#U.S. primary-care physicians
Explore tagged Tumblr posts
Text
“Economist” Magazine Also Predicts Lower World Population
Last month this blogger was surprised to learn about forecasted declines in world population and the resulting challenges of coping with such changes.[1] And earlier this week this blogger was also surprised to discover that due to the aging and forecasted retirement of many U.S. primary- care physicians, the U.S. will need to recruit foreign physicians to move to the U.S. and practice here and…
View On WordPress
#birth rates#fertility rates#Israel#pro-natal policies#The Economist#U.S. primary-care physicians#United States of America#world population
0 notes
Text
U.S. Primary Care Physicians Market Provide Accessible And Integrated Services To A Large Population
The U.S. primary care physicians market size is expected to reach USD 341.9 billion by 2030, based on a new report by Grand View Research, Inc. The market is projected to exhibit a CAGR of 3.2% from 2022 to 2030. An increasing number of Medicare beneficiaries in the country is expected to create high demand for Primary Care Physicians (PCP). According to a CDC survey in 2019, around 51.2% of physician office visits were made for primary care services.
According to the 2019 Patient-Centered Primary Care Collaborative’s (PCPCC) evidence report, there is a significant gap in investment in improving primary care services in the U.S. One of the main concerns is the growing shortage of primary care doctors and allied healthcare professionals. In a report published on the complexities of physician demand and supply in June 2020, the Association of American Medical Colleges (AAMC) estimated a deficit between 21,400 and 55,200 primary care physicians by 2033. Furthermore, there is a substantial difference between the average annual revenue and salary generated by a PCP in comparison to a specialist physician.
Gain deeper insights on the market and receive your free copy with TOC now @: U.S. Primary Care Physicians Market Report
The U.S. has one of the advanced healthcare systems and compared to any other developed nation its healthcare expenditure is two times higher. According to CMS, healthcare spending accounted for 17.7% of the GDP in 2019 and is expected to reach 19.7% in the next ten years. Primary care services act as a gatekeeper for the healthcare system and play a significant role in improving healthcare outcomes and reducing overall medical expenditure.
The onset of the COVID-19 pandemic resulted in income loss for primary care offices in the United States due to the substantial reductions in revenue caused by physical distancing. Based on volume data for general practices, general pediatric practices, family medicine practices, and general internal medicine practices, researchers from Harvard Medical School and the American Board of Family Medicine estimated that COVID-19 would cost primary care practices USD 15.1 billion in revenue.
#U.S. Primary Care Physicians Market Size & Share#U.S. Primary Care Physicians Market Latest Trends#U.S. Primary Care Physicians Market Growth Forecast#COVID-19 Impacts On U.S. Primary Care Physicians Market#U.S. Primary Care Physicians Market Revenue Value
0 notes
Text
Also preserved on our archive
This is directly tied to covid for a number of reasons including weakened immune systems from frequent infection and vaccine hesitancy strengthened during the pandemic.
By Eilis O'Neill
Whooping cough is spreading nationwide at the highest levels since 2014. There have been more than 16,000 cases this year — more than four times as many compared to the same time last year — and two confirmed deaths. And experts are concerned that the outbreak could worsen in the fall and winter months.
“More children are going back to school now, [which leads to] greater exposure,” said Dr. Eric Chow, the chief of epidemiology and immunization at the Seattle and King County public health agency. “We’re coming up on the kind of winter season when people are spending more time indoors with other people.”
The disease is most dangerous to babies: 1 in 3 who get it require hospitalization.
Whooping cough cases are especially high right now on the West Coast.
King County, where Seattle is, has seen more this year than any year since 2015 — “and the year isn’t even over yet,” Chow said. He said the county is still seeing new cases of whooping cough every week.
Why the big outbreak now? Experts say there are a number of possible explanations for the size of the current outbreak.
Doctors are testing for whooping cough more, so they’re identifying more cases.
It’s possible that the bacterium that causes the disease has mutated.
Also, people got behind on their vaccines during the pandemic, and they haven’t caught up.
“One of the challenges that we have with [the vaccine that protects against whooping cough] is that it is a five-dose series over the course of the first six years of a child’s life, so it does require regular visits to the primary care,” Chow said.
And, Chow said, not everyone can get to the doctor regularly.
But access isn’t the only problem.
“There still is a lot of vaccine hesitancy and anti-vaxers out there that will not vaccinate their kids,” said Dr. Tina Tan, a pediatric infectious disease physician at Northwestern University and the president-elect of the Infectious Diseases Society of America.
For the first couple of weeks, whooping cough looks like a mild cold, but then the coughing fits start.
Babies who get it “are going to be whooping when they cough,” Tan said. “And they may cough, cough, cough, cough, cough, and then look like they're not breathing at all.”
Tan said those pauses in breathing are life-threatening, and a sign that it’s time to go to the hospital.
Whooping cough can also lead to pneumonia and other complications.
But babies can’t get their first dose of the vaccine that protects against whooping cough, also called pertussis, till they’re 2 months old.
“That’s why it’s important for pregnant women to get the pertussis vaccine when they’re pregnant,” Tan said, “so that you can protect your baby for the first two months of life until they’re old enough to be vaccinated themselves.”
Even before the pandemic, only about half of pregnant women got the pertussis vaccine. Now, that number is even lower.
In King County, of the 12 babies who have been seen with whooping cough this year, none of their mothers got the shot during pregnancy.
Vaccine fears, and confidence Dr. Chow, with Public Health-Seattle & King County, said that’s a missed opportunity.
“Sometimes you require a kind of sit-down conversation with the patient who may be a little bit more hesitant or may have encountered misinformation,” he said, “so it just requires a longer time to build trust and rapport.”
Also, not all obstetrician/gynecologists offer the vaccine in their offices, and some people don’t have the bandwidth to go to a pharmacy for a shot.
At a playground in Seattle’s White Center neighborhood, Kay said she has two kids, ages 12 and 4, and she’s always been hesitant about vaccines.
Kay declined to give her last name because she’s concerned about revealing private medical information.
“With COVID, it even made it even more scary, because everybody started coming out saying, ‘The COVID shot’s not actually good for you,’” Kay said. “So I was like, ‘Maybe the other vaccines are bad too.’ And then I went down the rabbit hole of looking up kids who have supposedly gotten vaccinations and passed away.”
Experts say vaccines are very safe and can prevent diseases that once killed or harmed many babies, children, and adults.
Kay eventually got her 4-year-old daughter the shots required for daycare but nothing else.
“It's hard for me to get childcare, and it's just easier for me to say, ‘OK, just give me whatever she needs, just to get her into school,’” Kay said.
So her daughter did get the required whooping cough vaccines — but not any COVID shots, which are not mandated.
Aaron Sittinghorse was at the same playground with his 3-year-old daughter. He said the pandemic had the opposite effect on his thoughts about vaccines.
“It opened up my eyes to how important they are,” he said, “and so now, I'm a believer in vaccines. It's important, even if it's not for yourself, but for everybody around you.”
Sittinghorse said he saw on the news that there’s a whooping-cough outbreak right now, and it worries him a little — but not too much, because he and his family are up to date on their vaccines.
38 notes
·
View notes
Text
Orion Rummler at The 19th:
WILMINGTON — Sarah McBride won Delaware’s at-large U.S. House seat on Tuesday, Decision Desk HQ projects. She campaigned on expanding Delawareans’ access to health care — an effort on which she has focused her career in the state’s 1st Senate district. In January, McBride will be sworn in as the first out transgender member of Congress.
McBride’s ascension marks yet another milestone for the millennial state legislator. As the country’s first out transgender state senator, the first transgender person to speak at the Democratic National Convention and the first out trans woman to intern at the White House, McBride has repeatedly broken barriers in politics and proven that voters are ready to elect transgender candidates into elected office. Although McBride didn’t run for Congress to make history, the significance of her campaign for transgender Americans during a time of intense political backlash has propelled a national following behind her. That includes Daisy Hollman and Jimmy Fitzpatrick, two Californians who knocked on hundreds of doors for McBride across Delaware the week before Election Day.
[...] This election for Delaware’s seat in the House of Representatives had no incumbent for the first time in years, as U.S. Rep. Lisa Blunt Rochester stepped down to run for Delaware’s open Senate seat. McBride was projected to be the winner early on; she had robust fundraising and amassed key endorsements from state political leaders, including Blunt Rochester. Democrats have held Delaware’s at-large House seat for over a decade. On the campaign trail, McBride called for increased federal investments to support nurses, primary care physicians and independent health care clinics in Delaware. She touted her accomplishments as a state senator, including the passage of a statewide paid family and medical leave insurance program and a recently signed law that is expected to generate more than $100 million in new Medicaid funding for Delaware.
She faced a Republican opponent who endorsed transphobic policies. John Whalen III, a retired police officer, staked his campaign on cutting federal spending and restricting immigration. He also publicly endorsed Project 2025, the conservative Heritage Foundation’s blueprint for a second Trump administration. The plan equates the act of being transgender — or “transgender ideology” — to pornography.
Rep.-elect Sarah McBride (D) made herstory by being the first trans person to be elected to Congress by winning the DE-AL seat.
#Sarah McBride#2024 Delaware Elections#2024 Elections#2024 US House Elections#119th Congress#Delaware#Transgender#Delaware Politics
11 notes
·
View notes
Text
Chronic pain patients who use either opioids or cannabis are still finding it hard to find a new primary care physician, according to new research at the University of Michigan.
Lead author Mark Bicket, MD, and his colleagues surveyed more than 1,000 U.S. primary care physicians about whether they were accepting new patients with chronic non-cancer pain. The physicians were all based in states with medical cannabis programs.
Of the 852 physicians who said they were taking new patients, 80% said they would accept patients taking prescription opioids. But only 68% said they’d accept a patient using opioids daily.
In contrast, nearly 82% of doctors said they would take pain patients using medical cannabis. Only 60% would accept a patient using cannabis “obtained from other sources” — meaning the cannabis probably came from the black market.
“There’s a group of legacy patients with chronic pain who have been on long-term opioids for some time, and they may have to find a doctor, maybe because they’ve moved or their doctor has retired,” said Bicket, who is an anesthesiologist and pain researcher at Michigan Medicine. “For those patients in particular, finding someone else to help with their care is challenging.”
Making matters worse, pain patients are at higher risk of having a substance problem if they don’t have access to pain medication. (Read more at link)
I just went through the worst, my pain clinic closed but luckily my primary care NP says she’ll keep my prescription going while I try to find another pain doctor or even if I don’t. But when she inevitably retires, and she is older than me, what then? This shit is fucking terrifying.
#disability#chronic pain#ableism#spoonies#chronic illness#opioids#medical marijuana#medical bias#article
12 notes
·
View notes
Text
Notes on "Empire of Care : Nursing and Migration in Filipino American History"
Previous post:
Filipino nurse Patrocinio Montellano was a nurse who was interviewed for this book

