#upper motor neuron lesion
Explore tagged Tumblr posts
Text
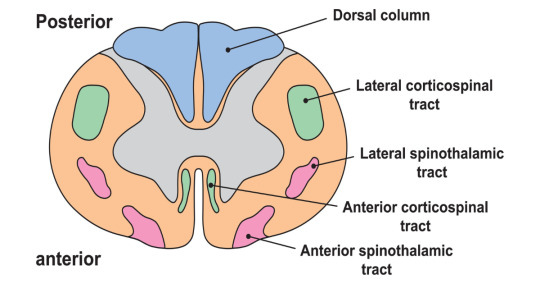
Spinal Cord: Tracts
This is the first part in a collection that goes over spinal cord injuries. We're just going to look at some of the tracts of the spinal cord first, so that I can better explain how injuries affect patients.
So first off, what does the spinal cord look like? Your spinal cord is a long collection of neural tissue with a distinct layout. The center of it has unmyelinated gray matter, while the outside has myelinated white matter. In the middle of the cord is the central canal, which is filled with cerebrospinal fluid. The entire cord is encased within the vertebral column, and spinal nerves exit between the vertebra. The top of the cord is attached to the brain, and the bottom ends within the lumbar spine as the conus medullaris. Spinal nerves continue into the sacrum as the cauda equina.
What are tracts? These are sets of specific neurons that carry out set functions. They can be generally separated into motor and sensory, and ascending or descending. Some are for visceral (organs) innervation, and others are for somatic (voluntary muscles) innervation. Each tract is made up of a lot of nerves, but each will usually synapse three times as it goes up or down the tract. Now let's get into some specific tracts. I'll only be going over the main ones, even though there are a lot more. Most of the others have to do with muscle fiber senses and reflexes, which are important but not that fun to talk about.
Ascending Sensory
The two most important ones are the dorsal column medial lemniscus (DCML) and spinothalamic (STT) tracts. The DCML carries sensory and proprioceptive information for the body. The information for the upper and lower limbs is separated into the fasciculus cuneatus and fasciculus gracilis, respectively. The fibers in the tract enter the spinal cord and travel up on the same side until they reach the medulla, where they cross over to the other side of the brainstem. Then, they continue to the brain and use the internal capsule to reach the VPL of the thalamus. From there, they can reach the primary sensory cortex.
The STT carries pain and temperature sensation. Once it enters the spinal cord, it goes up about two levels and then crosses over to the other side of the spinal cord. It also heads to the VPL of the thalamus before reaching the primary sensory cortex. The crossing over of the DCML at the medulla versus the STT around the level of innervation is very important in diagnosing spinal lesions.
The face has its own version of the DCML (principle trigeminal) and STT (spinal trigeminal), but these are a bit harder to grasp and not too relevant to the injuries I will discuss, so it's not too important to go into.
Descending Motor
The most important one is the corticospinal tract (CST). It descends from the precentral gyrus to the medulla, where it crosses over (this is why the right side of the brain controls the left side of the body). From there, it goes down to the spinal cord to synapse with a lower motor neuron.
It's important here to explain that upper motor neurons (UMN) and lower motor neurons (LMN) give rise to different symptoms when they are lesioned. UMNs go from the brain to the spinal cord, and when they are lesioned, everything "goes up." Muscle tone and reflexes increase, and you get spastic paralysis. With LMN lesions, which go from the spinal cord to the muscle, everything "goes down." Muscle tone decreases, as do reflexes. You also get flaccid paralysis.
The face also has its own version of the CST, called the corticobulbar tract. It uses the cranial nerves as LMNs. There is also the mesencephalic trigeminal nucleus, which is responsible for proprioception from the mandible and initiating the jaw jerk reflex.
Here's a pic of how everything is laid out in the spinal cord. I hope you can start to appreciate how we're going to fuck things up in the next post.
Alright, so there are the basics. This post was kinda boring, sorry, but I think the lesions post will make sense if you can understand what I'm talking about. This isn't required reading for that post (as if any of this is fucking required reading lmao), but more of an FYI if you want to know WHY certain lesions cause certain symptoms.
7 notes
·
View notes
Text
The brain stem: A pillar of motor function
The brain stem is a vital structure of the central nervous system, located at the base of the brain and connecting it to the spinal cord. It plays an essential role in many bodily functions, including the coordination of movement.
Role of the brain stem in motor function
The brain stem contains motor nuclei, groups of neurons involved in the control of movement. These motor nuclei receive information from the brain, cerebellum and spinal cord, and transmit it to the muscles via the cranial nerves and descending spinal cord pathways.

More specifically, the brainstem is involved in:
- Control of voluntary movements ♀️: The motor nuclei of the brainstem, in collaboration with the motor cortex, cerebellum and basal ganglia, are involved in the planning, initiation and execution of voluntary movements.
- Control of reflex movements ️: The brainstem contains reflex centers that control automatic and involuntary movements, such as coughing, yawning, swallowing and the blink reflex.
- Maintaining balance and posture : The brainstem receives information from the balance organs (inner ear) and the body's sensory receptors, and uses it to adjust posture and maintain balance.
- Controlling eye, head and facial movements ️: The motor nuclei of the brainstem control the muscles that move the eyes, head and face.
Structure of the brain stem
The brainstem is made up of three main parts:
- The mesencephalon: This is the upper part of the brainstem, containing motor nuclei involved in controlling eye movements and visual and auditory reflexes.
- Bridge: This is the middle part of the brain stem, containing motor nuclei involved in controlling head and facial movements, as well as nerve fibers connecting the brain to the cerebellum.
- Medulla oblongata: This is the lower part of the brain stem, containing motor nuclei involved in controlling vital functions such as breathing, heart rate and blood pressure.
Brain stem injuries
Brain stem lesions can lead to a variety of motor disorders, such as :
- Hemiplegia
- Ataxia
- tremors
- Balance disorders
- Speech disorders
- Swallowing disorders
- Breathing disorders
Conclusion
The brainstem is an essential structure of the central nervous system, playing a crucial role in the coordination of movement, as well as in many other vital functions.
Go further
#BrainStem#Neurology#CentralNervousSystem#Motricity#Movements#Coordination#Reflexes#Balance#Posture#Mesencephalon#Bridge#RachidBulb#BrainDamage#Hemiplegia#Ataxia#Trumbling#SpeechDisorders#SwallowingDisorders#BreathingDisorders#Health#Wellbeing
0 notes
Text
me and my silly little symptoms that indicate i have an upper motor neuron lesion (this makes no sense i have never had an injury beyond stubbing my toe)
#losing my mind#my physical therapy session was NOT SUPPOSED TO UNCOVER A NEW ISSUE WHY#wailing screaming crying#nat rambles#not star wars
1 note
·
View note
Note
The protagonist in my speculative fiction novel needs to have a problem that will eventually incapacitate him but starts with very subtle changes that become more apparent over time. I was thinking seizures, but that doesn't seem very subtle. Any ideas?
Actually, seizures are an excellent choice for what you are trying to accomplish. Seizures run the gamut from nearly imperceptible to impossible to ignore.
Let’s start with a definition of the term seizure, progress quickly through the different types, their etiologies (causes) and how they manifest, and finish up with a seizure disorder appropriate to your genre and protagonist.
Simply put, a seizure is an abrupt, abnormal electrical disturbance of the brain resulting in an aberrant motor (muscle) or sensory (thought or sensation) response.

Seizures can be caused by fever, head trauma, brain bleeding, chemical imbalance, drug/alcohol use, or a space-occupying lesion (a brain tumor or growing mass of any kind). For fiction purposes, we will be concentrating on the space-occupying lesions and how they affect Neurons ( the cells that allow the brain to send and receive information).
Motor neurons: The brain uses these to make muscles move.
Sensory neurons: This is how the brain receives information from the body and the outside world.
Seizures are classified into two general types: Generalized and Focal (Partial).
**When identifying seizure types, the terms Focal and Partial are interchangeable.**
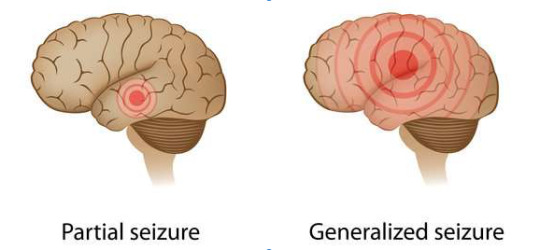
Generalized seizures tend to involve all areas of the brain. This category includes a number of subtypes:
Tonic-Clonic: Formerly referred to as a gran mal (French for great evil); this is what most people visualize when they hear the word seizure. The subject is on the ground, unresponsive, arms and legs jerking. The patient may drool or suffer incontinence (loss of bowel/bladder control). The episode lasts from a few seconds to several minutes. The event is dramatic and frightening to bystanders and the subject.
Absence: The subject stares into space as if ignoring you. These seizures last only a few seconds and are more common in the young.
Atonic: Sometimes called “drop-out” seizures, these are characterized by muscle weakness. The subject generally remains alert, but the muscles go weak and they drop what they are holding and may fall to the ground. These also are of short duration.
