#Paediatrics
Explore tagged Tumblr posts
Text



paeds rotation is nearly coming to an end 🥹 I only hope internal medicine is not too hard on me.
#medicine#medblr#medblog#junior doctor diaries#junior doctors#junior doctor#paediatrics#pediatriccare#neonatology
91 notes
·
View notes
Text
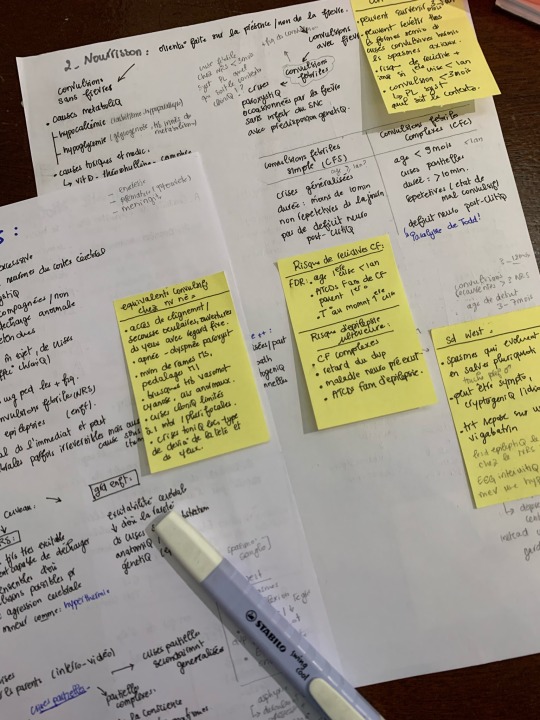


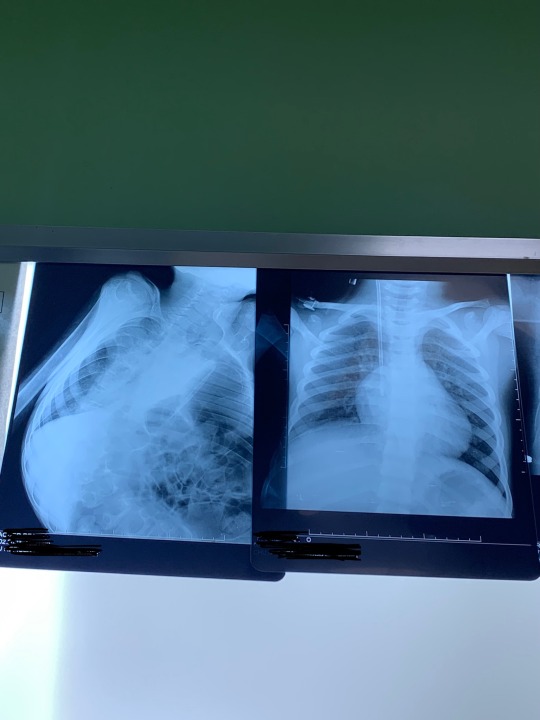
What paediatrics rotation look like
#studyblr#med life#medicine#studyspo#medblr#paediatrics#studygram#medical student#medical stuff#study motivation#100 days of productivity#medical studyblr#study notes#study aesthetic#college#studying#dark academia#random#rotation#medics#med student#linastudyblrsblog#studystudystudy#linastudyblrsbog
304 notes
·
View notes
Text
Someone reblogged one of my old posts where i mention emergency medicine and these days I can’t believe I almost chose that as a specialty. These days if i’m in the hospital past 6PM i want to throw up. If i see a patient older than 16 i’m just confused. I need a 45 minute break half way through a ward round to drink hot choccy and gossip. I was born to be a pediatric sub specialist.
8 notes
·
View notes
Text

+
51 notes
·
View notes
Text
23.08.2023
Major life update!
Got allotted into DNB paediatrics 2 weeks back. Was super thrilled when I found out that I got into an institute that was in my top 10 list. Past few days I have been travelling back and forth to visit the hospital I would be working and looking for places to stay for the next 3 years. Met my possible future co workers and had a great time getting to know them. Looking forward to this next great endeavour ✨
PS: Yes I have hoarded ebooks and study materials and clinical guides from my seniors already :p




