#Neuropathy Spectrum
Explore tagged Tumblr posts
Text
Being chronically ill is crazy because I’m essentially just living with multiple warning lights on my dashboard lit up but if an otherwise able bodied person suddenly had their body’s check engine light on they’d go into a coma
We built different
#chronically ill#chronic illness#chronic pain#costochondritis#inflammation#i’m physically disabled#pots#postural orthostatic tachycardia syndrome#fibromyalgia#hypermobility spectrum disorder#neuropathy#cold urticaria
179 notes
·
View notes
Text
Hypermobility is a spectrum disorder: its not all about subluxations!
There’s a very classic view of what hypermobility syndromes are or look like…in the case of hEDS, many joint subluxations and the like; basically, symptoms that affect joints, not taking into account a whole other range of symptoms that can often present themselves as well as, or instead of, major joint issues. Also a persistent viewpoint, maintained by GPs, that it is a rare condition (by the…

View On WordPress
#anomalous sensory experiences#articles#celiac disease#costochrondritis#dysautinomia#eye health#fibromyalgia#hEDS#Hypermobility#inflammatory bowel disease#interoception#mast cell activation syndrome#neuropathy#PoTS#spectrum conditions
22 notes
·
View notes
Text
Disabilities that You Should Consider Representing in Your Writing More… part 1
[large text: Disabilities that You Should Consider Representing in Your Writing More… part 1]
While all disabilities are underrepresented in basically all sorts of media, it’s hard to not notice the trend in what disabilities make up the majority of representation. It’s especially visible when having a blog like this, where we can see what disabilities writers even consider including in their writing, and which ones never come up.
One in four people are disabled. With eight billion people alive it means there’s a lot of disabled people, and a lot of reasons why they are disabled in the first place - but this diversity is rarely represented, even on this blog, and anyone who has been following for a while has probably noticed that fact.
To be blunt: there are disabilities other than “amputee” and “invisibly disabled mobility aid user”. Does that mean that it’s wrong to write either of those? No, and we don’t want to imply that it is. Does it mean that either of these have a lot of good representation? Absolutely not, half of all the amputee characters out there are written by people who don't seem to be even aware they're writing a disabled character. Does it mean that when you are deciding on what to give your character, you should think beyond (or along! people can be, and often are, multiply disabled!) just those two? Absolutely. Disability is a spectrum with thousands of things in it.
This is, simply, a list of common disabilities. This is just a few of them, as this is part one of presumably many (or, at least three as of right now). By “common” we rather arbitrarily decided on “~1% or more” - so at least 1 in 100 people has the disabilities below, which is a lot. Featuring!: links that you should click, sources of the % that are mostly just medical reports and might be hard to read, and quick, very non-exhaustive explanations to give you a basic idea of what these are.
Intellectual disability (about 1.5%) Intellectual disability is a condition we have written about at length before. It’s a developmental disability that affects things such as conceptualization, language, problem-solving, or social and self-care skills. ID can exist on its own or be a part of another condition, like Down Syndrome, Congenital Iodine Deficiency, or Fetal Alcohol Spectrum Disorders. This post covers a lot of basic information that you might need. We have an intellectual disability tag that you can look through!
Cancer survivors (5.4% in the US, about 0.55% worldwide) A cancer survivor is a pretty self-explanatory term. There is a lot of types of cancer and some of them are very common while others are very rare, which makes this a very diverse category. Cancers also have different survival rates. While not every survivor will have disabling symptoms, they definitely happen. Most of the long-term side effects are related to chemotherapy, radiation, and other medication, especially if they happened in children. They can include all sorts of organ damage, osteoporosis, cognitive problems, sensory disabilities, infertility, and increased rate of other cancers. Other effects include removal of the affected area, such as an eye, a spleen, breasts, or the thyroid gland, each of which will have different outcomes. Cancer, and cancer treatments, can also result in PTSD.
Diabetes (about 8.5%, ~95% of that are type 2) Diabetes is a group of endocrine conditions that cause hyperglycemia (high blood sugar) for various reasons depending on the type. The vast majority of people have type 2 diabetes, which can cause fatigue, poor healing, or feeling thirsty or hungry. A diabetic person will use insulin when needed to help manage their blood sugar levels. There are many complications related to diabetes, from neuropathy, to retinopathy, and chronic kidney disease, and there's a lot of disabilities that coexist with diabetes in general! You might want to check out the #how to write type 1 diabetes tag by @type1diabetesinfandom!
Disabling vision loss (about 7.5%) Blindness and low vision are a spectrum, ranging from total blindness (around 10% of legally blind people) to mild visual impairment. Blindness can be caused by countless things, but cataracts, refractive errors, and glaucoma are the most common. While cataracts cause the person to have a clouded pupil (not the whole eye!) blind eyes usually look average, with strabismus or nystagmus being exceptions to that fairly often (but not always). Trauma isn't a common cause of blindness, and accidents are overrepresented in fiction. A blind person can use a white cane, a guide dog or horse, or both. Assistive solutions are important here, such as Braille, screenreaders, or magnifying glasses. We have a blindness tag that you can look through, and you might want to check out @blindbeta and @mimzy-writing-online.
Psoriasis (about 2-4%) Psoriasis is a chronic skin condition with multiple subtypes; it can cause intense itching, pain, and general discomfort, and often carries social stigma. It’s an autoimmune and non-contagious disability that affects the skin cells, resulting in raised patches of flaky skin covered with scales. It often (30%) leads to a related condition, psoriatic arthritis, which causes joint pain, tenderness, and fatigue, among other things.
Stroke survivors (0.5-1%) A stroke survivor is a person who has survived any kind of stroke (ischemic, hemorrhagic, etc.). While the specific symptoms often depend on the exact location on where the stroke happened, signs such as hemiplegia, slurred speech, vision problems, and cognitive changes are common in most survivors to some degree. When someone has a stroke as a baby, or before they are born, it can result in cerebral palsy, epilepsy, and other disabilities. We have a brain injury tag that you can look through!
Noonan Syndrome (about 0.1-1% - mild is 1%, severe 0.1%) Noonan Syndrome is a disability that is almost never mentioned in any context, but certainly not around the topic of writing disabled characters. It’s a congenital condition that can cause cardiomyopathy, chronic joint pain, hypermobility, short stature, facial differences such as ptosis, autism, and various lymphatic problems among other things. Some people with Noonan Syndrome might use mobility aids to help with their joint pain.
Hyperthyroidism (about 1.2%) Hyperthyroidism is a condition of the endocrine system caused by hormone overproduction that affects metabolism. It often results in irritability, weight loss, heat intolerance, tremors, mood swings, or insomnia. Undertreated hyperthyroidism has a rare, but extremely dangerous side effect associated with it called a thyroid storm, which can be fatal if untreated.
Hypothyroidism (>5%) Hypothyroidism is an endocrine condition just as hyperthyroidism is, and it causes somewhat opposite symptoms. Due to not producing enough thyroid hormones, it often causes fatigue, depression, hair loss, weight gain, and a frequent feeling of being cold. It’s often comorbid with other autoimmune disabilities, e.g. vitiligo, chronic autoimmune gastritis, and rheumatoid arthritis. Extreme hypothyroidism can also be potentially fatal because of a condition known as Myxedema coma (or “crisis”), which is also rare.
Deafblindness (about 0.2-2%) Being DeafBlind is often considered to be an extremely rare disability, but that’s not really the case. DeafBlindness on its own isn’t a diagnosis - it can be caused by a wide range of things, with CHARGE syndrome (congenital), Usher syndrome (born deaf, becomes blind later in life), congenital rubella, and age-related deafness and blindness being some of the most common reasons. DeafBlindness is a wide spectrum, the vast majority of DeafBlind people aren’t fully blind and deaf, and they can use various ways of communication. Some of these could be sign language (tactile or not), protactile, the deafblind manual, oral speech (aided by hearing aids or not), the Lorm alphabet, and more. You can learn more about assistive devices here! Despite what various media like to tell you, being DeafBlind isn’t a death sentence, and the DeafBlind community and culture are alive and thriving - especially since the start of the protactile movement. We have a DeafBlindness tag that you can look through!
