#handbook of diagnosis and treatment of dsm 5 personality disorders
Explore tagged Tumblr posts
Text
Clinical Formulations of Narcissistic PD
Clinical formulations and case conceptualisations are introduced in this post.
These are all generalisations and theories of how NPD develops, not something that is supposed to be true for everyone with NPD.
Psychodynamic model
Freud suggests parents either overvaluing or neglecting (or both) a child can lead to NPD & especially inability to form healthy, lasting relationships and regulate self-esteem
"In other words, [NPD] is the outcome of insufficient gratification of the normal narcissistic needs of infancy and childhood."
Kohut theorises that narcissists' ability to form a cohesive sense of self and others was developmentally arrested in childhood, resulting in grandiosity & idealising others
"Narcissistic injury" = fragmentation of the self
Kernberg suggests grandiosity & exploitation result from maternal emotional abuse
Grandiosity is an "emotional escape valve"
Grandiosity & entitlement mask the "real self" that is "split off"
The real self unconsciously holds rage, fear, envy, deprivation
Defensive structure is same as BPD but difference is grandiosity
Biosocial model
NPD is primarily the result of environment, especially "parental indulgence and overvaluation, learned exploitive behavior, and only-child status"
Special treatment from caregivers leads children to believe that the "world revolves around them", and therefore they expect the same outside the home
When special treatment outside the home doesn't happen, they "experiment with demanding and exploitive tactics and subsequently develop considerable skill in manipulating others"
"At the same time they come to believe that most others are inferior, weak, and exploitable."
NPD is self-perpetuating through sense of superiority, lack of self control, sense of entitlement, and dismissing of those who reject their world / self-view
Cognitive-Behavioural model
Key feature of NPD is self-aggrandisement
Core beliefs:
> Deserving of special treatment
> Not bound by social norms and rules
Conditional beliefs:
> Others should be punished for not recognising their specialness
> To maintain that special status others should be subservient to them
Instrumental belief:
> Always strive to demonstrate their superiority
> See themselves as special, superior, entitled to special favors and treatment, and vulnerable to loss of status
> View others as inferior but potential admirers
Main pattern of behaviour is "seeking prestige, power, position, and wealth as a way of reinforcing their image of superiority", using "manipulation and guile" if necessary
The primary schema is superior & special (/ entitlement & grandiosity)
> Superior schema "shaped by flattery, indulgence, and favoritism"
> Special schema shaped by "rejection, limitations, exclusion, or deficits"
> Common denominator is the belief that the individual is different in some way
Three subtypes:
> Self-centered impulsive type
> Ruthless impression-management type
> Acceptance-oriented impression-management type
> Each type is centred around an impulse control deficit developed in childhood
> "Specifically, these individuals learned to seek reinforcers without having to work for them. This resulted in their development as self-indulgent, egocentric, and impulsive individuals."
> Ruthless & Acceptance-oriented types focus on creating favourable impressions with others, but struggle with long-lasting healthy relationships because of their empathy deficits
Interpersonal model
People with NPD were raised in an environment of "selfless not contingent" love, leading to insensitivity to others' needs
The caregiver was over-adoring, but there was also a constant threat of a "fall from grace", with pressure to be the perfect child
The constant overbearing love means that any criticism or disappointment hits very hard
"In short, there is extreme vulnerability to criticism or being ignored, together with a strong wish for love, support, and admiration from others. Noncontingent love and presumptive control of others is expected and even demanded. If support is withdrawn, or lack of perfection is evident, the self-concept degrades into severe self-criticism."
Integrative model
People with NPD are hypersensitive
Seen as exceptional children, leading to pressure to perform
As children likely had highly developed speech and interpersonal skills
Life purpose: "I’m special and unique, and I am entitled to extraordinary rights and privileges whether I have earned them or not."
World-view: "Life is a banquet table to be sampled at will. People owe me admiration and privilege."
Goal: "Therefore, I’ll expect and demand this specialness."
Defense mechanisms: rationalisation and projective identification
Parental injunction: "Grow up and be wonderful—for me."
"The illusion of specialness, disdain for others’ views, and a sense of entitlement lead to an underdeveloped sense of social interest and responsibility. This, in turn, leads to increased self-absorption and confirmation of narcissistic beliefs."
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#len sperry#handbook of diagnosis and treatment of dsm 5 personality disorders#personality disorder concepts#case conceptualisations#clinical formulations#pd info#npd#npd info#dogpost
175 notes
·
View notes
Text
a dissertation nobody asked for, ft. my dysphoric trans ass (on the subject of truscum, cisgender medicine, and stupid assholes)
BOY HOWDY DID THIS GET LONG
I know that nobody asked for this post, and definitely nobody needed it, but you know what? Fuck it. You’re getting this post anyway.
Very recently someone in the community outed himself (himself, because I’m aware that he uses he/him pronouns and am not a piece of shit who will misgender someone under guise of offering anonymity. Cough cough.) as a transmedicalist. A truscum, if you will, because we all know that they mean the same thing and anyone who tries to convince you otherwise is a bitchcoward and a bigot.
Very disappointing, yes, considering the amount of transgender people* I know exist in this community, myself included. Disappointing, frightening, and rage-inducing. Particularly because this revelation followed an encounter said truscum had with a close friend of mine. Which I admit might make me a little biased but shhh. Neither me nor my friend(s) started this. The contents of that conversation had between the truscum and my bro should have been handled privately like an adult but- hey, since we’re putting all this shit out there now, guess I get to put in my two cents! Awesome!
And because we apparently like to bring science into shit, let’s get a lil scientific up in this bitch.
*Note: transgender from here on will be used to refer to as the umbrella of non-cis gender identities just for context and ease of reference. And also because that’s what it is, fuck off.
So, guys. Let’s talk about dysphoria.
PART 1. SEMANTICS
Dysphoria. Most of you have heard of it, particularly those among us (both within and outside of the fantroll community) who happen to be transgender.
But what does it actually mean? Let’s look a little closer. Dysphoria, as defined by Merriam-Webster:
dysphoria (noun)
dys·pho·ria | \ dis-ˈfȯr-ē-ə \
Definition of dysphoria
: a state of feeling very unhappy, uneasy, or dissatisfied
— see GENDER DYSPHORIA
But this is just semantics. Let’s look at it, and gender oriented dysphoria in particular from a mental health perspective-
“Gender dysphoria is the feeling of discomfort or distress that might accompany a difference between gender identity, sex assigned at birth or sex-related physical characteristics. This type of distress doesn't affect everyone who is transgender.
Gender dysphoria is listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), a manual published by the American Psychiatric Association to diagnose mental conditions. Gender dysphoria is a diagnosis that is given to individuals who are experiencing discomfort or distress due to the difference between gender identity, sex assigned at birth or sex-related physical characteristics.”
This is from the Mayo Clinic, a nonprofit academic medical center based in Rochester, Minnesota, lauded as the best hospital in the nation for 2018-2019 by the U.S News and World Report. Do with that information what you will, but most would consider the Mayo Clinic (while not a good replacement for proper doctor’s visits and medical treatment) a pretty credible health resource.
But we’ll come back to this.
For now, let’s look at another definition. That of the word ‘opinion.’
PART 2: FACTS VS. OPINIONS VS. BELIEFS VS. PREJUDICE
opinion (noun)
opin·ion | \ ə-ˈpin-yən \
Definition of opinion
1a : a view, judgment, or appraisal formed in the mind about a particular matter
We asked them for their opinions about the new stadium.
b : APPROVAL, ESTEEM
I have no great opinion of his work.
2a : belief stronger than impression and less strong than positive knowledge
a person of rigid opinions
Opinions are inherently biased. It may be influenced by facts, but opinions in and of themselves are not fact. To borrow and paraphrase from Fowler, H. Ramsey. The Little, Brown Handbook. Boston: Little, Brown, 1986.:
When forming personal convictions, we often interpret factual evidence through the filter of our values, feelings, tastes, and past experiences. Hence, most statements we make in speaking and writing are assertions of fact, opinion, belief, or prejudice. The usefulness and acceptability of an assertion can be improved or diminished by the nature of the assertion, depending on which of the following categories it falls into:
A fact is verifiable. [Determinable by] ...researching the evidence. This may involve numbers, dates, testimony, etc. (Ex.: "World War II ended in 1945.") The truth of the fact is beyond argument if one can assume that measuring devices or records or memories are correct. Facts provide crucial support for the assertion of an argument. However, facts by themselves are worthless unless we put them in context, draw conclusions, and, thus, give them meaning.
An opinion is a judgment based on facts, an honest attempt to draw a reasonable conclusion from factual evidence. [Opinions are] potentially changeable--depending on how the evidence is interpreted. By themselves, opinions have little power to convince. You must always let your reader know what your evidence is and how it led you to arrive at your opinion.
Unlike an opinion, a belief is a conviction based on cultural or personal faith, morality, or values. Statements such as "Capital punishment is legalized murder" are often called "opinions" because they express viewpoints, but they are not based on facts or other evidence. They cannot be disproved or even contested in a rational or logical manner. Since beliefs are inarguable, they cannot serve as the thesis of a formal argument. (Emotional appeals can, of course, be useful if you happen to know that your audience shares those beliefs.)
Y’all get what I’m getting at, right?
Oh, but one more thing I’d like to add- And I think this one is important.
“Another kind of assertion that has no place in serious argumentation is prejudice, a half-baked opinion based on insufficient or unexamined evidence. (Ex.: "Women are bad drivers.") Unlike a belief, a prejudice is testable: it can be contested and disproved on the basis of facts. We often form prejudices or accept them from others--family, friends, the media, etc.--without questioning their meaning or testing their truth. At best, prejudices are careless oversimplifications. At worst, they reflect a narrow-minded view of the world. Most of all, they are not likely to win the confidence or agreement of your readers.”
We’ve all encountered our fair share of these sorts of prejudices, disguised as “opinions.” Because isn’t that a much sweeter word for what it is? It’s not bigotry to delegitimize the experiences of other transgender people, it’s just an opinion. Like which is the best ice cream flavour, or something equally harmless.
But when your opinion involves the dehumanization, invalidation, exclusion and harm of other people… Well, that’s not so harmless, is it?
Racism is prejudice influenced by opinions and beliefs. Transphobia is prejudice influenced by opinions and beliefs. They are not fact, they are not based in rational thinking, and in many cases they cannot be argued because these prejudices are willingly cultivated and held.
‘But, Eli!’ I know at least one truscum who may or may not be reading this might cry, ‘It’s a scientifically proven fact that transgender people need to have dysphoria to be trans!’
To which I say fuck you, this is why that isn’t true.
Let’s go back to the definition of gender dysphoria, shall we?
“Gender dysphoria is the feeling of discomfort or distress that might accompany a difference between gender identity, sex assigned at birth or sex-related physical characteristics. This type of distress doesn't affect everyone who is transgender.”
