#and treatment is basically... oxygen and sedation
Explore tagged Tumblr posts
Text
So I've been quiet on here a lot longer than planned.
The reasons are many. The reasons are varied.
The reasons are mostly fucking horrible.
Under a cut because it's long. Check tags for content warnings.
First was the expected absence: my parents came to visit me in Los Angeles over my birthday, so I spent the first half of October showing them around whenever I wasn't working a shift at my shitty department store day-job, or in class at UCLA.
Then, almost immediately after they went back to Australia, I got a second job working as a personal assistant for a composer. This was (and is) an extremely fun and rewarding job, but meant having one more thing on my weekly schedule, which was an adjustment.
Given that until halfway through last year, I'd been out of work since I immigrated in 2019, it took a while for me to get used to having so many concurrent responsibilities, and I'd just started to get a handle on things when I got sick right before the holidays. I took many covid tests -- all negative -- and eventually determined that it was just last year's strain of flu, which I hadn't managed to find time to get the shot for due to the aforementioned super busy schedule. I'm almost positive it was thanks to a particular customer at the aforementioned shitty department store job who coughed hard enough in my direction for their germs to get through my n95.
Anyway, last year's flu was a monster, and I spent a week in bed with a fever, then several more weeks being utterly drained and with a horrendous cough to match. It took a full month for me to recover, and then in mid-January, almost as soon as I started to catch up on all the things that had fallen behind while I was sick, things got bad, then good, then worse, then better, then much, much, much worse.
Basically, it starts with my dad being diagnosed with prostate cancer. He'd told me in October when they came to see me, but the surgery was scheduled for the tail end of January.
The surgery happened on a Monday, and it was a complete success. They got it all in one go. No chemo or radiation or further treatment needed at all. I spoke to him on the phone after he woke up, and he was in good spirits. Happy to have been given the all clear by his doctors.
I told him to watch Star Trek: Strange New Worlds & Evil while he rested up at home, because I'm writing specs for both this year and wanted him to be able to read them and know what was going on. He's the one who got me into sci-fi and horror, after all.
He went home.
He was home for two days.
He started feeling a bit rough on the Thursday. Short of breath. No appetite. Mum took him back to the hospital, just to be safe.
Turns out he'd had a mild heart attack. They couldn't figure out why. The echocardiogram didn't show any issues with his heart.
Then over the next couple of days, his breathing got worse. They took a scan of his lungs, and found that they were extremely inflamed. They'd given him covid tests but they came back negative. We told them about a work accident he had about 20 years ago, where a switchboard he'd been working on exploded in his face, and he'd suffered from inhalation burns among other things.
They thought that maybe something during the prostate surgery had caused irritation in his already damaged lungs, which put stress on his heart and caused the mild heart attack. He's never had any issues with his lungs since that accident, but they thought that maybe he'd just adapted to the damage over the years without realizing.
They kept trying different treatments to help his lungs heal. Nothing seemed to work. His breathing kept getting worse. They had him on as much oxygen as possible without intubating him, but it wasn't enough, so over that weekend they decided that they'd need to move him to another hospital with a more specialized lung unit.
When they were preparing to do that on the Monday night, he crashed. Another heart attack. Bigger, this time. They intubated him. Sedated him. Called my mum and told her to come in right away because things looked so bad.
But then he rallied. By the morning, though he was still sedated and intubated, the doctors were confident that with the right treatment at the specialized lung unit at the other hospital, he'd be okay. He was still in a rough condition, but stable. They transferred him to the other hospital.
He was given another covid test. This one came back positive.
My mum and brother called me once it was a reasonable time in Los Angeles to let me know what was going on, and the next day my brother booked me a flight back to Australia. I had to leave for the airport about five hours after my ticket was booked.
I got to Melbourne on February 1st.
For the next two weeks, dad was intubated, sedated, and in an isolation room. Every few days, they scanned his lungs again, and they were slowly improving.
Finally, he stopped testing positive, and was moved to a regular room in the ICU. Then he healed enough for them to extubate him and wake him up.
On February 13th, he was conscious enough to squeeze my hand when we went in to see him. On February 14th, he was conscious and capable of talking enough to ask a nurse in his ward to bring him his phone, and called mum first thing in the morning to wish her a happy Valentines Day.
Two days later, on Friday 16th, his lungs looked good enough on scans that they felt it was safe to do an angiogram, which they wanted to do just to double check that there weren't any issues with his heart that they missed with the echo.
They did the test. They found massive blockages. 90% blockage in one artery; significant blockages in two others.
Even though he'd barely recovered from covid, the blockages were bad enough that they scheduled him for open heart surgery on Monday 19th. They said without surgery there was a 100% chance that the blockages would cause another massive heart attack that he would not survive. They said there was about a 20% chance that he'd have complications, but only about 4% that they'd be serious/life threatening.
Like before, the surgery went well. Triple bypass, in the end. We got a call late on Monday afternoon to say that he was in recovery and looking good. His heart was functioning perfectly. They'd bring him out of sedation that night. Keep him in the ICU one or two days just as the standard post-op procedure. He'd spend a week or so in a cardiac ward after that, then head to a physical rehab ward for a couple of weeks until he could build back the muscle mass he'd lost while sedated.
We went in to see him the next day. Tuesday 20th. His 66th birthday.
He was tired, but looked good. Color in his cheeks. He made a couple of jokes. We left after about 45 minutes because he was pretty worn out, and we wanted to let him get some rest.
But then after, that his breathing started to get bad again. By Wednesday morning, they'd switched out the oxygen prongs in his nose for a big, high-pressure mask again. They called to let us know they were going to intubate him again so he could rest while his lungs recovered a bit more.
They struggled to get the tube in.
His lungs were deteriorating badly. He kept getting worse. We couldn't go in to see him because they were working on him all day.
At 9pm we got a call to say that he was just getting worse. They had him on 100% oxygen. He just wasn't absorbing it. His entire body was under massive strain. They were doing everything they could, but he just wasn't improving.
They said we should go in right away.
We got there by 10pm. My brother and his wife arrived about the same time. We went in to see him. He didn't look good. He looked pale. But he was warm, and he'd come back from the brink before, and we were sure he could do it again. We stayed with him for about an hour, and left not long after 11pm. Went back to my brother's place because they live closer to the hospital.
We were there about half an hour before they called us again. Just after midnight. He was gone.
That was about a week and a half ago, now. It still doesn't feel real. He was only 66. He hadn't even retired yet. He was working full time up until the week before Christmas, and had planned on going back to work a few days a week after he'd recovered from surgery. He never had any heart trouble, or lung trouble. He was active. He was fine.
My wife Zel and her mom flew in a couple of days after it happened. I barely remember anything from the past two weeks. Everything just feels fake.
I've been trying to write something to say at the funeral, which we've finally been able to arrange for next week -- it was delayed because we had to wait for dad to be released by the coroner. I don't think I'll be able to do it.
Anyway. That's where I've been.
It'll probably be a little while longer before I'm around here much, let alone posting with any regularity, because I'll be in Australia helping my mum & and my brother sort everything out. I have no idea how long I'll be dealing with stuff, or when I'll be able to make words cooperate enough to post anything, but I'll be back eventually.
I'm trying to keep an eye on Discord (I'm violetmatter over there) so you can find me there if you want. But yeah, I just wanted to let you guys know why I've been so quiet.
#cass says things#this is a very long#and heavy post#so i guess i should include some content warnings#uh#christ what do i even tag this with#cw: hospital#cw: health#cw: death#cw: parent death
58 notes
·
View notes
Text
U.S. medical volunteers in Rafah hospital say they've never seen a worse health crisis
Editor's note: This story contains graphic descriptions of injuries. AMMAN, Jordan — At one of the last functioning hospitals in Rafah, scenes of horror are conveyed in clinical descriptions as U.S. medical volunteers grapple with the effects of Israeli military operations and border closures after seven months of war in Gaza. "They tried to suture up the hole in the heart — they couldn't," Dr. Usman Shah, from California, explains to Dr. Ammar Ghanem about a patient wounded in an explosion. Ghanem, a vice president of the Syrian American Medical Society, is overseeing the intensive care unit and made a video on Friday of his conversation with Shah. "There was too much blood loss – the heart cavity, they tried to massage it but the heart cavity was empty," Shah says. The two are members of a team of U.S. and U.S.-trained doctors who arrived in Rafah 10 days ago as part of a medical mission organized by the Palestinian American Medical Association. Now, nearing the end of the mission, with Israel closing the main border crossing, they are unable to leave. In the video recorded Friday by Ghanem, Shah tells him about the other two patients who arrived that morning with non-survivable injuries. Shah, dressed in blue scrubs, relates in an even voice how the jaw of one of the patients crumbled under his hand when he touched him. In the only visible sign of distress, he massages his temple and briefly closes his eyes as he tells the story. Ghanem says conditions have worsened considerably since the border closure on May 7, with many of the local physicians and nurses unable to come to work because they have had to evacuate their families.
'Prioritizing patient lives'
Most of the doctors and nurses on the mission are experienced conflict zone volunteers. But Ghanem says they have never seen anything like this. "Unfortunately here I have to prioritize patient lives. When I say 'prioritizing patient lives' I mean I know that term but I never used it before until I came here," he said in an interview with NPR by video call from Rafah. The benign-sounding term refers to deciding whom to stop treating and let die in order to divert resources to those with a better chance of surviving. In one of two videos sent to NPR from the hospital Ghanem points out to a colleague one of his most difficult cases – an 18-year-old woman with a skull fracture so severe that brain material was visible. He said they did not have drugs strong enough to keep her sedated. He said they stopped treatment for a woman suffering from acute pancreatitis after two days because she required continued oxygen that might support several other patients. "So you see how sad this is?" he said in the interview. "I mean this patient is only like about 60 years old. We will not do this in the U.S. as you know, but this time of war and lack of resources that we are forced to do this." Ghanem, who did not want the hospital identified for security reasons, estimated that two to three patients a day die in the intensive care unit because of lack of supplies or equipment.
A lack of essential supplies
Part of the problem is that items critical for hospitals are banned by Israel which says they can be used by Hamas for military purposes. The list of items it considers dual-use include some water disinfection materials. The list does not cover all items that are reportedly banned. Save the Children has said it has had shipments rejected by Israel because they contained sleeping bags with zippers. An Israeli legal center, Geisha, has compiled a list of items that have been reported by organizations to have been rejected, including fishing rods and plastic sheets for tents.
[keep reading]
2 notes
·
View notes
Text
When you bring your pet to a veterinary hospital with a time-sensitive (or emergent) problem, they will likely ask you for two things; emergency consent and a CPR status. It's good to know what that means and have your answers ready in advance.
Emergency consent is permission to start medical treatment to stabilize an animal in unstable condition. In time-sensitive situations, it may not be appropriate to delay basic care long enough to speak to the owner in depth and provide an itemized treatment plan. This care may involve placing an IV catheter, starting fluids, running simple diagnostic tests, administering certain medications, and providing oxygen and/or heat support. They will often name a cost (say, $500), with the expectation that they won't go over that amount without returning to speak to you about your pet's status and their recommendations. You are fully within your rights to decline emergency consent, but depending on the situation the delay may adversely affect the outcome of the case. If you're not prepared for this question it can sound like a demand for money, but think of it more as a request for information about your financial situation; they don't want to inadvertently bankrupt you providing care you can't afford, but if you can afford it, it would be best to start now.
A CPR status is a guideline for what you want them to do if your pet goes into cardiopulmonary arrest while in the hospital. This condition quickly leads to death, but in some cases prompt intervention can return spontaneous circulation and ventilation. CPR for cats and dogs involves chest compressions similar to human CPR, as well as intubation and manual ventilation to provide oxygen, the use of emergency drugs such as lidocaine and atropine, and in rare cases, the use of a defibrillator. Depending on the cause of the arrest, success rates for CPR vary wildly. A healthy pet who arrests under anesthesia for an elective procedure may have up to a 50% chance of resuscitation, while an elderly pet in organ failure who arrests in the car on the way to the hospital may have a vanishingly small chance. There are costs associated with CPR, and even when it succeeds, post-resuscitation care typically involves a hospital stay and further treatment. There are certainly cases where a "Do Not Resuscitate" order may be the best choice for your pet, but it's a very personal decision. (Keep in mind that for safety's sake emergency vets will typically ask for a CPR status before admitting any patient to the ICU or starting a sedated/anesthetized procedure, so the question itself does not mean that your pet is on the verge of death. )
18 notes
·
View notes
Text

DENTAL SEDATION FOR CHILDREN: YAY OR NAY?
Have you been sitting on a dental chair, waiting for the dentist and praying that something - ANYTHING would happen that can whisk you away from the impending doom that you'll feel? As adults, surely we've all felt anxious, distressed, and edgy before but the unsettling sensation during dental appointments truly left impacts on us like no other. Now imagine how children go through with it.
Children don't possess proper coping skills regarding their dental experiences, making dental care to children quite challenging. This is a crucial aspect to acknowledge because once the children develop dental anxiety, dental fear and avoidance will start in which generally result in bad oral health. Sedation began to be practiced by dentists in the 1900's, it is not only to reduce pain but also to help with fear and anxiety that people feel before a dental procedure or even during a basic cleaning. According to Nelson (2022), it is estimated that 100,000–250,000 pediatric dental sedations are performed each year in the USA, and practitioners anticipate a need for more pharmacological behavior management in the future. High levels of pediatric dental disease, increasingly difficult child behavior, and parent expectations support a need for sedation services.
Sedation also may be used when several procedures need to be done at the same time, when the safety of a child may be compromised, or if your child has a strong “gag” reflex. Your child’s dentist will give the sedation. Once your child has received sedation, the dentist will give him or her an injection (shot) or injections in the treatment area to keep it pain-free during and after the procedure. The sedation medicine may last up to 6 hours after the treatment is done.
Types of Sedation:
Nitrous oxide
Often called “laughing gas,” nitrous oxide is a very safe, mild sedative that will help your child remain relaxed during dental procedures. Your child’s dentist will give the sedation with the use of a “space mask,” which carries air (oxygen) mixed with the medication.
Oral Sedatives
If your child is nervous, oral sedation may be used. It is taken by mouth or through the nose. This type of medicine will make your child a little drowsy, and will keep him or her relaxed and calm during the procedure. The medicine usually begins to work within 20 minutes.
IV Sedation
Intravenous (IV) sedation requires a needle to be inserted into your child’s vein, usually in the arm or hand. The biggest advantage to IV sedation is that the dentist can give your child more medicine during a longer procedure to keep him or her relaxed. Home preparation is required for this type of sedation.
Benefits or advantage of dental sedation to children
Dental procedures can be incredibly exhausting especially for the kids that had traumatizing experiences with a dentist and are also afraid just by looking at the dental instruments. Well, under the calming effects of sedation, children are more likely to sit still so our dentists and hygienists can work efficiently and effectively. According to dentiland.net there are seven possible benefits the patient can gain after receiving the dental sedative.
It Offers Choice - There are three kinds of sedation as mentioned above. These choices would help you to find the right fit for your child.
It Helps Manage Dental Anxiety - Any signs of anxiety in children is worth addressing early on to manage and reduce it. Sedation is a fantastic tool for dental anxiety relief as it helps to get the patient into a physiologically relaxed state, including deep breathing and a reduced heart rate. It will help prevent your child from panicking before or during the treatment.
