#astrocytoma
Explore tagged Tumblr posts
Text
Dr Fidaa
Dr. Fidaa Wishah, a distinguished pediatric radiologist, specializes in the intricate field of pediatric astrocytoma radiology. With a wealth of experience and a commitment to providing the highest standard of care for young patients, Dr. Wishah plays a crucial role in diagnosing and treating pediatric astrocytoma, a type of brain tumor that occurs primarily in children.
In the realm of pediatric radiology, Dr. Fidaa Wishah stands out for her expertise and dedication. She employs advanced imaging techniques to examine and analyze astrocytomas in pediatric patients, ensuring accurate and timely diagnoses. Her compassionate approach to working with children and their families sets her apart, creating a supportive environment during what can be a challenging time for both patients and caregivers.
Pediatric astrocytoma radiology involves the use of cutting-edge technologies such as magnetic resonance imaging (MRI) and computed tomography (CT) scans. Dr. Wishah leverages these tools to visualize and understand the intricacies of astrocytomas in children, enabling her to develop tailored treatment plans that prioritize the well-being and recovery of her young patients.
Understanding the unique challenges posed by pediatric astrocytoma, Dr. Fidaa Wishah collaborates closely with a multidisciplinary team of healthcare professionals. This collaborative approach ensures comprehensive care, considering not only the radiological aspects but also the broader medical and emotional needs of the child and their family.
As a pediatric radiologist, Dr. Wishah is dedicated to staying at the forefront of her field. She actively engages in research and continuing education, contributing to advancements in pediatric astrocytoma radiology. This commitment to ongoing learning reflects her passion for improving outcomes and enhancing the quality of life for children affected by astrocytomas.
In summary, Dr. Fidaa Wishah's expertise in pediatric astrocytoma radiology, combined with her compassionate approach, makes her a trusted and invaluable resource for families facing the challenges of childhood brain tumors.

#DrFidaaWishah#PediatricRadiology#Astrocytoma#PediatricHealth#MedicalExpertise#ChildhoodCancer#RadiologyCare#HealthcareInnovation
0 notes
Text
Virtual Consultations with Brain Surgeons Near Me: What to Expect
In recent years, the healthcare landscape has undergone a significant transformation, particularly in the realm of specialized medical services. One area that has seen considerable advancements is neurosurgery, where the emergence of virtual consultations has made it easier for patients to access expert care without the need for physical appointments. This article delves into what patients can expect when seeking virtual consultations with brain surgeons near them, ensuring they are well-informed and prepared for this innovative approach to healthcare.

The Rise of Virtual Consultations in Neurosurgery
The shift towards virtual consultations represents a broader trend within the medical field, where technology is leveraged to enhance patient experience and improve accessibility. Patients no longer need to travel long distances to meet with leading experts in neurosurgery; instead, they can connect with brain surgeons from the comfort of their homes. This approach not only saves time but also reduces the stress often associated with hospital visits.
Moreover, virtual consultations can be particularly beneficial for individuals with mobility issues or those living in remote areas. For many patients, finding a brain surgeon near me can be a daunting task, especially if there are limited options available locally. Virtual consultations break down these geographical barriers, allowing patients to consult with top-tier specialists regardless of their location.
Preparing for Your Virtual Consultation
When preparing for a virtual consultation with a brain surgeon, there are several key steps that patients should take to ensure a productive experience. Firstly, it is essential to gather all pertinent medical records and imaging studies, such as MRIs or CT scans. Having this information readily available will enable the surgeon to make a more accurate assessment of the patient's condition and provide tailored recommendations.
Additionally, patients should prepare a list of questions or concerns they wish to address during the consultation. This proactive approach not only helps in maximizing the time spent with the surgeon but also ensures that all important topics are covered. Patients should also check their technology setup prior to the consultation, ensuring that their internet connection is stable and that they have access to a device equipped with a camera and microphone.
What to Expect During the Consultation
Virtual consultations typically begin with an introduction, where the brain surgeon will discuss the patient's medical history and the purpose of the meeting. The surgeon may ask a series of questions to gain a comprehensive understanding of the patient's symptoms and previous treatments. Following this, the surgeon will review any uploaded medical records and imaging studies, providing insights based on the latest medical knowledge and their expertise.
Throughout the consultation, patients can expect a collaborative discussion regarding potential treatment options. The brain surgeon may outline various approaches, including both surgical and non-surgical options, and help the patient weigh the benefits and risks associated with each. This dialogue is crucial, as it empowers patients to make informed decisions about their health in partnership with their healthcare provider.
The Benefits of Virtual Consultations
One of the most significant advantages of virtual consultations is the increased accessibility to specialized care. Patients who may have previously felt overwhelmed by the prospect of traveling to a distant hospital can now receive expert opinions from the convenience of their homes. This increased accessibility can lead to earlier diagnosis and intervention, which is particularly important in the field of neurosurgery where timely treatment can make a substantial difference in outcomes.
Virtual consultations also offer flexibility. Patients can schedule appointments at times that suit their lives, reducing the need to take time off work or arrange for childcare. Furthermore, the ability to consult with multiple specialists virtually enables patients to gather diverse opinions before making critical medical decisions. This aspect is particularly valuable when navigating complex conditions that may require a multidisciplinary approach.
Follow-up Care and Ongoing Support
After the initial virtual consultation, patients can expect a clear plan for follow-up care. Depending on the condition, the brain surgeon may recommend additional tests, referrals to other specialists, or a follow-up consultation to monitor progress. Many surgeons also provide ongoing support through secure messaging platforms, allowing patients to ask questions and seek guidance as they navigate their treatment journey.
It’s important for patients to remain engaged with their healthcare team during this time. Keeping an open line of communication ensures that any emerging concerns can be addressed promptly. Additionally, patients should be proactive in adhering to the treatment plan discussed during the consultation, whether it involves medication management, lifestyle changes, or further diagnostic testing.
