#Premarin Tablet
Explore tagged Tumblr posts
Text
Premarin Tablet - Conjugated Estrogens (0.625mg) Pfizer Ltd - Pilcare - Exporter from India
Premarin Tablet is a female sex hormone (estrogen). It is a part of female hormone replacement therapy which helps in treating estrogen deficiency symptoms like hot flushes (red and warm face) and vaginal dryness.

#Premarin Tablet#Premarin Tablet Exporter from India#Premarin Tablet Pharmaceutical Medicine exporter in India
0 notes
Note
https://at.tumblr.com/ruthbaeddelginsburg/698643025153458176/1ff6rweijvln Isn’t this kinda terfy :/ they only know they were male by looking at DNA (Xy chromosomes present) and/or body structure like pelvis shape being narrow
Wait. are you calling me a terf? My friend who reblogged that post from me? The people who classify bog bodies? Unclear.
As for me, I literally just scrolled through a Wikipedia article and noticed a trend and decided it would be funny to joke about how we need more women bog bodies
Like. What the fuck are you even doing? What is your goal here? If you think I'm a terf (I'm a trans woman btw) then what do you gain by bringing this to me? A terf would just be like "lol yup" or something to that effect. If you think that I'm being "terfy" by implicitly accepting the gender categorizations of bog bodies by the people who research them then uhhh that's not what a terf is
Also! Bog bodies often have lots of remaining flesh! Like, look up the Tollund man. He's got a face still. It's been a bit since he shaved. Is it possible that's a trans woman? Sure I guess. But they had proto-Premarin around the time the Tollund Man died, so idk. Maybe there'd be titties. They definitely had shaving, and the Tollund Man had access to shaving equipment, but he hadn't in a little while. If I were a trans woman in 300ish CE I'd shave. Now, he was definitely in a pickle--probably being ritually executed--so maybe he (or she?) totally would have shaved more recently given the chance.
But we don't know that, and adding caveats about it would have spoiled my joke. Not only that but it would not make the world any safer or better for me and all the other trans women. And neither does your message.
Like. You or I could not know what signals, if any, would survive on even the most well preserved bog body of a trans woman that could indicate her gender. Maybe his leather cap is a very girly leather cap by iron age Danish standards. Maybe it's the manliest cap ever. We don't fucking know.
And anon, I want to live in the world where I can make a goddamn joke implying that we need more women bog bodies Because Feminism without someone like you cropping up to spoil it
I want you to think about what world you are creating by sending messages like this. You are the one harassing trans women, the time-honored tradition of terfs everywhere
Perhaps they should take more care in applying gender descriptions to bog bodies--that's an opinion you can have--but take that up with archeologists, not me
All you're achieving here is pissing off a trans woman who made a joke that actually, if you think about it for 10 seconds, includes the baked-in assumption that I and other trans women would be gendered correctly by future archeologists if we became bog bodies
In fact my joke works just as well in a world where all bog bodies are gendered correctly (assuming there still isn't gender parity)
So you're not even slightly right! You're just shit-stirring, I guess, trying to get a rise out of me? I've written several paragraphs here, are you satisfied, anon?
Is this what you wanted to achieve?
Who are you and what are you building?
Think about it
Think about it while walking into an acidic wetland to your doom. I want the next bog body to be you, specifically. Pack a bag of typical supplies for this time period and maybe a clay tablet or something, with some text written in multiple languages. Just to help out, you know?
If researchers in 1000 years misgender your preserved corpse you can bitch about it to me then and I'll listen
4 notes
·
View notes
Text
Why is there a shortage of HRT medicines in the UK?

What are HRT medicines?
Much has been reported about the shortage of HRT medicines in recent years. So, what are HRT and why is this shortage significant? HRT are medicines that help treat the symptoms of menopause . HRT is an abbreviation for Hormone Replacement Therapy. During menopause there is a decrease in hormone levels, HRT medications increase these levels so that the symptoms of menopause are reduced.
What are the symptoms of menopause?
These can vary person to person but the most common symptoms are irregular periods, vaginal dryness, hot flushes, mood changes, and sleep problems. Some women find menopause so debilitating that they find it difficult to work and in extreme cases can lead to severe mental health issues. Due to the varying and difficult nature of the symptoms, menopause can often result in strained relationships between the sufferer and their friends and family.
So, what is driving the HRT shortage?
There are multiple reasons for why there is a shortage of HRT medications.
· Increased demand in HRT medication. Prescriptions for HRT medicines have increased significantly over the last few years. Despite the treatments being available for decades, much more awareness around the condition and how it can be treated has resulted in many more patients approaching their doctor for treatment. The industry has had difficulty keeping pace with this rapid uptake of HRT. medication
· Supply chain issues.
Pharmaceutical manufacturers work in a global marketplace and supply chain issues can cause significant disruption to HRT availability. This was initially exacerbated by the Covid 19 pandemic. Multiple reasons, from factories having to reduce production, to difficulties in sourcing the active ingredient resulted in medicine shortages across the globe. Manufacturers are now playing catch up and are trying to boost production to match supply.
What medicines are being affected?
Every medicine in the HRT is being affected by availability issues. The below is a list of medications that have had issues with supply over the last 24 months.
Oestrogel (Pic)
Evorel Patches (pic)
Estradot Patches (pic)
Sandrena
Lenzetto
Vagifem vaginal tablets
Estraderm MX patches
Femoston
Femseven patches
Elleste Duet
Elleste Solo
Indivina
Kliofem
Kliovance
Livial
Novofem
Ovestin Cream
Premarin Tablets
Premique Low Dose
Progynova
Zumenon
What can you do if your HRT medicine is out of stock?
Your first port of call should be to contact your physician or GP to see if there is an alternative medicine you can take. Many HRT medicines have an identical active ingredient and can be used interchangeably with little disruption to your treatment. For example, Evorel Patches, Estradot Patches and Estraderm MX patches all contain estradiol as an active ingredient. This isn’t restricted to patches, Oestrogel, Sandrena and Lenzetto are all topical forms of HRT that your physician may recommend using interchangeably if they are well tolerated and treat the symptoms.
What can you do if you want your particular brand of HRT?
Due to the nature of HRT, many patients find that switching brands does not help their symptoms. Some patients are used to a certain brand of HRT and do not want to risk disrupting their stable regime. In this case it gets a little more tricky. Most HRT medicines are available intermittently and you will need to contact multiple pharmacies to see if you can source the medication. At Pharmacy Planet we have seen many customers order simply because the item is not available at other pharmacies.
