#interventional radiology procedures
Explore tagged Tumblr posts
Text

Orthopedic veterinary surgeons in Singapore specializing in fracture repair, TPLO surgery, spinal surgery, hip replacement, and orthopedic procedures for dogs and cats.
Web Page: https://beecroft.com.sg/beecroftsg/project-two-3amwl
#cancer operations dogs and cats#interventional radiology subs and stenting#orthopedic surgical procedures for dogs and cats#fracture repair Alexandra#fracture repair vet Singapore#TPLO surgery vet Singapore#Surgery tumor removal#Surgery tumour removal#Ear surgery Singapore#Spinal surgery dog Singapore#Hip replacement surgery dog Singapore#Fracture spine vet#Surgery airway#Orthopedic vet Singapore#Orthopaedic vet Singapore#Dog spinal surgery
2 notes
·
View notes
Video
youtube
Vertebroplasty and Kyphoplasty #chronicpain #pain #shorts #usa #painmana...
#youtube#radiologist interventionalradiology intervention usa procedures radiology injection interventionalradiologist painmanagement scienceonl
0 notes
Text
Introduction:
In the realm of modern medicine, certain techniques stand as pillars of innovation, revolutionizing the way procedures are performed and patient outcomes are improved. One such technique is the Seldinger Technique. Developed by Dr. Sven-Ivar Seldinger in 1953, this method has become a cornerstone in various medical procedures, from inserting central venous catheters to performing angiography and even certain types of biopsies.
In this comprehensive guide, we delve into the intricacies of the Seldinger Technique, its applications, and its significance in contemporary healthcare.
#CARDIAC CATHETERIZATION#CENTRAL VENOUS ACCESS#EMERGENCY MEDICINE#HEALTHCARE ADVANCEMENTS#INTERVENTIONAL RADIOLOGY#MEDICAL INNOVATION#MEDICAL PROCEDURES#MINIMALLY INVASIVE PROCEDURE#SPATIENT SAFETY#SELDINGER TECHNIQUE
0 notes
Text
How to have cancer

THIS WEEKEND (November 8-10), I'll be in TUCSON, AZ: I'm the GUEST OF HONOR at the TUSCON SCIENCE FICTION CONVENTION.

I've got cancer but it's probably (almost certainly, really) okay. Within a very short period I will no longer have cancer (at least for now). This is the best kind of cancer to have – the kind that is caught early and treated easily – but I've learned a few things on the way that I want to share with you.
Last spring, my wife put her arm around my waist and said, "Hey, what's this on your rib?" She's a lot more observant than I am, and honestly, when was the last time you palpated your back over your left floating rib? Sure enough, there was a lump there, a kind of squishy, fatty raised thing, half a centimeter wide and about four centimeters long.
I'm a 53 year old man with a family history of cancer. My father was diagnosed with lymphatic cancer at 55. So I called my doctor and asked for an appointment to have the lump checked over.
I'm signed up with Southern California Kaiser Permanente, which is as close as you come to the Canadian medicare system I grew up under and the NHS system I lived under for more than a decade. Broadly speaking, I really like KP. Its app – while terrible – isn't as terrible as the other apps, and they've taken very good care of me for both routine things like vaccinations and checkups, and serious stuff, like a double hip replacement.
Around the time of The Lump, I'd been assigned a new primary care physician – my old one retired – and so this was my first appointment with her. I used the KP app to book it, and I was offered appointments six weeks in the future. My new doc was busy! I booked the first slot.
This was my first mistake. I didn't need to wait to see my PCP to get my lump checked over. There was really only two things that my doc was gonna do, either prod it and say, "This is an extremely common whatchamacallit and you don't need to worry" or "You should go get this scanned by a radiologist." I didn't need a specific doctor to do this. I could have ridden my bike down to the KP-affiliated Urgent Care at our local Target store and gotten an immediate referral to radiology.
Six weeks go by, and my doc kind of rolls the weird lump between her fingers and says, "You'd better go see a radiologist." I called the Kaiser appointment line and booked it that day, and a couple weeks later I had a scan.
The next day, the app notified me that radiology report was available in my electronic heath record. It's mostly technical jargon ("Echogenic areas within mass suggest fatty component but atypical for a lipoma") but certain phrases leapt out at me: "malignant masses cannot be excluded. Follow up advised."
That I understood. I immediately left my doctor a note saying that I needed a biopsy referral and set back to wait. Two days went by. I left her a voice message. Another two days went by. I sent another email. Nothing, then a weekend, then more nothing.
I called Kaiser and asked to be switched to another Primary Care Physician. It was a totally painless and quick procedure and within an hour my new doc's intake staff had reviewed my chart, called me up, and referred me for a biopsy.
This was my second mistake. When my doctor didn't get back to me within a day, I should have called up KP and raised hell, demanding an immediate surgical referral.
What I did do was call Kaiser Member Services and file a grievance. I made it very clear that when I visited my doctor, I had been very happy with the care I received, but that she and her staff were clearly totally overloaded and needed some kind of administrative intervention so that their patients didn't end up in limbo.
This is a privilege. I'm a native English speaker, and although I was worried about a serious illness, I didn't have any serious symptoms. I had the ability and the stamina to force action in the system, and my doing so meant that other patients, not so well situated as I was, would not be stuck where I had been, with fewer resources to get un-stuck.
