#healthcare-acquired infection
Explore tagged Tumblr posts
Text
The Weather
As of September 13, 2024, national wastewater levels remain high. The CDC’s national wastewater map has contracted viral activity levels from ten grades of color to five grades of color while our map below maintains the original ten grades of color based on CDC data. We will adjust to the five grades in future reports. With schools in full session and the weather transitioning in northern regions to cooler temperatures, transmission continues to occur. Wastewater activity is either “High” or “Very High” in 37 states according to the Wastewater Surveillance System (NWSS) dashboard. Activity is “Moderate” in 8 states and the District of Columbia, and there is no data available for New Hampshire, North Dakota, Oregon, the U.S. Virgin Islands, and Guam.

According to the Wastewater COVID-19 National and Regional Trends dashboard, COVID wastewater levels have plateaued, remaining between high and very high in all regions except for the West, which is having a slight increase. The highest levels remain in the West as of 9/7/2024 (data captured on 9/13/2024).
In order to access local COVID wastewater levels, you can refer to the CDC’s state/territory trends page as well as the WastewaterSCAN dashboard. State and local public health wastewater trackers may also be available for example in Illinois, they are reporting over 80 locations. Also, the National Academies of Medicine recently published a second report stressing the importance of a robust wastewater surveillance system and its invaluable role in infectious disease surveillance. They recommend improving the consistency and quality of wastewater surveillance for COVID and other infectious diseases.

As of September 10, 2024, COVID levels are “likely growing” in 3 states and territories according to the CDC Center for Forecasting and Outbreak Analytics dashboard. Thirteen states have reached “stable or uncertain” levels, and 31 states are seeing “declining” or “likely declining”, while levels are “not estimated” in 4 states.
Note, this model utilizes emergency department visit data to estimate COVID transmission’s Rt, which is an estimate of the average number of new infections caused by each infectious person. An Rt greater than 1.0 indicates that infections are growing, while an Rt less than 1.0 indicates that they’re declining.

According to the CDC's COVID Data Tracker, there has been an increase to nearly 1,000 deaths and slightly more than 1,000 deaths per week from COVID during the entire month of August 2024. The last time this occurred was during the winter months of 2024. This total count of weekly COVID deaths is likely to be an underestimate due to limited COVID testing and reporting. The loss of these lives could have been prevented if layers of protections were consistently implemented in preventing infections.
A recent study published in the Annals of Internal Medicine highlights the importance of preventing infections especially during periods of high rates of transmission. It notes that COVID death rates were higher when healthcare systems faced a larger strain as a result of increased levels of transmission. Comprehensive policies that protect people and prevent healthcare-acquired COVID infections are needed to prevent healthcare system overload.
Variants
According to the CDC’s variant tracking dashboard, KP.3.1.1 remains the dominant variant of all currently circulating strains. Nowcast modeling projects that KP.3.1.1 will increase to 52.7% by 9/14/2024, followed by KP.2.3 at 12.2%, followed by LB.1 at 10.9%, and KP.3 at 10.6%, respectively. The most prevalent circulating variants are JN.1-derived, and closely related to both JN.1 and KP.2. Updated vaccination with any of the available options (Pfizer, Moderna, or Novavax) is recommended to better match current variants.

Vaccines and Treatment
Although the Bridge Access Program, covering the updated vaccines for uninsured and underinsured adults, has ended, several states including California’s Bridge Access Program and other departments of health have taken steps to partially address this major gap by either providing funding for no-cost access to COVID vaccines or using budgets to acquire a limited supply for their residents. Ultimately, the federal government must contribute resources to ensure no-cost access for all who are uninsured or underinsured. We continue to demand from the federal government to provide continued funding for the Bridge Access Program as well as the Vaccines for Adults Program. As people access the updated COVID vaccines, it is notable that a longer 1.5 inch needle may be needed for adults with higher body weights, in order to pass through subcutaneous tissue into muscle. Complete guidelines for vaccine administration in consideration of age, weight, and injection site can be found on the CDC's website.
It is important to seek treatment when facing a COVID infection. A recent study, reviewing population data of nonhospitalized individuals ages 18 and older during the period of January 2022 and December 2023, showed that nirmatrelvir/ritonavir (Paxlovid)—treatment for COVID—was less commonly used among those who identified as non-Hispanic Black and Latinx/e patients. Although the Test-to-Treat program prematurely ended, there continue to be programs available to ensure financial access to Paxlovid.
Wins
This is a reminder that another batch of no-cost COVID rapid antigen tests can be ordered and sent to your home address at the end of September 2024. Through the CDC’s Increasing Community Access to Testing (ICATT) program, no-cost access to COVID testing access is limited to those who are uninsured or underinsured at places including CVS, Walgreens, eTrueNorth, and other local sites as well as in New York City, which is supported by the NY Department of Public Health.
We are eagerly awaiting news on updates from the Centers for Medicare and Medicaid on mandatory reporting of COVID infections in healthcare systems, which begins November 1 thanks to our community’s advocacy. It is invaluable that all healthcare systems participate as case data is paramount for keeping track with current COVID trends and understanding the volume of healthcare acquired COVID infections.
Take Action
The National Institute of Health (NIH) is seeking public comment and feedback on the next phase of RECOVER clinical trials, which focus on Long COVID. Meetings will be held virtually and on-site between September 23 and 25 to solicit feedback and comments. Register to attend these virtual or on-site sessions by September 25, 2024. It is very important to participate and ask NIH to commit to studies that will result in developing a better understanding of Long COVID, effective treatments for Long COVID, and key approaches to preventing Long COVID.
Amid ongoing COVID spread, masking in healthcare remains central to safe access to healthcare. As we await implementation of COVID hospitalization reporting and prepare for CDC’s next Healthcare Infection Control Practices Advisory Committee meeting in November, you can use this letter campaign to ask your elected officials to take action for healthcare masking.
And finally, because all of us need access to the updated COVID vaccines regardless of our insurance status or ability to pay, use our letter template to demand free COVID vaccines for uninsured and underinsured adults nationally.
#op#links#img#covid#covid-19#covid19#covid 19#medical#pcdc#people's cdc#sars cov 2#sars-cov-2#cdc#disability#long covid#nih#mask up#covid isn't over#covid conscious#covid cautious#covid vaccines#vaccines#get vaccinated#covid testing#icatt#recover clinical trials#hicpac#bridge access program#healthcare-acquired infection#described in alt text
6 notes
·
View notes
Text
Okay so… my employer, a healthcare organization with many hospitals and clinics:
Does not regularly test its employees for covid, including the unvaccinated ones
Allows staff to have assignments with a mix of both covid positive and negative patients, requiring full PPE only when caring for the covid patient(s)
Limited the hours/days for testing and vaccination sites
No longer tests or screens hospital visitors
Generally no longer limits the number of visitors a patient can have (some exceptions obviously)
No longer requires employees, patients or visitors to mask unless they are COVID+ or have cold/flu symptoms (but who’s checking if visitor
And now has decided to no longer test asymptomatic hospital patients
And it had to be now? When cases are spiking and everyone’s got a “summer flu” or “just allergies”?
It’s like the higher-ups are sitting around their conference table brainstorming ways to make their facilities even more unsafe than they already are

