon monoxide transfer coefficient (KCO) and alveolar volume were also mildly reduced. Oxygen saturation was within normal limits.
These abnormalities were through advanced imaging techniques like dual-energy CT scans and ventilation-perfusion scans. These tests revealed a non-segmental and "patchy" perfusion abnormality in the upper lungs, suggesting that the problem was vascular, Price explained.
Cardiopulmonary exercise testing revealed further abnormalities in 41% of patients. Peak oxygen uptake was slightly reduced, and a significant proportion of patients showed elevated alveolar-arterial gradient and dead space ventilation during peak exercise, suggesting a ventilation-perfusion mismatch.
Over time, there was a statistically significant improvement in DLCO, from 70.4% to 74.4%, suggesting some degree of recovery in lung function. However, DLCO values did not return to normal. The KCO also improved from 71.9% to 74.4%, though this change did not reach statistical significance. Most patients (n = 26) were treated with apixaban, potentially contributing to the observed improvement in gas transfer parameters, Price said.
The researchers identified a distinct phenotype of patients with persistent post-COVID-19 infection symptoms characterized by abnormal lung perfusion and reduced gas diffusion capacity, even when CT scans appear normal. Price explains that this pulmonary microangiopathy may explain the persistent symptoms. However, questions remain about the underlying mechanisms, potential treatments, and long-term outcomes for this patient population.
Causes and Treatments Remain a Mystery Previous studies have suggested that COVID-19 causes endothelial dysfunction, which could affect the small blood vessels in the lungs. Other viral infections, such as HIV, have also been shown to cause endothelial dysfunction. However, researchers don't fully understand how this process plays out in patients with COVID-19.
"It is possible these patients have had inflammation insults that have damaged the pulmonary vascular endothelium, which predisposes them to either clotting at a microscopic level or ongoing inflammation," said Hinks.
Some patients (10 out of 41) in the cohort studied by the Imperial College London's researchers presented with Raynaud syndrome, which might suggest a physiological link, Hinks explains. "Raynaud's is a condition of vascular control or dysregulation, and potentially, there could be a common factor contributing to both breathlessness and Raynaud's."
He said there is an encouraging signal that these patients improve over time, but their recovery might be more complex and lengthy than for other patients. "This cohort will gradually get better. But it raises questions and gives a point that there is a true physiological deficit in some people with long-COVID."
Price encouraged physicians to look beyond conventional diagnostic tools when visiting a patient whose CT scan looks normal yet experiences fatigue and breathlessness. Not knowing what causes the abnormalities observed in this group of patients makes treatment extremely challenging. "We need more research to understand the treatment implications and long-term impact of these pulmonary vascular abnormalities in patients with long-COVID," Price concluded.
#long covid#covid#covid news#mask up#pandemic#covid 19#wear a mask#public health#sars cov 2#still coviding#coronavirus#wear a respirator#covid conscious#covid is airborne#covid isn't over#covid pandemic#covid19#covidー19
107 notes
·
View notes
Text
PLEASE READ BELOW
Hi! I am a UK based trans artist and writer looking to pursue a private hysterectomy. I run an Etsy store (you may even have one of my stickers or badges!) and work part time but am still struggling to save much of anything towards surgery due to debt, living costs, etc so I’m looking for a little bit of help!
The reason I am pursuing a hysterectomy now is due to having cervical ectropion. This condition is where the cervix is essentially inside out and causes bleeding and excruciating pain. Frustratingly enough the treatment for this condition worked for all of two weeks before returning straight back to how it used to be. Cervical ectropion is aggravated by fluctuating hormone levels, particularly estrogen, so if I was to ever experience atrophy and seek treatment for that it would only make my ectropion far worse. The NHS does not offer hysterectomies for this condition due to them deeming it “a harmless condition”. Funnily enough the only procedure they approve of to “treat” this is a tubal ligation which has nothing to do with the cervix (make it make sense).
