#adductor gait
Explore tagged Tumblr posts
Text
The Role of Physical Therapy in Hip Replacement Recovery
Physical therapy plays a crucial role in facilitating optimal recovery and rehabilitation following hip replacement surgery, under the guidance of skilled Hip Replacement Surgeon in Jaipur like Dr. Lalit Modi. This specialized therapy focuses on restoring mobility, strength, flexibility, and overall function of the hip joint and surrounding muscles. Here’s a comprehensive look at the role of physical therapy in hip replacement recovery:

1. Early Mobilization and Joint Flexibility: Immediately after surgery, physical therapists work closely with patients to initiate gentle exercises and movements that promote early mobilization of the hip joint. These exercises aim to prevent stiffness, improve joint flexibility, and maintain range of motion. Hip Replacement Surgeon in Jaipur emphasizes the importance of starting physical therapy early to encourage healing and minimize complications associated with prolonged immobility.
2. Strengthening Muscles: Physical therapy programs are designed to target specific muscles around the hip joint, including the quadriceps, hamstrings, gluteal muscles, and hip abductors and adductors. Strengthening these muscles not only supports the new hip joint but also enhances stability, reduces joint stress, and improves overall joint function. Dr. Lalit Modi, a dedicated Orthopedic Doctor in Jaipur, prescribes progressive resistance exercises tailored to each patient’s needs and recovery stage.
3. Gait Training and Balance Improvement: Physical therapists focus on gait training techniques to help patients regain proper walking patterns and balance. This includes practicing weight-bearing activities, using assistive devices like walkers or canes if necessary, and gradually progressing to unsupported walking. By addressing gait abnormalities early in the recovery process, Hip Replacement Surgeon in Jaipur ensures safe and efficient mobility restoration.
4. Pain Management and Rehabilitation Techniques: Physical therapists employ various modalities and techniques to manage pain effectively during rehabilitation. These may include manual therapy, heat or cold therapy, ultrasound, electrical stimulation, and massage therapy. These modalities help reduce inflammation, alleviate muscle soreness, and enhance patient comfort throughout the recovery period.
5. Patient Education and Home Exercise Program: Educating patients about their condition, surgical procedure, and rehabilitation goals is integral to the success of physical therapy. Dr. Lalit Modi, a respected Orthopedic Doctor in Jaipur, emphasizes the importance of compliance with prescribed exercises and home-based rehabilitation programs. These programs are designed to maintain progress achieved during therapy sessions and promote long-term joint health and function.
6. Functional Restoration and Return to Activities: As rehabilitation progresses, physical therapists focus on functional exercises and activities that mimic daily tasks and recreational pursuits. This includes stair climbing, getting in and out of chairs, bending to pick up objects, and participating in low-impact activities. By gradually reintroducing these activities, patients regain confidence in their ability to perform routine tasks independently.
7. Monitoring Progress and Adjusting Treatment Plans: Regular progress evaluations and follow-up appointments with Hip Replacement Surgeon in Jaipur allow physical therapists to monitor recovery milestones, assess joint stability, and adjust treatment plans as needed. This collaborative approach ensures that rehabilitation goals are met and potential complications are addressed promptly.
8. Comprehensive Care and Support: Above all, physical therapy provides patients with personalized care, support, and encouragement throughout the recovery journey. Dr. Lalit Modi, a dedicated Orthopedic Surgeon in Jaipur, emphasizes a multidisciplinary approach involving physical therapists, nurses, and other healthcare professionals to optimize patient outcomes and enhance overall quality of life post-surgery.
In conclusion, physical therapy is an essential component of hip replacement recovery, focusing on enhancing mobility, strength, and function while minimizing pain and complications. Under the guidance of experienced Hip Replacement Surgeon in Jaipur like Dr. Lalit Modi, comprehensive physical therapy programs play a pivotal role in achieving optimal outcomes and restoring patients’ independence and quality of life. For more information or to schedule a consultation, visit the Jaipur Joints website and explore how personalized orthopedic care can support your recovery journey.
0 notes
Text
It could not have been a worse day to run a marathon
It could not have been a worse day to run a marathon, Anne thought. It was a cold, wet day, and by mile 18, she had a "cramp" in her hamstring and into her butt. It continued to get worse and worse as it got colder and colder. First she described that her fourth toe went numb, then the entire bottom of her foot. By the time she got to mile 24, she relates being freezing, wet, miserable, and could not feel her left foot or calf! Quit? Never! It's not even in her vocabulary….Although her running friends that were doing their best to drag her to the Outdoor Extension Cord Factory finish kept encouraging her, Anne was convinced she had somehow severed her sciatic nerve with the muscle spasm in her butt! What was going on? Piriformis syndrome!Anne had just experienced a very rude introduction to her piriformis muscle.
This muscle arises from the sacrum, passes through the sciatic notch (an opening in the pelvic bone) and attaches to a bony prominence on the side of the thigh bone (greater trochanter). The piriformis muscle acts in outward rotation of the hip. The sciatic nerve exits the spinal cord and passes through the notch in front of the piriformis (in some people the nerve actually passes right through the muscle).What went wrong that day around White Rock Lake? Anne irritated her piriformis muscle by getting tired (because her pre-race training had been, when she was being honest with herself, less than adequate), which caused her to overpronate, and then she coupled that with running on uneven surfaces and progressively colder temperatures which caused Anne to tighten all of her muscles shivering anyway!
As the piriformis became inflamed, it swelled and compressed the sciatic nerve, which caused her foot to become progressively numb.Most piriformis injuries are caused by overuse or by forced rotation of the hip caused by running on uneven surfaces. You can also irritate your piriformis by falling on your butt and having a direct blow! Pain can usually be elicited early in piriformis syndrome with direct palpation or stretching of the muscle. Anne describes pain enough to jump off the massage table pain when her piriformis was palpated for a month after the marathon!Why me? Look at your training schedule and you may see an answer. Anne did! Inconsistant training coupled with worn out orthotics and an unusually cold day! Other factors come into play like tight hip adductor muscles and excessive pronation. If your adductors are tight, the piriformis has to work harder to abduct the hip before it can help in outward rotation. Also, when your foot excessively pronates (or rolls in) when pushing off, your whole leg rotates inward and the piriformis acts to externally rotate your hip and has to work overtime every time you push off.Can I keep running with piriformis syndrome? Yes and No.
You can run in the early stages; Warm up the piriformis before running and stretch before and after any activity. Decrease your mileage at least 30-50%, slow down and avoid hills and speed work as well as uneven surfaces. If you are finding that the muscle pain is causing you to alter your gait, slow down and start therapy before you end up with another injury. Think of it this way, as the piriformis tightens, the pelvis is actually pulled upward which gives you a functional leg length discrepancy. Major biomechanical injuries to your other leg and foot can occur due to compensation! In other words, piriformis tightness in the left hip can cause arch or knee pain in the right leg!What else could it be? The best answer to piriformis syndrome is to get a true diagnosis from a sports medicine physician. Lumbar spine injuries like a herniated disc or degenerative arthritis as well as a pelvic stress fracture can mimic piriformis syndrome.
1 note
·
View note
Text
Do you really understand a runner's hips ? Coaching out things you don't like to see doesn't make it a "fix".
"All the technique in the world doesn't compensate for the inability to notice"- Elliott Erwitt
Excerpt: "So if your remedy for this runner is to just add a "loaded Farmer's carry" on the opposite side, your thinking is right if it is a strength issue in the contralateral hip. IF it is an endurance issue you need a lighter weight and more unilateral Farmer's carrying. If it is a weight management issue, you may be poking the bear. Maybe it is a multitude of issues. "
There are loads of folks taking 'this' seminar series, or 'that' one, striving for 'this' certification or 'that' one. This is trememdous, it keeps the professions moving. But, all the technique in the world doesn't mean a thing if one cannot see, feel, test, or most importantly comprehend and express a client's primary flaw(s) in mobility and stability. The right tools in unskilled hands are useless, and arguably present risks for clients.
