#food for dogs with kidney disease
Explore tagged Tumblr posts
Text
youtube
Royal Canin Renal (Kidney) Dog Food Review - The Dog Nutritionist
Are you looking for the best kidney support food for your furry friend? Look no further than the Royal Canin Renal (Kidney) Dog Food Review by me (The Dog Nutritionist). Hi, I'm Cam Wimble, a certified Dog Nutritionist, and in this video, I dive deep into the ingredients of Royal Canin Renal Dog Food to see if it truly delivers the kidney support your dog needs.
Many dog owners rely on prescription dog food like Royal Canin Renal for kidney issues, assuming it's the best option. But is it really working? I'll uncover the truth in this review and suggest better alternatives if needed based on my experience working with dogs with kidney problems.
Let's debunk the myth of low-protein diets and explore why some kidney-support foods may not be as effective as you think. Cheap ingredients and lacking nutritional value could be harming your dog's health.
Don't settle for subpar dog food - visit www.thedognutritionist.com for more information on giving your dog the best care possible.
Treat your furry friend to the quality nutrition they deserve.
#renal dog food#kidney support dog food#royal canin renal dog food#Royal Canin renal food#dog food for kidney disease#royal canin renal dog food review#royal canin kidney support dog food review#best kidney support food for dogs#healthy dog food#homemade dog food#best dog food for kidney disease#dog nutritionist dog food recipes#raw dog food recipes#food for dogs with kidney disease#dog food review#homemade renal dog food#renal dog food review#dog food recipes#Youtube
1 note
·
View note
Text
Great news btw: juno has rapidly improved on his fluids!! Hes been really good about getting them in, and his appetite and energy and everything has gotten so much better. AND HES GAINING WEIGHT!!!
#he still ofc has kidney disease he cant get rid of#BUT!!! hes doing so much better and hes stealing the dog food even off his appetite stimulant#talk tag
7 notes
·
View notes
Link
This is an article about dog food for kidney disease
#healthlinkeg #doglovers #pet_care #dogs #pets
0 notes
Link
📋 Kidney Diet for Dogs Homemade: Complete Meal Plans for Your Pup is here to transform your furry friend's health! 🍲🐶 This video provides easy, nutritious, and delicious homemade recipes that can help manage your dog's kidney health effectively. Dive in to discover meal plans that are both tasty and beneficial for your pup's well-being. Don't miss out on these vital tips and recipes!
#kidney disease#homemade dog food#dog food#puppy food#dog care#dog health#dog mom#dog parent#pet parent#pet care#pet health
0 notes
Text

h8 this shit no she's a baby
#no but ok a close friend's dog just died and so i've been confronting the reality of pet mortality lately#and no i'm sorry she's 12 but she's baby#she's older than all of my nieces but she's BABY she will live forever#this is all to say i've been putting off getting her blood retested for the SDMA marker bc her having kidney disease is terrifying#in no small part bc i know i can't afford prescription kidney wet food#fuck fuck fuck fuck no she's BABY.
1 note
·
View note
Text
Day 43, Labs, Not The Awesome Dog Kind
I’m typing this up on Sunday before the superbowl so I don’t know who wins/won but I personally am pulling for the Chiefs. I like Patrick, he has a good vibe. Anyway, we have labs this morning (Monday) so hopefully we can find out what’s going on but if it’s anything like the past they will say the labs don’t show anything wrong so it must be ok. We’ll see in a matter of hours. The labs usually…

View On WordPress
0 notes
Text
hi guys i know this is kind of a big ask so im going to try to elaborate as many details as i can even if many of them are painful and private and i do want to give a content warning for mentions of animal injury and abuse
as some of you know, my sister is an addict and i am currently estranged from her. about a month and a half ago, her dog was abandoned at a rescue that partners with the animal shelter i volunteer at, tied up to their front door in the middle of the night with injuries that are presumed to be from being struck by a car.. severe road rash on his legs and paws and bruising, thankfully nothing broken. he received some medical treatment and was transferred to the shelter i volunteer at. during this time, my sister did not attempt to reclaim her dog and i assumed responsibility for him at an expense i and my family wasn’t exactly prepared for. due to his age and his illness and injuries, he would not have been a fit adoption candidate but i did not feel that he was ready for euthanasia. he is a good dog, still full of life and still making every effort to keep going, and he’s so deserving of spending his remaining time here comfortably despite what he has been through the past several months. the truth is, he has been abused and severely neglected. my brother in law knocked several of the dog’s teeth out and broke them (he is currently in jail), and both he and my sister were aware of the dog’s kidney disease but did not seek medical treatment for him and often allowed the dog to go days without food or water.
