#Diabetic health
Explore tagged Tumblr posts
Text
Top Benefits of Diabetes Holistic Care in San Antonio for Effective Management

Diabetes management is evolving, with more people turning to holistic care to complement traditional treatments. Holistic care focuses on addressing the whole person—body, mind, and lifestyle—rather than just the symptoms. For residents seeking diabetes holistic care in San Antonio, this approach can offer numerous benefits, from better blood sugar control to improved mental well-being. Let’s explore the top benefits of holistic care and why it's a growing choice in San Antonio.
Improved Blood Sugar Control
The primary goal of diabetes care is to keep blood sugar levels within a healthy range. Holistic approaches, such as dietary adjustments and stress management, help reduce blood sugar fluctuations.
Nutrient-Rich Diets: Holistic care promotes a balanced diet focused on whole foods, fiber, and low glycemic index items that naturally stabilize blood sugar.
Regular Exercise: Incorporating regular physical activity, from walking to yoga, improves insulin sensitivity and glucose absorption.
Enhanced Mental Health and Reduced Stress
Mental health plays a significant role in managing diabetes effectively. Chronic stress can increase blood sugar levels, which makes it challenging to manage diabetes.
Stress Reduction Techniques: Many holistic care practices, like meditation and deep breathing, reduce stress and support blood sugar stability.
Better Mood and Focus: Mindfulness and relaxation exercises help improve mental clarity, making it easier to follow diabetes care routines.
Personalized Care Tailored to Individual Needs
One of the strengths of diabetes holistic care in San Antonio is its adaptability to each person’s needs. Holistic practitioners consider personal health goals, lifestyle, and challenges to create a tailored diabetes management plan.
Customized Nutrition Plans: Holistic nutritionists can design a meal plan that meets dietary preferences and health needs.
Exercise Programs: Tailored programs can accommodate fitness levels and goals, ensuring exercise is enjoyable and sustainable.
Promotes a Sustainable Lifestyle Change
Unlike quick fixes, holistic care focuses on long-term, sustainable changes that improve overall health. Adopting this approach promotes consistency and long-lasting results.
Healthy Habits: Building a routine around balanced meals, physical activity, and self-care contributes to lasting lifestyle changes.
Motivation and Support: Holistic practitioners often work closely with clients, providing ongoing support to help maintain positive habits.
Encourages Natural Healing
Holistic care includes natural methods like herbal supplements, acupuncture, and massage therapy, which are designed to support the body’s natural healing processes.
Herbal Supplements: Herbs like fenugreek and cinnamon may improve insulin sensitivity when used alongside traditional treatment.
Alternative Therapies: Acupuncture and massage therapy can reduce stress and pain, which are common among those managing diabetes.
Focus on Preventative Care
Preventing complications is essential in diabetes management. Holistic care’s emphasis on overall well-being helps minimize risks associated with high blood sugar, such as heart disease and neuropathy.
Healthy Lifestyle Choices: Encouraging a diet rich in vitamins and minerals, regular exercise, and avoiding harmful habits are core to holistic care.
Regular Monitoring: Many holistic practitioners emphasize consistent monitoring of blood sugar, which helps detect early signs of complications.
Supports a Healthy Immune System
People with diabetes are often more susceptible to infections and slower healing. Holistic practices, such as dietary adjustments and stress management, can strengthen the immune system, offering better protection against infections.
Nutritional Support: Eating a variety of fruits, vegetables, and proteins strengthens immunity.
Reduced Inflammation: Exercise, a balanced diet, and stress reduction naturally lower inflammation, supporting immune health.
Where to Find Holistic Diabetes Care in San Antonio
San Antonio offers various resources for those seeking holistic diabetes care. Wellness centers, specialized health clinics, and individual practitioners offer services tailored to diabetes management.
Wellness Centers: These centers often combine multiple services, from nutrition counseling to acupuncture, providing comprehensive care.
Licensed Holistic Practitioners: Nutritionists, herbalists, and fitness experts in San Antonio can work together to design a diabetes holistic care plan that meets individual needs.
FAQs on Diabetes Holistic Care in San Antonio
Q1: Can holistic care replace my diabetes medication? No, holistic care complements but does not replace diabetes medication. Always consult your healthcare provider before making any changes to your treatment plan.
