#double mastectomy
Explore tagged Tumblr posts
Text
I think more cis butches who want top surgery should get it, not just because it pisses off TERFs and that's funny, but because it helps normalize a post double mastectomy body on women. ya know, the thing women with breast cancer dread to have? because as a society we treat breasts as a womanly body part, and when a woman gets a literal lifesaving procedure it's treated as a tragedy cuz they're 'mutilated' now? yeah, I don't know, I think normalizing top surgery in women is a Good Thing. treating post op results from a double mastectomy as "mutilation" is super fucked up all around and is yet another example of how TERF rhetoric hurts cis women too. TERFs are so fucking stupid that they consistently harm the "real" women they claim to care so much about. shocker.
995 notes
·
View notes
Text
i want y’all to know i got my top surgery at ~270 pounds and it looks fucking fine like you are not too fat to get top surgery and have it be flat and nice and feel better
#lost 17 pounds of tiddy that day#body positive#body positivity#fat liberation#fat positvity#top surgery#double mastectomy#bilateral mastectomy#trans men#trans man#trans#trans masc#trans positivity#queer positivity#ok to reblog#og#transblr
6K notes
·
View notes
Text
By: Beth Bourne
Published: Feb 27, 2024
Kaiser gender specialists were eager to approve hormones and surgeries, which would all be covered by insurance as “medically necessary.”
On September 6, 2022, I received mail from my Kaiser Permanente Davis Ob-Gyn reminding me of a routine cervical screening. The language of the reminder stood out to me: “Recommended for people with a cervix ages 21 to 65.” When I asked my Ob-Gyn about this strange wording, she told me the wording was chosen to be “inclusive” of their “transgender” and “gender fluid” patients.
Based on this response, several thoughts occurred to me. Could I expose the medical scandal of “gender-affirming care” by saying and doing everything my daughter and other trans-identifying kids are taught to do? Would there be the type of medical safeguarding and differential diagnosis we would expect in other fields of medicine, or would I simply be allowed to self-diagnose and be offered the tools (i.e. hormones and surgeries) to choose my own gender adventure and become my true authentic self?
If I could demonstrate that anyone suffering from delusions of their sex, self-hatred, or identity issues could qualify for and easily obtain body-altering hormones and surgeries, all covered by insurance as “medically necessary” and potentially “life-saving” care, then maybe people would finally wake up. I certainly had.
I was prepared for failure. I wasn’t prepared for how easy success would be.
* * *
I am a 53-year-old mom from Davis, CA. My daughter began identifying as a transgender boy (social transition) and using he/him pronouns at school during 8th grade. Like several of her peers who also identified as trans at her school, my daughter was a gifted student and intellectually mature but socially immature. This shift coincided with her school’s sudden commitment to, and celebration of, a now widespread set of radical beliefs about the biology of sex and gender identity.
She “came out” as trans to her father (my ex-husband) and me through a standard coming-out letter, expressing her wish to start puberty blockers. She said she knew they were safe, citing information she had read from Planned Parenthood and the World Professional Association for Transgender Health (WPATH). To say I was shocked would be an understatement. I was also confused because this announcement was sudden and unexpected. While others quickly accepted and affirmed my daughter’s new identity, I was apprehensive and felt the need to learn more about what was going on.
Events began escalating quickly.
During a routine doctor’s visit scheduled for dizziness my daughter said that she was experiencing, the Kaiser pediatrician overheard her father using “he/him” pronouns for our daughter. The pediatrician seemed thrilled, quickly asking my daughter about her “preferred pronouns” and updating her medical records to denote that my daughter was now, in fact, my son. The pediatrician then recommended we consult the��Kaiser Permanente Oakland Proud pediatric gender clinic, where she could get further information and (gender affirming) “treatment.” Now I was the one feeling dizzy.
As I began educating myself on this issue, I discovered that this phenomenon—minors, most often teen girls, suddenly adopting trans identities—was becoming increasingly widespread. It even had a name: rapid onset gender dysphoria, or ROGD. Thankfully, after learning about the potential side-effects of blockers and hormones, my ex-husband and I managed to agree not to consent to any medical interventions for our daughter until she turned 18 and would then be able to make such decisions as an adult.
Over the past five years, my daughter’s identity has slowly evolved in ways that I see as positive. Our bond, however, has become strained, particularly since I began publicly voicing my concerns about what many term as “gender ideology.” Following my daughter’s 17th birthday family celebration, she sent me an email that evening stating she would be cutting off contact with me.
While this estrangement brought me sorrow, with my daughter living full-time with her father, it also gave me the space to be an advocate/activist in pushing back on gender identity ideology in the schools and the medical industry.
I decided to go undercover as a nonbinary patient to show my daughter what danger she might be putting herself in���by people who purport to have her health as their interest, but whose main interest is in medically “affirming” (i.e., transitioning) whoever walks through their door. I am at heart a mother protecting her child.
* * *
My daughter’s sudden decision to become a boy was heavily on my mind in early September of 2022, when mail from my Kaiser Permanente Davis Ob-Gyn reminded me of a routine cervical screening with “Recommended for people with a cervix ages 21 to 65.” I was told that the wording was chosen to be “inclusive” of transgender and “gender fluid” patients.
Throughout the whole 231-day process of my feigned gender transition, the Kaiser gender specialists were eager to serve me and give me what I wanted, which would all be covered by insurance as “medically necessary.” My emails were returned quickly, my appointments scheduled efficiently, and I never fell through the cracks. I was helped along every step of the way.
Despite gender activists and clinicians constantly claiming that obtaining hormones and surgeries is a long and complex process with plenty of safety checks in place, I was in full control at every checkpoint. I was able to self-diagnose, determine how strong a dose of testosterone I received and which surgeries I wanted to pursue, no matter how extreme and no matter how many glaring red flags I purposefully dropped. The medical workers I met repeatedly reminded me that they were not there to act as “gatekeepers.”
I was able to instantly change my medical records to reflect my new gender identity and pronouns. Despite never being diagnosed with gender dysphoria, I was able to obtain a prescription for testosterone and approval for a “gender-affirming” double mastectomy from my doctor. It took only three more months (90 days) to be approved for surgery to remove my uterus and have a fake penis constructed from the skin of my thigh or forearm. Therapy was never recommended.
Critics might dismiss my story as insignificant on the grounds that I am a 53-year-old woman with ample life experience who should be free to alter her body. However, this argument for adult bodily autonomy is a standard we apply to purely cosmetic procedures like breast implants, liposuction, and facelifts, not “medically necessary” and “lifesaving” treatments covered by health insurance. Or interventions that compromise health and introduce illness into an otherwise healthy body. And especially not for children.
My story, which I outline in much more detail below, should convince any half-rational person that gender medicine is not operating like any other field of medicine. Based on a radical concept of “gender identity,” this medical anomaly preys upon the body-image insecurities common among pubescent minors to bill health insurance companies for permanent cosmetic procedures that often leave their patients with permanently altered bodies, damaged endocrine systems, sexual dysfunction, and infertility.