at this time, he needs further vet care; antibiotics, pain medication, treatment for his anxiety, medicated baths, and prescription dog food for his kidney disease. a family friend created a gfm to help us with these expenses and im asking y’all to help or share this anywhere you can, if you can. he has a long way to go but he’s not giving up yet. 🩵 if you have any questions or any details you want verified, please don’t hesitate to send me an ask and i will do my best to get back to you quickly!!
https://www.gofundme.com/f/help-steve-heal-support-his-medical-care?attribution_id=sl:d1bb7b4e-4220-4912-8a93-8c32f23dcf55&utm_campaign=man_sharesheet_dash&utm_medium=customer&utm_source=copy_link
354 notes
·
View notes
Text



hi, this is my dog! her name is magnolia mae and she's an elderly chihuahua-dachshund mix (estimated between 12-15 years old). she's a rescue we received from my roommate and best friend's late cousin about 5 years ago.
long story short, our sweet girl has been experiencing some severe and concerning health issues (extremely low RBC, WBC, Neutrophils, and Platelets), and she needs to have her bone marrow tested. this is extremely expensive (at least 1,200), and we're hoping to get some help. if you'd like more information on what's going on with her, that will be under the cut. otherwise, please consider using either of the below methods to help us take care of our sweet old girl!
ppal.me: @/daisyd0nati0ns (replace 0s with Os)
kof!: @/keeperesque
don't tag as d0nat!ons/etc, etc..
when we moved across the country during late 2020 to be with my wife, we brought her, as well as my elderly cat sampson and my two older rabbits, indie and digit.
2023, however, has not been kind to any of our pets. in february, we lost sampson to kidney failure - it was sudden and utterly heartbreaking. a month later, my wife found that digit had passed away in her sleep, and indie was put down shortly after due to health complications we could not afford to properly treat. since then, we've been extremely diligent with maggie's health - she eats special food for her kidneys, has vet appointments scheduled every 6 months, gets twice-daily walks, takes medication for her thyroid, and receives plenty of love.
unfortunately, starting with an emergency visit in september, maggie's been having severe problems with her blood - specifically an extremely low platelet count (33,000-55,000, normal levels are about 200,000), white blood cell count and neutrophils are extremely low, and she's extremely anemic. while she's on some medication to keep her stable, we aren't sure how long that will last, and it's taxing on her body.
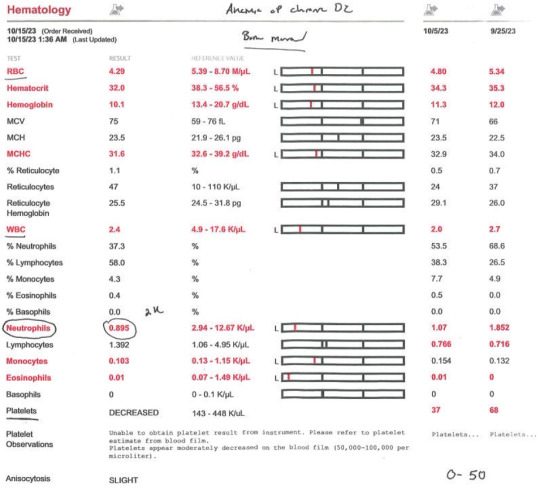
after ruling out infectious diseases, we need to take her in to have her bone marrow looked at. the procedure, at the low end, will cost around 1,200, and up to 1,600, depending.