The surgeon who did the biopsy was great. He removed my mass. It was a gross lump of yellowy-red gunk in formaldehyde. He even let me photograph it before it went to pathology (warning, gross):
https://www.flickr.com/photos/doctorow/54038418981/
They told me that the pathology would take 2-5 days. I reloaded the "test results" tab in the KP website religiously after 48 hours. Nothing was updated. After five days, I called the surgical department (I had been given a direct number to reach them in case of postsurgical infections, and made a careful note of it).
It turned out that the pathology report had been in hand for three days at that point, but it was "preliminary" pending some DNA testing. Still, it was enough that the surgeon referred me to an oncologist.
This was my third mistake: I should have called after 48 hours and asked whether the pathology report was in hand, and if not, whether they could check with pathology. However, I did something very right this time: I got a phone number to reach the specialist directly, rather than going through the Kaiser main number.
My oncologist appointment was very reassuring. The oncologist explained the kind of cancer I had ("follicular lymphoma"), the initial prognosis (very positive, though it was weird that it manifested on my rib, so far from a lymph node) and what needed to happen next (a CT/PET scan). He also walked me through the best, worst and medium-cases for treatment, based on different scan outcomes. This was really good, as it helped me think through how I would manage upcoming events – book tours, a book deadline, work travel, our family Christmas vacation plans – based on these possibilities.
The oncologist gave me a number for Kaiser Nuclear Medicine. I called them from the parking lot before leaving the Kaiser hospital and left a message for the scheduler to call me back. Then I drove home.
This was my fourth mistake. The Kaiser hospital in LA is the main hub for Kaiser Southern California, and the Nuclear Medicine department was right there. I could have walked over and made an appointment in person.
Instead, I left messages daily for the next five days, waited a weekend, then called up my oncologist's staff and asked them to intervene. I also called Kaiser Member Services and filed an "urgent grievance" (just what it sounds like) and followed up by filing a complaint with the California Patient Advocate:
https://www.dmhc.ca.gov/
In both the complaint and the grievance, I made sure to note that the outgoing message at Nuclear Medicine scheduling was giving out false information (it said, "Sorry, all lines are busy," even at 2am!). Again, I was really careful to say that the action I was hoping for was both a prompt appointment for me (my oncologist had been very insistent upon this) but also that this was a very broken system that would be letting down every patient, not me, and it should be fixed.
Within a couple hours, I had a call back from KP grievances department, and an hour after that, I had an appointment for my scan. Unfortunately, that was three weeks away (so much for my oncologist's "immediate" order).
I had the scan last week, on Hallowe'en. It was really cool. The gadget was awesome, and the rad-techs were really experienced and glad to geek out with me about the way the scanner and the radioactive glucose they infused in me interacted. They even let me take pictures of the scan visualizations:
https://www.flickr.com/photos/doctorow/54108481109/
The radiology report was incredibly efficient. Within a matter of hours, I was poring over it. I had an appointment to see the doc on November 5, but I had been reading up on the scans and I was pretty sure the news was good ("No enlarged or FDG avid lymph nodes are noted within the neck, chest, abdomen, or pelvis. No findings of FDG avid splenic or bone marrow involvement").
There was just one area of concern: "Moderate FDG uptake associated with a round 1.3 cm left inguinal lymph node." The radiologist advised the oncologist to "consider correlation with tissue sampling."
Today was my oncology appointment. For entirely separate reasons, I was unable to travel to the hospital today: I wrenched my back over the weekend and yesterday morning, it was so bad that I couldn't even scratch my nose without triggering unbearable spams. After spending all day yesterday in the ER (after being lifted out of my house on a stretcher), getting MRIs and pain meds, I'm much better off, though still unable to get out of bed for more than a few minutes at a time.
So this morning at 8:30 sharp, I started calling the oncology department and appointment services to get that appointment changed over to a virtual visit. While I spent an hour trying various non-working phone numbers and unsuccessfully trying to get Kaiser appointment services to reach my oncologist, I tried to message him through the KP app. It turns out that because he is a visiting fellow and not staff, this wasn't possible.
I eventually got through to the oncology department and had the appointment switched over. The oncology nurse told me that they've been trying for months to get KP to fix the bug where fellows can't be messaged by patients. So as soon as I got off the phone with her, I called member services and filed another grievance. Why bother, if I'd gotten what I needed? Same logic as before: if you have the stamina and skills to demand a fix to a broken system, you have a duty to use them.
I got off the phone with my oncologist about an hour ago. It went fine. I'm going to get a needle biopsy on that one suss node. If it comes back positive, I'll get a few very local, very low-powered radiation therapy interventions, whose worst side effect will be "a mild sunburn over a very small area." If it's negative, we're done, but I'll get quarterly CT/PET scans to be on the safe side.
Before I got off the phone, I made sure to get the name of the department where the needle biopsy would be performed and a phone number. The order for the biopsy just posted to my health record, and now I'm redialing the department to book in that appointment (I'm not waiting around for them to call me).
While I redial, a few more lessons from my experience. First, who do you tell? I told my wife and my parents, because I didn't want to go through a multi-week period of serious anxiety all on my own. Here, too, I made a mistake: I neglected to ask them not to tell anyone else. The word spread a little before I put a lid on things. I wanted to keep the circle of people who knew this was going on small, until I knew what was what. There's no point in worrying other people, of course, and my own worry wasn't going to be helped by having to repeat, "Well, it looks pretty good, but we won't know until I've had a scan/my appointment/etc."