I could attempt to get a hysterectomy through my GIC (Nottingham), however their communication is abysmal, I get one appointment a year with them and I cannot sit by and wait for the topic to come up on their terms, they never even spoke to me about top surgery (after telling me they would) leaving me to get that privately too, and I think even if they do approve a referral it’d take far too long and I would have little control in the situation. I simply cannot be in this pain for however long they wish to take to help me. Especially with how things are going for trans healthcare.
So I’m looking to get it privately. I have been recommended Mr Saurabh Phadnis with Nuffield Health in London due to him approving hysterectomies for many reasons and getting rid of everything you wish to remove and not just the bare minimum. I would like to go with him as I wish to remove everything including the cervix. My GP is happy to do a referral for him, so it is literally just a case of getting the funds. I was quoted an estimate of roughly £9000. I’m not going to ask for people to send me that amount as I know it is a huge sum to ask for. I’m hoping to raise as much as I can by about January/February time (through donations, etsy sales, and anything I can spare from my part time job) and look at taking out a loan for whatever is left over and if I can save even a third of the full amount that would help immensely.
A hysterectomy would truly change everything. I don’t want to take depo injections for the rest of my life, I don’t want to be in pain anymore and I don’t want to bleed randomly throughout the day because I dared to go for a walk. This is not just for transition purposes, this is so I can live without fear of further pain, more bleeding, being unable to treat potential atrophy because of an existing condition, HPV, cervical cancer, pregnancy scares etc.
If you'd like to donate:
ko-fi.com/transmonstera
cashapp: £transmonstera
Even if you can’t donate, please take a moment to share. It’d mean the world to me.
#also if anyone has any questions about cervical ectropion feel free to ask! it's not talked about a lot in terms of trans healthcare#trans#transgender#transsexual#queer#trans artist#kofi#transmonstera
317 notes
·
View notes
Video
324 Morris Minor 4 door (Series V) (1968) TPG 156 F by Robert Knight Via Flickr: Morris Minor 1000 Series V (1962-72) Engine 1098cc S4 OHV Production 847,491 (Series III and Series V) Registration Number TPG 156 F (Surrey) MORRIS ALBUM www.flickr.com/photos/45676495@N05/sets/72157623690377489... Designed by Sir Alec Issigonis for William Morris's Nuffield Group the Morris Minor made its debut at the 1948 Earls Court Motorshow . The original Minor MM series was produced from 1948 until 1953, the range included a 2 door and 4 door four seater saloon, and a convertible An instant success and the baby car of its day, the new car featured rack and pinion steering, torsion bar independent front suspension and superb handling. Although the Minor was originally designed to accept a flat-4 engine, late in the development stage it was replaced by a 918 cc S4 side valve engine. The Series II was substantially re-engineered following the merger of the Nuffield Organisations merger with Austin (forming BMC), Cosmetically the car now had raised front lights in the wings, rather than at the sides of the grille. As part of a rationalisation programme to reduce the production of duplicate components