Author: Boo Dhaliwal. The author is one of the clinical pharmacists working for Pharmacy Planet. Pharmacy Planet specializes in obtaining medicines that are difficult to source.
2 notes
·
View notes
Text
premarin - $1 billion of suffering and death

the cruelty in hrt
Drugs made from the urine of pregnant mares generate more than $1 billion in sales for Pfizer every year.
Due to its high oestrogen concentration, it is a key ingredient in many Hormone Replacement Therapy (HRT) drugs.
Premarin (PREgnant MARes' URIne) is the commercial name for the HRT medication manufactured by Wyeth Pharmaceuticals which is owned by Pfizer Pharmaceuticals.
abuses on pmu farms
For 6 months of their 11 - month pregnancies, the horses are confined 24/7 to stalls so small that they cannot turn around or take more than one step in any direction.
Around the world, hundreds of thousands of pregnant mares are kept on pregnant mare urine (PMU) farms. Here they must wear rubber urine-collection bags at all times, causing chafing and lesions. They are denied free access to water to increase oestrogen concentration.
Once the foals are born, they are taken away from their mothers – often forcibly. They are typically sold at auction by farmers where most are purchased by slaughterhouses.
Mares are then re-impregnated. This cycle continues for about 12 years until they are unable to become pregnant and are sent to slaughter.
Pfizer has PMU farms in the U.S. and Canada, as well as in China and India. They have purchased conjugated equine oestrogens in bulk from China and India since the 1980s. There are currently no nationwide laws in China that explicitly prohibit the mistreatment of animals.
If you’ve been prescribed HRT drugs like Prempak-C, Prempro, Premique, Premarin or the combined menopausal - osteoporosis drug Duavee, you have been prescribed a synthetic form of HRT that contains conjugated horse oestrogens.
plant - based alternatives to hrt
Plant - based and synthetic HRTs carry comparable benefits and risks.
Bio-identical hormones (BHRT) differ from conventional hormone replacement therapy, which by definition uses animal or synthetic hormones whose structures differ from those produced in the human body.
BHRT hormones are used as an alternative to HRT. They are compounds that have exactly the same chemical and molecular structure as hormones that are produced in the human body.
They are mostly derived from soya and yams which are chemically altered to become a therapeutic agent for humans and are thus cruelty free.
Transdermal gels and patches are suitable for vegans as well as pellets and implants. The vast majority of HRT tablets are not suitable for vegans as they tend to contain lactose and/or gelatine.
Some examples of alternative drugs include Estrace, Estratab, Climara, Cenestin, and Ortho-Est.
More information on the benefits and risks of BHRT may be found here:
https://www.healthline.com/health/bioidentical-hormone-replacement-therapy
With thanks to NEAVS, Wikipedia, Equine Advocates, Horse Fund and Last Chance for Animals.
Note: Whilst care has been taken to confirm the current availability of the HRT and BHRT mentioned some may have been discontinued since the sources were published.
Article originally posted in August 2021.
Image: Unsplash.
Graphic image by Elisabeth Mary.
#vegan#veganism#go vegan#govegan#go veg#goveg#hormone replacement therapy#hrt#bio - identical hormones#bhrt#premarin#premarin cruelty#pfzer cruelty#oestrogen
8 notes
·
View notes
Text
LGBT - How To Prepare For Your H.R.T. Meeting

SO YOUR SEEKING HORMONE REPLACEMENT THERAPY:
WHY?
Why do you want to seek hormone replacement therapy? What is the underlying cause to have you seek transformation? Is it because you’re sexually disadvantaged? A victim of abuse? A patient suffering from dysphoria of the body? Or have you been socially conditioned to alter your appearance? Knowing why is a must! Because 50% of those who undergo H.R.T. truly need it and 50% of those who undergo H.R.T. end up regretting it.
SEEK EDUCATION
Once you know why you want to undergo H.R.T.; you need to educate yourself about the benefits and risks of H.R.T..
If you are reading this article, then it is likely that you are in phase two and seeking education. Sadly, many (including myself) do not feel conformable bringing up this subject in public and have a difficult time doing the research online. There is so many ‘bad’ articles out there. Opinionated articles written by with pro-LGBT or anti-LGBT groups to push a narrative or agenda, using salacious data or failing to address the risks, both physiologically and psychologically to the patient.
If you can...talk to you Primary Care Physician or a center that specializes in LGBT services and ask for resources to make your own decision. Write articles, take notes, talk to your closes friends about the risks and benefits of H.R.T. and why you want to undergo this dramatic transition.
WHAT NEXT?
Prior to the clinical appointment with a physician, it is totally natural to feel nervous, anxious, excited, ambivalent, scared or all of there emotions all at once. When I was waiting, I felt all these emotions...I felt bipolar when it comes to the altering range of emotions.
One moment I am nervous (Will I be given the injection hormone? Or pills?), then anxious (time, place, money and open mindedness). Excited (I can’t believe I actually am doing this!), ambivalent (I pray this isn’t a phase...hate to ask my PCP for breast reduction!), scared (What if they deny me, or I take on too many female characteristics? Will my parents actually kill me if I beginning looking like a woman in two to six years? What will my friends think of me?).
One feeling I would add and that is: doubt
For 33 years I danced with doubt, and the last four months have been our grand ballroom dance. Even before I hear what they think, I already begun doubting myself, mostly because I realized that being on estrogen meant my transition was real, physical changes will happen and people will notice. No more hiding, no more Illuminati-like secrets...they will see and my brain will change as my testosterone levels are replaced with estrogen.
Even though I am scared, nothing will kept me from my appointment...I have been working my way to this point...it will be the greatest scientific experiment I will ever conduct...a second puberty occurring on my own body...I will document it to the tee. This might be a capstone in biological transformation that I’ve written and drawled so many times. I always placed myself in my characters shoes, but never could say what it was truly like...so now I will know!
The night after the call I kept thinking of all the things I was going to ask the doctor. Things the doctor might ask of me. HRT is like a transplant...if you are not mentally prepared, you will reject it! I ran simulation after simulation of different ways the appointment might go and my mind goes blank and the representative of me is left mumbling uh and um and yeah. I wanted to prevent this from happening, so I wrote down a few simulations. Sometimes it is better to have a list of questions prior to going into your appointment so you are collected and ready. It is also a great way to judge the doctor to see if they are the right one...remember...they are the one rebirthing you to your second birth!