Next, how to manage the process: this is a complex, multi-stage process. It began with a physician appointment, then a radiologist, then a pathology report, then surgery, then another pathology report, then an oncologist, then a scan, then another radiologist, and finally, the oncologist again.
That's a lot of path-dependent, interdepartmental stuff, with a lot of ways that things can fall off the rails (when my dad had cancer at my age, there was a big gap in care when one hospital lost a fax from another hospital department and my folks assumed that if they hadn't heard back, everything was fine).
So I have been making extensive use of a suspense file, where I record what I'm waiting for, who is supposed to provide it, and when it is due. Though I had several places where my care continuity crumbled some, there would have been far more if I hadn't done this:
https://pluralistic.net/2024/10/26/one-weird-trick/#todo
The title of this piece is "how to have cancer," but what it really boils down to is, "things I learned from my own cancer." As I've noted, I'm playing this one on the easiest setting: I have no symptoms, I speak and write English fluently, I am computer literate and reasonably capable of parsing medical/technical jargon. I have excellent insurance.
If any of these advantages hadn't been there, things would have been a lot harder. I'd have needed these lessons even more.
To recap them:
See a frontline care worker as soon as possible: don't wait for an appointment with a specific MD. Practically any health worker can prod a lump and refer you for further testing;
Get a direct phone number for every specialist you are referred to (add this to your phone book); call them immediately after the referral to get scheduled (better yet, walk over to their offices and schedule the appointment in person);
Get a timeframe as to when your results are due and when you can expect to get a follow-up; call the direct number as soon as the due-date comes (use calendar reminders for this);
If you can't get a call back, an appointment, or a test result in a reasonable amount of time (use a suspense file to track this), lodge a formal complaint with your insurer/facility, and consider filing with the state regulator;
Think hard about who you're going to tell, and when, and talk over your own wishes about who they can tell, and when.
As you might imagine, I've spent some time talking to my parents today as these welcome results have come in. My mother is (mostly) retired now, and she's doing a lot of volunteer work on end-of-life care. She recommends a book called Hope for the Best, Plan for the Rest: 7 Keys for Navigating a Life-Changing Diagnosis:
https://pagetwo.com/book/hope-for-the-best-plan-for-the-rest/
I haven't read it, but it looks like it's got excellent advice, especially for people who lack the self-advocacy capabilities and circumstances I'm privileged with. According to my mom, who uses it in workshops, there's a lot of emphasis on the role that families and friends can play in helping someone whose physical, mental and/or emotional health are compromised.
So, that's it. I've got cancer. No cancer is good. This cancer is better than most. I am almost certainly fine. Every medical professional I've dealt with, and all the administrative support staff at Kaiser, have been excellent. Even the doc who dropped the ball on my biopsy was really good to deal with – she was just clearly drowning in work. The problems I had are with the system, not the people. I'm profoundly grateful to all of them for the help they gave me, the interest and compassion they showed, and the clarity and respect they demonstrated in my dealings with them.
I'm also very grateful to my wife, my parents, and my boss at EFF, all of whom got the news early and demonstrated patience, love, and support that helped in my own dark hours over the past couple of months.
I hope you're well. But you know, everyone gets something, eventually. When you find yourself mired in a broken system full of good people, work the system – for yourself and for the people who come behind you. Take records. Make calls.
Look after yourself.

If you'd like an essay-formatted version of this post to read or share, here's a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2024/11/05/carcinoma-angels/#squeaky-nail
396 notes
·
View notes
Text


more hospital au svsss
in interventional radiology (or anything involving procedural x-rays) you need to wear a lead apron and thyroid guard.. there’s usually lots of spares but usually the regulars invest in their own. they are very heavy lol. but it does help keep you cozy in a freezing procedure room
#moshang#svs3#HEHE… I LOVE IR ATTENDING MOBEI JUN…..#cold. Authoritative. A little bit of a diva#the marriage of radiology and surgery…#lead is supposed to go down to like your thighs… SQHs knees are going to be so protected….#sqh is talking shit about neuro(rad?) attending SQQ asking for unreasonable neuro checks for the normal hospital floor#mbj doesnt know how to show affection except by continuing to bother his former scrub nurse#whos now been promoted to charge...#sqh is gonna let him.. hes addicted to the little nod mbj does when he hands him the right instrument without him having 2 ask for it..
84 notes
·
View notes
Note
Hi! Just found your blog and I think I’m in love, this is my new holy grail.
Could you give me a quick rundown of procedures that have to do with bone marrow? What are they, why are they done, etc.
PS: is there any niche topic you’ve been wanting to mention but have never been asked about? If so, now’s your chance to nerd out! :)
- 🦾
Oh dear anon, you've just activated me like a sleeper agent... I've already done a ton of research on bone marrow procedures for a whumpy daydream, and I just learned about it in school. Little did you know, this is the niche topic that I could talk about for days.
Bone marrow, baby!
So bone marrow in the innermost part of the bones and is most abundant in the long bones (femurs, humeruses, radiuses, ulnas, tibias, and fibulas) and pelvis. The primary function of bone marrow is to produce blood cells, including erythrocytes (red blood cells [RBCs]), leukocytes (white blood cells [WBCs]), and platelets). RBCs carry oxygen, WBCs fight infections, and platelets clump together to form clots and stop bleeding. The bone marrow cells that produce these blood cells are called hematopoietic [he-MAT-o-po-EE-tic] stem cells.