There are other subtypes of Generalized seizures, but the focus of our attention in this post is limited in scope and will deal primarily with the subtler and more fiction-worthy Focal variety.
Focal seizures are so named because they occur in a specific region of the brain and produce symptoms (at least initially) limited (focal) to that area.

The subject may have an altered mental status, but unlike a Generalized seizure, they are usually conscious and often aware and terrified by the manifestations of the seizure. We will explore two types of Focal seizures:
Complex Focal Seizures: These can cause blank stares, lip-smacking, pill rolling movements and laughing, crying, or screaming for no reason. This type of seizure is interesting and does have some obvious uses as a fiction vehicle.
Simple Focal Seizure: These seizures affect how we perceive our surroundings and can cause motor (movement) disorders or changes in mood or emotion. This type is especially well-suited to fiction. The following are a few of the possible symptoms:
Isolated involuntary twitching of fingers
Blank stares
Hallucinations: seeing, smelling and hearing things that are not there or morphing things that are there into something else.
Déjà vu sensations
Sudden mood or emotional changes
Dilated pupils
Seconday Generalized Seizure: This is a type of Focal seizure that spreads to the entire brain and can cause gran mal whole-body seizures. It can be because of multiple affected areas.
The inside of the skull is a closed space. When something foreign occupies that space, it exerts pressure on whatever structure is nearby. If the pressure becomes great enough, it will alter the signal passing through the Neurons causing a Focal abnormality. The nature of the abnormality depends on what part of the brain is sending or receiving the signal.

Now that you have a very basic idea of the nature of Focal (partial) seizures, let’s apply the principles to fiction.
For Example:
A young environmental scientist is taking water samples near an abandoned chemical plant. He is surprised to find tiny tadpole-like organisms swimming in the toxic runoff. The small creatures are whipping their tails and actually break the surface of the water. As he moves closer, there is a marked increase in activity. As he bends down to take a sample, one of the small red- brown creatures lands on his upper lip. Startled, he inhales deeply and feels a burning sensation in his nose. He sneezes, the sensation passes, and he returns to collecting samples. On the ride home, he develops an intense headache and ringing in his ears. He blows his nose many times, but cannot clear the noxious smell of the polluted water. Over the next several weeks, the headaches increase and he notices that he has developed an intermittent facial tic and an occasional uncontrollable twitching of his right index finger. He finds that he has difficulty forming words and misinterprets road signs and speech.
When he is found mumbling and walking in circles in the laboratory parking lot, his research partner takes him to the emergency room where a CT Scan reveals multiple small growths in various areas of his brain.
He is admitted to the hospital for further testing. That night, he complains to the nurse that he feels like “things” are crawling under his skin. She summons the on-call doctor who finds him naked on the floor having a gran mal seizure, his body covered with a red-brown rash.
Doctor Fiction expects someone to write this book and will look for it on the NYT Bestseller list next fall.
127 notes
·
View notes
Text
Behind This Mask is A Desperate Heart (Part 2)
Hospital AU
AU Summary: A fall. A single fall. It may seem like nothing until it’s all consuming. What happens when the doctors struggle to diagnosis the disease responsible for Virgil’s rapid deterioration?
Characters: Virgil, Logan, Patton, Roman, and very brief mention of Sympathetic!Deceit and Remy.
Pairings: Logince & Moxiety
Warnings: Discussion of anatomy and very brief, sympathetic deceit.
Word Count: 1865
Chapter 1 | Chapter 2 | Chapter 3 | Chapter 4 | Chapter 5 |
Virgil’s fingers curled around the stiff fabric resting in his palms as he meandered towards the white door frame. Twisting the iron knob as he went and shutting the heavy door behind him, Virgil pressed his back against the wooden plank, eyes fixed on the gown in his tight clutch.
One breath. Two breaths. By the third breath, Virgil had rested the white fabric across the sink’s rounded edge before slowly discarding his ebony attire beside the gown. With his attire stowed precariously on the sink, Virgil reached for the dotted, white hospital gown.
With the loose-fitted gown lightly brushing against his knees, Virgil noticed an abrupt tremble in his hands. To steady his shaking grasp, he clung to the upper edges of the bathroom sink as his gaze became transfixed on the mirror. His scanning eyes discerned the dangling of his bangs over charcoal eye shadow, his lips curled into a pout, and the oscillatory movements of his hands.
Grumbling, he let his grip falter from the sink and head hang low. He needed a moment. He needed a moment before seizing his clothes and emerging into his hospital suite. Frowning, Virgil shifted as his fingers trembled above the door knob. Twisting the knob and letting the door creak open meant that there really was something wrong with him.
“Mr. Poole?” A soft knock vibrated against the wooden frame.
“Oh- uh, yeah. Sorry,” snapping out of it, Virgil yanked open the door.
“I was going to assess some of your motor and sensory skills,” Logan allowed Virgil to pass him and perch cross-legged on the bed’s edge, but Virgil’s twitchy hands didn’t allude him.
“Go ahead, doc.”
“I’m going to start by testing your reflexes with a patellar reflex test, but I’m going to need you to situate your legs so that they’re dangling over the edge of the bed,” Logan slid his fingers into a set of thin, cyan gloves.
Virgil huffed, untangling his legs, and letting his feet hang.
With gloved digits, Logan skimmed his cold fingertips across Virgil’s lower leg in search for the band of tissue extending down from the patella. A few more calculating touches under Virgil’s shin, and Logan identified the patellar tendon and femoral nerve. And with a short reflex hammer, Logan struck the tendon…. Virgil’s muscles convulsed.
“Clonus,” Logan noted, scribbling the result onto a plastic clipboard in raven ink, “let’s try testing your musculocutaneous nerve.”
“Could you flex at the elbow for me?” Logan requested as a means to identify Virgil’s bicep tendon.
Virgil nodded, complying as Logan watched and palpated the antecubital fossa.
“You can relax your arm now,” Logan attentively took Virgil’s arm into his grasp with his thumb over the tendon to strike with the reflex hammer. Again, more contractions.
“Is that normal?” Virgil wore a half-frown.
“Well, no-,” Logan paused, laying his pen across his clipboard, “a normal reaction generates an easily observed shortening of the muscle. In your case, your muscles repetitively shortened after a single stimulation, which suggests that a pathologic process is affecting peripheral nerves that results in a reflex that is abnormal.”
“...huh?”
“Your muscles convulsed, which suggests there is condition affecting your nerves, but with hand tremors present, that was to be expected.”
“Any idea what it is yet?”
“Without more testing it’s hard to say, but I postulate the issue lies within your upper motor neurons. These are the neurons that carry motor information down the spinal cord to the lower motor neurons. The information that is sent from these neurons to the lower motor neurons signals muscles to contract, thus they are the source of voluntary movement. Increased muscle tone, reflexes, and weakness would all point to lesions on your upper motor neurons, but without more testing, we cannot be sure.”
“I see.”
“Speaking of such testing, I’m going to begin evaluating your muscle tone and then your gait.”
Virgil nodded, glance cast to the side.
“To start, I’m going to need you to relax for me again,” Logan clinically solicited.
To begin testing Virgil’s upper extremity muscle tone, Logan passively rolled the joints in Virgil’s wrist and upper arm to test for rigidity. Finding some resistance, Logan apacely scrawled it onto Virgil’s charts.
“Could you lie flat on your back now?”
“Uh, sure,” Virgil swung his legs over the mattress as he slanted back.
“Now, I’m going to need you to relax,” Logan repeated, pressing his palm above Virgil’s bare ankle. Moving to Virgil’s lower leg, Logan slipped his palm under his patient’s relaxed knee to suddenly bend the shin to test lower extremity muscle tone. More resistance.
“Hmm,” Logan nodded mostly to himself, “to test your gait, I’m going to need you to walk away from me and then back towards me.”
“Okay..,” Virgil sat up, shifting his frame so his feet brushed against the tile floor.
Planting his feet on the ground, Virgil strolled from the bed to the farthest wall before ambling back in the direction of the doctor. And during this process, Logan took note of Virgil’s stance, stability, and leg stiffness. He watched Virgil’s leg swings and arm swings observantly. His eyes inspected Virgil’s degree of knee bending and his rate and speed only to note a decreased left arm swing.
“Unsteady gait,” Logan jotted down.
“I take it that’s bad?” Virgil plopped back onto the bed, picking at his black nail polish.
“It just means a walking abnormality is present.”
“And?”
“And that could be caused by underlying conditions or injuries.”
“Does that mean it could be something like Parkinson’s disease?” Virgil’s heart rate quickened.
“It’s possible,” Logan admitted, “but we just can’t be sure with the little testing we’ve done.”
“My blood test can help though, right? That’s what you said earlier.”
“It’ll help us determine a diagnosis, but it’s likely the storm will delay it a couple days,” Logan glanced at Virgil apologetically, but it came off mechanically, “Anyhow, it seems optimal to take a short break from testing now.”
Collecting up his clipboard, Logan stood in the door frame, “And in the meantime, a nurse will periodically check up on you.”
