#Pulmonary Diseases
Explore tagged Tumblr posts
Text
Less than three months after U.S. Senator Tammy Baldwin and her colleagues launched an investigation into the four major American manufacturers of inhalers, three of the companies have relented, making commitments to cap costs for their inhalers at $35 for patients who now pay much more.
25 million Americans have asthma and 16 million Americans have chronic obstructive pulmonary disease (COPD), meaning over 40 million Americans rely on inhalers to breathe.
Inhalers have been available since the 1950s, and most of the drugs they use have been on the market for more than 25 years.
According to a statement from the Wisconsin Senator’s office, inhaler manufacturers sell the exact same products at a much lower costs in other countries. One of AstraZeneca’s inhalers, Breztri Aerosphere, costs $645 in the U.S.—but just $49 in the UK. Inhalers made by Boehringer Ingelheim, GlaxoSmithKline, and Teva have similar disparities.
Baldwin and her Democratic colleagues—New Mexico Sen. Ben Ray Luján, Massachusetts Sen. Ed Markey, and Vermont Sen. Bernie Sanders—pressured the companies to lower their prices by writing letters to GSK, Boehringer Ingelheim, Teva, and AstraZeneca requesting a variety of documents that show why such higher prices are charged in America compared to Europe.
As a ranking member of the Senate Committee on Health, Education, Labor, and Pensions, Baldwin recently announced that as a result of the letters they had secured commitments from three of the four to lower the out-of-pocket costs of inhalers to a fixed $35.00 rate.
“For the millions of Americans who rely on inhalers to breathe, this news is a major step in the right direction as we work to lower costs and hold big drug companies accountable,” said Senator Baldwin.
A full list of the inhalers and associated drugs can be viewed here.
It’s the second time in the last year that pharmaceutical companies were forced to provide reasonable prices—after the cost of insulin was similarly capped successfully at $35 per month thanks to Congressional actions led by the White House.
-via Good News Network, March 25, 2024
#united states#us politics#us senate#tammy baldwin#bernie sanders#big pharma#health care#us healthcare#inhaler#asthma#pulmonary disease#healthcare access#affordability#disability#good news#hope
4K notes
·
View notes
Text
Clinical Images and Case Reports Journal
About Journal
Clinical Images and Case Reports Journal (CICRJ) is a peer-reviewed indexed medical journal established Internationally which provides a platform to publish Clinical Images, Medical Case Reports, Clinical Case Reports, Case Series (series of 2 to 6 cases), Research and Clinical Videos in Medicine. Clinical image journal is a indexed journal accepting clinical images submission, journal of clinical images, journals publishing clinical images in medicine, clinical imaging submission journal and medical illustrations etc. Journal of clinical case reports publishes case reports in clinical medicine, clinical reports, journals accepting clinical case reports submission and journal of clinical cases. Journal of medical case reports publishing medical case reports, journals accepting medical case reports submission etc.
