#Cervical Spondylotic Myelopathy Treatment
Explore tagged Tumblr posts
Text
Pinched Nerve in The Spine: Radiculopathy - Symptoms, Causes, and Treatment
The spine consists of several individual bones known as vertebrae. These are interconnected together to form the spine. The spinal cord passes through a central canal in these vertebrae. From the spinal cord, the splitting of nerve roots occurs.
These roots travel between the bones of the spinal and different parts of the body. When the nerve root that leaves the spinal cord to other body parts becomes pinched, irritated, or damaged, it results in a medical condition known as radiculopathy. This condition is also known as a pinched nerve.

Types of Radiculopathy
Depending on where the condition happens in the spine, there are three types of radiculopathy. The symptoms of these types may range from mild to severe in individuals.
Cervical radiculopathy
Occurs due to pressure and compression of the nerve roots in the neck.
This portion of the spinal cord mainly affects the hands, arms, fingers, and shoulders.
Symptoms are usually visible in the hands and arms, which may include weakness or loss of sensation.
Lumbar radiculopathy
Occurs due to pressure and compression of the nerve roots in the lower back.
It may lead to sciatica, a condition that involves radiating pain in the sciatic nerve.
Thoracic radiculopathy
Occurs due to pressure and compression of the nerve roots in the upper back.
Chest pain is common in this condition.
There is a feeling of numbness and pain that moves to the front of the body in patients.
Causes of Radiculopathy and Risk Factors
Here are some of the commonly known causes of radiculopathy and the risk factors associated with it.
Change in size or shift in position of the tissues that surround the nerve root.
Herniated discs, also known as slip discs, are caused by to rupture of soft pads between spinal bones.
Bone spurs, bony outgrowths or projections resulting in constriction of the spinal passage. a condition in which the spaces within the spine get narrow.
Spondylosis is a wear and tear of the spinal disc with age.
Spondylolisthesis is a condition in which a vertebra slips out of its normal position onto the bone below it.
Spinal stenosis, narrowing of the spinal canal in the lower back.
Sciatica is pain travelling along with the sciatic nerve moving to the back of the thigh into the legs.
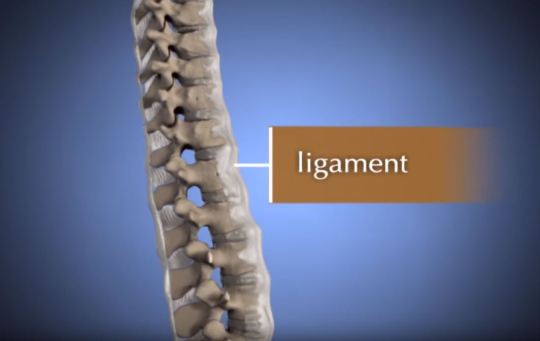
Thickening of spinal ligaments.
Spinal infections
Regular improper movements
Cancerous or non-cancerous growth in the spine
Radiculopathy Diagnosis
The diagnosis of radiculopathy begins with the patient giving a brief of their medical history to the doctor.
The doctor will ask questions about the type of symptoms, location of the pain, for how long has the pain been there, and also any other medical conditions which the patient is suffering from.
Once the medical history is known, the physician conducts a physical examination and tests.
This is to check the patient's muscular strength, reflexes, sensation, and also the possibility of any abnormalities.
Physical examination allows the medical practitioner to know the severity of the radiculopathy condition.
It also gives an idea about the location of the nerve root that is affected.
In some cases, radiculopathy diagnosis may require the use of advanced imaging techniques such as CT scan or MRI.
These tests aid in improving the visualization of the area where the problem lies.
In some cases, an expert like Dr Khanna orthopedic surgeon may also conduct a study on nerve conduction or Electromyography (EMG).
These tests help to know whether there is damage to the nerve or the problem is muscular.
Symptoms of Radiculopathy
The pinched nerve roots quickly become inflamed, which may result in the following symptoms:
Shooting pain in the back, legs, arms, and shoulders
Feeling of numbness and tingling sensation in the arms and legs.
Localized neck and back pain
Sharp pain when sitting idle or coughing
Sharp pain with movement
Hypersensitivity
Loss of sensation
Radiating pain in the shoulders
Skin numbness
Muscular weakness
Loss of reflexes
Sciatica
Non-surgical treatment for Radiculopathy
Conservative treatment is usually recommended before surgery. Here are some of the non-surgical treatment options for radiculopathy.
Physical therapy to strengthen the areas of pain.
Limitation or complete elimination of activities that cause radiculopathy pain and stains of the back and neck.
Immobilizing the affected area with
#Spine Care Specialists Indiana#Dr Khanna Orthopedic Surgeon#Orthopedic Spine Surgeon Munster#Minimally Invasive Lumbar Surgery Indiana#Neck Pain Treatment Munster#Best Spine Surgeon Indiana#Back Pain Treatment Munster#Osteoporosis Treatment Munster#Cervical Spondylotic Myelopathy Treatment#SI Joint Dysfunction Treatment#Sacroiliac Joint Dysfunction Treatment#Radiculopathy Treatment Munster#Spinal Stenosis Treatment Indiana#Lumbar Laminectomy Surgery Munster#Spondylolisthesis Treatment Munster#Spinal Cord Injuries Treatment Munster#Orthopedic Spine Specialist Indiana#Orthopedic Doctors in Munster Indiana#Best Orthopedic Doctors in Northwest Indiana#Back Pain Doctor in Northwest Indiana#Spine Treatment Indiana#Orthopedic Surgeon in Munster#Spine Doctors Indianapolis#Spine Surgery Indianapolis#Pain Management Munster Indiana#Cervical Disc Replacement Near Me#Cervical Disk Replacement Surgery#Minimally Invasive Surgery Indiana
2 notes
·
View notes
Link
#cervical spondylotic myelopathy#cervical spondylotic myelopathy symptoms#cervical spondylotic myelopathy treatment#cervical spondylotic myelopathy surgery
1 note
·
View note
Link
Spondolysis or Cervical Spondolysis is a medical condition which was once related to age. However, the scenario has completely altered now. For more information, just read our blog now.
