#esophageal dysmotility
Explore tagged Tumblr posts
Text
this is gonna get TMI and it will get sad and whiny so please don't feel obligated to keep reading.
it takes so many steps to be alive. all of the things you do subconsciously suddenly become arduous tasks when you have to do them manually. things like eating, drinking, sleeping, breathing, using the bathroom, it's exhausting having to think about and consciously or manually do even just one of those things.
I was officially diagnosed with dysautonomia a few months ago, although I have been struggling with my symptoms for over a decade and I've been in treatment for several years. I was also diagnosed with a neurogenic bladder that same month. this means I have to catheterize myself 3-4 times a day every day for the rest of my life, or until I can get a suprapubic catheter placed.
Y'ALL. self-cathing is beyond exhausting. it's a little bit of a genuine workout, especially when you're morbidly obese like me. I hate that I've gotten really good at it and that it doesn't take me long at all now. I didn't want to get good at it, I didn't want to have to have this skillset. I already have to know how to draw up and give an IM injection, how to flush an IV, how to reduce dislocated joints in myself and others... I am TIRED.
I'm sure a colostomy is also in my near future. I have the same problems in my colon that I have in my bladder, only it's also complicated by endometriosis in the walls of my colon and rectum. they haven't been completely infiltrated yet, but if this IUD doesn't do its job, then I'm definitely gonna start losing organs and my mind.
at this point I'm out of words to explain why I'm so cosmically fatigued but if I tag every diagnosis/condition I have maybe y'all can sorta get an idea.
sorry for ranting. I have to go cath myself now.
at least I do it under the supervision of the best medical advisor ever <3 all she asks for in return are kisses, cuddles, and crunchies <3<3

#neurogenic bladder#endometriosis#pernicious anemia#autoimmune gastritis#gastroesophageal reflux disease#celiac disease#multiple food allergies#asthma#long QT syndrome#inappropriate sinus tachycardia#dysautonomia#hyperadrenergic POTS#ehlers danlos syndrome#fibromyalgia#chronic hydronephrosis#idiopathic intracranial hypertension#rheumatoid arthritis#small fiber neuropathy#esophageal dysmotility#chronic fatigue syndrome#im sure im forgetting some but how am i supposed to remember all of them at once when the list is so long#cat :)#WHEELCHAIR USER#i forgot i cant even walk on my own#in my toddler era#i am sickly and not meant for this earth
8 notes
·
View notes
Text
Ask A Genius 1241: I have no idea, also aging
Scott Douglas Jacobsen: Here’s a topic. If you’re on Facebook and you like those zit-popping clips from Instagram or wherever, try searching for farrier or blacksmith recovery videos. They take out nails and rocks embedded in horse hooves. Sometimes, the hoof grows around the rock; they dig it out, and there’s pus and blood. Rick Rosner: As much as I like popping my zits, I’ve never watched a…
0 notes
Text
Me, trying to eat fast: "Oh wait, I have an esophagus disorder that literally makes this impossible and now I feel like I'm choking."
0 notes
Text
It's Gastroparesis Awareness Month
Hi! I have gastroparesis and I'm an insufferable know-it-all so let's talk about it!
Gastroparesis, or a paralyzed stomach, is a condition that causes delayed gastric emptying.
This can cause a range of symptoms and complications:
nausea
vomiting
early satiety/fullness
upper gastric pain
heartburn
malabsorption
dehydration
malnutrition
Gastroparesis can be treated by a gastroenterologist, but often needs to be managed by a motility specialist due to a lot of misconceptions about the condition. Providers, especially in the emergency department, will commonly misdiagnose gastroparesis as cannabis-hyperemesis syndome, cyclic vomiting syndrome, gastritis, food poisoning, etc.