Art by Filipino-American artist MYSTERIOUSxBEAUTY
She was an accomplished woman, furthering her nursing career in the US by taking post-graduate courses.
She eventually secured deployment through the aid of Americans such as William Musgrave, former director of the Philippine general hospital.

In 1924, she returned to the Philippines, becoming the field representative and nurse supervisor of the Philippine chapter of the American red cross.
None of this would have been able to happen had it been a few decades earlier - when the Philippines was under the colonial rule of the Spanish.
Under Spanish rule, Filipinos were only offered unequal opportunities rooted in gender by the education system implemented by the Spanish at the time.
Because of this, very few Filipino girls were permitted primary education given to them by Spanish charitable institutions.
Women were outright excluded from the University of Santo Tomas - the Spanish university in the Philippines

This was until 1879, when a school of midwifery was opened
When it came to specialised health care jobs, only midwifery was allowed for Filipino women to enter into
Traditionally, Filipino women would take on the role of the caretaker at home
Filipinos would also rely on indigenous healers

On the other hand, in Spanish medical institutions, usually Spanish Friars and Priests were the caretakers.
Sisters of Charity, along with a European nurse, arrived in the Philippines in 1862 to work at the San Juan de Dios hospital.

Spanish surgeons and male Filipino physicians would practice both generalised and specialised forms of healthcare.
In the 19th century, elite Filipino men (called ilustrados) were encouraged by the Spanish government to further their education in European countries.
Jose Rizal - a Filipino national hero and ilustrado was a doctor of medicine himself.

Filipino women were outside banned from these opportunities
US colonialism did implement some changes of opportunities that Filipino women were offered - as Montellano's story reveals.
The opportunities that were now offered were nursing, education - and travel opportunities to the U.S
These opportunities for both work and travel were closely linked.
Montellano's account demonstrates how like clockwork, the beginning of the U.S colonial rule marked significant transnational relations between the U.S and Filipino women
Montellano's socioeconomic and geographic mobility was enabled by these relations
Montellano was aided by American physicians and nurses in order to reach her employment goals in the United States
Montellano's experience in the US helped her secure an advanced nursing career upon her return to the Philippines.
Montellano notes that it was also her sheer determination and courage that helped her progress her career - even against her father's wishes.
The literature on women and imperialism challenges the perception of imperialism as masculine.
American women's participation in U.S. colonialism in the Philippines has been overlooked.
U.S. colonial nursing played a crucial role in American modernity and American women viewing themselves as civilised.
Filipino nurses' perspectives reveal the role of Filipinos and Americans in Philippine nursing.
Nursing and medicine legitimised U.S. colonial agendas and social hierarchies.
Western medicine is often seen as a humanitarian effort, making it difficult to critique its exploitative effects
Reynaldo Ileto noted that it was even difficult for the most nationalist Filipino writers to criticise the US sanitary regime as it saved countless Filipino lives.