We have said this many times, too many for certain, that what you see in your client is not their problem, it is their means of moving within their present abilities and dysfunctions for whatever reason (ie. lack of skill, endurance, strength, power etc). We have also said that a mere exercise, test or screen doesn't take one to the end zone either, they are also a mere piece of the bigger puzzle. An exercise or test also may only tell you what they are capable (or incapable of), but not why their pain or challenges exist. Thus, taking a failed test, and making it your client's new exercise does not necessarily create an environment for a remedy, it can in fact create one of a more durable compensation. And that is ok, if that is what you are searching for, if that is the emergency bandaid you need before the marathon in 3 weeks, but if you are swinging for the remedy, you may have to trudge the extra yard.
Last week we taught about some basic hip principles during our online class. Take this runner photo for example, below is a basic principle you must glean from the photo. It is a principle based off of remedial joint biomechanics, as incomplete as it is, the thought process should be one you consider and certainly comprehend. In this photo, this runner appears to have insufficient stance phase hip abductor (HAM) strength or endurance. This is in part notable because of the adduction of the contralateral thigh (this is a faulty swing leg pendulum mechanical event, and will undoubtedly lead to a cross over gait and a plethora of other gait problems).
Here is one question that should always come to mind: Are the stance phase hip abductors strong enough, or have enough endurance, to offset the body mass ? (see the line diagrams). Look at the diagram formula, and let us discuss. If the pelvis is to remain level (mostly), the D1 and D2 lever arms do not change, the D1 lever arm is always shorter and thus the HAM (Hip abductor muscle strength) will always have to be a large number to offset the BQ (body weight). If BW gets too large, there will be no HAM large enough to offset BW and the pelvis will dip, as in this runner's photo. So, it can be a weight issue, a HAM strength issue, a HAM endurance issue or both. Someone is going to win, and someone is going to pay if the system is not balances and durable. We see this in the failed frontal plane running mechanics all the time in our offices, this is a plague in runners. It is a major source of the spine, pelvis, hip knee and foot issues we see in runners. To fix these clients, you have to understand their mechanics. The latest rehab toy that you bought at after a jazzy seminar pitch doesn't replace the requisite knowledge one needs to have to understand a clients problem. Screens won't get you all the way, tests and pattern assessments won't get you all the way either. You have to do your learning part, the knowledge must precede your interventions.
So if your remedy for this runner is to just add a "loaded Farmer's carry" on the opposite side, your thinking is right if it is a strength issue in the contralateral hip. IF it is an endurance issue you need a lighter weight and more unilateral Farmer's carrying. If it is a weight management issue, you may be poking the bear. Maybe it is a multitude of issues. But, if it is a mobility issue, adding your Farmer's carry doesn't guarantee you will get the client to the promised land, and if it is a stability issue, perhaps you get close. * This article does not chase down deeper evaluation concepts such as narrow step width, femoral torsions, tibial torsions, swing phase gait mechanic failures, sagittal plane (A-P pelvis control) or rotational plane challenges to the system (failure to control limb rotation at the hip or at the foot) just to name a few. This article ONLY looked at the frontal plane concept, so hopefully one is gleaning how complex these biomechanics are. Hopefully one is gleaning at this point that this is not a spot corrective exercise prescription game, "here is the visually disturbing pattern, here is the exercise to eclipse that pattern". There does need to be some brain engagement in the process to do this right, and this means education and hands on clinical examination.
The Farmer's carry is a beautiful exercise when placed correctly in a client's regimen. There are many who say we take this game too completely, too precisely, too far, that we make this too complex and if one listens to us that one might develop stage fright to execute any intervention. Well, sorry, but we stand our ground. This is not an easy game. Too many people come to see us after intermediate regimens of training and lifting develop problems, problems that were not present at the initiation of their attempts to better they body. If one is being honest with themselves, they should ask themselves, could this have been prevented? Was the work prescribed part of the eventual deliverance? Injuries occur when loads exceed durability, skill, endurance, strength, power etc. One could make the case that if the prescriptions are correct, if the progressions are correct, that injury should be a rare thing. But injuries are not uncommon and those of us who are prescribing corrective exercises and workout regimens have to take self accountability if we are being honest with ourselves. Don't get us wrong, we are just as much a pupil on this bus as anyone else, we make mistakes all the time. But everyday we force ourselves to pause, consider, double check, reassess, to make sure that the developing patterns are sound, strong, durable and progressive, and ready for more. And when we get it wrong, we reexamine, and try again. It is all one can do.
Stir about your own clinical world with a jaundiced, questioning eye, and you should do just fine. And if you cannot get it right, get it close, prescribe something safe and watch and test for clues of developing problems in the near future. This we all call . . . . learning/ practice.
"All the technique in the world doesn't compensate for the inability to notice"- Elliott Erwitt
Shawn Allen, one of the gait guys
1 note
·
View note
Text
Scarlet Letters (TMNT Raphael x Reader)
Chapter 2/8: Patient X
After bringing Raphael in from the cold, you treat his wounds and hypothermia.
(Ch 1, Ch 2, Ch 3, Ch 4, Ch 5, Ch 6, Ch 7, Ao3)
You listen to the hitch of the stranger’s breath as you turn the key. You expect your logic and reason to speak up, to ring warning bells about inviting strangers into your home, but as you usher your companion into the apartment, you find yourself more relieved by their company than concerned.
They’ve accepted your help. They’ll soon be in from the cold. Under your care, they’ll suffer no further harm. You stare at the characters painted on their shell as they pass and wonder why this person’s safety is so important. You wonder why it’s so important to you.
As they lean awkwardly against the wall, awaiting direction, you know they’re trying desperately to hide their vulnerability. Though it goes against the desire of your compassionate heart, you stop yourself from reaching out in aid. You think a person like them, a warrior , must draw some sense of comfort from feeling in control. They are most at ease when they’re the strongest one in the room. You’ll let them hold onto that belief for a little while more. But they’ve lost a lot of blood. It’s likely they’ve been alone, braving sub-freezing temperatures, for hours. They sway where they stand. And when their eyes meet yours - unfocused and bloodshot - your breath catches in your chest.
You hold their gaze longer than you intended. It’s impossible to resist the pull it has on you. You get lost in the pain and confusion broadcasted through the green irises. An indeterminate stretch of time passes, where the stranger seems to speak to you only through their eyes.
Their eyes say: Run. They say: You should have stayed away. They say: I’m not worthy of this kindness. They say: Please don’t leave send me back out there to die.
It’s not until you break eye contact to lock the door behind you that find the words to say. “The kitchen’s past the living room.” You’re surprised to hear a tremor in your voice as you transfer your phone into your pants pocket. But the itch of fear under your skin is not borne out of worry over your own safety. It’s worry over theirs. Seeing the turtle’s unsteady gait and the way they take silent inventory of the room, you think they are more frightened than you are.
It feels foolish to hang your bloodsoaked jacket on the hook by the door, instead of tossing it directly into the small washing machine next to your bedroom, but you do it anyway out of habit. You’ll get to it later. Now, there are more important matters to which you must attend.
In the kitchen, you find the oversized turtle seated on a stool, fighting for long, even breaths. It appears to be an attempt at meditation. You take note that their choice of stool is far from the fully-stocked butcher’s block of knives. Perhaps their their position on the opposite side of the island counter is a deliberate show that they don’t mean you any harm. Or, perhaps they’re too weak to think through that far.
You let your entry into the kitchen be known by softly clearing your throat. With everything you do, you try to make it apparent that you mean your guest no harm. You know it’s dangerous to expose a person with hypothermia to direct heat, so a hot bath is out of the question - for now. You start with an offer of tea and leave the kettle steaming on the stove to lend moisture to the air.
The turtle accepts the drink with hands that shake and eyes that radiate trust. So much trust. You wonder if you’ve earned it. A fighter such as them doesn’t seem like one to trust easily, yet, even as you move behind their back, to retrieve the medical kit from the cabinet, they don’t show any concern at having you move in and out of their personal space. But they’re quiet, so you gently fill the silence.