#and I’m sure other hospitals around the US are exactly the same#we have learned nothing#very much not looking forward to the coming weeks and colder seasons now#it’s like they want us to all get sick???#healthcare#covid#Covid isn’t over#hospital acquired infections#wtf#wear a mask#you’re on your own kid#you always have been
0 notes
Text
"Seminario cited the recent report, “Employer-Reported Workplace Injuries and Illnesses,” that shows that the number of respiratory illnesses in the private health care and social assistance sector increased from 145,300 in 2021 to 199,700 cases in 2022, an increase of 37.5 percent.
...
As an industrial hygienist, Seminario was extremely critical that there were no experts in respiratory protection on the committee nor did it include engineers who developed ventilation guidelines. She believes that the HICPAC committee members are likely so opposed to respirators “because once you are into recommending respiratory protection, with that comes a full respiratory protection program from OSHA,” with penalties for violations.
An epidemiologist and consultant, Michael Olesen, echoed this, believing the changes reflect “pressure to remove liability from hospitals.” He added, “I take a very clear position that we should be having respiratory protection mandates in all healthcare settings right now.”
...
Many patients who spoke at the HICPAC meetings said they had gotten Covid-19 when they went to the hospital and that the new policies were keeping them from getting care.
Given that, Dr. Art Caplan, professor of medical ethics at New York University’s Grossman School of Medicine, previously told me that dropping masking requirements in hospitals is “utterly, completely, irresponsible.” Similarly, staff refusing to mask, even when a patient requests it, is a moral failure. “The first principle is, you must do what is in the best interest of your patient,” he said.
...
Several people were asked why they believe HICPAC is determined to water down protections. Consistently, respondents say, “to reduce liability.” Earlier in the pandemic, hospitals regularly tested patients and staff for Covid-19, and you could often tell where and how you became infected. Since staff are no longer masking and continue working when ill, and patients are not being tested on admission, you can no longer prove who infected you. Hospitals are the only ones who win in this scenario, absolving themselves of responsibility and liability."
#healthcare system complicity#this is immoral and unethical#cdc#hicpac#wear a mask#keep masks in healthcare#covid#rsv#flu#masks#respirators#n95 masks
767 notes
·
View notes
Text
Love in the big city and HIV
So, I have recently watched one of the best dramas of the year, “Love in the big city”, in which HIV is a major theme.
The show portrays really well the stigmatized scenario around HIV: as a person living with the virus, Go Young feels exactly as if he's carrying some kind of curse. He can't accept it, but who can blame him for that, if "Kylie", as he calls the virus, is always around like an inconvenient person? In his sex life, while applying to a job, and even while hanging out with friends.
Society doesn't make it easy for a person living with HIV to accept the condition and that's essential when it comes to healthcare, which is what I want to address today.
First, let me introduce myself: my name is Nico and I'm a Medicine student in Brazil. Here, we have probably one of the biggest public health system in the world, the Unified Health System (a.k.a. SUS). In this essay, I intend to share some general information about HIV, its treatment and prevention, by using some parts of “Love in the big city” to discuss this theme, because although the show did an amazing job when it comes to talking about it, there are some points I found needed some better explanation.
HIV is a sexually transmitted infection (STI) that can also be transmitted by the contact with infected blood (e.g: incompatible blood transfusion; use of shared needles) or from the mother to a child inside the womb or during labor. The virus uses a specific type of immune cell to multiply. Explaining it in a very simple way, he gets inside the cell, uses its components to produce new viral copies and then ruptures the cell membrane to release these new copies in the blood, killing the cell by doing so. For this reason, untreated HIV is very dangerous, since it can cause immunodeficiency (failure of the immune system), making the person susceptible to acquire opportunistic infections, which are diseases that usually don’t occur in people with regular immune systems. When someone has immunodeficiency caused by HIV, this person is diagnosed with Acquired ImmunoDeficiency Syndrome (AIDS). That being said, AIDS and HIV are not the same. There are many people living with HIV that don’t have AIDS, thanks to appropriate treatment.
There are multiple ways a person can discover about having HIV: you can be notified because the person you have had relations with discovered the infection, or by taking blood tests for blood donation, or in the worst case scenario, when you are already suffering from an opportunistic infection. Go Young, for example, discovered it because of the blood tests results while he was in the army. One thing I found very outrageous was that the physician instantly inferred that Go Young was gay because of that, but this is impossible, since anyone can get the virus, regardless of their sexual orientation. This appointment was like a death sentence: the unempathetic doctor as a ruthless judge, blaming the patient and not offering a single word of comfort. (Quite the opposite: he even asked that very intimate question about sex positions. Seriously, I wanted to punch this doctor so hard.)


Nonetheless, even if it was made in a very inappropriate way, diagnosis is still very important, because that is the only way one can have access to treatment. Each patient must be evaluated separately, since treatment may vary due to the different genetic subtypes of the virus and the person’s own body response. Medication can also be adjusted until satisfactory results are accomplished. Overall, all patients are submitted to a lifetime antiretroviral therapy in order to stop the virus from multiplying and to keep immune cells at a higher level. In the series, we can see Go Young asking for any antiretroviral in a pharmacy, but in real life, he would be very specific about the drugs.

If done properly, treatment can provide quality of life and long life expectancy (very similar to people who don’t have HIV), prevent opportunistic infections and, most importantly, transmission! Yes, that is exactly what you read: treatment can result in really low levels of HIV in the blood, which is called “undetectable viral load” if it happens for at least six months. There is even a saying which goes “Undetectable = untransmittable”. In this scenario the patient can even have sex without a condom with their partner, which is what happened with Go Young and Gyu Ho in the series. However, it is important to mention that this only applies to HIV: one can still get other STIs while having unprotected sex.


In addition to condoms and proper treatment, there are other ways of preventing HIV infection. Susceptible people can use the pre-exposure prophylaxis (PREp) medication, which highly reduces the risk of getting HIV from intercourse (and also from blood contact in a less effective way). There is also the post-exposure prophylaxis (PEP), which can prevent infection if taken within 72 hours after possible exposure. Treating other STIs, not sharing needles, using lubricant (less chance of injury during intercourse) and avoiding sex while in use of alcohol or drugs are some other habits we can do ourselves to minimize the risk of acquiring HIV.
Nevertheless, individual actions can help only until a certain point, given that the best prevention is the “combination prevention”, which includes not only behavioral and biomedical approaches, but also structural interventions. Every country should have their own public policies to assist people living with HIV and to prevent transmission. I’m proud to say that, in Brazil, thanks to our public health system, everyone has access to condoms, lubricants, tests, treatment, PREp and PEP - all free of charge. The system also has policies of damage control, providing all of these strategies to the population of risk, such as sex workers and people with a substance use disorder, including kits with individual needles to prevent sharing and, consequently, blood transmission. No wonder we are an international reference for HIV/AIDS treatment and prevention.
To conclude, I also need to remind you that you can actively help in this cause by simply showing support. As we all watched in “Love in the big city”, a person living with HIV faces all kinds of prejudice in society. Go Young carried a heavy burden for years, not being able to share it with anyone until Gyu Ho embraced him. Sometimes, patients have these prejudices themselves and it can deeply hinder treatment. I have seen this myself: a patient that denied the diagnosis and returned to the hospital sometime later with a severe health condition.
You can be the person that will accept and embrace this other person, who is only living with a chronic condition, such as many people who live with hypertension or diabetes, for example. You can be the person that will call out on others for their preconceived opinions. You can be the person who will share high-quality information to your friends, family, fellow workers or students (There are links in the last paragraph with reliable information for those who want to do some further research).
Finally, I can’t stress enough how much I loved “Love in the big city” for addressing so many types of love and so many sensitive topics, including this one, in such a beautiful way. It has been a long time since I had felt so connected to a story, to a character so human like Go Young.
I hope this essay provided a little bit of information to you. I mostly used the knowledge I have learned in college and sites of well-recognized organizations, such as the UNAIDS, the World Health Organization (WHO) and, for the Portuguese speakers, the Brazilian Ministry of Health (Ministério da Saúde). Thank you for reading, and please, feel free to send me any questions you might have, I’ll do my best to answer them. Also, if you notice any English mistakes, please let me know so I can correct them.
#love in the big city#HIV#aids#health and wellness#healthcare#medicine#SUS#Unified health system#Sistema único de saúde#Viva o SUS#Proteja o SUS#go young#gyu ho
55 notes
·
View notes
Text
Canterlot Medical Center Records:

∙Patient name: Dragon Fruit Punch ∙Species: Unicorn ∙Sex: Female ∙Age: 25 ∙Reason for Admission: ███████ █████
-Patient didn't feel many symptoms during the first days of infection. Noted feeling mildly feverish, achy, and painful knots in the back. -Patient was transferred from Ponyville Healthcare when she sprouted a form of psuedo wings only days after admission. Notably, she cannot fly with them, and they were gained with an explosion of magical energy similar to alicorn ascension. -Mane is sparkling and flowing with excess magic, and patient has gained unfounded magical prowess. She is overwhelmed with euphoria with her newly acquired power, as any pony in their position would be. -Despite this, patient noted that they're in a lot more pain and have seemingly had more trouble breathing. Princess Twilight Sparkle has taken a particular interest in this case and is closely working with us as we examine what is happening.




Just wanted to put the Flat/Original images here :)
20 notes
·
View notes
Text
Also preserved on our archive (Thousands of Covid-related news stories! Daily updates!)
By Hayley Gleeson
Thousands of patients caught COVID in NSW public hospitals last year and hundreds died, fuelling concerns among infection control experts and healthcare workers that hospitals are not taking strong enough precautions against airborne viruses.
NSW Ministry of Health data released under freedom of information laws shows at least 6,007 patients caught COVID in hospital in 2023 and 297 died — about 115 laboratory confirmed infections and six deaths per week, on average.
Similar figures were recorded in the first few months of 2024, with 1,729 patients catching COVID and 86 dying between January and April this year. For context, about 2,100 people died from or with COVID in NSW in 2023, suggesting about 14 per cent of those were patients who contracted the virus in hospital.
The data was released following an application by lawyer Peter Vogel who, for 18 months, was pointed between the Ministry of Health — which initially denied holding "complete and accurate records" of hospital acquired COVID infections — and the Clinical Excellence Commission, which directed Mr Vogel back to the Ministry of Health, which eventually released the data he had sought.
The figures are only a snapshot of the pandemic's ongoing impact on hospitals, and NSW Health would not clarify how it is collecting data on hospital acquired COVID infections or provide more detail on deceased patients' ages and genders, or data for previous years.
Still, experts say infection control protocols in hospitals are not good enough, with some doctors warning widespread indifference to COVID is costing too many lives and adding unnecessary pressure to a health system already under strain.
Hospitals know how to stop COVID spreading Stéphane Bouchoucha, president of the Australasian College for Infection Prevention and Control, said the new figures were "concerning and tragic" especially for the families of people who had died.
"We know how COVID is transmitted and we know how to prevent healthcare associated infections," Dr Bouchouca said — by ensuring good ventilation and air filtration, testing and contact tracing, isolating infected patients and requiring healthcare workers to wear masks.
If hospitals were recording similar numbers of deaths from golden staph infections, Dr Bouchoucha said, swift action would be taken. "But I think people react differently because it's COVID — 'It's alright, it's a respiratory disease, it's not so bad' — trying to minimise the fact it is still a healthcare associated infection," he said.
"This is the core business of infection prevention and control … The premise that we can allow some deaths, to me, is wrong."
For months experts and healthcare workers in several states have been warning that too many patients are catching COVID in health facilities, with Victorian data showing about 9 per cent of those who caught the virus in hospital last year died.
In NSW, hospitals have shifted from an "emergency" pandemic response to managing COVID in line with other transmissible infections. Local health districts now must conduct their own risk assessments and adjust infection control protocols accordingly. Staff are no longer required to wear masks unless they're caring for COVID patients, when they must use N95 respirators, which are significantly more effective at preventing transmission of respiratory viruses than surgical masks.
But some doctors say that guidance is not always enforced, with healthcare workers in some hospitals choosing to wear surgical masks around COVID patients. Others are concerned that COVID testing is not conducted frequently enough and that staff are discouraged from ordering PCR tests to save money.
'The government has some really serious questions to answer' Amanda Cohn, NSW Greens spokesperson for health and a former GP, said she was "surprised" to learn that data on hospital acquired COVID infections and deaths had been released because she had repeatedly asked Health Minister Ryan Park and Chief Health Officer Kerry Chant about it. Dr Chant told a Budget Estimates hearing last October that the Clinical Excellence Commission — the lead agency for infection prevention and hospital acquired infections — did not "collect and aggregate" it in a "systematic way".
"I have been reassured by the chief health officer that NSW Health is 'conscious of taking every step we can to minimise the risk of [COVID] transmission' in hospitals," Dr Cohn told ABC News. "But these figures make me very concerned that that's not the case."
Dr Cohn pointed to a recent study by the Burnet Institute and the Victorian Department of Health which found testing hospital patients for COVID on admission and staff wearing N95 respirators could prevent hundreds of deaths statewide and save the health system tens of millions of dollars each year.
"To know that those things aren't happening in New South Wales, meanwhile thousands of people are catching COVID in hospitals that should be safe — I think the government has some really serious questions to answer," she said.
Of particular concern, Dr Cohn said, is NSW Health's policy on taking transmission-based precautions — requiring healthcare workers to wear N95 respirators only when dealing with patients who are confirmed or suspected to have COVID.
"Only taking precautions after you know somebody is confirmed to be infectious is not good enough," she said, adding: "We need to see leadership from the health minister."
Dr Cohn said she had also spoken to many medically vulnerable patients who reported having to ask hospital staff to wear masks. "We would never expect people to have to individually ask their surgeon to wash their hands, we just expect that high standards are followed when we go into a health facility, that you will be safe."
Are hospitals prepared for future pandemics? Marilyn Cruickshank, professor of nursing at the University of Technology Sydney and a board member of the International Federation of Infection Control, said there were several factors likely influencing the drop-off in infection prevention and control efforts in NSW hospitals. These include high levels of exhaustion among healthcare workers since the onset of the pandemic, sector workforce challenges and budget restrictions — all of which are causing "strain and tension" in hospitals.
From a policy perspective, she added, high rates of vaccination against COVID and fewer deaths in recent years mean the "perceived risk" of the virus is much lower now than it was in, say, 2020. "It's not just that people don't want to do the right thing," Professor Cruickshank said. "There's a story behind it."
Still, she said, the new data suggests current infection prevention measures are "not good enough". "From a personal point of view, I would like to see staff continuing to mask in hospitals" using N95 respirators, Professor Cruickshank said — particularly those in emergency departments and wards that care for immunocompromised patients or other vulnerable groups like newborns.
"As healthcare workers, we should ensure that our hospitals are as safe as we can make them," she said. "So to me, it's a patient safety issue to try to keep the levels of hospital acquired COVID as low as possible."
However the "biggest change" she'd like to see is more support for hospital infection control teams, which need "good epidemiological skills and the resources to be able to quickly respond to outbreaks".
"Unfortunately, I don't think COVID will be the last pandemic that we see — there will be others in future," Professor Cruickshank said. "So we need people who are trained up to be able to deal with whatever comes next."
'It's too late for my mum' but we can still protect other patients For Ravi Fernando, whose 79-year-old mother Thelge died in hospital in August 2022, it's frustrating and upsetting to know patients are still dying after catching COVID in a place they should be safe.
Mr Fernando's mother was admitted to St George Hospital in Sydney's south after suffering a subarachnoid haemorrhage due to a ruptured brain aneurysm in late June 2022. She had successful emergency surgery and, for a few days, seemed to be recovering well in the ICU. But soon she began deteriorating and the hospital informed Mr Fernando that Thelge had caught COVID, most likely from one of her nurses.
A quality management consultant who has worked with aged care facilities, Mr Fernando was shocked but not surprised: most of the staff in ICU were wearing surgical masks, not N95 respirators, he said — some wore them down around their chin. "Maybe I should have raised concerns, but I wasn't in that frame of mind at the time," he said. "But I remember noticing that because back then, COVID was still a big deal."
Thelge was intubated and given antivirals only after Mr Fernando requested them, which still bothers him, but she died a couple of weeks later. An investigation by the Healthcare Complaints Commission (HCCC) found there was no evidence that her death was caused by COVID: St George Hospital's assessment concluded her COVID infection "did complicate the management" of her presenting condition but did not contribute to her death.
But Mr Fernando strongly disagrees. "She was clearly recovering before she got COVID … there was no question about that. Of course, aneurysms are complicated, so you never know, but there was a clear trigger for her deteriorating," he said. "The death of a loved one is distressing regardless. But when you know that it was preventable, it's very distressing."
Had St George Hospital "genuinely listened" to his family's feedback and improved its infection control protocols, he added, more deaths could have been prevented (the HCCC said it was "satisfied" with the hospital's COVID safe protocols). "It still would have been too late for my mum, but at least others are not going to be hurt in a similar way," Mr Fernando said.
ABC News requested interviews with the Health Minister Ryan Park and Kathy Dempsey, NSW Chief Infection Prevention and Control Practitioner and Healthcare Associated Infection Advisor at the Clinical Excellence Commission — NSW Health declined on their behalf.
NSW Health also did not respond to specific questions including about whether it was comfortable with current levels of illness and death in hospitals, if it would be reviewing infection control policies and whether it had conducted audits and upgrades to ventilation and filtration systems.