It’s probably worth mentioning that we have received little to no asks in general for almost all the disabilities above, and it’s certainly not due to what mods answer for. Our best guess is that writers don’t realize how many options they have and just end up going for the same things over and over.
Only representing “cool” disabilities that are “not too much while having a particular look/aura/drama associated” isn’t what you should aim for. Disabled people just exist, and all of us deserve to be represented, including those whose disabilities aren’t your typical “cool design” or “character inspo”, and literally all of us deserve to have good, informed representation. Sometimes we are just regular people, with disabilities that are “boring” or “too much”, and don’t make for useful plot points.
mod Sasza (with huge thank you to mod Sparrow, Rot, and Virus for their contributions with research)
#mod sasza#disabled character ideas#writing guide#writing resources#writing help#writing advice#writeblr
2K notes
·
View notes
Text
The Doctor being disabled.
Every incarnation sitting somewhere on the autism spectrum. Their stims and behaviors vary between incarnations.
First doctor with alexithymia. On Gallifrey it was fine, ignored. A "superior race" that prided itself in observation without interference doesn't put too much stalk in compassion. But meeting humans up close with Barbara and Ian started him down a path of learning to put words to his own feelings as well as others.
As his body aged he also developed arthritis. The cane was for mobility as much as it was for style. He learned the hard way that aspirin is not Gallifreyan friendly (he survived the small dose, but it scared the hell out of Susan).
Two with lots of physical stims. All his gestures and wringing his hands, grabbing onto companions.
Dyspraxic Two. Chicken scratch handwriting, stumbling over his words and his feet. He really leans into tactile sensations whether it's the texture of his clothes or holding onto a companion, it was always grounding for him.
Third tended to shut down more than his first two since the constant stress and frustration of exile had him already wound pretty tight. He'll lock himself in the lab and just put himself on autopilot until he recharges enough to deal with whatever shenanigans are happening.
Three has tinnitus that of various sounds including almost like the tardis materialization sound. He often has to look up to check if the Master is showing up to bother him or not.
Four has ADHD alongside with autism. He struggles with constantly running from responsibility and wanting to have some sense of control of situations.
It's one of those snowballs of procrastination causing anxiety which causes him to procrastinate further. Unless it's urgently life threatening, his stress response is freeze.
Five masks and suppresses his emotions in an attempt to blend with neurotypicals more since he's self-conscious of his previous "eccentricity" as Four. It causes a lot of strain between him and Tegan after Earthshock.
Peripheral neuropathy causing muscle weakness in his legs cause of the difficult regeneration. Look how much he falls over and leans on the tardis console, he can't stand straight for long periods of time without aids. Usually has braces, but will use a cane around the tardis (would use the wheelchair but it's dead in the Castrovalva river).
Six gets overstimulated easier than some, especially by noises and textures. Usually that with things not going accordingly tends to set off meltdowns. Ever since he hurt Peri he turns his energy on himself instead.
Bipolar Six. He tends to handle mania better than depression, at least when he has too much energy he knows he can spend it and try to get it out. He'll usually park the tardis somewhere his companion can enjoy and shut himself away in the cloister room or zero room when at the worst of his lows.
Also type 1 diabetic six, regenerating from poison fucked with his metabolism. He is careful to take care of his blood sugar, but he's terrible at remembering to stay hydrated. That's why Mel is always shoving carrot juice at him.
Seven has ADD (yes I know it's technically "ADHD of the predominantly inattentive type" but ADD is easier). ADD as in he's always in his own head, always five points ahead of the conversation. His train of thought is incomprehensible to most, but there is a string of logic to it.
Dyspraxic Seven with an abnormal gait and stance. Bad posture makes him look shorter than he is. Only he can read his own handwriting, which he insists is not as bad as it is.
#I'll do Eight and the rest in another post#This one is getting long#Doctor Who#Headcanons#Classic Who#First Doctor#Second Doctor#Third Doctor#Fourth Doctor#Fifth Doctor#Sixth Doctor#Seventh Doctor
791 notes
·
View notes
Note
hello this is kind of heavy and no pressure at all to answer. and apologies because im sure you must have answered this before. but do you go through like a pain management flow chart for your patients and if so what are some of the steps? my dad is having some medical issues and i want to be able to help him manage his pain as much as i can. thank you and enjoy wasteland!
I work in a hospital setting so my pain management care plan is part of an interdisciplinary team in that setting. It's relatively easy for me to get, say, IV pain meds for a patient with extreme breakthrough pain. I don't know how well my approach would translate outside of that setting, I'm not palliative care trained, and I don't personally deal with chronic or acute pain (which is why I'm answering this publicly so other people can chime in), but in broad strokes:
First: Define pain. What type of pain is it? Muscle pain? Indigestion? Neuropathy? Surgical site? Stiffness from lack of movement? Is part of the pain also the fear of the pain? Sometimes when pain has been bad for a long time, or even has been bad in a short-term but very notable way, the idea of hurting that bad again is traumatizing. That fear of pain can, unfortunately, make you focus more on the pain you're feeling because now it's not just the physical sensation of pain, it's also the psychological impact of it.
Then, how does the pain affect you? Is it stopping you from sleeping? Is it stopping you from eating? Is it making you short-tempered or depressed? Does it make it difficult to focus on things? Does it make you nauseated? Anxious? Isolated? Do you feel like you need to hide it from those who care about you?
Everything pain is and affects is a place where you can intervene. Some of these interventions will be very small and would, if they were the only intervention, feel completely inadequate. Pain relief is rarely "you do one thing and you're done." You're addressing pain on multiple fronts, and sometimes that doesn't mean your focus isn't just the reduction of pain but the restoration of what pain has taken away. It's possible the worst part of pain for you isn't the pain itself but, for example, the immobility it causes. Are there different ways you can learn to move? Can you get a grabber? Can you get a shower chair? Can you find physical therapy exercises that help you regain strength or stop you from deconditioning to the degree you're able? What mobility aids might restore movement to you?
And if returning mobility is not possible at this time or ever, how can you modify your environment to support you? Can you figure out what bothers you the most about that immobility and mitigate that? If it's annoying that not being able to leave bed makes you bored, what can be within arm's reach? If it's frustrating that being too painful to move means you feel isolated from other people, can you make wherever you are more central? If pain makes having your bed on the second floor unfeasible, can you move your bed to the first floor? How can you adapt the environment around you?
I'd encourage movement too, to the degree it is possible. Being in the same position HURTS. If it feels good to stretch but you can't do it by yourself, can someone help you with range of motion? (You can look up "passive range of motion" to get an idea of how to do that.) This doesn't need to be exercising, just exploring the joy of moving your body. Related to movement is physical touch. I love lotions and medicated creams for pain patients because you can turn them into massages. Just be careful with pressure and be open about what hurts and what feels good. At the most gentle end of the spectrum is something called the M Technique which isn't even massage, it's like guided gentle touch. Give the body something else to feel.
Different medications work better with different types of pain. This part is hard to talk about in general because of the specificity of some pain med regiments. Tylenol is great, but be cautious with how much you are taking (acetaminophen overdoses are no joke) and remember that there's a point where more tylenol doesn't mean more pain relief. Opioids are great, but they can be very dangerous and aren't well-indicated for a lot of types of chronic pain. Even if opioids work best, I'd encourage you to be working on pain reduction on multiple fronts, as opioids are so controlled, it is easy to lose access to them. If opioids give you enough pain relief to do physical therapy, then make sure to do that physical therapy. Medications are amazing and I love them and I give out PRNs like crazy, but similarly to how I can't just take my depression meds and stop being depressed, pain medication works best in conjunction with other strategies. Those other strategies though can literally be something like "tramadol takes away the pain enough I can focus on something, and what I want to do with that focus is to watch a movie I've been meaning to rewatch for a while now but haven't had the spoons for." Sometimes all you will want to do when you get pain meds is sleep because you can't when you're hurting. Sleep is wonderful; how can you arrange your sleeping place and habits to make sleeping even more of a delight?