Conclusion
As the demand for specialized medical care continues to grow, the advent of virtual consultations with brain surgeons represents a significant leap forward in patient accessibility and convenience. This innovative approach not only allows for expert advice from the comfort of home but also fosters a collaborative relationship between patients and their healthcare providers.
For those seeking a trusted partner in their neurosurgical journey, Robert Louis MD offers comprehensive virtual consultations that cater to individual needs and circumstances. By prioritizing patient engagement and personalized care, Robert Louis MD stands out as a leader in the field, ensuring that patients receive the expert guidance they deserve. Whether you are exploring treatment options or seeking a second opinion, reaching out to Robert Louis MD can be the first step towards a healthier future.
0 notes
Text
#Anaplastic Astrocytoma Market#Anaplastic Astrocytoma Market Share#Anaplastic Astrocytoma Market Size#Anaplastic Astrocytoma Market Forecast#Anaplastic Astrocytoma Market Report#Anaplastic Astrocytoma Market Growth
0 notes
Text

another round of tests and all looks still fine! u dont wipe me off this world that easy, god damn it! ✊
(for newer followers: i have gr3 IDH1 anaplastic astrocytoma - rare brain cancer that will eventually grow back worse and kill me)
36 notes
·
View notes
Text

“An 11-year-old girl who was misdiagnosed with sickness bugs and migraines was assessed by doctors about 30 times before they found that she had a brain tumour, according to her mother.
Tia Gordon, from Northampton, was admitted to hospital as an emergency despite previous visits to GPs, A&E and calls to 111.
Imogen Darby, Tia’s mother, said her daughter’s glasses prescription had also been changed four times before the tumour was found.
Darby had sought help regarding Tia’s migraines and vomiting for more than three years, before being told that the wait for an MRI scan would be at least eight months. It was only when Tia’s balance and ability to walk were affected that she was given an emergency scan, which found a brain tumour measuring about 3.5cm.”
Darby said: “I was told Tia had stomach bugs and migraines. The first thing I was told, because it was the summer, [was that] she just needed to drink more water.
“After probably a year, she got diagnosed with migraines and they gave her paracetamol for that. She was also given another medication for that and her final diagnosis in January from paediatrics was migraine with sickness.
“Over more than three years, I took Tia to doctors, she was refused MRIs, she was refused to be seen by emergency paediatrics, I called 111, I went to A&E. She had her glasses changed four times, she was given medication and she had a consultant, but it took for her to be unable to walk for her to get the care she needed.”
Darby first noticed Tia’s symptoms in March 2020 when she started vomiting with increasing frequency. Darby twice tried to get her daughter referred to emergency paediatrics, but was declined both times and told it was not an emergency.
Later, Tia began holding her neck in an unusual way and complained about stiffness, for which she was referred to a physiotherapist.
Despite several visits to A&E and calls to GPs and the NHS’s 111 service, Tia’s remained undiagnosed. From November 2023 to January 2024, Tia was vomiting violently every day, and began to lose her balance. “She was tipping her milk out in the kitchen sink,” Darby said. “She was standing there and … she didn’t notice she was doing it at all.”
After a phone call from Tia’s school, which said Tia was holding her neck and was off balance, Darby took her to Northampton General Hospital. While there, Tia was unable to walk in a straight line, and a CT scan revealed a pilocytic astrocytoma — the most common type of brain tumour in children.
Tia was taken to Queen’s Medical Centre in Nottingham, where she had a ten-hour operation to remove the tumour. “It was quite a horrendous day,” Darby said. “They managed to get 96 per cent of it out.”
Tia called the growth her “astronaut tumour”. Since the procedure, she gets very tired and can sometimes lose her balance. Her recovery will consist of an MRI scan every three months for the next five years, and she is having regular physiotherapy and meetings with neurologists.
She is keen to get back to her hobbies. Darby calls her “Dr Doolittle” due to her love for animals, and added that Tia is a keen reader and enjoys playing dodgeball.
Cameron Miller, director of external affairs and strategy at the Brain Tumour Charity, said “We wish Tia all the best with her continuing treatment and thank Imogen for sharing her story.
“Sadly, it’s one that we often hear. For many brain tumour patients, it simply takes too long to be diagnosed — and this is one of the reasons why we’re calling for a National Brain Tumour Strategy.”
94 notes
·
View notes
Text
Alrighty.. just putting this here for safekeeping and so maybe it’ll be easier to explain. On Feb 17, 2024 my boyfriend at the time woke up around 9:30 am to me having a seizure. He took me to a research hospital in the area and we got to the ED around 11 am. They did a CT and an MRI and have found what they called a 4 cm tumor in my right frontal lobe. I had another MRI in the middle of March and got more measurements on the size of the tumor. Based on the measurements, I did the math and found it was 119 cubic cm (about the size of a billiards ball). I had a right frontal craniotomy on April 1, 2024. They were able to remove the entire tumor and my MRI the evening after surgery showed no residual tumor. I’ve met with an oncologist and we waited for pathology results. Pathology came back as a Grade 3 Astrocytoma with the IDH1 mutation. I have started 500 mg of Tibsovo daily to keep it from growing back, or at least slow it down. There isn’t a cure for brain tumors, so we just wait for it to come back and do surgery again. If you’ve read this far into my real life shit, I appreciate any well wishes, thoughts, and prayers if you’re religious. I try to keep my spirits up and handle things rationally but some days that is a little more difficult. I’m stuck on antiseizure medication for at least a year from my latest seizure (luckily it’s still just the seizure in Feb 2024) and cannot drive per my state’s laws for a year from the last seizure as well.
Luckily my job has been flexible with me since February but trying to get back to full time hours is a struggle, especially if I want to take care of myself as well (bathing, eating, cleaning, etc). Also, lots of back and forth with insurance companies and the hospital and lots of scans and follow up appointments.
6 month MRI was clean. “No progression” and “stable burden of disease”. Joint pain has been mostly managed with new meds.
