#neuroimmune
Explore tagged Tumblr posts
Text
Thing about being disabled in youth is they say it’s not so bad, could be worse, will get better. I’m getting older + sicker in new ways with every year. Empty masturbatory words of empathy shut-off. Their support however? Could have spared me the anguish of spoonie isolation.
28 notes
·
View notes
Text
Very rude that fun spoons are still spoons
#my body is committing hate crimes against me#me/cfs#PEM#post exertional neuroimmune exhaustion#fibromyalgia#chronic illness#disability#migraine#postural orthostatic tachycardia syndrome#chronic fatigue#chronic pain#pots#gastroparesis#MCAS#interstitial cystitis#hEDS
1K notes
·
View notes
Text
May is ME/CFS Awareness Month!
ME/CFS stands for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Chronic Fatigue (CF), a symptom of many chronic illnesses, is not the same as Chronic Fatigue Syndrome (CFS). There is a push for ME/CFS to be exclusively known as Myalgic Encephalomyelitis (ME) in the future
ME/CFS is a complex, fluctuating, chronic medical condition affecting multiple body systems and symptoms can change unpredictably
Post-exertional malaise (PEM) is the hallmark of ME/CFS
More on symptoms: Symptoms of ME/CFS
ME/CFS affects an estimated 836,000 to 2.5 million Americans, the majority of those diagnosed being AFAB
An estimated 90% of people with ME/CFS are undiagnosed
About 25% of people with ME/CFS are bedbound or housebound for long periods
Most of those diagnosed never regain their pre-disease level of functioning
The root cause of ME/CFS is unknown
Possible triggers include: viral infections (such as mono, the flu, or COVID-19), bacterial infections, physical or psychological stress, and immune system changes. There may also be a genetic component
There is no cure or approved treatment for ME/CFS
However, some symptoms can be treated. For example, PEM is treated by pacing. More on treatments: Treatment of ME/CFS
ME/CFS costs the US economy about $17 to $24 billion annually in medical bills and lost incomes
The ME Association and the CDC have more in-depth articles on ME/CFS for more information
#me/cfs#me/cfs awareness month#me/cfs awareness#myalgic encephalomyelitis#chronic fatigue syndrome#millions missing#chronic illness#disability#invisible disability#neuroimmune disorder#fatigue#post exertional malaise#pem#post exertional malaise awareness#pem awareness#post viral illness#me awareness#cfs awareness#long covid#awareness month
124 notes
·
View notes
Text
anyway it kinda sorta feels like my life is just now starting.
#i'm 25 and for the first time i'm not wondering what's wrong with me.#now i KNOW what's wrong with me and that means i can HANDLE IT.#and look at me. i'm handling it!!!!#i can't believe i spent my entire life thinking i was weak and lazy.#i am. perhaps. very strong and brave for spending my entire adult life so far advocating for myself#in the face of family and professionals who all tried to convince me i just needed to try harder.#like. maybe actually i'm a bad bitch for being the only one out here fighting for answers#even when the answers were fucking scary and nobody else believed in my experiences!!#i've had irl folks cringe at how open i am about my diagnoses. but like.#i'm autistic i've got adhd and bipolar ii and i'm disabled with hEDS and associated neuroimmune conditions#and i'm going to be SO annoying about it because I WORKED HARD TO FIGURE THIS SHIT OUT.#SORRY IF IT MAKES YOU RE-EVALUATE YOUR ASSUMPTIONS ABOUT ME. ABOUT PEOPLE LIKE ME.#because i've re-evaluated my assumptions about me. and i feel so much fucking peace.#because i'm finally learning how to take care of myself properly.#and for the first time since i was 18 years old. i feel genuinely hopeful that i might actually get to enjoy my life.#ANYWAY Uhh i gotta go to bed. GOODNIGHT.#izzy.txt
21 notes
·
View notes
Text

leonora carrington - the hearing trumpet
this womb’s a house 🕳 reading this in a flare
6 notes
·
View notes
Text
There's so much to do and so much I WANT to do but i am. sososick
3 notes
·
View notes
Text
I feel insane seeing stuff like this because this research already exists for Myalgic Encephalomyelitis, a post viral condition caused by multiple types of viral infections that a LOT of people with "Long Covid" meet the diagnostic criteria for.
