#Neonatal critical care
Explore tagged Tumblr posts
Text
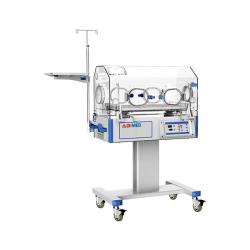
Infant Incubator
An infant incubator is a specialized medical device designed to provide a controlled environment for premature or critically ill newborn infants, also known as neonates or preterm babies. These devices create a warm, humidified, and oxygen-rich atmosphere to mimic the conditions of the mother's womb, helping to support the baby's growth and development while providing essential medical care.
0 notes
Text
Neonatal Critical Care Equipment Market Global Opportunity Analysis and Industry Forecast, 2024-2032
Neonatal critical care equipment encompasses a wide range of specialized devices and tools designed to support and sustain the health of newborns, particularly those in need of intensive medical care. This category includes ventilators, incubators, infusion pumps, monitors, and phototherapy units, among others, all engineered to address the unique and often urgent needs of critically ill or premature infants. In neonatal intensive care units (NICUs) around the world, such equipment plays a crucial role in stabilizing vital functions, managing respiratory and cardiac issues, and providing life-saving care to the most vulnerable patients.
The Neonatal Critical Care Equipment Market size was estimated at USD 3.01 billion in 2023 and is expected to reach USD 5.78 billion by 2032 with a growing CAGR of 7.52% during the forecast period of 2024-2032.
Future Scope
The future of neonatal critical care equipment lies in enhancing accuracy, reliability, and integration through technological advancements. Innovations like AI-powered monitoring, non-invasive respiratory support systems, and advanced infusion devices are expected to redefine neonatal care. Additionally, trends toward personalized and remote monitoring will allow for real-time adjustments, minimizing risks and ensuring tailored care for each infant. As healthcare systems worldwide focus on improving NICU capabilities, neonatal critical care equipment will see increased investment in research and development, ultimately raising the standard of care for newborns.
Trends
Several trends are influencing neonatal critical care equipment, including the integration of IoT (Internet of Things) and AI (artificial intelligence) for predictive analytics in monitoring newborns. The adoption of compact, multi-functional devices has also become popular, minimizing equipment footprint and providing more space and accessibility in NICU settings. Additionally, non-invasive ventilators and portable monitoring units are gaining traction, as they reduce the physical strain on infants while enhancing the efficiency and mobility of care. These trends reflect a growing emphasis on reducing infant stress and improving NICU workflows, which are essential for neonatal care quality.
Applications
Neonatal critical care equipment is crucial in managing various conditions, such as respiratory distress, jaundice, congenital abnormalities, and infections in newborns. Incubators maintain controlled environments to regulate temperature and humidity for premature infants, while ventilators support respiratory function. Phototherapy units treat jaundice by breaking down bilirubin in the bloodstream. Additionally, infusion pumps deliver precise doses of medications and nutrients, and advanced monitoring systems track heart rate, oxygen levels, and blood pressure to guide timely interventions. These applications make neonatal critical care equipment essential for newborn survival and recovery.
Key Points
Neonatal critical care equipment includes ventilators, incubators, infusion pumps, and monitoring systems.
Trends include AI and IoT integration, non-invasive respiratory support, and compact device design.
Applications focus on managing respiratory distress, infections, and jaundice in NICU settings.
Future innovations will prioritize personalized care and real-time monitoring.
Get a Free Sample Copy of the Report: https://www.snsinsider.com/sample-request/4036
Conclusion
Neonatal critical care equipment is vital for ensuring the health and survival of critically ill or premature infants. As technology continues to evolve, NICUs are becoming more equipped to provide advanced, precise, and personalized care. With increasing emphasis on non-invasive solutions and integrated monitoring, the future of neonatal critical care equipment promises improvements in both patient outcomes and operational efficiency, ultimately supporting the specialized needs of newborns in intensive care.