MIGHT accompany a difference between those things, and DOESN’T affect everyone who is transgender. Interesting take coming from a scientific source, right? It’s almost like transmedicalist/truscum thinking is based off prejudice, rather than opinion; much less fact.
Especially considering dysphoria wasn’t even a word we (we meaning transgender people) chose for ourselves in the first place. It was picked by the American Psychiatric Association’s board of trustees to replace the term “Gender Identity Disorder” (GID)
Disorder. A sickness. Because Western medicine, practiced primarily by cisgender people (be they medical experts or not) has never been kind to transgender people. The word doesn’t mean what transmedicalists or truscum think it does. It doesn’t make you more valid than our fellow trans siblings just because the perceptions held by you or others of what your body and gender are worth make you miserable.
Wanna read up a little more on this? Check out these links:
THIS IS WHAT I WISH PEOPLE WHO IDENTIFY AS ‘TRUSCUM’ WOULD TRY TO UNDERSTAND.
Not All Transgender People Have Dysphoria – And Here Are 6 Reasons Why That Matters
Transgender People, Gender Identity and Gender Expression
PART 3: THE COMMUNITY (™)
If you’re dysphoric, my heart goes out to you. I’m dysphoric too. Dysphoric enough to transition despite the medical costs- because I was tired of feeling trapped in other people’s perceptions of me. But you know what? I love that there are transgender people who don’t feel defined by this persistent sensation of wrongness.
You shouldn’t be defined by that. Even dysphoric trans people know (or should, for the sake of their health) that your unhappiness isn’t the only thing that makes you transgender. In fact, in the least unhealthy cases, it’s only the smallest fraction of the gender experience. Being transgender and exploring your gender identity consist of a broad spectrum of emotions. The fact that some of us (US. WE are a community, and have to treat each other as such) get to snip that little fraction out of the spectrum is beautiful.
We’re made stronger by how different we all are, not weaker.
PART 4: IN CLOSING
Whether you’re dysphoric or not, whether you identify with a gender binary or not, you are worthy of celebration and validation and love. All of us have it rough- frankly speaking, cisgender people as a whole barely tolerate us even when our identities do follow the narrative most commonly accept us. It’s not our place to judge, or shun, or invalidate one another.
And as both a personal goodbye and a TL;DR to truscum who like to treat gender identity like a competition, like something you get to gatekeep and police, fuck you. Our identities are ours to decide, our experiences to forge, and if that happens to not include transitioning or dysphoria, no matter what your reasons are that doesn’t make you less valid.
Fuck you, for painting your bigotry as an opinion. Fuck you for hurting the feelings of other transgender people. And fuck you for making posts trying to paint yourself as anything other than an asshole so full of internalized transphobia and misery that you can’t look past it to respect other people and act like that’s only your opinion UWU
Anyway, trans rights.
#ooc#jesus this is so long#nobody's gonna read this#But I'm PISSED#trans rights#I hate terfs#And transmeds/truscums#All those motherfuckers#fuck that
38 notes
·
View notes
Text
Postpartum Anxiety: Symptoms, Causes, Treatment
New Post has been published on https://depression-md.com/postpartum-anxiety-symptoms-causes-treatment/
Postpartum Anxiety: Symptoms, Causes, Treatment

Postpartum anxiety is anxiety that occurs after giving birth. It is normal to be stressed and have anxious feelings after having a baby. After all, your life has undergone a huge change in taking on the responsibility of caring for your baby, often on little to no sleep.
While some amount of anxiety is completely normal during this period, postpartum anxiety refers to overwhelming anxiety and uncontrollable worry that inhibits your daily functioning. With postpartum anxiety, you may experience intrusive thoughts and physical symptoms, and find it difficult to take care of your baby and yourself.
Atipati Netiniyom / EyeEm / Getty Images
It is unclear exactly how many people experience postpartum anxiety—estimates of this condition range from 4.4% to 18%. One systematic review of 58 studies on postpartum anxiety found a prevalence rate of 8.5%.
Seeking diagnosis and treatment for postpartum anxiety will not only help you feel better, but it can support your baby’s development and keep you involved in your daily life, relationships, and the activities that are meaningful to you.
Postpartum Anxiety vs. Postpartum Depression
Unfortunately, postpartum anxiety is not as well-studied or publicized as its counterpart, postpartum depression, even though some research indicates that postpartum anxiety is actually more common than postpartum depression.
One study found that about 35% of people who experience postpartum anxiety will also have postpartum depression.
Definition of Postpartum Anxiety
There are no official diagnostic criteria for postpartum anxiety, but one definition is that it’s an anxiety disorder that occurs in the time period from immediately post-birth up to a year post-birth.
Most commonly, postpartum depression presents as generalized anxiety disorder (GAD), but other anxiety disorders such as obsessive-compulsive disorder (OCD) can also occur in the postpartum period.
Symptoms of Postpartum Anxiety
Symptoms of postpartum anxiety can include:
Intrusive or persistent thoughts
Excessive worry
Insomnia
Avoidant behaviors
Tension
Dry mouth
Nausea
Irregular heartbeat
Fatigue
Shakiness or trembling
Panic attacks
How these symptoms manifest will look different from person to person. You may find yourself constantly worrying that your baby is breathing and find it difficult to concentrate or focus on anything else as this worry consumes you.
You may avoid breastfeeding due to worry and anxiety about latching. Or you may be overwhelmed with physical symptoms like nausea or even chest pain.
If these symptoms are disproportionate to the situation and prevent you from functioning within your normal relationships, roles, and activities, it is important to have a conversation with your doctor.
If you are having suicidal thoughts, hallucinations, or are a risk to yourself, your baby, or others, there is help available. Contact the National Suicide Prevention Lifeline at 1-800-273-8255 for support and assistance from a trained counselor. If you or a loved one are in immediate danger, call 911.
For more mental health resources, see our National Helpline Database.
Diagnosis
Diagnosis of postpartum anxiety can be challenging or missed for multiple reasons. First, many anxiety symptoms may be considered “normal” in the postpartum period.
These symptoms include fatigue, irritability, insomnia, tension, and difficulty concentrating. As such, it may be difficult for physicians to identify a clinical anxiety disorder in the postpartum period.
Second, unlike postpartum depression, there is no official postpartum anxiety definition within the “Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition” (DSM-5), which is the handbook of the American Psychiatric Association used by healthcare professionals to diagnose mental health conditions.
Currently, the DSM-5 specifier (a diagnosis extension used to clarify a disorder) “with peripartum onset” can only be used for mood disorders, such as depression, and not for anxiety disorders.
The lack of criteria in the DSM-5 makes it difficult to categorize postpartum anxiety as generalized anxiety disorder (GAD), especially since a GAD diagnosis requires a history of six months of symptoms.
A person who develops anxiety in the postpartum period may not have this history. Therefore, some researchers encourage clinicians to diagnose postpartum anxiety if the criteria for GAD have been met over a one-month period instead.
Third, there has been an under-recognition of anxiety disorders within the peripartum and postpartum populations. This means that anxiety, specifically among people who are pregnant or who have recently given birth, is not well-researched. As a result, there are no anxiety screening tools available that are designed specifically for the postpartum population.
The State Trait Anxiety Inventory (STAI) is a general screening tool for anxiety that has been studied for use in the postpartum population. Research indicates that this tool can accurately diagnose postpartum anxiety with screening at both four and eight weeks postpartum.
A psychological interview, or conversation with your doctor, may also be used to diagnose postpartum anxiety. Your doctor will ask you questions to determine if your anxiety is causing significant distress or is functionally limiting (inhibiting your ability to perform normal activities) and meets the DSM-5 criteria for an anxiety disorder.
Causes
Like all anxiety disorders, there is not a clear cause and effect for postpartum anxiety. Additionally, there is a lack of research on the causes of postpartum anxiety.
Neurobiological research has found both similarities and differences in brain activity between postpartum anxiety and anxiety in the general population. This may indicate that there is a different set of causes for postpartum anxiety.
In some cases, the natural stressors of the perinatal period may contribute to developing postpartum anxiety. Normal worries and fears around the baby’s well-being, the mother’s well-being, the partner’s well-being, and more all have the potential to grow out of control.
When these worries become persistent and lead to functional impairment (the inability to carry out certain activities in your daily life), postpartum anxiety may be diagnosed.
Unlike anxiety among the general population, pregnancy-related hormonal changes may also contribute to postpartum anxiety. One theory is that postpartum estrogen withdrawal may lead to anxiety.
During pregnancy, estrogen levels increase significantly and then rapidly drop to below prepregnancy levels after childbirth and throughout the postpartum period.
This theory was supported by a 2016 study using mice and a 2020 study using hamsters. However, human studies still need to be performed to draw decisive conclusions.
Treatment
Despite postpartum anxiety’s potentially having different causes than anxiety in the general population, it typically is treated in the same way. However, in choosing a treatment plan that is right for you, your doctor should take into consideration your postpartum status, including whether you are breastfeeding.
Psychotherapy
Cognitive behavioral therapy (CBT) is the first-line treatment for mild and moderate postpartum anxiety. Mindfulness training and relaxation techniques also are effective treatments for lowering anxiety levels and symptoms in the postpartum population.
Medication
Medication typically is a second-line treatment for postpartum anxiety and is used in moderate to severe cases. This is due to the possibility of some drugs being transferred via breast milk to the baby.
Your physician will consider this when prescribing your medication and will usually start with the lowest possible dose before titrating up (raising the dosage gradually).
Medications used to treat postpartum anxiety include selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), buspirone, benzodiazepines, or tricyclic antidepressants. Of these, SSRIs are the most studied and frequently used during the peripartum and postpartum periods.
Risk Factors
There are various factors that may make a person more likely to develop postpartum anxiety. Risk factors include:
High perceived stress
Low partner social support
History of pregnancy loss
History of multiple births
Diagnosis of other anxiety or mood disorders
Family history of anxiety disorders
Early breastfeeding cessation
One 2016 study found that people at highest risk of developing postpartum anxiety are those who are multiparous (have previously given birth) and have an existing psychiatric history and high levels of stress from diverse sources.
Having multiple risk factors increases your chances of having postpartum anxiety, and this can include taking care of multiple children, including your newborn, during the postpartum period. Notably, a different study found that childcare stress, maternal self-esteem, and depression did not play a significant role in postpartum anxiety.
Coping
Take comfort in knowing there are good reasons for experiencing feelings of postpartum anxiety. First, realize that caring for a new baby is hard, and there is nothing you did to cause your postpartum anxiety.
Here are some ways you can cope with your postpartum anxiety:
Talk to your partner, friends, and family about your worries and need for support.
Balance caregiving duties equally with your partner or a loved one.
Recruit family members or babysitters to help.