i also have pdfs available for anyone skeptical of these claims or who want proof of treatment.
we're not sure if we'll be able to save her, but we would at least like to know what's happening so we can make an informed decision on how to proceed, instead of watching and waiting for the worst. anything over the price of her procedure will, of course, go towards related expenses, such as treatments or end-of-life care.
if you read all of that, thanks. again, please consider helping us out!!
ppal.me: @/daisyd0nations (0 is an o)
kof!: @/keeperesque
have an extra maggie pic :)

#not peach#please rb and stuff#really anxious abt posting this but we are kind of desperate atm#i don't rlly talk a lot about my personal life online anymore fjkdlfs#so this is weird#and with her being so sick lately i don't have a lot of reasons to post pics 'cause it's jsut her sleeping in her beds mostly...
140 notes
·
View notes
Text
Leptospirosis: What it is, what it does, and how you can protect yourself and your pets.
People always have questions about leptospirosis (lepto) when they come into the clinic, especially in regards to the vaccine. This post will hopefully clear up those questions or any confusion regarding lepto and its vaccine, and why it's so serious. The information in this post comes from my formal education as a LVT, as well as other sources including the CDC, PAHO, and AVMA. If I missed anything or you see something that's incorrect, please let me know!
First and foremost: What is leptospirosis?
Leptospirosis is a bacterial disease that effects human and non-human animals. It's caused by bacteria in the genus Leptospira. In humans, it can cause a wide range of symptoms that can be very general. This leads to misdiagnoses. Animals such as dogs, livestock, and certain wildlife are all susceptible to infection.
How is leptospirosis spread?
Lepto is most often spread through contact with the urine of an infected animal. This is especially the case (but not the only case) with wild rodents. Infected dogs can seem healthy, but still pass the bacteria on in their urine. In urine-soaked soil, the bacteria can survive for weeks to months.
Dogs typically become infected when their mucous membranes or open wounds come into contact with urine or urine contaminated surfaces (like soil or water). Infection can also be spread through urine-contaminated bedding or food, or the tissues from the carcass of an infected animal. There have been rare instances where lepto has been transmitted by bite or breeding. A pregnant dog who is infected may pass the bacteria to her puppies through the placenta.
Humans contract lepto pretty much the same way: through contact with urine from an infected animal or urine-contaminated surfaces.
What are the signs and symptoms?
In humans:
High fever
Headache and muscle aches
Chills
Jaundice
Vomiting and diarrhea
Redness of the eyes
Abdominal pain
Rash
Humans can also be asymptomatic, which is particularly concerning. It usually takes anywhere from 2 days to 4 weeks post-exposure to the infection source before any symptoms are displayed. The illness begins abruptly and it may occur in 2 phases. The first phase is where you will see a lot of the general symptoms listed above. The person infected may recover for a period of time, but become ill again. The second phase is more severe, leading to kidney or liver failure, and possible meningitis. The illness can last a few days to 3 weeks or longer.
Without treatment, recovery can take several months.
In dogs:
Signs and symptoms may vary slightly depending on the strain of the infected bacteria. The signs are also very general in dogs, but the most common ones include:
Loss of appetite
Vomiting and diarrhea
Lethargy
Abdominal pain
Jaundice
Dehydration
Increased thirst and urination
Weight loss
Stiffness or muscle pain
The disease can also progress to kidney and liver failure in dogs, with damage to other organ systems also noted in the literature. Lepto can also cause bleeding disorders, which can lead to blood in urine, vomit, feces, or saliva, and petechiae on the mucous membranes or light colored skin.
Who is most at risk?
For humans, those who are most at risk include those who work with animals or outdoors where you come into contact with wildlife. The Pan American Health Organization (PAHO) also mentions that sewer workers and military personnel are at-risk populations. Farmers (and generally people who work with livestock) also make the list, as do veterinarians, veterinary technicians, and veterinary assistants.