#spondylotic changes#spondylosis#cervical spondylosis treatment#cervical spondylosis symptoms#spondylosis treatment#spondylosis neck#spondylosis causes#cervical spondylosis headache#cervical spondylotic myelopathy#cervical spondylosis with radiculopathy#degenerative spondylosis#cervical spondylosis surgery#neck collar for cervical spondylosis#cervical spondylitis treatment#early cervical spondylosis#cervical and lumbar spondylosis#cervical spondylosis exercise#exercises for cervical spondylosis#dizziness with cervical spondylosis
0 notes
Photo

On the 🎙with Dr. Rory Murphy, neurosurgeon at @barrowneuro, and Dr. Benjamin Davies & Iwan Sadler, founders of myelopathy.org @cervicalmyelopathy. We discussed the importance of visuals in patient education, the unfortunate lack of reliable information on Cervical Spondylotic Myelopathy (CSM), and how Dr. Murphy is showing illustrations and animations to his patients with CSM to help fill the knowledge gaps—since cervical myelopathy can lead to permanent spinal cord injury and paralysis if left untreated, it’s critically important that patients understand the nature of the disorder and available treatment options. Please check out myelopathy.org, link in my bio, and help raise awareness of CSM. The podcast will be available soon. #visualeducation #medicalillustration #patienteducation #myelopathy #awareness #spinalcordinjury #medicalanimation #visualartist #educational #resources #medicalart #cervical#spine #stenosis #spinalcord #disorder (at Barrow Brain and Spine) https://www.instagram.com/p/CMM9-4yHhi2/?igshid=sdhe7thuasaj
#visualeducation#medicalillustration#patienteducation#myelopathy#awareness#spinalcordinjury#medicalanimation#visualartist#educational#resources#medicalart#cervical#spine#stenosis#spinalcord#disorder
2 notes
·
View notes
Text
Ayurveda Treatment for Cervical spondylosis
https://www.rahaayurveda.com/ Cervical spondylosis is a degenarative cascade due to age and lifestyle related changes in the vertebral column.
Common disease of middle age and old age.. Now a days increasing number of younger age people also suffers from this due to deranged posture ergonomics Eg: Text Neck Syndrome(due to over use of mobile phones)
The symptoms happens due to reasons which ranges from degenerative vertebrae degenarative disc disease to cervical spondylotic myelopathy which may eventually cause compression to exiting nerve roots and spinal cord.
The symptoms starts insidiously and vary from neck stiffness, unilateral or bilateral deep aching neck and shoulder, radiating pain and numbness to one or both arms, head ache, dizziness Patients may later develop progressive weakness of upper limbs and lower limbs,and inabilitu to control bowel and bladder urges
How to tackle this????? This morbid condition can be prevented and treated by the timely intervention through Ayurveda.
Unique ayurveda treatments like Snehana, Swedana gives appreciable results. Abhyanga, Elakizhi, pizhichil, njavarkizhi are some of them. 'Nasya 'which is a part of panchakarma therapy is the best treatment for neck and head related conditions.
The medicines for such treatments are selected as per the prakrithi (body constitution )of patient and stage of disease.
Stress relief therapies, yoga, physical rehabilitation adds to the best treatment outcome
Medicines, diet modifications and life style alterations through can well prevent the onset and progress of cervical spondylosis.
0 notes
Text
Cervical pain symptoms and treatment
WHAT IS CERVICAL SPONDYLOSIS?
Cervical pain symptoms and treatment
Cervical Spondylosis
Cervical spondylosis is a typical, age-related problem of the cervical spine that is situated in the neck area. This condition is otherwise called neck joint inflammation or cervical osteoarthritis. With age, the cervical plates bit by bit face mileage bringing about the breakdown of the construction. The liquid present between the cervical plates is lost which makes the spine stiffer, prompting cervical torment. This outcomes in changes during the bones, plates, and joints at the spine of the neck.
Because of the liquid drying out and degeneration of the plates and ligament in the encompassing region, unusual development or spray of bones called osteophytes can happen prompting the narrowing of the section from where spinal nerves leave, causing a connected condition called cervical spinal stenosis.
What is Spondylosis?
Spondylosis is an umbrella term that is utilized to portray any degeneration of the spinal line. Spondylosis manifestations include intense pain and back in advanced age. Cervical spondylosis is pervasive among moderately aged and old individuals with over 85% of individuals more seasoned than 60 years being a casualty of this problem that causes cervical neck torment. Early cervical spondylosis can likewise happen yet it is uncommon.
Spondylitis versus Spondylosis
Spondylitis and spondylosis both influence the spinal rope however there is an essential contrast between the two. The significance of spondylitis is that it is the aggravation of at least one regular cervical vertebrae prompting torment in the spine. Cervical spondylosis generally alludes to any sort of degeneration of the spine. Along these lines, despite the fact that the impacts of both the illnesses may be comparable, their starting point and cause are totally extraordinary. Understanding the distinction among spondylosis and spondylitis is significant on the grounds that it assists the specialists with deciding the course of treatment and the right drugs for the patient.
What is cervical lordosis?
