#nephrostomy posting
Explore tagged Tumblr posts
Text
First time out of the house in like three weeks and it’s to go to the fuckin hospital lol
#she speaks#nephrostomy posting#I’m fine I’m going to get my ct scan#and then back tomorrow to get the tube removed 🙌🙌🙌#I have to sit sideways in the car lmao
5 notes
·
View notes
Text
Hey. I had two cocktails tonight and I'm feeling it mister krabs
#i do not drink i just smoke lots of weed#whats up everybody i havemt posted about my life here recently#my mom has been hospitalized for like two months and she just got an ileostomy things are looking better than they were.#i have been under immense amounts of stress ! haha#my dad was also in the hospital last weekend to have a nephrostomy placed#im being sent to uptown for a seminar for work in less than two weeks that i gotta drive back n forth from both days#the cocktails were good for someone who hates the taste of alcohol
1 note
·
View note
Text
Leukocytes or nitrites present 75% sensitivity and 82% specificity; all you need for simple cystitis
Culture positive if >10^5 CFU or 10^2 CFUs with symptoms; necessary for pyelonephritis/complicated UTI
CT will show obstruction, calculi, gas-forming infections
Men: STI, prostatitis, urethritis
Tx: Macrobid 100 mg x5 days, Bactrim DS bid x3 days
Pyelo: FQs, CTX, zosyn, cefepime if low risk for MDR
Meropenem, IV FQs, CTX, zosyn, cefepime for high risk MDR
Recurrent UTIs: pyridium, post coital abxs, urogyn referral, daily ppx with Bactrim, Macrobid, or Keflex
Pyelo f/u: PRN, urology, or urogyn f/u
Highest prevalence among uncircumcised males <3 months
In peds pts, enterococcus is not a contaminant in the urine culture as it typically is in adults
You want to avoid renal scarring; any other organism other than E.coli has increased risk of causing renal scarring in kids
US recommended in kids <2 years with first febrile UTI, any age with recurrent UTI, any age with fam hx of kidney/uro disease, poor growth, HTN, failure to respond to tx
Voiding cystourethrogram for anatomical eval and for reasons listed above
Simple cystitis tx:
Infants: cephalosporin; Keflex 50-100 mg/kg qd divided bid x5 days. Allergy? Can use Bactrim, Augmentin, rarely ciprofloxacin
Pts 1 month to 2 years: IV CTX, gentamicin; cefdinir 14 mg/kg qd divided bid x10 days
If no improvement in 48-72 hours, change abxs and pursue imaging
For infants, you need to do f/u imaging if not done in hospital
Pregnant women have acute cystitis, not simple cystitis because pregnant women are not simple
Abxs in pregnancy: beta lactam, Macrobid (not in first trimester), Fosfomycin; duration of therapy is 5-7 days
Bactrim avoided during pregnancy. Cefpodoxime is another one safe in pregnancy.
Pyelo in pregnancy: consider intraamniotic infection and placental abruption; it’s not an indication for delivery. Can tx with IV CTX or zosyn.
You have to recheck UA after treatment of asymptomatic bacteriuria in pregnant pts; 30% don’t clear it
Macrobid and Bactrim should be avoided in pregnancy; Macrobid more so in the first trimester; avoid Bactrim throughout pregnancy
Febrile neonate: tachypnea, irritability, cyanosis, poor feeding; <1% of term infants have UTIs. Limited data for preterm infants.
Term infants tend to get E. coli. In preterm infants, coagulase neg staph and Klebsiella are more common; really small premies can have candida.
Hematogenous spread can occur in premies.
Neonates: UA, culture, blood culture, lumbar puncture; imaging, voiding cystourethrogram
Broad spectrum abxs in babies: Ampicillin and gentamicin for 10 to 14 days
CTX can increase serum free bilirubinà increased jaundice
Kids can have impaired renal growth that resolved
Catheter Associated UTI = CAUTI; no need to screen unless pt is symptomatic
Pyuria is not enough to diagnose UTI in pts with indwelling catheters; you need a culture, which you compare to previous culture. Percutaneous nephrostomy tubes, stents – get urology involved. Tx with broad spectrum abxs until you get culture results. Tx 7-14 days. Levofloxacin x5 days if not severely ill; 3 days for pts under 65 w/o upper UTI sxs
For transplant pts, there’s more resistance to cipro and Bactrim
For transplant pts with simple cystitis: FQs, 3rd gen cephalosporins x10-14 days; zosyn, meropenem, cefepime if complicated and call ID
Do not screen (these are guidelines, not what we always do): peds pts, functionally impaired adults, long term care facility pts, diabetics, pts w/ renal transplants, pts with spinal cord injuries
4 notes
·
View notes
Text
What Are the Benefits and Risks of Percutaneous Nephrolithotomy (PCNL)?

Percutaneous Nephrolithotomy (PCNL) is a minimally invasive surgical procedure used to remove large kidney stones that cannot be treated effectively with other methods. If you are considering this procedure, it’s crucial to understand both its benefits and risks. In this blog, we will explore the advantages and potential complications of PCNL, and highlight how the Best Urology Hospital in Jaipur, Shekhawati Hospital, can provide expert care for this treatment.
Understanding Percutaneous Nephrolithotomy (PCNL)
PCNL involves making a small incision in the patient's back to access the kidney directly and remove the stones. It is typically recommended for stones that are too large, too numerous, or too complex to be treated with less invasive methods like shock wave lithotripsy or ureteroscopy.
Benefits of Percutaneous Nephrolithotomy (PCNL)
1. Effective Removal of Large Stones
PCNL is highly effective in removing large or complex kidney stones that are not amenable to other treatment methods. It can handle stones larger than 2 centimeters, staghorn calculi, and stones that are resistant to other forms of treatment.
2. Minimally Invasive Approach
Unlike open surgery, PCNL is minimally invasive, which means it involves smaller incisions, less pain, and shorter recovery times. This approach significantly reduces the risk of infection and minimizes blood loss during the procedure.
3. High Success Rate
PCNL has a high success rate, often above 90%, in completely removing kidney stones. This leads to immediate relief from symptoms such as pain, urinary obstruction, and recurrent urinary tract infections.
4. Quick Recovery
Patients typically experience a quicker recovery compared to open surgery. Most patients can return to normal activities within a few weeks, with a significant reduction in discomfort and downtime.
5. Reduced Need for Multiple Procedures
For large or complex stones, PCNL often eliminates the need for multiple procedures. This is particularly beneficial for patients with large stone burdens, as it reduces overall treatment time and associated risks.
Risks of Percutaneous Nephrolithotomy (PCNL)
1. Bleeding
One of the primary risks associated with PCNL is bleeding, as the procedure involves creating an access tract to the kidney. While most cases of bleeding can be managed conservatively, some patients may require blood transfusions.
2. Infection
As with any surgical procedure, there is a risk of infection. However, this risk is minimized with the use of antibiotics and sterile techniques. It is important to monitor for signs of infection post-surgery, such as fever, chills, or persistent pain.
3. Injury to Surrounding Organs
Although rare, there is a risk of injury to surrounding organs such as the bowel, liver, or spleen during the procedure. This risk is minimized by using imaging guidance and experienced surgical techniques.
4. Residual Stones
In some cases, small fragments of stones may remain in the kidney after the procedure. These residual stones might require additional treatments, such as shock wave lithotripsy or follow-up PCNL procedures.
5. Postoperative Pain
While PCNL is less invasive than open surgery, patients may still experience pain at the incision site and discomfort from the nephrostomy tube placed during the procedure. Pain management strategies are employed to ensure patient comfort.
Why Choose Shekhawati Hospital for PCNL?
As the Best Urology Hospital in Jaipur, Shekhawati Hospital is renowned for its expert care in performing PCNL. Here’s why Shekhawati Hospital stands out:
1. Experienced Urologists
Shekhawati Hospital boasts a team of highly skilled urologists with extensive experience in performing PCNL. Their expertise ensures precise execution and optimal outcomes.
2. State-of-the-Art Facilities
The hospital is equipped with cutting-edge technology and modern surgical facilities, ensuring that patients receive the best possible care.
3. Comprehensive Care
From preoperative assessment to postoperative follow-up, Shekhawati Hospital provides comprehensive care to ensure a smooth and successful recovery for patients undergoing PCNL.
4. Patient-Centric Approach
Shekhawati Hospital is dedicated to patient care and comfort. The medical team works closely with patients to provide personalized treatment plans and compassionate support throughout the treatment journey.