#Respiratory Medicine#Pulmonary Diseases#Clinical Oncology#Endocrinology & Diabetology#Dentistry & Oral Medicine#ENT / Otolaryngology#Surgery & Clinical Practice#Pediatrics & Geriatrics#Orthopedics & Rheumatology#Ophthalmology#Pandemics & Epidemics#Cancer & Tumor Study#Neurology & Neuroscience#Nephrology & Renal Diseases#Microbiology & Biotechnology#Hematology & Blood Research#Genetics & Molecular Biology#Gastroenterology & Hepatology#Pharmaceutics & Drug Delivery#Dermatology & Skin Care#Cardiology & Heart Diseases#Andrology#Obstetrics & Gynecology#Anesthesiology & Pain Relief#Infectious Diseases#Pathology- Anatomic & Clinical#Physical Medicine & Rehabilitation#Physiotherapy#Allergy & Immunology#Sleep Disorders & Sleep Studies
0 notes
Text
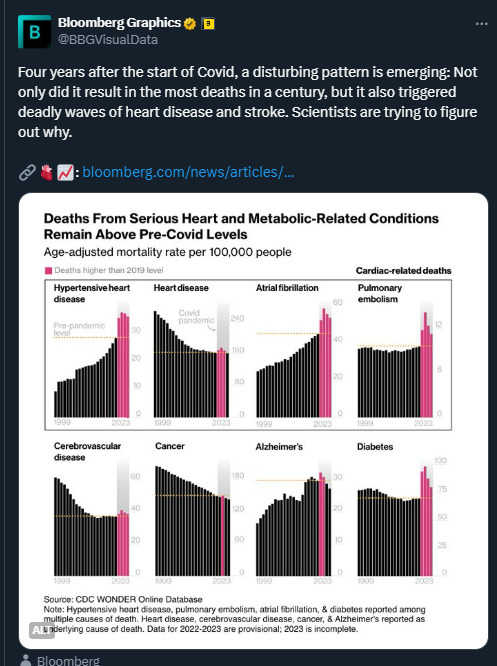
Statistics don't lie It just blows my mind that people can't see or understand that COVID is a dangerous virus that can damage your body. Getting infected multiple times will have serious consequences for many.
#covid#sars cov 2#long covid#heart issues#heart damage#diabetes#cancer#alzheimers#pulmonary embolism#atrial fibrillation#cardiovascular disease#hypertensive heart disease
252 notes
·
View notes
Text
Went to my second PFT test and the lady was like,
“Have you ever had a CT scan???”
Me: “No… just a bunch of X-Rays. Never find anything on it, but I’m still hacking up a storm so they just throw more prednisone at me.”
Doctor: “…You should think about getting by a CT scan. Because this isn’t making SENSE.”
Sister: “THAT’S WHAT WE’VE BEEN SAYING.”
Doctor: “…Welp. I’mma make some notes. Here’s another bottled water and while I shouldn’t give you a couple puffs of Albuterol because your numbers aren’t low enough you’re kinda dying so I’m gonna make ANOTHER note and give it to you anyway. We’re also gonna rerun the first test again after the Albuterol just to see how much it opened your lungs up so your specialist can compare the numbers.”
Me: “…I’m gonna HATE the number three after today.”
Doctor: “Hehe. They all do.”
Anyways. I crashed after getting home. Still kinda nauseous but eyyyy was finally able to use my inhalers and nebulize. Woooooooo.
Now I just gotta convince the doc to actually schedule a CT scan during my next appointment in the next few days… assuming I can actually get to it. ☠️
#anyways she’s also tossed a pulmonary rehab brochure at me since I can’t do basic stuff around the house without DYING so that’s gonna be#something to look at#brochure? pamphlet. booklet. I dunno#she’s convinced I got some kind of interstitial lung disease because I’m ‘too young’ to not be able to do basic work and my chronic cough#just. does not make sense. fun fun#hearing my sister tell the doc about how I always look like a ghost on bad days where I cant breathe have me like-#me: so on a scale of one to Danny Phantom how ghost do I look today#my sister: I’d say you’re about an eight right now#ramblings
7 notes
·
View notes
Text
i love making fucked up diseases and illnesses for my ocs to bear based on my wikipedia binges
#i also like exploring what lifelong complications they have#so far we got a prion disease x rabies hybrid#and pulmonary fibrosis from burned lung tissue#its all a wip but i can loredrop if anyone is curious#yote yaps
5 notes
·
View notes
Text
youtube

#j hubbell#jthemthey#trans#transgender#nonbinary#witch#wizard#video#pipe#pipe smoker#you shouldn't inhale anything heated into your lungs unless you want Chronic obstructive pulmonary disease#scrolls#gay#queer#gender#high heels#witch hat#thank you#whatever#Youtube
5 notes
·
View notes
Note
could you pls make a pvfmd flag for my friend? ty in advance!