Q2: Is exercise necessary for holistic diabetes care? Yes, physical activity is a vital part of holistic care as it helps regulate blood sugar, improves insulin sensitivity, and supports overall health.
Q3: Are herbal supplements safe for diabetes management? Some herbal supplements may support blood sugar management, but consult a healthcare professional to ensure they’re safe and effective alongside your medication.
Q4: How often should I see a holistic practitioner for diabetes care? Regular visits every 4-6 weeks are beneficial for monitoring progress, adjusting plans, and addressing any challenges.
Q5: What should I look for in a holistic care provider? Look for certified professionals with experience in diabetes care, such as registered dietitians, licensed acupuncturists, or naturopathic doctors, who have a deep understanding of diabetes holistic care in San Antonio.
Conclusion
Holistic diabetes care offers multiple benefits that support long-term health and improved blood sugar management. With a focus on lifestyle changes, stress reduction, and natural therapies, this approach is gaining popularity among people in San Antonio. By embracing a holistic approach, individuals can experience a higher quality of life, reduced stress, and an empowered approach to managing diabetes.
0 notes
Text
Diabetic retinopathy is a potentially blinding complication of diabetes that causes damage to the retina. Diabetes is a disease where there are high blood sugar levels, which can cause damage to blood vessels throughout your body. In the retina, diabetes can affect the tiny blood vessels that nourish it. When the vessels are damaged, they can leak serum, blood, and lipids into the retina, distorting vision. This eye disease will affect almost 80% of those who have had diabetes for at least 20 years and is the leading cause of blindness in individuals, aged 20-64.
#diabetic retinopathy#diabetic#diabetes#eye care#diabetic health#eye health#northeast ohio eye surgeons
0 notes
Text
Embracing Change: A Personal Update on My Diabetes Journey
Hey everyone! 🌟 I've been away focusing on my health, but I'm back with a new routine and feeling great! Check out my latest blog post for the full update and more diabetes tips. 💪✨ Read more 👉 #DiabetesJourney #HealthUpdate
Hey everyone, I wanted to address the gap in my blog posts. Recently, my diabetes management took a hit, and I needed to refocus on my health. Managing diabetes is a full-time job, and sometimes, even the most dedicated need to recalibrate. I’ve started a new routine and sought additional help. I’m happy to report things are improving, and I’ll be back to sharing insights and tips…
#Blood Glucose#Blood Sugar Balance#Diabetes Management#Diabetes Support#Diabetic Experiences#Diabetic Health#Health and Wellness#health update#Insulin Management#Lifestyle Management#Managing Diabetes#Mood Swings#new routine#personal health journey#Personal Narrative
0 notes
Text
If you have diabetes, you should have your eyes examined at least once a year by the ophthalmologists at the Cleveland Eye Clinic.
0 notes
Text
A new treatment combining ReCET and semaglutide could eliminate the need for insulin in type 2 diabetes, with 86% of participants in a study no longer requiring insulin therapy. The treatment was safe and well-tolerated, and further trials are planned to confirm these results.
Groundbreaking research presented at UEG Week 2024 introduces a promising new treatment approach for type 2 diabetes (T2D) that has the potential to greatly reduce or even eliminate the need for insulin therapy.
This innovative approach, which combines a novel procedure known as ReCET (Re-Cellularization via Electroporation Therapy) with semaglutide, resulted in the elimination of insulin therapy for 86% of patients.
Globally, T2D affects 422 million people... While insulin therapy is commonly used to manage blood sugar levels in T2D patients, it can result in side effects... and further complicate diabetes management. [Note: Also very importantly it's fucking bankrupting people who need it!!] A need therefore exists for alternative treatment strategies.
Study Design and Outcomes
The first-in-human study included 14 participants aged 28 to 75 years, with body mass indices ranging from 24 to 40 kg/m². Each participant underwent the ReCET procedure under deep sedation, a treatment intended to improve the body’s sensitivity to its own insulin. Following the procedure, participants adhered to a two-week isocaloric liquid diet, after which semaglutide was gradually titrated up to 1mg/week.
Remarkably, at the 6- and 12-month follow-up, 86% of participants (12 out of 14) no longer required insulin therapy, and this success continued through the 24-month follow-up. In these cases, all patients maintained glycaemic control, with HbA1c levels remaining below 7.5%.
Tolerability and Safety
The maximum dose of semaglutide was well-tolerated by 93% of participants, one individual could not increase to the maximum dose due to nausea. All patients successfully completed the ReCET procedure, and no serious adverse effects were reported.
