#Infectious disease
Explore tagged Tumblr posts
Text
Common Symptoms Were Fatigue and Decreased Exercise Tolerance, According to a 2022 Survey
Inequities In the Prevalence and Severity of Symptoms Observed Across Race, Ethnicity, Gender, and Neighborhood Poverty
December 26, 2024 — Today, the New York City Health Department announced that 80 percent of adult New Yorkers infected with COVID-19 who were surveyed experienced at least one symptom lasting one month or longer. According to the results of the COVID-19 Experiences Survey in 2022, the most common symptoms were fatigue and decreased exercise tolerance. While post-acute symptoms may resolve within 12 weeks, many people will go on to develop Long COVID, an infection-associated chronic condition characterized by symptoms lasting three months or longer.
“This survey shows us that the symptoms following COVID-19 infections are a significant public health issue for New Yorkers. Black and Latino communities, women, transgender people, and those living in low-income neighborhoods were more likely to have symptoms, highlighting the disproportionate impact of the pandemic on marginalized communities,” said Acting Health Commissioner Dr. Michelle Morse. “We must invest in a comprehensive long-term response to the COVID-19 pandemic that focuses on prevention through engagement with health care providers and community members. Services for people experiencing the long-term physical, mental, social, and economic impacts of COVID-19 infection should be accessible to all.”
Post-acute symptoms are those that last one month or longer. To better understand experiences of COVID-19 post-acute symptoms, the Health Department conducted the COVID-19 Experiences Survey in November and December 2022. Adult New Yorkers who were members of the probability-based NYC Health Panel were invited to take the survey if they had confirmed or suspected COVID-19; 2,081 people completed the survey online or by phone in English, Spanish, Russian, Simplified Chinese, or Traditional Chinese. The results provide insight into how post-acute symptoms relate to health care seeking, social and demographic factors, disability, and mental health.
Some respondents reported many symptoms at different levels of severity, while others reported few symptoms, only mild symptoms, or none at all. Inequities in the prevalence and severity of post-acute symptoms after COVID-19 were observed across race/ethnicity, gender, and neighborhood poverty levels.
The prevalence of mild symptoms was similar across socio-demographic groups.
Moderate symptoms were more prevalent among Latino and Asian/Pacific Islander adults compared with white adults, and among people living in high poverty neighborhoods compared with people in low poverty neighborhoods.
Severe symptoms were more prevalent among women and transgender or non-binary adults compared with men, among Latino and Black adults compared with white adults, and among people living in very high and high poverty neighborhoods compared with low poverty neighborhoods.
Increasing symptom severity was associated with activity limitations and depression. Those with at least one severe symptom were more likely to report activity limitations compared with those who reported no post-acute symptoms (60 percent vs. 6 percent), which may result in social, economic, and mental health difficulties.
People with at least one severe post-acute symptom reported 10 days of reduced ability or complete inability to carry out usual activities or work in the past month, compared with 6 days for moderate symptoms, 3 days for mild symptoms, and 1 day for no symptoms.
One in three adults (33 percent) with at least one severe post-acute symptom after COVID-19 had probable depression, higher than those reporting only mild symptoms (6 percent) or no symptoms (2 percent).
Black and Latino New Yorkers, women, transgender adults, and those living in low-income neighborhoods were most likely to report severe symptoms, reflecting the disproportionate impact of the ongoing pandemic in these communities.
To address inequities in awareness about the long-term health impacts of COVID-19 and the importance of preventing new infections, the NYC Health Department partners with community and faith-based organizations to serve as trusted messengers and provide tailored and culturally resonant public health outreach to NYC communities.
Anyone can become very sick from COVID-19. To find a COVID-19 or flu vaccination site, visit nyc.gov/vaccinefinder or call 212-COVID-19 (212-268-4319).