Hello I don't take requests for pride flags currently. Sometimes I still do some when the flag asked is related to an hyperfixation and the like, so feel free ask whenever you wan to just in case. /serious
#PVFMD#paradoxical vocal fold motion disorder#physical disability#asthma#pulmonary disease#dyspnea#disability pride
3 notes
·
View notes
Text
Unga bunga saw a new condition this morning and I'm giddy to flesh out my knowledge w medical journals for fun heehee
#Creepy chatter#Hemosiderosis :3#Technically it's idiopathic pulmonary hemosiderosis but I'm starting base level and then going into spec manifestations#Still riding the high of my one and only ever case of diabetic myonecrosis#So unusual that there wasn't anything really in place to capture it#I BREAK the International Classification of Diseases 10th clinical modification#I FIND the myonecrosis I SLAP the guidelines around bc they didn't consider diabetic manifestations#The cool thing was the patient was THRIVING! :D what a kick ass doctor to whip that shit into nearly sub-clinical levels#Medical cw
3 notes
·
View notes
Photo
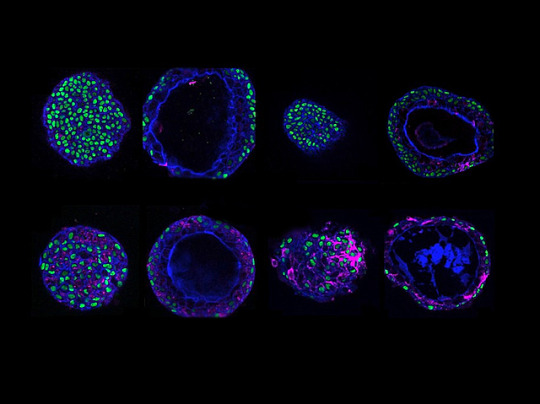
COPD meets COVID
Persistent wheezing, coughing and breathlessness. These are all symptoms of chronic obstructive pulmonary disease (COPD). Add a lung infection on top of COPD and these symptoms worsen. To better investigate how COPD affects lung infection at an individual level, researchers created organoids – lab-grown tissues that mimic organs – using tissue samples collected from the airways (bronchi) and nasopharyngeal areas of healthy and COPD patients. Fluorescence microscopy of nasopharyngeal (pictured, left) and bronchial (right) organoids from healthy (top) and COPD (bottom) individuals revealed more goblet cells (magenta) in COPD organoids – this mimics what's seen in COPD patients. SARS-CoV-2 infection of COPD organoids showed that viruses replicated more in bronchial than in nasopharyngeal organoids. This is also in line with real-life disease, where the bronchi are the main site of infection in severe COVID-19 cases. This lab-grown system may therefore prove useful in modelling lung disease and infection in individual cases.
Written by Lux Fatimathas
Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore and Programme in Emerging Infectious Diseases, Duke-NUS Medical School, Singapore, Singapore
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in Nature Communications, December 2022
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#covid19#covid#copd#chronic obstructive pulmonary disease (copd)#organoids#immunofluorescence#sars-cov-2
8 notes
·
View notes
Text
A Miracle for World PH Day 2023
TRIGGER Warning: Mention of Miscarriage in this post and unflattering photos of myself.
in December of 2019, I noticed a significant difference in my health. Shortness of Breath, even when walking a short distance, heart palpitations, cough & wheezing, chest pain and occasional nose bleeds. Untreated Anxiety and Depression associated with my Bipolar Disorder, Uncontrolled Diabetes and Intermittent Asthma were believed to be the cause of these symptoms despite my growing concerns. Each year my symptoms worsened. In February 2022, it had gotten so bad that I could not walk from my bedroom to my kitchen without feeling like I had just ran a marathon. My pulmonologist agreed that my condition was rapidly worsening and begged me to give a CPAP another try. I was also switched to the highest dosage of Advair and regular use of my emergency inhaler. My PCP told me to get my A1C down and consider weight loss surgery to expedite my weight loss journey. I was determined to do everything they advised, this way I could prove to them that something more serious was occurring. At this time, I had already quit smoking and began lowering my A1C.