Join a support group of new parents, many of which can be found online.
Try to maintain a balanced diet, which is possible through batch cooking, meal delivery services, and more.
Engage in mindfulness and relaxation practices, such as clinical aromatherapy or yoga.
A Word From Verywell
Coping with caring for a new baby and all the life changes your baby brings can be worrisome. For some people, these worries may manifest in postpartum anxiety. If you are struggling with excessive fears, intrusive thoughts, insomnia, and physical symptoms such as muscle tension, dry mouth, nausea, and more, then you may have postpartum anxiety.
While it is normal to feel anxious after childbirth, it is not normal for these worries to take over your life. Talk to your doctor about postpartum anxiety and the treatments that are available to you.
Source link
0 notes
Text
Learn about service of Chemical Dependence
Identifying a medication dependency (" material use disorder") needs a thorough examination and also frequently includes an evaluation by a psychiatrist, psycho therapist or qualified alcohol as well as medication professional. Laboratory tests, such as blood or pee examinations, are utilized to evaluate substance abuse, but they can not detect dependency. Nevertheless, Chemical Dependency Treatment Near Me can be utilized to manage it.
Diagnosis
You certainly wish to know about What Is Nicotinamide Adenine Dinucleotide. For the medical diagnosis of a compound use disorder, many psychological wellness experts use the requirements of the Diagnostic as well as Statistical Handbook of Mental Illness DSM-5
Treatment
Although there is no remedy for drug dependency, the Chemical dependency treatment options described below can aid you get over a dependency and also keep you far from drugs. The therapy you receive will rely on the medications you take and the associated psychological or medical disorders you might have. Lasting follow-up is essential to prevent relapse.
Chemical dependency treatment programs
Therapy programs generally provide the following:
Household, group or individual treatment sessions
Concentrate on comprehending the nature of addiction, quit utilizing drugs and protect against relapse
Degrees of care as well as locations that differ according to your requirements, such as outpatient, domestic as well as inpatient programs Detoxing
The objective of detoxing, additionally called "removal of contaminants" or "withdrawal therapy," is to permit you to stop using the addictive drug as rapidly and also safely as feasible. For some people, it may be safe to undergo Post Traumatic Stress Disorder Treatment. Others may need admission to a hospital or domestic treatment facility.
Abstinence from various categories of medicines, such as antidepressants, stimulants or opioids, produces different side effects and also requires different techniques. Detoxification may be composed in the gradual decrease of the dose of the drug or short-lived replacement by other materials, such as methadone, buprenorphine or a combination of buprenorphine and naloxone.
Opioid overdose
When a case of opioid overdose happens, the emergency group or, in some states, any person who witnesses an overdose can administer naloxone (an opioid villain). Naloxone turns around the results of opioids temporarily.
While naloxone has actually been on the market for many years, administration systems such as Narcan (a naloxone nasal spray) as well as Evzio (a naloxone injection gadget) are currently available, although they can be really costly.
Evzio is a little shot device that overviews the customer through voice instructions and immediately presents the needle into the thigh to use the naloxone shot. Regardless of the technique of administration, look for instant clinical attention after making use of naloxone.
Behavior modification
As part of a treatment program for medicine addiction, you can conduct behavioral therapy - a kind of psychiatric therapy - with a psycho therapist or psychoanalyst, or obtain mental counseling from an accredited alcohol and also medication therapist. Treatment and also psychological therapy can be private, group or family. The specialist or counselor can:
Assist you to get ways to face your compulsion to medications
Suggest methods to avoid medications and also avoid relapse
Offer pointers on just how to treat a regression, if it occurs
Speak about problems connected to your job, your legal issues and also your connections with family and friends
Include relative to aid them acquire better interaction skills as well as give assistance
Address other mental health problems
#Chemical Dependency Treatment Near Me#Chemical dependency treatment#Post Traumatic Stress Disorder Treatment
0 notes
Text
What Is PMDD – Symptoms and Treatments for Premenstrual Dysphoric Disorder
The (incredibly sexist) joke about premenstrual syndrome (colloquially PMS) is that it drives people to do mean, crazy things. But if you've ever had PMS yourself, you understand.
youtube
There are few things more disorienting than watching your body inflate every month with water retention, or having agonizing headaches for a week just because your period is coming. So yeah, maybe it makes you a little mean. But wouldn't anyone who feels like shit half of every month be mean, too? (Yes.)
A small percentage of people who menstruate feel this even more, and have something called premenstrual dysphoric disorder (PMDD), which is essentially an extreme version of PMS that comes with symptoms similar to clinical depression. Like PMS, PMDD is tied to the menstrual cycle. But unlike PMS, PMDD is severe enough that it has a negative effect on your school/work life, your personal life, and your general ability to function in the two weeks before your period starts.
Two specialists, Dr. Shari Lusskin, a clinical professor of psychiatry, obstetrics, gynecology and reproductive science at Mount Sinai's Icahn School of Medicine, and Dr. Alexandra Sacks, a reproductive psychiatrist in New York City, explained what makes PMDD so bad, and what a doctor looks for when diagnosing it.
What causes PMDD
Like most disorders related to women's health, doctors aren't yet totally sure what causes PMDD, though Sacks said it's certainly something researchers are interested in. The leading theory is that it's rooted in a sensitivity to the natural hormone fluctuations that occur during the menstrual cycle.
"In women who have PMDD, the hormone changes in their menstrual cycle may impact their serotonin levels, which is a chemical in the brain that your brain cells use to regulate all sorts of physical, emotional and behavioral experiences but includes mood, attention, sleep [and] pain," Sacks said.
Per the theory, your hormones and brain are connected by a system called the hypothalamic-pitutiary-gonadal axis, and through this system, hormonal fluctuations produced by the ovaries (part of a normal menstrual cycle) impact the hypothalamus and pituitary areas of the brain, which impacts mood. Sacks clarified that women with PMDD don't necessarily have high or low levels of hormones or any physical problems with their ovaries — it's more a matter of how sensitive your body is to the levels of hormones present.
PMDD vs. regular PMS
According to a 2018 study in Clinical Obstetrics and Gynecology, about three to eight percent of menstruating women meet the diagnostic criteria for PMDD. It was added to the DSM-5, a handbook used by medical professionals to diagnose mental health disorders, in 2013. "This gave it much greater legitimacy for the millions of women who were suffering worldwide," Sacks said. "And it just speaks to the importance of how much more research is needed in the field of women's mental health."
Lusskin said "up to 80 percent of women have premenstrual syndrome" and experience mood and body changes (like bloating and breast tenderness). "But they don't meet the criteria for PMDD, which is defined as having at least thirty percent worsening — you have to have a significant decrease in mood with a substantial impact on functioning."
The symptoms for PMDD are similar to those of PMS, but more severe. Sacks said to officially diagnose someone with PMDD, a doctor will look for five or more combined emotional, physical, and behavior symptoms. These are things like mood swings, anxiety, a feeling of hopelessness, trouble concentrating, change in appetite, trouble sleeping or oversleeping, breast tenderness or swelling, bloating, et cetera. And they should be severe enough that they impact your day-to-day function when you're experiencing them.
PMDD vs. clinical depression
If the symptoms of PMDD look familiar it's because they are. Part of what makes PMDD tricky to diagnose is that it so closely resembles other mental disorders, particularly clinical depression and anxiety. Lusskin said the key difference between PMDD and general mood disorders is that PMDD is linked to the menstrual cycle and symptoms don't persist all month long. For a PMDD diagnosis as opposed to clinical depression, doctors look for symptoms that start around the time of ovulation (about two weeks after the first day of your period) and subside shortly after your next period starts, according to Lusskin.
To identify a pattern, Lusskin said your doctor will ask you track your symptoms in real time instead of retrospectively, when it's easy to point at any symptoms you were having and blame them for the period that you know showed up three days later. What the doctor is looking to rule out is symptoms that last all month long but get worse around the time of your period, which would technically be something more like depression or panic disorder than PMDD.
Sacks said the doctor will look for symptoms that accompanied every menstrual cycle for the past year, but may only ask you track symptoms for two months in a row before making a diagnosis and starting treatment. They'll also ask about medical history (to rule out other mood disorders) and ask about any recent changes in birth control.
"You really want to see this as a pattern in your life not impacted by anything else — not other conditions or medications," Sacks said. If it seems that your symptoms only started showing up or got worse around the time you switched birth control medication, your doctor will offer the option of switching to a different contraceptive before diagnosing with PMDD.
Is it Normal to Feel Sad After Sex?
Treating PMDD
Even though the symptoms are similar, differentiating between PMDD and depression or PMS is important because the treatment options are subjective to each condition. Like depression, PMDD is also often treated with an SSRI. But unlike depression, a doctor might suggest you only take an SSRI during the two weeks of the month that your symptoms appear for PMDD, while someone with depression takes an SSRI continuously.
There's also a difference in how quickly the SSRI kicks into action. "SSRIs have a quick onset of action for PMDD, within one to two days," Lusskin said. "Whereas it takes up to six or eight weeks to get a response for depression." The research on this is still being conducted, but medical professionals believe this quick action has something to do with the fact that SSRIs can impact how progesterone and estrogen impact mood. Researchers believe PMDD is a hormonal sensitivity, so this would make sense.
It may also help to level out hormonal fluctuations. Another common treatment option is to prescribe the birth control pill Yaz, which has been shown in clinical studies to reduce symptoms of PMDD because, unlike most other contraceptives, it contains drospirenone (a synthetic version of the hormone progesterone). Yaz also targets another hormone that works as a diuretic and therefore helps to reduce some of the physical symptoms of PMDD, like water retention that causes bloating.
Sacks added that your doctor may also suggest talk therapy and lifestyle approaches, like increasing exercise, decreasing alcohol and drug use, decreasing caffeine and sugar intake, and just generally eating and acting healthfully (which feels incredibly counterintuitive when you're depressed, but c'est la vie).
The important thing to not about treatment for PMDD is that it's highly individualized. While there isn't a cure, per say, treatment can help some women feel much more "normal" leading up to their period, so to speak. Which is just to say that, if you think you're experiencing PMDD, you should absolutely bring it up with your doctor. Whether it's PMDD or something else (like depression or another mood disorder) there's almost certainly something that can be done to help you feel less "meh."
And if you ever experience severe thoughts of hopelessness or feel suicidal, whether it's in the two weeks before your period or at any time during the month, don't wait to set an appointment with your doctor. You can call 9-1-1 or the National Suicide Prevention Lifeline 24/7 at 1 (800) 273-8255. You can also text the Crisis Text Line anytime at 741741.
Source
http://cosmopolitan.com/sex-love/a18735059/pmdd-symptoms-treatment-facts/
0 notes
Text
Wait, what? (Vol. I)
One of the most confusing parts of parenthood is that we have to navigate several professional worlds outside our own to gain access to what our children may need: educational, medical, health, legal... it’s enough to make you go home and crack open a Bota Box.