Reynaldo Ileto, Filipino historian
The introduction of professional nursing in the Philippines had both liberating and exploitative aspects.
This chapter highlights a period of transnational mobility in Filipino American history.
American and Filipino nurses shaped Philippine nursing through travel, teaching, training, and practice.
This multidirectional mobility has been overlooked in Asian American histories.
The formation of a gendered labor force laid the foundation for significant migrations of Filipino nurses later in the twentieth century.
#the philippines#Philippines#philippine history#Filipino#Filipino history#Pinoy#US colonialism#us imperialism#U.S colonialism#U.S imperialism#US colonisation#U.S colonisation#American colonialism#American imperialism#American colonisation#America#USA#u.s#asia#Asian history#South East Asia#South East Asian history#History#Colonial history#Filipino American#Next post on this will feature heavy racism rip#asian american#Asian American history
17 notes
·
View notes
Text
STAT: In counties with more Black doctors, Black people live longer, 'astonishing' study finds
Black people in counties with more Black primary care physicians live longer, according to a new national analysis that provides the strongest evidence yet that increasing the diversity of the medical workforce may be key to ending deeply entrenched racial health disparities.
The study, published Friday in JAMA Network Open, is the first to link a higher prevalence of Black doctors to longer life expectancy and lower mortality in Black populations. Other studies have shown that when Black patients are treated by Black doctors, they are more satisfied with their health care, more likely to have received the preventive care they needed in the past year, and are more likely to agree to recommended preventive care such as blood tests and flu shots. But none of that research has shown an impact on Black life expectancy.
The new study found that Black residents in counties with more Black physicians — whether or not they actually see those doctors — had lower mortality from all causes, and showed that these counties had lower disparities in mortality rates between Black and white residents. The finding of longer life expectancy persisted even in counties with a single Black physician.
“That a single Black physician in a county can have an impact on an entire population’s mortality, it’s stunningly overwhelming,” said Monica Peek, a primary care physician and health equity researcher at UChicago Medicine who wrote an editorial accompanying the new study. “It validates what people in health equity have been saying about all the ways Black physicians are important, but to see the impact at the population level is astonishing.”
“This is adding to the case for a more diverse physician workforce,” said Michael Dill, the director of workforce studies at the Association of American Medical Colleges and one of the study co-authors. “What else could you ask for?”
Lisa Cooper, a primary care physician who directs the Johns Hopkins Center for Health Equity and has written widely on factors that may explain why Black patients fare better under the care of Black doctors, called the study “groundbreaking” and “particularly timely given the declining life expectancy and increasing health disparities in the U.S. in recent years.”
“These findings should serve as a wake-up call for health care leaders and policymakers,” she told STAT.
The team of researchers, from the Health Resources and Services Administration of the U.S. Department of Health and Human Services and the AAMC, started their work by analyzing the representation of Black primary care physicians within the country’s more than 3,000 counties during 2009, 2014, and 2019. Even this first step resulted in a stark finding: Just over half of the nation’s counties had to be excluded from analysis because they contained not a single Black primary care physician.
“I knew it was a problem,” said Dill, “but ooh, those numbers are not good.”
The team’s analysis of the 1,618 counties that had at least one Black primary care physician in one of the three years found that the more such physicians a county contained, the higher life expectancy was for Black residents. (They’d like to repeat the analysis in the future to see how counties with Black doctors fared during the Covid-19 pandemic, which disproportionately affected people of color.)
The team found life expectancy increased by about one month for every 10% increase in Black primary care physicians. While extending life by a few months may not sound like much given that the life expectancy gap between Black and white Americans nationally is nearly six years, picking up such a signal on a population level is significant, the authors said.
The study found that every 10% increase in Black primary care physicians was associated with a 1.2% lower disparity between Black and white individuals in all-cause mortality. “That gap between Black and white mortality is not changing,” said John Snyder, a physician who directs the division of data governance and strategic analysis at HRSA and who was one of the lead authors. “Arguably we’ve found a path forward for closing those disparities.”
The study did not directly address the reason Black people fare better in counties with more Black physicians, nor does it prove a cause-and-effect relationship. While earlier research suggests “culturally concordant” medical care is of better and higher quality for patients, the new study indicates that one factor may be that Black physicians are more likely to treat low-income and underinsured patients, taking on new Medicaid patients more than any other racial or ethnic group, for example. The study found that improvements in life expectancy were greatest in counties with the highest rates of poverty.
“I wasn’t expecting that,” said Rachel Upton, an HHS statistician and social science analyst who was one of the report’s lead authors. “It shows having Black physicians is not only helpful across the board, but it’s particularly useful with counties with high poverty.”
Many studies have found that communication is improved when patients and physicians are of the same race. Owen Garrick co-authored a 2019 study in Oakland, Calif., finding that cardiovascular disease could be curbed more in Black patients who are seen by Black doctors because they are more likely to engage in preventive health care. He noted during his study that Black patients were not only more likely to talk with Black doctors about subjects like upcoming birthday parties or weddings, they were also more likely to invite them to the events.
But good communication is not the only factor: A 2020 study found that in infant care, where verbal communication from the doctor is not an issue, mortality rates for Black infants were reduced when they were treated by Black physicians; the authors suggested stereotyping and implicit bias may play a role when doctors treat patients outside their racial and ethnic groups.
The current study looked past the patient-doctor relationship and showed that patients may fare better simply by living in counties with Black doctors even if they are not directly treated by those doctors. Living in a county where Black doctors work and thrive “may be a marker for living in a community that better supports Black lives,” Snyder said.
Another factor, said Peek, is that Black physicians may be more likely to do unpaid health-related work outside of the health care system, such as providing expertise to community organizations, being politically involved in health-related matters, and encouraging medical societies to advocate for public health.
That’s the case with Peek, who has spent two decades working with a nonprofit that helps Black women in public housing become health navigators and advocates. She also spends a good deal of time providing a second opinion to her network of friends and family — and their friends and families — who do not personally know any physicians and may have issues of mistrust with the medical system.
“With my non-Black colleagues, it’s like ‘Both my parents were doctors! Everyone’s a doctor!’” she said. “Their social network is not all paranoid when they enter the health care system.”
She said the study also pointed to problems with racism within medicine and bias toward Black patients that has created a “chasm” between non-Black physicians and their Black patients. She’s struck, she said, by the number of Black people who come up to her after she speaks at a local church to give her their detailed medical history and ask her opinion because they don’t trust their own medical team. “I look like them,” Peek said. “They trust I have their best interest at heart.”
The authors of the new paper said they were not advocating segregated care and all doctors should improve their cultural competency. Patients of all races and ethnicities would be helped by increased diversity in the physician workforce, they said.
But increasing the number of Black physicians remains a stubborn problem. Despite decades of attention to the matter, a 2021 study showed the number of Black and Native American medical students, particularly males, has stagnated. The AAMC has reported a recent uptick in admissions of Black medical students, possibly due to a renewed focus on diversity in recent years, but an upcoming Supreme Court decision expected to limit the use of race as a factor in admission could cut into such gains.
The current study did not address how the presence of physicians from other groups underrepresented in medicine, including Hispanic and Indigenous people and Pacific Islanders, affects health outcomes. Upton said she hoped other researchers could focus on such groups in the future and that more researchers would conduct “within group” studies to examine the health of people within a single racial or ethnic group and not just examine how such groups compare to other, usually white, populations.
“Oftentimes we just look at the disparities,” she said. “I would like people to be looking at how people are doing within their own groups and what can help within those groups.”
#Black Doctors#Black Life#Black Healthcare#In counties with more Black doctors#Black people live longer#Black Healthcare with Black Doctors
5 notes
·
View notes
Text
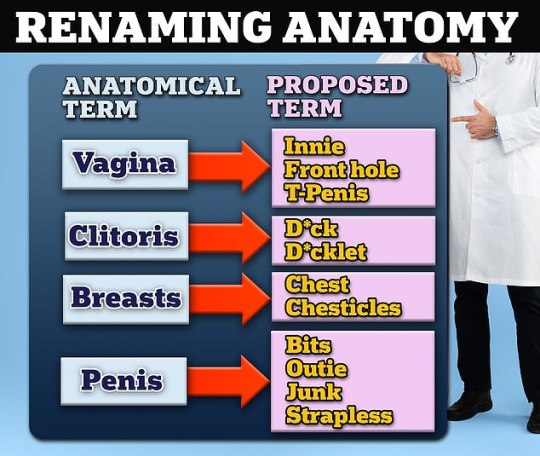
What is the new speak word for ass? As in Dr Ilana Sherer should pull her head out of her ass? Because no self respecting woman is calling her clitoris a "dicklet"
Prominent doctor at the American Academy of Pediatrics proposes renaming penises 'outies', vaginas 'front holes' and clitorises 'd*cklets'
Dr Ilana Sherer is a pediatrician from California who providers transgender care
She gave a presentation at the AAP National Conference in Washington, DC
READ MORE: Academy of Pediatrics backs transgender care for minors
By ALEXA LARDIERI U.S. DEPUTY HEALTH EDITOR DAILYMAIL.COM
PUBLISHED: 14:46 EDT, 23 October 2023 | UPDATED: 05:03 EDT, 24 October 2023
A top pediatrician has called for child doctors to start calling the vagina a 'front hole' and the penis an 'outie.'
Dr Ilana Sherer, a pediatrician in Dublin, California, gave a presentation Sunday at the American Academy of Pediatrics (AAP) National Conference and Exhibition and called for more gender neutral terminology for body parts.
Her proposals, given during a workshop entitled 'Discussing Gender and Sexuality in the Primary Care Office,' included referring to the vagina as an 'innie,' 'front hole,' or 'T-penis' and the clitoris as 'd*ck' or 'd*cklet.'
She also proposed calling breasts 'chest' or 'chesticles.' For male anatomy, Dr Sherer recommended pediatricians call the penis 'outie,' 'junk,' 'strapless,' or 'bits.'


e-mail
Top
+99Home
614
View comments
A top pediatrician has called for child doctors to start calling the vagina a 'front hole' and the penis an 'outie.'

ADVERTISEMENT
Dr Ilana Sherer, a pediatrician in Dublin, California, gave a presentation Sunday at the American Academy of Pediatrics (AAP) National Conference and Exhibition and called for more gender neutral terminology for body parts.
Her proposals, given during a workshop entitled 'Discussing Gender and Sexuality in the Primary Care Office,' included referring to the vagina as an 'innie,' 'front hole,' or 'T-penis' and the clitoris as 'd*ck' or 'd*cklet.'

She also proposed calling breasts 'chest' or 'chesticles.' For male anatomy, Dr Sherer recommended pediatricians call the penis 'outie,' 'junk,' 'strapless,' or 'bits.'
+5
View gallery
Pediatrician Dr Ilana Sherer gave a presentation at the American Academy of Pediatrics National Conference and Exhibition and called for more gender neutral terminology for body parts

Slides from Dr Ilana Sherer's presentation offer advice on how to talk to pediatric patients about gender and sexual identity, including new terms to use to address genitalia
Dr Sherer is a general pediatrician at Palo Alto Medical Foundation/Sutter Health.
She is board certified by the AAP, an organization to advance child health and well-being, as well as the profession of pediatrics, and serves on the organization's Executive Committee for LGBTQ Health and Wellness.
Some in the medical community have been calling for gender-neutral body terminology for years, recommending 'upper body' for breasts, 'erectile tissue' for penis and 'internal gonads' for ovaries.
They argue it creates a more inclusive space for people who may not identify as one gender or sex and are not comfortable using gender-specific terminology.
But doctors have previously warned against politicizing medical language because it could confuse public health messaging, especially for people for whom English is not their first language.
Dr Leonora Regenstreif, a family physician in Canada, told DailyMail.com: 'Health providers don't need to be "cool." We can just politely and respectfully use clinical, anatomical language.
'Kids might giggle or snicker but they will likely be even more put off if we try to "match" their word choices, which may be based on pornographic or inappropriate online resources.'
The physician said a few questions, modified for the age of the patient, like 'are you sexually active?' and 'Have you had intercourse with someone with a penis?' are adequate.
She added: 'Any more detail than this - like suggesting novel words like "front-hole" or "dicklet" - are unnecessary and prurient.'
Furthermore, Dr Julia Mason, a pediatrician in California, told DailyMail.com: 'I am concerned that pediatricians are encouraging dissociation from young people's sexed bodies in the doctor's office, where terms need to be simple and clear.'
Dr Mason added that during Dr Sherer's presentation, she noted rates of unintended pregnancy are high among girls who identify as lesbians.
'I worry about kids being provided with incomplete information, leading to uninformed behavior and unintended consequences,' Dr Mason said.