#031-24
MEDIA CONTACT: Chantal Gomez [email protected]
Gomez, Chantal. “Health Department Finds Most Adult New Yorkers Infected with COVID-19 Experienced Symptoms Lasting One Month or Longer.” Health Dept. Finds Most Adult NYers Infected With COVID-19 Experienced Symptoms Lasting 1 Mo or Longer - NYC Health, NYC Health, 26 Dec. 2024, www.nyc.gov/site/doh/about/press/pr2024/nyc-adults-with-covid-19-experienced-symptoms-one-month-or-longer.page.
I’d like to highlight that date: December 26, 2024.
#op#links#usa#nyc#public health#covid#long covid#covid-19#sars-cov-2#sars cov 2#covid19#covid 19#long covid awareness#covid isn't over#still coviding#covid conscious#pandemic#coronavirus#covid pandemic#coronavirus pandemic#infectious disease#infectious diseases#disability#chronic illness#post-acute covid-19#covid cautious
50 notes
·
View notes
Text
Incubation Periods List
Hi all!
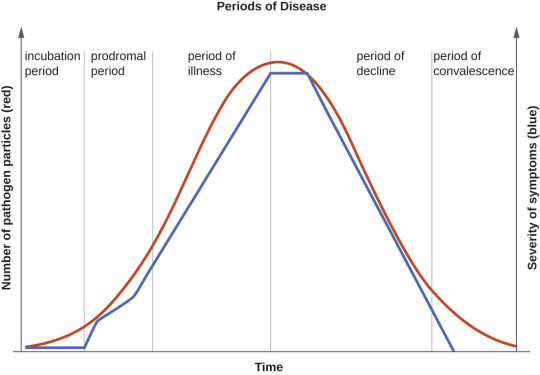
The following is a list of incubation periods for various infectious diseases for all your writing needs. An incubation period is the amount of time between exposure to an infectious agent (bacteria, virus, protozoa or prion) and the person having the first symptoms of the resulting illness. Knowing this is helpful in creating a timeline for your story.
Anthrax: Incubation period of 1-60 days
Avian Flu: Incubation period 3-9 days
Botulism: Incubation period 12-72 hours
Chikungunya: Incubation period 3-7 days
Chlamydia: incubation period 7-21 days
COVID-19: Incubation period 5-10 days
Creutzfeldt-Jacob Disease: Incubation period 10-20 years
Dengue: Incubation period 5-7 days
Diphtheria: Incubation period 2-5 days
Ebola: Incubation period 2-21 days
Hantavirus: incubation period 1-8 weeks
Hepatitis A: incubation period about 28 days
Herpes: Incubation period 2-12 days
Herpes Zoster/Varicella (Chickenpox): Incubation period 14-16 days
Herpes Zoster (Shingles): Incubation period- technically none, as this is a reactivation of the virus that causes chickenpox
HIB: Incubation period 2-10 days
HIV: Incubation period 1-6 weeks to prodrome, approximately 10 years to AIDS
Influenza: Incubation period 1-4 days
Legionnaires Disease: Incubation period 5-6 days
Leprosy: Incubation period 9 months to 20 years
Lyme Disease: Incubation period 3-30 days
Malaria: Incubation period 7-30 days
Measles: Incubation period 10-12 days
Meningitis, Bacterial: Incubation period 2-10 days
Meningitis, Viral: Incubation period 3-10 days
Monkeypox: Incubation period 1-2 weeks
Mumps: Incubation period 16-18 days
Norovirus: Incubation period 12-48 hours
Pertussis: Incubation period 7-10 days
Plague: Incubation period 2-8 days
Pneumococcal Pneumonia: Incubation period 1-3 days
Polio: Incubation period 7-10 days
Q-Fever: Incubation period 2-3 weeks
Rabies: Incubation period 20-90 days
RSV: Incubation period 4-6 days
Smallpox: Incubation period 7-17 days
Syphilis: Incubation period 10-90 days
Tetanus: Incubation period 3-21 days
Tuberculosis: Incubation period 2-10 days
Typhoid: Incubation period 6-30 days
Typhus: Incubation period 1-2 weeks
West Nile Virus: Incubation period 2-6 days
Yellow Fever: Incubation period 3-6 days
Zika: Incubation period 3-14 days
177 notes
·
View notes
Text
youtube
Dr. Anthony Fauci voluntarily testified before a House committee and debunked MAGA Republican conspiracy theories regarding the COVID-19 pandemic.