There are several commonly known causes of gastroparesis like vagus nerve damage from diabetes, injury to the stomach, and stomach surgery like hernia repair or bariatric surgery. There are also idiopathic cases with no known cause. Other causes of gastroparesis are:
Connective tissue disorders like HSD and EDS (commonly hEDS and cEDS)
Post-viral (like COVID, viral gastritis, mononucleosis/Epstein-Barr)
Restrictive eating disorders
Autoimmune diseases like Systemic sclerosis (scleroderma), Lupus, Hashimoto's
Central nervous system disorders
Gastroparesis also has common comorbidities with conditions like:
POTS and other forms of dysautonomia (POTS, EDS, and gastroparesis are a common triad of diagnoses)
MCAS
SMAS (which can also present with similar symptoms to GP)
Intestinal dysmotility and esophageal dysmotility disorders (known as global dysmotility)
PCOS with insulin resistance
Endometriosis
SIBO/SIFO
Chronic intestinal pseudo-obstruction
Migraines
Certain medications like Ozempic and other drugs in that class act on the digestive system to delay gastric emptying, which has caused people to be diagnosed with gastroparesis. Some people report that their cases have not gone away since stopping the medication, others report feeling better after stopping. Other drugs like opiates and narcotics can cause delayed gastric and intestinal motility as well, but these are commonly known side effects of those painkiller classes.
Gastroparesis is classed based on severity and graded based on how you respond to treatment.
Severity of delay ranges from mild to very severe, and this is based on your actual stomach retention calculated at 4 hours into a gastric emptying study.
The grading scale ranges from one to three, one being mild and three being gastric failure.
There is no consistent single treatment that is proven to work for gastroparesis, and there is no cure. Treatments can consist of:
Diet changes (3 Step Gastroparesis Diet, liquid diet, oral sole source nutrition)
Prokinetic (motility stimulating) drugs
Anti-nausea medications
Proton-pump inhibitors
Gastric stimulator/gastric pacemaker
Pyloric botox and dilation
G-POEM/pyloroplasty
Post-pyloric tube feeding
Gastric venting/draining
Parenteral nutrition
IV fluids
Other surgical interventions like gastrectomy or rarely, transplant
Gastroparesis is a terrible disease and I hope that if any of these symptoms resonate with you that you can get checked out. I was misdiagnosed for a long time before getting a proper gastroparesis diagnosis, and all it took was a gastric emptying study. This is ESPECIALLY true if you're having post-COVID gastrointestinal problems that are not improving. I almost died from starvation ketoacidosis because of how serious my GP got in a short period of time post-COVID (I had GP before COVID), and now I'm tube reliant for all my nutrition and hydration.
Stay safe friends!
658 notes
·
View notes
Text
my swallowing is so genuinely slow and ineffective I can feel it
it's taking 30+ seconds for each of these fries to get to the bottom of my esophagus and they're just sitting at the top of my throat for most of that time. I'm beginning to worry I have esophageal dysmotility. I already have dysphagia it's just poorly studied. it's getting worse :/ fuck you lupus
#systemic lupus erythematosus#physical disability#physically disabled#chronic illness#chronically ill#dysphagia
11 notes
·
View notes
Text
day 1 of weightloss
60 lbs gained in a year. I hate looking in the mirror. I don't recognize myself. tpn has ruined my body. I can't eat or drink but my doctor has taken me off the tpn now. I have a feeding tube but can't tolerate tube feeds. I'm terrified and I know what's to come. I've been here before. 205.0 lbs today. last time I was here I wasn't starting malnourished. I dropped to 107. I don't mind having a small body but I don't feel good when I do. I'm more comfortable in my skin when I'm smaller. this is where I'll be weighing in and documenting my journey.
I have a paralyzed stomach (extremely severe gastroparesis), Ehlers danlos syndrome, hereditary alpha tryptase syndrome, eosinophilic esophagitis, chronic diarrhea, intestinal dysmotility, esophageal dysmotility, vocal cord disfunction, POTS, inappropriate tachycardia, migraine, brain tumor (left cingulate gyrus glioma), intractable nausea and vomiting, and the list continues.
When I first got sick with everything the weight melted off with me doing nothing. Now the pounds packed on and wont stop. I'm assuming bc the tpn. I want them to fall off again but I can't exercise. I literally lay in bed all day otherwise I pass out or dislocate or puke... I just don't want to hate myself when I look in the mirror, but I'm also not in the position to actively try to lose weight. I'm pretty much leaving it up to nature.