“Okay…,” Virgil sighed.
With Virgil taken care of, Logan strode down the long, achromatic hallway with his clipboard pressed up against his chest and his framed eyes fixed on the nurse’s station. His shoes squeaking against newly polished floors captured the attention of patients and doctors alike. And as he passed Dr. Whittaker reviewing a patient’s extensive charts, Logan offered him a polite smile.
Now standing over the cubed nurse’s station, Logan watched as Patton’s fingers built a bridge between words, “Salutations, Patton.”
Tearing his gaze from the new monitor, Patton grinned, “Hello, Logan.”
“I’d appreciate it if you could check up on Virgil Poole for me before your shift ends in a couple hours. Maybe take a neurological history for me?” Logan didn’t waste time with idle chatter.
“Sure thing,” Patton’s eyes and nose crinkled, “I’ll pay him a visit.”
“Thanks Pat- ...Oh, Great,” Logan frowned, turning on his heel at the mere sight of Dr. Wilson’s poised approach.
“Trying to avoid me, spectacles?” Dr. Wilson tsk’d.
“Attempting to,” Logan muttered under his breath.
Feigning an offended gasp, Dr. Wilson placed his palm over his chest.
“But you adore our little chats, Lo,” he purred, inching close enough to Logan to count the careless stippling of freckles across his cheeks.
“How are you, Roman?” Patton kindly interjected, fingers resting atop black keys.
Flustered, Logan glanced down and away. He didn’t deny it.
“Much better now that Lo’s back,” Roman grinned wide like a Cheshire cat.
“I was only gone a week.”
“And a terrible week it was.”
---
Virgil peered out the frosted-over window through slats in the flimsy blinds, watching as specks of snow colored the road in ivory as the chilly air of the ceiling vent caressed his exposed skin.
“Mr. Poole?”
Virgil exhaled, shifting on the mattress to face the doorway, “more testing?”
“Just here to collect a neurological history if that’s alright,” one of Patton’s palms rested against the door frame while the other seized a clipboard.
“Go ahead, I guess,” Virgil raised his downcast eyes and shrugged slightly.
“I can come back later,” instantly noticing Virgil’s hunched posture, Patton shifted his feet to retreat.
“No- it’s fine. Ask away,” Virgil peered up before picking again at the remaining flecks of nail polish clinging to his nails.
“Okay..,” Patton reluctantly stepped into the darkened room, brows knitted into a frown, “Do you have a history of head injury or seizures?”
“No,” Virgil brushed away unattached, onyx, polish particles onto the stiff sheets.
“Have you ever had surgery involving the nervous system?” Patton continued, pen tip pressed against papers shoved under the board’s metal clip.
“No.”
“Have you ever been treated for a neurological problem?”
Another ‘no.’
“Have you ever had a serious injury?”
“If it matters, I broke my leg when I was nine,” Virgil rested his head in his now unbusy palm, gaze flitted to his crossed legs.
“How were you treated?” Patton momentarily glanced up from the charts.
“The doc had me wear a cast and use crutches for six weeks,” Virgil shrugged. He had been sketching - sketching wolves and bluishly radiant moons in the aged tree flourishing by his hinged, bedside window when he fractured his femur. Dropping his pen from the branch had sealed Virgil’s destiny as his balance departed with his attempt to capture it.
“Do you have any residual effects from breaking your leg?”
“..No.”
Another scribble from Patton.
“Do you have any other medical problems?”
“Uh,” Virgil paused hesitantly, peering up to inspect Patton’s expression, “...anxiety.”
“What about prescriptions?” Patton inquired, tilting his head, “are you currently taking any prescribed or over the counter medications?”
“No.”
Sighing, Patton scrawled the same answer in black pen on Virgil’s messy charts, “Could you tell me about your family’s medical history?”
“Dad died of a heart attack and mom’s out of the picture,” Virgil huffed bluntly, shrugging with his eyes.
“Any brothers, sisters, or cousins?” Patton donned a half-frown.
“Nope, no, and no,” Virgil mumbled, missing the distraction that unwinding the threads of his coal-colored hoodie brought him.
“Aunts? Uncles?”
“Not that I know about.”
“Oh..,” Patton frowned.
“That all you need?” Virgil cleared his throat.
“Uh-,” Snapping out of his haze, Patton replied, “yeah.”
“That’s all I need,” He quickly clarified, rubbing the back of his neck.
As Patton turned on his heel to leave, his steps faltered. He was incapable of halting his thoughts from sprinting painfully back in time to Remy. Shaking his head, Patton stopped in his footsteps and shifted to face Virgil, “Do you, uh, have anyone that will visit you? ”
“What?” Virgil tilted his head, shoulders visibly slumping once he processed the question.
Patton knew it wasn’t his right to pry, but he asked anyway.
“I’m sorry,” Patton rapidly backtracked, “I- I really shouldn’t have asked.”
“It’s whatever,” Virgil huffed, looking at his bare nails.
“I could come and check up on you occasionally if you’d like,” Patton rushed through his words.
“Uh-,” Virgil angled his head, unsure of what to make of the offer, “...sure.”
Tag list (ask to be added): @bunny222
#moxiety#logince#patton sanders#virgil sanders#sanders sides#roman sanders#logan sanders#ts virgil#ts logan#ts roman#ts patton#ts remy#thomas sanders#sanders sides fic#hospital au#logicality#analogical#flirting
49 notes
·
View notes
Photo
These color-coded illustrations show the superior (dorsal) surface and the inferior (ventral) surface of the cerebellum. The cerebellar peduncles are cut to provide this view. The ventral surface of the cerebellum is the roof of the fourth ventricle. The anterior, middle, and flocculo-nodular lobes of the cerebellum are traditional anatomic subdivisions with well-described syndromes derived from lesions. The vermis, paravermis, and lateral hemispheres are cerebellar cortical zones that have specific projection relationships with deep cerebellar nuclei (vermis with fastigial nucleus and lateral vestibular nucleus; paravermis with globose and emboliform nuclei; lateral hemispheres with dentate nucleus) which, in turn, provide neuronal feedback to specific upper motor neuronal systems that regulate specific types of motor responses. These relationships are key to understanding how the major upper motor neuronal systems are coordinated for specific functional tasks. https://www.instagram.com/p/CaVEF-pr31Q/?utm_medium=tumblr
0 notes
Text
If you haven’t heard of Hirayama’s Disease before, you’re not alone. Hirayama’s Disease is a neurological condition that primarily affects the lower cervical cord in young males, and is classed as a rare disease. Little is known about how it works, but the good news is that it’s not as serious as it may sound. Here, we offer a brief introduction to what Hirayama’s Disease looks like.
Understanding Hirayama’s Disease
Hirayama’s Disease is a rare neurological condition that causes gradually progressive atrophy of the muscles in the arms and forearms. Also known as monomeric amyotrophy (MMA), it primarily impacts young males in their late teens and early twenties. It was first defined by Keizo Hiramaya in Japan in 1959 as juvenile muscular atrophy. Hirayama’s Disease primarily affects young males in countries like India, Sri Lanka, Japan, Taiwan, and Singapore, although there have been cases in non-Asian countries too. The disease typically progresses the fastest in the first few years before stabilizing by itself.
Symptoms for Hirayama’s Disease
Typically, Hirayama’s Disease will manifest as a sudden weakness in one or both arms, leading to difficulty performing daily activities like writing or playing games. The classic symptoms for Hirayama’s Disease include:
Weakness in the hands and/or forearms
A ‘wasted’ appearance of the hands
Tremors in the hands
Unilateral / asymmetrically bilateral muscular atrophy
Excessive sweating of the palms
Impaired palmar grasp (the reflex by which one instinctively grasps something placed in the hand)
Hypertonia (in some cases)
Mild worsening of symptoms when exposed to the cold
Slow progression in the initial years followed by spontaneous stabilization
It is the disease’s tendency to stabilize it on its own, that separates it from motor neuron disease, which it is often mistaken for. There is also no sensory impairment in the hands.
Diagnosing Hirayama’s Disease
Patients who have been exhibiting symptoms for Hirayama’s Disease should visit the clinic right away. The doctor will examine the patient’s medical history and take notes on any family history of neurological conditions, before running multiple tests including blood, stool, thyroid, and urine. The diagnosis of Hirayama’s Disease is typically by exclusion, once the doctor has ruled out other possible culprits such as motor neuron disease, brachial plexopathy, multifocal motor neuropathy, and spinal cord tumours. An MRI can also detect signs like asymmetric Spinal Cord Atrophy, upper motor neuron lesions, and forward displacement of the posterior subdural sac upon neck flexion.
Treatment for Hirayama’s Disease
Hirayama’s Disease is a self-limiting condition, as the progression stabilizes on its own after some years. In addition, regular physiotherapy can help to restore strength in the arm and hand muscles and avoid secondary problems like joint stiffness or immobility.
In short, while it may be alarming to suddenly feel your hands and arms become weaker, Hirayama’s Disease is among the least serious forms of atrophy and will in fact cease progressing on its own. With early detection and intervention, you can keep the symptoms well under control and enjoy all the activities you love.