While Donald Trump and his lickspittles were telling Americans to drink bleach, take useless malaria pills, stick ultraviolet lights up their butts, and eat horse paste, Dr. Fauci headed an effort to develop vaccines for COVID-19.
A reminder to people with short memories who view the Trump administration as some sort of bucolic paradise: The last quarter of that administration included the worst government response to an infectious disease outbreak since 1920. Trumpsters who want us to ignore Trump's horribly botched response to the pandemic are like cruise-liner enthusiasts who want us to ignore the last 2% of the voyage of the Titanic.
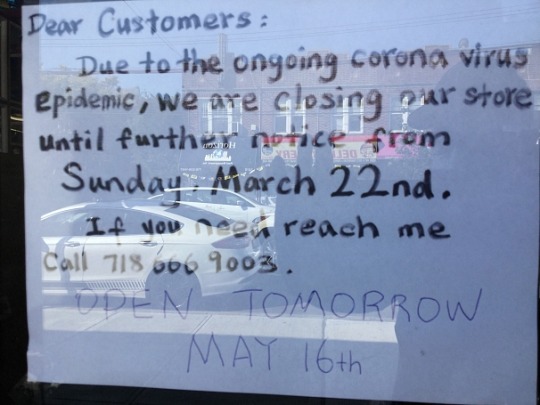
Economic activity ground to a halt in 2020 as the US slid into a recession. I took this picture of a sign at a dollar store which had been completely closed for almost two months.
The whole Trump clan was disdainful of the sacrifices hundreds of millions of Americans were making.
Why has the U.S. COVID-19 response been so bad? Jared Kushner, Vanity Fair suggests.
At Times Square Jared and Ivanka's contemptuousness was made into an ad before Election Day.

If you are looking for the Original Sin of Trump's pandemic response, it was on January 22nd when he basically told CNBC's Joe Kernen that COVID-19 was nothing to worry about.
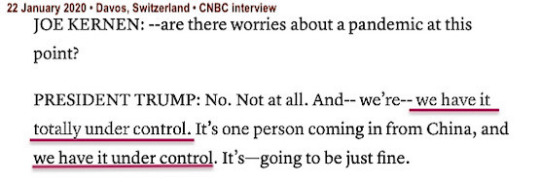
Of course it wasn't "just fine".
Trump did not declare a state of emergency for seven weeks. That gave the virus plenty of time for it to spread throughout the US.
Republicans know that their Dear Leader totally mishandled the pandemic response. That's why they repeatedly try to make Dr. Fauci a type of scapegoat for Trump's horrendous incompetence. Dr. Fauci has spent his entire career fighting disease. Donald Trump has spent his entire career narcissistically promoting himself.
Harry Truman had a sign on his desk saying: "The Buck Stops Here!" If Trump had a sign on his Oval Office desk (which he seldom used except for photo ops) it would be: "It's Everybody's Fault But Mine!"
Don't be hesitant to remind people of how awful 2020 was. And point the finger of blame at the orange blob who was responsible for the catastrophe.
#anthony fauci#covid-19#coronavirus#pandemic#infectious disease#us house of representatives#maga#republicans#marjorie taylor greene#conspiracy theories#donald trump#trump's botched pandemic response#jared kushner#the 2020 recession#lawrence o’donnell#raul ruiz#election 2024#vote blue no matter who
51 notes
·
View notes
Text
“If you ever prescribe an aminoglycoside, and the patient doesn’t come back complaining because it fucked up their digestion, it’s because they didn’t take it.”