To my surprise, June 30, 2022 it was confirmed that I was pregnant. It shocked me because a couple years ago in 2020 I suffered a miscarriage at 16 weeks. I was advised to consider birth control because my body could not hold a fetus. Well... they were wrong about that one! The doctor confirmed a healthy fetus made it’s way and there was a heartbeat. It was a miracle and I knew God had other plans for me. I prayed every day and every night, thanking my heavenly Father and thy Earthly Mother for all the blessings they bestowed upon me; also asking for guidance, clarity and strength to lead me in the right direction.
I began to communicate with my Perinatologist more as I learned to trust her. During an appointment in September 2022, I opened up and told her,
Doctor, something is wrong with me and I need someone to listen to me. I can’t do my seated exercise anymore and that concerns me. I can’t even walk in place but for 4 minutes, then I have to stop and lay down. I think something is wrong with my heart. I’ve been having these issues before I was pregnant. Please help me. I want to live.
She asked me had I seen a cardiologist. I explained to her that after an urgent care visit in May I was put on a heart monitor for a few weeks but no results were communicated to me. She fought to get my referral to a cardiology approved. My visit with the cardiologist in October is when I was told, I have Pulmonary Hypertension. An ultrasound of my heart confirmed that I had heart disease and heart failure.
My breath was too short for a sigh of relief. The weight on my chest applied pressure instead of being lifted. I was in my third trimester of pregnancy, when a right heart catheterization confirmed my diagnosis in November 2022. Then, the cardiology team with my healthcare provider advised for my care to be transferred to out-of-network team that can provide the care that I needed. I had gained over 40lbs in fluid due to heart failure and my new health team was confident that we could reverse it before labor.
My mother was in fear that she would lose her only daughter. I was in fear that I would never get to hold my daughter. My love was afraid that he would lose me and be alone. My father was scared and speechless. Everything made sense in these moments and everything mattered. It mattered who was there and who wasn't. It mattered where I was and where I was going. It mattered how and why.
3 weeks away from my due date, a team of 20+ assembled in the cardiac care unit to bring Zenobia in to the world. My father waited at home by the phone, my mother waited alone in the labor & delivery room and my love was by my side as they tilted me back and began to operate. After 4 hours of pre-op and 45 minutes of surgery, it was a success. My daughter was born, healthy and strong. Doctors, Nurses and many people stopped by to visit me when I left ICU, curious to meet the miracle baby and her parents. A nurse who was not in my station came to visit and said,
"I hope you don't mind that I came to visit. Although I'm not your nurse, I was on call when the entire floor heard that you were being transferred to the cardiac operating room. Every nurse gathered and we prayed for you. Everyone is celebrating you, a miracle."
My eyes filled with tears and joy. Other doctors and their students came to visit and were glad to see me. Another nurse encouraged me to tell my story and document my journey because it will inspire others. The doctors that worked directly with my care and surgery were impressed, proud and says that I'm their model story.


That was almost 4 months ago in January 2023 but also when my journey began. My team was honest with me, that labor and delivery was the least of their concern. Surviving postpartum, preparing for cardiac therapy and rehabilitation was top priority. I would be lying if I said it is easy. Most days I am sad. Learning to adjust to my new way of life has been challenging and difficult to accept. I promised myself to do all that I can to live, to change and to never give up. Meeting people who have PH and joining the association has been a great help to me and how I learned of World Pulmonary Hypertension Day on May 5, 2023.

One thing I have learned since giving birth with Pulmonary Hypertension is how much time and creating memories mean to me. Also, how important it is to talk about how you’re feeling no matter how that looks for you or how it makes anyone else feel. It’s easy to look down and frown when you’re faced with this challenge. Make the conscious decision today, right now to look up and forward. Be good to yourself and your body. When you need to rest, do so and don’t feel bad for not being able to push through on bad days. You’re a survivor, a PHighter.