For dogs, it's all of them. "All dogs are at risk of leptospirosis, regardless of age, breed, lifestyle, geographic location, time of year, and other factors." (source: AVMA)
Situations that can increase the risk of your dog contracting leptospirosis are listed below:
Exposure to drinking from slow-moving or stagnant water sources (this includes puddles)
Roaming on rural property
Exposure to wild animals or farm animals, even if it's only in the yard
Contact with other dogs (such as in urban areas, dog parks, boarding, or training facilities.
How is leptospirosis treated and diagnosed?
Disclaimer: I am NOT a medical doctor or DVM, but I am an LVT. If you think you're experiencing these symptoms, PLEASE go see your doctor. If you think your dog or any of your other animals are experiencing these symptoms, PLEASE take them to your vet.
Diagnosis in non-human animals:
Unfortunately, routine blood tests alone cannot diagnose leptospirosis. That's why it's important for your vet to use all information available to them (i.e. diagnostics, signs and symptoms, lifestyle, etc). There WILL be abnormal results for blood work, most likely high liver and/or kidney values and high white blood cell count. There are specific tests available for diagnosing lepto, such as the DNA-PCR and MAT tests. Both may be needed to reach or confirm a diagnosis. False negatives are possible, so your pet may be treated as if they have leptospirosis, even if the test results are negative. False positives are exceedingly rare.
Diagnosis in humans:
Leptospirosis is diagnosed in a similar fashion in humans. A physical exam, blood work, and urinalysis will likely be run. The same style of tests are used: DNA-PCR and MAT.
Treatment in non-human animals:
Leptospirosis is treated with antibiotics and supportive care. Doxycycline is most commonly used, and will likely be prescribed for 2 weeks or more. Supportive care includes hospitalization with IV fluids and management of electrolyte levels. Additional medications and procedures may be necessary.
Treatment in humans:
The treatment is similar in humans, with antibiotics (usually doxycycline). Your doctor may also suggest to take ibuprofen and monitor yourself at home for less severe cases. If the case is severe, then you'll likely spend time in the hospital. Additional medications or procedures may also be necessary.
Outcomes:
In non-human animals:
Leptospirosis is responsive to treatment with antibiotics. Complete recovery is possible, but some animals that survive may be left with chronic kidney and liver disease. Some animals may not survive if the infection has gotten to the point where it causes severe organ damage or the ability of blood to form clots.
In humans:
You can survive leptospirosis. Most cases have either very mild symptoms that go away on their own, or none at all. Without treatment, leptospirosis can cause kidney damage, meningitis, liver failure, trouble breathing, and even death. PLEASE go see a doctor if you think you're experiencing any of these symptoms, especially together.
Prevention
How can you prevent infection and protect your pets?
For dogs, there's the leptospirosis vaccine. This is an annual vaccine that vaccinates against multiple strains of Leptospira. If you're worried about your dog having a vaccine reaction, let your vet know and they can administer an injection of diphenhydramine (generic benadryl) beforehand, OR you can ask them what the appropriate dose is for your dog and give them the respective amount at home (in tablets or liquid). Vaccine reactions are uncommon, but if they do happen, it's usually immediately after exposure to the vaccine. You can ask to stick around in the lobby/waiting area of your vet clinic for a few extra minutes if you're still concerned.
Limit your dog's access to standing water. Don't let them drink from it. Prevent rodent problems where you can by properly storing food items in appropriate containers, securing your garbage, and patching up any access points into your house if you see them. Try to avoid contact with wildlife, when possible.
For humans, the recommendations remain similar. Don't wade or swim in stagnant water, ESPECIALLY if you have open wounds. Avoid contact with wildlife. WASH YOUR HANDS, often and appropriately. USE PPE if you work in a veterinary setting and properly clean and disinfect surfaces and equipment. Make sure you know or research the area that you're in if you like swimming and boating. Check to see if there have been any recent lepto infections. Cover your scrapes and wounds with waterproof bandages and wear water shoes if possible.