“May I touch you?” You ask before setting the first aid box on the counter and pulling up a stool for yourself. Your companion gives a slow nod. Now that you are positioned in front of them, their eyes never stray from your hands.
Donning a pair of latex-free gloves, you tell them, “I’ll have a better idea of what we’re dealing with once I get you cleaned up. Looks like you may need stitches.” Although this can’t be good news for the turtle, you receive a nod of understanding in reply. “This is going to hurt,” you warn, like they aren’t gritting their teeth against excruciating pain already.
The peroxide bubbles over the wounds to their soft side and then the laceration on their thigh. Though their resolve hadn’t faltered while you cleaned the injury to their side, their response to their thigh injury is not so unreactive. The turtle clenches one of their fists atop the counter and their green eyes disappear behind tightly closed lids. Your patient releases a low hiss through their teeth.
To ease the peroxide’s sting, you blow on the cut along the adductor muscles. Under different circumstances, bringing your mouth so close to the inside of a person’s thigh could be considered fun, foreplay even. But as your hands frame the wound, catching excess antiseptic and wiping away blood, the intimacy is anything but sexy.
The lesion isn’t deep, but every move and flex of the muscle opens the wound. A good bandage will suffice. Same with the injuries to the side of your patient’s body. The only area that looks in need of stitches so far is a split lip.
You dab analgesic on the cuts to their face and mirror the turtle’s frown. It takes a moment for you to realize that your companion’s attention has shifted from your hands to the needles and string you’ve laid on the counter.
“I can be quick,” you say to ease their concern. Stitches aren’t part of your job description, but thanks to a rise in gang-related crime, the clinic has been overbooked and overrun with emergency walk-ins often enough that stitching up small wounds is old hat.
You hold the stranger’s face in your hands. As if of their own mind, your fingers stroke their cheeks along the underside of the threadbare mask you have yet to ask about and they have yet to remove. Their eyes flit from the floor to meet your gaze and drop again. Tracing the bottom edge of the red bandana with a caress, you decide now isn’t the time to discuss it.
“You’re going to be OK,” you start to say, but even as the words escape your lips, you worry. Their skin is clammy and pale. Cold-blooded animals need external sources of warmth. You let the press of your palms linger on their emerald skin, lending their warmth for a minute, for two. You could be imagining things, but you think that your companion sighs in relief, that they lean into your touch.
There’s no time to waste on wonder. Your patient isn’t only weak from blood loss and the fatigue of a fight, it’s possible their hypothermia is advancing.
Your fingers stitch faster than you thought you could manage; but, then again, your patients have never sat this still before. They’ve never demonstrated such patience and fortitude while under duress.
When you’re done, you cradle their face in your hands once more as if to admire your handiwork. Their cheeks are even colder than before. You force your voice to be steady as you say, “Let’s get you into a warm bath.” It’s more an order than a suggestion.
Using the countertop as support, the man-sized turtle pushes themself to stand. Still, they haven’t said a word.
You’re under their arm in an instant to offer what support you can, but a knock on the door jars your attention. The turtle squares off their shoulders at the interruption. Despite injury and fatigue, they’re taking on a fighting stance and staggering toward the wall. Years of self-defense training inform you of the obvious; this stranger fully intends to defend your home from whomever has come.
Their caution has alarms sounding off in your head. Seeing them ready to attack reminds you that their wounds aren’t the result of an accident. There had been a fight on Purple Dragon terf, and it is as likely for the person at your door to be a member of the gang looking for retribution as it is to be a friend.
A large green hand reaches for you, but a lack of coordination is another symptom of hypothermia. It takes a second try for the hand to land on your forearm. The grip is delicate, trembling.
“I’ll get rid of them,” you say reassuringly, before gently removing yourself from their hold. You signal for your companion to wait as you check the peephole. You won’t let them expose themself, especially not in their current state.
Seeing your landlord’s daughter on the other side of the door fills you with the anxiety brought on by the risk of being found harboring an unexpected, highly unusual, guest; but the relief of seeing her instead of a Dragon is enough to ease the tension in your shoulders. You whisper to the hulking figure in the shadow of the hall, “It’s OK.”
Leaning heavily against a closet door, your companion gives a nod. Their breaths come in harsh gasps, though they are trying to hide their struggle. You’ll do a more thorough exam and listen to their lungs after they’ve warmed up.
You’ll make things with Lori quick.
Pulling open the door just enough to make conversation, you’re hit by a blast of cold air and sleet. "Hey, Lor. Everything good?“ you greet the young woman at your doorstep.
“Ma sent me down to bring you this,” Lori says, nudging the space heater at her feet. “She knows it gets colder here than the other units. Though I dunno how useful it would be if any more ice builds up on the power lines.”
To bring an end to the conversation, you accept the heater without argument. “Thanks. Tell her, thanks.”
“If you wanna ride out the storm with us upstairs, you’re more than welcome-” Lori’s invitation is cut short when her gaze lands upon the fresh bloodstain on the thigh of your scrubs.
“Crazy night at the Urgent Care,” you explain, forcing a stiff chuckle. “You should get home. I’m good here.” You drag in the space heater and wrap your arms around yourself to emphasize the fact that every second at the door is a second Lori is forcing you to face the cold without a jacket. (And it’s not like you can put on the blood stained coat without drawing additional concern and/or suspicion.)
“Yeah, well,” Lori raises her hand in farewell, “stay safe.”
You spare a glance over your shoulder but find the corridor empty of your red banded companion. To Lori, you offer a tight smile and a hurried, “You too,” before closing the door.
“Where did you go?” You ask the empty hallway as you drag the wheeled space heater behind you.
Hunched over the back of the couch, your companion shivers where they stand. You abandon the space heater in an instant.
When you take the turtle by the arm, they don’t flinch. In fact, you experience a touch of deja vous. They’re leaning into you - you’re almost positive - but you can’t waste time reading into it. They’re only seeking your warmth, you tell yourself. Their temperature needs regulation ASAP. And turtles, you think, have an affinity for water.
“You. Bath. Now.”
By the time your patient is standing beside the tub, they look so pale and shaky and weak you are sure they’re about to faint. Quickly, you adjust the water at the faucet and help them in.
Although their mouth is drawn in an unreadable line, a sound like a purr rolls from the turtle’s throat as they sink into the deep bathtub. You’re glad you decided to spring for the deluxe remodel and double-wide tub. Anything smaller, you think, would be too tight a fit for the turtle’s giant shell.
You don’t dare turn on the harsh overhead lights, opting instead for the softer lamp of the vanity across from the bath. It’s the least you can do when stripping your companion of their privacy, but they haven’t voiced a wish for you to leave the room. They haven’t made any indication that they’re made uncomfortable by your company.
Water sloshes in gentle waves as you soak a washcloth. Using it, you try to warm your patient’s forehead and cheeks with slow presses of the wet cloth. You try to ease their unspoken concerns with hushed words of hope and encouragement for their recovery.
Once it seems like they’re regaining some color in their cheeks, the turtle sits forward. There’s enough room for you to wash their back, but only just.
You dip the washcloth into the bath. It’s properly soaked when you raise it again, but you pause. Your stomach flips. It seems silly that after helping the turtle clean the rest of their body you’d be hesitant to bring the cloth to their shell, but this feels different. Though a part of you wonders if the carapace is sensitive to touch at all, your heart races at the thought of feeling its bumps and edges under your palm.
Holding your breath, you squeeze warm water over the hard scales and watch it run in rivulets through the patterns of the shell - some natural and others caused by old scars and new wounds. It’s mesmerizing. The water passes over the kanji and the paint dissolves into the water, red, but thin compared to the blood that continues to seep through the turtle’s bandages. You bring your hand down against the shell to rub at the writing and your patient tenses before you both release a long breath.
“Can you feel this?” you ask in a whisper.
“Yeah,” they say and you’re shocked by the deep tone of their voice and the heavy accent on their tongue.
