#National College Health Assessment
Text
The first part of the article implies that there is a backlash against people calling themselves nonbinary yet they admit that more students are identifying has trans.
The national backlash against trans and nonbinary young people may have led fewer nonbinary students to disclose their gender identity in their applications to college for this fall.
That is according to my analysis of how students who applied to college through the Common App identified their gender. The Common App is a good barometer because more than 1 million students use it annually to apply to more than 1,000 U.S. schools.
For the most recent admissions cycle, 1.88% of students, or 23,620 individuals, chose a nonbinary gender term to describe themselves, down from 2.2%, or 25,959 individuals, in the last cycle.
That may not seem like a large drop, but it is a huge change from the past few years, when the number of students indicating that they were nonbinary had skyrocketed. For example, on one of the largest surveys of college students, the American College Health Association’s National College Health Assessment, the percent of students identifying as nonbinary more than doubled from 2020 to 2022, going from 2.5% to 5.1%. Then, in spring 2023, the rate of increase slowed significantly to 5.5%, and there was no increase in the percent of nonbinary students in spring 2024.
Different data, same trend
The much lower percentage of nonbinary students on the Common App than the National College Health Assessment may seem noteworthy in itself, but this is because of differences in how the data is collected.
The Common App shows a much smaller nonbinary population because its users are typically 17- and 18-year-olds. At this age, students may not yet recognize or understand their gender identity. They also may be filling out the form with family members to whom they are not out so would not feel that they could disclose. And even if they are out to their families, applicants may hold back out of concern that indicating their gender identity could result in discrimination and harm their prospects of admission.
In contrast, the National College Health Assessment is filled out online voluntarily by college students at all class levels. Because the participants are older and the survey is anonymous, the percentage of students willing to indicate that they are nonbinary is much higher.
Still, the trend is the same. Students seem less willing to identify as nonbinary on forms and surveys today.
Facing public hostility
The lack of growth in nonbinary students disclosing could be a one-year aberration. After all, the percent of students who identified as trans women and men on both the Common App and the National College Health Assessment rose this past year.
But unlike most trans female and male students, nonbinary students are typically not changing their bodies through hormones and surgeries. Thus, they are often not readily seen by others as part of the trans community and have a choice about whether to disclose their gender identity. It seems that a growing number are choosing not to be out due to the anti-trans environment in many parts of society.
The public discourse today around gender diversity is often harsh. Democratic presidential nominee Kamala Harris, for instance, was ridiculed by right-wing activists on social media for telling an audience what her pronouns are. Leading up to the 2024 Summer Olympics in Paris, middle-distance runner Nikki Hiltz, who identifies as trans and nonbinary, was criticized on social media for competing in the women’s 1500 meters even though they had the right to do so because they were assigned female at birth and were not on testosterone.
And in June 2023, billionaire Elon Musk, owner of X, formerly Twitter, said the social media platform would regard the words “cisgender” and “cis” as slurs, even though these are the terms commonly used to refer to non-trans people.
In addition, there has been a huge spike since 2023 in bills introduced and passed by state legislatures that target trans and nonbinary youth. These bills seek to ban minors from receiving gender-affirming health care, keep trans women from participating on women’s school sports teams, stop trans and nonbinary people from using school bathrooms consistent with their gender identity and prevent the teaching of material about LGBTQ+ people. This huge increase in anti-trans bills and laws corresponds to when students seemingly became less willing to indicate on the Common App that they are nonbinary.
Rise in anti-trans bills proposed by state lawmakers
Legislation targeting trans people often focuses on education and health care. The chart shows legislation introduced by state lawmakers each year. Not all of those bills actually pass. In 2024, as of early September, 45 of 652 proposed bills had passed.
A bar chart shows a large increase in the number of bills proposed in the past two years, about four times more than the previous years. The charts shows legislation introduced - a small percentage of that legislation actually passes.

The effect of state policy
One possible indication that nonbinary young people are reacting to the political climate by not disclosing their gender identity comes from my analysis of Common App data. I found that 32.7% of students who marked themselves as nonbinary lived in one of the 24 states with bans on gender-affirming care for young people, whereas 51.3% lived in one of the 16 states that protect access to this care. In contrast, cis female and male students were more likely to be from a state with one of these anti-trans laws and less likely to be from a trans-supportive state.
If a growing number of nonbinary students are indeed choosing not to be out publicly, or at least not to indicate their gender identity on the Common App and surveys such as the National College Health Assessment, it suggests that they feel they have to be closeted in some contexts. But I believe that in deciding not to disclose, they are showing their agency and resilience in the face of oppression and possible discrimination.
Whether nonbinary young people are out, they are not going away and will continue to make up a sizable percentage of trans college students.
#Less college age students are identifying has trans nonbinary#The Common App#More students identified has trans#National College Health Assessment#Only the TQ+ could complain about more male students heading off to college identifying as women and expecting access to women's spaces
1 note
·
View note
Text
Boys as young as 14 have been asking their teachers how to choke girls during sex, a teacher has told the BBC.
Dr Tamasine Preece, who teaches at Bryntirion Comprehensive in Bridgend, said some children now felt it was a normal part of sex and asked if "a soft squeeze on the neck is OK".
Health experts said pornography was a key contributor and that there was no safe way to strangle someone.
One woman, Sophie Henson, who was strangled until she passed out, said choking should not be normalised as part of sex.
It comes after warnings following the death of 26-year-old dancer Georgia Brooke, who was choked to death during sex with her boyfriend.
Dr Preece, the school's curriculum lead for health and wellbeing, said there had been questions "creeping in, such as 'How can I choke someone safely?'".
She added: "I’ve certainly been told by some children that they think that girls really want to be choked - with one saying girls are mad for it."
Johanna Robinson, Wales’ national adviser on violence against women and girls, has heard similar examples.
"I’ve spoken to sexual health nurses who told me men in college were asking questions like 'How do I safely strangle my partner?' One young person was quoted to me asking 'What do I do if I need to resuscitate my partner?'.'"
Last year, Sophie Henson was strangled by her ex partner as part of an aggressive situation.
"He gripped me by the throat so tight, I thought I was going to die," said the 24-year-old from Bridgend.
"I felt like a dead fish, my mouth was open, my body was so limp."
Sophie said she felt carrying out the act previously in the bedroom had blurred the lines, making it more acceptable.
"He'd say, 'You liked it 10 minutes ago during sex, why don't you like it now?'"
She's now warning other women to seek out and assess the risks before consenting to it as part of sex.
She said stories of it being normalised among young people were "worrying".
"Everyone is entitled to their bedroom manners, but there's no way it is safe," she added.
"There is a risk factor and it shouldn't be experimented with lightly - do your research and ask questions."
Her ex-partner Zach Pennell was convicted of coercive control and intentional strangulation in January this year.
Dr Preece said conversations needed to include consent and how that must continue throughout sex.
She encourages conversation in her classroom, so teenagers understand consent is needed rather than "just blindly accepting it" and encourages children to talk to their parents as well.
She added: "Rather than just choking specifically we talk about the fact there should be no abuse of any kind in sexual relationships.
"We can shy away from these issues or we can be realistic that they’re happening and making sure that we’re the ones having conversations with our children rather than leaving it to tech companies."
Ms Robinson echoed this message, saying: "How much harm do we need to see happen before we’re brave enough to have these conversations?
"I don’t think young people realise the potential harm - it can take little pressure to cause damage or cause someone to be unconscious.
"Helping young people to understand that is a first step."
Dr Kate Howells, an associate specialist in sexual health, believes more people think strangulation is expected, with "a lot" of young women telling her it had happened to them.
She believes instant access to porn for anyone with a phone is a key factor for it.
"People are watching it from a very young age and, for a lot of young people, it is their first sexual experience and therefore they’re almost looking to porn to learn about sex and what to do to be good at sex.
"If young people are seeing that kind of messaging from pornography rather than loving or caring, respectful messages then they'll think that's what they need to do - whether they feel comfortable with it or not."
#radblr#radical feminism#radfem#gender critical#radical feminist#terfblr#terf safe#radfem safe#article#sexuality#strangulation
553 notes
·
View notes
Text
The Courage to Follow the Evidence on Transgender Care.
(WOW, the New York Times -- which a couple years ago had an ad about a qu**r girl who wished for a world in which J.K. Rowling wasn't the author of Harry Potter -- has published yet another opinion piece about trans, this one about the Cass Review. Personally, I think he's too lenient, but at least he's bringing attention to the review to Americans. )
(For those who can't read the NYT page, here's the text.)

Opinion, David Brooks, April 18, 2024.
Hilary Cass is the kind of hero the world needs today. She has entered one of the most toxic debates in our culture: how the medical community should respond to the growing numbers of young people who seek gender transition through medical treatments, including puberty blockers and hormone therapies. This month, after more than three years of research, Cass, a pediatrician, produced a report, commissioned by the National Health Service in England, that is remarkable for its empathy for people on all sides of this issue, for its humility in the face of complex social trends we don’t understand and for its intellectual integrity as we try to figure out which treatments actually work to serve those patients who are in distress. With incredible courage, she shows that careful scholarship can cut through debates that have been marked by vituperation and intimidation and possibly reset them on more rational grounds.
Cass, a past president of Britain’s Royal College of Pediatrics and Child Health, is clear about the mission of her report: “This review is not about defining what it means to be trans, nor is it about undermining the validity of trans identities, challenging the right of people to express themselves or rolling back on people’s rights to health care. It is about what the health care approach should be, and how best to help the growing number of children and young people who are looking for support from the N.H.S. in relation to their gender identity.”
This issue begins with a mystery. For reasons that are not clear, the number of adolescents who have sought to medically change their sex has been skyrocketing in recent years, though the overall number remains very small. For reasons that are also not clear, adolescents who were assigned female at birth are driving this trend, whereas before the late 2000s, it was mostly adolescents who were assigned male at birth who sought these treatments.
Doctors and researchers have proposed various theories to try to explain these trends. One is that greater social acceptance of trans people has enabled people to seek these therapies. Another is that teenagers are being influenced by the popularity of searching and experimenting around identity. A third is that the rise of teen mental health issues may be contributing to gender dysphoria. In her report, Cass is skeptical of broad generalizations in the absence of clear evidence; these are individual children and adolescents who take their own routes to who they are.
Some activists and medical practitioners on the left have come to see the surge in requests for medical transitioning as a piece of the new civil rights issue of our time — offering recognition to people of all gender identities. Transition through medical interventions was embraced by providers in the United States and Europe after a pair of small Dutch studies showed that such treatment improved patients’ well-being. But a 2022 Reuters investigation found that some American clinics were quite aggressive with treatment: None of the 18 U.S. clinics that Reuters looked at performed long assessments on their patients, and some prescribed puberty blockers on the first visit.
Sign up for the Opinion Today newsletter Get expert analysis of the news and a guide to the big ideas shaping the world every weekday morning. Get it sent to your inbox.
Unfortunately, some researchers who questioned the Dutch approach were viciously attacked. This year, Sallie Baxendale, a professor of clinical neuropsychology at the University College London, published a review of studies looking at the impact of puberty blockers on brain development and concluded that “critical questions” about the therapy remain unanswered. She was immediately attacked. She recently told The Guardian, “I’ve been accused of being an anti-trans activist, and that now comes up on Google and is never going to go away.”