I hope this post answered a lot of your questions! Thanks for reading.
Sources under the cut.
Sources:
#animals#pets#dogs#leptospirosis#zoonotic diseases#infectious diseases#vet med#vetblr#petblr#dogblr#my posts
47 notes
·
View notes
Text



I had to say goodbye to Jack today.
She had been steadily losing weight and I thought it was just because she was getting old. But in the last couple days she RAPIDLY lost weight. The vet said it was end stage kidney disease.
She was ready to go. She only held on for a heartbeat of a second after the injection. I was holding her paw and petting her head. She was the best cat in the whole world.
Jack was my first pet that was all mine. I met her when she was 3 weeks old at my first college summer job in 2013. They said “do you want a kitten?” when she was old enough for a home. Of course I wanted a kitten! She was spunky and sassy and hated everyone but me.
Once she turned 8, she started getting friendlier to others too. She liked being with the dogs and beating up the other cats. She loved stealing food and enjoying Ben’s tuna water. Jack liked sleeping and would always purr even if you just looked at her. She liked riding on your shoulder and she liked to cuddle.
When I got in the car after she passed, I plugged my phone in. The same song always comes on. Adio (Acoustic version) by Agathadamion. But it weirdly started halfway through the song. The word “Farewell” rang through my car’s speakers before turning off by itself.
If that wasn’t a sign, I don’t know what is.
I love you so much, Jack. I hope you wait for me. I hope you’re not in pain anymore. I hope you get to see Rudy.
73 notes
·
View notes
Text
TW: pet death


Hey guys. I know I don’t post very often. I don’t even know how to start this other than that Joe died unexpectedly this morning and it’s devastating.
My sister took him to the ER last night because he had a seizure then was acting lethargic/in pain/had pale gums. They had just thought it was a sprain but the vet did bloodwork and his RBCs were critically low. The vet told them it was either cancer or that he ingested something toxic, and knowing that Joe has pancreatitis and my sister and BIL watch his access to food like a hawk I had a feeling it was the former. They took him 2 internal med specialists before the vet said it was likely a tumor on his spleen that ruptured and my sister/BIL opted to not do a splenectomy. My sister was calling me the entire time and asking for advice and it just…sucked? To know what the answer likely would be but to know that they would want to truly know the cause (as would I, even knowing what the likely outcome would be regardless). Especially because my sister is 6 months along with their first and they were super excited to introduce Joe to the baby since he adores kids. And now he’s gone.
She’s been MIA for most of the day aside from announcing it to the family but I know she’s processing it - she sent a picture to us of shortly before/after he passed. I’m also in this weird spot where I’m grieving him too, I lived with him until he was like four and then I practically lived at my sister’s apartment with him for another year or two, plus of course I see him constantly because my sister is my best friend and he’s Taylor’s dad. I love him. I was his third favorite person, behind my sister and BIL of course. I literally just saw him on Saturday when we had a family day painting the nursery and he was acting completely normal including playing with Taylor and begging for human food. But also I’m the one having to explain to everyone about what exactly happened medically and helping them process that there was nothing to be done. The only one I’ve been able to grieve to is Ian which is…not fun. I’ve been barely holding it together at work.
I’m just so so worried about my sister. She’d have a hard time with this normally, much less with her being so excited for her baby boys to meet. And I want to make her feel better but it seems like she just wants space. I’m going to give them a few days then see if I can drop off eggs this weekend and go see them. I also know the next time she sees Taylor isn’t gonna be easy cause now she’s all that Liz has left of her two favorite dogs. We had even just been discussing how Joe was her heart dog.
And I’m also worried about Taylor. She’s officially the same age as her mom was when Sandy passed from kidney disease and she has about a year and a half to be Joe’s age. Luckily she hasn’t had any seizures, which both Joe and Sandy started having by this age. All her bloodwork values are good aside from a consistently elevated ALP that our normal vet thinks is just “her normal.” This has definitely cemented my desire to get Taylor’s liver checked by ultrasound before accepting that though. I really hope we don’t find anything and that the specialist isn’t worried. Even if we do find something “early” or if we do annual ultrasounds, if it’s the same cancer as Joe’s then it’s just a ticking time bomb that we can’t really do anything about. But of course she’s still a little hellion that doesn’t act like any nine-year-old dog I know.