I moved in with my “friends” who turned into girlfriend, fiancée, and wife very quickly (we had a hand fasting ceremony Oct 6, 2024) and her husband became my boyfriend as well. Being in a functional throuple is new to them, so there have been some hiccups but everything is looking up. 💜
9 month post op MRI came back with no suspicious activity to suggest disease progression or recurrence, so that’s a win! I’m almost able to legally drive in Arkansas again (very stupid seizure law here). The wifey’s husband and I are not pursuing a relationship right now to keep our household as stable as possible, but I think it’s for the best long term ☺️
Well folks! We made it to a year. MRI was also exactly the same as January so we are graduated to 4 months until my next MRI! It’s been one hell of a year since having literal brain surgery, but we made it. My wife, her hubby and their toddler moved a few states away to their other house, so it’s been just my cat, two of her kittens, and me in the house…. But that’s not lasting for long because my daddy is moving here!!
84 notes
·
View notes
Text
Neoplasms of the CNS
This is going to be a long one, so I apologize. This topic can be kinda boring and difficult, but it's good to know for anyone in med school. A lot of this stuff is also pretty high-yield for boards, so yay.
I'm going to go over a lot of different types, give you some basic facts, and show (and tell) you what it looks like. Hope you have a fun time reading :D
Glial Tumors
Glial cells are little helper cells in the brain. Gliomas are tumors made of these cells. You have three subtypes: pilocytic astrocytomas, diffuse low-grade gliomas (low grade astrocytomas and oligodendrogliomas), and malignant gliomas (anaplastic astrocytomas and glioblastomas). Glioblastomas are the most aggressive gliomas.
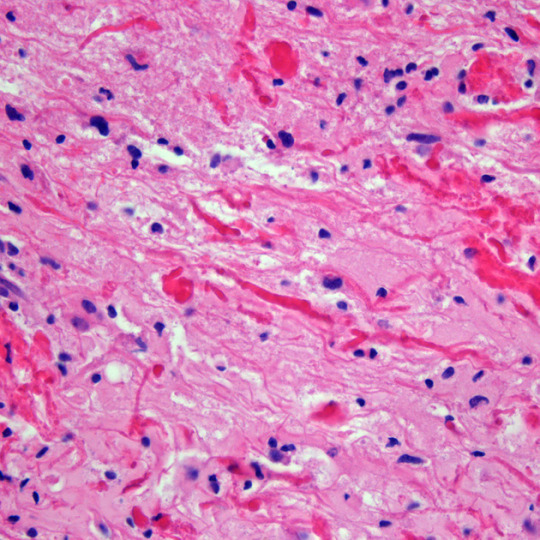
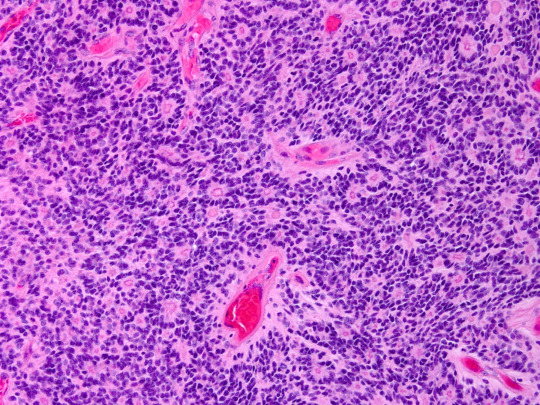
Pilocytic astrocytomas are the most common primary brain tumor in children. They are well-circumscribed and grow very slowly. They prefer the cerebellum and brainstem. Their most distinguishing feature are the Rosenthal fibers (pilocytic means fiber) and red inclusions. These can usually be treated with resection alone. Look how pretty it is:
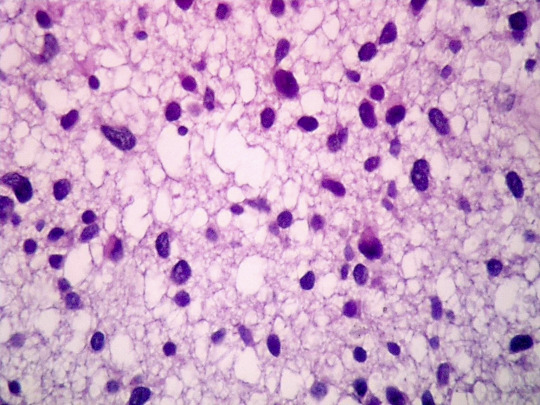
Low grade gliomas are the majority of adult brain tumors. They are infiltrating and are WHO grade 2-4. Both diffuse astrocytomas and oligodendrogliomas are going to be basically in the middle of the brain. Oligodendrogliomas prefer white matter of the cerebral hemispheres and infiltrate to the cortex. Microcalcifications are common. Oligodendrogliomas have a "fried egg" and "chickenwire" appearance, but this is usually stated as uniform cells with clear cytoplasm and branching, delicate blood vessels on board exams.

Diffuse astrocytomas show irregular, angulated, and hyperchromatic nuclei, and have a tendency to recur, spread, and progress to higher stages.
Now to the malignant gliomas. Malignant astrocytomas are the most common primary brain tumor in adults. You'll see a hypercellular glioma with poorly differentiated astrocytes. It tends to recue, and shows significant nuclear atypia and miotic activity (it's dividing!!). These can develop from other types of astrocytomas or de novo. They usually progress to glioblastoma.