PREPARING FOR DAY ONE:
Here are three areas to focus on during the first appointment...
1) To assess the providers knowledge and comfort with the different forms of treatment being oral, epidermal or endodermis.
2) To go over side effects and what to expect from starting on estrogen. This is a good way to see if the doctor knows the risks and emotional effects at which stage.
3) And to begin building a relationship with a healthcare provider that hopefully will be based on trust and openness.
It is important to be able to assess the provider’s knowledge and comfort because you want someone that can properly screen for any health issues that may be a problem in the future (I.e. heart trouble, cancer, blood clots and stroke).
Since I am Gender Neutral (closely related to Gender Fluid), it would be in my best interest to communicate with the provider that there are some things I am looking to physically change (I.e., breasts, fat distribution around the hips and butt, feminine features in the face and hair growth decrease on chest with halting male pattern baldness on head), but others that I wish to remain the same (I.e., penis, male facial features and muscular support that I have).
Lastly, having a provider that is up-to-date with the different types of dosing and methods to administer hormones is always helpful because then you are given options, options are extremely important when it comes to hormone therapy because a certain method may work well for one person, but not so well for another. (as seen in Operation B.O. H.R.T.)
SAMPLE QUESTIONS FOR PROVIDER:
So, when learning about the provider, questions that may help you assess their knowledge and comfort are as follows:
What methods do you give as options when prescribing hormones to your patients?
1a) Current options for estrogen, antiandrogens include: injectable, sublingual or oral, and transdermal.
1b) 17-beta estradiol (estradiol) is most commonly delivered to transgender women via a transdermal patch, oral or sublingual tablet, or injection of a conjugated ester (estradiol valerate or estradiol cypionate). No outcome studies have been conducted on injectable estradiol valerate or cypionate, presumably due to their uncommon modern use outside of transgender care settings; due to this limited use manufacturers have little incentive to produce this medicine, and shortages have been reported. Other delivery routes for estradiol such as transdermal gel or spray are formulated for the treatment of menopausal vasomotor symptoms and while convenient and effective in some transgender women, in others these routes may not be able to achieve blood levels in the physiologic female range. Compounded topical creams and gels also exist from specialty pharmacies; if these are to be used it is recommended that the prescriber consult with the compounding pharmacist to understand the specific details and dosing of the individual preparation. Compounded estradiol valerate or cypionate for injection also exists, and may be an alternative in times of shortage or more cost effective for those who must pay cash for their prescriptions.
Conjugated equine estrogens (Premarin®) have been used in the past but are not recommended for a number of reasons, including inability to accurately measure blood levels and some suggestion of increased thrombogenicity and cardiovascular risk. Equine estrogens are obtained from the urine of pregnant, catheterized horses; no evidence exists to suggest that these estrogens are superior to bioidentical human estradiol.
Ethinyl estradiol is a synthetic estrogen used in contraceptive preparations and is associated with an increased thrombotic risk. In the context of contraception, ethinyl estradiol has more consistent and reliable cycle control and as such is better tolerated, balancing out the potentially increased risk of VTE. In the setting of gender affirmation there is no need for cycle or bleeding regulation, and thus the use of ethinyl estradiol and its inherent risks are not warranted.
General Side effects of estrogens may include migraines, mood swings, hot flashes, and weight gain.
Spironolactone is the most commonly used androgen blocker in the U.S. Spironolactone is a potassium sparing diuretic, which in higher doses also has direct anti-androgen receptor activity as well as a suppressive effect on testosterone synthesis. Doses of 200mg daily in non-transgender women being treated for hair loss have been described as safe, though doses of up to 400mg/day have been reported without negative effect. Hyperkalemia is the most serious risk but is very uncommon when precaution is taken to avoid use in individuals with renal insufficiency, and use with caution and frequent monitoring in those on ACE inhibitor or ARB type medications. Due to its diuretic effect, patients may experience self-limited polyuria, polydipsia, or orthostasis.
5-alpha reductase inhibitors include finasteride and dutasteride. Finasteride blocks 5-alpha reductase type 2 and 3 mediated conversion of testosterone to the potent androgen dihydrotestosterone. Finasteride 1mg daily is FDA-approved for male pattern baldness, while the 5mg dose is approved for management of prostatic hypertrophy. Dutasteride 0.5mg more effectively blocks the type 1 isozyme, which is present in the pilosebaceous unit and therefore may have more dramatic feminizing effects. Since these medications block neither the production nor action of testosterone, their antiandrogen effect is less than that encountered with full blockade. 5-alpha reductase inhibitors may be a good choice for those unable to tolerate, or with contraindications to the use of spironolactone. 5-alpha reductase inhibitors may also be an option for use as a single agent in patients seeking partial feminization, or for those who continue to exhibit virilized features or hair loss after complete androgen blockade or orchiectomy.
1c)
Hormone Low Dose Medium Dose Maximum Dose
Comments
Estradiol oral/sublingual
1mg/dat 2-4mg/day 8mg/day if >2mg
Recommended divided bid dosing
Estradioltransdermal
50mcg 100mcg 100-400mcg
Max single patch dose available is 100mcg. Frequency of change is brand/product dependent. More than 2 patches at a time may be cumbersome for patient.
Estradiol valerate IMa
<20mg 2wk 20mg 2wk 40mg 2wk
May divide dose into weekly injections for cyclical symptoms.
Estradiol cypionate IM
<2mg 2wk 2mg 2wk 5mg 2wk
May divide dose into weekly injections for cyclical symptoms.
Spironolactone
25mg qd 50mg bid 200mg bid
N/A
Finasterride
1mg qd N/A 5mg qd
N/A
Dutasteride
N/A N/A 0.5mg qd
N/A
Are you familiar with the different methods and doses used? Are you open to trying different methods/doses?
2a) The answers to these questions will let you know how open your provider is, and also how knowledgeable they are regarding advances and new forms of treatment in transgender healthcare.
How many transgender clients do you currently work with?
3a) If you are the first, second, or third, you are most likely going to be learning together. If you are with a provider of over 20, 30 or 100, then they most likely are more experienced.
Do you follow the most up-to-date and current guidelines for transgender care?
4a) Although the World Professional Association of Transgender Health is not the only organization that provides Standards of Care, they are the most well-known. WPATH SOCv.7. is the old model. ICATH is the modern model.
Do they know other providers in different areas of transgender health in case you need a referral for specific care?