"NSW Health continues to closely monitor and assess the way we respond to acute respiratory infections, including COVID-19, to keep patients, staff and visitors to our health facilities safe," a spokesperson said.
"We remind the community if they are experiencing cold or flu symptoms, they should stay at home, where possible, to protect others. If someone has cold or flu symptoms and they need to go out, they should wear a mask to protect others. Symptomatic people should also avoid visiting high risk settings like hospitals, aged and disability care facilities or people who are at higher risk of severe illness."
#mask up#covid#pandemic#wear a mask#public health#covid 19#wear a respirator#still coviding#coronavirus#sars cov 2#Australia
12 notes
·
View notes
Text
Sociopaths, a term often used to describe those living with antisocial personality disorder, who operate within their daily lives without a “conscience,” can be characterized as acting without feelings of guilt, remorse, or shame coupled with a tendency to reject the concept of responsibility.
Antisocial people will intentionally make others angry or upset and use harsh and cruel indifference as they manipulate or attack others.
Clinically speaking, there is no defined difference between a sociopath and a psychopath although some have drawn this line at acting with low moral conscience (sociopath) and no moral conscience (psychopath) or having no regard for someone else’s rights or feelings (sociopath) and taking pleasure in robbing another of their rights, freedom, or well-being (psychopath).
My colleagues and I have discussed psychopathy in the previous president elsewhere as an example. Recognizing these nuanced differences exist, I will use the term sociopath and sociopathy here for brevity’s sake.
There appear to be at least three forms of this public political/governmental sociopathy present today. The first are those individuals for whom sociopathic tendencies are deep-seated and a core feature of who they are – the former president being a prime example. A second form includes the scores of Republicans and right-wingers who have decided to play the role or act sociopathic for their own personal gain. This includes hard-line MAGA members such as Marjorie Taylor Greene, Lauren Boebert, Kari Lake and Matt Gaetz, who decided to infect themselves with contagious sociopathy.
Look at the case of Florida Gov. Ron DeSantis whose impressive on-paper resume includes graduation from Yale University (where he served as captain of the baseball team) and Harvard law school (with honors), distinguished service in the United States Navy including a legal role with Seal Team One and a deployment to Iraq. On paper, he is highly accomplished and embodied what we as Americans tend to hold in high regard … until he acquired contagious sociopathy.
Coincident with his departure from active military service and rise to Congress and the Florida governorship, he apparently chose to include antisocial tendencies in his political and public persona. He believes in unregulated gun ownership (despite brutal killings in his state’s own schools), he attacks the rights of women with his restrictive abortion laws, he suppresses legislation that would support the LBGTQ+ community, and he seeks to diminish the plight of historically maltreated groups (such as African Americans) with his attempts to bury the past.
In another high-profile example, the U.S. Supreme Court was constitutionally designed as a third arm of our democratic republic that was supposed to serve independently from the other Branches in an apolitical manner … now its majority is infested with contagious sociopathy. In just the last year (and weeks), they sociopathically overturned Roe v. Wade and severely undercut women’s healthcare rights, ruled in favor of discrimination, and ruled against students struggling under the mountain of student debt…all while facing accusations of improper gifts, hypocrisy, and politicization … in other words, with contagious sociopathy.
The third group with contagious sociopathy are the passive enablers of widespread acts of manipulation and cruelty ranging from long-serving, establishment leaders like Sen. Mitch McConnell (R-KY) all the way to the throngs of people clad in Confederate flags and MAGA idolatry whose inaction and permissiveness serves as a large-scale petri dish by which contagious sociopathy can flourish. It cannot go without mentioning that the processes of cultism are at play here as well.
It should be noted that the term I have been using – contagious sociopathy – is not mutually exclusive from what we have been observing with the perversion of Christian thought to suit sociopathic behaviors and the rise of fascism in the U.S. (Ruth Ben-Ghiat has written extensively on the latter). In addition, and in no way trying to simplify or underestimate the factors underlying American racism, the racist platforms of the far right and GOP, have provided a type of currency by which contagious sociopathy can spread – many have argued that the ascension of Donald Trump allowed closeted racists to become public racists. Racism includes the antisocial tendencies of demeaning, manipulating, and harming others without remorse as a key feature.
One cannot talk about contagious sociopathy without considering righteousness – a term describing the phenomenon by which malicious acts – including harming and killing others – are justified as long as the bad actor can consider the ‘victims’ to be an enemy. This is a bedrock of the Trump and MAGA attacks on the Left and any that criticize or oppose them.
I have written and said it before and I will do so again: The contagious spread of sociopathy has provided us with potential and actual leaders who embody the worst that humanity has to offer according to moral, legal, religious/spiritual, and societal norms…and they continue to run on this platform.
About the author: Seth D. Norrholm, PhD (Threads: neuropsychophd) is an Associate Professor of Psychiatry and Behavioral Neurosciences at Wayne State University School of Medicine. Dr. Norrholm has spent 20 years studying trauma-, stressor-, anxiety-, depressive-, and substance use-related disorders and has published over 120 peer-reviewed research articles and book chapters. The primary objective of his work is to develop “bench-to-bedside” clinical research methods to inform therapeutic interventions for fear and anxiety-related disorders and how they relate to human factors such as personality, genetics, and environmental influences. Dr. Norrholm has been featured on NBC, ABC, PBS, CNN, Politico.com, The New York Times, The New York Daily News, USA Today, WebMD, The Atlantic, The History Channel, Scientific American, Salon.com, The Huffington Post, and Yahoo.com.
12 notes
·
View notes
Note
there’s no happy ending for claudia! i am screaming into the void 😵💫😵💫😩
there really isnt. when shes like ‘i couldve been married , cleaning up after my own babies’ before leaving its all lies shes telling herself bc lestat&louis reading her diary was such an untold violation of her own self n really a break in her own fantasy. claudia too was given n played along into a childhood + a family she was otherwise denied, until she became too old to play along anymore. its one thing to baby a .. say. 16 year old vampress w the body of a 14 year old, its a different ballgame when shes in her 20s n 30s in that same body. unchanging even as her mind grows. & lestat + louis both wanted to give claudia all the things they never had in their own roles they occupied as her parents but when confronted w/ what claudia actually said she wanted, they not only couldnt provide but eventually failed her in some way. truly, she was on the verge of death when louis found her and there was no way out. like louis pushing thru the wall w vampire strength was the only way claudia could have avoided the flames. & even if she survived the fires somehow w/o being saved, life trajectories for physically disabled ppl , especially young girls, of that extent in that era was awful. skin grafting technology had barely took off n only rly became a thing after world war i& extensive grafts n surgery claudia in this hypothetical would need is p exclusive for wealthy ppl who could afford it even to this day much less back b4 the us developed a centralized healthcare system. so shed probably die from her injuries or some acquired infection related to her injuries were it not for the vampirism. where book!claudia is more easily a blank slate for this family archetype bc of her even smaller self + the fact that she spent some of her early years catatonic, show!claudia is an older child with more of a foundational ego & self built from years of neglect n trauma. so thats why its even more disappointing what unfolds, bc her life has sort of become a self fulfilling prophecy of being neglected & hurt. show claudia’s will is ingrained in her that seeps thru, where its something of an acquired trait that arrives squarely from being made a vampire in the book. all this to say was whether book or show, there was no happy ending for a dying girl in a foregone time, and making this girl a vampire was just drawing out her inevitable end.
74 notes
·
View notes
Text
I have made it to the ER and just got admitted.
This is my second ER visit since my 32nd bday. The first one was when I was having flu/respiratory symptoms (turned out to not be covid, flu, or RSV - maybe just a cold - and honestly shouldn’t have gone and just rode out the wave of being sick (I was running a fever)).
This visit… may have a kidney infection! Or at risk for sepsis! Or a fucking impossible UTI! Or very chronically inflamed!
I don’t fucking know which is why I’m here as I devolve into more and more pain.
I’m so close to breaking down crying.
Even tho I technically work for this hospital. I haven’t been in this particular ER since my 32nd bday (with my ex-spouse).
I was here ALL the time.
And like… subjectively, I *feel* healthier than any of those times… mainly bc I’m not in a fucking horrible relationship and etc.
But objectively I really may be at risk for sepsis.
The bacteria that infected me is something that I’m 60-90% sure I acquired during my last bladder instillation appointment.
And I’m also 90% sure that these people here (which is really the fault of the healthcare system and not them personally) will not get why I am so worried or even how much pain I’m in (I mask my pain well unless I can’t handle it anymore or if I’m near intimate partners (I have no intimate partners currently)).
Pain is rising.
And I am SO FUCKING TIRED.
And angry.
And hopeful I guess?
Idk a lot.
—
Still mentally feeling sound :/
But that’s gonna go downhill pretty soon as the pain/dizziness/fatigue rise.
And this time, I have no asshole of an ex-partner to stand up for me (as much I complain about them… they did stand up for me during hospital visits from time to time).
#health update#chronic illness#will they take me seriously this time?#healing#disability#interstitial cystitis#UTI#possibly kidney infection#possible sepsis risk#trauma#healthcare trauma#healthcare#neurodivergence#audhd#autistic#adhd#prose
9 notes
·
View notes
Text
The Weather
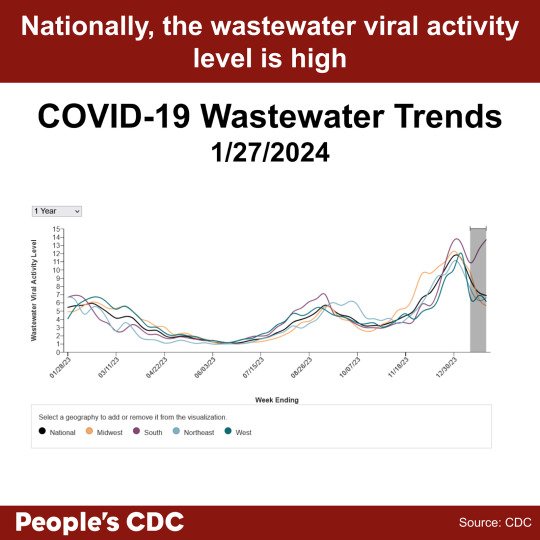
More than half of all US states remain at high to very high levels of SARS-CoV-2 detected in wastewater since January 25, 2024. As more people face reinfections, COVID remains a serious disease and we recommend that you continue to take precautions as the risk for infection is high at this time.