Bone marrow dysfunction can manifest in clinical disorders such as anemias (sickle cell, beta thalassemia, aplastic), malignancies (leukemia, myeloma, lymphoma, polycythemia vera), and other non-anemia deficiencies (leukopenia [deficiency of WBCs], neutropenia [deficiency of neutrophils, a type of WBC], thrombocytopenia [deficiency of platelets]). These disorders can co-occur and result from each other. Some medications like chemotherapy and some anti-infectives can also suppress the bone marrow.
Procedures involving the bone marrow include aspiration and biopsy, donation, and transplant.
Bone marrow aspiration and biopsy: This is a procedure to take a sample of the bone marrow for the purposes of diagnosing any of the above disorders. It is not performed if the patient has bleeding disorders like hemophilia. This is usually an outpatient procedure done in an interventional radiology (procedures are guided by x-ray or other imaging methods) unit. The patient will be admitted to the unit and asked to change into a gown, then will get an IV and have a full set of vitals taken (temperature, heart rate, respiratory rate, blood pressure, oxygen saturation). They will be asked to sign a consent form after the procedure and its risks and benefits have been explained. When it's time for their procedure, the patient will be wheeled in a hospital bed to the procedure room (see the image below) by a nurse.

All staff involved in the procedure will be wearing lead-lined aprons, surgical masks, and goggles. In the procedure room, they will move from the bed to a table, or will be assisted if needed, and positioned on their stomach with a pillow under their hips. They will be hooked up to a cardiac monitor and put on an end-tidal CO2 sampling nasal cannula (see the image below).

They may or may not be given fentanyl and midazolam (Versed) through their IV for pain relief and mild sedation. They will still be awake and aware during the procedure. I've seen people make small talk with the staff for their entire procedures. The patient will then be draped everywhere except for the site (over one of the iliac crests of the pelvis) of the procedure. The radiologist will inject lidocaine into the skin around the site and clean it with betadine (a disinfectant similar to iodine). The radiologist will then make a small incision at the site and insert a needle containing a fine tube down to the bone (see the image below).
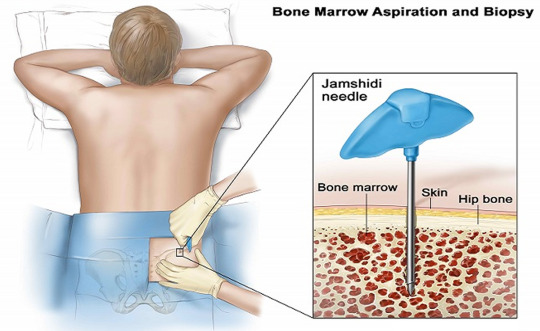
The radiologist will work the needle into the bone with a twisting motion. The patient won't feel pain, but some people have said that the sensation of the needle twisting into the bone can be uncomfortable. When the needle penetrates the marrow, it will be removed, leaving the tube to which a syringe will be attached and marrow drawn up. Patients have reported feeling an uncomfortable sucking sensation during this part. Once this is done, the tube will be removed and a biopsy needle (see the image below) will be inserted into the same incision to take a separate sample.

A twisting motion is also used here. The radiologist will then put a pressure dressing on the site. After the radiological equipment has been turned off and the patient disconnected from the monitoring equipment, the staff will move them back to the hospital bed and the nurse will wheel them back to their cubicle in the unit. They will be positioned so that their weight is on the incision to maintain pressure and control bleeding. The patient will stay at the hospital for a few hours while the meds wear off and the nurses monitor them for bleeding, after which they will be discharged with instructions to call the doctor if they experience any excessive bleeding. They should have someone else drive them home.
Bone marrow donation: To be a bone marrow donor, a person has to be between 18 and 35 years old; not have HIV/AIDs, rheumatoid arthritis, systemic autoimmune diseases, bleeding disorders, brain injury, cancer or prior cancer treatments within 5 years of the donation, chronic pain that is treated with medications, chronic Lyme disease, diabetes that requires insulin, heart disease, hepatitis B/C, or kidney disease; and be a match to the intended recipient's human leukocyte antigen (HLA) and blood type. (Note: people can donate to bone marrow banks and be matched anonymously to recipients with their same HLA type) HLA types are different from blood types and are most commonly matched between people of the same ethnic background and family members, especially siblings. The donor will have to undergo extensive tests to ensure that they are healthy enough to undergo the procedure and for their bone marrow to be used for transplant; these include blood tests, tests for all types of infections, an electrocardiogram, and a chest x-ray. Bone marrow stem cells may be harvested from a regular blood donation or from bone marrow aspiration. The procedure for donation is the same as for aspiration, only the patient may be put under general anesthesia and intubated and the doctor will pull off about 1-2 pints of bone marrow. The patient may have to stay in the hospital overnight.
