#Test FODMAP
Explore tagged Tumblr posts
Text
Régime FODMAP : Guide Complet et Conseils Pratiques

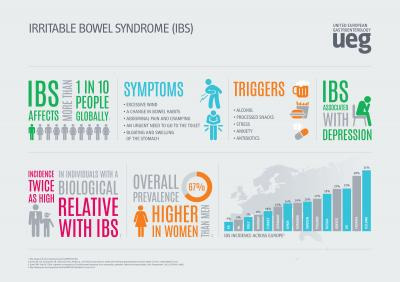
Le régime FODMAP est devenu un sujet brûlant dans le domaine de la nutrition et de la santé digestive. Mais qu'est-ce que le régime FODMAP, exactement, et comment peut-il aider ceux qui souffrent de troubles gastro-intestinaux tels que le syndrome du côlon irritable (SCI) ?
Qu'est-ce que le Régime FODMAP ?
Les FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, And Polyols) sont des sucres fermentescibles présents dans de nombreux aliments courants. Pour certaines personnes, ces composés peuvent être difficiles à digérer, entraînant des symptômes désagréables tels que ballonnements, gaz, douleurs abdominales et diarrhée.
Le régime FODMAP est une approche diététique qui vise à réduire la consommation de ces sucres fermentescibles afin de soulager les symptômes du SCI et d'autres troubles gastro-intestinaux. En éliminant ou en réduisant les aliments riches en FODMAP de l'alimentation, de nombreuses personnes ont constaté une amélioration significative de leurs symptômes digestifs.
Les Principes du Régime FODMAP
Le régime FODMAP se décompose en plusieurs phases :
Phase d'élimination : Pendant cette phase, les aliments riches en FODMAP sont éliminés de l'alimentation pendant une période de temps déterminée, généralement de deux à six semaines.
Phase de réintroduction : Une fois la phase d'élimination terminée et les symptômes soulagés, les aliments FODMAP sont réintroduits un par un pour déterminer lesquels peuvent être tolérés et en quelle quantité.
Phase de personnalisation : En fonction des réponses individuelles, un régime alimentaire personnalisé est établi pour chaque personne, en tenant compte des aliments tolérés et de leurs quantités.
Aliments à Éviter et Aliments Autorisés
Pendant la phase d'élimination du régime FODMAP, il est important d'éviter les aliments riches en FODMAP tels que :
Les oignons et l'ail
Les produits laitiers contenant du lactose
Les légumineuses
Certains fruits tels que les pommes, les poires et les cerises
Certains légumes tels que les choux, les champignons et les asperges
En revanche, de nombreux aliments sont autorisés dans le cadre du régime FODMAP, notamment :
Les viandes maigres
Le poisson
Les œufs
Les céréales sans gluten, comme le riz et le quinoa
Certains fruits et légumes à faible teneur en FODMAP, comme les fraises, les bananes et les carottes
Conseils Pratiques pour Suivre le Régime FODMAP
Suivre un régime FODMAP peut sembler intimidant au début, mais avec un peu de planification et de créativité, il est tout à fait possible de manger délicieusement tout en respectant les principes du régime. Voici quelques conseils pratiques pour vous aider en cours de route :
Planifiez vos repas à l'avance : En planifiant vos repas à l'avance, vous pouvez vous assurer de toujours avoir des options adaptées au régime FODMAP sous la main.
Familiarisez-vous avec les étiquettes nutritionnelles : Apprenez à repérer les aliments riches en FODMAP sur les étiquettes nutritionnelles afin de prendre des décisions éclairées lors de vos achats.
Expérimentez avec de nouvelles recettes : Essayez de nouvelles recettes et techniques de cuisson pour diversifier votre alimentation tout en respectant les principes du régime FODMAP.
Consultez un professionnel de la santé : Si vous envisagez de suivre le régime FODMAP, consultez d'abord un professionnel de la santé, de préférence un diététicien ou un nutritionniste spécialisé dans les troubles gastro-intestinaux.
Conclusion
Le régime FODMAP est une approche diététique prometteuse pour soulager les symptômes du syndrome du côlon irritable et d'autres troubles gastro-intestinaux. En suivant les principes du régime et en faisant preuve de créativité dans votre alimentation, vous pouvez réduire vos symptômes digestifs et améliorer votre qualité de vie.
Si vous souhaitez lire plus d’informations sur le régime FODMAP, visitez → Régime FODMAP : Guide Complet et Conseils Pratiques
#Régime FODMAP#Aliments pauvres en FODMAP#Intolérance aux FODMAP#Recettes adaptées au FODMAP#Régime d'élimination FODMAP#Sensibilité aux FODMAP#Aliments riches en FODMAP#Tableau FODMAP#Liste FODMAP#Directives FODMAP#Plan de repas FODMAP#Liste de courses FODMAP#Diététicien spécialisé en FODMAP#Livre de recettes FODMAP#Test FODMAP#Application FODMAP#Collations adaptées au FODMAP#Restaurants adaptés au FODMAP#Phase d'élimination FODMAP#Phase de réintroduction FODMAP#Conseils de cuisine FODMAP#Ingrédients adaptés au FODMAP#Desserts adaptés au FODMAP#Légumes adaptés au FODMAP#Fruits adaptés au FODMAP#FODMAP meal plan#FODMAP app
1 note
·
View note
Text
the doctors have banned me from eating foods i like tommorow. and im supposed to lock in???? in this state
#the irony of them recommending the other food i might be allergic to to have the day before my allergy test is not lost on mr#*me#but yeah. soft drinks. lactose. honey. canned fruit. um. fodmap#my posts
5 notes
·
View notes
Note
Do you have any proven IBS friendly recipes you'd care to share on The Mind Palate? It's so hard to think of new things to cook when you tolerate like 5 vegetables 🥲.