* * *
Detailed Timeline of Events
On October 6, 2022, I responded to my Ob-Gyn’s email to tell her that, after some thought, I’d decided that maybe the label “cis woman” didn’t truly reflect who I was. After all, I did have some tomboyish tendencies. I told her I would like my records to be changed to reflect my newly realized “nonbinary” identity, and that my new pronouns were they/them. I also voiced my desire to be put in touch with an endocrinologist to discuss starting testosterone treatment.
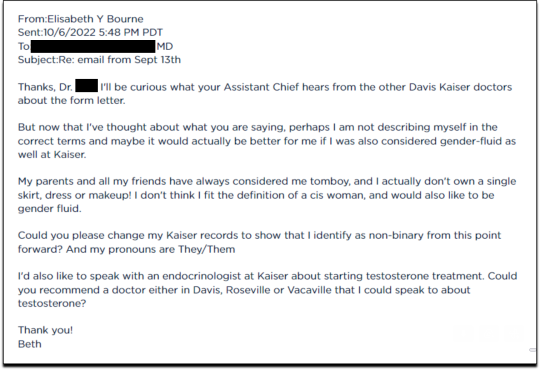
Fifteen minutes later I received an email from another Kaiser doctor informing me that my medical records had been changed, and that once my primary doctor returned to the office, I’d be able to speak with her about hormone therapy.
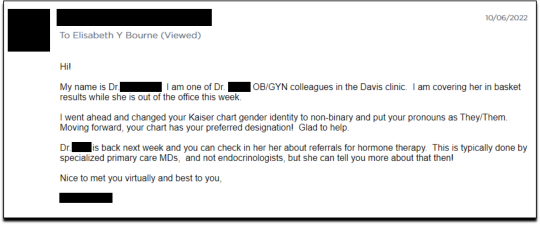
I responded the following day (October 7, 2022), thanking her for changing my records, and asking if she could connect me with someone who could help me make an appointment for “top surgery” (i.e., a cosmetic double mastectomy) because my chest binder was rather “uncomfortable after long days and playing tennis.”
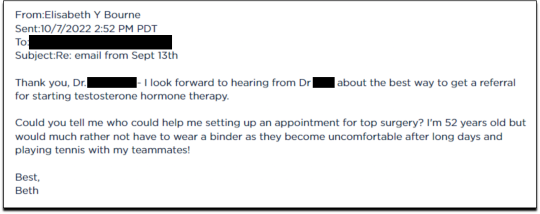
She told me to contact my primary care MD to “get things rolling,” and that there were likely to be “preliminary evaluations.”
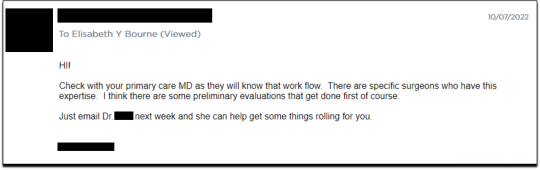
Six days after contacting my primary care MD for a referral, I received an email from one of Kaiser’s gender specialists asking me to schedule a phone appointment so she could better understand my goals for surgery, so that I could get “connected to care.” This call to review my “gender affirming treatment options and services” would take 15-20 minutes, after which I would be “booked for intake,” allowing me to proceed with medical transition.
This wasn’t an evaluation of whether surgical transition was appropriate, it was simply a meeting for me to tell them what I wanted so that they could provide it.
On October 18, I had my one and only in-person appointment in preparation for top surgery. I met in Davis with my primary care physician, Dr. Hong-wen Xue. The assessment was a 10-minute routine physical exam that included blood tests. Everything came back normal. Notably, there was not a single question about why I wanted top surgery or cross-sex hormones. Nor was there any discussion of the risks involved with these medical treatments.
The following week, on October 24, I had a phone appointment with Rachaell Wood, MFT, a gender specialist with Kaiser Sacramento. The call lasted 15 minutes and consisted of standard questions about potential drug use, domestic violence, guns in the house, and whether I experienced any suicidal thoughts. There were no questions from the gender specialist about my reasons for requesting a mastectomy or cross-sex hormones, or why I suddenly, at 52, decided I was “nonbinary.”
After the call, Kaiser emailed me instructions about how to prepare for my pre-surgery intake video appointment to evaluate my mental health, scheduled to take place on November 15. The email stated that prior to my appointment, I should research hormone risks on the WPATH website, and to “research bilateral mastectomy and chest reconstruction surgery risks and recovery” on Kaiser’s website.
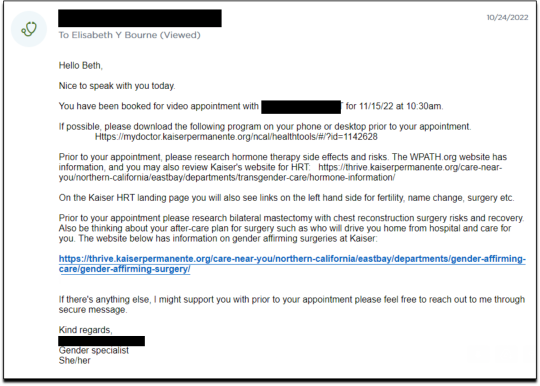
I decided to request a “gender-affirming” double mastectomy and phalloplasty. Kaiser sent me a sample timeline for gender transition surgery preparation (see below) that you can use as a reference for the process. I also asked for a prescription for cross-sex hormones (testosterone) as needed and recommended by Kaiser.
[ Source: Kaiser Permanente, Top Surgery - EXPLORING YOUR SURGICAL OPTIONS ]
Pre-Surgery Mental Health Video Appointment, Part I
This “Mental Health Visit” assessment was conducted over Zoom. The Kaiser gender specialist started with questions addressing my marital status, race, gender identity, and other demographics. She asked whether I was “thinking of any other surgeries, treatments in the future.” The list she read included “gender-affirming” hysterectomies, bottom surgeries such as metoidioplasty and phalloplasty, vocal coaching, support groups, and body contouring. “Anything else you might be interested in doing?” she asked. I said that I’d perhaps be interested in body contouring. I was also assured that all the procedures would be covered by insurance because they were considered “medically necessary.”
I dropped in several red flags regarding my mental health to see the reaction, but all were ignored. For instance, I revealed that I had PTSD. When the therapist asked me about whether I had experienced any “childhood trauma,” I explained that I grew up in Mexico City and had been groped several times and had also witnessed men masturbating in public and had been grabbed by men in subways and buses. “I was a young girl, so [I had] lots of experiences of sexual harassments, sexual assault, just the kind of stuff that happens when you are a girl growing up in a big city.” “So, you know,” I finished, “just the general feeling that you are unsafe, you know, in a female body.”
The therapist did not respond to my disclosure that trauma could be the cause of my dysphoria. Instead of viewing this trauma as potentially driving my desire to escape my female body through hormones and surgery, she asked whether there is anything “important that the surgery team should be aware of” regarding my “history of trauma,” such as whether I’d be comfortable with the surgeon examining and marking my chest prior to surgery.
When asked about whether I had had any “psychotic symptoms,” I told her that while I had had no such symptoms, my mother had a delusional nervous breakdown in her 50s because she had body dysmorphia and became convinced she had a growth on her neck that needed to be removed. I told her that my mother was then admitted to an inpatient hospital for severe depression. I asked her whether she ever sees patients with body dysmorphia and whether I could have potentially inherited that from my mother. She told me that psychosis was hereditary, but that it was “highly unlikely” that there was any connection between body dysmorphia and gender dysphoria.
