#neuroregeneration
Explore tagged Tumblr posts
Text
youtube
#Spinal cord injury#neuroregeneration#nanomedicine#mitochondrial therapy#silica nanoparticles#dual-responsive nanoparticles#targeted drug delivery#neuroprotection#regenerative medicine#oxidative stress#inflammation control#apoptosis inhibition#cellular repair#tissue regeneration#advanced therapeutics#biomaterials#neuroscience research#precision medicine#theranostics#medical breakthrough.#Youtube
2 notes
·
View notes
Text

Causes Of Optic Nerve Damage.
The optic nerve is made up of nerve fibers that send signals to the brain. In the case of optic atrophy, something is interfering with the optic nerve’s ability to communicate these impulses. The interference can be caused by numerous factors, including: Stroke of the optic nerve, known as anterior ischemic optic neuropathy. A tumor that is pressing on the optic nerve. Optic neuritis is an optic nerve inflammation caused by multiple sclerosis.
https://www.globalstemcellcare.com/ey...
#OpticNerve#StemCells#OpticNerveRepair#StemCellTherapy#OpticNerveRegeneration#NeuroRegeneration#StemCellsForVision#NeuroScience#VisionRestoration#OpticNerveDamage#StemCellResearch#EyeHealth#StemCellTherapyForEyes#Ophthalmology#Neurodegeneration#GSCC#GlobalStemCellCare
0 notes
Text
Future curative therapy for the inherited metabolic disorder IEMS: cell therapy and neural regenerative medicine
Cell therapy is the transfer of whole cells into a patient to replace or repair damaged tissue or cells. Cell therapy treats disease or trauma by transferring healthy cells into a patient’s body to grow, replace or repair damaged tissue. The cells used in cell therapy may come from the patient (autologous cells) or from a donor (allogeneic cells). 一、 Introduction to Cell Therapy1. Understanding…

View On WordPress
0 notes
Text

Dr. Suga Syoujirou (434334633)
Gender: Male Age: 24 Department: Biology Specialty: Neuroregeneration and Neural Repair Likes: Cats Dislikes: Green peppers Fact: Has a chronic ear condition that requires him to wear a hearing aid.
"I'd like to report an incident that involves Dr. Toranosuke and I'd really prefer not to file it directly with him." Read Staffside here!
84 notes
·
View notes
Text

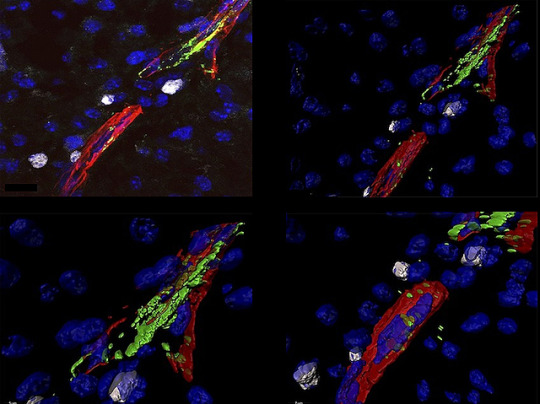
Sugar and Sprouts
Love sugar? Too much can damage your blood vessels, increasing your risk of diabetes and cardiovascular disease. Love artificial sweeteners? Unfortunately, they too may increase your risk of cardiovascular disease. Researchers investigated in zebrafish embryos. Fluorescence microscopy revealed exposing embryos to lots of sugar or artificial sweeteners caused excessive blood vessel sprouting (angiogenesis) along the length of the body (pictured) – a process linked to diabetic complications in humans, including cardiovascular disease. Looking closer at embryos exposed to artificial sweeteners, they found cells lining their blood vessels (endothelial cells) developed into cells that promote sprouting. Analysing the RNA of these cells revealed changes in gene activity, notably reduction of one, Foxo1a (highlighted in red in the vessels along the fish embryo), was underlying the increase in sprouting when the embryos were exposed to sugar. Further experiments confirmed activity of this gene played the same role in embryos exposed to artificial sweeteners, uncovering how these sugar alternatives can negatively affect blood vessels.