Although wastewater levels have dropped for multiple US regions, wastewater levels in the South have climbed higher than we’ve seen for any region this season and are currently the second highest peak we’ve experienced in the duration of the pandemic. This is a particularly concerning rebound as at the beginning of the year, Southern levels were experiencing a sharp decline. CDC’s national and regional wastewater data over time also show high levels nationally. As a reminder, the last two weeks are provisional data, indicated by a gray shaded area on the graph, therefore these values may change as additional wastewater sites report data. We want to remind you that multiple layers of precautions will protect against a COVID infection.
Wins
We thank many of you this week for joining us and in signing on with our letter to the ACLU regarding the actions taken by the CDC’s Healthcare Infection Control Practices Advisory Committee (HICPAC) that previously weakened already insufficient protocols employed within healthcare settings. We had many concerns with the actions taken by HICPAC. As a result of your actions, as well as support by many of our allies at previous HICPAC meetings, the CDC responded on January 23, 2024, with a request to consider clarification questions in distinguishing masks and N95 respirators. The CDC asked HICPAC to consider these questions prior to submission to the Federal Register for more public comment. This success demonstrates the importance of working together and holding the CDC accountable for ensuring safe healthcare settings for all patients and healthcare workers. You may also submit an additional comment or a reply to the CDC’s official response to HICPAC at the bottom of the news release.
As many healthcare systems and public health departments have restored masking in healthcare settings only when facing public pressure, without further action this important measure may not last. We ask you to support national and local groups to advocate for everyone’s safety in maintaining universal masking in all healthcare and healthcare-like settings. Universal masking can become a standard of preventative care rather than a short term response to infectious disease already surging.
Variants
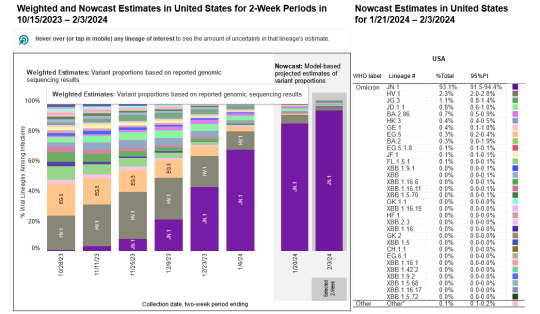
JN.1 remains the dominant variant in the United States, and is approximately 93.1% of circulating variants as of 2/3/2024. HV.1 drops even further to 2.3%, and all other variants are estimated to make up less than 2% each. The updated 2023-2024 COVID vaccines updated with the XBB.1.5 variant were recently shown by a MMWR report to be at least 49% to 60% effective against symptomatic infections during the Fall season, from late September 2023 to mid-January 2024. By ensuring additional precautions including testing, masking, ventilation, and air filtration, the additive effect will ensure a higher effectiveness.
Vaccine uptake remains limited with only 21.8% of adults and 11.6% of children receiving the updated COVID vaccine as of 2/02/24. The Bridge Program remains available for those underinsured or without insurance for no-cost access to these vaccines.
Hospitalizations
A downward trend continues with new hospital admissions, currently at 22,636 the week of January 27, 2024. We still do not know the total number of hospital-acquired infections, since reporting over these numbers was halted in May of 2023. Despite this decrease in new hospital admissions, please consider that wastewater levels are still high nationwide, and that hospitalization does not reflect the current amount of circulating virus. Please continue to exercise caution and wear a well-fitting respirator indoors.