Here’s a handy primer of jargon and acronyms (we special ed teachers especially LOVE jargon, and I apologize on my people’s behalf). Bookmark this one and remember that language should NEVER be a barrier in your involvement in decision making for your child. An additional rule of thumb: please never be afraid to ask what something means. You don’t look dumb and you aren’t bothering anyone; you sound mature and curious. Promise.

THE WELL INFORMED MAMA’S GLOSSARY, VOL. I (504 – A)
504 Plan: Section 504 is a federal law that prohibits discrimination and provides for accommodations for any documented disability which affects a life function. Sometimes this is a very good idea, indeed; sometimes, it’s a consolation prize when a Team decides against an IEP. It does not have the “specialized instruction required” piece of an IEP. As in: “Johnny’s 504 gives him extended time on assessments because of his processing speed.”
AAC: Augmentative and Alternative Communication – This includes any alternative means to oral communication, namely speech devices (aligning visuals to “speak” from a computer, often handheld) and PECS (picture communication – more to follow on that one for sure). We see this most often in autism and in apraxia. This is a huge topic but please remember that taking away someone’s “talker” (speech device) is the same as covering a speaking person’s mouth with tape. Not OK. As in: “My son used his AAC device to request he stay home from school and watch Octonauts.”
ABA: Applied Behavior Analysis - An evidence based, systematic, frequent therapy that individuals with autism (or anyone who wants to modify behavior or increase communication) may access. The “client” is exposed to programs that build tolerance, add desirable behaviors, or decrease unsafe or nonfunctional behaviors, for example. It’s the only recognized “treatment” for autism and is mandated by law to be covered by insurance (thanks, Autism Speaks). As in: “Sorry I can’t make it to playgroup, we have ABA today. And tomorrow. And the next day.”
ABS: Adaptive Behavior Scale - aka “The Vineland” - This is the assessment your Early Intervention specialist busts out to rank and file your baby; a necessary evil I suppose. They use observation, interaction using specifically mapped out questions/tasks, and talking to mom and dad to score your little one in four “domains” (skill areas): Communication, Daily Living Skills, Socialization, and Motor Skills. As in: “Bobby didn’t qualify for EI this year because her scores on the ABS were typical.”
Accommodations: A change in the way something is presented (presentation, time or setting, response) that does not change the intention of what is being taught. In other words, it changes how we teach, not what we teach. Good accommodations level the playing field and are NOT an advantage. Some are universal (or should be) and some need to be in an IEP or 504 plan. As in: “If these gen ed teachers don’t give Sally her accommodations on her quiz again, I’m going to lose my shit.”
Advocate: 1. One who does her homework in order to be the voice of someone she loves. 2. Someone we pay when we are too exhausted or enraged to carry on effectively. As in: “That girl advocates like a mother.”
ADHD: Attention Deficit Hyperactivity Disorder – this used to be either ADD or ADHD; now it’s all officially ADHD and then you get a “type” as a bonus prize – hyperactive, inattentive, or combined. In Massachusetts, for example, ADHD is actually listed under health impairment on the IEP as a disability category, and you really want a pediatrician or psychologist to deliver this diagnosis even with school-based testing (more on that later). Kids with ADHD are among my favorite humans: buzzy, busy, dreamy, kinetic, original. They need help. That’s fine, but you’ll often find they’re brilliant, too. As in: “That kid with ADHD in Sally’s class sits on a yoga ball instead of a chair.”
APE: Adapted Physical Education – Adapted or modified PE/gym, including the use of assistive equipment or a different curriculum, so that a student with a gross motor disability or a developmental delay can take PE. There are different levels of qualifications to teach APE and how it all works varies from state to state. I’m learning more about this myself right now. As in: “We may need to put APE in his IEP.”
Apraxia: Apraxia of Speech – This is a disorder in which the brain sends incomplete signals to the mechanical parts of the body that “do the talking.” Apraxia has no bearing on cognitive capacity (intelligence) so always assume competence when interacting with a person with apraxia. Some will move on from apraxia with intensive speech therapy; some will not. Many will end up seeking AAC. As in: “A child with apraxia still has something to say.”
Articulation: aka “artic” – The understandability or clarity of speech. Completely separate from receptive language. May include consonant confusion, dropped syllables, lisps, or mumbling. Many kids with speech delays who learn to speak later than is typical, and kids with frequent ear infections, have artic issues. As in: “Henry’s articulation is a mess, but his vocab is on point.”
ASD: Autism Spectrum Disorder(s) - This the formal name for an autism diagnosis in the official medical handbook DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition), which saw big changes in 2013. (For the record, I take issue with “disorder,” but I’ll get into that later.) It covers a wide range of presentations of autism, a developmental and neurological difference, that used to be differentiated into categories like PDD-NOS (Pervasive Developmental Delay - Not Otherwise Specified in very young children) and Asperger’s (now classified as “high functioning autism” - also problematic, but that’s that). Side note – autistic is not a dirty word or dehumanizing descriptor, and one instance where people-first language is not a must. As in: “My ASD/autistic kiddo ate a vegetable this one time.” Now, importantly, in education, autism does not apply as a disability category if a child’s educational performance is adversely affected primarily because the child has an emotional disturbance, but a mental illness can be co-morbid with autism. (Confused? That’s OK. I got you. Stay tuned.)
ASL: American Sign Language - its own language and culture for a subset of deaf Americans; the signs are also used by some in the nonverbal community to communicate, and sometimes simplified for little ones. Signing in infancy and toddlerhood can help prompt language later on. As in: “Noah signs ‘more’ when we tickle him because he is an adorable baby-god.”
Asperger’s Syndrome: The name for a specific type of autism that medical professionals now call “high functioning autism.” This one is chock full of problematic assumptions about really cool, deeply neurodiverse and aware individuals. Many are verbal, but not all, and many feel challenged by social nuances or other communication demands. It may also encompass sensory sensitivities or executive functioning deficits. Or not. Many proudly call themselves “Aspies” and were diagnosed prior to the 2013 DSM-5 update. As in: “Will Big Bang Theory ever tell us outright if Sheldon has Asperger’s?”
AT: Assistive Technology - Any tool, electronic device or hardware, or any software, that helps a student access learning by removing barriers to access. Assistive tech includes communication devices, speech to text and text to speech programs, word prediction software, simply using a Chromebook to type, using an iPad or other tablet to submit work, audiobooks from Learning Ally, and much more. The possibilities are exciting, and can be a little tricky, too. You can request an AT evaluation from a public school just like any other assessment (tip: say eval and not consult). As in: “Hank’s plan has assistive tech. He needs to turn in his worksheets digitally or no one can read his handwriting.”
Auditory Processing Disorder: FYI, nobody really says “APD,” they say “auditory processing.” May also be called “Central Auditory Processing Disorder,” and then we do frequently use CAPD as an acronym. Anyhoo, this is a hearing issue that affects the way kids experience the world and learn, because it makes processing auditory information very challenging. They can hear, but have trouble telling the difference between sounds. Requires speech therapy and sometimes seeing an audiologist for medical intervention. Can frequently be mislabeled as ADHD. As in: “Billy’s not being fresh; he’s not following the conversation because he has auditory processing disorder.”
To be continued…
0 notes
Text
What every parent needs to know about 'gaming disorder'
yahoo
Video game addiction is a term that has been used for years by parents and mental health professionals who believe that it’s a real disorder. Now, there’s more weight behind their argument: The World Health Organization (WHO) has including “gaming disorder” as a new mental health condition listed in the 11th edition of its International Classification of Diseases.

Your child may love video games. But how do you know if he or she is addicted? Photo: Getty Images.
According to WHO, there are three major criteria for the diagnosis of gaming disorder: Gaming takes precedence over other activities so much that a person often stops doing other things, a person continues gaming even when it causes issues in their life or they feel that they can’t stop, and gaming causes significant distress and impairments in a person’s relationships with others, as well as their work or school life. If your child gets sucked into a game for a few days, but goes back to normal after that, they wouldn’t qualify: Instead, people must engage in this behavior for at least 12 months, WHO says.
It’s worth noting that WHO’s stance on gaming addiction is different from that of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the handbook used by health professionals in the U.S. and other countries to help diagnose mental health disorders. The DSM-5 calls out “Internet Gaming Disorder” but says it’s a condition that warrants more clinical research and experience before it can be classified in the book as a formal disorder.
WHO says on its website that all people who participate in gaming should be aware that gaming disorder is a real condition, and that it’s important to be mindful of how often they play video games. However, they also point out that gaming disorder only affects a small amount of people who game.
It’s only natural that the news would make you give your child’s gaming system the side-eye.
In general, parents should limit the amount of screen time their children have daily, and gaming is included in that, along with TV, computers, phones, and tablet use, Gina Posner, MD, a pediatrician at MemorialCare Orange Coast Medical Center in Fountain Valley, Calif., tells Yahoo Lifestyle.
Screen time isn’t recommended at all for kids who are 18 months or younger, but for children who are older than that up to five, it’s generally recommended that they have not more than one hour of screen time, she says. For those who are six and up, it’s more at the parents’ discretion. “The maximum amount of screen time should be two hours a day, but less is always better,” Posner says.
Posner says that it’s important to set clear limits for your child when it comes to screen time and gaming. For example, say that your child has to do their homework first and/or get out and play for an hour before they’re allowed to game. And even then, make it clear that they’re only allowed to do so for a set period of time.
If your child starts fussing when they’re not allowed to be gaming all day, it’s a clear sign that you need to cut back, Posner says.
Treatment for gaming disorder is generally based in cognitive behavioral therapy, which would generally be done in two phases, Simon Rego, PsyD, chief psychologist at Montefiore Medical Center/Albert Einstein College of Medicine, tells Yahoo Lifestyle. The first is raising awareness for your child that their gaming is a problem, and looking for triggers and cues that could make the gaming habit better or worse. A mental health professional would also address problematic thoughts associated with either stopping playing or the thoughts that keep them gaming, he says.
The goal then is to step down the behavior from something that’s pathological to problematic, and then being able to manage it in a “reasonable way,” Rego says. People don’t necessarily have to quit gaming altogether, but they do need to learn to better manage it with parameters, like only gaming with friends during select times during the day vs. doing it at night alone in their room.
If you suspect that your child has a gaming disorder, it’s important to seek help for it.
Just know that this is still a new diagnosis and you may need to do some sleuthing to find someone who specializes in this kind of behavior.
Read more from Yahoo Lifestyle:
Here’s what happens during a home birth, like the one of James Van Der Beek’s wife
Little boy grows hair long just so he can donate it, regardless of gender stereotypes
Shop 16 floral summer wedding dresses just like Meghan Markle’s
Follow us on Instagram, Facebook, and Twitter for nonstop inspiration delivered fresh to your feed, every day.