0 notes
Text
How Hyper-Hypothermia Units Enhance Patient Recovery: Mercury Healthcare

In the realm of modern medicine, precision and control over patient conditions during and after treatment are crucial for successful outcomes. Hyper-hypothermia units play a significant role in this aspect, providing essential temperature regulation that enhances patient recovery. These units, designed to either elevate or lower body temperatures as required, are vital in various medical treatments and surgical procedures. Mercury Healthcare, a leading manufacturer and supplier in India, stands at the forefront of this technology, offering top-quality hyper-hypothermia units that ensure optimal patient care and recovery.
Understanding Hyper-Hypothermia Units
Hyper-hypothermia units are medical devices used to control a patient's body temperature. Hyperthermia refers to raising the body temperature, while hypothermia involves lowering it. These units are equipped with advanced technology to precisely manage temperature, ensuring that it stays within the desired range. This control is crucial in various medical scenarios, including surgeries, post-operative care, and specific treatments for conditions like cancer and cardiac arrest.
Enhancing Patient Recovery
Optimizing Surgical Outcomes
During surgeries, maintaining an optimal body temperature is critical. Hyper-hypothermia units ensure that the patient’s body temperature remains stable, reducing the risk of complications such as infections or excessive bleeding. This stability contributes to better surgical outcomes and faster recovery times.
Post-Operative Care
After surgery, patients often face the challenge of maintaining stable body temperatures. Hyper-hypothermia units aid in this by providing consistent temperature management, which is essential for healing and reducing post-operative complications. Patients benefit from quicker recovery times and improved overall outcomes.
Cancer Treatment
Hyperthermia therapy, where body tissue is exposed to high temperatures, is a promising approach in cancer treatment. It can enhance the effectiveness of radiation and chemotherapy. Hyper-hypothermia units enable precise control of the temperature, ensuring the therapy's effectiveness while minimizing damage to healthy tissues.
Cardiac Arrest and Trauma Care
Inducing hypothermia in patients who have suffered cardiac arrest or severe trauma can significantly improve survival rates and neurological outcomes. Controlled cooling slows down the body's metabolic processes, protecting vital organs, especially the brain, from damage. Hyper-hypothermia units are indispensable in emergency settings for such critical interventions.
Neonatal Care
In neonatal care, maintaining the right body temperature for premature or ill infants is vital. Hyper-hypothermia units provide the necessary thermal support to these vulnerable patients, enhancing their chances of survival and reducing complications.
Why Choose Mercury Healthcare?
When it comes to selecting the best hyper-hypothermia units, Mercury Healthcare emerges as the leading manufacturer and supplier in India. Here’s why:
Advanced Technology: Mercury Healthcare’s hyper-hypothermia units are built with state-of-the-art technology, ensuring precise and reliable temperature control. This advanced technology is crucial for enhancing patient recovery in various medical scenarios.
Quality Assurance: Mercury Healthcare adheres to stringent quality standards, ensuring that every unit is thoroughly tested and certified. This commitment to quality guarantees that healthcare providers receive only the best equipment for their patients.
Comprehensive Support: Understanding the critical nature of their equipment, Mercury Healthcare provides exceptional customer support, including training, maintenance, and technical assistance. This ensures that healthcare facilities can effectively utilize their hyper-hypothermia units to enhance patient care.
Customized Solutions: Recognizing that different medical scenarios require specific temperature management, Mercury Healthcare offers a range of hyper-hypothermia units tailored to various medical needs, ensuring optimal functionality and effectiveness.
Conclusion
Hyper-hypothermia units are pivotal in modern medical treatments, significantly enhancing patient recovery by providing precise temperature control. From optimizing surgical outcomes to supporting critical care and neonatal patients, these units are indispensable in healthcare settings. Mercury Healthcare, as the best hyper-hypothermia units manufacturer and supplier in India, stands out with its advanced technology, commitment to quality, and comprehensive support. Trust Mercury Healthcare for top-tier hyper-hypothermia units that ensure optimal patient care and recovery.