I enthusiastically waved more mental health red flags, waiting to see if she would pick up on any of them.
I’m just wondering if my feelings, or perseverating, or feeling like these breasts make me really unhappy and I just don’t want them anymore!...I’m just not sure if that’s a similar feeling to body dysmorphia? How do you decide which one is gender dysphoria and general body dysmorphia, and just not liking something about your body? Feeling uncomfortable with your body? And I did have an eating disorder all through college. I was a distance runner in college so I had bulimia and anorexia, you know. So I don’t know if that’s related to gender dysphoria?
The therapist replied, “I completely appreciate your concerns, but I am going to ask you questions about your chest, about your expectations. And then I’ll be able to give you an assessment.” She also said the main difference between my mom’s situation and mine was that my mom didn’t really have a growth on her neck, whereas it’s “confirmed” that I actually have “chest tissue.” Furthermore, she said that while “historically there has been all this pressure on patients to be like ‘Are you really, really sure you want hormones? Are you 100% sure?’ We are a little more relaxed.” She continued, “As long as you are aware of the risks and the side-effects, you can put your toe in the water. You can stop ‘T’ [testosterone], you can go back and do it again later! You can stop it! You can stop it! You know what I mean?”
Because we ran out of time, I scheduled a follow-up phone meeting on December 27, 2022 with a different gender specialist to complete my mental health assessment for top surgery.
Pre-Surgery Mental Health Video Appointment, Part II
During this meeting, Guneet Kaur, LCSW, another Kaiser gender specialist (she/her/they/them pronouns) told me that she regretted the “gatekeeping vibe” of the meeting but assured me that since I have been “doing the work,” her questions are essentially just a form of “emotional support” before talking with the medical providers.
She asked me about what I’d been “looking into as far as hormones.” I told her that I’d be interested in taking small doses of testosterone to counterbalance my female feelings to achieve “a feeling that’s kind of neutral.”
When she asked me about me “not feeling like I match on the outside what I feel on the inside,” I dropped more red flags, mentioning my aversion to wearing dresses and skirts.
I don’t own a single dress or a skirt and haven't in 20 years. I think for me it’s been just dressing the way that’s comfortable for me, which is just wearing, jeans and sweatshirts and I have a lot of flannel shirts and, and I wear boots all the time instead of other kinds of shoes. So I think it’s been nice being able to dress, especially because I work from home now most of the time that just a feeling of clothing being one of the ways that I can feel more non-binary in my everyday life.
She responded, “Like having control over what you wear and yeah. Kind of that feeling of just, yeah, this is who I am today. That’s awesome. Yeah.”
She then asked me to describe my dysphoria, and I told her that I didn’t like the “feeling of the female form and being chesty,” and that because I am going through menopause, I wanted to start taking testosterone to avoid “that feeling of being like this apple-shaped older woman.” “Good. Okay, great,” she responded, reminding me that only “top surgery,” not testosterone, would be able to solve my chest dysphoria. (Perhaps it was because all these meetings were online, they didn’t notice I’m actually fit and relatively slender at 5’-5” and 130 pounds, and not apple-shaped at all.)
She told me that we had to get through a few more questions related to my medical history before “we can move on to the fun stuff, which is testosterone and top surgery.”
The “fun stuff” consisted of a discussion about the physical and mood changes I could expect, and her asking me about the dose of testosterone I wanted to take and the kind of “top surgery” technique I’d prefer to achieve my “chest goals.” She told me that all or most of my consultations for surgeries and hormones would be virtual.
The gender specialist told me after the appointment, she would submit my referral to the Multi-Specialty Transitions Clinic (MST) team that oversees “gender expansive care.” They would follow up to schedule a “nursing call” with me to review my medical history, after which they’d schedule my appointment with a surgeon for a consultation. Her instructions for this consultation were to “tell them what you’re wanting for surgery and then they share with you their game plan.”
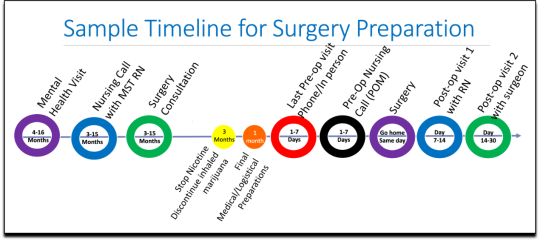
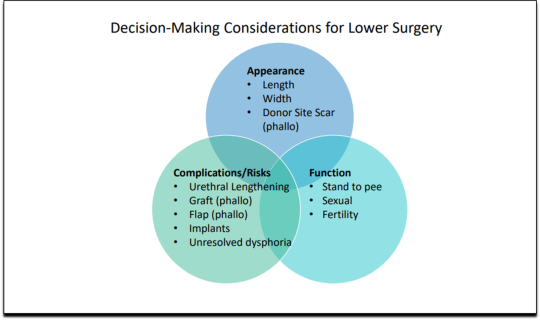
[ Decision-making slide to help me identify my goals for top surgery–flat chest, nipple sensation, or minimal scarring. Source: Kaiser Permanente, Top Surgery - EXPLORING YOUR SURGICAL OPTIONS ]
She told me that Kaiser has a team of plastic surgeons who “only work with trans and nonbinary patients because there’s just so much need for them.” She asked about my priorities for chest surgery, such as whether I value flatness over nipple sensation. I learned about double incision top surgery with nipple grafts, as well as “keyhole,” “donut,” “buttonhole,” and “Inverted-T” top surgeries.
By the end of the hour-long appointment, I had my surgery referral and was ready for my “nursing call” appointment.
Nursing call with Nurse Coordinator from the Transgender Surgery and Gender Pathways Clinic at Kaiser San Francisco
On January 19, 2023, I had my nursing call with the Nurse Coordinator. He first said that “the purpose of this call is just for us to go through your chart together and make sure everything’s as accurate as possible.” Once that was done, my referral would be sent to the surgeon for a consultation.
He asked me about potential allergies and recreational drug use, and verified that I was up to date on mammograms, pap smears, and colon cancer screenings, as well as vaccines for flu and COVID. I verified my surgical history as well as my current medications and dietary supplements.
He told me about a “top surgery class” available for patients where one of the Kaiser surgeons “presents and talks about surgical techniques and options within top surgery,” and includes a panel of patients who have had top surgery. I signed up for the February 8th class.
Within 10 minutes he told me that he had “sent a referral to the plastic surgery department at Kaiser Sacramento,” and that I should be hearing from them in the next week or two to schedule a consultation.
Appointment for Testosterone
On January 27, I had a 13-minute online appointment with a primary care doctor at Kaiser Davis to discuss testosterone. The doctor verified my name and preferred pronouns, and then directly asked: “So, what would you like to do? What kind of physical things are you looking for?”
I told her I wanted facial hair, a more muscular and less “curvy” physique, and to feel stronger and androgynous. She asked me when I wanted to start, and I told her in the next few months. She asked me if I was menopausal, whether I had ovaries and a uterus, although that information should have been on my chart.