60 notes
·
View notes
Text
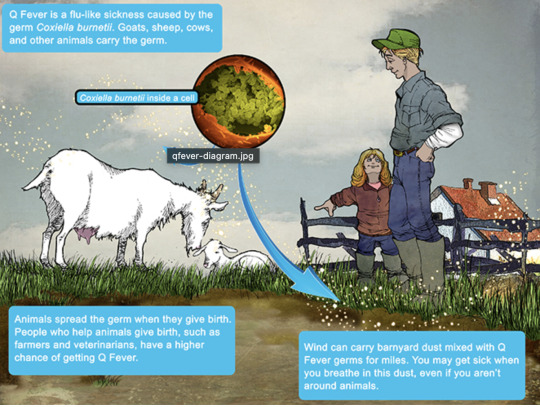
Q Fever
Aka, Query fever. What a weird name for a disease. Imagine telling people that's what you got.

in the 30s-40s, an Australian pathologist in QLD/Brisbane, came across an outbreak of the same or similar illness among abbatoir or slaughterhouse workers.
At the time, he called the disease "Q" fever or query as a temporary name until the pathogen could be identified. Unfortunately it stuck.
decades later, now nobel prize winner and virologist, MacFarlane Burnett isolated and identified the microbe responsible. I think this discovery contributed to his prize. i forget already.
Microbe responsible: Coxiella burnetti. Named for Burnett and HR Cox, the American bacteriologist who found the genus Coxiella where C burnetti falls under.
Initially they felt it was related to Rickettsia, responsible for Rocky Mountain Spotted Fever, but as science progressed, this was disproven.
Now for a Case Report
A 55 yo Italian man with a history of aortic valve replacement was diagnosed with pyrexia of unknown origin twice. Further signs included myalgias/splenomegaly/night sweats. The 2nd time he was admitted for PUO he deteriorated rather dramatically and was put on meropenem and teicoplanin.
A host of organisms was tested for on serological testing based on the man's travel and epidemiological history, all negative. Even a rheumatological panel was done, also less revealing. He also had a history of MGUS (a haem disoder), which is kind of a red herring here.
Cultures were negative, no vegetations were seen on a TTE - so they did consider IE. Which is an important differential for PUO.
Eventually a PET-CT was done (often favoured when investigations do not yield much for a sick patient with fevers), finally revealing a focus of infectious on his ascending aorta, where he'd also had previous surgery done. And in a round about way, they also further identified Coxiella Burnetti. He was treated doxycycline and hydroxychloroquine. As it's so rare in Italy, it wasn't really considered even though he mentioned rural travel.
Bottomline: Q Fever is an important consideration in the work up for culture negative IE. Further to this, always consider IE in the differentials for PUO particularly if they're at increased risk for IE (prosthetic valves, damaged valves, select congenital heart issues, previous IE). IE can present with night sweats, fevers, weight loss and splenomegaly. It can be insidious and chronic in nature. other risk factors can be more suggestive as we'll get into below.
Causative organism
Coxiella burnetti, it's a zoonoses - i.e. transmissible from animals. Special powers: very tough/hardy, can survive extreme environments (high temps and UV light etc.) over prolonged periods and is resistant to many common disinfectants/surface cleaners.
It's an intracellular pathogen and gram negative coccobacilli (PINK!)
name coccobaccili reminds me of cocopuffs.
it's mainly associated with farm animals, which the CDC so wholesomely displays on its website on Q fever (wtf).

goats, sheep, cattle typically (but many other animals, even birds, dogs and horses can be reservoirs)
in particular bodily fluids - amniotic fluid, placenta, faeces/urine, milk etc.
you can get it through unpasteurized milk and through inhaling it if it lands on dust in the area
ever visit a farm or petting zoo lately? OMG WASH YOU HANDS.

That said, it's typically inhaled in inorganic dust. You inhale it, it goes to the lungs, and then the bloodstream.
Increased risk for Coxiella burnetti (What to take on history of exposures and when to strongly consider it)
live on a farm or near one
exposure to a farm
work as a vet on a farm
farm worker, dairy workers, researchers on these animals/facilities
slaughterhouse/abbatoir
Also from CDC:
Clinical presentation
Most won't get sick after exposure and remain asymptomatic, a very small minority does. even though it is highly infectious.
incubation time is 2-3 weeks (consider this time in your history of exposure, did they work on the farm 2-3 weeks ago as opposed to yesterday).