“Does it hurt?“ You lay your tingling palm on their shell to marvel at its texture.
“No,” they say shortly. “…it’s…” Your companion exhales another shaky breath. “It don’t hurt.”
You take up washing their back again and listen to the turtle’s slow and shallow breathing.
“Ya always take in strangers?” they ask gruffly.
In response to the accusation, you introduce yourself with the hope they’ll answer in kind.
“Raphael,” they say with a huff, turning to catch your eye. Their gaze is soft despite the hard edges the turtle insists on maintaining.
You offer a warm smile as you swipe the washcloth over your patient’s wide shoulders and neck. Their pulse is getting weaker, and slower. Their eyes are starting to spend more time closed than open. You’re surprised that they have been able to stay awake this long.
With a halting reach, you bring your hands to their mask. The weight of their hand on yours stops you from untying the knot behind their head. But the need for pause is brief. You receive a nod of consent before Raphael slowly brings their hand down to the water again.
The knot is tight, but your nimble fingers have no trouble untangling the long tails of the mask. Setting the bandana to soak in the sink with the other bands and wraps you’ve removed from the warrior’s arms, hands, and feet, you take a peek at the mirror. You have a view of the turtle’s full face for the first time. Your heart clenches as what was for so long a hardened expression droops into a sleepy frown.
You wonder if the change in Raphael’s expression has anything to do with being unmasked, or if it’s all a result of the need to recover from the night’s events. Returning to the side of the tub, you offer another smile. You bring the washcloth to Raphael’s cheek again to wipe at the clear line where the bandana had protected the top half of the turtle’s head from the elements. Raphael’s breath hitches at the attention you give.
Your voice breaks despite your resolve. "Not so much a stranger anymore, now, are ya Raphael?“
A hint of amusement flashes through their bleary eyes as their upper lip curls in what could have been the beginnings of a smile, had the movement not pulled the fresh stitches and turned the expression into a grimace of pain.
⁂
Raphael’s not a person of many words, but you learn that he was separated from his brothers during a rooftop fight before he fell. By your professional assessment, and from what he’s told you, it was the stun of the fall that kept him immobile long enough for the cold to wrack his system.
You’re almost through rinsing the last of the soap and grime from his shell when the slur of his words takes a turn for the worse. Raphael’s eyes blink heavily, though they try to hold your gaze. He slumps against the back of the tub. “…don’ think… I’m gun’…”
Following his retreat. you rise up on your knees and grab his shoulder in the hope you can keep him awake long enough to get him to a bed or the couch - somewhere he can have a proper rest. Nonetheless, his head lolls forward, and no matter how insistent you are as you squeeze his arm or pat his cheek or speak his name, you can’t keep him from slipping into unconsciousness.
#tmnt x reader#raphael x reader#tmnt raphael#tmnt raph x reader#hurt/comfort fic#gender neutral reader#bayverse tmnt#bayverse raphael
131 notes
·
View notes
Text

@sauinese // heacanons:
hc + muscles!
asking the questions the people are afraid to ask i see !!!
ferdinand’s body is built / toned for three predominant things: balance, strength, and flexibility. why ? you have probably already guessed the answer: horsemanship. i do not think people who have never ridden a horse realize quite how hard it is to do so correctly. ferdinand has been riding horses his entire life and he has certainly reaped the benefits, so to speak.
riding horses requires a shocking amount of balance and core strength: not only are you sitting on something unsteady, moving, and fast, but you are also incredibly uncomfortable ( this is where flexibility comes into play; a lot of first-time riders complain about soreness / discomfort because, yeah, traveling by horse sucks ----- it leaves you totally sore ). add onto that the additional weight of armor and weapons ----- and not just holding them, either: actually using them ! ----- and you are talking damn impressive strength and posture requirements.
as for specific muscles, horseback riding predominantly works the legs / adductors: quads, hamstrings, glutes … to be frank, he has thighs and a butt of steel. he has been riding long enough that stirrups are a laughable crutch and riding bareback is perfectly comfortable. this is part of what makes him such a great, er, great knight. he can hold a heavy axe in one hand and a heavy shield in the other, covered head-to-toe in heavy armor and his butt is still not leaving that saddle.
his entire body is very toned due to the constant tension of flexing and contracting while riding, so his muscles are overall tight rather than bulky. staying light also helps with posting ( rising out of the saddle every other stride at faster gaits ) and speed on horseback. if you look at his food preferences, he dislikes heavy foods like red meat and dairy and prefers vegetables and lean meats like fish and poultry; he keeps his meals light and controlled to avoid gaining too much muscle bulk.
in conclusion, he certainly does not have the heavy muscle that people like raphael and jeritza do, but there is a reason flayn correctly states that he is surprisingly strong for how slender he appears, and that reason is horses.
#❂ ┊ ❝ 𝐭𝐡𝐞 𝐦𝐚𝐫𝐤 𝐨𝐟 𝐧𝐨𝐛𝐢𝐥𝐢𝐭𝐲 ! / headcanon.#*thru tears* i am so sorry i made it about horses again#also yeah fun fact this dude f*cking hates cheese ? he hates basically every meal that has a lot of cheese in it haha#sauinese
2 notes
·
View notes
Text
Deductions from gait analysis observations!
As some reductionists will know Sherlock Holmes was an excellent one for examining gait and he could tell by the length of a mans stride how tall he was. This is far fetched but the gait is to my surprise very useful for certain deductions about a persons medicals state. Perhaps by examining how people walk as a reductionist you would be able to tell more important things than how tall they are even though this is usually relative to foot size. There are four phases of stance states in walking where the observed leg is on the ground and four phases of swing states where the observed leg is off the ground. The first phase is initial contact where there is a heel that makes contact and then a foot but when there is no heel strike it could be cerebral palsy. If the gluteus Maximus is not functioning properly then it could be a result of polio myelitis and may be seen by leaning back. A forward lean can happen after back surgery or due to an L3, L4 weakness or knee injury.
Briefly the other phases of stance are:
Loading response- there is a slight bend in front knee, pronation in foot, rotation of the hip and initial contact foot flattened, the muscles involved are the gluteus Maximus+ hamstrings
Midstance- pelvis has a slight drop on the swing side and you go from hip flexion to maximum hip flexion during gait. The illiosoads are working overtime and the gluteus mediums holds the pelvis upright.
Terminal stance- extension of the hip essentric activation of the illiosoads. Knee is moving to full extension. You go from pronates to supinate foot muscles
That concludes the initial stance phases then there are the foot positions in terminal stance which are forefoot Varus where the big toe of the foot is more superior then caused by a deformity in the forefoot varus but a rear foot valgus is the opposite where the pinkies are more superior on the foot.
The four swing phases are preswing, initial swing, mid swing and terminal swing
Some of the difficulties in walking through all phases are included here which can give you a vocabulary from which to diagnose gait patterns and deduce pathology in my next post.
Antalgic gait- decreased weight bearing
Ataxic gait- staggering with wide steps because of wide base of support.
Equinus gait- toe walking up on toes; can be due to habit or club foot
Gluteus Maximus gait- a backwards lurch
Gluteus mediums gait- contra lateral pelvis will drop during stance it can be bilateral creating a wobbling pelvis if there is a bilateral compensated lateral trunk lean it’s funny cause they wobble from side to side.
Hemiplegic gait- circumducted can indicate spastic plantar flexors or arthritis of the ankle foot
Parkinsonism gait- festinating short rapid steps and difficulty initiating movement
Weak quadriceps gait- hyperextend knee can indicate having had back surgery is seen in a forward lurch or lean
Scissor gait- one foot in front of the other can be cerebral palsy or weak adductors
Weak dorsiflexors- case of a functionally linger leg, if there is an increased toe in pattern it is due to femeral anteversion and if it is an increased toe out pattern then it is due to femeral retroversion
This may sound like a lot of jargon but knowing what to look for is the first step of observation in the Sherlock Holmes deduction repurituire of skills and this is one thing that you can look up on YouTube if you are still curious. The mental diseases that can be seen in walking patterns are nearly endless so I will post further on the topics of deductions regarding diseases.