The doctor said she wanted me to come in to get some labs so she could check my current estrogen, testosterone, and hemoglobin levels before starting hormones. Then “we'll set the ball in motion and you'll be going. We’ll see you full steam ahead in the direction you wanna go.”
That was it. I made an appointment and had my lab tests done on February 12. My labs came back on February 14, and the following day, after paying a $5 copay at the Kaiser pharmacy, I picked up my testosterone pump. That was easy!
Top Surgery Consultation
On the same day I received my labs, I had a Zoom surgery consultation with Karly Autumn-Kaplan, MD, Kaiser Sacramento plastic surgeon. This consultation was all about discussing my “goals” for surgery, not about whether surgery was needed or appropriate.
I told the surgeon that I wanted a “flatter, more androgynous appearance.” She asked me some questions to get a better idea of what that meant for me. She said that some patients want a “male chest,” but that others “want to look like nothing, like just straight up and down, sometimes not even nipples.” Others still wanted their chest to appear slightly feminine and only “slightly rounded.” I told her that I’d like my chest to have a “male appearance.”
“What are your thoughts about keeping your nipples?” she asked. “Are you interested in having nipples or would you like them removed?” I told her that I’d like to keep my nipples, but to make them “smaller in size.” She asked me if I’d like them moved to “the edge of the peck muscle” to achieve “a more male appearance.” I said yes.
I was asked to show my bare chest from the front and side, which I did. Then she asked me how important it was for me to keep my nipple sensation. I replied that it was important unless it would make recovery more difficult or there were other associated risks. She highlighted the problem with the free nipple graft, saying that removing the nipple to relocate it means “you're not gonna have sensation in that nipple and areola anymore.” However, some nipple sensation could be preserved by keeping it attached to “a little stalk of tissue” with “real nerves going to it,” but that would require leaving more tissue behind. I told her I’d go for the free nipple graft to achieve a flatter appearance. It was also suggested I could skip nipple reconstruction entirely and just get nipples “tattooed” directly onto my chest.
She told me I was “a good candidate for surgery,” and put me on the surgery wait list. She said that the wait time was between three and five months, but a cancellation could move me up to a sooner date. Also, if I wanted surgery as soon as possible, I could tell the surgery scheduler that I’d be willing to have any of the other three surgeons perform my mastectomy. Outpatient top surgery would cost me a copay of $100.
They contacted twice, in February and March, notifying me of cancellations. If I had accepted and shown up on those dates, they would have removed my breasts. This would have been less than five months from the time I first contacted Kaiser to inform them of my new “nonbinary” gender identity.
How Far Can I Go?
I decided to see how easy it would be for me to get approved for a phalloplasty. Known euphemistically as “bottom surgery,” phalloplasty is the surgical creation of an artificial penis, generally using tissue from the thigh or arm.
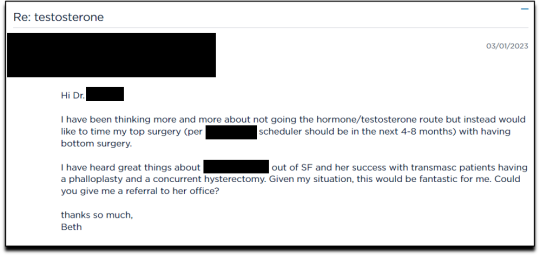
I sent an email on March 1, 2023, requesting to have a phalloplasty and concurrent hysterectomy scheduled alongside my mastectomy.
Two weeks later, on March 16th, I had a 16-minute phone call with a gender specialist to discuss my goals for bottom surgery and obtain my referral.
During the call, I explained to the specialist that I wasn’t sure about taking testosterone anymore because I was already quite athletic and muscular, and that taking testosterone didn’t make much sense to me. Instead, I wanted bottom surgery so that I wouldn’t feel like my “top” didn’t match my “bottom.” I told her:
But what I really wanted was to have bottom surgery. So this way when I have my top surgery, which sounds like it could be very soon, that I’ll be aligned, that I won’t have this sense of dysphoria with one part of my body and the other part feeling like it matched who I am. So yeah. So I just did a little bit more research into that. And I looked at the resources on the Kaiser page for the MST clinic and I think I know what I want, which is the hysterectomy and then at the same time or soon after to be able to have a phalloplasty.
I told her that I wanted to schedule the top and bottom surgery concurrently so that I wouldn’t have to take more time off work and it would save me trips to San Francisco or Oakland, or wherever I had to go for surgery.
None of this gave the gender specialist pause. After a brief conversation about some online resources to look over, she told me that she would “submit the referral now and we’ll get this ball rolling.”
Bottom surgery would cost me a copay of $200, which included a couple of days in the hospital for recovery.
Phalloplasty Surgical Consultation with Nurse Coordinator
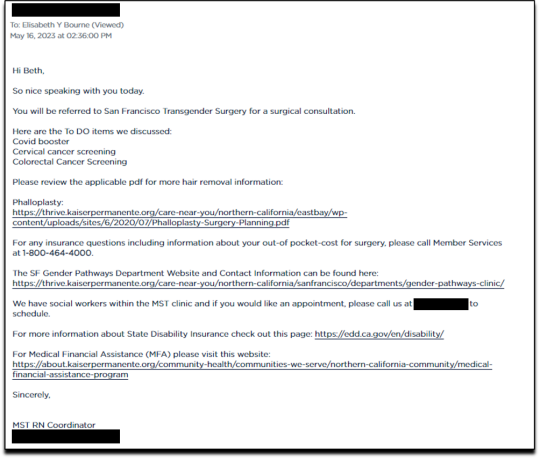
On May 16, 2023, I had a short surgical consultation with a nurse coordinator to go through my medical history. This was similar to the consultation for top surgery but included information about hair removal procedures for the skin on my “donor site” that would be fashioned into a makeshift penis. They also went over the procedures for determining which donor site—forearm or thigh—was more viable.
After only 15 minutes, she submitted my referral to the surgeon for another surgical consultation.
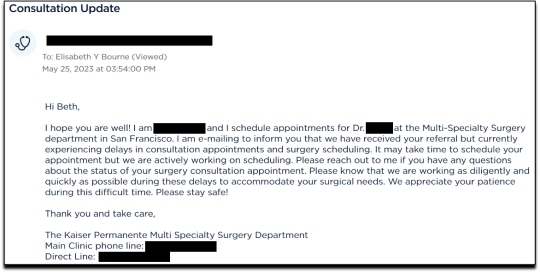
On May 25 I received an email from my phalloplasty surgeon’s scheduler, informing me that they have received my referral and are actively working on scheduling, but that they are experiencing delays.
I ended my investigation here once I had the referral for the top and bottom surgery. I never used my testosterone pump.
Final Thoughts
In fewer than 300 days, based on a set of superficial and shifting thoughts about my gender and my “embodiment goals” triggered by the mere mention of “gender” in a form letter from my primary care physician, and driven by what could only be described as minor discomforts, Kaiser Permanente’s esteemed “multi-disciplinary team” of “gender specialists” was willing, with enthusiasm—while ignoring mental health concerns, history of sexual trauma, and rapidly escalating surgical requests—to prescribe life-altering medications and perform surgeries to remove my breasts, uterus, and vagina, close my vaginal opening, and attempt a complex surgery with high failure and complication rates to create a functionless representation of a penis that destroys the integrity of my arm or thigh in the process.