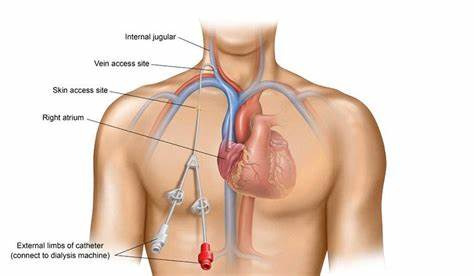
Bone marrow transplant: This is officially called a hematopoietic stem cell transplant (HSCT) and is usually done for leukemia, lymphoma, myeloma, polycythemia vera, aplastic anemia, severe immunodeficiency disorders, sickle cell anemia, beta thalassemia, and other disorders of the bone marrow or immunity. Stem cells can be taken from the recipient before their illness became serious, a related or unrelated donor, or umbilical cord blood. It is often a last resort treatment due to its high cost (up to $500,000) and potential for graft rejection. Before transplantation, the patient will receive high-dose radiation and chemotherapy (myeloablative therapy) to destroy their existing bone marrow. Once the myeloablative therapy has been completed, stem cells will be infused through a central venous catheter (see the image below), which the patient will certainly already have if they have cancer.
Ideally, the cells will seed in the bones and multiply to fill them (engraftment). This can take 2-4 weeks, or may never occur. The patient may not achieve full immunity for months or years. The patient may be in the hospital from the start of myeloablative therapy to 100 days after the transplant. Following the transplant, the patient will be on a regimen of medications to suppress their immune system to avoid graft-versus-host disease (GVHD; rejection of the donor stem cells resulting in a systemic inflammatory reaction). The patient may or may not be on this regimen for the rest of their life; if they never experience GVHD, they may not. They will have to be on the lookout for signs of graft rejection and secondary cancers (due to the myeloablative therapy) for the rest of their life.
Thanks for letting me nerd out and happy whumping!
#whump#hospital whump#anon ask#🦾#bone marrow aspiration and biopsy#bone marrow donation#bone marrow transplant
9 notes
·
View notes
Text
By Greg Hunter January 5, 2025
There is no wonder why everyone is in the dark about the deaths and disabilities caused by the CV19 bioweapon vax.
According to Dr. Michael Yeadon (who worked at Pfizer for 20 years bringing new drugs to market), more than five billion people around the world took the CV19 vax, at least 200 million were in the US alone. Try to do an internet search of negative effects from the CV19 vax, and one of the first things that pops up is from the CDC that says, “Most side effects are mild to moderate.”
According to Dr. Betsy Eads, that is a total lie, and what Dr. Eads sees in the hospitals everyday tells the real story that is being covered up by just about everybody involved. Dr. Eads says, “There is a boom on procedures in the hospitals. These doctors are making big bucks. . . . They are doing procedures for things like cardiac catheterizations, fishing out blood clots, interventional radiology . . . for blood clots that go to the brain and cause strokes. You are talking about big procedures, long hospital stays, and you are talking about a lot of money being made, not just for the doctors and the hospitals, but for the whole system. It’s broken, and it’s all about money. It’s not about health and healing.”
The numbers of adverse events from the CV19 injections are vastly underreported, according to multiple studies. One study says, “Fewer than 1% of vaccine adverse events are reported.” CV19 vax truth teller Steve Kirsch has just listed several of these studies on his Substack. Kirsch also listed a long list of facts that say “COVID vaccines are unsafe and that the medical community should not be trusted.”
11 notes
·
View notes
Text
I got a job.
Which is kind of nifty I guess. I feel like it removes some of my stress although I knew I wouldn't have an issue finding a job, its just that the unknown makes us feel like we are continuously poor and homeless when that isn't the case.
An old classmate of mine from nursing school had messaged me some odd days ago saying she was leaving her job because her commute was really long and she wanted to know if I wanted it. She said she loved her job otherwise. I was actually going to wait until we moved to start applying for jobs because a lot of places want you to start ASAP and I don't want to apply too early. But she had already recommended me to her manager and he contacted me with a referral link to fill out. Did a virtual interview and he told me he knew he was already going to offer me the job.
HR already sent me an acceptance package and stated they wanted to pay me a relocation fee. Just an FYI this is for an Interventional Radiology nurse position, which I suppose I do have a bit of experience in with my previous position. IR is considered a cush or "soft" nursing job, but this is with a lvl1 trauma center and I'm not that familiar with the type of high acuity cases that they do. The last time I worked in a lvl1 trauma center it was primarily preop/PhaseII and a smidgeon of pacu. I wasn't in the thick of super acute/sick patients. So I don't really know what to expect in IR. It SOUNDS like they just want somebody who is familiar with and knows how to push meds for conscious sedation. They have techs who scrub in with the doctor. That was primarily what I was nervous about was trying to learn how to scrub for so many different types of procedures (cause they said they do about 40 different types) and I was like "oh lord thats a lot to learn and prove myself on, in a short orientation". But they told me that I would just be doing the conscious sedation and thats it. Which takes a lot of stress off. I don't know how to scrub..so..
anyway, coincidentally at the same time I accepted the position, somebody posted on the nursing reddit saying something like "those of you who want to work in IR because its a soft nursing job, WE DONT WANT YOU" I mean, I work hard and I split myself into 1400 pieces to try and help everybody so I'm not coming in to just sit and play on my phone.
The downsides to this job is that there is on-call and then I'd be making less money than what I was getting paid 5 years ago and rent prices have skyrocketted. Which is really sad. It has pretty much doubled. So less pay and more expensive CoL. We are already expecting to have to pay around 2000-2200/mo on rent alone for nothing super special. Not including pet rent and then utilities.