This article mentions that ME/CFS is a "similar complex condition" but that's DEEPLY underreporting the similarities. The phrase "post exertional malaise" (now researchers are trying to replace it but this article uses that phrase) was INVENTED for ME/CFS. It's the only known condition, before "long covid", that causes these kinds of symptoms after exertion!
It's good to know for sure that it's the same mechanisms at play when the inciting viral infection is Covid and not, for instance, Epstein-Barr or RSV, but half the time it doesn't seem like researchers are making comparisons at all, just reinventing the wheel and acting like "long covid" is a totally new phenomenon with no previous point of comparison. There are literally drugs in human trials to try to treat the mitochondrial dysfunction in ME, this dysfunction is well-established and fairly well understood and I feel insane when ppl report on long covid without mentioning that there is already a named and studied condition that accounts for this subset of symptoms!!
SOME researchers are drawing comparisons but they're largely ME researchers who everyone else is largely cignoring because of the widespread perception that ME is a fake disease for lazy women.
That same perception btw is why "graded exercise therapy" (GET), or exercise gradually increasing in intensity, cwas for years the go-to treatment despite MOUNTAINS of evidence that it makes ME patients sicker. Some end up permanently bedbound and unable to even eat or drink without a feeding tube/IV because the damage is so bad! The GET recommendation was finally changed only in the past few years in the US and the UK, and many doctors hate that they're not allowed to recommend it anymore, because they insist despite the evidence that ME/CFS is psychological and ME patients are just "deconditioned" and too lazy to do anything about it.
Now the same kind of "treatment" is being recommended for long covid patients despite evidence showing exercise is having the same kinds of cellular effects as it does in ME patients. "Taking PEM into account" sounds gentler but I'm deeply concerned about the reinvention of GET for patients who meet all the criteria for an illness that's been shown definitively to become permanently worse with GET. This mitochondrial damage is progressive in ME, and there's no reason to believe patients who meet all the criteria of ME after Covid won't experience the same progression if they force themselves past their energy envelope in such a systematic way.
The additional finding that T cells — part of the immune system's arsenal — had infiltrated the muscles of long COVID patients also caught Iwasaki's attention, possibly indicating "an autoimmune response within the muscle cells."
This autoimmune response is well-researched for ME. Every time you overexert, you're injuring your cells more and more. It's deeply worrying that rebranded GET is being recommended for long covid patients who meet the criteria for ME when research like this study keeps showing it's the same phenomenon.
Full Transcript at the link; 3-minute listen.
Quote:
By taking biopsies from long COVID patients before and after exercising, scientists in the Netherlands constructed a startling picture of widespread abnormalities in muscle tissue that may explain this severe reaction to physical activity.
Among the most striking findings were clear signs that the cellular power plants, the mitochondria, are compromised and the tissue starved for energy.
"We saw this immediately and it's very profound," says Braeden Charlton, one of the study's authors at Vrije University in Amsterdam.
The tissue samples from long COVID patients also revealed severe muscle damage, a disturbed immune response, and a buildup of microclots.
"This is a very real disease," says Charlton. "We see this at basically every parameter that we measure."
#IT'S M.E. LITERALLY 50% OF LONG COVID PATIENTS JUST HAVE M.E.#myalgic encephalomyelitis#please fund more mitochondrial drug research instead of forcing so many patients to get permanently sicker like we have been over this w ME#it's really upsetting to see patients who have a chance to never be as sick as I am#be told that they'll get better if they do the same things that made me and so many other ME patients permanently sicker#it's malpractice on a huge scale and i feel insane about how few people are calling it out#there's probably more people with ME now than at any previous time in our lifetimes and those numbers will keep skyrocketing as long as cov#d is allowed to run rampant#and they are getting really really bad care EVEN THOUGH WE HAVE SO MUCH RESEARCH NOW#oh there's also some really exciting stuff w antihistamines to target the neuroimmune symptoms being studied btw
30K notes
·
View notes
Text
Bacterial Meningitis: Study Finds Neuroimmune Axis That Exacerbates Host Defenses
Bacterial Meningitis: Study Finds Neuroimmune Axis That Exacerbates Host Defenses. #BacterialMeningitis #NeuroimmuneAxis #HostDefences #CGRP #RAMP1 #BrainInvasion #MenigitisResearch #MedicalNews #Healthcare #ScienceNews
Bacterial meningitis is a life-threatening infection that affects more than 2.5 million people annually, according to recent studies. Recently, researchers discovered that Nav1.8+ nociceptors signal immune cells in the meninges via the neuropeptide calcitonin gene-related peptide (CGRP) during infection; this neuroimmune axis suppresses host defenses further increasing the risk of bacterial…

View On WordPress
0 notes
Text
ARE VACCINES CAUSING CANCERS IN ALL OF US?