#Best hyper-hypothermia units for patient recovery#Benefits of hyper-hypothermia units in surgeries#Post-operative care with hyper-hypothermia units#Cancer treatment hyper-hypothermia therapy#Cardiac arrest hypothermia treatment benefits#Neonatal care hyper-hypothermia units#Top hyper-hypothermia units manufacturer in India#Mercury Healthcare hyper-hypothermia units review#Advanced hyper-hypothermia technology in healthcare#How hyper-hypothermia units improve surgical outcomes#Best temperature control devices for patient care#Reliable hyper-hypothermia units supplier in India#Quality hyper-hypothermia units for hospitals#Customized hyper-hypothermia solutions for medical treatments#Hyper-hypothermia units for trauma and emergency care#Effective use of hyper-hypothermia units in neonatal ICU#Why choose Mercury Healthcare for hyper-hypothermia units#How to maintain hyper-hypothermia units in hospitals#Top-rated hyper-hypothermia units for critical care#Impact of hyper-hypothermia units on patient recovery times
0 notes
Text
#Fetal and Neonatal Critical Care Equipment Market#Fetal and Neonatal Critical Care Equipment Market Trend#Fetal and Neonatal Critical Care Equipment Market Demand#Fetal and Neonatal Critical Care Equipment Market Insights#Fetal and Neonatal Critical Care Equipment Market Growth
0 notes
Text
Flint, Michigan, has one of the [United States]'s highest rates of child poverty — something that got a lot of attention during the city's lead water crisis a decade ago. And a pediatrician who helped expose that lead problem has now launched a first-of-its-kind move to tackle poverty: giving every new mother $7,500 in cash aid over a year.
A baby's first year is crucial for development. It's also a time of peak poverty.
Flint's new cash transfer program, Rx Kids, starts during pregnancy. The first payment is $1,500 to encourage prenatal care. After delivery, mothers will get $500 a month over the baby's first year.
"What happens in that first year of life can really portend your entire life course trajectory. Your brain literally doubles in size in the first 12 months," says Hanna-Attisha, who's also a public health professor at Michigan State University.
A baby's birth is also a peak time for poverty. Being pregnant can force women to cut back hours or even lose a job. Then comes the double whammy cost of child care.
Research has found that stress from childhood poverty can harm a person's physical and mental health, brain development and performance in school. Infants and toddlers are more likely than older children to be put into foster care, for reasons that advocates say conflate neglect with poverty.
In Flint, where the child poverty rate is more than 50%, Hanna-Attisha says new moms are in a bind. "We just had a baby miss their 4-day-old appointment because mom had to go back to work at four days," she says...
Benefits of Cash Aid
Studies have found such payments reduce financial hardship and food insecurity and improve mental and physical health for both mothers and children.
The U.S. got a short-lived taste of that in 2021. Congress temporarily expanded the child tax credit, boosting payments and also sending them to the poorest families who had been excluded because they didn't make enough to qualify for the credit. Research found that families mostly spent the money on basic needs. The bigger tax credit improved families' finances and briefly cut the country's child poverty rate nearly in half.
"We saw food hardship dropped to the lowest level ever," Shaefer says. "And we saw credit scores actually go to the highest that they'd ever been in at the end of 2021."
Critics worried that the expanded credit would lead people to work less, but there was little evidence of that. Some said they used the extra money for child care so they could go to work.
As cash assistance in Flint ramps up, Shaefer will be tracking not just its impact on financial well-being, but how it affects the roughly 1,200 babies born in the city each year.
"We're going to see if expectant moms route into prenatal care earlier," he says. "Are they able to go more? And then we'll be able to look at birth outcomes," including birth weight and neonatal intensive care unit (NICU) admissions.
Since the pandemic, dozens of cash aid pilots have popped up across the nation. But unlike them, Rx Kids is not limited to lower-income households. It's universal, which means every new mom will get the same amount of money. "You pit people against each other when you draw that line in the sand and say, 'You don't need this, and you do,' " Shaefer says. It can also stigmatize families who get the aid, he says, as happened with traditional welfare...
So far, there's more than $43 million to keep the program going for three years. Funders include foundations, health insurance companies and the state of Michigan, which allocated a small part of its federal cash aid, known as Temporary Assistance for Needy Families.
Money can buy more time for bonding with a baby
Alana Turner can't believe her luck with Flint's new cash benefits. "I was just shocked because of the timing of it all," she says.