for similar vehicles, the Minor drivetrain was completely replaced with an Austin-derived engine, gearbox, prop shaft, differential and axle casing. The more modern Austin-designed 803 cc (49.0 cu in) overhead valve A-series engine, designed for the Austin A30 which proved more lively than the 918cc SV it replaced. An estate version was introduced in 1952, known as the Traveller featuring an external structural ash (wood) frame for the rear bodywork, with two side-hinged rear doors. A horizontal slat grille was fitted from October 1954,[ as well as a new dashboard with a central speedometer 269,838 examples of the Series II had been built when production ended in 1956 In 1956, the Minor received a major programme of updates as the Series III Minor 1000. Now powered by a 948cc variant of the BMC A-Series engine, which increased fop speed from 63mph to 75mph. the engine was mated to a revised gearbox with longer ratios and a shorter gearchange. A series of changes to the body pressings allowed a wraparound rear windscreen and a curved front screen In 1961 the semaphore-style trafficators were replaced by flashing direction indicators In 1962 the final Series Minor 1000 (ADO 59) was launched the 'Series IV' designation having been assigned to the Morris Mini Minor. A new, larger 1098cc version of the BMC A Series engine with a Harry Weslake designed cylinder head Although fuel consumption suffered moderately at 38 mpg, the Minor's top speed increased to 77 mph and a significant increase in torque, this revised engine was mated to a new stronger gearbox and the size of the front drum brakes increased. The interior was refreshed, and revised again in 1964. Diolch am 92,828,339 o olygfeydd anhygoel, mae pob un yn cael ei werthfawrogi'n fawr. Thanks for 92,828,339 amazing views, every one is greatly appreciated. Shot 23.04.2022 at the Bicester Spring Scramble, Bicester, Oxfordshire 158-324
#Morris#British#1960s#1968#Morris.Minor#BMC#BMC.A.series#Sir.Alec.Issigonis#William.Morris#Swinging.Sixties#ADO58#Bicester.April.2022#TPG156F#Registered.in.Surrey#1945-70#Auto#Automobile#Car#cars#Classic#Motor#worldcars#flickr
21 notes
·
View notes
Text
We tend to talk about the decline in young adults’ home ownership as if it were a universal phenomenon. This is wrong. The share of 25-to-34-year-olds who own their own home in the US is six percentage points lower today than it was in 1990. In Germany it’s down eight points, in France just three, but in Britain the drop is 22 points. It’s a similar story with incomes, where Britons in their thirties are tracing the same trajectories as their forebears while Americans are leaving theirs in the dust. The conveyor belt of socio-economic progress may have slowed elsewhere in the west, but in Britain it has sheared in two, leaving a generation stranded below. As Rob Ford, professor of political science at the University of Manchester, put it to me, this has completely changed the political calculus for young people. In the old Thatcherite world, young Britons had realistic expectations of upward mobility and home ownership, and their political interests naturally lay with the party of homeowners and low taxes. Today none of these things are true. The sense of betrayal is palpable. Ben Ansell, professor of comparative democratic institutions at Nuffield College, Oxford has shown that young Britons have lost the belief in social mobility that was a given for their parents’ generation. Applying his methodology internationally, I find that just 39 per cent of British under-30s trust that hard work will bring rewards, far below those in the US (60 per cent) and Germany (49), and also far below the 60 per cent of British 70-somethings who believe the same because it was true for them.