Dr Celine Busch, lead author of the study, commented, “These findings are very encouraging, suggesting that ReCET is a safe and feasible procedure that, when combined with semaglutide, can effectively eliminate the need for insulin therapy.”
“Unlike drug therapy, which requires daily medication adherence, ReCET is compliance-free [meaning: you don't have to take it every day], addressing the critical issue of ongoing patient adherence in the management of T2D. In addition, the treatment is disease-modifying: it improves the patient’s sensitivity to their own (endogenous) insulin, tackling the root cause of the disease, as opposed to currently available drug therapies, that are at best disease-controlling.”
Looking ahead, the researchers plan to conduct larger randomized controlled trials to further validate these findings. Dr. Busch added, “We are currently conducting the EMINENT-2 trial with the same inclusion and exclusion criteria and administration of semaglutide, but with either a sham procedure or ReCET. This study will also include mechanistic assessments to evaluate the underlying mechanism of ReCET.”
-via SciTechDaily, October 17, 2024
--
Note: If it works even half as well as suggested, this could free so many people from the burden of the ongoing ridiculous cost of insulin. Pharma companies that make insulin can go choke (hopefully).
#would be super interested to hear from people with expertise in the area about how this sounds#obviously it's a small sample size#but they're going to do more trials#and LOOK at that effectiveness rate#insulin#diabetes#healthcare#medicine#diabetic#type 2 diabetes#public health#medical news#good news#hope
3K notes
·
View notes
Text
The Dexcom G6
There’s plenty of different ways and plenty of different brands of glucose monitors to help you keep track of your blood sugar. The Freestyle Libre is a pretty insurance friendly choice and a quick go to for many diabetics both type 1 and type 2.
But for those who can afford it, I use and recommend the Dexcom G6. It’s a wonderful setup that I’ve used twice in two different periods of my diabetic journey. I mention this because I’ve had two very different experiences with it based on my knowledge at the different points in time.
For beginners - I don't actually recommend using this if you’re only just starting out as a diabetic. While it is an amazing tool for later use, there is a catch to it. See, it reports your glucose levels in intervals of somewhere between fifteen to twenty minutes. On top of that it can take up to thirty minutes for insulin to kick in. As a beginner I found it very easy to “chase” after perfect numbers. I’d take medicine, get impatient, take even more, send myself into hypoglycemia, eat way too much and wind up with high blood sugar, then repeat the cycle. Be wary of this.
For average to experienced diabetics - Its amazing. Get it, use it. It’s a great way to avoid the constant pricking of your fingers. To stop being frustrated over how calloused your fingertips are getting and making it harder to draw blood. As a more experienced diabetic who understands better how insulin works now, my A1C has never been better than my second time using the Dexcom. Some perks to the Dexcom: 1. You can either use the App, or the hand held device delivered with your first package. I personally use the hand held device, as it’s more accurate and more easily picks up the signal from the monitor.
2. Super easy to charge. Comes with its own adapter and cord, and it doesn't even take two hours to fully charge it.
3. It’s water resistant! It’s waterproof up to a point, but best not to push its limits. However for just taking a bath or shower, or taking a normal swim in a pool, this thing will last you without issue. The adhesive is pretty good, though it can come slightly loose from hot water. However, its never come loose enough to ever be an issue for me.
4. If you miss one alert, it’s relentless in making sure you’re made aware. Especially good if you’re a heavy sleeper, if you miss an alert, every five minutes or so it will alert you again, while also progressively beeping louder each time. It gives me a lot of peace of mind for if my blood sugar dips during the night while i’m asleep. (I speak only for the handheld, as I’ve never tried the app. I dont know if the app also does this.)
5. Simple and easy applicator. I admit I’ve never used any other auto glucose monitor other than the Dexcom, but the applicator makes it so easy to put on. Do you feel it? Yes. But It feels like an itch, not painful and never has been for me.
6. It can later be used in conjunction with an insulin pump. I dont have any experience in this, as I still manually inject my insulin, but its a cool feature nonetheless.
Pretty awesome right? But it can be a little confusing when you first get the kit, so let me give you a nutshell layout of all the parts and what they do!

