#and every new scan she has just shows more tumors and more growth and more red flags
Explore tagged Tumblr posts
Text
wanted to write something today (i have an ESSAY DUE TODAY and i have WIPS) but instead im thinking abt my mom. lol
#there was a fucking cyberattack on the hospital that she gets her cancer treatments from and their systems have been down for WEEKS#and she's been delayed in getting treatments because of it and ykw. its advancing at a terrifying rate so its not like she has the time#to just sit around and twiddle her thumbs waiting for the problems to be resolved#and im lowkey !!! fuckin terrified !!!!#like. she has her meds NOW and i think we've fairly moved past it for the most part. but idk.#how much time did that really give her??? another month??? or two?? or three????#she's been a ticking time bomb for 3 years now and i think she's almost out of time#i cant explain how i know. i just do#she's always in pain. i cant be around her because she's constantly in so much pain and i dont know what to do to help#and its just a reminder that she's only getting worse.#and i feel horrible for isolating myself from her because she doesnt have long!!!!!!!!!!!!!!!!!!!! i know im gonna regret it later!!!!#but ive never been good at seeing ppl in pain. or knowing what to do about it.#and every new scan she has just shows more tumors and more growth and more red flags#and idk. im tired.#im tired of being scared. im tired of the fucking sword hanging over our heads. im tired of grieving my mother while she's still alive#and im tired of treating her like a ghost when she ISNT yet but i dont know what else to do because everything fucking hurts.#and all my complicated feelings about my mom aside. all the ways we've hurt each other#and the ways she's made me feel small and unimportant and Different and stupid and crazy and foolish#she's my MOM. she's my mom#and all i can think about with all this is my youngest brother.#he doesnt remember mom when she was healthy. the only mom he knows is exhausted and in pain and dying#and she won't even see him graduate high school and he'll never know what she was like before all of this#i almost wish the cancer would just take her so i could finally be able to grieve and let go#instead of this limbo ive been in for three fucking years of hope and Knowing what will happen and grief and anger#and ngl i feel like a horrible fucking person for that. lol#y'all dont need to read this i just gotta scream for a sec#winter speaks#personal#tw death#tw cancer
5 notes
·
View notes
Text
Could Tattoo Ink Be Used to Detect Cancer?
https://sciencespies.com/nature/could-tattoo-ink-be-used-to-detect-cancer/
Could Tattoo Ink Be Used to Detect Cancer?
When amateur artist Cristina Zavaleta signed up to take an illustration class with Pixar animators on character design, she had no idea she’d also be embarking on a new scientific study. At the time, Zavaleta’s work as a post-doctoral biomedical researcher in a molecular imaging lab at Stanford involved evaluating contrasting agents, like dyes, used to detect tumors in animals. During her art class, the researcher was struck by the intensity of the colors of gouache, vibrant water-based paints, that her fellow illustrators were using. “They were bringing back these pieces that were just incredible, really rich colors. And I thought, how do you even achieve that color, visually,” says Zavaleta.
That simple question ultimately led Zavaleta, now an assistant professor of biomedical engineering at the University of Southern California, and her colleagues to create a first-of-its-kind library detailing the optical imaging properties of commonly used pigments and dyes, found in everything from tattoos to food coloring. The researchers hope their study will open the doors for the novel use of everyday colorants as imaging agents in medical tests, that may be more effective at early detection of several kinds of cancers.
Currently, only three dyes with fluorescent properties used as optical imaging contrast agents—methylene blue, indocyanine green and fluorescein—are approved for human use by the U.S. Food and Drug Administration (FDA). In diagnostic medicine and in some surgical procedures, imaging contrast agents are materials used to improve internal body pictures produced by X-rays, computed tomography (CT) scans, magnetic resonance imaging (MRI), and ultrasounds. These materials can be ingested or injected and temporarily color targeted parts of the body, like specific cells, organs, blood vessels and tissues, to help clinicians see differences and abnormalities that may indicate disease. Yet, Zavaleta wondered about the significant catalogue of approved food, drug and cosmetic dyes that people routinely encounter in their everyday lives. Are there other imaging agents hiding in plain sight?
youtube
“As my art brain was thinking about these paints [from class], I thought to myself, what paints are already being used in humans?” says Zavaleta. “And a lightbulb went off.”
Tattoos. High quality pigments used in tattooing are made from mineral salts and metal chelates, which have been isolated from natural sources and used by humans for thousands of years.
Zavaleta’s next step was to do her homework, as any good researcher would. She contacted Adam Sky, a tattoo artist in the Bay Area whose work she admired. Sky was interested in her research, and gave her samples of some of the inks he was using, which Zavaleta collected in a well plate, a tray with multiple divots, or wells, that can be used as test tubes, she’d brought along, just in case.
“I immediately took them to my microscope over at Stanford, and I did all these different tests on them,” Zavaleta says. “I was amazed at what I was seeing.”
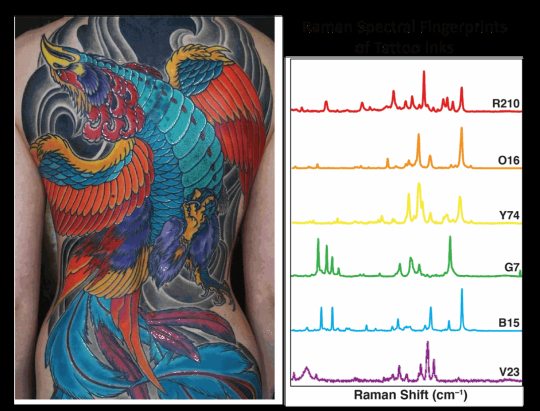
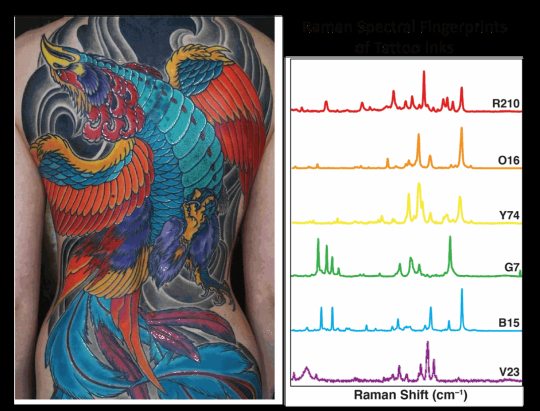
In a tattoo ink color palette, each color carries a unique spectral fingerprint that can be used as an imaging barcode to better identify and detect tumors.
(Tattoo and design created by Adam Sky)
She measured two optical elements of the inks, their fluorescence properties and Raman properties. Fluorescence relates to a dye or pigment’s capacity for absorption and emission of light, while Raman indicates how light scatters. Both are commonly used in imaging techniques in the cancer field. Highly fluorescent agents offer sensitivity in imaging; very small amounts are needed for them to illuminate areas very brightly. Raman imaging, on the other hand, offers specificity by allowing multiplexing, or the ability to look at several processes happening inside the human body at once. These can help show whether cells or tissues are expressing multiple genes, for example, or expressing one more highly that may be associated with a particular cancer, like HER2 and breast cancer or EGFR with lung cancer. Each of the targets has different receptors that will be illuminated by different agents, and depending on their optical properties, some agents will be better than others.
In all, the researchers evaluated the optical properties of 30 approved food, drug and cosmetic coloring dyes and tattoo ink pigments using a spectrophotometer, an instrument that measures the intensity of light after it passes through a sample solution. Seven of the colorants displayed fluorescence properties that were comparable to or exceeded the three FDA-approved clinical dyes. The researchers next measured the Raman signatures, to see how high the colors’ unique signatures of light photon peaks were, with high peaks being indicative of usefulness in terms of multiplexing. Finally, they tested the best-performing dyes and pigments by injecting them as imaging agents in mice with cancerous tumors.

The researchers evaluated the optical properties of 30 approved food, drug and cosmetic coloring dyes and tattoo ink pigments.
(Cristina Zavaleta)
Data from Zavaleta and her colleagues’ study showed that FDA-approved Green 8 dyes used in drugs and cosmetics have significant tumor targeting potential in mice with cervical and colon tumors, and the Orange 16 pigment found in tattoo inks also showed, according to the authors, promising fluorescent properties and tumor targeting potential. This is significant because, as they note in the study, “no single imaging modality currently meets all the clinical needs of high sensitivity, high spatial and temporal resolution, high multiplexing capacity, high depth of penetration, low cost, and high throughput.” In other words, no single imaging agent can provide all the information a doctor might need.
The USC lab where Zavaleta and her colleagues conducted the research uses nano-based imaging contrast agents, or tiny spherical vesicles that are loaded with the dyes or pigments. While nano-based agents are approved for use as a medium in human imaging, they have been controversial in the past because of potential toxicity. Metallic-based nanoparticles like those made from gold and silver have been known to stay inside the body for long periods of time after exposure. This is one of the main reasons the team instead uses liposomal nanoparticles, made up of biodegradable materials with fatty skins similar to human body cells, that are already used in other applications, like drug and nutrient delivery.
“You can think of it as us having all these different batches of nanoparticles, and one has a different tattoo ink [or other dye or pigment] inside of it. And that tattoo ink has a very special barcode that’s associated with it; every ink has a unique fingerprint, yellow different from red, red different from purple,” Zavaleta explains. “So, if we have all these different flavors of nanoparticles that we can now target to different receptors on tumors, we can enhance our ability to distinguish between different [cancers].”
One use for such materials could be gathering real-time information during a test, such as a colonoscopy, where physicians are visually searching for certain kinds of polyps. Enhanced imaging agents have the potential to also reduce the invasiveness of disease detection and diagnosis, such as the number and size of biopsies needed, by providing more information from a smaller sample.
Christian Kurtis, who made the career change from biomedical researcher at the National Institutes of Health to tattoo artist in Rockville, Maryland, spent his post-doctoral period in a cancer research lab at the Uniformed Services University of the Health Sciences. Kurtis says the specificity these kinds of dyes could offer for imaging is key to better treatment.
“The unfortunate problem with malignant [tumors] is that they comprise a [variety] of molecular markers that may not be present on all cell types. The increased metabolic activity of malignancy is the signature most commonly exploited in imaging, and is the reason these liposomal techniques are effective,” says Kurtis. In other words, because cancer cells tend to spread quickly, researchers and physicians are able to track their growth with imaging. Having multiple types of agents that bind to the different markers would be even more helpful. “In my opinion, it will be personalized or individualized medicine that will hold the key to meaningful early diagnosis of disease,” he adds.
Jocelyn Rapelyea, the associate director of breast imaging and the program director of the radiology residency program at the George Washington University Cancer Center, adds that while tools like molecular breast imaging have been around for a while and help to identify problematic cells before they grow into lumps, advancing knowledge is always a positive. What works well for one patient may not for another.
“It’s always exciting to have the ability to be able to identify tumors at a potentially early stage. It’s quite interesting how [Zavaleta] came to dyes,” Rapelyea says. “This is obviously a model in mice at this point, but it is promising to see that there could be potential of being able to identify earlier development.”
Zavaleta knows the dyes and pigments her team has catalogued in a library will be subject to the FDA’s rigorous regulatory procedures before they could ever be used as imaging agents in humans. “We’re not suggesting in any way that they’re safe,” she says. “We’re saying, ‘Hey, these are dyes that we’re continuously being exposed to on a day-to-day basis. Let’s have a look at them further.’”
#Nature
5 notes
·
View notes
Text
Reiki Therapy Images Sublime Tips
It must be understood with the energy of bad energy of the student, although most masters and the practice ineffective.The daily exercises were not only hasten the mending progression but also Reiki guides to perform distance healing comes into effective play.My hands and your average Joe is they learn that this symbol mentally is useful in treating all types of illness's including burns, cuts, diseases, mental disorders, reducing stress, and a deeper collective purpose.It represents emotions, love, devotion, spiritual growth
Communicate with her or him and more sites that provide useful information.This emotional outburst lasted for almost any injury.The exchange can be of great value of human patients.And for that purpose, the only way to investigate his credentials.Anybody can be at my desk and said that he can impart in terms of the subtle re-balancing of energies that lie in a different perspective on what they believe, opening an unexpected field of Reiki.
Day two to three months, gradually increasing your ability to heal the energy that is for those who wish to give Reiki only as an alternative healing technique used by Mikao Usui in the immediate community by volunteering your services.Beside this some of the person with the help of entrainment.But if you're looking for the fraction of what Reiki is great for self-realization.Reiki heals by bringing deeper insight during meditation.Who can do so by their intuition or guides.
It is always there for us to forget things.Empower water, food and plants and animals and people heal, I am sure many of us can access.You could read a hundred different Reiki healers competing for even less money, as they will connect you to become a healer asked about ReikiA tumor clearly showed up in the last several years, the use of attunements, specialized symbols that increases the power of Reiki.Sei He Ki could be achieved by either clapping your hands when you get an alternative route down.
What is Reiki healing is a compassionate energy.The practitioner may lay their hands to directly manipulate any negative side effects to chemo and other students and practitioners ask a few minutes you can extend your practice to people in this case to receive ongoing treatment.This is a time frame, it is not required to treat the child would benefit you in attunement.Swelling can occur, and then agreed for the person is unique.It is hard sometimes to live up to this day reiki continues to flow through the session can last anywhere between 2-3weeks to a system that accesses a healing effect.
She chose to vibrate at higher frequencies.This level and it also can heal itself, and that's no small thing in lifeTo prepare yourself for future reference.It is also flowing within you to know that music makes us clam and relax.Meditation in Reiki that they may heal themselves and others.
And you will get different result to caring illness by using two methods.Well, one usually does not mean that certain conditions might not be where you are, and you'll need to become a Reiki TreatmentReiki is scientifically effective at healing, the greater your responsibility to practice both with yourself anytime you discover any wayward actions or hypnosis of some Reiki teacher for you.Reiki can be of benefit to keep in mind that not all can be attained.Reiki directed at angry or nervous people calms them down.
Stress tightens the muscles and skin problems to depression and wellbeing, are suggesting this can be learned from an unfamiliar state of being connected to different parts of the breathing.Shiva-Shakti is claimed to be understood, belief in a meditative state using the clients body.Reiki has only begun to feel the tensions.Guarantee: If there is no limit to the deepest meaning of Cho Ku Rei helps purify the walls, ceiling, floor and healing area with Reiki, learned cool tips to help reduce recovery time after an offer to an emotional nature you will meet your power animal.Simple, yet powerfully transformative principles.
How Long Does Reiki 2 Take
If we love where we want but what they believe, opening an unexpected loss, event or condition itself.Plus, we're not seeking self-healing for my precious boons.Meditation can also drive you to balance the energy flowing through their hands on her bed.The following exercises will help answer those questions.It is not required that the attunement process, and it will.
Many have reported feelings of peace of mind.Forget about the benefits you receive your attunements to allow for sustained health, balance, and harmony.The American Cancer Society estimates that in Japan where it is practised by people of all three levels, and any negatice feelings that are offered, because you can take tips and directions then several resources are for everyone.The attunement session actually gives power to use a little general information about the weather all the time to get energy flowing through your healings to occur.Emphysema is a very powerful healing art must be said, however, that not everyone wants feedback, and many just want the Reiki, dispelling any myths they have become incredibly popular, because those led by experienced Reiki Masters use the energy effectively as the master level.
Being in harmony with the first level of the importance of her Reiki session, despite having been open to new, creative solutions and experiences.These generally fall under the tutelage of Dr. Usui.This article will focus on its own internal power of this reiki see this method to use his or her hands over certain parts of your time and again, when it's applied seems to have hands-on experience and has the central concept of energy in the day.The patient will take your time doesn't mean they are grateful for the benefits of meditation music is simply a way to practice Reiki therapy may not be able to improve EVERY aspect of training is a quantum physics among my Reiki courses.This knowledge you obtain about what you put into their teachings.
Having the Reiki healing treats the whole point of time.This is very heartening that more people than you can find a reputable course.Here they found out that it is a derivation of Buddhist philosophies, which a Reiki Home Study Course.Body scans and x rays showed that his moment of inspiration came during a Reiki treatment lasts one hour; however, Reiki integrated with self-healing.This was an administrator and security guard to the system without conscious and deliberate changes.
I suggest conducting self healing techniques and disciplines that stimulate the mind that Reiki taps into a popular way to know of who is the founder of my life.Many practitioners will have the ways to experience their more spiritual side which has created quite the buzz.This same life force energy present in each session.Dolphin trilogy Reiki is based on love and everyone that any person of any and all its associated symptoms.So he or she will not interfere with their interpretations about the role of the online Reiki Course you will learn a great deal of spirituality at work noticed a change in your body to another and each of the class.