Me and my spouse were jokingly talking about me joining the service for the benefits. While its been brought up to me before in the past, I didn't think I had it in me to join the military. Now I'm actually kind of taking it seriously. I already talked to a recruiter but they aren't making it easy to get in contact with them which makes me think they're going to tell me they werent interested. But hypothetically, if I joined the military nurse corps, I'd go in as an officer, get officer pay, get BAH, get a retirement, continue the lifestyle of which I've become accustomed and if they have my specialty available, I would just continue doing the job I've become accustomed to. It was actually kind of enlightening.
If I have to work my booty off being full time, on call, making less than my mom as a secretary and I have to continue being a nurse....I mean, I dunno..people say that the military can't compete with civilian hospitals, but I kind of beg to differ. To me, it seems like they're offering a lot more.
But if military says "no, we don't need your specialty", I do have a job waiting for me for when we move.

#illustration#sketchbook#watercolors#drawing#sketch#realmedia#traditionalart#artblog#mixedmedia#animalart#militaryspouse#milspouse#artistblog#lifeblog
3 notes
·
View notes
Text
Healthcare's AI revolution: Innovations and Prospects - Sachin Dev Duggal
Innovations in Healthcare Through AI
AI has already made significant advancements in various aspects of healthcare. One notable innovation is diagnostics. These data sets assist medical professionals in making better diagnoses using artificial intelligence algorithms that examine medical data like imaging studies, laboratory results, and electronic medical records. By doing this, AI tools have improved the accuracy of CT scans and simplified work procedures, thereby hastening outcomes and improving their dependability, which is greatly needed, especially in radiology, whose timely correct diagnosis significantly impacts patients’ lives.
The healthcare sector is undergoing a transformation through artificial intelligence (AI), which is enhancing diagnosis, improving patient care, and streamlining work. With the progress of technology, AI can change how healthcare is provided, making it more efficient, personalized, and accessible. Sachin Dev Duggal has been advocating for the impact of AI in healthcare and expressing how it could reshape medicine in the future.
Additionally, there are other instances where artificial intelligence plays an important role in enabling very early disease detection. Complex machine learning systems can identify data patterns that may signal the onset of cancerous diseases at stages when they are still curable. For instance, AI systems have demonstrated high accuracy rates when predicting the probability of developing lung cancer, thereby enabling earlier interventions with better survival rates than ever before. This new orientation towards preventive intervention rather than treatment represents a big shift from the traditional approach to health care.
AI is revolutionizing healthcare, which includes improvements to diagnosis, customization of treatments, and operational efficiency. Integrating AI into healthcare, as highlighted by Sachin Dev Duggal and other thought leaders, will improve patient outcomes and make healthcare more accessible and efficient. This means that to address the challenges facing the health industry and guarantee a healthier tomorrow, we must embrace these technological advancements.
#artificial intelligence#AI#technology#sachin dev duggal#sachin duggal#builder.ai#builder ai#sachin dev duggal news#sachin duggal news#builder.ai news#builder ai news#sachin dev duggal builder.ai#sachin duggal builder.ai#ai news#tech news#sachindevduggal#software development#innovation#sachinduggal#sachin dev duggal ey
2 notes
·
View notes
Text

Orthopedic veterinary surgeons in Singapore specializing in fracture repair, TPLO surgery, spinal surgery, hip replacement, and orthopedic procedures for dogs and cats.
Web Page: https://beecroft.com.sg/beecroftsg/project-two-3amwl
#cancer operations dogs and cats#interventional radiology subs and stenting#orthopedic surgical procedures for dogs and cats#fracture repair Alexandra#fracture repair vet Singapore#TPLO surgery vet Singapore#Surgery tumor removal#Surgery tumour removal#Ear surgery Singapore#Spinal surgery dog Singapore#Hip replacement surgery dog Singapore
1 note
·
View note
Text
FACT NUMBER ONE because I will be disowned from the profession unless I mention this
Radiographers =/= Radiologists!
Radiographer (UK) = person trained up to BSc degree level and often above, who can choose to specialise in a particular field. Radiographers can become involved in / perform basic or advanced procedures depending on skill level and training, or can train to interpret radiological images for diagnosis. Then there's a whole different branch of Radiography devoted to planning treatment & blasting cancers with radiation! I believe rads in the USA aren't trained to the same level and don't require so many qualifications/do as much, but correct me if I'm wrong!
Radiologist = qualified doctors who specialise in interpreting radiological images and performing procedures that require the use of radiography - e.g., inserting IVC filters, unfreezing shoulder joints with fluoro, CT biopsy, a million more...
So, if you have imaging done, you are more likely but not guaranteed to be in the room with a Radiographer, not a Radiologist! But if you have an interventional procedure using certain imaging modalities, the Radiologist is more likely to be leading the procedure with the Radiographer assisting! Buuuuuuut more and more Radiographers are becoming Advanced Practitioners in stuff like........ PPCIs for STEMI treatment, and doing the whole procedure themselves, so this isn't a guarantee!
10 notes
·
View notes
Video
youtube
What is IR pain management #intervention #chronicpain #pain #shorts #usa...