Quicker Dental Procedures - if the patient is being relaxed it may lead to less extended procedure. But if a patient is anxious, they might move around in the chair or show discomfort, making the dentist pause his or her next phase of the treatment. That’s why it’s a win-win situation in which the patient settles quickly allowing the dentist to finish the procedure less time consuming.
Manage The Gag Reflex - this is a typical response in patients when a dentist examines the back of the mouth, that often happens with young children. Receiving sedatives before the treatment lowers the risk of damage and minor injuries inside a patient's mouth from gagging while a dentist is conducting an examination.
It Reduces Pain - Managing pain is one of the most important tasks of a dental practitioner when handling children. Sedation is one way of making your child comfortable throughout the treatment and avoiding distress for it can help reduce pain before, during, and after your child’s dental treatment.
It Aids Complex Procedures - Sedation will help ensure the dentist has the best chance of completing a procedure accurately, minimizing the risk of follow-up surgery or complications.
It Helps Relieve Parent Anxiety - No parent likes to see their kid struggling to have their dental treatment accomplished. Unfortunately children can sense when their parents feel anxious, and that can make your child more anxious and nervous. By choosing sedation, you have added reassurance that your child will be just fine.
Effects of Sedative Drugs/IV or Gas.
Children react to these sedatives differently depending on their tolerance level. It is important that the dentist determine the right amount of sedation needed by the patient so that the patient will not suffer any unexpected side effects. The most common side effects associated with intravenous sedation are headaches, dizziness and nausea.
In conclusion, dental fear and anxiety is a common problem in pediatric patients. Children are not little adults; they differ physically, psychologically, and emotionally. Thus, the effect of dental procedures may cause trauma and discomfort to the children in which it could lead to more serious psychological and emotional issues. Dental sedation can allow dentists to provide treatment with minimal said trauma and discomfort and also preserving their trust. On the other hand, it also has countless risks - even permanent damages and is seen with much apprehension. Nonetheless, dental sedation to children continues to grow and is seen more with opportunity than adversity. "Therefore, practitioners should strive to reduce patient risk by carefully selecting patients who are medically optimized for sedation and instilling a culture of safety into clinical practice", Nelson and Xu (2022).
References:
Nelson, T. M., & Xu, Z. (2015). Pediatric dental sedation: challenges and opportunities. Clinical, cosmetic and investigational dentistry, 97-106
https://www.dentiland.net/benefits-of-sedation-dentistry-for-children-in-tijuana .
3 notes
·
View notes
Text
VETERANS' DAY, 2024: A Day of Remembrance for Veterans Denied Medical Treatments Part 2

“Let us solemnly remember the sacrifices of all those who fought so valiantly, on the seas, in the air, and on foreign shores, to preserve our heritage of freedom, and let us reconsecrate ourselves to the task of promoting an enduring peace so that their efforts shall not have been in vain.” President Dwight D. Eisenhower Eric Koleda, USAF Vietnam Era Veteran, National Director, TreatNOW State Legislative Efforts, President and Co-Founder, HBOT4KYVETS.com The Veteran Suicide Epidemic: A Proven, Safe, and Effective Alternative Treatment Denied TBI Veterans Every day 20+ American Veterans succumb to suicide. That's over 151,000 since 2003. Pain overcomes their desire to live. Their torment is induced by over 70,000+ IED blast wave explosives, combat, and training injuries that lead to Traumatic Brain Injury and Post Traumatic Stress Disorders. They went to War for America. Over 877,000 came home with signature invisible brain wounds. It’s an estimated annual economic impact of $118.1 billion to care for all TBI/PTSD Veterans. We can treat and heal for ½ of 1 percent of the $4.7 trillion life time cost. We owe our Veterans the best America can provide and we are denying them basic safe and effective treatments. Police, Fire and EMT First Responders also suffer high suicide rates from many of the same Traumatic experiences of death and carnage. The Veterans Health Administration has prescribed over 847 million opioid pills from 2006 to 2014 to palliate the TBI/PTSD symptoms. Couple this with over 100 off-label prescription medications and it's been a suicide cocktail mixture. It has been a bandage on an arterial bleed. Improved cognitive and behavioral counseling helps but there are no FDA approved prescriptions for TBI; current standard of care has resulted in failed medical interventions. The VA Will Not Look Around Them, they only sedate our Veterans and make our most affected Veterans minimally functional with their families, at work, or permanently disabled, homeless, depressed, and/or unemployed. Hyperbaric Oxygen Therapy (HBOT) uses oxygen, approved by the FDA for use in 14 indications. And it works, used 100,000 plus times in the US and worldwide. Safety and efficacy were demonstrated in 21 clinical trials. Ten states have enacted legislation, appropriating $32.3 million for HBOT treatments. HBOT is observed to eliminate Suicide Ideation! Veterans diagnosed with TBI / PTSD who receive HBOT begin normal sleep patterns, experience reduced nightmares, improved "in the moment" life with family, and gain the ability to return to normal life and sometimes employment. The Obvious Question: Since HBOT Works to Heal TBI/PTSD, Why Isn't the Veterans Administration Using It? CBS Sunday Morning, 10 Nov 2024, broadcast an international piece on the use of Hyperbaric Oxygen for PTSD and brain wounds. Doctors and researchers in Israel and here in the US have perfected protocols for treating and healing PTSD/TBI using HBOT. Twenty years of peer-reviewed research and clinical evidence convinced the Israeli Defense Force years ago to use HBOT for its brain wounded soldiers and civilians. The program explores reasons to use the proven safe and effective here in the US. An interview with Congressman Greg Murphy, MD (R-NC) made this comment when speaking about the VA's ghosting attempts to pass legislation to demand use of HBOT: "If its being offered in Israel and they're having such good results, why the hell aren't we offering it in the United States . . . . . and if there is a treatment that has shown such definitive results, I believe it is medical malpractice not to offer that to our Veterans." The VA did not agree to comment for the program. You may view the program here. Reasons for the VA intransigence, with our responses, can be found here. Take care of yourselves, and if you can, a Veteran too. ****************************** The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, get patients off most of their drugs, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma from AHI and Burn Pits. Diabetic Foot Ulcers have become a major emphasis. www.treatnow.org Heal Brains. Stop Suicides. Restore Lives. TreatNOW Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made. Read the full article
#braininjury#brainwound#HBOT#HBOTTreatment#hyperbaricchamber#hyperbaricoxygen#HyperbaricOxygentherapy#MilitarySuicide#posttraumaticstressdisorder#PTSD#suicideideation#SuicidePrevention#TBI#TBItreatment#traumaticbraininjury#VeteranSuicide
0 notes
Text
Fulminating (The Mandalorian)
(Din suffers a complication after nearly drowning on Trask. He and the Child recover together. Maybe it's enough. 5000 words, canon-compliant, angst, medical whump, hurt/comfort, sign language. Set during Chapter 11: The Heiress. Don't say I didn't warn you about the whump - but the comfort's there, too.)
Thank you to @lastwordbeforetheend, @art3mys and @honestlyhufflepuff for helping talk me through this! You can also find this story on AO3 if you prefer.
***
The air streams past him, tugging at the free edge of his cloak as he descends. He tilts his head upward, watching Bo-Katan and her cruiser climb to the edge of the atmosphere. They’ll take the ship, and he’ll take the Jedi’s name.
It’s not the deal he wanted -- hell, they aren’t the Mandalorians he wanted -- but she gave him what he needed in the end, and he’ll respect that.
He coughs, chest feeling heavy, and lowers his head as the air rushes past. That’s better.
He aches as the rush of the fight leaves him. He’s not getting any younger, and while firefights are what he’s built himself for, taking an entire cruiser hadn’t been on his agenda. Especially coming off the disastrous crash landing on the ice planet with the kid and the passenger; he’d hit his head pretty badly in the landing, beskar helmet or no, and he still feels a nagging headache now that the action’s over. He scowls under the helmet.
The Rising Phoenix burns clean as the docks rise up before him, and he lands clumsily, staggering. He’s got to work on that. In all the traveling lately, his training has slipped. Koska in particular has given him some ideas for how to better utilize the Phoenix in combat, and he’ll have to consider incorporating the techniques into his own fighting style.
Din pulls a deep breath as he straightens up, slightly winded by the landing. Time to collect the kid and get going.
Leaving would be a good idea, if not for the fact half the port is still quiet. He glances around, realizing it’s still early in the morning and the Mon Calamari he paid to tend to the Crest is nowhere in sight. Fine. Maybe he and the kid will grab some sleep in the inn. How long has it been since they got any rest?
His feet fall heavy on the wooden docks, his boots scuffing. Yeah. A room might do them good.
***
It takes him a good twenty minutes to make his way through the narrow alleys to the Frogs’ home. He’s a little slower than usual, though he’s got good reason to be weary. The door slides open at his knock and the happy couple greets him, gesturing to a water-filled dish on their table. A tadpole splashes back and forth, and Din’s foundling stares at it with wide eyes and half-opened mouth, barely noticing that Din has come for him.
Din almost hates to pull the kid away. He’s downright enchanted by the tadpole (the kid better have minded his manners!), curious and fascinated and protesting as Din scoops him up. He congratulates the couple on their child and heads out into the alley, the kid chattering away unintelligibly. He’s been using that little voice of his much more lately, and though Din hasn’t picked out any words he understands, it’s a comforting sound. He chuckles a bit at the kid’s chatter, the laugh slipping into a brief cough that he swallows down. He wishes, not for the first time, that he could understand what the kid has to say.
The kid’s voice burbles cheerfully in his ears. Probably telling him all about his exciting night, staying with the Frog family. Maybe he’s asking where Din has been, or wondering where they’re going next. Din hasn’t a clue. He tries to pay attention, but finds it strangely difficult to concentrate and walk at the same time.
It’s not far to the inn. Half a klick at most. He’s walking at a normal pace, not running, not sprinting.
So why, then, is he breathing so hard?
He pauses against the wall of a small fishery shop, leaning against it slightly in a way that would look casual to a passing observer. He takes a deep breath, then coughs wetly, chest rattling.
You’re fine, he tells himself firmly, but his chest rises and falls like he’s been running.
His helmet swivels left, right. Quarren, Mon Calamari, humans, they scurry past Din and the child, but more than a few turn to stare at the two of them. This is too open. He needs to get back under cover until he can figure out what’s going on. You are both predator and prey, intones the Armorer, and oh, he knows it. His gut clenches a warning.
The Phoenix roars on his back, carrying them the rest of the way. He holds on to the kid with both arms and the kid giggles, enjoying the ride, but Din just focuses on breathing.
***
The innkeeper stares at him. “One night, then?” he grunts.
Din reaches into his hip pouch, pulls a stack of credits out, more than what’s needed. He forces himself to slow his breathing, though his chest hurts with the effort. He swallows. Modulates his voice to sound gruff and intimidating. “One night. And no questions.”
The innkeeper nods, holding his hands out in an appeasing gesture. “Whatever you say, Mando.” He tosses Din a fob to unlock the room. “Up the stairs, third door on the left. Food sent up to the room’s extra.”
Din merely nods. The kid, nestled in the crook of his arm, looks up at him, frowning. His ears sag down to his collar, and he wraps one hand over Din’s wrist.
Din makes his way to the stairs, shoving past a few Quarren there for their breakfast. They grumble, but they get out of his way; news travels fast about what a Mandalorian can do when pressed. They clear a path for him as he approaches the narrow stairs. With his back to the barroom, no one able to see him directly, he allows himself the luxury of a few deep breaths before he begins. He needs every one.
The flight of stairs isn’t long. Fifteen steps, maybe. But he has to grab the handrail with his free hand, gripping it tightly. His head swims, and the inside of his chest sears, burns, aches. He sucks air through an open mouth, shivering.
“Dank farrik,” he hisses, and regrets the extra breath expended on the curse. He has to rest halfway up the stairs, slumping against the wall with his head spinning.
He makes it up the rest of the flight, through the hallway, to the third door on the left. It slides open and he stumbles through the doorway, barely noticing the door sliding closed behind him as he staggers to the lumpy four-poster bed. He sets the kid down carefully before he sinks onto the bed with a thump. He struggles to remove the Rising Phoenix. He manages to rest it on the floor at his feet, and stays leaning forward, curled up over himself.
What’s wrong with me?
He desperately tries to run the possibilities. Poison? No, no, nothing’s broken his skin, he hasn’t eaten since he left the ship.… He shivers again. Is he sick? This doesn’t feel like any sickness he’s ever known before, coming on so fast like this, hitting so hard…
He sits huddled on the edge of the bed, panting. His helmet’s sensors chime at him. Normally vital signs are measured in the background, but he forces himself to focus on the corner of the display through his visor, where it flashes a warning: Blood oxygen level below 90%.
Oxygen… lungs… going under the water after the kid, struggling as the seal on his helmet slipped, as the seawater rushed up over his face, into his mouth and nose --
But I was fine, he tries to tell himself. He tries to remember if he inhaled the water or if he spat it back out, but all he remembers is frantic choking, flailing, a confusing jumble of cold and weight and struggle. I was fine --
He coughs again, the action bowing him over himself, and he gags on fluid in the back of his throat. He retches, gulps, tastes something metallic. Blood.
Fuck. Fuck.
His mind races. Battlefield first aid is taught to all Mandalorians, but he doesn’t remember what he’s supposed to do here. What here even is. His mind blanks for a second, or an eternity.
He suddenly remembers a function of his helmet he’s rarely used. He toggles it on with a jerky swipe over his vambrace. He can’t carry an entire tank of oxygen with him, since it’d be a clear explosion hazard in his line of work, but the helmet does have emergency oxygen concentrator ability. Enough to double the atmospheric content for low-O2 planets. He breathes deeply of the fortified air, and for a moment he feels a little calmer. This’ll fix things. Just need a little more air, a little rest, I’ll be fine --
It’s not enough.
The display in his helmet says it’s concentrating the oxygen at maximal levels, but damn it, it’s not enough. He wheezes, straining.
The display says a lot of things now. It’s going fucking haywire, streaming readings for his heart rate, his oxygen, spiking or crashing in ways he’s never seen. He forces himself to focus on the room beyond him instead of the screeching vitals, tries to focus on fishnets lining the dingy walls, a cramped closet refresher, a little wooden table to sit at, a round window letting in muted daylight.
It’s not working. Din drags in breath after frantic breath, coughs again, feels something frothy in the back of this throat. He tastes metal. He’s -- he’s suffocating --
No. No. This is just a sickness, I just have to get through the worst of it, just breathe -- just breathe --
But he wants to tear his helmet off, he’s so hungry for air, he wants -- he needs --
Firm pressure on his lap, movement, something besides the flail of his chest. It’s the kid. He’s almost forgotten about him in his struggle, and seeing the kid calms him slightly. Just slightly.
He manages to lower his head, though it makes him dizzy. The kid’s dark eyes stare up at him, his little face scrunched up and worried.
“I’m fine,” Din gasps, though clammy sweat clings to him inside his suit, though his heart still races. Does the kid understand him? He coughs, the sound harsh and wracking. “I just need to -- rest --”
Rest. Yeah. Yeah, that should help. Maybe he’ll be better off laying down in a different position. Holding the kid against him, he tries to ease himself down on the rumpled bedding. But as soon he’s down, he realizes it’s wrong -- on his back, he feels his armor crushing him -- smothering him --
He jerks upright, clawing at his chest, undoing the catches of his armor. His cuirass loosens and falls to the bed beside him. He leaves it. The pressure eases, barely.