At least Joe got to see everyone (minus Chief and Bandit) this last weekend. And he got to see Chief and Bandit the weekend before on Memorial Day. I just wish we’d known.
I’m not ready yet, I just want at least 3 more years with her.

#TW pet death#Joe#I’m so sad#just have to take deep breaths#and my sister is texting some of the most devastating stuff and my heart is breaking for her all over again
12 notes
·
View notes
Photo

Poor Flynnie has to have an ultrasound scan on Thursday :( He is STILL having some pretty severe gut problems, 2 months after they started... Plus, the most recent blood test we did showed up some slightly “off” results, nothing major but various levels were a bit higher, or lower than they should be - including some stuff related to kidney function.
After seeing the results, the vet asked me to get a urine sample. It turns out Flynn’s losing protein in his urine & his urine is also too dilute. High protein levels in urine often happens because a dog has chronic kidney disease but it can also be a temporary issue, due to infection/inflammation, (or other illnesses... like cancer, which I hope is very unlikely to be the cause here). Regardless of the reason it is happening, it puts a strain on the kidneys. Or, in Flynn’s case, a strain on his kidney. Singular. Flynn only has 1 kidney... so we really can’t mess around with this. He’s now on a “renal diet” & if it’s safe, may start on ACE inhibitors to reduce strain on his kidney. The ultrasound will look at both Flynn’s gut & his kidney, so I guess we’ll just have to wait & see if anything shows up.
I lost Barney, less than 3 weeks ago - after he’d had the exact same infection as Flynn. Barney went from having mild kidney disease, to being in kidney failure in the space of less than a month. Barney was very elderly, of course... but, still... I don’t know what is going on with Flynn. He’s been treated twice for giardia infection, we’ve been manically cleaning to prevent reinfection, he’s on probiotics & was on GI food. He is an apparently otherwise healthy dog & he really should be getting better by now & instead, if anything he seems in some ways worse than he was 6-8 weeks ago. Argh, I am so stressed. My poor little guy :(
112 notes
·
View notes
Text
(Voiceover to a montage of preparing raw dog food)
“Wolves die from diseases like lyme and parvo and rabies… but our domestic dogs die from cancer, and diabetes, and kidney dysfunction, and all the metabolic diseases. And wolves don’t die from any of those things. Clearly this is big kibbles fault, follow to homestead with me ✨”
Paraphrasing but I saw this on instagram and it bugged me. I’m not getting anywhere arguing with someone who drinks raw milk and thinks that’s safer than GM food. But like hmm maybe part of it is because domestic dogs tend to live longer without dying from injuries. Also wolves definitely can get cancer...
Like I’m not an expert on wolves but blaming kibble is a choice. Nutrient requirements in dogs have been well studied. Feeding your dog a diet that has passed AAFCO feeding trials will ensure they get proper nutrition and is far safer than feeding them raw meat, eggs, and milk.
#people try to make the same argument with humans and it’s silly#hmm it’s almost like our ancestors had a much shorter lifespan and would just die if they faced complications that are survivable now#‘wolves dont die from cancer’ is also a wild claim
2 notes
·
View notes
Note
Hi Jess, I have a Karluk question for you! What exactly was wrong with the expedition's supply of pemmican? Wikipedia says Stefansson said it was a lack of fat, but Niven's book describes the disease as coming from too much fat and protein. Are there any clear answers as to what actually made it faulty?
Hi! This is a great question, and I wanted to do a little research before I responded to make sure I got the details right.
First, what exactly is pemmican? It's one of the staple foods of polar exploration, a nutritionally balanced combination of dried meat, fat, and sometimes a small amount of carbohydrates. It's easy to transport, calorie dense, can be formulated to feed men or dogs, and doesn't spoil easily, making it ideal for long voyages. Indigenous peoples were making and using pemmican for centuries before the Europeans "discovered" it.