So, here we go...
2 notes
·
View notes
Text
A Case of Complementary Treatment for Idiopatic Polymyositis

Abstract
A case of idiopatic polymyositis treated both with conventional and homeopathic complementary treatment is presented, pointing out the main characteristics of the case and showing the advantages in associating both methods; the combination of conventional and complementary therapies made possible the avoidance of tracheostomy for a severe esophageal dysmotility.
Keywords: Idiopatic polymyositis; Esophageal dysmotility; Complementary treatment
Abbreviation: Polymyositis PM
Introduction
Polymyositis (PM) is a systemic disease and one of several idiopathic inflammatory myopathies, together with dermatomyositis and sporadic inclusion body myositis. [1,2] Dysphagia secondary to oropharyngeal and esophageal involvement occurs in about one third of patients and may lead to aspiration pneumonia.
Read More About This Article: https://crimsonpublishers.com/acam/fulltext/ACAM.000673.php
Read More About Crimson Publishers: https://crimsonpublishers.com/
#complementary journals#alternative medicine#crimsonpublishers llc#open access journals#peer review journals
0 notes
Text
best gastroenterologist in adyar
Why would you see a gastroenterologist?
A gastroenterologist is a doctor specialized in diagnosing and treating intestinal problems. Gastroenterologists are sometimes called "GI doctors" because they specialize in conditions that affect the gastrointestinal (GI) system. Gastroenterologists comprehensively understand how the digestive system and its structures work. They primarily treat conditions that affect specific areas of the body, such as:
Stomach
Small intestine
Colon
Rectum
Esophagus
Pancreas
Gallbladder
Liver
Bile ducts
For this you need to consult best gastroenterologist in Adyar!
When to see a gastroenterologist?
Abdominal Pain or Discomfort
Chronic Digestive Issues
Changes in Bowel Habits
GI Disease Screening/Treatment
Endoscopic Procedures
Liver/Gallbladder/Pancreas Concern
Latest Technology related to Gastroenterology
Capsule endoscopy
Single balloon enteroscopy
Endoscopic ultrasound (EUS)
Endoscopic retrograde cholangiopancreatography (ERCP)
High resolution esophageal and anorectal manometry
Hydrogen breath test
What is the job of a gastroenterology specialist?
Liver disease is central focus area of a gastroenterology specialist. Huge number of patients with acute and chronic liver disease (cirrhosis) due to hepatitis B, C, A and alcohol.
The gastroenterology specialists provide advice and suggest measures to the patients with liver disease because of alcohol intake, liver viruses, etc.
Treatment for liver failure and portal hypertension
Treatment for acute &chronic pancreatitis
Treating the upper & lower gastrointestinal bleeding
Oesophageal disorders such as hiatus hernia, reflux dysmotility, etc
Gastric/duodenal disease like gastric ulcer
Intestinal and colorectal diseases like motility disorders, malabsorption, bleeding, infections, irritable bowel disease, colitis, Crohn's disease, etc.
𝐆𝐄𝐂𝐋𝐈𝐍𝐈𝐂&𝐄𝐍𝐃𝐎𝐒𝐂𝐎𝐏𝐘𝐂𝐄𝐍𝐓𝐑𝐄 – Best gastroenterologist in Adyar
This hospital was established to meet the special needs of patients with gastrointestinal diseases. It provides the latest modality of high-quality tertiary services in gastroenterology. The center has a highly qualified medical team of medical professionals led by Dr.S.Ganesh, best gastroenterology specialist in Chennai supported cutting-age equipment such as laparoscopic surgical equipment, video endoscopes, fully equipped ICUs, and highly advanced OT equipped with an image intensifier. Emergency and elective care is given for widespread liver and gastrointestinal diseases from the simplest to the most complex.