The kid in his lap lets out a wail, and Din realizes that the kid knows.
What if I don’t -- what if he’s alone -- if this gets worse -- His heart rate jumps at the unfinished thought, pounding until he can feel the veins in his neck throbbing, the pulse thready. He slumps against the post at the end of the bed, wrapping a hand protectively around the kid. No. I’ll be fine.
He has to be fine. For both of them. He wishes he could tell the kid --
***
Grogu feels, sees, senses ripples in the Force, just as he senses ripples in the water where a frog might be near. Most of the time, it comforts him, feeling its swirls and eddies.
It isn’t comforting now. It’s scary. The Force is disturbed, the ripples churning waves. His protector, his person clings to him, and Grogu feels fear panic wrong.
Grogu flinches, his stomach hurting. He doesn’t know what’s happened to the man, but there’s something in the man’s chest that isn’t right, something that shouldn’t be there, something that makes it not work the way it’s supposed to. Grogu tilts his head up and rests one hand against the man’s armor, whimpering.
The man is shaking. His voice catches. “It’s -- it’s all right,” he chokes, but Grogu can feel how hard he’s working to breathe, how his voice sounds different. It sounds wet.
Grogu whimpers again, tries to reach out in the Force. He has to help him! The man flickers in the Force in a way Grogu remembers once from a misty dream, the day he sent the fire back; he was so sleepy after the flames ran away. But the man feels like he did then, faint and far away, and this time, Grogu understands what it means. Faint and far away and fading.
Grogu tries to talk to the man. Tries to tell him that he can help. He makes his voice loud, but the man’s breathing is louder. It’s not working.
He gets to his feet in the man’s lap, hurriedly bracing his hands against the man’s laboring chest. This close he can hear the wrongness inside him even without the Force, his ears catching terrible crackles over the man’s pounding heart. It shouldn’t sound like that. He knows it in a way he doesn't have the words for.
The man is soft without the armor, but the cloth and leather he wears are still thick and hard to get through, under Grogu’s hands. Grogu tries to reach, tries to make the Force inside the man move and change. He’s done it before, he has to try now, has to try to help him --
But it’s hard to shift the Force inside the man. He’s still wrapped in most of his armor, no skin to touch. Maybe one of the Masters from long ago could fix the man without touching him, without pressing skin to skin, but Grogu doesn’t know how. He wraps his claws around the heavy vest the man wears under the armor, and he cries at him, trying to make him understand.
“Please --” the man rasps. “It’s -- don’t be afraid --” He coughs again, thin reddish fluid beading at the bottom of his helmet. Flickering -- far away --
Grogu sinks into the man’s lap, breathing hard himself. The man’s fear is overwhelming, making it hard for Grogu to think. He’s felt it before from him when things got scary, but always the man’s bravery was bigger, more powerful, so much brighter in the Force than his fear.
But it’s all that Grogu can feel from him now.
He has to do something. The man still flickers. He looks around wildly, sees the man’s hand, limply resting against the bottom of Grogu’s robe.
“Hey, buddy,” the man wheezes. “You’ll be -- okay --”
Grogu is already pulling at the man’s wrist. He’s seen a little flash of skin here before, where the glove meets the armor. He fumbles with it, but it’s on too tight for him to budge.
“What --”
Grogu pulls hard at the glove, and the man helps weakly with his other hand, his fingers clumsy. The glove slips down at the wrist, exposing light brown skin, a thumb. The man crumples against the post at the end of the bed, the line of him all wrong, head rolled to his shoulder. He’s so faint.
Grogu curls one hand around the man’s thumb, presses the other hand against his palm. The man’s skin is cool and sweaty and calloused. Grogu holds his hand as hard as he can, and he closes his eyes, and he reaches.
He can't make sense of what he feels through the Force. Water, but there shouldn’t be water here. Breathing, but the air doesn’t help. Grogu concentrates, but it’s hard. It’s not like when that other man’s arm was hurt in the dark by the creatures, when Grogu could reach out and feel the way the poison wasn’t supposed to be there, the way the arm wanted to be normal again. The Force flowed to the hurt part, and it made it like it was before.
But now he’s confused, the fear so loud and painful, making it harder for Grogu to understand the problem with the water and the air and the lungs. He clutches the man’s skin, claws digging into his strong hand. He tries to do what he can, tries to tell the man’s chest to be normal, to work, to help.
The Force shimmers. It flows, and something goes out of him, into the man.
But it’s not like before. The other man’s arm got better so quickly, the poison disappearing, the flesh coming back to itself. It doesn’t feel that way now; he’s not sure what it feels like. It feels… like something slow, like something calm and quiet, like something gentle.
Grogu lets go of the man’s hand, his mouth twisting. He knows he didn’t understand enough, didn’t get it quite right. He lets out a soft wail, sinking down into the man’s lap and staring dejectedly at his hands.
He hears a quiet, tired voice. Feels the man shift, feels his hand with the rolled-up glove brush against his cheek. Grogu looks up through sleepy eyes and sees the man’s helmet upright again, looking steadily at him.
“Kid?” A long, ragged breath. A hoarse voice. His shoulders rise and fall with big breaths, but not as fast as before.
The man pulls him closer, and Grogu’s ears swivel. The crackles are getting softer. Going away.
“Thanks, kid,” the man whispers.
Grogu gazes up at the man, and he manages a tired little smile. The man is getting brighter in the Force. No more flickering. And underneath the man’s fear, Grogu senses brave again.
***
Din isn’t sure how long he’s been sitting there, leaning against the post at the end of the bed, holding the sleeping kid in his lap. He only knows he’s been working, and it is work, at breathing.
In, and out.
In, and out.
His helmet display flashes numbers at him. They aren’t normal. Oxygen, heart rate, respirations. But hell, they’re so much better than they were.
He doesn’t know what the kid did. The bare skin of his hand tingles in the cool air, and he’s almost afraid to cover it up again, in case it reverses what the child did to him.
For him.
All he really remembers -- things are hazy, even though it was at most only a few hours back -- is the panic, darkness at the edges of his sight, a terrible, unending hunger for air.
And then something quiet and soft, gently washing over him. It was enough.
He coughs again, but it’s easier than before. The rattle’s faint, thin, clearing. He’s not a medical droid, but he’s sure of it anyway: he’s going to make it.
The kid yawns beside him, half-wrapped in Din’s ragged cloak. He squints up at Din, his expression wary. Worried.
“Hey, buddy,” he says, his throat raw. “Are you okay?”
The kid whines a little, his ears swinging low at the way Din’s voice sounds so rough. Din feels an ache that has nothing to do with his lungs and everything to do with the kid’s anxious face.
“Don’t worry. I’m gonna be fine,” Din manages. “You helped me. Saved me.” The words are hard to force out, but he knows they’re important. Hell. What the kid must have seen -- what he must have thought was going to happen -- He freezes, remembering a dark cellar, explosions, a day of red robes in the smoke.
No. That’s not gonna happen. Not to him.
Din cradles the kid into a hug, his ears brushing against Din’s chest and shoulder. The kid hugs him back as hard as he can with his small arms, and he can feel the child trembling.
“Hey, hey,” Din murmurs, though he’s getting winded with all the talking. “I’m sorry I --” He huffs, keeps going even though it’s difficult. “I’m sorry I scared you.”
The kid reaches up to rest one clawed hand against the cheek of the helmet. Din blinks, startled at the closeness, but the kid keeps his hand against the beskar. Din mirrors the gesture, resting the knuckles of one hand against the child’s soft cheek.
“We’ll be okay. You and me, pal. Understand?” he asks gently.
The kid blinks those large, dark eyes, and Din wonders if he’s failed to reach him. Then the child lowers his hands, letting out a cheerful babble with a tilt of his head, and the tension in Din’s chest and gut falls away.
Yeah. He’ll be okay.
The kid chirrups again, voice rising in a question. Din thinks he recognizes what the kid is asking. “You hungry?”
Food. He dimly remembers a few ration bars, tucked in at the back of his belt, swiped from the Crest before they’d left. He sets the kid down beside him, then pulls out two bars and unwraps them both for the kid. Din’s thirsty, after everything, but the idea of food holds no interest yet.
“Here,” Din rasps. “Eat.” He carefully straightens up, taking a moment to slowly swing his legs over the edge of the bed. What normally takes a second leaves him breathless.
He gets to his feet, using the bedpost for support. He’s still wearing boots, his armor aside from the cuirass. It’s all so much heavier than it should be. He lets out a hiss between his teeth and crosses the room to the refresher, one step at a time. Water.
Once inside the refresher he sinks down onto the seat, removing his helmet and setting it into his lap. He glances up and sees his face in the cracked, streaky mirror, the skin blotchy and pale, hair a matted tangle, eyes swollen. There’s residue on his face, dried pinkish red around his mouth and nose. The sight makes him run cold.
It had been so close.
He flicks the water on, strips off his gloves and sets them into his upturned helmet. He cups his hands together beneath the faucet, the cold water spilling over the edges of his palms.
He drinks, and it’s enough.
***
The ship awaits them. Unfortunately, it's barely better off than it was when they left it. The Razor Crest drips with Mon Calamari detritus, rope rigging and tangles of seaweed crisscrossing the ship's hold. Din shakes his head, stepping aboard with the kid in his arms. It’s not great. It’ll do to limp along to something better.
He allows himself a faint chuckle, putting himself in the same category.
He’s mostly recovered. He can still feel it, the way his lungs don’t fully expand the way they should, the way he gets a little winded when he’s up and walking around. But he’s so much better than he was, and getting better every day. Thanks to the kid, and his powers.
He glances down at him; he seems fascinated by the Crest’s new decorations. Din brushes a hand over the back of the kid’s head and the little one coos, reaching out to bat at a clump of seaweed.
“You like this, huh?” he asks. “Don’t get used to it.” Soon as I’m up to it, this stuff’s getting spaced.
The kid giggles at the slimy seaweed in his hands, and Din softens. Maybe he’ll leave it up for a little bit, anyway.
He carefully takes the ladder up into the cockpit, only huffing a little. He’s grateful for the way he takes oxygen in, the way it sustains. He finally turned off the oxygen concentration function of his helmet this morning, and he hasn’t missed it. It’s a good feeling, one that’s been growing as he’s gotten closer to recovery.
He doesn’t remember much of the past few days. He remembers the Quarren innkeeper hollering outside about their time being up, until Din lurched to his feet and shoved a pile of credits at him through the crack in the door. He remembers the innkeeper, mollified, bringing up bowls of steaming soup and leaving them out in the hall for Din to slowly bring inside, one at a time. He remembers how good it tasted, rich and briny and hot, hot, hot. He remembers sighing so loudly the kid’s ears twitched, and the kid let out the longest, tiniest, happiest sigh Din had ever heard.
***
He remembers a realization.
He had found it hard to talk on the second day, between the lingering heaviness in his chest and the bone-deep exhaustion. The kid, though, had seemed to bounce right back after using his powers, and had taken to relentlessly exploring the room for things to do.
Din watched him roam, crawling under the bed, playing with the empty drawers of the dinged-up dresser, trying to climb up the wall to see out the window. The kid was gonna hurt himself if he wasn’t careful, and Din couldn’t afford another scare. He reached out and planted the kid on his lap the next time his circuit around the room brought him close.
Inspiration struck. So it was hard to speak. So what? He had options.
He held up a finger. The kid watched keenly.
Look here, he signed in Tusken, fingers splitting and then rising up to his visor. The kid tilted his head, focusing.
We can talk like this. A wide sweep, a hand raised up near the mouth, palms spreading wide. Din waited. The kid had seen him use Tusken before, but for some reason, Din had never tried it with the kid. He’d always seemed to understand Basic well enough for how young he seemed to be, but he’d never spoken a word of it that Din could make out. He wondered why he hadn’t tried this earlier.
Do you understand? Din asked, hands flattening, circling, ending with a soft point of the index finger. He asked it a few times, varying the speed and size of the question, trying to see if the child understood.
The kid’s ears quivered, as if trying to catch something far in the distance. He held out his small three-fingered hands, and tried a clumsy sign for you.
Din leaned forward, hitching a sharp breath at the effort. Do you understand me?
The kid signed you again. Tried it a few times, the word smoothing out the more he tried, getting clearer.
Good job. It was hard to say if the kid really got it, or if he thought it was just a game. But it was promising to see his ears perking up, his dark eyes wide and interested, his mouth in a toothy, tiny grin.
Din smiled beneath his helmet. If this worked, they might be able to understand each other a lot better. The kid could ask him for help. Din could make it clear what was off limits and not to be bothered with. It was heartening as hell, a bright spot glimmering in the midst of some of the shittiest days he’d had in years.
And then a name swam into his head, causing his hands to drop, slowly, back into his lap.
Ahsoka Tano.
It wasn’t going to matter soon if the kid learned Tusken or Basic. He’d be back with the Jedi.
And Din would be alone, again.
His hands, trembling, spoke for him. Fingers flashed much too quickly for a beginner to learn; phrases scaffolded in front of him, words in motion, hands unfolding with meaning he knew the kid couldn’t hope to guess. The little one gazed up at him.
Thank you for saving my life --
I promise I’ll help you, no matter what --
I’m really going to miss you, kid --
Din’s eyes stung. He blinked once, twice, and stilled his hands. He’d said too much. The kid reached out and held onto his palms, his hands weighing almost nothing at all against Din’s own.
Din swallowed, looking into those trusting eyes. “Okay, kid,” he said hoarsely. “Come on. Let’s try again.”
***
Din shakes the memory off. He knows what he has been quested to do, that Mandalorians keep their word. He’s promised to find the place the kid belongs, and he would rather die -- nearly did -- than leave that promise unfulfilled.
The door to the cockpit slides open, and Din groans. The Mon Calamari’s handiwork is even more ridiculous here than in the rest of the ship. A dangling fishnet slaps him in the helmet, and he shoves it aside irritably as he buckles the kid into his favorite seat. Even through the helmet, the whole place stinks of brine.
“Mon Calarami,” he grumbles. “Unbelievable.”
He powers up the ship, starts easing it into the atmosphere. The ship shakes beneath him, clearly wounded. He can tell by the feel and the instrumentation that the ship should hold together for travel… barely.
A strange noise catches his attention, and he reaches out, grabbing some kind of sea creature that looks like it was about to pounce on the kid. The child burbles with delight and Din shakes his head. If it’s not one thing, it’s another. He squeezes until he’s sure the creature’s dead, then hands it to the kid for a snack. It’s not as hideous as some of the things he’s seen him eat, anyway.
“I finally know where I’m taking you,” Din tells him. “But it’s gonna be a bumpy ride.”
The starfield opens up before them. He takes a deep breath -- hold together, now -- and punches it to hyperspace. The stars ribbon past them, and Din leans back in his seat, relieved. It’ll be enough to get somewhere safe. Before they find the Jedi.
The ship vibrates around them, and Din makes a running list in his head of things he needs to check, wiring that needs to be redone, processes to recalibrate, repairs that need to be made, Mon Calamari detritus that needs to be jettisoned. He could start work on it now. Get it done. It'd be the efficient thing to do.