This is the applicator. You don't have to load anything into it. There is a number on the bottom on some paper that you use to help link it to your handheld device. But after removing that, all you do is take that orange tab off, press it to wherever you want your patch to be, then press the button! It inserts the sensing needle in flawlessly. I recommend rubbing along the adhesive to make sure it sticks well after using the applicator. The patch lasts ten days before needing replaced. Each applicator is only good for one use, then you discard it.

Here’s your transmitter. This tiny part is what takes the info from the patch/sensing needle, and as per its name, transmits it to your handheld/app. This piece is not automatically in the patch when you apply it to your body. You have to push it into the patch after application until it clicks. Doesn’t hurt in the slightest. It lasts for three months and can be reused until then. The patch, once taken off, can bend at a certain spot to easily remove the transmitter for the next patch.

Here’s a quick photo of what it looks like when the transmitter is locked into place inside of the patch. Warning! The adhesive can itch if you’re sensitive like me! I used to think this might be the needle poking me but trust me, that needle is not moving.
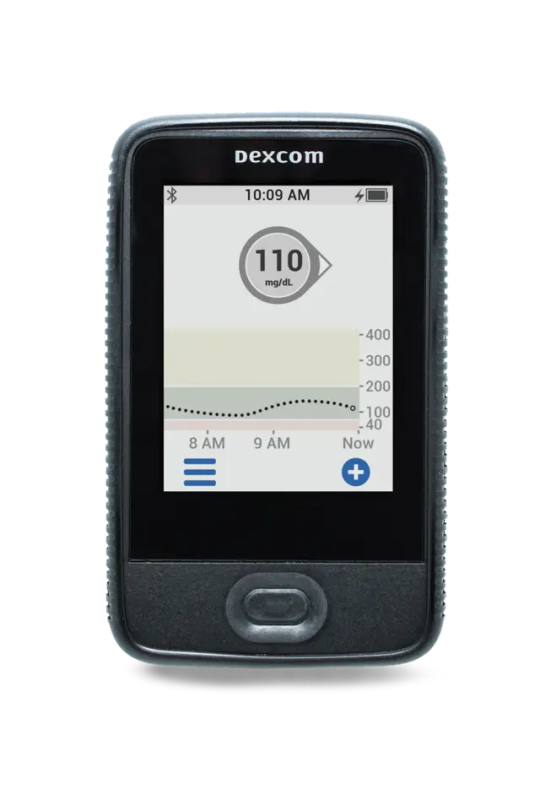
Here is the handheld device that comes with your supplies! I can personally attest that everything about this device appears as you see it in the picture. It shows you your last reported numbers, what time they’re recorded, and the arrow next to your number tells you if you’re headed up, down or steady. When setting it up it’ll ask you for basics like date and time, but it also asks you what you consider to be high blood sugar and low blood sugar, making it pretty easy to set goals for yourself as you slowly work to better control your blood sugar. I personally use the default settings. Anything below 70 is too low, and anything above 200 is too high. I still aim to stay within 90 to 150, but 200 is a good max limit I have for myself.
Something to know now that you know all your pieces; when setting up your Dexcom for the first time, it asks for a number, found either on the outside of the box, or on the bottom of the transmitter. Use the transmitter because there are at least four different numbers on the box your stuff comes in. There is only one number on your transmitter and that is the number you’re looking for. Makes it a lot easier. You’ll have to repeat this process every three months when you get a new transmitter.
To nutshell my nutshell, the only numbers you will need to be concerned with are:
The number found on the flat bottom side of your applicator, used when setting up each patch every ten days.
The number on your transmitter, used during first setup and then every three months.
Other than those, you don't need worry about any other numbers you see or find on boxes. You don’t even need to keep the boxes, though I tend to for easy storage of my applicators.
Another thing to note is that they send you 3 months worth at a time, so it’s easy to keep track of when you need a new transmitter. You need it when you simply run out of your whole batch of applicators.
And last thing I’ll say! As of this post there is a newer Dexcom out there, one meant to be worn on your arm rather than your belly. I have not used this and have no knowledge of how similar it may be to the Dexcom G6. Any questions on that should be sent to your doctor or endocrinologist.
DISCLAIMER: As always I am not a doctor or licensed medical professional. These are simply my experiences and observations as a type 1 Diabetic. You’re welcome to ask me about my experiences and personal journey but for any serious issues please seek professional help from your doctor or endocrinologist.