#news#_revsp:wp.yahoo.style.us#psychology#mental health#gaming disorder#_author:Korin Miller#health#_uuid:e033c674-445c-381a-b8be-c95a2233aa81#_lmsid:a0Vd000000AE7lXEAT#WHO#DSM#video games
0 notes
Text
Clinical Formulations of Histrionic PD
Clinical formulations and case conceptualisations are introduced in this post.
These are all generalisations and theories of how HPD develops, not something that is supposed to be true for everyone with HPD.
Psychodynamic model
Histrionics lack relationships with maternal caregivers so turn to paternal caregivers for love and attention
Learn that they can get attention through sexualised behaviours
Men with HPD may be hypomasculine (effeminate) or hypermasculine if their paternal caregiver is emotionally unavailable
Biosocial model
Mood swings, very emotional
Biggest influences are environmental: caregivers’ reinforcement of attention-seeking & manipulative behaviours and histrionic role models
Children learn they can use cuteness, charm, attractiveness & seductive behaviours to get what they want/need (attention from caregivers)
Histrionics are externally focused and largely ignore their internal worlds
Histrionic behaviours are self-perpetuating
Cognitive-Behavioural model
Two main underlying assumptions: “I am inadequate and unable to handle life by myself” and “I must be loved by everyone to be worthwhile.”
Need attention and approval from others, and in a similar way to DPD feel they are inadequate to look after themselves and need others
Hypersensitive to rejection & criticism (similar to DPD, NPD and AvPD)
Feel they must perform for others to gain approval and self-esteem
Thinking is “impressionistic, global, and unfocused” and leads to over-generalisation, emotional dysregulation, and splitting
Two subtypes:
The controlling type, who tries to gain control through dramatics and manipulation; they struggle with reading others’ emotions and are shallow, self-centred, and uncomfortable without immediate assurance; lack empathy.
The reactive type tries to gain approval and reassurance.
Interpersonal model
People with HPD learnt that their entertainment value and appearance was more important to others than their worth as a person
Learnt that physical appearance and charm can be used to manipulate others
Their childhood homes were unpredictable and probably involved substance abuse
The unpredictability was dramatic and interesting (unlike the “primitive” and life-threatening chaos associated with BPD)
Histrionics were likely rewarded (i.e. had their physical and emotional needs met) for their disabilities, illnesses and complaints
Histrionics “exhibit a strange fear of being ignored, together with a wish to be loved and taken care of by important others, who can be controlled through charm or guile.”
Integrative model
Histrionics experience reactive mood swings and have high levels of energy
They are hyper-responsive and externally oriented
“The self-view of the histrionic will be some variant of the theme “I am sensitive and everyone should admire and approve of me.” The world-view will be some variant of “Life makes me nervous so I am entitled to special care and consideration.” Life goal is some variant of the theme “Therefore, play to the audience, and live in the moment.””
Cargivers’ style based in reciprocity, i.e. “I’ll give you attention if you do what I want”, with minimal or inconsistent discipline and probable neglect
Internal experiences of HPD are “denial of one’s real or inner self; a preoccupation with externals; the need for excitement and attention-seeking, which leads to a superficial charm and interpersonal presence; and the need for external approval. This, in turn, further reinforces the dissociation and denial of the real or inner self from the public self, and the cycle continues.”
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#clinical formulations#case conceptualisations#case conceptualisation#hpd#hpd info#pd info#dogpost#len sperry#handbook of diagnosis and treatment of dsm-5 personality disorders#this has been in my drafts for 10 months LOL#also re reading this its like 'people w hpd were neglected and so they try to get their needs met thru trying to get ppl to love them#which is OBVIOUSLY manipulative and selfish right?? /sarcasm#personality disorder concepts
49 notes
·
View notes
Text
Results! So in order of most to least common, we have:
Borderline PD (31%)
Avoidant PD (25.8%)
Schizoid PD (17.3%)
Narcissistic PD (7.4)
Schizotypal PD (5.2%)
Paranoid PD (3.7%)
Obsessive-Compulsive PD (3%)
Dependent PD (2.6%)
Histrionic PD (2.2%)
Antisocial PD (1.8%)
271 people participated, so we had 81 people with BPD compared to 4 people with AsPD.
I'm surprised that AvPD is so high in the poll, but even more surprised that SzPD came in third.
So how does this compare with Actual Academic Studies?
The most recent estimates given in the DSM-5-TR are *:
BPD: 2.7% - very dissimilar, a huge 28.3% difference
AvPD: 2.1% - very dissimilar, a huge 23.7% difference
SzPD: 1.3% - very dissimilar, a huge 16% difference
NPD: 1.6% - pretty dissimilar, a 5.8% difference
StPD: 0.6% - pretty dissimilar, a 4.6% difference
PPD: 3.2% - fairly similar, only a 0.5% difference
OCPD: 4.7%, fairly similar, a 1.7% difference
DPD: 0.4% - fairly similar, a 2.2% difference
HPD: 0.9% - fairly similar, a 1.3% difference
AsPD: 3.6% - fairly similar, a 1.8% difference
So their prevalence order is: OCPD -> AsPD -> PPD -> BPD -> AvPD -> NPD -> SzPD -> HPD -> StPD -> DPD.
Interestingly we have the top 3 being very dissimilar to the DSM rates, in the middle with NPD & StPD being not either very similar or dissimilar, and the final five being fairly similar.
Why are this poll's results so different in some places and similar in others? I'm not a psychiatric researcher so I don't know the ins and outs of epidemiology, so I can only guess that more people with BPD, AvPD & SzPD follow me than people with other PDs! Also important to note that this poll included self-diagnosis, and had a small sample size (and obviously didn't do any screening or whatnot). Not to mention clinical diagnosis bias in PDs (HPD, NPD, AsPD & BPD in particular).
[* cited from Morgan, T. A. & Zimmerman, M., 'Epidemiology of Personality Disorders', in Handbook of Personality Disorders: Theory, Research, and Treatment, 2nd Edition. New York, Guilford, 2018, pp. 173–196]
This poll is inclusive of self-diagnosis.
#dogreblog#personality disorders#antisocial personality disorder#avoidant personality disorder#borderline personality disorder#dependent personality disorder#histrionic personality disorder#narcissistic personality disorder#obsessive compulsive personality disorder#obsessive-compulsive personality disorder#paranoid personality disorder#schizoid personality disorder#schizotypal personality disorder#dogpoll#epidemiology
54 notes
·
View notes
Text
Personality Disorder Concepts: Defining Characteristics
These are the defining characteristics of PDs, each of which are different depending on the PD in question.
Triggering event(s).
The situations that trigger a maladaptive response that is reflected in the person’s behavioral, interpersonal, cognitive, and affective styles. Triggering events can be intrapersonal (e.g. failing an exam), or interpersonal (e.g. being criticised).
ASPD: Social standards and rules.
AVPD: Close relationships; being social/in public.
BPD: The expectation of meeting goals; maintaining close relationships; real or imagined abandonment.
DPD: The expectation that they can rely on themselves; being alone.
HPD: Relationships, particularly with those they're attracted to.
NPD: Self-evaluation, either by themselves or others.
OCPD: Unstructured situations; meeting other’s standards (in all aspects of life: work, family, etc).
PPD: Close relationships; personal questions.
STPD: Close relationships.
SZPD: Close relationships.
Behavioral style
The way in which the person reacts to a triggering event.
ASPD: Impulsive, irritable, aggressive; irresponsible and struggles to keep commitments; relies on themselves, uses cunning and force; risk-taking and thrill-seeking.
AVPD: Tense and self-conscious; controlled speech & behaviour; appear apprehensive and awkward; self-criticising and overly humble.
BPD: Self-damaging behaviours (self-harm, self-sabotage, suicidal ideation); aggression; achieve less than they could (e.g. in work or school); chronic insomnia & irregular circadian rhythms (”body clocks”); feel helpless & empty void.
DPD: Docile, passive, non-assertive, insecure, and submissive; doubts themselves & lacks self-confidence.
HPD: Charming, dramatic, expressive; demanding, self-indulgent, inconsiderate; attention-seeking, mood swings, impulsive, unpredictable, and superficial.
NPD: Self-centred, egotistical, self-assured; dominates conversations; seeks approval and attention; impatient, arrogant, hypersensitive.
OCPD: Perfectionists; workaholics; dependable, stubborn, possessive; indecisive, prone to procrastination.
PPD: Always tense and hypervigilant; defensive, argumentative, guarded.
STPD: Eccentric, bizarre; strange speech; struggles with work and school and often become drifters and wanderers; avoids long-term commitment and looses touch with society’s expectations; dissociative.
SZPD: Lethargic, inattentive, eccentric; slow and monotone speech; rarely spontaneous; indifferent.
Interpersonal style
The way they relate to others.
ASPD: Deceitful; irritable, antagonistic and aggressive; disregards their and other’s safety; distrustful; lacks empathy; competitive.
AVPD: Sensitive to rejection; want acceptance but are too scared; withdraw and avoid when afraid; test people to see if they’re safe to interact with.
BPD: “Paradoxical instability”; splitting (idealise & cling vs devalue & dismiss); sensitive to rejection; “abandonment depression” & separation anxiety; superficial yet quickly developed and intense relationships; “extraordinarily intolerant” of being alone.
DPD: People-pleasers, self-sacrificing, clingy & needs reassurance; over-compliant & over-reliant on others; want others to be in control of their lives; avoids arguments; puts themselves down so they can receive the support of others; urgently seeks a new relationship when one ends.
HPD: Needs attention; flirtatious, manipulative; lacks empathy; overestimates intimacy of relationships.
NPD: Exploitative; self-indulgent; charming, pleasant & endearing; lacks empathy; irresponsible; jealous; needs approval and admiration.
OCPD: Very aware of social hierarchy; deferential to superiors and haughty to subordinates; polite and loyal; insist that their way is the right way to do things, because they are anxious to ensure perfection; stubborn; devoted to work which interferes with relationships.
PPD: Distrustful, secretive, suspicious, tend to isolate themselves and avoid intimacy; hypersensitive to criticism; bears grudges and blames others; reluctant to open up for fear of vulnerability.
STPD: Loners; socially anxious, apprehensive, suspicious and paranoid, which doesn’t fade as they get to know people; tends to live on the margins of society and relationships; often choose jobs with minimal social interaction that are usually below their skill level; indifferent to social norms.
SZPD: Aloof, loners, reserved, solitary; socially awkward; tend to fade into the background; happy to remain alone.
Cognitive style
How the person perceives and thinks about a problem and its solution.
ASPD: Impulsive; realistic; very aware of social cues; prone to executive dysfunction.
AVPD: Hypervigilant; distracted and preoccupied with their fears of rejection.