Turner is due soon with her second child, a girl. She lives with her aunt and her 4-year-old son, Ace. After he was born, her car broke down and she was seriously cash-strapped, negotiating over bill payments. This time, she hopes she won't have to choose between basic needs.
"Like, I shouldn't have to think about choosing between are the lights going to be on or am I going to make sure the car brakes are good," she says...
But since she'll be getting an unexpected $7,500 over the next year, Turner has a new goal. With her first child, she was back on the job in less than six weeks. Now, she hopes she'll be able to slow down and spend more time with her daughter.
"I don't want to sacrifice the time with my newborn like I had to for my son, if I don't have to," she says."
-via NPR, March 12, 2024
#united states#flint michigan#michigan#cash aid#basic income#poverty#poverty relief#child poverty#mothers#pregnancy#prenatalcare#healthcare#healthcare access#public health#child development#good news#hope
351 notes
·
View notes
Text
“Here is the biggest tragedy. Even if this child survives, she was born an orphan.”

A baby girl was delivered an emergency cesarean section from the womb of her mother, who was killed in an Israeli attack on the Gaza Strip.
The baby’s family, like thousands of displaced Palestinians, were seeking shelter in Gaza’s southern city of Rafah. On Saturday night an Israeli air strike hit their residence, killing her father, mother and four-year-old sister.
Despite inadequate equipment, medical workers were able to stabilise the newborn’s critical condition by administering air into her mouth and gently tapping her chest.
The baby, weighing 1.4 kg, was stable and improving gradually, said Mohammed Salama, a doctor caring for her. Her mother, Sabreen al-Sakani, had been 30 weeks pregnant.
Following the air strike, she was transferred to an incubator at a nearby hospital’s neonatal intensive care unit with the words “The baby of the martyr Sabreen al-Sakani” written on tape across her chest.
At least 19 people, including 13 children, were killed overnight in intensified strikes on Rafah, Palestinian health officials said. Asked about the casualties in Rafah, an Israeli military spokesperson said various militant targets were struck in Gaza including military compounds, launch posts and armed people.
“Did you see one man in all of those killed?” said Saqr Abdel Aal, a Palestinian man whose family members were among the dead, grieving over the body of a child in a white shroud.
“All are women and children. My entire identity has been wiped out, with my wife, children and everyone.”
📸: Reuters/Mohammed Salem
#free Palestine#free gaza#I stand with Palestine#Gaza#Palestine#Gazaunderattack#Palestinian Genocide#Gaza Genocide#end the occupation#Israel is an illegal occupier#Israel is committing genocide#Israel is committing war crimes#Israel is a terrorist state#Israel is a war criminal#Israel is an apartheid state#Israel is evil#Israeli war crimes#Israeli terrorism#IOF Terrorism#Israel kills babies#Israel kills children#Israel kills innocents#Israel is a murder state#Israeli Terrorists#Israeli war criminals#Boycott Israel#Israel kills journalists#Israel kills kids#Israel murders innocents#Israel murders children
49 notes
·
View notes
Text
Katharina. Scene from the German history drama series "Charité" (S03E06). A young female gymnast is checked in the hospital after fainting. Nina Kunzendorf as German pediatrician Inge Rapoport (1912-2017).
Sidenote:
Inge Rapoport fled the Nazi regime to the USA in 1939 and completed her medical training there before she moved to the GDR in 1952 where she pioneered improvements in neonatal medicine. Rapoport famously defended her doctoral thesis at the age of 102 after her initial doctorate degree had been denied by the Nazis.
She was criticized for defending the socialist dictatorship in the GDR. In her view the system provided a more just society and superior health care standards compared to western states.
27 notes
·
View notes
Text
A critical review of a Wendigoon video, pls read it all if you're interested and pls be civil♡♡
Uhm so we all know wendigoon right? Beloved horror youtuber, for good reasons too, his videos have such a comforting vibe that I rewatch them whenever I'm feeling depressed, but recently I got to thinking about a couple of things and they are making me.... slightly uncomfortable with his videos.