Written by Lux Fatimathas
Image from work by Xiaoning Wang, Jinxiang Zhao and Jiehuan Xu, and colleagues
Affiliated Hospital of Nantong University, Nantong Laboratory of Development and Diseases, School of Life Science; Co-innovation Center of Neuroregeneration, Nantong University, Nantong, China
Image contributed by the authors under a Creative Commons Attribution 4.0 International (CC BY 4.0) licence
Published in eLife, October 2024
You can also follow BPoD on Instagram, Twitter , Facebook and Bluesky
#science#biomedicine#immunofluorescence#biology#blood vessels#cardiovascular diseases#diabetes#sugar#sugar substitutes#zebrafish#angiogenesis
12 notes
·
View notes
Text
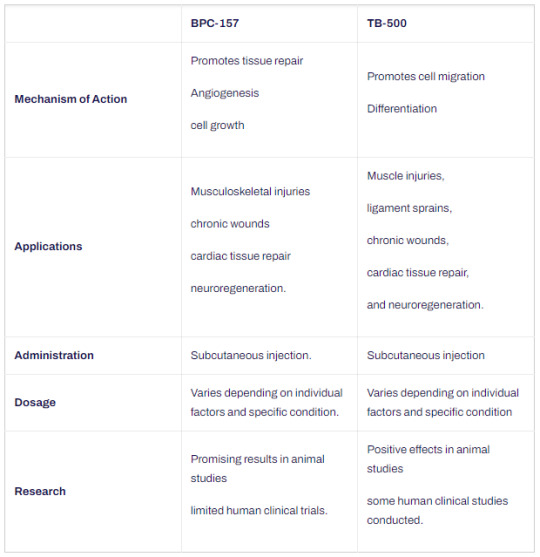
BPC-157 VS TB-500
1. What is BPC-157?
BPC-157 (also known as PL 14736, BPC 157) is a pentadecapeptide comprising 15 amino acids. It is derived from the body protection compound (BPC) found and isolated from human gastric juice. Animal studies have demonstrated its ability to expedite the healing process for various types of injuries, including muscle, tendon, and ligament damage. Moreover, BPC 157 has exhibited organ-protective properties and has been found to aid in the prevention of gastric ulcers.
2. What is TB-500?
Thymosin Beta-4 is a peptide consisting of 43 amino acids. In animal models, Thymosin Beta-4 has demonstrated the ability to enhance blood vessel growth, regulate wound healing, decrease inflammation, and reducel oxidative damage in both the heart and central nervous system. It plays a significant role in protecting, repairing, regenerating, and remodeling injured or damaged tissues. Additionally, Thymosin Beta-4 has garnered considerable attention in anti-aging research.
3. BPC-157 VS TB-500
The following is a comparison of BPC-157 and TB-500 (tb500 peptides).
(1) BPC-157
Mechanism of Action: BPC-157 promotes tissue repair, angiogenesis, and cell growth.
Applications: It is beneficial for musculoskeletal injuries, gastrointestinal disorders, and neurodegenerative conditions.
Administration: BPC-157 is typically administered through subcutaneous or intramuscular injection.
Dosage: There is no standardized dosage established for BPC-157S Research: Promising results have been observed in animal studies, but limited human clinical trials have been conducted.
(2) TB-500
Mechanism of Action: TB-500 promotes cell migration, differentiation, and tissue repair.
Applications: It is commonly used for muscle injuries, ligament sprains, chronic wounds, cardiac tissue repair, and neuroregeneration.
Administration: TB-500 is administered via subcutaneous injection.
Dosage: The dosage varies depending on individual factors and specific conditions.
Research: Positive effects have been observed in animal studies, and some human clinical studies have been conducted.