BPD: Inflexible (splitting) & impulsive; difficulty learning from the past; external loss of control leads them to blame others to avoid feeling powerless; emotions fluctuate between hope and despair; unstable self-image and fragmented sense of self; unable to tolerate frustration; brief psychotic episodes; dissociation; intense rage; difficulty focusing & processing information.
DPD: Suggestible and persuadable; optimistic, sometimes to the point of naïveté; uncritical; minimises difficulties and are easily taken advantage of.
HPD: Impulsive, dramatic; vague; suggestible; relies on intuition; avoids reflection and introspection as so to avoid realising their dependency on others; needs approval from others; has separate real/inner/private & constructed/outer/public selves; tendency to mimic speech patterns.
NPD: Focuses on feelings rather than facts; compulsive lying (to themselves as well as others); inflexible, impatient, persistent; superiority; unrealistic goals of success, power, ideal love.
OCPD: Rule & detail oriented; difficulty with prioritising; inflexible, unimaginative; conflicted between assertiveness & defiance vs obedience & pleasing people.
PPD: Mistrustful; hypervigilant; focuses on feelings (of paranoia) rather than facts; brief psychotic episodes; their need to find evidence for their paranoid suspicions gives them a tendency for authoritarianism.
STPD: Scattered; obsessive and tends to ruminate; superstitious, bizarre fantasies; vague ideas of reference (thinking things are about them when they’re not, e.g. someone laughing is directed at them) and magical thinking (thinking they caused something to happen by thinking about it); dissociative.
SZPD: Distracted; difficulty organising their thoughts; vague and indecisive; difficulty with introspection and reflection.
Affective style
How the person expresses and experiences emotions.
ASPD: Superficially expresses emotions; avoids emotions that will make them vulnerable; rarely feels guilt, shame or remorse; unable to tolerate boredom, depression, & frustration and needs stimulation.
AVPD: Shy & apprehensive; feels empty, sad, lonely & tense; depersonalisation.
BPD: Mood swings; inappropriately intense anger; feelings of emptiness, boredom, a “void”; emotional dysregulation.
DPD: Insecure & anxious; lacks self-confidence & fears being alone; fears abandonment & rejection; often sad or somber.
HPD: Displays intense, extreme emotions but may only feel them shallowly; sensitive to rejection; mood swings; need reassurance that they are loved.
NPD: Presents as self-confident and nonchalant; when criticised or rejected (”narcissistic injury”) they experience extreme shame which is often redirected into anger (”narc rage”/shame redirect); splitting; lacks empathy and so has difficulty with commitments.
OCPD: Somber, difficulty expressing feelings; avoids emotions that will make them vulnerable; comes across as stiff and stilted.
PPD: Cold, aloof, humourless; difficulty expressing feelings; tendency for anger and jealousy.
STPD: Cold, humourless, aloof; difficult to engage with; suspicious and mistrustful; hypersensitive; may react inappropriately for the situation or not at all.
SZPD: Humourless, cold, aloof; indifferent; lacks empathy; emotionally and socially distant; difficulty responding to other people’s feelings.
Temperament
The response pattern that reflects the person’s energy level, emotions and intensity of emotions, and how quick they react.
ASPD: Irresponsible, aggressive and impulsive.
AVPD: Irritable.
BPD: Passive (dependent subtype); hyperreactive (histrionic subtype); irritable (passive-aggressive subtype).
DPD: Low energy; fearful, sad or withdrawn; melancholic.
HPD: Hyperresponsive; needs attention from others.
NPD: Active and responsive; has special talents and developed language early.
OCPD: Irritable, difficult, anxious.
PPD: Active and hyperresponsive (narcissistic subtype); irritable (obsessive-compulsive and passive-aggressive subtypes).
STPD: Passive (schizoid subtype); fearful (avoidant subtype).
SZPD: Passive, difficulty experiencing pleasure and motivation (anhedonia).
Attachment style
Discussed in this post.
ASPD: Fearful-dismissing.
AVPD: Preoccupied-fearful.
BPD: Disorganised.
DPD: Preoccupied.
HPD: Preoccupied.
NPD: Fearful-dismissing.
OCPD: Preoccupied.
PPD: Fearful.
STPD: Fearful-dismissing.
SZPD: Dismissing.
Parental injunction
The expectation (explicit or implied) from caregivers for how the child should be or act.
ASPD: “The end justifies the means.”
AVPD: “We don’t accept you, and probably nobody else will either.”
BPD: “If you grow up, bad things will happen to me [caregiver].”; overprotective, demanding or inconsistent parenting.
DPD: “You can’t do it by yourself.”
HPD: “I’ll give you attention when you do what I want.”
NPD: “Grow up and be wonderful, for me.”
OCPD: “You must do/be better to be worthwhile.”
PPD: “You’re different. Keep alert. Don’t make mistakes.”
STPD: “You’re a strange bird.”
SZPD: “Who are you, what do you want?”
Self view
The way they view and conceptualise themselves.
ASPD: Cunning & entitled.
AVPD: Inadequate & frightened of rejection.
BPD: Identity problems involving gender, career, loyalties, and values; self-esteem fluctuates with emotions.
DPD: Pleasant but inadequate, fragile.
HPD: Needs to be noticed.
NPD: Special, unique and entitled; relies on others for self-esteem.
OCPD: Responsible for anything that goes wrong, so they must be perfect.
PPD: They're alone and disliked because they're different and better than others.
STPD: Different than other people.
SZPD: Different from others; self-sufficient; indifferent to everything.
World view
The way they view the world, others, and life in general.
ASPD: Life is dangerous and rules get in the way of their needs. They won’t be controlled or degraded.
AVPD: Life is unfair; even though they want to be accepted, people will reject them, so they'll be vigilant & demand reassurance; escapes using fantasies and daydreams.
BPD: Splits between people and the world as either all-good or all-bad, resulting in commitment issues.
DPD: Other people need to take care of them because they are unable to.
HPD: Life makes them nervous, so they need attention and reassurance that they're loved.
NPD: Life is full of opportunities; they expect admiration and respect.
OCPD: Life is unpredictable and expects too much, so they manage this by being in control and being perfectionists.
PPD: Life is unfair, unpredictable, demanding, and dangerous; they need to be suspicious and on guard against others, who are to blame for failures.
STPD: Life is strange and unusual; others have special magic intentions, so they are curious but also cautious when interacting with the world.
SZPD: Life is difficult and dangerous; if they trust no one and keep their distance from others, they won’t get hurt.
Maladaptive schema
Discussed in this post.
ASPD: Mistrust/abuse; entitlement; insufficient self-control; defectiveness; emotional deprivation; abandonment; social isolation.
AVPD: Defectiveness; social isolation; approval-seeking; self-sacrifice.
BPD: Abandonment; defectiveness; abuse/mistrust; emotional deprivation; social isolation; insufficient self-control.
DPD: Defectiveness; self-sacrifice; approval-seeking.
HPD: Approval-seeking; emotional deprivation; defectiveness.
NPD: Entitlement; defectiveness; emotional deprivation; insufficient self-control; unrelenting standards.
OCPD: Unrelenting standards; punitiveness; emotional inhibition.
PPD: Abuse/mistrust; defectiveness.
STPD: Alienation; abandonment; dependence; vulnerability to harm.
SZPD: Social isolation; emotional deprivation; defectiveness; subjugation; undeveloped self.
Optimal diagnostic criterion
One key criterion for each personality disorder, based on its ability to summarise all criteria for that PD, accurate description of behaviour, and the predictive value (ability to predict if the person has the PD or not).
ASPD: Aggressive, impulsive, irresponsible behavior.
AVPD: Avoids activities that involve being social out of fear of criticism, disapproval, or rejection.
BPD: Frantic efforts to avoid real or imagined abandonment.
DPD: Needs other people to be responsible for most major parts of their lives.
HPD: Uncomfortable not being the centre of attention.
NPD: Grandiose sense of self-importance.
OCPD: Perfectionism that interferes with life.
PPD: Paranoia, without evidence, that others are trying to harm, exploit or deceive them.
STPD: Thinking, speech, behavior, or appearance that is odd, eccentric, or peculiar.
SZPD: Doesn’t want or enjoy close relationships.
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#len sperry#handbook of diagnosis and treatment of dsm-5 personality disorders#dogpost#pd info#personality disorder concepts#cluster a#cluster b#cluster c#personality disorders#*reads this and is both reassured and hits home that im bpd & stpd*
555 notes
·
View notes
Text
Personality Disorder Concepts: Attachment Styles
Attachment is the “emotional bond” between a child and their caregiver. It’s relevant to personality disorders since it influences the child’s “capacity to form mature intimate relationships in adulthood”. It “influences and organizes motivational, emotional, and memory processes that involve caregivers”. Attachment is associated with “emotional regulation, social relatedness” and the “development of self-reflection and narrative”, all things that are impacted by personality disorders.
Attachment Styles
Attachment styles are made up of two dimensions:
the distinction between self and others
“valence”: positive vs. negative evaluation
Most people will exhibit more than one attachment style.