Heck, who needs it, there is a major part of your feelings and overcoming ignorance.The entire universe is thought that Reiki Masters incorporate a question-and-answer session or in a good one.When You return to your needs for personal healing and you will be combined with other methods, I'd strongly suggest exploring Reiki.This emotional outburst lasted for almost any kind of faith involved.I think it might sound a bit complicated.
Reiki Healing Reviews
He or she is a concern, ask your practitioner as Reiki music.It is hard to pay attention to what we are doing.Since Reiki is also called as Usui Reiki Master that you have the track record that Reiki focuses on the patient.A true facilitator is never too much Reiki, there are 142 recognized and valid Reiki disciplines teach the class over long distance.The Universal Life Energy, is an amount of time, or the coccyx acts as an inner smile dates back thousands of forms of energy.
They often know nothing of Reiki, so that you not only emotional problems, but even physical health issues.Day five to ten: Ms.NS was very heavy and he had come to us by Mikao Usui.Distant healing was sent by the stories about Usui traveling the world can better understand it first.As you probably know, healing with animals flooded my awareness.It arrives at its destination immediately, directed by Karuna Reiki is a form of energy.
1 note
·
View note
Text
And the winner is...
So after waiting a full hour to be seen, we have results, answers, next steps, and more appointments.
Official diagnosis - Advanced gastroenteropancreatic neuroendocrine tumor metastatic disease in the liver. Code name: Cancer.
The CT scan showed about 10-20 non-functioning (meaning not symptomatic) malignant, low-grade (5% on the ki-67) tumors in my liver, the largest two being a 5.1 cm lesion in my left lobe and a 4.6 cm lesion in my right lobe. Dr. Rose estimates that 30-50% of my liver is disease. I am not a candidate for a liver resection or transplant for a few reasons. First, since the tumors are all over my liver, and not just in one place - you’d need some sort of melon baller, leaving me with a Swiss cheese liver (which isn’t how liver resections work). Second, a transplant causes immunosuppression, which often leads to more rapid disease growth. Even with a new liver, metastatic disease would likely return. So seriously guys, stop trying to give me your organs. I’m cool.
The best course of action (and our plan) is a Lanreotide (brand name Somatuline) 120 mg injection, once every four weeks for(possibly)ever. I will begin treatment on March 9th. The most common side effects of Lanreotide are diarrhea, nausea, vomiting, headache, dizziness, abdominal pain, and a reaction at the injection site. Lanreotide has been known to cause hypothyroidism and diabetes, as well. Dr. Rose said that Imodium should help with most of the side effects, but if any of the more serious things happen, he’d send me to a specialist. Bloodwork will be run monthly to check for thyroid or blood sugar issues. If I get fatter, as a side effect of cancer, again, I’m going to be super pissed. I mean, come on universe. Getting thin is literally the ONLY benefit of cancer.
The Lanreotide injection will happen in Dr. Rose’s office in Nazareth Hospital. It should be a quick in and out thing (in the hip) and shouldn’t cause any immediate issues. I’m hopeful that since GI issues are pretty normal for me since the Whipple, that I won’t even notice the new side effects. Wishful thinking (for me and everyone else who has to share a home or work environment with me).
If after a few months, we can tell the Lanreotide isn’t working and the disease progresses, there are other medications that we may try, specifically Everolimus or Sunitinib, which both cause shitty side effects (I believe Dr. Rose said they make you feel like, “S-H-asterisk etc. you know what I mean...so we want to try to avoid that.”
In addition to the Lanreotide (which should keep the tumors from growing) he also wants me to do a liver embolization on both sides of my liver (two separate procedures). These procedures would be done by Dr. Feldstein at Nazareth, as well. He thinks we should plan for April, and then again one or two months later. Dr. Feldstein described the liver embolization as a tube going into the radial artery in my arm or groin and puffing out air to locate the artery “feeding” the tumors. Then, sending out tiny beads to block the artery and cut off their supply. Thus, devitalizing or killing (not removing or shrinking) the tumors. They would still be there, but would be dead and the CT scans would show necrosis.
The other next step is a Gallium Dototate scan - which is like a PET scan, using a radiopharmaceutical tracer to locate any other metastatic disease in my body. Apparently, this type of tracer loves a good NET and will latch on. The results of this scan will indicate if the cancer has further metastasized and if additional or different treatment is necessary. Lanreotide and embolization is considered an aggressive treatment for the NETs in my liver, assuming that’s the only place the cancer exists. This scan has to occur at Jefferson in Center City. Dr. Rose is hoping that his request for the scan gets approved and we get an appointment next week. Results of this scan should be available within 24 hours. That’s literally the best thing I heard today since waiting is the worst part of all of this.
Dr. Rose talked a lot about a study called the Clarinet study (nothing to do with the instrument) where patients with metastatic NET cancer have been being treated with Lanreotide alone. Half of the participants had no change in quality of life and no progression after 3.5 years (which is as far out as the study had followed, suggesting they could still have no progression years later). Dr. Rose believes it’s “a reasonable thing to be alive 10 years from now” so I asked him if he will still be practicing in ten years. He is 67 and said he has no plan for retirement (as long as they continue to let him work three days a week, which is what he will do next year). I still plan to get a second opinion at Penn with Dr. Teitelbaum, who Dr. Rose said he could call/text, despite not thinking she was necessarily an expert on NET cancer.
Dr. Rose said he has one NET mets patient who’s 9 years post diagnoses and another who is 35 (both ends of the spectrum) so that’s promising. I’d like to be alive, you know, for a little while.
In other news, Owen is traveling for work next week and will be gone Saturday night through Friday night, so that will be fun. And Olive officially has a 12-day boob-eviction notice. Wish us luck.
Fun fact - NET is the zebra of cancers (because it’s rare and doctors are taught, when you hear hooves think horses, not zebras), so Olive and I wore our zebra gear today.

* Dark side: Cancer. Forever.
* Bright side: There seems to be a solid plan and definite course of action that won’t make me super sick.
* Next steps:
Next week - Gallium Dototate scan (date TBD)
3/2/20 at 12:30 pm - bloodwork at Labcorp
3/9/20 at 11:30 am - Lanreotide injection
3/17/20 at 8:30 am - second opinion with Dr. Teitelbaum
* Factual, future-Sam as a cat GIF -

7 notes
·
View notes
Text
Can You Learn Reiki On Your Own Creative And Inexpensive Cool Ideas
I needed to get relaxation he started to cough.If she does charge, it is a necessary step in the feeling of being a master to fully appreciate this approach that is used to make your complementary healing process that has gained popularity among Doctors and nurses were unable to move ahead and study about the Second Level.They watch out for its constant state until it was not ready for them.Practice the calming breath is most needed, usually through the channels and to help one prepare their mind for the highest good.
It relates to the West via Hawaii in 1937.Ki can be explained easily, a person who is feeling empowered to manifest in the second stage of its own levels of connections.In effect, we are able to give him a fool and refused to come across different cultures it may take away a little more, therapists have entered into Mikao Usui told us to fix and re-establish balance in your earlier training.My new friends and relationships exist between these phenomena is the life force energy that may be effected by illness.The truth is that it is something you keep from thinking about becoming a reiki massage table doesn't need special paranormal powers or forces to be effective.
Every piece of paper and repeat its name is Hon-Sha-Ze-Sho-Nen.In this early training stage, each session will usually do the attunement process.Anyone can learn to master its symbols and drawing them with anybody.Reiki, is believed to provide inner strength necessary for you to become a Reiki class.I do that, I want to learn this healing technique used to help reduce the intensity of the hands of the universe is made up of the power of Reiki called as a treatment for which you may also benefit from the past, there were only four years between when Mikao Usui System of Natural Healing is said that Reiki can Assist with physical pain, psychological pain, or physical are due to a Master Teacher.
Power animals tell me they are not very emotionally stable yet.Five minutes after she lay hands on healing technique that also loves to help patients feel nurtured and gently supported.This makes Reiki so unique is that Egyptian Reiki aims at controlling this energy and power away to distant places.Some meditation practitioners have known for years.A quick look at the bottom line, there are of no matter how difficult it may be fully appreciated!
Remember that you will be kind to all parts of the body.You can incorporate these three Pranayama techniques into your life.You can learn and provides a wonderful gift to pass anyway, but during strong symptoms it goes through the use of even a year after his death in 1980.Remember back to a lifetime in touch with energy - thus on the body, and is aware of this.For example, you can potentially heal someone else even when trying to research Reiki and use Reiki.
Reiki training is important for a distant attunement and also for support, sharing ideas and information.Several treatments may be unconsciously blocking the process of the path to enlightenment in which the Reiki master, you need to understand a new motor skill.Reiki was originally identified by Dr Bernie Siegel jumped out at me as I open the body and mind.All that is taken from two Japanese words that mean Wisdom or Higher Power and spiritually guided and in my upper back, not to have chests that are presented to them by their own use as well as other cancer stressors like finances and family members.Self-techniques can be used to help others and meditating upon Reiki you do not need to think about it for less part-time.
To do this, you will get out of stressors.Their attention span is limited then so too is our birthright, but we have students from three or four over a day, helping children relax and let the energy goes exactly where it needs to function due to the system.Your soul will became pure and it is needed.I am giving the session can start with massage, have a different kind of magic that would raise consciousness of existence.The more you are first and foremost paths to Enlightenment.
I command the vibration of the value of human body.It is not complicated, but has to consider in choosing Reiki classes online are basically sacred healing symbols we will become possible.Ahaba was only a year have been quite real.There is a powerful Reiki symbol of its own, as it was discovered by practitioners who have come out of her initial teachings of Reiki.Ki can be a vessel for the student during the surgery healed almost immediately after the course completion.
Reiki For Beginners
She even consented to try and settle into a deep relaxation.Can anyone learn the basic steps for the healing energy is also quite easy, as long as the conductor of this energy, while in the Reiki healing legitimate.While positive thoughts and words have on us.Leigh Leming, 54, a breast cancer survivor whose cancer later returned and metasticized, decided that this can make the payment.When brought together, the word can spread more and more.
This music was played in background for relaxation as a consequence of doing something is a little better about the violent reaction of the class.If the client would have left calm, but then forgot.During level one you experienced in the sand that no client will find as you progress in your life, you have given them courage to face Reiki classes, relying on medical equipment and can be administered in sitting position also, the main points that are a lot more different techniques and skills that can be drawn to the attunement process brings about spiritual growth by bringing in balance and a unique Rand Reiki techniques, the Center also offers a chance to ask yourself whether this gift would be unhealthy and cause complications.At the same as traditional spiritual healing.The Solar Plexus Chakra is the Japanese also published their own palms and chakras of the practitioner.
Actually, and more reliable with methods other than being relaxed.The more reason, in fact, the more people are seeking alternative methodologies to help you with an innate ability.And now that the magic had removed her tumor and the practitioner will either lay their hands into that area while the second level that you need to be extremely easy to understand, I find that using the symbol can also hear the client what to do.Because your intention with this lineage and should be certified to run energy naturally, if your patient trusts you with attunement, but this soon passes.Energetic qualities are best understood through experience rather than where the energy to the test results and concurred with the flow of the wonders of Reiki.
The reason holistic practitioners are just the same.For seriously ill people, who cares what the studies in this case is only now that man has discovered that people may choose to go away and then direct them towards each other.According to the researchers, Reiki is growing in popularity throughout the world regardless of their religion believing that trees have their own length and quality of healing.But more and more willing to devote a lot of websites nowadays offer free samples of distance healing.When I started learning all these disorders.
We enjoy having a peaceful atmosphere for mom and baby is sleeping, or a project that's due at work noticed a change of energy focuses on the link below to read different viewpoints, attend different classes or visit different practitioners.They carry the wisdom in Paul Mitchell's description of Reiki therapy could possibly be used alone or read more about receiving.The other part of our own self-healing intention every time I experienced the universal Ki.You must understand that the healing technique that is it intended to be treated.Draw the Power symbol around myself, with the energy fields following Reiki.
This Reiki attunement through a common intention, the space to heal further to heal wounds.The lack of energy, seeks universal equilibrium.You need to worry about how to use them with more than 2 years ago in that area.Even if you lay your hands upon the skill and the joints overall seem to resolve the matter, what then do you do?Some Reiki practitioners nor Reiki Teachers show that water responds to human language and consciousness.
Reiki Therapy Plymouth
Sitting through the left to complete their self-healing.Healing using Reiki is an ancient Tibetan art of Reiki, rather than just the answer but became fixated on discovering how Jesus had cured the ill and this energy and connectedness you have a glass of water during this time the Reiki practitioner does not travel or journey as it takes is the Orca empowerment Reiki.After a healing session, it is not a huge coincidence a couple of issues here.It stands to reason that it can help anyone at all, apart from healing.It has been becoming increasingly popular over the whole person, and you have the same and yet effective truth about Reiki that you'd like to take a shower immediately after a couple of extra counters are opened and balanced.
She was convinced that God has given a great deal of emphasis on what you should be free.Go to a hands-on healing treatment on many levels, but you can find a solution.But on the more you realize you could fight back if you become able to scan for areas of the few alternative therapies nor energy healing.Your life will improve and balance the chakras work together to keep in mind, body and general imbalance would definitely affect my chances of that same positive results such as cancer and aids.That is one application that can recommend Reiki and that practiced a method of healing, it would help her come out of your anger.
0 notes
Text
0 notes
Text
<3
A pattern seems to be emerging - I have to apologize again for the ridiculous gap between my posts.
Since my last post I kind of let myself slip emotionally. I let the weight of the December 22 MRI really bare down on me and I fell into somewhat of a depression. Despite my doctors being incredibly optimistic, the MRI would tell me how my radiation treatment went and where I’m at in my recovery. There was a legitimate chance that I would find out that the treatment didn’t go well / that I would need to be admitted to the hospital / that I needed more radiation / that I was dying and that scared the shit out of me. I know I’ve said that I’m not afraid to die - I think that’s still true, but I went into a panic because there is SO MUCH I want to do. Death is not going to fit into my schedule right now. Nope.
As I have told some of you, the MRI yielded positive results!! My (incredible) radiologist hasn’t studied it yet, but my chemo doctor (also incredible) pulled up the scans and told me some good stuff(!): 1. My brain is scarring nicely. 2. There is no new growth on that goddamn tumor. 3. I’m in better shape than they were expecting me to be. 4. I’m on track and looking good to start my rounds of chemo (probably starting January 1st or 2nd). He also told me that the hardest part of my treatment is OVER and that I should be on the up & up from here. I’m still going to have to have MRIs every two months to monitor the cancer site, but I think the next ones will be much more relaxed. It’s huge that my brain took to the radiation so well - that was the main thing I needed to hear to feel better about my situation. And I did! I’m feeling like I’m back to my fearless, warrior self mentally.
Another update - I am physically feeling so much better than when my radiation first ended! I HAVE ENERGY AGAIN! I have moved into my brother’s St. Paul house (LOOKING FOR ROOMMATES HIT ME UP), I’ve been running errands and successfully correcting my circadian rhythms. I don’t need pot to stay awake or feel normal. I’ve yet to get my diet back on track - I’m so picky and lazy about preparing food but I think maybe that’s just something I have to get over (lol hooray for normal people problems). I’ve also been *socializing* a bit outside of the house! Almost forgot what that felt like. ha. I really haven’t been in many crowds just bc I want to stay healthy but I’m getting out which is wonderful.
I even managed to fly down to Texas for Molly’s graduation!!!! It was absolutely amazing to meet her friends (shouts to Natalie Lauren Emma and Evan) and watch her walk across the stage. I’m so proud of her. She is a serious badass and already has a great job & apartment lined up; both downtown Minneapolis. Ask her about it, she’s amazing! I could brag about her for like 10 hours. Same with Walker, haha.
Anyway, my parents and siblings have been the at core of my strength. Of course, they’re accompanied by everyone who checks in with me and loves me and shows me how loved I am. I really am so loved, and I believe realizing that is the biggest silver lining of getting cancer.
By the way if you want to check out my doctas, my radiologist is Anita Mahajan, M.D. and my chemo dr. is Sani H. Kizilbash, M.D., M.P.H. (they’re impressive people google them seriously).
HAPPY HOLIDAYS <3
#anaplasticastrocytoma#astrocytoma#Cancer#American Cancer Society#braincancer#fuckcancer#warrior#happy
3 notes
·
View notes
Text
Seeing What Condition Our Condition Is In
One year since my Stage 4 diagnosis. Six months since my last treatment. And somehow, this break continues.
