#ARDS
Explore tagged Tumblr posts
Text
🤣🤣🤣🤣🤣

#royalty is not celebrity#merch your royalty#just call me harry#using your office for personal gain#can't buy credibility#lies and the lying liars who tell them#unsussexful#grifters gonna grift#surrogacy isn't a crime but lying is#irs audit Archewell#ards#acute relevance deficiency syndrome
47 notes
·
View notes
Note
Inspector, you're so good at drawing!! Is it something you do often?
oi, fanks ards! nah, but sumtimes i drew stuff fer the younger kids back in the east end, to cheer em up an wotnot.
@dearestwoods got me these crayons fer christmas, so ive tried em out, an ive been watchin 'im paint a bit too. but im jus 'avin sum fun wivvit, aint nuffin more to it.
2 notes
·
View notes
Text
Bangor Swim Festival
After a couple of weeks of racing for the older #teamlarne athletes, attention turned to some of the you get members of our team. A group of 10 travelled to Ards to take part in the 2024 Bangor Swim Festival. A level 1 meet this gave an opportunity for these young swimmers to race over all 4 strokes and on IM (some for the 1st time. Across 43 swims #teamlarne produced 23 personal vest times…
0 notes
Text

Signs and Symptoms of Bronchitis
Chronic Cough: Lasts for at least three months a year for two consecutive years. Excessive Mucus Production: Ongoing production of mucus. Wheezing: Whistling sound when breathing. Shortness of Breath: More noticeable during physical activity. Frequent Respiratory Infections: Increased susceptibility to colds and flu.
DR. K. RAVI VISAKHAPATNAM CONTACT :9390398062
#pulmonologist#treatment#ravichestclinic#clinic#diabetologist#vizag#medicalcare#dizirina#somanthmedicals#tuni#yendada#viproad#poornamarket#jagadhmba#ferryroad#gopalapatnam#vizianagram#anakapalli#chest#heart#panic#attack#ards#breathing#lungdisease#asthmaattack#exercise#asthma#breath#bronchitis
0 notes
Text
Respiratory Distress Syndrome: Top 10 Signs and Recovery Strategies
Experiencing sudden breathing problems, persistent cough, or chest tightness? These could be signs of Acute Respiratory Distress Syndrome (ARDS), a serious lung condition. This audio highlights key symptoms, causes, and recovery strategies for managing ARDS effectively.
0 notes
Text
Innovative Use of ECMO in a COVID-19 Patient with Acute Respiratory Distress Syndrome
Extracorporeal membrane oxygenation (ECMO) has emerged as a critical intervention for patients with severe respiratory failure, including those suffering from acute respiratory distress syndrome (ARDS) due to COVID-19. The innovative use of ECMO in such patients can be a lifesaving measure when conventional ventilation strategies fail. Here's an in-depth look at this approach:
ECMO Overview
ECMO is an advanced life support technique that provides prolonged cardiac and respiratory support by removing blood from the patient's body, oxygenating it outside the body, and then returning it to the patient. There are two main types of ECMO:
Veno-venous (VV) ECMO: Primarily used for severe respiratory failure where the heart is still functioning adequately.
Veno-arterial (VA) ECMO: Used for both cardiac and respiratory failure.
COVID-19 and ARDS
ARDS is a severe lung condition characterized by rapid onset of widespread inflammation in the lungs, leading to respiratory failure. COVID-19 can trigger ARDS, causing critical illness in affected patients. Despite optimal mechanical ventilation and medical therapy, some patients may not improve, necessitating the use of ECMO.
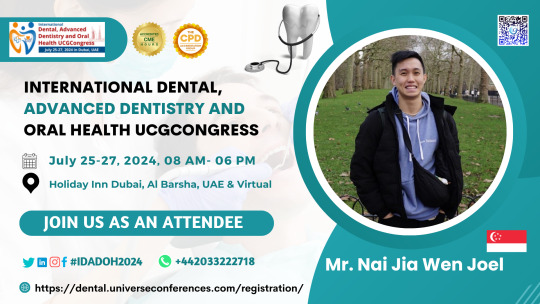
Register here: https://dental.universeconferences.com/registration/