Conclusion
Percutaneous Nephrolithotomy (PCNL) offers numerous benefits for patients with large or complex kidney stones, including effective stone removal, a minimally invasive approach, and a high success rate. However, it is important to be aware of the potential risks, such as bleeding, infection, and injury to surrounding organs. Choosing a reputable medical facility like the Best Hospital in Jaipur, Shekhawati Hospital, ensures that you receive expert care with advanced technology and experienced professionals. If you are considering PCNL, consult with the specialists at Shekhawati Hospital to understand how this procedure can help you achieve optimal health outcomes.
0 notes
Text
Lupine Publishers | Safety and Efficacy Assessment of Pcnl in The Pediatric Population: A Single Centre Experience

Abstract
Introduction and Objective: Renal stone disease in children is on the rise with increased incidence and better modalities to diagnose the disease. Hence there is a necessity to strategize the evaluation and treatment of children with kidney stones. Our study was conducted to assess stone distribution, stone burden, and efficacy of PCNL in pediatric age group. Methods: All paediatric patients with renal stone disease who subsequently underwent PCNL at our department from January 2017 to December 2020 were analysed. Results: 84 patients ranging 1-18 years were analysed. Pain abdomen was the most common presenting symptom (61.9%) followed by fever (19.04%). The mean stone size was 2.16cm with equal side distribution. Most stones were located in the lower calyx (38%). The mean operative time was 65 minutes. Exposure to radiation from C arm ranged from 1.6-8.3 minutes. Complete stone clearance was achieved in 90.47% with a mean post- drop in Hb value to 0.72 gm/dl. Mean duration of nephrostomy tube in situ was 2.4 days and with a mean hospital stay of 3.8 days. Calcium oxalate was the most common type of stone (48%) Conclusion: PCNL is safe and effective treatment for pediatric renal calculi with minimal morbidity and increased stone free rates irrespective of stone size. Proper patient selection, surgical skill and postoperative care contribute towards the success of the procedure
Keywords: Pediatric PCNL; Pediatric Renal Calculi; Renal Stone Disease
Introduction
The prevalence of renal stone disease in children ranges from 5 to 15%. Stone disease has a higher risk of recurrence in the pediatric age group making it crucial to identify the most effective method for complete stone removal to prevent recurrence from residual fragments. The optimal management of for pediatric stone disease is still evolving [1,2]. Currently, ESWL is the procedure of choice for treating most upper urinary tract calculi in the pediatric population. However, a higher incidence of metabolic and anatomical abnormalities in pediatric patients has led to increased recurrence. Moreover, ESWL has relatively less efficacy for stones >1.5cm. Surgical intervention should be preferred in such cases so as to minimize the need for retreatment [3-5]. Percutaneous nephrolithotomy (PCNL) is less invasive than open surgery which can be a good candidate for complex and large burden stones [6]. Several studies over time with different power and limitations have reported safety and efficacy of PCNL leading to its consideration as the treatment of choice for children with stone larger than 15mm [7-9]. The advent of newer, finer instruments and increase in experience of endourological techniques such as tubeless PCNL, mini-perc, ultra-mini perc and micro-perc has resulted in reducing the morbidity rate among patients without affecting the outcomes in terms of clearance [10-14]. Therefore, our study was conducted to assess the safety and efficacy of PCNL in the pediatric age group in terms of (1) renal stone distribution & stone burden (2) the outcomes of PCNL including stone clearance, operative time, hospital stay, haemoglobin changes and (3) the associated complications of PCNL.
Materials and Methods
A prospective study was conducted at our hospital from January 2017 to December 2020 after obtaining institutional ethical committee clearance. All pediatric patients posted for PCNL at MS Ramaiah Medical College were considered in the study. The patients compatible for the study were interviewed and after obtaining informed and written consent they were enrolled in the study. Inclusion Criteria: All the patients below the age of 18 years undergoing PCNL. Exclusion Criteria: Anatomic abnormalities of the kidney (horseshoe kidney/malrotated kidney); Bleeding disorders; deranged renal function. Patients were initially evaluated with a detailed medical history and a thorough clinical examination followed by a battery of investigations including CBC, RFT, Serum electrolytes, serum levels of calcium, phosphorus, alkaline phosphatase, uric acid, total protein, carbonate, albumin, parathyroid hormone (if there is hypercalcaemia), blood group & Rh typing, HbsAg, HIV, HCV, Urine: Routine & Microscopy, Urine: Culture & Sensitivity. For imaging –ultrasonography was used as a first study followed by spiral CT KUB if no stone was found. Intravenous pyelography was performed when a need arose to delineate the calyceal anatomy prior to percutaneous or open surgery. A sterile urine culture was confirmed before surgery. In patients with evidence of infection, antibiotics were given preoperatively to clear the infection prior to surgery. All patients received broad-spectrum antibiotics beginning 12 h prior to the procedure and these were continued until 5 days postoperatively. All PCNL are performed under general anaesthesia. The patient initially placed in lithotomy position and a ureteric access catheter was placed under fluoroscopic guidance. The patient was then turned prone. After initial puncture, the tract was dilated using metallic or Teflon dilators. Paediatric PCNL was performed using adult instruments and clearance assessed intraopeartively by fluoroscopy. Ureteric stents and nephrostomy tubes were placed in most patients at the end of the procedure. Baseline patient characteristics, intraoperative and post-operative data were collected and analysed. Perioperative complications were classified using the modified Clavien Dindo system. In case of a supra-costal puncture, a chest X-ray was obtained subsequently in the post op period. An x ray of kidney ureter bladder was taken at 48 hours after PCNL. If needed a re-look procedure was done. The patient was followed up with an ultrasound & serum creatinine at 3 months, DMSA scan after 6 months to know the functional status of kidney & amount of renal scarring. Statistical analysis was performed using SPSS 22. Categorical variables were presented as number and percentage (%), whereas continuous variables were presented as mean ± standard deviation and median (Table 1).
Results
84 patients ranging between 1-18 years of age were analysed with the mean age of study population of 11.04 years. Pain abdomen was the most common presenting symptom (61.9%) followed by fever (19.04%) with 4/84 having had prior surgical intervention for stone disease (Figure 1). The mean stone size was 2.16cm with equal side distribution. Most stones were located in the lower calyx (38%) followed by renal pelvis – 33%, middle calyx 17% and upper calyx 12% (Figure 2a). The total operative time ranged from 30 minutes to 120 minutes with a mean of 65 minutes. Exposure to radiation from C arm ranged from 1.6-8.3 minutes. Intraoperative location of stone, puncture and after clearance are shown in Figures 1a,1b,1c. Complete stone clearance was achieved in 90.47% with a mean post- drop in Hb value to 0.72 gm/dl. Mean duration of nephrostomy tube in situ was 2.4 days and with a mean hospital stay of 3.8 days. Intra-operative and post-operative complications in the study population are depicted in Table 2. Calcium oxalate was the most common type of stone (48%) (Figure 3).
Discussion
Although short wave lithotripsy (SWL) is considered the treatment of choice for symptomatic upper urinary tract calculi in children, but not a preferred option in patients with large stone burden, owing to higher rates of failure and residual stones. In such cases, PCNL with proven advantages can be safely advocated as a suitable treatment option in order to avoid numerous SWL sessions under anesthesia. Despite pediatric PCNL being described as early as 1985 by Woodside et al. [6], pediatric surgeons had their reservation in performing PCNL in children. This apprehension was due to the fear of parenchymal damage, early exposure to radiation and risk of major complications associated with the surgery. However, Dawaba et al. [9] proved the fear to be baseless by demonstrating that PCNL in paediatric population improved overall renal function without causing renal scarring. Similarly, Mor et al. reported no significant scarring or loss of renal function in radionuclide renal scans (19). He concluded that adult type tract dilation to 24Fr to 26Fr was not associated with significant renal function loss [19]. The size, number and site of tracts are not well defined in pediatric PCNL. While Gunes et al. reported a higher complication rate in children <7 years operated with adult sized instruments [17], Desai et al. observed that intraoperative bleeding during PCNL in children is related to the size and number of tracts and suggested the need for technical modifications in children [20]. Although this calls for reduction in tract size, it may have an effect on the clearance rates. In our study, 54(64.28%) underwent standard PCNL vs 30(35.71%) underwent Miniperc. We used amplatz sheath sizes in the range of 16F-28F. Size of tract dilatation was based on dilatation of pelvicalyceal system, the stone burden and no of punctures. Our clearance rates & transfusion rates were found to be similar in miniperc & standard PCNL. Our results are in concurrence with Bilen et al. who reported that smaller tracts did not significantly affect stone-free rates but achieved lower transfusion rates [21]. They concluded that a 20Fr tract was as effective as working with adult sized devices and did not significantly increase the operative time. (18) Provided the quality of the puncture and subsequent tract is high, there is no greater morbidity than that reported from miniperc. Large tracts and instruments can facilitate more rapid and complete stone clearance (Table 3).