Instead, Din turns to the kid. “Hey. You wanna practice what we learned?” His hands flash before him as he speaks, tracing out the sentence structure in Tusken. “You can do it.”
He knows he doesn’t need to bother. He can speak again without losing his breath, and what’s more, he knows the kid will leave him soon. He knows it’s not enough time to teach proficiency, that it probably won’t make a difference for the kid in the long run.
But the kid likes it, and Din does, too. Maybe that’s enough.
The kid stares at him intently, moves his small hands in little circles, makes a fist. He grins, clearly pleased with himself.
Din laughs, hands shifting in affirmation, echoing the kid’s words. “That’s right, kid.”
The kid’s hands sign again, repeating the phrase Din had gone on to teach him, the signs clumsy but clear.
You. And me.
#the mandalorian#din djarin#grogu djarin#grogu#clan mudhorn#the mandalorian fanfiction#noromo mando#whump#noncardiogenic pulmonary edema is the diagnosis if anyone is wondering#and treatment is basically... oxygen and sedation#it ain't fun!#my Mando fic
111 notes
·
View notes
Note
Omg a BTS and a new sneak peak for my little med brain to analyze! Let’s get into it! Disclaimer I work with some patients on ventilators but mostly those with brain injuries. Sometimes they have other issues like heart problems but that parts mostly guess work! Im pretty confident about medical stuff in general but the specific about hypothermia and it’s effects might be off but it’s my best guess!
Let’s start with the BTS pic in the ICU room. Same HR as before so nothing new there. Still no BP even though there’s a place for it (SHOW ME THE BP YOU COWARDS). His O2 is the only new/interesting thing on the monitor. Like I said before 94% is still normal though lower than the 100 we’ve seen. The wavelength is also kind of all over the place (it should be more smooth like a big squiggly line as he breathes in and out). The fact that it’s jumping around indicates he’s kind of struggling to pull air in and out (if he is breathing with support of the vent) or if the oxygen is not getting absorbed well by the lungs themselves (if he’s just using the vent entirely). I’m leaning more toward the first on just based on the way the wave looks to me and my experience. I can also see his respiratory rate near his O2 reading and it’s really high at 56. A normal respiratory rate is 20-30 but I’ve never seen it on the monitor like that (usually we just count it) so I don’t trust that this is entirely accurate. They can set the ventilator to a specific respiratory rate if he is dependent on it to get him a specific amount of oxygen (for example we hyperventilate patients that have brain injuries but I don’t think that’s what’s happening here).
This brings me to the vent again! The O2 wave makes me feel like he is on a spontaneous mode and breathing on his own with support from the vent. I agree with the other anon that his PEEP says 5.2 but that’s the only number I can make out haha. Like I said before 5 is normal so 5.2 is good! This supports my breathing on his own theory as well. I can’t tell his FiO2 but if the other anon is right and it’s 100% it could indicate he’s having a hard time absorbing the oxygen which could indicate lung issues such as pneumonia or fluid like I said before! Also a detail I never saw before is the little string hanging from the tube near his mouth. It’s called a cuff and it’s basically a really small tube the connects to a small balloon that’s down in his throat. You inject air through the tube to inflate the cuff and the balloon inflates to keep the tube in place and make sure no air leaks around the tube. This will be important cause they need to deflate the cuff before they take the tube out. Whenever I see vents and extubations on TV they almost always skip this part but maybe we will se it this time! But anyway I love those kind of details!
Now the scene! I’m theorizing base son what I said above about him breathing on his own and maybe having pneumonia that the doctors have him sedated so he can rest and he doesn’t fight the ventilator. They could also be doing the thing they did after he was shot and saying that lack of oxygen when his heart stopped could have caused brain damage. Either way the meds or a brain injury could cause weird dreams so there’s that! In terms of the medical stuff, the monitor rears it’s ugly head again because the doctor says he’s bradycardic but there’s just a big old red X on the monitor and it’s making a sound like there is no heartbeat at all. So does he have a slow heart rate or none at all? Make it make sense show! The doctor also tells the nurse to push epi (and then she doesn’t and isn’t even near the IV to be able to do that but whatever) and this is a valid treatment for bradycardia and cardiac arrest to get the heart to beat faster/beating again. They would probably start him on a high dose and then titrate it down to control it. I’m still on the theory that he has an arrhythmia especially because in the woods before his heart stopped Tommy shocked him for v-tach which is short for ventricular tachycardia which is a very fast heart rate. The fact that it’s jumping around from fast to slow is very characteristic of an arrhythmia. A good long term treatment for this would be a implantable defibrillator and/or pacemaker but we will see! They could also control it with medications but it would probably take a while to regulate it. All this to say that things aren’t looking good for our boy! I can’t wait to analyze all the medical stuff after the episode! Sorry this got so long but there’s so much to unpack here! Bless this ice storm for feeding my hunger for medical accuracy! Thanks for reading 💙
please never apologise for sending these messages because they are amazing and you are the best. i was so excited to see this when i woke up this morning.
that's such an interesting detail about the cuff! i'm not like 100% clear over what it means haha but i get excited about this stuff anyway. honestly every piece of info here is golden and i'm probably raising my expectations too high for how much attention they're going to pay to it but it's fun to think about while we wait.
thank you so much!!! 💚💚💚
4 notes
·
View notes
Text
Hifu Skin firm
remove Cellulite - Is Cellulite lotion a Fraud?
Content
Cellulite decrease.
Cryo, Improving The lovely video Game.
exactly How Does The Femiwand Treatment work?
Facelift treatment
Aftercare program.
Skin tightening Up, making Use Of Hifu By Levura.
" We after that use a Sodashi cream including hazelnut oil and also cypress to maintain skin smooth and also supple, decongesting any locations of cellulite and also delicately stimulating the endocrine system, which manages skin cells," claims Ostronska. Cellulite does become worse with age and this is largely down to the fact that as women grow older we produce less estrogen. Estrogen is a hormone responsible for keeping capillary streaming smoothly, so, when there is less in the body it can cause poor blood circulation, less collagen production and the malfunction of connective tissue. All of this integrated together can increase the lumpy fat under the surface of the skin and lead to more visible cellulite. This does not always connect to weight gain or shedding tone-- it is typically an inevitable concern. The 2nd significant source of the orange peel result of cellulite is when fat cells press against the skin.
Cellulite reduction.
Can you feel a prolapsed uterus with your finger?
Insert 1 or 2 fingers and place over the front vaginal wall (facing the bladder) to feel any bulging under your fingers, first with strong coughing and then with sustained bearing down. A definite bulge of the wall under your fingers indicates a front vaginal wall prolapse.
You have actually drank gallons of water, body-brushed up until your skin is red raw and also registered to every sweat-inducing exercise you can. Yet, somehow, that bothersome spot of cellulite still refuses to move.
youtube
Weight reduction does seem to boost the appearance of cellulite and also workout with good diet, although not verified, are practical suggestions with other health and wellness benefits. Specific treatments include massage, dry body brushing as well as tights covers, although there is very little science behind these therapies for cellulite.
youtube
" Watery" Cellulite-- this type of cellulite shows up and also somewhat soft to the touch. In some females, it may trigger sensitivity, varicolored skin, crawler capillaries, heavy legs, tingling in the legs and fluid retention. It is believed that watery cellulite is the outcome of blood circulation troubles because of physical inactivity or a sedentary way of living. To eliminate watery cellulite you need to work out regularly during the treatment. ' Not just does it assist maintain body fat levels lower, it likewise boosts blood circulation as well as muscular tissue tone in cellulite-prone locations. Improved circulation will keep both the skin and also connective tissue healthier, along with aiding with the elimination of waste and excess fluid retention which once again worsens the appearance of cellulite,' exposes Dr Dressmaker.
There are numerous techniques and also products that declare to deal with or lower the appearance of cellulite from topical creams, oils, body scrubs and massagers. Cellulite happens when fat down payments press with connective tissue underneath the skin, leading to the skin having a lumpy and also dimply look.
You may also have a prostate biopsy, which reveals the place of the cancer and exactly how likely the cancer is to expand and spread outside the prostate.
These tests will assist your specialist target the location of the prostate that requires to be treated.
As HIFU is fairly brand-new expertise concerning the long-lasting advantages and impacts is increasing on a daily basis.
Results from trials and early situations in the very first five years are highly urging with lifestyle end results far better than a lot of other standard treatment options.
The HIFU procedure commonly lasts in between 1-4 hours, depending on the size of the prostate, as well as is either done under basic anaesthesia or an epidural and also IV sedation.
If https://bristol.lipo-sculpt.co.uk/ opts for a body contouring treatment, fat cells are eliminated using lipolysis.
Optimum cosmetic results are possible with just one therapy session, the case study pictures below offer an instance of the arise from HIFU treatment.
lose stomach weight as well as an absence of physical exercise can enhance the likelihood of cellulite appearing. This is due to the fact that an unhealthy lifestyle suggests you are more likely to build up fat cells which will push on skin, triggering it to dimple. Not just this however being less active for long periods of time will affect your circulation, as well as a lack of blood circulation will restrict your bodies regrowth as well as repair work. Overeating particular foods such as those that are processed, high in sugar or salt can also enhance your chances of cellulite developing. Cellulite types in locations with the least flow so, without task, it is extremely difficult to move. Day-to-day energising motions as well as skin warming exercises will have you biding farewell to dimpled skin if you are consistent with it.
Cryo, Improving The stunning video Game.
Can a guy tell if a girl is virgin?
It's possible, but not guaranteed that he won't know. Will he be able to tell you're a virgin by looking at you naked? No. In fact, some experts say there may be no way to tell if a woman is a virgin, even with gynecological tests.
" The radiofrequency likewise tightens up the skin which further aids with improving the cellulite," states Dr Edwin. That stated, although it might lessen the look of cellulite temporarily, our bodies will continue to make more afterward. Scientists do not actually know what creates cellulite, however it's believed to be connected to the body's inability to eliminate toxin, fat as well as liquid. It becomes trapped under the skin as well as causes coarse tissue to become hard, that is the dimpling impact we see. " I like all 3 of the functions that the Onda often tends to provide, I such as the truth that it is an efficient cellulite decrease technology as well as there is nothing else innovation that does the same non-surgically. We provide therapy to men and women and are seeing excellent results with both.
This makes the orange peel look even more noticeable, as a few of the skin is now being pushed out, while other sections are being pulled in. The treatment entails placing probes on the areas of the cellulite which then send out radial waves called shockwaves. The shockwaves then work to interrupt the fat cells and also break down the sclerotic fibrous cells. This cells is what is accountable for much of the uneven as well as lumpy look of cellulite. A more method it works is by firming the skin by increasing the collagen manufacturing and motivating lymphatic drain. So, Fat freezing toning Warwick are purged away, enhancing the skin's look. 3D Shockwave treatment can be utilized on the upper legs, butts, abdominal area, arms, hips as well as knees.
What is vaginal tightening?
Vaginoplasty is a procedure that aims to "tighten up" a vagina that's become slack or loose from vaginal childbirth or aging. Some surgeons claim it can even improve sensitivity -- a claim the American College of Obstetricians and Gynecologists (ACOG) has strongly challenged.
Plainly females have cellulite extra prevalently than males, however, with the ageing process of guys there is estrogenization and also we are seeing skin comparable to cellulite. Person safety and security is a priority, as well as what we locate with the Onda is that we can be rest assured that it is one of the safest therapies we can offer our people, especially when it is related to tissue damage, to burns and to adverse outcomes". One option to deal with cellulite available in centers is Radiofrequency. This modern technology functions by warming the skin as well as breaking coarse cells, while ultrasound breaks up the fat cells. Incorporating these treatments offers clinics with an excellent remedy to cellulite decrease however, the visual market along with people continue their search for a purpose-built, devoted treatment remedy.
Why does my girlfriends VAG smell like BO?
When sweat mingles with fluids in and around your vagina, your natural scent may change. The odor may grow stronger if you're sweating a lot, like during warm months or after exercise.
just How Does The Femiwand Treatment work?
Cellulite appears when fat cells under the skin press versus connective tissue, causing the skin to dimple. Due to just how cellulite is created, it is near impossible to totally remove at home, however there are a few things you can do in the house to help reduce the occurrence of cellulite.
Facelift treatment
' However a mix of correct diet plan as well as exercise will certainly reduce the layer of fat underneath the skin, making cellulite less noticeable. A healthy and balanced diet plan can also boost the skin as well as connective tissue; making them more powerful, healthier and much more flexible. Remaining moisturized and eating well will certainly avoid water retention which aggravates the appearance of cellulite,' she clarifies. Researchers have actually worked for years to look for reliable as well as resilient therapies for cellulite with little success.
You can utilize this therapy as part of a fat reduction programme or as a standalone therapy, both delivering visible and superior outcomes. 3D Shockwave treatment is effective enough to decrease the appearance of also the hardest cellulite, training and firming the skin. The wall surfaces of the blood vessels are developed by an elastic tissue that allows a fluid flow of the blood. When these wall surfaces shed flexibility, the rate of the blood flow is reduced. As opposed to being excreted, excess fluids as well as waste products obtain pressed in the direction of the adipocyte cells where they connect to the fat cells triggering cellulite and swelling. The transportation of oxygen and nutrients is additionally decreased creating the metabolism to reduce. The existing technique to help reduce the look of cellulite starts with suggestions to increase workout as well as optimize the diet plan.
Aftercare program.
How do you relax pelvic floor spasms?
Place one hand on your chest and another hand on your belly, just below your rib cage. Take a deep breath in to the count of three, and then exhale to the count of four. When you inhale, your pelvic floor relaxes, and as you exhale, your pelvic floor returns to its resting state.
Skin firm, utilizing Hifu By Levura.
No one needs to ever feel ashamed that they have cellulite or like it is something that they merely must eliminate. Cellulite is perfectly regular and is something that over 90% of all ladies have to some level.
To assist avoid cellulite, lowered processed foods as well as fabricated foods which contain sugar, ingredients and also chemicals. Dairy as well as high fat items, sugar as well as high sugar items are all believed to add to the dreaded 'orange peel' skin. If your task has you sat behind a workdesk 8 hrs a day, attempt to include workout during your lunch break, or after job.

ONDA An innovative new non-surgical body forming equipment like nothing else. Supplying fat decrease, cellulite reduction, as well as skin tightening up treatments without downtime. " A bit like waxing, there's no discreetness with this therapy yet it is, weirdly, relaxing. My therapist started with a mild peeling to help start damaging down fat cells. A lymphatic drainage massage utilizing Cellcosmet's anti-cellulite oil was alongside urge circulation and assist the body to eliminate toxins. The massage therapy is a solid pressure and concentrates on the areas that are more than likely to harbour these fatty accumulations.
Gradually, your body normally generates much less as well as less collagen and elastin, and as lady age, the female body produces much less oestrogen as well as cells blood supply is lowered, this decreases the amount of collagen in the connective cells fibers. When connective tissue fibres weaken, the bulging worsens raising the look of cellulite on the skin's surface.

Running, swimming and also quick walking are some of the best kind of workouts for raising blood flow and loosening the fat tissues from those difficult to budge areas. A radiofrequency handpiece is used with a tiny specialist suggestion to break the connective tissue strands and release the fat to produce an also skin contour.