Innovative Uses of ECMO in COVID-19 ARDS
Early Implementation: In some cases, early use of ECMO in COVID-19 ARDS patients has shown better outcomes compared to delayed use. Initiating ECMO before the patient’s condition deteriorates severely may prevent further complications.
Prolonged ECMO Support: COVID-19 patients often require longer durations of ECMO support compared to other causes of ARDS. Innovations in ECMO management, such as improved anticoagulation protocols and better infection control measures, have allowed for safer prolonged use.
Mobile ECMO Units: To expand access, mobile ECMO units have been developed, allowing ECMO initiation in hospitals without ECMO capabilities, followed by transfer to specialized centers.
Personalized Ventilation Strategies: During ECMO, lung-protective ventilation strategies are employed to minimize further lung injury. Tailoring these strategies to the individual patient’s needs has been crucial in improving outcomes.
Integration with Other Therapies: Combining ECMO with other treatments such as prone positioning, advanced ventilator strategies, and novel pharmacotherapies (like antiviral drugs and immunomodulators) has been explored to enhance patient recovery.
Register here: https://dental.universeconferences.com/registration/
Case Report Example
Patient Profile: A 45-year-old male with no significant past medical history presents with severe COVID-19 pneumonia progressing to ARDS. Despite maximal conventional ventilation and prone positioning, the patient’s oxygenation status continues to deteriorate.
ECMO Intervention:
Indication: Persistent severe hypoxemia (PaO2/FiO2 ratio < 80 mmHg) despite optimal ventilatory support.
ECMO Type: VV ECMO initiated to provide respiratory support.
Management: Anticoagulation managed with heparin to maintain an activated clotting time of 180-220 seconds. Regular monitoring for potential complications such as bleeding, thrombosis, and infection.
Ventilation Strategy: Ultra-low tidal volume ventilation (<4 ml/kg predicted body weight) with driving pressures kept below 15 cm H2O.
Outcome: After 25 days on ECMO, the patient showed significant improvement in lung function. ECMO was successfully weaned, and the patient was extubated shortly thereafter. Full recovery was achieved over the next few weeks with continued respiratory therapy.
Register here: https://dental.universeconferences.com/registration/

Conclusion
The innovative use of ECMO in COVID-19 patients with ARDS has shown promising results, especially when integrated with comprehensive critical care strategies. Early initiation, personalized treatment plans, and multidisciplinary approaches are key to improving outcomes in this critically ill population.
Important Information: Conference Name: International Dental, Advanced Dentistry and Oral Health UCGCongress Short Name: IDADOH2024 Dates: July 25-27, 2024 Venue: Dubai, UAE Email: [email protected] Visit: https://dental.universeconferences.com/ Call for Papers: https://dental.universeconferences.com/submit-abstract/ Register here: https://dental.universeconferences.com/registration/ Call Us/What Sapp Us: +12073070027 / +442033222718
#ECMO#COVID19#ARDS#CriticalCare#RespiratoryFailure#InnovativeTreatment#IntensiveCare#MechanicalVentilation#LifeSupport#MedicalInnovation#PatientRecovery#Healthcare
0 notes
Text




“Loch Ard” 🦢🍂 by | Daniel Casson
Loch Ard, the Trossachs National Park, Scotland
#loch ard#landscape#nature#autumn#landscape photography#lake#forest#fall#swan#animals#scotland#curators on tumblr#uploads
3K notes
·
View notes
Text
Going through questions:
Both polymyalgia rheumatica (PMR) and giant cell arteritis (also known as temporal arteritis) are chronic inflammatory diseases. PMR is a common chronic inflammatory condition in adults >age 50, although prevalence varies among different countries and populations. Approximately 1 in 5 patients with PMR will have or develop giant cell arteritis, while approximately 50% of patients with giant cell arteritis have or have had PMR.
Giant cell arteritis can affect any medium or large artery, particularly the extracranial carotid branches. The temporal artery is often involved, and the ophthalmic artery may also be affected. This can result in neuro-ophthalmic complications, including permanent blindness. For this reason giant cell arteritis with ophthalmic symptoms is considered a medical emergency. Patients with PMR should be evaluated for symptoms of giant cell arteritis, such as visual changes, new-onset headaches, jaw claudication, or scalp tenderness. Giant cell arteritis is confirmed with a temporal artery biopsy, while PMR is diagnosed using a scoring system of signs and symptoms. The treatment of choice for both conditions is high-dose oral prednisone, tapered over months to years as symptoms abate.
Antineutrophil cytoplasmic antibody–associated vasculitis, polyarteritis nodosa, Takayasu arteritis, and granulomatosis with polyangiitis (formerly called Wegener’s granulomatosis) are not uniquely associated with PMR.
The goal fasting blood glucose level in patients with gestational diabetes is <95 mg/dL. A fasting glucose level <80 mg/dL is associated with increased maternal and fetal complications. The goal 2-hour postprandial glucose level is <120 mg/dL and the goal 1-hour postprandial glucose level is <140 mg/dL.
Chest radiographic findings in acute respiratory distress syndrome (ARDS) include bilateral airspace opacities but not a localized infiltrate as with pneumonia or a flattened diaphragm as with COPD. Clinically, ARDS will often present similarly to pneumonia or heart failure with dyspnea, hypoxemia, and tachypnea. However, ARDS typically does not respond to supplemental oxygen or diuretic therapy. Patients may decompensate quickly and require mechanical ventilation. The Berlin classification required mechanical ventilatory support in the definition of ARDS, but the COVID-19 pandemic has demonstrated that some patients with mild ARDS can be treated with noninvasive respiratory support.
1 note
·
View note
Text
The hope is that a drop of solution containing these nanocarriers, delivered to the lungs via the nose, could treat acute respiratory distress syndrome (ARDS), one of the most frequent causes of respiratory failure that leads to putting patients on a ventilator. In ARDS, inflammation spiraling out of control in the lungs so seriously burdens the immune system that immune cells are unable to tend to the initial cause of the damage.
0 notes
Text
Acute respiratory distress syndrome