This describes the supposedly meticulous, lengthy, and safety-focused process that a Kaiser patient must undergo to embark on a journey to medically alter their body. No clinician questioned my motivations. No one showed concern that I might be addressing a mental health issue through radical and irreversible interventions that wouldn’t address my amorphous problems. There were no discussions about how these treatments would impact my long-term health, romantic relationships, family, or sex life. I charted the course. The clinicians followed my lead without question. The guiding issue was what I wanted to look like.
No other medical field operates with this level of carelessness and disregard for patient health and welfare. No other medical field addresses issues of self-perception with surgery and labels it “medically necessary.” No other medical field is this disconnected from the reality of the patients it serves.
Kaiser has traded medicine for ideology. It’s far beyond time we stop the ruse of considering “gender-affirming” interventions as anything approaching medical care.
This isn’t the first time Kaiser Permanente has been in the news for completely disregarding medical safeguards in the name of “gender-affirming care.” As girls, Chloe Cole and Layla Jane became convinced that they were born in the wrong body and were actually boys on the inside. Doctors at Kaiser ignored their underlying conditions and instead prescribed testosterone and removed their breasts. Both Cole and Jane have since detransitioned and are currently suing Kaiser.
The fact that children and vulnerable adults are being exploited in this massive ideological experiment is not just tragic; it’s deeply disturbing, especially considering it has evolved into a billion-dollar industry.
I hope that by sharing my story, I can bring more focused scrutiny to the medical scandal unfolding not just at Kaiser but also at medical centers and hospitals across the Western world. These institutions have completely abandoned medical safeguards for patients who claim to be confused about their “gender,” and I aim to awaken more parents and assist them in protecting their children.
--
==
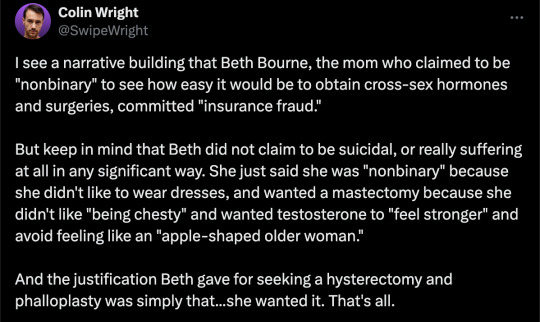
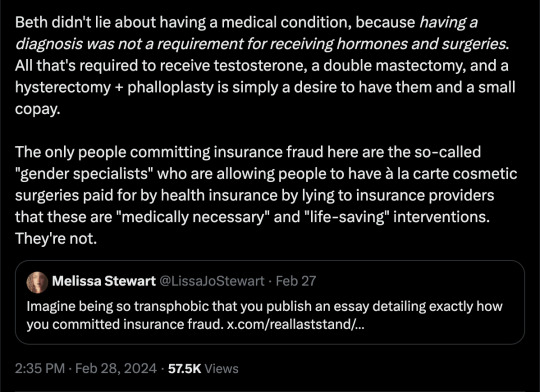
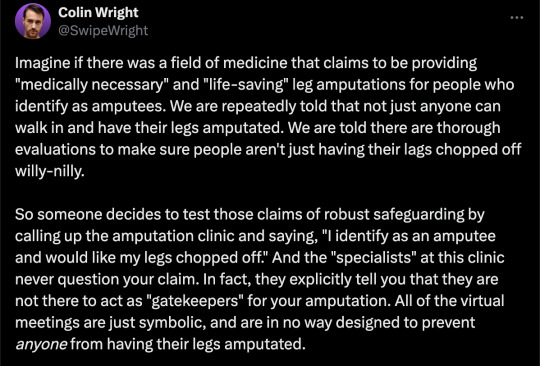
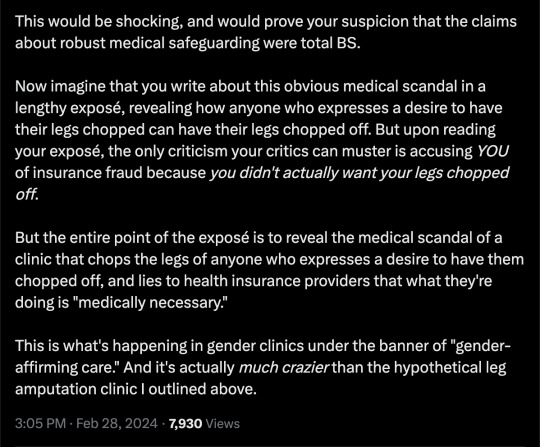
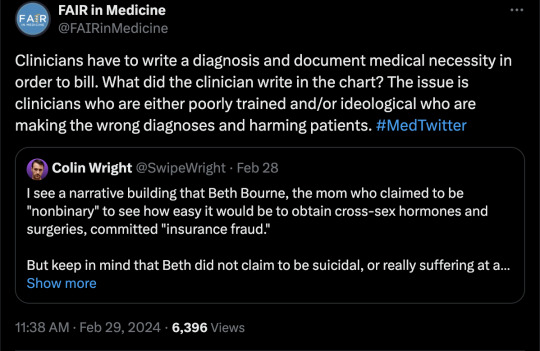
This is completely insane.
Apologists online are running around saying, but she didn't mean it, she was lying, she was pretending...
It doesn't matter.
Any kind of security, penetration or integrity test is insincere too. When security researchers compromise Microsoft's operating system or Google's browser or whatever, "but they didn't mean it" is not a defence to a discovered security flaw. It doesn't matter that the security researchers didn't plan to steal data or money or identities. The flaw in the system is there regardless.
It doesn't matter that it was insincere. Because the workers didn't know that. They never checked, never asked questions, never tested. They had been taught and instructed to never ask any questions. They did what they were supposed to. And the system failed spectacularly. Because that's what "gender affirming care" means.
Additionally, the claim that Beth Bourne committed fraud is an outright lie. A patient cannot bill. They do not have the authority. The medical clinic is the only one that can bill, and they must supply a diagnosis and a medical necessity.
If they didn't diagnose her and just wrote down what she said, then they committed fraud. If they claim they did diagnose her, then they committed fraud, because the diagnosis they concocted was bogus. This, by the way, is actually going on. Clinics are reporting fake endocrine and other disorders to get blockers, hormones and other interventions. Jamie Reed and other whistleblowers have documented evidence of this. Beth Bourne is not responsible for what the clinic does. They have medical licenses and legal responsibility. Not her.
Additionally, anyone who actually read the article would know how she tested the system. She said things like, "I've always been not that feminine. So, maybe I get my boobs removed." And they said, "sure." Instead of saying, "wait, why do you think that?" Framing it as her lying is itself a lie. They violated their ethical obligations. That much is incontrovertible. And it's directly the result of "gender affirming care," where clinics and clinicians rubber-stamp anything deemed "trans" based entirely on ideological, not medical, grounds.