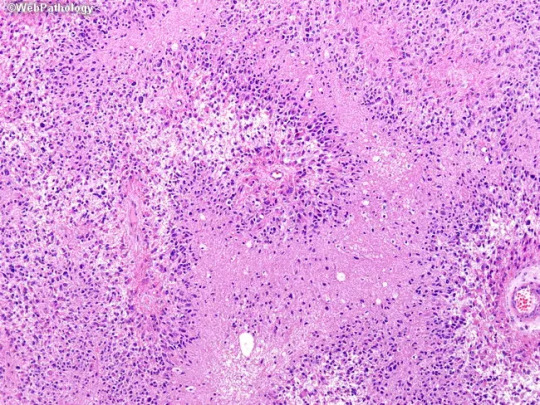
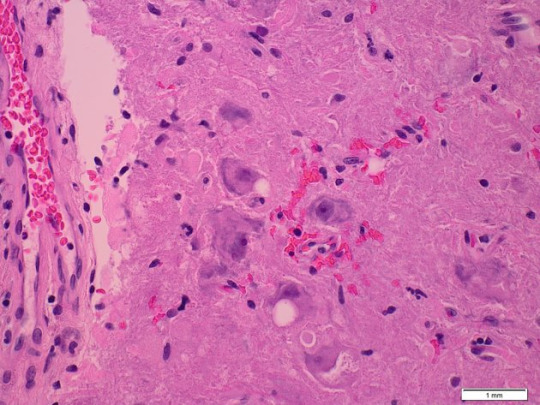
Glioblastomas are the most common and most malignant gliomas. They are poorly defined, infiltrating, and will distort the brain. Some people say they look like butterflies on MRI (I say these people are full of shit). You'll see serphintine or psuedopalisading necrosis and microvascular proliferation. The morphology of the cells is highly variable (from giant and bizarre to small and tightly packed). There is about a one year median survival from disgnosis.
Medulloblastomas
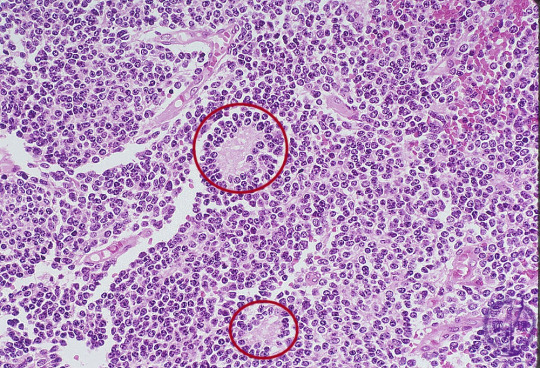
This is the most malignant brain tumor in children, and is only found in the cerebellum (by definition, obviously). All of them are WHO grade IV. The classic (aka the kind on board exams) is composed of sheets of densly packed cells with round to oval nuclei (or sometimes carrot-shaped lol), and little cytoplasm. They are poorly differentiated and primitive. In 40% of them, there are Homer-Wright (neuroblastic) rosettes (circled below).
Sometimes you see spinal drop metastasis of these, which means the tumor has spread to the spinal cord. This will show up as a "sugar coated" spinal cord on MRI. If the tumor compresses the 4th ventricle, you'll also see increased intracranial pressure.
Ependymomas
These are slow-growing tumors that originate from either the walls of the ventricles or the spinal canal. In kids, they're usually in the brain. In adults, they're usually in the spine. There are like nine subtypes, but the most common feature on histology is perivasuclar psuedorosettes. They have a poor prognosis.
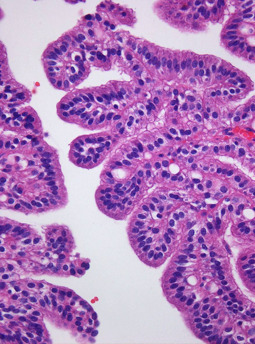
Choroid Plexus Papillomas
These come from the cuboidal cells of the choroid plexus within the ventricles (the things that make CSF). 85% are in kids less than 5 years old, and most are found in the lateral ventricles. They look like cauliflower. Under the microscope, they show papillary structure with delicate fibrovascular cores, with a cuboidal lining. Complete resection is the main treatment.
Neuronal Tumors
We're only gonna talk about gangliocytomas, gangliogliomas, and dysembryoplastic neuroepithelial tumors, but there are other types. Gangliocytomas are the most common tumors associated with chronic temporal lobe epilepsy, but they are rare overall. They show prominent single nucleoli and cytoplasmic basophilic Nissl substance. They also may have pilocytic elements. They may progress to gangliogliomas.
Dysembryoplastic neuroepithelial tumors are low-grade tumors that are seen in kids. Usually they cause seizures. You'll see multinodular lesions in the cortices (usually temporal). Histology looks like prominent clusters of oligodendroglial-like cells, which seem to float in cystic spaces. Resection is the treatment, and usually stops the seizures.
Meningiomas
These are the most common benign tumors in adults, with resection being the primary treatment (unless they're radiation-induced, those fuckers are aggressive). These are attached to the dura mater and compress the brain without invading it. The meningothelial subtype is the only one you need to know the histology of. It has characteristic whorls (can be mineralized) called psammoma bodies. Grossly, they look like an egg yolk.

Primary CNS Lymphomas
PCNSL are usually diffuse large B-call lymphomas. Therefore, they express CD markers. Grossly, they are circumscribed and somewhat necrotic. On histology, they have lymphoid-appearing cells around blood vessels. They're honestly not that interesting in my opinion.
Craniopharyngiomas
These are benign and their origin has to do with some embryology I don't care to explain here. They have neuroendocrine effects, and can usually not be reached for resection, and are therefore considered a lifelong illness. They're usually cystic, solid, and calcified all at once (yum). They are separated into adamantinomatous (kids and adults) and papillary (only in adults). You'll see palisading epithelial cells and wet keratin.

CNS Metastasis
Most common tumor of the CNS, and can occur at any age. Lung cancer is the most common primary tumor. You're going to see edema, and usually they lodge at the gray-white junction. They will be well circumcised and will have histology consistent with the primary lesion.
Peripheral Tumors
We got Schwannomas, Neurofibromas, and Malignant peripheral nerve sheath tumors (MPNSTs). Schwannomas are painless and slow rowing, and just kinda look like a round knot on a nerve. Histologically, they are biphasic, with Antoni A (tight) and Antoni B (loose) areas. You'll also see nuclear palisading with Verocay bodies.