5a) You may have some health complications that require monitoring by a specialist. Or in the future you may require specialist care for something (it doesn’t have to be trans related) so having other provider’s names is always helpful. If your current provider has a trans-friendly referral list it may also be a sign that they are more knowledgeable and connected.
Questions to ask about hormones:
What are the side effects?
1a) If there are things they go over that causes you concern, ask for more information.
How will hormone therapy affected my fertility/reproductive options?
2a) If you are considering or would like the option of having (biological) kids in the future, then being informed of options and also risks with being on hormones therapy is something you should consider.
What is the general timeline for seeing changes?
3a) The World Professional Association for Transgender Health (WPATH) has a general timeline that can show you the expected changes as noted below:
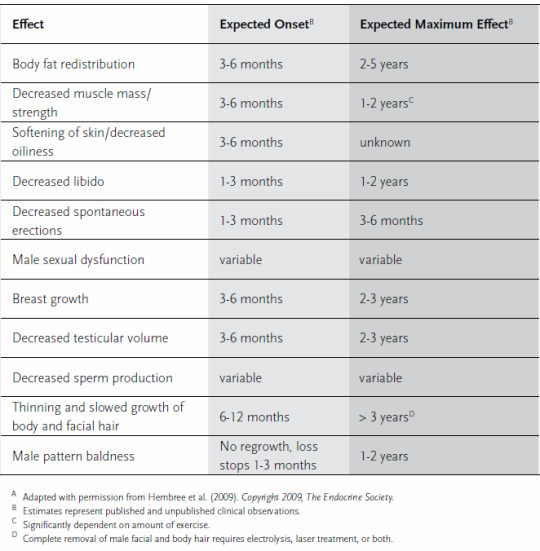
Body Fat Redistribution
3-6 months to show 2-5 years to finalize
Decreased Muscle Mass/Strength
3-6 months to show 1-2 years to finalize
Softening Of Skin/Decreased Oiliness
3-6 months to show Unknown
Decreased Libido
1-3 months to show 1-2 years to finalize
Decreased Spontaneous Erections
1-3 months to show 3-6 months to finalize
Male Sexual Dysfunction
Variable Variable
Breast Growth
3-6 months to show 2-3 years to finalize
Decreased Testicular Volume
3-6 months to show 2-3 years to finalize
Decreased Sperm Production
Variable Variable
Thinning And Slowed Growth Of Body And Facial Hair
6-12 months to show > 3 years to finalize
Male Pattern Baldness
No Regrowth, loss stops 1-3 months 1-2 years to finalize
QUESTIONS TO BUILD A RELATIONSHIP WITH THE PROVIDER:
What questions do they have for you?
1a) Question they ask may bring up more things that you wanted to ask them, but hadn’t thought of before.
Finally, if you are ready and feel good about your relationship with the provider then ask,
When can I get started!?
#gender nonconforming#transgender#gender bender#gender transformation#gender#non-conforming#nonconforming#nonbinary#transfiormation#transformation#trans#tg#lgbtq#lgbtqa#lgbtpride#lgbtq community#lgbt#body#body dysphoria#dysphoric#dystopia#estradiol#advocacy#advocate#mtf hrt#ftm hrt#hrt#ipath#wpath#cedarriverclinics
170 notes
·
View notes
Text
Premarin Coupon Available
Premarin is a brand name for conjugated estrogens used to treat menopausal symptoms and low estrogen levels. It is also used to prevent osteoporosis in postmenopausal women, and to reduce the risk of heart disease and stroke. Premarin is manufactured by Wyeth Pharmaceuticals, a subsidiary of Pfizer.
Premarin is available in tablet form and is taken orally. It is also available as a cream, vaginal ring, and injection. If you are taking Premarin, talk to your doctor about the risks and benefits of this medication.
If you are considering taking Premarin, you may be wondering about the Premarin cost. Premarin is a brand name medication, and brand name medications can be expensive. However, there are ways to save on the cost of Premarin. One way is to use a Premarin coupon.
Premarin coupon is available from a variety of sources such as MedsEngage. You can find them in newspapers and magazines, as well as online. When you use a Premarin coupon, you can save on the cost of your prescription. In some cases, you may be able to get a free trial offer of Premarin. This can be a great way to see if the medication is right for you before you commit to a long-term treatment plan.
0 notes
Photo
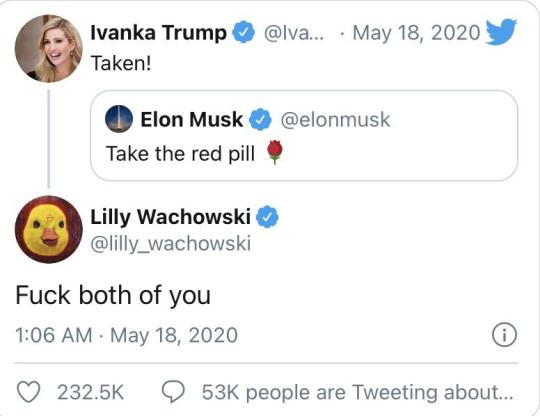
Just to remind people who use 'red pill' as synonymous for becoming conservative: the pill scene is actually a trans allegory and Lilly Wachowski has confirmed it; the red pill represents an estrogen maroon tablet called Premarin, which is used for MtF hormone therapy, whereas the blue pill is a sleeping tablet. Lilly Wachowski does not support you, so kindly go screw yourself.
20K notes
·
View notes
Photo

Premarin tablets is recommended by WHO to treat #hot flashes and vaginal dryness requirement visits our website https://rizocheminternational.in/ or for any information contact us (+91)9634771940.#COVID__19,#HIV,#medicines,#pharmaceutical,#wholesaler, #healthcare #Medicines,#Exporter #internationalbusiness
0 notes
Text
Estrogens, Conjugated (Systemic)


Brand Name: Premarin
Common Dosage Forms:
Tablets: 0.3 mg, 0.45 mg, 0.625 mg, 0.9 mg, 1.25 mg
Premarin Intravenous: 25 mg conjugated estrogens per Secule (vial)
*Also available in a formulation with methyltestosterone
FDA Indications/Precautions:
Indications for oral dosage route:
Vasomotor symptoms associated with menopause: 1.25 mg daily started on day five of cycle if menstruating, otherwise therapy is started arbitrarily.