Testing and Treatment
A study published in Clinical Infectious Diseases (CID) found that SARS-CoV-2 viral load peaks around the fourth day of symptom onset. This may suggest why tests do not seem to be picking up positive cases early on. This does not mean that transmission is unlikely prior to the fourth day of symptoms, but rather, one should continue to employ serial testing and isolation measures beyond the first few days of illness. If you have tested negative on day one or two with a rapid antigen test (RAT), you may still have a COVID infection, unless you test negative on day four or five with a RAT.
Because of a lack of RAT sensitivity, people may mistakenly believe they do not have COVID, and both enter isolation too late and exit isolation prematurely, leading to increased transmission within the population. For this reason, it is important to wear a high quality respirator at the onset of COVID-like symptoms, regardless of a negative test. We must demand for more sensitive testing and no-cost access to better tests (such as PCR), as well as an infrastructure that allows for longer sick leave and sick-time pay. At this time, limited testing options remain at no cost including the Test to Treat program and Walgreens PCR program as well as treatment options including the no cost antiviral program operated by Pfizer and supported by Health and Human Services. Remember to check for regional offerings as well such as the “Express Testing” PCR program in New York City, which could be more accessible to you.
Vaccines
On February 1, the CDC published in its Morbidity and Mortality Weekly Report (MMWR) that the most recently updated monovalent XBB.1.5 booster offered 54% increased protection against symptomatic (self-reported) COVID. Note, the study was limited as it did not evaluate the effectiveness against asymptomatic COVID cases. The CDC recommends that all individuals older than 6 months of age should receive the updated vaccine. If you have not yet received your vaccine, please do so.
Current updated vaccines being somewhat effective against symptomatic acute infection is not enough, and we should demand for sterilizing immunity of COVID through vaccines. Intranasal vaccines, which may induce a more robust mucosal immunity based on animal models, seem to be in the pipeline. However, it is unclear whether production of such vaccines is receiving appropriate funding or will be available to the public anytime soon.
The CDC Advisory Committee on Immunization Practices (ACIP) is having a meeting on February 28-29th and COVID vaccines will be on the agenda. We will be sending information on a request for actions in the coming few weeks on how to participate in ensuring the CDC takes appropriate steps to protect the public from ongoing COVID infections.
Take Action
Further research and investment is needed for effective treatments against Long COVID. PCORI, the Patient-Centered Outcomes Research Institute, is seeking individuals to represent patient voices on their advisory panels. This is an invaluable opportunity to advocate for Long COVID research as this research and funding organization has an annual budget of nearly 300 million dollars for medical research. Applications are due March 29, 2024 and those selected to be on their advisory panels can participate virtually. Lending your voice to this is invaluable.
We must also ensure constant access to no or low cost high quality masks and respirators. Request that the federal government ensure that there remains ongoing local manufacturing of high quality masks and N95 respirators to prevent a future shortage by contacting your representatives.
Many people rely on pulse oximeters in healthcare and at-home settings as a medical device to check blood-oxygen levels during an active COVID infection and recovery. For several decades, it has been established that these medical devices have failed to measure accurately when used with darker skin color. In response, a recent lawsuit has been filed against 12 manufacturers. In addition, the FDA is currently seeking comments through the Federal Register on this matter. We ask you to submit a public comment asking the FDA to act immediately and ensure future pulse oximeters are properly manufactured to support all people.
#op#covid#covid vaccine#covid 19#long covid#covid isn't over#covid19#mask up#covid pandemic#pandemic#covid-19#sars cov 2#sars-cov-2#coronavirus pandemic#coronavirus#pcdc#people's cdc#wear a mask#covid news#covid conscious#covid cautious#covid variants#covid vax#covid variant#medical news#medical#uspol#img#links#described in alt text
23 notes
·
View notes
Text
lol I think my dad is slamming shit around the house because I sent him a text with long covid info and told him he needs to upgrade from a cloth mask if he doesn't want covid to disable him because acquiring other conditions from an infection is so common.
y'all weren't cloth masks only recommended because there weren't enough n95s for healthcare workers if everyone got them?
here's the link if anybody needs a resource to share:
#masking#covid#chronic illness#disability#me/cfs#personal#ableism#chronic fatigue syndrome#chronically ill#disabled#long covid
19 notes
·
View notes
Text
The Role of Ertapenem 100 mg in Modern Antibiotic Therapy
In recent years, the growing challenge of antibiotic resistance has prompted healthcare professionals to explore newer therapeutic options. Among these, Ertapenem 100 mg has emerged as a significant player in modern antibiotic therapy. This broad-spectrum antibiotic belongs to the carbapenem class and is renowned for its effectiveness against a variety of infections, particularly those caused by Gram-negative bacteria. In this blog, we will delve into the importance of Ertapenem, its applications, and its availability through Ertapenem 100 mg injection manufacturers in India, exporters, suppliers, and distributors.