I have so much to look forward to. Raising my daughter, therapies and rehabilitation and none of it will be easy but I give praise to the Most High for this blessing. Thank you Lord for blessing every hand that was laid upon me. Thank you for hearing my prayers. Thank you for every person who prayed for me. Thank you for those who have been there and rooting for me. Thank you for giving me the strength and bravery to share what you have done for me and what you will continue to do. Thank you to everyone following me, befriending me and joining me. I got you. Let’s live, let’s fight for a cure.

#worldphday#worldphday2023#pulmonary hypertension#pulmonary#pulmonology#cardiology#heart disease#lung disease#pregnancy#women health
3 notes
·
View notes
Text
https://www.literaturepublishers.org/
Clinical Images and Case Reports Journal
Submit Manuscript or email at
#Respiratory Medicine#Pulmonary Diseases#Clinical Oncology#Endocrinology & Diabetology#Dentistry & Oral Medicine#ENT / Otolaryngology#Surgery & Clinical Practice#Pediatrics & Geriatrics#Orthopedics & Rheumatology#Ophthalmology#Pandemics & Epidemics#Cancer & Tumor Study#Neurology & Neuroscience#Nephrology & Renal Diseases#Microbiology & Biotechnology#Hematology & Blood Research#Genetics & Molecular Biology#Gastroenterology & Hepatology#Pharmaceutics & Drug Delivery#Dermatology & Skin Care#Cardiology & Heart Diseases#Andrology#Obstetrics & Gynecology#Anesthesiology & Pain Relief#Infectious Diseases#Pathology- Anatomic & Clinical#Physical Medicine & Rehabilitation#Physiotherapy#Allergy & Immunology#Sleep Disorders & Sleep Studies
0 notes
Text
today's vetted campaigns. please continue to donate if you have the means and share as widely as you can regardless. the individuals on here go through so much every day just to communicate their stories to us - let's uphold that trust by showing them as much support as we can.
july 15th:
Hadeel Mikki (pregnant and needs perinatal care), her husband Waseem, their two young daughters, and Hadeel's mother and two brothers (they are the only survivors of her family) (€5,091/€35,000) - @hadeelmekki, verified by @/90-ghost
Aspiring doctor Malak Dader, her six siblings (they've already lost her teenage brother, and two of her younger brothers need medical treatment), and her parents (one injured, one sick with hepatitis) (€110/€25,000) - @malakabed, verified by @/90-ghost
Mohammed Al-Habil (needs urgent surgery after being shot in the leg), his five siblings (one of whom is immune-compromised and has congenital heart disease), their mother, and his widowed sister-in-law ($5,713 CAD/$70,000 CAD) - @mohammedalhabil2000, verified by @/90-ghost
Hanaa Jad Al-Haq, her husband Muhammad Hammad, and their little son Yousef (£2,675/£20,000) - @henomohammed, @hanaajad123, #246 on @/nabulsi and @/el-shab-hussein's spreadsheet
Salam, her husband Mohammad, and their two little children (€17,365/€40,000) - @save-salam-family, verified by @/90-ghost
Aya Maher, her three younger siblings (two under 18), and their mother (€4,920/€25,000) - @ayamaher444, #216 on @/el-shab-hussein and @/nabulsi's spreadsheet
The AlBalawi family of ten, including several children and two chronically ill members who need treatment (€24,200/€50,000) - @bisanalbalawi18, @elbalawi, @yasminalbalawiigaza, verified by @/90-ghost