Btw did you know there's another website called "mind palate", just without the "the"?
As regards IBS: I wouldn't dare share recipes purporting to be useful for other folks with this issue, as every kind of IBS is different. And even for any single IBS-haver, a recipe that's safe for you one week might not be safe for you two weeks later... because the ingredients have varied, or the relative amounts of them have varied, or something you're having with them might differ in ways that throw off their interaction with your gut. :/ This is a pain in the butt, but (shrug) here we are.
To manage my IBS—as there is at present no known cure, no matter what some people claim—I use the well-known Monash University FODMAP-based approach. When I started using it a few years ago—on realizing that some food-related symptoms I was experiencing mapped very closely onto descriptions of IBS symptoms—the abdominal troubles I was experiencing decreased by sort of 95% almost immediately.
The message was too straightforward to ignore. I immediately started adjusting my diet along FODMAP-conscious lines in an Every-Woman-Her-Own-Test-Tube sort of way, and quickly started discovering what gave me the most trouble. (To my intense annoyance, the chief answer to this question, among various others, was "onions and garlic." Two of my absolutely favorite things, and I find it hard to express how INCREDIBLY PISSED OFF this makes me.)
I'm also lactose-intolerant, but for that all I have to do is take a pill. As regards other IBS-triggering foods, there's no known way to stop the bad effects once they start. Some medications will let you offset some of the worst effects in their very early stages... if you take the meds soon enough. But you can't usually tell for sure until six to eight hours or so after a given meal whether "you chose poorly...", and whether you're going to spend the next two to three days bedridden, in more or less constant abdominal pain, and useless for any kind of work.
(sigh) Anyway. I'm fortunately not troubled too much by vegetables as a class.* Though I find (to my intense annoyance) that when I'm lucky enough to be in the right parts of Europe around Spargelzeit, asparagus is pretty much now off my menu. Like many other IBS-managing folk, I do have to be very careful around beans, pulses in general, and some kinds of fruit; and I have to limit my serving sizes/consumption.
(shrug) It's all an ongoing challenge. I had sixty-plus years of eating any damn thing I pleased, in whatever amounts I pleased, whenever I pleased. Now I have to very closely read ingredients labels to make sure there's nothing in a given innocuous-looking bag of snacks that's going to land me on my back for days. :) If it gets no worse than this for me, I'm sure I can cope. I'm just glad I'm in the EU, where detailed ingredients labeling is mandated even for street food stalls, and is also clearer than it is in a lot of other parts of the world.
Meanwhile: I'm sorry not to be of more help to you in this regard. I wish you good fortune in your journey to find safer veggies.
As regards other people's "mind palate" branding and websites: There are five or six different versions of the domain name out there. They don't bother us. I've been a Sherlockian for more than sixty years, and I'll make my puns (from newer variants on the great Theme) where I please. Those other users of the site name or similar domains? (shrug)
*...BTW, it's been brought to my attention recently that a rumor was making the rounds that I'm a vegetarian. (Once again, and not for the first time, wondering how the hell these things get started...?!) 😄 I'm an omnivore, and have never from the beginnings of my time in public life/fandom claimed to be otherwise. (And plainly, no one who's bought into this has ever seen me getting to grips with a steak. Vide this recent steak, last October I think, at Davy Byrnes—"the Moral Pub" as James Joyce once called it—in Dublin. It was yummy. And in the middle of it I had the concept for a really unusual novel occur to me. Meanwhile, that Hollandaise was lovely.)

(...but shrugging in a helpless way about the rumor) Maybe somebody saw me pass on all the meat-ish possibilities at some convention banquet in favor of the vegetarian one? That would simply have been because it looked better than anything else on offer. But right now, because of the IBS, meat and fish are (maybe paradoxically) safest for me. Go figure.
...Meanwhile—all that aside—as a fan of the place's cuisine for many years, I direct everyone's attention to the noble and excellent restaurant Hiltl (known to its fans as Hiltl Vegi), the world's oldest continuously operating vegetarian restaurant, in Zürich: a place old enough for Sherlock Holmes to have eaten there (and where I hope to send him yet). Come for the (predominantly Indian) lunch buffet. Stay for the wine list (one of the best in the city). :)
206 notes
·
View notes
Text
No new chapter this week for "Trust Me"
So, I won't be able to update on feb 19 as I had planned for my starscream fic : c
A lot has happened, like oh man... I'm starting to believe in the fanfic author's curse x.x Long story short: I hadn't slept well for three weeks now. My heart had been causing issues, keeping me awake. Currently in mexico and got checked out by doctors - US doctors did not take my issues seriously for the past year and just blamed my issues due to stress. Mexican doctors found out through tests that i got a heart arrhythmia, and they are not sure if it's permanent, or caused by the infection in my blood stream that they found out too... which is causing me to have low levels of iron too.
Luckily, i am starting treatment to get rid of the infection, and boost my iron levels back up. Hopefully the heart arrhythmia is not permanent and i can sleep properly again.