Female hypogonadism: 2.5-7.5 mg per day in divided doses for 20 days, rest for 10 days, then repeat this schedule until bleeding occurs. If bleeding occurs before the 10 days are over, begin a 20 day estrogen-progestin cyclic regimen with Premarin 2.5-7.5 mg per day in divided doses for 20 days and during the last five days of those regimen give an oral progestin. If bleeding occurs before this regimen is completed, discontinue and resume on the fifth day of bleeding.
Female castration and primary ovarian failure: 1.25 mg a day (cyclically), adjusting dosage to the lowest level that will provide effective individual patient response.
Breast cancer (for palliation only): 10 mg three times a day for at least three months.
Prostatic carcinoma (for palliation only): 1.25-2.5 mg three times a day. Effectiveness can be judged by phosphate determinations as well as by symptomatic improvement.
Prevention of postmenopausal osteoporosis after other non-estrogen treatments have been considered: 0.625 mg daily.
Indications for intravenous dosage route:
Abnormal uterine bleeding due to hormonal imbalance in the absence of organic pathology (intravenous): One 25 mg injection given slowly. May be repeated in 6-12 hours.
Pharmacology/Pharmacokinetics: Premarin is a mixture of naturally occurring estrogens derived from pregnant mares’ urine. It is composed of estrone, equilin, and 17-alpha-dihydroequilin along with other less prevalent estrogens. Estrogens enter cells of responsive tissues (female genital organs, breasts, hypothalamus, pituitary) and are transported into the nucleus. Inside the cell nucleus, estrogens stimulate specific RNA and protein synthesis. Estrogens also decrease the release of follicle-stimulating hormone (FSH), luteinizing hormone (LH), and luteotropic hormone due to an effect on the pituitary or hypothalamus. Estrogens are important in the development and maintenance of the female reproductive system and secondary sex characteristics.
Drug Interactions: Barbiturates, rifampin, and/or hydantoins may increase metabolism and elimination. May increase the toxic effects of corticosteroids.
Contraindications/Precautions: Use is contraindicated in patients with known or suspected cancer of the breast except in selected patients being treated for metastatic disease. Do not use in patients with known or suspected estrogen-dependant-neoplasia, known or suspected pregnancy, undiagnosed abnormal genital bleeding, or in patients with (or history of), thrombophlebitis, thrombosis, or thromboembolic disorders, except when used in treatment of breast or prostatic malignancy. ESTROGEN-ALONE THERAPY INCREASES THE RISK OF STROKE, DEEP VEIN THROMBOSIS, ENDOMETRIAL CANCER, IN WOMEN OVER 65 YEARS OF AGE, AND IN PROBABLE DEMENTIA. Do not use in nursing mothers. Because of increased fluid retention, use with caution in patients with hypertension, asthma, epilepsy, migraine, and cardiac or renal dysfunction. Use with caution in patients with a history of jaundice during pregnancy, diabetes, impaired liver function, and metabolic bone disorders. Pregnancy Category X.
Adverse Effects: Rash, acne, alopecia, hirsutism, abnormal menstrual bleeding, edema, changes in weight, cholestatic jaundice, changes in cervical erosion and cervical secretions, mental depression, pyrexia, insomnia, nausea, and somnolence.
Patient Consultation:
May be taken with food or milk is GI upset occurs.
Read patient information sheet carefully.
Discontinue therapy and consult physician if pregnancy is suspected.
If a dose is missed, take it as soon as possible and return to dosing schedule.
Store in a cool, dry place away from sunlight and children.
Report any severe side effects to your physician, including pains in the legs, coughing blood, abnormal vaginal bleeding, skin yellowing, and abdominal pain.
0 notes
Text
What You Should Do to Stop Sex From Hurting After Menopause
Tips to fix vaginal dryness for good
Sex does not have to hurt
Pleasurable sex after menopause is within your grasp. Vaginal burning and irritation after sex are not acceptable. Insertion of the penis should not feel like something is tearing. Penetration should not feel like sandpaper. These are classic symptoms of vaginal dryness and vulvar atrophy. You do not have to live with it. Painful intercourse, dyspareunia, is a complex issue with many causes. We will focus attention on vaginal dryness, a condition affecting 50–70% of women after menopause. You do not have to ignore vaginal dryness.
Doctors should ask, and patients should speak up
Both doctors and patients have opportunities to change the perception of postmenopausal intercourse pain. Both parties recognize menopausal symptoms like hot flashes. Vaginal pain, vaginal dryness, and sexual issues often get missed or ignored. Doctors don’t always ask. Patients don’t always tell. Both should improve. Doctors and patients must overcome the misconception that the physiological genital changes are an unimportant and unchangeable aspect of aging.
How do I know if I have vulvar-vaginal atrophy
The medical term for postmenopausal dryness is vulvar-vaginal atrophy (VVA). No specific tests are needed. The first step in making the diagnosis is asking the right questions. Symptoms include inadequate lubrication, pain during insertion, post-coital irritation, vaginal burning, or inhibited ability to achieve orgasm. Some may experience frequent urinary tract infections or painful urination after sex. Some may experience discomfort with exercise, especially bike riding.
What causes atrophy?
Estrogen is a hormone produced by the ovaries. Hormone production decrease as one approaches menopause. The ovaries stop producing hormones at menopause. The cells lining the vagina are sensitive to estrogen. Low estrogen decreases blood flow to the vagina. When deprived of estrogen, the cells thin out and provide less moisture.
What causes a drop in estrogen?
Menopause
Breastfeeding
Surgical menopause (removal of the ovaries)
Medications such as Lupron, antidepressants, and antihistamines
Chemotherapy and radiation for cancer treatment
What does a lack of estrogen due to the vagina?
The dropping hormone levels cause the tissue lining the vagina to thin and lose elasticity. The labia majora flatten out, the labia minora shrink, and the hymenal remnants retract. The vaginal length may shorten. The vaginal walls narrow and become less elastic and stretchy.
Symptoms of vaginal atrophy
Sexual discomfort (Dyspareunia: pain, irritation, or bleeding
Indequate vaginal lubrication during sexual stimulation
Vaginal dryness
Frequent bladder infections
Inhibited ability to achieve orgasm
Frequent urinary tract infections
Pain during urination
Vaginal discomfort with exercise
Slippery when wet

Photo by Skitterphoto
Sexual Lubricants are your best friend
The first step is to invest in a sexual lubricant. Buy a small bottle of a few different brands to test what works for you. Not all lubricants are the same. Most lubricants available at a local pharmacy are water-based. Water-based lubricants are the safest for use with condoms to prevent sexually transmitted infections. They do not break down latex in condoms or sex toys. Water-based lubricants dry out quickly, making them suboptimal for postmenopausal women.