Each individual has an ordinary bend of the spine which is known as lordosis. The deficiency of cervical lordosis alludes to the circumstance where an individual's spinal bend curves strangely and in an expanded manner internal. This can prompt exorbitant tension on the spinal rope that causes torment, distress, and outrageous deadness. The deficiency of cervical lordosis is regularly one of the contributing reasons for serious instances of cervical spondylosis.
What is Cervical Vertebrae?
Cervical vertebrae of the spine are the most slender and most sensitive bundle of seven hard rings present between the foundation of the skull and the thoracic vertebrae at the storage compartment.
2.
Bolt
Manifestations OF CERVICAL SPONDYLOSIS
Cervical Spondylosis
Cervical spondylosis manifestations can fluctuate from one individual to another and the degree of cervical spine torment relies upon the age of the influenced individual. A portion of the normal spondylosis side effects are:
Extreme solidness at the neck prompts manifestations of cervical torment in neck
Hefty cervical spondylosis migraine that may begin at the fundamental cervical spondylosis torment spaces of the neck
Torment in the shoulder and arms that outcomes in the powerlessness to move the hands
Inability to appropriately turn the head around because of outrageous torment
Spondylosis indications show granulating clamor or sensation when endeavors are made to turn the neck around
With enough rest and appropriate rest, cervical agony indications will in general improve. The manifestations of cervical torment are greatest toward the beginning of the day and afterward again around evening time before bed.
On the off chance that osteophytes cause cervical stenosis in the cervical bone, it squeezes the spinal line prompting a condition called cervical spondylotic myelopathy. The myelopathy significance is only it alludes to any illness of the spinal line. The beginning of this auxiliary condition can bring about the accompanying manifestations of spondylosis:
A sensation of unusual shivering, deadness, and shortcoming in the fringe areas like the arms, hands, feet, and legs
Absence of equilibrium and coordination which prompts strolling and development hardships
The spondylosis neck bone prompts strange reflexes and causes irregular muscle fits
The event of incontinence or the deficiency of power over one's urinary bladder and defecations
3.
img
Reason for CERVICAL SPONDYLOSIS
The typical mileage of the bones in the spinal string are the primary cervical spondylosis causes that outcome in degenerative spondylosis. Other potential reasons for cervical agony can be the accompanying:
Bone Prods or Unusual Outgrowths of Bones called Osteophytes:
As the spine declines and gets more vulnerable because of advanced age, the body reacts by developing new and additional issues that remains to be worked out the spine more grounded. This strange arrangement of bones or cervical osteophytes is called bone prods. These additional bones can squeeze the spine, for example, the nerve and the spinal string in the cervical area prompting a terrible instance of cervical circle illness.
Dried out Spinal Plates:
The spinal string is comprised of little bones called vertebrae which comprises of little liquid filled circles. The liquid in the middle of the bones is thick and behaves like cushion like pads that ingest the shock of substantial exercises like lifting, curving and different developments. With age, the liquid can get dried out driving because of a condition called plate parching. This makes the bones rub against one another during exercises that cause neck spondylosis and brings about intense agony in the risky space of the neck.
Herniated Circles:
In this condition, spinal circles foster breaks in them that outcome in spillage of the liquid present between them. This interior padding material that breaks out can press against the spinal nerves and bones bringing about deadness of the arms and serious agony.
Injury:
Any kind of neck injury because of a mishap can prompt the beginning of gentle cervical spondylosis which speeds up the maturing interaction of the cervical spine.
Firmness of the Tendon:
Tendons are groups of stringy connective tissue that interfaces bones and ligaments together. With age, these tendons can become stiffer that influences the general neck development prompting a cervical issue at the neck.
Unnecessary Pressure and Abuse:
Individuals who are utilized in areas that require hefty liftings like development work and more inclined to foster neck spondylitis and spondylosis. Since the beginning, this sort of occupation squeezes the neck and spinal rope prompting early lumbar spondylosis and side effects of cervical spondylosis.
4.
img
Hazard Elements OF CERVICAL SPONDYLOSIS
The most serious danger factor of cervical spondylosis is maturing and subsequently, it can't be totally kept from occurring. Yet, there are positively different variables that can speed up the beginning of this condition. Such factors include:
Neck injury because of a mishap
Business related distressing exercises that require substantial actual activities like truly difficult work
Helpless stance which means going through a similar neck developments or standing firm on your head in an awkward footing for a delayed timeframe, particularly for individuals who maintain work area sources of income. This is called dull pressure.
Hereditary components and family ancestry
Smoking
Being overweight and inert for a significant stretch of time
5.
Bolt
STEPS TO Forestall CERVICAL SPONDYLOSIS
There are sure cervical spondylosis home treatment estimates that can be applied to forestall this condition. These home solutions for cervical agony include:
Keep great consideration of the neck and shoulder locale. Try not to stack weighty articles on the head or neck. Try not to rest on a high-pad.
For individuals with work area occupations, focus on the stance you by and large will in general follow during work. Try to extend enough in the middle of your work hours. The fixing of your cervical spine is significant for the duration of the day. Recline your head every so often.
Swimming is viewed as a casual exercise for cervical agony. Try to swim regularly and perform general proactive tasks. Try not to be dormant for an extensive stretch of time. Exercise for cervical spondylitis is educated for individuals experiencing indications regarding spondylitis in the neck
6.
img
Analysis OF CERVICAL SPONDYLOSISCervical Spondylosis Analysis
How to fix cervical torment? This relies upon how well the illness is analyzed in any case. Making a precise analysis of the condition includes precluding other potential factors that can cause neck torment overall. Based on the consequences of tests, the specialist may allude the patient to a muscular subject matter expert or a nervous system specialist for additional cervical spondylosis treatment. Determination tests include:
1. Actual Assessments:
The previously set of material science tests to decide the legitimate course of spondylosis treatment incorporates testing the reflexes of the patient and check for the presence of muscle shortcoming and shortages in the tangible nerve work. For cervical spondylitis treatment, specialists additionally run tests to decide the scope of neck development and the overall condition of the general strolling development to comprehend cervical treatment important. This load of tests assist the specialist with comprehension if the spinal nerves and lines are under any kind of additional pressing factor. To affirm the finding of cervical spondylosis, specialists will arrange imaging tests and nerve work tests.