"Judy Mikovits, PhD is a biochemist and molecular biologist with more than 33 years of experience. Internationally known, a veritable “rock star” of the scientific world, she served as the director of the lab of Antiviral Drug Mechanisms at the National Cancer Institute before directing the Cancer Biology program at EpiGenX Pharmaceuticals. She later developed the first neuroimmune institute. Her early work focused on cancer and HIV, her latest on Chronic Fatigue Syndrome and autism. She has published more than 50 peer-reviewed articles."
In 2011, she made the discovery that destroyed her career. She found that at least 30% of our vaccines are contaminated with gammaretroviruses. Not only is this contamination associated with autism and chronic fatigue syndrome, it is also associated with Parkinson’s, Lou Gehrig’s disease, and Alzheimer’s.
The retroviruses contaminating vaccines originate from mice used for research. Dr. Mikovits asks, “How many new retroviruses have we created through all the mouse research, the vaccine research, gene therapy research? More importantly, how many new diseases have we created?”
“When they destroyed all of our work, and discredited everything I or Frank Ruscetti had ever published, and arranged for the publication of my mug shot in Science, the NIH very deliberately sent the message to researchers everywhere about what would happen to any honest scientist who dared ask those important questions.”
#world economic forum#wef#the great awakening#government corruption#bill gates#democrats#fjb#vaccines#nih#national institute of health#cdc#leukemia#alzheimers#lou gehrig's diseáse
169 notes
·
View notes
Text
Sometimes chronic pain patients use rescue meds on days that aren't even that dire, bc we're fucking sick of the constant background noise of pain and need a goddamn break every once in a while. When it never stops, it makes me feel like I'm on thin ice. I'm so scared of falling.
75 notes
·
View notes
Text
Went to my PCP this morning. She suggests it's neurological and I need a sleep study. I know enough about medicine to know that my blood results clearly point to something being wrong with the red and white blood cells.
I'm losing my mind.
I've been back at my mom's for over two months now. How am I getting sicker? I planned at least a month to recover from health assessments how am I worse?