John Burn-Murdoch, Why are young people deserting conservatism in Britain but nowhere else?
106 notes
·
View notes
Text

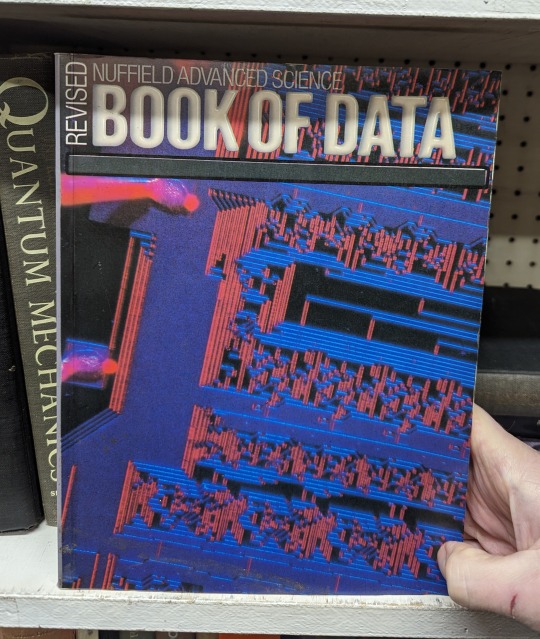

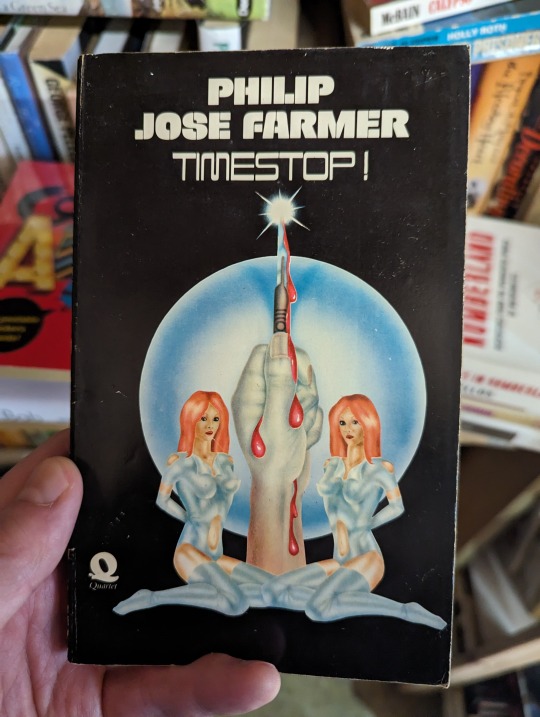

More books that caught my eye lately:
Timescape - Gregory Benford (1980)
Book of Data - Nuffield Advanced Science (1984)
Where Wizards Stay Up Late: The Origins of the Internet - Katie Hafner/Matthew Lyon (1996)
Cyber Way - Alan Dean Foster (1990)
Timestop! - Philip José Farmer (1960)
Fly Fishing - J.R. Hartley (1991)
76 notes
·
View notes
Text
I managed to get my answers on the ECHR consultation in just under the wire - two hours ahead of the deadline.
I also emailed the Joint Equalities Committee on the governments proposal of Mary-Ann Stephenson as the new head of the ECHR and copied in my MP, from whom I have received a series of particularly insulting very clearly boilerplate replies to every subject I have ripped my own heart out digging up personal fears, traumas and pain emailing about in detailed letters with both extensive factual references and extremely personal accounts of how I and people I love have been affected.
I’m writing one more email to him today regarding the Disability “Reforms” - intense and very clearly ideologically-driven cuts filled with measures that are *horrifically cruel* and, while referring to the need to “cut the benefits bill*, are full of measures that will horrifically impact millions of disabled people’s capacity to work and pay taxes because the vote on these is *tomorrow*.
I have been in a massive health flare-up since March after I broadly crashed out of the Nuffield Joint Pain programme in a storm of PEM - post-exertional malaise, a common effect of chronic fatigue conditions where one can handle a period of exertion which can be extended by careful pacing, but one will eventually will absolutely crash out and experience a period of limited function - sometimes so limited that one cannot even care for oneself in the most basic ways - that is usually at least twice the period of exertion and can be many times it.
I am not discounting the effect the absolute political war on every marginalised person in the UK and the ongoing horrific, genocidal complicity of the UK government to the actions of the Israeli government has had on me during this, tbh. I have such limited energy and I’m spending everything I’m not using on survival and the limited part of caring I do for my brother on the parts of campaigning abled people often dismiss as “slacktivism” - writing letters to my own MP and government ministers, campaigning on my FB group, Tumblr and BlueSky, sharing petitions, even calling government ministers and MPs occasionally on the phone despite the truly ridiculous effect this has on my energy levels, and, of course, giving mutual aid from my own limited finances - mostly to families in Palestine.
I still haven’t made it to an in-person protest yet because of quite how much the sensory overstimulation and energy expenditure of being upright in a load public space without rest, even in my wheelchair, would have on me. I try extremely hard not to feel bad about this.