2. Imaging Tests:
X-Beam Imaging - To check for the presence of bone spikes and other strange development of spinal bones
Registered Tomography (CT) Sweep - To get nitty gritty pictures of the cervical district
X-ray Output - This strategy includes the utilization of radiowaves that assist the specialist with deciding the presence of squeezed nerves
Myelogram - For this situation, an infused stacked with a tracer color is utilized to feature the spaces of the c spine, Combined with CT Sweep or X-Beams, specialists can discover better pictures of the influenced regions.
3. Nerve Capacity Tests:
Electromyogram (EMG) - This test is utilized to decide whether the nerves of the body are working in an ordinary manner. EMG records the entry of nerve signals in the body by estimating the electrical movement of the nerves.
Nerve C
Comments
0 notes
Photo

Congrats to my boss, Mark Schornak, for his getting his artwork on the cover of this month’s Journal of Neurosurgery: Spine. Mark unfortunately doesn’t illustrate as much as he used to since he’s busy managing the Neuroscience Publications department, so it’s a real treat to see new work from him (he’s old school and draws his illustrations out with pencil and adds color in Photoshop using a mouse 🤯). The name of the article is “Functional improvement in hand strength and dexterity after surgical treatment of cervical spondylotic myelopathy: a prospective quantitative study” Check it out online at thejns.org #journalcover #medicalillustration #journal #coverart #publication #neurosurgery #textbook #medicalart #sciart #scienceillustration #textbooks #medschool #physiciansassistant #neuro #neuroscience #spinesurgery #teaching #technique #spines #medicine #spine #photoshopdrawing #digitalpainting #magazinecover #article #brainsurgery #spinalcordinjury (at Barrow Brain and Spine) https://www.instagram.com/p/CBirqI7nh_m/?igshid=1k8gzwmfng5w3
#journalcover#medicalillustration#journal#coverart#publication#neurosurgery#textbook#medicalart#sciart#scienceillustration#textbooks#medschool#physiciansassistant#neuro#neuroscience#spinesurgery#teaching#technique#spines#medicine#spine#photoshopdrawing#digitalpainting#magazinecover#article#brainsurgery#spinalcordinjury
3 notes
·
View notes
Text
Anterior Cervical Interbody Fusion System-Best way to recover for spine deceases
Anterior cervical discectomy and fusion are considered to be the gold standard for the treatment of indicative degenerative round disease. Dissimilar interbody combination techniques have been proposed in order to reinstate the physiological altitude of the intervertebral space and lordosis of the cervical backbone after taking away the offending disc and osteophyte. The autograft is the most normally used fusion material.
Anterior Cervical Interbody Fusion System:
Interbody fusion cages have been urbanized to avoid the complications related to bone harvesting from the giver site while rising instant stability of the cervical spine after decompression and promoting skinny fusion. Various authors suggested the use of frontal cervical fusion with a cage containing bone substitutes. Pleasing results were obtained regarding the fusion rates even though fusion was delayed as compared with that in a cage containing autograft.
The present learning was undertaken to appraise prospectively the efficiency of implanting Anterior Cervical Interbody Fusion System containing β-tricalcium phosphate for the healing of cervical radiculopathy and/or myelopathy. An additional reason for this study was to assess the fusion rates and outcomes in patients with or without aimlessly assigned plate fixation.
A diversity of bone graft replacements, interbody cages, and frontal plates have been used in cervical interbody fusion, but no inhibited study was conducted on the clinical presentation of β-tricalcium phosphate and the result of supplemented anterior plate fixation Occipital Certical Fixation System Exporters.
The purpose of this potential, a randomized scientific study was to assess the efficiency of implanting Anterior Cervical Interbody Fusion System cage containing β-TCP for the action of cervical radiculopathy and/or myelopathy, and the fusion rates and outcomes in patients with or without aimlessly assigned plate obsession. Sixty-two patients with cervical radiculopathy and/or myelopathy due to yielding disc herniation or spondylosis were treated with one- or two-level discectomy and fusion with interbody cages containing β-TCP. They were arbitrarily assigned to receive supplemented frontal plates. The patients were followed up for 2 years postoperatively.

The radiological and scientific outcomes were assessed during a 2-year follow-up. The grades showed that the fusion rate after surgery in patients treated without anterior cervical plating was considerably lower than that with plate fixation, but victorious bone fusion was achieved in all patients of both groups at a 6-month follow-up appraisal. Patients treated without anterior plate obsession had cage subsidence at last follow-up. No difference was found concerning improvement in spinal curving as well as neck and arm pain, and revival rate of JOA score at all time intervals between the two groups.
Based on the findings of this learning, Anterior Cervical Interbody Fusion System cage containing β-TCP following one- or two-level discectomy proved to be a successful treatment for cervical spondylotic radiculopathy. Supplemented anterior plate fixation can encourage interbody fusion and avoid cage subsidence but do not recover the 2-year outcome when compared with those treated without anterior plate fixation.
Worldwide Market study Report offers up-to-date information and chronological data on the Cervical Interbody Fusion Cages market.