0 notes
Text
Spinal Cord: Tract Lesions
This is the second part of this series. The first explains these tracts, but it really is just to make this easier to understand. Not required to read for this post.
Here, we're going to look at different lesions in the cross section of the spinal cord to see how transverse cuts affect the nervous system. This post won't really get into different levels of lesions and very specific injuries, that will be in the next post.
Also FYI: contralateral means opposite side and ipsilateral means same side.
Brown Sequard Syndrome
This is a lesion affected the entire half of the spinal cord (right or left). It can be due to penetrating trauma, disk herniations, tumors, tuberculosis, or demyelinating diseases. It will affect the dorsal columns (DCML), spinothalamic tract (STT), and the cerebrospinal tract (CST).
Alright so since we know the STT crosses the midline about two levels above where it enters the cord, we know that there will be a loss of pain and temperature sensation on the contralateral side of the body two levels below the lesion. We can also know that there will be a thin strip of ipsilateral loss.
Because the DCML does not cross the midline until the medulla, we can know that there will be an ipsilateral loss of fine touch and proprioception below the level of the lesion.
Now for the CST. There will be lower motor neuron (LMN) signs at the level of the lesion, as the synapse of it and the upper motor neuron (UMN) is lesioned. LMN signs include decreased muscle tone and reflexes, and flaccid paralysis. The UMNs will be cut off below the level of the lesion, giving us UMN signs: increased muscle tone and reflexes, and spastic paralysis.
This is because the LMNs below the lesion are fine, and just receive no "refined" signals from the UMN, leaving them to do their own thing. When the LMNs are lesioned however, they freak the fuck out and go limp. So the muscle receives no signal whatsoever. And the UMNs are in the spinal cord so obviously if the wire is cut there is no signal down the tract.
Another thing is that if this lesion is above T1, then you get ipsilateral Horner's syndrome, which will lead to a droopy eyelid, pupil constriction, and absence of sweating on that side. This is due to damage to the sympathetic nerve fibers, which leaves parasympathetic function unopposed.
Central Cord Syndrome
This is due to something pressing outwards from the central canal of the spinal cord. Most likely, it will be due to the formation of a syrinx, which is a cyst in the middle of the spinal cord. This can be formed due to trauma, or be due to something like an Arnold-Chiari I malformation.
This will generally affect the anterior white commissure (how fibers cross in the spinal cord). This will affect the STT, which will lead to a bilateral loss of pain and temperature sensation below the level of the lesion, as fibers from both sides are compressed as they try to cross over to the other side. Typically, syrinxes are found in the cervical area, which leads to a cape-like distribution of sensation loss.
If the syrinx gets bigger, it will also start to compress the CST. This will first lead to LMN signs, and then UMN signs as it gets bigger.
Anterior Cord Syndrome
This affects the anterior 2/3rds of the spinal cord from injury to the anterior spinal artery (you only have one). It leads to deficiency in the CST, STT, and autonomic fibers. You'll see a bilateral loss of pain and temperature, UMN signs bilaterally, and bladder dysfunction (aka pissing one's pants).
Posterior Cord Syndrome
This is rarer, as you have two posterior spinal arteries. However, if both get damaged, it will cause a lesion to the posterior 1/3rd of the cord. This affects the DCML.
Another posterior lesion of the DCML is Tabes dorsalis, which is an advanced form of neurosyphilis. This is a demyelinating disease. It will also affect the DCML (obviously).
Since the DCML is bilaterally fucked, you will get a loss of fine touch and proprioception below the level of the lesion.
Subacute Combined Degeneration
This is a demyelinating disease that affects the DCML and lateral CST. It is due to a lack of Vitamin B12 (this is found in animal products, so vegetarians might want to supplement). It can also be caused by nitric oxide gas inhalation.
SCD usually starts with an increase incidence of falling as proprioception is affected. There will also be a tingling or numb sensation in the hands and feet, as well as UMN signs. Because of how the topography (fuck is that the right word??) of the spinal cord is, the hands and feet (called a "stocking and glove" distribution) will be more affected.
Conus Medullaris Syndrome
Alright, the conus medullaris is the end of the spinal cord and it plays a role in bowel, bladder, and sexual function. It is somewhere around the T12 to L2 vertebrae (it's a lot higher than most people think. Your spinal cord really isn't that long). A lesion will result in sudden and (usually) symmetrical symptoms, and both UMN and LMN signs. The LMN signs will cause the legs to be floppy and areflexic. Some people get what's called "saddle anesthesia," which is numbness in the areas where your ass and legs would touch a saddle.
Bowel and bladder dysfunction will present very soon after the lesion. This will cause decreased rectal tone, urinary retention, and an absent bulbocavernosus reflex. That last one is tested using the anal wink test. This is a reflex that makes the bunghole "wink" at you when you stroke the glans penis or clitoris (look at how much you're learning today :D).
Cauda Equina Syndrome
So the conus medullaris gives off a bunch of spinal nerves that continue through the vertebral canal in order to exit at the correct level. It looks like a horse's tail, no joke. A lesion between L2 and the sacrum will cause injury to these nerves.
The symptoms will usually be gradual and asymmetric. There will be motor impairment, but remember these are spinal nerves, so it will only be LMN signs that we see. The bowel and bladder dysfunction is similar to those in CMS. The main difference here is that we only get LMN signs and that they are typically asymmetric.
End Notes
The next post will go into a bit more fun stuff for writing. Most because I think a lot of people don't know what level of the spinal cord leads to what. But it can be really confusing, so no worries. We'll look at more specific injuries like stabbing someone in the spine. I know you guys like that, lol.
3 notes
·
View notes
Photo
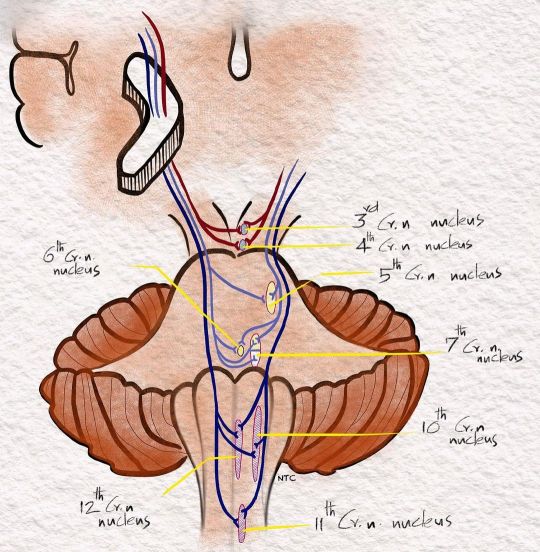
Corticobulbar fibres- The lower part of the face receives UMN fibres from the opposite side alone while the upper part of the face and all other motor cranial nerves get bilateral innervation For discussion of this image follow ‘Clinical neurology with KD’ podcast episode one -Approach to weakness, in Apple podcast, Spotify or Google podcast. Full notes are available on the neurologyteachingclub.com website The corticobulbar fibres arise from the lower third of the motor homunculus. They descend in corona radiata and genu of the internal capsule to reach the brainstem. In the midbrain, it is in the medial part of the cerebral peduncle. In the basis pontis, the corticobulbar fibres are intermixed with the corticospinal tract. All motor cranial nerves receive corticobulbar fibres from the bilateral motor cortex except the lower part of the face. The lower part of the face gets corticobulbar fibres only from the contralateral motor cortex. That is why the lower part of the opposite face alone is affected in lesions involving the motor cortex, corona radiata or internal capsule. The other cranial nerves are spared as they get 50% of their fibres from the unaffected side. So a patient with a right internal capsule lesion will have left hemiplegia with left upper motor neuron facial palsy as the lower face gets its upper motor neuron only from the opposite side. The left lower part of the face alone is affected, and the facial palsy is on the same side of hemiplegia. The facial deviation is to the opposite side of hemiplegia. The eye closure will be normal as the upper part has bilateral representation. All other motor cranial nerves lose 50% of their upper motor innervation, but they will be asymptomatic as the rest 50% takes up the function. #clinicalneurologywithkd #neurologyteachingclub #NTC #neurology #neurosciences #neuro #clinicalneurology #medicine #clinicalmedicine #kdpodcast #mbbs #medicos #doctors #neuroanatomy #casediscussion #medicinecase #casepresentation #medicineresidents #residency #neuroimages #NEET #finalmbbs #approachtohemiplegiapodcast #mcq #neetpg #uppermotorneuron #corticospinaltract #pyramidaltract #corticobulbartract #umnfacial https://www.instagram.com/p/CWPUQ87vtVK/?utm_medium=tumblr
#clinicalneurologywithkd#neurologyteachingclub#ntc#neurology#neurosciences#neuro#clinicalneurology#medicine#clinicalmedicine#kdpodcast#mbbs#medicos#doctors#neuroanatomy#casediscussion#medicinecase#casepresentation#medicineresidents#residency#neuroimages#neet#finalmbbs#approachtohemiplegiapodcast#mcq#neetpg#uppermotorneuron#corticospinaltract#pyramidaltract#corticobulbartract#umnfacial
0 notes
Link
Upper motor neuron refers to the motor neurons of the cerebral cortex and their axons which terminate at the brainstem and spinal cord while the lower motor neu
0 notes
Photo