#disabled#disability#chronic illness#chronic fatigue#pem#post exertional malaise#chronic pain#chronically ill#echr consultation bullshit#trans rights#eugenic bullshit#uk politics
10 notes
·
View notes
Text


tom mckay (william shakespeare) dedication (2016) behind the scenes
back in 2016, nuffield theatre had a weekly rehearsal blog for dedication but unfortunately, none of the photographs were archived on the wayback machine :"( (which distresses me greatly......) thankfully i was able to find at least these two pics :')
if you want to read the rehearsal blogs anyways here are all four posts!!
week 1 week 2 week 3 week 4
#tom mckay#dedication (2016)#kicking crying screaming why didn't become a tom fan sooner..........i could've saved these pics.........#i was 15 when this play premiered and was deep into kpop so there's no way i would've stumbled upon (or cared tbh) about thisNOOOOOOOO#this is so sick and twisted#if 13 year old me had seen him in julius caesar.....................i would've started this archive acc immediately afterwards........#younger me 10000% would've had the fattest crush on him.........(as if i dont have a massive platonic crush on him currently lol)
11 notes
·
View notes
Text
We've been having a lot of medication shortages recently. And for a long time, we've known that brexit was a key component, but nobody talks about brexit any more.
For example, recently it was creon - a treatment that supplements pancreatic enzymes for patients whose pancreases don't work sufficiently well.
I've had multiple patients come in angry or in distress because one of their specialist medications has been either discontinued by the UK manufacturers or is no longer being imported. These are often medications that can't easily be switched to something else without specialist advice, and there's not always a good readily available alternative. And even if there is, sometimes it's not a medication we can prescribe until you are seen by a specialist. Which sucks when there's often a 6 month to 1 year wait to see them.
To make matters worse, whilst we get notified by big shortages, your hospital docs and GPs prescribing the meds really have no way of knowing what local stocks are like most of the time until a patient or pharmacy contacts them to let them know when there's a shortage.
Though there are one or two websites we can use for larger pharmacy chains, most of the time, I have no way to check if there are local shortages. It's not built into our prescribing software.
We usually have to rely a lot on on pharmacies to keep track of shortages, monitor their stock and let us and patients know what is or isn't available.
If you're noticing shortages in your medication, talk with your pharmacy, your GP and your specialist team if you can. But just as importantly, consider raising it with your MP. Hold politicians as a group accountable for the ways in which their policies impact our healthcate system. Make sure they are aware.
8 notes
·
View notes
Text
The NHS in England is facing a “ticking timebomb” when it comes to retaining young staff, nursing leaders have warned, after new analysis showed its generation Z workers are becoming more stressed and unhappy over time.
A new report by the Nuffield Trust shows soaring dissatisfaction rates among staff in the health service’s youngest cohort, aged 21 to 30 – based on analysis of NHS surveys.
Researchers found that, between 2013 and 2023, stress levels in clinical staff aged 21 to 30 rose by 14 percentage points. In 2023, more than half (52%) said they had been made unwell through work-related stress in the previous year, compared with 38% in 2013.
But the proportion of older NHS workers – aged between 51 and 65 – who had become ill for the same reason decreased across the same period, dropping from 43% to 40%.
The report also found that the proportion of young NHS staff unhappy with their salary has doubled, from 10% in 2013 to 22% in 2023. But in older staff, there has been a much smaller increase, from 11% in 2013 to 12% in 2023.
11 notes
·
View notes
Text

Triple Threat
This is a mind on the brink of collapse – a collection of brain cells, or neurons, developed in a lab from the stem cells of a Parkinson’s disease patient. These neurons produce the chemical messenger dopamine, and are the first to show signs of the disease onset. Since the patient carried three copies of a particular gene called synuclein – a trait strongly linked to Parkinson’s disease and the degradation of neurons that it entails – these neurons are already experiencing the early stages of damage. This model of dopamine-producing neurons is a platform to investigate the molecular processes underpinning the disease, and if one picture tells 1,000 words, then this image, a composite of 8,000 individual images and coloured according to depth from top right to bottom left, could have a very detailed story to tell about Parkinson’s disease and new approaches to treatment.