With this in mind, I looked at the two competing claims you mentioned. First, I found the citation in the Wikipedia article, and since I have Stef's (ridiculous) book The Friendly Arctic, I double checked it. The quote is accurate, but there's some missing context. In this passage, he was actually talking about pemmican that was specifically formulated for dogs! There was dog pemmican and man pemmican (and confusingly enough, the Karluk also had 2 different kinds of man pemmican-- more on that later). In the passage below you can see that Stef is complaining about the dog pemmican being deficient in fat, and how he claims it affected dog performance.


(In general, though, it's important to note that Stef had a... tenuous relationship with the truth. I would fact check anything he said as a matter of principle.)
To examine Niven's claim, I called in the big guns, by which I mean I consulted with an actual expert with their Ph.D. in all things polar and a special interest in Stef's shenanigans! They are on tumblr, but I'm not sure if they're OK being tagged, so I will just thank them anonymously for their help 🥰 Anyway, between the two of us, we were unable to find any studies specifically examining the relationship between pemmican (faulty or otherwise) and nephritis, a kidney disease diagnosed by the doctor who examined the Karluk survivors. To the best of our knowledge, no testing was ever done on the bodies of the deceased, but since the symptoms of the survivors lined up with the symptoms of nephritis, there's no compelling reason to doubt this diagnosis.
So how do we know the pemmican caused the nephritis? Officially, we don't! However, we have a LOT of evidence indicating that it did. Niven does a great job documenting all of this in The Ice Master. We know that people have been surviving on pemmican in the Arctic for centuries without developing nephritis. We know that in order to be a nutritionally balanced survival food, pemmican needs to have a specific ratio of protein to fat. We know that Stef did not personally oversee the production of his pemmican, as some previous expedition leaders had done (which is especially hilarious considering that later in his career he would conduct some disastrous experiments involving feeding pemmican to United States troops, so clearly he had an interest in the stuff). We know he did not submit it to purity testing to ensure that it was safe and nutritionally balanced because he was in too much of a hurry. We know that the men strongly preferred the Hudson's Bay brand of pemmican over the Underwood brand because the Underwood brand made them ill, and they reached a point where they couldn't choke down any more of it, even though they were starving. We know that high fat and/or protein diets without carbohydrates can be very bad for your kidneys, especially if you have other preexisting medical conditions (like, for example, a weakened immune system due to exposure and starvation and stress).
I am not a doctor and I do not play one on the Internet, but if I had to guess, I would say there was a problem with the Underwood pemmican, most likely that the fat to protein ratio was off or it was somehow contaminated. This is also the conclusion that Niven reached, and her research for this book was impeccable, so I have no reason to doubt her! We will, of course, never know with complete certainty what caused the nephritis, but the men clearly thought it was the pemmican, and I believe them.
I'm sure this is WAY more than you ever wanted to know about pemmican, but if you want to know more, I can hook you up with some more sources! If you're interested in polar foods in general, check out Hoosh by Jason C. Anthony, which focuses specifically on Antarctica, but there's definitely some overlap with the Arctic! And I hope this helps!
18 notes
·
View notes
Text




Foxy Lady from Cat Crew California in Hollister, California
Click here for more information about adoption and other ways to help!
Click here for a link to Cat Crew California's main website.
Foxy is one of our beautiful special needs adult kitties. She came to our rescue as a stray, skinny and missing more than half of her fur. She was so trusting and loving from the beginning, thankful to be safe and off the streets.
This quirky, sassy, loving lady will win you over with her raspy meows, abnormally short fluffy tail, and spunky attitude.
She is learning how to be an indoor house kitty and sometimes gets over excited/stimulated while getting pets, which means she may swat or give a love nip. She has improved significantly in the last few months and her foster is actively working on showing her pets can be a calming treat.