Nonspecific acute infectious symptoms:
nonspecific systemic fevers/malaise/arthralgias/myalgias--> key is high fevers though and can be associated with headache and photophobia.
non specific GI - N/V/diarrhoea
respiratory ones - SOB or cough, consider it as atypical cause of community acquired pneumonia.
rare: hepatitis and jaundice (granulomatous) or encephalitis with neurological complications such as demyelinating disease or CN palsies, also haemolytic anaemia and HLH (yikes)

really it's the history of exposure that will lead you down the garden path to Q fever.
Chronic Q fever is perhaps worse, and can present as culture negative IE/PUO. Months/years later, as B symptoms as above above + LOW/LOA, night sweats. More likely to occur if you are predisposed for IE as above, have a weakened immune system for any reason, including pregnancy.
Chronic Q fever has a mortality of 10% if left untreated. About <5% of those with acute Q fever develop this if left untreated. Speculation is that it's more of an autoimmune process or abnormal immunological response to the bacteria.
To be honest, most who walk in the door with community acquired pneumonia get treated empirically for atypicals anyway, (standard course of doxycycline), so we hardly really ponder the question of Q fever in every patient. But if they present chronically and did not have atypical cover at the onset of acute symptoms, then it's something important to consider.
Other important conditions - can cause complications in pregnant women and 20% will get post Q fever syndrome. like chronic fatigue.
investigations
Serology! nice and easy. Look for IgG antibodies in the chronic presentation. Or PCR. Down side to serology - can take 2-3 days for the body to make said antibodies to the bacteria for detection. PCR can be done on any fluids/tissue sent.
Cultures useless, hence it fall under the umbrella of culture negative (hard to grow outside a host cell, it is an obligate intracellular pathogen).
Other hints on bloods (as serology/PCR takes time to return) - elevated or low platelet's, transaminitis with normal bili, opacities in CXR with hilar lymphadenopathy, CSF will show raised protein levels if done when encephalitis is suspected.
imaging can also support the diagnosis.. as illustrated by the case report.
Treatment
Acute disease - as standard for atypical bugs, doxycycline 100 mg BD for 14 days. Alternatives - TMP SMX or Clarithromycin.
Chronic Q fever or IE:
native valves: doxycycline and hydroxychloroquine (200 TDS) for 18 months
prosthetic: same but 24 months
why hydroxy: enhances the action of doxycycline (increases the pH of the phagolysosome)
Follow-up: look for 4 fold decrease in IGG
Sources:
CDC
Stat Pearls
Wiki as linked above
#australian history#medblr#medblrs#infectious disease#infectious diseases#q fever#coxiella#coxiella burnetti
75 notes
·
View notes
Text
Sometimes I think about that conversation I had in some breakroom somewhere that went something like:
Co-Worker: Man. Wouldn't it suck if there was a disease where you shit yourself to death? Me: ...There is. It's called cholera. Lots of people die of it every year.
And he was gobsmacked.
38 notes
·
View notes
Text




David Bruce – Scientist of the Day
David Bruce, a Scottish physician and microbiologist, died Nov. 27, 1931, at age 76.
read more...
#David Bruce#medicine#infectious disease#histsci#histSTM#19th century#history of science#Ashworth#Scientist of the Day
16 notes
·
View notes
Text
Grudgingly I had to give up dicking around on the Internet and go do some house cleaning. I'm listening to Mary Roach tell me about cholera dynamics when I remember, and I want to tell Tumblr—
Did you know that the same specialist predator/prey population dynamics over time that you usually see described in terms of Canadian lynx and snowshoe hare also apply perfectly well to Vibrio cholerae and its most common bacteriophage?
And that this is a major factor in why pathogenic cholera outbreaks — caused mostly by only one lineage of V. cholerae bacteria — eventually fade even if the population isn't wholly infected by cholera or wiped out by it?
The world is a wild and fascinating place.
49 notes
·
View notes
Text
People. Will. Die.