But yah, i've been exhausted due to not sleeping well, some days i don't sleep, some i slept for 1-3 hours. I was given sleeping pills that for some reason only help me sleep for 4-5 hours.
that's why I won't have a new chapter out : c. I am writing, but slowly. And I will do my best to finish the chapter as soon as i can since i also don't like not writing anything v.v
But yah, this fanfic author curse is starting to scare me, ahhh x.x. especially since the next chapter is one i've also been excited to write (megatron stuff and starscream too) Honestly, I'm just so glad to find out the issues i've been having were not in my head... and i was for sure sick from something :/
Peeps, if you feel something is wrong with your health, for sure push peeps to take it seriously. cause geez, it's crazy how some docs don't take it seriously and give u treatments without doing important tests first. I was legit put into a fodmap diet during the time the infection was attacking my abdomen organs -.-. Anyway, I hope next time i post something on tumblr is for the new chapter or some good news : )
I thank you all for the support. I truly appreciate you all <3
#Starscream#transformers#tf#tfe#transformers earthspark#fanfiction#writing#author#fanfic author#Megatron#Optimus Prime
61 notes
·
View notes
Text
Story time: Rage
A year ago, I went to my doctor because I was having unusual stomach-related symptoms that had progressed from annoying to painful.
He looked at my chart and started asking me questions about my anxiety. Even when I emphasized that yes, I had an anxiety disorder but it had never manifested in stomach symptoms before, he continued to ask me questions about my home life and stress levels. "Oh, you're planning your wedding? I'm sure that's very stressful."
He then asked if I was on medication for my anxiety and suggested a follow-up with my therapist. When I pressed for any other recommendations to address my symptoms, he suggested I try a low fodmap diet and keeping a food journal for a few months to identify trigger foods.
I tried the low fodmap diet. I kept a food journal.
My symptoms got progressively worse.
When we moved to Denver, I had to wait 3 months for a new patient visit to establish care with a GP here. I explicitly requested a female doctor. When I finally got in, she was immediately concerned when I told her about the last 11 months of issues that were now actively impacting my quality of life. She didn't ask me a single question about my anxiety. She ordered a bunch of tests and referred me to a GI doc (also a woman) who ordered more tests. Less than 24 hours after the GI doc's test results came back, I'm now on three antibiotics to treat a (what is now raging) bacterial infection. Because it's been going on for so long and my symptoms have progressively worsened, there are concerns about long term damage to my stomach and digestive tract.
But no, dude. It was probably my silly female anxiety about planning my wedding.
#anger#medical shit#i'm only seeing female doctors from here on out#gender bias#healthcare#peep deacon with his new squeaky toy in the background#mylife#the tiniest of violins
225 notes
·
View notes
Text
I’ve been looking for some recipes to share that’s good for dietary restrictions. “Why?” You may ask.
Well, it’s because I’ve been thinking about potlucks. Neighborhood block parties. About people coming together and feeding each other and enjoying each other companies and having fun.
But anywho, I’m thinking of putting them all on one post. Except for this particular article because unfortunately America Test Kitchen has 2 free articles per month for people who don’t subscribe to them. So while I’ll still post the link, I’m also having the article underneath the cut. Enjoy the food ideas to share with others!
Recently, I hosted a four-day gathering for nine people with 10 different dietary restrictions. To say I was worried would be a vast understatement.
We had everything: no gluten, no meat, no dairy, no mushrooms, and much more. All had varying degrees of importance from “just a preference” to “just in case, do we know where the closest hospital is?”
Many restaurants are aware and accommodating of dietary issues, but it can be difficult when this problem arises at home. You can’t make different dinners for everyone.
We’ve compiled a list of suggested meals and preparation styles to cook for a crowd where everyone—including the host—enjoys the dinner, feels included, and stays healthy.
(But first, an important disclaimer: There's more to cooking for people with special diets than just choosing a recipe. If you're cooking for someone with severe allergies, make sure they're comfortable with your serving setup.)
Spread-Style Meals That Offer Ultimate Flexibility
My coworkers are food lovers and problem solvers. When I asked them what they would serve in this scenario, they all had the same answer: DIY-style meals offer the most flexibility for the diners and the least amount of stress for the cook.
Build-it-yourself meals allow people to select what foods work for them and avoid the ones that don't, without putting the responsibility on you.
For tackling this kind of meal, we suggest taking inventory of all guests' allergies (and the level of cross-contamination they allow) and then creating a themed dinner with choose-your-own elements. Make sure each person has at least one option at every step.
Here are a few of our favorites:
1. Build-Your-Own Bowls
Bring Sweetgreen home by making a couple plain bases, a few simple proteins, and some roasted veggies, and ending it all with a topping and sauce bar.
Bases: Everyday White Rice, Foolproof Oven-Baked Brown Rice, Quinoa Pilaf with Herbs and Lemon, Basic Farro Pilaf
Proteins: Pan-Seared Chicken Breasts, Garlicky Broiled Shrimp, Teriyaki Tofu, tempeh steaks, sautéed eggplant with plant-based meat
Veggies: Skillet-Roasted Carrots and Parsnips; Skillet-Roasted Broccoli; Kale with Garlic, Red Pepper Flakes, and Lemon; Roasted Sweet Potatoes
Sauces: Hummus with Smoked Paprika, dairy-free green goddess dressing, Roasted Garlic Chimichurri, Lemon Aioli, Tzatziki Sauce, Red Pepper–Almond Sauce
Toppings: Microwave-Fried Shallots, shichimi togarashi, Microwave Cheese Crisps, Gim, Chili Crisp
2. Make-Your-Own Pizza
Whether you have an indoor or outdoor pizza oven or you simply make them on the grill or in your oven, making your own pizza is one of the easiest DIY meals because it mostly just requires the host to chop toppings and stretch dough.