Understanding Ertapenem
Ertapenem is a synthetic beta-lactam antibiotic that offers potent activity against a wide range of bacterial pathogens. Its unique structure allows it to penetrate bacterial cell walls effectively, making it suitable for treating complex infections, including those originating from intra-abdominal sources, skin and soft tissue infections, and pneumonia. Given the rising rates of resistance to commonly used antibiotics, Ertapenem provides a vital alternative for clinicians seeking reliable treatment options.
The Need for Effective Antibiotics
The World Health Organization (WHO) has recognized antibiotic resistance as one of the most significant global health threats. With an increasing number of bacterial strains becoming resistant to traditional therapies, the role of advanced antibiotics like Ertapenem has become crucial. The ability of Ertapenem to maintain its efficacy against resistant strains makes it an essential component of modern treatment regimens.
Applications of Ertapenem 100 mg
Ertapenem is indicated for various infections, including:
Intra-abdominal Infections: It is often used to treat complicated intra-abdominal infections due to its broad spectrum of activity.
Skin and Soft Tissue Infections: Ertapenem is effective against multiple pathogens commonly responsible for skin infections.
Pneumonia: This antibiotic is also a go-to treatment for community-acquired pneumonia.
Complicated Urinary Tract Infections: Ertapenem can be a critical option when dealing with complicated cases.
The versatility of Ertapenem makes it a valuable asset in a clinician's toolkit, particularly for patients who have not responded to other antibiotic therapies.
Availability in India
Ertapenem 100 mg Injection Manufacturers in India
India has a robust pharmaceutical industry, recognized for producing high-quality medications at competitive prices. Numerous Ertapenem 100 mg injection manufacturers in India are dedicated to maintaining stringent quality standards while ensuring that their products meet international guidelines. These manufacturers play a vital role in making Ertapenem accessible to healthcare facilities across the country and abroad.
Ertapenem 100 mg Injection Exporters in India
The global demand for effective antibiotics has led to an increase in Ertapenem 100 mg injection exporters in India. These exporters are crucial in supplying this essential medication to international markets, contributing to India's reputation as a leader in the global pharmaceutical landscape. The adherence to quality and regulatory standards has helped these exporters establish strong relationships with healthcare providers worldwide.
Ertapenem 100 mg Injection Suppliers in India
A reliable supply chain is fundamental for the availability of Ertapenem in hospitals and clinics. Numerous Ertapenem 100 mg injection suppliers in India ensure that healthcare institutions receive timely deliveries of this critical antibiotic. These suppliers work closely with manufacturers to maintain a steady stock, facilitating uninterrupted access to essential medications.
Ertapenem 100 mg Injection Distributors in India
The role of Ertapenem 100 mg injection distributors in India is equally important. They bridge the gap between manufacturers and healthcare providers, ensuring that the product reaches the end-users efficiently. Distributors are vital in managing logistics, handling regulatory compliance, and addressing the needs of various healthcare institutions. Their efforts ensure that doctors have immediate access to this antibiotic, particularly in emergency situations.
Best Indian Pharma Industry 2024
The best Indian pharma industry 2024 is characterized by innovation, quality, and a commitment to addressing public health challenges. With a focus on research and development, Indian pharmaceutical companies are continually improving their product offerings. The introduction of advanced antibiotics like Ertapenem is a testament to the industry’s efforts to combat antibiotic resistance. The commitment to maintaining high manufacturing standards and complying with international regulations has solidified India’s position as a trusted source for pharmaceuticals worldwide.
Conclusion
The role of Ertapenem 100 mg in modern antibiotic therapy cannot be overstated. As antibiotic resistance continues to pose significant challenges to healthcare, the importance of effective and reliable treatments like Ertapenem becomes even more critical. The collaboration among Ertapenem 100 mg injection manufacturers, exporters, suppliers, and distributors in India has made this essential antibiotic readily available to healthcare providers, ensuring that patients receive the best possible care.
In 2024, as the best Indian pharma industry continues to evolve, the ongoing development and distribution of innovative antibiotics will remain pivotal in the fight against infectious diseases. By prioritizing access to effective medications, we can work towards a healthier future and combat the ever-growing threat of antibiotic resistance.
#Ertapenem 100 mg for injection distributors in India#Ertapenem 100 mg for injection suppliers in India#Best Indian pharma industry 2024#Ertapenem 100 mg for injection exporters in India#Ertapenem 100 mg for injection manufacturers in India
3 notes
·
View notes
Text

Please join us in sending a letter to congress via Resistbot, to maintain masking in healthcare settings.
Please text PRIKQU to 50409 and the Resistbot will take care of getting the letter sent on your behalf.
Demand Masks in Healthcare
As my representatives in Congress, I am asking you to intervene with the CDC and with all levels of the Administration in regards to Covid-19.
We MUST have N95 masks or equivalent worn by all staff with patient contact in healthcare facilities-hospitals, outpatient centers, and nursing homes.
The HICPAC advisory committee to the CDC is proposing to weaken infection control measures. They are incorrectly saying that surgical masks are as protective as N95s, cherry-picked their data, and ignored abundant evidence to the contrary.
Further, some hospitals (like MGH) are not honoring requests from patients that staff wear a mask. This would appear a violation of ADA standards for accommodation and is unconscionable, resulting in patients delaying necessary care because they risk a deadly hospital-acquired Covid infection.
Dr. Cohen like the rest of the Administration is pretending that Covid is over and is focusing on the "urgency of normal." They are pushing people to go back to unmasked offices with inadequate ventilation, when teleworking has worked very well.
On July 20, 900 experts sent a letter to Dr. Cohen asking her and HICPAC to make their processes transparent, to seek the input of a variety of stakeholders, and to listen to experts in ventilation and aerosols. See https://journals.sagepub.com/doi/10.1177/10482911231195898. This has fallen on deaf ears.
On 8/25, in "The Check-in with Dr. Cohen," a Q&A session, Dr. Cohen tells people to wash their hands and stresses "it's important to use all the tools we have in our toolbox to protect ourselves." Not once did she mention masks or ventilation, both critically important since we know that Covid is primarily transmitted by aerosols.
The CDC states its mission is Saving Lives, Protecting People.TM They have abdicated in meeting their responsibility.
#resistbot#please send a letter to congress to help keep health facilities safe for everyone#cdc#mandy cohen#cdc director#covid#masks in healthcare#keep masks in healthcare
52 notes
·
View notes
Text
How Adult Male Circumcision Improves Sexual Health

Adult male circumcision, the surgical removal of the foreskin from the penis, has been practiced for centuries for various reasons, including religious, cultural, and medical purposes. Beyond its traditional significance, research has increasingly highlighted the potential benefits of adult male circumcision for sexual health. In this article, we’ll explore the evidence-backed ways in which adult male circumcision can enhance sexual health and well-being.
Reduced Risk of Sexually Transmitted Infections (STIs):
One of the most compelling reasons cited for adult male circumcision is its role in reducing the risk of sexually transmitted infections (STIs), including HIV. Numerous studies have demonstrated that circumcised men are at lower risk of acquiring HIV, herpes simplex virus (HSV), human papillomavirus (HPV), and other STIs compared to uncircumcised men. This is believed to be due to the decreased surface area and moist environment under the foreskin, which can facilitate the transmission and replication of pathogens.
Lower Risk of Penile Cancer:

Adult male circumcision has also been associated with a reduced risk of penile cancer, a rare but serious condition that affects the tissues of the penis. The removal of the foreskin eliminates the moist and bacteria-prone environment that may contribute to the development of penile cancer. While penile cancer is relatively rare, circumcision offers a preventive measure that can lower the risk of this disease.
Improved Hygiene:
The removal of the foreskin through adult male circumcision simplifies genital hygiene and may reduce the risk of certain infections and irritations. Without the foreskin, it’s easier to clean the penis, as there are no folds or creases where bacteria and debris can accumulate. This improved hygiene can contribute to overall genital health and comfort, reducing the likelihood of unpleasant odors or infections.
Enhanced Sexual Satisfaction:
Some studies suggest that adult male circumcision may lead to increased sexual satisfaction and pleasure for both men and their partners. This is thought to be related to changes in penile sensitivity and sensation following circumcision. While individual experiences may vary, some men report heightened sexual sensitivity and improved erectile function after undergoing circumcision, which can positively impact sexual satisfaction and intimacy.
Reduction in Foreskin-Related Issues:
Uncircumcised men may experience foreskin-related issues such as phimosis (tight foreskin), paraphimosis (inability to retract the foreskin), or recurrent infections. Adult male circumcision can alleviate these problems by removing the foreskin entirely, eliminating the need for ongoing treatment or management of foreskin-related conditions. This can lead to improved genital comfort and function, enhancing overall sexual health and well-being.
Psychological Benefits:
In addition to the physical benefits, adult male circumcision may have psychological benefits for some individuals. For men who choose circumcision for personal or cultural reasons, undergoing the procedure can bring a sense of empowerment, confidence, and cultural identity. Feeling more comfortable and confident in one’s body can positively influence sexual self-esteem and relationships.
Conclusion:
Adult male circumcision offers several potential benefits for sexual health, including reduced risk of STIs, lower risk of penile cancer, improved hygiene, enhanced sexual satisfaction, resolution of foreskin-related issues, and psychological well-being. However, it’s important to note that circumcision is a personal decision, and individual experiences and preferences may vary. Before considering circumcision, it’s essential to consult with a healthcare provider to discuss the potential risks, benefits, and implications of the procedure. Ultimately, the decision to undergo adult male circumcision should be informed by careful consideration of one’s health, cultural beliefs, and personal preferences.
3 notes
·
View notes
Text
Title: The Six Most Dangerous Diseases: A Closer Look