Further research is necessary to establish the efficacy and safety of both BPC 157 and TB 500 in humans. When considering their usage, dosage, and potential interactions, it is advisable to consult with a healthcare professional.
Additionally, individuals interested in comparing the benefits (tb 500 benefits) and potential differences between TB-500 and BPC-157 should seek professional guidance. It’s also important to note that there is a specific blend dosage available for BPC-157 and TB-500 (BPC-157 TB-500 blend dosage), which may offer unique effects.
3 notes
·
View notes
Text
Why Neuroquiet is the Next Big Thing in Neuroscience

Neuroscience has long been a field of rapid advancements, with groundbreaking discoveries in brain function, neuroplasticity, and mental health. One of the most promising emerging concepts in this field is Neuroquiet, a revolutionary approach to understanding and optimizing neural activity. Unlike traditional neuroscience models that focus primarily on stimulation and excitation, Neuroquiet emphasizes the power of neural silence, rest, and modulation in enhancing cognitive function, mental well-being, and neurological health.
This article delves into why Neuroquiet is the next big thing in neuroscience, exploring its scientific foundation, potential applications, and its role in reshaping our understanding of brain function.
Understanding Neuroquiet
Neuroquiet is based on the principle that quiet neural states play a crucial role in cognition and overall brain health. While traditional neuroscience has focused on excitatory activity, recent research highlights the importance of neural inhibition, rest, and synchronization in optimal brain function. The concept suggests that periods of reduced activity are not just passive states but active processes that contribute to memory consolidation, emotional regulation, and even neuroprotection.
The Science Behind Neuroquiet
Several key findings in Neuroquiet support the importance of quiet neural states:
Neural Inhibition and Cognitive Clarity
The brain operates on a balance between excitatory and inhibitory signals. Too much excitation leads to neural overload, while proper inhibition allows for focused thinking and decision-making.
Studies on gamma-aminobutyric acid (GABA), the brain’s primary inhibitory neurotransmitter, reveal that higher GABA levels improve focus, reduce anxiety, and enhance cognitive function.
The Role of Rest in Brain Optimization
Rest states, including sleep and meditation, allow for synaptic pruning, the process of removing unnecessary neural connections to optimize brain efficiency.
Research on default mode network (DMN) activity shows that quiet brain states are essential for creativity, self-reflection, and problem-solving.
Neuroprotection and Longevity
Continuous neural activity can lead to oxidative stress, neuroinflammation, and cognitive decline. Neuroquiet promotes brain longevity by reducing stress-related damage and enhancing neural repair mechanisms.
Studies on meditation, breathwork, and deep relaxation show that these practices reduce cortisol levels, slow down brain aging, and improve neuroplasticity.
Applications of Neuroquiet
The potential applications of Neuroquiet span across multiple disciplines, including mental health, cognitive enhancement, neurorehabilitation, and artificial intelligence (AI).
1. Mental Health and Stress Reduction
Neuroquiet offers a scientific foundation for mindfulness, meditation, and breathwork as effective tools for managing stress, anxiety, and depression.
Techniques that promote Neuroquiet, such as progressive relaxation and vagus nerve stimulation, can significantly improve emotional resilience and reduce mental fatigue.
2. Cognitive Enhancement and Learning
By understanding the role of quiet brain states in memory consolidation, educators and cognitive trainers can implement better learning strategies.
Techniques like spaced repetition, deep focus periods, and strategic breaks can optimize knowledge retention and cognitive performance.
3. Neurorehabilitation and Recovery
Neuroquiet can play a crucial role in stroke recovery, traumatic brain injury (TBI) rehabilitation, and neurodegenerative disease management.
Non-invasive brain stimulation techniques, guided relaxation therapies, and biofeedback systems are being developed to harness Neuroquiet principles for faster healing and neuroregeneration.