It gives a key investigation on the market position of the Cervical Interbody Fusion Cages manufacturers with the most excellent facts and figures, significance, meaning, SWOT study, expert opinions, and the latest developments across the sphere. The Report also works out the market size, Cervical Interbody Fusion Cages Sales, Price, proceeds, Gross periphery and Market Share, cost arrangement, and growth rate. The statement considers the profits generated from the sales of This Report and technologies by a range of application segments.
The investigation covers the existing Anterior Cervical Interbody Fusion System Cages market size of the market and its expansion rates based on 6-year records with company sketch of Key players/manufacturers.
Short explanation:
Anterior interbody cages are titanium cylinders that are located in the disc gap. The cages are absorbent and allow the bone graft to cultivate from the vertebral body through the cage and into the subsequently vertebral body.
The cages proffer outstanding fixation, so most patients do not require extra instrumentation or post-operative back braces for support.
Cervical Interbody Fusion Cage is extensively used in the healing of Spinal Diseases, manage Spinal Deformity Development, Guard of Spinal Nerves, and Others. The most quantity of Cervical Interbody Fusion Cage is for the action of Spinal Diseases.
If you want a healthy body and keep yourselves fit, kindly Visit us for more information at MJ Surgical.
0 notes
Text
Amyotrophic Lateral Sclerosis
Authored by Aymeé Hernández

Abstract
Amyotrophic Lateral Sclerosis (ALS) is a neurodegenerative disorder of unknown cause. More of 400.000 persons are affected by ALS at world level. It is characterized by diffuse involvement of cortical, bulbar and spinal motor neurons. Physiopathology is very complex, there are a lot of changes into the neurons and glia that cause apoptosis and cellular degeneration. The diagnostic of this disorder is based in demonstrating of abnormalities of upper and lower motor neurons. It is based in neurophysiological studies and clinical signs, it is supported by Scorial criteria. New images methods could diagnosis and prognosis evolution of ALS patients and this methods show some important structural and functional abnormalities in nervous structures.
Keywords: Amyotrophic lateral sclerosis (ALS); Magnetic resonance image; Tensor of diffusion
Go to
Introduction
Amyotrophic Lateral Sclerosis (ALS) is a neurodegenerative disease of the voluntary way.
Upper and Lower motor neuron could degenerate. It the 3th more frequent neurodegenerative disease, overcome by Alzheimer and Parkinson Diseases. Some famous people like: Lu Gehrig, Jason Becker and Stephen Hawking have been affected by ALS [1].
Epidemiology
A. World Incidence: 2 x 100 000 inhabitants.
B. World Prevalence: 5 - 8.5 x 100 000 inhabitants.
C. Number of persons affected to world level: 400.000
D. Death in a year to world level: 100.000
E. Relation Man/Women: 2:1
F. Age of presentation: 40-60 years.
G. Survival: 3-5 years, 10 percent of the cases survival 1o or more years [2,3].
Forms of presentation
A. Familiar form (10% of cases).
B. Sporadic form (90% of cases) [2-4].
Go to
Physiopathology
In ALS a multifactorial mechanism is proposed. Some factors are being in relation with ALS, some of them are: contact with heavy metals, organic solvents, organophosphorus substances, organochlorine substances, Selenium, Calcium, Magnesium, Manganese, Mercury, Lead, Cupper, Aluminum, Chrome, Tobaccoand Alcohol habits, Electric and Ellectro-magnetic fields. There are a lot of changes at cellular and molecular levels in neurons and glias. Superoxide Dismutase 1 enzyme (SOD1) dysfunction is the most general mechanism in ALS, it cause high levels of free radicals into de cell, destabilization of some important proteins and transporters, high levels of glutamate neurotransmitter outside the cell, glutamate mediated excitotoxicity, abnormalities of axonal transport, abnormalities of endoplasmic reticulum and mitochondria, abnormal proteins accumulation into the cells (Cytoplasmic Inclusions) . All of this changes could provoke apoptosis and neural degeneration [5,6].
Go to
Diagnosis
Symptoms and signs include: muscular weakness, spasticity, hyper reflexia, clonus and Babinski sign, fasciculation, hypotonia and muscular atrophy. Diagnosis is based in Scorial criteria, it is support by clinical and neurophysiological examination and image techniques. Differential diagnosis of ALS is obligated with cervical spondylotic myelopathy, medullar tumor, syringomyelia. There is no an effective treatment for ALS [7-10].
New diagnosis techniques
Now days some magnetic resonance image techniques have been applied to diagnosis and prognosis the evolution of ALS patients, and some parameters have demonstrate abnormalities in non-motor structures:
A. Voxel based morphometry: It has showed diminish of gray matter in pre-central and frontal medium gyrus; diminish of white matter of upper frontal region, pre-central and lower temporal gyrus.
B. Diffusion Technique: It has showed:
1. Increase of Mean Coefficient of Diffusion (MCD) in precentral, post-central, lower frontal, angular, supramarginal and medium temporal gyrus, insula, putamen nucleus, orbito-frontal white matter, internal capsule, corpus callosum and cerebellum.
2. Diminish of Fractional Anisotropy (AF) in white matter in pre-central, lower frontal and pre-motor areas.
3. Cortical Thickness: It is diminished in primary motor cortex, lower parietal region and lower temporal gyrus.
4. Volumetric Analysis: Diminish of volume of hippocampus, basal ganglia and limbic structures. Increase of volume of lateral ventricles [11-15].
Go to
Conclusion
Some markers of ALS need to be founded, new image techniques could be good candidates to show structural and functional abnormalities of nervous system structures in ALS patients.