Most of the stone burden was located in lower calyx (38%) in most of our cases with staghorn calculus noted in 4 patients. Single tract access was done in 72 patients with lower calyceal puncture being used mostly (43%) (Figure 2b). Multiple punctures were required in 12 cases (14.2%). We did not find any significant increase in complications following an upper calyceal puncture or with multiple punctures in our study which is comparable to Sedat Oner et al. who concluded that an upper pole approach did not prolong operative time or add to the complications, making it a good alternative. A surgeon who has reached competence at performing PCNL should therefore not hesitate to use a superior caliceal approach in pediatric patients if deemed appropriate for stone removal [22]. Our length of hospital stay duration of nephrostomy tube in situ is comparable to previously published data. 42.85% of our cases were tubeless, which is safe when performing uncomplicated PCNL [34]. Prior renal surgery on the same side didn’t have any impact on outcome of PCNL [35]. Aldaqadossi et al. have suggested that a previous open pyelolithotomy or nephrolithotomy does not affect the efficacy and morbidity of subsequent PCNL in pediatric patients [35]. We achieved a complete clearance rate of 90.47% which is similar to the published literature. Residual calculi noted in 8 cases were managed by ESWL. The complication rate during and after PCNL in paediatric patients varies widely in the literature. The difference in complication rates may be explained by the difference in stone burden location and experience of the surgical team. Our complication rate was 9.52% with fever being the most common. The lower incidence in complications could be attributed to the surgeon expertise at our center.
Limitations
Our study population was from single referral center, which may not be generalizable considering small sample size. Another limitation is the lack of comparative groups such as ESWL/RIRS while evaluating the efficacy of PCNL.
Conclusion
PCNL is safe and effective treatment for pediatric renal calculi with minimal morbidity and increased stone free rates irrespective of stone size. Proper patient selection, surgical skill and postoperative care contribute towards the success of the procedure and reduces the complications.
For more Lupine Journals please click here: https://lupinepublishers.com/index.php
For more Journal of Urology & Nephrology Studies articles please click here: https://lupinepublishers.com/urology-nephrology-journal/index.php
#journal of urology & nephrology studies#submission#open access journals#nephritis#lupine journals#lupine publishers#urology#articles#nephrology
0 notes
Text
Lupine Publishers | Safety and Efficacy Assessment of PCNL in the Pediatric Population: A Single Centre Experience

Abstract
Introduction and Objective: Renal stone disease in children is on the rise with increased incidence and better modalities to diagnose the disease. Hence there is a necessity to strategize the evaluation and treatment of children with kidney stones. Our study was conducted to assess stone distribution, stone burden, and efficacy of PCNL in pediatric age group.
Methods: All paediatric patients with renal stone disease who subsequently underwent PCNL at our department from January 2017 to December 2020 were analysed.
Results: 84 patients ranging 1-18 years were analysed. Pain abdomen was the most common presenting symptom (61.9%) followed by fever (19.04%). The mean stone size was 2.16cm with equal side distribution. Most stones were located in the lower calyx (38%). The mean operative time was 65 minutes. Exposure to radiation from C arm ranged from 1.6-8.3 minutes. Complete stone clearance was achieved in 90.47% with a mean post- drop in Hb value to 0.72 gm/dl. Mean duration of nephrostomy tube in situ was 2.4 days and with a mean hospital stay of 3.8 days. Calcium oxalate was the most common type of stone (48%).
Conclusion: PCNL is safe and effective treatment for pediatric renal calculi with minimal morbidity and increased stone free rates irrespective of stone size. Proper patient selection, surgical skill and postoperative care contribute towards the success of the procedure.
Keywords:COVID-19; post-covid manifestations; long covid; gastrointestinal disorders; dysbiosis; dyspepsia; microbiome; probiotics
Introduction
The prevalence of renal stone disease in children ranges from 5 to 15%. Stone disease has a higher risk of recurrence in the pediatric age group making it crucial to identify the most effective method for complete stone removal to prevent recurrence from residual fragments. The optimal management of for pediatric stone disease is still evolving [1, 2]. Currently, ESWL is the procedure of choice for treating most upper urinary tract calculi in the pediatric population. However, a higher incidence of metabolic and anatomical abnormalities in pediatric patients has led to increased recurrence. Moreover, ESWL has relatively less efficacy for stones >1.5cm. Surgical intervention should be preferred in such cases so as to minimize the need for retreatment [3-5]. Percutaneous nephrolithotomy (PCNL) is less invasive than open surgery which can be a good candidate for complex and large burden stones [6]. Several studies over time with different power and limitations have reported safety and efficacy of PCNL leading to its consideration as the treatment of choice for children with stone larger than 15mm [7-9]. The advent of newer, finer instruments and increase in experience of endourological techniques such as tubeless PCNL, mini-perc, ultra-mini perc and micro-perc has resulted in reducing the morbidity rate among patients without affecting the outcomes in terms of clearance [10-14].
Therefore our study was conducted to assess the safety and efficacy of PCNL in the pediatric age group in terms of
a) Renal stone distribution & stone burden
b) The outcomes of PCNL including stone clearance, operative time, hospital stay, haemoglobin changes and
c) The associated complications of PCNL.
Materials and Methods
A prospective study was conducted at our hospital from January 2017 to December 2020 after obtaining institutional ethical committee clearance. All paediatric patients posted for PCNL at M.S. Ramaiah Medical College were considered in the study. The patients compatible for the study were interviewed and after obtaining informed and written consent they were enrolled in the study.
Inclusion Criteria:
All the patients below the age of 18 years undergoing PCNL.
Exclusion Criteria:
Anatomic abnormalities of the kidney (horseshoe kidney/malrotated kidney); Bleeding disorders; deranged renal function.
Patients were initially evaluated with a detailed medical history and a thorough clinical examination followed by a battery of investigations including CBC, RFT, Serum electrolytes, serum levels of calcium, phosphorus, alkaline phosphatase, uric acid, total protein, carbonate, albumin, parathyroid hormone (if there is hypercalcaemia), blood group & Rh typing , HbsAg, HIV, HCV, Urine: Routine & Microscopy, Urine: Culture & Sensitivity. For imaging –ultrasonography was used as a first study followed by spiral CT KUB if no stone was found. Intravenous pyelography was performed when a need arose to delineate the calyceal anatomy prior to percutaneous or open surgery. A sterile urine culture was confirmed before surgery. In patients with evidence of infection, antibiotics were given preoperatively to clear the infection prior to surgery. All patients received broad-spectrum antibiotics beginning 12h prior to the procedure and these were continued until 5 days postoperatively. All PCNL are performed under general anaesthesia. The patient initially placed in lithotomy position and a ureteric access catheter was placed under fluoroscopic guidance. The patient was then turned prone. After initial puncture, the tract was dilated using metallic or Teflon dilators. Paediatric PCNL was performed using adult instruments and clearance assessed intraoperatively by fluoroscopy. Ureteric stents and nephrostomy tubes were placed in most patients at the end of the procedure. Baseline patient characteristics, intraoperative and post-operative data were collected and analysed. Perioperative complications were classified using the modified Clavien Dindo system. In case of a supra-costal puncture, a chest X-ray was obtained subsequently in the post op period. An x ray of kidney ureter bladder was taken at 48 hours after PCNL. If needed a re-look procedure was done. The patient was followed up with an ultrasound & serum creatinine at 3 months, DMSA scan after 6 months to know the functional status of kidney & amount of renal scarring. Statistical analysis was performed using SPSS 22. Categorical variables were presented as number and percentage (%), whereas continuous variables were presented as mean ± standard deviation and median.
Results
84 patients ranging between 1-18 years of age were analysed with the mean age of study population of 11.04 years. Pain abdomen was the most common presenting symptom (61.9%) followed by fever (19.04%) with 4/84 having had prior surgical intervention for stone disease. The mean stone size was 2.16cm with equal side distribution. Most stones were located in the lower calyx (38%) followed by renal pelvis – 33%, middle calyx 17% and upper calyx 12% . The total operative time ranged from 30 minutes to 120 minutes with a mean of 65 minutes. Exposure to radiation from C arm ranged from 1.6-8.3 minutes. Intraoperative location of stone, puncture and after clearance are shown in figures 1a,1b,1c. Complete stone clearance was achieved in 90.47% with a mean post- drop in Hb value to 0.72 gm/dl. Mean duration of nephrostomy tube in situ was 2.4 days and with a mean hospital stay of 3.8 days. Intra-operative and post-operative complications in the study population are depicted. Calcium oxalate was the most common type of stone (48%).