The oculomotor nerve (III) emerges from the ventral surface of the brain stem in the interpeduncular fossa, at the medial edge of the cerebral peduncle. In conditions of increased intracranial pressure in the anterior and middle cranial fossa, such as that caused by a tumor, edema from injury, or other space-occupying lesions, the brain stem can herniate through the tentorium cerebelli, a rigid wing of dura. The resultant transtentorial herniation can compress the third nerve on one side that is ipsilateral fixed and dilatated pupil resulting from parasympathetic disruption and paralysis of medial gaze resulting from motor fiber disruption and compressing the cerebral peduncle on that same side, resulting in contralateral hemiparesis. The medullary pyramids contain the descending corticospinal tract fibers from the ipsilateral cerebral cortex, particularly from the motor and premotor cortex. The major crossing of the corticospinal tract takes place in the decussation of the pyramids (80%), producing the crossed, descending, lateral corticospinal tract in the spinal cord. An infarct in the upper reaches of the anterior spinal artery or the paramedian branches of the vertebral artery can result in damage to the ipsilateral pyramid (contralateral hemiparesis); to the ipsilateral medial lemniscus (contralateral loss of epicritic somatosensory sensations such as fine, discriminative touch, vibratory sensation, and joint position sense); and the ipsilateral hypoglossal nerve (cranial nerve XII; paralysis of the ipsilateral tongue, which deviates toward the weak side when protruded). This condition is called Dejerine's syndrome. The hemiparesis is not spastic and is characterized by mild loss of tone, loss of fine hand movements, and a plantar extensor response (Babinski's sign). It appears that isolated damage to the pyramids does not result in spasticity. Damage to other descending systems, from either the motor-related cortices or other upper motor neurons in the brain stem, must accompany pyramidal tract damage to produce spasticity. Thus, the term pyramidal tract syndrome, when used to describe spastic hemiplegia, is anatomically incorrect https://www.instagram.com/p/CaQIiIgL3yy/?utm_medium=tumblr
0 notes
Text
Lupine Publishers | Pupil Functions in Diabetes Mellitus
Lupine Publishers | Trends in Ophthalmology Open Access Journal
Abstract
Pupil is innervated by autonomic nerve system. As a result, its dimension or actions well reflects the autonomic nervous system function. Pupillary autonomic neuropathy is considered an early symptom of the development of systemic autonomic neuropathy. Pupil tests present suitable and easy methods for evaluation of autonomic nervous system function. Most patients with autonomic nervous system disorders show data of sympathetic or parasympathetic deficits in the pupil, and these findings can be detected using a combination of clinical signs, pupillometric and pharmacological tests.
Introduction
As a circular aperture in the middle of iris, along with leading aqueus humor from posterior chamber to anterior chamber, pupil has functions like regulating the amount of light entering the orbit, increasing the focusing depth, decreasing the spheric and chromatic aberrations. Under normal circumstances pupil has a diameter between 2-6mm with an average diameter of 3 mm. In neonatal period/babyhood pupilla has a smaller diameter that reachs its normal size at around 7-8 ages. On the other hand it is observed smaller in size in the old age, related on atrophy of iris stroma (1).
The muscles in the iris stroma are responsible miosis and mydriasis of pupil. These muscles are examined in two groups. The encircling muscle fibers all around the pupil are settled in the iris and they are named as circular and sphincter muscles innervated by parasympathetic system. When they contract miosis of pupil happens. The parasympathetic nerve fibers leading to miosis start from Edinger-Westphal nucleus and end in ciliary ganglion and nerve fibers that start from ciliary ganglion end in circular muscles (Figure 1).The other muscle fibers located perpendicular to the pupil are radial (dilatator) fibers. These fibers are sympathetically innervated and lead to mydriasis. The start point of the fibers that bring sympathetic impulses to the radial muscles is posterior hypothalamus. Nerve fibers originating from this region descend from mesensephalon and pons and end in the Budge ciliospinal center which is located in between 8th cervical and 2nd thoracic spinal segments of the medulla. 2nd nerve fibers for pupil which start from this region leave the medulla especially from 1st thoracic spinal segment. After being neighbor on apex of lung while ascending, these fibers join sympathetic chain at the level of inferior cervical ganglion. Fibers passing directly through the inferior and middle cervical ganglions end in upper cervical ganglion. 3rd nerve fibers starting from the upper cervical ganglion enter the cranium with internal carotid artery and communicates with ophthalmic branch of trigeminal nerve in the cavernous sinus. Sympathetic fibers reach the radial muscles, responsible for mydriasis, through the ciliary ganglion by the nasociliary nerve and the long ciliary nerves (Figures 1-2).
The tract of pupillary light reaction is composed of an afferent way that takes light impulse to the central nervous system, and an efferent way that takes the response to the iris muscles. This tract is composed of an arc containing four neurons. First neuron is in between retina and pretectal nucleus which is in the middle brain at the level of superior colliculus. Ganglion cells that start from retina end in this center. Light reaction starts with the excitation of retinal photoreseptors by light. Impulses, coming from temporal half of the retina by nerve fibers not crossing at the optic chiasma, reach the pretectal nucleus by passing through the optic tractus on the same side. However impulses coming from nasal half of the retina crosses in the chiasma and reach the pretectal nucleus by passing through the contralateral optic tractus. Nerve fibers responsible for light reaction leave the optic tractus and reach out the pretectal nucleus without a stop by lateral geniculate nucleus. The second neuron is the neuron that connects the pretectal nucleus, on one side, to both Edinger-Westphal nuclei. This neural tract is the reason of symmetric constriction of pupils at the same time when a light impulse is given. The third neuron starts with Edinger-Westphal nucleus. These parasympathetic nerve fibers interfere with the motor fibers that come from other nuclei of nervus occulomatorius and they reach the ciliary ganglion in orbita. The course of these fibers in the nervous occulomatorius is important. These superficial fibers that course between the brain stem and cavernous sinus are sensitive to pressure in this region. A lesion that presses on nervus occulomatorius in this region leads to 3rd cranial nerve palsy that also affects the pupil. The fibers related to pupil take part in the center of the nerve after the cavernous sinus. For this reason, even there are lesions in this area that cause external ophthalmoplegia, pupil fibers are preserved even. After the enterance of nervous occulomatorius into the orbita, the nerve fibers related to pupil leave the nerve and reach the ciliary ganglion within the inferior branch that goes to the inferior oblique muscle, while the fourth neuron starts from ciliary ganglion and ends in the circular muscles of iris. In orbita the ciliary ganglion is located in the extraocular muscle conus, just behind the eye ball. Only the nerve fibers that bring pupil’s light reaction form synapses in the ciliary ganglion, while the others don’t form any synapses while ending in their related places. Figure 1 Neural pathways related to accomodation start from retina like the fibers responsible for light reaction. Unlike the fibers related to light reaction, they reach the visual cortex by the route of chiasma, optic tractus and optic radiation. The source of the impulses that lead to accomodation is the peristriat cortex that is located in the 19th area on the superior end of calcarin fissure. The impulses that excite from here somehow activates the Edinger-Westphal nucleus. Fibers that start from Edinger-Westphal nucleus and come in orbita with nervus occulomatorus, reach the ciliary ganglion. A group of postganglionic nerve fibers that leave from here, goes to ciliary muscle for accomodation, another group goes to medial rectus muscle for convergence and another group goes to circular muscle of iris for miosis (1).
The examination of pupil reactions provides information about autonomic nerve system of the eye. In order to set out the functions of ocular autonomic nerve system, either pharmacological tests that show the denervation hypersensivity, or measurement methods like time of pupillary cycles that show the integrity of pupillary reflex arc can be used. In diabetes, there are some changes occur in pupil, as there are in all structures of the eye. In diabetic people, pupil is smaller than normal values, and its response to mydriatics is lower. The reason of pupil being smaller in diabetes is because of impairment of the balance between sympathetic and parasympathetic innervation. Being longer than the nerve trace of parasympathetic innervation makes the sympathetic innervation more vulnerable to development of sympathetic neuropathy. A neuropathy in sympathetic innervation causes the parasympathetic system become effective resulting in the pupil smaller in size. Failure in accomodation, can be seen in diabetes. Factors like infiltration of glycogen in the ciliary muscle, diabetic neuropathy or changes in lens structure can lead to failure in accomodation.