For more open access journals in juniper publishers please click https://juniperpublishers.com/
For more articles on Open Access Journal of Neurology & Neurosurgery Please click on https://juniperpublishers.com/oajnn/
Open Access Journal of Neurology & Neurosurgery in Full text in Juniper Publishers
https://juniperpublishers.com/oajnn/OAJNN.MS.ID.555609.php
0 notes
Text
How to Find Best Brain Tumor Treatment Hospital in India ?
Treatment for a brain tumor differs depending on several factors such as a person's age, general health, and the size, location, and type of tumor. Treatment of brain cancer is usually complex. Most treatment plans involve several consulting doctors. Surgery to remove the tumor is typically the first option once a brain tumor has been diagnosed. The purpose of surgery is to confirm that the abnormality seen during testing is indeed a tumor and to remove the tumor. If the tumor cannot be removed, a sample of the tumor will be taken to identify its type. Radiation and chemotherapy are other modalities may also be used. Spine and Brain India directed by Dr. Arun Saroha offers one of the best brain tumor treatment in India.
Delhi is a hub for medical tourists flocking in from all corners of the world to receive superlative treatment from the best in the field. Dr. Arun Saroha is a noted neurosurgeon available in Delhi and Gurgaon with over 20 years of experience treating a wide variety of neurological conditions varying from acute pain to the most complex spinal deformity in both adult and pediatric patients. He has successfully performed over 7000 procedures with patients from different parts of the world. He is one of the best brain tumor doctor in Delhi who has the highest expertise in treating different types of brain tumor in adults as well as pediatric patients. He is well known for recommending the most effective and safest treatment options, delivering expert care tailored to the needs of the individual patients.
Dr. Arun Saroha is the Director of Neurosurgery at Max Hospital, Saket New Delhi and Gurgaon. Max Hospital is one of the top hospital in India offering the best brain and spine treatment using the latest technologies that increases the precision of the surgeon’s work and thereby improving the outcome of the treatment. In addition to the advanced technologies being utilized, correct diagnosis is the key to effective treatment. Doctors in India are known for their accurate diagnosis and best treatment at affordable rates as compared to Western countries.
The best brain surgeon in Delhi and Gurgaon, Dr. Arun Saroha, is also one of the very few in the country who treats pediatric neurosurgical conditions, including hydrocephalus, chiari I malformations, a rachnoid cysts, spine disorders including tethered cord, spinal tumors, vascular malformations, head and spine trauma. The particular types of brain conditions that arise in children differ in important ways from those found in adults. For children, particular risks and benefits correspond to particular treatments in ways that may be different than for adults.
Most of the hospitals in India are internationally accredited, thus enhancing customer’s access to better healthcare services and meeting their expectations. The accredited healthcare organization practices and delivers continuous quality services and functions in the best interests of all patients giving importance to access, affordability, efficiency and quality healthcare services.
Spine and Brain India headed by Dr. Arun Saroha, one of the best brain surgeon in Delhi and Gurgaon is dedicated in providing comprehensive diagnosis and treatment for all types of brain and spine conditions including Cervical, Thoracic and Lumbar Disorders, Disk Herniation, Spinal Stenosis, Spondylolisthesis, Spondylotic Myelopathy, Brain and Spine Trauma, Brain Tumors for both adult and pediatric patients.
youtube
#brain tumor surgery#SPINE AND BRAIN INDIA#best brain surgeon in Delhi and Gurgaon#best brain and spine treatment#Dr. Arun Saroha#best brain tumor doctor in Delhi#Brain Surgery in Gurgaon#Brain tumor doctor in Delhi NCR
0 notes
Link
Comprehensive Myelopathy Spinal Cord Surgery in India. Myelopathy describes any neurologic deficit related to the spinal cord. It can be cervical, thoracic or lumbar, the most common of which is cervical spondylotic myelopathy and is caused by arthritic changes the cervical spine. If your symptoms are mild, you may find relief with non-surgical treatments. These include pain medication, activity modification or physical therapy. Any treatment program should be under the guidance of a medical professional because with myelopathy the spinal cord is being overly compressed.
#Comprehensive Myelopathy Spinal Cord Surgery in India#Comprehensive Myelopathy Spinal Cord Surgery in Delhi#Best Hospital for Comprehensive Myelopathy Spinal Cord Surgery#Best Doctors for Comprehensive Myelopathy Spinal Cord Surgery
0 notes
Text
Cervical pain symptoms and treatment
Cervical pain symptoms and treatment is a typical, age-related problem of the cervical spine that is situated in the neck district. This condition is otherwise called neck joint pain or cervical osteoarthritis. With age, the cervical plates steadily face mileage bringing about the breakdown of the design. The liquid present between the cervical circles is lost which makes the spine stiffer, prompting cervical torment. This outcomes in changes during the bones, plates, and joints at the spine of the neck.
Because of the liquid lack of hydration and degeneration of the plates and ligament in the encompassing region, strange development or spray of bones called osteophytes can happen prompting the narrowing of the entry from where spinal nerves leave, causing a connected condition called cervical spinal stenosis.
What is Spondylosis?
Spondylosis is an umbrella term that is utilized to depict any degeneration of the spinal string. Spondylosis manifestations include intense undeniable irritation and back in advanced age. Cervical spondylosis is common among moderately aged and old individuals with over 85% of individuals more seasoned than 60 years being a survivor of this problem that causes cervical neck torment. Early cervical spondylosis can likewise happen yet it is uncommon.
Spondylitis versus Spondylosis
Spondylitis and spondylosis both influence the spinal rope however there is a fundamental distinction between the two. The importance of spondylitis is that it is the irritation of at least one run of the mill cervical vertebrae prompting torment in the spine. Cervical spondylosis for the most part alludes to any sort of degeneration of the spine. Along these lines, despite the fact that the impacts of both the illnesses may be comparable, their starting point and cause are totally extraordinary. Understanding the contrast among spondylosis and spondylitis is significant in light of the fact that it assists the specialists with deciding the course of treatment and the right prescriptions for the patient.