Discussion
Although short wave lithotripsy (SWL) is considered the treatment of choice for symptomatic upper urinary tract calculi in children, but not a preferred option in patients with large stone burden, owing to higher rates of failure and residual stones. In such cases, PCNL with proven advantages can be safely advocated as a suitable treatment option in order to avoid numerous SWL sessions under anesthesia. Despite pediatric PCNL being described as early as 1985 by Woodside et al, [6] pediatric surgeons had their reservation in performing PCNL in children. This apprehension was due to the fear of parenchymal damage, early exposure to radiation and risk of major complications associated with the surgery. However, Dawaba et al, [9] proved the fear to be baseless by demonstrating that PCNL in paediatric population improved overall renal function without causing renal scarring. Similarly, Mor et al reported no significant scarring or loss of renal function in radionuclide renal scans [15-19]. He concluded that adult type tract dilation to 24Fr to 26Fr was not associated with significant renal function loss [19]. The size, number and site of tracts are not well defined in pediatric PCNL. While Gunes et al reported a higher complication rate in children <7 years operated with adult sized instruments [17]. Desai et al observed that intraoperative bleeding during PCNL in children is related to the size and number of tracts and suggested the need for technical modifications in children [20]. Although this calls for reduction in tract size, it may have an effect on the clearance rates.
In our study, 54(64.28%) underwent standard PCNL vs 30(35.71%) underwent Miniperc. We used amplatz sheath sizes in the range of 16F-28F. Size of tract dilatation was based on dilatation of pelvicalyceal system, the stone burden and no of punctures. Our clearance rates & transfusion rates were found to be similar in miniperc & standard PCNL. Our results are in concurrence with Bilen et al who reported that smaller tracts did not significantly affect stone-free rates but achieved lower transfusion rates [21]. They concluded that a 20Fr tract was as effective as working with adult sized devices and did not significantly increase the operative time [18]. Provided the quality of the puncture and subsequent tract is high, there is no greater morbidity than that reported from miniperc. Large tracts and instruments can facilitate more rapid and complete stone clearance.
Most of the stone burden was located in lower calyx (38%) in most of our cases with staghorn calculus noted in 4 patients. Single tract access was done in 72 patients with lower calyceal puncture being used mostly (43%) (Figure 2b). Multiple punctures were required in 12 cases (14.2%). We did not find any significant increase in complications following an upper calyceal puncture or with multiple punctures in our study which is comparable to Sedat Oner et al who concluded that an upper pole approach did not prolong operative time or add to the complications, making it a good alternative. A surgeon who has reached competence at performing PCNL should therefore not hesitate to use a superior caliceal approach in pediatric patients if deemed appropriate for stone removal [22-25].
Our length of hospital stay duration of nephrostomy tube in situ is comparable to previously published data. 42.85% of our cases were tubeless, which is safe when performing uncomplicated PCNL [26-34]. Prior renal surgery on the same side didn’t have any impact on outcome of PCNL [35]. Aldaqadossi et al have suggested that a previous open pyelolithotomy or nephrolithotomy does not affect the efficacy and morbidity of subsequent PCNL in pediatric patients [35]. We achieved a complete clearance rate of 90.47% which is similar to the published literature. Residual calculi noted in 8 cases were managed by ESWL. The complication rate during and after PCNL in paediatric patients varies widely in the literature. The difference in complication rates may be explained by the difference in stone burden location and experience of the surgical team. Our complication rate was 9.52% with fever being the most common. The lower incidence in complications could be attributed to the surgeon expertise at our centre.
Limitations
Our study population was from single referral center, which may not be generalizable considering small sample size. Another limitation is the lack of comparative groups such as ESWL/RIRS while evaluating the efficacy of PCNL.
Conclusion
PCNL is safe and effective treatment for pediatric renal calculi with minimal morbidity and increased stone free rates irrespective of stone size. Proper patient selection, surgical skill and postoperative care contribute towards the success of the procedure and reduces the complications.
For more Lupine Publishers open access journals please visit our website:
https://lupinepublishers.com/index.php
For more Current Trends in Gastroenterology and Hepatology articles please click here: https://lupinepublishers.com/gastroenterology-hepatology-journal/index.php
#open access journals#gastric ulcers#hepatitis#submissions#peptic ulcer#articles#gastroenterocolostomy#gastroenteralgia#liver#gastrointestinal
0 notes
Text
Interventional Radiology Procedures
OPD Procedures:
FNAC & Biopsy
Percutaneous Drain Placement
Ascitic and pleural fluid aspiration
Day Care Procedures:
Biopsy: Liver, Renal, Lung
Chemotherapy Catheters and ports
Laser Treatment of Varicose Veins
Varicocele Embolization
Abscess Drainage/Chest Tube Placement
Bronchial Artery Embolization
Uterine Artery Embolization
Acute & Chronic mesenteric ischemia
Pseudoaneurysm Repair
RFA for osteoid osteoma
Billiary Procedures:
Percutaneous transhepatic Cholangiography (PTC)
Percutaneous transhepatic biliary Drainage (PTBD)
Biliary Stenting
Dilatation of benign biliary stricture
Percutaneous Cholecystostomy
Preoperative tumor embolization
Liver & Tumor Treatment:
Conventional Chemoembolization
Doxorubicin Drug Eluded Chemoembolization
Y-90 Sir Sphere Radioembolization
Ablation: Radiofrequency Ablation (RFA)
PAIR
Pre and post liver transplant:
Portal vein embolization
Hepatic vein stenting
Biliary Drainage and aspiration
Portal Hypertension and GI bleed:
Transjuglar intrahepatic portosystemic shunts (TIPS)
Hepatic outflow recanalization
Partial splenic embolization
BRTO
Renal Procedures
Renal Biopsy
Renal Angiography
Renal Angioplasty
Renal Stents
Preoperative tumor embolization
Percutaneous Nephrostomy Tube Placement
Ureteral Dilatation
Treatment of Ureteral Occlusion
Urinary Tract Dilatation for Lithotripsy
TAG-
Interventional Radiology Procedures,
Interventional Radiologist in Delhi
0 notes
Text
An Unexpected Hiatus
So I know it’s been a while since I last posted. A couple things happened because of that. First I was in the hospital for over a week due to kidney failure. Don’t worry, I’m okay now after a couple sessions of dialysis and a nifty new nephrostomy tube in my backside. Second while I was at the hospital I had my laptop with me and it stopped working last week. So without that I wasn’t able to keep up with my daily posting like I normally do. Now that I’m home I have access to another computer to get back to my routine. Of course all my data and files are on my laptop but I can access some stuff from the cloud thank god. So I’m back people! Let’s get back to the art!
2 notes
·
View notes
Text
Wow. Three years...
It's been three years since I last posted here. So much has happened I don't really know where to start.
But, for anyone who still remembers me or cares, here is a break down....
*I have been diagnosed with Fibromatosis. A benign cancer that is crushing my internal organs (start strong I always say)
*Because of said tumour I also have two Nephrostomy bags, which were put in a month ago when I was so sick, I was in hospital for two weeks.
*I graduated university with a 2:1 in film and television production
* Interned at my first job in the field
* I was lead actress in a short film that has since won two awards.
* I have also been cast lead in a feature by the same director. The excitement is real.
* I got engaged! A man named Ethan proposed to me after dating me for 3 months, because he found out I was seriously ill and he loves me. 3 and half years later we are still going strong.
*I lost my nana. Her and grandad will always live in a special place in my heart. I'm glad I was there for her last days.
*I wrote and directed my own short film, which has an original score and I'm so proud of.
*Lastly I started a page on Facebook to help me talk and vent about chronic illness. I was also in a short documentary about my struggles, which is interesting.
And... That's everything intresting. If you still remember me (Changed from Erurainia to LadyEru) feel free to message me, some of you literally saved me when I was younger. Know that I will always appreciate that.