21 notes
·
View notes
Text
The gait associated with an upper motor neuron lesion is referred to as a spastic, scissoring gait. The patient’s legs cross over each with each step. This gait is also associated with tight hip adductors.
3 notes
·
View notes
Photo

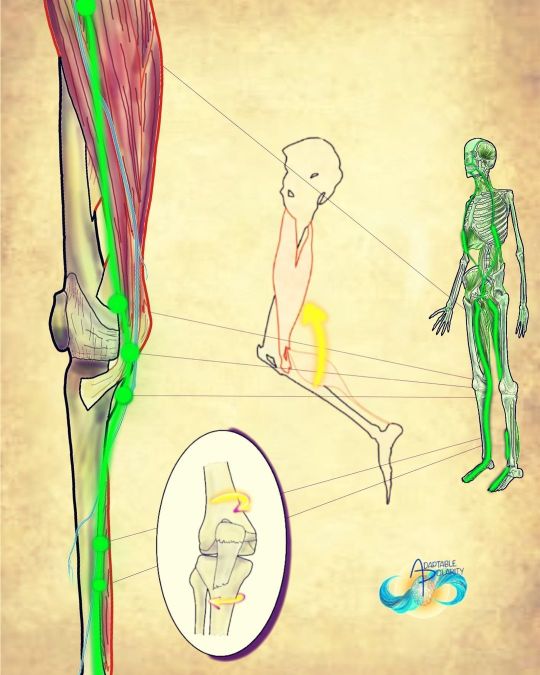
The inner coil? The ipsi coil? Stumbled upon this coil from tracing the liver and spleen meridians. I haven’t seen this documented before and so I started playing with it. When placed into gait, I really feel it highlighted in suspension, and then I can accentuate it with placing all my weight into the front foot… Feeling the coil from left neck, through my right shoulder into my right obliques, coiling through adductors counter balancing the lateral line. What’s interesting to me, if you scroll back through some of my earlier posts tracing spiral lines through fascia, there’s a big toe to eye connection previously found. Much clearer now. #fascia #fascialfitness #fascialtraining #fasciatraining #fascialstretchtherapy #myofascialtherapy #myofascial #energeticanatomy #Spiral #Spirallines #lateralline #coil #coiling #spiraling #Movement #structuralintegrationthroughmovement #movementismedicine #gait #walking #walkingislife #walkingisgoodforthesoul #walkingismytherapy #itsallconnected #Anatomy #anatomyart #anatomystudying #adaptablepolarity https://www.instagram.com/p/Cm14vO1JTVU/?igshid=NGJjMDIxMWI=
#fascia#fascialfitness#fascialtraining#fasciatraining#fascialstretchtherapy#myofascialtherapy#myofascial#energeticanatomy#spiral#spirallines#lateralline#coil#coiling#spiraling#movement#structuralintegrationthroughmovement#movementismedicine#gait#walking#walkingislife#walkingisgoodforthesoul#walkingismytherapy#itsallconnected#anatomy#anatomyart#anatomystudying#adaptablepolarity
0 notes
Text
GROIN OR INNER THIGH PAIN DUE TO ADDUCTOR SPRAIN - REMOVEMYPAIN
Adductor Strain
What is adductor strain?
Adductor muscles are a group of five muscles located in the inner thigh. These muscles help to bring the legs close to each other and stabilise the pelvis during standing and walking.
Strain, injury or imbalance of the adductor muscles is a common cause of inner thigh and groin pain, especially amongst individuals who are physically active or in competitive sports. Soccer players are commonly affected and as per one study adductor strains account for 10% of all injuries in soccer players. Other sports where associated with adductor injuries include hockey, basketball, tennis, figure skating, baseball, horse riding and karate. Tight adductor muscles can lead to hip, knee and back pain and affect our gait. Of all the adductor muscles, one called adductor longus is the one most frequently injured.
What are the symptoms of adductor sprain?
Common presenting features include:
Groin, inner thigh and lower abdominal pain. In some cases, the pain is intense at the beginning of athletic activity and is later replaced by a dull ache
Pain on sitting cross legged or when with coughing/ sneezing
Pain on activity such as
Lifting one leg as while stepping down from height or getting out of car
Turning or changing direction
Walking. In mild cases pain may be provoked by more strenuous activities such as running, kicking or performing lunges
Bruising or swelling in the painful area in severe cases
Localised tenderness in the upper inner thigh, close to where the adductor muscles attach to the pubic bone
Adductor strains are classified as
First degree: Pain without loss of strength or range
Second degree: Pain with loss of strength
Third degree: Complete disruption of muscle or tendon fibers with loss of strength
What causes adductor strain?
Adductor strains form a significant proportion of groin injuries. In a study among European soccer players, adductor muscle injuries were the second most common (23%) after hamstrings (37%). Risk factors contribution to injury include
Previous hip or groin injury
Overuse, fatigue and muscle imbalances
Weak adductors with poor flexibility
Poor hip/pelvic stability and strength
Running on hard surfaces, excessive running
Footwear
Training associated factors such as inadequate stretching, and lower levels of sport-specific training changes in training intensity, volume or type of training
Age- tendons become less able to absorb force as they age
Biomechanical abnormalities including excessive pronation or leg-length discrepancy
Genetic factors such as poor collagen
Adductor sprain can be of sudden or gradual onset. Acute injury is associated with sporting actions such as suddenly changing direction at speed, sudden acceleration in sprinting, sliding sideways or kicking. One study analysed the videos of acute adductor injuries in professional male football players and found that majority of injuries occurred in non-contact situations (71%). Common injury actions included change of direction (35%), kicking (29%), reaching (24%) and jumping (12%).
How is this condition diagnosed?
Diagnosis can be usually made clinically. MRI is used for confirming the diagnosis and assessing severity especially in chronic injuries unresponsive to conservative treatment modalities. Ultrasound scan is the alternative imaging option.
MRI Scans can give prognostic information as tears involving >50% of the cross-sectional area, tissue fluid collection, or deep muscle tears indicate more severe injury with prolonged recovery. The location of the tear is important as tears at the junction of the muscle with tendon (musculotendinous junction) can be more aggressively rehabilitated compares to one close to the joining of the tendon with bone, due to differences in the blood supply of the two areas. Tendons can be viewed as ropes tying the muscles to the bones. The musculotendinous junction is the most common site of injury in a muscle strain.
What are the treatment options for adductor strain?
Once the diagnosis has been established, treatment and prognosis are influenced by factors such as
Location of tear as those at the junction of the muscle with the bone can be dealt by aggressive rehabilitative treatment
Degree of strain/ tear
Duration of symptoms- acute or chronic
Presence of any biomechanical abnormalities such as muscular imbalances, leg length discrepancy
Acute injuries are initially treated with rest, ice, compression anti-inflammatory drugs and physical therapy with further management dependant of factors discussed earlier. Early treatment is recommended, and injections are used as required.
Education about load management and avoiding provoking factors is important. Activities like running can be replaced with swimming, walking, cycling as having baseline activities is preferred to absolute rest. Specific and individualised exercise programs have a role. A slowly progressive loading program can be used to improve strength and control of adductors, pelvis and lower limbs. The aim of the treatment initially is preventing further injury and inflammation and proving an optimal environment for healing to take place. As recovery occurs, this changes to restoration of range of motion and prevention of atrophy and then subsequently to regaining strength and flexibility.
Injections
This option is considered for individuals’ not responding to conservative measures. Injections are used in combination with physical therapy can help in confirming the diagnosis, providing early, lasting relief and possibly facilitation early return to usual activities. The options include
Steroid injections
PRP with or without needle tenotomy
Obturator Nerve block
Regardless of whichever option is used, ultrasound guidance is valuable in improving accuracy and reducing complications. Sometimes injections of the muscle in the lower abdomen (rectus abdominis muscle) are performed at the same time.