#keto#health#type one diabetes#diabetes#Dexcom G6#TT1#type 2 diabetes#type 1 diabetes#glucose monitor#Type two diabetes#Diabetic health
1 note
·
View note
Text
Healthcare can be expensive depending on the country you live in, but it is impossible to attain when you live in a country/place where no doctors can perform the procedures that you need. It may be due to lack of equipment, lack of specialized doctors, or no hospitals at all.
I am raising $ for my friend's mother Nabila @nabila60 This is urgent. Her life is at risk RIGHT NOW and we don't know how much longer she can hold on without treatment. If you answered this poll, please reblog it to reach more people. If you have ever had expensive hospital visits, please show sympathy to a mother who will die without treatment. You can save a life! Every donation counts.
#vetted by 90 ghost#vetted by association#im sure other people vetted her but i havent checked the spreadsheets in a bit#palestinian#free gaza#free palestine#vetted fundraisers#hospitals#medication#cost of living#diabetic#palestine#anti capitalism#healthcare#health and wellness
1K notes
·
View notes
Text

So much heavy lard keeping me trapped to the bed
#death feedee#death feederism#fat girls#death feedist#dying from obesity#extremely obese#fattened to death#fatty piggy#feedee encouragement#feedee feeder#obese feedee#sexy obese#obese gainer#obese belly#obese piggy#fat cow#feedee piggy#greedy piggy#female death feeder#ssbbw feedee#feedee girl#diabetic feedee#health issues#dumb wh0re#glorify obesity
532 notes
·
View notes
Text

In the 5th century BCE, Sushruta, a renowned Indian surgeon, first identified diabetes by observing that diabetics’ urine attracted ants due to its sweetness. He noted that the condition primarily affected wealthier individuals and linked it to a diet high in rice and sweets.
163 notes
·
View notes
Text

#chronic illness#actually chronically ill#chronic illness memes#chronic fatigue#chronic pain#health issues#long haul covid#long covid#covid19#type one diabetes#type one diabetic#actually diabetic#I AM TIRED OF BEING SICK AND TIRED!!#dysautonomia
1K notes
·
View notes
Text
I created a GFM for a dental emergency. 🦷🚨
I have a bit of a predicament, guys. Spanning the past two years — and I cannot take it anymore.


I never ask for help like this, but this is getting more serious than I can handle anymore on my own. If you have the time to check this out, **even if all you can do is share this post to get it around on Tumblr, I'd appreciate that. Please and thank you!
#black tumblr#black twitter#go fund me#gfm#type 1 diabetes#type 1 diabetic#fundraiser#donations#oral surgery#dental hygiene#wisdom teeth#signal boost#us healthcare system#dental health#us health insurance#dental pain#tooth extraction#oral surgeon#mutual aid#community support#t1d#blm#gofundme#go fund her
145 notes
·
View notes
Text
We ask your questions so you don’t have to! Submit your questions to have them posted anonymously as polls.
#polls#incognito polls#anonymous#tumblr polls#tumblr users#questions#polls about language#submitted may 29#health#diabetes
153 notes
·
View notes
Text
Feasting with Finesse: Preparing for Thanksgiving with Diabetes
🍂 Navigating Thanksgiving with diabetes? Join me on 'Beyond The Blood Sugar' as I share tips for a worry-free holiday feast that's both delicious and diabetes-friendly. 🍂
As the leaves turn and the air chills, Thanksgiving approaches with the promise of warmth, gratitude, and, of course, a bounty of food. For those of us managing diabetes, this holiday can bring its own set of worries – will I be able to enjoy the feast without throwing my blood sugar out of whack? But fear not! With a pinch of planning and a spoonful of strategy, we can savor the Thanksgiving…
View On WordPress
#Active Holidays#Blood Glucose#Blood Sugar Balance#Carb Counting#Diabetes Management#Diabetes Support#Diabetes-Friendly Recipes#Diabetic Experiences#Diabetic Health#Gratitude and Health#Health and Wellness#Healthy Thanksgiving Tips#Holiday Eating#Insulin Management#Lifestyle Management#Mindful Eating#Mood Swings#Personal Narrative#Thanksgiving Preparation#Turkey Talk
0 notes
Text
Every year all of the big diet companies have to come up with some brand new labeling for their plans in order to encourage people to get on the January weight loss train.