#personal#personal thoughts#welcomeback#tumour#cancer#Fibromatosis#chronically sick#chronic fatigue#chroniclife#chronic pain#Still me#Fighter#reintroduction#allow me to reintroduce myself
2 notes
·
View notes
Text
IM FUCKING FREE
#she speaks#omfg it felt so weird coming out#but I’m free I’m finally FUCKING FREEEEEEEEEE#nephrostomy posting
4 notes
·
View notes
Text
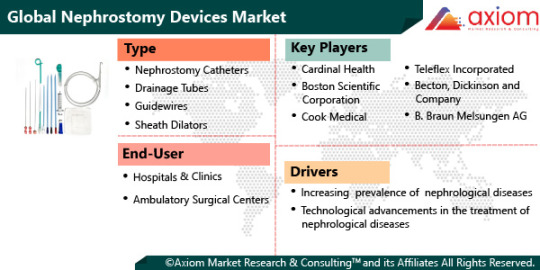
Nephrostomy Devices Market Size Estimation, Consumption, And Growth Opportunities Till 2028
COVID-19 IMPACT ANALYSIS ON GLOBAL NEPHROSTOMY DEVICES MARKET
The exclusive COVID-19 impact analysis report by Axiom MRC provides a 360 degree analysis of micro and macro-economic factors on the global nephrostomy devices market. In addition, complete analysis of changes on the global nephrostomy devices market expenditure, economic and international policies on supply and demand side. The report also studies the impact of pandemic on global economies, international trade, business investments, GDP and marketing strategies of key players present in the market. During COVID-19, stringent lockdown measures and restrictions in movement caused a massive supply chain crisis and also resulted decline in economic growth .During COVID-19 pandemic, global nephrostomy devices market was adversely affected due to supply chain distribution, which has certainly affected the market growth to a major extend. There was a severe effect in the supply of essential medical supplies and equipment such as atomizer, life-support machine, oxygen generator, etc. In the post COVID-19 phase, the market is expected to witness new growth opportunities and is expected to have an emerging demand in the upcoming years.
To know the scope of our report get a sample on https://www.axiommrc.com/request-for-sample/11360-nephrostomy-devices-market-report
MARKET OVERVIEW- GLOBAL NEPHROSTOMY DEVICES MARKET
MARKET DRIVERS
The global nephrostomy devices market is driven by increase in prevalence of nephrological and urological diseases such as kidney stone, bladder obstruction, urinary retention, bladder cancer, prostate cancer, hydronephrosis and other diseases. According to the National Center for Biotechnology Information (NCBI), 12% of the population in the world suffers due to kidney stones complications globally. Along with this, the rise in the number of procedures for percutaneous nephrostomy, is also expected to stimulate market growth in overall nephrostomy devices market in the coming years. Also, percutaneous nephrostomy offers certain advantages over conventional procedures. These include advantages like minimal blood loss, smaller incisions, reduced duration of hospitalization, etc. The rise in demand for minimally invasive procedures and growth in health awareness among the general population for availing better quality of life would help in the market growth in the coming years. All of the above mentioned factors are expected to boost the growth of the market in the upcoming years.
MARKET OPPORTUNITY
The market is expected to have growing new growth opportunities with rise in investment in research and development activities by the manufacturers to develop innovative and safer nephrostomy devices. In this market research, technological development plays a critical role for the production of products like drainage tubes, nephrostomy catheters, and sheath dilators among others. The investment in research and development certainly support for the production of precise nephrostomy devices with better precision and high efficiency. Likewise, growth and diversification of nephrostomy devices market along with increased collaboration with government agencies in providing better treatment facilities for treatment of urological diseases is expected to create new market opportunity during the projection period.
MARKET RESTRAINTS
The global nephrostomy devices market is expected to have market restraints like the stringent regulations imposed by the regulatory authorities for the production and quality of nephrostomy devices. This factor is expected to create hurdles for the market growth during the forecast period.
MARKET GROWTH CHALLENGES
The major growth challenge for the market is high cost of nephrostomy devices. Also others factors like risks associated with nephrostomy devices which includes issues like severe bleeding (haemorrhage), tube dislodgement, tube blockage, serious infection, damage to adjacent structures, etc. These factors are expected to be major growth challenge for the market.
CUMULATIVE GROWTH ANALYSIS
The report provides in-depth analysis of global Nephrostomy devices market, market size, and compound annual growth rate (CAGR) for the forecast period of 2022-2028, considering 2021 as the base year. With increasing demand for various Nephrostomy devices in various applications has led the increasing demand for market and is expected to witness the growth at a specific CAGR from 2022-2028.
MARKET SEGMENTAL OVERVIEW
The global nephrostomy devices market comprises of different market segment like type, end-user, and geography.
NEPHROSTOMY DEVICES MARKET BY TYPE
By type, the nephrostomy devices includes key segments of nephrostomy catheters, drainage tubes, guidewires, sheath dilators and others. The nephrostomy catheters segment is likely to have growing demand in the market. The nephrostomy catheters is benefits that are provided by them. These advantages includes, it can decrease the bleeding volume and pipes shedding rate due to which the efficiency is enhanced in comparison to other devices. The increasing usage of nephrostomy catheters in treatment of different urological diseases is expected to create ample of new growth opportunity for the market. On the other hand, drainage tubes segment is anticipated to witness growth at higher growth rate over the estimated time period.
NEPHROSTOMY TREATMENT DEVICES MARKET BY END-USER
The nephrostomy devices market is significantly studied for end-users like hospitals & clinics, ambulatory surgical centers and others. The hospitals and clinics segment is anticipated to lead in the global market from 2022 to 2028. Hospitals and clinics provide advanced care to their patients and offer reimbursements at some point of surgeries, accordingly witnessing exceptional growth. The ambulatory surgical centers is also expected to improve its growth in the projection period due to the advantages of providing a less complicated procedure and increased access. Furthermore, the growing demand for reduction in the surgical and post-surgical expenditure and the growing occurrence of urological diseases is predicted to be a number of the high-effect growth drivers for the ambulatory surgical centers section. Also research and development centers are expected to be a prominent growth segment in the upcoming years.
NEPHROSTOMY DEVICES MARKET BY GEOGRAPHY
The global nephrostomy devices market is studied for the following region North America, Europe, Asia-Pacific and Rest of the world (RoW). North America is anticipated to lead in the nephrostomy devices market during the forecast period (2022-2028). The region is likely to have growth rapid pace due rise in prevalence of diseases like urinary retention and kidney stones which has propelled the rise in demand for the nephrostomy devices. Another factor for market growth in the North America region is rapid adoption of technologically advanced devices. Also, rise in percutaneous nephrostomy procedures within the US has fuelled market growth within the nephrostomy devices market. Furthermore, increasing availability for different devices with varieties of technological advantages has indeed gained consumer attention which has driven the market growth.
COMPETITIVE LANDSCAPE ANALYSIS
The competitive landscape analysis of Nephrostomy devices market is majorly focused on expanding the global growth of nephrostomy devices with new product launches, partnership/ agreement and merger & acquisitions which has boosted the market growth at highest pace. Besides, presence of wide range of manufacturers operating in the market offers range of nephrostomy devices in different application to fulfill the required demand has further contributed healthy growth in the market.
The key players studied in market are Cardinal Health, Boston Scientific Corporation, Cook Medical, Teleflex Incorporated, Becton, Dickinson and Company, B. Braun Melsungen AG, Coloplast Group, Olympus Corp., Argon Medical Devices, Smith & Nephew, Uresil, Stryker Corporation among others.
RECENT DEVELOPMENT:
August 2019: Researchers at the Mayo Clinic reported development of a legitimate penile traction therapy (PTT) device for men with Peyronie’s disease that may work when used for just 30 to 90 minutes daily.
February2017: Cook Medical had launched Universa along with the two sets of percutaneous urinary drainage. The brand included foley catheters and ureteral stents in different configurations and sizes to meet the specific preferences and needs of patients and physicians.
Buy now Nephrostomy Devices Market Report https://www.axiommrc.com/buy_now/11360-nephrostomy-devices-market-report
About Us:
Axiom Market Research & Consulting™ is a full-service market research and data analytics company providing key market intelligence to global companies to take informed business decisions pertaining to their marketing strategy, investments, new product launches, market competition, consumer or end users, social media trends etc.
Axiom Market Research & Consulting™ offers market research services such as syndicated market research, custom market research, business consulting, and consumer/end user surveys. Under Business to Consumer (B2C) market research offerings, Axiom MRC assists its clients in finding quantitative information/preferences of its brands and services such as, awareness, usages, satisfaction, tracking, ethnicity etc. Axiom MRC offers data collection services through online surveys, social media, data processing and interpretation.
Axiom MRC with its experienced team of research and data analysts, has delivered more than 5000+ Market Research Projects, 3800+ Data Analytics Projects, 1200+ Business Support Projects and has a 800+ Global Client Base. Axiom Market Research & Consulting™ aims to become the preferred market research and data analytics company by providing key market intelligence solutions for client’s business growth.