Steroid injections: There are quick to work, commonly performed injections. Steroids have anti-inflammatory effects and it may be all that is required to reduce the pain and help you actively engage with physical therapy. Some studies have shown better effects if the duration of symptoms is less that 6 weeks and hence the importance of early treatment. Post injection graded increase in activities can be commenced once the pain remains controlled for two weeks.
Platelet Rich Plasma (PRP): PRP injections are commonly used for treatment of tendinopathy and the evidence supporting their use is slowly accumulating. The procedure involves spinning one’s blood in a special machine which separates the platelets (containing the growth factors) from the other blood components. This concentrated platelet layer is then injected into the problem area to induce tissue healing. These injections take time to work with benefits becoming apparent 6 to 12 weeks after treatment. PRP injections are frequently used in combination with needle tenotomy which essentially implies repeated puncturing of the tendon to promote blood flow to the area and induce long-term healing.
Obturator Nerve Block: This injection can have added effect on top of the injections discussed previously. Obturator nerve supplies most of the adductor muscles and hence blocking this nerve can help in reducing the pain signals being transmitted. Injury or compression of the nerve leads to symptoms similar to adductor sprain and is addressed as obturator neuralgia. Obturator neuralgia can also be secondary to adductor strain and is a known cause of exercise induced groin, inner thigh pain. In this situation obturator nerve block can be especially useful.
Surgery: This option may be considered for acute complete tears with limb weakness or chronic tears with non-satisfactory response to other treatment modalities for a minimum of 6 -12 months. Surgery involves tendon release or dividing the tendon (tenotomy) and this may help to reduce the pain
Restarting activities: Return to play and activity is guided by symptom recovery as well as progress with treatment. Too soon a return is risk factor for repeat injury, which can cause chronic symptoms. Generally, after an acute strain return to sports is recommended on regaining 70% of strength and a painless range of motion. This can be usually achieved between 4 to 8 weeks, although can take up to 6 months chronic injuries. Maintaining adductor strength at a minimum of 80% of abductor strength has been shown to reduce adductor injuries.
Tags - Sport Injury Treatment in Delhi, Pain Treatment in Delhi, Best pain specialist in Delhi
For more information link - www.removemypain.com
See our documents - https://www.pearltrees.com/bestremovemypain/item437605870
#Sport Injury Treatment in Delhi#Pain Management in Delhi#Pain specialist doctor in Delhi#Dr. Amod Manocha#Removemypain
0 notes
Text
Sciatica Symptoms & Causes — Treatment by Sarwarpro
Sciatica Symptoms & Causes — Treatment by Sarwarpro
Most of us have felt numbness and tingling sensations from a sleeping foot/leg. This disappears after a few steps on bare ground. This is due to temporary compression of the sciatic nerve. However, the condition can become debilitating if it continues for more than a few weeks.we are provide best physiotherapist treatment in delhi.
Sciatica can be more of a symptom than a disease caused by sciatic nerve compression. The nerve may be compressed at the spine level or along its entire course.
The sciatic nerve, the longest nerve in the body, is the thickest. It is the terminal branch in the lumbosacral complexus.
The ventral root comprises L4, S1, and S3 nerve roots. The nerve can be divided into two parts: the tibial and peroneal.
Ventral divisions of the ventral rami L4, L5, and S1 form the tibial portion.
The ventral rami L4, L5, and S1 form the peroneal portion.
Course
The sciatic nerve is located in the pelvis and passes through the greater Sciatic notch below (or sometimes through the Piriformis Muscle) to reach the gluteal region.
It is located deep below the gluteus maximus. To enter the back of the thigh, it crosses superior, obturator internet, inferior, and quadratus femoris. To enter the lateral side of the thigh, it curves around to the greater trochanter.
It is located in the back of your thigh and lies close to the biceps femoris superficial to the adductor Magnus.
It splits into its terminal branches at the back.
It gives out terminal, articular and muscular branches throughout its life.
Muscular branches
The gluteal area, located at the back of your thigh, is not covered by branches. However, the short head of the biceps is supplied from the peroneal portion.
Branch articular:
The nerve has no branches in the peroneal and gluteal regions. However, it does have a single branch that runs to the hip joint from the back of the tibial portion.
Terminal branches
This nerve is then divided into the common peroneal and tibial nerves.
Sciatica Symptoms:
* Leg pain
* radiating leg pain
* Numbness/ tingling
* Muscular weakness
* Gait dysfunction/ abnormal walking
* Sensitivity
* Heat and cold alteration/burning sensation in your leg
Reflex impairment
* Paresthesia/dysesthesia and oedema in lower extremity
* Some symptoms may be exacerbated by increased intra-abdominal tension (cough, constipation etc.
Causes
* PIVD (prolapsed intravertebral disk)
* Spinal Stenosis
* Spondylolisthesis
* Nerve entrapment (piriformis syndrome)
Inflammatory conditions for spines/ malignancies
Traumatic pathologies
Management
Sciatica Physiotherapy
The patient is taught preventive and precautionary measures to reduce severe pain episodes. In addition, the patient is taught proper posture, ergonomics and back care. As being inactive can lead to worse outcomes, patients should be inactive.
A physiotherapist’s goal is to reduce pain through manual and therapeutic techniques.
For those who are suitable, chiropractic adjustments may be used.
Dry needling and nerve mobilization are two methods that can help relax the nerve. You can choose to do exercises depending on whether the activities are causing or alleviating the patient’s pain.
To improve spinal stability, the physiotherapist should emphasize Core strengthening.
A rehabilitation program that includes gait training and strengthening the lower limbs is recommended if there is any weakness.
We have seen thousands of patients with sciatica problems. Most of these cases have been treated successfully, and most people can live pain-free lives.
For more information visit Sarwarpro
0 notes
Text
Top Reasons You Should Love Horse riding
Horses for a long time have been great friends, offering both companionship and transport. In addition to all that, gaited horse riding supplies great physical and mental exercise for all those looking for a nontraditional method of achieving complete bodywork out.

People who love racehorses will usually tell you a moving story of how racehorses have influenced their lives. They could point out that horses get them sane. They could claim better physical wellness. Is there be proof in the scientific books that human beings reap the benefits of interacting with horses? Therefore, what do us actually know about how our lives are influenced by getting fun with racehorses?
Therapeutic riding for anyone with physical or mental afflictions is well recorded in scientific resources, showing the physical, mental, and interpersonal great things about racehorses used as therapy for folks with extra requires. A few conditions treated with gaited horse riding consist of post-traumatic pressure disorder, depression, epilepsy, autism, multiple sclerosis, polio, and imperfect paralysis.
For all those folks not experiencing these conditions, what benefits can horse riding offer? Since it works out, comparable physical, mental, and social benefits could be achieved by just about anyone who rides racehorses. The only real contraindications pointed out in the medical literature is: severe allergic reactions to race horses; physical afflictions in which there isn't enough muscle control to securely ride; no fascination with horses; intense fear, panic, or disorderly behavior; when riding triggered pain for the ride.
Everybody else is likely to enjoy the of gaited horse riding. That most likely includes you.
Strength
The position and stability that has needed makes it a must that cyclists build primary stabilization simply by engaging the pelvic, stomach, and back muscles. Remaining straight on an unsteady surface just as a horse's back requires over all primary engagement, in order to get control of your motions.
Flexibility
With the concurrent use of different parts of your body, improved flexibility is one of the numerous benefits that originate from regularly riding racehorses. On a horse, you will be keeping posture, shifting your hip and legs, controlling reins, and getting into suitable positions when you notice your horse's motions.
Cardio Exercise
Combined with the need for core strength, the parts of the body that sustain the heaviest workout, to ensure good positioning from the rider are the pelvic muscle and inner thighs. Blending the adductors where to keep the saddle and posting, or rising the horse's jogging, tones of muscles and encourages motion on the rider's behalf. An added bonus to these impacts, that could be overlooked, is the cardio exercise that horse riding provides. Taking into consideration the use of the complete body, even the easiest workouts just need more energy, effort, and cardio than any other means of exercise.