4. Artificial Intelligence and Brain-Inspired Computing
Neuroquiet has implications for AI and computational neuroscience, where neural silence can improve energy efficiency and decision-making in artificial systems.
The concept is inspiring new models in neuromorphic computing, where AI mimics the brain’s inhibitory-excitatory balance to enhance efficiency.
The Future of Neuroquiet in Neuroscience
The integration of Neuroquiet into neuroscience research and clinical practice is still in its early stages, but the growing body of evidence suggests that it has the potential to transform how we approach brain health and cognitive performance.
Research and Innovations
Future research will focus on developing biomarkers for neural quietness, allowing for more precise tracking of brain states in real-time.
Advanced neuroimaging technologies will provide deeper insights into how Neuroquiet states contribute to well-being and performance.
Innovations in wearable neurotechnology will make it easier for individuals to monitor and optimize their neural quiet states.
Integrating Neuroquiet into Everyday Life
As awareness of Neuroquiet grows, more individuals will adopt lifestyle practices that enhance neural quietness, such as meditation, deep breathing, and digital detoxing.
Companies and organizations may integrate Neuroquiet principles into workplace productivity models to reduce burnout and enhance employee well-being.
Personalized neurofeedback and brain-training programs will likely incorporate Neuroquiet-based strategies for optimized mental performance.
Conclusion
Neuroquiet is set to redefine neuroscience by shifting the focus from neural excitation to the power of quietness in optimizing brain function. Its implications for mental health, learning, neurorehabilitation, and AI make it one of the most exciting frontiers in the field. As research continues to uncover the profound benefits of neural quiet states, Neuroquiet will play a pivotal role in shaping the future of brain science, therapy, and human potential.
0 notes
Text
Stem Cell Therapy for Multiple Sclerosis: A Promising Frontier in Treatment

Multiple sclerosis (MS) is a challenging autoimmune disorder that affects millions worldwide. As researchers continue to seek more effective treatments, stem cell therapy has emerged as a promising avenue for managing and potentially modifying the course of this disease. This blog post explores the current landscape of stem cell therapy for MS, its potential benefits, challenges, and what patients should know.
Understanding Stem Cell Therapy for MS
Stem cell therapy for MS aims to achieve three primary goals:
Reduce inflammation and demyelination
Repair or replace damaged nerve tissue
Promote neuroregeneration
These objectives address the core issues of MS, potentially offering hope for improved outcomes and quality of life for patients.
Types of Stem Cells Used
Researchers are exploring several types of stem cells in MS treatment:
Mesenchymal Stem Cells (MSCs): Derived from bone marrow, fat tissue, or umbilical cord tissue.
Hematopoietic Stem Cells (HSCs): Obtained from bone marrow or peripheral blood.
Neural Stem Cells (NSCs): Sourced from fetal brain tissue or induced pluripotent stem cells (iPSCs).
Each type of stem cell offers unique properties and potential benefits in treating MS.
Potential Benefits
Stem cell therapy shows promise in several areas:
Reduced relapse rates
Improved cognitive function
Enhanced motor function
Decreased fatigue
Potential for disease modification
These benefits could significantly improve the lives of MS patients, offering hope for better management of symptoms and potentially slowing disease progression.
Current Research and Trials
The scientific community is actively investigating stem cell therapies for MS through various approaches:
Autologous Hematopoietic Stem Cell Transplantation (AHSCT)
Mesenchymal Stem Cell Transplantation (MSCT)
Neural Stem Cell Transplantation (NSCT)
These trials aim to establish the safety and efficacy of different stem cell therapies in treating MS.
Challenges and Limitations
Despite its promise, stem cell therapy for MS faces several challenges:
Variability in stem cell sources and protocols
Limited understanding of MS pathology
Potential risks (infection, graft-versus-host disease)
High cost and limited accessibility
Researchers and clinicians are working to address these challenges to make stem cell therapy a more viable option for MS patients.