Overview
Acute respiratory distress syndrome (ARDS) is a severe medical condition characterized by fluid buildup in the lungs that leads to difficulty breathing and reduced oxygen levels in the blood. ARDS typically occurs as a complication of another underlying medical condition, such as pneumonia, sepsis, or trauma. The exact cause of ARDS is not fully understood, but it is thought to involve an excessive inflammatory response in the lungs triggered by an injury or infection. This inflammation can cause damage to the alveoli, which are tiny air sacs in the lungs responsible for exchanging oxygen and carbon dioxide between the lungs and bloodstream. Symptoms of ARDS can include rapid breathing, shortness of breath, low blood oxygen levels, chest pain, cough, and fatigue. Treatment typically involves addressing the underlying cause of the condition, as well as providing supportive care to maintain adequate oxygen levels and prevent complications. This may include mechanical ventilation, supplemental oxygen therapy, and medications to reduce inflammation or prevent infection. ARDS is a serious condition that can be life-threatening, especially if left untreated. However, with prompt and appropriate treatment, many patients with ARDS are able to recover fully or improve significantly over time.
Symptoms
The symptoms of acute respiratory distress syndrome (ARDS) typically develop rapidly and can include: - Shortness of breath: This is often the earliest symptom of ARDS, and it can quickly progress to become severe. - Rapid breathing: Patients with ARDS often experience rapid breathing, also known as tachypnea. This is the body's natural response to low oxygen levels. - Low blood oxygen levels: A hallmark of ARDS is a drop in the level of oxygen in the bloodstream, which can lead to oxygen deprivation in the body's organs and tissues. - Chest pain: Patients with ARDS may experience chest pain or discomfort, especially during deep breathing or coughing. - Cough: A persistent cough is common in patients with ARDS, although it may not always be present. - Fatigue: ARDS can cause a general feeling of fatigue and weakness, which can be exacerbated by the difficulty breathing. If you experience any of these symptoms, it is important to seek medical attention immediately, as ARDS can be life-threatening if left untreated.
When to see a doctor
If you experience any symptoms of acute respiratory distress syndrome (ARDS), it is important to seek medical attention right away. ARDS is a serious condition that can be life-threatening if left untreated, and early diagnosis and treatment are critical for the best possible outcome. In particular, seek emergency medical care if you experience: - Severe shortness of breath that interferes with your ability to speak or move - Rapid, shallow breathing - Bluish tint to the lips or face - Confusion or altered mental state - Chest pain or tightness - Rapid heart rate If you have been diagnosed with an underlying condition that increases your risk of developing ARDS, such as pneumonia, sepsis, or trauma, it is important to monitor your symptoms closely and seek medical attention if they worsen or if you develop new symptoms.
Causes
Acute respiratory distress syndrome (ARDS) is typically caused by an injury or inflammation in the lungs that leads to fluid accumulation and reduced oxygen levels in the bloodstream. The most common underlying causes of ARDS include: - Pneumonia: This is the most common cause of ARDS, especially in people who are hospitalized. - Sepsis: Sepsis is a serious bloodstream infection that can lead to inflammation throughout the body, including the lungs. - Trauma: Severe injuries, such as those sustained in a car accident or a fall, can damage the lungs and lead to ARDS. - Aspiration: When food, drink, or other substances are inhaled into the lungs, they can cause inflammation and damage that can lead to ARDS. - Inhalation injury: Exposure to smoke, fumes, or other toxic substances can cause damage to the lungs that can lead to ARDS. - Drug overdose: Certain drugs, such as opioids, can depress the respiratory system and lead to ARDS. - Other underlying medical conditions: ARDS can also occur as a complication of other medical conditions, such as pancreatitis, burns, or transfusion reactions. It's important to note that not everyone who experiences these underlying conditions will develop ARDS, and some people may develop ARDS without an obvious underlying cause.
Risk factors
Certain factors may increase a person's risk of developing acute respiratory distress syndrome (ARDS), including: - Age: ARDS can occur at any age, but it is more common in older adults. - Smoking: Smoking can increase the risk of developing lung-related conditions that can lead to ARDS. - Chronic lung disease: People with pre-existing lung conditions, such as chronic obstructive pulmonary disease (COPD), may be more likely to develop ARDS. - Immune system dysfunction: Certain conditions that affect the immune system, such as HIV/AIDS, can increase the risk of developing ARDS. - Alcohol abuse: Excessive alcohol consumption can weaken the immune system and increase the risk of infection, which can lead to ARDS. - Obesity: Obesity can put additional stress on the respiratory system and increase the risk of developing lung-related conditions that can lead to ARDS. - Trauma: Severe injuries, such as those sustained in a car accident or a fall, can increase the risk of developing ARDS. - Certain medical treatments: Certain medical treatments, such as mechanical ventilation, can increase the risk of developing ARDS as a complication. It is important to note that not everyone with these risk factors will develop ARDS, and some people may develop ARDS without any known risk factors.
Complications
Acute respiratory distress syndrome (ARDS) can lead to a number of complications, including: - Multiple organ failure: ARDS can cause low oxygen levels in the bloodstream, which can lead to damage in other organs, such as the kidneys, liver, and brain. - Infections: People with ARDS are at increased risk of developing infections, such as pneumonia, as a result of their weakened immune system. - Blood clots: People with ARDS are at increased risk of developing blood clots, which can lead to complications such as deep vein thrombosis (DVT) or pulmonary embolism (PE). - Collapsed lung: In some cases, ARDS can cause a condition known as pneumothorax, where air leaks into the space between the lung and chest wall, causing the lung to collapse. - Psychological effects: People who have survived ARDS may experience psychological effects, such as post-traumatic stress disorder (PTSD), depression, or anxiety. - Long-term respiratory problems: Some people who have survived ARDS may experience long-term respiratory problems, such as difficulty breathing or reduced lung capacity. It is important to work closely with your healthcare provider to manage any complications that may arise as a result of ARDS. Read the full article
#Acuterespiratorydistresssyndrome#ARDS#care#Causes#dress#full#health#long-term#men#risk#symptoms#Treatment
0 notes
Link
From July 2022
One year post discharge, both pulmonary function tests and echocardiography were normal. However, six patients with persisting dyspnea on exertion showed impaired volitional diaphragm function and control based on ultrasound, magnetic stimulation and balloon catheter-based recordings. Diaphragm dysfunction with impaired voluntary activation can be present 1 year after severe COVID-19 ARDS and may relate to exertional dyspnea.
0 notes
Text