And if you find a medication that works, use it consistently. It is always easy to keep pain level than it is to address a pain spike. Don't wait until symptoms are at their worst to address them. Figure out what it feels like when your symptoms are ramping up, and intervene early.
Sometimes medications that aren't explicitly for pain can still help. If anxiety makes pain worse, consider an anxiety medication. If coughing hurts, can you get a numbing spray from your throat to make it less sensitive so you cough less?
I don't know how useful this is to you and your family. Hopefully it's at least something to think about. Think about palliative care (which is about the management of symptoms of illnesses rather than the treatment of illnesses) as not just taking away bad sensations but restoring good ones. You can't always get someone to a place with no pain. But what can you do to enhance life in the presence of that pain? There is a psychological aspect to pain, it's a parasite that drains you and makes you feel like you are nothing but a body that hurts and won't stop hurting. I want to make clear, I'm not saying pain is only in your mind. Bone mets and nerve pain exist whether you're cheerful about it or not. But pain doesn't have to mean suffering, it doesn't have to take away the things that make you you. Address pain through medication and therapies, but also remember that protecting, promoting, and prioritizing the parts of yourself that you most value and give you the most joy will help give your life so much substance that pain can't rob it all. You aren't doing one big thing. You are doing a thousand small things that make life easier, better, more suited to yourself and your abilities, and more aligned with the parts of life that you that give your life meaning.
(And a note in particular for being the family member of someone in pain--ultimately, they are going through this alone. It is their body. What can you make smoother for them? How can you protect their dignity and their privacy without making them feel abandoned or alone? How can you make it so your reaction to their pain is not part of their burden? Like for the six hundred other hypothetical questions in this endless post, the answers will be highly personal and will take time to figure out. Be patient and calm.)
#nursing tag#oops! sorry! it’s an essay with I think no definite answers for you#and also an extrapolation of my in hospital work and my home health work#long post
154 notes
·
View notes
Text
Modern au where Leo knows asl bc he got auditory neuropathy spectrum disorder (or he is deaf) and this is really annoying and exhausting. But Jason knows cause sometimes he get in long periods of being non verbal
30 notes
·
View notes
Text
Double trouble: Hypermobility may increase Long Covid risk - Published Aug 6, 2024
“For a middle-aged woman who hasn’t had any actual injuries, I’ve had a huge amount of physical therapy,” says Liza DiLeo Thomas, a 52-year-old emergency medicine doctor in New Orleans and mom to five kids. “My neck muscles were always weak, my knees were bad. In retrospect, I was actually hypermobile, I just didn’t realize it.”
Hypermobility is a catch-all term for a spectrum of disorders characterized by joints capable of moving beyond the normal range of motion, often due to abnormalities in connective tissue. The most common of these disorders, which range from mild to severe, is known as Hypermobile Ehlers Danlos Syndrome (HEDS).
HEDS seems to be more common in women and also may be connected to some cases of Long Covid. A recent study found that people with the condition were 30% more likely not to have recovered fully from Covid-19 infection, based on symptom surveys.
“I got my first Covid infection in March of 2020,” Thomas told The Sick Times. “After [my] second infection, I never recovered.”
Thomas has not been able to return to work in the ER. Worse still, her kids brought home more Covid-19 infections, and each reinfection over the course of the next three years triggered novel, debilitating symptoms, such as painful skin rashes and mild myelitis, an inflammation of the spinal cord. “I believe I’ve had Covid a total of five times,” she said.
In April 2021, she ended up at the office of Tulane University School of Medicine neurologist Michele Longo, who was helming a new Long Covid clinic. Longo and her colleagues have discovered that vulnerability to Long Covid may sometimes be linked to hypermobility.
Longo referred Thomas to multiple specialists, including Dr. Jacques Courseault, founder of Tulane’s specialty hypermobility clinic, launched in 2022. It is one of the few of its kind in the world. Collaboration between that clinic and Longo’s Long Covid clinic has yielded novel clues to the connection between the two conditions.
“The specialist at the clinic pushed along my iliotibial band and other parts of my leg,” recalled Thomas. “And he said, ‘Your muscle pain is not due to muscle damage. You’re hypermobile.’” Muscles will chronically contract to stabilize weak joints in hypermobile individuals, leading to chronic pain.
That insight gave clues to what might be off balance in Thomas’ body, and pointed the way for treatments that helped improve her function, including antihistamines, low-dose naltrexone, and lots of saltwater to help increase blood volume, as she was later diagnosed with dysautonomia and small fiber neuropathy. With her condition better managed, she now works part-time for the same hospital in an administrative role, mostly from home.
How a connective tissue disorder might increase risk of Long Covid Longo, the Tulane neurologist, is the kind of doctor who listens closely to her patients
“My migraine headaches brought me to neurology as a profession,” she told The Sick Times. “I’ve been living my whole life in that space of having a chronic condition that does not have a biomarker. That lends itself very well to believing my patients and empathizing with them.”
Early in the pandemic, she started seeing chronically ill individuals who were much younger than her typical patient, and who had not recovered from an acute Covid-19 case.
At her Long Covid clinic, she began to notice that some of her patients were hypermobile. She diagnosed them via the traditional Beighton scoring system — a simple in-office test which checks the flexibility of joints such as the fingers, elbows, knees, and spine. Then, she sent them over to the EDS clinic, where Courseault inevitably confirmed her suspicion. “Every patient I sent him was indeed hypermobile,” she said.
This past April, Longo and colleagues published a report on five hypermobile females with Long Covid aged 33 to 51. Once diagnosed and treated at the EDS clinic for common issues associated with hypermobility, they began to see some improvements. Longo and colleagues are now putting together a case series on fifty patients.
Read the rest at either link!
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#still coviding#public health#wear a respirator#long covid
14 notes
·
View notes
Text
State: I am old, fat and (deservedly) unloved. The diagnosed ADHD does not respond go treatment, and the highly probable position somewhere on the spectrum doesn't help. Peripheral neuropathy is worsening, taking with it my fine motor skills, balance and sense of touch. I'm avoiding opioids as long as possible for the nerve pain, so I avoid the addiction both my parents died with. Current painkiller has side effects not quite a bad. Burns and small cuts are almost daily, and if I don't stop using power tools I'm going to lose an appendage. If I don't die tripping down yet another flight of stairs. I seem to be progressing at the same rate as my dad did with memory-problems-leading-to-dementia, just at an age 20 years younger than he did. So, fifteen years tops until I'm in memory care.
Plan: Well, I'm off to school to try to train to make the world a better place, if I still can, before I die.
4 notes
·
View notes
Text
Diabetes

Introduction to Diabetes
Diabetes, a metabolic disorder characterized by chronic hyperglycemia, arises from abnormalities in insulin secretion, insulin action, or both. The condition’s prevalence has reached epidemic proportions globally, with significant health, economic, and social implications.
Types of Diabetes
Type 1 Diabetes: This autoimmune disease results from the destruction of pancreatic beta cells, leading to absolute insulin deficiency. Genetics and environmental triggers play pivotal roles in its pathogenesis. Despite being less common than Type 2 diabetes, its onset during childhood or adolescence significantly impacts individuals’ lives.
Type 2 Diabetes: Predominantly a disorder of insulin resistance, Type 2 diabetes accounts for the majority of diabetes cases worldwide. Lifestyle factors, genetic predisposition, and obesity contribute to its development. Its insidious onset often leads to delayed diagnosis and increased risk of complications.
Gestational Diabetes: Occurring during pregnancy, gestational diabetes poses risks to both maternal and fetal health. Hormonal changes and insulin resistance characterize its pathophysiology. Effective screening and management are crucial to prevent adverse outcomes.
Other Types of Diabetes: Variants like MODY, LADA, and secondary diabetes present unique challenges in diagnosis and management, requiring tailored approaches to care.
Epidemiology and Prevalence
Diabetes prevalence varies across demographics, with disparities observed in age, gender, ethnicity, and socioeconomic status. The escalating burden of diabetes underscores the urgent need for targeted prevention and management strategies.