What is cervical lordosis?
Each individual has an ordinary bend of the spine which is known as lordosis. The deficiency of cervical lordosis alludes to the circumstance wherein an individual’s spinal bend curves unusually and in an expanded manner internal. This can prompt inordinate tension on the spinal line that causes agony, distress, and outrageous deadness. The deficiency of cervical lordosis is frequently one of the contributing reasons for extreme instances of cervical spondylosis.
What is Cervical Vertebrae?
Cervical vertebrae of the spine are the most slender and most fragile bundle of seven hard rings present between the foundation of the skull and the thoracic vertebrae at the storage compartment.
Bolt
Side effects OF CERVICAL SPONDYLOSIS
Cervical Spondylosis
Cervical spondylosis side effects can differ from one individual to another and the degree of cervical spine torment relies upon the age of the influenced individual. A portion of the normal spondylosis indications are:
Extreme firmness at the neck prompts indications of cervical agony in neck
Hefty cervical spondylosis migraine that may start at the principle cervical spondylosis torment spaces of the neck
Agony in the shoulder and arms that outcomes in the powerlessness to move the hands
Inability to appropriately turn the head around because of outrageous torment
Spondylosis indications show granulating clamor or sensation when endeavors are made to turn the neck around
With enough rest and appropriate rest, cervical agony side effects will in general improve. The side effects of cervical torment are most extreme in the first part of the day and afterward again around evening time before bed.
In the event that osteophytes cause cervical stenosis in the cervical bone, it squeezes the spinal rope prompting a condition called cervical spondylotic myelopathy. The myelopathy significance is only it alludes to any infection of the spinal rope. The beginning of this auxiliary condition can bring about the accompanying manifestations of spondylosis:
A sensation of unusual shivering, deadness, and shortcoming in the fringe areas like the arms, hands, feet, and legs
Absence of equilibrium and coordination which prompts strolling and development challenges
The spondylosis neck bone prompts strange reflexes and causes arbitrary muscle fits
The event of incontinence or the deficiency of authority over one’s urinary bladder and solid discharges
img
Reason for Cervical pain symptoms and treatment
The typical mileage of the bones in the spinal line are the fundamental cervical spondylosis causes that outcome in degenerative spondylosis. Other potential reasons for cervical torment can be the accompanying:
Bone Spurs or Abnormal Outgrowths of Bones called Osteophytes:
As the spine deteriorates and gets more fragile because of advanced age, the body reacts by developing new and additional unresolved issues the spine more grounded. This strange development of bones or cervical osteophytes is called bone spikes. These additional bones can squeeze the spine, for example, the nerve and the spinal rope in the cervical district prompting an awful instance of cervical circle infection.
Got dried out Spinal Disks:
The spinal string is comprised of little bones called vertebrae which comprises of little liquid filled circles. The liquid in the middle of the bones is thick and behaves like cushion like pads that retain the stun of hefty exercises like lifting, winding and different developments. With age, the liquid can get got dried out driving because of a condition called circle drying up. This makes the bones rub against one another during exercises that cause neck spondylosis and brings about intense agony in the risky space of the neck.
Herniated Disks:
In this condition, spinal plates foster breaks in them that outcome in spillage of the liquid present between them. This inward padding material that breaks out can press against the spinal nerves and bones bringing about deadness of the arms and serious agony.
Injury:
Any kind of neck injury because of a mishap can prompt the beginning of gentle cervical spondylosis which speeds up the maturing interaction of the cervical spine.
Solidness of the Ligament:
Tendons are groups of stringy connective tissue that associates bones and ligaments together. With age, these tendons can become stiffer that influences the general neck development prompting a cervical issue at the neck.
Inordinate Stress and Overuse:
Individuals who are utilized in areas that require substantial liftings like development work and more inclined to foster neck spondylitis and spondylosis. Since the beginning, this sort of occupation squeezes the neck and spinal line prompting early lumbar spondylosis and manifestations of cervical spondylosis.
img
Hazard FACTORS OF CERVICAL SPONDYLOSIS
The most serious danger factor of cervical spondylosis is maturing and thus, it can’t be totally kept from occurring. However, there are surely different elements that can speed up the beginning of this condition. Such factors include:
Neck injury because of a mishap
Business related distressing exercises that require weighty actual activities like hard work
Helpless stance which means going through a similar neck developments or standing firm on your head in an awkward foothold for a delayed timeframe, particularly for individuals who maintain work area sources of income. This is called dreary pressure.
Hereditary variables and family ancestry
Smoking
Being overweight and dormant for an extensive stretch of time
Bolt
STEPS TO PREVENT CERVICAL SPONDYLOSIS
There are sure cervical spondylosis home treatment estimates that can be applied to forestall this condition. These home solutions for cervical agony include:
Keep great consideration of the neck and shoulder district. Try not to stack weighty articles on the head or neck. Try not to rest on a high-pad.
For individuals with work area occupations, focus on the stance you by and large will in general follow during work. Try to extend enough in the middle of your work hours. The fixing of your cervical spine is significant for the duration of the day. Recline your head sometimes.