0 notes
Link
🍴 Esophageal dysmotility is a condition that affects the muscles in the esophagus, making it difficult to swallow food and liquids. This can lead to discomfort, pain, and even malnutrition. While medication and surgery are common treatments, diet can also play a significant role in managing symptoms. 🥦 A diet that is low in fat, high in fiber, and includes plenty of fruits and vegetables can help reduce symptoms of esophageal dysmotility. Eating smaller, more frequent meals and avoiding foods that are difficult to swallow, such as tough meats and dry bread, can also be beneficial. 🍎 Additionally, it is important to stay hydrated and to avoid drinking alcohol and caffeine, which can irritate the esophagus. Working with a registered dietitian can help individuals with esophageal dysmotility create a personalized diet plan that meets their specific needs and helps manage their symptoms.1. Understanding Esophageal Dysmotility: Causes and SymptomsEsophageal dysmotility occurs when the muscles in the esophagus don't work properly. It can be caused by nerve damage, muscle disorders, or certain medications. Symptoms include difficulty swallowing, chest pain, and heartburn. Treatment options include medication, lifestyle changes, and surgery. 🧐 Common causes of esophageal dysmotility include diabetes, Parkinson's disease, and scleroderma. Certain medications, such as antidepressants and muscle relaxants, can also contribute to the condition. Diagnosis may involve tests such as esophageal manometry or a barium swallow. 🤔 Symptoms of esophageal dysmotility can vary from person to person. Some may experience difficulty swallowing, while others may feel chest pain or heartburn. In severe cases, food may become stuck in the esophagus, leading to choking or aspiration. 🤕 Treatment for esophageal dysmotility depends on the underlying cause and severity of symptoms. Medications such as proton pump inhibitors or muscle relaxants may be prescribed. Lifestyle changes such as eating smaller meals and avoiding trigger foods can also help. Surgery may be necessary in severe cases. 💊 In conclusion, esophageal dysmotility is a condition that affects the muscles in the esophagus. It can be caused by a variety of factors, and symptoms can range from difficulty swallowing to chest pain. Treatment options include medication, lifestyle changes, and surgery. Early diagnosis and treatment can improve outcomes. 🙌2. The Role of Diet in Managing Esophageal DysmotilityEsophageal dysmotility is a condition that affects the muscles in the esophagus, making it difficult to swallow food and liquids. While there is no cure for this condition, managing symptoms through diet can help improve quality of life. Soft, moist foods are easier to swallow than dry, hard foods. Chew food thoroughly and take small bites. Avoid foods that are difficult to swallow, such as tough meats, raw vegetables, and bread. Acid reflux can worsen symptoms of esophageal dysmotility. Avoiding trigger foods and eating smaller, more frequent meals can help reduce acid reflux. Avoid spicy and acidic foods, such as citrus fruits and tomatoes. Limit caffeine and alcohol intake. Elevate the head of your bed to reduce nighttime reflux. Staying hydrated is important for managing esophageal dysmotility. Drinking plenty of water and avoiding carbonated beverages can help prevent dehydration and reduce symptoms. Drink water throughout the day, especially with meals. Avoid carbonated beverages, which can cause bloating and discomfort. Consider drinking warm liquids, such as tea or broth, to help soothe the esophagus. Working with a registered dietitian can help develop a personalized diet plan for managing esophageal dysmotility. Keeping a food diary can also help identify trigger foods and track symptoms. Consult with a registered dietitian for personalized dietary recommendations. Keep a food diary to track symptoms and identify trigger foods. Stay positive and patient. Managing esophageal dysmotility through diet takes time and effort. 