Written by Anthony Lewis
Image captured at the Micron Bioimaging Facility, Oxford
Image from work by Nick Gatford
Molecular Neurodegeneration Research Group, Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, UK
Image supplied and copyright held by Nick Gatford
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#biology#immunofluorescence#stem cells#parkinson's disease#dopamine#synuclein#neurons#neuroscience
15 notes
·
View notes
Text
https://www.telegraph.co.uk/health-fitness/conditions/cancer/the-little-known-cancer-thats-linked-to-the-gut/
“The surge in cases of cancer in the under-50s has made many of us worry, with bowel, breast and lung cancers among those increasing most rapidly. But what is more surprising is that rates of aggressive gallbladder cancer have risen even more sharply, affecting many more women than men, particularly those who have had children. It’s also more likely in those who have suffered from the common problem of gallstones.
The figures are alarming, with cases having doubled in British people aged between 24 and 49 in the past three decades, according to Cancer Research UK. But the good news is that there are measures you can take to limit the risk of the disease, through changes to your diet and lifestyle.
Here, our experts explain what exactly the cancer is, the reasons it is spiking in younger people and what we can do to increase our chances of avoiding it.
What is gallbladder cancer?
The gallbladder is an apple-sized organ near the liver and is primarily responsible for storing bile, a substance produced by the liver and used by the body to break down the fats we eat.
Thousands of years ago, humans might have eaten one big meal every few days and “we might have needed that extra boost of bile to help us digest it, if the liver couldn’t produce it fast enough,” says Dr Anita Balakrishnan, a consultant hepatopancreatobiliary (HPB) surgeon at Addenbrooke’s Hospital and an associate lecturer at the University of Cambridge..
“The gallbladder is a vestigial organ, like the appendix – now we don’t really need it for normal digestion, and sometimes it causes trouble.’”
Cancer occurs when healthy cells in the gallbladder develop genetic mutations that cause them to grow and multiply out of control. Just over 1,000 cases have been diagnosed in the UK each year, equivalent to about three per day and, “sadly, it’s an aggressive cancer,” says Dr Balakrishnan.
What are the risk factors?
According to Cancer Research UK, women account for 71 per cent of cases. In women who have given birth, particularly those who have had five or more children, the risk is increased.
The reason for this is not fully known, but women are two to three times more likely to suffer from gallstones, which are a major risk factor for gallbladder cancer. Oestrogen can increase cholesterol levels in bile and decrease gallbladder contractions, which can lead crystals to form in the bile and create stones. During pregnancy, the gallbladder also grows in volume.
“Having gallstones doesn’t necessarily mean you’ll get cancer, but they cause inflammation of the gallbladder, which puts people at a higher risk,” says Mr Shahid Farid, a consultant surgeon with a specialism in gallbladder surgery at Nuffield Health Leeds Hospital.
People with a family history of gallbladder cancer are five times more likely to develop the disease, and it is more common in people of Asian descent.
Smoking and obesity also increase the risk, with the rise in obesity since the mid-1990s believed to be a major factor in the increase in cancer among younger people, in particular.
What are the main symptoms, treatment and survival rate?
Unfortunately, gallbladder cancer is often a silent disease which becomes symptomatic only in its later stages.
“Any symptoms people have are usually non-specific, such as tiredness and perhaps some abdominal discomfort,” says Mr Farid.
Eventually, symptoms can include jaundice, pain in the upper right abdomen, weight loss, nausea and vomiting. “By that stage, it has usually grown beyond the gallbladder and is at an advanced stage,” he says.
It is often detected by chance during operations, for instance to remove gallstones, and if it is contained within the gallbladder, the five-year survival rate is 60-70 per cent. If it has spread to local tissues or lymph nodes, survival rates are almost 30 per cent, while if it has spread to more distant areas, rates are under 5 per cent.
If possible, treatment involves surgery, along with chemotherapy.