As Cass writes in her report, “The toxicity of the debate is exceptional.” She continues, “There are few other areas of health care where professionals are so afraid to openly discuss their views, where people are vilified on social media and where name-calling echoes the worst bullying behavior.”
Cass focused on Britain, but her description of the intellectual and political climate is just as applicable to the U.S., where brutality on the left has been matched by brutality on the right, with crude legislation that doesn’t acknowledge the well-being of the young people in question. In 24 states Republicans have passed laws banning these therapies, sometimes threatening doctors with prison time if they prescribe the treatment they think is best for their patients.
The battle lines on this issue are an extreme case, but they are not unfamiliar. On issue after issue, zealous minorities bully and intimidate the reasonable majority. Often, those who see nuance decide it’s best to just keep their heads down. The rage-filled minority rules.
Cass showed enormous courage in walking into this maelstrom. She did it in the face of practitioners who refused to cooperate and thus denied her information that could have helped inform her report. As an editorial in The BMJ puts it, “Despite encouragement from N.H.S. England,” the “necessary cooperation” was not forthcoming. “Professionals withholding data from a national inquiry seems hard to imagine, but it is what happened.”
Cass’s report does not contain even a hint of rancor, just a generous open-mindedness and empathy for all involved. Time and again in her report, she returns to the young people and the parents directly involved, on all sides of the issue. She clearly spent a lot of time meeting with them. She writes, “One of the great pleasures of the review has been getting to meet and talk to so many interesting people.”
The report’s greatest strength is its epistemic humility. Cass is continually asking, “What do we really know?” She is carefully examining the various studies — which are high quality, which are not. She is down in the academic weeds.
She notes that the quality of the research in this field is poor. The current treatments are “built on shaky foundations,” she writes in The BMJ. Practitioners have raced ahead with therapies when we don’t know what the effects will be. As Cass tells The BMJ, “I can’t think of another area of pediatric care where we give young people a potentially irreversible treatment and have no idea what happens to them in adulthood.”
She writes in her report, “The option to provide masculinizing/feminizing hormones from age 16 is available, but the review would recommend extreme caution.” She does not issue a blanket, one-size-fits-all recommendation, but her core conclusion is this: “For most young people, a medical pathway will not be the best way to manage their gender-related distress.” She realizes that this conclusion will not please many of the young people she has come to know, but this is where the evidence has taken her.
You can agree or disagree with this or that part of the report, and maybe the evidence will look different in 10 years, but I ask you to examine the integrity with which Cass did her work in such a treacherous environment.
In 1877 a British philosopher and mathematician named William Kingdon Clifford published an essay called “The Ethics of Belief.” In it he argued that if a shipowner ignored evidence that his craft had problems and sent the ship to sea having convinced himself it was safe, then of course we would blame him if the ship went down and all aboard were lost. To have a belief is to bear responsibility, and one thus has a moral responsibility to dig arduously into the evidence, avoid ideological thinking and take into account self-serving biases. “It is wrong always, everywhere, and for anyone, to believe anything upon insufficient evidence,” Clifford wrote. A belief, he continued, is a public possession. If too many people believe things without evidence, “the danger to society is not merely that it should believe wrong things, though that is great enough; but that it should become credulous, and lose the habit of testing things and inquiring into them; for then it must sink back into savagery.”
Since the Trump years, this habit of not consulting the evidence has become the underlying crisis in so many realms. People segregate into intellectually cohesive teams, which are always dumber than intellectually diverse teams. Issues are settled by intimidation, not evidence. Our natural human tendency is to be too confident in our knowledge, too quick to ignore contrary evidence. But these days it has become acceptable to luxuriate in those epistemic shortcomings, not to struggle against them. See, for example, the modern Republican Party.
Recently it’s been encouraging to see cases in which the evidence has won out. Many universities have acknowledged that the SAT is a better predictor of college success than high school grades and have reinstated it. Some corporations have come to understand that while diversity, equity and inclusion are essential goals, the current programs often empirically fail to serve those goals and need to be reformed. I’m hoping that Hilary Cass is modeling a kind of behavior that will be replicated across academia, in the other professions and across the body politic more generally and thus save us from spiraling into an epistemological doom loop.
#cass review#the cass review#cass report#the cass report#transgender#trans#trans insanity#the tide is turning#gender critical#gender ideology#gender identity#gender cult#gender madness
51 notes
·
View notes
Text
By Michael T. Kelly
On June 12, New York Gov. Kathy Hochul expressed support for a mask ban on subways and at protests while other politicians in New York City, Los Angeles and North Carolina are considering or have already passed laws that ban masks in public spaces. Disability, civil liberties and other activists have raised alarm regarding how mask bans, even with formal exemptions for health and religious reasons, offer no guarantee of fair enforcement and can stigmatize masking in general during an ongoing pandemic. This said, I argue that we should oppose mask bans due to two vital functions.
Firstly, banning masks will enable easier surveillance of oppressed groups. Surveillance technology to catch protesters has increased around the world in light of the visible outpouring of support for the pro-Palestine movement. Additionally, activists have used masks to protect themselves from repression, surveillance and doxing by right-wing provocateurs.
To quell campus movements, police and administrators have threatened protesters in Florida, Ohio and Texas with arrest for wearing masks. Students at several colleges face code of conduct charges for pro-Palestine protests, and there has been explicit targeting on prospects for future employment and student loan forgiveness. Indeed, these acts are consistent with the United States’ long record of state surveillance against Black, Indigenous, civil rights and anti-imperialist groups.
Secondly, mask bans downplay COVID-19 and thus avoid its social and political lessons. COVID-19 has been a world health crisis, taking the lives of at least seven million people globally and 1.2 million people in the U.S. COVID infections have risen in 38 states this summer, and some hospitals and venues have even reinstated mask mandates. Long COVID remains a widespread illness, affecting 6.8% of U.S. adults with fatigue, blood clots, lung, heart and neurological issues.
The first lesson of COVID some politicians are eager to bury is that combatting a contagious, airborne respiratory virus is inherently collective and interdependent. It requires a state-directed public health response. Discourses of individual responsibility, “choice” or risk assessment are ill-suited: Is the choice to not mask based on accurate information? Does this choice impinge on other people’s freedom to inhabit public space? Would a mandate affirm a social right to protect oneself and others from illness and make spaces more accessible?
While many people in the U.S. may have had COVID and been asymptomatic or recovered, this is simply not the case for many immunocompromised people, who have suffered isolation, hospitalization and death at significantly higher rates. As disability justice authors have long pointed out, people with disabilities always face the burden of adjusting their lives against an assumed, ableist normal. No assurance of masking effectively endangers many immunocompromised and high-risk people. Under the social model of disability, institutional neglect to enforce COVID mitigation is what creates disability as a form of social oppression.
The activist movements some politicians now condemn have led the way in public health practice. Participants at the Columbia University student encampment wore masks, while people with disabilities and activists have engaged in education and tough conversations regarding the importance of masking, even in leftist spaces.
Also, because COVID is a world-scale problem, it requires international cooperation that would weaken U.S. military, economic and geopolitical hegemony. In 2020, the U.S. and European Union blocked a proposal at the World Trade Organization to waive intellectual property (IP) protections so Global South nations could begin building productive capacity for vaccines and medical technology. Intellectual property regimes and patents have been a mainstay of U.S. policy since World War II through trade agreements and multilateral banking institutions like the International Monetary Fund and World Bank. Patent holders can hoard technology and resources that Global South nations might otherwise access freely or more cheaply. This financial power allows the U.S. to impose unilateral economic sanctions on official enemy states – Venezuela, Iran, Syria, North Korea, Nicaragua and Zimbabwe – which block medicine, food and technology, harming the population. Moves away from masking and COVID awareness further downplay the ongoing urgency to end IP and sanctions regimes for the sake of global public health.
Thus, structural changes to U.S. society are needed to address the underlying social conditions that spread illness. We can learn from the 1951 Civil Rights Congress’ We Charge Genocide petition that defined genocide as the “willful creation of conditions making for premature death, poverty and disease.”
On housing, failure to extend eviction moratoria in 2021 – a gift to landlords and real estate capital who treat homes as financial assets or sources of rent revenue – led to over 10,000 additional deaths. On criminal justice, there were calls to decarcerate as prisons are incubators of COVID, and continue questioning the social function of prisons at all. On employment, vulnerability to COVID in the workplace helped catalyze a wave of labor organizing. By downplaying COVID and banning masks, its most visible reminder, politicians help bury these important lessons.
Universities remind students and staff that their policies are consistent with county, state and CDC legal guidelines. But adherence to the U.S. Government’s public health orders is not sufficient when laws are inadequate or unjust. We can and should define our own ethos around disability, national and social liberation. Mask mandates, political education on who is vulnerable as well as public health measures to provide masks can enlist, educate and organize people toward that political project. Legislation that does not protect the vulnerable needs opposition. People should be enabled and encouraged to think for themselves when it comes to contemplating the extent to which lawmakers have the responsibility to protect their constituency.
#mask up#covid#pandemic#covid 19#wear a mask#coronavirus#public health#sars cov 2#still coviding#wear a respirator#disability justice
8 notes
·
View notes
Text
By: Azeen Ghorayshi
Published: May 13, 2024
After 30 years as one of England’s top pediatricians, Dr. Hilary Cass was hoping to begin her retirement by learning to play the saxophone.
Instead, she took on a project that would throw her into an international fire: reviewing England’s treatment guidelines for the rapidly rising number of children with gender distress, known as dysphoria.
At the time, in 2020, England’s sole youth gender clinic was in disarray. The waiting list had swelled, leaving many young patients waiting years for an appointment. Staff members who said they felt pressure to approve children for puberty-blocking drugs had filed whistle-blower complaints that had spilled into public view. And a former patient had sued the clinic, claiming that she had transitioned as a teenager “after a series of superficial conversations with social workers.”
The National Health Service asked Dr. Cass, who had never treated children with gender dysphoria but had served as the president of the Royal College of Pediatrics and Child Health, to independently evaluate how the agency should proceed.
Over the next four years, Dr. Cass commissioned systematic reviews of scientific studies on youth gender treatments and international guidelines of care. She also met with young patients and their families, transgender adults, people who had detransitioned, advocacy groups and clinicians.
Her final report, published last month, concluded that the evidence supporting the use of puberty-blocking drugs and other hormonal medications in adolescents was “remarkably weak.” On her recommendation, the N.H.S. will no longer prescribe puberty blockers outside of clinical trials. Dr. Cass also recommended that testosterone and estrogen, which allow young people to develop the physical characteristics of the opposite sex, be prescribed with “extreme caution.”
Dr. Cass’s findings are in line with several European countries that have limited the treatments after scientific reviews. But in America, where nearly two dozen states have banned the care outright, medical groups have endorsed the treatments as evidence-based and necessary.
The American Academy of Pediatrics declined to comment on Dr. Cass’s specific findings, and condemned the state bans. “Politicians have inserted themselves into the exam room, which is dangerous for both physicians and for families,” Dr. Ben Hoffman, the organization’s president, said.
The Endocrine Society told The New York Times that Dr. Cass’s review “does not contain any new research” that would contradict its guidelines. The federal health department did not respond to requests for comment.
Dr. Cass spoke to The Times about her report and the response from the United States. This conversation has been edited and condensed for clarity.
What are your top takeaways from the report?
The most important concern for me is just how poor the evidence base is in this area. Some people have questioned, “Did we set a higher bar for this group of young people?” We absolutely didn’t. The real problem is that the evidence is very weak compared to many other areas of pediatric practice.