Building Self-Confidence
Even though earlier mentioned physical function might sound intense, gaited horse riding can offer restorative benefits as well. Horses are big animals and may be misunderstood as “intimidating.” It actually is amazing how understanding how to manage and connect to with these amazing pets can build self-confidence and minimize fear. It is through these approaches these highly smart animals can show us much about us.
While horse riding obviously offers a great way to get physical activity, the connections made out of horse’s fun certainly provide us a boost in a physical and mental capability. The freedom and state of mind of the horse is generally felt through our connection with the horses, and we can say thanks to them sharing their spirit.
0 notes
Text
The muscle they named wrong?
Why would you name a muscle after its supposed function when its function is actually something totally different? Probably due to what made sense from how it looked, not by how it acted. Of course, we are talking about the abductor hallucis.
Think about all the anatomy you have learned over the years. Think about all the taxonomy and how it was done: sometimes by thename of the discoverer and more often by its anatomical location. The abductor hallucis seems to be the latter.
The abductor and adductor hallicus function from approximately midstance to pre swing (1-4) (toe off), applying equal and opposite rotational vectors of force (in an ideal world) of the proximal phalynx of the hallux. This should resolve into a purely compressive force (5). In a closed chain environment, the transverse head of the adductor hallicus should act to prevent “splay” of metatarsals, along with the lumbricals and interossei (6), providing stabilzation of the forefoot (7) and rearfoot (8) during preswing, while the oblique head serves to help maintain the medial longitudinal arch.
The abductor hallicus is actually a misnomer, as it most cases it is not an abductor but rather a plantar flexor of the 1st ray, particularly the proximal hallux, (assisting the peroneus longus) and supinator about the oblique midtarsal joint axis (5). In the majority of cases, there doesn’t appear to be a separate, distinct insertion of the adductor hallicus to the base of the proximal phalynx, but rather a conjoint insertion with the lateral head of the flexor hallicus bevis into the lateral sesamoid and base of the proximal phalynx (9-11), emphasizing more of its plantar flexion function and stabilizing actions, rather than abduction.
In one EMG study of 20 people with valgus (12) they looked at activity of adductor and abductor hallucis, as well as flexor hallucis brevis and extensor hallucis longus. They found that the abductor hallucis had less activity than the adductor. No surprise here; think about reciprocal inhibition and increased activity of the adductor when the 1st ray cannot be anchoroed. They also found EMG amplitude greater in the abductor hallucis by nearly two fold in flexion.
So, the abductor hallucis seems to be important in abduction but more important in flexion. Either way, it is a stance phase stabilizer that we are beginning to know a lot more about. As for the name? You decide...
Dr Ivo Waerlop, one of The Gait Guys
1. Basmajian JV, Deluca CJ . Muscle Alive. Their Functions Revealed by Electromyography Williams and Wilkins. Baltimore, MD 1985, 377
2. Root MC, Orien WP, Weed JH. Normal and Abnormal Function of the Foot. Clinical Biomechanics, Los Angeles, CA 1977
3. Mann RA. Biomechanics of Running. In Pack RP. d. Symposium on the foot and leg in running sports. Mosby. St Louis, MO 1982:26
4. Lyons K, Perry J, Gronley JK. Timing and relative intensity of the hip extensor and abductor muscle action during level and stair ambulation. Phys Ther 1983: 63: 1597-1605
5. Michaud T. Foot Orthoses and Other Forms of Conservative Foot Care. Newton MA 1993: 50-55
6. Fiolkowski P, Brunt D, Bishop et al. Intrinsic pedal musculature support of the medial longitudinal arch: an electromyography study. J Foot & Ankle Surg 42(6) 327-333, 2003
7. Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual. Williams and Wilkins, Baltimore 1992; 529
8. Kalin PJ, Hirsch BE. The origin and function of the interosseous muscles of the foot. J Anat 152, 83-91; 1987
9. Owens S, Thordarson DB. The adductor hallucis revisited. Foot Ankle Int. 2001 Mar;22(3):186-91. Am J Phys Med Rehabil. 2003 May;82(5):345-9.
10. Brenner E.Insertion of the abductor hallucis muscle in feet with and without hallux valgus. Anat Rec. 1999 Mar;254(3):429-34.
11. Appel M, Gradinger R. [Morphology of the adductor hallux muscle and its significance for the surgical treatment of hallux valgus][Article in German] Orthop Ihre Grenzgeb. 1989 May-Jun;127(3):326-30.
12. Arinci I, Geng H, Erdem HR, Yorgancioglu ZR Muscle imbalance in hallux valgus: an electromyographic study. Am J Phys Med Rehabil. 2003 May;82(5):345-9.
#halluxvalgus #halluxabductovalgus #bunion #footmuscleactivity #gait #thegaitguys
3 notes
·
View notes
Text
Getting Started Using a Treadmill

Getting Starting Using a Treadmill
You’ve bought your first treadmill. Maybe it was because it is more convenient and less expensive than going to the gym. Or maybe you want less impact on your joints than you would get from running outside. Here are a few observations and tips that you find useful while using your treadmill. Treadmills are Easier! First, you will find that running on a treadmill seems easier than running outside. This is partially due to the different position that the treadmill puts your body in. When running outside, you actually lean forward a bit to move forward. On a treadmill, the belt is moving your feet back so your body will naturally adjust to a more upright position. Not having to move forward actually makes the running easier. However, if you adjust the incline of the treadmill to a one to three degree angle, you will be forced to lean forward and it will feel more like running outside. Not actually going anywhere also means the air is not moving over your skin to cool as well as If you were running through the air. That is why you may feel hotter and sweat more than when running outside. It also explains why many treadmills come with fans and cup holders built in. Running on a treadmill can also be easier than running outside because you set the built-in programs to match your goals and the programs adjust your intensity and time accordingly. All you have to do then is do what the program is making you do! How-To Many “heart rate programs” built in to treadmills will adjust the incline and speed of your workout to reach or maintain a target heart rate. Most home treadmills come with “contact” heart rate monitors that read your pulse by holding onto the handles. This is fine for periodic checks, but it is better to let your arms swing freely while running and not grab the handrail. Therefore, there are also wireless heart rate monitors available the wrap around your chest and transmit data directly to your treadmill. Most trainers will advise you to start out slowly (“warm up”) and end slowly (“cool down”). The purpose of the warm up seems to be to prevent injury to cold muscles by suddenly using them, but there seems to be little evidence for this. Both the warm up and cool down advice seems to have been handed down as conventional wisdom without much evidence behind them. You may feel a little uneasy when you first get off the treadmill after a workout. This seems to have something to do with seeming to move forward while actually being stationary and then seeming to move forward while actually moving forward!. Don’t worry. The brain adjusts quickly and then it’s back to reality!
How High Should I Adjust My Treadmill Incline?
The assumption under this question arises from a study (Jones, Journal of Sports Science, August 1996) that showed that a 1% treadmill incline offsets the lack of “wind” effect that occurs when moving forward over ground, making running on the treadmill with its incline set at 1% roughly equivalent to running over ground. However, the Jones study found this equivalent only when his subjects ran at speeds of a kilometer is less than five minutes. That makes sense that a fast pace would produce that sort of resistance, but that’s much faster than most people will run. It turns out that the biomechanics of running on a treadmill are not significantly different than those of running over ground. According to published research, gaits, joint movements, and power trajectories were essentially the same in both forms of running. See the study here: http://www.ncbi.nlm.nih.gov/pubmed/18460996 It has often been said that treadmill running is easier because the treadmill is actually moving you forward, while in over ground running you need to do that yourself. However, this 2008 study places this in doubt. Of course, the “give” of the treadmill’s cushioning, as well as the length of the runner’s stride also affect the perceived and real difficulty of the running both on a treadmill and over ground.
What Muscles Do You Use on the Treadmill?