#phtooftheday#medstudlife#studyblr#neetpg#studysthetics#medstudynotes#neetpg2023#study mood#first aid#inicet#paediatrics#pediatrics#paediatrician#dnbpaediatrics#to new beginnings#study notes#med studyblr#new studyblr#desi studyblr#new medblr#medblr#medblog#studywithme#indian studyblr#studyinspo
35 notes
·
View notes
Text
Tarsal scaphoiditis: when your child's foot hurts
Tarsal scaphoiditis, also known as Köhler-Mouchet disease, is a condition that mainly affects young boys aged around 5. It is characterised by necrosis (death) of the navicular bone in the foot, a small bone located in the arch of the foot.

What are the symptoms?
- Pain in the inner arch of the foot, often aggravated by walking.
- Lameness.
- Difficulty carrying weight on the affected foot.
What are the causes?
This condition is often associated with static disorders of the foot (flat foot, hollow foot).
How can the diagnosis be confirmed?
X-rays show the characteristic changes in the navicular bone.
What is the treatment?
Treatment is generally conservative and includes
- Rest and avoidance of strenuous physical activity.
- Analgesics to relieve pain.
- Plantar orthoses to correct static disorders of the foot.
In the majority of cases, recovery is spontaneous.
Go further
2 notes
·
View notes
Text
i lowkey wanna be a paediatrician but I’m so scared.. isn’t med school stressful and stuff? Im not that interested in medicine I just wanna work with kids 😭
#this is what makes us girls#girl blogger#girl blog aesthetic#paediatrics#any tips?#school#ughhhh#med school#medicine#hospital
5 notes
·
View notes
Text