Continued cuts will kill people. Period. Full Stop. Please write your elected officials. Go to your University ombudsman. The targeted dismantling of medical research will negatively impact us all.
4 notes
·
View notes
Text

The Last of the Famous International Playboys |2024| continuing...
#photography#the last of the famous international playboys#2024#infectious disease#syphilis#psa#get tested#uw medicine#south lake union#penicillin#ouch#personal
7 notes
·
View notes
Text
Q. When is a follow-up chest x-ray indicated after treatment for pneumonia?

A. Get AP and lateral chest xrays if the patient hasn't improved after 48-72 on the appropriate antibiotics, or in 4-6 weeks if there is recurrent pneumonia in the same location or complications such as abscess or empyema. Otherwise, no need for a "test of cure." Patients at risk of lung cancer due to smoking history should have targeted screening. Image of pleural effusion by Ian Bickle (Radiopaedia).
5 notes
·
View notes
Text
Hey guys ALERT! im leaving for florida on friday and um you may be aware that pesky mod black has been on vacation so i was taking over bt UM! yah i have to pack and stuff so there might not be a weekly this week and if there is one please forgive me it might be like. just doodle dump or something😓unless she cook but me i do not want to stress her since i have more free time
but i think i can start cooking today and tomorrow cause i have to lock in and pack thursday night mostlyu
Tabby im coming tabby watch out tabby ima see you tabby ima equius up this nepeta....🐱👤 @rabbitsdontstarve WATCH OUT!
#mod cheren#update#also um next week idk wat doing cause me ima be busy AF!#ALSO I HAVETO WAKE UP AT LIKE 5 AM BRO#ive been drawing one million trollified version of them so...if that does not interest you....my sincerest apologies.#tabby#florida!tom x california!tabby au#starbucks vanilla frappuccino chilled coffee drink#airport#infectious disease
5 notes
·
View notes
Text

Jerk it, MAGA.
#MAGA#MAGAts#anti-vaxxers#anti-vaxxers murder children#polio#infectious disease#vaccinations#Donnie D-Cups#Fuckstick von Clownface#RFK Jr
2 notes
·
View notes
Text
“Vancomycin is a bad antibiotic, get over it.”
#medicine#med school#medblr#antibiotics#infectious disease#vancomycin#you know since it has bad tissue distribution#takes ages to start having an effect#you have to adjust dose according to blood concentration#etc#will i prescribe it in a heartbeat if i suspect mrsa? of course#but you only use it because it’s what you have
28 notes
·
View notes
Text
A thought, regarding Cujo: I think Donna's apparent symptoms of rabies at the end were psychosomatic.
Cujo's rapid infection is just barely within the bounds of plausible, but Donna's next-day symptoms and later recovery aren't. She also doesn't actually display normal human symptoms of rabies, in particular biting the paramedic: the urge to bite things doesn't really show up in rabid humans. If rabies causes aggression in humans at all, they display it via the usual human means of expressing aggression, such as using fists or their voice.
She does, however, display stereotypical canine symptoms of rabies. Donna doesn't really know how rabies works, medically, but she has a common knowledge understanding of it combined with the hellish example Cujo set. After the horrific experience she just went through, she loses it from stress and trauma and temporarily embodies what her subconscious thinks is happening. For a little while there, she believed her rage was coming from a rabies infection, and her mind made it real.
The paramedic she bit went through the rabies treatment course because you do not fuck around with rabies and he did get bitten by someone who might have been rabid, but the treatment Donna got was in fact the normal rabies immune globulin and vaccination course, along with treating her wounds.
#original posts#what's up I just read the book#waiting for the film to come in from one of the other libraries in my local library system#stephen king#cujo#meta#rabies#infectious disease
14 notes
·
View notes
Text



Carlos Chagas – Scientist of the Day
Carlos Chagas, a Brazilian clinical physician and microbiologist, died Nov. 8, 1934, at the age of 55.
read more...
#Carlos Chagas#microbiology#infectious disease#histsci#histSTM#20th century#history of science#Ashworth#Scientist of the Day
28 notes
·
View notes