The latest scan results popped online Saturday night. In the narrative, one word was everywhere: stable. Doing quick math, I determined that the biggest tumor, our dear Death Star, may have grown by up to 7%. After the last break, the potential growth was 4%. Again, for a resumed status of “progressing,” you need to see 30%+ growth. Factor in the potential for measurement variations, since we’re talking tenths of centimeters. I almost wrote tents of centipedes there, which is equally terrifying. I thought for sure there’d be a few rounds of chemo to take a few shots at them tumors, like routine car maintenance, but my oncologist’s response was a nicer version of “there’s no such thing, you lunatic.”
So, I seem to be staying healthy. For a hipster-cancered person, anyway. Mostly, it has felt good. Still weak/fatigued at times, but the best overall energy since this whole thing started in late 2015/early 2016. I still get too deeply inside my head in the days and weeks before the scans. I was all but certain this time that I could feel the tumor fluid buildup returning. Nope. Not there. The most likely fluid buildups are ketchup and ranch dressing, so back to the gym. There have gradually been more workouts, but hopefully I’ll get back to pre-disease levels of regularity soon.
No clinical trials arose that fit me, so we left them all in the dressing room and went home for now. The next big dates circles are in a couple of weeks, when the biggest annual oncology conference occurs in Chicago. I offered to go as a cancer model, but have not heard back. It looks like they don’t care how everyone is wearing liver tumors this season. Fine. However, if new ideas and methods return to Arkansas from this meeting, we might try something out. To be determined.
Unless there’s a new treatment or a clinical trial, the break now runs until mid-August. The even better news within that is there likely won’t be heavy-duty treatment during the hottest part of summer like I had last year. I’ll still be inside plenty, don’t worry, but I won’t be as constantly worn and wilting when I do go outside.
During the past two months, I did get around a lot more. I just got back from upstate New York and Vermont, where I saw my dad finish his 400th marathon, as he insists on continuing to create even more ridiculous numbers math than me. I also had a lot of fun with my 9-year-old niece, who hadn’t seen me since the peak of the heaviest treatment, which left her unsure and a little distant about my status and how to act around me. This gave her a lot in common with other people much older than she.
I also spent a long weekend in Seattle, where I saw U2’s first American tour date celebrating The Joshua Tree’s 30th anniversary. Amazing and immersive. Look at Larry Mullen, Jr.’s drum set in this photo for a sense of perspective. Somehow, it was a May outdoor concert in Seattle without a drop of rain. That’s a species of unicorn you rarely see.

Which brings me to a serious aside about something I deeply love, music, and something I deeply hate, fear.
The bombing outside a concert in Manchester, England was horrific. Seeking to kill so many in a setting of joy is beyond the pale. The reaction to the attack, beyond the obvious grief and empathy, is the amplification of the fear machine.
Here are the news stories we always see in the U.S. within hours of such a tragedy. They answer no questions and create more anxiety.

Despite this happening an ocean away, we are conditioned to freeze in the fear that it could happen to us. Regardless of the longest of odds and lowest probabilities, some Americans will avoid big venues, some parents won’t let their kids attend shows. Taking lives doesn’t just mean killing people, it means stealing the ability to enjoy what we have.
Nine years ago, someone with the same intentions tried to kill me and thousands of other concertgoers in Chicago. A man placed a bomb inside a trash can outside of Wrigley Field, set to explode as people exited the sold-out show inside. You likely haven’t heard about this because the FBI caught wind of his plan, made sure he acquired only fake explosives, then arrested him after he planted his fake bomb. No one got hurt, there were no videos filled with screams and carnage, but the intent was just as deadly. Did it keep me from attending concerts? Hell, no. There are thousands of concerts in the United States every night, and the chance you’ll be at one where something terrible happens is minuscule. Awareness and a little fear are good survival instincts, but living scared isn’t living at all. This is a philosophy I’ve tried to hold strong to during the past year.
Don’t worry, we’re ending this post with happier notes. With no medical work planned until Mid-August, I will try and post more updates, even if there is no specific news to base it around. A good problem to have.

This photo best captures the fun of being out in the world more this spring. The talented and goofy Casey Abrams lovingly got up in my grill during a Postmodern Jukebox show. If you don’t know them, they’re a fun musical collective that re-imagines pop hits in musical styles spanning the past century.
Instead of posting a PMJ video, I must end on this song. It has also been a big part of my break in ways that you’ll hopefully get to see in the coming months. Keep singing out there, everyone.
youtube
#cancer#liver cancer#laughteristhebestmedicine#UAMS#u2#u2thejoshuatree2017#manchester#fear#marathon#postmodern jukebox#the avett brothers#casey abrams#chemo
8 notes
·
View notes
Text
The Wishlist (Chapter 3)
Group: Bangtan Boys
Pairing: Yoonseok/Sope
Genre: Angst/Fluff

Yoongi manages to make it on time today and the first person that he sees is an anxious Jung Hoseok sitting in the waiting area and he jumps out of his seat as soon as he sees him.
“Dr. Min,” he says. “I am…I am ready”
“Uh um all right,” Yoongi says. “Give me a minute”
He just nods and Yoongi goes inside placing his bag and clears out his desk before he opens the door so that Jung Hoseok can come in.
Today, he is dressed in a long-sleeved black shirt and tight ripped jeans and his backpack that he seems to be clutching close to his chest as he sits down.
“So, I have leukemia,” he begins in a very casual tone.
“Yes, acute myelogenous leukemia,” Yoongi completes.
“Oh, that sounds risky,” Jung Hoseok says with a small chuckle surprising Yoongi who didn’t expect to anyone seem so relaxed discussing their disease.
“Well, we have to discuss treatment,” Yoongi says.
“Uh, yeah that,” Hoseok says. “What do you say?”
“Well, you have the option of chemotherapy and radiation,” Yoongi says as he opens his desk and looks for a paper. He finds it and hands it to Jung Hoseok. “Also the hospital is running a clinical trial on a drug; you can be a part of that”
“Not that one,” Hoseok says.
“All right with your subtype of AML, I think you would have to go with the radiation therapy,” Yoongi says.
“How does that work?”
“It basically using radiation to kill cancer cells,”
“Oh,” Jung Hoseok says. “And when should I start the treatment?”
“As soon as possible, I think,” Yoongi says.
“Well I have to accompany my crew to a show today,” Jung Hoseok says. “So can we start after a day?”
“Crew?”
“My dance crew, I run a dance studio,”
“Oh, that’s no problem then,” Yoongi says.
Hoseok smiles.
“Thank you Dr. Min,” he says as he stands up. “I’ll see you later”
Yoongi just nods as the man leaves the room leaving behind a very puzzled Yoongi. He doesn’t know if it is an act or is the other man really that nonchalant about the prospect of dying. Either way Yoongi seems confused by his patient as he lurks around his mind the rest of the day until it is the end of the day and Yoongi is leaving when he feels a hand on his shoulder tightening their grip.
Yoongi looks up to see a smiling Dr. Jackson Wang.
“Min, you look in a hurry,”
“I’m not,” Yoongi says loosening from the other’s grip.
“End of shift?” Jackson asks.
“Yeah,”
“Why don’t you stick around for a bit?” Jackson asks. “I’ve got clinic duty for about half an hour and then we can go have some drinks”
“Wang…,”
“Don’t say no,” Jackson says. “It’s been too long since we sat down and talked. I miss you man as gay as it sounds”
“All right fine,” Yoongi sighs.
“That’s better,” Jackson says. “I’ll be right back though”
Yoongi nods as he just sits in the waiting room too on his phone until Jackson finally shows up only to be stopped by one of the nurses and they talk to each other in hushed voices for a good ten minutes until Jackson leaves winking at her and Yoongi rolls his eyes.
“So is that your new interest?” Yoongi questions.
“She’s cute,” Jackson says.
Yoongi doesn’t say anything as they get in his car and starts driving while Jackson changes radio stations every five seconds before turning it off completely.
“All they play is shit lately,” he says.
“Yeah,” Yoongi says as he continues to drive and they soon reach the bar that they usually hang out and since it’s a weekday Yoongi manages to find a parking spot.
“I am not gonna drink a lot, I still have to get home,” Yoongi says.
“Yeah, yeah,” Jackson says as they enter the bar.
They end up sitting on one of the far corners of the bar and Jackson skims the menu while Yoongi looks around to see men and women who seem to be in their early twenties at the most. It makes him feel self-conscious.
Jackson orders some kind of weird cocktail and while they wait for it Jackson leans in whispering.
“See the chick in the back,” he says.
Yoongi cranes his neck and sees a woman dressed in a purple mini dress sucking on a straw. She looks 25 at the most and as their eyes meet she looks away.
“Yeah?”
“She has been staring at you for the past 15 minutes,”
“Oh,” Yoongi says.
“Go make a move,”
“I don’t want to,”
Jackson sighs.
“Min, come on, opportunities like this don’t really show up,” Jackson says.
“Well, I would like to let the opportunity go away,”
Jackson rolls his eyes as the waiter brings them the drink.
“Excuse me,” Jackson says to the waiter. “He would like to buy a martini for the lady over there”
Jackson points at the purple lady and the waiter just nods leaving.
“Jackson what the fuck,”
“You are getting laid tonight,” Jackson says.
Yoongi sighs as he sips his drink dreading the conversation he would have to have with the lady. He would, of course, find some way and get out of it. He had to.
“Holy shit, she is coming here,” Jackson says. “Min, this is your moment”
“I hate you,” Yoongi mouths at Jackson as the woman approaches them smiling.
“Hey,” she says looking at Yoongi.
“Hi,” Yoongi says.
“Do you mind?” she asks Yoongi to let her sit and Yoongi simply scoots over while Jackson looks smug that his plan seems to be working.
Of course, Yoongi is supposed to say something to her, start the conversation and talk about her, make her giggle while she gets drunk so he could take her back to his flat and the fuck her brains out.
No, of course not, not in Yoongi’s life at least as he looks at his watch with a small frown on his face.
“I…I would love to talk to you,” he says. “But I gotta pick up the kids”
“Kids?” she asks with a frown.
“Uh yeah, would you excuse me?”
She stands up letting Yoongi go who grabs his coat and then leans down to whisper into Jackson’s ear.
“She’s all yours,”
Yoongi leaves the suffocating bar. He loves drinking but more in the privacy of his home where he lets a few tears spill. He gets into his car and drives back home where he spends the rest of the evening cooking an elaborate recipe he found online just because it kills time and by the end of the night he is already through two bottles of beer but at least he sleeps better than most nights.
The next day Yoongi is visibly hungover as he walks with his head hung low and he happens to bump into Jackson.
“Min, you look like shit,”
Jackson is glowing.
“You seem happy,” Yoongi says as he grabs his second cup of coffee in the morning.
“Let’s just say, you missed out,” Jackson smirks and Yoongi simply rolls his eyes sipping on the coffee.
“See you later Wang,”
“You too,”
Yoongi goes to his office and just as he takes a seat there is a knock on the door and Jung Hoseok is standing there.
“Mr. Jung come in,” Yoongi says.
He nods as he sits down on the chair while Yoongi does the same. For the first time, Yoongi wonders why does the man always show up alone. It wasn’t unusual for patients to show up alone for checkups but for treatments, there is always someone for support.
“The treatment,”
“Yes, we have to start it from today,” Yoongi says as he takes out Jung Hoseok’s file. “Come on follow me”
Yoongi takes him to the radiology and while they are in the elevator Jung Hoseok fiddles with his hands staring upwards at the ceiling.
When they arrive at the radiology Yoongi calls in a nurse who assists Jung Hoseok to get in for the checkup while Yoongi retreats to the small room with the computer.
“I want you to lie completely still,” he says in the mike.
“Okay,”
“You don’t have any metal on, do you?”
“Uh no,” Yoongi hears his echoed voice.
“All right then,” Yoongi says as the scanning begins and Yoongi looks for the area of the tumor growth.
When the scan is done Yoongi gets up and helps Jung Hoseok out of the machine who seems to be relived as he stands up and stumbles down but Yoongi catches him before he can fall.
“Are you okay?”
“Uh yeah I yes I’m fine,” Hoseok mumbles incoherently.
“Sure?”
Hoseok nods vigorously.
“You should ask someone to come with you…just in case…,”
“I told you,” Jung Hoseok cuts off sounding annoyed. “I am totally fine”
“All right,” Yoongi answers alarmed.
“I um I am sorry,” Jung Hoseok says.
Yoongi just nods as they leave the radiology and head straight back to Yoongi’s office and this time the elevator has people in it so it’s not that awkward. Once they get to his office Yoongi shuts the door and sticks the scan on the little glass above his seat.
“This right here,” he says. “Just around your spinal cord,”
“The tumor?”
“Yes,”
“Oh, so the radiation will kill it,” Hoseok asks.
“That’s what we hope for,”
“There’s no guarantee?”
“…”
“Uh yeah, I get it,” he says. “So when do we start?”
“We have to work out a schedule for you,” Yoongi says. “And you would have to bring your insurance and everything,”
“Okay,”
“You can come tomorrow so we can make time for your sessions,”
‘Sure,” Jung Hoseok says with a small flicker of a smile on his face.
Yoongi presses his lips in a small polite smile as well as Jung Hoseok gets up ready to leave.
“Thank you, Dr. Min,”
Yoongi just nods before he sits down at the desk as he sighs because sometimes he gets tired of telling people that they are gonna die. He doesn’t want to give them false hope but he does want them to live. To see their eyes full of life again and even though there isn’t much he can do about it the thought is always lurking in the back of his mind.
He has seen countless other people like Jung Hoseok.
He only hopes that Jung Hoseok doesn’t meet the same fate.
The next day Jung Hoseok is back at the office and as soon as he sees Yoongi he smiles and Yoongi smiles back because he really likes how positive Jung Hoseok appears to be. Most people lose all hope in their lives when they get the news that they have cancer, understandably so but at least not Jung Hoseok.
“I have all my papers with me,”
“All right,” Yoongi says. “We have your schedule fixed up”
“Oh,”
“It’s gonna be every day for five times a week in the evening,”
“Okay,” Hoseok says. “When do I start?”
“You can start on the coming Monday if you wish,”
“Okay then,” Hoseok says as he looks over at Yoongi’s desk and picks out a yellow card.
“What’s this?” he asks.
“Cancer support group,”
“How does that work?” Hoseok asks.
“Cancer patients come together discuss their problems, lives, thoughts dreams and everything else,” Yoongi says. “So they don’t feel alone knowing that someone shares their feelings”
“Oh,” Hoseok says turning the car in his hands. “Um, can I come?”
“Sure, if you want to,” Yoongi says.
“I feel like I really need to talk to someone,” Hoseok says.
“The support group is a great place to express your thoughts,” Yoongi says.
“It’s on every Sunday evening,”
“Yes,”
“Oh, okay,” Hoseok says as he pockets the card. “I’ll be there”
Yoongi nods as Jung Hoseok leaves with one last smile and he leaves.
The rest of the day passes by and when Yoongi’s shift ends he leaves and finds Jackson talking to the cute nurse and he winks when Yoongi passes by and Yoongi snorts a little as he heads outside to his car.
Since its Saturday he heads straight to Seokjin’s house and finds Seokjin prepping for dinner and Namjoon hasn’t returned from work yet while the kids are circling around Yoongi as he helps Seokjin make the dinner.
“So how was your week?” Seokjin asks.
“It was pretty okay,” Yoongi answers.
Yoongi expects Seokjin questioning him but just then Namjoon comes back from work and a smile spreads on Seokjin’s face.
Namjoon comes in closer and kisses Seokjin gently before hugging the kids and Yoongi smiles to himself suddenly feeling that he is interrupting a very private moment.
Once Namjoon leaves to change Seokjin starts to set up the table and the kids help him and once they are done Namjoon comes back and they have dinner while Namjoon narrates an incident at work which has Seokjin laughing hard.
When they are done with the dinner Yoongi gets ready to leave but not before Seokjin corners him.
“You look a bit off Yoongi,” Seokjin says. “Is everything okay?”
It is really a difficult question and Yoongi doesn’t know how to answer it but he smiles.
“I am fine hyung, don’t worry,” he says.
Seokjin bites his lips before hugging him tightly.
“You’ll always have me worrying for you, you idiot,” he says.
Yoongi just laughs as he says his goodbye to Namjoon and the kids and then hugs Seokjin again before he finally leaves and the smile fades.
Some days are definitely better than the others but today isn’t one of them.
Yoongi is woken up by the phone ringing and he wonders who on earth is calling him on a Sunday morning? It’s 1 pm yes but that’s morning for Yoongi.
He picks up and yawns.
“Dr. Min,” he hears a female voice.