The first and biggest thing comes from this video which is about the game "Faith: the Unholy Trinity" which is a game about demons, possession, baby sacrifice, exorcism, etc. All told from a very Christian pov (as most media tends to be) which is no problem, the problems start when we delve a little deeper into the uncomfortable implications about the main possessed girl Amy and her story.
Tldr, she started volunteering at a what is clearly supposed to be an abortion or neonatal care clinic where a demonic cult uses it as a front to sacrifice babies for the evil causes... which idk if you can start picking up on the very concerning implications of that.
Now Wendigoon spoke with the creator of the game who explained that the (what I will call) corruption route that the mc goes through is to make it clear that someone doesn't just get possessed by demons, that they have to go out of their way to get to that point.
And we know that Amy was a good girl before she volunteered in the abortion clinic, which when u visit it (starts in the video at about 2 hours 12 mins) it is made clear immediately that it is not... great.
You first see a letter from the owner who tells the who I assume is the secretary to notify him before returning any calls from the health department because they don't want another "surprise inspection" (the owner is revealed to be a demon and a cult leader btw :))
When you walk further into the clinic, you are met with a disturbing and grotesque demon (which is usual for a horror game but please try to see how the underlying message is clear) where a cop (who is 100% a good guy and hasn't been indoctrinated into the cult) helps you int defeating it. There are also stretchers covered in the blood of the sacrificed corpses under them. It is also made clear that they are injecting the women who seek treatment there with a substance to make them hallucinate and so they don't wake up during the "procedure".
And if you want to get a secret ending, you have to go back and fight a demonic lady who unleashes demonic babies at you who look a whole lot like fetuses but that is just my opinion.
The whole game revolves around a demon cult leader who made an abortion clinic to use the 'babies' as sacrifices and to experiment on the women. If that isn't the most right-wing reactionary Christian pro-life talking points, idk what is.
The issue is that Wendigoon doesn't address the blatant demonising of neonatal care/abortion clinics and the disgusting pro-life implications that are baked deep into the game's DNA, he just keeps praising it and it's creator without batting an eye at any of this. And the comments don't even acknowledge it!
This isn't to cancel wendigoon or anything, I've just been thinking about this specific video for a while and I want to get my thoughts somewhere bc I personally didn't see much talk ab this.
#youtube#youtube drama#wendigoon#faith: the unholy trinity#pro life#pro life rhetoric#ugh#there's also alot of us-centrisim in his videos but i don't expect anything more from youtubers tbh#calling other cultures' cryptids 'just another bigfoot/ lochness monster“ is a bit iffy#but it's not my place to talk ab it#im pro choice in case you were confused#oup i forgor to add tw#tw abortion#cw abortion#tw possession#cw possession
46 notes
·
View notes
Link
Rise in respiratory conditions requiring neonatal intensive care unit treatment, as well as the introduction of new technologies, are driving the growth of...
0 notes
Text

This year's Extra Life stream is a go! Come celebrate my birthday and help raise money for my local children's hospital.
November 2-3, 2024
Saturday - TTRPG Day
1:00 PM: Kobols Ate My Baby
Sunday - Game Day
12:00 PM - 3:00 PM: Challenge Stardew
3:30 PM - 5:00 PM: Lethal Company
5:00 PM - End: Gartic Phone
All times are in PST $5 donation incentives will be live during Stardew
Watch at: twitch.tv/glazedeemon
⬇️ Extra Life info below the cut! ⬇️

Here’s a little information on Extra Life and why we are fundraising again for them this year.
What does Children’s Miracle Network Hospitals do?
Every day, Children’s Miracle Network Hospitals treat:
235 kids for diabetes
295 babies in neonatal intensive care units
2,128 kids for cancer
2,329 kids for surgeries
16,200 kids with trauma
Each year, 10 million kids enter member hospitals of Children’s Miracle Network Hospitals for care. The money raised goes directly to the hospital to:
Fund critical treatments and pediatric medical equipment
Make sure the hospitals can provide charitable care to those in need
Help cover specialized services not covered by insurance
(cit: 2023 Children’s Miracle Network Hospitals, extra-life.org)
🍩 Donate Here 🍩
@valiantsystem @rinaberd @ragingsystem
10 notes
·
View notes
Text
Every day in Gaza, I wake up grateful to be alive. I check on my wife, my three children, and my elderly parents who are living with me at the moment, and then I get straight to work – because lives depend on it.