Almost all ingredients can be store-bought, but if you feel like elevating the experience with a few homemade options, we have some suggestions.
Dough: Classic Pizza Dough, gluten-free pizza dough, thin-crust whole-wheat pizza
Sauce: No-Cook Pizza Sauce, Basic Pizza Sauce, Perfect Pesto, alfredo sauce
Toppings: Caramelized Onions, pepperoni, roasted vegetables, anchovies, Spicy Honey, dollops of homemade ricotta
3. Burrito/Taco Bar
For this simple spread, make a variety of proteins and vegetables, buy any additions, have a few homemade salsas on hand, and let your guests decide whether or not to use flour, corn, or other types of GF or dietary-specific tortillas.
Fillings: Plant-based chorizo, shredded chicken, sweet and spicy fried fish, grilled steak, bean and vegetable
Salsas: Fresh Tomato, Roasted Tomato–Lime, Salsa Roja, Quick Tomatillo, Mango-Mint, fresh corn and avocado
Additions: Tangy Apple-Cabbage Slaw, Bell Pepper Slaw, Chipotle and Pepita Guacamole
Single Recipes for Multiple Dietary Requirements
When you don’t want to prepare an entire spread and instead just feel like making one dish that has several dietary accommodations baked in, we have some options for you.
I asked my coworkers: Whether vegan, vegetarian, soy-free, nut-free, gluten-free, or peanut-free, what do you make when trying to accommodate multiple diets?
1. Japchae
This was my go-to meal when cooking for my large, dietary-restricted crowd and it was a hit. The base noodles, Korean sweet potato noodles, are naturally gluten-free and hold onto sauce really well. To keep the dish gluten-free, I used tamari instead of soy sauce which generally contains wheat. To accommodate a pescatarian and someone with a mushroom allergy, I just cooked these elements separately and left them on the side for people to sprinkle onto their own plates.
Who It’s Good For: Those following dairy-free, gluten-free, peanut-free, tree nut–free, soy-free (using tamari), vegetarian, and vegan diets.
2. Breakfast Casserole
Essentially a crustless quiche in a baking dish, a breakfast casserole is great for a varied crowd because you can swap any protein, vegetable, or spice in or out depending upon your group's dietary needs. One of our members raved, “One of us is dairy-free, the other has celiac, so this was perfect to please everyone."
Who It’s Good For: Those following dairy-free, gluten-free, soy-free, peanut-free, tree nut–free, or vegetarian (provided they eat eggs) diets.
3. Red Lentil Soup
This soup is spiced, rich, and nourishing because of the thick texture and nutrients that simmered red lentils bring. To make this a complete meal, pair it with a hearty salad and serve dressings on the side.
Who It’s Good For: Those following gluten-free, dairy-free, peanut-free, nut-free, soy-free, vegetarian or vegan (if you use vegetable broth instead of chicken broth) diets.
4. Vegan Barbecue Tempeh, Mushroom, and Bell Pepper Skewers
Tempeh is an awesome, naturally gluten-free (most often; check your brands) vegetarian protein for grilled skewers. You can add any vegetables, or even fruit, to your skewers and the same glaze can be used for any meat skewers you make separately.
Who It’s Good For: Those following gluten-free, dairy-free, peanut-free, nut-free, soy-free, vegetarian or vegan diets.
5. Walkaway Ratatouille
Most ratatouille recipes call for labor- and time-intensive treatments like salting and/or pressing to remove excess moisture from the vegetables. Not only is this meal largely hands off and fuss-free, but it's also ready in under an hour, and it’s chock-full of vegetables while accommodating some of the most common dietary restrictions.
Who It’s Good For: Those following dairy-free, gluten-free, peanut-free, tree nut-free, soy-free, vegetarian, and vegan diets.
6. Falafel
Like a cross between a spread meal and a single dish, making falafel the centerpiece of your dinner allows you to provide lots of pita, sauces, and toppings on the side for people to choose from while you only have to cook one main element. Though this recipe uses all-purpose flour, an equal amount of chickpea flour can be substituted for a gluten-free version. To accommodate this substitution, we increase the water.
Who It’s Good For: Those following dairy-free, gluten-free, peanut-free, tree nut-free, soy-free, vegetarian, and vegan diets.
7. Chili-Spiced Chicken Thighs and Potatoes
This recipe is a great example of a jazzed-up protein that is still widely applicable to different dietary needs without sacrificing flavor. It can serve as a complete meal as is, or for a vegetable element you can add some simply dressed greens on the side.
Who It’s Good For: Those following dairy-free, gluten-free, peanut-free, tree nut-free, and soy-free diets.
8. Best Prime Rib
Provided your guests eat meat, you’re in luck. Though this is technically a plain protein, there is nothing plain about a centerpiece-worthy prime rib. Serve it with any vegetable sides, salads, or potatoes to round out the meal.