The second big takeaway for me is that we have to stop just seeing these young people through the lens of their gender and see them as whole people, and address the much broader range of challenges that they have, sometimes with their mental health, sometimes with undiagnosed neurodiversity. It’s really about helping them to thrive, not just saying “How do we address the gender?” in isolation.
You found that the quality of evidence in this space is “remarkably weak.” Can you explain what that means?
The assessment of studies looks at things like, do they follow up for long enough? Do they lose a lot of patients during the follow-up period? Do they have good comparison groups? All of those assessments are really objective. The reason the studies are weak is because they failed on one or more of those areas.
The most common criticism directed at your review is that it was in some way rigged because of the lack of randomized controlled trials, which compare two treatments or a treatment and a placebo, in this field. That, from the get-go, you knew you would find that there was low-quality evidence.
People were worried that we threw out anything that wasn’t a randomized controlled trial, which is the gold standard for study design. We didn’t, actually.
There weren’t any randomized controlled trials, but we still included about 58 percent of the studies that were identified, the ones that were high quality or moderate quality. The kinds of studies that aren’t R.C.T.s can give us some really good information, but they have to be well-conducted. The weakness was many were very poorly conducted.
There’s something I would like to say about the perception that this was rigged, as you say. We were really clear that this review was not about defining what trans means, negating anybody’s experiences or rolling back health care.
There are young people who absolutely benefit from a medical pathway, and we need to make sure that those young people have access — under a research protocol, because we need to improve the research — but not assume that that’s the right pathway for everyone.

[ The Tavistock Gender Identity Development Service in London, which until recently was the National Health Service’s sole youth gender clinic in England. ]
Another criticism is that this field is being held to a higher standard than others, or being exceptionalized in some way. There are other areas of medicine, particularly in pediatrics, where doctors practice without high-quality evidence.
The University of York, which is kind of the home of systematic reviews, one of the key organizations that does them in this country, found that evidence in this field was strikingly lower than other areas — even in pediatrics.
I can’t think of any other situation where we give life-altering treatments and don’t have enough understanding about what’s happening to those young people in adulthood. I’ve spoken to young adults who are clearly thriving — a medical pathway has been the right thing for them. I’ve also spoken to young adults where it was the wrong decision, where they have regret, where they’ve detransitioned. The critical issue is trying to work out how we can best predict who’s going to thrive and who’s not going to do well.
In your report, you are also concerned about the rapid increase in numbers of teens who have sought out gender care over the last 10 years, most of whom were female at birth. I often hear two different explanations. On the one hand, there’s a positive story about social acceptance: that there have always been this many trans people, and kids today just feel freer to express who they are. The other story is a more fearful one: that this is a ‘contagion’ driven in large part by social media. How do you think about it?
There’s always two views because it’s never a simple answer. And probably elements of both of those things apply.
It doesn’t really make sense to have such a dramatic increase in numbers that has been exponential. This has happened in a really narrow time frame across the world. Social acceptance just doesn’t happen that way, so dramatically. So that doesn’t make sense as the full answer.
But equally, those who say this is just social contagion are also not taking account of how complex and nuanced this is.
Young people growing up now have a much more flexible view about gender — they’re not locked into gender stereotypes in the way my generation was. And that flexibility and fluidity are potentially beneficial because they break down barriers, combat misogyny, and so on. It only becomes a challenge if we’re medicalizing it, giving an irreversible treatment, for what might be just a normal range of gender expression.
What has the response to your report been like in Britain?
Both of our main parties have been supportive of the report, which has been great.
We have had a longstanding relationship with support and advocacy groups in the U.K. That’s not to say that they necessarily agree with all that we say. There’s much that they are less happy about. But we have had an open dialogue with them and have tried to address their questions throughout.
I think there is an appreciation that we are not about closing down health care for children. But there is fearfulness — about health care being shut down, and also about the report being weaponized to suggest that trans people don’t exist. And that’s really disappointing to me that that happens, because that’s absolutely not what we’re saying.
I’ve reached out to major medical groups in the United States about your findings. The American Academy of Pediatrics declined to comment on your report, citing its own research review that is underway. It said that its guidance, which it reaffirmed last year, was “grounded in evidence and science.”
The Endocrine Society said “we stand firm in our support of gender-affirming care,” which is “needed and often lifesaving.”
I think for a lot of people, this is kind of dizzying. We have medical groups in the United States and Britain looking at the same facts, the same scientific literature, and coming to very different conclusions. What do you make of those responses?
When I was president of the Royal College of Pediatrics and Child Health, we did some great work with the A.A.P. They are an organization that I have enormous respect for. But I respectfully disagree with them on holding on to a position that is now demonstrated to be out of date by multiple systematic reviews.
It wouldn’t be too much of a problem if people were saying “This is clinical consensus and we’re not sure.” But what some organizations are doing is doubling down on saying the evidence is good. And I think that’s where you’re misleading the public. You need to be honest about the strength of the evidence and say what you’re going to do to improve it.
I suspect that the A.A.P., which is an organization that does massive good for children worldwide, and I see as a fairly left-leaning organization, is fearful of making any moves that might jeopardize trans health care right now. And I wonder whether, if they weren’t feeling under such political duress, they would be able to be more nuanced, to say that multiple truths exist in this space — that there are children who are going to need medical treatment, and that there are other children who are going to resolve their distress in different ways.
Have you heard from the A.A.P. since your report was published?
They haven’t contacted us directly — no.
Have you heard from any other U.S. health bodies, like the Department of Health and Human Services, for example?
No.
Have you heard from any U.S. lawmakers?
No. Not at all.
Pediatricians in the United States are in an incredibly tough position because of the political situation here. It affects what doctors feel comfortable saying publicly. Your report is now part of that evidence that they may fear will be weaponized. What would you say to American pediatricians about how to move forward?
Do what you’ve been trained to do. So that means that you approach any one of these young people as you would any other adolescent, taking a proper history, doing a proper assessment and maintaining a curiosity about what’s driving their distress. It may be about diagnosing autism, it may be about treating depression, it might be about treating an eating disorder.
What really worries me is that people just think: This is somebody who is trans, and the medical pathway is the right thing for them. They get put on a medical pathway, and then the problems that they think were going to be solved just don’t go away. And it’s because there’s this overshadowing of all the other problems.
So, yes, you can put someone on a medical pathway, but if at the end of it they can’t get out of their bedroom, they don’t have relationships, they’re not in school or ultimately in work, you haven’t done the right thing by them. So it really is about treating them as a whole person, taking a holistic approach, managing all of those things and not assuming they’ve all come about as a result of the gender distress.
I think some people get frustrated about the conclusion being, well, what these kids need is more holistic care and mental health support, when that system doesn’t exist. What do you say to that?
We’re failing these kids and we’re failing other kids in terms of the amount of mental health support we have available. That is a huge problem — not just for gender-questioning young people. And I think that’s partly a reflection of the fact that the system’s been caught out by a growth of demand that is completely outstripping the ability to provide it.
We don’t have a nationalized health care system here in the United States. We have a sprawling and fragmented system. Some people have reached the conclusion that, because of the realities of the American health care system, the only way forward is through political bans. What do you make of that argument?
Medicine should never be politically driven. It should be driven by evidence and ethics and shared decision-making with patients and listening to patients’ voices. Once it becomes politicized, then that’s seriously concerning, as you know well from the abortion situation in the United States.
So, what can I say, except that I’m glad that the U.K. system doesn’t work in the same way.
-
When asked after this interview about Dr. Cass’s comments, Dr. Hoffman, the A.A.P.’s president, said that the group had carefully reviewed her report and “added it to the evidence base undergoing a systematic review.” He also said that “Any suggestion the American Academy of Pediatrics is misleading families is false.”
--



#Azeen Ghorayshi#Dr. Hilary Cass#Hilary Cass#Cass review#Cass report#medical scandal#medical malpractice#medical corruption#gender affirming care#gender affirming healthcare#gender affirmation#sex trait modification#religion is a mental illness
14 notes
·
View notes
Text


group of senior clinical psychologists have apologised for the role their profession played in the promotion of transgender ‘medical’ treatments to children in the UK following a damning report which found that such interventions were done on “shaky foundations”.
In a joint letter published by the left-wing Guardian’s sister paper The Observer, 16 unnamed “senior clinical psychologists”, including some who actually worked in the now-discredited Gender Identity Development Service (GIDS) clinics that prescribed hundreds of children life-altering puberty-blocking drugs, said that their profession led the way in pushing children into such a direction.
“These were psychology-led services. Whether intentionally or not, and many were doing their best in an impossible situation, it was clinical psychologists who promoted an ideology that was almost impossible to challenge,” they wrote.
“It is also our professional body, the British Psychological Society, that has failed (despite years of pressure) to produce guidelines for clinicians working with young people in this complex area; and that, forced into making an official response for the first time, now minimises its own role in events and calls for ‘more psychology’ as the answer. We are ashamed of the role psychology has played,” the group added.
They said that what occurred at GIDS clinics was a “multi-factorial systemic failure” but said that those within the psychology profession should be “fully examined” and held accountable for the role they played, noting that many “failed to carry out proper assessments of troubled young people, and thus put many on an ‘irreversible medical pathway’ that in most cases was inappropriate; and who failed in their most basic duty to keep proper records.”
The admission comes in the wake of a National Health Service-sponsored report from leading paediatrician Dr Hilary Cass, which argued that the NHS should no longer provide puberty-blocking drugs to children under the age of 18, given that many of that their prescription was “built on shaky foundations”.

The Cass report went on to say there is little evidence to support the so-called ‘gender affirming’ claim that hormone-altering treatments improved children’s mental health and that there has been little investigation into the potential ramifications such drugs have on the “cognitive and psychosexual development” of the children as they age.
Additionally, it argued that because many children will naturally grow past feelings of gender dysphoria “for most young people, a medical pathway will not be the best way to manage their gender-related distress”.
A preliminary version of the report forced the NHS to order the closure of the Tavistock Centre and its controversial Gender Identity Development Service clinic, which served as the nation’s top transgender clinic for children. Cass argued that the treatments offered by Tavistock were “not a safe or viable long-term option” for children.
The clinic has long faced criticism over the apparent lax standards used to determine if children were displaying signs of transgenderism, with former governor of the Tavistock and Portman NHS Foundation Trust, Dr David Bell, whistleblowing in 2022 to reveal that that staff would make such decisions based on flimsy evidence, such as if young girls failed to show interest in “pink ribbons and dollies“.
Last year, a re-examination of a 2011 study from University College London Hospitals (UCLH) and the Tavistock Centre — which claimed that there were no negative impacts of puberty blockers on the psychological function of 12 to 15-year-olds — overturned the initial claims, with University of Essex Professor of Psychology Susan McPherson and social scientist David Freedman finding instead that 34 per cent of children placed on puberty-blocking drugs saw their mental health “reliably deteriorate”.
While many in the United States continue to advocate for medical interventions for allegedly transgender children, there is a growing consensus in Europe against the practice, with progressive countries such as Denmark, Finland, Norway, Sweden, and the UK having all begun to restrict transgender treatments for children. Last month, a report commissioned by French senators asserted that providing children with life-altering transgender drugs will be remembered as one of the “greatest ethical scandals in medical history” and called for the practice to be restricted in France as well.