Introduction:
In our ever-evolving world, where medical advancements are constantly being made, some diseases continue to pose significant threats to human health. These diseases, often life-threatening and difficult to treat, have claimed countless lives throughout history. In this article, we delve into the six most dangerous diseases that have left a lasting impact on global health.
1. HIV/AIDS:
Human Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome (AIDS) remain one of the most dangerous diseases, affecting millions worldwide. HIV weakens the immune system, leaving individuals susceptible to opportunistic infections. Since its discovery in the 1980s, AIDS has claimed over 32 million lives, highlighting the importance of education, prevention, and access to antiretroviral treatments.
2. Malaria:
Malaria, caused by parasites transmitted through infected mosquitoes, remains a significant global health concern. It primarily affects tropical and subtropical regions, causing over 400,000 deaths annually. Efforts to control malaria include mosquito control, bed nets, and antimalarial drugs, yet challenges such as drug resistance and climate change persist.
3. Tuberculosis (TB):
Tuberculosis is an airborne bacterial infection that mainly affects the lungs but can spread to other parts of the body. With over 1.4 million deaths in 2019, TB remains a formidable threat, particularly in impoverished and densely populated areas. Multidrug-resistant TB strains pose additional challenges to treatment and eradication.
4. Ebola Virus Disease:
Ebola gained global attention due to its rapid spread and high mortality rate during outbreaks. The virus causes severe bleeding, organ failure, and death. While outbreaks are sporadic, they have proven devastating, requiring swift containment efforts and international collaboration to prevent further loss of life.
5. Cancer:
Cancer encompasses a range of diseases characterized by uncontrolled cell growth. It is a leading cause of death worldwide, with variations in incidence and mortality rates depending on the type of cancer and region. Advances in early detection, treatment modalities, and personalized medicine are crucial in the ongoing battle against cancer.
6. Cardiovascular Diseases:
Cardiovascular diseases, including heart disease and stroke, collectively account for the highest number of deaths globally. Risk factors such as unhealthy diets, lack of physical activity, smoking, and high blood pressure contribute to their prevalence. Public health campaigns promoting heart-healthy lifestyles and access to quality healthcare play a vital role in reducing the burden of these diseases.
Conclusion:
While medical progress has enabled us to better understand, prevent, and treat many diseases, the six mentioned above continue to pose significant challenges to global health. Effective strategies, international cooperation, and ongoing research are essential in addressing these dangerous diseases and minimizing their impact on individuals and communities around the world.
#disease#health#fitness#our flag means death#1950s#80s#bmw#cars#cute#barbie#drawing#ferrari#rwby#succession
3 notes
·
View notes
Text
Also preserved on our archive
This letter writer believes a priority of the next B.C. government should be to improve COVID-19 prevention in healthcare facilities.
Dear Premier:
If you want to start fixing healthcare, there are three easy and obvious moves you can make. Currently, your government is doing none of these, but you could change this.
To begin with, we must acknowledge the simple fact that we are not “post-COVID” nor “post-pandemic.”
In May 2023, WHO [World Health Organization] declared COVID-19’s emergency phase to be over but at no point did it declare the pandemic to be over. We may all be done with COVID, but COVID is not done with us.
First, it’s time to improve COVID prevention in healthcare facilities. Doing so will significantly relieve pressure on hospital beds and reduce the number of health care workers off sick.
Recently, four Fraser Health Authority hospitals — Surrey Memorial, Delta, Royal Columbian and Abbotsford Regional Hospital — all had COVID-19 outbreaks.
The situation is likely no better in B.C.’s other health authorities. We only know about Fraser Health because unlike the others, it is more transparent.
When there are already too few hospital beds, the last thing we should be doing is infecting patients who are in hospital for another reason, and needlessly prolonging their hospital stays.
For the week of Sept. 8, stats from the Canadian Nosocomial (Hospital-Acquired) Infection Surveillance Program, with data from 78 hospitals, including 16 in BC, show that 34.1 per cent of patients in hospital with COVID, acquired their infection while admitted for another medical condition.
This is a major failure by public health and Infection Prevention and Control (IPAC).
Before the pandemic began, Canada already had one of the lowest numbers of hospital beds per population out of the OECD countries. That number had never kept up with our population growth let alone with our aging demographic.
Now add to that problem lengthened hospital stays, increased COVID hospitalizations and outbreaks, and an explosion in chronic diseases and disability following repeated COVID infections.
Second, Premier Eby, you should be ensuring that British Columbians get access to the new updated COVID vaccines immediately. This would prevent COVID-19 hospitalizations, lessen transmission and disease severity and would also protect health care providers and keep them on the job.
I know that going into an election you’d much rather not talk about COVID. However, delaying COVID vaccines until after the election, or under the guise of co-administering it with influenza vaccine, is only repeating last fall’s error.
Vaccination should always occur before infections peak. This year, the United States sped up its vaccine approval and started vaccinating at the end of August.
Health Canada has already approved the 2024-25 updated COVID-19 vaccines, what are we waiting for?
Third, I understand Premier that you would much rather delay the re-introduction of masks (preferably well fitted and high grade) in healthcare until after the election, but that would also be a mistake.
Recall what happened in 2020, it wasn’t until two days after the election that new regulations came into effect, and by then it was too late to stop the spread.
Yes, votes matter, but so do voters’ health.
Finally, Premier, there is no longer any serious debate that COVID is spread through the air, not by the hands. Keeping COVID out of all healthcare facilities will require cleaning the air.
Yes, you can still wash your hands, but to prevent COVID infections, it’s the air that matters.
Appallingly, in 2024, B.C. public health and infection prevention and control (IPAC) leaders at hospitals and the Provincial Infection Control Network of BC still continue to push for handwashing and surface cleaning to protect against COVID.
Clearly this strategy is not working, as health care facilities outbreaks keep happening and patients and health care workers keep getting infected, with some dying and others developing Long COVID.
At this point in the pandemic, repeating the same error over and over while expecting different results is beyond madness, it is reckless and incompetent.
British Columbians deserve better public health and IPAC leaders. Health care workers should be able to rely on effective workplace health and safety measures to protect them from getting sick on the job. But most of all, patients should not fear infections whenever they seek medical care or are admitted to a hospital.
In summary, Premier Eby, getting updated COVID vaccines into arms now and bringing masks and clean air into all health care settings will help preserve BC’s health care capacity now.
"A B.C. that works for all British Columbians" needs a functioning healthcare system.
Currently, British Columbians have neither.
- Lyne Filiatrault, retired B.C. emergency physician
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator
7 notes
·
View notes