We can decrease the look of unwanted cellulite using the latest Venus Legacy innovation, which combines Multi-Polar Radio Frequency, Pulsed Electro Magnetic Area as well as VariPulse Innovation to generate heat deep under the skin's surface. This assists to reduce fat cells, minimize quantity and stimulate natural recovery. This process likewise raises collagen and elastin production, tightening and also lifting the skin. If you do not typically take pleasure in a standard massage or you desire a treatment that will certainly deliver instantaneous outcomes-- smoother, softer and also stronger skin that's Instagram-worthy-- after that a professional salt scrub is your best choice. " The PH equilibrium of Himalayan salt is unbelievably near that naturally found in our body," exposes Ostronska. It's additionally among the very best therapies for guaranteeing you obtain a restful night's sleep ... Coastline body goals worth going for.
#hifu treatment#facelift#fat freezing#femiwand#Cryo#Cryopen#cellulite#Femiwand treatment#skin tag removal#Bucks vaginal tightening#hifu facial#fat freezing service#cryolipolysis#Bodybuilding for Weight Loss#lose stomach weight#fat legs treatment#Anti aging hifu#Mens facelift treatment#Double chin removal#coolsculpting#wart removal#cellulite treatments#Non surgical facelift#body and face toning#Lipo freeze
1 note
·
View note
Text
replacing An Excess Skin With A Facelift.
Hifu Treatment
Content
What Can I expect during My Cryopen therapy?
two therapies.
Cryomatic Ii Cryo Console.
contact united States Today For Your Cryo storage Space Solutions (or Anything Else Gas Or Cryo Related).
Femiwand vaginal Area tightening treatment Edinburgh.
See Our providers.
What Can I Do To lessen Cellulite?
There is nothing that I feel can be improved at Cadogan Cosmetics. I was dealt with as well as cared for very well the location was very clean.

Cosmetic surgery outcomes as well as benefits can differ and also are various for each person. Therefore, https://luton.hi-fu.co.uk/ can not ensure specific results. Mr Alamouti is among our top boob job, fat reduction & abdominoplasty surgeons.
Nevertheless, it is essential to remember that although your external look will certainly look healthy and balanced and recovered, inside your body will certainly still take 6 to eight weeks to recover completely. The outcomes of the Principle ™ Facelift procedure will certainly leave your with a natural, fresh as well as vibrant appearance that lasts up to ten years. I really feel so excellent regarding myself and also can not think how much far better I appear to look. I would very advise having surgical treatment with Amir at Bella Vou. I really feel much more youthful and also revitalised in my look, as well as it's all thanks to Bella Vou.
Mr Super qualified in Medication in 1987 and also learnt Bariatric surgical treatment in 2001. We'll exist to assist throughout your journey, from yourfirst consultationto completion of yourcomprehensive aftercareprogramme. Facelift surgery can offer you a more vibrant and renewed appearance. Consent By ticking this box you consent to obtain marketing material by means of email, text, post and telephone calls from The Medical facility Team and Transform and any third parties directly related to your care.
Can you get frostbite from cryotherapy?
Frostbite is possible if someone has wet clothing or is overly sweaty during the session. Make sure the client is completely dry before they enter the cryotherapy chamber. If not make sure they dry off any water or excess sweat from working out with a towel.
What Can I anticipate during My Cryopen treatment?
Hi-Fu.co.uk hifu Daventry: full feature set will certainly ask you concerning the results you're wishing for and also deal with you to attain the best end result. Springfield Medical facility opened up in 1987 and is just one of Essex's leading private healthcare facilities. It is a 64 bedded device containing fifty 8 private bedrooms 4 of which are 2 bedded moms and dad as well as child areas and a high observation system with 2 beds. The operation is performed under a basic anaesthetic and also normally takes two to three hours.
What is the cost of ThermiVa?
The Non-Invasive, Non-Hormonal Option Average Cost: $2,650. Range: $1,250 to $3,900 for 3 treatments for the first year. One follow-up appointment per year: $1000-$1500 per year afterwards. ThermiVa is NOT covered by insurance or Medicare.
Tea and coffee are high in caffeine, so we suggest you to keep those to a minimum. Also, attempt to stay clear of foods that are high in sugar and salt as high as feasible. These include the advancement of a blood clot, nausea or vomiting as well as vomiting, as well as postoperative pain. As the surgical treatment entails the use of an anaesthetic representative, it is likewise feasible that you may create anaesthetic issues. At the end of the surgical procedure, the registered nurses will certainly move you to a recovery space. Below, you will slowly wake up from your anaesthetic under close guidance.
My skin is tighter and also more flexible, stretch marks are hardly noticeable, as well as I make certain I wouldn't even get approved for abdominoplasty surgery anymore.
As the ultrasound waves are focused throughout the treatment areas, you will certainly really feel small quantities of power transmitted with to accurate depths under the skin.
Dr Dhillon will evaluate the skin and assistance figure out if HIFU is the most appropriate treatment to deal with any type of concerns patients might have, factoring in the condition of the skin and the individual's unique goals.
A full HIFU face as well as neck procedure normally takesbetween minutes, while an upper body treatment on its own will certainly take about thirty minutes.
A gel is applied to the location that will be treated as well as the ultrasonic tool is overlooked the skin.
Routine touch-up treatments will certainly aid keep the skin producing new collagen and also prolong the longevity of results.
Some clients delight in an initial result immediately complying with the treatment, yet the ultimate results will take place in simply 2 to 12 weeks, as exhausted collagen is renewed as well as renewed.
There is no special prep work or recovery as well as usually on the face it usually takes one treatment to obtain a recognizable outcome on the body a program of 4 therapies generally obtains the preferred outcomes.
two therapies.
The procedure takes in between 1 - 1.5 hrs, can be performed either under local anaesthetic or sedation, and is treated as a day case. The natural aging process will certainly proceed from the factor accomplished following the procedure.
You want to redefine your face by lowering loose, drooping skin. The appearance of your face is making you look older than you feel.
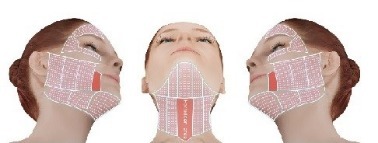
Cryomatic Ii Cryo Console.
We have actually invited an option of the country's very best specialists to join us at the Cadogan Center to ensure that you can be sure that whatever the nature of your treatment, you will be seeing one of the top professionals in the country. A 'mini-lift', or 'mini-facelift', is an innovative anti-ageing procedure that uses the most recent minimally intrusive medical strategies to transform the clock back on the age of your face by about 10 years. I really felt entirely safe and guaranteed, he explained every little thing in fantastic information and I really felt really confident that I would get the appearance I wanted, and also I did I'm thrilled with the end result. Among the Bella Vou group will certainly give you a phone call the day after surgical treatment to see to it you're well, have actually had a great evening, and to address any kind of questions. Prep work for your treatment can help reduce the danger of infection and also boost recovery. Shower and also laundry hair everyday as well as quit smoking cigarettes as well as e-cigarettes to minimize the danger of healing issues. Sometimes people present earlier, in their early forties as well as the treatment can be successful in the seventies, eighties or even nineties.
youtube
The benefit of the Principle ™ Facelift is that it is under local, not a general anaesthetic, making it much safer for individuals with existing clinical issues. Bella Vou is committed to offering fulfillment, the highest possible requirements of treatment, and a very personal touch throughout the client journey. The highly-skilled, professional personnel are enthusiastic concerning helping people achieve the results they desire, but likewise making their experience delightful, stress and anxiety, and convenient. You will have little bruising, swelling, or scarring complying with the Concept ™ Facelift. Many people can go back to their normal regular within an issue of days.
get In Touch With united States Today For Your Cryo storage Space Solutions (or Anything Else Gas Or Cryo Related).
How can a 60 year old lose belly fat?
Burn more calories than you eat or drink. Eat more veggies, fruits, whole grains, fish, beans, and low-fat or fat-free dairy; and keep meat and poultry lean. Limit empty calories, like sugars and foods with little or no nutritional value. Avoid fad diets because the results don't last.
I feel more certain, I felt there was a more youthful person waiting to venture out, it has actually made a great difference to me and also how I feel. The entire experience has actually been superb as well as I'm over the moon with my outcomes. The treatment defined on this web page might be adjusted to meet your individual needs, so it is very important to follow your medical care professional's guidance and also raise any kind of inquiries that you might have with them. Also after you've left medical facility, we're still looking after you every step of the means. Once you're ready to be discharged, you'll need to prepare a taxi, pal or relative to take you house as you will not be able to drive. You must additionally ask if they can run some light tasks such as looking for you as you won't be really feeling up to it.
Woodland Hospital has 28 solitary areas, all with en collection facilities, 10 short remain beds as well as a 2 bedded high dependency device. If you would like to talk with somebody what is included and also just how much the procedure will set you back, call our team on, or leave us a message via our online query type here. Other sorts of facelift include the mid-face lift and composite facelift and also include lifting much deeper layers of the face. A healthy diet regimen is an essential factor in assisting you to heal and recoup after a facelift. Eat great deals of healthy and balanced environment-friendly veggies, fresh fruit, and high-protein foods such as chicken, fish and also legumes.
Does Cryo hurt?
HOW WILL MY BODY REACT TO THE COLD TEMPERATURE? Cold air therapy in the whole-body chamber uses dry, oxygenated air, so you won't experience shivering, goosebumps or other reactions that you might associate with being cold. Because of this technology, unlike an ice bath or immersion, cryotherapy is not painful.
There are many various other anti-ageing solutions readily available, both surgical and also non-surgical. Ask for a telephone call from among our client advisors or publication an appointment at the Cadogan Center if you would love to review your problems in more information. You may function from home the following day, yet it will certainly rely on just how sensitive you are to the discovery of current surgical treatment, as to when you head out to fulfill individuals. The factor is that you will certainly not be jeopardising the result by going out. Our Surgical Client Expert, Ellie, addresses our patients most regularly asked inquiries. Adhering to the procedure, you will certainly recuperate in our ambulatory healing rooms for in between two to three hrs, depending on the scale of the procedure. Once our professional nursing team more than happy that your first recuperation is full and also you are secure to return home, you will be permitted to leave the Clinic come with by a good friend or participant of your family members.
Femiwand vagina tightening Up therapy Edinburgh.
The results of Mini Face Lifting surgical treatment are anticipated to be stable for 3-- 5 years, however note that as you mature your face will certainly transform throughout the years. For instance, the tissues around the cheek will remain to be influenced by the aging adjustments and also gravity. People can go back to their normal day-to-day tasks after 1 week, however prevent difficult exercise/ activity for 6 weeks including any contact sporting activities. Mini Facelift Surgery usually takes approximately 1 -2 hrs to carry out depending on the complexity of the surgery. Muscles additionally shed their size and stamina as well as with loss of bone particularly around the upper as well as lower jaws, the face handles the regular functions of aging. The skin loses collagen as well as hyaluronic acid, with sun-damage and contamination, pigmentation, fine blood vessels as well as wrinkles show up.
Is Cryoskin better than coolsculpting?
The product of these improvements is Cryoskin: a treatment system that is faster and more effective than coolsculpting. Cryoskin fat-freezing treatments are faster than coolsculpting and are more customizable. Cryoskin technicians hold an instrument that gets cold, then they move it around your targeted areas.
The skin loses flexibility and also ends up being lax, fat reductions and also comes to be displaced by gravity creating the common jowls, level cheek and reduced eye bags. Please supply a little more information so we can obtain the most effective member of our team to call you back each time to match you. The Cadogan Clinic is an award-winning boutique exclusive healthcare facility on Sloane Street in the heart of Chelsea. We offer one of the most sophisticated medical and also non surgical strategies in our fully-fitted consulting rooms, advanced operating theaters and purpose-built aesthetics as well as laser collection. The Micro-Lift treatment is made to assist alleviate very early indications of aging and also moderate loss of flexibility loss. Picking a surgeon who is an expert in their field and also concentrates on face-lifts will certainly make certain you get the very best outcomes possible.
Clifton Park Medical facility which opened in 2006, is located just outside York city centre. The healthcare facility has actually been rated 'Great' by the Care Top Quality Compensation and also has 24 beds, 2 theatres, a day situation system, a huge outpatients department with x-ray facilities and on-site physiotherapy, including a tiny fitness center location. Free auto auto parking is offered for simple accessibility to our easily positioned hospital just outside of York city centre. Our health center is registered with the Treatment Quality Payment and has superior facilities. We offer fixed price packages for our facelifts so you can feel confident there won't be any economic surprises. We suggest you to refrain from any type of exhausting activity for the very first 8 weeks. You can expect to return to work after one to two weeks, and after 3 weeks if you have likewise had a blepharoplasty.
You can contact our clinical cosmetic team anytime, day or evening if you have any worries or questions. Timberland Hospital is just one of Northamptonshire's leading exclusive hospitals situated in Kettering.
Both nurses who I handled were superb, as well as the whole team got along however specialist, and actually put my mind comfortable. That I was able to remain later than I probably required after my surgical treatment to harmonize my husbands routine was substantially valued. If you have any type of concerns or questions please phone call to talk to among our consultants or demand a recall to talk at a time that suits you.
#hifu treatment#facelift#fat freezing#femiwand#Cryo#Cryopen#cellulite#Femiwand treatment#skin tag removal#Bucks vaginal tightening#hifu facial#fat freezing service#cryolipolysis#Bodybuilding for Weight Loss#lose stomach weight#fat legs treatment#Anti aging hifu#Mens facelift treatment#Double chin removal#coolsculpting#wart removal#cellulite treatments#Non surgical facelift#body and face toning#Lipo freeze
1 note
·
View note
Text
Some Things I’ve Learned After My Family and I Tested Positive for Covid 19
It started as my younger brother just thought he had a sinus infection and my dad got the chills near August 18th. My dad went to the doctor 2 times by himself and wasn’t tested and told he was ok and to just rest at home. On August 25th, my mom accompanied my father to the hospital and demanded for him to get tested for Covid 19. It was a Tuesday and his results came back positive within hours. He had a health history of having Chronic Bronchitis, Diabetes, and High Blood Pressure. They were simply told for him to take Tylenol and rest at home. There was no guidelines or safety protocols to address him being at high risk for worsening at home...just go home and come back if it gets worse. I am so angry he was blown off when he went on his own and was not tested as well as when he was sent home after testing positive with no advice on how to effectively treat at home. I started to feel fatigue on the same day, August 25th. I went to get tested on August 26th and my results came back positive in less than 4 hours. I was told by my doctor that I had been contagious since the weekend before even though I exhibited no symptoms. So now when I see a table for screening for temperature checkers, I know how misleading it is to the public. Having a fever first for this virus is not accurate and giving the public the false illusion of health. Once you’re exposed to Coronavirus and infected, you are contagious without exhibiting any symptoms for 3 to 4 days since it’s incubating. The symptoms are not continuous while ill, they come and go like the cough, diarrhea, headaches, chills, sneezes, and other symptoms. My older brother caught it and he coughed bits of blood in his phlegm but I did not. My sister has problems with asthma and she was infected so she did nebulizer treatments at home. On August 27th, my mom tried to wake my dad up from bed and he was unresponsive. She immediately called 911 and EMS was dispatched. Once here they tested his sugar level and he was at 49 which is terribly low. His wrists were folding in and it looked like he was having a seizure. EMS gave him the glucose shot to get his sugar levels back to normal and he looked like he was really feeling the injection which made him very disoriented. EMS decided to take him to the hospital with his gold necklaces and gold cross and pendant on. EMS did not tell us to take his jewelry off and my mom and I were in too much shock to interrupt them taking him away to retrieve his personal items. Needless to say his jewelry went missing and my dad never returned home but I believe the doctors should have effectively educated us on how to treat at home. We had no glucose injection and if he needed to to breathing treatments, I would have sanitized my C-Pap machine and let him use it. I know my dad did not have a good experience in the hospital even though the medical teams did their best but he had anxiety with the treatment and they sedated him. His respiratory issues became worse and believe they should have given him a better mask that would not hurt the bridge of his nose but have nasal pillows with a mouth guard that kept the mouth shut so he wouldn’t get as dehydrated with a dry mouth. The pressure of the oxygen seemed to due more harm then good then he started to have pneumomediastinum. I visited my dad 3 times in ICU. The first visit he was wearing the nasal pillows and was able to talk. He looked so scared and sad repeating, “God, please help me. I want to live God, please don’t let me die.” I was so heartbroken seeing him this way. He was upset before being placed in ICU because his gold chains, cross, and St. Joseph pendant were nowhere to be found. I went to several churches during that time and prayed so hard. I went to St. Joseph’s Church on Tulane and bought a very basic but humble wooden cross for him. I visited him a 2nd time all by myself and gave him the cross and told him not to worry about the jewelry that went missing. He was in a nose and mouth bi-pap mask but could not talk although he tried to. I spent four hours with him, holding his hands, massaging his hands, feet, neck, and prayed and told him so much. The third time I visited, I could see him declining and I pretty much had a nervous breakdown after that where I was admitted to a Behavioral Health Center. I came around the day after he passed and knew I had to get better to help my family, especially my mother. I am trying to find out what happened to his belongings and see why he was turned away by doctors in the beginning. I know none of this will bring him back but I have to try and put the pieces together so I can file grievances. It feels like everything has happened so fast and he had been so careful for almost 6 months with not getting Coronavirus. I have cried, cried, cried, prayed, prayed, prayed, and have asked why, why, why.