Don't expect to see anything like this in the US. American Leftist never admit being wrong. Never
6 notes
·
View notes
Text
"More than 1,000 Australians die unnecessarily in hospital each year due to avoidable failures by surgeons, according to experts calling for a senate inquiry.
Graham Beaumont, PhD, and Dr John North are both long-term members of audit committees that review surgical mortality in Australia.
They say patients are dying every day as a result of poor decisions to operate, communication issues, and lacklustre teamwork in operating theatres, as well as incentives for doctors to pursue “futile and unnecessary surgeries”.
Beaumont, a member of the Australian and New Zealand Audit of Surgical Mortality committee of the Royal Australasian College of Surgeons, said it was “reasonable to suggest there are in excess of 1,000 avoidable patient surgical deaths per annum across the nation based on the data in the public domain”.
“This figure could be several magnitudes higher because decisions to operate made by surgeons are not routinely scrutinised to assess the futility and necessity of surgical interventions. This figure is the great unknown,” he said."
...
"Beaumont said international research showed up to 90% of avoidable deaths in surgery exhibit a breakdown in aspects of the soft skills required to communicate, work with others and make consistently good decisions."
...
"Ian Harris, a professor of orthopaedic surgery at UNSW, agreed the current medical system needs a review, questioning the influence of money on decision making.
“The medical system that we have in Australia is not fit for purpose,” he said. “It’s a medical system that incentivises, rewards and measures healthcare activity – turnover – not health.”
Harris said not all surgeons understand the evidence for particular procedures and tend to operate based on what they see other surgeons do.
“Spine fusion for back pain is a good example. There is not very good evidence for it. It’s quite invasive, risky and costly, and takes a long time to recover,” he said.
“Payment for the public hospital surgeon is around $500 to do a spine fusion but in the workers’ compensation sector the surgeon can bill $20,000 for the same procedure – a procedure that may not help the patient,” he said.
“The rate of spine fusion is much higher in privately insured patients in Australia than non-privately insured patients.
“So knee replacements, spine fusions, knee arthroscopies are rewarded, incentivised, counted and institutionalised as part of the healthcare system – delivering these products to people without necessarily making patients better.”"

emphasis mine
reminder that doctors wield much more horrifying power than other authorities in the system and will use it for their own purposes
103 notes
·
View notes
Text
Monday, July 1, 2024
Despair in the air: For many voters, the Biden-Trump debate means a tough choice just got tougher
(AP) The sound you might have heard after the presidential debate this past week was of voters falling between a rock and a hard place. Apart from the sizable and pumped-up universe of Donald Trump’s supporters, the debate suddenly crystalized the worries of many Americans, a portion of President Joe Biden’s supporters among them, that neither man is fit to lead the nation. Heading into the first debate of the general election campaign, voters had faced a choice between two strikingly unpopular candidates. They then watched as Trump told a stream of falsehoods with sharpness, vigor and conviction, while Biden struggled mightily to land debating points and even to get through many sentences. It added to doubts about the 81-year-old Democratic president’s fitness to be in office for four more years. Now, the options are even more dispiriting for many Democrats, undecided voters and anti-Trump Republicans. More than a few people came away from watching the debate very conflicted.
“Rural Studies”
(NYT) Kristin Lunz Trujillo grew up proud of her family’s way of life. She spent summers getting ready to show cattle at the county fair. During the school year, she rushed home after class to feed the chickens on her family’s corn and soybean farm. Neither of her parents went to college, but they encouraged their daughter when she decided to go to Carleton, a liberal arts school a two-hour drive from their farm in Minnesota. Despite being physically close to home, Ms. Lunz Trujillo was surprised by how foreign her upbringing seemed at the college. She was dismayed when she checked out the farm club and learned that its members wanted to brew kombucha, not milk cows. When an art history teacher asked students which famous paintings they’d seen in person, Ms. Lunz Trujillo stayed quiet, because she had never been to an art museum. This sense of cultural alienation molded her research when she became a political scientist: What is rural identity? How does it shape a person’s politics? This year, Ms. Lunz Trujillo, now an assistant professor at the University of South Carolina, was reading a new, best-selling book that cited her research to explore those same questions. But “it seemed to be more of a hit piece on rural America,” she said. “White Rural Rage,” by the journalist Paul Waldman and the political scientist Tom Schaller, is an unsparing assessment of small-town America. Rural residents, the authors argued, are more likely than city dwellers to excuse political violence, and they pose a threat to American democracy. Ms. Lunz Trujillo excoriated the book in an opinion piece for Newsweek as “a prime example of how intellectuals sow distrust by villainizing” people unlike them.
Beryl strengthens into hurricane in Atlantic, forecast to grow into major storm entering Caribbean
(AP) Beryl grew into a hurricane Saturday as it churned toward the southeastern Caribbean, with forecasters warning it was expected to strengthen into a dangerous major storm before reaching Barbados late Sunday or early Monday. A major hurricane is considered Category 3 or higher, with winds of at least 111 mph (178 kph). A hurricane warning was issued for Barbados, St. Lucia, Grenada, and St. Vincent and the Grenadines. A tropical storm warning was posted for Martinique and Tobago and a tropical storm watch for Dominica.
CDC warns of increased risk of dengue fever infections
(Yahoo) Federal health officials are warning that dengue fever risks are elevated in the United States as cases in the Americas for the first half of 2024 are already more than double last year's rates. This year has also set a record for global cases of the potentially fatal mosquito-borne illness, the Centers for Disease Control and Prevention said in a June 25 advisory. Rising global temperatures are fueling a similar boom of dengue-infected mosquitoes, the CDC said. That's particularly concerning during the summer when Americans are more likely to travel to territories and countries with high rates of the virus, including to Puerto Rico, which has declared a public health emergency due to its nearly 1,500 cases of the illness, the agency said.
One gun, 34 dead: Inside Ecuador’s war on black-market weapons
(Reuters) The gun—a 9-millimeter pistol—blazed a violent trail even by the standards of one of Ecuador’s most dangerous neighborhoods, the Nueva Prosperina precinct of Guayaquil. Shell casings from bullets fired by the weapon, recovered at the scenes of 27 separate violent incidents, were linked to 34 deaths, according to a police forensic unit. And a police forensic official told Reuters the authorities believe the pistol remains on the streets. The havoc attributed to a single firearm exemplifies the challenges for President Daniel Noboa’s crackdown on an explosion of violent crime and homicides since 2020, fueled by a sharp increase in smuggled weapons during the same time, many of them from the United States. Ecuador recorded 7,994 murders last year, a nearly six-fold increase since 2020.
Britain’s Young Voters Are Frustrated
(NYT) As the flag of a British workers union flapped behind him on a blustery June morning, Liam Kehoe was on strike with colleagues outside Royal Liverpool University Hospital, demanding better pay for porters, cleaners and catering staff. Their wages have failed to keep up with the surge in the cost of living, and many said they were living paycheck to paycheck. Mr. Kehoe, 26, serves food in the hospital. Thinking of the life that his parents built on salaries earned as a nurse and a truck driver, Mr. Kehoe says that young people have been left with far worse prospects after 14 years of a Conservative-led government. “If you go back 30 years ago, houses were a bit more affordable, life was a little bit easier,” he said. “Nowadays, it’s like you can’t afford anything.” Polls suggest more than half of voters under 35 plan to vote for Labour on Thursday, compared with 27 percent of voters over 65. While the gap between young and old in politics is not new, the extent of the split in Britain in recent years is exceptional.
France’s exceptionally high-stakes election has begun
(AP) Voters across mainland France began casting ballots Sunday in the first round of an exceptional parliamentary election that could put France’s government in the hands of nationalist, far-right parties for the first time since the Nazi era. The outcome of the two-round election, which will wrap up July 7, could impact European financial markets, Western support for Ukraine, and how France’s nuclear arsenal and global military force are managed. Many French voters are frustrated about inflation and economic concerns, as well as President Emmanuel Macron’s leadership, which they see as arrogant and out-of-touch with their lives. Marine Le Pen’s anti-immigration National Rally party has tapped and fueled that discontent, notably via online platforms like TikTok, and dominated all preelection opinion polls. A new coalition on the left, the New Popular Front, is also posing a challenge to the pro-business Macron and his centrist alliance Together for the Republic.
7 killed and dozens wounded after missiles slammed into a town in southern Ukraine, officials say
(AP) Russian missiles slammed into a town in southern Ukraine, killing seven civilians, including children, and wounding dozens more, local authorities reported. Ukrainian officials published photos of bodies stretched out under picnic blankets in a park in Vilniansk, and deep craters in the blackened earth next to the charred, twisted remains of a building. Thirty-six people were wounded in Saturday evening’s attack, authorities said, and declared a day of mourning Sunday. Vilniansk is in Zaporizhzhia region, less than 30 kilometers (20 miles) from the local capital and north of the front lines, as Russian forces continue to occupy part of the province.
For India’s garbage pickers, a miserable and dangerous job made worse by extreme heat
(AP) The putrid smell of burning garbage wafts for miles from the landfill on the outskirts of Jammu in a potentially toxic miasma fed by the plastics, industrial, medical and other waste generated by a city of some 740,000 people. But a handful of waste pickers ignore both the fumes and suffocating heat to sort through the rubbish, seeking anything they can sell to earn at best the equivalent of $4 a day. “If we don’t do this, we don’t get any food to eat,” said 65-year-old Usmaan Shekh. “We try to take a break for a few minutes when it gets too hot, but mostly we just continue till we can’t.” Shekh and his family are among the estimated 1.5 to 4 million people who scratch out a living searching through India’s waste—and climate change is making a hazardous job more dangerous than ever. In Jammu, a northern Indian city in the Himalayan foothills, temperatures this summer have regularly topped 43 degrees Celsius (about 110 Fahrenheit).
US, Europe warn Hezbollah to ease strikes on Israel and back off from wider Mideast war
(Politico) U.S., European and Arab mediators are pressing to keep stepped-up cross-border attacks between Israel and Lebanon’s Iran-backed Hezbollah militants from spiraling into a wider Middle East war that the world has feared for months. Iran and Israel traded threats Saturday of what Iran said would be an “obliterating” war over Hezbollah. Hopes are lagging for a cease-fire in Israel’s conflict with Hamas in Gaza that would calm attacks by Hezbollah and other Iranian-allied militias. With the stalled talks in mind, American and European diplomats and other officials are delivering warnings to Hezbollah—which is far stronger than Hamas but seen as overconfident—about taking on the military might of Israel, current and former diplomats say. The Americans and Europeans are warning the group it should not count on the United States or anyone else being able to hold off Israeli leaders if they decide to execute battle-ready plans for an offensive into Lebanon.
Gaza’s remaining hospitals will stop working in two days, health officials warn
(Washington Post) Gaza’s remaining hospitals, health centers and oxygen stations will stop working within 48 hours as the fuel needed to operate generators runs out, Gaza’s Health Ministry said in a statement shared to Telegram noon local time Sunday. Israel’s closure of the vital Rafah border crossing last month severed key supply lines, limiting access to food, fuel and medical supplies inside the enclave, aid groups say. A United Nations report released earlier this month said that more than 1 million people in Gaza are expected to “face death and starvation” by mid-July. Many of Gaza’s medical facilities have already been damaged, raided or evacuated since Oct. 7. Israel has made hospitals a key target of its military campaign, alleging Hamas uses them for militant activity. In other instances, fighting between Israeli forces and militants has struck hospitals and clinics.