Dr Ilana Sherer is a general pediatrician at Palo Alto Medical Foundation/Sutter Health in Dublin, California
During her presentation at the AAP Conference, Dr Sherer was not speaking on behalf of the organization and her recommendations have not been adopted or implemented by the medical organization. The AAP has not commented on Dr Sherer's presentation.
When it comes to LGBTQ care, in 2021, the AAP advised doctors treating patients identifying as transgender to ask them what words they would like used when referring to various body parts.
Guidance from July 2022 instructs parents to use 'correct names for body parts' when talking to young children and discussing body development and sexuality.
In August, the AAP voted to stand by its 2018 guidance that supports LGBTQ access to counseling, hormone therapy, puberty blockers and, occasionally, surgery for minors under 18 years old.
Any guidance from the AAP is not binding for doctors, but advice announced by a prominent medical advisory body is often implemented by healthcare providers as best practices.
In trans girls, options include tucking male genital with medical tape or specialized underwear and padding with breast forms of silicone gel, padded bras and padded underwear to accentuate the hips and butt. Additional options include vocal training, makeup tutorials and wigs.
In trans boys, options include binders like compression garments, and 'packing,' which includes a penile prosthesis and a 'stand to pee device.'
A medical option includes prescribing birth control to patients who are menstruating, which will stop them from their getting periods.
Other points of Dr Sherer's presentation outlined potential 'non pharmacologic treatment for body dysphoria' for trans girls and trans boys.
Dr Sherer's presentation also outlined how to ask patients about gender, including asking their preferred pronouns, gender identity and sexual orientation, and if they identify as male or female, or neither.
To get more information on a child's sexual orientation, Dr Sherer said doctors should ask patients if they are in an intimate relationship and what 'parts of your body do you use/have you used for sexual pleasure?
Other questions relate to monogamous relationships, previous and 'side' partners, the genders of a patient's partners and what body parts they use for sexual pleasure.
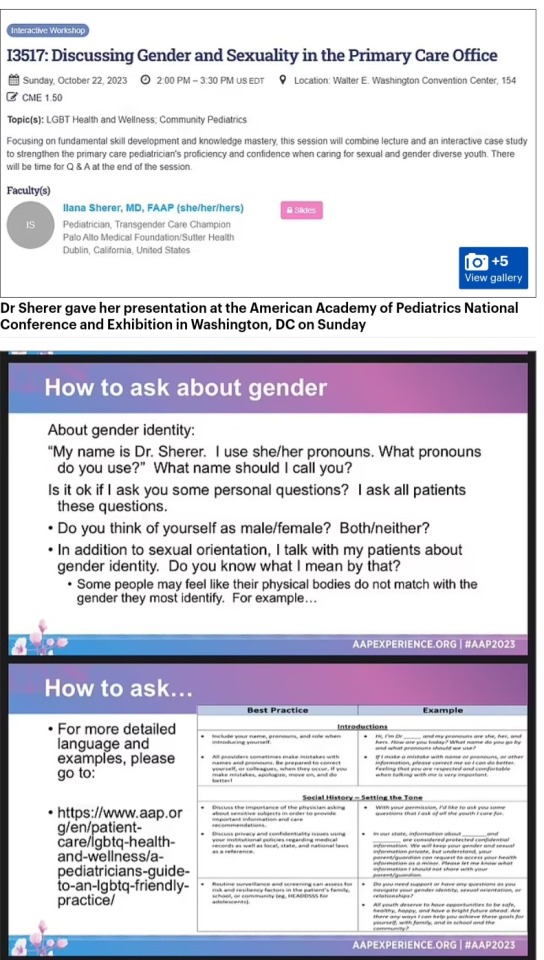

The California pediatrician's workshop also recommended doctors 'think about your office' and said they should display affirming signs and posters, ensure staff have adequate inclusivity training, hire a diverse staff that represents patient identities, have all-gender bathrooms, inclusive medical forms, include preferred pronouns on patient charts and display pronoun stickers on staff ID badges.
Similar recommendations were released by the AAP in June 2021.
The mission of the AAP is to 'attain optimal physical, mental, and social health and well-being for all infants, children, adolescents, and young adults.'
The mission continues: 'Children have optimal health and well-being and are valued by society. Academy members practice the highest quality health care and experience professional satisfaction and personal well-being.'
The medical care of trans patients has been politicized into a hot-button issue and is becoming a key political battleground heading into the 2024 Presidential Election.
Local and national politicians have been fighting and enacting legislation that limits and even outlaws gender-affirming care for trans children, which can include hormone therapy, puberty blockers and genital reconstruction.
Up until the wave of state bans began in 2020 and 2021, there were no restrictions at the federal level for access to these treatments, which in some cases are irreversible.
However, as of May 2023, 20 states have enacted legislation, executive actions, or other policies that restrict or ban healthcare for transgender youths, and more than 100 additional bills are under consideration.
All of the states are Republican or Republican-leaning, and all but one voted for former President Donald Trump in the 2020 election.
Much of the political debate in recent years has been amid concerns that minors who get gender-affirming care are too young to make such a life-changing decision and are not fully aware of the risks.
For example, studies suggest those who are transgender are six times more likely to suffer from autism, and up to 70 percent of trans youths are depressed.
Other studies, including one by the National Institutes of Health, suggest patients are happier after the surgery, further complicating the issue.
There are concerns among Republican lawmakers about the lack of long-term safety data on puberty blockers and hormone drugs, which have seen other countries like the UK and Scandinavia restrict access in minors.
The Food and Drug Administration approved puberty blockers 30 years ago to treat children with precocious puberty - a condition that causes sexual development to begin much earlier than usual.
Sex hormones - synthetic forms of estrogen and testosterone - were approved decades ago to treat hormone disorders or as birth control pills.
The FDA has not approved the medications specifically to treat gender-questioning youth, but they have been used for many years for that purpose 'off label.'
Doctors who treat transgender patients say those decades of use are proof the treatments are not experimental.
Dr Sherer and the AAP could not be reached for comment
#Dr Ilana Sherer#AAP National Conference#American Academy of Pediatrics (AAP)#'Discussing Gender and Sexuality in the Primary Care Office#Ok I can't argue with calling a penis junk#Executive Committee for LGBTQ Health and Wellness
2 notes
·
View notes
Note
my hot take is that u.s medical transition is the opposite side of norway’s medical transition for being shitty to us. I had no support or therapy or guidance getting HRT at 16. My doctors had never even met another trans person before me. I taught them. That is a horrifying place to be. Imagine then regretting that decision or having medical complications??? Like I’m happy with myself but theres no support for transition or detransition in the U.S unless you’re rich and voluntarily decide to pursue extra support like therapy and bloodwork
most of this sounds like my experience, tbh. I had to explain HRT and transgender existence to my primary care physician. you have to be rich to be able to transition (unless you fit an extremely narrow set of characteristics, including but not limited to skinny, white, attractive, binary, healthy, happy but not too happy, absolutely not a single gender nonconformist bone in your body, neurotypical, heterosexual, and wanting a complete and binary transition, in which case you MIGHT get considered for state covered HRT and surgeries). needless to say my top surgery cost me 53000 NOK (~$5000) and I pay 460 NOK (~$43) a month for my T gel. theres no support for it, because it has not been deemed "medically necessary" like it would if I had gotten a diagnosis through Rikshospitalet. oh yeah, you need to be diagnosed with transsexualism I mean Sex/Gender Incongruity in order to even qualify for care.
I performed at a pride event last weekend (i am a drag performer). we needed bodyguards to get safely between the stage and our hotel. norway is a hyper conservative hellhole with a facade of social welfare.
#the transsexualism diagnosis was only changed in the last few years btw. its the same thing now but with a prettier name#my point is i dont think theyre opposite i think they r the same
5 notes
·
View notes
Text
The Role of MIPS in Enhancing Patient Care and Provider Performance
The Merit-based Incentive Payment System (MIPS) has emerged as a cornerstone of value-based care in the U.S. healthcare system. By aligning provider performance with patient outcomes, MIPS incentivizes quality care, fostering improved healthcare delivery across the board.