Neurofibromas are either solitary or plexiform. They will present with pain and loss of function. On histology, you'll see myxomatous matric and collagen fibrils leading to intense staining with reticulin.
MPNSTs are highly malignant and aggressive, and are difficult to diagnose. Grossly, you'll see necrosis. Histologically, you'll see hypercellularity, atypia, and pleomorphism.
Neurocutaneous Syndromes
You got neurofibromatosis 1 and 2, tuberous sclerosis, and Von Hippel Lindau disease. With NF1, you have a mutation on chromosome 17, which causes dark skin spots, cutaneous neurofibromas, Lisch nodules on the iris, optic gliomas, seizures, etc.
NF2 is from chromosome 22, and the patient will also sometimes have meningiomas and ependymomas. The biggest thing is bilateral vestibular schwannomas, causing hearing loss, vertigo, and facial weakness. Also common are juvenile cataracts.
Tuberous sclerosis is a disorder of cellular differentiation and proliferation. You'll see ash leaf spots, facial and fingernail angiofibromas, shagreen patches, heart tumors, renal tumor, retinal tumor, lung tumor, epilepsy, etc.
Von Hippel Lindau disease is caused by a deletion on chromosome 3. It is characterized by hemangioblastomas in the retina and CNS. You'll see symptoms from local mass effect and hemorrhage. Patient may also have renal cysts, pheochromocytomas, or pancreatic tumors.
And that's all the ones I want do, I'm not interested in going neuro, so I won't get into the dirty details. They don't really matter unless you want to be a brain surgeon or something.
13 notes
·
View notes
Note
Hi!!
in honor of protocol, tell us ab either A Growing Collection or Hollow Stars!! :)
yayy hi lo!! omg im so excited for s2 of protocol aaa!!! i can honestly do both bc theres not a whole lot to one of them atm lol
'a growing collection' is a web-alligned statement fic im working on!! the basis is it's the statment of a college student regarding an unusual and concerning change in their roommate's behavior, a downward spiral that eventually culminates in an encounter with an avatar of the web!
'hollow stars' is a much more in depth one that im super excited about!! it's a gerard keay x michael shelly alternate timeline where michael survives the great twisting after being marked by the spiral, and due increasing health issues doctors are able to find gerry's brain tumor in time. most of the story is going to revolve around relearning how to do a lot of things together, especially when gerry is in recovery and going in and out of the hospital. they might meet some friends from other timelines but overall the focus is on them learning to live in a new world and being able to put trust into each other. (also unrelated to plot but fun bit: the word astrocytoma, aka the type of brain tumor that gerry has in this version, roughly comes from the greek roots 'hollow stars' hence the title!!)
thanks for the ask!!!!
#faun answers#asks#ask game#tag game#wip game#the magnus archives#the magnus protocol#tma#tmagp#gerard keay#gerry keay#michael shelly#gerrymichael#doorkeay#tma spoilers
11 notes
·
View notes
Text
I kindly ask for your support today as I'll be leading the surgery to remove an IV astrocytoma from one of our patients. I'm feeling quite nervous. Your good vibes mean the world to me 🙏😊
78 notes
·
View notes
Text
Fidaa Wishah
Dr. Fidaa Wishah, a distinguished pediatric radiologist, specializes in the intricate field of pediatric astrocytoma radiology. With a wealth of experience and a commitment to providing the highest standard of care for young patients, Dr. Wishah plays a crucial role in diagnosing and treating pediatric astrocytoma, a type of brain tumor that occurs primarily in children.
In the realm of pediatric radiology, Dr. Fidaa Wishah stands out for her expertise and dedication. She employs advanced imaging techniques to examine and analyze astrocytomas in pediatric patients, ensuring accurate and timely diagnoses. Her compassionate approach to working with children and their families sets her apart, creating a supportive environment during what can be a challenging time for both patients and caregivers.
Pediatric astrocytoma radiology involves the use of cutting-edge technologies such as magnetic resonance imaging (MRI) and computed tomography (CT) scans. Dr. Wishah leverages these tools to visualize and understand the intricacies of astrocytomas in children, enabling her to develop tailored treatment plans that prioritize the well-being and recovery of her young patients.
Understanding the unique challenges posed by pediatric astrocytoma, Dr. Fidaa Wishah collaborates closely with a multidisciplinary team of healthcare professionals. This collaborative approach ensures comprehensive care, considering not only the radiological aspects but also the broader medical and emotional needs of the child and their family.
As a pediatric radiologist, Dr. Wishah is dedicated to staying at the forefront of her field. She actively engages in research and continuing education, contributing to advancements in pediatric astrocytoma radiology. This commitment to ongoing learning reflects her passion for improving outcomes and enhancing the quality of life for children affected by astrocytomas.
In summary, Dr. Fidaa Wishah's expertise in pediatric astrocytoma radiology, combined with her compassionate approach, makes her a trusted and invaluable resource for families facing the challenges of childhood brain tumors.
Visit us on : https://drfidaawishah.com Address: 2000 Mowry Ave, Fremont, CA 94538.