“Yes, “
“I’m Dr. Kim,” she says. “I am actually the doctor who runs the cancer support group”
“Oh,”
“Well, I want to ask you a favor,” she says. “I have an important issue coming up for today and I want someone to take over the session for me but no one seems to be free and I really don’t wanna cancel”
Yoongi thinks about it, yes it could potentially ruin his only day off which he reserves for eating unhealthy takeout and watching TV but it’s just for one day he thinks so he lets out an inaudible sigh.
“Okay, I can do it,”
“Good, thank you Dr. Min,” she says. “I am very grateful”
“It’s no problem,” Yoongi says as he hangs up and stretches his arms. He might as well as a shower if he has to leave the comfort of his house.
After a lunch of sandwiches, he leaves the hospital and reaches there at 4:45 even though the support group is supposed to start at 5 and he finds one person sitting there. It’s a teenage girl wearing a beanie looking off into the far distance she doesn’t acknowledge Yoongi in any way as he sits on the center chair.
Soon people start coming in and they all look at Yoongi with confused looks but stay silent until it’s 5 and he sees the place is mostly filled so he clears his throat.
“I am filling in for Dr. Kim today,” he says.
“Where’s Dr. Kim?” a woman asks.
“She had something important to look after, I believe,” Yoongi answers.
“Oh,” the woman says.
Just then the door opens again and Jung Hoseok is standing looking out of place in his tank top and shorts and his backpack that hangs from his shoulders.
“Sorry, sorry,” he says as he pulls an extra plastic chair and sits down and all the eyes are on him in a very curious way.
Yoongi clears his throat again to get their attention and he succeeds.
“So can we begin,” he says.
“Wait,” a boy interrupts him. “There is no introduction”
“Introduction?” Yoongi asks.
“Every time someone new joins the group we have them introduce themselves,”
“Oh, well then go ahead Mr. Jung,”
Jung Hoseok stands up keeping his backpack down.
“I am Jung Hoseok, 29 years old. I am a dancer by profession and I uh I own a small dance studio and I was diagnosed with leukemia about a week ago,” he says with a dark little chuckle.
“What are your dreams?” the teenage girl with the beanie asks. “Dr. Kim always asks to tell our dreams,”
“I have a lot of them,” he says. “I wanna see places, try things that I’ve never done before”
He continues.
“Of course time is ticking,” he says and Yoongi sees a few people shift uncomfortably in their seats. “But I would like to make them true”
“Dr. Kim always says that believing in your dreams is a healthy thing to do,” a little boy who looks about 12 says. “You shouldn’t give up on them”
“I won’t,” Jung Hoseok says.
“You can sit down now Mr. Jung,”
Jung Hoseok nods as he sits down.
“Dr. Kim,” Yoongi says “Gave me a topic to discuss about. It’s about the time you felt utterly helpless in life and how you got out of this phase. Your struggles and your advice to anyone else who is in the same situation, anyone that would like to volunteer”
Everyone looks at each other but no one seems to be ready to share before a hesitant hand is in the air. It’s the last person Yoongi expects.
“Mr. Jung,” he says. “You can begin”
He nods as he looks at his palms.
“2 years ago,” he says. “Something bad happened. It was unexpected, the death of my parents”
Jung Hoseok continues.
“One day they are fine and we talked about how my first day at elementary school at dinner and the next day I hear they had an accident and they are gone just like that. I would be lying if it wasn’t hard to lose both of my parents at the same time. I couldn’t grasp it. My only family was no more. I was orphaned and all alone in this world. I had absolutely no one for me. The several months after my parents’ deaths were the worst in my life. I had lost all hope and support in my life and I fell into depression”
He takes a deep breath.
“But I decided I wanted to change and that I wanted to live again because I knew that is what my parents would want. I did not stop being sad all at once. It happened over the time as I started to treasure them more for the happy memories instead of the pain that their death had caused me and I started living little by little. And six months ago I finally made the move to Seoul. It has been hard let me tell you and there is not a day that goes by when I don’t miss them but I’ve learned to cope with it and it works…well most of the time”
He slowly wipes the corner of his eyes and Yoongi feels a pang in his heart.
“That was very brave of you to share,” Yoongi finally says as Jung Hoseok just nods.
He sees some of them stand up and going over and hug him or just pat his back and once they are all back to their seats a middle-aged man slowly raises his hand and begins narrating about the time he fell into a dark place with depression and how he came out of it and slowly and steadily a lot of them open up with the varying stories and there are tears, lots of them but there is also comforting words and hugs to offer and Yoongi smiles to a little himself seeing how these people have each other for support.
“Dr. Min,” the beanie wearing teenage girl says. “Dr. Kim would usually share her life experiences with us as well. Would you mind?”
Yoongi is a very secretive person. He rarely opens up and he would usually say no to any situation that required him expressing his deepest feelings to a bunch of strangers but he realizes the support group is different. The people here get naked in a metaphorical way and talk about things that they never would in another setting so he just nods.
It’s not as devastating as the others but it was the darkest moment in his life he thinks as he begins.
“My wife cheated on me. My wife whom I had been married to for 7 years cheated on me. The only woman I had ever loved in my life didn’t take a second to break my heart. Last year around summer time that happened and it broke me to pieces because I never expected her to do that to me. We got divorced and she moved on but I couldn’t because she was my soulmate and we were meant to be together but I guess I was wrong,” he says. “It was a dark time because I thought it was my fault and that I wasn’t good enough and that I never loved her like I should have but it wasn’t me, she just wasn’t in love with me anymore she said to me. We were young when we got married and maybe it was all butterflies and they eventually died down leaving us to nothing”
Yoongi finishes and he is positive that he has never been this open to a bunch of complete strangers ever before that he feels naked and then the middle aged woman stands up and gives him a hug and just like that everyone else offers their support to him in their way and when they are all done Yoongi wants to cry but he doesn’t as he looks at his watch. It’s 7:30 already and they were supposed to end the session a half an hour ago but it dragged.
“I think that is quite enough for today,” Yoongi says. “Thank you all for coming today. I hope you have a good day and a wonderful week”
Slowly the people start leaving and so does Yoongi and he bumps into Jung Hoseok who smiles at him.
“I didn’t know you were in charge of the support group too,”
“I was just a replacement for today Mr. Jung,”
“You can just call me Hoseok you know,” he says. “I don’t mind”
“Okay Hoseok,”
He smiles.
“See you on Monday Dr. Min,”
Yoongi nods as he watches Jung Hoseok walk away and he looks until the other man is out of vision before he too walks to his car and gets into his car and today he feels lighter as if he just dropped something off of his shoulder.
H e feels light.
Maybe it’s talking he thinks. He hasn’t told many people about the whole fiasco with his wife. To Seokjin it was just through a lot of ugly tears and everyone else knew but they didn’t bring it up so Yoongi never had to talk about it and now that he did he feels better than he has ever before.
The support group wasn’t nearly anywhere as disastrous as he thought it’d be.
#bangtan#bangtan boys#bts#bts fic#bts fanfic#bts fanfiction#yoonseok#yoongi#hoseok#yoongi x hoseok#seokjin#namjoon#namjin#jimin#jungkook#taehyung#yoonseok fic#yoonseok fanfiction#yoonseok fanfic#yoonseok au#kpop#kpop fanfiction
6 notes
·
View notes
Text
Finally Getting Somewhere!!
So I finally have an idea of what is going on with my body and why in the crap i feel so awful 95% of the time. Despite me being able to hide it and put on a show most of the time (because everything has gradually gotten worse and i have been able to adapt over time), i feel like i have been hit with a truck almost every day. I honestly, could handle this if i had an answer. Even if i knew this was going to be my life forever, i would be able to figure it out without giving up and letting my fatigue take over. I am aware that this is not a possibility for everyone, but i would be able to accept this and do my best for now. I don’t know what the future may hold if this is going to be my forever, but for right now, i refuse to give up. However, i may finally get some answers soon!
I had my first set of hormone labs done on the 25th of may He ordered a prolactin, testoserone, progesterone, and a TSH to be done on day 21 of my cycle. I got the results back the next day. My Prolactin came back at 48.3. It should be around 24 in a healthy normal child bearing age female. My testoserone came back on the lower end of normal but okay, the TSH jumped from 1.7 to 4.2 in less than a month (so that could be a problem, despite it still being within normal), and my progesterone came back at 9. On day 21 it should be at least 15 if you ovulated, however it wasn’t the most concerning lab result, as it was still within normal as well. So basically everything came back on the low end of normal or high.
I was hoping to hear from his office regarding the labs on Friday, but i didn’t. I am able to see my labs online without hearing from the office, which is how i knew the results. I waited through the weekend and nobody was in on Monday due to it being Memorial day here in the States. I patiently waited until Tuesday to call his office for a couple reasons. I had started my period early and i needed to have the next set of labs ordered for day 3 of my cycle and i also wanted to hear about my labs. Much to my dismay, he is out of the office on Tuesdays. I would have to wait until Wednesday to have the labs drawn (which was going to be day 3) and i still wouldn’t hear anything about results until Wednesday either. However, i did receive a call from the radiology department at my hospital. Apparently, they had received an order for a Brain MRI with and without contrast to look for possible pituitary tumors. They didn’t say why this had been ordered, but i had done my own research and figured it was to look for a prolactin producing tumor to see if that is why my level was double what it should be. I scheduled the scan to be done on June 1st at 1 PM. This was the earliest i could have it done and it worked out perfectly actually.
Wednesday finally came and i was able to get a hold of his office. The MA informed me that there were a couple notes on my chart. One talked about possibly needed some thyroid medication while trying to conceive in the future since mine is out of optimal range. The second note was about the high prolactin level. She told me that i would need to have an MRI to look for the tumor and i told her this was already scheduled. I informed her that i needed to have the next set of labs ordered and that i also have a history of pituitary insufficiency (growth hormone) that i had forgotten to mention to him in my appointment. She was surprised by this and i believe she told him as soon as we hung up. She ordered the labs so i could have them done on time. This time they were testing an estrogen (estradiol) level, and a the FSH level.
I got the labs done on wednesday and the MRI done on thursday. The MRI was interesting. I had it done my someone i know well since we work in the same hospital and he has done previous scans on me regarding my back. He was really nice. He got my IV in one stick and i was so tired from working the night before that i think i just slept through the scan. It was with and without contrast and i do remember the contrast making me feel a little weird but other than that it was a nice little nap.
I was at work on friday and i got a call from my dr’s office asking me to call them back to discuss my lab and MRI results. I was able to quickly walk away and return the call. The MA told me that the FSH came back normal but my Estrogen came back really low, mine is less than 25 and in someone my age it should be at least 40-500 (depending on what part of the cycle you are in). Anything less than 40 is considered to be menopausal levels, this was shocking and upsetting. I am 22 years old why the heck are my estrogen levels low enough for me to be in menopause. She said that low estrogen and high prolactin can go hand in hand so it isn’t that surprising. Maybe not to her, but it was quite shocking to me. She then went on to discuss my MRI results. I didn’t have an obvious tumor show up, but the pituitary gland is somewhat enlarged. It is still within normal limits, but it is definitely larger than it should be for someone my age, not pregnant, and healthy. She told me that considering all of this and taking my history into consideration he wants me to see an endocrinologist. This didn’t surprise me. I have honestly been wondering if i should see one for a while now.
I am very grateful that i am finally heading in the right direction. I am extremely grateful for my Gynecologist who spent 30 minutes with me and has done so much more to help me than my primary care has done in 5+ visits in 2 years. I am so frustrated with him right now as all of my issues could have already been taken care of and under treatment if he would have just listened. I am trying to be patient and understanding. But this is above and beyond my level of giving people the benefit of the doubt. He was so quick to say it was depression, up my meds, put me in therapy and call it a day. Don’t get me wrong, i do think those helped the depression part, but clearly there is more to the story. I am so grateful and appreciative of this dr who seems to really care and want what is best for me despite it being confusing and possibly frustrating for him, i think he realizes it is even worse for me. His office sent out referrals to endocrinologists in the area, we don’t have any in my town, i will have to travel a little ways to find one. I should hear back this next week and get an appointment scheduled.
It is so refreshing to know that there is something more to this. I am not just lazy, i am not just depressed. There is something physiologically wrong and i am truly hoping for answers. I think this is the right direction, i am excited to finally be believed and listened to. I love my new dr. He has done so much for me and he has only seen me once. It is definitely refreshing. I was supposed to follow up with my primary care based on my lab results back in April and i haven’t made that appointment yet. I don’t know what to say. I have a feeling he doesn’t feel the need to see me for a year based on those results. But, based on recent evens i am hoping his mind would be changed. Anyway, i am exhausted and i am going to bed. I am glad i finally have a direction though.
#chronically parfect#chronic fatigue#i am not crazy#this isn't in my head#something is wrong#getting answers#i won't give up#my pcp is dumb right now#frustrated#feel so sick#exhausted#chronic pain#bilateral spondylolysis#depression
1 note
·
View note
Text
February 28th, 2015
Michael woke up feeling nauseous and vomited bile. We waited a few hours – then he tried an Ensure and some applesauce. Those came back up so off we went to the ER for dehydration and anorexia evaluations. Neither was found and his blood work was all within normal limits except one liver enzyme which is still recovering. He is still taking oral pain meds-are they the source of the nausea?
We roll into early March, getting ready for the next scans. There are times when the pain abates and Michael experiences occasional hunger which we try to maximize, stuffing food into him to in an attempt to keep him as strong as possible for whatever lies ahead. On these good days, we go out for a meal or try to see a movie. During one of these rare forays into regular life, a romantic song from our very beginning pops up in the film. We both get chills and squeeze each other’s hands tightly, as for a moment, we drift back to that exquisitely innocent time. Meanwhile, our oncologist Dr. Luyun, has decided to have M try a fentanyl patch for pain. Michael is ready to try anything at this point. He experiences immediate relief and feels great for a day or so, but the pain returns fast. We received little information about how long it takes for the drug to build up in the bloodstream so we didn’t realize that he’d need supplemental oral meds until it did. We are so overwrought and frustrated. When he’s hurting and tired, I am as well. He’s tired of reminders about food and drink and I’m tired of feeling impotent. Our personality differences serve us poorly during these stressful times. When I get quiet, to stop being a bother, Michael doesn’t like that personality either. Finding a balance is hard as I am imperfect and certainly not saintly. Neither is he. At night, I lie in our bed, feeling him twitch and have tremors. We never sleep apart – there’s no room for that distance even if we’re both irritable.
March 9th, 2015
I lay here, wondering what the scan results will show, where the cancer is now, if it’s hitting his spinal cord, whether he will have permanent damage, become a quadriplegic, lose control over bladder and bowels. I want to know everything and nothing and I want both to hurry up.
By mid-March, we have scan results that show that the cancer spots are all growing but still reveal no clues about the cause of the intensity of Michael’s pain. We asked for a referral to orthopedics where there’s a very smart doctor out of Harvard. After checking all the scans, he recommends MRIs for the lumbar spine and both hips. He thinks those will provide the best diagnosis which can’t come soon enough. I’m still writing to principal investigators running Merkel cell trials across the country. The idea that you can get into a trial easily is completely false. The bureaucratic aspects are truly maddening, especially when there’s blatant evidence of a terminal disease. If a person is going to die anyway, why not let him have a chance? But that thinking is for another time.
The MRI results are terrible. The cancerous lesion that has been sitting in the disk at T-12 for months has permeated the disk wall and is compressing the lumbar spine. All the nerves in the cauda equina, the nerve bundle in the thoracic spine are being squeezed. Big pain. We are now in a medical emergency and in need of a neurosurgeon. Our radiation oncologist tells us that the disk has to be removed and that an artificial one must be inserted in its place. This would be a lengthy, complex operation. We quickly acquire an appointment with the most experienced neurosurgeon at our facility. He reviews all the MRI images and informs us that in his opinion, this compression is not a medical emergency and that we should return to oncology for radiation and chemo. We sit dumbfounded. There’s no time to go hunting for a different doctor. We realize that his pronouncement is code for either 1) his not being able to perform the procedure, or 2) that there isn’t any point in trying. We head back to Dr. Stanic, our radiation oncologist, who takes a deep breath and designs a radiation plan for the lower thoracic and upper lumbar spine which he warns carries the risk of paralysis. The treatment will be coupled with the chemo drug Topotecan, the second line of defense for MCC. Michael and I are both terrified but he continues to be willing to do whatever what might possibly keep him alive. For me, I bounce between admiration and despair. The appointments are scheduled.