Clinics and Centers Offering Stem Cell Therapy for MS
Several institutions worldwide are at the forefront of stem cell therapy for MS:
Cleveland Clinic (USA)
University of California, San Francisco (USA)
Medtravellers Stem Cell Therapy (India)
San Raffaele Hospital (Italy)
Apollo Hospitals (India)
It’s important to note that insurance coverage for these treatments is limited, and most are still considered experimental.
Before Considering Stem Cell Therapy
If you’re an MS patient considering stem cell therapy, it’s crucial to:
Consult a neurologist or MS specialist
Research reputable clinics and trials
Understand potential risks and benefits
Ensure informed consent
Conclusion
Stem cell therapy represents a promising frontier in the treatment of multiple sclerosis. While challenges remain, ongoing research and clinical trials offer hope for improved outcomes and quality of life for MS patients. As with any emerging treatment, it’s essential for patients to stay informed, consult with medical professionals, and carefully consider their options.
Source Link:- https://www.medtravellers.com/blog/stem-cell-therapy-for-multiple-sclerosis-ms/
0 notes
Text
#Advanced Education and e-Learning#Audiology programmes#Optometry programmes#Neuroscience programmes#Speech & Language programmes
0 notes
Text
UP patient with BILATERAL OPTIC ATROPHY and TINNITUS received retrobulbar exosome and stem cell therapy.
Optic nerve disorders can cause vision problems in one or both eyes because the optic nerve carries images from the eye to the brain. Stem cell treatment is a promising option for helping with these issues. By placing special stem cells into the eye's jelly-like center, we can improve the layer of nerve cells in the retina and help these cells move into the optic nerve. This method has shown high probability of better results, offering hope for people with optic nerve disorders.
Email id- [email protected] Ph no- +91 82876 76389 https://www.globalstemcellcare.com/eye-disorder/stem-cell-treatment-for-optic-nerve-atrophy/
#Stemcell#Exosome#AdvanceTreatment#CellRegeneration#BILATERALOPTICATROPHY#BilateralOpticAtrophy#Tinnitus#ExosomeTherapy#StemCellTherapy#VisionHealth#Neuroregeneration#Ophthalmology#InnovativeTreatment#OpticNerveHealth#RegenerativeMedicine#PatientCare#ClinicalResearch#EyeHealth#Neuroscience#VisionRestoration#TherapeuticAdvancements
0 notes
Text
Patient's Attendant Share His Experience After Stem Cell Therapy For Cerebral Palsy
Stem cell therapy holds promise in the treatment of cerebral palsy, a complex neurological disorder affecting movement and posture. This innovative approach involves the use of undifferentiated cells, capable of differentiating into various cell types, to repair damaged tissues and promote functional recovery.
In cerebral palsy, stem cell therapy aims to replace or repair damaged brain cells, enhance neuroregeneration, and modulate the inflammatory response.
Email id- [email protected]
Ph no- +91 9650760803
#cerebralpalsy#stemcelltherapyforcerebralpalsyinindia#costofcerebralpalsytreatment#stemcelltherapyforcpchild#stemcells#cerebralpalsytreatment#seizure#epilepsy#specializeg_growt_factor#supportive_therapy#beststemcellcenterinindia#stemcelltreatment#exosometherapy#dietconsultant#physiotherapysession
0 notes
Text
Not Just Clots
Neurons are wrapped in a fatty material called myelin which acts like an insulator keeping nervous signals on their intended path. As this wrapper is damaged in multiple sclerosis (MS), stimulating re-myelination from its producer cells – oligodendrocytes – is a therapeutic goal. Here, the influence of the blood's platelets on oligodendrocyte progenitor cells is revealed – manipulating platelets presents possibilities for MS treatments
Read the published research article here
Image from work by Amber R Philp and colleagues
Laboratory of Stem Cells and Neuroregeneration, Institute of Anatomy, Histology and Pathology, Faculty of Medicine, Universidad Austral de Chile, Valdivia, Chile
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in eLife, August 2024
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#immunofluorescence#biology#neuroscience#brain#neurons#myelin#multiple sclerosis#platelets
4 notes
·
View notes
Text
There are, interestingly so, magazines that his friends at Dynatox send him. Cutting-edge biotechnology that some of their sister companies are developing, shrouded in secrecy. Neuroregeneration. There are protocols aiming to restore life to deceased organisms using advanced cellular reprogramming and medicine techniques, a fusion of the new and old. DNA is being tested. The theory is based upon the profound understanding of cellular dormancy and reversible metabolic stasis. They’re all big words that Terry recognizes vaguely from some of his private schooling, but a note Margaret attaches draws his attention. For John.