The Ayyad family of eight, four of whom are children ($24,842/$35,000) - @aymanayyad82, @mayadayyad81, @aymanayyad1, verified by @/nabulsi
Munna Tashmali and her five children (this is the third time they've lost their home) (£3,269/£30,000) - @monashamali, verified by @/nabulsi
Maha Ibrahim, her husband Ahmed Al-Habil, and their two young children, one who is immune-compromised, and the children's sick grandfather (kr34,626 NOK/kr1,067,200 NOK) - @mahaibrahim12, @ahmedkhabil, #79 on butterfly effect project's spreadsheet
Ahmed Baalousha, his wife Islam, their three children (one a newborn), and Ahmed's parents and sister (€15,802/€50,000) - @5735765, @mahmoudbalousha4, #124 on @/nabulsi and @/el-shab-hussein's spreadsheet
Mohammed Al Manasra (needs treatment for chronic respiratory illness and a leg injury), his wife (also sick, needs chemotherapy), their three little children, and their cat (the family has already lost many extended members) (€26,790/€40,000) - @save-mohamed-family, #192 on @/el-shab-hussein and @/nabulsi's spreadsheet
Hanaa Al-Lulu (needs treatment for a painful foot growth) and her family (€2,628/€40,000) - @enghanalulu, verified by @/90-ghost
Mohammed Hijazi and his elderly parents, including his severely injured father (€2,106/€20,000) - @savemohammedfamily, verified by @/90-ghost
Maysaa Balousha (suffers from pulmonary fibrosis and is deteriorating without treatment), her husband Muhammad, and their four children ($118/$60,000) - @tamer200333, extended family of Mahmoud Balousha (#124 on @/el-shab-hussein and @/nabulsi's spreadsheet)
Mahmoud Saleh and his family (they've already lost several members, including Mahmoud's father and niece) (€5,265/€20,000) - @mide404, verified by @/nabulsi
Helping Siraj Abudayeh, his wife, and their three young children rebuild their destroyed home ($6,449 CAD/$82,000 CAD) - @siraj2024, #219 on @/nabulsi and @/el-shab-hussein's spreadsheet
Eman, Ahmad, and their two little children (€1,653/€15,000) - @zain-leen1993, @leen-gaza, verified by @/90-ghost
not yet vetted:
Mohammad Taysir, his wife Basma, and their two little children (€0/€50,000) - @yazanfamily
Mahmoud Alkhaldi and his family of five, including his little nephew ($235/$50,000) - @mahmoudalkhaldi
Shimaa, her little daughter Juri, and several members of her husbands family (€331/€50,000) - @shimaashaban22
your help, even if it seems insignificant to you, can bring life and hope to so many people. now is not the time to give in to despair or allow apathy to stifle our actions. here is something you can do. don't pass it by.
28K notes
·
View notes
Text
Lynette Chambers - phaware® interview 494
Lynette Chambers, a 9-year PAH (pulmonary arterial hypertension) patient, has also been diagnosed with pulmonary fibrosis (PF). She shares her journey, from struggling with daily activities to being admitted to the hospital with severely low oxygen levels. Lynette discusses the emotional challenges of facing a terminal illness and the difficulty of balancing work and family time. Despite the hard reality, Lynette emphasizes the importance of gratitude, making others feel better, and being the best version of oneself. She finds strength in her family, especially her grandchildren, and strives to create lasting memories and make a positive impact on those around her.