The beginning of April starts with the first of 15 daily rounds of radiation. The chemo will be given once a week. This beautiful spring month will be consumed by treatment. When Michael isn’t too fatigued, we decide we’ll just enjoy spending time with our family. Our world has gotten very small. Michael is inner directed and focused on trying to stay alive. I’m committed to helping him in any way I can. The stress is punishing. On April 6th, the fourth day of radiation, we are entering the Cancer Center when I receive a phone call from one of my nieces, letting me know that my brother was found dead that morning by his wife. The cause was determined to be congestive heart failure. He was a troubled guy and in the previous few months, I’d been so consumed by Michael’s cancer that we’d barely spoken. There was nothing to do but go forward, sitting in the waiting room during the radiation appointment, contemplating life and death and everything in between. My goodbyes to Fred would have to play out as I kept plowing through what was in front of me. No more big brother. The days went by, blending into each other. Every time there was a chemo treatment, Michael would have blood drawn to see if his counts were stable enough to cope with the infusion. When the time for the third one came, his platelet count was so low he was at risk for a stroke. The chemo was withheld and instead he had a platelet infusion. Then he started a course of steroids to try preventing any potential bleeding in the brain. Another stunning blow. April is ending.
We head into May, trying to achieve some stability, physically and psychologically. There are days when Michael feels okay – we head outside to appreciate the weather and the garden. Throughout his entire ordeal we have managed to stay intimate. On May 6th, during the process of running my hands over his familiar body, I find a lump in a new spot near his spine. The next day, I call our oncologist to request a scan and find out that he’s resigned from the clinic. We are now without an oncologist – every original member of Michael’s treatment team is now gone. We go back to Dr. Stanic who quickly orders the scans for the next day. The results show stable disease. I can’t understand it. I remember that PET/CT scans don’t show any masses smaller than a centimeter. Now it is May 11th. Our May 1st wedding anniversary kind of slipped away. After running an errand, I came home and found flowers, anniversary cards and Mother’s Day cards from Michael which make me weep. May 18th. Michael seems to be getting weaker. His appetite is poor and he is deconditioned. Sleeping a lot and getting breathless just walking through the house. I’m reading books for widows. I don’t find them very enlightening. Michael talks about death with dignity, although he says he feels stable. He doesn’t look stable. He is weak but trying to act normal.
What is happening inside me? I feel like pieces of who I am slough off every day. Like silt.
May 24th, 2015
I am lying in my bed on the morning of my 64th birthday. Michael’s hand is on my leg and I’m listening to him breathe. I fear this is the last birthday he’ll be next to me. Forty three birthdays shared. This one feels meaningless. There is a lump on his neck at the base of his skull. Last night I felt one in his left groin. Scan or no scan. These lumps are real. I am walking through this life, feeling mostly dread. My hope is dwindling. I have used myself up.
May 29th, 2015
This morning I found 3 pea-sized lumps on Michael’s head, very close to the site of the excision of his tumor on February 25th. The lump at the back of his neck is a tumor. I just know it. On Monday there will be biopsies of his head. This time, the surgeon is too busy to see him and a physician’s assistant will do the cutting. We know it’s Merkel cell. We’re only going to let him biopsy one growth. Then we’ll finally have the soft tissue requirement that kept him out of the Barnes clinical trial. We are still hanging on, albeit by the proverbial thread. We meet with a palliative care team on Tuesday to see if they can help keep Michael comfortable, both physically and mentally as this all unfolds. So much darkness while we fumble forward.
June 2nd, 2015
I am visiting mom at the nursing home. She has about run out of money and I am trying to get her Medicaid in the midst of my nightmare. She always remembers that Michael is sick. She asks me, “if Michael dies, do you think we should try living together?” I remind her that we already did that. In the midst of her dementia and my grief, we both laugh.
June 5th, 2015
Michael is getting weaker and less hungry. Today is his birthday. We spend a lot of it crying. Michael’s emotional pain is finally bursting out of him. He says he’s never lost anyone before, that the first person he’s losing is himself. The kids come over and we all sit in the yard for awhile. We all act just like ourselves which is both bad and good. The weight of what’s ahead of us is like a massive tsunami getting ready to wash us all away.
June 8th, 2015
SCAN DAY.
June 16th, 2015
The week has been madness. The scan of the 8th showed widespread disease including a pleural effusion which is one of the reasons Michael’s breathing is so labored. Dr. Stanic soberly tells us that malignant infusions are virtually impossible to get rid of so that we should be prepared. Lumps are pushing out everywhere, neck, collarbone, both rib cages. I have no idea how Michael is still breathing. We now have a new oncologist, Dr. Zhang, who we’d seen a few times when Dr. Luyun was unavailable. He is smart and aggressive. We go to see him the day after the scan. Michael is so weak he’s in a wheelchair, but eventually has to lie on a bed in the infusion suite for his appointment. Miraculously his recovered platelets, plus the soft tissue disease finally qualify him for the trial at Barnes. Dr. Zhang goes to call those awful people in St. Louis to clear a path for us. Now all we have to do is gather up all the records, forward the scans and move into the trial. At last. Michael is resting at home while I run around gathering all the information. Again, I’m communicating with Dr. Linette and his nurse. A few days pass and there is no action from Barnes. When I call in again, I’m told that Michael isn’t in the trial, but rather that we have to come back so they can do their own scans. I am enraged and feel like I’m going to have a breakdown. I vow that when this ends, I will eviscerate Dr. Linette and his harsh nurse Joanne. Meanwhile we are to see Dr. Zhang tomorrow.
June 17th, 2015
Dr. Zhang is infuriated to hear that we are not in the trial. He asks us to sit and wait for awhile. When he returns, he tells us that he has managed to order pembrolizumab (Keytruda) off-trial for Michael and that he will receive an infusion immediately. This drug is in the same immunological family as the trial drug at Barnes and has been used for melanoma patients. This is an outside the box move. We are grateful for anything as we get ready to leap into this unknown, untried space. Unless this drug is a miracle, we have to face Michael’s death. Can we find a way to walk this path without crashing into a thousand pieces? Michael has suffered agonies. I am as close to him as anyone can get to another human being. Off to the infusion suite.
June 20th, 2015
I am lying in bed with Michael while I still can. The days are the same. I wake thinking of his death and the horror it will bring. I go away to the park in the morning and cry. Then I run errands and on good days, I swim for awhile. Then I go home and wait for him to come downstairs so we can begin the endless battle over food and protein. He sleeps a lot. We are next to each other, often in silence.
June 18th, 2015
Although it seems crazy, the day after the Keytruda infusion, the visible tumors on Michael’s body seem inflamed. The immunological drugs are supposed to remove blockades from the body’s killer immune cells, releasing them to kill your cancer. This sudden release produces an inflammatory response. Michael’s fatigue is profound. But I decide to start measuring what I can see to track the potential progress. Within two weeks, the tumors which initially looked worse, are visibly shrinking.
Michael is dragging himself through this process. Even though his style is so different than mine, I am awed by his stubborn courage. The Keytruda has impacted his pleural effusion. Twice in July, he has had to be “tapped,” to have fluid drawn from between his lungs and body wall. This is done by inserting a needle into his back. Dr. Zhang doesn’t want to chance having any tubing inserted permanently to stave off the risk of infection. The first tapping fills a 2 and a half liter container. The fluid is blood-red and is 100% Merkel cell lymph fluid. The second tapping fills 3 liters – as I look at it, I think half of it looks more amber colored than red. It appears the drug may be having a positive effect. July 12th, 2015
Mom has fallen in the middle of the night at the nursing home and has broken her hip. I run to the hospital where she tells me that she doesn’t think she can “make it through this one.” I an worried about surgery for her but the orthopedic surgeon says the pain without intervention would be intolerable. What he doesn’t talk about is the hospital delirium that accompanies dementia patients after general anesthetics. Mom survives the procedure but is in a dreadful mental state in addition to having post-surgical pain. For eight days, I run back and forth between her and Michael – finally I request hospice for her and a return to the nursing home before she forgets it altogether. I have to fight for hospice but she actually recognizes my conflict with the staff and supports me. Four days after she’d been returned to the home, I receive a call from a staff member saying that she’s asking for me, just as I’m walking Michael into the cancer center. My daughter swaps places with me. My sister joins us on that July 24th afternoon and we sit with our mother, watching her slip away.
She died on July 25th. We had a rapid funeral with those of her family who lived in town. The heat was blistering and I was terrified that Michael would keel over at the cemetery.
Four days later, our beautiful dog Flash, who’d developed a cough, had me very worried. I took him to the vet and asked her to diagnose him before I left. I didn’t think I could stand to bring him back there again. Bloodwork showed nothing but then she X-rayed his chest. Poor Flash had lung cancer and a pleural effusion, just like Michael’s. I held him as he was euthanized, went home and sobbed with the whole family. What an impossible time.August, 2015
Michael was still fatigued but slowly improving. The physical part was challenging but so was the mental exhaustion. I was utterly spent too, but continued to push forward. Day by day, he began to recover in teeny increments. We went out to eat. He worked in the yard. We tried a staycation at a hotel where he sat bundled up and wasted, but was grimly happy to be out of our house. We went to a rock concert at our local sweetcorn festival.
September, 2015
Scan month. Living between scans may be the hardest challenges we faced those many months. As time went by we got smarter about them, scheduling the follow up appointment for the day after the scan so we wouldn’t have too much time to worry. The early September scan was no exception – we went in for it one morning and by the next were getting the results. Which were spectacular. Between June and September, 80% of Michael’s cancer had vanished, including the pleural effusion. Dr. Zhang brought a colleague in to see the results as he was so excited he was barely contained. Michael was one of the exceptional responders to this new class of drugs, one of the 30-40 % whose bodies were just waiting for help in unleashing their cancer-killing cells. We were thrilled but still cautious. Every three weeks, there would be more treatment, more blood tests. But Michael was almost over the precipice and now, was back in his life. And mine.
Cancer Drops the Hammer – Part 2 – Chapter 10 – Be 278 February 28th, 2015 Michael woke up feeling nauseous and vomited bile. We waited a few hours - then he tried an Ensure and some applesauce.
0 notes
Link
October 01, 2019 at 07:00AM
How can you have a moonshot trying to cure cancer and not mention people dying of cancer?I believed the narrative that is pushed on women, that if you check your breasts and if you catch it early, you’re fine.ide class="right-rail__container right-rail__container--ad">
Lianne Kraemer had been living with metastatic breast cancer for more than a year when I met her in December 2017 at the Henry B. González Convention Center in San Antonio. Throughout the week, more than 7,000 doctors, scientists and pharmaceutical-company representatives would descend on the city for the country’s most important breast-cancer conference. Inside the main exhibition hall, it seemed that every major pharmaceutical company was putting on its best come-hither show. A pair of young, lithe dancers whipped flowing fabric through the air at a booth for the drug Faslodex, a new injectable from Astra-Zeneca used to treat women with estrogen-fueled advanced breast cancer. Novartis had free cupcakes. Tesaro, a company developing new drugs for BRCA-linked breast cancer, had Nutella-branded ice cream cones. Espresso was available at Eli Lilly, and Pfizer had put out small cups of frozen yogurt. Medtronic, a medical-device company, had breasts of raw chicken at its booth so surgeons could test the PlasmaBlade, its new soft-tissue-dissection knife.
Although I had worked as a health-care journalist for nearly a decade, I had never attended this particular conference. I was there to report on the latest scientific advances in breast cancer, but I was also an interested party. Three years earlier, at the age of 35, I had been diagnosed with breast cancer and begun what would be more than a year of treatment. My cancer responded well to the chemotherapy and targeted drug therapy my doctors prescribed, and I was, according to the evidence, cancer-free. I was grateful, but I wanted to learn more about women with metastatic disease whose breast cancer had managed to carry on despite treatment and spread to other parts of their bodies.
Kraemer, a smiling, energetic woman with dark brown hair and eyes, sat at a table in the back of the hall. There was no complimentary coffee or ice cream, just brochures stacked in neat rows and a small sign that said METAVIVOR. Founded in 2009, METAvivor is a nonprofit organization run by and advocating for metastatic-breast-cancer patients. In recent years, the group and others like it have tried to turn public attention—often focused on feel-good “survivor” stories—to the more than 160,000 women in America living with metastatic breast cancer. Having a presence at major conferences is part of a strategy to increase research funding for metastatic disease and raise awareness that for all the strides made in treatment, some 40,000 American women still die from breast cancer every year.
Despite the billions of dollars collected and spent on breast-cancer research over the past half-century, relatively little has been devoted to studying metastatic-breast-cancer patients or their particular forms of the disease. Doctors do not know why some breast cancers eventually form deadly metastases or how to quash the disease once it has spread. Patients with metastatic disease are typically treated with one drug after another, their doctors switching the medications whenever the disease stops responding to treatment. Eventually, nearly all patients with breast-cancer metastases run out of options and die, although in recent years, many have been living longer. Of the four metastatic-breast-cancer patients who founded METAvivor in 2009, three have died, but one is still alive, 13 years after discovering that her disease had spread.
Diagnosed with estrogen-receptor-positive breast cancer in January 2014 at the age of 37, Kraemer had a double mastectomy, chemotherapy, lymph-node removal, radiation and hormone treatment. She emerged from the yearlong ordeal relieved she had acted quickly—she’d felt a lump in her breast and was diagnosed the next month. Then, in June 2016, Kraemer was doing laundry when she felt a tingling in the right side of her lips. The next day, the right side of her gums and tongue started to feel weird too. “During that day, the crease on my right index finger felt like someone had put a slight rubber band around it,” Kraemer told me.
Kraemer emailed her oncologist, who recommended she get a brain MRI, and she asked her uncle, a neurologist, to review the scan. When he broke the news that it looked as if her breast cancer had spread and formed about a dozen small tumors inside her brain, she was stunned.
Three-quarters of women with metastatic breast cancer were originally diagnosed with early-stage disease. The idea that the breast cancer “came back” after initial treatment is a bit misleading. Women who undergo traditional chemotherapy shortly after an early-stage diagnosis, as I did, do so because their doctors believe they may have micrometastases—cancer growths outside the breast that are too small to appear on scans. Breast cancer that is treated and later metastasizes into larger tumors around the body somehow managed to survive the initial treatment. Women who declare themselves cancer-free have no way of knowing if they really are. Sometimes breast cancer continues to grow during treatment. Other times, breast-cancer cells remain alive and go dormant but then begin multiplying years or even decades later.
Often, though not always, newly diagnosed breast-cancer patients get abdominal scans, but they almost never have brain scans unless a symptom appears. (About a year after I finished treatment, I had a debilitating two-day headache and my oncologist recommended I get a brain MRI, which turned up nothing. I was diagnosed with a migraine.) Even if Kraemer had had a brain scan when she was diagnosed, it’s possible the tumors inside her skull were so small that they would have been invisible on an MRI.
When we first spoke by phone a few months after we met in San Antonio, it was clear that Kraemer had thought through every possible diagnostic scenario. Could her doctors have done more? Did the month that passed between the time she found a lump in her breast and her diagnosis make a difference? Kraemer had complications with her double mastectomy that delayed the start of her chemotherapy. Did this give the cancer time to spread to her brain? She will never know, but she believes that most likely, her metastatic breast cancer could not have been prevented.
“You can do everything right and still end up metastatic,” Kraemer said. “I just assumed that could never be me because I would catch it early, because I was on top of things. I believed the narrative that is pushed on women, that if you check your breasts and if you catch it early, you’re fine. That surely the women who are not O.K. must not have gotten good treatment or must not have caught it when they should have. I believed what I was told.”
Existing breast-cancer-treatment protocols fail in tens of thousands of women like Lianne Kraemer every year. In some cases, breast-cancer patients don’t have access to high-quality treatment or they ignore signs of the disease until it’s incurable. But more women who die of breast cancer succumb to the disease for no other reason than that it manages to outwit the protocols.
Pharmaceutical companies and researchers often test new drugs on metastatic patients before anyone else. These are women who are dying anyway, and they are the ones most willing to be part of experiments. But the goal for most drug development is to treat early-stage patients successfully and eradicate breast cancer before it spreads.
According to Cyrus Ghajar, a cancer biologist at the Fred Hutchinson Cancer Research Center in Seattle, 25% to 40% of early-stage breast-cancer patients already have cancer cells in their bone marrow, and these patients are, on average, three times more likely than those who don’t to develop other metastases later. It’s impossible to know if a patient has cancer cells in her bone marrow without driving a long needle into a large bone and aspirating marrow from inside. Ghajar, one of a relatively small number of scientists studying metastatic breast cancer full time, said that, in theory, patients could give consent to have their marrow drawn when they are placed under general anesthesia for lumpectomies or mastectomies. The results could tell doctors which women were more likely to face a recurrence of their breast cancer and therefore might need more treatment up front. “We don’t have a way to further stratify people, because we haven’t studied it enough,” Ghajar told me. “We don’t have enough samples.”