#anemia it's clearly a type of anemia#ow..#chronic illness#I'll take neuroimmune maybe for the inflammation but not for the funky blood cells#vent
3 notes
·
View notes
Text
hey, it’s severe myalgic encephalomyelitis awareness day. i’m hopeful that things will change. i’m hopeful that people will learn about us.
infographic credit; see more here
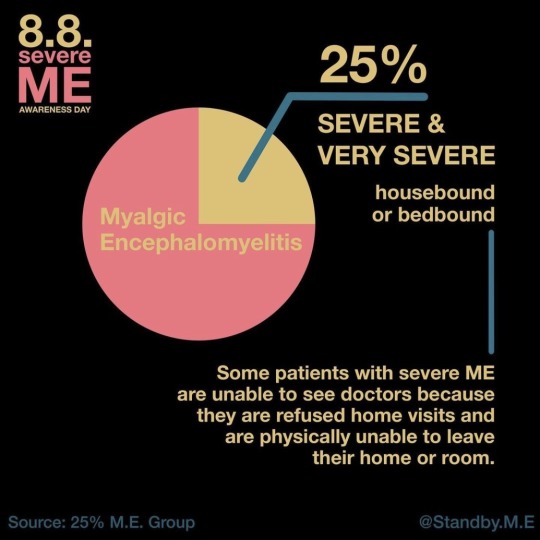
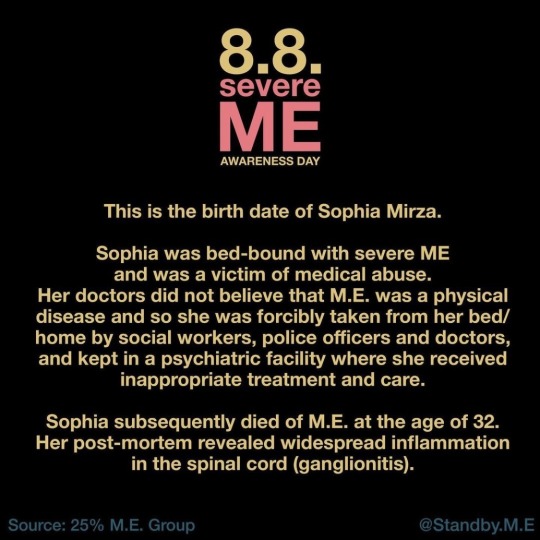
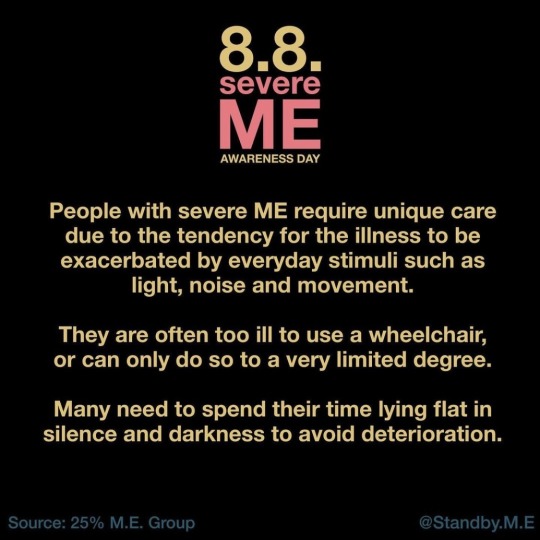
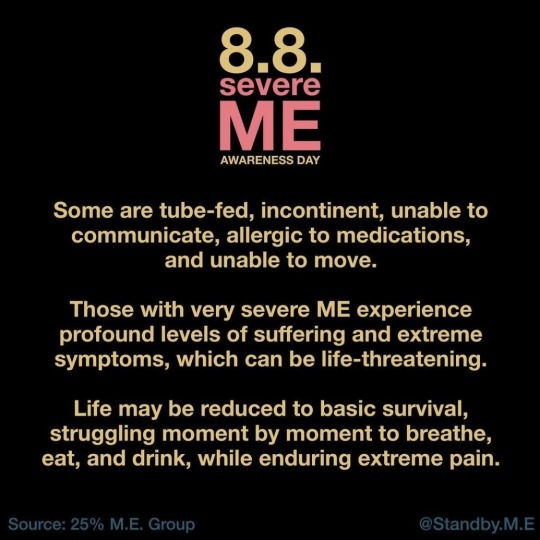
please hold us in your heart. ME itself is not rare (it’s over 5x more common than MS), but it’s really rare to find someone who actually knows what severe ME is! ME has been misrepresented as a vague fatigue syndrome. it is not. it’s a complex multisystem illness with a predictable pattern of neuroimmune crashes that come 24-72 hrs after physical or sensory exertion. it can become progressive and fatal. millions of people with severe ME are isolated and neglected by doctors whose knowledge of ME is based on outdated research.
it seems as though long covid can sometimes progress into ME, so cases are increasing, but many of us have had it for decades already. it crushed my life when i was a kid. but i’m still hopeful.
#i will never shut up about M.E.#myalgic encephalomyelitis#severe myalgic encephalomyelitis#chronic illness#txt#id in alt text#medical neglect#medical abuse#< trigger tagging
472 notes
·
View notes
Text
How COVID-19 might increase risk of memory loss and cognitive decline - Published Aug 7, 2024
Of all frightening ways that the SARS-COV-2 virus affects the body, one of the more insidious is the effect of COVID-19 on the brain.
It is now clear that many patients suffering from COVID-19 exhibit neurological symptoms, from loss of smell, to delirium, to an increased risk of stroke. There are also longer-lasting consequences for the brain, including myalgic encephalomyelitis /chronic fatigue syndrome and Guillain-Barre syndrome.
These effects may be caused by direct viral infection of brain tissue. But growing evidence suggests additional indirect actions triggered via the virus’s infection of epithelial cells and the cardiovascular system, or through the immune system and inflammation, contribute to lasting neurological changes after COVID-19.