He sinks into the water. Dormancy. John is only dormant, frozen to time. Terry thinks about dipping him in the warmth of these pools, pulling him out as John baptized Jesus, resurrecting him in some ceremonial action. It’s a silly thought, and yet.
And yet.
Chapter 2 of In a Real Death Waltz is out! This time, we see what happens following the events of the cage :-) Hope you enjoy reading!
1 note
·
View note
Text
Can Spinal Cord Injuries be repaired? Spine doctor in Dwarka, Delhi
In Dwarka, Delhi, a beacon of hope shines for those affected by spinal cord injuries. With advancements in medical science, the question arises: Can Spinal Cord Injuries be repaired? Dr. Nagesh, a renowned spine doctor in Dwarka, Delhi, leads the charge in exploring this frontier.
Spinal cord injuries, once considered irreversible, now face a new era of possibility. Dr. Nagesh's practice integrates cutting-edge research with compassionate care, offering patients a pathway towards recovery. Through innovative treatments such as stem cell therapy, neuroregeneration, and advanced surgical techniques, Dr. Nagesh strives to restore function and improve quality of life for those with spinal cord injuries.
Furthermore, Dr. Nagesh's clinic serves as a hub for interdisciplinary collaboration, fostering partnerships with leading researchers and clinicians worldwide. By harnessing collective expertise, they aim to accelerate progress in spinal cord repair and redefine the limits of rehabilitation.
Beyond medical interventions, Dr.Nagesh emphasizes holistic support, recognizing the profound impact of spinal cord injuries on mental, emotional, and social well-being. Through tailored rehabilitation programs and comprehensive patient education, individuals are empowered to navigate their journey towards healing with resilience and optimism.
In Dwarka, Delhi, the quest to repair spinal cord injuries is not merely a question, but a beacon of hope illuminating the path towards a brighter future. Dr. Nagesh and their team stand at the forefront, dedicated to turning the tide of adversity into opportunities for restoration and recovery.\
You can contact us by:
Phone: +91 9818776763
Email: at Dr. Nagesh Chandra, Top Neurologist in Delhi
Website: Best Brain & Spine Treatment in Delhi
Visit us: at Dr. Nagesh Chandra, Top Neurologist in Delhi
#SPINE DOCTOR IN DELHI#SPINE SURGERY IN DELHI#SCOLIOSIS TREATMENT IN DELHI#NEUROSURGEON IN DELHI#BEST NEUROSURGERY SPECIALIST IN DELHI
0 notes
Text
Fighting Parkinson's: Insights into the Parkinson's Disease - Drug Pipeline Landscape
Parkinson's disease (PD) is a progressive neurodegenerative disorder that affects millions of people worldwide, causing a range of motor and non-motor symptoms that can significantly impact quality of life. While there are currently medications available to manage symptoms, there remains an urgent need for more effective treatments that can slow or halt the progression of the disease. In this article, we delve into the Parkinson's disease drug pipeline landscape, examining promising therapies and innovations that offer hope for patients and caregivers.