Try a silicone-based lubricant
For monogamous couples at low risk for sexually transmitted infections, a silicone-based lubricant may be more effective and pleasurable. Silicone-based lubricants stay slippery longer avoiding the frustration of rapid drying and messiness of reapplication. Silicone-based lubricants will break down latex condoms or latex in sex toys. Penchant Premier is a great product that comes in tasteful and discreet packaging. Avoid products with Parabens or Glycerin. These chemicals are irritants for some users. Avoid flavored or heated lubricants at first. Apply lubricant to the vagina, clitoris, and penis before insertion. Make it a part of foreplay. This simple trick can improve sexual pleasure for many postmenopausal women.
Foreplay, foreplay and more foreplay
Communicate your needs to your partner. Many women require more attention to foreplay to achieve stimulation. Better stimulation leads to more natural lubrication and an increase in vaginal elasticity. Your partner may be unaware of the physiological changes with menopause. Do not be afraid to communicate your needs. What worked for both of you in the past may need to change. Do not be afraid to teach your partner. Speak up and communicate your needs. Menopause is an excellent opportunity to talk about sex with your partner and revitalize your relationship.
Take your vagina to the gym
There are a variety of medications that can help treat vulvar vaginal atrophy. Each medication works differently, but all have the same basic effects of bulking up the cells lining the vagina. Bulked up vaginal cells produce more moisture. Lubrication improves, and the vaginal walls avoid trauma during penetration.
Vaginal Estrogen
Menopause leads to a decrease in the production of estrogen by the ovaries. Estrogen can be placed directly into the vagina to bulk up the vaginal cells. A very low dose of estrogen is effective when placed directly in the vagina. The low dose offsets many of the risks associated with the use of estrogen. Vaginal estrogen comes in a variety of forms.
Estrogen cream (Estrace/Premarin)
Estrogen tablets (Vagifem)
Estrogen rings (Estring, Femring)
Vaginal suppositories (Imvexxy)
DHEA Supplementation
Many women do not want to take estrogen. DHEA hormone is a highly effective alternative. Prasterone, sold under the brand name Intrarosa, uses the hormone DHEA to treat vaginal atrophy. Before menopause, DHEA levels are high. As the ovaries stop functioning, DHEA levels fall. Prasterone is inserted into the vagina once a day. This plant-derived form of DHEA converts into estrogen targeting the underlying cause of dryness. It is FDA indicated for painful intercourse.
Selective estrogen receptor modulators (SERMS)
Ospemifene (Osphena) is the only FDA approved oral drug for vaginal dryness and painful intercourse. It is not estrogen. Osphena works by acting on the hormone receptors directly. Direct targeting of the vaginal tissue increases the thickness of the superficial and parabasal vaginal cells.
Topical Sildenafil
Sildenafil, sold as Viagra, is used to treat erectile dysfunction in men by increasing blood flow to the penis. Some women benefit from the application of a pea-size amount of compounded Sildenafil cream directly to the clitoris before intercourse. Sildenafil cream increases blood flow to the clitoris, which may improve pleasure and help with orgasm. It is not FDA approved for this use.
Vaginal Moisturizers
There are multiple products available over the counter to help increase vaginal moisture. We recommend a locally produced product called Prevleaf Soothe. The basic idea is to prevent dryness and improve the ph balance. While these do not treat the underlying cause of atrophy, they may be useful for day to day use.
Don’t be afraid to speak up about vaginal dryness

Photo by Clément Falize on Unsplash As we grow older, our bodies change. We do not have to accept all the changes. We use reading glasses as our vision fails. We apply Rogaine for our regressing hairline. We do not have to live with painful sex just because we are aging. There is no cause for shame or embarrassment. Speak up and communicate your needs to your doctor and your partner. You owe it your self to enjoy sex throughout your life. Blog by: Dr. Jeff Livingston Blog Photo By: Gabriel Matula on Unsplash

The Amazon links used are tied to Amazon.com Proceeds generated are donated to the Irving ISD Teen Parenting program, a drop out prevention program for students who are pregnant or parenting.
0 notes
Link
How to moisturize vagina
Vaginal Dryness: Causes and Moisturizing Treatments
IN THIS ARTICLE Causes Diagnosis Medication Other Products Normally, the walls of the vagina stay lubricated with a thin layer of clear fluid. The hormone estrogen helps maintain that fluid and keeps the lining of your vagina healthy, thick, and elastic. A drop in estrogen levels reduces the amount of moisture available. It can happen at any age from a number of different causes. It may seem like a minor irritation. But the lack of vaginal moisture can have a huge impact on your sex life. Fortunately, several treatments are available to relieve vaginal dryness.

Causes Vaginal dryness is common symptom of menopause -- and close to one out of every three women deals with it while going through "the change." It becomes even more common afterward. It also makes the vagina thinner and less elastic. This is called vaginal atrophy. Estrogen levels can also drop because of: Childbirth and breastfeeding Radiation or chemotherapy treatment for cancer Surgical removal of the ovaries Anti-estrogen medications used to treat uterine fibroids or endometriosis Other causes of vaginal dryness include: Sjögren's syndrome (an autoimmune disorder that attacks cells in the body that produce moisture) Allergy and cold medications Certain antidepressants Douching Not enough foreplay before sex No matter what the cause, vaginal dryness can be extremely uncomfortable. It can lead to itching, burning, and painful intercourse. Diagnosis Any burning, itching, or discomfort in the area is worth a call to your doctor or gynecologist. They'll ask about your past health and find out how long you've had symptoms and what seems to make them worse or better. Your doctor will do a pelvic exam, checking your vagina for any thinning or redness. The exam will help rule out other possible causes for your discomfort, including a vaginal or urinary tract infection. The doctor may also remove cells from your vaginal wall or cervix for a Pap test. Medication The most common treatment for vaginal dryness due to low estrogen levels is topical estrogen therapy. These replace some of the hormone your body is no longer making. That helps relieve vaginal symptoms, but it doesn't put as much estrogen in your bloodstream as the hormone therapy you take in pills. Most women use one of three types of vaginal estrogen: Ring (Estring): You or your doctor inserts this soft, flexible ring into your vagina where it releases a steady stream of estrogen directly to the tissues. The ring is replaced every 3 months. Tablet (Vagifem): You use a disposable applicator to put a tablet into your vagina once a day for the first two weeks of treatment. Then you do it twice a week until you no longer need it. Cream (Estrace, Premarin): You use an applicator to get the cream into your vagina. You'll typically apply the cream daily for 1 to 2 weeks, then cut back to one to three times a week as directed by your doctor. Any estrogen product can have side effects, such as vaginal bleeding and breast pain. Topical estrogen may not be recommended when you: Have breast cancer, especially if you're taking an aromatase inhibitor Have a history of endometrial cancer Have vaginal bleeding but don't know why Are pregnant or breastfeeding There isn't much research on the long-term use of topical estrogen, but doctors believe it's safe. Other Products You can buy a vaginal moisturizer like glycerin-min oil-polycarbophil (Replens) at your local drugstore or supermarket. A drug taken orally An oral drug taken once a day, ospemifeme (Osphena), makes vaginal tissue thicker and less fragile, resulting in less pain for women during sex. The FDA warns that Osphena can thicken the endometrium (the lining of the uterus) and raise the risk of stroke and blood clots. Take your time before having sex to make sure that you're fully relaxed and aroused. Apply a water-based lubricant (Astroglide, K-Y) to help enjoy intercourse more. Avoid using douches, bubble baths, scented soaps, and lotions around the sensitive vaginal area. These products can worsen dryness.