Who It’s Good For: Those following dairy-free, gluten-free, peanut-free, tree nut-free, and soy-free diets.
9. Chicken Shawarma
Instead of going out for shawarma, we were able to create a home version by using the broiler and boneless chicken thighs. Chicken shawarma allows guests to assemble their own pita pockets with as much or as little sauce and vegetables as they desire. To accommodate more diets, make roasted tofu as a vegetarian option and provide gluten-free pita.
Who It’s Good For: Those following gluten-free, peanut-free, tree nut-free, and soy-free diets.
Allergy-Friendly Swaps We Love
Sometimes a recipe is so close to fitting your restrictions but doesn't quite work because of an ingredient or two. We have a few standby swaps that are typically fine in small amounts without significantly altering the overall recipe.
* Swap tamari for soy sauce when you need to be gluten-free.
* Swap sunflower seed butter for peanut butter when you need a peanut- or tree nut–free alternative.
* Swap vegan, non-dairy milks for cow’s milk. We like oat milk when baking due to its higher sugar content and almond milk in savory applications because it is more neutral.
* Swap garlic or onions for garlic oil when alliums can cause an issue, such as with the Low FODMAP diet.
#Solarpunk#food#recipes#dietary restrictions#block party#potluck#vegan#vegetarian#food allergies#gluten free#peanut allergy#party#meal#website articles#cooking
16 notes
·
View notes
Note
I kind of want to hear more about like Jamie trying to manage having a chronic illness while also being like a professional athlete. (although we are giving our issues with things to people I have a strong feeling Roy is prone to like tension headaches. )
You lot are feeding me well tonight :)))))
Listen - IBS Jamie is purely for my own joy tbh there is nothing in canon even if I did make a list of some things that could apply >>>> you can find it here
It's a bullshit diagnosis anyway, cause even doctors don't know what is wrong and say it to dismiss you. So I can see him having all these issues and when he does all the tests there is nothing wrong with him and they say it's all in his head and he has to learn to live with it and manage it (there are some studies that bring on the hypothesis that there might be a link to physical, emotional or sexual abuse in childhood and with trauma in general which fits the bill with him, but I am too dumb to actually understand them but oh hey this is fiction we can do what we want!)
From my experience, exercise can be both a very good and a very bad thing. Usually fine during, but when you push too much you might feel unwell and we know he 100% over-does it. I can see him struggling with accepting he needs to put limits in place, he has to allow his body to rest and has to have regular meals etc He would be very frustrated with it. Personally it's actually fucked up my confidence massively as my therapist put it "have you ever thought that your lack of confidence also comes from not being able to ever trust your own body?" funny lady isn't she my own Doc
I think Roy having his own chronic issues (that man hurts just look at him lol but I can see headaches for sure) is actually very understanding once Jamie manages to open up about it which takes a long time >> bootroom breakdown is so spot on for being in the middle of a flare when you are still expected to operate at 110% but you're exhausted, lack of sleep is making it worse, you're bloated as fuck and your tummy hurts and you can't bother with anything (hair, personal care etc) and you just want to curl up and cry >>> Roy helping him put things in place to help like making a meal plan with the doctors of low fodmap items and ensuring the canteen is aware, always having cozy clothing around that is loose around the waist and a heat pad ready to go in the office, well stocked cabinet of ibs friendly tea (he's a tea guy anyway!), he suggest a meditation/yoga session for the afternoons and he makes jamie keep a food/symptoms diary (which then he ends up keeping cause jamie is not organised at all and roy is sorting out 90% of hid meals anyway!!). He also makes him see Dr Sharon because stress can make it worse!
Oh and Roy does gift him this too:

13 notes
·
View notes
Text
Man I am so sick of the holistic medicine supplement industry. Especially this new obsession with "gut health" and "liver health". Girl you do not need to take 5000 dollar vitamins to clean your body of toxins when your liver works properly and if It didn't you need medical intervention. Or Like your gut isn't struggling with permeability or full of parasites randomly if you have digestive issues for real you need to see a doctor and get help. Parasites require testing to diagnose and medication to stop. Stop with the "cleanses" and pseudoscience and then stop looping it back with diet culture like "erm you need to eat this way because otherwise you're poisoning your gut!" No actually maybe actually food is fine and if you have issues with certain foods something else is going on (ie a fodmap food triggering ibs, lactose triggering lactose intolerance, tomatoes triggering Gerd, etc) or even something worth medical attention. Stop it with "clean food" explode actually I'm so sick of it all
8 notes
·
View notes
Text

Spinach Frittata Recipe
Serving: 8
Ingredients
1 tablespoon olive oil
1 small leek white and light green parts only, halved and sliced into half moons; sub with your favorite onion
1 clove garlic minced
4-5 ounces baby spinach see notes for frozen spinach
8 large eggs
1/2 cup half and half sub with your favorite dairy or non-dairy milk
1/2 cup crumbled feta cheese
2 tablespoons chopped fresh dill
Salt and pepper to taste
Directions
Preheat the oven to 400° degrees. Heat the olive oil in a medium 10" cast iron or heatproof skillet over medium heat. Add the leek and cook 3 minutes until softened. Add the garlic and cook 30 seconds more. Add the baby spinach and cook 2-3 minutes or until completely wilted, then pour the mixture out onto a cutting board and roughly chop.