0 notes
Note
I regret to inform you that you’ve just been diagnosed with Acute Lymphoblastic Leukemia, Acute Myeloid leukemia, Kaposi Sarcoma, Primary CNS Lymphoma, Anal Cancer, Appendix Cancer, Astrocytomas Brain Cancer, Atypical Teratoid Brain Cancer, Bile Duct Cancer, Bladder Cancer, Bone Cancer, Brain Tumors, Bronchial Tumors, Lung Cancer, Burkitt Lymphoma, Carcinoma, Germ Cell Tumor, CNS Lymphoma, Cervical Cancer, Cholangiocarcinoma, Chronic Lymphocytic Leukemia, Chronic Myelogenous Leukemia, Colorectal Cancer, Craniopharyngioma, Cutaneous T-Cell Lymphoma, Endometrial Cancer, Introcular Melanoma, Retinoblastoma, Gallbladder Cancer, Gastric Cancer, Gastrointestinal Neuroendocrine Tumors, Gastrointestinal Stromal Tumors, Head and Neck Cancer, Heart Tumors, Hepatocellular Cancer, Hodgkin Lymphoma, Kidney Cancer, Leukemia, Lung Cancer, Liver Cancer, Lip and Oral Cavity Cancer, Laryngeal Cancer, Melanoma, Mycosis Fungoides, Myelogenous Leukemia, Myloproliferative Neoplasms, Mesothelioma Malignant, Nasal Cavity and Paranasal Sinus Cancer, Neuroblastoma, Nasopharyngeal Cancer, Panceatic Cancer, Papillomatosis, Paraganglioma, Pheochromocytoma, Pituitary Tumor, Penile Cancer, Prostate Cancer, Rectal Cancer, Rhabdomyosarcoma, Retinoblastoma, Salivary Gland Cancer, Kaposi Sarcoma, Osteosarcoma, Skin Cancer, Vascular Tumors, Stomach Cancer, Throat Cancer, Oropharyngeal Cancer, Hypopharyngeal Cancer, Thyroid Cancer, Thracheobronchidal Cancer, Thymoma, and Thyric Carcinoma.
-Dr. Homeless
oh shit
5 notes
·
View notes
Text

“Doctors Suck” (part 1)
TW: This story talks a lot about death and leukemia and this chapter takes place in a hospital!!
Masterlist - Next




As I open my eyes, the searing lights above me scar me. I blink rapidly, trying to get the pain to go away faster, even if it never indeed does. Once my eyes semi-adjust, my nose is hit with the burning-my-nosehairs-off smell of the chemicals. Every time I smell it, I just imagine the people who clean the rooms frantically scrubbing to try and scrub the death that occurs here. But can you honestly do that? It’s always there, never gone; the smell and everything that comes with it may leave, but the thought, the reminder, if you will, is always there. Somedays, I wonder if anyone’s died in this room I’m in. I wonder who they were and why they were here. Who misses them daily; who has that ache in their hearts that makes it hard to move on? Who can not look at a hospital anymore because it reminds them of that person’s last moments? Those last breaths? Those last “I love you”s? I make stories about those kids. I think I do it to make me feel more comfortable with the idea of dying.
Now, I know that leukemia has one of the higher survival rates, but there’s always that little voice in your head telling you, “This could be your last day, you know?” or “You could die today.” Like little Layla. She was 11. She loved animals, everything from snakes to dogs, fairies, and princesses. Her favorite color was blue for two reasons. One was that blue reminded her of her dad’s eyes. The second is that her favorite princess, Cinderella, is dressed in blue. She had a pilocytic astrocytoma brain tumor, but they caught it too late. I like to believe she’s having so much fun dancing with a prince in a blue dress; her kingdom is full of fairies and animals. Or how about little Miss Maeve? Maeve got diagnosed with leukemia, like me, but at seven years old instead of 10 like me. Even though she was so young, while she was here, in this bed, she found that she loved computers. She was exceptionally good at coding. I knew Maeve. She went to school with me; we were the best of friends. I sometimes see her sister Bronwyn around. I don’t think any of the Rojas will ever be the same. I think that’s the other scary part about death. The idea that I’m leaving all these people behind without me. I don’t want to leave them hurting like that.
Maeve, however, had a saying. “I’ll be in a better place with better beds.” I have to agree with her on this. The beds here are so uncomfortable. It feels like I’m laying on a bed of rocks with a scratchy sheet. Why are the beds so uncomfortable? Isn’t the whole point of hospitals to help people with their problems? If so, then why are we having the most uncomfortable beds on the face of the Earth in a place where you are supposed to be focused on healing yourself? Half the time, I am focused on the fact that I can never get super comfy in this stupid bed. This bed is covered in a total of 5 blankets, four pillows, and ten stuffed animals. And even still, it is not that comfy. All this just made it slightly more bearable.

a/n: RAGHDHSODNRKR first (writing) post!!! this i think will probably be one of the longer sections for this chapter mostly just cause it sets the tone and whatever. this chapter is just so long that i physically couldn’t post THAT many words in one post. the amount of just stuff that NEEDED to be said in this first chapter is crazy. anyways i hoped yall enjoyed oh em gee!!
Masterlist
tags: @wish-i-were-heather , @shattered-glass-roses , @a-menace-to-society-01 , @balladofareader , @lovethornes (im sure others said yes or something like it but i don’t remember who sooooo just tell me if you want to be tagged ig)
#emi writes <3#my untitled story#writing#original story#story#original writing#original work#stories
10 notes
·
View notes
Text
𝘼-𝙕 𝙇𝙄𝙎𝙏 𝙊𝙁 𝘿𝙄𝙎𝙀𝘼𝙎𝙀𝙎/𝙄𝙇𝙇𝙉𝙀𝙎𝙎𝙀𝙎 𝙁𝙊𝙍 𝙎𝙄𝘾𝙆𝙁𝙄𝘾/𝙒𝙃𝙐𝙈𝙋
— A
Anemia.
Adenomyosis.
Asthma.
Arterial thrombosis.
Allergies.
Anxiety.
Angel toxicosis ( fictional ).
Acne.
Anorexia nervosa.
Anthrax.
Atma virus ( fictional ).
ADHD.
Agoraphobia.
Astrocytoma.
AIDS.
— B
Breast cancer.
Bunions.
Borderline personality disorder.
Botulism.
Barrett's esophagus.
Bowel polyps.
Brucellosis.
Bipolar disorder.
Bronchitis.
Bacterial vaginosis.
Binge eating disorder.
— C
Crohn's disease.
Conjunctivitis.
Coronavirus disease.
Coeliac disease.
Chronic migranes.
Coup.
Cushing syndrome.
Cystic fibrosis.