Contact Us:
Axiom Market Research & Consulting™
3 Germay Dr. Ste 4 - 4666
Wilmington DE 19804
U.S.:- + 1 (845) 875-9786
U.K.:- + 44 (0) 20 3286 9707
Email: [email protected]
Website: https://www.axiommrc.com/
Blog: https://industrywatch24.com/
Follow On
LinkedIn: https://www.linkedin.com/company/axiom-market-research-and-consulting/
Twitter: https://twitter.com/AxiommrcCom
0 notes
Text
AKI
So basically for acute kidney injury you’re seeing an elevated creatinine. If you see that, you want to get the BUN to creatinine ratio. If it’s greater than 20, then you know that it’s pre-renal. That means there’s not enough perfusion to the kidneys. Could be due to heart failure with reduced ejection fraction or something causing decreased intravascular volume or cirrhosis.
If the BUN to creatinine ratio is not greater than 20 then it could be post renal AKI and that means there’s some sort of obstruction preventing outflow like a kidney stone or bladder cancer or BPH. So you would do a renal ultrasound to assess for that. Could show hydroureter or hydronephrosis. Then obviously remove the obstruction. You could put a Foley and if they have BPH, give them tamsulosin. Nephrostomy tube is the obstruction is at the level of the ureter.
If it’s not premium pre- or post-renal, then it’s intrarenal and that could be glomerulonephritis or acute tubular necrosis or acute interstitial nephritis. You could do urine analysis to look for red blood cell casts, which you see in glomerulonephritis, white blood cell casts, which you see in acute interstitial nephritis. Acute tubular necrosis shows muddy brown casts, seen in rhabdomyolysis. Nephrotic range proteinuria would be 3.5 g of protein in the urine a day.
3 notes
·
View notes
Text
Interventional Radiology Drainage Procedures Market is Booming Worldwide According to New Research Report
Interventional Radiology Drainage Procedures Market: Introduction
According to the report, the global interventional radiology drainage procedures market was valued at US$ 0.67 Bn in 2020 and is projected to expand at a CAGR of ~7% from 2021 to 2031. An abscess is an infected fluid collection within the body. Percutaneous abscess drainage uses imaging guidance to place a needle or catheter through the skin into the abscess to remove or drain the infected fluid. It offers faster recovery than open surgical drainage. In terms of type, the global interventional radiology drainage procedures market has been classified into catheter, stent, and others. Drainage catheters are available in different sizes, shapes, and types. An interventional radiologist will choose a catheter according to the type of fluid, along with other factors. High prevalence of target diseases and increase in preference for minimally invasive surgeries boost the growth of the global interventional radiology drainage procedures market.
Request a PDF Brochure - https://www.transparencymarketresearch.com/sample/sample.php?flag=B&rep_id=78248
North America dominated the global interventional radiology drainage procedures market in 2020 and the trend is anticipated to continue during the forecast period. High prevalence of diseases and well-established healthcare infrastructure that enables proper diagnosis and adoption of cost-effective minimally invasive procedure for abscess drainage can be attributed to the region’s large market share.
Asia Pacific is expected to be a highly lucrative market for interventional radiology drainage procedures during the forecast period. Majority of countries in Asia Pacific are developing countries and a number of players are making significant investment in the region. These factors propel the growth of the market in Asia Pacific. The rise in technological advancements in countries in terms of healthcare and medical research is anticipated to fuel the growth of the market in the region.
Request for Analysis of COVID19 Impact on Interventional Radiology Drainage Procedures Market - https://www.transparencymarketresearch.com/sample/sample.php?flag=covid19&rep_id=78248
Rise in Patient Preference for Minimally Invasive Surgeries, Cost-effective Drainage Procedures to Drive Global Market
The demand for minimally invasive surgeries has increased significantly over the past few years. Advantages such as fewer post-surgery complications & side effects, faster recovery, and shorter hospital stay prompt patients to opt for minimally invasive surgeries. Minimally invasive procedures utilize advanced technology to reach internal organs through small incisions leading to decreased pain, low risk of infection, shorter hospital stay, quicker recovery, less scarring, and reduced blood loss compared to traditional surgeries. Hence, rise in the number of minimally invasive surgeries is expected to drive the global interventional radiology drainage procedures market during the forecast period.
Interventional radiology procedures are less expensive than invasive procedures and other treatment alternatives. Moreover, existing reimbursement policies for image-guided drainage procedures drive the market. According to a survey conducted by the Urgent Care Association of America (UCAOA), about 51% of urgent care revenue is currently reimbursed by private insurance and 14% by Medicare. According to industry experts, favorable insurance coverage is anticipated to influence the global interventional radiology drainage procedures market by penetrating the sub-urban areas.
Request For Custom Research - https://www.transparencymarketresearch.com/sample/sample.php?flag=CR&rep_id=78248
Catheters to Dominate Global Market
In terms of type, the global interventional radiology drainage procedures market has been classified into catheter, stent, and others. The catheter segment has been segregated into multipurpose drainage catheters, nephrostomy drainage catheters, biliary drainage catheters, cholecystectomy catheters, and others. The catheter segment dominated the global interventional radiology drainage procedures market in 2020 and the trend is likely to continue during the forecast period. The growth of the segment can be attributed to the increase in demand for catheters, owing to the rise in cases of target diseases. In June 2020, Boston Scientific Corporation launched DIRECTSENSE Technology, a tool for monitoring the effect of radiofrequency (RF) energy delivery during cardiac ablation procedures in the U.S.
Abdomen to be Key Application Area
Based on application, the global interventional radiology drainage procedures market has been categorized into abdomen, pelvis, and others. The abdomen segment dominated the global interventional radiology drainage procedures market in 2020. Percutaneous computed tomography-guided catheter drainage is the standard treatment for most intra-abdominal abscesses, as it avoids anesthesia and possibly difficult laparotomy. It also prevents the possibility of wound complications from open surgery and could reduce the length of hospitalization.
Request For Discount - https://www.transparencymarketresearch.com/sample/sample.php?flag=D&rep_id=78248
Hospitals to be Promising End Users
In terms of end user, the global interventional radiology drainage procedures market has been classified into hospitals, specialty clinics, and ambulatory surgical centers. The hospitals segment dominated the market in 2020. The segment is expected to expand at the highest CAGR from 2021 to 2031. The growth of the segment can be attributed to increase in adoption of interventional radiology (IR) in hospitals due to technological advancements such as real-time imaging systems.
North America to Lead Interventional Radiology Drainage Procedures Market
The global interventional radiology drainage procedures market has been split into five major regions: North America, Europe, Asia Pacific, Latin America, and Middle East & Africa. North America dominated the global market in 2020, followed by Europe. North America accounted for a major share of the global interventional radiology drainage procedures market in 2020, owing to rise in adoption of new technology and increase in number of various disorders. The interventional radiology drainage procedures market in Asia Pacific is anticipated to expand at a higher CAGR from 2021 to 2031. The expansion of the interventional radiology drainage procedures market in the region can be ascribed to rise in prevalence of disorders and increase in awareness about the diagnosis and newer technologies available for the treatment.
Buy now Interventional Radiology Drainage Procedures Market Report - https://www.transparencymarketresearch.com/checkout.php?rep_id=78248<ype=S
Competition Landscape
The global interventional radiology drainage procedures market is fragmented due to the presence of a large number of leading players. Key players operating in the global market include AngioDynamics, BD, Boston Scientific Corporation, Cook Medical LLC, Teleflex Incorporated, UreSil, LLC, Merit Medical Systems, APR Medtech Ltd., Argon Medical Devices, Inc., Rocket Medical plc, Optimed, and Bioteque Corporation. New product development through robust R&D activities and mergers & acquisitions are the key strategies adopted by these players to expand business in the global interventional radiology drainage procedures market
More Trending Reports by Transparency Market Research:
https://www.prnewswire.com/news-releases/adhesion-barriers-market-to-ride-on-the-back-of-rising-need-to-address-post-operative-complications-market-to-exhibit-steady-growth-at-7-cagr-during-2019-to-2027-301324412.html
https://www.prnewswire.com/news-releases/emergence-of-europe-as-a-hub-for-advanced-drug-delivery-systems-to-benefit-the-pharmaceutical-excipients-market-tmr-301327924.html
https://www.prnewswire.com/news-releases/increased-preference-over-conventional-systems-in-medical-imaging-to-boost-pacs-and-ris-market-transparency-market-research-301333813.html
About Us
Transparency Market Research is a global market intelligence company, providing global business information reports and services. Our exclusive blend of quantitative forecasting and trends analysis provides forward-looking insight for thousands of decision makers. Our experienced team of analysts, researchers, and consultants, uses proprietary data sources and various tools and techniques to gather and analyze information.