#Beth Bourne#undercover#undercover investigation#gender identity ideology#queer theory#nonbinary#non binary#top surgery#bottom surgery#double mastectomy#bilateral mastectomy#gender affirming care#gender affirming healthcare#gender affirmation#affirmation model#medical scandal#medical malpractice#medical corruption#religion is a mental illness
827 notes
·
View notes
Text
I got my top surgery over 2.5.yrs ago and I wanted to share some tips for pre- and post-op care! I got a double mastectomy with free nipple grafts and I'm loving my results.
Pre-Op:
-If you smoke or vape, try to quit for as long as possible before your surgery date, ideally at least a couple months. Don't use nicotine while healing either. Nicotine constricts your blood vessels and this can impede healing. If you're getting nipple grafts like me, it can be the difference between the grafts healing successfully or falling off.
-for the love of all that is holy, FOLLOW YOUR SURGEONS EATING RESRTICTIONS BEFORE SURGERY. Anesthesia can cause you to regurgitate and aspirate, which can lead to pneumonia and be deadly. This is MUCH more likely if you eat food too soon before going under. If you get bad stomach issues like reflux, ask for anti-nausea meds to be given IV before you wake up. I almost aspirated right as I woke up even though I didn't eat beforehand bc of my acid reflux.
-You may want to make a lot of things more easily accessible to prepare for recovery. You'll want to be able to reach things like cups, bowls, silverware, medications, toiletries, clothing, etc easy to reach without having to reach above your shoulders.
-if you can, prep some comfort meals that are easy to reheat in the microwave or oven. This is especially helpful if you plan on being mostly self-sufficient during recovery.
-get plenty of loose-fitting button up shirts. They are by far the easiest thing to put on after top surgery.
Post-Op:
-if you want less visible scars, I HIGHLY recommend using silicone scar tape or silicone scar gel once your surgeon says it's ok. The tape is generally cheaper, reusable and washable by hand with soap and warm water. Two rolls lasted me my whole recovery and my scars are now barely visible. The gel is easier to apply and more sensory friendly, but more expensive. You can get both online.
-your chest will be swollen for up to a few weeks after surgery. This swelling may be assymetrical at first (mine was). Try to be patient and not pass any judgements on the quality of your results during this time. You can always get a revision after 6 months if you're still not happy with it, but don't freak out right away as things will take time to settle.
-your brain is adjusting to a major, sudden change to your body. It's okay if you feel some mixed emotions while you process this. Try to journal or talk about it with someone you trust. I know my brain does not cope well with change and while I never once regretted my surgery, it took a little bit of time to get used to my body looking different even if it's the way I wanted to look.
-make sure you empty your drains on time if you have them and keep your compression vest on. This will help you heal as best you can and reduce swelling.
-don't use heat or ice! Ice will restrict blood flow to areas that need blood flow to heal and heat can amplify swelling and inflammation.
-touch your chest along the length of your scars as much as you tolerably can. You will most likely have nerve damage from surgery and touching/massaging gently will help your nerves know how to re-grow and process sensation properly. I have pretty much full sensation in the center of my chest where I touch very often while the ends of my scars under my armpits (where I don't touch often) still have reduced sensation.
- Gently massaging your scars with two fingers once the scabs are healed can also help prevent knots and bumps in the scar tissue. Don't cause yourself pain, only do it if it's tolerable.
-FOLLOW ALL YOUR SURGEONS INSTRUCTIONS!! If they tell you to do something or not do other things, there is a good reason.
I'm also happy to answer asks and messages about my experience with getting top surgery! Take your time in deciding if this is right for you and know I love you all either way <3
#ftm top surgery#transmasculine#ftm#gender affirming care#gender affirming healthcare#top surgery#double mastectomy
48 notes
·
View notes
Text

top surgery <3
#transgender#gender#gender envy#queer#trans#trans representation#lgbt#transition goals#lgbtqia#gnc#FTM#MTF#transmasc#transfem#trans icons#gay icons#elvira#gender goals#gender affirmation#gender inspo#gender euphoria#double mastectomy#top surgery
55 notes
·
View notes
Text
hey i haven't mentioned it because it hasn't felt real but i'm literally getting top surgery next week!! wowee!!!!!!
#top surgery#mastectomy#double mastectomy#needless to say i am focusing on this in these trying times#disclaimer: i am not trans
44 notes
·
View notes
Text
I'M TIT-FREE, MOTHAFUCKAAAAAAAAAZ
#lgbtq#lgbt#trans#transmasc#transgender#lgbtq+#ftm#trans joy#top surgery#double mastectomy#mastectomy#chest surgery
73 notes
·
View notes
Text
I figured it's time I talk about my surgical transition experience. There's plenty of false narratives out there and I want to counter what I can with truth and personal experience.
The first procedure I received this year in late January was a transvaginal ovarian-hysterectomy. That means they cut out my uterus and ovaries (and the connecting fallopian tubes) without making any abdominal incisions (removed through the vagina). I'd had a consultation with the surgeon performing the operation a few months prior where we discussed any concerns and went over potential side effects as well as specifying I wanted my ovaries removed as well. When the day of the procedure came I went to the hospital, the nurses were really kind and I got to see the surgeon again one last time for any last minute concerns before I went into the surgical suite.
Waking up post surgery I was elated to learn the surgery had gone super smoothly, the surgeon said I'd lost less than a teaspoon of blood. I stayed in hospital for the remainder of the day and ended up going home around 9pm. They'd given me a pain meds prescription, and that kept things during recovery at a quiet 2-3 on the pain scale. Most of what I felt was a general soreness in the area, it was a lot like the sensation of period cramps. It took only 3 weeks before I felt pretty much 100% I still wasn't fully healed but by then there wasn't any pain, even slight.
Now I'm just nearing the end of my 2 month full recovery time and I'm clear to have penetrative sex. The worst part of the recovery I'd say was the basically instant menopause I had to go through for a while. The hot flashes were the worst, get a fan for yourself if you're planning on getting this procedure.
The end of February is when I got my second procedure, a double masectomy aka top surgery. Normally transition surgeries wouldn't be so close together in timeline but I had school starting in May but I couldn't emotionally afford to wait until the semester is over to get the surgery done. Additionally, political circumstances also lead to me making the decision to push up the date of my surgery, I was terrified that if I was to wait another year that it might be illegal by then.
Similar to the first operation, I'd had a consultation appointment several months prior that addressed any questions and concerns to help me decide if the procedure was right for me. I was way less nervous this time around because I'd already been through one surgery and had a better idea of what to expect in terms of pain and recovery.
The experience of check-in and preparation for the second surgery was pretty much the same as the first with one exception, I decided to forego the nipple grafts last minute (and I don't regret the decision. less risk of complication/infection, I wouldn't likely retain sensation, getting nipple tattoos instead gives me direct control over size and shape) so I had to meet with the surgeon beforehand the day of. My direct input was accommodated and my questions answered the day of, it was awesome.
I went under anesthesia feeling a sense of peace that I'd wake up feeling more like myself than I had since before puberty. I'm a month recovered now and I'm just so pleased with the results! The pain was so worth it!
Feel free to ask respectful questions about my experiences.