Cellulitis.
Coma.
Cooties ( fictional ).
COPD.
Chickenpox.
Cholera.
Cerebral palsy.
Chlamydia.
Constipation.
Cancer.
Common cold.
Chronic pain.
— D
Diabetes.
Dyslexia.
Dissociative identify disorder.
Dengue fever.
Delirium.
Deep vein thrombosis.
Dementia.
Dysthimia.
Diphtheria.
Diarrhoea.
Disruptive mood dysregulation disorder.
Dyspraxia.
Dehydration.
— E
Ebola.
Endometriosis.
Epilepsy.
E-coli.
Ectopic pregnancy.
Enuresis.
Erectile dysfunction.
Exzema.
— F
Fusobacterium infection.
Filariasis.
Fibromyalgia.
Fascioliasis.
Fever.
Food poisoning.
Fatal familial insomnia.
— G
Gonorrhoea.
Ganser syndrome.
Gas gangrene.
Giardiasis.
Gastroesophageal reflux disease.
Gall stones.
Glandular fever.
Greyscale ( fictional ).
Glanders.
— H
Hookworm infection.
Hand, foot and mouth disease.
Hypoglycaemia.
Herpes.
Headache.
Hanahaki disease ( fictional ).
Hyperhidrosis.
Heat stroke.
Heat exhaustion.
Heart failure.
High blood pressure.
Human papillomavirus infection.
Hypersomnia.
HIV.
Heart failure.
Hay fever.
Hepatitis.
Hemorrhoids.
— I
Influenza.
Iron deficiency anemia.
Indigestion.
Inflammatory bowel disease.
Insomnia.
Irritable bowel syndrome.
Intercranial hypertension.
Impetigo.
— K
Keratitis.
Kidney stones.
Kidney infection.
Kawasaki disease.
Kaposi's sarcoma.
— L
Lyme disease.
Lassa fever.
Low blood pressure.
Lupus.
Lactose intolerance.
Lymphatic filariasis.
Leprosy.
— M
Measles.
Mad cow disease.
Mumps.
Major depressive disorder.
Malaria.
Malnutrition.
Motor neurone disease.
Mutism.
Mouth ulcer.
Monkeypox.
Multiple sclerosis.
Meningitis.
Menopause.
Mycetoma.
— N
Norovirus.
Nipah virus infection.
Narcolepsy.
Nosebleed.
Nocardiosis.
— O
Obsessive-compulsive disorder.
Osteoporosis.
Ovarian cyst.
Overactive thyroid.
Oral thrush.
Otitis externa.
— P
Pancreatic cancer.
Pneumonia.
Pelvic inflammatory disease.
PICA.
Premenstrual dysphoric disorder.
Psoriasis.
Parkinson's disease.
Panic disorder.
Polycystic ovarian syndrome.
Plague.
Postpartum depression.
Pediculosis capitis.
Psychosis.
Post-traumatic stress disorder.
— Q
Q fever.
Quintan fever.
— R
Rubella.
Rabbit fever.
Rotavirus infection.
Ringworm.
Restless legs syndrome.
Rhinovirus infection.
Rosacea.
Relapsing fever.
Rheumatoid arthritis.
Rabies.
— S
Shingles.
Sore throat.
Stutter.
Separation anxiety disorder.
Smallpox.
Scoliosis.
Septic shock.
Shigellosis.
Sepsis.
Social anxiety disorder.
Stroke.
Scarlet fever.
Schizophrenia.
Sleep apnea.
Sun burn.
Syphilis.
Sickle cell disease.
Scabies.
Selective mutism.
Salmonella.
Sensory processing disorder.
— T
Thyroid cancer.
Tuberculosis.
Thirst.
Trichuriasis.
Tinea pedis.
Tourette's syndrome.
Trachoma.
Tetanus.
Toxic shock syndrome.
Tinnitus.
Thyroid disease.
Typhus fever.
Tonsillitis.
Thrush.
— U
Urinary tract infection.
Underactive thyroid.
— V
Valley fever.
Vertigo.
Vomiting.
— W
White piedra.
Withdrawal.
Whooping cough.
West nile fever.
— X
Xerophthalmia.
— Y
Yersiniosis.
Yellow fever.
— Z
Zygomycosis.
Zika fever.
Zeaspora.
26 notes
·
View notes
Note
what kind was it? my fiancee has a prolactinoma. have a good day
right lateral intraventricular pilocytic astrocytoma👍
3 notes
·
View notes
Text
Oshi no Ko: Lies & Love. Aromantic Coded Narratives
I'm going to edit this more, but I'm pushing it out to feel better.
This post is an incredibly cut down and curated version of a longer academic style paper on this topic. If there are any confusing bits or inaccuracies, let me know. A lot of this is rewritten for a more digestible format.
This post is going to talk about spoilers for a majority of the Oshi no Ko manga,the short story, "45510" and the song it inspired "Idol" by Yoasobi. I will also discuss relationships with power imbalances and the sexual relationships between two minors, as Ai Hoshino was 16 when she had children. There will not be explicit detail but it is important to keep in mind the conditions of Ai's relationships.
There will be major spoilers so if you are waiting for Season 2 of the anime, don't read on. I highly encourage everyone to read the manga if you can. If you haven't started it and have just found it through this post, start by watching the anime if it is available, it is excellently produced.

Some Background:
Oshi no Ko was written by Aka Akasaka, known author of Kaguya-Sama Love is War & Renai Daikou. A lot of his work is introspective on the nature of relationships and love, Oshi no Ko being no different.
Oshi no Ko follows the story of two twin siblings, Aqua and Ruby Hoshino reincarnated fans of their new mother, Ai Hoshino. Ai Hoshino was the famous main idol of the idol group B-Komachi. The two of them previously new eachother as a doctor and patient before the latter passed away from Anaplastic astrocytoma, a form of brain cancer, and the other stabbed by Ai's stalker.