Our data repository is continuously updated and revised by a team of research experts, so that it always reflects the latest trends and information. With a broad research and analysis capability, Transparency Market Research employs rigorous primary and secondary research techniques in developing distinctive data sets and research material for business reports.
Contact
Transparency Market Research,
90 State Street, Suite 700,
Albany, NY 12207
Tel: +1-518-618-1030
USA - Canada Toll Free: 866-552-3453
Website: https://www.transparencymarketresearch.com/
0 notes
Text
Juniper Publishers- Open Access Journal of Case Studies

Acute Tubular Necrosıs after Nephrectomy: Case Presentatıon
Authored by Ebru Canakci
Abstract
Acute renal failure (ARF) has a clinical presentation with declining renal function and glomerular filtration rate within hours-days. Ischemic ATN, contrary to prerenal azotemia, is not immediately cured upon the recovery of renal perfusion. In its severe form, renal hypoperfusion leads to bilateral renal cortical necrosis and irreversible renal insufficiency. Ischemic ATN often develops as a result of major surgical intervention, trauma, severe hypovolemia, sepsis and severe burns. Acute kidney injury (AKI) is one of the frequently encountered causes of morbidity and mortality in hospitals. The aim of this study is to present the case with ATN after major surgery and subsequent permanent kidney injury in light of the information from the literature.
Keywords: Nephrectomy; Acute Tubular Necrosis; Hemodialysis
Introductıon and Objectıve
Acute renal failure (ARF) has a clinical presentation with declining renal function and glomerular filtration rate within hours-days. Although there are several differences in the definition; it can be described as an increase in the serum creatinine level; at a rate of at least 50% of the basal level or more than 0.5mg/dL [1]. According to “Kidney Disease Improving Global Guidelines (KDIGO) 2012” AKI is diagnosed if any one of the following three conditions are present:
a) Increase in the serum creatinine levels by 0.3mg/dL or over within 48 hours
b) Known or estimated increase in the serum creatinine levels by ≥1.5 fold of the basal level within the last 7 days
c) Micturation of < 0.5ml/kg/hr within the last 6 hours.
Ischemic or nephrotoxic acute tubular necrosis (ATN) makes up of more than 90% of the renal ARF. Other than these, large vessels, glomerular microvessels and diseases of tubulointerstitium can also lead to renal ARF [2,3]. Ischemic ATN, contrary to prerenal azotemia, is not immediately cured upon the recovery of renal perfusion. In its severe form, renal hypoperfusion leads to bilateral renal cortical necrosis and irreversible renal insufficiency. Ischemic ATN often develops as a result of major surgical intervention, trauma, severe hypovolemia, sepsis and severe burns. Nephrotoxic ATN is linked to endogenous or exogenous toxins. Toxins cause intrarenal vasoconstriction, direct tubular toxicity and/or intratubular obstruction and thus lead to ARF [4]. Acute kidney injury (AKI) is one of the frequently encountered causes of morbidity and mortality in hospitals. The aim of this case presentation is to emphasize the importance of diagnosing AKI that can develop during the postoperative period of a major surgery and planning the appropriate treatment protocol.
Case Presentatıon
A 52-year-old male patient with no previous history of renal disease was scheduled for left-side nephrectomy with a diagnosis of renal collecting duct tumor. The patient had a history of smoking, with 20 packets/year. He was not on any continuous medication. Hb was 14gr/dL. There were no pathologies in other laboratory parameters. The patient’s BMI was 30kg/m2, Mallampati score was Class II and the patient was in ASA II risk level. Consultation with a pulmonologist was requested because of his smoking history. Respiratory function test was within normal levels. The patient was taken to surgery upon requesting sufficient blood. The patient was scheduled for laparoscopic left side nephrectomy. Operation lasted 8 hours. The patient underwent intraoperative ECG monitorization and invasive blood pressure monitorization and his perioperative average arterial pressure was maintained over 60mmHg. Perioperative micturation was closely monitored, it was maintained at or above 0.5ml/kg/hour. There was 500ml perioperative blood loss, the patient did not have intraoperative blood transfusion. Considering the major surgery and the weight of the patient, intraoperative fluid exigency was calculated and fluid requirement was met. At the end of the surgery, the patient woke up without any complications and firstly taken to recovery unit and then to surgical intensive care. At the postoperative 48th hour, the patient had oligoanuria and had respiratory failure. ATN and acute lung edema was suspected. Serum creatinine level was 7mg/dL and arterial blood gas had metabolic acidosis. Lung x-rays showed Kerley -B lines and stasis ralles were heard in both lungs. Right jugular hemodialysis catheter was placed and the patient was taken to emergency hemodialysis, 4 liters of ultrafiltration was performed. After hemodialysis (HD) the patient still had respiratory problems and thus non-invasive mechanical ventilation was performed. In the follow-up monitorization, serum creatinine levels did not decrease and the patient was taken to hemodialysis every other day. Renal Doppler USG revealed renal cortical necrosis. On his 7th day in the emergency care unit, the patient was transferred to nephrology unit. The patient was followed up for 3 more days in the nephrology unit without any complications and was scheduled for arteriovenous-fistula surgery. After recommending controls in the nephrology outpatient clinic and hemodialysis every other day, the patient was discharged.
Discussion
Clinically, ATN can be analyzed in three phases: Initiation, maintenance, and recovery.
Initiation phase
It is the period where exposure to ischemic or toxic event and damage to parenchyma occur. This phase can last hoursdays and ATN can potentially be prevented in this phase.
Maintenance phase
It is the phase where parenchyma damage settles and GFR is stabilized at 5-10ml/min. It usually lasts 1-2 weeks. In this phase, micturation level is at its lowest. Uremic complications mostly occur during the maintenance phase.
Recovery phase
It is the phase of renal tissue repair and regeneration and renal function recovery. It lasts approximately 4 weeks. The initiation of recovery is understood when micturation progressively increases and serum creatinine levels start decreasing within a couple of days. Post-ATN diuresis is based on osmotic diuresis, which is related to the clearance of the accumulated water and salt and solutes. Sometimes, inappropriate and excess amounts of diuresis can be seen. At this phase, problems in fluid-electrolyte balance can be seen [5-7].
ARF treatment strategy depends on the etiology. Prerenal azotemia rapidly regresses upon the recovery of renal perfusion. Hemorrhage is replaced with erythrocyte suspension, and plasma loss (burn, pancreatitis) is replaced with isotonic fluids. Urinary and gastrointestinal losses are usually hypotonic. For this reason, the initial treatment should be with 0.45% NaCl [8].
In postrenal azotemia, the goal is to eliminate the obstruction (catheter, nephrostomy, stent). In 5% of patients, a syndrome, which causes temporary salt loss develops [9]. Renal -intrinsic- ARF treatment can be studied under four headings: precautions, specific treatments, treatment of complications and dialysis [10].
Precautions
Maintaining optimal cardiovascular function and intravascular volume are the most important actions. Diuretics, NSAID drugs, ACE inhibitors and other vasodilators should be used very carefully, especially in individuals with hypovolemic and renovascular disease [11].
Drug levels must be followed up in aminoglycoside and cyclosporine use. Diuretic stress and alkalinization of the urea are useful in urate, methotrexate nephropathy and rhabdomyolysis. N-acetyl cysteine can be preventive in radiocontrast nephrotoxicity and acetaminophen toxicity [12].
While certain interventions that regulate hemodynamic status and decrease cellular damage were found useful in the experimental studies, their clinical benefits have not been shown [13].
Treatment of complications
The most important points in ARF treatment are the maintenance of fluid-electrolyte balance, improvement of acidosis, improvement of diet, and treatment of uremic signs and symptoms. Treatment approaches should be determined according to the characteristics of the patient [14].
Acute oliguric-intrinsic-renal ARF mortality is around 50% (15% in obstetric patients, 30% in toxin-associated ARFs, and 60% in ARFs after trauma-major surgery). Presence of oliguria and creatinine levels higher than 3mg/dL at the time of diagnosis are indicators of poor prognosis. In elderly patients with multiple organ failure, mortality rate is high. With the failure of more than three organ systems in ARF, mortality is almost 100% [15]. The most common cause of mortality is the infection, followed by fluid-electrolyte imbalances. Death, as a direct complication of uremia, is rare (2.3%) [16]. Renal function is recovered in most patients. In 5% of the patients, however, it is irreversible. In our case, permanent renal injury was suspected and fistula surgery was planned, and the patient was admitted to hemodialysis program (HD) every other day. Approximately 15% of the cases proceed into terminal renal insufficiency. In 50% of the cases, subclinical functional defects remain [17].