I’m hoping to address some things in regards healthcare in the way they’ve been handling treatment measures at home with zero instruction especially towards those with comorbidities. Although I am healthy now after going through having the virus, my job won’t take me back until I test negative which could take an additional 2 more months since it takes about 3 months for the virus to shed completely. I’m using this time to mourn my father and to make some changes in my life. Losing my father has been devastating for me but I’ve know people who’ve lost both parents consecutively so grateful my mom’s case was mild. I hope my story can help someone in some way if the get this vicious virus. I still feel it will be a while before these crazy times to end.
Love and light,
G
1 note
·
View note
Text
The measure of oxygen your blood conveys all through your body is pivotal for rest quality and your wellbeing when all is said in done
and sound blood oxygen levels during rest is needy upon your nature of relaxing. In case you’re one of 54 million individuals in the United States with rest apnea, your oxygen admission is being disturbed, which can prompt a huge number of medical problems.

What is beat oximetry? What’s more, how can it sway rest?
Heartbeat oximetry is a noninvasive and easy test that quantifies the oxygen level in your blood (or your oxygen immersion level). It rapidly distinguishes even little changes in how proficiently oxygen is being conveyed to the limits farthest from the heart, including the legs and the arms.
A heartbeat oximeter is a little gadget that cuts on a body part, similar to a finger, a toe, an ear cartilage and the temple. It’s frequently utilized in a basic consideration setting like a crisis room or a medical clinic, and a few specialists may utilize it in office as a feature of a standard exam.

When the beat oximeter is joined to a body part, little light emissions go through the blood estimating the measure of oxygen. It does this by estimating changes of light retention in oxygenated or deoxygenated blood. A heartbeat oximeter will disclose to you your oxygen immersion levels alongside your pulse.
When breathing gets upset during rest (called a quit breathing occasion or SBE), as may happen in obstructive rest apnea, the oxygen levels of the blood may more than once fall. Drawn out drops in oxygen levels during rest are known to prompt an assortment of wellbeing difficulties like sorrow, coronary illness, hypertension, diabetes and that’s only the tip of the iceberg.
For what reason may I need beat oximetry?
There are numerous circumstances where your PCP will need to quantify your blood oxygen level with a heartbeat oximeter, including:
· During or after medical procedure or strategies that utilization sedation
· To check an individual’s capacity to deal with expanded movement levels
· To check if an individual has minutes when breathing quits during (rest apnea)
Heartbeat oximetry is likewise used to check the wellbeing of an individual with any condition that influences blood oxygen levels, for example, coronary episode, cardiovascular breakdown, constant obstructive aspiratory malady (COPD), iron deficiency, lung malignant growth and asthma.
Heartbeat oximeters and rest apnea
On the off chance that you are being tried for rest apnea, a rest specialist will utilize beat oximetry during a rest study to assess how frequently you quit breathing during the night. The beat oximeter contains a red light sensor that radiates through the outside of your skin to gauge your heartbeat (or pulse) and the oxygen substance of your blood. The oxygen level in your blood is estimated by shading: exceptionally oxygenated blood is progressively red, while blood that is low in oxygen is increasingly blue. This progressions the recurrence of the light frequency that is reflected back to the sensor. These information are recorded for the duration of the evening of your rest test and are recorded on a chart. Your rest specialist will audit the diagram at the finish of your rest test to decide whether there were unusual drops in your oxygen level during your rest test. In the event that you have visit plunges in blood oxygenation, it’s possible you have rest apnea.
What is a decent oxygen level during rest?
An oxygen immersion level more than 95 percent is viewed as typical. Anything under 92 percent oxygen in your blood might be an indication that you have breathing issues during rest, which could mean you have rest apnea or another turmoil like serious wheezing, COPD or asthma. Be that as it may, it’s significant for your primary care physician to see how much time you went through with oxygen immersion under 92 percent.There can be drops in oxygen levels that are not long enough or low enough to be called irregular or undesirable for your body. For instance, a few seconds with 80 percent oxygen immersion for multiple times in a single night may not be an explanation behind concern.
In the event that you need to find your blood oxygen levels during your rest, you could go to a rest lab to have a short-term rest study, or you can utilize a heartbeat oximeter to screen rest at home.
The beat oximeter can be an extremely helpful clinical gadget for rest apnea patients. It’s a lot less expensive than a rest study, and it can uncover significant data about your rest quality or how viable is your rest apnea treatment.
Best Pulse Oximeters for Coronavirus
Wednesday, 18 March 2020 | Frances
In the tumult of the current coronavirus flare-up, access to testing is constrained. With side effects of the disease extending from gentle to serious, it very well may be hard to tell whether you ought to be stressed in the event that you begin to feel sick. Be that as it may, there is an approach to screen lung wellbeing at home.
Heartbeat oximeters give a qucik and simple approach to check blood oxygen levels
In the US, patients with milder side effects of coronavirus are being sent home with gadgets known as heartbeat oximeters. These astute machines measure the measure of oxygen in your blood, which can give you pieces of information about your lung wellbeing and how well oxygen is being siphoned around your body.
Timesco produce the absolute most precise heartbeat oximeters available and our specialists have incorporated this guide so you locate the correct one for you, regardless of whether you’re a specialist or stay-at-home parent. Peruse on to find how a heartbeat oximeter can support you.
The Dangers of Coronavirus
There is no uncertainty that coronavirus represents a noteworthy hazard to our populace’s wellbeing. While most of those contaminated just experience mellow sickness, others have created unmistakably progressively genuine respiratory conditions, or even respiratory disappointment. To shield ourselves from such entanglements, it can assist with watching out for our respiratory capacity in the event that we begin to catch side effects, including:
High fever
· Another, persistant hack
· Counteraction Over Detection with Hand Sanitiser
· Relisan Alcohol Hand Sanitiser (500ml)
Relisan Alcohol Hand Sanitiser (500ml)Pulse oximeters are an important device for coronavirus location, however nothing can supplant great cleanliness practices to forestall disease. The Relisan Alcohol Hand Sanitiser (500ml) adequately eliminates germs, microscopic organisms and infections following 30 seconds, making it a phenomenal first line of safeguard against disease.
Key Features: 70% denatured liquor adequately kills infections and microbes in 30 seconds.
Shop Now
In what capacity Can a Pulse Oximeter Help?
In progressively genuine instances of disease, coronavirus can make harm your lungs, making it hard for your body to get enough oxygen. A heartbeat oximeter utilizes a brisk, easy, non-obtrusive strategy to quantify the ensure your oxygen levels, or ‘oxygen immersion levels’, are inside a sound range (ordinarily around 95% to 100%).
Taking a perusing is basic: a brace like gadget is put on your finger, ear cartilage or toe and little light emissions go through your blood. The beat oximeter than measures the measure of light consumed by oxygenated and deoxygenated blood. On the off chance that your oxygen immersion is excessively low, you’ll have the option to look for clinical consideration straight away.
· Our Best Pulse Oximeter for Coronavirus
· Timesco C29 Fingertip Pulse Oximeter
Timesco C29 Fingertip Pulse OximeterThe Timesco C29 Fingertip Pulse Oximeter is our pick for the overall best heartbeat oximeter for coronavirus. In addition to the fact that it measures your oxygen immersion inside an all-inclusive scope of 70% — 100%: ±2% exactness, it additionally permits you to check if your heartbeat is in a solid range (60 to 100 pulsates every moment). Your readings can be gotten to in a visual waveform, so you can spot changes at an opportune time.
Key Features: Measures wide scope of oxygen immersion levels just as heartbeat.
Shop Now
· Look at Out Full Range of Coronavirus Protection
· The Best Pulse Oximeter for Home Use
· Timesco CN130 Fingertip Pulse Oximeter
Times CN130 Fingertip Pulse OximeterYou can work the Times CN130 Fingertip Pulse Oximeter with only a bit of a catch, settling on it an incredible decision for the patient’s checking their indications as home. The red, single-shading LED screen is anything but difficult to see and readings are introduced in a far-reaching style. It additionally includes a heartbeat bar for a visual portrayal of the heartbeat.
Key Features: Easy to utilize and worked with a just bit of a catch.
Shop Now
The Best Pulse Oximeter for Frequent Monitoring
Times CF3 Fingertip Pulse Oximeter
Times CF3 Fingertip Pulse OximeterFor the individuals who need to screen their indications all the more habitually, the Times CF3 Fingertip Pulse Oximeter is an unquestionable requirement. Fit for 30 hours of ceaseless use with the 2 x AAA batteries gave, the oximeter is intended for lower power utilization, so it won’t run out regardless of whether you take a few readings per day. The showcase brilliance can likewise be diminished, so you won’t upset an accomplice whenever utilized during the night.
Key Features: 30 hours of persistent use, low force utilization, and low force pointer
With these Timesco heartbeat oximeters, you can loosen up realizing you can watch out for your wellbeing. Whichever you pick, you’ll have the option to get too snappy, precise data about your body’s working at whatever point you need it. In the event that you’d like increasingly respiratory help, investigate our scope of Breathing Apparatus.
1 note
·
View note
Text
China/Wuhan nCoV Government Report
Epidemic situation of new coronavirus infection on January 23, 2020 (All times in Chinese timezone) As of 24:00 on January 22, the China Health Emergency Office had received a total of 571 confirmed cases of pneumonia of new coronavirus infection in 25 provinces (autonomous regions, municipalities) in China, including 95 severe cases and 17 deaths (all from Hubei Province). A total of 393 suspected cases were reported in 13 provinces (autonomous regions and municipalities).
At 00:00 on the 22nd, 24 provinces (autonomous regions and municipalities) reported 131 new confirmed cases and 8 new deaths, of which 5 were males and 3 were females, with the exception of 1 except 53 years old, and the rest were 65 Elderly people over 5 years old and 5 cases over 80 years old have chronic and basic diseases such as postoperative cancer, liver damage, hypertension, coronary heart disease, diabetes, and Parkinson. 13 provinces (autonomous regions and municipalities) reported 257 new suspected cases. A total of 25 provinces (autonomous regions and municipalities) reported epidemics nationwide, and 4 provinces including Hebei, Liaoning, Jiangsu and Fujian were added.
At present, 5,897 close contacts have been traced, 969 people have been released from medical observation, and 4,928 people are still receiving medical observation.
Medical history of all 17 deaths...
Zeng XX, male, 61 years old, has a history of liver cirrhosis and myxoma. Fever started on December 20, 2019, with cough and weakness. She was hospitalized in the Department of Respiratory Medicine of Wuhan Puren Hospital on the 27th, transferred to the ICU on the 28th, was endowed with mechanical intubation on the 30th, and transferred to the ICU of Jinyintan Hospital on the 31st; Shock coma when entering. On January 1, ECMO support, anti-infection, anti-shock, and corrective acid symptomatic supportive treatment. At 20:47 on January 9, the heart rate of the patient suddenly became zero, and the ECMO blood flow rate decreased rapidly to 0.2 liters / minute. Rescue immediately. By 23:13, the heart rate was still 0, and clinical death was announced.
Xiong XX, male, 69 years old, was admitted to Wuhan Red Cross Hospital for 2 days due to fever and cough for 4 days, and exacerbated with dyspnea. On January 3, 2020, a tracheal intubation was connected to a ventilator to assist breathing. Myocardium The enzyme profile persists. Transferred to Jinyintan Hospital on January 4. Admission diagnosis was acute respiratory distress syndrome, respiratory failure, severe pneumonia, unconsciousness, pleural effusion, and aortic atherosclerosis. A CT scan of the patient's chest revealed large ground-glass opacities in both lungs. ECG: ST segment changes. After admission, he was treated with intensive care, ventilator-assisted breathing, prone ventilation, and symptomatic and supportive treatments such as CRRT, anti-infection, and liver protection. His condition did not improve. Septic shock, microcirculation failure, coagulation dysfunction, and internal environment disorders Sexual aggravation. At 00:15 on January 15, the patient's heart rate dropped to 0, and norepinephrine, epinephrine, pituitary, and dopamine were continuously pumped into the anti-shock therapy. The patient failed to recover spontaneous breathing and heartbeat until 0:45. The electrocardiogram at the bedside showed total cardiac arrest, and clinical death was declared.
Wang XX, male, 89 years old, has a history of hypertension, cerebral infarction, and cerebral softening. Due to urinary incontinence, she was referred to the Department of Urology, Tongji Hospital on January 5, 2020, and was transferred to the emergency department on January 8 due to drowsiness and unconsciousness. The examination revealed lung infection (viral pneumonia) and acute respiratory failure. On January 8th, a physical examination revealed that the patient had 77mmHg and showed hypoxia. Lung CT showed double lung patch shadow, bilateral pleural effusion, and pleural adhesion. Blood routine showed a progressive increase in white blood cell count and a low lymphocyte count. On January 9th, he was transferred to the outpatient clinic for emergency treatment and was given symptomatic supportive treatment. On January 13, the ventilator was assisted with positive pressure ventilation. Drowsiness occurred on January 14th. With ventilator-assisted ventilation, blood oxygen saturation fluctuated between 50% and 85%. Entered the Infectious Diseases Ward on January 15. Before transfer at 10:30 on January 18, Bp140 / 78mmHg, SPO2 85% under non-invasive ventilator-assisted ventilation. During the transfer, the patient suffered a respiratory arrest, continued rescue for 2 hours, and the treatment was invalid. The clinical death was announced at 13:37 on January 18, 2020.