3. Foods to Avoid for Esophageal Dysmotility PatientsEsophageal dysmotility patients should avoid certain foods that can worsen their condition. Here are some of the foods to avoid: Acidic foods: Citrus fruits, tomatoes, and vinegar can irritate the esophagus. Spicy foods: Hot peppers, chili powder, and curry can cause heartburn and reflux. Fatty foods: Fried foods, high-fat meats, and creamy sauces can slow down digestion. Carbonated drinks: Soda, beer, and sparkling water can cause bloating and reflux. Caffeinated drinks: Coffee, tea, and energy drinks can relax the esophageal sphincter. Alcoholic drinks: Wine, beer, and spirits can irritate the esophagus and stomach. It's also important to avoid eating large meals, eating too quickly, and lying down after eating. Instead, try to eat smaller, more frequent meals, chew your food well, and stay upright for at least 30 minutes after eating. Consult with your doctor or a registered dietitian to create a personalized diet plan that meets your nutritional needs and avoids triggering your symptoms. 🍎🥦🥕4. Recommended Nutrients and Supplements for Esophageal DysmotilityEsophageal dysmotility can cause difficulty swallowing and other digestive issues. Here are some recommended nutrients and supplements to help manage symptoms: Probiotics: Help maintain a healthy gut microbiome. Choose a high-quality supplement or consume fermented foods like yogurt and kefir. Magnesium: Can help relax the esophageal muscles. Consult with a doctor before taking supplements. Vitamin D: Can improve muscle function. Get your daily dose from sunlight or a supplement. Omega-3 fatty acids: Can reduce inflammation. Consume fatty fish or take a supplement. Fiber: Can aid digestion and prevent constipation. Choose whole grains, fruits, and vegetables. It's important to note that supplements should not replace a healthy diet and lifestyle. Consult with a healthcare professional before taking any new supplements. Additionally, managing stress and maintaining a healthy weight can also improve symptoms of esophageal dysmotility. Remember to always prioritize your health and well-being. 🌟5. Meal Planning Tips for Esophageal Dysmotility PatientsEsophageal dysmotility patients need to plan their meals carefully to avoid discomfort and complications. Choose soft, moist foods that are easy to swallow. Avoid foods that are tough, dry, or crunchy. Eat slowly and take small bites. Stay hydrated by drinking plenty of water. It's important to avoid trigger foods that can worsen symptoms. Avoid spicy, acidic, and fatty foods. Limit caffeine and alcohol intake. Avoid carbonated drinks and chewing gum. Choose low-fat, low-acid foods. Try to eat smaller, more frequent meals throughout the day. Avoid eating large meals that can put pressure on the esophagus. Plan meals ahead of time to ensure balanced nutrition. Consult with a registered dietitian for personalized advice. Consider using a food journal to track symptoms and identify trigger foods. Don't eat within three hours of bedtime to reduce the risk of reflux. Elevate the head of your bed to prevent nighttime reflux. Wait at least two hours after eating before lying down. Avoid late-night snacking. Consider eating a light snack before bedtime if needed. Remember to chew well and take your time when eating. Take breaks between bites to allow the esophagus to clear. Use a straw to make drinking easier. Try pureed or blended foods if swallowing is difficult. Stay positive and experiment with new recipes and foods. 6. Lifestyle Changes to Improve Esophageal Dysmotility SymptomsEsophageal dysmotility can be improved by making certain lifestyle changes. Here are some tips: Eat smaller meals to avoid overloading the digestive system. Chew food thoroughly to make it easier to swallow. Avoid eating before bedtime to reduce reflux symptoms. Quit smoking to reduce the risk of esophageal cancer. Avoid alcohol and caffeine as they can irritate the esophagus. Stay hydrated to keep the digestive system functioning properly. Exercise regularly to improve overall health and digestion. Yoga and meditation can also help reduce stress and improve digestion. Consider working with a registered dietitian to develop a healthy eating plan that meets your individual needs. They can also help you identify trigger foods that worsen symptoms. It's important to maintain a healthy weight as obesity can worsen esophageal dysmotility. Speak with your doctor about safe and effective weight loss strategies. Finally, be patient and consistent with lifestyle changes. It may take time to see improvement, but the effort is worth it. 