#trans healthcare#transmasculine#important information#truth#important#nonbinary#surgery#top surgery#bottom surgery#inspiring#trans rights#trans visibility#tdov 2024#happy tdov#tdov#transgender#trans#hysterectomy#ovarian hysterectomy#masectomy#double mastectomy#lgbtq#lgbt#lgbtqia#lgbtqia+#trans day of visibility#trans day of vengeance
70 notes
·
View notes
Text
One Week Post-Op (DI Top Surgery update, TW MENTION: Surgical procedure, surgical complications, medical transition, top surgery drains, Hematoma)
Wow, holy crap, my surgery was a week ago already!
I met with my surgeon yesterday for my first follow up! It was really nice to be able to talk about the small hematoma (a blot clot, more or less!) in my left side, and have her concretely tell me that it’s breaking down the way it’s supposed to, that the neon color drainage IS normal (for a person with a hematoma)… And I got my right side drain out!!! The left will continue to stay in until (at least) my follow up a week from today. The hematoma needs to reliquify slowly and drain, either via my drain or by spreading to the surrounding porous tissue by converting to bruising. That being said, my bruising is gonna WORSEN before it’ll get better, but bruising is a good sign that my hematoma is healing. Swelling is pretty consistent on the left, and she said that everything looks amazing, all things considered!
I realized yesterday that I will never again have to deal with underboob sweat, that weird “tuck your shirt under them so your skin doesn’t stick and get all sweaty gross,” or having to “rest them” while leaning on a table. That was a trippy realization, that at some point I did that for the last time, and now I’m just free of it. I was able to soooorta tilt to my right while sleeping last night, and as a side sleeper, I’m ecstatic about that. I looked at my pre-op photos for the first time since surgery this morning and I’m gonna be honest… I’m already forgetting what they felt like. It feels so dissociated bc my brain just so easily clicked into “Yep, this is what my chest is supposed to look like.” Even with the incisions and bruising it still feels like MY (flat) chest just had some surgery. And that’s a super fucking cool feeling, having my chest feel like MINE, finally feel familiar.
My mom thanked my surgeon yesterday for “that (my) smile” and said “it was an overnight difference with him. I can just see him glowing with relief.” I think that’s a pretty accurate anecdote to leave this update off on. More to come as things progress.
Side note- If anyone has any questions about top surgery, drains, hematomas, or anything adjacent, I’m happy to talk! My DMs are always open. I’m by no means an expert or qualified doctor, but I’m always happy to share my experience in the hope that it helps someone else.
#nonbinary#genderqueer#top surgery#trans#transgender#genderfluid#lgbtq#lgbtq community#lgbtqia#trans pride#post op#surgery update#trans journey#transmasc#ftm transition#ftm#ftm surgery#chest masculinization#double mastectomy#double incision#transmasculine#trans healthcare#trans guy#trans experience#trans joy#trans masc#transblr#trans boy#trans nonbinary#trans visibility
26 notes
·
View notes
Text
24 notes
·
View notes
Text


I've been thinking a lot about the way people talk about breast cancer and the way in bringing awareness people often center the very part of the body you lose in order to survive, so I wanted to portray the body of a woman post double mastectomy as beautiful.
#art#artists on tumblr#breast cancer awareness#double mastectomy#my art#mine#digital art#breast cancer#i rather want to make more art of her#maybe make her one of my ocs
37 notes
·
View notes
Text
Post-Top Surgery Weight Gain: Will My Breasts Grow Back? (Nope!)
I've had a couple people message me asking about this privately, and it was something I had a fear of when I was getting ready for top surgery, so I wanted to address it in a public post:
After top surgery, your breasts will NOT grow back, even if you are not on testosterone. No, not even if you gain weight.
The chest is, to borrow Shrek's wisdom, like an onion, and has many layers. The ones top surgery is concerned with are the chest wall (muscle), the breast tissue, fat, and skin, in that order.
Your chest wall is a bunch of muscle that protects your organs. This will not be removed or touched. Your breast tissue sits on top of that, and this is what will be removed during surgery, leaving just enough tissue to make your chest proportional to your body. Very few people have totally flat chests. On top of this is body fat, much of which will also be removed or reshaped during surgery. Then there is your skin, and your nipples. Typically nipples (including areola, the area around your nips) will be taken off, trimmed down to a smaller 'masculine' shape, then grafted back on. Or you don't have to get your nipples back at all! I didn't, so it's up to you.
To reiterate: your breast tissue will NEVER regrow. Your nipples and areola will NEVER regrow, regardless of if you are on T or not.
However, FAT may fluctuate in this area. If you lose weight, whether on T or not, you will probably lose fat here and may have loose skin, which many surgeons can address in revisions. If you gain a substantial amount of weight and are not on T, you may gain more fat here- take a look at your close female relatives. When they gain weight, do they gain it in their breasts and side-boob area? When they lose weight, do they go down a cup size?
If you are on T, testosterone will change the way your body distributes the weight it gains. Look at your close male relatives. I'd be willing to bet money that when they gain weight, they gain it predominantly in their stomach. When you are on T, your body will probably begin to redistribute the way it gains fat to a more 'typically male' pattern, like the stomach, as opposed to hips, thighs, and chest.
Something to keep in mind, especially for fat people but really for anyone getting top surgery: YOUR ANGLE IS DIFFERENT! Look down at your chest right now, pre op. You can see aalllll the way down your cleavage. But if you asked someone standing in front of you if they could see all your cleavage, they could not. Even if you were naked, you seeing your own chest from a top-down angle makes things look further out/rounder/bigger than how other people see you.
Please keep this in mind when you look at your surgery results- the fat that was left behind and reshaped on me looks bigger/rounder to me, looking down, than to other people looking at me. And this is only in resting position! Move your arms around (once it's safe dont do this freshly out of surgery please dear god), raise them over your head, put them out to your sides and T pose. Look at the way the fat moves under your skin and around your body; how it looks 'flatter' in some positions and 'rounder' in others. This is totally normal! This is what skin and fat are supposed to do, and do on everyone who has skin and fat! These are NOT breasts, and they will NEVER be breasts again.
I hope this helps some peoples fears be assuaged. I know it can feel silly to ask if your breasts will grow back, but it is a valid fear, especially for plus size people, and it is also a fear I hope is now at rest. Your breasts will never come back. You're gonna look and feel great.
tl;dr- no, your boobs will never come back after top surgery, regardless of whether you are on T or not. you might have leftover fat here or gain fat here, but this is a universally human experience, and happens to cis men just as much as any other person. also, your angle viewing your own chest from the top-down is a misleading optical illusion that is not accurate to what other people see looking at you front on.