My name is Lynette Chambers. I’ve been diagnosed for nine years now. I was in the hospital with congestive heart failure and they did a whole bunch of tests and decided that I had PAH. So, I’ve been going through a journey with congestive heart failure and PAH. Now, nine years later, I’ve been diagnosed with pulmonary fibrosis. I was at work, I was running a swimming pool company. I was running around getting stock and dealing with clients and stuff, and I was finding that I was really short of breath. After I was done talking to a person, it was like, I can’t get a full breath. For me, it was really scary because I thought there’s something wrong that I can’t breathe. Then, I went home, I could breathe fine. I drove home. Then, I got out of the car and went to walk up to the house. I couldn’t walk all the way up our sidewalk, which is like maybe 10 feet from the car to the house. I would have to stop, take a breath, go up our four stairs, stop, take a breath, and then go in the house and sit on the couch and try and recuperate. As the days went on, it just got harder and harder and became a lot more evident that I can’t lift stock, I can’t run from one end of the store to the other. I would recuperate on the drive home. Once I got there, I couldn’t make it into the house. It wasn’t a fluid motion. I went, okay, there’s something really wrong. I’ve always been active. I’d always taken my kids camping, done all kinds of things, water-skiing, downhill skiing. I couldn’t do any of that. I was just so fatigued the whole time. So, I went, no, there’s something going on here. I had a shower and I couldn’t get out of the shower. I had to sit on the edge of the tub. Then I got to where I felt a little bit better and I decided, no, I better go in. I went into the hospital. My oxygen level was at 48% and my heart rate was 174 over 94. So they went, “Okay, you’re admitted and that’s where you’re staying.” I was admitted into St. Boniface Hospital for two and a half weeks, while they tried to figure out what was going on. That’s when they did all the tests. At first they said, “No, it’s just congestive heart failure.” Then, they went, “But your oxygen went to 48. So that tells us there’s something in the lungs.” So they started doing more tests, like echocardiogram, all of that. Then, they went, “Okay, this definitely PH,” and that’s where it stayed. I’ve had my cardiologist put me in touch with another doctor who deals with my PAH, and then I have a cardiologist that deals with my heart. Then, I have a respirologist who now diagnosed me with PF after doing a CAT scan. I was in the hospital in and out from December to March five times with what they thought was pneumonia. My respirologist went, “Nobody gets pneumonia five times in a row.” I would go from one med to another. She said, “No, I want a CAT scan of the heart and lungs today.” I got a CAT scan and she phoned me at work and said, “Are you sitting down?” I said, “No, but I’ll take you and I to a boardroom.” So we went to the boardroom and she said, “You have PF.” I said, “Okay, what’s PF?” She said, “It’s pulmonary fibrosis, which is a scarring of the lung tissue, making it harder to breathe and suffocating the lung on its way up.” I said, “Okay, what are we doing?” She said, “Well, I’m not sure yet, because it is terminal. So whatever we do, I want you to understand you’re not going to get better.” I said, “Okay, well, we knew that with PAH.” She said, “No, this one’s different and you’re just going to find it harder and harder to breathe.” So we’re now in the testing process of finding out what meds will work for both or where we’re going to go from here, what tomorrow will look like. When I first was diagnosed with PAH, I thought, “Okay, this is it. I’m done.” But then, I started reading and reading and reading. I heard more stories about people lasting 20, 30 years. That was great. But then when I was told I have PF, and I started looking into that and I asked, “What does that look like?” Because when I was first diagnosed with PAH, my doctor said, “You’re going to be dead in two to five years.” It was left at that. There was no empathy, there was nothing. It was more of a, just so you know. Then, when I got the PF and I started looking, I didn’t find anybody that had had the disease more than seven years. So, then I started in my head going, okay, I have two grandchildren. One turned three and one is six. I’m not going to see them graduate. I’m not going to see them grow up. It’s a reality check and it’s hard, because you want to think, well, I can keep working because I have that energy and I love my job. So you want to keep doing that. But then in the back of your head is how much quality time am I missing with my family by being at work? So it’s a, could I afford to just not work? So there’s this whole piece emotionally where you’re going, what am I missing by doing this? Or what will I miss if I don’t do this? Amazon and I are best friends and I order everything I can, so my grandchildren have