0 notes
Text
Big Pharma Forces Women to Choose Between Dry Vaginas or Dry Bank Accounts
Costs of products that improve women’s sex lives by treating a dry vagina, a taboo yet common condition, are on the rise here in the U.S. It’s bad enough to face the unfair stigma of needing medication that has anything to do with your vagina, but Big Pharma has decided to make that experience even more difficult. American women deserve to know that those much-needed products are sold at international online pharmacies for a fraction of the price tag at their local pharmacy.
The New York Times’ Katie Thomas recently published an article, Prices Keep Rising for Drugs Treating Painful Sex in Women, that highlighted this quiet conversation in the corner of the drug prices crisis. Your EpiPens and asthma inhalers are perhaps easier to gripe loudly about than meds related to personal matters. “It’s just infuriating that the price has gone up and up and up for no good reason,” said Cynthia Pearson, the executive director of the National Women’s Health Network, who expressed frustration at the lack of attention due to the stigma.
Women have seen prices on drugs, such as Estrace cream and Estring, more than double in the last five years. The article goes on to report that one woman “has resorted to ordering her drug from overseas at a cost of about $80 for a three-month supply,” which is great news for that savvy lady, but unfortunately leaves the reader hanging on how to safely order their own medication from abroad. After all, shopping for medications online can be quite treacherous: the internet is a landmine of scammers and sellers of counterfeit medication. Peer-reviewed and independent research demonstrates that when consumers use PharmacyChecker-verified pharmacies to buy medications purchased online, they receive lawfully-manufactured, high-quality medication. Not to mention those meds are typically sold at a much lower price than available at local U.S. pharmacies.
Vagifem sold in the U.S., mentioned in the article, is actually manufactured in Denmark. At U.S. pharmacies, just 8 tablets of Vagifem 10 mcg can cost women around $200, but it’s sold at international online pharmacies for as low as $20, a 90% savings. Premarin Vaginal Cream is a whopping 98% cheaper if women order through an online pharmacy in the United Kingdom that’s been verified by PharmacyChecker. Premarin sold in the U.S. is manufactured in Canada.
Vagina may be a stigmatized word, but saving money on meds? Now, that’s something to shout about.

The post Big Pharma Forces Women to Choose Between Dry Vaginas or Dry Bank Accounts appeared first on PharmacyChecker Blog.
from PharmacyChecker Blog https://ift.tt/2sSSjAh via IFTTT
0 notes
Text
Drugs by letter B
Drug Name PROGRAF 5MG CAPS Hikma Pharmaceuticals PLC PROGRAF1MG CAPS Hikma Pharmaceuticals PLC PURINOL 100 MG Hikma Pharmaceuticals PLC 300 PURINOL 300 MG Hikma Pharmaceuticals PLC 125 PENAMOX 125MG-5ML SUSP Hikma Pharmaceuticals PLC 250 PENAMOX 250MG-5ML SUSP. Hikma Pharmaceuticals PLC PENAMOX CAPS 250MG Hikma Pharmaceuticals PLC PENAMOX CAPS 500 MG Hikma Pharmaceuticals PLC BETACORT 4MG-ML AMP Hikma Pharmaceuticals PLC PROVERA 5MG TAB PFIZER Percolone Pamidronate Procureamide Pronestyl Bisoprolol PROTOPIC 0.03% OINTMENT Astellas Pharma PROTOPIC 0.1% OINTMENT Astellas Pharma BALAD RIYADH PHARMA PANADOL COLD & FLU CAPLET GLAXOSMITHKLINE (GSK) PANADOL SINUS CAPLET GLAXOSMITHKLINE (GSK) Propulsid BLOPRESS 16 MG TABLETS APM BLOPRESS 16 PLUS TABLETS APM BLOPRESS 8 PLUS TABLETS APM BLOPRESS 8MG TAB. APM PEDOVEX 75MG F.C. TABLETS TABUK PHARMACEUTICAL MANUFACTURING CO. PLAVIX 75 MG TABLET sanofi-aventis BETATEN 100MG F.C. TABS NATIONAL PHARMACEUTICAL INDUSTRIES CO BETATEN 25MG F.C. TABLETS NATIONAL PHARMACEUTICAL INDUSTRIES CO 50MG BETATEN 50MG F.C.TABLET NATIONAL PHARMACEUTICAL INDUSTRIES CO PRESLO 100MG F-C TABLETS JAMJOOM PHARMACEUTICALS COMPANY PRESLO 50MG F-C TABLETS JAMJOOM PHARMACEUTICALS COMPANY PROGYLUTON TAB BAYER SCHERING PHARMA prent Bydureon BYETTA 250 MCG / ML PRE - FIIED PEN BAXTER PHARMACEUTICAL SOLUTION LLC Premarin PK-MERZ MERZ PHARMACEUTICAL BETAFERON 8MIU \ ML VIAL BAYER HEALTHCARE PEGASYS 135 MCG-0.5ML PRE-FILLED SYRINGE ROCHE PEGASYS 180 MCG-0.5ML PRE-FILLED SYRINGE ROCHE PEG-INTRON 100MCG \ 0.5ML VIAL SCHERING-PLOUGH PEG-INTRON 100MCG-0.5ML VIAL SCHERING-PLOUGH PEG-INTRON 120MCG \ 0.5ML VIAL SCHERING-PLOUGH PEG-INTRON 120MCG-0.5ML VIAL SCHERING-PLOUGH PEG-INTRON 150MCG \ 0.5ML VIAL SCHERING-PLOUGH PEG-INTRON 150MCG-0.5ML VIAL SCHERING-PLOUGH PEG-INTRON 50MCG \ 0.5MLVIAL SCHERING-PLOUGH INTRON 80MCG \ 0.5ML VIAL SCHERING-PLOUGH PEG-INTRON 80MCG-0.5ML VIAL SCHERING-PLOUGH Progest Prometrium PROSTIN VR AMP PHARMACIA UPJOHN PROCTOLAR CENTER SUPPOSITORY ARAB CENTER FOR PHARMACEUTICALS & CHEMICAL IND. CO. Proleukin BONAMAX 35MG TABLETS RIYADH PHARMA BONAMAX 70MG TABLETS RIYADH PHARMA PENBRITIN VIAL 250 MG SMIITHKLINE BEECHAM BARACLUDE 1MG F.C. TABLETS BRISTOL-MYERS SQUIBB BI PRETERAX ARGININE 5MG-1.25MG F.C. TAB SERVIER PRETERAX ARGININE 2.5MG-0.625MG F.C. TAB SERVIER Perebron Benicar PATADAY 0.2% OPHTHALMIC SOLUTION ALCON LABORATORIES PATANOL 0.1% OPHTHALMIC SOLUTION ALCON LABORATORIES ATROVENT 500MCG-2ML UDV (SOLUTION FOR INHALATION) BOEHRINGER INGELHEIM
English