Patient Chen X, male, 89 years old, had previous hypertension, diabetes, coronary heart disease, frequent premature ventricular contractions, and coronary stent implantation. The patient developed symptoms on January 13, 2020. There was no obvious inducement of asthma 4 hours before the consultation, and he felt dyspnea and no fever. On January 18, she went to the emergency department of Wuhan Union Medical College for treatment due to severe breathing difficulties. The patient was old and had a positive pathogenic examination of Chlamydia pneumoniae, no A and B flow, a new coronavirus positive, and CT of the lung: typical changes in viral pneumonia. At 23:39 on January 19, 2020, his condition deteriorated, and the rescue died.
Li XX, male, 66 years old, previously had COPD, hypertension, type 2 diabetes, chronic renal insufficiency, ascending aortic artificial aorta replacement in 2007, abdominal aortic stent placement in 2017, Cholecystectomy, multiple organ damage. The patient was admitted to Wuhan Iron and Steel General Hospital on January 16, 2020 for 6 days due to intermittent cough, headache, fatigue and fever. Chest CT on January 16 showed bilateral pneumonia, fibrosis of the left upper lung, and nodules of the left upper lung. Dyspnea occurred on January 17 and blood gas analysis revealed type 1 respiratory failure. Symptoms such as oxygen inhalation, anti-infection, anti-virus, and sputum treatment were given. At 10:10 on January 20, the patient suddenly reduced the finger pulse oxygen to 40%. He had been given non-invasive ventilator-assisted ventilation. The patient was again informed of severe respiratory failure, and asked again whether to undergo tracheal intubation. . At 10:35 on January 20, the condition deteriorated and the rescue died.
Wang XX, male, 75 years old, was admitted to Wuhan Fifth Hospital at 17:19 on January 11, 2020 due to fever with cough, sputum for 5 days, and vomiting for 2 days. Previous history of hypertension and hip arthroplasty. The admission temperature was 38.2 ° C, accompanied by fatigue, anorexia, cough, nasal congestion, dizziness, and headache. There was no obvious chills, chills, and sore muscles and joints. A CT of the chest revealed an interstitial lung infection. After being admitted to the hospital, she was in critical condition and was given oxygen, anti-infection, anti-virus, phlegm, fever, and fluid rehydration as appropriate. The patient's condition worsened progressively, and she was transferred to the ICU on January 15 for mechanical ventilation. At 11:30 on January 20, the family members expressed their understanding of the condition and are now required to stop the ventilator and pull out the tracheal tube for observation. The tracheal intubation ventilator assisted breathing and CPR rescue are no longer required. He was pronounced dead at 11:25 on January 20.
Yin XX, female, 48 years old, had previous diabetes and cerebral infarction. On December 10, 2019, there was no cause of fever (38 ° C), sore body and fatigue, and cough and sputum gradually appeared. Anti-infective treatment in primary hospitals did not improve for 2 weeks. On December 27th, chest tightness and shortness of breath occurred. After the activity, it was obvious. Tongji Hospital was given non-invasive ventilation and conventional anti-infective treatment. The condition still worsened. On December 31st, she was transferred to Jinyintan Hospital and given symptomatic treatments such as high-flow oxygen inhalation of nasal catheter. Hypoxia condition has not improved significantly, and the condition is still worsening. On January 14, 2020, chest CT showed diffuse mechanized changes in both lungs, some with traction bronchiectasis, especially in the lower lungs. At 11:50 on January 20th, tracheal intubation was performed, and analgesia and sedation were given. The terminal oxygen saturation and blood pressure continued to decline, and then the heart rate decreased. Eventually, the rescue failed.
Liu XX, male, 82 years old, was admitted to Wuhan Fifth Hospital at 15:41 on January 14, 2020 due to chills and soreness in the whole body for 5 days. She was given ECG monitoring, non-invasive ventilator assisted breathing, anti-infection, anti-virus and symptomatic treatment. On January 19, he had unclear speech, and his left limb was weak. Considering a stroke, the disease progressed, and respiratory failure continued to worsen. At 00:30 on January 21, the patient's sudden heart rate decreased progressively, the heart sounds were not heard, the aortic pulse disappeared, and he was rescued immediately. The family members still refused mechanical ventilation of the intubation and continued rescue. The heart rate remained unrecovered. The clinic was announced at 1:18 death.
Luo XX, male, 66 years old, no inducement cough on December 22, 2019, mainly dry cough, no fever; December 31, chest tightness, shortness of breath, obvious after the activity, went to the central hospital for treatment; 2020 He was transferred to Jinyintan Hospital on May 2nd, and his imaging findings showed diffuse lung lesions with "white lung-like" changes. After admission, symptomatic treatment such as nasal high-flow oxygen was given. Refractory hypoxemia is difficult to correct. At 10:00 on January 12, the tracheal intubation ventilator assisted breathing, sedation, body temperature of 36.7 ° C, respiratory distress, and continued active antibacterial treatment. On the day, the oxygenation of the patient did not improve significantly. The inspiratory oxygen concentration of the ventilator had been reduced to about 50%, and the partial pressure of arterial oxygen was 80mmHg. The patient had a long course of disease, extremely poor immune function, and there was a risk of septic shock. At 9:50 on January 21, the rescue failed.
Zhang XX, male, 81 years old, was admitted to Wuhan First Hospital on January 18, 2020 due to fever for 3 days. Admission to the chest CT showed infectious lesions in both lungs. Considering viral pneumonia, the patient's renal function and pulmonary infection continued to worsen. On the morning of January 22, 2020, consciousness gradually appeared, and the respiratory heart rate and blood pressure continued to decline. He refused rescue measures such as chest compressions and tracheotomy. The patient stopped breathing at 10:56 on January 22 and declared clinical death.
Zhang XX, female, 82 years old, has a history of Parkinson's disease for 5 years, orally takes Medopa. Onset on January 3, 2020, he was diagnosed with "viral pneumonia and respiratory failure" on January 6 at the Integrated Traditional Chinese and Western Medicine Hospital of Hubei Province due to "fever, cough, chest tightness and fatigue". He was transferred to Wuhan Jinyintan Hospital on January 20, and his condition was progressively worsened. On January 22, he was treated with tracheal intubation ventilator to support treatment, and his respiratory failure did not improve. On January 22, 2020, he was declared invalid by rescue at 18:00. .
week XX, male, 65 years old, January 11, 2020 due to shortness of breath accompanied by fatigue for 3 days, increased 3 days into Wuhan First Hospital. At the time of admission, the patient had difficulty breathing, chest tightness, shortness of breath, and acute illness. He was diagnosed with severe pneumonia, acute respiratory failure, and liver damage. At 19:00 on January 21, a decrease in heart rate and blood pressure, disappearance of light reflection by both pupils, and immediate treatment of tracheal intubation, artificial chest compressions, cardiac strengthening and other treatments. At 19:54, the autonomic rhythm was not restored, and clinical death was declared.
Hu XX, female, 80 years old, became ill on January 11, 2020. He was admitted to China Resources Wuhan Iron & Steel General Hospital on January 18, 2020 due to fever, cough, wheezing, and dyspnea. He was transferred to Wuhan Jinyintan Hospital on January 20, 2020 because of a new coronavirus positive. He has a history of hypertension for more than 20 years, a history of diabetes for more than 20 years, and a history of Parkinson's disease. After admission, she was in critical condition, intensive care, anti-infection, ventilator-assisted breathing, and symptomatic supportive treatment. However, the patient's condition did not improve, persistent hypoxemia, unconsciousness, mechanical ventilator-assisted breathing, invalidated after rescue at 16:00 on January 22, 2020, and clinical death was declared.
Lei XX, male, 53 years old. He had been treated in a community hospital for fever in early January, but it was not effective after a few days of treatment, and fever, cough, and chest tightness worsened. On January 13, 2020, he went to the emergency department of Tongji Hospital. CT showed bilateral lung infection and respiratory failure. He was critically ill on January 18 and was treated with non-invasive ventilator support. On January 20, 2020, he was transferred to Wuhan Jinyintan Hospital for isolation and treatment. . He was admitted to hospital with anti-infection and anti-shock, ventilator-assisted respiratory support treatment, and the patient's condition did not improve. Respiratory failure continued to worsen. At 4 o'clock on January 21, the rescue was invalid, and clinical death was declared.
Wang XX, male, 86 years old, was admitted to Xinhua Hospital on January 9, 2020 due to fatigue for one week. No fever, diabetic hypertension, and colon cancer 4 years after surgery. After admission, CT of the lungs showed multiple ground glass shadows in both lungs, obvious hypoxia, difficulty in eating, rapid breathing, and lethargy. The family refused to be intubated and only inhaled oxygen through the nose. At 17:50 on January 21, 2020, the heartbeat stopped breathing and declared clinical death.
Yuan XX, female, 70 years old. On January 13, 2020, the city's No. 1 Hospital was owing to the continued high fever. At the time of admission, he had blurred consciousness, acute illness, weakened heart sounds, and thick breathing sounds in both lungs. Imaging results showed severe pulmonary infection. Consider severe pneumonia with severe respiratory failure. That is, symptomatic treatment such as active anti-infection and oxygen inhalation is given, but respiratory failure is difficult to correct. The patient was pronounced dead on January 21, 2020 due to respiratory failure.
Zhan XX, male, 84 years old. The patient was admitted to the Fifth Hospital of the City for 3 days due to fever, cough and wheezing at 17: 4 on January 9, 2020. Previous history of chronic bronchitis, unstable angina pectoris, coronary stenting, hypertension, gastrointestinal bleeding, renal insufficiency, hyperlipidemia, hyperuricemia, lacunar cerebral infarction. Due to the exacerbation of the disease and persistent high fever, the patient was transferred to the ICU on January 18th for anti-infection and symptomatic supportive treatment. At 10:16 on January 22, the patient stopped breathing, his heart rate gradually slowed down, and clinical death was announced at 10:52.
Source: http://www.nhc.gov.cn/yjb/s3578/2020...ed2e3c8a.shtml
2 notes
·
View notes
Text
Managing emergencies in general practice
New Post has been published on https://petnews2day.com/pet-industry-news/pet-travel-news/managing-emergencies-in-general-practice/
Managing emergencies in general practice
With the current workforce shortages, general practices are seeing more emergent cases and often have fewer options for transfer. While general practices are not stocked with the wide range of medications and diagnostics that emergency and specialty hospitals have, there are still many basic stabilization measures that can be taken in a general practice setting.
Just as veterinarians develop a systematic approach to the physical examination to ensure nothing is missed, we can develop a similar systematic approach to managing emergency presentations. Improving comfort with initial assessment and treatment of emergency cases can help to improve patient outcomes.
Triage
All team members should feel comfortable with patient triage. First, assess the ABCs:
Airway – Is there an open airway?
Breathing – What is the respiratory rate, effort, and pattern?
Circulation – What is the heart rate and rhythm, pulse quality, capillary refill time, and blood pressure?
Any abnormalities in these systems should prompt action to initiate stabilization measures. Patients with concerning vital signs or who present in distress should be brought to the immediate attention of a veterinarian. Staff members should be familiar with normal vital signs and know that critical cats tend to be bradycardic and hypothermic. When in doubt, staff members should alert a doctor as it is better to overreact to a stable patient than underreact to an unstable patient.
Additional key areas to evaluate include neurologic status, palpation of the urinary bladder (especially in ADR cats), body temperature, and pain levels. A PCV, TS, blood glucose, and azo stick (if available) can provide helpful information from a small amount of blood. A full examination should be performed following stabilization of essential systems.
Initial Stabilization
Veterinarians can work with the team to direct stabilization of the patient while a nurse or assistant obtains a full patient history. Initial stabilization efforts will depend on which systems are affected and may include oxygen therapy, intravenous fluid boluses, sedation, warming or cooling measures, administration of anticonvulsants, dextrose administration, control of active hemorrhage, and pain control.
If a patient presents with an occluded airway—which is uncommon in veterinary patients—establishing an open airway should be top priority. The external extraction technique (XXT), which is used to dislodge a ball or round object from the throat of an unconscious dog with a fully occluded airway, is helpful.
For patients presenting in respiratory distress, oxygen and sedation are typically the first-line stabilization measures. Handling and stress should be minimized for these patients. Many medications can be given IM until intravenous access can be obtained. Do not rush these patients into radiology to obtain a diagnosis. No patient should die in radiology!
Instead, look and listen to how the patient is breathing to direct therapy. For example, with a dog presenting with a heart murmur and crackles, the top differential would be heart failure and furosemide should be administered. For patients presenting with decreased or dull breath sounds and/or a paradoxical breathing pattern, pleural space disease should be suspected and thoracocentesis performed. Although this procedure can be intimidating, it is more likely that a patient will die from untreated pleural space disease than a negative thoracocentesis.
Cardiovascular stabilization begins with gaining intravenous access and providing fluid support. Fluid boluses should be given in small aliquots of isotonic crystalloids. Administration of smaller boluses followed by reassessment is now recommended. Generally, 10-20 mL/kg in cats and 20-30 mL/kg in dogs is a good starting place. It is important to have a resuscitation endpoint, which is a target heart rate, blood pressure, pulse quality and/or mentation. After the initial bolus, reassess parameters and repeat boluses until you reach the target endpoint. In trauma cases, where there is potential for internal hemorrhage, consider hypotensive resuscitation, which is a target systolic blood pressure of 90 mmHg.
Pain control is often needed but should be withheld until full neurologic assessment can be performed. NSAIDs should be avoided in patients with trauma and cardiovascular compromise because of potential for poor perfusion to the kidneys and GI tract. In an emergency clinic with a wide range of available medications, short-acting, full-mu opioids are preferred as they provide excellent pain control, doses can be titrated easily, and they can be withdrawn quickly to allow for reassessment of neurologic status as needed. Medications like injectable fentanyl are not often carried in general practice, so a full- or partial-mu agonist opioid can be administered. When in doubt about which medication to use, consult with your local emergency clinic prior to transfer.
If you are not able to stabilize a patient with the available equipment and medications in your clinic and the client wants continued care, refer the client when the pet is as stable as possible. Emergency veterinarians are often willing to get on the phone and help walk their general practice partners through stabilization measures for these patients to maximize the change of the patient arriving at their clinic alive.
Client Communication
In an emergency, it is essential to gain a client’s trust quickly so that the team—which includes the veterinarian, nursing staff, and client—can make the best possible decisions for the pet. General practitioners often have an advantage with their existing clientele as they have an established relationship prior to an emergency presentation. Veterinary professionals should be clear and honest with the client about the patient status and what the team is doing to stabilize them early in the conversation. CPR orders should be obtained for all patients to allow quick action in the event the patient arrests.
Clients should be advised of recommended diagnostics and treatment as well as if transfer to an emergency of specialty hospital may be recommended. Planting the idea of transfer in the client’s mind early in the process can help to guide their decision-making. Be clear about the financial investment each step of the way, but always talk care first, money second.
Throughout the patient work-up, keep the client updated on the findings and on the prognosis. Some owners need to hear a poor prognosis multiple times or from multiple people before comprehending the reality of the situation, especially in an emergency.