One of the methods that give some information about pupillary reflex arc is the measurement of pupillary cycle time. It practically gives information about the afferent and efferent ways of pupillary light reaction and the integrity of iris. This test is done by biomicroscope. The examination room is provided to be dark and the patient is waited at least two minutes to adapt to the darkness. The light of biomicroscope is set to be in horizontal position and 6x0.5 mm in size. The patient places his head on biomicroscope and he is looked at a small red light which is at least 5 metres away to avoid accomodation. Then the light of biomicroscope is slowly brought on the edge of the pupil to drop it on the retina. The pupil constricts by the effect of light. For this reason retina is exposed to darkness again and pupil tends to dilate again. Meanwhile again by the effect of light that is brought before, the pupil constricts and enlarges in a rhythmic process. When the rhythmic process starts, the time of 100 processes of constriction dilatation is determined by keeping a chronometer in milisecond (ms) type. The duration of this process can be determined both by a single time or by summing up 50+50 or 30+30+40 processes in order to get a total time of 100 constriction dilatation processes. While normal duration is between 850 ms and 950 ms, for applications done in specific clinics, it is better to determine the normal values of people in the same conditions who are in similar age groups (Figure 3).
It is shown that depending on the poor glisemic control of patients with diabetes melliltus, autonomic neuropathy can develop frequently and by affecting especially cardiovascular system vital complications can occur. At the same time it is found that symptoms of ocular autonomic neuropathy are the precursors of symptoms of systemic autonomic neuropathy. Pupil changes in diabetes can be grouped as below.
Pupil Changes in Diabetes
Myopathic causes: The storage of glycogen in iris muscles of people with diabetes has been shown in studies. There are two main muscle groups in iris as known. Being one of these muscle groups as mentioned before, circular muscle fibers that sorround the pupil are innervated by occulomotor nerve and responsible for miosis. The other muscle group is located perpendicularly to the pupil that is innervated by sypmpathetic nerve system and responsible for mydriasis. Accumulation of glycogen in iris muscles lead to contraction disfunctions. Histologically apart from accumulation of glycogen in iris muscles, vacuoles ares seen in the iris epithelium. These vacuoles are accepted as a sign of acute diabetes and thought of originating from abnormal storage of glycogen (2).
Neuropathic causes: Pupil changes developed by neuropathic causes, can be examined under three major headings.
Optic Neuropathy: Ischemic optic neuropathy are more seen in patients with diabetes. The form of pupil change in optic neuropathy is afferent pupillary defect. The direct pupillary light reaction is weaken or lost in the eye where optic neuropathy has developed. In the other eye it is the same subject for the indirect pupillary light reflex (3-5).
Cranial Neuropathy: Pupil changes can come out depending on affected occulomotor nerve that is one of the cranial nerves. In such a case there are findings like efferent pupillary defect. There are also findings added to the table which develop depending on affected motor fibers. Parasympathetic nerve fibers taking part in the third neuron start from Edinger-Westphal nucleus and extend to the ciliary ganglion that is located in the orbita. Because of the course of nerve fibers in the occulomotor nerve, any lesion located in a region between the brain stem and cavernous sinus and presses on occulomotor nerve, leads to 3rd nerve pasly which also affects pupil. On the other hand in the lesions locating after the cavernous sinus, pupillary fibers can be preserved. After the occulomotor nerve enters the orbita, the fibers that bring the pupillary light reflex reach the ciliary ganglion within the inferior branch that goes to inferior oblique muscle. In the occulomotor nerve palsy, superior, medial and inferior recti with inferior oblique muscles are affected. However usually because of ptosis developed by affected levator palpebralis superior muscle, patients don’t complain about diplopia. Usually pupil is not affected in diabetic occulomotor nerve palsy. Nevertheless it should be kept in mind that there are also diabetic palsies in which the pupil is affected.
Autonomic Neuropathy:
a) Sympathetic
b) Parasympathetic
In long lasting diabetes, a decrease in physiological hippus and a smaller pupil in size are detected. These effects are thought to result from selective diabetic autonomic neuropathy that rather shows itself significantly more in sympathetic system than parasympathetic system. Diabetic autonomic neuropathy which is a complication of diabetes, manifests itself as pupillary disfunction in the eye. Autonomic neuropathy is asymptomatic in the early stage and it can be reversible by glisemic control in the early stages of diabetes. In order to aviod permanent pathologies, scanning of autonomic disfunction is substantial. Pupil tests would be a method for the diagnosis of such a case at the earliest time. Pfeifer et al have shown that autonomic pupil disfunction has shown itself as miosis, and they has stated that this situation was due to impairment of balance between sympathetic and parasympathetic innervation, in favor of parasympathetic system (6).
Clark has determined that there are parasympathetic denervation supersensivity with %2,5 metacolin and sympathetic denervation supersensivity with %0,5 phenylephrin in patients with diabetic retinopathy. They had also determined a significant relationship between proliferative diabetic retinopathy and autonomic neuropathy. They had found that in proliferative cases, the incidence of rate of the parasympathetic retinopathy was %36, sympathetic neuropathy was %38; where as in nonproliferative cases they were %6 and %5 respectively (7).
Cahill et al have argued that the pupil responses to the %4 cocaine were same both in diabetics and control group, and for this reason they had argued that in both groups the sympathetic tract was intact (8). In the same study they had suggested that the changes in the superior cervikal ganglion were causing denervation hypersensivity in sympathetic tracts and this was the reason for the pupillary changes in diabetics. On the other side, (9) have studied the denervation sensivity of aproclonidin. They have shown the denervation sensivity in diabetic cases and found it to be proportionate to the duration and severity of the disease (5).
Söylev et al. (10) have studied the response to diluted pilocarpine in groups of diabetic patients with or without retinopathy and in control group. They have found a response to diluted pilocarpine more in diabetic group with retinopathy, according to diabetic group without retinopathy and control group (10). At the same time they have detected that marked mydriasis developed with diluted phenylephrine in diabetic group with retinopathy, which was found significantly different comparing to the other groups.
Clark et al. (11) have detected the rate of the defect in pupillary reflex arc as %88,5 in patients with proliferative diabetic retinopathy. They have also mentioned that this result was the earliest sign of autonomic nerve disfunction (11). Pena et al. (12) emphasized that the pupillary symptoms were the earliest evidence of autonomic nerve disfunction.
In our study the pupil cycle time was found longer in diabetic cases. At the same time the rate of inability of measuring pupil cycle time was found more in the diabetic group. Pupil cycle time was found related both with the existence of diabetic retinopathy and the level of periferic retinopathy (13). As seen in all structures of eye, there are some changes in diabetes that can be seen in the pupil, too. These changes can be basicly myogenic or neurogenic. As a complication of diabetes, diabetic autonomic neuropathy can show itself as pupillary disfunction in the eye, so early diagnosis is significant. Pupil findings usually come out in direct proportion to the length and severity of diabetes (14). Rarely they can be seen in the early stages of diabetes; even sometimes before the somatic neuropathy. The findings of cardiovascular system among the systemic autonomic neuropathy findings are vitally important. By determining the abnormalities of pupillary function earlier, growth of autonomic function abnormalities of cardiovascular system may be prevented and measures for diabetic regulation may be taken. Autonomic neuropathy is asymptomatic in early phase and it can be reversible by glisemic control in early stages. From this point, scanning for autonomic disfunction is important to prevent permanent pathologies. Pupil tests can be methods for diagnosis of this situation in the earliest time
https://lupinepublishers.com/ophthalmology-journal/pdf/TOOAJ.MS.ID.000122.pdf