A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
source https://www.medicineonline.tk/2019/06/drugs-by-letter-b-drug-name-prograf-5mg.html
0 notes
Text
At the point when Sex Gives You More Pain Than Pleasure
New Post has been published on http://www.withallwomen.com/at-the-point-when-sex-gives-you-more-pain-than-pleasure/
At the point when Sex Gives You More Pain Than Pleasure
As menopause hits, estrogen levels drop, and what regularly takes after is dryness and diminishing of the vaginal tissues. The awkward side effects can incorporate a vibe of snugness, dryness and extreme torment or consuming—barely a hot situation. A dry vagina isn’t just annoying however can mean excruciating sex, a typical grievance of upwards of 46 percent of postmenopausal ladies. What’s more, the numbers are likely higher, in light of the fact that numerous ladies feel a disgrace or are excessively humiliated, making it impossible to discuss it.Medicinally known as dyspareunia, this torment—which can occur previously, amid and after sex—may create because of the vaginal dryness, known as vulvovaginal decay. It additionally may have other mental or physical causes, including vaginismus or genital damage. Vulvovaginal decay—the diminishing, drying and irritation of vaginal tissues—is regular around menopause, because of declining levels of estrogen. Whatever the reason, vaginal torment can put a strain on the best of connections, sap confidence and influence a lady’s personal satisfaction. The outcomes can reach a long ways past excruciating sex itself. Dreading torment, ladies may automatically tense their vaginal muscles or maintain a strategic distance from or shun sex inside and out, additionally confusing issues. (adsbygoogle = window.adsbygoogle || []).push();
Luckily, there are medicines, which in some cases require a multifaceted methodology.Low-measurements vaginal estrogen. Vaginal estrogens are otherwise called estradiol and contain a similar kind of estrogen your body makes. It helps by reestablishing vaginal blood stream and enhancing the vaginal tissue’s thickness and flexibility. Since the estrogen goes specifically into the vagina, there’s less danger of symptoms than with oral estrogen, as it won’t raise the coursing blood levels of estrogen altogether.Vaginal estrogen is accessible in two creams (Estrace Vaginal Cream and Neo-Estrone or Premarin Vaginal Cream), a tablet (Vagifem), or a vaginal ring (Estring). Most up to date to the market is Imvexxy, an implement free vaginal embed that comes in two dosages.The North American Menopause Society prompts utilizing the most minimal successful measurements to restrict symptoms, which are uncommon however can incorporate migraine, sickness, bosom torment or vaginal consuming or agony.
You may be interested in this article Advantages of Strength Training As You Age
In spite of the fact that the American College of Obstetricians and Gynecologists (ACOG) says that there’s no expanded danger of disease repeat among ladies who are being dealt with for bosom tumor or those with a past filled with it, this gathering of ladies is as yet encouraged to talk about the dangers and advantages with their social insurance experts. Ointments. These come in fluid or gel frame and are connected specifically to the vagina or vulva (the external piece of the vagina) previously or after sex to ease torment from dryness. Greases work by diminishing contact and can likewise be connected to an accomplice’s penis preceding intercourse. Oils go to work quickly and are not ingested into the skin, giving impermanent alleviation from dryness and excruciating sex. Ointments are accessible over-the-counter and might be water-, silicone-or oil-based. Know that oil-based oils like oil jam or infant oil can cause vaginal bothering and may cause breaks in latex condoms.
(adsbygoogle = window.adsbygoogle || []).push();
Lotions. Intended to be connected frequently (not only before sex), lotions have longer-term impacts than greases and can keep going for up to four days. They’re consumed into the skin and stick to the vaginal covering, which assists with vaginal solace since they mirror its normal dampness and sharpness. Pelvic floor active recuperation. Despite the fact that this is moderately new and hasn’t been examined broadly, specialists point to its wellbeing and viability. Physical advisors can noninvasively release tight tissues in the pelvic territory utilizing rub and delicate weight and train activities to reinforce pelvic floor muscles.
You may be interested in this article What to Eat for Breakfast for Weight Loss
Different techniques that can help oversee dyspareunia incorporate directing and self-care. Treat your vagina tenderly: Use gentle cleanser or plain water to wash yourself and pat, as opposed to rub, dry. Avoid items that contain fragrances (like air pocket showers or douches) that might bother. Wear combatable-fitting cotton clothing, which is more breathable and wicks away dampness, and maintain a strategic distance from tight-fitting apparel. (adsbygoogle = window.adsbygoogle || []).push();
0 notes
Text
Bachmann Coupon Savings
Videos Boscov’s Coupon Codes – Offers.com PREMARIN® (conjugated estrogens tablets, USP) | Safety Info source http://www.rslayouts.com/bachmann-coupon-savings/
0 notes