1. Understanding MIPS
MIPS is part of the Quality Payment Program (QPP) introduced under the Medicare Access and CHIP Reauthorization Act (MACRA). It consolidates previous quality reporting programs into a streamlined system that evaluates healthcare providers based on four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability.
2. Driving Patient-Centric Care
MIPS emphasizes patient outcomes by rewarding providers who deliver high-quality, efficient care. Metrics focus on reducing hospital readmissions, improving preventive care, and managing chronic conditions effectively. This approach shifts the emphasis from volume to value, ensuring better health outcomes.
3. Incentivizing Innovation
To perform well under MIPS, providers must embrace innovation. This includes adopting advanced electronic health records (EHRs), telehealth platforms, and data analytics tools. These technologies not only streamline operations but also enhance patient engagement and satisfaction.
4. Encouraging Collaboration
MIPS fosters collaboration among healthcare teams by promoting integrated care. Coordinated efforts between primary care physicians, specialists, and allied health professionals ensure comprehensive and continuous patient care.
5. Balancing Financial and Clinical Goals
MIPS aligns financial incentives with clinical objectives. Providers who excel in delivering value-based care receive positive payment adjustments, creating a win-win scenario for both patients and healthcare organizations.
6. Challenges and Opportunities
While MIPS offers numerous benefits, providers face challenges such as administrative burdens and compliance complexities. However, leveraging specialized tools and consulting services can simplify participation and maximize performance.
Conclusion
MIPS represents a transformative shift in U.S. healthcare, placing patient outcomes at the forefront. By fostering quality, innovation, and collaboration, MIPS is enhancing both patient care and provider performance.
youtube
SITES WE SUPPORT
MIPS Flyer Marketing – Wix
0 notes
Text
Top 5 Common Conditions Treated by Internists in Brooksville, Florida | Springhill Primary Care
In Brooksville, Florida, managing your health involves partnering with skilled healthcare providers who can guide you through a range of medical needs. At the core of adult healthcare are internists — physicians specialized in diagnosing, treating, and preventing a variety of diseases in adults. Internists not only address immediate health concerns but also focus on long-term wellness, disease prevention, and patient education, embodying a holistic approach to primary care.
In this article, we’ll highlight the top five common conditions treated by internists in Brooksville, Florida, especially at Springhill Primary Care. This list can help you better understand when to consult an internist and how they can help you maintain a healthier, more active lifestyle.