https://lupinepublishers.com/ophthalmology-journal/fulltext/pupil-functions-in-diabetes-mellitus.ID.000122.php
For more Lupine Publishers Open Access Journals Please visit our website: https://lupinepublishersgroup.com/
For more Trends in Ophthalmology Please Click
Here: https://lupinepublishers.com/ophthalmology-journal/
To Know more Open Access Publishers Click on Lupine Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers Follow on Twitter : https://twitter.com/lupine_online
0 notes
Photo
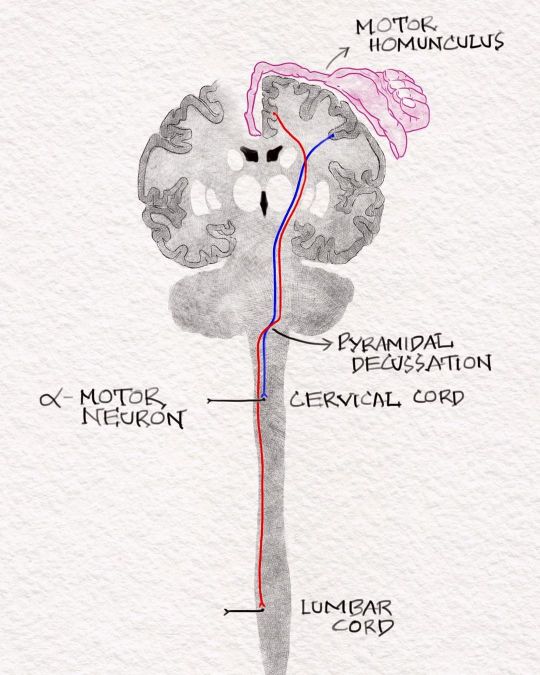
Schematic diagram showing the Upper Motor Neuron. For discussion of this image follow ‘Clinical neurology with KD’ podcast episode one -Approach to weakness, in Apple podcast, Spotify or Google podcast. Full notes are available on the neurologyteachingclub.com website. The corticospinal tracts are excitatory and mostly use glutamate as the neurotransmitter. It starts in the motor cortex and ascents in corona radiata to reach the anterior 2/3 of the posterior limb of the internal capsule. In the internal capsule, the fibres to the upper extremity are arranged more anteriorly. They lie close to the corticobulbar fibres, which travel in the genu of the internal capsule. The corticospinal fibres then ascend down in the middle 3/5 of the cerebral peduncle in the midbrain, basis pontis and the medullary pyramids. At the lower end of the medulla, 75%-90% of fibres cross over to the opposite side to form the lateral corticospinal tract in the spinal cord. The fibres then ascend down through the cervical, thoracic, lumbar and sacral spine to reach the corresponding spinal segment it innervates and synapses with alpha motor neurons at that level. A lesion anywhere in this pathway from the motor cortex through corona radiata, internal capsule, midbrain, pons, and medulla and then crossing to the opposite side in lateral corticospinal tract in cervical, thoracic, and lumbar spine can produce weakness with UMN features like spasticity, hyperreflexia and upgoing plantar. #clinicalneurologywithkd #neurologyteachingclub#neurologypodcast #NTC #firstpodcast #neurology #neurosciences #neuro #clinicalneurology #medicine #clinicalmedicine #kdpodcast #mbbs #medicos #doctors #neuroanatomy #casediscussion #medicinecase #casepresentation #medicineresidents #residency #neuroimages #neurophysiology #NEET #mcq #neetpg #uppermotorneuron #corticospinaltract #pyramidaltract https://www.instagram.com/p/CWPTyUYvuNn/?utm_medium=tumblr
#clinicalneurologywithkd#neurologyteachingclub#neurologypodcast#ntc#firstpodcast#neurology#neurosciences#neuro#clinicalneurology#medicine#clinicalmedicine#kdpodcast#mbbs#medicos#doctors#neuroanatomy#casediscussion#medicinecase#casepresentation#medicineresidents#residency#neuroimages#neurophysiology#neet#mcq#neetpg#uppermotorneuron#corticospinaltract#pyramidaltract
0 notes
Video
Clonus - (from the Greek for "violent, confused motion") is a series of involuntary, rhythmic, muscular contractions and relaxations. Clonus is a sign of certain neurological conditions, particularly associated with upper motor neuron lesions involving descending motor pathways, and in many cases is, accompanied by spasticity. Just about every definition of clonus talks about the involuntary movement but you can learn to work with it. I know how to trigger most of my bodies responses and how to suppress them. I normally don't go through this shaking while working on the balance board but wanted to show what clonus looks like, and turning it off and on. I regularly excersice and do activities that are the hardest for my body so I can learn to tolerate them or improve the signal. It's been fascinating to me that I can somewhat find the neuro pathways that were damaged by going through certain movements positions. Always learning 😁 #quadriplegic #tetraplegic #sci #spinalcordinjury #paralyzed #improve #everydamnday #recovery #rebuild #gymlife #balance #consistancy #dedication #clonus #physicaltherapy #neuro #neurology #hope #faith #grateful #myjourney #believe
#dedication#rebuild#gymlife#sci#myjourney#improve#faith#paralyzed#recovery#grateful#hope#neuro#everydamnday#quadriplegic#believe#neurology#consistancy#spinalcordinjury#clonus#physicaltherapy#tetraplegic#balance
1 note
·
View note
Text
300+ TOP PHYSIOLOGY Objective Questions and Answers
PHYSIOLOGY Multiple Choice Questions :-
1. Damage to sensory area 1 of the cerebral cortex results in a) Loss of perception of pain b) Loss of tactile and two point discrimination c) Loss of perception of touch d) Loss of only tactile discrimination Ans:b 2. Volume of CSF is about a) 50ml b) 100ml c) 150 ml d) 200 ml Ans:c 3.Dissymmetria is seen in a) Extra pyramidal lesions b) Cerebellar lesions c) Pyramidal lesions d) Cortical lesions Ans:b 4.Floculonodular lobe of cerebellum is concerned with a) Equilibrium b) Co-ordination c) Baroreception d) Chemoreception Ans:a 5.In the postnatal period the greatest growth in the grey matter of the C.N.S is of a) Neuron cell number b) Length of axon c) Dendritic tree d) Size of Perikaryon Ans:c 6.CSF production per minute a) 0.30-0.35 ml/min b)0.5ml/min c)2ml/min d) 1 ml/min Ans:a 7.Function of GABA on CNS is a) Neuronal inhibition b) Neuronal activation c) Glial cell inhibition d) Glial cell activation Ans:a 8.The EEG rhythm having lowest frequency is: a) Alpha b) Beta c) Delta d) Theta Ans:c 9.Medial geniculate body is concerned with a) Hearing b) Vision c) Smell d) Taste Ans:a 10.True statement regarding CSF is a)Daily production b)CSF analysis rules out active secretion as a cause of formation of CSF c)It flows from III ventricle to the IV ventricle d) Produced only by choroid plexus Ans:c

PHYSIOLOGY MCQs 11. In cerebellar disease, all the statements are correct except a) The Romberg's sign is positive b) There is Adiodokokinesia c) There is pendular knee jerk d) There is involuntary tremor Ans:d 12.Swallowing center is situated in a) Midbrain b) Pons c) Medulla d) Cerebellum Ans:c 13.Hyper kinetic syndromes such as chorea and athetosis are usually associated with pathological changes in: a) Motor areas of cerebral cortex b) Anterior hypothalamus c) Pathways for recurrent collateral inhibition in the spinal cord d) Basal ganglia complex Ans:d 14. An EEG: a)Provides indication of intelligence b)Tends to show waves of smaller amplitude during deep sleep than of alert state c)Show waves with a lower frequency during intense thought than during sleep d)Is bilaterally symmetrical Ans:d 15.The following is true about brain metabolism except a) Use fatty acid in starvation b) In resting state 60% of total energy utilized c) Ketone bodies are used in starvation d) Has no energy store Ans:a 16.Satiety center in hypothalamus is regulated by: a) Gastric dilatation b) Blood glucose levels c) Blood insulin leve d) All of the above Ans:b 17. In hippocampus EEG waves are a) Alpha wave b) Beta wave C) 65 mm of Hg b)55mmofHg Ans:d 18.EEG with spike and dome pattern is characteristic of epilepsy a) Jacksonian b) Grandmal c) Petitmal d) Temporal lobe Ans:c 19.Buerger waves (alpha waves) of EEG have the rhythm per sec of: a) 0-4 b)4-7 c)8-13 d) 13-30 Ans:c 20.All the following are more in CSF compared to plasma except a)Mg b)Cl c)HC03 d) Glucose Ans:d 21. During light sleep, the sleep spindles that appear have the frequency of: a) 1 -2/sec b) 6-12/sec c) 14-16/sec d) 21 -26/sec Ans:c 22.Up to what systolic pressure is the brain capable of auto regulation a) Dorsomedian nucleus of hypothalamus b) Ventromedian nucleus of hypothalamus c) Perifornical region d) 75mmofHg Ans:a 23. pH of CSF is: a) 7.13 b) 7.23 c) 7.33 d) 7.40 Ans:b 24.Temporal lobe lesion causes: a) Homonymous upper quadrantinopia b) Homonymous lower quadrantinopia c) Bitemporal hemianopia d) Binasal hemianopia Ans:a 25.Hyperphagia results from lesion of a) Thalamus b) Cerebral cortex c) Ventromedial region of supra-optic nucleus d) Ventrolateral region of supra-optic nucleus Ans:c 26. Delta waves in EEG are seen in a) Deep sleep b) REM sleep c) Awake with eyes open d) Awake with eyes closed Ans:a 27. Nightmares are seen in a) REM sleep b) NREM stage II c) NREM stage III d) NREM stage IV Ans:a 28. Which of the following are true of median eminence a) Portion of ventral hypothalamus b) Hypothalamo hypophyseal vessels arise here c) Outside the blood-brain barrier d) All are correct Ans:d 29. Unconscious kinesthetic sensations are carried by a) Posterior columns b) Ventral spinothalamic tract c) Anterior spinothalamic tract d) Lateral spinothalamic tract Ans:a 30. Crossed extensor reflex is a a) Withdrawal reflex b) Postural reflex c) Monosynaptic reflex d) Sympathetic reflex Ans:a 31.Renshaw cell inhibition is an example of a) Feed-forward inhibition b) Oscillating motor activity c) Circuitry for bio feedback d) All of the above Ans:a 32.Arousal response is mediated by a) Dorsal column b) Reticulo activating system c) Spinothalamic tract d) Vestibulo cerebellar tract Ans:b 33.All are seen in a spinal reflex except a) Summation b) Fatigue c) Memory d) Adaptation Ans:b 34.First change to occur in the distal segment of cut nerves a) Myelin degeneration b) Axonal degeneration c) Mitosis of Schwann cell