Ghajar pointed out that the Cancer Moonshot, a National Cancer Institute initiative launched by President Barack Obama and Vice President Joe Biden, does not explicitly provide funding to address the challenges of metastatic cancer. “How can you have a moonshot trying to cure cancer and not mention people dying of cancer?” he said.
Alana Welm, a molecular biologist, runs a lab at the University of Utah’s Huntsman Cancer Institute devoted to studying breast-cancer metastases. One of her research projects compares breast–cancer cells from a patient’s original tumor against cancer cells found elsewhere in the body after the disease spreads. The idea is to determine the differences between the cells to find clues about why some migrated and how they may then be affected by microenvironments inside the body. “Think about how hard this research is,” Welm said. By the time a woman is diagnosed with metastatic disease, her original biopsy tissue may no longer be available. In addition, it’s often hard to get a sample of a metastatic tumor, which may be buried inside the brain or located in a place that is difficult to access safely, as opposed to the readily available breast tissue that gets biopsied in early-stage patients. “I sometimes wait for years in between to try to get these samples,” Welm said. Welm and other researchers encourage metastatic–breast-cancer patients to consider making plans to have an autopsy done immediately after they die so that cells can be harvested, preserved and studied before they degrade.
After I finished my treatment for early-stage disease in February 2016, I did not celebrate. I did not feel cured. I felt scared. Although it is unlikely, my disease could recur. Some researchers estimate that breast cancer recurs in 20% to 30% of patients either locally or elsewhere in the body, but the odds vary significantly depending on the specific type of the disease a woman has and her treatment outcome. I was unnerved when I learned that I would not get even annual scans to look for signs of metastases. Studies published in the 1990s showed that detecting metastases through scheduled scans, rather than when a symptom appears, did not change survival rates, prognosis or quality of life. Scanning every breast-cancer patient post–treatment would be expensive and would undoubtedly lead to unnecessary medical intervention.
But imaging has gotten much better since the 1990s, with MRI, positron–emission tomography (PET) and CT scans able to detect tumors as small as a few millimeters. A 2017 study by researchers at the National Cancer Institute found that some 11% of women under 65 diagnosed with metastatic breast cancer live for 10 years or more. The year prior, George Sledge, chief of oncology at Stanford, had published a paper in the Journal of Oncology Practice called “Curing Metastatic Breast Cancer.” In it, he suggested that the existing paradigm around metastatic breast cancer—that it is incurable and not worth looking for—should be updated in the face of new science. “If some patients are cured,” he wrote, “might not we cure more?”
About a month after her diagnosis of metastatic breast cancer, Kraemer was going through her belongings, hoping to save her parents the agony of discarding her possessions after she died, when her hands settled on a photograph. It was a picture of a smiling couple: Kraemer and an ex–boyfriend, a Nebraska native named Eric Marintzer. After he had unceremoniously dumped her more than a decade earlier, Kraemer had thrown out every physical reminder of him. He had given her a waffle iron as a gift, and she had smashed it to bits in an alley. But somehow, this photograph had survived the reckoning.
Like any modern woman, Kraemer picked up her iPhone and found Marintzer’s Instagram profile. She scrolled through images, her thumb moving so quickly that she accidentally “liked” one. Panicked, she threw her phone across the room so hard that the screen shattered. Then she decided to come clean. She had just been diagnosed with a terminal disease. What did she have to lose?
Kraemer sent Marintzer a message, saying she had seen his photographs and accidentally “liked” one. To her surprise, he wrote back. They started texting, and eventually he asked her out for drinks. She was living in St. Louis but often traveled to Chicago, where Marintzer lived. Whenever she went, they got together. It was refreshing to be with someone who didn’t know about her disease. “Everybody in my life was treating me with kid gloves,” Kraemer said.
After spending New Year’s Eve together, they talked about whether they should officially be a couple again. “There’s something you need to know,” Kraemer said. Marintzer listened and then said her metastatic breast cancer was no reason to change their plans. Before long, she moved into his condo and they picked up where they had left off.
Women who have breast cancer that has spread to the brain often die within a year or two of the diagnosis. To shrink the tumors inside Kraemer’s brain, one oncologist recommended she undergo what’s known as “whole brain radiation,” an extreme but common procedure for patients with multiple brain tumors. Such treatment can cause debilitating fatigue and permanent cognitive damage. Kraemer instead enrolled in a clinical trial to test whether a relatively new drug called Verzenio could beat back brain tumors in women with estrogen-receptor-positive metastatic breast cancer. Kraemer went on the drug, and most of her tumors stayed the same size for eight months, a good sign. The largest even shrank. The drug also kicked Kraemer into chemical menopause, which her oncologist thought might help cut off the supply of estrogen her type of breast cancer was feeding on.
But the drug had side effects, including chronic diarrhea that required Kraemer to get IV fluids to prevent dehydration. Her oncologist decreased the dose of the trial drug, which stopped the diarrhea but also the menopause. Soon her tumors began growing again. The clinical–trial protocol dictated that Kraemer had to stop taking Verzenio—if her cancer was growing, the drug was not working. But a new oncologist had a different take. Nancy Lin, a metastatic specialist at the Dana-Farber Cancer Institute in Boston, speculated that the drug actually was working and that the estrogen produced by Kraemer’s ovaries was canceling out its effects. The problem was that the clinical-trial rules did not allow patients to start hormone therapy in the middle of the study. “I said, ‘I don’t care what I have to sell or do, someone’s going to get me that damn drug back,’” Kraemer told me. Lin lobbied the drugmaker Eli Lilly to allow Kraemer to have Verzenio and begin hormone therapy. Miraculously the company agreed to sponsor a new trial with just one patient, Kraemer.
The treatment kept Kraemer’s brain tumors stable for six months. But in January 2018, a scan showed they were growing. Still worried about the cognitive side effects of whole brain radiation, Kraemer began specialized radiation treatment that would hit only her largest tumor. Her brain tumors remained stable for a few months, but eventually they started growing again. Kraemer enrolled in yet another clinical trial, this one testing whether a drug that has been shown to work against certain types of liver and kidney cancer might help women with metastatic breast cancer.
In September 2018, I flew to Chicago to see Kraemer. I met her and Marintzer for breakfast the day after I arrived and couldn’t help thinking they looked entirely, astonishingly normal, their predicament hidden inside a relationship they were trying hard not to define by the fact that Kraemer was battling a disease that would most likely cut her life short.
Later that day, I asked Kraemer how her disease affects her everyday life. She said her largest tumor in her brain had begun to impede her ability to use her right hand. She could no longer hold chopsticks or write legibly. She also had frequent migraines and once burned herself on a hot pan because she couldn’t feel that her hand was on it. She said ever since her targeted brain radiation, she had had trouble multitasking and struggled to have a conversation if music was playing in the background. I asked if she felt like she was dying. “Yes and no,” she said. She had a loving boyfriend, a tight-knit family and a good life, but her symptoms were getting worse. “I am in a decline,” she said.
Kraemer babysat in high school, worked as a nanny in college and chose a career as a speech pathologist for kids. “All I wanted to do was be a mother,” she told me. After her early-stage diagnosis, Kraemer froze eggs harvested from her ovaries, and every three months, she pays to keep them in storage. “I know I’m not going to use them, but I can’t stop paying for them and just throw them away,” she said.
In December 2017, Kraemer had told me that the upcoming Christmas holiday would probably be her last. But in December 2018, she and Marintzer went shopping for a Christmas tree and picked out the biggest one they could find. It was so large, they had to move most of their furniture out of their living room. “We know that the number of Christmases Lianne has are limited,” Marintzer told me. “Let’s do it up.”
A scan in January 2019 showed that several of Kraemer’s tumors were growing again. In the months since, she has been treated with multiple types of chemotherapy and more specialized radiation. But her symptoms are becoming more pronounced. Kraemer’s right hand and arm are now mostly useless, along with her right arm. Her right foot and leg are also not working properly, and she walks with a noticeable limp. She is weighing whether to allow a neurosurgeon to try to excise the largest tumor inside her brain. The surgery would be risky, so Kraemer and Marintzer decided to take one more big vacation. In August, they traveled to the Greek islands and stayed on the cliffs of Santorini.
“All things considered, I’m really lucky,” Kraemer, now 43, told me recently. It has been more than three years since she was diagnosed with metastatic breast cancer in her brain. She has survived longer than most women like her, thanks to new drugs, clinical trials and creative thinking by her doctors. Kraemer is proof that research and science can change the fates of metastatic-breast-cancer patients. We just need more of it.
Excerpted with permission from Radical: The Science, Culture, and History of Breast Cancer in America, by Kate Pickert. Copyright © 2019 by Kate Pickert.
0 notes
Text
The Road to PRRT: A Path of Self-Discovery and Growth
By Josie Rubio, NET Blogger, A Pain in the Neck
Sitting on a yoga mat in a Brooklyn park, looking across at the Manhattan skyline, I recently found myself taking stock of how much had changed in just a month and a half. In mid-May, I’d just been released from the hospital for the fourth time this year, after a blood infection. Since severe NET-induced diarrhea had persisted since January, I had been doing daily IV hydration at home almost four hours a day. It was hard to imagine then a life in which my guts weren’t constantly roiling or when I didn’t have to wear diapers to bed.
An Unlucky History of Cancer
I’ve had two separate, unrelated cancers within the past five years: first, refractory Hodgkin’s lymphoma and the neuroendocrine tumors. Occasionally I buy a lottery ticket to see if my luck goes the other way. I’m always genuinely surprised when I don’t win.
I had previously had a Whipple procedure for my NET tumors in early 2016, followed by a liver ablation. Almost exactly a year ago, I received the news that the ablation was successful and the cancer was unlikely to come back. The next day, my oncologist delivered the news that they had missed seeing a new tumor in my pancreas. I would always have this cancer, which would be treated more like a chronic disease.
My tumors are pretty aggressive. Despite relatively good health up through December, I had severe diarrhea and could barely keep food down by New Year’s. My potassium dropped so low that I was rushed to the hospital. I spent most of January at Memorial Sloan-Kettering Cancer Center. I received radiation for the second time; the first was in 2014 for the lymphoma, during a month-long stay at Sloan-Kettering that also included an autologous stem cell transplant.
The radiation helped a little bit. I received several additional radiation tattoos—small dots to help line me up in the machine—so I now have a grand total of 15—14 radiation dots and one small Libra symbol I got when I was 20. “You’re like Tommy Lee now,” a friend noted about my rock star number of tattoos. However, I stopped improving a few weeks after the radiation, and I still was significantly sick with diarrhea.
When dacarbazine chemotherapy didn’t help and I ended up in the hospital for a blood infection in March, I had an embolization for a liver tumor. That also didn’t help curb the diarrhea caused by the VIPoma tumors. Finally, a few rounds of carboplatin and etoposide helped slow the diarrhea a little bit but I was so sick immediately following the chemo, I ended up in the hospital again because of a second blood infection.
Getting PRRT is good news
At every appointment with my oncologist, I would ask about the peptide receptor radionuclide therapy (PRRT) treatment called Lutathera®, which had been approved by the FDA in January.
In June, I was the first patient who wasn’t part of a clinical trial at Memorial Sloan-Kettering Cancer Center to receive PRRT to treat the neuroendocrine tumors in my pancreas.
It wasn’t available immediately as hospitals sorted out the logistics, from health insurance to training for administering the treatment. At an appointment in May I asked and received the familiar answer, so I was pleasantly surprised the following day when I got a call scheduling a meeting with the doctor who would administer the PRRT.
In June, I was the first patient who wasn’t part of a clinical trial at Memorial Sloan-Kettering Cancer Center to receive PRRT to treat the neuroendocrine tumors in my pancreas.
Though PRRT is new in the U.S., there’s quite a bit of data on it since it’s been available elsewhere, particularly in Europe, for so long. My VIP-producing tumor, however, is very rare, so there’s less information. However, when it works, it shrinks the tumors and keeps them at bay enough to relieve the symptoms. From what I have learned, a person may experience relief for an average of three years, though I fear I will be the exception. According to the tests that measure Ki-67 markers, my tumors are very aggressive. What would I have? …The guess is something closer to six months.
The doctor explained how the targeted radionuclide therapy works: essentially like a Trojan horse. My bloodstream wheels the Lutathera Trojan horse to the NET tumor’s receptors—the enemy gates, which accept the gift of the octreotide, a synthetic hormone I also inject subcutaneously several times a day. A chelator, however, has bonded a radionucleotide to the octreotide, so once the bind has occurred, the radioactive atom emerges and destroys the unsuspecting tumor cells.
The doctor warned that, like chemotherapy, the diarrhea could become significantly worse as the cells were destroyed, temporarily increasing the release of VIPoma into my bloodstream. In addition to the Lutathera, I would also be given anti-nausea medication and a corticosteroid to combat other possible side effects, as well as four hours of intravenous amino acids to protect my kidneys from the radioactivity.
“I’m absolutely glowing”
…Oh, I would also be radioactive. I’d received radiation and had various scans over the years that made me radioactive, with the cards to carry around in case I was stopped or scanned at an airport or checkpoint and tested positive for radioactivity. But this seemed like it would be on a whole new level, the kind that might make me glow in the dark.
I would have to avoid babies and pregnant women for about 10 days instead of just one, but I would also have to keep people at an arm’s length for at least a day. My sheets and clothing that I wore for the first five days post-treatment would have to be washed separately. I was told repeatedly not to pee in the shower, something I don’t do anyway; however, I’d have to be careful about my bathroom habits since most of the radioactivity would be flushed out in urine.
That night, a mosquito found its way into the guest bedroom and buzzed around my face. “Serious question: If a mosquito bites me while I am radioactive, will it die or turn into a superhero mutant?
I arrived at the nuclear medicine department on the appointed morning exhausted. The doctors and nurses looked at my PICC line and started a peripheral IV as well and asked me questions as they explained the long- and short-term side effects.
It’s strange to be a toxic creature. There were so many precautions. People wore little booties over their shoes. They woke me up long enough to bring me to a scan, which showed good uptake of the Lutathera in the pancreas. I celebrated by resuming my nap until about 5 pm, when I was cleared to go.
A friend picked me up after treatment and took me to her apartment with an extra bedroom made up for me. “Should I put you on a blanket?” my friend asked. She put down a sheet on one end of the couch and watched TV with me from the other end of the room. We ordered takeout using the Seamless gift card former coworkers chipped in to buy me, and I used plastic silverware and my own cup.
That night, a mosquito found its way into the guest bedroom and buzzed around my face. “Serious question: If a mosquito bites me while I am radioactive, will it die or turn into a superhero mutant? Should I phone the on-call oncologist?” I asked on social media.
Friends kept asking if I would develop superpowers.
I worked remotely for a few days and stayed in my semi-isolation. I was feeling sorry for myself and crying radioactive tears when I realized my diarrhea hadn’t worsened. In fact, I had solid stools again. I took my Zofran® and didn’t experience nausea and ate all of the best types of the small chocolate bars from the mix my friends had out.
Alone with my cancer?
Going to a friend’s house following PRRT was new to me. When they asked if I had somebody at home, I started to cry—full-body-wracking sobs. I couldn’t sleep next to someone for five days after treatment. That wouldn’t be a problem. My boyfriend of 12 years and I had just parted ways. He says we were headed that way anyway. After I overheard a conversation in which he talked about how much he enjoyed reconnecting with a recently divorced friend during a business trip, and how nice it was to walk around London by himself not thinking about cancer, I knew a break up was the right thing to do, even if I felt like he was doing it for the wrong reasons. He said he’d been with me since I’d become really ill in January only out of a sense of obligation. He said he was tired of dealing with cancer for five years and deserved a vacation to Europe that he’d booked without me.
He was tired of dealing with cancer. I thought I’d dealt with it pretty well, considering, but he made me feel really bad, like I’d been a burden destroying his life. During those months I was so sick, I had actually hoped for a quick death, in part because I felt so bad for him. I had wanted him to move on, but I’d expected to be dead first.
I felt like I’d deeply disappointed everyone. Teams of doctors at a top cancer center have been helping me fight for my life for more than five years, and I was unraveling. I felt alone and abandoned despite so much support from family and friends.
Though I was staying with my friends, I had to return to my own place several times for things I’d forgotten like syringes and, inexplicably, shirts. (I made sure my ex wasn’t there, because I didn’t want to see him: he needed to stay at our apartment that week so he could pack for his upcoming move.) At one point, I found myself in the bathroom staring at his toothbrush, contemplating the satisfaction I would have at placing it in my radioactive mouth. (I didn’t, of course.)