Brush olive oil from the bottom of the pan around the edges of the skillet (or add more oil if needed), then add the spinach mixture back to the pan and spread evenly across the bottom.
Beat the eggs with the half and half until well blended, then whisk in the feta cheese, chopped dill, salt and pepper to taste until combined. Pour the egg mixture over the top of the spinach mixture.
Cook the frittata on the stove top over medium heat just until the edges begin to set (about 2 minutes), then place in the oven. Bake for 8-10 minutes or until puffed and golden on top. Remove from heat and allow to cool slightly. Enjoy!
Notes
Pro tip: 4-5 ounces of baby spinach sounds like a lot, but it cooks down considerably. Chop the spinach after cooking to make it much easier!
I have not tested this recipe with chopped frozen spinach, but it should work no problem. Simply thaw it first and squeeze out excess water.
Omit the leek and garlic if following a Low FODMAP diet.
Leftover frittata keeps well in an airtight container in the refrigerator for up to 3 days.
(Source)
12 notes
·
View notes
Text

Eating healthy but still struggling with Bloating, Acidity and poor Gut health? You’re not alone! Your gut might be reacting to certain foods high in FODMAP's.
FODMAP stands for:Fermentable – These carbs ferment in your gut, causing bloating. Oligosaccharides – Found in wheat, onions, and garlic. Disaccharides – Lactose-rich foods like milk and cheese. Monosaccharides – Excess fructose in apples, honey, and mangoes. And Polyols – Sugar alcohols hiding in chewing gum and stone fruits.
These short-chain carbohydrates are poorly absorbed in the small intestine, leading to gas, bloating, and digestive discomfort for people with sensitive stomach. For people with IBS (Irritable Bowel Syndrome) or gut sensitivities, limiting high FODMAP foods can make a significant difference in how they feel every day.
High vs. Low FODMAP Foods: What’s the Difference?
Knowing what to eat (and what to avoid) is key to maintaining a healthy gut. Here’s a breakdown:

High FODMAP Foods to Avoid
These foods can be tough on digestion, leading to bloating, gas, and discomfort. Keep an eye out!
❌ Vegetables: Onion, garlic, cauliflower, mushrooms, drumsticks ❌ Fruits: Apples, pears, mangoes, watermelon, chikoo (sapota) ❌ Dairy: Cow’s milk, paneer, curd (regular yogurt), soft cheeses ❌ Legumes & Grains: Whole wheat roti, maida (refined flour), rajma (kidney beans), chana (chickpeas), toor dal ❌ Sweeteners: Honey, jaggery (in excess), artificial sweeteners (sorbitol, xylitol) Swapping out high-FODMAP foods with low-FODMAP alternatives can make digestion easier and keep your tummy happy!
Low FODMAP Foods to Enjoy
These foods are gentle on your gut and help support healthy digestion:
✔️ Vegetables: Carrots, zucchini (tori), bell peppers, spinach (palak), bottle gourd (lauki) ✔️ Fruits: Bananas (firm/yellow), oranges, strawberries, kiwi, papaya ✔️ Dairy Alternatives: Almond milk, lactose-free yogurt, hard cheeses (cheddar, parmesan) ✔️ Grains & Protein: Oats, quinoa, rice (white & brown), eggs, fish, paneer (small portions), tofu ✔️ Sweeteners: Maple syrup, coconut sugar (in moderation), jaggery( in moderation)
Pro Tip: If you love fruit but struggle with bloating, swap apples for bananas and honey for maple syrup!
How FODMAPs Affect Your Gut Health
FODMAPs play a crucial role in digestion, but for some, they can cause significant discomfort. These short-chain carbohydrates pull extra water into the gut and ferment in the colon, leading to bloating, gas, and unpredictable digestion. If you often feel heavy, sluggish, or experience irregular bowel movements after meals, high-FODMAP foods might be the culprit.
A low-FODMAP diet is particularly beneficial for individuals with Irritable Bowel Syndrome (IBS), chronic bloating, or gut inflammation. By reducing high-FODMAP foods, many people experience relief from digestive distress, improved gut motility, and reduced abdominal discomfort. However, the goal is not to eliminate FODMAPs permanently. Instead, it’s about identifying your personal tolerance level through a phased approach—starting with elimination, followed by reintroduction, and then personalizing your diet.
Low FODMAP Diet for Better Digestion
A low FODMAP diet can help you identify the foods that trigger your symptoms and find what works best for your gut. Here’s how to get started:

1. Elimination Phase
· Remove all high-FODMAP foods from your diet.
· Focus on low-FODMAP options like rice, carrots, bananas, and eggs.
· This helps reset your gut and reduce symptoms like bloating and cramping.
2. Reintroduction Phase
· Gradually add back one high-FODMAP food at a time (e.g., onions, milk, or apples).
· Wait a few days before testing another food to see how your body reacts.
· Track your symptoms in a food journal to spot patterns.
3. Personalization Phase ✅
· Identify which foods you can tolerate and which trigger discomfort.
· Create a balanced diet with both high and low FODMAP foods that suit your digestion.
· Enjoy a gut-friendly lifestyle without unnecessary restrictions!
Pro Tip: The goal isn’t to avoid FODMAPs forever but to find your unique tolerance level and eat comfortably!
Take Control of Your Gut Health Today!
Making small changes in your diet can lead to big results! If you struggle with bloating or digestive issues, try switching to low-FODMAP foods and notice the difference. A well-balanced gut improves digestion, enhances energy levels, boosts mood, and supports overall well-being.