The five styles are:
secure: positive view of self and others
preoccupied: negative view of self, positive view of others
dismissing: positive view of self, negative view of others
fearful: negative view of self and others
disorganized: fluctuating positive and negative views of self and others
Preoccupied style: DPD, OCPD & HPD
Negative view of self (“a sense of personal unworthiness”)
Positive view of others
Tend to be very “externally oriented in their self-definitions”, i.e. look to others to define them
Dismissing style: SZPD
Positive view of self (“a sense of self that is worthy and positive”)
Negative view of others, which “typically manifests as mistrust”
See themselves as “emotionally self-sufficient”
See others as emotionally unresponsive
Therefore they “dismiss the need for friendship and contact with others”
Fearful style: PPD
Negative view of self and others
Expectation that others are untrustworthy & will reject them
Don’t trust themselves or others
Believe themselves to be “special and different”
Hypervigilant against threats and “unexpected circumstances”
Preoccupied-fearful style: AVPD
Negative view of self
Fluctuates between negative and positive view of others
Want to be liked and accepted but fear rejection and abandonment, so they avoid and withdraw
Fearful-dismissing style: ASPD, NPD, STPD
Fluctuates between negative and positive view of self
Negative view of others
See themselves as “special and entitled”
Acknowledge their need for others, as well as others’ potential to hurt them
Use others to meet their needs but are fearful and dismissing of them
Disorganized style: BPD
Fluctuates between negative and positive view of self and others
This style develops from trauma
Associated with dissociation & PTSD
Seems to shift among the other attachment styles
(More on disorganised attachment & dissociation)
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#pd info#attachment styles#disorganised attachment#its interesting that stpd is included with aspd & npd cuz i dont normally see those together but it makes sense#(esp as im stpd & considering if i have npd &/or aspd traits)#len sperry#dogpost#handbook of diagnosis and treatment of dsm-5 personality disorders#personality disorder concepts
265 notes
·
View notes
Photo
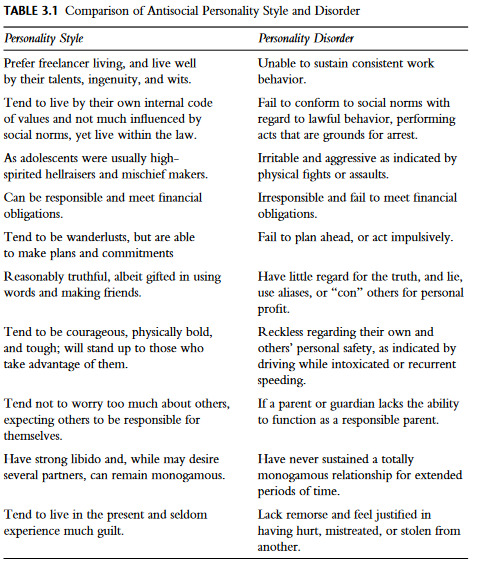
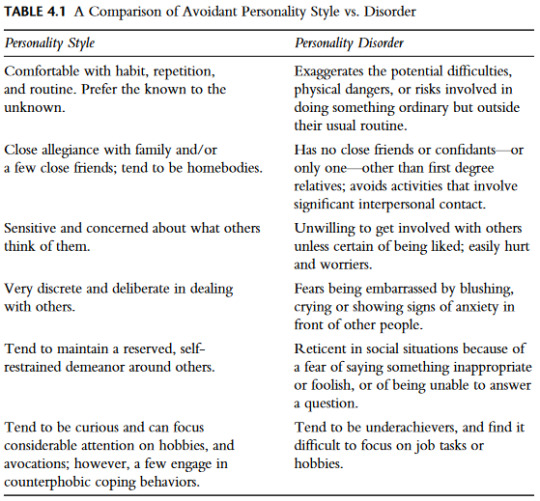
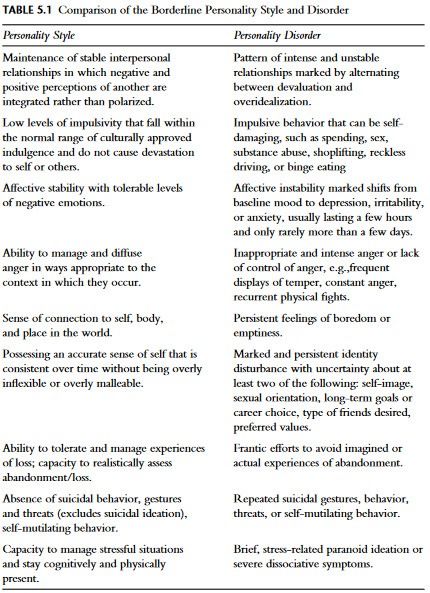
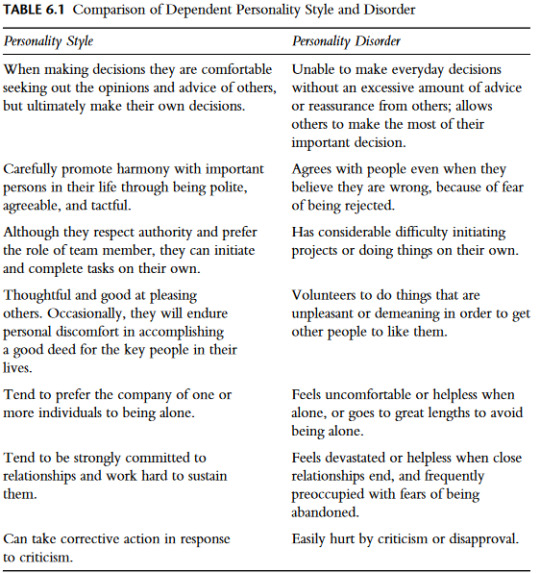
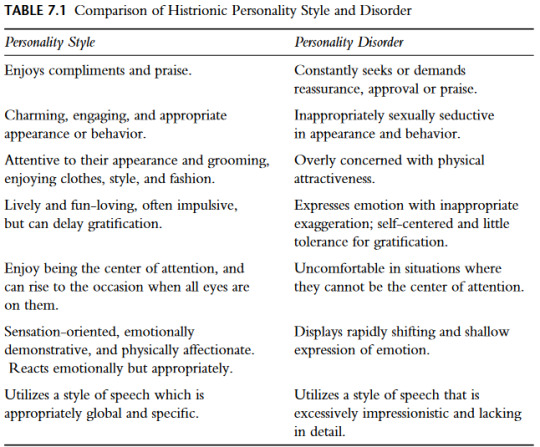
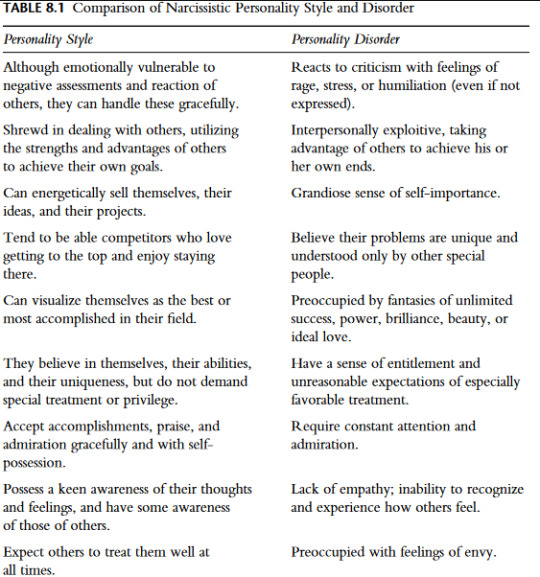
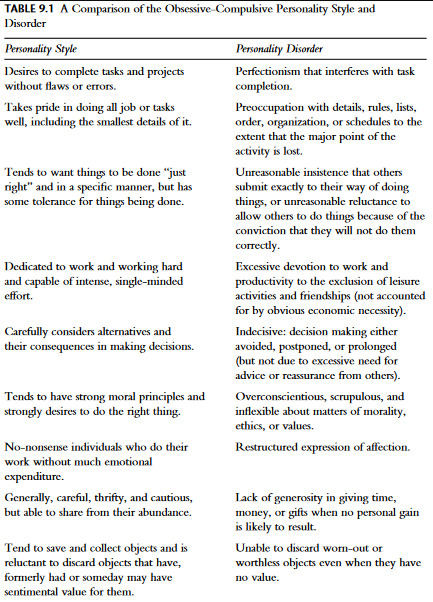
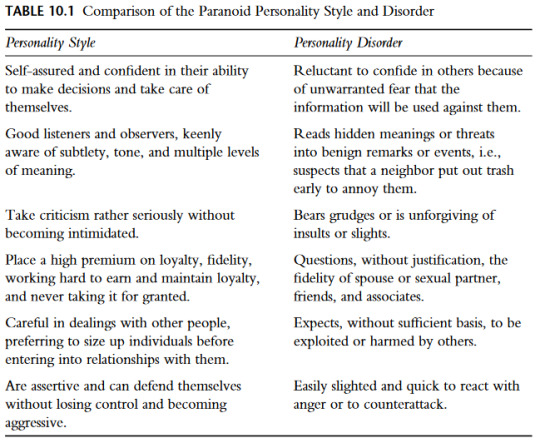
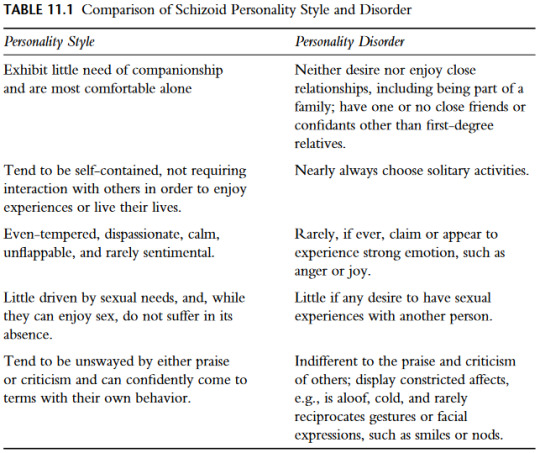
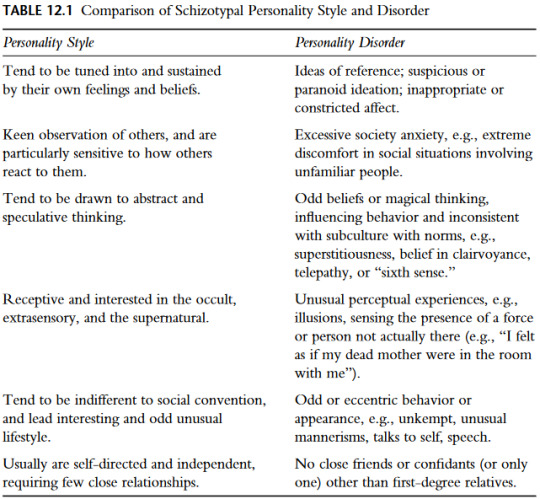
Comparison of Personality Styles vs Personality Disorders
- From Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders by Len Sperry (2016)
#putting them all in one post for ease#dogpost#pd info#len sperry#handbook of diagnosis and treatment of dsm-5 personality disorders#aspd#aspd info#avpd#avpd info#bpd#bpd info#dpd#dpd info#hpd#hpd info#npd#npd info#ocpd#ocpd info#ppd#ppd info#stpd#stpd info#szpd#szpd info#personality disorders vs styles
189 notes
·
View notes
Text
Clinical formulations of Avoidant PD
Clinical formulations and case conceptualisations are introduced in this post.
These are all generalisations and theories of how AVPD develops, not something that is supposed to be true for everyone with AVPD.