or whatever he said
#it‘s still dark as hell as far as i can see#zappenduster#ard you will pay for your crimes#tatort saarbrücken#spatort#adam schürk#leo hölzer#das ende der nacht#das fleißige lieschen
333 notes
·
View notes
Note
Happy birthday Gina!!! I hope you have a wonderful day!! 😊
fanks ards!!!
2 notes
·
View notes
Photo

As The Bard once said, “To be(ard) or not to be(ard).” The outcome will be decided by your vote.
SHAVE IT.
SAVE IT.
944 notes
·
View notes
Text

Happy Dusserah DR. K. RAVI VISAKHAPATNAM CONTACT :9390398062
#pulmonologist#treatment#ravichestclinic#clinic#diabetologist#vizag#medicalcare#dizirina#somanthmedicals#tuni#yendada#viproad#poornamarket#jagadhmba#ferryroad#gopalapatnam#vizianagram#anakapalli#chest#heart#panic#attack#ards#breathing#lungdisease#asthmaattack#exercise#asthma#breath
0 notes
Text






Ard Skellig
endless Witcher 3 gifs
#witcher#witcher 3#tw3#the witcher 3#witcheredit#the witcher#witchergif#dai's gifs#gamingedit#gamingscenery#thewitcheredit#ard skellig#skellige gif#skellige
271 notes
·
View notes