By making mindful food swaps and identifying your triggers, you can take control of your gut health without feeling restricted. Start with simple adjustments, like replacing high-FODMAP dairy with lactose-free alternatives, and choosing gut-friendly fruits like bananas and oranges over apples and mangoes.
Consistency is key! Staying hydrated, and managing stress through mindful eating can further enhance digestive comfort. If symptoms persist, consulting a nutritionist or dietitian can help you create a customised low-FODMAP plan tailored to your needs.
Your gut health plays a vital role in your daily life—nourish it well, and your body will thank you! Ready to take the first step? Start by making one small change today and experience the difference for yourself.
Your gut deserves to feel its best!
Disclaimer: The information provided in this blog is for educational purposes only and is not intended to replace medical advice. If you have digestive issues, food intolerances, or suspect Irritable Bowel Syndrome (IBS), consult a qualified healthcare professional or a registered dietitian before making dietary changes. The Low FODMAP diet should be followed under guidance, as long-term restrictions may lead to nutritional deficiencies. Always listen to your body and seek professional advice for personalized recommendations. For more information please reach supertums team at www.supertums.com
2 notes
·
View notes
Text
Fun new dietary/gastrointestinal mystery: am I actually allergic to oranges (ate a can of mandarin oranges to test), bizarrely allergic/intolerant of chocolate now (been eating a pan of brownies (and also other food)) for the last 3 days, or just coming down with food poisoning (damn it slightly undercooked brownie is delightful)
Edit: oh, I also ate almonds. I thought I'd ruled those out as an allergy but if it's the stupid fodmap intolerance shit, stacking potential allergen + a few fodmaps could do it. Urgh
#i hate dry brownies but i guess if/when i make my next batch i should bake the shit out of them & eat them w/o also eating oranges#and try oranges again in like a week or two w/o eating chocolate to see if the gastric pain repeats#owwwwwwwww
4 notes
·
View notes
Note
what foods do you recommend for constipation?
This is going to be unique to each individual, as the cause of constipation is going to vary from person to person. There’s not a “one size fits all”, approach, which is why it’s good to work with a doctor and specialist- if and when possible -to get care curated to your specific needs. Otherwise, you just gotta do your research and really monitor yourself and your symptoms.
If you don’t have any diagnosed digestive disorder, the first step would be to increase fiber (via fruits, vegetables and grains), cut down on fatty foods, sugars and diary, increase water consumption, and try walking/exercise.
If you have IBS or SIBO, these things might not work for you. You may be suggested to eat yogurt or other foods with probiotics to help balance and regulate the bacteria in your gut. You’ll also be asked to do a low FODMAP diet/restrictive diet/keep a food diary to see if certain foods cause the constipation. The diet you need to accommodate IBS or SIBO will be unique to the individual.
If you have food intolerances or food allergies that cause constipation, you’ll have to get tested for allergies and do a restrictive diet with a food diary as well. The diet you need to accommodate food intolerances/allergies will be unique to the individual.
You’ll also be asked about your BMs, if there’s any irregularities or cause for concern, you’ll be sent to a specialist who will give you a colonoscopy to make sure you don’t have something obstructing your bowels and causing constipation. Dietary changes, if needed, will be unique to the individual.
4 notes
·
View notes
Note
Do you mind if I ask what symptoms you had with the intestinal stuff? I have several food intolerances & I have been very careful but everything seems to bloat me up & im not sure if im just getting more sensitive or if its a symptom of an infection/something more serious I should look in to…
So I had H Pylori for nearly a year before Doctor #2 elected to do tests instead of discounting my symptoms as anxiety.
I pretty much stayed bloated/gassy at all times and within an hour of eating I’d get cramps that would then last for hours afterward. Also really bad heartburn. I was a 6/7 at all times on the Bristol stool chart. It was definitely worse when I had fodmaps but even on a no-fodmap diet I was constantly uncomfortable at best and in serious pain at worst.
I also had a bunch of dermatitis issues—my scalp was the worst spot, but also around my nose, eyelids, and corners of my mouth. Random little rashy spots that would pop up with no rhyme or reason, especially since I’m really careful about my skin/hair care routines. Since treatment, those have all gone away.
I really wish I’d pushed back on the first doctor a lot harder, because it’s wild how fast I started feeling better once they got me on a treatment plan, and I could have avoided 8+ months of misery. I’m still not back to normal— my stomach is more sensitive than it used to be– but I’m so much better than I was.
At the very least, go see a doc and get testing done to rule out the obvious things!
28 notes
·
View notes
Text
ah damn
so here's an example of the difficulties of two specialized diets at odds
I got a bean and rice burrito meal kit because I'm trying to keep kosher so I'm picking more vegetarian things; I can have the cheese on the burrito because there's no meat right
the other thing i'm doing is low-fodmap. I knew I had an issue with guacamole, I can have like 1/8 of an avocado for fodmaps. But I figured the little single serve cup would be okay.
you know what I didn't think about looking up until after I cooked it? the beans. meal kit gave me like half a can black beans and a whole can of pintos, for two burritos.
I can have about a 1/10 of a can of either for fodmaps, and they have the same fodmaps so I don't want to stack them.