The Parkinson's disease drug pipeline is a dynamic and rapidly evolving space, with pharmaceutical companies, academic institutions, and research organizations around the world actively pursuing novel therapeutic approaches to address the underlying pathology of the disease. These approaches target various aspects of PD pathology, including the loss of dopamine-producing neurons in the brain, the accumulation of abnormal protein aggregates known as Lewy bodies, and the neuroinflammation and oxidative stress that contribute to neuronal damage.
One area of active research in the Parkinson's disease drug pipeline is the development of disease-modifying therapies that aim to slow or stop the progression of the disease by protecting and preserving dopamine-producing neurons in the brain. These therapies target mechanisms involved in neuronal survival, neuroprotection, and neuroregeneration, with promising candidates including growth factors, neurotrophic factors, and small molecules that modulate cellular pathways implicated in PD pathogenesis.
Request the sample copy of report @ https://www.globalinsightservices.com/request-sample/GIS31241
Another focus of research in the Parkinson's disease drug pipeline is the development of symptomatic therapies that address the motor and non-motor symptoms of the disease, such as tremors, rigidity, bradykinesia, and cognitive impairment. These therapies aim to improve quality of life and functional independence for patients by enhancing dopamine signaling, restoring neurotransmitter balance, and targeting specific symptom clusters associated with PD. Promising candidates in this category include novel formulations of existing medications, as well as innovative drug delivery systems that improve bioavailability and reduce side effects.
Additionally, there is growing interest in the development of disease-modifying therapies that target alpha-synuclein, a protein implicated in the pathogenesis of PD due to its role in the formation of Lewy bodies and neuronal toxicity. Strategies to inhibit alpha-synuclein aggregation, promote its clearance from the brain, or prevent its spread between neurons hold promise for slowing disease progression and potentially preventing the onset of PD in at-risk individuals.
Furthermore, the Parkinson's disease drug pipeline is increasingly incorporating innovative approaches such as gene therapy, cell-based therapies, and precision medicine strategies that target specific genetic subtypes of the disease. Gene therapy approaches involve delivering therapeutic genes directly to the brain to restore normal cellular function, while cell-based therapies involve transplanting dopamine-producing cells or stem cells into the brain to replace damaged neurons and restore motor function. Precision medicine approaches involve tailoring treatment regimens based on individual patient characteristics, such as genetic mutations, biomarker profiles, and disease stage.
In conclusion, the Parkinson's disease drug pipeline is a promising and dynamic field that holds hope for millions of patients worldwide. With advancements in basic science, drug discovery, and clinical research, researchers and clinicians are making significant strides towards developing more effective treatments that can slow, stop, or even reverse the progression of the disease. While challenges remain, including the need for better biomarkers, more reliable animal models, and improved clinical trial design, the collective efforts of the scientific community offer optimism for the future of Parkinson's disease treatment and management.
0 notes
Text
What is the difference between physiotherapy and Neurotherapy?
In the realm of healthcare, both physiotherapy and neurotherapy play crucial roles in improving patients' well-being and restoring functionality. However, despite some similarities, these two disciplines differ significantly in their approaches and focus areas.
Physiotherapy:
Physiotherapy, also known as physical therapy, encompasses a broad spectrum of treatments aimed at enhancing mobility, function, and quality of life. It addresses musculoskeletal and neurological conditions through exercise, manual therapy, and other modalities. Here are some key aspects of physiotherapy:
Musculoskeletal Focus: Physiotherapy primarily deals with conditions affecting muscles, bones, joints, and soft tissues. Common issues include sprains, strains, fractures, arthritis, and post-surgical rehabilitation.
Range of Techniques: Physiotherapists employ a diverse range of techniques, including exercises, stretches, massages, ultrasound therapy, electrical stimulation, and heat/cold therapy. These interventions are tailored to address specific patient needs and goals.
Functional Rehabilitation: The ultimate goal of physiotherapy is to restore optimal function and mobility. Therapists work closely with patients to improve strength, flexibility, balance, and coordination, enabling them to perform daily activities with greater ease.
How does Physiotherapy work?