This year, Weight Watchers is going further than they’ve ever gone before, by announcing that they have created a new system to give their members access to prescriptions for drugs like Ozempic and Mounjaro.
Let me remind you that these drugs only work while you’re taking them. As soon as you stop, all of your appetite comes back. Your desire to eat returns, and because it has been artificially suppressed it may feel much stronger and less controllable than it was before you took the drugs. Many people who come off these drugs, usually because of cost (because insurers are balking at coverage for weight loss) or shortages (because so many people are taking them for weight loss, which is leaving the diabetics who need them up shit creek) or side effects report that the first weeks are really difficult, mentally painful and often binging occurs.
Additionally, all of these drugs carry a real risk of creating a terribly painful and potentially deadly condition called Gastroparesis, in which your gastrointestinal system just stops functioning, you cannot digest and process food at all.
You do not need to lose weight to be healthy. You do not need to lose weight to be beautiful or attractive, to have success, or love. You do not need to lose weight in order to pursue fitness. If you have particular health needs or goals that can only be achieved by changing the way you eat, (e.g. lowering cholesterol or blood glucose or addressing gastro issues) that does not mean that you need a weight loss diet plan, just one designed toward your needs.
But more than anything, you do not ever need to put another penny into the coffers of the multibillion dollar weight loss industry, which, if it actually had a way to take a fat person and make them thin permanently (something that cannot even be achieved by surgeries that drastically rearrange digestive systems) would be a multi quadrillion dollar industry instead. 
#cw: weight loss#cw: weight loss drugs#weight watchers#ozempic#mounjaro#diabetes drugs for fat people#new year new you old bullshit#health at every size#fatphobia
393 notes
·
View notes
Text
"A 25-year-old woman in China is the first person worldwide to have type 1 diabetes reversed through stem cell therapy.
The therapy used the patient’s own cells to create personalized stem cells, which were then used to grow fresh insulin-producing islets.
This breakthrough offers hope for millions with diabetes, potentially eliminating the need for daily insulin injections and reducing complications.
In a groundbreaking medical achievement, a 25-year-old woman in Tianjin, China, has had her type 1 diabetes reversed through a novel stem cell therapy. This marks the first time such a feat has been accomplished globally, offering new hope for millions living with the chronic condition.
The patient, who had been struggling with type 1 diabetes, underwent a pioneering treatment that involved converting her own cells into personalized stem cells. These stem cells were then used to grow fresh clusters of ‘islets,’ the hormone-producing cells in the pancreas responsible for regulating blood sugar levels.
As Nature reports, this therapy’s unique approach of transplanting the newly created islets into the patient’s upper abdomen near her pancreas sets it apart from previous islet transplant methods. This strategic placement allows for easier monitoring via MRI, a significant advantage over traditional liver transplants.
“I can eat sugar now,” the woman said on a call with Nature. After over a year since the transplant, she says, “I enjoy eating everything — especially hotpot.” The woman asked to remain anonymous for privacy reasons.
Experts are astonished at the results, according to Timesnownews. “They’ve completely reversed diabetes in the patient, who was requiring substantial amounts of insulin beforehand,” said Dr. James Shapiro, a transplant surgeon and researcher at the University of Alberta in Edmonton, Canada.
The implications of this breakthrough are far-reaching, as it could potentially revolutionize the way we treat diabetes. By using a patient’s own cells to create personalized stem cells, this therapy bypasses the limitations of donor islet shortages and the need for immunosuppressive drugs, which have hindered the success of conventional transplant methods.
‘If this is applicable to other patients, it’s going to be wonderful,’ diabetes researcher Daisuke Yabe of Japan’s Kyoto University told reporters via Daily Mail.
As the world watches closely, the success of this case sparks hope for the millions of individuals living with type 1 diabetes. It represents a significant step forward in regenerative medicine and paves the way for further research and development in the field."
-via Gadget Review, September 30, 2024
#diabetes#type 1 diabetes#stem cell therapy#stem cell treatment#stem cell research#china#asia#medical news#public health#good news#hope
2K notes
·
View notes
Text
The levels of caffeine in your blood could affect the amount of body fat you carry, a factor that in turn could determine your risk of developing type 2 diabetes and cardiovascular diseases. Those are the findings of a 2023 study that used genetic markers to establish a more definitive link between caffeine levels, BMI, and type 2 diabetes risk.
Continue Reading.
70 notes
·
View notes