1. Hypertension (High Blood Pressure)
Overview: Hypertension is a condition where the force of the blood against the artery walls is consistently too high. If untreated, it can lead to serious health complications like heart disease, stroke, and kidney damage.
Symptoms: Often, hypertension is called the “silent killer” because it may not present symptoms until it reaches a severe stage. Some patients may experience headaches, vision problems, or chest pain.
Treatment: Internists in Brooksville emphasize early detection through routine screenings. Treatment often includes lifestyle changes, such as a low-salt diet and regular exercise, combined with medication when necessary. Regular check-ups allow for monitoring blood pressure and making adjustments to treatment as needed.
Why See an Internist: Internists are well-equipped to monitor and manage hypertension. They’ll look at your overall health and work on preventing complications that could arise from unmanaged high blood pressure.
2. Type 2 Diabetes
Overview: Type 2 diabetes is a chronic condition that affects the body’s ability to process blood sugar, leading to dangerously high blood glucose levels. It’s common in the U.S., particularly in areas with high rates of obesity and sedentary lifestyles.
Symptoms: Symptoms may include excessive thirst, frequent urination, fatigue, and blurred vision. Left untreated, it can lead to severe complications, including cardiovascular disease, kidney failure, and nerve damage.
Treatment: Treatment for Type 2 diabetes includes dietary changes, regular physical activity, monitoring blood sugar levels, and medications. For some patients, insulin therapy may be required.
Why See an Internist: Managing diabetes requires a comprehensive approach, and internists are skilled in coordinating care across multiple aspects of health. They can monitor blood sugar levels, prescribe medications, and provide lifestyle guidance, offering patients the tools they need for long-term management.
3. Respiratory Infections (Chronic Bronchitis and COPD)
Overview: Respiratory conditions, including chronic bronchitis and chronic obstructive pulmonary disease (COPD), are particularly prevalent in Florida due to factors like humidity, allergens, and exposure to respiratory irritants. Chronic bronchitis is characterized by inflammation in the airways, while COPD can severely impair breathing over time.
Symptoms: Common symptoms of respiratory conditions include persistent cough, wheezing, shortness of breath, and frequent respiratory infections.
Treatment: Treatment often involves medications like bronchodilators and corticosteroids, along with lifestyle modifications such as smoking cessation and pulmonary rehabilitation.
Why See an Internist: Internists can diagnose the root cause of respiratory issues and help manage chronic conditions with a tailored treatment plan. Their goal is not just symptom relief but also reducing flare-ups and preserving lung function over time.
4. Arthritis and Joint Pain
Overview: Arthritis, particularly osteoarthritis, is a frequent concern among adults in Brooksville. It’s a degenerative joint disease that causes pain, stiffness, and decreased mobility, often in the knees, hips, and hands.
Symptoms: Common symptoms include joint pain, swelling, stiffness, and reduced range of motion, which can affect daily activities.
Treatment: While there is no cure for arthritis, treatments can significantly reduce discomfort. An internist may recommend a combination of physical therapy, medications like NSAIDs (nonsteroidal anti-inflammatory drugs), and lifestyle changes such as weight management to reduce joint strain.
Why See an Internist: Internists can provide an accurate diagnosis, monitor symptoms, and develop a comprehensive treatment plan that may include medications, physical therapy, and even referrals to orthopedic specialists when needed.
5. Cardiovascular Disease (Including High Cholesterol)
Overview: Cardiovascular disease remains a leading cause of mortality, and managing it effectively requires a proactive approach. High cholesterol, which can contribute to heart disease, is especially common in adults, putting them at greater risk for heart attacks and strokes.
Symptoms: Often, cardiovascular diseases go unnoticed until they present as a major event, like a heart attack. However, warning signs can include chest pain, shortness of breath, and fatigue.
Treatment: Treatment for cardiovascular disease focuses on lifestyle interventions and medications. Managing cholesterol, for example, involves diet changes, exercise, and statins (cholesterol-lowering medications).
Why See an Internist: Internists are trained to look at the big picture of a patient’s health. In treating cardiovascular disease, they can help you make important lifestyle changes, monitor cholesterol levels, and manage medications effectively. With regular check-ups, internists can track improvements and detect any potential issues before they become critical.
Why Choose Springhill Primary Care in Brooksville, Florida?
At Springhill Primary Care in Brooksville, our internists are dedicated to providing comprehensive care tailored to your needs. We understand the unique health challenges in our community and prioritize patient education, preventive care, and the early detection of common health issues. By partnering with an experienced internist, you can benefit from:
Personalized Care Plans: Every patient receives a treatment plan that addresses their individual health profile and lifestyle.
Preventive Health Focus: Regular screenings and check-ups ensure that potential issues are caught early, preventing complications.
Coordinated Care: We work closely with specialists and support services to ensure holistic, coordinated care.
Patient-Centered Approach: At Springhill Primary Care, we believe in empowering patients to take charge of their health with informed, accessible care.
Final Thoughts
Internists play a pivotal role in adult healthcare, especially for residents in Brooksville, Florida, where a proactive approach to managing common conditions can lead to better long-term health. If you’re experiencing symptoms of any of these common conditions or are simply looking to establish a preventive health plan, schedule a consultation with an internist at Springhill Primary Care. Our team is committed to helping you achieve optimal health through personalized, compassionate care.
Ready to take the next step? Contact Springhill Primary Care in Brooksville today to schedule your appointment and start your journey to a healthier, happier you!
#Brooksville doctor#Brooksville medical clinic#Brooksville healthcare#Brooksville family doctor#Brooksville physician#Internist Brooksville#primary care Brooksville#family medicine Brooksville#doctor near me Brooksville#healthcare provider Brooksville#Spring Hill Primary Care#Brooksville health clinic
0 notes
Text
Navigating the Maze: Understanding Health Care Costs and Insurance
The landscape of health care costs and insurance in the United States can be bewildering, with its complex interplay of policies, providers, and payers. As medical costs continue to rise, understanding this intricate system is crucial for anyone looking to manage their health expenses effectively. This article delves into the factors driving healthcare costs, the role of insurance, and strategies for consumers to navigate this challenging environment.
The Dynamics of Health Care Costs
Factors Driving Costs: Healthcare spending in the U.S. is influenced by a range of factors, including technological advancements, an aging population, the prevalence of chronic diseases, administrative costs, and the pricing transparency of healthcare services. Innovations in medical technology, while improving quality of life and treatment outcomes, often come with high costs. Additionally, the administrative expenses associated with health insurance and healthcare facilities continue to rise, further inflating overall healthcare costs.
Impact of Pricing Opacity: One of the less discussed but significant contributors to high healthcare costs is the lack of pricing transparency. Patients often need help getting clear information about the cost of treatments or procedures beforehand, which can lead to surprisingly high bills after the fact. This opacity makes it challenging for consumers to compare prices and choose less expensive options, reducing the natural market pressures that typically control costs.
Understanding Health Insurance Coverage
Types of Health Insurance Plans: Navigating health insurance begins with understanding the different types of plans available:
HMOs (Health Maintenance Organizations): These plans offer a network of healthcare providers that patients are required to use. They typically require referrals from a primary care physician to see specialists.
PPOs (Preferred Provider Organizations): PPOs provide more flexibility, allowing patients to visit whatever in-network physician they choose without a referral and offering limited coverage for out-of-network providers.
High-Deductible Health Plans (HDHPs): These plans have higher deductibles but lower premiums. They are often paired with Health Savings Accounts (HSAs), allowing individuals to save money tax-free for medical expenses.
The Role of Medicare and Medicaid: Government-provided healthcare plays a crucial role in managing healthcare costs for specific populations. Medicare primarily serves those over 65 and certain younger individuals with disabilities, while Medicaid covers some low-income families and individuals, including children, pregnant women, elderly adults, and people with disabilities. Understanding eligibility and benefits under these programs can significantly affect an individual's financial planning for health care.
Strategies for Managing Out-of-Pocket Expenses
Comparative Shopping for Health Care: As the push towards transparency continues, more tools and resources are becoming available to help consumers compare the costs of care. Websites and apps now offer information on the cost of various medical services across different providers, allowing patients to make more informed decisions based on cost and quality.
Preventive Care: One of the most effective ways to reduce health care costs is by focusing on preventive care. Many insurance plans cover preventive services like vaccinations, screenings, and annual check-ups at no extra cost. Utilizing these services can help catch health issues early, potentially avoiding expensive treatments later.
Negotiation and Payment Plans: Patients can sometimes negotiate costs with providers, especially for costly procedures or for those paying out of pocket. Additionally, many healthcare providers offer payment plans that allow patients to pay off their bills over time without interest, making significant expenses more manageable.
The Future of Health Care Costs and Insurance
Policy Changes and Innovations: With health care reform a constant topic of debate, potential changes to insurance markets, drug pricing laws, and coverage mandates could significantly alter the landscape of health care costs and insurance. Innovations such as telemedicine and personalized medicine also hold the potential to reduce costs by improving efficiency and tailoring care to individual needs.
Consumer Education and Advocacy: As consumers become more educated about the intricacies of health care and insurance, they can better advocate for changes that will benefit them. Understanding one's rights and responsibilities, staying informed about legislative changes, and participating in community advocacy can empower consumers to influence how health care will evolve in the future.
Understanding health care costs and insurance is crucial for managing personal finances and ensuring access to necessary medical care. By educating themselves about the factors influencing costs, the details of their insurance coverage, and strategies for minimizing out-of-pocket expenses, individuals can take more control over their healthcare decisions. This knowledge not only helps in making informed choices but also in advocating for a more transparent and equitable health care system.
0 notes
Text
‘It has not gone away’: As COVID-19 cases rise in Colorado, health experts call for continued vigilance
Wearing a high-quality mask, cleaning the air and other protective measures continue to be important as CDC now says SARS-CoV-2 is a year-round threat
Wearing a high-quality mask, cleaning the air and other protective measures continue to be important as CDC now says SARS-CoV-2 is a year-round threat
Flu and RSV have come and gone this year, so if cold-like symptoms have been putting a damper on your summer plans these past few weeks, Colorado health experts say it’s very likely the coronavirus is to blame.