After having eaten half a burrito (so we're at... like an ok amount of black beans probably but a like double-treble the safe amount of pintos) I am now scraping the filling off so I can finish off the cheese tortilla will some rice on
This is so pathetic ugh
and I was told by the doctor that whatever blood test they did says I'm not celiac so I didn't need to worry about wheat, but I'm looking up what fodmaps are in a tortilla or bread and it's the same fodmaps as beans and like. I am remembering that as a child I always ordered double-rice-no-beans at Mexican restaurants and so far there's been so many things in the the low fodmap diet that like. confirm my preferences and comfort foods. so like maybe I don't gotta worry about gluten specifically but maybe I do actually gotta limit my bread??
anyway keeping track of this shit is exhausting and if I had been having like a beef or chicken burrito I probably woulda had a lot less beans to worry about? Meat is rarely if ever an issue with fodmaps but it's super an issue with kosher and i'm just. so tired
pikuach nefesh I should eat what sustains me but I also feel like?? if it's possible to navigate this I should? that there should be a way
11 notes
·
View notes
Text
Finding Your Best IBS Treatment Plan
Irritable bowel syndrome (IBS) is a common digestive disorder estimated to affect 10-15% of the entire population. Symptoms like cramping, abdominal pain, bloating, constipation and diarrhea can range from mild to completely debilitating.
While no medical cure exists for IBS, the good news is that many effective IBS treatment options are available to significantly ease symptoms. It simply requires working with your doctor to discover the best personalized treatment plan.
Getting Properly Diagnosed
Since IBS is what’s known as a diagnosis of exclusion, the first step is to rule out the possibility of other inflammatory bowel diseases like Crohn’s or Celiac with specific testing. These may include:
Stool tests check for underlying infections or other gut issues
Blood tests look for markers of inflammation indicating disease
Colonoscopy visually examines the large intestine
Food sensitivity testing reveals if certain foods worsen symptoms
Once other conditions are ruled out, your doctor will make an official IBS diagnosis, the details of which will guide your treatment plan.
IBS Treatment Plans Depend on Type
There are four types of IBS, classified by what digestive symptoms are most prominent:
IBS with Constipation (IBS-C): Hard, infrequent stools IBS with Diarrhea (IBS-D): Frequent loose, watery stools.
IBS with Mixed Bowel Habits (IBS-M): Alternating constipation and diarrhea IBS Unspecified: Insufficient abnormality of stool consistency
Identifying your IBS type allows your doctor to select suitable therapies.
Lifestyle Treatments for IBS Relief
Certain at-home care strategies may significantly control IBS flare-ups including:
IBS Diet - Limiting intake of high FODMAP foods like dairy, beans, wheat, onions, cabbage, and artificial sweeteners can ease stool issues in 75% of IBS patients.
Stress Reduction - Stress dramatically exacerbates IBS problems, so relaxation techniques like meditation, yoga, massage are key.
More Exercise – Moderate activity at least 30 minutes daily calms the nervous system tied to digestive function.
Probiotics - These healthy gut bacteria in supplement form have been shown in studies to reduce bloating and pain.
Peppermint Oil - Shown to reduce spasms and cramping pain. Use enteric-coated capsules.
Prescription IBS Medications
If lifestyle adjustments aren’t providing enough relief, many traditional and newer medications can be very effective, including:
Antispasmodics – Helps relax intestinal muscles to reduce painful cramping and spasms
Antidiarrheals – Slows motility and stool frequency for IBS-D
Laxatives – Helps alleviate constipation with IBS-C
Low-dose Antidepressants – Alters pain signaling pathways between the brain and digestive system
Newer Agents - Prescription medications acting on neurotransmitters recently approved specifically for IBS-C and IBS-D.
Last Resort: FMT for IBS
For patients failing standard IBS treatment, research shows great promise for fecal microbiota transplantation (FMT).
This involves transplanting healthy donor stool containing balanced communities of gut bacteria into the patient’s colon via scope or enema.
Results demonstrating FMT eliminates IBS symptoms in many patients suggests disruptions to the gut microbiome play a key role in IBS development.
Finding Your Optimal Treatment Combination
Since IBS is multifactorial in cause, most experts recommend utilizing a combination approach tailored to your specific symptoms patterns.
This can mean exploring herbal supplements like peppermint capsules or artichoke leaf extract while also prioritizing daily stress-reduction practices and a modified FODMAP diet under the guidance of a registered dietician.
Your doctor may also suggest rotating various categories of medications every few months to achieve lasting relief without building tolerance.
Be patient and keep your physician informed of how you’re responding to each new IBS treatment addition or modification. It often requires tweaking strategies over several months before discovering your unique formula for success.
Hope for Life Without IBS Misery
If you feel like you’ve tried everything for your difficult-to-treat IBS with little success, don’t lose hope. The treatments options area is rapidly evolving!
Whether its emerging micobiome research showing fantastic success with FMT for stubborn IBS cases or newly approved medications targeting specific IBS symptom pathways, effective tools for relief are available.
Stay focused finding the right gastroenterologist who will personalize a therapy plan that finally quiet your symptoms for good. With a thoughtful multi-pronged approach, you can get your life back and start feeling like yourself again!
2 notes
·
View notes
Text
FODMAP diet sounds like hell i'm sorry. the list of what you "can't eat" is just too long???
i swear getting tested for mold poisoning should be a mandatory thing BEFORE anyone gets diagnosed with any illness that has overlapping symptoms
2 notes
·
View notes