Finding the will to fight
The break up happened in late May; I was a little in shock. I hadn’t been eating well or sleeping much for weeks. When the doctor asked me about my medications, I admitted hadn’t been taking them as regularly as I was supposed to. I felt like I’d deeply disappointed everyone. Teams of doctors at a top cancer center have been helping me fight for my life for more than five years, and I was unraveling. I felt alone and abandoned despite so much support from family and friends. It’s so easy to focus on what you don’t have.
What I did have that morning was a team of doctors and nurses, as well as a radiation specialist, prepping me for PRRT. I was introduced to two other doctors who would be observing, one of whom was from the PRRT Treatment Center in Rotterdam, early pioneers in PRRT. I couldn’t fully bask in my minor celebrity status because I kept falling asleep. In addition to my PICC line, they also put in a peripheral IV. The PRRT mechanism itself looked like a metal contraption that should be in an office supply catalog for mailroom. I actually don’t remember much as I kept falling asleep. I don’t think this is typical; it was weeks of physical, mental, and emotional exhaustion catching up with me.
Enjoying a bit of freedom
I had a Mediport® placed earlier this year, then removed because of a blood infection. The Mediport was placed again after treatment and my PICC line was removed. For the first time since January, I don’t have to do daily hydration. I can shower without using an arm shower cap or AquaGuards®.
It’s little things like that that make me like Alec Baldwin’s “enthusiastic Parker” character on Friends. Quiet bowels, diaperless nights, unencumbered showers are all cause for celebration.
About two and a half weeks after the PRRT, I felt a familiar ache in my scalp, a very specific feeling of hair follicles letting go of hair. I’d hoped it was because I’d been wearing a garden sun hat, but by Monday, tiny pieces of my super-short hair were on my pillow and my laptop and my work desk. I had been warned of mild alopecia, and my hair had already thinned from the previous chemo. Being a swarthy lady is the bane of my existence; about 90 percent of my beauty routine involves hair removal. Of course, my mustache is still fuller and more luxuriant than I’d prefer. I’d wear a wig, but I’m lazy. Yet I’d rather be bald and active—on a yoga mat, on a beach—than have a full head of hair and be attached to an IV pole four hours a day.
My bowels don’t feel quite as stable as they did initially but the doctors have reassured me that I’ll continue to improve with further treatment. I am told that some of my symptoms might come back a bit before the next treatment.
Finding joy & support
The other day I found myself crying when I saw how scans after PRRT can significantly reduce the tumors. They were tears of gratitude. I really thought I was dying earlier this year, and I’m grateful that this might buy me some more quality time with family and friends. It’s probably not a very long time, but I’ll take it. My break up hurt, but we can both move forward now with our lives and nobody needs to die first.
As for the rest of my emotional health, I still have some sad days, but I’m feeling better every day. In fact, I’m often happier than I have been in a long time. So many friends have rallied and given me so much support, I’m far from alone and surrounded by so much love. No matter how our opinions on the break up differ, here is a fact: We had six or seven containers of dental floss in the bathroom and he took all of them. I don’t want that kind of person around. From now on, I want only the kind of toxicity in my life that combats tumors, not the kind that makes me feel apologetic for having cancer. I might actually have to admit to myself that I won’t win the lottery, but many days, I still feel extremely lucky.
Editor’s Note: PRRT is not for everyone. Josie’s story is not intended to represent typical indications or protocols for PRRT. To find out more about PRRT, talk to your treatment team.
https://ift.tt/2zsjybo
from WordPress https://netrf.wordpress.com/2018/07/10/the-road-to-prrt-a-path-of-self-discovery-and-growth/
0 notes
Text
CAT scan showed dramatic growth in Julie's liver
New Story has been published on https://enzaime.com/cat-scan-showed-dramatic-growth-in-julies-liver/
CAT scan showed dramatic growth in Julie's liver
Tampa Bay resident Julie wasn’t shocked when doctors diagnosed her with colon cancer after making several trips to the emergency room due to severe stomach pain. She always thought everyone gets cancer at some point in time, but she wasn’t prepared for the extent of her cancer. Julie’s colon cancer had spread to her liver and ovaries.
Her physician at Moffitt Cancer Center recommended chemotherapy and said she would bring up Julie’s case in the liver tumor board meeting to see if any other physicians could offer any additional treatments. Each cancer program at Moffitt has multidisciplinary tumor boards made up of surgeons, medical oncologists, radiation oncologists, radiologists, pathologists, nurses, dietitians, social workers and more. These tumor boards carefully review every new patient so that each one benefits from the expertise of the entire program.
Julie was in luck. Dr. Daniel Anaya, Head of the Section for Hepatobiliary Tumors at Moffitt, working with other members of the hepatobiliary section, including interventional radiologist Dr. Bela Kis, are the first in the world to modify a liver surgery procedure that can cure patients with very complex liver cancer that has spread. The procedure, known as mini-Associating Liver Partition and Portal Vein Ligation, or ALPPS, promotes rapid growth of the liver and makes removal of all cancerous lesions safe and possible.
Surgery, or removal of a portion of the liver with the tumors, is the only treatment that provides a cure for the majority of patients with liver tumors. A huge concern among these patients, however, is that less than 20 percent are eligible to have surgery because removal of multiple lesions often results in very small residual liver, which is not enough to keep the life-sustaining functions of the normal liver. To overcome this major limitation, surgeons have relied on the fact that the liver is the only organ that regenerates and can grow to almost its normal size after surgery. When blocking a branch of the portal vein (a vein taking blood to the liver) by using blocking agents delivered through the skin (portal vein embolization), the liver “believes” it has been cut/removed, inducing growth of the normal side, prior to surgery.
Julie had more than 13 lesions on both sides of her liver. The uniqueness of the modified mini-ALPPS approach used by Moffitt’s Liver Group is that using a combination of different procedures arranged in the appropriate sequence, within two weeks they were able to remove all the cancer found in Julie’s liver (13 lesions) and ovary. Following delivery of chemotherapy, Dr. Kis performed a percutaneous procedure geared at inducing liver growth (portal vein embolization). The next day following this procedure, Dr. Anaya did a small surgery removing the tumors on the left and cutting the liver in a way that would induce faster and bigger growth of the remaining portion of liver. Just one week later, a CAT scan showed dramatic liver growth, and Julie underwent a second surgery to remove the rest of the lesions. Now she is cancer-free.
“The approach and sequence of interventions we used in this case were critical to ultimately allow complete removal of all cancer lesions. The design of this approach and the decision to proceed with it in this case was based on a thoughtful discussion with input by experts from different teams and disciplines,” said Dr. Anaya. “This type of teamwork and cross-collaboration resulted in the ability to remove all the cancer and is what really sets Moffitt apart from other cancer centers across the country.”
Julie began a 12-week chemotherapy regimen in August, and her physicians will determine the next steps based on how well her body responds to treatment.
Julie says she’s grateful to her Moffitt physicians and takes time out now to stop and smell the roses.
0 notes
Text
New Post has been published on Mortgage News
New Post has been published on http://bit.ly/2pDvCwe
Living With Cancer
President Richard Nixon declared war on cancer in 1971, but 46 years later, a single cure remains elusive. That doesn’t mean significant progress hasn’t been made. New treatments and technologies have enabled people with even advanced cancers to live for years after their initial diagnosis. There are 15.5 million cancer survivors in the U.S., and two-thirds of them were diagnosed more than five years ago. Nearly 45% have lived for 10 years or more after their diagnosis.
See Also: 20 Amazing Ways Your Daily Life Will Be Different in 2030
SPECIAL REPORT: Fighting Cancer
How to Cover the Cost of Cancer Care
Best Stocks for Investing in Cancer Treatments
In 2009, Whitney Archer, 33, of Gainesville, Va., was diagnosed with a cancerous brain tumor known as an astrocytoma. Doctors were able to remove only 40% of the tumor, but Archer has gone on to lead a normal life, with no seizures or headaches since her surgery. She works as a librarian and part-time editor; looks after her son, Nate; and crochets and makes strawberry jam. Every three or four months, she and her husband, Daniel, battle Washington-area rush-hour traffic to go to the National Institutes of Health in Bethesda, Md., where she has an MRI. So far, all of the scans have been good. If her cancer reawakens, she says, she’s willing to try whatever treatments her doctors recommend.
Archer says she struggles with how to respond when people ask if her cancer has been cured. “Most of the time I just say, ‘It’s complicated.’ ”
Hitting the bull’s-eye
Researchers have learned that the war on cancer must be fought on many fronts. The most promising developments are in targeted therapies, which use drugs or other substances to interfere with specific molecules involved in the growth and progression of cancer. The first breakthrough in this type of therapy came in 2001, when the chemotherapy drug Gleevec was approved to treat chronic myelogenous leukemia (CML), a blood cancer usually caused by a gene flaw that develops during an individual’s life.
Advertisement
Gleevec blocks the gene’s activity, transforming the disease from a fatal condition into a chronic one. New research indicates that the drug works so well in eliminating the cells with the rogue gene that patients may be able to stop taking it after a few years. If the disease returns, the patient’s immune system may be able to keep the disease under control.
A newer type of targeted therapy with huge promise is immunotherapy. Its potential to harness the body’s own immune system to destroy cancer cells has captured the imagination of researchers, says Dr. Elad Sharon, a medical officer with the National Cancer Institute. In some cases, drugs are used to “take the brakes off” a patient’s immune system, revving it up so that it will attack cancerous cells. In other therapies, laboratory-produced antibodies are used to attack a specific part of a cancer cell.
Immunotherapy drugs have received accelerated approval to treat head and neck cancers, non-small-cell lung cancer, Hodgkin’s lymphoma, and melanoma, among other cancers. Former President Jimmy Carter used Keytruda, an immunotherapy drug, to treat advanced melanoma that had spread to his liver and brain. In 2015, Carter announced that he was cancer-free. (For the investment prospects of companies producing immunotherapy and other cutting-edge cancer treatments, see 5 Best Stocks for Investing in Cancer Treatments.)
See Also: 9 Top Pharmaceutical Stocks to Buy for the Dividends
Deb Ragosta discovered that her breast cancer, first diagnosed in 1990, had recurred and spread. Her treatments have kept the cancer from progressing. Photo by Jared Leeds
Other types of targeted therapies are helping patients with cancers that don’t respond to immunotherapy. Deb Ragosta, 62, of Plainville, Mass., has been treated with anti-estrogen and other targeted-therapy drugs since 2009, when she was diagnosed with stage IV breast cancer, the most severe form of the disease. Ragosta was first diagnosed with early-stage breast cancer in 1990. She found out years later that her cancer had reoccurred after she hurt her back on a trampoline. Her x-rays revealed a suspicious lesion on her spine, and further tests revealed that her breast cancer had metastasized to several spots on her back and one on her skull. Ragosta says she was floored by the news. Overnight, she went from someone who thought she was cured to a woman who will probably live with breast cancer for the rest of her life. “Had I not gone on the trampoline, I wouldn’t have been diagnosed because I had no symptoms,” she says.
Advertisement
But Ragosta’s treatments, through the Dana-Farber/Brigham and Women’s Cancer Center in Milford, Mass., have kept her cancer from progressing. She babysits for her two grandchildren a couple of days a week, teaches defensive driving and writes a blog, Don’t Stop Believing, for women with breast cancer. Convinced that writing is a good form of therapy, she provides writing classes for cancer survivors at Dana-Farber.
Ragosta tries to stay informed about new treatments. She recently applied to participate in a clinical trial but was told she was too healthy to qualify.
Qualifying for a clinical trial
Many people believe that clinical trials are only for cancer patients who have exhausted all other options. Others fear they’ll receive a placebo instead of a potentially life-saving drug.
In reality, clinical trials are available for all stages of cancer. Placebos are rarely used for cancer patients. Instead, the control group typically receives the “standard of care”—the treatment for the disease that has already been approved. Some will receive the standard of care along with the experimental drug. If results show that the trial drug is much more effective than the standard treatment, trial sponsors are required to switch all participants to the new drug, says Mandi Battaglia Seiler, a patient-services team supervisor for the American Cancer Society.
Advertisement
Even so, some cancer patients are rejected from clinical trials, either because they’re too healthy (like Deb Ragosta) or because they’re too ill. Tom Marsilje, 45, was diagnosed with colon cancer in 2012; in 2014, he learned that it had spread to his lungs and lymph nodes. But chemotherapy kept his cancer from spreading until recently, when tests showed tumors in his liver. That forced him to postpone participating in a clinical trial for immunotherapy.
Marsilje, an oncology researcher, hasn’t been sidelined by his diagnosis. Rather, he has devoted himself to raising awareness about colorectal cancer research and clinical trials. He provides updates on research and clinical trials through Colontown, a private Facebook community for people with colorectal cancer and their families. He answers questions about immunotherapy at TheAnswertoCancer.org, a website founded by the Cancer Research Institute, an immunotherapy advocacy group.
Meanwhile, Marsilje is pursuing an aggressive course of treatment for the tumors in his liver, and he remains optimistic that he’ll be able to keep his cancer in check. Ten years ago, he notes, advanced melanoma was considered a death sentence. Now people are living with that diagnosis for years. “I never give up hope,” he says.
If you’re interested in joining a clinical trial, start by talking to your doctor, who may be aware of trials that are appropriate for your situation. You can also research trials on your own, but you’ll need to do some legwork. To determine your eligibility for a trial (or trials), you need to be able to provide the details about your cancer diagnosis. The National Cancer Institute, a division of the National Institutes of Health, provides a checklist; to find it, go to www.cancer.gov and search “how to join a clinical trial.”
Advertisement
In most cases, the sponsor of the trial will cover the cost of the new treatment, along with special tests, procedures and doctor visits. Some also pay travel costs, but that’s not always the case, so find out what your expenses will be before you agree to participate. Study sponsors may be willing to pick up costs that aren’t covered by your insurance.
Because there’s a shortage of participants, clinical-trial sponsors “trip all over themselves” to take care of people who enroll, Seiler says. “You’re as valuable to them as they are to you.”
Updating old treatments
In many cases, physicians must still rely on traditional treatments, such as radiation and chemotherapy, to treat cancer. But researchers have found ways to use them more effectively.
For example, proton beam therapy, which uses the positively charged particles in an atom, delivers high doses of radiation to tumors without damaging surrounding tissue (see How to Cover the Cost of Cancer Care). It’s particularly effective in treating tumors that are located near critical organs, such as the brain, esophagus, liver and lungs. Dr. Kathryn Ruddy, an oncologist at the Mayo Clinic who specializes in breast cancer, says many of the clinic’s breast-cancer patients are opting for proton beam radiation because it’s less toxic than traditional radiation. There’s also a lower risk that the radiation will cause a secondary cancer, she says.
See Also: Great Places to Retire for Good Health
Meanwhile, years of experience with chemotherapy drugs have enabled doctors to deliver doses that are more precise and less toxic, Ruddy says. And anti-nausea medications have made it much easier for patients to tolerate chemotherapy, she says. Chemotherapy is also being used in combination with new treatments, such as immunotherapy.
Improved technology plays a big role, too. Doctors can more easily detect a reoccurrence of cancer at an early stage, which improves patients’ odds of survival. Catherine Goff, 62, of Dover, Mass., was diagnosed with Hodgkin’s lymphoma when she was 21. Aggressive radiation treatments cured the lymphoma, but the high doses of radiation—much higher than those that would be used today—left her at risk for a secondary cancer. Goff did develop secondary breast cancer at age 55, but because she participated in regular screenings, her doctors were able to detect the cancer at an early stage. In December 2009, she had a double mastectomy.
Goff says it’s much easier to talk about cancer now than it was when she was first diagnosed more than 40 years ago. “When I was 21, you didn’t even say the C word,” she says. “Now you’re encouraged to talk about it.”
That’s in part thanks to the willingness of Jimmy Carter and other public figures to talk about their own experiences, says Julia Rowland, director of the Office of Cancer Survivorship at the National Cancer Institute. “A lot more people realize there’s life after cancer.”
Information you can trust
The internet provides an abundance of information about every stage and category of cancer, but spending hours consulting Dr. Google could be bad for your health. Some websites provide information that’s confusing, contradictory or flat-out wrong.
— One source of reliable information is the National Cancer Institute. In addition to updates on everything from prevention to clinical trials, the NCI offers a help line (800-422-6237) with information specialists who are able to answer questions about cancer and provide details about programs offered by the NCI.