🍎🥦🏋️♀️💧 In conclusion, managing esophageal dysmotility with diet is possible. A low-fat, low-acid, and low-fiber diet can help reduce symptoms. It's important to avoid trigger foods and eat smaller, more frequent meals. Remember to stay hydrated and chew food thoroughly. Consult with a healthcare provider and a registered dietitian for personalized recommendations. With the right diet and lifestyle changes, you can improve your quality of life. 🍎🥦🍇 https://fastdiet.net/managing-esophageal-dysmotility-with-diet/?_unique_id=6480b2ec3c08e
#Uncategorised#Dietforesophagealdysmotility#Esophagealdysmotilitydietplan#Esophagealdysmotilitymanagement#Esophagealdysmotilitynutritiontips#Esophagealdysmotilitytreatment
0 notes
Photo
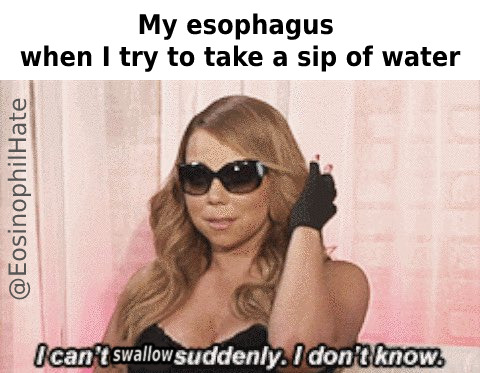
#dysphagia#esophageal dysmotility#eosinophilic esophagitis#chronic illness#chronically ill#chronic illness meme#EoE#eosinophilic gastrointestinal disease#eosinophilic gastrointestinal disorders#eosinophilic disorders#eosinophilic disease#fibromyalgia#esophagus#esophageal motility disorders#My esophagus doesn't work#GERD#esophagitis#achalasia#neurological disorder
171 notes
·
View notes
Note
Theres motility specialistist?!? <- Guy who has been diagnosed with gp for 7 years. I was diagnosed at 14 and had a hard enough time finding a gastroenterologist that would see me, and then I turned 18 during COVID and I just... gave up on professional treatment for a while. To be fair I only have a mild to moderate case (I think) but damn...
Yes! They specialize in esophageal, gastric, and intestinal dysmotility! I highly encourage seeing if there are any in your area.
If you have the luxury of travel, some clinics will do one in-person appointment and then do the rest via telehealth. They can be put through out of network exceptions if you’re in the US. Mayo Clinic and Cleveland Clinic have the leading motility clinics that I’m aware of, but there are other motility specialists.
List of US Neurogastroenterologists and Motility Specialists (r/gastroparesis)
G-PACT list of US Motility Doctors
The Association of Gastrointestinal Motility Disorders also has lists of physicians, centers, dietitians, and other experts from around the world.
22 notes
·
View notes
Text
Dysphagia is the umbrella term for difficulty swallowing. Many different things can cause dysphagia, from MS to achalasia to esophageal spasms. A lot of different things can be covered under the term.
Me? I have 'severe esophageal dysmotility' which is description and not a diagnosis - because we still don't know why this started up over 2 years ago 😅 I have dubbed it "throat no work disease" for the time being lmao
* fingers guns * and its not only elderly people who deal with dysphagia. I am 23 and have severe problems with my throat muscles. When i have a bad flare up i cant even get water down properly~ Such is the way of existence ✨️
#its rare disease day apparently so hey on topic to talk about XD#rare for me as in “literarly no idea whats going” level lmao#disability#medical cw
15 notes
·
View notes
Text
Please help me.
I'm a disabled 22 year old who is in 10k+ worth of medical debt and can no longer afford to buy food or my prescriptions that keep me alive.. Any help you can offer means the world to me. I’m really struggling and my health is starting to decline fast, Ive just been told after three appeals my disability hearing wont be for a year and a half. In my state you have to be working/volunteering at least 24 hours a WEEK to qualify for food stamps (or be on disability). I dont know what to do anymore... I’m currently on 10 different medications (20 a day when certain ones are multiplied), prescribed vitamins, daily infusions through my port-a-cath for fluids, I get a cocktail infusion for muscle spasms and I’ll be starting Ketamine infusions for my severe pain from multiple of my diseases.
Please read my full story on gofundme to find out more including my illnesses names, treatments, mobility aids I use, etc..