Symptoms and Causes

Hyperglycemia-induced symptoms like polyuria, polydipsia, and unexplained weight loss serve as clinical indicators for diabetes diagnosis. Understanding the complex interplay of genetic, environmental, and lifestyle factors elucidates the condition’s etiology.
Complications
Diabetes complications encompass a spectrum of microvascular and macrovascular disorders, significantly impacting quality of life and life expectancy. From diabetic retinopathy to cardiovascular disease, nephropathy, neuropathy, and diabetic foot complications, the ripple effects of uncontrolled diabetes are profound.
Diagnosis and Tests

Accurate diagnosis relies on comprehensive evaluation, including fasting glucose, oral glucose tolerance tests, and hemoglobin A1c measurements. Screening recommendations aim to identify at-risk individuals early, facilitating timely intervention and risk reduction.
Management and Treatment
Diabetes management strategies encompass pharmacotherapy, lifestyle modifications, patient education, and multidisciplinary care. Individualized treatment plans address glycemic control, blood pressure management, lipid optimization, and prevention of complications.
Prevention
Prevention initiatives target modifiable risk factors through health promotion, public health interventions, and community engagement. Emphasizing the role of nutrition, physical activity, and behavioral changes empowers individuals to mitigate their diabetes risk.
Outlook and Prognosis
Prognostic factors such as glycemic control, adherence to therapy, comorbidity burden, and psychosocial support influence long-term outcomes. Enhanced collaboration among healthcare providers, policymakers, and stakeholders is essential to improve diabetes prognosis globally.
Living With Diabetes

Coping with diabetes requires resilience, self-management skills, and social support networks. Empowering individuals through education, self-monitoring tools, and peer support enhances their capacity to navigate the challenges of daily diabetes management.
Impact on Individuals and Society
Diabetes exerts a profound socioeconomic burden, encompassing healthcare costs, productivity losses, and reduced quality of life. Addressing the psychosocial dimensions of diabetes care is integral to fostering holistic well-being and societal resilience.
Future Directions and Research

Advancements in diabetes research, including precision medicine, digital health technologies, and novel therapeutics, offer promising avenues for disease management and prevention. Collaborative research endeavors aim to translate scientific discoveries into tangible clinical benefits.
Conclusion
In conclusion, diabetes represents public health challenge necessitating a comprehensive, patient-centered approach. By fostering awareness, promoting early detection, and advancing evidence-based interventions, we can mitigate the impact of diabetes on individuals, families, and communities worldwide.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at [email protected] for assistance.
#assignment help#healthcare#medical students#nursing student#nursing school#medical school#medical student#medicine#health tips#health and wellness#health#health & fitness#diabetes#diabetic#medical help#medical assistance#pharmacy student#pharmacy technician#homework help#academic assignments#expert assignment writers
2 notes
·
View notes
Text
Unlock Your Brain's Potential: Expert Neurological Care in Aurangabad

Your nervous system is the command center of your body, orchestrating everything from your simplest movements to your most complex thoughts and feelings. When neurological issues arise, impacting memory, mobility, sensation, or clarity, seeking the expertise of the best neurologist in Aurangabad is a crucial step towards regaining control and well-being.
At www.akashkharat.hhcldoctorsites.com, we are dedicated to providing comprehensive and cutting-edge care for a wide spectrum of neurological disorders. Our clinic has earned a reputation as a trusted center for advanced neurological disorders treatment in Aurangabad, driven by our commitment to a patient-centric approach and the deep expertise of our specialists.
Understanding the Role of Your Neurologist in Aurangabad
A neurologist in Aurangabad is a highly trained medical professional specializing in the diagnosis and treatment of conditions affecting your brain, spinal cord, and intricate network of nerves. From common ailments like debilitating migraines to complex neurodegenerative diseases such as Alzheimer's and Parkinson's, our neurologists possess the knowledge and skills to provide accurate diagnoses and tailored treatment plans. We commonly address conditions such as:
· Epilepsy and various seizure disorders
· Stroke and its resulting paralysis
· Alzheimer's disease and other forms of dementia
· Multiple sclerosis and other demyelinating diseases
· Peripheral neuropathy and muscle weakness
· Migraines and other chronic headache disorders
Timely and accurate diagnosis, coupled with evidence-based treatment, is paramount in improving the long-term outcomes and enhancing the quality of life for individuals facing these challenges.
Why Our Clinic Stands Apart for Neurological Care
Choosing our clinic means entrusting your care to a team that blends advanced medical technology with genuine compassion. We pride ourselves on collaborating with some of the most accomplished neurologists and neurosurgeons in Aurangabad, ensuring that you receive personalized and highly effective care at every stage.
Our commitment to excellence is reflected in:
State-of-the-art diagnostic capabilities: We utilize cutting-edge imaging and neurophysiological testing to ensure precise and timely diagnoses.
Individualized treatment strategies: We develop customized medication regimens and therapeutic interventions tailored to your specific condition and needs.
Comprehensive neuro-rehabilitation and follow-up: Our care extends beyond initial treatment, focusing on long-term recovery and improved function.
Integrated surgical expertise: When surgical intervention becomes necessary, our skilled neurosurgeon in Aurangabad provides seamless and expert care, from intricate brain surgeries to complex spinal procedures, prioritizing patient safety and optimal recovery.
Your Destination for Neurological Disorders Treatment in Aurangabad
Finding reliable and comprehensive neurological disorders treatment in Aurangabad is now within your reach. Our clinic offers the unique advantage of integrating expert neurology and neurosurgery services under one roof. This streamlined approach ensures seamless transitions between diagnostic evaluations, medical management, and surgical interventions when required, providing a holistic and patient-centered experience.
We understand the profound impact that neurological conditions can have on your life and are dedicated to providing unwavering support throughout your journey. Our ultimate goal is to alleviate your symptoms, restore lost function, and empower you to live a fuller, more meaningful life.
Take the First Step Towards a Healthier Nervous System
Don't let neurological symptoms dictate your life. If you or a loved one is experiencing concerning signs such as persistent dizziness, unexplained memory loss, recurrent seizures, or progressive muscle weakness, we urge you to seek expert neurological evaluation without delay. Visit www.akashkharat.hhcldoctorsites.com today to schedule your consultation with the best neurologist in Aurangabad. Take proactive control of your neurological health—because a healthy brain is the foundation for a vibrant life.
#brain and spine hospital aurangabad#best spine specialist aurangabad#brain specialist aurangabad#best neurosurgeon in aurangabad#best neurologist aurangabad#neurologist in aurangabad#neurosurgeon aurangabad#brain specialist hospital in aurangabad#brain and spine neuro clinic in aurangabad#spine specialist aurangabad
0 notes
Text
Why Are More People Facing Hearing Issues Today?

One of the most important senses is the sense of hearing. It helps us connect to the world around us. We use our ears everyday in all spheres of our life, may it be for listening to our favorite music, talking with friends and families, watching movies and taking in the sounds of nature. However, a growing number of people are dealing with hearing issues in the modern environment. The elderly are no longer the only ones who face this problem. Hearing loss affects even young people, teens, and toddlers. Why is this taking place? What are our options? Let's examine the reasons for hearing loss and simple, straightforward ways to avoid it.
What is Hearing Loss?
Hearing loss means not being able to hear as well as someone with normal hearing. It can happen in one ear or both. Sometimes it comes on slowly, and sometimes it can happen all of a sudden. The level of hearing loss can range from mild to complete deafness.
There are four main types of hearing loss:
Conductive Hearing Loss: This happens when sounds cannot pass through the outer or middle ear properly. It might be caused by earwax, infection, or a problem with the ear bones.
Sensorineural Hearing Loss: This is the most common type. It happens due to damage in the inner ear or hearing nerve. It is usually permanent.
Mixed Hearing Loss: This is when both conductive and sensorineural hearing loss are present.
Auditory Neuropathy Spectrum Disorder (ANSD): A condition where the inner ear and auditory nerve function normally, but there is a problem with the transmission of signals to the brain.
Why Are Hearing Problems Increasing in the Modern World?