Intermittent hemodialysis is the most frequently used renal replacement therapy in ARF. Hemodialysis treatment largely depends on the rate of nitrogenous waste formation and whether fluid tolerance is good. HD treatment of 4 hours, 3 sessions per week provides sufficient replacement for oligoanuric patient. In patients with significant level of residual renal functions (as in non-oliguric patients), weekly number of HD sessions can be less. On the contrary, daily HD can be required for patients with severe hypercatabolism or cannot tolerate excessive fluid [18].
Conclusion
In conclusion, it should be kept in mind that in cases who underwent major surgery, ATN can develop during the postoperative period. Postoperative care after major surgery must be performed in the intensive care unit. Hourly follow up of micturation and hemorrhage, and close hemodynamic follow up must never be neglected. In the case of ARF, cooperation between the intensivist and the nephrologist may ensure that the patient recovers from the renal injury with minimum damage. In tertiary intensive care units, nephrologist must perform like an intensive care nephrologist and must not neglect his/her daily visit to the intensive care unit.
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php
#juniper publishers contact info#juniper publishers journals#Surgical case reports#Emergency Medicine#Hospice and Palliative Medicine#Infectious Diseases
0 notes
Text
PCN catheter
Receive embryologic typical turn of events; the human kidney is usually located between T12 and L3 spine (right to a great extent slightly lower than the left). It is usually calculated with the shaft of his boss increasingly dorsal and median while the low post is more ventral and horizontal.
Kidney had their sagittal plane (through the hilum) are coordinated in the direction of the sagittal plane of the body. Therefore, the kidneys tend to reverse 30 to 50 degrees from the coronal plane of the body and tend internal 30 to 50 degrees from the sagittal plane.
The right kidney is generally a few centimeters lower or second rate compared with one kidney side. At the point when patients are likely, the two kidneys will in general move slightly superior.
PCN arrangements can endanger some organ covers and structures including the pleura, stomach, intestine, spleen, and liver. Of these, pleural and abdominal injuries are the most famous. Pleural stretching out to the lower edge of the twelfth rib along the paravertebral line. In this way, limited pleural injury when the composition of PCN is below the twelfth rib. The position at the top of the twelfth rib will usually cut the stomach.
A PCN Catheter little, plastic round tube with a pipe-shaped tip. It is embedded into the lower midsection inherent individual and system settings of water containing substances that destroy microbes. In general, this is done through an endoscope or a camera or a small laser gadget. These treatment strategies require a medical procedure; that as it may, it is less obtrusive than the usual method of phlebotomy, to the system, for example, intraduodenal and tonsillectomy.
Some physical side effects of PCN is torture abdomen, swelling, difficulty breathing, walking, fever, and weight loss. The original inconvenience that may occur given the intricacies of the circulatory system, including apoplexy and rectum malignant growth. It is conceivable to endure inconveniences such as in the most extreme case, that as possible. In this way, PCN catheters are used in medicine.
Percutaneous nephrostomy (PCN) catheters are used for short preoccupation associated with obstruction of urinary calculi optional.
Other normal signs include:
· The transfer of urine from the kidney collecting frame when repairing fistula or hole came about because of terrible injury or iatrogenic, threatening or burning fistula, or haemorrhagic cystitis,
· Treatment of obstructive uropathy nondilated,
· Treatment of involvement is identified with a kidney transplant,
· Access to mediation, for example, direct current mix to dissolve stones, chemotherapy, and anti-toxin or antifungal treatment,
· Decompression of various nephric or perinephric fluid (eg urinomas, abscess).
Percutaneous nephrostomy (PCN) is an intervention method that is used to calm the framework obstructed kidneys' meeting. It is a strategy that is well sheltered used for making a channel for gadget embedding’s, rocks evacuates, or to take a very small network for assessment, narrowing dilated ureter and ureteral stenting. This strategy should be performed by radiologists master in interventional radiology or urologist.
The scope of the PCN catheter position has been extended and is generally used in the strategy of symptoms and restorative. Gastroenterology disposables & Pigtail catheter manufacturers try and are supported by a specialist before filing for clinical use.
Used for temporary or perpetual waste and urine from the kidney system by immediately cutting checks denominated in distal
· Highly radiopaque for better representation
· Pigtail tip design for maintenance of the distal tip in the renal pelvis
· Soft and Flexible material for solace patients
0 notes
Text
Nurse Ramble
I was feeling or thinking, call it what you may. I figured I would type. Its not like I have some grand point to make, in fact, this is probably going to be in every way disjointed rambling.
I saw a photograph today with text on it, a meme of a statue with a delirious grin that said “when the customer tells a bad joke but you got bills to pay.” Its funny, I get the joke, I think its so true. On the flip side, from a nurses perspective I feel like every time I laugh at some dumb joke I bring joy into the room and I LOVE making my patient feel good. I learned, even, to really like stupid jokes. Gives you a ten-second break. Comedic relief.
I had a lady this week who I fought for all day, multiple calls to the doctor thru the day, numerous interventions on her BP, BG, nephrostomy tubes, skin breakdown, mental status you name it. When she finally came to in the afternoon and she was alert and (mostly) oriented, she didn’t like me at all. But she didn’t see what I had done for her. I am less satisfied because of that. Should I be? No. I probably intervened at a time, where if I had just observed she might have declined. I maybe saved her life. I don’t know. I still want my patients to like me.
Her niece hated me too. At the end of the day the niece showed up, “I could just scream at the day shift!” I am the day shift. I explained everything to her. She still wasn’t happy. Can’t change someone who is set on being upset before they even walk in the door.
Back to the positive. One patient who I grew close to got discharged and she thought I was an angel. I did literally nothing special for her. At all. There were very few changes in her condition that ever required intervention, but she loved me. Isn’t that the way it goes? You do your best, and those that require the most work oftentimes have no appreciation for you. I still smile for them and I still try my hardest. I don’t give a shit about HCAHPS, I genuinely want my patients and families to be happy. Even if the patient dies, I want them/ the family to know we did our best, and I want them to appreciate that.
Oncology is very alike other specialties and very different too. Med-surg is somehow a whole other world but with the same physical skill set. Its the emotional and psychological skills that differ. I’m not a person who is in touch with emotions very much. Maybe I’m a realist? Maybe I’m an idealist? I can’t pin it down even though its inside of me. I LOVE oncology, but I am in awe when I see another nurse with more emotional intelligence than me. I just can’t be convinced that it can be learned. Its more of an inherent way of being. I feel like typing this out is somehow the most emotionally intelligent I get.
When my patients cry, I just hug or hold hands. I can’t find words, but I think maybe just the gesture could be enough comfort. Sometimes there isn’t words anyone could say anyway when it comes to the big C.
Cancer. Why are people so afraid? That’s not a serious question, I understand why they are afraid. I don’t get it when they beat around the word though. Its only 6 little letters. God, though, does it pack a punch. One patient didn’t know “leukemia” means cancer. No one had ever explained it to her. She went an entire week thinking she had some benign blood disorder or something. My stomach dropped, and here comes the lack of emotional intelligence. “Yes leukemia is cancer. I can get you some printed information if you would like.” I could kill myself for being so insensitive.
I started travel nursing, and went all the way across the country. Sometimes I work days, sometimes nights. I really don’t care either way. Turns out, I really like having residents around! Convenience maybe. There’s nothing worse than having to call a sleeping doctor. I love day/night rotations where someone is always awake and they’re not irritated that you called at 4 am because they were up working anyways. Last hospital, the doctor got friggin mad at me because he didn’t know his patient had an NG tube for feeding. THE DOCTOR DIDN’T KNOW. THATS HIS JOB. Turns out GI had ordered it, and I guess the teams don’t COMMUNICATE? That’s fucked up, I think. He was mad and told me I should have called GI. It was 7 am. I told the day shift nurse to call GI. It’s a 24 hour job, nursing.
Some teams of nurses are really great about that, taking on what the last shift couldn’t get done. Some teams have this idea that you have to “get everything done” as if the patient quits being a patient at 7 PM and everything starts over at 7:30 when report is over. That’s bullshit btw. Sick human beings don’t stop being sick human beings just because nurses have to go home. I believe the best in people until they show me otherwise, and I give the last shift the benefit of the doubt. I know they did everything they could until the clock ran out and then it’s time to go home. I take over from there.
Some nurses are really bullies. You can read through some posts from earlier this year to see my bullying story. “You” being whoever is reading this. If anyone read this. Doubt it. Its too long lol.
This typing has helped. Maybe I’ll write a book about nursing in a few years, if I ever figure out how to keep my thoughts from being so scrambled.
1 note
·
View note