Thank you so much for taking your time to read this, reblogging and donating.
http://www.gofundme.com/ellatherese
http://www.paypal.me/tachypomerleau
#chronic illness#ehlers danlos syndrome#dysautonomia#autonomic dysfunction#autonomic disorder#autoimmune disease#asthma#postural orthostatic tachycardia syndrome#neurocardiogenicsyncope#orthostatic hypotension#orthostatic intolerance#inappropriate sinus tachycardia#esophageal dysmotility#dysmotility of the esophagus#chronic pain disorder#fibromyalgia#chronic fatigue syndrome#myalgic encephalomyelitis#myalgic encephalopathy#mcas#mcad#allergies#gofundme#disabled#disability#chronically ill#spoonie#ibs#gastritis#gerd
1 note
·
View note
Text
Double Booked: My Busy Day of Disappointments
Double Booked: My Busy Day of Disappointments
I went to another appointment at my urologist’s office. It was originally scheduled as a bladder instillation, but last week’s instill gave me a massive Urinary Tract Infection (UTI). We discussed my options, which were few to begin with and decided to continue with the series of instillations before moving onto one of the surgical options. I was really disappointed to learn that there is only…

View On WordPress
#autoimmune#autoimmune disease#autoimmune flare#autoimmune life#autoimmune warrior#chronic disease#chronic illness#chronic pain#crest syndrome#esophageal dysmotility#esophagram#flare#ic flare#interstitial cystitis
0 notes
Text
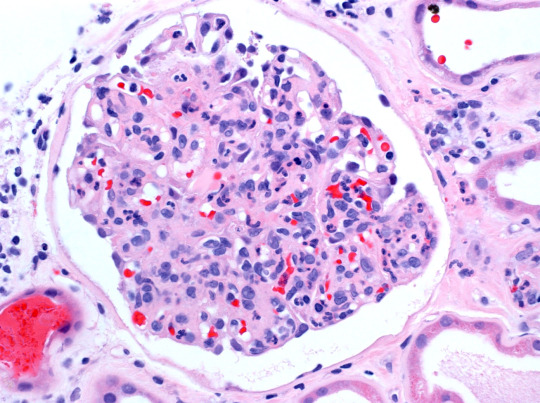
Eosinophilic Esophagitis Disease Is Now A Leading Cause Of Food Impaction And Dysphagia
Eosinophilic Esophagitis
Due to a compromised mucosal barrier in the oesophagus and a reverse immunological response mediated by Th2 interleukins, esophageal fissures/lesions, fibrosis, and dysmotility develop in Eosinophilic Esophagitis. There is a 7% chance that eosinophilic esophagitis will be genetically inherited. Eosinophilic esophageal disease is now a major contributor to food impaction and dysphagia due to its rise in prevalence in recent years. Because it is a chronic inflammatory disease, patients must continue to be managed in order to prevent symptoms from getting worse. EoE can be treated with anything from medication to a strict elemental diet. Foods that cause inflammation may need to be cut out of the diet. Their buildup at a specific site on the body indicates the presence of allergic disorders.
The patient's age may have an impact on the symptoms, which might vary greatly. Asthma instances linked to the condition are rising, and so are awareness of it and diagnosis rates. People with this illness may also develop eczema in addition to the symptoms.An excessive amount of eosinophils (a specific type of white blood cell) are found in the oesophagus in Eosinophilic Esophagitis a chronic immunological illness of the digestive system. Food travels through the oesophagus, a tube, from the mouth to the stomach. The term "allergic esophagitis" also applies to eosinophilic esophagitis. The immune system of the body includes eosinophils. They are essential for immune system control and provide defence against some illnesses. Their buildup at a specific site on the body indicates the presence of allergic disorders.
Explore More About This Blog@ https://bit.ly/3ORGDqb
3 notes
·
View notes
Text
I do not recommend the Barium swallow test. The three stages of swallowing three glasses of white chalky liquid, swallowing barium pop rocks, and then finishing it off with a barium pills cocktail was enough to never want me to swallow anything ever again. Anywho, I’ve got some narrowing of tubes, a Hiatal hernia, and esophageal dysmotility. You know what is annoying that the hospital has an app that gives you instant results which gives you weeks to ponder what ailment will eventually kill you while you wait to talk to the doctor. Just another thing to add to my health chart.
11 notes
·
View notes