What can we do to minimise our risk?
1. Maintain a healthy weight
Being overweight and obese is the second biggest cause of cancer in the UK, after smoking. Several studies have found a link between an increased risk of gallbladder cancer and a BMI of over 25, with the World Cancer Research Fund stating that the risk increases by 25 per cent per 5 kg/m2 increase in BMI.
One recent Norwegian study found a concerning 47 per cent increased risk in women per 5 kg/m2 increase in BMI, while the increased risk in men was smaller and not statistically significant. It also showed a decreased survival rate for overweight and obese women with gallbladder cancer.
“Eating a healthy diet and staying within a healthy BMI range will help avoid gallbladder cancer,” says Dr Balakrishnan. “Giving up smoking and keeping alcohol consumption under recommended limits is also vital.”
2. Look after your microbiome
In recent years, scientists have increasingly focused on the microbiome, the ecosystem of bacteria which populates the gut, when searching for causes of the increase in early-onset cancers.
“Research into the influence of the microbiome on cancers including gallbladder cancer is still in its early days, but it’s only logical that it plays a part,” says Mr Farid. “Our microbiome can contribute to inflammation, and that can predispose us to cancer.”
A Chinese study from 2023 investigated the microbiome of patients with biliary tract cancers, of which gallbladder cancer is one. It found patients with the disease had increased levels of the Enterobacteriacae bacteria, and decreased levels of others including Clostridia, suggesting an imbalance. Both are associated with inflammation.
We can boost the diversity and good bacteria in our microbiome with fermented foods such as kefir, sauerkraut and kimchi, and prebiotic foods like mushrooms, onions, garlic, asparagus, leeks and apples, which feed the bacteria in our gut.
Good bacteria such as Clostridia can naturally be found in food such as vegetables, while high-fibre foods such as fruit, wholegrains and nuts will also nurture the microbiome.
3. Avoid fried, fatty foods and sugary drinks
The link between different types of diet and higher rates of gallbladder cancer is still being researched, but some studies have highlighted certain principles by which it’s best to live.
Eating too many fatty and fried foods have been linked to an increased chance of getting the disease because they raise cholesterol which is linked to gallstones, which are in turn strongly linked to gallbladder cancer.
Red meat, and particularly processed meat containing nitrates, is also associated with a higher risk, so cutting down to 455g of cooked lean red meat per week is recommended.
Drinking sugar-sweetened and artificially sweetened beverages has been shown to double the risk of gallbladder cancer when individuals drank 400ml or more per day. This is thought to be because increased sugar consumption is linked to a higher BMI, and also to Type 2 diabetes, which increases the risk of cancer.
Ultra-processed foods (UPFs) are linked to a higher incidence of all cancers, and researchers believe they may be a major driver of the increase in cancers among under-50s. “Reducing the amount you consume and eating unprocessed food where possible is best,” says Mr Farid.
4. Eat the DASH diet
One Swedish study revealed that two types of healthy diet are associated with a lower risk. One is the Dietary Approach to Stop Hypertension, or DASH, which includes fruits, vegetables, whole grains, low-fat dairy, and lean protein from chicken, fish, beans and nuts. It avoids foods high in salt, saturated fat, and added sugar. The second is the Mediterranean diet, which follows very similar principles.
One Indian study reported that eating sweet potatoes was associated with a lower risk of gallbladder cancer, along with green chillis, radish, mango, orange and melon – all of which contain high levels of antioxidants.
5. Exercise regularly
Regular physical activity has been shown to be likely to reduce the risk of gallbladder cancer, and studies have shown it can increase the diversity of the gut microbiome.
“Exercise also promotes cell turnover in a different way to when you’re sedentary,” says Mr Farid. “It also reduces the amount of fat and also inflammatory cytokines in your blood. So it’s one of the most important things you can do to modify your risk of many cancers, including gallbladder.””
6 notes
·
View notes