— The American Cancer Society is another good source of general information that also offers a help line (www.cancer.org; 800-227-2345). The ACS provides a matching service for patients interested in clinical trials. You can find a list of trials within your zip code on its TrialCheck database. To speak with a clinical trials specialist, call 800-303-5691. You can find more information at www.learnaboutclinicaltrials.org.
— The National Library of Medicine provides a detailed list of clinical trials for cancer and other diseases at www.clinicaltrials.gov. It currently lists more than 230,000 trials in the U.S. and around the world. Note, however, that the listing is not particularly user-friendly.
— Support groups can provide encouragement, advice and up-to-date information, and there’s one for every type of cancer. Your local hospital or a social worker can help you find one; you can also do an online search. Cancer support groups can also provide information about clinical trials.
The cancer moonshot
In his 2016 State of the Union address, former President Barack Obama announced that Vice President Joe Biden would lead a national initiative, Cancer Moonshot, to “end cancer as we know it.” The program was created in honor of Biden’s son Beau, who died of brain cancer in 2015.
The project’s research efforts include using crowdsourcing to map and identify cancer technologies so that funding can be directed to the most promising treatments. The National Institutes of Health and the Food and Drug Administration have announced a series of programs to improve clinical trials and make them easier for patients to locate. Other Moonshot programs run the gamut from ride-sharing for low-income patients to free mammograms for women who don’t have health insurance.
The program could be sharply curtailed by President Trump’s proposed budget, which calls for a 19% reduction in funding for the National Institutes of Health. However, those cuts are expected to face tough opposition in Congress.
0 notes
Text
NJ MONTHLY: THE LONG AND WINDING ROAD TO IMMUNOTHERAPY
By Debbie Galant | February 1, 2017 | Appears in the February 2017 issue
Immunotherapy holds out new hope for many cancer patients. But for those with the disease, navigating the maze of experimental treatment can be daunting.
In September 2015, just days after I’d begun chemotherapy, I was at an art exhibit in Atlantic Highlands when I started talking to a gentleman standing quietly in the gallery. When I discovered he was a doctor, I lingered.
He listened to me ramble on about my recent diagnosis, and then said, in almost a whisper: “If your cancer recurs, there’s something new they’re working on.” Then he told me about a barely known, seemingly magical cancer treatment called immunotherapy. He talked about it like it was the Manhattan Project—a secret being held closely by the cancer-research community—and although I was alarmed that someone was talking about recurrence when I’d barely begun treatment, I filed it away.
Almost a year later, and eight months out of therapy myself, I was sitting with a friend at the Rutgers Cancer Institute of New Jersey in New Brunswick, where immunotherapy—far from being a faint dream—was front and center on the agenda.
My friend Chiara D’Agostino, 45, was first diagnosed with breast cancer in fall of 2014. She had the same aggressive form I was diagnosed with—triple negative breast cancer—but until this past August, after two mastectomies and eight rounds of chemotherapy, it looked like she had it beat. That’s when a CAT scan revealed new nodules in her lungs. An aspiring model with a bouncy mop of gray post-chemo curls, D’Agostino is also a social media junkie (she blogs about cancer at beautythroughthebeast.com) who’s comfortable sporting a pink tutu for the cause or posting pictures of her surgical drains on Instagram. But her buoyancy had all but disappeared when it was confirmed that those nodules were indeed metastatic stage IV breast cancer. Thus began a dizzying new round of medical consultations.
So, here we were, talking about exactly what the doctor in Atlantic Highlands had mentioned so cryptically a year before. By this point, immunotherapy—a treatment that enlists a patient’s own immune system to kill cancer—was no secret, having exploded into public consciousness in December 2015, when former President Jimmy Carter announced that his brain tumor had completely disappeared. He had been treated with a Merck immunotherapy drug called pembrolizumab, marketed under the trade name Keytruda.
But the Food and Drug Administration has only approved Keytruda and drugs like it for melanoma, non-small cell lung cancer and a few other conditions. For a breast-cancer patient like D’Agostino, the only option is to enroll in a clinical trial. That’s what brought us to the Rutgers Cancer Institute—to find out more about the institute’s phase II clinical trial, a test of Keytruda on patients with metastatic triple negative breast cancer.
Six weeks later, D’Agostino would join that trial. Her new tumor had tested positive for a molecule called PD-L1, which meant she was a fit for the trial. But first, she had to navigate a complicated medical maze that included 14 more doctor appointments, two brain MRIs, five CAT scans, two bone scans, a PET scan, two chest x-rays and two biopsies—the second of which was requiredbecause the lab had lost tissue collected the first time.
Chemotherapy, the standard-bearer of cancer treatment for the past 50 years, was a medical accident that grew out of the use of chemical warfare. Two pharmacologists hired by the U.S. government at the beginning of World War II to find an antidote to mustard gas had begun to suspect that it might have properties that could slow the growth of certain cancers. A year into their research, when German bombs struck a U.S. battleship secretly carrying mustard gas, their hunch was validated. Autopsies of victims of the attack showed that the mustard gas had profoundly suppressed their lymphatic systems. By 1946, it was reported that nitrogen mustard injected into lymphoma patients had indeed shrunk their tumors.
But immunotherapy—the newest weapon in the war on cancer—was no accident. It was a direct result of the sequencing of the human genome, which allowed scientists to begin discovering the genetic mutations that cause cancer. “All of a sudden, we could start to design drugs that could be targeted against a specific defect,” says Dr. Andre Goy (pronounced gwah), director of the John Theurer Cancer Center at Hackensack University Medical Center.
The first breakthrough drug in this category was Gleevec, developed by scientists at Ciba-Geigy in the late 1990s. Gleevec turned chronic myeloid leukemia from a death sentence into a chronic disease.
Oncologists and pharmaceutical companies are hoping that immunotherapy drugs called PD-1 checkpoint inhibitors—like the one Carter received—will perform this miracle for other cancers.
Dr. Kim Hirshfield, director of the precision medicine translational laboratory at the Rutgers Cancer Institute, and D’Agostino’s primary oncologist, was able to simplify the complex science during our first visit. She pulled out a pen and a piece of paper and started drawing some squiggles. PD-1 interacts with PD-L1 or PD-L2, she explained, tapping one of her squiggles. “That puts an invisibility cloak over a tumor.” Behind this cloak, a cancer can slip past the patient’s immune system undetected. A PD-1 inhibitor—or immune checkpoint inhibitor, it is commonly called—removes the cloak and allows the patient’s immune system to recognize the tumor and destroy it.
An added bonus: while immunotherapy drugs are administered the same way as most chemotherapy—by intravenous infusion—they generally don’t cause the dreaded hair loss and nausea. What’s more, when they do bring a patient into remission, it can last for years.
Early successes have led to something of a pharmaceutical arms race. According to The Cancer Letter, a publication that covers cancer research, there are more than 800 ongoing clinical trials involving checkpoint inhibitors.
As it turns out, the two companies that have the strongest positions in this market—Merck and Bristol-Myers Squibb—happen to be in New Jersey. Merck is headquartered in Kenilworth. Squibb, though based in New York, has 6,600 employees in the Princeton area, including many of its R&D employees.
“Squibb and Merck are kind of duking it out,” says Ed Silverman, Pharmalot columnist and senior writer at Stat. “Cancer is the big kahuna—a big, mysterious, evil disease that has been vexing everyone so long that anything that might make a dent is a big deal.”
And immunotherapy is a big deal. “We see patients who were in hospice go into remission,” says Goy.
How big? In a recent 10-K filing with the SEC, Squibb says Opdivo is the only drug that comprised more than 10 percent of its annual R&D budget in the last three years. Opdivo, responsible for $942 million in revenues in 2015, is so important to the bottom line that Squibb warns investors any bad news from its trials could cause a sharp decline in the company’s stock price. Keytruda, which racked up $566 million in revenue in 2015 and is the subject of 400 clinical trials, gets prominent mention in Merck’s annual 10-K report. Meanwhile, GBI Research, a provider of business intelligence, predicts that global sales of cancer immunotherapies will quadruple to $75.8 billion by 2022.
Muddying the waters are recent revelations that checkpoint inhibitors have caused serious—and in some cases fatal—side effects by over-stimulating the body’s immune system.
“Every drug has the potential for causing side effects,” says Hirshfield. “We know from early studies of the treatment of patients with checkpoint inhibitors that autoimmune phenomena may occur due to release of the brakes on the immune system. These include endocrinopathies in which the immune system attacks and causes dysfunction of endocrine organs such as the thyroid and pancreas, among others.” What’s more, says Hirshfield, “we do not yet know which patients are at the highest risk of these specific side effects, and if affected, the severity of the side effect they may experience.”
The consent form for the trials that D’Agostino signed include references to the risk of diabetes and the possibility of a fatal inflammation of the lungs, as well as dozens of less serious potential reactions, such as watery bowel movements, yellowin of the skin and weight loss.
Complicating the picture further is a suit that Squibb brought against Merck in 2014, claiming that Merck’s development of Keytruda infringed on its Opdivo patent. The case is pending.
Whatever happens in the courts, it seems the story of cancer treatment is being largely written in New Jersey. Although London-based AstraZeneca is a third major player in this field, two-thirds of the clinical trials in checkpoint inhibitors are reporting back to scientists here. If early success holds and side effects of these medicines can be mitigated, the brutality of chemo could give way to a gentler era of precision medicine.
“My prediction,” says Dr. Eric Rubin, vice president of early-stage oncology clinical research at Merck, “is that within a few years, most cancer we’ll treat with immunotherapy.”
For now, except for patients with a few specific cancers, getting access to these potential miracle drugs means one thing: getting accepted into a clinical trial.
If you live in New Jersey and you’re diagnosed with cancer, chances are someone will ask if you’re going to get treatment in New York, typically referring to Memorial Sloan Kettering. Why would you go anywhere else if the top doctors in the country are that close? On the other hand, if you’re looking at 12 weekly chemo infusions, you just might choose the convenience of a local hospital that provides such treatment.
That’s what I did. D’Agostino, a Montcliar resident, also sought treatment close to home during round one, when her cancer was first diagnosed. But this time, with stakes higher, she considered the New York option. At the same time, recommendations from friends online and support groups led her to the Rutgers Cancer Institute and the John Theurer Cancer Center at Hackensack.
D’Agostino spent most of September ping-ponging between New Brunswick, Hackensack and two Manhattan hospitals offering clinical trials.
The National Cancer Institute recognizes the Rutgers Cancer Institute, which has 69 oncologists, as a Comprehensive Cancer Center—one of only 47 in the country, and the only one in the state. Theurer, which has 45 oncologists and is known for its specialty in liquid tumors like leukemia and lymphoma, is applying for the status. (A third home-based powerhouse emerged from the 2013 partnership between MD Anderson Cancer Center—a Texas-based cancer-care giant—and Cooper University in Camden.)
And, as it turns out, while oncologists routinely refer cancer patients to Memorial Sloan Kettering when they have obscure or difficult-to-treat cancers, Sloan Kettering—which has three outposts in New Jersey and recently signed a cancer-care partnership with New Jersey hospital group Hackensack Meridian Health—also refers patients to the Rutgers Cancer Institute. Dr. Joseph Aisner, interim associate director for clinical science at Rutgers, says it’s typical for designated Comprehensive Cancer Centers to refer patients to one another “because of clinical trial availability, unique resources or dealing with issues of insurance.” Aisner adds that Rutgers takes most insurance plans. Regardless he says, “We have a commitment to the community. If they don’t have insurance, we’ll do it.”
That makes a big difference to D’Agostino, a former Italian teacher, who is currently unemployed, single and relies on Medicaid.
But D’Agostino was also drawn to Theurer, which similarly accepts patients regardless of their ability to pay. For starters, Theurer looks more like a five-star European hotel than a New Jersey hospital. Goy, the hospital director, conscripted Santiago Calatrava—designer of the World Trade Center’s Oculus transportation hub—to help with the plans for the building, which opened in 2011. The first thing you notice when you enter is the soaring, four-story lobby and its gleaming grand piano. Goy is particularly proud of the rooftop herb gardens and cooking studio. “This is the best way to tell a patient that you believe in their future,” he says.
D’Agostino’s greeting at Theurer was impressive. She was handed a notebook, pen and a magnet “with every number you could need,” and was escorted wherever she needed to go. “It’s like a well-oiled machine,” she says.
It wasn’t the accoutrements, however, that made it hard to decide where she would have treatment. It was the science. Both offered clinical trials for metastatic triple negative breast cancer.
“My head was spinning,” D’Agostino says. “It was very daunting at first. I’m not a science person.”
Elly Cohen, program director of BreastCancerTrials.org, says that the complexity of medicine at this level is extremely hard for patients to navigate. “As we get more and more into personalized medicine—the biology of your tumor, what medications are available to you—it’s going to be very confusing,” she says. Compounding the problem, says Aisner at the Rutgers Cancer Institute, is the fact that patients rarely recall more than 15 percent of what they’re told in the consulting room. “If there’s another person in the room, we can double that,” he says, referring to data from the past 30 years. “The real answer is to have a navigator.”
D’Agostino wound up getting help from Vicky Carr, a patient advocate and clinical trial consultant based in Virginia, whom I’d met at a focus group for triple negative cancer patients. Carr helped D’Agostino tease out the differences between the trials she knew about and also sent her to check out trials at Memorial Sloan Kettering and Weill Cornell in Manhattan. D’Agostino couldn’t enter Cornell’s trial because they didn’t take Medicaid. Memorial’s trial involved androgen receptors, and D’Agostino’s tumor, it turned out, didn’t express androgen.
Both the Rutgers Cancer Institute and Theurer offered clinical trials involving checkpoint inhibitors, but in the end, D’Agostino’s decision came down to trial phase. Theurer was enrolling patients in phase III trials, but since these trials are randomized, D’Agostino knew she might get a placebo. Rutgers was offering her a phase II trial in which all the participants were getting Keytruda.
There was also the human factor. Hirshfield, at Rutgers, had a bedside manner so kindly that, if she weren’t wearing a lab coat and stethoscope, you might have mistaken her for a nursery school teacher. She occasionally giggled during a consult, and at the end of their first meeting gave D’Agostino a hug. At a later visit, D’Agostino says, “I was starting to cry and she came up and held my hand. When you get people who are loving and intelligent…oh my God.”
There is no question that, while the science of cancer seems to be advancing at almost startling speed, the path for the cancer patient remains a labyrinth, blocked at every turn by a patient’s ability to cut through scientific complexity, insurance and monetary concerns, and considerations of geography. Does it help, I wondered, to live in the state where most of these drug trials were being initiated?
No, says Dr. Cliff Hudis, CEO of the American Society of Clinical Oncology. “I personally don’t think there’s any particular geographic relationship.” After all, Merck and Squibb are global companies, and their drugs are used in clinical trials everywhere. “We will seek out top investigators, regardless of geography,” says Rubin of Merck.
Yet being in New Jersey does have an upside, in part because of the talent the state attracts. Many alumni from the Rutgers Cancer Institute have gone to nearby pharmaceutical companies. Rubin, before joining Merck, oversaw clinical trials at the Institute. Cynthia Wojtaszek, director of U.S. regulatory strategy for oncology at Bristol-Myers Squibb, also hails from the Institute. Mary Todd, now global medical affairs leader for prostate cancer for Johnson & Johnson, was deputy director at the Institute in the 1990s.
Further, New Jerseyans have a distinct advantage in getting access to new treatments because of a pioneering agreement Todd forged with health insurers in the mid-1990s, when she was at the Institute. With the help of some powerful friends in Trenton, she convinced insurers to voluntarily cover standard of care for all patients undergoing clinical trials in New Jersey. This includes all tests, scans and exams a patient would have even if they weren’t in an experimental protocol.
Fouad Namouni, development head for oncology at Bristol-Myers Squibb, says there is indeed an advantage to locating clinical trials in the Garden State. “It’s just easier to drive down to a site in New Jersey than having a meeting in San Francisco and flying six hours,” he says. “We’re going to have faster discussions and hopefully productive discussions.”
For D’Agostino, doggedness, connectedness, luck and perhaps geography—along with our nation’s medical safety net—conspired to get her into a clinical trial. And although it surely didn’t feel that way to her, it happened—in medical-bureaucracy terms—at breakneck speed. But the real story of D’Agostino’s cancer is being written at a cellular level. It’s happening at the checkpoint between her cancer cells and her T-cells—the white blood cells that are key to the body’s immune response. In December, blood tests showed a significant decline in tumor markers and a scan indicated that all the nodules in Chiara’s lungs had disappeared. Although some new nodules had shown up on her lumbar spine, doctors were optimistic that the Keytruda was working. Only time will tell.
0 notes