The state — just like pretty much the rest of the country — is experiencing a rise in COVID-19 cases this summer due to two different strains from the Omicron family – KP.2 and KP.3. Nicknamed “FLiRT” by variant trackers to help the public better understand the wide variety of circulating strains of the virus, these two strains combined — which may be better able at getting past the body’s defenses due to mutations in the spike protein — accounted for nearly 55% of all strains circulating across the state as of June, the most recent data the state has.
“Since about April of this year, we've started noticing an increasing trend in the number of COVID cases that have been going on in the state of Colorado,” said Dr. Ming Wu, a primary care physician at AdventHealth in Littleton. “We've seen more cases in the clinics, people testing positive for COVID.”
Data from the state confirms those observations. COVID-19 cases have been on an upward trend since mid-May in Colorado, with nearly 1,300 new cases reported in just the last week alone, according to the latest data from the Colorado Department of Public Health and Environment (CDPHE). Those numbers are likely an undercount, however, since most people now test at home — if at all — and the majority don’t report their results to state or federal health authorities.
Hospitalizations for COVID-19 in Colorado have also increased to levels not seen since March, with 111 people hospitalized for the disease as of Tuesday compared to 66 at this same time last year — a nearly 70% increase when comparing year-to-year. It's not clear, however, how accurate this picture really is since hospitals are no longer required to report COVID-19 hospital admissions to the federal government.
Across the country, emergency room visits for COVID-19 increased to 23.5% as of July 6, according to the U.S. Centers for Disease Control and Prevention (CDC), with about 1.3 hospitalizations per 100,000 people. Though the numbers might seem concerning, they are still lower than last winter, when 7.7 hospitalizations per 100,000 people were reported by the CDC.
Concentrations of the virus in wastewater — which has replaced case numbers as a more reliable metric to show how prevalent the virus might be in the community — have also increased over the past several weeks across the state, with more than half of all treatment facilities showing steady increases in viral replication since early May, when none were, according to CDPHE data.
“The fact that we still have thousands — 2,000 cases — every week that are (being) reported is of concern,” said Dr. May Chu, a clinical professor at the Colorado School of Public Health. “It should tell us that we shouldn't forget that SARS-CoV-2 is still amongst us. It has not gone away.”
Though it may be surprising to some to see a rise in COVID-19 cases over the summer, Chu said that ever since SARS-CoV-2 appeared on the map, Colorado — along with the rest of the country — has always had a summer surge.
Chu said that virologists like herself expect that as the virus continues to circulate in people for the foreseeable future, “that a regular pacing might occur and then we can begin to predict when it could occur, probably along with the other respiratory viruses.”
It’s not clear if that will ever come to pass, however, as the CDC quietly admitted in an update posted over the Fourth of July holiday that SARS-CoV-2 is likely to remain a year-round threat given “there is no distinct COVID-19 season like there is for influenza (flu) and respiratory syncytial virus (RSV)."
In its update, the CDC recommended a multi-layered approach so you can protect yourself against infection and prevent others from becoming infected with SARS-CoV-2. The multi-layered approach includes getting vaccinated, wearing a well-fitting, high-quality mask, ventilating indoor spaces, practicing proper hand hygiene, and following CDC quarantine guidance if you test positive for the virus.
What’s causing the uptick in cases this summer? CDC officials say a number of factors could be at play, including new variants that are not just more transmissible but better able at getting past our body’s defenses, as well as decreasing immunity from previous infections and vaccinations.
Though the newer “FLiRT” variants have mutations that make them more transmissible, Chu said those mutations aren’t statistically important as their rate of transmission only varies slightly compared to previous strains. However, because many different strains of the virus are circulating at the same time, “you can imagine that there’s a lot more virus growing,” she said.
“Part of it too is a bit of the virus variation. The virus still is young enough that it'll keep changing based on environmental circumstances,” Chu said, adding that “as it changes, it could get worse or it could get less infectious. We actually don’t know.”
Wu, on the other hand, attributed the rise in COVID-19 infections to the low uptake of vaccines across the state.
Data from the CDPHE shows about 30% of Coloradans ages 5 and up have only gotten 3 doses of the COVID-19 vaccine (up to 6 doses are available now for certain groups of people).
“A lot of patients have said, you know, I've gotten enough COVID vaccines. I don't want this one, and so they haven't gotten it,” Wu said.
What you can do to protect yourself and others this summer While COVID-19 vaccines can protect you from getting seriously ill, they might not protect you against SARS-CoV-2 infection, both experts said.
“If you’re in a room that's tightly closed, with a lot of people that you don't know, you should mask because that increases the chance the transmission,” Chu said. “If you are the vessel for the reproduction of that virus, you're going to … make yourself sick, and other people are likely to get it from you. So you just have to be careful.”
Wu agreed, adding other measures like handwashing and socially distancing from others if you're sick could help protect not just yourself but others as well.
“If you do feel ill and you need to go out, wear a mask to protect your neighbor. If you sneeze and your germs aren't spreading everywhere, you're preventing your neighbor from getting that virus and so you're protecting the community,” he said.
If you test positive for COVID-19, Chu recommends calling your healthcare provider immediately and seek antiviral treatment like Paxlovid “as soon as you can” as it’ll help you from getting worse.
Those looking for added protection should get vaccinated now against COVID-19, both experts said, though if you want to wait it out a little longer, an updated COVID-19 vaccine targeting the most recent variants will be available later this year.
The threat of Long COVID remains after infection Though scientists and other health experts have seen a trend toward less severe outcomes and more typical symptoms of the flu with each new wave of the coronavirus, an encounter with COVID-19 doesn’t come without risks.
“With flu, there is not the residual Long COVID symptoms that about 8% of people suffer from. Flu doesn’t have that. RSV doesn’t have as much of that,” Chu said. “It is a risk and because this virus is still adapting to people, you're going to have lots of cases.”
While people who have had severe COVID-19 are at increased risk of developing Long COVID, CDC officials have said Long COVID can affect anyone, including children. Commonly reported symptoms include fatigue, brain fog and post-exertional malaise (PEM), but more than 200 symptoms have been associated with the condition which can affect various organs of the body, including the brain, the heart, the lungs, the kidneys, the reproductive system, among others.
The illness can last for weeks, months, or even years, and can be debilitating “in ways that significantly limit the daily activities of affected individuals,” according to the latest annual report on Long COVID in Colorado. It’s believed Long COVID has affected 10% of the state’s population so far.
Chu said that while scientists have been able to learn more about Long COVID since the start of the coronavirus pandemic four years ago, “the outcome at the moment still doesn’t tell you exactly how we can predict – one, if you can get Long COVID, and two – what your symptoms are (going to be). We're still gathering that information.”
Which is why Chu said it’s important for Coloradans to remember that COVID-19 is still around us and to be aware of the risk each infection can bring.
“If you are able to mitigate it, or reduce it by masking, by the various different kinds of practices that we've all known about for (years) now that continue to be in effect, then the risk of (developing Long COVID) gets lower,” she said.
#covid#covid 19#mask up#pandemic#coronavirus#sars cov 2#wear a mask#public health#still coviding#wear a respirator#covid news#covid pandemic#covid isn't over#the pandemic isn't over
18 notes
·
View notes
Text
CHIP Health Insurance: Ensuring Comprehensive Coverage For Kids And Teens
The Children’s Health Insurance Program (CHIP) is a lifeline for families across the United States, providing affordable and comprehensive health coverage for children and teens who fall just above the Medicaid income threshold. Administered jointly by federal and state governments, CHIP was established to make healthcare accessible for millions of kids, reducing financial barriers and ensuring that essential health services are within reach for families of varied income levels. Let’s delve into how CHIP works, its benefits, and why it remains a cornerstone for children’s healthcare in the U.S.
What is CHIP?
CHIP is designed to cover children and, in some cases, pregnant women who do not qualify for Medicaid but cannot afford private health insurance. It targets families with incomes up to around 300% of the federal poverty level, although this varies by state. CHIP has been instrumental in closing the healthcare gap by offering a range of benefits that ensure young people have access to preventive, emergency, and routine care. By alleviating financial burdens, CHIP promotes the well-being of children and teens, allowing them to grow up healthy and strong.
Key Benefits of CHIP Coverage
CHIP offers a wide range of essential services tailored to the unique health needs of children and teenagers. Some of the major benefits include:
Preventive Care
CHIP emphasizes preventive care, which includes regular check-ups, immunizations, and screenings. These services are vital for early detection of health issues, helping to prevent serious illnesses and maintain overall health. By covering these services, CHIP ensures that health issues are identified and managed early, reducing the risk of more severe conditions later on.
Doctor Visits and Hospital Care
With CHIP, families have access to affordable primary and specialist visits. This means children can see a physician when they need to, without worrying about the high costs associated with healthcare. Additionally, CHIP covers emergency services and hospital stays, offering a safety net when unexpected medical situations arise.
Vision and Dental Services
CHIP is unique in its inclusion of vision and dental care. Vision services, including eye exams and glasses, are covered to ensure that children’s sight issues are addressed, a critical factor for their academic and personal development. Similarly, CHIP covers preventive dental care like cleanings and fillings, which are vital for maintaining good oral health and preventing tooth decay.
Behavioral and Mental Health Services
Recognizing the importance of mental health, CHIP includes behavioral and mental health services. Children and teens have access to counseling, therapy, and other mental health services. This coverage is crucial for addressing issues like anxiety, depression, and behavioral disorders, ensuring that children receive the support they need during their formative years.
Prescription Medications
CHIP also covers prescription medications, which allows children to access necessary medications for chronic or acute conditions. This reduces out-of-pocket costs for families, making treatments more accessible and ensuring children adhere to prescribed therapies.
Why CHIP Matters Today
The importance of CHIP extends beyond healthcare access—it significantly impacts child development and family stability. Studies show that children with consistent healthcare coverage perform better in school and have fewer behavioral problems. CHIP’s role in supporting both physical and mental health leads to better educational outcomes, healthier family dynamics, and a more productive society.
Furthermore, CHIP reduces financial strain on families, allowing parents to focus on other essential aspects of their lives, like housing, education, and career growth, instead of worrying about unexpected medical bills.
How to Apply for CHIP
Applying for CHIP is straightforward and typically done through a state’s health department or a centralized online portal. Each state sets its income limits, eligibility criteria, and specific benefits, so families should check their state’s guidelines to determine if they qualify. Many states provide enrollment assistance to guide families through the process.