everything. Part of that is because I want them to remember me. I want them to know that Ama loves them, and I may not be there in person, but I will always be there. So, yeah, there’s that emotional thing that you do go through. I think when you’re being given a diagnosis of a terminal illness, there’s always that human component of this is your reality. This is where you are at. I have a husband that I love more than anything. I’m not going to get to grow old with him. We think when we get married that that’s why we marry is we’re going to grow old with our best friend and I won’t. It’s a challenge to get up every morning and know today may be your last day. You try not to think that way, and you try and be positive, because I believe positivity creates everything, but it’s really tough to put yourself back in there. I do believe that we’re all born and made for a reason and you do what you can do. I’ve been very blessed through my life. I’ve been a foster parent of 30 kids since I was 19. I have my own biological children and I’ve adopted children, so I’ve been very, very blessed in the life that I have. But it’s still hard to think that it’s going to end and I can’t do more and be more. For me, I need to be more to everyone and do whatever I can. If I can make somebody smile, I will. If I can help out in any way, shape or form, that’s who I am. This disease makes it harder to know that you’re not going to be there to make those changes. You can’t make a difference the way you’re used to. I have learned, and I’m very blessed to have learned this. One of the ladies I worked with said to me, we were talking about gratitude, and she said, “Take 15 minutes a day and write down five things that you’re grateful for. Read that at night before you go to bed. The next day you get up, have your day, take your 15 minutes and write down five things you’re grateful for.” Do you know I’ve been doing that for almost eight months? Not once have I written the same thing twice. You look back at that and you go, wow, look at all of this that I’m grateful for. That makes you go through the next step and go to the next day and see what five things you come up with at the end of that day. My family is my strength. I look at my grandchildren. If you watch the innocence in a child, it’s so amazing. I watch my grandchildren and I listen to them. It makes you want to be better. They make you want to do more, because it’s just so incredible how they look at things. People are arguing and fighting outside, and my granddaughter’s picking flowers. I said, “What are you picking flowers for?” She said, “Maybe they’ll be happy.” She wanted to take these two people flowers. She’s six years old. All she sees is two people who need something. That makes you want to be better. That makes you want to do more, realizing that the smallest token is the largest gift that you can give someone. The most important takeaway for all of us in life is be the best that you can be. Be true to you, but be the best that you can be. If you can say to someone who looks like they’re having a hard day, “I really like that blouse. That’s nice.” They smile and they feel better about themselves. It’s a two-second thing. It doesn’t mean anything to you, but it sure does to the person on the receiving end. I think that that’s the biggest thing for me is you need to try and make everybody feel better. It makes you feel better inside, knowing that you’ve made someone smile. You’ve given someone something to take from their day. If it’s part of their gratitude post, great. If not, better luck next time. My name is Lynette Chambers, and I’m aware that I’m rare. Learn more about pulmonary hypertension trials at www.phaware.global/clinicaltrials. Engage for a cure: www.phaware.global/donate #phaware Share your story: [email protected] Like, Subscribe and Follow us: www.phawarepodcast.com. @phacanada
Listen and View more on the official phaware™ podcast site
0 notes
Text
youtube
#COPD#prognostic models#serum biomarkers#acute exacerbations#chronic obstructive pulmonary disease#AECOPD#predictive modeling#respiratory health#pulmonary disease#patient outcomes#risk assessment#chronic disease management#respiratory therapy#biomarker analysis#precision medicine#healthcare innovation#clinical research#disease progression#inflammation markers#treatment strategies#Youtube
0 notes
Text
Lynda Obst: A Pioneering Producer and Advocate for Women in Hollywood
Lynda Obst: A Trailblazer in Hollywood Lynda Obst, a dynamic New York journalist who made her mark as a Hollywood producer, passed away on Tuesday at her Los Angeles home at the age of 74. Her brother, Rick Rosen, confirmed that the cause of death was chronic obstructive pulmonary disease. Renowned for her distinctive booming laugh and her unapologetic honesty, Ms. Obst was a vibrant personality…
#chronic obstructive pulmonary disease#Contact#female creators#film industry#Hollywood producer#Interstellar#Lynda Obst#Nora Ephron#Sleepless in Seattle#women&039;s advocacy
0 notes