There are several reasons why more individuals are experiencing hearing problems in the fast-paced world of today. Given below are some of the major reasons:

Read More:
0 notes
Link
Abstract
Purpose
Peripheral neuropathies with autonomic nervous system involvement are a recognized cause of gastrointestinal dysmotility for a wide spectrum of diseases. Recent advances in wireless motility capsule testing allow improved sampling of regional and whole gut motility to aid in the diagnosis of gastrointestinal motility disorders and may provide additional insight into segment-specific enteric involvement of peripheral neuropathies affecting autonomic nervous system function.
Methods
We utilized standardized autonomic nervous system (ANS) reflex assessment and wireless motility capsule testing to evaluate 20 individuals with idiopathic autonomic neuropathy and unexplained gastrointestinal symptoms. Additionally, we examined the relationship between quantifiable autonomic neuropathy and gastrointestinal dysmotility at specific neuroanatomical levels. Symptom profiles were evaluated using the 31-item Composite Autonomic Symptom Score questionnaire (COMPASS-31) and compared to wireless motility capsule data.
Results
We found that transit times were predominately abnormal (delayed) in the foregut (10 of 20; 50%), while contractility abnormalities were far more prominent in the hindgut (17 of 20; 85%), and that motility and symptom patterns, as assessed by the COMPASS-31 GI domain items, generally corresponded. Finally, we also found that there was neuroanatomical overlap in the presence of autonomic reflex abnormalities and WMC-based transit and/or contractility abnormalities.
Conclusions
We found that transit times were predominately abnormal in the foregut and midgut, while contractility abnormalities were far more prominent in the hindgut in individuals with idiopathic autonomic neuropathy. There was a high rate of agreement in segmental wireless motility capsule data with neuroanatomically corresponding standardized ANS function measures (e.g., cardiovagal, sudomotor, adrenergic). Expanded sudomotor testing, including additional neuroanatomical segments, could provide additional indirect assessment of visceral involvement in ANS dysfunction.
0 notes
Text
Mitochondrial Dysfunction in Primary Mitochondrial Disease
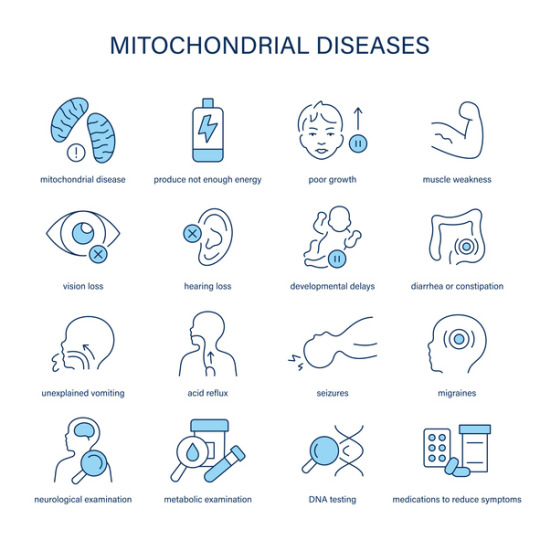
Introduction
Primary Mitochondrial Disease (PMD) refers to a group of genetic disorders resulting from defects in mitochondrial function. Mitochondria play a crucial role in energy production through oxidative phosphorylation (OXPHOS), and their dysfunction leads to a wide spectrum of clinical manifestations affecting multiple organ systems. PMD primarily arises from mutations in mitochondrial DNA (mtDNA) or nuclear DNA (nDNA) encoding mitochondrial proteins, resulting in impaired energy metabolism and increased cellular stress.
Pathophysiology of Mitochondrial Dysfunction
Mitochondrial dysfunction in PMD is primarily caused by defects in the electron transport chain (ETC), which is responsible for ATP synthesis. The ETC comprises five protein complexes embedded in the inner mitochondrial membrane. Mutations affecting these complexes disrupt ATP production, increase the production of reactive oxygen species (ROS), and lead to metabolic imbalances such as lactic acidosis.
Complex I (NADH: ubiquinone oxidoreductase) and Complex IV (cytochrome c oxidase) deficiencies are among the most common defects in PMD. These impairments reduce the efficiency of ATP production, leading to an energy crisis in high-demand tissues such as the brain, muscles, and heart. Additionally, defects in mitochondrial dynamics, including fission and fusion processes, further contribute to cellular dysfunction.
Genetic and Biochemical Basis
PMD is genetically heterogeneous, with mutations in over 350 known genes. These mutations can be inherited in a maternal, autosomal recessive, or dominant manner. Some commonly affected genes include:
MT-ND genes (encoding Complex I subunits)
SURF1 gene (involved in Complex IV assembly)
POLG gene (critical for mtDNA replication and maintenance)
PDHA1 gene (encoding a subunit of the pyruvate dehydrogenase complex)
Mutations in these genes impair the synthesis of key mitochondrial components, leading to energy production failure, oxidative stress, and apoptotic signaling.
Impact on the Nervous System
The nervous system is highly dependent on mitochondrial energy production, making it particularly susceptible to dysfunction. Mitochondrial defects in PMD often manifest as progressive neurodegenerative disorders, including:
Developmental delay and cognitive impairment
Seizures and epilepsy
Hypotonia and muscle weakness
Ataxia and movement disorders
Peripheral neuropathy
Histopathological findings in affected individuals often reveal spongiform degeneration, gliosis, and neuronal loss, particularly in the basal ganglia, cerebellum, and brainstem. These changes contribute to progressive neurological decline.
Effects on Other Organ Systems
Beyond the nervous system, mitochondrial dysfunction in PMD affects multiple organs due to the ubiquitous need for ATP. Key systemic manifestations include:
Musculoskeletal System: Myopathy, exercise intolerance, and rhabdomyolysis are common due to inadequate ATP supply for muscle contraction and maintenance.
Cardiovascular System: Cardiomyopathy, conduction abnormalities, and arrhythmias result from mitochondrial defects in cardiac muscle, leading to impaired contractility and electrical activity.
Metabolic System: Lactic acidosis and metabolic decompensation occur due to defective oxidative metabolism, leading to systemic energy deficits.
Gastrointestinal System: Dysmotility, feeding difficulties, and pancreatic dysfunction are observed, contributing to malnutrition and failure to thrive.
Endocrine System: Mitochondrial dysfunction affects hormone-producing glands, resulting in diabetes, hypothyroidism, and adrenal insufficiency.
Cellular and Molecular Consequences
Mitochondrial dysfunction in PMD leads to several cellular-level consequences, including:
Increased ROS production, causing oxidative stress and damage to lipids, proteins, and DNA.
Dysregulation of apoptosis, leading to premature cell death and tissue degeneration.
Defective calcium homeostasis, impairing neuronal and muscular function.
Impaired mitochondrial biogenesis, reducing the ability of cells to compensate for energy deficits.
Conclusion
Primary Mitochondrial Disease is a complex, multisystem disorder driven by genetic defects in mitochondrial function. The resulting energy production failure impacts the nervous, muscular, cardiovascular, metabolic, and endocrine systems, leading to severe clinical manifestations. Understanding the molecular and biochemical mechanisms underlying PMD is crucial for advancing diagnostic and research efforts. Continued investigation into mitochondrial biology and genetic contributors will enhance our knowledge of this debilitating disease.
#Mitochondrial#Dysfunction#PMD#Energy#Production#System#Defects#Complex#Leading#Mutations#ATP#These#Disease#Genetic#Resulting#Oxidative#Metabolic#Genes#Nervous
0 notes
Text
neuro surgery hospital in sector 70
Best Neurosurgery Hospitals in Sector 70: Comprehensive Guide to Expert Care for Neurological Conditions
Neurosurgery is a highly specialized field of medicine that involves the diagnosis, treatment, and surgical intervention of conditions affecting the brain, spine, and nervous system. Given the complexity of these conditions, it is crucial to seek expert care from top-rated neurosurgery hospitals to ensure the best possible outcomes. Sector 70, a rapidly developing area, is home to some of the best neurosurgery hospitals that provide cutting-edge technology and skilled professionals to cater to a wide variety of neurological issues.