Kenya’s urban population is growing. The need for affordable housing is, too
(AP) In the heart of the crowded Kibera neighborhood in Kenya’s capital, Jacinter Awino shares a small tin house with her husband and four children. She envies those who have escaped such makeshift homes to more permanent dwellings under the government’s affordable housing plan. The 33-year-old housewife and her mason husband are unable to raise the $3,800 purchase price for a one-room government house. Their tin one was constructed for $380 and lacks a toilet and running water. “Those government houses are like a dream for us, but our incomes simply don’t allow it,” Awino said. Kenya’s urban areas are home to a third of the country’s total population of more than 50 million. Of those in urban areas, 70% live in informal settlements marked by a lack of basic infrastructure, according to UN-Habitat.
2 notes
·
View notes
Text
Immigration estimates for 2023 notably surpassed prior projections, as we explain in a recent analysis. This piece explores what we know about where recent U.S. immigrants live, though data limitations mean the picture is necessarily incomplete. We specifically focus on one sub-population of interest: non-dependent immigrants arriving in the last two calendar years without a college degree. As we document in a 2022 policy proposal, recently arrived immigrants without a college degree are most likely to pose short-term fiscal challenges to states and localities even as that same group is likely beneficial for the federal budget.
The data suggest that there are increasing numbers of new arrivals across the country. Specifically, between 2018 and 2023, 42 states in the contiguous U.S. had increases in the share of their adult populations comprised of non-college immigrants who had arrived within two years. In turn, there is increasing pressure on the federal government, which reaps substantial positive fiscal gains from immigration over the long run, to distribute resources to a growing number of communities who face disproportionate near-term budget strains.
In our previous analysis, we describe some of the important aggregate economic effects of the increase in immigration. We document the boost to economic output and consumer spending, for example. In addition, “for 2024 we estimate sustainable employment growth will be between 160,000 and 200,000, approximately double the sustainable level that would have occurred in absence of the pickup in immigration according to the pre-pandemic projections…” Prior research also shows that immigration is good for the federal budget. In a comprehensive study, the National Academies of Sciences, Engineering, and Medicine estimates each additional immigrant, on average, directly contributes $1,208 (in 2023 dollars) more in tax revenue each year than they receive in federal benefits, and that net benefits over a 75-year horizon exceed $326,000 (in 2023 dollars) for an immigrant and their descendants.
To understand the effects of immigration at the sub-national level, we explore the geographic distribution of recent immigration. That distribution matters because where immigrants settle determines where labor supply is expanded and which communities see increases in demand for goods and services. In addition, the fiscal effects of immigration are different for state and local governments than for the federal government. Localities disproportionately pay for the benefits most often available to newly arrived immigrants, such as education and health care. In the short run, new migrants typically are a net fiscal negative for state and local government budgets. In the long run, the fiscal impacts are positive even at the state and local level as immigrants’ incomes rise. Nonetheless, most of the fiscal gains accrue at the federal level.
A Hamilton Project policy proposal by two of the authors of this piece explore the geographic distribution of immigrants that likely put more fiscal pressure on sub-national governments: immigrants who have arrived within five years who are not dependents and have not received a bachelor’s degree, which we defined as “impact index immigrants.” In this piece, to better assess changes since immigration started to rebound in 2021, we examine more recent impact index immigrants. That is to say, we examine the trends for those who have arrived in the U.S. during the reference year or the year prior.
Of course, there is nothing immutable about the fact that impact index immigrants improve the federal budget but put pressures on sub-national governments. As we previously proposed and return to in the conclusion below, the federal government should fund localities with a high proportion (which we define as over 0.5 percent) of impact index immigrants through transparent funding streams targeted at health and education.
2 notes
·
View notes
Text
Israel Has Damaged or Destroyed More Than Half of Gaza’s Infrastructure
Israel has likely destroyed or damaged more than 137,000 structures in Gaza, according to a United Nations report.
In all, Israel has damaged or completely destroyed 137,297 structures, per the agency’s report, accounting for 55 percent of all structures in Gaza.
According to UNOSAT’s analysis, Israel’s attacks have likely damaged or destroyed more than 135,000 housing units.
The assessment only includes an examination of infrastructure up to May 3. By now, the total number of destroyed buildings is likely higher, particularly in the southern Gaza city of Rafah, where Israel has orchestrated numerous rocket attacks and launched a ground invasion in recent weeks.
Israeli forces have intentionally bombed hundreds of health care facilities and hospitals since October; currently, no hospitals in Gaza are operating at full capacity, even as hundreds of thousands of Palestinians are in desperate need of medical care. These strikes have killed at least 723 health care workers, according to a World Health Organization report published in May.
Israel’s attacks have also targeted educational centers, destroying all 12 of Gaza’s colleges and universities. In total, Israel has severely damaged or destroyed 80 percent of schools in Gaza, conducting 212 “direct hits” on at least 53 of them, according to the U.N.
A separate investigation by Al Jazeera’s Sanad Verification Agency finds that Israel has “systematically demolish[ed] neighborhoods” on the borders of Gaza in order to create an expansive “buffer zone,” including creating a “central axis” dividing line known as the Nezarim axis, dividing Gaza in two. The areas within these zones have been made “uninhabitable,” according to the report, with destruction rates in these zones reaching 80-90 percent.
2 notes
·
View notes
Text
“One reason for the despair is the fact that young women experience a hormonal shift during adolescence that often makes them strangers to themselves. One minute life is beautiful and they bubble over with joy. The next minute the world is conspiring against them and they cry for reasons they don't fully understand. These shifts in emotions are a result of the fact that the main neurotransmitters of the adolescent brain all have a major impact on mood. Especially for a teenage woman, fluctuating levels of estrogen and progesterone exert a powerful influence over these neurotransmitters, creating a perfect emotional storm.1 It's helpful when a girl can be informed of these facts prior to adolescence so that she doesn't think there's something wrong with her if she finds herself in tears during a television commercial.
As if these physiological factors aren't difficult enough, women's lives are often spiced up with unstable relationships, gossip, strained friendships, family issues, and a host of other problems. It's hardly a smooth ride. A college survey revealed that 47 percent of college female students felt so depressed during the previous year that it was sometimes hard for them to function.2 When you add sexual activity to the equation, teenage girls become more than three times as likely to be depressed as abstinent teens.3 One student e-mailed me after a broken sexual relationship to say, "I feel like the gross stuff in the road after the snow is kinda melted and cars have been driving on it for a while."
-Jason and Crystalina Evert, How to Find Your Soulmate Without Losing Your Soul
1 David Walsh, Why Do They Act That Way? (New York: Free Press, 2005), 63-64.
2 The American College Health Association, National College Health Assessment, Spring 2006.
3 Robert Rector et al., “Sexually Active Teenagers Are More Likely to Be Depressed and to Attempt Suicide,” The Heritage Foundation, June 3, 2003; Martha W. Waller et al., “Gender Differences in Associations between Depressive Symptoms and Patterns of Substance Use and Risky Sexual Behavior among a Nationally Representative Sample of U.S. Adolescents,” Archives of Women’s Mental Health 9, no. 3 (May 2006): 139-50.
#Depression#mental health#woman#girls#quotes#Jason Evert#Crystalina Evert#Jason and Crystalina Evert#How to Find Your Soulmate Without Losing Your Soul
3 notes
·
View notes
Text
The idea that the internet causes mental illness arouse because the majority of Americans were already mentally ill and social media was initially designed to gather like minded individuals into echo chambers where they began to believe their mental illnesses were normal, and then began exhibiting those behaviors as normal around other people in public, eventually causing mass psychosis and division in America spread via the internet. This phenomenon eventually spread to our military effectively making the biggest threat to national security the military themselves. The CIA had to step in on America’s own soil. I would write a thesis on this but I never went to college because that was another place where the mentally ill obviously liked to gather, and if everyone involved caught the digitally viral psychosis, America was going to get nuked, since it I was able to extrapolate this inevitable outcome by observing people’s behavior on the internet, then so did Russian, Israeli, and Chinese intelligence. Most of you were put into a trance by a CIA/NSA mental health task force to avoid a catastrophic apocalyptic situation. This is all the fault of U.S. politicians and high ranking military personnel who refused to take the CIA’s psychological assessments and scientific data seriously because they had something to hide.😎🥳🫡
4 notes
·
View notes
Text
How to Become an Aspiring Medical Professionals in the US?

Aspiring medical professionals in the US embark on a rigorous and rewarding journey that requires dedication, perseverance, and a passion for helping others.
Here's a comprehensive guide to becoming a medical professional in the United States:
Educational Requirements:
a. Undergraduate Degree: Complete a bachelor's degree in any major, but it's recommended to focus on science-related fields like biology, chemistry, or physics to prepare for medical school prerequisites.
b. Medical School (MD or DO): Earn a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO) degree. Medical school typically takes four years and involves a combination of classroom learning, laboratory work, and clinical rotations.
2. Premedical Preparation:
a. MCAT (Medical College Admission Test): Take and score well on the MCAT, a standardized test that assesses your scientific knowledge and problem-solving skills.
b. Shadowing and Volunteering: Gain hands-on experience in healthcare settings by shadowing physicians, volunteering in hospitals, or participating in research projects.
c. Extracurricular Activities: Demonstrate your commitment to healthcare and community service through extracurricular activities related to medicine or public health.
3. Medical School Application:
a. Strong Academic Record: Maintain a high GPA in your undergraduate studies, particularly in science courses.
b. Letters of Recommendation: Secure strong letters of recommendation from professors, mentors, and physicians who can attest to your academic and personal qualities.
c. Personal Statement: Craft a compelling personal statement highlighting your motivations, experiences, and aspirations in the medical field.
4. Residency Training:
a. Match Process: After medical school, participate in the National Resident Matching Program (NRMP) to match with a residency program in your desired speciality.
b. Specialization: Residency training typically lasts three to seven years, depending on the speciality, and provides in-depth clinical training under the supervision of experienced physicians.
c. Board Certification: Once you complete a residency, you become eligible to take and pass the board certification exam for your speciality.
5. Licensure and Continuing Medical Education:
a. Medical License: Obtain a medical license from the state where you intend to practice.
b. Continuing Medical Education (CME): Commit to lifelong learning by completing CME courses to stay up-to-date with the latest medical advancements and maintain your license.
6. Career Options:
a. Physician: Choose from a wide range of medical specialities, such as internal medicine, pediatrics, surgery, family medicine, or psychiatry.
b. Physician Assistant: Work under the supervision of a physician to provide comprehensive medical care.
c. Nurse Practitioner: Provide primary and specialized healthcare services independently or in collaboration with physicians.
d. Other Medical Professionals: Explore various healthcare professions, including dentists, pharmacists, optometrists, and audiologists.
Once you are ready to join organizations to offer your services, you need a platform to help you get a job. Check MedCadre, and you will get what you seek as an aspiring medical professional.
How does MedCadre help Aspiring Medical Professionals?
MedCadre is a one-stop solution to find the right job for you. The platform helps aspiring medical professionals get placement in the medical field.
All you have to do is visit the website, click on the form, and fill it out with relevant information. Once we verify your Resume, we will get back to you.
Becoming a medical professional in the US is a challenging yet fulfilling career path. With dedication, perseverance, and a passion for helping others, you can make a significant impact in your patients' lives and contribute to advancing healthcare.