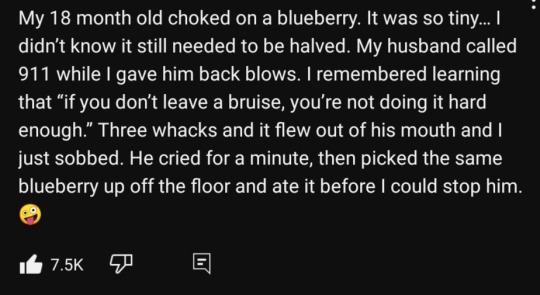
Me: perfectly fine during a trek or a hike
Also me: trips and almost falls flat on my face while walking on flat ground
#textposts#youtube#youtube comments#youtube comments section#choking#choking but not the kind you're thinking of#baby food#parenting#paediatric#paediatrics#paediatrician#babies#toddlers#grapes#surgery on a grape#firstaid#eat off the floor#YouTube comments section is legit a goldmine sometimes#youtube on Tumblr
8 notes
·
View notes
Text
Highlights of the internship - Week 10:
• I inserted orogastric tube to a neonate. It is inevitable to think “what if I do something wrong and hurt them?”
• I am normally confident with my suturing, I have had a lot of practices but I have never tried it on a child before. On a child, who obviously cries out loud and screams. I was nervous but I am glad to say that I have handled it pretty well; on chin, knee, arm, etc. I have had the chance to do it on many kids in the ER.
• I was going to attend an amputation operation, offered to me by the orthopaedics attending and intern, but the last minute change in their schedule made me miss it :’)
• On my first day at the ward, I was alone and I have admitted 9 patients on my own. The information on the papers being so comprehensive that history taking and doing examination took a long time, I could not sit and rest for a minute. Towards the end of the day, the resident saw me and said, “you have worked so much today and you seem like you are done with life now.” Well, that is because I am.
• I had to draw blood from my mother, whose veins are not prominent at all and will never show up even with tourniquet. So I had to try the middle of her forearm, I was sucessful but she has bruise in that area now :’)
• There was a 3-month-old boy I admitted to the ward and I was there when he was discharged but they came back during my night shift in the ER. We come across there and the mother recognised me when she saw me; “we had to come back and he will be hospitalised again.” Apparently, when she went to the ward that day, she said: “Dr. (my name) was our doctor.” 🥹🥹
#paediatrics#internship#6th year#medical student#medical stuff#medical school#medblr#night shift memories
9 notes
·
View notes
Text
Looking at a Systematic Review of Environmental Risk Factors for Child Stunting
Child stunting, characterized by impaired growth and development, is a significant public health concern globally. While nutrition plays a crucial role, there are other environmental factors that contribute to this condition. In this blog post, we will delve into the findings of a systematic review conducted by Vilcins et al. (2018) to highlight the key environmental risk factors associated with child stunting. This research sheds light on the multifaceted nature of stunting, beyond nutritional aspects, and provides valuable insights for effective interventions.
Household Air Pollution:
The systematic review by Vilcins et al. emphasizes the impact of household air pollution on child stunting. Exposure to indoor air pollution from sources like solid fuel for cooking and heating, such as biomass or coal, can lead to respiratory infections and chronic inflammation. These conditions can impair a child's growth and development. For instance, in regions where solid fuel is commonly used, such as parts of Africa and Asia, children exposed to high levels of indoor air pollution have an increased risk of stunting.
2. Water, Sanitation, and Hygiene (WASH) Practices:
Inadequate access to clean water and sanitation facilities significantly contribute to child stunting. Vilcins et al. highlight how poor WASH practices, including limited access to clean water for drinking and hygiene, and inadequate sanitation facilities, increase the risk of infectious diseases and nutrient deficiencies. For example, in areas where open defecation is practiced, the risk of stunting is higher due to the increased likelihood of fecal-oral transmission of diseases like diarrhea and intestinal parasites.
3. Environmental Contaminants:
The presence of environmental contaminants, such as heavy metals and pesticides, is associated with child stunting. Exposure to these pollutants, either through contaminated soil, water, or food, can interfere with a child's growth and development. For instance, in agricultural communities where pesticides are extensively used, children may be exposed to these harmful substances, which can impair their cognitive development and contribute to stunting.
4. Poor Housing Conditions:
Inadequate housing conditions, including overcrowding, lack of ventilation, and dampness, are identified as risk factors for child stunting. These conditions increase the likelihood of respiratory infections, which can impact a child's nutritional status and growth. For example, in slum areas with crowded living spaces and insufficient ventilation, children are more susceptible to respiratory illnesses, leading to stunting.
Vilcins et al.'s systematic review highlights the environmental risk factors associated with child stunting beyond nutritional aspects. Household air pollution, poor WASH practices, exposure to environmental contaminants, and inadequate housing conditions all contribute to stunting. Addressing these factors requires comprehensive interventions that improve access to clean energy, promote proper WASH practices, reduce environmental pollution, and enhance housing conditions. By understanding and addressing the environmental risk factors associated with child stunting, policymakers, health professionals, and communities can work together to develop effective strategies for prevention and intervention. It is through targeted actions and investments in improving environmental conditions that we can reduce child stunting rates and ensure healthier futures for children worldwide.
References!
Vilcins, Dwan, Peter D. Sly, and Paul Jagals. "Environmental risk factors associated with child stunting: a systematic review of the literature." Annals of global health 84.4 (2018): 551.
#medical anthropology#medicine#global health#global medicine#child stunting#paediatrics#social determinants#systemic review#anthropology#scientific literacy#environmental factors
2 notes
·
View notes
Text