d) Sprouting Ans:b 35.Maximum increase in pain threshold occurs in which phase of sleep a) Phase I b) Phase 3 c) Phase 4 d) REM sleep Ans:d PHYSIOLOGY Objective Questions with Answers 36.Below pressure, CSF absorption stops a)60mmCSF b)68mmCSF c)80mmCSF d)50cmCSF Ans:b 37.Phagocytosis in the CNS is done by a) Astrocytes b) Schwann cells c) Microglia d) Oligocytes Ans:c 38.The condition known as REM sleep is: a)That point at which the individual becomes aware and alert b)Referred to paradoxical sleep c) Characterized by total lack of all muscular activity d) Characterized by slow high voltage regular EEG activity Ans:b 39.Gag reflex is mediated by cranial nerve: a)VH b)IX c)X d)XII Ans:b 40.Hypertonia indicates a) Upper motor neuron injury b) Lower motor neuron injury c) Cerebellar lesion d) Autonomic imbalance Ans:a 41.What is not true for respiration center? a)Situated in the medulla and pons b)Sends out regular bursts of impulses to expiratory muscles during quiet respiration c)sends out regular impulses to expiratory muscles during quiet respiration d)Is inhibited during swallowing and vomiting Ans:c 42.In brain ischaemia, systemic blood pressure rises, this is called: a) Monro-kellie doctrine b) Cushing reflex c) Auto regulation d) White reaction Ans:b 43.Vestibular fibers relay in a) Vermis b) Lateral geniculate body c) Floculonodular lobe of cerebellum d) Auditory cortex Ans:c 44.Vomiting center is situated in the a) Hypothalamus b) Amygdala c) Pons d) Medulla Ans:d 45. Broca's area a) Is situated in temporal lobe d) It is synonymous to Wernicke's area c) Is an area of hearing b) Is supplied by middle cerebral artery Ans:c 46.Crude touch sensations are carried by a) Lateral spinothalamic tract b) Posterior columns c) Ventral spinothalamic tract d) P)tramidal tract Ans:c 47.One of the following is a function of hypothalamus a) Swallowing b) Vomiting c) Respiration d) Homeostasis of temperature Ans:d 48.Blood brain barrier is maximum permeable to: a)Na+ b)K+ c) Chloride d)CO, Ans:d 49.The basic postural reflex is a) Crossed extensor reflex b) Golgi tendon reflex c) Flexor reflex d) Positive supporting reflex Ans:c 50.All of the following manifestations are seen in cases of cerebellar damage in human beings except a) Loss of non-declarative/reflexive memory b) Loss of adjustment of ve9tibulo-ocular reflex c)Static tremor and rigidity d) Ataxia, atonia and asthenia Ans:c 51.Which of the following reflexes disappear in the absence of functional connections between the spinal cord and the brain? a) Swallowing reflex b) Seating reflex c) Withdrawal reflex d)Erection of penis e) All of the above Ans:a 52. In the Neurohypophysis, secretory granules accumulate in: a) Pituicytes b) Nerve endings c) Intercellular spaces b) Association fibers Ans:b 53. Conduction in which type of nerve fibers is blocked maximally by pressure a) C fibers b) A-alpha fibers c)A-Beta d)A-gamma Ans:c 54.Prosapagnosia is a) Inability to recognize faces b) Inability to draw c) Inability to count d) Inability to smell Ans:a 55. Pain sensitive part in CNS is a) Durameter b) Piameter c) Brain d) Pial vessels Ans:a 56.Wallenberg degeneration is seen in a) Proximal cut end of nerve with cell body b) Distal cut end of nerve without cell body c) Both the free ends of the cut nerve d) All are true Ans:a 57.When sensory area-I of the cerebral cortex is ablated a) Perception of pain is completely abolished b) Perception of touch is completely abolished c)There is loss of tactile localization but two point discrimination is not bolished d)There is loss of tactile discrimination as well as two-point discrimination Ans:d 58.Injection of hypertonic saline into which area causes diuresis a) Supraoptic nucleus b) Paraventricular nucleus c) Preoptic nucleus d) Posterior pituitary Ans:a 59.A unilateral upper motor neuron lesion in the internal capsule is best characterized by a)Diminished use of contra lateral appendages below the lesion b)Muscle fasciculations c)Ipsilateral hypotonicity Ans:a 60. Source of EEG a) A potential of pyramidal cells b) A potential of ganglion cells c)EPSP and IPSP of cortical cells which behave like dipoles d)After potentials of parietal cortex Ans:c 61. Decerebrate animal results from the following experimental procedure: a) Removal of the cerebrum b) Tran section at the upper border of midbrain c) Inter collicular transection d) Section above the thalamus Ans:c 62.CSF pressure (lumbar) a)70-180mmCSF b)50-100mmCSF c)>200mmCSF d) 150-250 mm CSF Ans:a 63.Which of the foUowing sensation is not carried through posterior column? a) Touch b) Proprioception c) Visceral pain d) All of the above Ans:c 64. Stereo anesthesia is due to lesion of a) Nucleus Gracillis b) Nucleus cuneatus c) Spinoreticular tract d) Subarachnoid space Ans:b 65.Broca's area is present in a) Superior temporal Gyrus b) Precentral gyrus c) Post central gyrus d)Inferior frontal gyrus Ans:d 66.The cerebellum: a)Has a totally inhibitory output from its cortex b)Has only excitatory signal output from its deep nuclear layers c)Has conscious interpretation of motor activity d)Has inhibitory influence on muscle tone in humans Ans:a 67.Hypothalamus regulates all except a) Food intake b)Temperature c) Anticipatory rise in heart rate d) Hypophysis Ans:c 68.Loss of feel of size & shape of a object is seen in lesions of a)Tractus solitarius b) Tractus cuneatus c) Lateral spinothalamic tract d)Spinoreticular tract Ans:b 67.The reticular formation is a diffuse collection of: a) Only sensory neurons b) Only motor.neurons c) Only autonomic centers d) All the above Ans:d 68.CSF is principally secreted by a) Choroid plexus b) Arachnoid granulation c) Floor of fourth ventricle d)Periaqueductal grey Ans:a 69.Paralysis agitans is accompanied by imbalance of neurotransmitter contents in a) Globus pa'llidus and substantia nigra b) Locus ceruleus c) Putamen d) Caudate nucleus and subthalamic body Ans:a 70.In Rrown-Sequard syndrome sensation, that is lost at the same side of lesion is a) Pain b) Touch c) Temperature d) Proprioception Ans:d PHYSIOLOGY Questions and Answers pdf Download Read the full article
0 notes
Text
Pediatric Meningiomas- A Case Report and Review of the Literature_ Crimson Publishers

Pediatric Meningiomas- A Case Report and Review of the Literature by Adrian Kelly*, Tshepang Tau and Tshilidzi Sidiki in Crimson Publishers: Annals of Medicine and Surgery
Background: Pediatric meningiomas are relatively rare accounting for only 3% of intracranial neoplasms. As such most of the literature on pediatric meningiomas exists in the form of isolated case reports or as a case series with small patient numbers. Despite this scarcity of literature several important features distinguish pediatric meningiomas from those that occur in adults. These include unique risk factors; a male predominance; larger tumor sizes at presentation; unusual sites of occurrence including intraventricular and parenchymal; higher World Health Organization histological grades; more aggressive clinical behavior and an increased tendency for recurrence. We present a 12-year-old male patient whom presented to our unit with a left fronto-parietal convexity meningioma of an alarming size.
Methods: A 12-year-old male patient presented to our unit with an eight-month history of a progressive headache complicated by a two-week history of vomiting. He also complained of progressive weakness of the right side of his body which had worsened to a point that he was no longer independently ambulant. General examination revealed craniomegaly with tortuous scalp veins. Neurological examination revealed a right upper motor neuron facial nerve palsy and a right hemiplegia of 2/5. Radiological investigation revealed an extremely large left fronto-parietal dural based space-occupying lesion which crossed the midline. Due to the adolescent’s progressive neurology he was taken to the operating room for emergency resection of the lesion. Gross total resection was achieved, and histopathological analysis confirmed the lesion to be a fibroblastic meningioma.
Result: Post-operatively the patient demonstrated a complete resolution of his hemiplegia and at three weeks post operatively he was already independently ambulant with power 4/5 on the previously hemiplegic side.
Conclusion: Despite the notorious features that characterize pediatric meningiomas, as well as an often-intimidating radiological appearance, adherence to standard Neurosurgical operating principles has the best chance of ensuring a successful outcome.
For more Open access journals in Crimson Publishers Please click on: https://crimsonpublishers.com/
For more Articles on Annals of Medicine and Surgery Please click on link: https://crimsonpublishers.com/smoaj/index.php
For more details, follow the below URL https://www.linkedin.com/company/crimsonpublishers
Follow on Linkedin: https://linkedin.com/in/chyler-henley-ba9623175
Follow on Medium:https://medium.com/crimson-publishers/crimson-publishers-journals-f29e22da8f5c
#Surgical medicine Open access Journal#Peer Review Journal of Surgical medicine Open access Journal#Crimson publishers llc
0 notes