Submit your Resume to MedCadre to enhance your career in the medical profession.
visit our site by clicking the link: https://medcadre.com/careers
#medical professionals#physician assistant#nurse practitioner#nursestaffing#healthcarestaffing#allied staffing
3 notes
·
View notes
Text
who clinic
Kensington Clinic is a free-standing clinic providing confidential care for aspiration abortion, medication abortion and miscarriages up to the 20th week of pregnancy. You will be treated with respect, understanding and expert care. Clinic is accredited by the Alberta College of Physicians and Surgeons and the National Abortion Federation.
Request Appointment
Visit the Appointments Page for more information.
Support Through Every Step
Question Mark Icon
Making a Decision
We believe every person should be able to freely make choices about their pregnancy. Our experienced staff can provide accurate information and compassionate counselling to assist you in making a decision that’s right for you.
Calendar Icon
Your Appointment
A doctor’s referral is not required and services are covered by Alberta Health Care. Appointments can be booked by calling the clinic between 8:00am and 4:30pm Monday to Friday (not including statutory holidays); or you can request an appointment through our website and we will call you within 1 business day with the appointment information.
Clipboard Icon
Procedures & Aftercare
Kensington Clinic offers medication and aspiration abortions, as well as procedures to help you manage a miscarriage. For your convenience and privacy, pre-operative services including ultrasound and labs, are provided at the clinic on the day of your procedure.
bortion
There are a few types of procedures provided at Kensington Clinic:
Medication Abortion from 6 to 10 weeks
Aspiration Abortion from 6 to 16 weeks
Dilation and Evacuation from 16 to 20 weeks
It is important to know the duration of your pregnancy. This is measured by the number of weeks from the first day of your last normal menstrual period. If you are travelling a long distance from Calgary, or your pregnancy is 12 weeks or more, we recommend you obtain an ultrasound before coming for your appointment to ensure we will be able to provide the care you need. When you book your appointment, a receptionist will ask for the first day of your last menstrual period, and which type of procedure you are booking for.
Medication Abortion
Medication abortion is done in Canada using a combination of medications, together called Mifegymiso. Mifegymiso includes two medications that are taken over two days.
If your pregnancy is between 6 and 10 weeks (70 days), counting from the first day of your last normal menstrual period, you may choose either a medication abortion or an aspiration abortion. Please read about both types of procedures before booking your appointment.
All assessments including ultrasound and lab work (including a blood test for Rh type and pregnancy hormone) are done on the day of your appointment, meaning you do not have to go anywhere other than Kensington Clinic for the evaluation of your pregnancy.
Before you receive the medication, we will do an ultrasound to confirm you are no more than 10 weeks (70 days) pregnant. If you are eligible for a medication abortion, you will meet with our counsellor to discuss the steps in detail. You will then meet with a nurse who will take your medical history and do blood work. After this, the physician will start the treatment.
Mifegymiso
Mifepristone: You will take the first medication, mifepristone, in the clinic. Mifepristone will destabilize the lining of your uterus to end the pregnancy. Once you take this medication these effects are not reversible.
Misoprostol: You will be given the second medication, misoprostol, to take home on the day of your appointment. You will insert the misoprostol tablets into your vagina or into the cheeks of your mouth 24-48 hours after you take the mifepristone. You may choose the time of day you take the misoprostol, but be aware that you will start to bleed heavily within 1-4 hours. As you can expect to have heavy bleeding and strong cramping, you should choose a time when you are safe to rest. The bleeding and cramping may continue for several hours. After that, bleeding may continue off and on for up to 6 weeks.
There is a 2-5% failure rate with these medications.
Side Effects
Most people will need pain medications such as extra strength ibuprofen and acetaminophen to help with the pain associated with medication abortion. Heavy bleeding resulting in soaking 1-2 large pads every hour may occur for several hours, with on and off bleeding for up to 6 weeks. Nausea, vomiting, diarrhea, fever, chills, headaches and fatigue are common side effects of the medications. Some people will find these side effects to be intense. If you are unsure you are can manage these symptoms at home, you should choose an aspiration abortion instead.
Medication Abortion vs Aspiration Abortion
Please consider carefully which type of procedure best suits you. Although there is bleeding and cramping with both aspiration and medication abortions, bleeding and cramping will be more intense and of greater duration with a medication abortion. Our staff will be happy to answer any questions you may have before you make your decision. However, if you book for one type of appointment and change your mind on the day of the appointment, you will have to rebook an appointment on another day. Please read the Comparison of Early Abortion Options
Medication Abortion Aspiration Abortion
How far along in the pregnancy can I be?
6 to 9 weeks (63 days) from the first day of
your last menstrual period.
6 to 20 weeks from the first day of day of
your last menstrual period.
Is it safe?
With both medication and aspiration abortions, there is a small risk of complications, but
abortion is at least 10 times safer than continuing a pregnancy.
Is follow-up required?
Yes. You will need to complete follow-up in 6
weeks to ensure the pregnancy has ended.
This will involve a urine test, a blood test or a
vaginal ultrasound.
No. The doctor will ensure the abortion is
complete during your appointment. You are
not required to return to the clinic for followup unless you have concerns.
How is the abortion done?
Medication causes the abortion. Heavy
bleeding with clots is common as the
pregnancy is passed, and this can continue
for several hours.
The doctor opens the cervix and removes the
pregnancy from the uterus using instruments
and suction. This usually takes 5-10 minutes.
How painful is it?
Cramps can be very strong for a number of
hours during the medication abortion. Pain
medication (such as Tylenol and Advil) can
help.
You will be given local anesthetic and IV
sedation during the procedure, and this will
help relieve pain. You may feel some cramps
during the procedure and right afterwards.
How much will I bleed?
You could have light to heavy bleeding for 1-4 weeks after either type of abortion.
Can the abortion fail?
The medication works 97% of the time. The aspiration is successful over 99% of the
time.
Can I still have children afterwards?
YES. Neither type of abortion lowers your chances of getting and staying pregnant in the
future.
P a g e | 2 of 2
Medication Abortion Aspiration Abortion
Pros and Cons of Each Type
PROS PROS
No instruments in your body 1. Single step process that is over in a few
minutes
2. No anesthesia is given 2. Anesthesia is given
3. It may feel more like a miscarriage 3. There is less risk of a failed abortion or
going to the hospital.
4. You can choose to have someone with
you while you are at home, or you
can be alone.
4. Medical staff are with you during the
abortion.
5. You can drive yourself home after the
appointment. 5. It can be done later in the pregnancy.
CONS CONS
It takes longer to complete the abortion 1. A physician inserts instruments inside
the uterus.
2. Bleeding can be very heavy and cramps
can be severe. This can last for hours.
2. Anesthetics and sedation can cause side
effects, such as drowsiness and
dizziness.
3. Other side effects of the medication
include flu-like symptoms which may
be unpleasant.
3. You cannot drive yourself home as you
will be sedated (legally impaired for 24
hours).
4. You may need to take more time off
from work or school to manage the
side effects.
4. You need to fast (no food or drink) on
the day of the procedure. You can eat
and drink normally once it is over.
5. You may see the pregnancy tissue as
the abortion happens at hom Aspiration Abortion / D&C
An aspiration abortion is done entirely in our clinic on the day of your appointment. All assessments including an ultrasound are done in the clinic so you do not have to go anywhere other than Kensington Clinic for evaluation of your pregnancy. After the ultrasound, you will meet with our counsellor to discuss the procedure in detail. You will then meet with a nurse who will take your medical history prior to your procedure. During the procedure, you will receive sedation that helps makes you feel comfortable and relaxed.
6 to 12 weeks — If your pregnancy is between 6 and 12 weeks, the doctor gently opens the cervix a small amount in our comfortable procedure room. Once the cervix is opened appropriately, the doctor uses gentle suction to clean out the contents of the uterus. The doctor may use a spoon-shaped instrument (curette) to check the walls of the uterus for any tissue that may remain. The doctor will check to ensure all of the pregnancy is removed and the procedure is complete. The procedure will last less than 10 minutes, but your appointment will take 3 hours.
13 to 16 weeks — If your pregnancy is 13 weeks to 16 weeks, you will first be given a medication before the procedure called Misoprostol. Misoprostol softens the cervix and makes dilation easier. Misoprostol takes about 2 hours to work, so you will be given a recliner to rest in. The procedure will last up to 15 minutes as described above. Your appointment will take 4-5 hours.
You will rest in the recovery area after the procedure is over. There is generally no follow-up required after an aspiration abortion. Most patients return to normal activities the following day.
Medication Abortion vs Aspiration Abortion
Please consider carefully which type of procedure best suits you. Although there is bleeding and cramping with both aspiration and medication abortions, bleeding and cramping will be more intense and of greater duration with a medication abortion. Our staff will be happy to assist you and answer your questions and concerns before you make your appointment. However, if you book for one type of appointment and change your mind on the day of the appointment, you will have to rebook an appointment on another day. Please read the. Dilation and Evacuation
16 to 20 weeks — If you are over 16 weeks, the procedure will occur over 2 days. The cervix needs to be opened by inserting laminaria (osmotic dilators) the day before the abortion. These absorb moisture and expand, gently opening the cervix. They are left in overnight. Plan to be in the clinic 2-3 hours on the first day.
The next morning you will return to the clinic and be given Misoprostol tablets to aid in softening the cervix. These take approximately two hours to work, so you will be given a comfortable recliner to rest in. When you are ready, the physician will remove the laminaria and complete the procedure. On the second day, the procedure will take 10 to 30 minutes. Expect to be in the clinic for 4-5 hours on the second day.Miscarriage
Kensington Clinic offers timely care for treatment of miscarriages and fetal demise.
Your physician may refer you or you may book your own appointment.
When a pregnancy ends on its own, it is called a spontaneous abortion or miscarriage. Miscarriages are common, occurring in 25% of pregnancies. A miscarriage usually cannot be prevented and is no one’s fault.
There is no right or wrong way to emotionally feel about a miscarriage. Experiencing a miscarriage holds different meaning to everyone. Some want to explore ways to remember the pregnancy. Others may want to just focus on getting through the procedure on the day of the appointment. You can speak with a counsellor at Kensington Clinic if you want to explore ways to feel supported, remember the pregnancy, care for the pregnancy remains, or discuss a plan for further support after the surgical procedure. Our staff can provide resources and referrals in the community for support after a miscarriage. One organization is the Pregnancy & Infant Loss Support Centre.
You have options when it comes to caring for pregnancy remains and a counsellor will support you with whichever feels right for you. Options include:
The Silent Hopes Memorial is a program where pregnancy remains lost to miscarriage are cremated and interred at a memorial garden in Calgary. There is no charge for this program.
Private arrangements including burial or cremation can be arranged through a funeral home of your choice or the clinic will recommend a local funeral home to support you with this.
The clinic will care for the pregnancy remains in a regulated manner and no further involvement is required on your part.
If your pregnancy is very early, your doctor may have given you options to treat your pregnancy loss, including:
Waiting (expectant management) for the pregnancy to expel on its own.
Treatment with a medication called Mifegymiso will cause your uterus to contract and help your body expel the pregnancy. This is successful about 90% of the time within 2-3 days of taking it. Heavy bleeding and cramping are normal with this process. If unsuccessful, you may require a D&C.
Treatment with a procedure (D&C) to remove the pregnancy from your uterus. A procedure for miscarriage involves the removal of the pregnancy and placental tissue from the uterus. This is called Uterine Aspiration or Dilation and Curettage (D&C) for pregnancies up to 15 weeks by ultrasound.