In Conclusion
CHIP stands as a testament to the value of investing in children’s health. By ensuring that essential services are accessible, CHIP application in PA promotes a future where every child can lead a healthy, fulfilling life, regardless of their family’s financial situation. This program remains a vital resource for American families, protecting the health of millions of children and offering peace of mind to parents nationwide.
0 notes
Text
Do pain patients on long-term opioid therapy make irrational decisions? Is their mental capacity so diminished by opioids that they shouldn’t be involved in treatment decisions with their doctors? The answer to both questions is often yes, according to a controversial new op/ed published in JAMA Internal Medicine. At issue is a recent update to the CDC’s opioid prescribing guideline, which calls for shared decision-making (SDM) when a prescriber considers tapering a patient or abruptly discontinuing their opioid treatment. The guideline was revised last year after reports of “serious harm” to patients caused by forced tapering.
“In situations where benefits and risks of continuing opioids are considered to be close, shared decision-making with patients is particularly important,” the 2022 guideline states. But that advice about consulting with patients goes too far, according to the lead author of the JAMA op/ed, Mark Sullivan, MD, a professor of psychiatry at the University of Washington and a longtime board member of Physicians for Responsible Opioid Prescribing
“The value of SDM has been recognized for many years but also has its limitations, including where patients make irrational or short-sighted decisions,” Sullivan wrote. “Long-term opioid therapy induces a state of opioid dependence that compromises patients’ decisional capacity, specifically altering their perception of the value and necessity of the therapy; and although patients with chronic pain are not usually at imminent risk of death, they often can see no possibility of a satisfying life without a significant and immediate reduction in their pain.”
Sullivan and his two co-authors, Jeffrey Linder, MD, and Jason Doctor, PhD, have long been critical of opioid prescribing practices in the U.S. In their conflict of interest statements, Sullivan and Doctor disclose that they have worked for law firms involved in opioid litigation, a lucrative sideline for several PROP members...
...“In the case of opioid prescribing, and especially opioid tapering, working to persuade the patient is almost always the best clinical strategy. But there are circumstances (opioid use disorder, diversion, serious medical risks) where tapering should occur even if the patient objects,” Sullivan wrote. Opioid diversion by patients is actually rare. The DEA estimates that less than one percent of oxycodone (0.3%) and hydrocodone (0.42%) will be used by someone they were not intended for.
As for patients on opioids behaving “irrational,” Sullivan and his co-authors cite an op/ed published 33 years ago in The New England Journal of Medicine (NEJM). But that article doesn’t even discuss opioids or tapering, it’s about whether patients and doctors should collaborate in making decisions about end-of-life medical care. It also makes an important disclaimer that “even the irrational choices of a competent patient must be respected if the patient cannot be persuaded to change them." Sullivan rejects that approach to opioid treatment...
...In a rebuttal to Sullivan’s op/ed also published in JAMA Internal Medicine, Mitchell Katz, MD, and Deborah Grady, MD, disputed the notion that a patient’s choices shouldn’t be respected. “Primary care professionals generally highly value the inclusion of the patient’s perspective in decision-making, consistent with the principles of patient autonomy and self-determination, and are loathe to go against a patient’s wishes,” they wrote. “As primary care professionals, we have found it helpful to tell patients that it is not recommended to take more than a specific threshold of opioids and that we do not want to prescribe something that is not recommended. However, that does not mean sticking to rigid cut points for dose and duration of opioid use, abandoning patients, or having them undergo too rapid a taper.”
Others questioned JAMA’s decision to publish Sullivan’s op/ed. “While I recognize the editors’ legitimate intellectual interest in providing a forum for open discussion on the opioid policy space, I question their decision to publish an editorial that represents an ongoing call for broad, ill-defined reductions in opioid prescribing,” said Chad Kollas, MD, a palliative care specialist who rejects the idea that patients shouldn’t be involved in their healthcare choices. “Errantly embracing a lower evidentiary standard for medical decision-making capacity creates an unacceptable risk for harm to patients with pain by violating their rights of medical autonomy and self-determination.” (Full article at link)
So essentially a man with a bias against opioids and who makes money litigating against uses a 33 year old op ed to assert pain patients shouldn't have a say in their medical care because we irrational. Proof of that irrationality is that if we have to deal with severe chronic pain with no relief, we may contemplate suicide. So fucking irrational, right? 🤬
This man is fucking cruel and inhumane. He works for an organization (PROP) that has had direct influence on the 2016 CDC Opioid Guidelines which lead to many pain patients committing suicide or dying from complications due to forced tapering and withdrawals. And this man has been given a platform to assert that our desire to not exist in severe daily pain is irrational. Fuck him!
#disability#chronic pain#ableism#opioids#chronic illness#medical bias#suicide cw#forced tapering#spoonies#PROP#cdc guidelines#article
27 notes
·
View notes
Text
The Global Office Based Labs Market is projected to grow from USD 24,540 million in 2023 to an estimated USD 42,798.92 million by 2032, with a compound annual growth rate (CAGR) of 7.20% from 2024 to 2032. In recent years, the healthcare industry has witnessed significant advancements, particularly in the way outpatient care is delivered. One such development is the emergence and growth of the office-based labs (OBLs) market. These facilities, which offer specialized procedures outside of traditional hospital settings, have garnered attention for their ability to provide efficient, cost-effective care. With the shifting dynamics in healthcare, particularly around value-based care, office-based labs are poised to play a pivotal role in the future of outpatient procedures. In this article, we will explore the current state of the OBL market, the factors driving its growth, challenges, and what the future may hold.Office-based labs are medical facilities typically located in physician’s offices or outpatient centers where minimally invasive procedures are performed. These labs are most commonly associated with interventional procedures, such as vascular, endovascular, and cardiology-related treatments. Unlike ambulatory surgery centers (ASCs), OBLs are smaller, more specialized facilities that focus on specific types of procedures, offering convenience and efficiency to both physicians and patients.
Browse the full report at https://www.credenceresearch.com/report/office-based-labs-market
Key Market Drivers
1. Cost Efficiency: One of the primary drivers of the office-based labs market is the cost savings they offer compared to hospital-based outpatient procedures. Hospitals have higher overheads, which translate into more expensive services. OBLs, by contrast, can deliver similar or even superior quality of care at a fraction of the cost, which appeals to both patients and insurance providers.
2. Technological Advancements: Innovations in medical technology have made it possible for complex procedures to be carried out in non-hospital settings. Minimally invasive tools, advanced imaging techniques, and improved anesthesia options enable physicians to perform procedures safely and effectively in OBLs.
3. Shift Toward Outpatient Care: Healthcare systems across the world are moving towards outpatient care, primarily driven by the focus on value-based care. This shift encourages healthcare providers to deliver high-quality care while reducing costs. Office-based labs fit well into this model, allowing patients to receive care in a more convenient, lower-cost setting without sacrificing quality.
4. Increasing Prevalence of Chronic Diseases: Conditions such as cardiovascular disease, diabetes, and peripheral artery disease are on the rise globally. These conditions often require ongoing, non-invasive or minimally invasive treatments that can be performed in an office-based lab setting. As the incidence of these diseases continues to climb, so too does the demand for OBL services.
5. Favorable Regulatory Environment: Regulatory bodies, particularly in the U.S., have been supportive of office-based labs. The Centers for Medicare and Medicaid Services (CMS) have approved reimbursement for many procedures performed in OBLs, further driving their adoption.
Market Size and Growth
The global office-based labs market is expected to grow significantly over the coming years, with North America currently holding the largest market share. The market is expanding rapidly in Europe and Asia-Pacific as well, fueled by the increasing prevalence of chronic diseases and a growing preference for outpatient procedures. The market’s growth trajectory is supported by the continued increase in healthcare expenditure, greater awareness about minimally invasive procedures, and rising demand for cost-effective healthcare solutions.
Challenges Facing the OBL Market
Despite the clear benefits and rapid growth of office-based labs, the market is not without its challenges:
1. Regulatory Hurdles: While the regulatory environment is generally favorable, there are still complexities involved in establishing and maintaining an OBL. Each facility must meet stringent requirements related to safety, accreditation, and reimbursement, which can create barriers to entry for smaller practices.
2. Competition with Hospitals: OBLs, by nature, reduce the revenue stream for hospitals that traditionally performed these procedures. Hospitals may respond by leveraging their resources to retain patients or by entering the OBL market themselves, creating competition for independent labs.
3. Physician Training and Recruitment: Successfully running an OBL requires a skilled team of healthcare professionals. Recruiting and retaining experienced physicians and staff can be a challenge, particularly as demand for specialized care continues to rise.
4. Reimbursement Issues: While many procedures are reimbursed by CMS, reimbursement rates can vary, and some private insurance providers may not cover all the procedures performed in an OBL. This inconsistency in payment can affect the profitability of OBLs.
The Future of Office-Based Labs
The future of the office-based labs market appears bright, particularly as the healthcare industry continues to embrace outpatient care models. Advances in medical technology, a greater focus on patient convenience, and the cost benefits offered by OBLs suggest that this market will continue to expand. Additionally, as more procedures become viable for office-based settings, the scope of services offered by these labs will grow.
However, to sustain this growth, OBL operators will need to navigate regulatory challenges, ensure consistent reimbursement for their services, and continue to invest in skilled staff and cutting-edge technology. Collaboration with hospitals and other healthcare providers may also be key to maximizing patient outcomes and minimizing competition.
Key players
Koninklijke Philips N.V.
GE Healthcare
Siemens Healthineers
Medtronic
Cardiovascular Systems, Inc.
Envision Healthcare
Surgery Care Associates, Inc.
Surgery Partners
Fresenius Medical Care
Terveystalo Healthcare
Healthway Medical
Quorum Health
HCA Healthcare
Tenet Healthcare
Mednax
Segments
Based on Modality
Single Specialty
Multi-Specialty
Hybrid
Based on Service Type
Peripheral Vascular Intervention
Interventional Radiology
Endovascular Therapy
Cardiovascular
Others
Based on Region
North America
US
Canada
Latin America
Brazil
Argentina
Mexico
Rest of Latin America
Europe
Germany
UK
Spain
France
Italy
Russia
Rest of Europe
Asia Pacific
China
India
Japan
Australia
South Korea
ASEAN
Rest of Asia Pacific
Middle East
GCC
Israel
Rest of Middle East
Africa
South Africa
North Africa
Central Africa
Browse the full report at https://www.credenceresearch.com/report/office-based-labs-market
About Us:
Credence Research is committed to employee well-being and productivity. Following the COVID-19 pandemic, we have implemented a permanent work-from-home policy for all employees.
Contact:
Credence Research
Please contact us at +91 6232 49 3207
Email: [email protected]
Website: www.credenceresearch.com
0 notes