I am a neuroscientist specializing in how memories are formed, the role of immune cells in the brain and how memory is persistently disrupted after illness and immune activation. As I survey the emerging scientific literature, my question is: Will there be a COVID-19-related wave of memory deficits, cognitive decline and dementia cases in the future?
The immune system and the brain Many of the symptoms we attribute to an infection are really due to the protective responses of the immune system. A runny nose during a cold is not a direct effect of the virus, but a result of the immune system’s response to the cold virus. This is also true when it comes to feeling sick. The general malaise, tiredness, fever and social withdrawal are caused by activation of specialized immune cells in the brain, called neuroimmune cells, and signals in the brain.
These changes in brain and behavior, although annoying for our everyday lives, are highly adaptive and immensely beneficial. By resting, you allow the energy-demanding immune response to do its thing. A fever makes the body less hospitable to viruses and increases the efficiency of the immune system. Social withdrawal may help decrease spread of the virus.
In addition to changing behavior and regulating physiological responses during illness, the specialized immune system in the brain also plays a number of other roles. It has recently become clear that the neuroimmune cells that sit at the connections between brain cells (synapses), which provide energy and minute quantities of inflammatory signals, are essential for normal memory formation.
Unfortunately, this also provides a way in which illnesses like COVID-19 can cause both acute neurological symptoms and long-lasting issues in the brain.
During illness and inflammation, the specialized immune cells in the brain become activated, spewing vast quantities of inflammatory signals, and modifying how they communicate with neurons. For one type of cell, microglia, this means changing shape, withdrawing the spindly arms and becoming blobby, mobile cells that envelop potential pathogens or cell debris in their path. But, in doing so, they also destroy and eat the neuronal connections that are so important for memory storage.
Another type of neuroimmune cell called an astrocyte, typically wraps around the connection between neurons during illness-evoked activation and dumps inflammatory signals on these junctions, effectively preventing the changes in connections between neurons that store memories.
Because COVID-19 involves a massive release of inflammatory signals, the impact of this disease on memory is particularly interesting to me. That is because there are both short-term effects on cognition (delirium), and the potential for long-lasting changes in memory, attention and cognition. There is also an increased risk for cognitive decline and dementia, including Alzheimer’s disease, during aging.
How does inflammation exert long-lasting effects on memory? If activation of neuroimmune cells is limited to the duration of the illness, then how can inflammation cause long-lasting memory deficits or increase the risk of cognitive decline?
Both the brain and the immune system have specifically evolved to change as a consequence of experience, in order to neutralize danger and maximize survival. In the brain, changes in connections between neurons allows us to store memories and rapidly change behavior to escape threat, or seek food or social opportunities. The immune system has evolved to fine-tune the inflammatory response and antibody production against previously encountered pathogens.
Yet long-lasting changes in the brain after illness are also closely linked to increased risk for age-related cognitive decline and Alzheimer’s disease. The disruptive and destructive actions of neuroimmune cells and inflammatory signaling can permanently impair memory. This can occur through permanent damage to the neuronal connections or neurons themselves and also via more subtle changes in how neurons function.
The potential connection between COVID-19 and persistent effects on memory are based on observations of other illnesses. For example, many patients who recover from heart attack or bypass surgery report lasting cognitive deficits that become exaggerated during aging.
Another major illness with a similar cognitive complications is sepsis – multi-organ dysfunction triggered by inflammation. In animal models of these diseases, we also see impairments of memory, and changes in neuroimmune and neuronal function that persist weeks and months after illness.
[You’re too busy to read everything. We get it. That’s why we’ve got a weekly newsletter. Sign up for good Sunday reading. ]
Even mild inflammation, including chronic stress, are now recognized as risk factors for dementias and cognitive decline during aging.
In my own laboratory, I and my colleagues have also observed that even without bacterial or viral infection, triggering inflammatory signaling over a short-term period results in long-lasting changes in neuronal function in memory-related brain regions and memory impairments.
Does COVID-19 increase risk for cognitive decline? It will be many years before we know whether the COVID-19 infection causes an increased risk for cognitive decline or Alzheimer’s disease. But this risk may be decreased or mitigated through prevention and treatment of COVID-19.
Prevention and treatment both rely on the ability to decrease the severity and duration of illness and inflammation. Intriguingly, very new research suggests that common vaccines, including the flu shot and pneumonia vaccines, may reduce risk for Alzheimer’s.