This girl LOVES food. She has gone from skin and bones to a nice floofy chonk since joining our crew. She has also learned that cat beds are comfy and cat toys are not strange or scary.
Foxy was diagnosed with chronic kidney disease after being examined by our veterinarian. At this point, she requires no special diet or medications, but may have a shorter life expectancy than a healthy cat.
In her current foster home, Foxy has another senior kitty as her roommate and they coexist well. She also shows interest in other cats in the home. She has also met kittens, sniffs them, and walks away. We do not know how she feels about dogs. She would most likely do best as the only pet in the home or possibly with other cats with proper/patient introductions.
Foxy is approximately 5-8 years old. Foxy Lady is spayed, microchipped, and vaccinated.
18 notes
·
View notes
Text
Okay time for another PSA to not let your pet cats free roam outdoors ever. (If you think you don't have the space indoors for a cat to be happy or the willingness to give your cat what it needs indoors then don't have a cat. That means you can't take care of it so don't get it. Also, you clearly don't care about a cat's "natural needs" if you don't also keep it fully up to date on health check ups/vaccinations, give it enrichment and feed it only pure raw meat at home. They're obligate carnivores. Kibble is why they develop and die of kidney issues.)
They indisputably cause incredible damage to ecosystems and due to the way they became domesticated to eradicate pests, they are built to kill and maim indiscriminately and with extreme prejudice. Your pet cat does not hunt to eat when it has a safe bed and food at home. It hunts to slaughter. Because it's instincts say so, even if you think it's a chill lazy cat (what are the feather and mouse toys for but to satisfy those instincts?).
Whether or not a direct attack kills a small animal, it will most certainly still die of complications (like ruptured air sacs in birds -an incredibly painful way to go-, blood loss, disability, necrosis, cellulitis, and septicemia), countless serious infections from the cat's claws and mouth, inhalation of blood/stomach contents, or other infection from exposure to the environment. That is if it totters along on its will to survive, suffering, and manages to escape the next predator that comes along.
And if you couldn't care less about the local ecosystem and countless species that have gone extinct by cats under our very noses, you should worry about your cats' safety and the possibility of infection and parasites that they bring home to you and transmit to other pets, people, and homes they visit.
Cats will be run over or killed/injured by people, either by accident or intentionally (many people see any kind of small animal as target practice for their car or dart gun or whatever else and don't care if it's a cat. Maybe they even do it to protect their livestock, e.g. chickens, rabbits). Cats will get into fights with other animals. Cats will get eaten by coyotes. Cats will hide or shrug off injuries. Cats will meet other cats from different circumstances. Cats will carry rabies or be bitten by a vector animal and the only way to test for rabies is to take a slice of the brain (i.e., kill the animal in question). Cats will walk back into your yard and home with everything they picked up along the way, if not on their body then in their mouths after grooming and in their litterbox. Putting your cat, yourself, and others in that sort of danger is more neglectful than keeping them indoors. Letting them bring everything back to your home is negligent. Letting them infect and harm other animals is negligent ("dangerous" dogs who stay in their own yards get euthanized for less). It does not matter what part of the world you live in. Letting your pet cat outdoors is neglect and malicious behavior.
And in case you think you're not at risk from disease from your own cat or you want relevant, recent news to back this up, here's an article X , posted 07 August 2023, about a UK man contracting a completely unknown bacterium from a stray cat, initially resistant to certain antibiotics, that started to kill the infected flesh, and here's the scientific study about identifying the bacteria X
Who knows what your own cat gets up to outside or what other animals they meet?
#outdoor cats#biology#science#wildlife conservation#medicine#veterinary medicine#if this post gets views i just know im still gonna get hate cuz wow this topic shouldnt be this controversial#i had this whole post drafted and went looking for studies to cite and that article came up before i even hit the search bar#this has been a psa#this also is not to say that people who did this in the past are evil or anything. there is a difference between not knowing better and#making a choice or choosing to ignore new information rather than learning#or having info delivered to you in a way that didnt tell you what was wrong about it
15 notes
·
View notes