The two of them live a regular life as Ai's children until she is murdered by the same stalker that killed Aqua in his past life. After her passing they follow in the footsteps of their mother and enter the world of Japanese Entertainment in pursuit of getting revenge on their unknown father who they blame everything on.
Both of them have a very pragmatic view of the world, but they aren't the focus. Lets talk about Ai.
Ai Hoshino, 45510 & Idol:
The main point of this post is to argue that Ai lies somewhere on the Aromantic spectrum. There are some light pieces of evidence for her also being asexual, but not nearly as defintive as her aro-ness.
Ai Hoshino is the driving force of the narrative despite her story only making up around 10% of the manga. The main reason I want to talk about her is how she is displayed in Idol and "45510". For this I'll be using a fan translation by u/64990022 on Reddit the link for which can be found here.
The short story follows another member of B-Komachi looking back on Ai's popularity with jealousy.
In this we get to see an old interview of Ai's which holds her perspective on love: "I think affection comes from trust. What was it, payback? Like, to return affection with affection. But I'm a coward. I can’t believe in the words “like,” “love,” or “affection” very much. I don’t know, I’ve never really fallen in love with someone before.” This is the core of Ai's identity as an idol and how she performs. She doesn't understand love and how to be affectionate towards other people. Additionally, she doesn't seem to understand the point of marriage: “I can’t imagine it at all. Marriage? Me? Even if you say you want to marry me, how much of that is true? I can understand when people want to be with someone they like, but why marriage? Is it an expression of love? To prove that you would stay forever with that person? If that’s it then maybe I understand a little.”
Personally, I think that this rings true as an aro perspective on love and affection, not understanding the conventions of love and instead coming up with her own. Without being told that its normal to not have the ability to fall in love, Ai has given her feelings its own definition in an objective sense.
She reached the conclusion that lying was the greatest form of love, all stemming from her experience as an idol and observing the world of fans. To her, idols expressed their love to their fans all the time in their words, but none of them truly meant their words. While this is most likely true, we can see how this came to a head in the construction of the stage persona of Ai in the lyrics of "Idol" by Yoasobi;
" That "I love you" again Now, everybody is lured and captivated by you The pupil that you got The words you vocalize Even when untrue, it's your perfected Ai "
Every expression of love is a lie to captivate the audience, but to Ai, even if its untrue, its an expression of care and appreciation.
" So strong, it's you, unrivalled idol There cannot be weaknesses to find The brightest star is residing in you The gaps and shortcomings, don't show 'em Dammit, dammit Parts nobody wants to know should remain hidden One and only If it's different, no way, no way Such a true love, it's the realest Ai "
Despite not knowing how to love, Ai believe she'd give her fans the most appreciation she could by lying to them. Things like this aren't uncommon in the lives of young aros, claiming to have a crush or to love someone to fit in with the expectations people have for them. Despite all of this, she did hope that one day she would feel a 'true' love towards someone, which ended up being her children right before her death.
The Father
This is where the spoilers actually begin. Despite Ai being in a relationship with someone, there isn't much proof that this relationship was anything within the realm of healthy if not completely manipulative.
The twins' father and Ai's ex-boyfriend was Hikaru Kamiki. He was a child actor the same age as Ai, 15, and shortly after the two of them meet Ai becomes pregnant and gives birth at the age of 16. At this point Hikaru Kamiki has had multiple of these relationships and, to the reader, is known to be a serial killer of women in the entertainment industry, luring them in before killing them. He is suspected to, if not almost fully confirmed to have leaked the address of Ai to her stalker as well as which hospital she was staying in.
Needless to say, their relationship is incredibly brief and ends as soon as Ai becomes pregnant and is forced into hiding. The entirety of their relationship is shown as being based around meeting up around hotels and lacks an air of romance commonly seen in teen romances. He most likely manipulated Ai into a relationship with the intent of murdering her but there is some evidence to him actually being in love with her as he brings flowers to her grave on the anniversary of her death.
At time of posting, we don't know enough about him or their relationship to draw many conclusions but as he is the only partner Ai has every had, omitting their relationship felt disingenuous.
TLDR;
Ai's treatment of love as a whole relates greatly to an aro lens of love and the institutions of love in society. Lying about love is not uncommon among aro experiences. Idol is a bop no matter the language and its a really good aro song.
#aromantic#asexuality#manga rec#aspec coded character#ai hoshino#oshi no ko#this isn't done#but i'm tired#read Oshi no Ko#its so good#idol yoasobi#45510
31 notes
·
View notes
Text

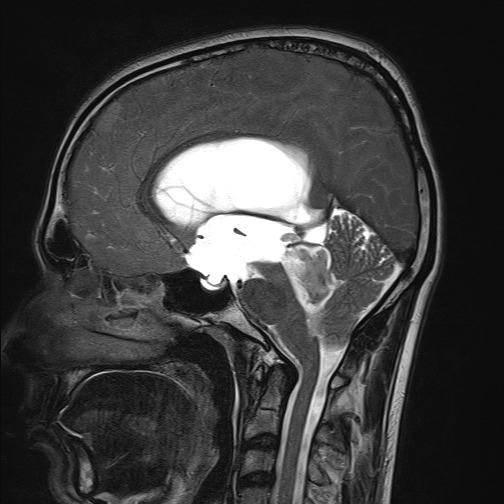
A posterior fossa tumor arising from the fourth ventricle in a child is likely an ependymoma (image 1, Case courtesy of Jini P Abraham, Radiopaedia.org, rID: 98653).
A tumor arising from the brainstem, particularly the pons, is likely a diffuse midline glioma, although pilocytic astrocytomas and gangliogliomas can also arise here (image 2, Case courtesy of Jeremy Jones, Radiopaedia.org, rID: 68486).
#TeachingRounds#FOAMed#FOAMRad#pediatrics#neurology#pedsneuro#neurosurgery#radiology#pedsrad#neuroradiology#peds
7 notes
·
View notes