Perhaps you’re using your treadmill to lose weight or improve your cardiovascular capacity. Treadmills are one of the best pieces of equipment for that. However, you may not realize that the beneficial effect that treadmill workouts can have on your muscles themselves. Following is a rundown one some of main muscles you work and strengthen by running or walking on a treadmill. Your Heart The heart is perhaps the most important muscle involved in cardiovascular exercise. That’s why they call it “cardio.” The heart really is a muscle and its strength contributes not just to overall health, but to the capacity of your other muscles as well. Regularly raising the heart rate both strengthens the heart for immediate use and improves its endurance. This then also improves the “vascular” part - blood flow -as well as the “aerobic” part – lungs. Your blood vessels and lungs may not be muscles, but their health depends partially on a strong heart. Quadriceps The quadriceps are the large muscles on the front of the thighs. They are involved every time you straighten your leg or move your foot forward. They contribute to your thighs looking either strong or skinny. Calves You already know your calf muscles are on the back of your leg between the ankle and the knee. Calves are “tightly knit,” with many more muscle cells per area than bigger muscles. This allows them to withstand very high frequency, high repetitions use for prolonged periods. Calf muscles also tend to cramp, especially in older people. Strengthening and stretching them can help prevent these cramps. Hamstrings The hamstrings are the muscles on the back of your thighs that bring your feet back toward your buttocks. The hamstrings are often overlooked, probably because you can’t see them! Yet they contribute a major portion of the force in your stride. Some people tend to “pull” or strain their hamstrings, but stretching can help prevent his. The latest thinking is that stretching after your workout is more effective than stretching before your workout. Glutes Yes, that’s them. The muscles no one forgets the name of. They keep all the rest of things working well together. Did you notice that these muscles also look much better on people who run or walk a lot? All the Rest There are many smaller and less noticeable muscles that are also strengthened and toned by treadmill workouts. These include the adductors and abductors (inside and outside of upper legs) and the many muscles of the feet. Because these muscles are all worked in the natural motions of running and walking, they are exercised in exact proportion to what is needed by those movements. Therefore, the most important thing about them is to just move! You can view our treadmills for sale by clicking here. Read the full article
0 notes
Photo

One of the more challenging knee pain that we have fixed. The knee cap was severely off track and the quad muscles are wasted away (first pic). The femur is also externally rotated. The second picture shows the result after a soft tissue release and exercise therapy session on the quad, adductor and gluteal muscles. Client was also que to correct her gait and standing posture. The goal is to let client move with less pain, strengthen up her quad and gluteal muscles and correct her standing and walking posture for the next 2 to 3 sessions. Most importantly, lots and lots of encouragement from #orthopex . . . . . . #sgsports #marathonsg #sgfitness #sgcycling #sgfitfam #sgrunning #spartan #sgfootball #sgfitspo #sgrunners #sgfit #anklepain #lowerbackpain #kneepain #kneeinjury #kneerehab #lowerback #painfreeliving #lowerbackinjury #sportsinjury #shoulderpain #sghealthy #fitnessSG #ironmantraining #injuryrecovery #injuryprevention #injuryrehab #sportstherapy #sportsnutrition #bhfyp This is not a diagnostic but a general information. Seek medical advice if in doubt. https://www.instagram.com/p/BzgAdtABCD3/?igshid=q52w6vpznf2n
#orthopex#sgsports#marathonsg#sgfitness#sgcycling#sgfitfam#sgrunning#spartan#sgfootball#sgfitspo#sgrunners#sgfit#anklepain#lowerbackpain#kneepain#kneeinjury#kneerehab#lowerback#painfreeliving#lowerbackinjury#sportsinjury#shoulderpain#sghealthy#fitnesssg#ironmantraining#injuryrecovery#injuryprevention#injuryrehab#sportstherapy#sportsnutrition
0 notes
Text
Osteitis Pubis
Osteitis Pubis is the inflammation of the pubic symphysis; the point where the left and right pubic bones meet at the front of the pelvic girdle. Individuals who are most at risk of Osteitis Pubis are those who participate in running events, especially distance runners. Weight lifters, ice skaters and dancers are also vulnerable to Osteitis Pubis, and people who have recently had prostate or bladder surgery.
Causes
Osteitis Pubis is predominantly caused by repetitive contraction of the muscles that attach to the pubic bone and the pubic symphysis, and while many things can be attributed to this, they can all be categorized into two main groups: Overload (or training errors); and Biomechanical Inefficiencies.
Overload (or training errors): Osteitis Pubis is commonly associated with sports that require a lot of running, change of direction or weight bearing activity. Other overload causes include:
Exercising on hard surfaces, like concrete;
Exercising on uneven ground;
Beginning an exercise program after a long lay-off period;
Increasing exercise intensity or duration too quickly; and
Exercising in worn out or ill-fitting shoes.
Biomechanical Inefficiencies: The major biomechanical inefficiencies contributing to Osteitis Pubis are faulty foot and body mechanics and gait disturbances. Other biomechanical causes include:
Poor running or walking mechanics;
Subluxation of the sacroiliac joints;
Tight, stiff muscles in the hips, groin and buttocks;
Muscular imbalances; and
Leg length differences.
Exercises
The following exercises are commonly prescribed to patients with osteitis pubis. You should discuss the suitability of these exercises with your osteopath prior to beginning them. Generally, they should be performed 3 times daily and only provided they do not cause or increase symptoms.
Transversus Abdominus Retraining. Begin this exercise in lying or standing. Slowly pull your belly button in “away from your belt line” and breathe normally. Your rib cage should remain relaxed and should not elevate during this process. You should be able to feel the muscle contracting if you press deeply 2cm in from the bony process at the front of your pelvis. Practise holding this muscle at one third of a maximal contraction for as long as possible during everyday activity (e.g. when walking etc.) provided it does not increase your symptoms. Repeat 3 times daily
Adductor Stretch. Begin this exercise by standing tall with your back straight and your feet approximately twice shoulder width apart. Gently lunge to one side, keeping the other knee straight, until you feel a stretch in the groin or as far as you can go without pain (figure 3). Ensure the stretch is pain-free. Hold for 15 seconds and repeat 4 times at a mild to moderate stretch provided there is no increase in symptoms.
Bridging. Begin this exercise lying on your back in the position demonstrated (figure 4). Slowly lift your bottom pushing through your feet, until your knee, hip and shoulder are in a straight line. Tighten your bottom muscles (gluteals) as you do this. Hold for 2 seconds and repeat 10 times provided the exercise is pain free.
0 notes
Photo
Movement, Muscles & Meridians: deep frontline fascia and the Liver channel The knee again… the Liver channel provided a small little swerve, literally and figuratively, in my theories, and then the ah-ha! Do knees rotate? Seems the debate is more so, is it the femur that internally rotates or tibia externally? There’s a component here where I’ve felt called to add knee flexion and the deeper hamstring. So at the Knee we have the adductors, hamstrings and even Sartorius for fun and “medial” knee rotation. If I’m looking at gait and when the knee is flexed, hip adducted, and some sort of rotation occurring at the knee while closing the kinematic chain at the foot? What happens? What moves? After 4 meridians of pursuit through the knee, we have a medial acupoint. In fact, one above, below and then at the level of the Knee joint with popliteal connections (just to emphasize that deep frontline of fascia and cure my curiosity surrounding the little knee muscle’s fascial inclusion). #muscles #movement #meridiansystem #meridians #meridian #myofascial #myofascia #fascia #fascial #deepfrontline #livermeridian #kneerotation #internalfemurrotation #externaltibialrotation #kneemechanics #biomechanics #gait #gaitanalysis #rotationalanalysis #knees #kneepaintreatment (at Santa Cruz, California) https://www.instagram.com/p/CgM4WrurM6V/?igshid=NGJjMDIxMWI=
#muscles#movement#meridiansystem#meridians#meridian#myofascial#myofascia#fascia#fascial#deepfrontline#livermeridian#kneerotation#internalfemurrotation#externaltibialrotation#kneemechanics#biomechanics#gait#gaitanalysis#rotationalanalysis#knees#kneepaintreatment
0 notes