If you are over 16 weeks by ultrasound when you miscarried, the procedure to remove the pregnancy and placental tissue is called Dilation and Evacuation (D&E). You can read about the risks of these procedures here.
If you have chosen to treat your miscarriage with a D&C, or your pregnancy is at a stage where your safest option is to be treated with a D&C or D&E, your doctor can refer you to a hospital or Kensington Clinic for the procedure. You may also book your own appointment at Kensington Clinic. At Kensington Clinic we will make every effort to see you within a few days of your referral or request.
Procedures are done using IV sedation. You may feel very drowsy and not remember much after, but you will not be completely asleep. For procedures under 16 weeks, you can expect to be in the clinic for 2-3 hours. For procedures over 16 weeks, your stay in the clinic may be closer to 4-5 hours, or you may be required to come for two appointments on consecutive days. When you book your appointment, we will let you know what you can expect. You must arrange to have someone drive you home.
We will require copies of all the diagnostic investigations that have determined your pregnancy has ended or is non-viable. If you and your doctor have established you are eligible for genetic testing to determine the cause of your miscarriage, your doctor will need to forward the appropriate requisitions for the tests to us and Kensington Clinic will ensure this is done.
For more information or to book an appointment,Risks of Procedures
Aspiration Abortion or D&C
Uterine aspiration, D&C, and D&E are some of the most common procedures in Canada. The rate of complications is less than 2% and most complications are minor and easily treated. If compared to pregnancy and childbirth, these procedures have fewer complications. However, like any procedure there are risks you should be aware of.
Infection in the uterus occurs in 0.1 to 2% of aspiration procedures. You will be given one dose of antibiotics before your procedure to help prevent this from happening.
Retained tissue (some pregnancy tissue is left in the uterus). This occurs in 0.5 to 1% of aspiration procedures. Further medical care may be necessary.
Continued pregnancy or failed abortion. This is rare with aspiration abortions and more likely if the uterus has an unusual shape, if the pregnancy is very early (less than 6 weeks), or if the pregnancy is not in the uterus. You may have to return for another visit or be referred to another physician. With a normal pregnancy in a normal uterus, there is less than a 0.1% chance of this occurring.
Post-abortion hematometra. This is a rare condition where blood builds up more quickly than it can come out. It is unpleasant but is not dangerous, and is treated by repeating the uterine aspiration procedure. This condition occurs in about o.1% of procedures.
Excessive bleeding or hemorrhage. Occurs in about 0.1% of procedures. It is sometimes caused by failure of the uterus to contract or by retained tissue. Usually this can be controlled by medications in the clinic. If heavy bleeding cannot be controlled in the clinic, transfer to hospital would be required.
Injury to the uterus or other internal organs occurs in less than 0.1% of procedures. Transfer to a hospital and surgery to repair the injury may be required. Removal of the uterus is required in approximately 1 in 10,000 procedures.
Allergic reaction to any of the medications given to you, or to latex or other materials in the clinic. Most reactions can be treated in the clinic. A very severe reaction would require transfer to a hospital.
The risk of death related to surgical abortion is about 1 in 1,000,000. Most deaths are related to general anaesthesia or other medical circumstances. The risk of death during pregnancy and childbirth is ten times greater.
Medication Abortion
Retained tissue (some pregnancy tissue is left in the uterus). This occurs more frequently in medication abortions. Sometimes the uterus is unable to expel the tissue and further medical care is necessary.
Continued pregnancy or failed abortion. There is a 2-5% failure rate with these medications and if they have failed to induce an abortion the doctor will discuss a treatment plan with you.
Excessive bleeding or hemorrhage. It is sometimes caused by failure of the uterus to contract or by retained tissue. As this will be happening outside the clinic, you should contact the clinic if you are experiencing hemorrhage, and you may need to proceed to the hospital for medical care.
Infection in the uterus occurs rarely. You may need antibiotics to manage the infection.
Allergic reaction to any of the medications given to you can rarely occur. A very severe reaction would require visit to a hospital.
The risk of death related to abortion is about 1 in 1,000,000. Most deaths are related to excessive bleeding. The risk of death during pregnancy and childbirth is ten times greater
2 notes
·
View notes
Text
Abstract
Purpose:
The goal of the National Center for Medical Education Development and Research Center (NCMEDR) is to support the education and training of medical students in the care of vulnerable populations. Access to primary care services in the US is fundamental to the health and wellness of all people regardless of their socioeconomic status. LGBQ+ persons, (lesbian, gay, bisexual, transgender, queer, and other sexual and gender minority), Persons Experiencing Homelessness (PEH), and Migrant Farm Workers (MFW) are among the most underserved, marginalized, and socially vulnerable groups in the US. NCMEDR in the Department of Family and Community Medicine at Meharry Medical College was established in part, with funding from the Department of Health and Human Services (DHHS) and the Health Resources and Services Administration (HRSA). NCMEDR was developed to provide educational pathways for transforming medical education and clinical practice in the US by ascertaining whether medical students were being trained to provide primary care, and behavioral health services to LGBTQ+ persons, PEH, and MFW. Here we focus on the impact of the COVID-19 pandemic on these specific populations because they represent marginalized groups that have been heavily impacted by the pandemic, have poor social determinants of health (SDOH), and are more likely to be uninsured, and are less likely to engage primary care providers outside of emergency room care.
Methods:
In this study, a scoping literature review was conducted to assess the impact of COVID-19 on primary care of LQBTQ+ persons, PEH, and MFW.
Results and Discussion:
The pandemic provided a serious health disparities gap for the defined vulnerable populations under review by the NCMEDR. The pandemic identified the need for transformative measures for clinical practices, medical education, and health care policies required for implementation to improve health care for vulnerable groups. We make recommendations for interventions with defined populations that may influence clinical, environmental health, and SDOH in the COVID era.
Conclusions:
The COVID pandemic directed the need for medical schools, health care and social organizations to intervene in new and different ways in vulnerable and marginalized communities. The recommendations provide a model for advancing health equity, access, quality, utilization, care coordination, and treatment.
PDF Link: www.fortunejournals.com/articles/a-scoping-review-on-the-impact-of-covid-19-on-vulnerable-populations-lgbtq-persons-persons-experiencing-homelessness-and-migrant-f.pdf
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator
5 notes
·
View notes
Text
By: Bernard Lane
Published: Apr 14, 2024
Nine of the 15 gender clinics in a landmark international survey for the Cass review have admitted they do not routinely collect outcome data on their young patients.
This survey, together with a new evaluation of treatment guidelines for gender dysphoria, gives unprecedented insights into the workings of gender clinics around the world offering puberty blockers and cross-sex hormones to minors.
In the 2022-23 survey, six clinics said they “routinely collected some outcome data”: one of these clinics gave no further detail; one noted the number of patients discontinuing treatment; another used measures of quality of life; two were taking part in cohort studies; and the sixth clinic repeated some baseline assessments. Nine clinics acknowledged “not routinely collecting outcome data.”
The report of the survey results1, published by researchers from the University of York earlier this month, identified clinics by country, not name. Of the clinics that took part, Australia and the Netherlands were prominent with five and four clinics respectively.
Poor data collection was central to the controversy over the London-based Tavistock youth gender clinic.
The Cass review had planned to run a data-linkage study—with help from adult gender clinics—to learn the outcomes of the Tavistock’s 9,000-odd former patients.
The missing long-term data would allow clinicians, young patients and parents to make informed decisions about treatment. The review said it was to be the largest study of its kind in the world.
However, six of the seven adult clinics refused to co-operate. One stated reason was that “the study outcomes focus on adverse health events, for which the clinics do not feel primarily responsible.”
Another adult clinic said, “The unintended outcome of the study is likely to be a high-profile national report that will be misinterpreted, misrepresented or actively used to harm patients and disrupt the work of practitioners across the gender dysphoria pathway.”
On April 12, however, The Times newspaper reported that the uncooperative adult clinics had “bowed to pressure to share [the] missing data”.
Mostly medical
In the York University international survey, ordered by the Cass review, all 15 youth gender clinics said they used a multi-disciplinary team, but researchers concluded there was a “paucity” of psychosocial therapy interventions such as psychotherapy or cognitive behaviour therapy. Five clinics did not offer any of these non-medical interventions in-house.
All gender clinics told researchers that “genital reconstructive surgery”—the creation of a pseudo vagina, for example—was “accessible only from age 18.” The youngest age for “masculinising chest surgery” (a double mastectomy) was reported as 16. In fact, there are documented cases in Australia of 15-year-olds approved for transgender mastectomy. Genital surgery is legally available to minors2 in Australia and practised in America.
“Only five clinics reported routine discussion of fertility3 preferences, and only two discussed sexuality4. Finland was the only country to report routinely assessing for history of trauma5,” the final Cass report says in its commentary on the survey.
In separate studies for the Cass review, three independent reviewers evaluated the quality of 21 guidelines for treatment of gender dysphoria in minors.
Included were international guidelines (from the Endocrine Society and the World Professional Association for Transgender Health or WPATH); documents from North America (for example, the 2018 policy statement from the American Academy of Pediatrics); from Europe (the guideline of the UK Royal College of Psychiatrists, for example, and Denmark’s); as well as guidelines from the Asia-Pacific and Africa.
“WPATH has been highly influential in directing international practice, although its guidelines were found by the University of York appraisal process to lack developmental rigour,” the Cass report says.
The York researchers chart patterns of “circular” cross-referencing between guidelines to create a misleading impression of consensus in favour of the medicalised “gender-affirming” treatment approach.
“The guideline appraisal raises serious questions about the reliability of current guidelines. Most guidelines have not followed the international standards for [rigorous and independent] guideline development. Few guidelines are informed by a systematic review of empirical evidence [the gold standard for assessing the evidence supporting a health intervention] and there is a lack of transparency about how recommendations were developed,” the Cass report says.
“Healthcare services and professionals should take into account the variable quality of published guidelines to support the management of children and young people experiencing gender dysphoria. The lack of independence in many national and regional guidelines, and the limited evidence-based underpinning current guidelines, should be considered when utilising these for practice.”
The Cass report says it is “imperative” that gender clinic staff be “cognisant of the limitations in relation to the evidence base and fully understand the knowns and the unknowns.”
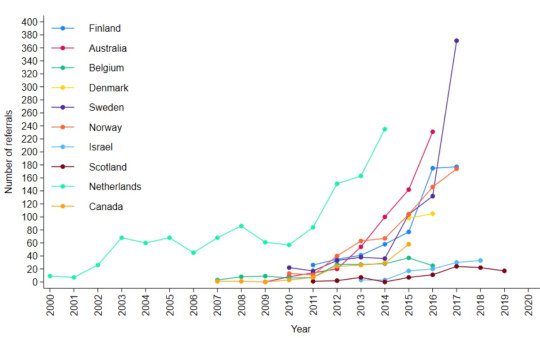
[ Chart: Number of youth gender clinic referrals over time by country. Source: Cass report ]
Bum steer
Staff at the Tavistock clinic misled patients and parents, or failed to correct their misconceptions, according to a new report from the Multi-Professional Review Group (MPRG) given oversight of treatment decisions from 2021.