This article will explore some of the leading neurosurgery hospitals in Sector 70, highlighting their expertise, facilities, and commitment to providing high-quality care to patients suffering from neurological disorders.
Why Choose a Specialized Neurosurgery Hospital?
Neurosurgical procedures are intricate and require highly skilled professionals, advanced equipment, and well-equipped facilities. Here are a few reasons why selecting the right neurosurgery hospital is critical:
Specialized Expertise: Neurosurgeons are highly trained professionals who specialize in surgeries of the brain, spine, and peripheral nervous system. They possess the expertise to treat a range of conditions from traumatic brain injuries to complex spinal surgeries.
Advanced Diagnostic Tools: The best neurosurgery hospitals are equipped with state-of-the-art diagnostic tools like MRI, CT scans, and electrophysiological monitoring, which help in the accurate diagnosis of neurological conditions and the planning of effective treatment.
Comprehensive Treatment Options: Specialized neurosurgery hospitals offer a full spectrum of care, from non-surgical treatments like physiotherapy and medication to complex surgeries like tumor removal or spinal fusion.
Post-Surgical Care: Recovery after neurosurgery can be challenging, and it is essential to have access to comprehensive post-operative care. Hospitals in Sector 70 offer specialized neuro-rehabilitation services, ensuring patients recover effectively and regain optimal functionality.
Patient-Centered Care: Renowned hospitals in Sector 70 focus on providing personalized care. They take the time to understand each patient’s needs, concerns, and treatment preferences, ensuring that every individual receives the best possible care suited to their condition.
Key Neurological Conditions Treated at Neurosurgery Hospitals
Neurosurgery hospitals in Sector 70 offer treatment for a variety of neurological conditions, including but not limited to:
Brain Tumors: Removal of malignant and benign tumors, including gliomas, meningiomas, and pituitary tumors.
Spinal Disorders: Treatment for conditions like herniated discs, spinal stenosis, scoliosis, and fractures of the spine.
Traumatic Brain Injuries (TBI): Surgical and non-surgical treatment for patients suffering from head injuries, skull fractures, and intracranial hemorrhage.
Epilepsy: Surgical interventions for patients with intractable epilepsy, including resective surgeries and deep brain stimulation.
Neurovascular Disorders: Treatment for conditions such as aneurysms, arteriovenous malformations, and stroke.
Spinal Cord Injuries: Surgical interventions to manage and treat spinal cord injuries resulting from trauma or disease.
Peripheral Nerve Disorders: Treatment for conditions affecting peripheral nerves, such as carpal tunnel syndrome, brachial plexus injuries, and peripheral neuropathy.
Top Neurosurgery Hospitals in Sector 70
The following hospitals in Sector 70 are known for their exceptional neurosurgical care. These hospitals provide cutting-edge treatment options, experienced neurosurgeons, and modern infrastructure to ensure the best possible outcomes for patients.
1. Neuro Care Hospital
Specialization: Comprehensive Neurosurgery and Neurology Services Neuro Care Hospital is one of the most renowned neurosurgery centers in Sector 70. It specializes in a wide array of neurological conditions, from brain and spinal disorders to vascular abnormalities. The hospital is known for its multidisciplinary approach, offering comprehensive care to patients requiring neurosurgery, neuro-rehabilitation, and post-operative care.
Why Choose Neuro Care Hospital:
State-of-the-Art Facilities: The hospital is equipped with advanced diagnostic tools like MRI, CT scanners, and neuro-navigation systems, ensuring accurate diagnosis and treatment planning.
Highly Experienced Neurosurgeons: The team consists of board-certified neurosurgeons with years of experience in handling complex neurological cases.
Minimally Invasive Surgeries: Neuro Care Hospital offers minimally invasive techniques for conditions like spinal stenosis and herniated discs, ensuring faster recovery and minimal scarring.
Comprehensive Rehabilitation: In addition to surgery, the hospital offers extensive rehabilitation services to aid recovery after neurosurgical procedures.
Patient Testimonials: Patients have praised the hospital for its high-quality care, skilled surgeons, and excellent patient management. The hospital’s emphasis on post-operative care ensures patients recover with minimal complications.
2. Sector 70 Neuro Surgery & Spine Centre
Specialization: Advanced Spine and Brain Surgery Sector 70 Neuro Surgery & Spine Centre is known for its advanced approach to spinal and brain surgery. The hospital is equipped with the latest surgical tools and offers a range of services to treat conditions such as spinal cord injuries, brain tumors, and degenerative spine diseases.
Why Choose Sector 70 Neuro Surgery & Spine Centre:
Expertise in Spinal Surgery: The center is well-known for its expertise in treating spinal disorders, including disc replacements, spinal fusion, and scoliosis correction.
Advanced Neurosurgical Techniques: The center uses cutting-edge technologies such as 3D imaging, robotic surgery, and intraoperative neuro-monitoring to improve surgical precision.
Personalized Treatment Plans: Surgeons at the center develop individualized treatment plans based on the specific needs of each patient.
Post-Operative Care: The hospital’s dedicated neuro-rehabilitation team ensures that patients have access to therapy and support during their recovery.
Patient Testimonials: Patients have lauded the hospital for its skilled neurosurgeons, effective surgical techniques, and exceptional post-operative care. Many patients report a quick recovery and a noticeable improvement in their quality of life.
3. Brain and Spine Institute
Specialization: Brain Tumor Surgery, Epilepsy Surgery, Spinal Cord Injury Brain and Spine Institute in Sector 70 is a premier facility specializing in both brain and spine surgeries. The hospital boasts a team of expert neurosurgeons and neurologists who work together to provide comprehensive care to patients with brain tumors, traumatic brain injuries, epilepsy, and other neurological disorders.
Why Choose Brain and Spine Institute:
Multidisciplinary Team Approach: The hospital offers a team of neurosurgeons, neurologists, oncologists, and rehabilitation specialists who work collaboratively to deliver the best treatment for complex neurological conditions.
Brain Tumor and Epilepsy Surgery: The hospital is renowned for its success in performing delicate surgeries to remove brain tumors and treat epilepsy.
Spinal Disorders Expertise: The hospital offers expert treatment for a range of spinal issues, including scoliosis, herniated discs, and spinal fractures.
Comprehensive Support Services: The hospital also provides psychological counseling, pain management, and physical therapy, ensuring that patients receive holistic care.
Patient Testimonials: Patients often praise the hospital’s ability to handle complex neurological conditions and provide detailed explanations of treatment options. Many patients have also mentioned the supportive and caring nature of the hospital’s staff.
4. Sanskriti Neuro Center
Specialization: Neurovascular and Minimally Invasive Neurosurgery Sanskriti Neuro Center is a leading hospital in Sector 70 for patients needing treatment for neurovascular disorders, such as aneurysms, strokes, and arteriovenous malformations. The center is known for its minimally invasive techniques and high success rates in treating brain and spinal conditions.
Why Choose Sanskriti Neuro Center:
Advanced Neurovascular Care: The center offers cutting-edge treatments for conditions like brain aneurysms and strokes, using minimally invasive endovascular techniques.
Minimally Invasive Surgery: Sanskriti Neuro Center is committed to reducing patient recovery time by employing minimally invasive surgical techniques, which often result in smaller incisions and less post-operative pain.
Integrated Care: The hospital offers integrated care that includes diagnostic services, surgical procedures, post-operative rehabilitation, and long-term follow-up.
Patient Testimonials: Patients have spoken highly of the center’s ability to provide quick and effective treatment for life-threatening conditions like strokes and aneurysms. Many appreciate the compassionate care and thorough communication from the team.
5. Advanced Neurosurgery Centre
Specialization: Pediatric Neurosurgery and Brain Surgery Advanced Neurosurgery Centre in Sector 70 is known for its pediatric neurosurgery division, specializing in treating children with neurological conditions. The center also provides exceptional care for adults with brain and spinal disorders.
Why Choose Advanced Neurosurgery Centre:
Pediatric Neurosurgery: The center has a team of specialists who are skilled in treating children with conditions such as hydrocephalus, brain tumors, and congenital spinal disorders.