#youtube#radiologist interventionalradiology intervention usa procedures radiology injection interventionalradiologist painmanagement scienceonl
0 notes
Text
Sound Vascular & Vein

Sound Vascular & Vein is committed to providing the highest level of patient care in interventional oncology, radiology, and endovascular treatment. We offer personalized, outpatient treatments for arterial disease, arthritic pain, spinal compression fractures, men’s & women’s health, and vein & vascular care. Our experienced doctors, leading-edge technology, and safe, private OBL center can provide life-changing procedures. Some conditions and treatments include peripheral arterial disease (PAD), liver cancer, benign prostatic hyperplasia (BPH), uterine fibroids (UFE), venous issues, varicose veins, enlarged prostate, leg pain/cramps, prostatic artery embolization (PAE), genicular artery embolization (GAE). Schedule an appointment today!
2 notes
·
View notes
Text
Interventional Radiology Resources
Cases
DartRad | IR Cases
SVUH Interventional Radiology Cases
Learning
The Kinked Wire
Neuroangio.org
Backtable VI Podcasts
Dartmouth Interventional Radiology Papers
SIR Guidelines - Apps on Google Play
C.R.E.A.T.E IRAD
SVUH Interventional Radiology Cases
TeachingIR by Jeff Elbich
AUR Radiology Resident Core Curriculum Lecture Series | VIR Imaging
SIR RFS Clinical Companion
SIR RFS IR Procedure Guides
IR Clinical Companion
SIR RFS Webinars
Stepwards IR Primer
Calculators
SIR Guidelines - Apps on Google Play
3 notes
·
View notes
Text
Discover Why Supreme Hospital is the Best Hospital in Faridabad

Supreme Hospital, located in the heart of the city, is widely recognized as the Best Hospital in Faridabad, offering top-notch healthcare services across multiple specialties. With a commitment to clinical excellence, advanced technology, and compassionate care, Supreme Hospital has become the trusted choice for patients seeking comprehensive medical treatment in Faridabad and the surrounding regions.
Our Specialties
Supreme Hospital provides an extensive range of specialties to cater to diverse healthcare needs:
Neuro Sciences: Advanced treatment for neurological disorders.
Cardiac Sciences: Comprehensive cardiac care including diagnostics and interventions.
Gastro Sciences: Expert care for gastrointestinal conditions.
Renal Sciences: Specialized nephrology services.
Critical Care: 24/7 intensive care units for critical patients.
Orthopaedics & Joint Replacement: Advanced orthopedic treatments and surgeries.
Mother and Child Care: Comprehensive obstetrics and pediatrics services.
Ophthalmology: Eye care services including surgeries.
ENT & Head and Neck Surgery: Treatment for ear, nose, throat, and related conditions.
Dermatology & Cosmetology: Skin care and cosmetic treatments.
Urology & Andrology: Treatment for urinary and male reproductive systems.
General & Laparoscopic Surgery: Minimally invasive surgical procedures.
Internal Medicine: Comprehensive adult medical care.
Respiratory Medicine: Treatment for respiratory disorders.
Paediatrics & Neonatology: Child and newborn care.
Physiotherapy and Rehabilitation: Post-treatment recovery services.
Anesthesiology: Pain management and anesthesia services.
Dentistry: Comprehensive dental care.
Endocrinology: Treatment for hormonal disorders.
Bariatric Surgery: Weight loss surgical procedures.
Interventional Radiology and Imaging: Advanced diagnostic imaging services.
24/7 Emergency and Support Services
Understanding the critical nature of emergencies, Supreme Hospital offers round-the-clock services:
Emergency Services: Immediate medical attention for urgent cases.
Blood Bank: Available 24/7 to meet transfusion needs.
Pharmacy: In-house pharmacy operating round the clock.
Dialysis: Continuous dialysis services for renal patients.
Laboratory Services: Comprehensive diagnostic tests available anytime.
Commitment to Quality and Compassion
At Supreme Hospital, patient well-being is paramount. The hospital adheres to international quality standards, ensuring that every patient receives compassionate and personalized care. The dedicated medical professionals work tirelessly to provide treatments that are both effective and empathetic.
Community Outreach and CSR Initiatives
Beyond clinical services, Supreme Hospital is deeply involved in community welfare:
Weekly OPDs for BPL Patients: Providing medical consultations to the underprivileged.
Monthly Medical Camps: Extending healthcare services to remote areas.
Patient Education Programs: Informative sessions to promote health awareness.
Subsidized Pharmacy Services: Affordable medicines for BPL patients.
School Health Programs: Health check-ups and awareness in schools.
Disaster Relief Contributions: Active participation in relief efforts during natural calamities.
First-Aid and BLS Workshops: Training sessions for emergency response.
Loan Facilities for Medical Devices: Financial assistance for stents and pacemakers.
Subsidized Treatment for the Needy: Affordable healthcare services for the underprivileged.
Why Choose Supreme Hospital?
NABH Accredited: Ensuring adherence to high-quality healthcare standards.
Experienced Medical Team: Skilled professionals across various specialties.
State-of-the-Art Infrastructure: Modern facilities and equipment.
Patient-Centric Approach: Personalized care tailored to individual needs.
Affordable Healthcare: Quality services at reasonable costs.
Supreme Hospital's unwavering commitment to excellence, compassion, and community service solidifies its position as the Best Hospital in Faridabad. Whether it's routine check-ups or complex surgeries, patients can trust Supreme Hospital for comprehensive and compassionate care.