As one of the only organisations still operating in northern Gaza, we at MAP are continuing our vital work despite the challenges. Here in the north, there are no safe places to go. We face severe shortages of food, water, electricity, and gas. But it is your support that enables us to deliver life-saving aid where it is needed most.
Since Israel’s military offensive began almost a year ago, at least 296 aid workers have been killed in Gaza. Every day I take a personal risk, knowing I could be targeted at any moment. Yet, despite the fear and devastation, we push forward.
One of our most critical efforts has been providing drugs, such as surfactant, to the only remaining neonatal intensive care unit at Gaza’s Kamal Adwan Hospital. Surfactant is a life-saving drug for premature babies which helps their lungs function properly. Without these medicines, these babies would not be able to breathe and could even die. Thanks to your generosity, we have saved many lives and reunited newborns with their parents.
Your donations have also helped us deliver food parcels and hygiene kits to more than 57,000 people displaced from their homes. Despite the constant threats, we are determined to maintain the health and dignity of Palestinians.
Thank you for standing with us
Mahmoud Shalabi
Deputy Director of Programmes in Gaza, Medical Aid for Palestinians
#free palestine#free gaza#palestine#gaza#i stand with palestine#gaza relief#medical aid for palestinians
8 notes
·
View notes
Text
A child that faces a bedridden life. A girl with intellectual disabilities raped by a family member. Victims of domestic violence or reproductive coercion. There are a variety of distressing reasons women have later stage terminations.
There is no easy definition of when an abortion is considered “late” or “late-term”. It is generally considered anything after 20 weeks’ gestation, but the states and territories have a patchwork of legislation with various milestones.
What is clear is that later terminations are the new target of anti-abortion activists, now that abortion has been decriminalised across Australia.
On Wednesday South Australia’s upper house voted on legislation that would force women seeking an abortion after 27 weeks and six days – an extremely rare occurrence – to be induced, to deliver the child alive, and keep it or adopt it out.
It was narrowly defeated – nine were in favour and 10 opposed from the 22-person house. The president only casts a deciding vote, while a prominent Liberal critic of the bill, Michelle Lensink, is absent for cancer treatment.
The Liberal frontbencher Ben Hood, who introduced the bill, says the woman’s right to end a pregnancy is kept because the pregnancy ends when the baby is born.
“The innovation of this bill is that it allows a mother to end her pregnancy throughout all nine months and indeed right up to birth,” he says.
The Greens have a different label for it: “forced birth”.
About 1% of all terminations are carried out after 20 weeks.
According to SA Health data gathered in the 18 months after abortion reform in the state, fewer than five terminations were performed after 27 weeks.
Terminations at that point can only be done with the approval of two doctors, and only if it is necessary to save the life of the pregnant person or save another foetus, or poses significant risk of injury or mental health of the pregnant person, or if there is a significant risk of serious foetal anomalies.
Hood said in the upper house on Wednesday night that his bill did not “force birth”. He said any termination at 28 weeks already involved “birth” because women had no other option in how to remove the foetus from the body.
“The only difference is that the baby will have a chance to live,” he said.
He has previously said that, once born, if the baby “isn’t compatible with life”, it would then be given palliative care.
He said on Wednesday night the babies would be admitted to neonatal units, “receiving the best medical attention available if the mother does not wish to keep the baby”.
Adoption would be a compassionate alternative, he said.
Hood indicated on ABC radio that he was not abandoning his mission.
The attorney general, Kyam Maher, says the “Trumpian” bill would wind back abortion care and poses a “real and significant danger, not only to the physical health and safety of all women, but to women’s fundamental right to bodily autonomy”.
He also hit out at the vitriol, nastiness and inflammatory attacks deployed in the campaign.