Adult Brain and Spine Surgery: The hospital offers comprehensive services for adults, including brain tumor surgeries, spine surgeries, and spinal cord injury treatment.
Family-Centered Care: The hospital places a strong emphasis on involving families in the treatment and recovery process, especially in pediatric cases.
Patient Testimonials: Parents of pediatric patients have highly praised the hospital for its compassionate care and the expertise of the surgeons. Adult patients have also reported excellent outcomes and high satisfaction with the care provided.
Conclusion: Choosing the Right Neurosurgery Hospital in Sector 70
Selecting the right neurosurgery hospital is critical to achieving successful outcomes for complex neurological conditions. Whether you need brain tumor surgery, spinal cord treatment, or trauma care, Sector 70 offers a variety of top-rated hospitals with highly experienced neurosurgeons and state-of-the-art facilities.
When choosing a neurosurgery hospital, it’s essential to consider factors such as the hospital’s expertise in the specific condition you are dealing with, the technologies and procedures they offer, and their approach to post-operative care. By choosing a reputable hospital in Sector 70, you can be confident that you are receiving the best possible care for your neurological health.
0 notes
Text
Diabetes Management Early Detection and Management of Diabetic Neuropathy in a Clinical and Homecare Setting The objective of this study is to examine early detection and management of diabetic neuropathy in a clinical and homecare setting and specifically through examination of articles published after 2002. The information from each source will be summarized listing the strengths and weaknesses of each article in separate paragraphs. As well, this work will utilize table or graphs to present the findings. O'Reilly, Caryl Ann (2005) Managing the Care of Patients with Diabetes in the Home Care Setting, Diabetes Spectrum, July 2005. Vol. 18. No. 3. Retrieved from: http://spectrum.diabetesjournals.org/content/18/3/162.full The work of O'Reilly (2005) reports that more patients than ever before are released earlier from hospitals and rehabilitation center and that those with diabetes are included in this trend. Diabetes is reported to be ranked second following congestive heart failure as the primary diagnosis at the time of entry into home care. The home health care nurse role is growing in importance with patients being discharged early from hospitals and rehabilitation center as this makes a requirement of nursing management at home that is more sophisticated in nature. In fact, as noted by O'Reilly "These nurses are often the only professional who has a complete overview of a patient's medical regimen and, therefore, responsibility for the coordination of care." (2005) In addition home health care nurses serve as the liaison between health care team member, family members, caregivers and patients. Home care agencies are the point of referral for acute episodes of care and these agencies use the Outcome and Assessment information Set (OASIS) for determining the needs of patients. 2. McLaughlin, Sue (2005) From Research to Practice/Diabetes Care in Special Settings: Meeting the Challenges: Diabetes Care in Special Settings Diabetes Spectrum July 2005 18:143-145. Retrieved from: http://www.vnsny.org/research/projects/1_implemetation.html McLaughlin (2005) writes that the number of individuals in the home care setting receiving care for diabetes is growing rapidly. Proper management is stated to require that patients "understand the complexities of the disease, manage their diet, adhere to medication regimens and make other lifestyle changes." McLaughlin reports a study with the purpose of determining if an evidence-based quality improvement strategy would help elderly, homebound persons with diabetes in home care achieve better control of blood glucose levels; increase confidence in their ability to take medications as prescribed and manage their diabetes; and reduce their emergency department use." The study is reported to build on the design of the Implementation and Evaluation of Health Outcomes Management and Evaluation (HOME) Plans for Home Health Patients with Congestive Heart Failure's project and represents Phase II of this effort. Home health care nurses were randomly assigned to the intervention group (n=143) or the control group (n=126). Nurses in the intervention group received training on how to help patients improve their ability to take medications as prescribed. Use was a specialized assessment of patients' knowledge about diabetes medication management and provided patient education where necessary. Nurses also helped patients set goals for adherence to medication regimens, and patients received telephone support for 12 weeks to help them achieve these goals. Nurses in the control group provided usual care. All patients received care from the Visiting Nurse Service of New York." Findings in the study state that compared with patients that received usual care, patients in the intervention group "had a small but significant reduction in blood glucose levels. Patients in the intervention group reported more confidence in their medications as prescribed but they expressed more doubt about their ability to manage their diabetes in general." There was reported to be no significant difference in the use of the emergency room department between the two groups. The study concluded that an intervention that is evidence-based to improve adherence to diabetes medication regimens for patients who are elderly and homebound is one that is feasible and that can produce desired results. 3. Chavis, Selena (2010) No Better Time for Telehealth. For the Record, 1 Mar 2010. Vol. 22, No. 4. Retrieved from: http://www.fortherecordmag.com/archives/030310p20.shtml The work of Chavis (2010) reports a study referred to as the DREME study in which 172 patients were diagnosed with diabetes. The participants ranged in age from 18 to 64 years of age and were chosen for the six-month study starting in April 2008. The remote monitoring process was comprised by a cell phone, a glucometer marketed by SymCare, and a Bluetooth cradle. The study is reported to have centered around "patient satisfaction with disease management services and changes in glycemic control." ( ) Outcomes reported by the study include that outcomes "…revealed significant improvements in both areas." ( ) Of the 172 participants, 87 participated as standard disease management patients (DM-Standard) and 85 participated as disease management patients with remote monitoring (DM-Plus). Compared with DM-Standard, the DM-Plus group reported greater satisfaction with their disease management experience in terms of believing program staff were helpful, articulate, better educated, and accessible. The results also showed the DM-Plus group improved self-care and had more stable glycemic control. 4. Isaac, Jennifer (nd) Remote Monitoring Reduces Hospitalizations, Improve Nurse Productivity. Edge Runners. Date Unknown. Retrieved from: http://www.aannet.org/files/public/PresbyterianHomeHealthcare_template.pdf The work of Isaac reports a system in which the patients are referred through various sources, including a review of new hospital admissions that identifies patients with specific diagnoses. The study design is such that the telehealth RN visit the patient once or twice weekly, providing services similar to what a home visit nurse would provide -- checking vital signs, providing condition-related education and ensuring adequate self-care. Furthermore, the nurse conducted a review of the equipment to ensure it was working properly. Telehealth services are stated to generally continue for 6-8 weeks, monitoring services may continue for patients who are officially discharged from home care (and therefore no longer receive in home visits) but who could benefit from additional monitoring and education. Additionally, telehealth patients are asked to measure their vital signs, weight and oxygen saturation levels routinely. The telehealth software records these results and prompts patients to answer specific questions. Data was sent to a Web site for the telehealth RN for review and in the alert the RN of any matter needing attention. RN calls patients when alerted, or if patients do not enter information on a routine basis. RNs can perform additional assessments in response to the daily assessment data through a phone call. Study findings show that the telehealth system has "…contributed to reduction in hospitalization rates among congestive heart failure patients, from 19% to 12.2% at the end of 2007. During the first quarter of 2008, the CHF hospitalization rate for telehealth patients dropped to 8%." ( ) In addition, the telehealth system has enhanced productivity; the patient load for telehealth RN is higher than that of visiting home health nurses. Telehealth RNs can conduct 6-8 visits per day, versus 5 for home health nurses, by eliminating travel time to remote areas. The system has enhanced RN productivity; the patient load for telehealth RNs is higher than that of visiting home health nurses. Telehealth RNs can conduct 6-8 visits per day, versus 5 for home health nurses, by eliminating travel time to remote areas. There is a savings of approximately $4,900-$8,000 is saved for each CHF hospitalization prevented, given an estimated 3- to 5-day length of stay. Surveys of participating patients indicate satisfaction rates of 96% with the telehealth service and Presbyterian Home Healthcare has a dedicated staff for the Telehealth Department of 