Diagnostics and Initial Treatment
Once the patient is stable, consider performing some initial diagnostics and treatment prior to transfer. This can help to reduce costs to clients, may provide information that ultimately changes the recommendations for transfer, and clarify prognosis. Initial diagnostics may include bloodwork, radiographs, urinalysis, and collection of effusion samples for further testing. If your clinic does not have in-house laboratory equipment and you are sending the patient to another hospital for continued care, you can consider sending any blood drawn prior to administration of fluids or other medications with the client.
Consider initial treatment when possible, such as fluid therapy for dehydrated or hypovolemic pets and unblocking cats with urinary obstruction. By doing more in the primary care facility, you are helping improve the pet’s stability and comfort, reducing the client’s financial investment, and helping the emergency clinic that will have one less procedure to perform or test to run when the pet arrives.
Finding a balance between providing emergency care without derailing the entire schedule in a general practice setting can be challenging and clear communication with clients coming for regularly scheduled appointments about an ongoing emergency can help to manage expectations and decrease frustration around wait times.
Decision to Transfer
The final step in the process is deciding to transfer the pet for continued care. Ultimately, the decision to transfer belongs to the client. The following questions should be considered prior to transfer:
Will the patient benefit from continued, emergent care?
Can the client afford continued care?
Can the hospital where you intend to transfer the patient handle the case?
The first 2 questions require discussion with the client regarding patient prognosis, recommendations for care, and estimates of cost. Be honest with clients about the prognosis. Most clients would prefer to make the decision to euthanize their pet with their primary veterinarian, where the doctor and team are familiar. Some clients will not be ready to make the decision to euthanize until hearing the information again after arriving at the emergency facility, and this is okay too, as long as you have tried to share the information with them prior to transfer.
The final question requires practitioners to have knowledge of what local emergency and specialty hospitals can manage. For instance, a non-specialty emergency hospital is likely not the best place to transfer a down dog in need of back surgery. Developing a relationship with your local emergency and specialty hospitals can help to guide the decision of which clinic is best for an individual patient. Another consideration is potential for clinics to be at capacity of diverting patients, which has become much more common since the COVID-19 pandemic.
Call ahead to the hospital where you intend to send the pet to make sure that the clinic can take the pet, find out estimated wait times, and a general cost estimate. You can also ask to speak to an emergency doctor regarding what else you can or should do for a patient prior to transfer. Preparing clients for estimates, wait times, and expectations of the emergency visit (ie, will a needed ultrasound be available today or will the patient be hospitalized overnight before further testing?) can help reduce stress on arrival at the emergency clinic.
Before the patient leaves your hospital, provide copies of records and all diagnostic results to the referral hospital, including any medications administered and the time given. Anticipating potential complications that could occur during transport, especially if the owner has a large distance to cover, can be helpful. Consider giving sedation prior to travel if you have not already done so during your stabilization process. If portable oxygen is available, send it with patients in respiratory distress. If patients have been having seizures, a dose of rectal or intranasal diazepam can be sent with the client.
Ultimately, emergency cases can be very rewarding to manage, especially when you and your team are prepared with a plan prior to patient arrival.
Kate Boatright, VMD, a 2013 graduate of the University of Pennsylvania, is a practicing veterinarian and freelance speaker and author in western Pennsylvania. She is passionate about mentorship, education, and addressing common sources of stress for veterinary teams and recent graduates. Outside of clinical practice, Boatright is actively involved in organized veterinary medicine at the local, state, and national levels.
0 notes
Text
friendly PSA for writers: EMT/paramedic edition
they are NOT the same thing
wHAT? i know. i was surprised too. turns out it’s a pretty important distinction though, and you’ll save any emergency first responders from eyeball twitching and possible aneurysms by getting it right in your writing. so here goes:
EMT: stands for Emergency Medical Technician. certification requires about 200 hours of class and a practical and written test. 16 year olds can get certified what they CAN do: perform CPR, give oxygen, manage bleeding, take vitals (heart rate, blood pressure, etc.), splint/wrap/dress injuries, open an airway with a short tube up the nose or a hook-like device that keeps a person’s tongue out of their throat, spray narcan up the nose to treat drug overdoses, deliver babies (rare but awesome) what they can NOT do: anything “invasive.” this basically means that they can’t break the skin of a patient. so no injections, no IVs, no intubation, etc. administering Epi Pens is the exception
paramedic: certification requires two years of school, a whole lot of tests, and a lot of on the job training what they CAN do: everything an EMT can, plus everything they can’t. paramedics are the ones who can give people drugs, do invasive procedures like sticking a needle in someone’s chest to reinflate a collapsed lung or performing a tracheotomy, put in IVs, intubate, monitor cardiac patterns, plus a whole bunch of other stuff what they canNOT do: formally diagnose patients, prescribe drugs, sedate people without their consent if they’re mentally competent (saw that in a book once and almost hit the ceiling)
so who shows up on an ambulance when you call for one? it depends. some ambulances are staffed by EMTs, who call for paramedics when they get a case that requires more advanced treatment. sometimes ambulances are already staffed by paramedics. sometimes you get one of each.
i’m sure there’s stuff i’m leaving out, but this is the general idea.
so save a first responder: don’t use EMT and paramedic interchangeably
#writing#writing advice#paramedics#emt#so many fics and even published books have made me wince because of this#but i get that a lot of people don't know about it#also i'm procrastinating studying for finals#mine
1K notes
·
View notes
Text
Reviewing questions:
ARDS is basically caused by anything that leads to inflammation in the alveoli (pancreatitis, trauma, near drowning). There are three phases of ARDS: exudative (week 1), proliferative (week 2), and fibrotic (week 3). In the exudative phase, you get exudate in the alveoli. You get macrophages and necrotic cells in the alveoli and the formation of hyaline membranes (the cellular debris becomes organized to form hyaline membranes). In the proliferatie phase, you get proliferation of fibroblasts and interstitial inflammation as the cells try to repair the damage. In the fibrotic phase, which doesn't always occur, the whole alveolus is surrounded by fibrotic tissue; it's pulmonary fibrosis. Sepsis can cause injury to the pulmonary endothelium or epithelium, which can lead to ARDS. CXR will show white out that can't be explained by cardiac causes and the pt will be hypoxemic.
Even if you survive ARDS, you can have an increased A-a gradient that lasts for a while or even forever (it would be forever if you ended up with pulmonary fibrosis as a result of the ARDS).
As you age, you lose compliance of the chest wall and elastic recoil of the alveoli. You lose elastin in the alveoli, so they can't snap back as well, thus you have increased residual volume and decreased FVC.
In chronic bronchitis, the mucus glands in the bronchial wall submucosa increase in size, causing increased bronchial wall thickness. The Reid Index indicates the severity of chronic bronchitis. It's the thickness of the submucosal mucous glands/thickness of the bronchial wall from the basement membrane of the epithelium to the cartilage. The normal Reid Index is 0.4; anything higher than that is more severe chronic bronchitis.
Small Cell Lung Cancer is a neuroendocrine tumor (so it will stain positive for chromagranin, synaptophysin, and CD56 [neural cell adhesion molecule, or NCAM], neuron-specific enolase), associated with smoking; the tumor is centrally located. Histologically, it shows small round cells with little cytoplasm and hyperchromic nuclei with lots of divisions. It has 3 paraneoplastic syndromes (Cushing's syndrome, Lambert-Eaton Syndrome, and SIADH). For some reason, SCLC is also called oat cell carcinoma.
In pts on treatment for asthma who still have exacerbations despite being on an PRN SABA (albuterol), ICS (e.g., mometasone), and LABA (e.g., formoterol), if the pt has high IgE levels, he can try omalizumab, which binds IgE so it can't cause mast cell crosslinking and degranulation of leukotrienes and histamine. Omalizumab is an anti-IgE antibody.
Type II pneumocytes make surfactant, which is transported in lamellar bodies to the cell surface of pneumocytes. I don't recall learning about lamellar bodies, but I knew that type II pneumocytes make surfactant and regenerate type I pneumocytes. Type I pneumocytes do gas exchange.
Secondary polycythemia (increased hematocrit) occurs as a response of the kidneys to chronic hypoxemia. Hypoxemia-> hypoxia in the tissues-> cells in the cortex and medulla of the kidneys release erythropoietin to stimulate RBC production so there will be more RBCs to carry more O2. Secondary polycythemia can occur in pts with COPD or other conditions that cause chronic hypoxemia. So if you have a pt with OHS, he can have higher than normal Hct as a result of the chronic hypoxemia. Oxygen saturation less than 92% is hypoxemia.
Neutrophils and macrophages can make elastase, which degrades the elastin in the alveoli. Other proteinases besides elastase are cathepsin G, and Matrx Metalloproteinase (MMP). Anti-proteases counteract the proteases. Alpha-1 antitrypsin stops neutrophil elastase from breaking down elastin in alveoli. Other antiproteases are alpha-2 macroglobulin and Tissue Inhibitors of Metalloproteinases (TIMPs).
Elastase is a neutral protease found in alveolar fluid. Neutrophil elastase is inhibited by alpha-1 antitrypsin. Macrophage elastase is inhibited by TIMPs.
Atopic asthma presents with eosinophils and Charcot-Leyden crystals in the sputum. I remembered the crystals from a pulm lecture given by one of the fellows a few weeks ago, so I got the question on it right. T helper 2 cells release IL-5, which summons eosinophils. Charcot-Leyden crystals are bunches of eosinophil membrane protein seen in atopic (extrinsic) asthma. TH2 cells also release IL-4, which causes B cells to make IgE.
Ketamine (NMDA antagonist) can be used to induce anesthesia in pts who are hemodynamically unstable or who have bronchospasm and need to be intubated. Ketamine causes increased catecholamine release, which can increase blood pressure. This is desirable in a pt who has low BP and needs to be intubated. Ketamine's sympathomimetic effects lead to increased HR, contractility, bronchodilation, and cerebral blood flow. You wouldn't use propofol in a hypotensive pt, as that would cause even lower BP. Ketamine is also analgesic.
Etomidate is a GABA receptor agonist. It does not affect BP, cardiac output, or HR, so it's hemodynamically neutral. It decreases cortisol synthesis. Well that's interesting, because isn't cortisol also involved in blood pressure? I guess cortisol would take longer to start impacting blood pressure control, so that's why it doesn't affect BP when used for induction. But I guess it causes adrenocortical suppression over time. So it wouldn't be used in pts with sepsis.
Propofol is a GABA agonist; good for longer sedation; but decreases BP due to vasodilation.
OSA can lead to pulmonary HTN and right heart failure because of the hypoxic vasoconstriction that occurs in response to hypoventilation. The hypoxemia in these pts also causes systemic HTN and sympathetic stimulation of the heart. Chronic sleep apnea that goes untreated can lead to arrythmias, CAD, and sudden cardiac death!
In cystic fibrosis, there are no, or few properly functioning CFTR channels, so you can't get Cl- out of the respiratory epithelial cells. As a result, there is increased movement of Na+ into respiratory epithelial cells and water follows the Na+. This is why respiratory secretions are thickened in CF.
The pathophysiology of CF was not explained well to us when we learned this in school! What happens in the sweat ducts is different from what happens in the respiratory epithelium in CF. In the normal respiratory epithelium, CFTR channels inhibit the ENac channels through which Na+ is reabsorbed. This allows more Na+ and H20 to stay in the mucus so that the mucus can stay watery and be easily coughed up. In CF, you have no or few properly functioning CFTR channels. Therefore, chloride can't move out of respiratory epithelial cells, so you can't inhibit Na+ reabsorption by the epithelial cells. Thus excess Na+ is reabsorbed and excess water follows the Na+, leading to dry respiratory secretions. In the sweat ducts of normal people, the opposite occurs--CFTR channels cause increased absorption of Na+ via ENac channels. In CF, there are no/few functioning CFTR channels, so you can't reabsorb Na+, thus the sweat has increased NaCl-> salty sweat.
The CFTR channel is an ATP-gated channel. It opens when ATP binds to it. In CF, the CFTR channel can't bind ATP, so the channel won't open and chloride ions in the respiratory epithelium can't leave cells.
Pts can have increased sweat chloride levels or normal sweat chloride levels (normal if the CFTR mutation is mild). If sweat chloride is normal, you can make the diagnosis of CF by measuring the nasal transepithelial potential difference with the nasal transepithelial potential difference test. In this test, NaCl solution is applied to the nasal mucosa. If the pt has CF, the pt's respiratory epithelial cells can absorb the Na+, but not the Cl- in the applied solution, so the transepithelial voltage difference is more negative because negatively charged chloride ions can't be absorbed by the respiratory epithelial cells.
In the sweat ducts of normal pts, CFTR channels reabsorb Cl- and that causes reabsorption of Na+. In pts with CF, mutated CFTR means no reabsoption of NaCl, so the sweat is salty.
Ok, I was confused about what actually happens with the CFTR and the Na+ and Cl-. CF causes decreased ability to reabsorb Na+ and Cl- from the sweat, hence salty sweat in CF pts. But in the respiratory epithelium, the inability to get Cl- out of the cells causes increase Na+ reabsorption into cells-> water reabsorbed into cells-> dry respiratory secretions.
#ARDS#hyaline membrane#chronic bronchitis#Reid Index#NCAM#omalizumab#ketamine#propofol#etomidate#anesthesia#cystic fibrosis#TIMPs#TIMP#MMP
2 notes
·
View notes
Text
Adverse effects of smoking | Smotect
Cigarette smoking is the biggest preventable gamble factor for dreariness and mortality in created nations. Sensational changes in the predominance of cigarette smoking in the last part of this century (i.e., a decrease among men and an increment among ladies) have diminished flow smoking levels to around one-fourth of the grown-up populace and have diminished contrasts in smoking pervasiveness and smoking-inferable infections between the genders. Every day smokers smoke cigarettes to keep up with nicotine levels in the mind, basically to stay away from the adverse consequences of nicotine withdrawal, yet in addition to adjusting temperament. Normal smokers display higher and lower levels of pressure and excitement, individually than nonsmokers, as well as higher impulsivity and neuroticism quality qualities.
Smokers of cigarettes increment smoking power, smoking rate, or inward breath to keep up with levels of nicotine, as estimated by plasma levels of nicotine in both not obligatory and research facility smoking settings ( 43–46 ). Estimated nicotine levels in the blood vessel and venous flow show that singular smokers can acquire plasma nicotine levels of 20–50 ng/mL ( 46–48 ). Smokers experience excitement and sedation at the same time from every cigarette; be that as it may, they likewise experience lower harmony levels of excitement and higher balance levels of pressure than nonsmokers. Subsequent to smoking discontinuance, mean excitement and feelings of anxiety are expanded and decreased, individually, recommending that smoking cigarettes might add to the expanded pressure saw in smokers.
Explicit smoking-related issues that need treatment include:
Diminished HDL (great) cholesterol and expanded circulatory strain (expanding takes a chance for coronary failure and stroke). Erectile brokenness. Lower oxygen to the heart and different tissues in the body (expanding gambles for coronary corridor sickness, fringe course infection, and diabetes). More regular routine diseases like colds, particularly in kids living with smokers. More unfortunate lung work (capacity to get sufficient oxygen) prompting COPD, asthma, bronchitis, or emphysema.
To know more about smoking side effects and prevention visit : https://smotect.com/
0 notes