Assessment and Evaluation: The process begins with a thorough assessment by a qualified physiotherapist. This assessment involves gathering information about the patient's medical history, current symptoms, mobility limitations, and functional goals. Physical examinations, including tests of strength, flexibility, balance, and range of motion, are also conducted to identify areas of concern.
Individualized Treatment Plan: Based on the assessment findings, the physiotherapist develops a customized treatment plan tailored to the patient's specific needs and goals. This plan may include a combination of therapeutic exercises, manual therapy techniques, modalities, and education on self-management strategies.
Therapeutic Exercises: Exercise therapy is a cornerstone of physiotherapy. Patients are guided through a series of exercises designed to improve strength, flexibility, endurance, balance, and coordination. These exercises are selected to target specific muscle groups or movement patterns related to the patient's condition.
Neurotherapy:
Neurotherapy, on the other hand, focuses specifically on conditions affecting the nervous system, including the brain, spinal cord, and peripheral nerves. It involves targeted interventions aimed at improving neurological function and managing symptoms related to neurological disorders. Here are some key aspects of neurotherapy:
Neurological Disorders: Neurotherapy is designed to address a wide range of neurological conditions, such as stroke, traumatic brain injury, spinal cord injury, multiple sclerosis, Parkinson's disease, and neuropathy.
Specialized Techniques: Neurotherapists utilize specialized techniques tailored to stimulate neural pathways, enhance neuroplasticity, and promote neuroregeneration. These may include neurofeedback, cognitive rehabilitation, sensory integration therapy, and neuromuscular re-education.
Functional Restoration: Similar to physiotherapy, neurotherapy aims to restore function and improve quality of life. However, it places particular emphasis on optimizing neurological function, facilitating recovery of lost abilities, and maximizing independence in daily activities.
How does neurotherapy use?
Assessment and Evaluation: The process typically begins with a comprehensive assessment conducted by a qualified neurotherapist. This assessment may include gathering information about the patient's medical history, symptoms, cognitive functioning, and behavioral patterns. Additionally, neuroimaging techniques such as EEG (electroencephalography) may be used to measure brainwave activity and identify any aberrant patterns associated with the patient's condition.
Identification of Treatment Targets: Based on the assessment findings, specific treatment targets are identified. These targets may vary depending on the patient's symptoms and underlying neurological condition. Common treatment goals include improving attention, concentration, memory, mood regulation, and cognitive function.
Neurofeedback Sessions: Neurotherapy primarily involves neurofeedback sessions, during which the patient is connected to a neurofeedback system that monitors brainwave activity in real time. Typically, sensors are placed on the scalp to measure electrical signals produced by the brain. These signals are then processed and displayed on a computer screen as visual or auditory feedback.
Long-Term Maintenance and Follow-Up: After completing a course of neurotherapy, patients may benefit from periodic maintenance sessions to sustain treatment gains and address any relapse or new symptoms that arise over time. Follow-up assessments and monitoring help track progress and adjust treatment as needed to support ongoing well-being.
Key Differences:
While both physiotherapy and neurotherapy share the overarching goal of improving patients' health and function, they differ in their scope and focus areas. Physiotherapy primarily addresses musculoskeletal conditions and rehabilitation, whereas neurotherapy specializes in neurological disorders and interventions targeted at the nervous system.
In summary, physiotherapy and neurotherapy are complementary disciplines within the field of rehabilitation, each offering valuable expertise in distinct areas of healthcare. By understanding the differences between these two modalities, individuals can make informed decisions about their treatment options and access the most appropriate care for their needs.
For individuals seeking the best neurotherapy and physiotherapy agency in Bangladesh, Care 24 BD stands out as a reputable provider offering comprehensive services tailored to neurological and musculoskeletal rehabilitation needs. With a team of skilled professionals and a commitment to excellence, Care 24 BD strives to deliver personalized care and positive outcomes for every patient.
1 note
·
View note