#trans men#plus size ftm#plus size top surgery#fat liberation#fat ftm#fat transmasc#trans man#trans masc#transgender#trans#transmasc#ftm#double mastectomy#top surgery#queer#queer pride#trans pride#bilateral mastectomy#mastectomy#og#transblr
371 notes
·
View notes
Text
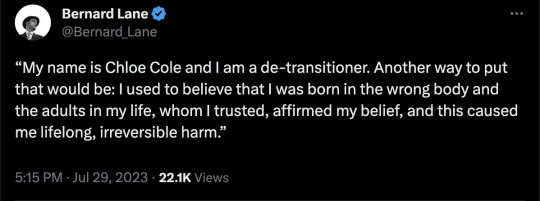
By: Chloe Cole
Published: July 28, 2023
On Thursday, her 19th birthday, Chloe Cole testified to Congress with a “final warning” that medical treatments to change the gender of confused children is horrific. Cole, who was given surgery as a teenager to become male and soon regretted it, said what she needed most was therapy, not a scalpel. Here is what she told lawmakers:
My name is Chloe Cole and I am a de-transitioner.
Another way to put that would be: I used to believe that I was born in the wrong body and the adults in my life, whom I trusted, affirmed my belief, and this caused me lifelong, irreversible harm.
I speak to you today as a victim of one of the biggest medical scandals in the history of the United States of America.
I speak to you in the hope that you will have the courage to bring the scandal to an end, and ensure that other vulnerable teenagers, children and young adults don’t go through what I went through.
Deceit & coercion
At the age of 12, I began to experience what my medical team would later diagnose as gender dysphoria.
I was well into an early puberty, and I was very uncomfortable with the changes that were happening to my body. I was intimidated by male attention.
And when I told my parents that I felt like a boy, in retrospect, all I meant was that I hated puberty, that I wanted this newfound sexual tension to go away.
I looked up to my brothers a little bit more than I did to my sisters.
I came out as transgender in a letter I sent on the dining room table.
My parents were immediately concerned.
They felt like they needed to get outside help from medical professionals.
But this proved to be a mistake.
It immediately set our entire family down a path of ideologically motivated deceit and coercion.
The general specialist I was taken to see told my parents that I needed to be put on puberty-blocking drugs right away.
They asked my parents a simple question: Would you rather have a dead daughter or a living transgender son?
The choice was enough for my parents to let their guard down, and in retrospect, I can’t blame them.
This is the moment that we all became victims of so-called gender-affirming care.
I was fast-tracked onto puberty blockers and then testosterone.
The resulting menopausal-like hot flashes made focusing on school impossible.
I still get joint pains and weird pops in my back.
But they were far worse when I was on the blockers.
Forever changed
A month later, when I was 13, I had my first testosterone injection.
It has caused permanent changes in my body: My voice will forever be deeper, my jawline sharper, my nose longer, my bone structure permanently masculinized, my Adam’s apple more prominent, my fertility unknown.
I look in the mirror sometimes, and I feel like a monster.
I had a double mastectomy at 15.
They tested my amputated breasts for cancer.
That was cancer-free, of course; I was perfectly healthy.
There is nothing wrong with my still-developing body, or my breasts other than that, as an insecure teenage girl, I felt awkward about it.
After my breasts were taken away from me, the tissue was incinerated — before I was able to legally drive.
I had a huge part of my future womanhood taken from me.
I will never be able to breastfeed.
I struggle to look at myself in the mirror at times.
I still struggle to this day with sexual dysfunction.
And I have massive scars across my chest and the skin grafts that they used, that they took of my nipples, are weeping fluid today, and they’re grafted into a more masculine positioning, they said.
After surgery, my grades in school plummeted.
Everything that I went through did nothing to address the underlying mental health issues that I had.
And my doctors with their theories on gender that all my problems would go away as soon as I was surgically transformed into something that vaguely resembled a boy — their theories were wrong.
The drugs and surgeries changed my body, but they did not and could not change the basic reality that I am, and forever will be, a female.
Depths of despair
When my specialists first told my parents they could have a dead daughter or a live transgender son, I wasn’t suicidal.
I was a happy child who struggled because she was different.
However at 16, after my surgery, I did become suicidal.
I’m doing better now, but my parents almost got the dead daughter promised to them by my doctors.
My doctor had almost created the very nightmare they said they were trying to avoid.
So what message do I want to bring to American teenagers and their families?
I didn’t need to be lied to.
I needed compassion.
I needed to be loved.
I needed to be given therapy that helped me work through my issues, not affirmed my delusion that by transforming into a boy, it would solve all my problems.
We need to stop telling 12-year-olds that they were born wrong, that they are right to reject their own bodies and feel uncomfortable with their own skin.
We need to stop telling children that puberty is an option, that they can choose what kind of puberty they will go through, just like they can choose what clothes to wear or what music to listen to.
Pseudoscience
Puberty is a rite of passage to adulthood, not a disease to be mitigated.
Today, I should be at home with my family celebrating my 19th birthday.
Instead, I’m making a desperate plea to my elected representatives.
Learn the lessons from other medical scandals, like the opioid crisis.
Recognize that doctors are human, too, and sometimes they are wrong.
My childhood was ruined along with thousands of de-transitioners that I know through our networks.
This needs to stop. You alone can stop it.
Enough children have already been victimized by this barbaric pseudoscience.
Please let me be your final warning.
Thank you.
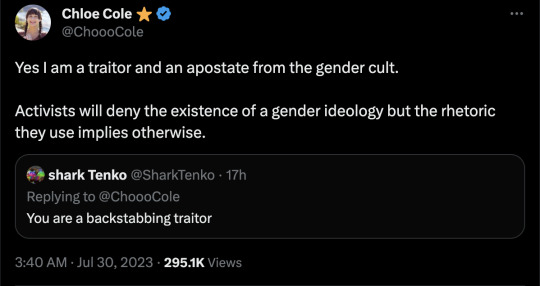
Might as well call her a murtad and kufr.
"The medical industry mutilated me, maybe don't mutilate other kids," shouldn't require bravery or renouncing an ideology.
Reminder: A minor under the age of 18 is too young to agree to a cellphone contract. 🤦♀️
#Chloe Cole#detrans#detransition#gender ideology#queer theory#medical malpractice#medical scandal#medical mutilation#gender affirming#gender affirming care#affirmation model#double mastectomy#gender cult#sex trait modification#genderwang#religion is a mental illness
1K notes
·
View notes
Text

Serafin is scheduled to have top surgery at the end of October! They only have $630.00 of their $3,000.00 goal raised! Anything helps!
https://gofund.me/1fb94734
#fundraiser#go fund them#top surgery#gender confirmation surgery#trans fundraiser#transmasculine#transmasc#transmasc top surgery#transmasculine top surgery#double mastectomy#transgender#transgender go fund me#gofundme#donations#crowdfunding#trans community#trans pride#trans man#trans rights
19 notes
·
View notes
Text
My top surgery went well, currently healing and I am getting better everyday! My drains came out and my sutures will be able to come out on this week!
Thanks to everyone who donated and if you want to help please donate anything will help me pay for the debt. If you can’t sharing is a great way to help too THANK YOU 🧡
8 notes
·
View notes
Text

I’m just over 3 weeks post-op. I’m so happy with my chest and I finally like what I see when I look in the mirror. I made this based on a picture I took of myself (and then I replaced my tattoos with generic object options). I feel like this is the perfect place for me to share it.
#transmasc#trans man#they/them#top surgery#scars#double mastectomy#gender affirming care#artwork#my artwork#chest#post op#healing#miki ratsula#elephant in the room#new chest
8 notes
·
View notes