“I’d encourage those who’ve been involved in this sort of debate to reflect on whether the hyper polarised US style of personal politics really reflects well on SA,” he says.
The bill bears similarities to so-called “born-alive” laws, which have percolated in the US for years. A federal “born alive” bill in Australia was found to have no legal, ethical or medical basis to support it.
The Katter’s Australian party leader, Robbie Katter, has proposed similar legislation in Queensland.
Both Katter and Hood have thanked the anti-abortion activist Joanna Howe for her work on their legislation. Howe wants “an Australia where abortion is unthinkable”.
Hood thanked Howe on Wednesday and said the other people who informed the bill wanted to remain anonymous. Several earlier speakers noted that Hood’s bill was drafted by Howe and anonymous experts while the review that informed decriminalisation involved thousands of experts and many respected institutions who did not remain anonymous, and that it involved months of investigation and a 560-page report.
Abortion has also crept up as a serious issue in the lead-up to the Queensland election after Labor accused the Liberal National party of a “secret plan” to limit abortion rights and the LNP failed to quell the speculation.
The various campaigns have been accused of using misinformation in an attempt to limit access to terminations.
Reasons women might need a late termination include foetal abnormalities, life-threatening conditions, and psycho-social reasons such as the baby being the result of rape or incest.
‘We can’t do this to the baby’
Tiffany’s first baby had spina bifida.
Her baby would have been paralysed from the neck down. She chose a termination. Six years later, Tiffany* was pregnant again. At the 20-week scan, she was told this baby also had spina bifida, but it was not as bad.
“They said wait another two weeks, we’ll do another scan and we’ll go from there,” she says.
“You’re stressing, you’re freaking out. Two weeks felt like an eternity.”
After waiting two weeks and undergoing another scan, Tiffany was again told it didn’t look too bad and she should do another scan in two weeks.
“At 24 weeks, it got worse,” she says.
“He started developing fluid on the brain. It was affecting his nerves, down the spine. It went from numb toes to ‘he’s not going to be able to walk’.”
Another two weeks, another scan. “Everything was failing,” she says. “We did all these tests because I needed to make sure I was making the right decision … we sat down and said ‘we can’t do this to the baby’. He’d be bedridden, have surgery after surgery, a lifetime of hospital visits.”
At 28 weeks, she had the procedure.
An SA Law Reform Institute review of abortion law heard about a girl with an intellectual disability who had been sexually abused by a family member and did not realise she was pregnant until late in the pregnancy.
She made it clear she did not want the pregnancy to proceed. If she had not been able to have an abortion, if she had been forced to have the child, it would have had a “severe and adverse affect on her”, the institute said in its report.
Jacquie* and her husband had a two-year-old and another baby on the way.
They did the usual testing, including a 16-week scan and an amniocentesis. “We got the results back and they said everything was fine,” she says. “But I had a gut feeling and remember saying to my hubby that something was just off.”
At 24 weeks, they got a call. “They said they got the results wrong,” she says. “We thought, ‘shit’. So we were told at 24 weeks that our child did have Down syndrome and we had to make a choice within 24 hours.
“We just had to make the decision around our family and what was best for us. To this day we never say it was the right decision. It was the best choice for us at that time. We had to think about our little one.”
Jacob Mangelsdorf is a counsellor at Red Tree Foundation, an organisation which supports people grieving the loss of a child.
He says the parents that come to him are suffering an “incredibly complex grief”.
“We’re not talking about an easy choice. We’re not talking about something that’s without a high level of complexity,” he says.
“It’s not just losing that baby, it’s about processing that loss and the decision, [thinking] ‘in some ways I made that choice to end that baby’s life’.
“There’s always that little part of their brain grappling with that. It’s really important to acknowledge that the mum at that point has had 20-something weeks to bond with that baby.”
Tiffany says hospitals and health authorities need to do better in supporting women going through horrific experiences like hers. And people need to stop judging others, she says.
“Everyone has an opinion and their own beliefs.
“But if you’re not in my shoes, you don’t know.”
* Full names have not been used to maintain privacy of those interviewed
6 notes
·
View notes