These shortcomings of clinicians included playing down the extent of the unknowns of hormonal treatment; not explaining that puberty blockers are being used unlicensed and off-label; not challenging the reassuring but false parallel with the licensed use of puberty blockers for precocious (premature) puberty; not discussing the possibility that blockers will pause or slow psychosexual development; and not sharing figures showing the vast majority of children started on puberty blockers will go on to cross-sex hormones supposed to be taken lifelong.
The MPRG was also troubled by clinical documents showing misunderstanding of “the outcome of physical treatments” on the part of patients and parents.
In the York University study of treatment guidelines for gender dysphoria, only two were recommended for use by all three reviewers. These were recent, more cautious policies from Finland and Sweden. Both followed independent systematic reviews showing the evidence base for hormonal and surgical treatment of minors to be very weak and uncertain. Like the Cass review itself, the 2020 Finnish and 2022 Swedish guidelines recognise that puberty blockers are experimental and should not be routine treatment.
Although all the guidelines in the study agreed on the need for a multidisciplinary team to treat gender-distressed minors, the “most striking problem” shown by analysis of these documents was “the lack of any consensus6 on the purpose of the assessment process”, the Cass report says.
“Some guidelines were focused on diagnosis, some on… eligibility for hormones, some on psychosocial assessment, and some on readiness for medical interventions7.
“Only the Swedish and [the 2022] WPATH 8th version guidelines contain detail on the assessment process8. Both recommend that the duration, structure and content of the assessment be varied according to age, complexity and gender development.
“Very few guidelines recommend formal measures/clinical tools to assess gender dysphoria, and a separate analysis demonstrated that the formal measures that exist are poorly validated.”
Nor was there any consensus on “when psychological or hormonal interventions should be offered and on what basis.”
A survey of staff at the Tavistock clinic, undertaken as part of the Cass review, found specialists divided on whether or not “assessment should seek to make a differential diagnosis, ruling out other potential [non-gender9] causes of the child or young person’s distress.”
Arguing for an ambitious research program well beyond a possible clinical trial of puberty blockers, the Cass report says the field of youth gender dysphoria is one of “remarkably weak evidence” where health professionals are “afraid to openly discuss their views” because of vilification and bullying.
“Although some think the clinical approach should be based on a social justice model, the NHS works in an evidence-based way,” the report says.
“The gaps in the evidence base regarding all aspects of gender care for children and young people have been highlighted, from epidemiology through to assessment, diagnosis10 and intervention. It is troubling that so little is known about this cohort and their outcomes.
“Based on a single Dutch study, which suggested that puberty blockers may improve psychological wellbeing for a narrowly defined group of children with gender incongruence [or dysphoria], the practice spread at pace to other countries.
“Some practitioners abandoned normal clinical approaches to holistic assessment, which has meant that this group of [gender-distressed] young people have been exceptionalised compared to other young people with similarly complex presentations.”
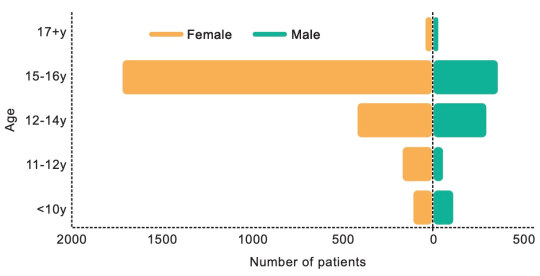
[ Chart: Age and sex on referral to the Tavistock clinic from 2018-2022. Source: Cass report ]
Who to trust?
The Cass report says the missing evidence “makes it difficult to provide adequate information on which a young person and their family can make an informed choice.”
“A trusted source of information is needed on all aspects of medical care, but in particular it is important to defuse/manage expectations that have been built up by claims about the efficacy of puberty blockers.
“The option to provide masculinising or feminising hormones from the age of 16 is available, but the [Cass] review would recommend an extremely cautious clinical approach and a strong clinical rationale for providing hormones before the age of 18. This would keep options open during this important developmental window, allowing time for management of any co-occurring [non-gender] conditions11, building of resilience, and fertility preservation, if required.”
The review stresses that “consent is more than just capacity and competence. It requires clinicians to ensure that the proposed intervention is clinically indicated as they have a duty to offer appropriate treatment. It also requires the patient to be provided with appropriate and sufficient information about the risks, benefits and expected outcomes of the treatment.”
“Assessing whether a hormone pathway is indicated is challenging. A formal diagnosis of gender dysphoria is frequently cited as a prerequisite for accessing hormone treatment. However, it is not reliably predictive of whether that young person will have long-standing gender incongruence in the future, or whether medical intervention will be the best option for them.”
Advocates for the gender-affirming approach assert that detransition and treatment regret are vanishingly rare, whereas suicide risk for those denied medical intervention is claimed to be very high.
The Cass report says: “It has been suggested that hormone treatment reduces the elevated risk of death by suicide in this population, but the evidence found did not support this conclusion.”
“The percentage of people treated with hormones who subsequently detransition remains unknown due to the lack of long-term follow-up studies, although there is suggestion that numbers are increasing.”
The report cites three reasons why the true extent of detransition is unlikely to be clear for some time—patients who decide medicalisation was a mistake may not wish to return to their former clinic to announce this fact; there is a post-treatment honeymoon period and clinicians suggest it may take 5-10 years before a decision to detransition; and the surge in patient numbers only began within the last decade.
Faced with uncertainty and a lack of good evidence, those with responsibility—from health ministers and hospital managers down to gender clinicians—rely on treatment guidelines supposed to advise on clinical practice according to the “best-available” evidence and expert opinion.
In the York University guideline analysis, the 21 documents were rated on six domains, the key two being the rigour of their development and their editorial independence.
“[Rigour] includes systematically searching the evidence, being clear about the link between recommendations and supporting evidence, and ensuring that health benefits, side effects and risks have been considered in formulating the recommendations,” the Cass report says.
Only the Finnish and Swedish guidelines scored above 50 per cent for rigour. Only these two documents, the Cass report says, link “the lack of robust evidence about medical treatments to a recommendation that treatments should be provided under a research framework or within a research clinic. They are also the only guidelines that have been informed by an ethical review conducted as part of the guideline development.”
“Most of the guidelines described insufficient evidence about the risks and benefits of medical treatment in adolescents, particularly in relation to long-term outcomes. Despite this, many then went on to cite this same evidence to recommend medical treatments,” the report says.
“Alternatively, they referred to other guidelines that recommend medical treatments as their basis for making the same recommendations. Early versions of two international guidelines, the Endocrine Society 2009 and WPATH 7th version guidelines, influenced nearly all the other guidelines.
“These two guidelines are also closely interlinked, with WPATH adopting Endocrine Society recommendations, and acting as a co-sponsor and providing input to drafts of the Endocrine Society guideline. The WPATH 8th version cited many of the other national and regional guidelines to support some of its recommendations, despite these guidelines having been considerably influenced by the WPATH 7th version.
“The circularity of this approach may explain why there has been an apparent consensus on key areas of practice despite the evidence being poor.”
Sometimes these gender-affirming guidelines seek to buttress a strong evidence claim with a citation to a study that is weak or involves a different patient group.
The Cass report notes that, “The WPATH 8th version’s narrative on gender-affirming medical treatment for adolescents does not reference its own systematic review [of the evidence], but instead states: ‘Despite the slowly growing body of evidence supporting the effectiveness of early medical intervention, the number of studies is still low, and there are few outcome studies that follow youth into adulthood. Therefore, a systematic review regarding outcomes of treatment in adolescents is not possible’.”
Despite WPATH insisting such an evidence review is not possible, this is precisely what health authorities and experts have undertaken since 2019 in several jurisdictions—Finland, Sweden, the UK National Institute for Health and Care Excellence, Florida, Germany, and University of York research commissioned by the Cass review.
Yet in the 8th and current version of its guideline, WPATH makes the confident statement that, “There is strong evidence demonstrating the benefits in quality of life and well-being of gender-affirming treatments, including endocrine and surgical procedures… Gender-affirming interventions are based on decades of clinical experience and research; therefore, they are not considered experimental, cosmetic, or for the mere convenience of a patient. They are safe and effective at reducing gender incongruence and gender dysphoria”.
But WPATH “overstates the strength of the evidence” for its treatment recommendations, the Cass report says.
--
1 In the survey, there was one clinic each from Belgium, Denmark, Finland, Northern Ireland, Norway and Spain. The response rate was 38 per cent.
2 In Australia there is no good public data on trans surgery for minors.
3 Early puberty blockers followed by cross-sex hormones are expected to sterilise young people and may also impair future sexual function.
4 Some sizeable proportion of gender clinic patients might grow up in healthy bodies and accept their same-sex attraction were it not for trans medicalisation, according to testimony from detransitioners, clinicians’ reports and data.
5 Trauma from a history of sexual abuse, for example, or exposure to domestic violence is thought to be among the many possible underlying causes of what presents as gender dysphoria. The Multi-Professional Review Group (MPRG), given oversight of Tavistock treatment decisions from 2021-23, was troubled by the lack of curiosity by the clinic’s staff about the effect of a child’s “physical or mental illness within the family, abusive or addictive environments, bereavement, cultural or religious background, etc.”
6 Critics of the “gender-affirming” treatment approach say it is not mainstream medicine because the “trans child” in effect self-diagnoses while clinicians avoid differential diagnosis and attribute mental health disorders and other pre-existing issues to a “transphobic” society.
7 “In most cases [at the Tavistock clinic] children and parents were asking to progress on to puberty blockers from the very first appointment”, according to the MPRG.
8 In the MPRG’s opinion, the patient notes from the Tavistock “rarely provide a structured history or physical assessment, however the submissions to the MPRG suggest that the children have a wide range of childhood, familial and congenital conditions.”
9 Once referred to the Tavistock, patients typically were no longer seen by child and adolescent mental health services.
10 According to the MPRG, gender dysphoria in the diagnostic manual DSM-5 “has a low threshold based on overlapping criteria, and is likely to create false positives. Young people who do not go on to have an enduring cross-sex gender identity may have met the criteria in childhood. And early to mid-childhood social transition may be influential in maintaining adherence to the criteria. Sex role and gender expression stereotyping is present within the diagnostic criteria—preferred toys, clothes, etc—not reflecting that many toys, games and activities [today] are less exclusively gendered than in previous decades.”
11 The MPRG said it was “notable that until the child and family’s first appointment at [the Tavistock] they have received little, if any, support from health, social care, or education professionals. Most children and parents have felt isolated and desperate for support and have therefore turned for information to the media and online resources, with many accessing LGBTQ+ and [gender dysphoria] support groups or private providers which appear to be mainly ‘affirmative’ in nature, and children and families have moved forward with social transition. This history/journey is rarely examined closely by [Tavistock clinicians] for signs of difficulty [or] regret.”
==
Critics have described "gender affirming care" - that is, sex-trait modification - as "medical experimentation." This is incorrect. In a medical experiment, you actually collect data and monitor the participants in the experiment. They don't do that. They're cowboys violating all medical ethics - "first, do no harm" - for ideology, money or both.
#Bernard Lane#Cass review#Cass report#Dr. Hilary Cass#Hilary Cass#gender affirming care#gender affirming healthcare#gender affirmation#medical scandal#medical malpractice#sex trait modification#medical corruption#World Professional Association for Transgender Health#WPATH#ethics violations#medical ethics#unethical#gender ideology#gender identity ideology#queer theory#intersectional feminism#religion is a mental illness
11 notes
·
View notes