0 notes
Text
Cone Beam Computed Tomography Market Key Players Growth Strategies and Business Models to 2033
Introduction
Cone Beam Computed Tomography (CBCT) has revolutionized diagnostic imaging across various medical fields, including dentistry, orthopedics, otolaryngology, and interventional radiology. The technology offers high-resolution 3D imaging with lower radiation exposure compared to conventional CT scans, making it a preferred choice for precision diagnosis and treatment planning. This article explores the CBCT market, highlighting key drivers, challenges, trends, and future growth prospects.
Market Overview
The CBCT market has witnessed substantial growth due to the increasing demand for advanced imaging solutions in healthcare. The global CBCT market size is expected to expand significantly, driven by technological advancements, rising prevalence of dental disorders, and increased adoption of minimally invasive diagnostic procedures.
Download a Free Sample Report:-https://tinyurl.com/2k2pr6at
Key Market Segments
The CBCT market can be segmented based on:
Application
Dental imaging
Orthopedic imaging
ENT imaging
Others (vascular, respiratory, etc.)
End-User
Hospitals
Dental clinics
Specialty clinics
Research institutions
Geography
North America
Europe
Asia-Pacific
Latin America
Middle East & Africa
Market Drivers
Several factors contribute to the growth of the CBCT market:
Growing Prevalence of Dental Disorders
The increasing incidence of dental conditions such as cavities, periodontitis, and orthodontic disorders has fueled the demand for CBCT in dental clinics and hospitals. CBCT provides detailed 3D imaging, allowing precise diagnosis and treatment planning, particularly in implantology and endodontics.
Technological Advancements
Ongoing innovations in CBCT technology, including higher image resolution, reduced radiation exposure, and software enhancements with AI integration, have expanded its application scope. Improved imaging quality allows better diagnosis and treatment planning, enhancing patient outcomes.
Rising Adoption of Minimally Invasive Procedures
CBCT is widely used in minimally invasive procedures due to its ability to provide high-resolution imaging while minimizing radiation exposure. It plays a crucial role in guided surgeries and complex dental and orthopedic procedures.
Increasing Investments in Healthcare Infrastructure
Governments and private organizations are investing heavily in healthcare infrastructure, particularly in emerging economies. The expansion of dental and medical imaging facilities is propelling CBCT adoption.
Market Challenges
Despite its advantages, the CBCT market faces several challenges:
High Cost of Equipment
CBCT machines are expensive, making them less accessible for small clinics and developing regions. The high initial investment and maintenance costs can be a barrier to market expansion.
Radiation Concerns
Although CBCT uses lower radiation compared to traditional CT, concerns about radiation exposure persist. Regulatory agencies impose stringent guidelines, which can impact the widespread adoption of CBCT technology.
Limited Reimbursement Policies
In many countries, insurance and reimbursement policies for CBCT scans are not well-established. This can discourage healthcare providers from investing in the technology, affecting market growth.
Key Market Trends
Integration of AI and Machine Learning
Artificial Intelligence (AI) is transforming CBCT imaging by enhancing image reconstruction, automating diagnosis, and reducing processing times. AI-powered CBCT solutions can provide precise analysis and assist healthcare professionals in making informed decisions.
Portable and Compact CBCT Devices
The demand for portable and compact CBCT devices is rising, particularly in dental practices and small clinics. These devices offer flexibility, ease of use, and affordability, making CBCT technology more accessible.
Increasing Adoption in Orthopedics and ENT
While CBCT has been widely used in dentistry, its adoption in orthopedics and ENT applications is growing. The ability to capture high-resolution images of bone structures and soft tissues is driving demand in these specialties.
Expansion in Emerging Markets
Developing regions, particularly in Asia-Pacific and Latin America, are witnessing rapid growth in healthcare infrastructure. The increasing number of dental clinics and hospitals, along with a rising middle-class population, is creating new opportunities for CBCT manufacturers.
Competitive Landscape
The CBCT market is highly competitive, with key players focusing on product innovation, partnerships, and strategic acquisitions. Major companies operating in the market include:
Planmeca Oy
Carestream Health
Dentsply Sirona
Vatech Co. Ltd.
J. Morita MFG. Corp.
NewTom (Cefla Group)
CurveBeam
PreXion Corporation
Strategies Adopted by Market Players
Product Innovations: Companies are developing CBCT systems with enhanced image quality, faster processing, and lower radiation exposure.
Mergers & Acquisitions: Leading companies are acquiring smaller firms to expand their market presence and technological capabilities.
Geographic Expansion: Players are expanding their operations in emerging markets by establishing new distribution networks and partnerships.
Future Outlook
The CBCT market is expected to witness continued growth due to:
Advancements in imaging technology, including AI integration and real-time 3D visualization.
Rising healthcare awareness, particularly in emerging economies.
Expansion in application areas, including pain management, oncology, and cardiovascular imaging.
Despite challenges such as cost barriers and regulatory constraints, the CBCT market holds promising potential for the future. Innovations in affordability and accessibility will further drive adoption across different medical disciplines.
Conclusion
Cone Beam Computed Tomography (CBCT) is a game-changing imaging technology that has significantly enhanced diagnostic precision in various medical fields. With technological advancements, increasing healthcare investments, and growing demand for high-quality imaging, the CBCT market is poised for robust growth in the coming years. However, addressing cost concerns and regulatory challenges will be crucial for maximizing its global adoption.Read Full Report:-https://www.uniprismmarketresearch.com/verticals/healthcare/cone-beam-computed-tomography
0 notes