Psychodynamic model
Shyness, shame, withdrawal & avoidance are defense mechanisms against embarrassment, rejection, humiliation and failure
Shame & fear of vulnerability/exposure of the self to others are interconnected
Avoidants feel ashamed about their perceptions of themselves as weak, incapable, defective
Shame a result of childhood experiences, and not living up to their ideal self
Shame is a defense mechanism designed to protect by perceiving others’ neutral or positive actions or words as negative, and by avoiding and withdrawing from social situations where they could be judged
Biosocial model
High sympathetic nervous system (flight & fight) vs low autonomic arousal (fawn & freeze)
Results in hypervigilance (fight) against threats (being judged), shyness, timidity and avoidance (flight)
AVPD results from caregivers and peer groups’ rejection
Caregiver rejection is frequent and/or intense
Peer rejection reinforces the caregiver rejection, and reduces self-worth and self-confidence, creating self-criticism
Results in avoidance, hypersensitivity and excessive introspection
Hypersensitivity means they interpret small criticisms or even positive or neutral statements as rejections, and this lowers their self-esteem even further
Cognitive-Behavioural model
Avoidants fear being rejected so they don’t initiate or accept relationships
The conflict between their need for connection and fear of rejection is unbearable, so they withdraw
They also withdraw cognitively and emotionally from things that would make them feel uneasy or dysphoric
View themselves as incompetent socially and in school & work, as inadequate and different from others
View others as criticising, judgemental and uncaring
View criticism as being based solely on their perceived inadequacies
Use strategies like distraction, rationalisation, and excuses for when they feel sad and anxious
Interpersonal model
Avoidants grew up with relatively normal attachment processes, but their caregivers were very controlling when it comes to social image and reputation
Noticeable flaws were seen as embarrassing and humiliating
They were expected to be seen as perfect, and they were mocked and degraded if they weren’t
Results in hypersensitivity to rejection and judgement
Integrative model
Avoidants were likely irritable and fearful as babies and were likely slow to warm up to caregivers
View themselves as inadequate and fear rejection
View the world as unfair and criticising, but they still want connection
They need reassurance, but stay hypervigilant for judgement, and use fantasies and daydreams as escape methods
Tendency for catastrophic thinking
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#personality disorder concepts#case conceptualisations#clinical formulations#len sperry#handbook of diagnosis and treatment of dsm-5 personality disorders#pd info#avpd#avpd info#dogpost#*dysphoria here meaning unease; unsatisfied; unhappy etc
127 notes
·
View notes
Text
Personality Disorder Concepts: Prototypic Descriptions
Prototypic descriptions are brief descriptions that "capture the essence of how a particular disorder commonly presents", i.e., a summary of the key features of the disorder. The following are the protoypic descriptions of the DSM-5-TR personality disorders, summarised from Sperry:
ASPD
Antisocials displayed symptoms of Conduct Disorder from early childhood, and their manipulative and irresponsible behaviour continued into adulthood. They lack empathy and use others for their own gain. Because they can’t tolerate boredom, they are reckless, impulsive thrill-seekers and disregard their safety and others'. ASPD is over-diagnosed in prisons and detention centres.
AVPD
Avoidants are frightened and anxious, which makes them socially awkward. They are hypersensitive to criticism and rejection, and the fear of being embarrassed and humiliated causes them to withdraw and avoid social interaction. They crave connection with others, and may have trusted people with whom they can relax and feel safe.
BPD
Borderlines are terrified of being abandoned, which leads to intense relationships that often end in disappointment when they split on their favourite person. They are prone to self-damaging behaviours, and self-harm and suicide attempts are common. They have a fragmented, confused sense of self. They are often impulsive and prone to anger.
DPD
Dependents feel inadequate and fragile and need others to rely on. They struggle with being alone and find it nearly impossible to make their own decisions. They are submissive and are more than willing to put others’ needs and views above their own. They will do whatever it takes to get others to care for them, to give them affection, and give direction to their lives.
HPD
Histrionics are dramatic, charming and intense people. Their emotions are both intense and shallow at the same time. Their interests and attitudes are easily influenced by what others think and value. They need attention and reassurance that they are loved from others, so they often overestimate the intimacy of relationships.
NPD
Narcissists have a grandiose sense of self-importance, specialness and uniqueness that leads them to feel entitled and privileged. They expect and need admiration and respect from others to fuel their self-esteem. They lack empathy, so they have difficulty recognising the needs, concerns, or feelings of others. Criticism, rejection and failure leads to massive feelings of shame which is often redirected into anger.
OCPD
Obsessive-compulsives are perfectionists and need to get every detail right. As such, they are anxious and want to be in control of situations, so to avoid mistakes. They find comfort in schedules, rules and details, but their devotion to perfection interferes with their relationships and life outside of work or school. They have a tendency to hoard and are unusually tight with money, just in case.
PPD
Paranoids believe that the world is dangerous and that others will try to harm, exploit and deceive them if they open up. They are always on guard to any sign of threat. They hold on to grudges, never forget a slight, nor pass up a chance for revenge.
STPD
Schizotypals are eccentric, disorganised people whose emotions and speech are strange and blunted. Their strange beliefs are associated with ideas of reference and magical thinking, but don't extend to full-blown psychosis. It's not uncommon for schizotypals to be misdiagnosed as being autistic.
SZPD
Schizoids are uncomfortable being around others and just want to be left alone. Connection with others is scary and difficult, so they tend to keep to themselves. They come across as awkward, distant, and overly formal, and may be described as “cold fish”.
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#len sperry#handbook of diagnosis and treatment of dsm-5 personality disorders#dogpost#pd info#personality disorders#personality disorder concepts#prototypic descriptions#i have no idea what cold fish means btw that just what sperry said
141 notes
·
View notes
Text
Clinical Formulations of Antisocial PD
Clinical formulations and case conceptualisations are introduced in this post.
These are all generalisations and theories of how ASPD develops, not something that is supposed to be true for everyone with ASPD.
Psychodynamic model
Similar to NPD, both form a pathological grandiose self
ASPD self is based on aggressive introject (internalised self), “stranger self-object”
Stranger self-object reflects caregiver as a stranger who can’t be trusted, is neglectful and abusive
Detachment from caregiver & lack of object permanency leads to detachment from relationships & emotions in adulthood
Attempts to bond with others are sadistic, destructive and controlling
Antisocials don’t see others as separate people so can’t feel empathy for them, or remorse for their actions
Biosocial model
Low serotonin creates tendency for impulsivity and aggression
Antisocials often have childhood trauma
Were difficult to comfort as babies, which may have interfered with normal attachment process
Low stimulation levels in the limbic system, responsible for emotions and behaviour, especially in survival situations (as abusive environments are)
Lack of capacity for fear results in impulsivity and inability to learn from experience
Caregiver abuse, absence and neglect intersects with antisocials’ behaviour as children and as adults; they feel abandoned and unwanted
From this they learn that they must look out for themselves since no one else will, which ties in with their manipulation and lack of remorse as adults
Cognitive-Behavioural model
Antisocials’ behaviour is “persistently irresponsible”
They view themselves as strong, clever and self-sufficient
View others as weak, vulnerable and exploitable, so they will manipulate or victimise them
Dismiss others’ thoughts and feelings as irrelevant to them
Difficulty planning for the future, so they orient themselves entirely in the present
Treatment revolves around managing impulsivity and anger
Core beliefs:
They must look out for themselves
They must be aggressive so others don’t try to dominate and abuse them
They are allowed to break rules
They rationalise their thoughts, feelings and actions (e.g., “I can’t afford this thing, and I want it, so stealing it is ok”)
Conditional beliefs:
If they don’t manipulate and exploit others, they won’t get what they want or need
Instrumental beliefs:
They must get others before they can get them
Take what they need, even if it doesn’t belong to them
Interpersonal model
Antisocials often experience childhood abuse and neglect
Results in adults with ASPD neglecting and exploiting others, and fiercely protecting their autonomy
Childhood trauma is internalised and often results in substance abuse, criminal behaviour, irresponsibility and neglecting duties
Likely as children to take over caregiver’s responsibilities, since no one else did
This results in continuing controlling behaviour and difficulty with emotional bonding as adults
People with ASPD may present as friendly and sociable, but emotionally detached and without regard for others
Integrative model
Antisocials often had “difficult child” temperaments during childhood; they were unpredictable, intense, tended to withdraw from situations, and had low, irritable moods
See themselves as strong, capable, cunning and tough
See the world as full of rules to keep them from getting what they want and need, so they disregard the rules
Defense mechanisms are often acting/lashing out and rationalising their behaviour, feelings and thoughts
Their caregivers were either abusive and hostile, or provided such good role models that their child could not and would not meet such high standards
Caregivers believed that “the ends justify the means”, which was modeled and reinforced in their child
Family structure tends to be disorganised and disengaged
Antisocials need to be powerful and in control, because they fear being abused and humiliated
This results in a denial of vulnerability and “soft” emotions, and being uncooperative
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#personality disorder concepts#clinical formulations#len sperry#handbook of diagnosis and treatment of dsm-5 personality disorders#dogpost#aspd#aspd info#pd info#case conceptualisations
117 notes
·
View notes
Text
Personality Disorder Concepts: Maladaptive Schemas
Schemas are broad, pervasive themes in people’s view of themselves and others that develop during childhood. They are self-defeating, dysfunctional patterns, that can interfere with life.
There are 18 schemas, grouped into 5 domains. Each domain represents an important component of a child’s core needs.
Disconnection and Rejection
Abandonment/Instability: Believing that others won’t or can’t provide reliable and stable support.
Mistrust/Abuse: Believing that others will abuse, humiliate, cheat, lie, manipulate, or take advantage.
Emotional Deprivation: Believing that others won’t provide emotional support.
Defectiveness/Shame: Believing that they [the person with a PD] are defective, bad, unwanted, or inferior.
Social Isolation/Alienation: Believing that they are alienated, different from others, or don’t belong.
Impaired Autonomy and Performance
Dependence/Incompetence: Believing that they can’t function fully without considerable help.
Vulnerability to Harm or Illness: Fearing that disaster is just around the corner and that nothing can stop it.
Enmeshment/Undeveloped Self: Believing that they must be extremely emotionally close with others at the expense of a fully developed, independent sense of self.
Failure: Believing that they are doomed to fail.
Impaired Limits
Entitlement/Grandiosity: Believing that they are superior and above rules and norms.
Insufficient Self-Control/Self-Discipline: Believing that they are unable to demonstrate self-control and tolerate frustration.
Other-Directedness
Subjugation: Believing that they must meet the needs of others in order to avoid retaliation or criticism.
Self-Sacrifice: Believing that they must meet the needs of others at the expense of their own.
Approval-Seeking/Recognition-Seeking: Believing that they must be constantly trying to belong and be accepted, at the expense of not developing a true sense of self.
Hypervigilance and Inhibition
Negativity/Pessimism: Overly focusing on the negative while dismissing the positive.
Emotional inhibition: Avoiding spontaneity at all costs, including actions, feelings and communication, in order to avoid disapproval, shame, embarrassment and feelings of losing control.
Unrelenting Standards/Over-criticising: Believing that constantly trying to meet unrealistically high standards is essential to be accepted and to avoid criticism.
Punitiveness: Believing that mistakes should be harshly punished.
Some schemas are associated with certain PDs; for example punitiveness is associated with OCPD, and mistrust/abuse is associated with ASPD & PPD.
- From Sperry, Handbook of Diagnosis and Treatment of DSM-5 Personality Disorders (2016)
#[schemas arent exclusive to pd literature btw]#len sperry#handbook of diagnosis and treatment of dsm-5 personality disorders#schema modes#maladaptive schemas#personality disorder concepts#dogpost#pd info
127 notes
·
View notes