2.3 staff nursing FTEs and a technician who deals with all installs and troubleshooting. The work of Stachura and Dhasanshina (nd) reports that a study was conducted examining the benefits of technology for use in intensive blood glucose management and reports a randomized trials and meta-analyses conducted by Canadian researchers for determining where use of technologies can improve glycemic control or that of blood sugar control in Type 1 DM patients. The report states that the researchers used "wire telephone modem communication between patients' homes and a research computer. In a randomized trial of patients on an intensive insulin regimen that initially had failed to achieve glycemic control, the researchers found better overall glycemic control in patients receiving multiple daily insulin injections or continuous subcutaneous insulin infusion. Telehomecare enhanced adherence to self-monitoring, which is essential for achieving glycemic control. Meta-analyses showed that telehomecare was equivalent to intensive usual care (pooled HbA1c change from baseline: mean difference 0.2%, 95% Confidence Interval -- 0.2 to 0.6%)." (Stachura and Dhasanshina, nd) Video conferencing and data collection from glucose meters were install the homes of all patients. Population Intervention Comparison Outcomes Nurses received training on how to help patients improve their ability to take medications as prescribed. Use was a specialized assessment of patients' knowledge about diabetes medication management and provided patient education where necessary. Nurses also helped patients set goals for adherence to medication regimens, and patients received telephone support for 12 weeks to help them achieve these goals. Nurses in the control group provided usual care. All patients received care from the Visiting Nurse Service of New York. Small but significant reduction in blood glucose levels. Patients in the intervention group reported more confidence in their medications as prescribed but they expressed more doubt about their ability to manage their diabetes in general 172 diabetes patients 18 to 64 years of age - 87 Standard Disease Management remote monitoring by cell phone, Symcare Glucometer and Bluetooth Cradle 85 Standard Disease Management with Remote Monitoring DM plus group reported greater satisfaction with their disease management experience in terms of believing program staff were helpful, articulate, better educated, and accessible. The results also showed the DM-Plus group improved self-care and had more stable glycemic control. Referred through various sources, including a review of new hospital admissions that identifies patients with specific diagnoses monitoring services system has "…contributed to reduction in hospitalization rates among congestive heart failure patients, from 19% to 12.2% at the end of 2007. During the first quarter of 2008, the hospitalization rate for telehealth patients dropped to 8%." ( ) In addition, the telehealth system has enhanced productivity; the patient load for telehealth RN is higher than that of visiting home health nurses. Telehealth RNs can conduct 6-8 visits per day, versus 5 for home health nurses, by eliminating travel time to remote areas. The system has enhanced RN productivity; the patient load for telehealth RNs is higher than that of visiting home health nurses Other studies reported by Weinstock and Starren (2006) include the following and their findings: (1) In a randomized trial (Medicare/type 1 dm / 1yr/control and intervention group/improvement reducing average blood sugar levels from 8.35 to 7,42%/less response in control group; (2) Studies document that telehomecare and remote monitoring improve knowledge of patients concerning self-management of diabetes and brought about improvement of patient self-monitoring and improved quality of ambulatory care for the disease." Summary and Conclusion Home monitoring of individuals with diabetes has been shown to be effective in the management of diabetes. References Zieger, Anne (2009) Studies Offer Mixed Grades for Remote Diabetes Care. 6 July 2009 Retrieved from FierceHealthIT at: http://www.fiercehealthit.com/story/studies-offer-mixed-grades-remote-diabetes-care/2009-07-06 O'Reilly, Caryl Ann (2005) Managing the Care of Patients with Diabetes in the Home Care Setting, Diabetes Spectrum, July 2005. Vol. 18. No. 3. Retrieved from: http://spectrum.diabetesjournals.org/content/18/3/162.full McLaughlin, Sue (2005) From Research to Practice/Diabetes Care in Special Settings: Meeting the Challenges: Diabetes Care in Special Settings Diabetes Spectrum July 2005 18:143-145. Retrieved from: http://www.vnsny.org/research/projects/1_implemetation.html Read the full article
0 notes
Text
Finding the Best Neurologist in Jalandhar at Capitol Hospital

When it comes to neurological health, finding the right specialist can make all the difference. If you’re searching for the best neurologist in Jalandhar, Capitol Hospital stands out as a beacon of excellence in advanced neurological care.
Located in the heart of Jalandhar, Punjab, our hospital combines cutting-edge technology, a compassionate approach, and a team of highly skilled neurologists to provide world-class treatment for a wide range of neurological conditions.
Why Choose Capitol Hospital for Neurological Care?
Capitol Hospital is renowned as one of the top multi-super-specialty hospitals in North India, with a dedicated Department of Neurosurgery and Neurosciences. Our commitment to patient-centered care, state-of-the-art facilities, and a team of experienced professionals make us the preferred choice for those seeking the best neurologist in Jalandhar.
Here’s what sets us apart:
1. Expert Neurologists with Advanced Training
At Capitol Hospital, our neurologists are among the finest in the region, bringing years of expertise and specialized training to the table. They are skilled in diagnosing and treating complex neurological disorders, including stroke, epilepsy, Parkinson’s disease, multiple sclerosis, and brain tumors.
2. Comprehensive Neurological Services
We offer a full spectrum of neurological care under one roof, making Capitol Hospital a one-stop destination for all your brain and spine health needs. From advanced diagnostics to personalized treatment plans, our services include:
✅ Stroke Management: Rapid diagnosis and intervention to minimize brain damage and enhance recovery. ✅ Epilepsy Treatment: Medication management and surgical options for seizure control. ✅ Neurodegenerative Disorders: Expert care for conditions like Parkinson’s and Alzheimer’s. ✅ Headache and Migraine Care: Tailored therapies to alleviate chronic pain. ✅ Neuro-Oncology: Advanced treatment for brain and spinal cord tumors.
3. Cutting-Edge Technology
Capitol Hospital is equipped with the latest diagnostic and treatment tools, including 256-slice CT scans, 3Tesla MRI machines, and neurophysiology labs for EEG, EMG, and nerve conduction studies. This advanced infrastructure allows our neurologists to accurately diagnose conditions and deliver precise, effective treatments, solidifying our reputation as home to the best neurologist in Jalandhar.
4. 24/7 Emergency Care
Neurological emergencies like strokes or severe seizures require immediate attention. Our hospital operates round-the-clock, with a dedicated stroke unit and emergency services staffed by expert neurologists and critical care specialists. This ensures that patients receive timely intervention when every second counts.
5. Multidisciplinary Team Approach
At Capitol Hospital, our neurologists collaborate with neurosurgeons, physiotherapists, rehabilitation experts, and other healthcare professionals to provide comprehensive care.
Conditions Treated by the Best Neurologists in Jalandhar at Capitol Hospital
Our neurologists are adept at managing both common and rare neurological conditions. Some of the key conditions we treat include:
✅ Stroke: Immediate thrombolysis and rehabilitation services. Epilepsy: Advanced diagnostics and surgical interventions when needed. ✅ Movement Disorders: Including Parkinson’s disease and dystonia. ✅ Multiple Sclerosis: Targeted therapies to manage symptoms and progression. ✅ Neuromuscular Disorders: Expert care for conditions affecting nerves and muscles. �� Chronic Pain: Solutions for migraines, neuropathy, and other pain syndromes. No matter the complexity of your condition, our team is equipped to provide the highest standard of care.
Why Capitol Hospital is Home to the Best Neurologist in Jalandhar?
Capitol Hospital’s reputation as a leader in neurological care is built on trust, expertise, and a relentless commitment to patient outcomes. Here’s why patients across Punjab and beyond choose us:
●) Proven Track Record: Thousands of successful treatments and satisfied patients. ●) Patient-Centric Care: We prioritize your comfort, dignity, and recovery. ●) Convenient Location: Situated on NH-44, Jalandhar-Pathankot Road, near Reru Chowk, we’re easily accessible to residents of Jalandhar and surrounding areas. ●) Cashless Facilities: We partner with leading insurance providers for a hassle-free experience.
Book Your Appointment Today
If you or a loved one is experiencing neurological symptoms — whether it’s persistent headaches, unexplained numbness, or a diagnosed condition — don’t wait to seek expert care. Contact Capitol Hospital to consult with the best neurologist in Jalandhar. You can book your appointment online through our website or call us at +91 9915021515 or +91 8427584275. Our team is available 24/7 to assist you.
Read More: https://www.capitolhospital.com/department-of-nuclear-medicine
0 notes