Swimming is viewed as a casual exercise for cervical torment. Make a point to swim regularly and perform general proactive tasks. Try not to be inert for a significant stretch of time. Exercise for cervical spondylitis is instructed for individuals experiencing manifestations with respect to spondylitis in the neck.
img
Determination OF CERVICAL SPONDYLOSIS
Cervical Spondylosis Diagnosis
How to fix cervical torment? This relies upon how well the illness is analyzed in any case. Making a precise analysis of the condition includes precluding other potential factors that can cause neck torment by and large. Based on the aftereffects of tests, the specialist may allude the patient to a muscular subject matter expert or a nervous system specialist for additional cervical spondylosis treatment. Determination tests include:
Actual Examinations:
The originally set of physical science tests to decide the appropriate course of spondylosis treatment incorporates testing the reflexes of the patient and check for the presence of muscle shortcoming and shortfalls in the tactile nerve work. For cervical spondylitis treatment, specialists additionally run tests to decide the scope of neck development and the overall condition of the general strolling development to comprehend cervical treatment fundamental. This load of tests assist the specialist with comprehension if the spinal nerves and strings are under any kind of additional pressing factor. To affirm the finding of cervical spondylosis, specialists will arrange imaging tests and nerve work tests.
Imaging Tests:
X-Ray Imaging – To check for the presence of bone spikes and other unusual development of spinal bones
Processed Tomography (CT) Scan – To get point by point pictures of the cervical district
X-ray Scan – This technique includes the utilization of radiowaves that assist the specialist with deciding the presence of squeezed nerves
Myelogram – For this situation, an infused stacked with a tracer color is utilized to feature the spaces of the c spine, Coupled with CT Scan or X-Rays, specialists can discover better pictures of the influenced regions.
Nerve Function Tests:
Electromyogram (EMG) – This test is utilized to decide whether the nerves of the body are working in an ordinary manner. EMG records the section of nerve signals in the body by estimating the electrical action of the nerves.
Nerve Conduction Study – Cervical pain symptoms and treatment al pain symptoms and treatment,
0 notes
Text
Questions about cervical spondylosis
Questions about cervical spondylosis
Q: What are the symptoms of cervical spondylosis? How to self-test self-test cervical spondylosis?https://www.shrewsburychiro.net/
A: There are certain differences in the symptoms of different types of cervical spondylosis. Patients can self-examine according to the symptoms to see if they are stained.
First, cervical spondylosis. It is more common, and it is also the earliest symptom of cervical spondylosis. It is mainly caused by neck symptoms. The incidence of young and middle-aged patients is mostly caused by local pain, neck discomfort or limited mobility.

Second, nerve root type cervical spondylosis. The patient had neck pain and stiff neck, followed by shoulder pain or upper limb pain. The upper limbs have a heavy feeling, the grip strength is reduced, sometimes the object falls, and the fingers have numbness. What everyone needs to pay attention to is that many people think that the neck does not hurt, and the shoulder pain is frozen shoulder. Shoulder pain in shoulder inflammation has two characteristics, one is a limited function, one is nighttime pain, the more night, the more painful. In the shoulder pain of cervical spondylosis, the area often exceeds the elbow (the pain of the frozen shoulder is not more than the elbow) and is released to the upper limbs, and even to the hand. By pressing your cervical vertebra, if the upper limb pain occurs, the doctor indicates that you are radiculopathy.https://twitter.com/ShrewsburyChiro/status/839594211880087554
Everyone often has a misunderstanding that hand numbness is caused by cervical spondylosis, but it is not. Hand numbness caused by cervical spondylosis, often with arms and numbness. If the hands are numb, especially in the morning, the hands are swollen, and after the activity, the hand is increased, which may be caused by peripheral neuropathy. For example, carpal tunnel syndrome. The numbness caused by straining, trauma, and fatigue of the wrist require an EMG examination.
Third, vertebral artery type cervical spondylosis. Most of the symptoms are dizziness, dizziness, and even falling; sometimes nausea, vomiting, unclear vision, tinnitus, and deafness. Often expressed as a turn of the eyes black, a bow is also black. At this time, you need to make a nuclear magnetic or open-position film. It is best to do a cerebral vascular ultrasound to see the condition of the vertebral artery to determine whether you have vertebral artery type cervical spondylosis.
Many young people will also have dizziness and confusion. For example, if they get a dizzy bed, they will faint when they stand up again. Especially the girls with weak constitution may be dizziness caused by dieting hypoglycemia, not cervical vertebrae. Disease, need to pay attention to distinguish. In addition, otolithic disease, also known as benign paroxysmal positional vertigo, refers to vertigo and nystagmus of a transient paroxysmal episode that occurs when the head moves rapidly to a specific head position. If you can't identify the cause of dizziness, you can go to the hospital to check to see if it is cervical vertigo, or otogenic vertigo, or postural vertigo.
Fourth, sympathetic cervical spondylosis, the symptoms are more complicated, often have migraine, post-occipital pain; or unclear vision, photophobia, tearing, eye swelling, eyelids can not lift; or tinnitus, hearing impairment, facial Hemp and so on.
Fifth, cervical spondylotic myelopathy, most of the symptoms are slow, not easy to find, often expressed as feeling that stepping on cotton, walking roots without roots, lower limbs numbness, walking instability, trunk tightness and so on. There may also be symptoms of upper limbs, such as numbness in the hands or inactivity.
These are the main types of cervical spondylosis, and there are mixed types, that is, the above two or more types of symptoms appear at the same time.
Q: What are the risks of cervical spondylosis to the human body?
A: Cervical spondylosis has a great impact on quality of life and work quality, and even affects emotional and mental health. If the patient with orthopedics has a long course of the disease and repeated pain, he often suffers from "multi-faceted pinching" of pain, hemp, acid, bloating, and wood. However, everyone should not have a large psychological burden, because symptomatic treatment can be given to all stages of cervical spondylosis. Early cervical spondylosis can be cured by rehabilitation. Therefore, if symptoms appear as soon as possible, don't drag it. Check it and let the doctor give you the best treatment.
0 notes
Text
0 notes