26-01-2024
peds rotation goes on
107 notes
·
View notes
Text




But first coffee
#study aesthetic#studyblr#medicine#med life#studyspo#coffee#coffetime#studygram#medical student#studying#university#paediatrics#medblr#study with me#studystudystudy#studyblog#100 days of productivity#photography#dark academia aesthetic#dark academia#linastudyblrsblog
109 notes
·
View notes
Text
A relatively new problem in paediatrics is that as technology improves, as we have better early detection and better therapies, more of our patients are surviving to adulthood (which is fantastic!!!) but the adult medical world is woefully underprepared to support these people.
I’ve known so many colleagues with so many stories about how they transitioned someone to adult care who had been doing really well, who then died within a couple months. We care for children until age 16, but many of our kids with chronic and complex conditions we keep until 18/19 in the hospital - and for those with life-limiting conditions some people will continue to see them in clinic until they die.
I don’t think this is individual adult physicians’ fault, but it does show an inability of the system to support adults with disabilities compared to children - it’s harder to get, for example, daily chest physio, good multidisciplinary care, carers at home to the true extent that they are needed. It’s also related to a lack of knowledge, which to some degree is fair - many adult physicians didn’t learn about cerebral palsy, or many of the epilepsy or genetic syndromes, because those people just didn’t live to see an adult neurologist in the past.
However, this is no excuse. The world has changed for the better, people who used to die at 5 are reaching adulthood! But the medical world needs to adapt and improve and make room so that these gains can continue well into adulthood.
The world isn’t kind to anyone with disabilities, but particularly to adults. The lack of support is egregious but, in my opinion, fixable.
#medblr#pediatrics#paediatrics#sorry for the rant we had a rehab lecture today and it reminded me of some of the really lovely kids i’ve met#and the comparison to the adults i met back when i worked in an adult ED#And just the massive difference in support#not that paeds is perfect!!!! many things we could improve on#and i know all specialties are improving all the time
6 notes
·
View notes
Text




13.09.2023
Had a busy couple of days. I am currently waiting for my official announcement for my course commencement. Until then I decided to tutor at a nearby coaching institute and I was kept busy, also it helps me pay for my Uworld.
Last Sunday I got a day off and I decided to meet my closest friends from school. We have know each other for over a decade and a half and our lives are so different now, but like every time we meet and hangout it feel like nothing has changed. So had lunch and decided to go beach hopping, while we reached the beach it was too sunny so we decided to wait for sometime, when we noticed this huge black cloud moving towards the beach from the sea. And our dumbasses were like yeah we ll go to the sea when the cloud comes closer because it will be less sunny then🤡. Long story short as soon as it got cloudy we walked towards the sea and the cloud bursted into a heavy 5mins rain and we all got wet👍🏽. Got my car covered in sand and rain water. Anyways had a good time.
Today I have an evening full of free time. Planning to read some neonatology. As I said before, I feel that I have a lot of unclear topics when it comes to neonatology. I am currently reading AIIMS NICU protocols, because I feel the language used is simple and I can cover the book faster and I feel that it will be enough for my first year residency.
#phtooftheday#medstudlife#studyblr#studysthetics#neetpg#medstudynotes#neetpg2023#study mood#first aid#inicet#uworld#neonatal#neonatology#paediatrics#medical student#med student#med studyblr#medblr
6 notes
·
View notes
Text
Renander's disease: when your child's big toe causes pain
Renander's disease is a condition that affects the sesamoids of the big toe, the small bones under the head of the first metatarsal. It often appears in children around the age of 10.

What are the symptoms?
- Pain under the head of the first metatarsal, i.e. under the big toe.
- Possible lameness.
- Difficulty walking or carrying weight on the foot.
How can the diagnosis be confirmed?
X-rays show characteristic lesions on the sesamoids.
What is the treatment?
- Conservative treatment: Rest, ice, painkillers and foot orthoses to relieve the sesamoids.
- Surgical treatment: Exceptional, this may be considered in cases of persistent pain despite prolonged conservative treatment.
Go further
2 notes
·
View notes
Text
Highlights of the internship - Week 18:
• The last two days of paediatrics — FINALLY. And the start of internal medicine.
• When I said goodbye to the small surgical procedures room’s staff, they were like, “oh nooo. But we were so used to seeing you. We can gather signatures for you to keep you here ahaha.” 🥹🥹
• Going to miss only ob/gyn part of this hospital.
• At general medicine, I started in endocrinology clinic. We were supposed to get there 30 minutes earlier than the doctor and start admitting the patients, taking their history and getting them ready for the doctor. When she comes, we start admitting them together. This will be the sum of my two weeks here.
• I had the night shift of the first day. I don’t like the first day night shifts!! Nothing requiring an intern really happened so it was calm, at least.
• I got a text from my friend about our gynaecologic oncology attending. He told the nurses she and I are his favourites and firsts, the ob/gyn doctors of the future 🥹🥹🥹 stoppp 🥹🥹🥹
#medical student#medical stuff#medical school#medblr#6th year#internship#paediatrics#internal medicine#night shift memories#ob/gyn#endocrinology
6 notes
·
View notes