Additionally, several emerging treatments for COVID-19 are drugs that suppress excessive immune activation and inflammatory state. Potentially, these treatments will also reduce the impact of inflammation on the brain, and decrease the impact on long-term brain health.
COVID-19 will continue to impact health and well-being long after the pandemic is over. As such, it will be critical to continue to assess the effects of COVID-19 illness in vulnerability to later cognitive decline and dementias.
In doing so, researchers will likely gain critical new insight into the role of inflammation across the life-span in age-related cognitive decline. This will aid in the development of more effective strategies for prevention and treatment of these debilitating illnesses.
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#public health#still coviding#wear a respirator#long covid
34 notes
·
View notes
Text
ME/CFS is not a mental illness. Medical professionals are beginning to categorize it as a neuroimmune disorder.
Chronic fatigue is not a mental health issue nor is it psychosomatic.
166 notes
·
View notes
Text
Shoutout to the Sonic Movie 3 trailer for making me bring back this au that I’ve had since I was 16
He is more Biolizard-like and she has more neuroimmune symptoms🗣️🗣️‼️


#sonic the hedgehog#sonic au#shadow the hedgehog#maria robotnik#ark siblings#ARK SIBLINGS UPON YE#the biolizard ?#ig#neuro-immuno deficiency syndrome#NIDS#the ark#sonic adventure 2#also he can talk to artificial chaos#and the cute baby chaos in chao garden#ask me about my au#explodes#auto immune disease
12 notes
·
View notes
Text
this is very angry, but i really just want to yell somewhere outside of just the narcolepsy tags bc yknow I'm physically disabled!!! it sucks!!!!
another issue with narcolepsy!!! is that the media and mainstream depictions of it are so fucking insultingly simple and do NOTHING to represent the devastation it can cause and how physically disabling it is.
Sleep is something fundamental to health. if your sleep is disordered and impaired and you aren't getting enough good restorative sleep, you are going to suffer long term health impacts and horrible quality of life. you have to be a fucking ambassador with an encyclopedic knowledge of how it's not the funny "fall asleep when emotional disorder" (that's called cataplexy and it isn't falling asleep, it's muscle weakness and a loss of muscle control. it's also only in type 1 narcolepsy) or the "falls asleep anywhere and you're refreshed :) disorder" (for many people, it's not being "refreshed", it's just Not Being As Tired and it doesn't last very long) or the simple "it means you're sleepy all the time"
it's often severe sleep cycle disturbances during both night AND day and feeling tired all. the. time. because your brain can't properly regulate sleep cycles so you can't get enough deep sleep. ever.
imagine never getting enough sleep fucking ever. It doesn't matter how MUCH you sleep, because your brain can't moderate your sleep cycles properly and you can't go into the stages of sleep that your brain and body need. imagine the impact that would have on your brain and body. imagine your own brain literally not physically fucking working right. imagine the full body, unrelenting fatigue.
it's a severe neurological and neuroimmune (at least N1 usually is neuroautoimmune) disorder and it's actually severely underdiagnosed because not enough people have access to the specific kind of sleep studies they (insurance companies tbh) require to diagnosis it
when are people going to realize we are fucking suffering and stop overwhelmingly handwaving or treating narcolepsy like a punchline or funny quirk?
everyone who thinks it's cute or quirky actively contributes to how horribly we are treated and how little we are taken seriously unless we sit there with essays that spoonfeed how critical proper sleep cycling is to longterm health and quality of life.
even then, why should anyone care about us physically? all that matters is that we're considered productive under capitalism. doesn't matter what severe health issues you continue to stack up
stimulants and wakefulness promoting agents are the first line treatment and they do fucking NOTHING to tackle the sleep cycle issues at night. in fact, they often make insomnia even worse. nobody gives a shit about narcoleptics' physical health as long as they're capable of being productive and "awake" and it's utterly repulsive.
(This all also applies a lot to idiopathic hypersonmnia, too, which shares a lot of overlap w narcolepsy type 2)
also ppl w [insert mental illness or neurodevelopmental disorder here] who want to compare it to a neurological sleep disorder: don't you even fucking Start. you know full well I'm talking about different things.
#narcolepsy#physically disabled#neurological disorder#sleep disorder#neurologically disabled#ive been having a bad time of it lately#disability vent
11 notes
·
View notes