#cervical spondylotic myelopathy surgery
Explore tagged Tumblr posts
Text
Pinched Nerve in The Spine: Radiculopathy - Symptoms, Causes, and Treatment
The spine consists of several individual bones known as vertebrae. These are interconnected together to form the spine. The spinal cord passes through a central canal in these vertebrae. From the spinal cord, the splitting of nerve roots occurs.
These roots travel between the bones of the spinal and different parts of the body. When the nerve root that leaves the spinal cord to other body parts becomes pinched, irritated, or damaged, it results in a medical condition known as radiculopathy. This condition is also known as a pinched nerve.

Types of Radiculopathy
Depending on where the condition happens in the spine, there are three types of radiculopathy. The symptoms of these types may range from mild to severe in individuals.
Cervical radiculopathy
Occurs due to pressure and compression of the nerve roots in the neck.
This portion of the spinal cord mainly affects the hands, arms, fingers, and shoulders.
Symptoms are usually visible in the hands and arms, which may include weakness or loss of sensation.
Lumbar radiculopathy
Occurs due to pressure and compression of the nerve roots in the lower back.
It may lead to sciatica, a condition that involves radiating pain in the sciatic nerve.
Thoracic radiculopathy
Occurs due to pressure and compression of the nerve roots in the upper back.
Chest pain is common in this condition.
There is a feeling of numbness and pain that moves to the front of the body in patients.
Causes of Radiculopathy and Risk Factors
Here are some of the commonly known causes of radiculopathy and the risk factors associated with it.
Change in size or shift in position of the tissues that surround the nerve root.
Herniated discs, also known as slip discs, are caused by to rupture of soft pads between spinal bones.
Bone spurs, bony outgrowths or projections resulting in constriction of the spinal passage. a condition in which the spaces within the spine get narrow.
Spondylosis is a wear and tear of the spinal disc with age.
Spondylolisthesis is a condition in which a vertebra slips out of its normal position onto the bone below it.
Spinal stenosis, narrowing of the spinal canal in the lower back.
Sciatica is pain travelling along with the sciatic nerve moving to the back of the thigh into the legs.
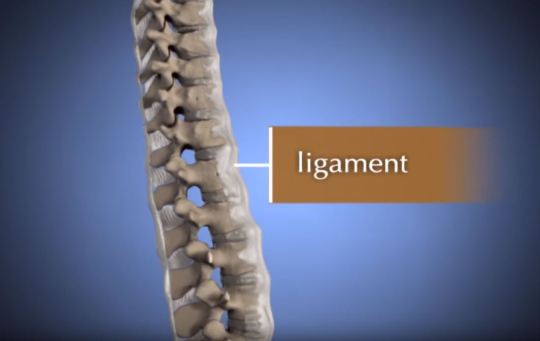
Thickening of spinal ligaments.
Spinal infections
Regular improper movements
Cancerous or non-cancerous growth in the spine
Radiculopathy Diagnosis
The diagnosis of radiculopathy begins with the patient giving a brief of their medical history to the doctor.
The doctor will ask questions about the type of symptoms, location of the pain, for how long has the pain been there, and also any other medical conditions which the patient is suffering from.
Once the medical history is known, the physician conducts a physical examination and tests.
This is to check the patient's muscular strength, reflexes, sensation, and also the possibility of any abnormalities.
Physical examination allows the medical practitioner to know the severity of the radiculopathy condition.
It also gives an idea about the location of the nerve root that is affected.
In some cases, radiculopathy diagnosis may require the use of advanced imaging techniques such as CT scan or MRI.
These tests aid in improving the visualization of the area where the problem lies.
In some cases, an expert like Dr Khanna orthopedic surgeon may also conduct a study on nerve conduction or Electromyography (EMG).
These tests help to know whether there is damage to the nerve or the problem is muscular.
Symptoms of Radiculopathy
The pinched nerve roots quickly become inflamed, which may result in the following symptoms:
Shooting pain in the back, legs, arms, and shoulders
Feeling of numbness and tingling sensation in the arms and legs.
Localized neck and back pain
Sharp pain when sitting idle or coughing
Sharp pain with movement
Hypersensitivity
Loss of sensation
Radiating pain in the shoulders
Skin numbness
Muscular weakness
Loss of reflexes
Sciatica
Non-surgical treatment for Radiculopathy
Conservative treatment is usually recommended before surgery. Here are some of the non-surgical treatment options for radiculopathy.
Physical therapy to strengthen the areas of pain.
Limitation or complete elimination of activities that cause radiculopathy pain and stains of the back and neck.
Immobilizing the affected area with
#Spine Care Specialists Indiana#Dr Khanna Orthopedic Surgeon#Orthopedic Spine Surgeon Munster#Minimally Invasive Lumbar Surgery Indiana#Neck Pain Treatment Munster#Best Spine Surgeon Indiana#Back Pain Treatment Munster#Osteoporosis Treatment Munster#Cervical Spondylotic Myelopathy Treatment#SI Joint Dysfunction Treatment#Sacroiliac Joint Dysfunction Treatment#Radiculopathy Treatment Munster#Spinal Stenosis Treatment Indiana#Lumbar Laminectomy Surgery Munster#Spondylolisthesis Treatment Munster#Spinal Cord Injuries Treatment Munster#Orthopedic Spine Specialist Indiana#Orthopedic Doctors in Munster Indiana#Best Orthopedic Doctors in Northwest Indiana#Back Pain Doctor in Northwest Indiana#Spine Treatment Indiana#Orthopedic Surgeon in Munster#Spine Doctors Indianapolis#Spine Surgery Indianapolis#Pain Management Munster Indiana#Cervical Disc Replacement Near Me#Cervical Disk Replacement Surgery#Minimally Invasive Surgery Indiana
2 notes
·
View notes
Link
#cervical spondylotic myelopathy#cervical spondylotic myelopathy symptoms#cervical spondylotic myelopathy treatment#cervical spondylotic myelopathy surgery
1 note
·
View note
Link
Spondolysis or Cervical Spondolysis is a medical condition which was once related to age. However, the scenario has completely altered now. For more information, just read our blog now.
#spondylotic changes#spondylosis#cervical spondylosis treatment#cervical spondylosis symptoms#spondylosis treatment#spondylosis neck#spondylosis causes#cervical spondylosis headache#cervical spondylotic myelopathy#cervical spondylosis with radiculopathy#degenerative spondylosis#cervical spondylosis surgery#neck collar for cervical spondylosis#cervical spondylitis treatment#early cervical spondylosis#cervical and lumbar spondylosis#cervical spondylosis exercise#exercises for cervical spondylosis#dizziness with cervical spondylosis
0 notes
Text
Spinal Laminoplasty Market to Grow at a CAGR of 4.3% During the Forecast Period 2021-2026
"Increasing Prevalence of Spinal Disorder Such as Spinal Stenosis, Spinal Tumours, Spondylotic, Rheumatoid Arthritis in the Geriatric Population Are the Major Factors Driving the Growth of the Market."
Spinal Laminoplasty Market size in 2020 is estimated to be $5.1 Billion, growing at a CAGR of 4.3% during the forecast period 2021-2026. Spinal Laminoplasty is a spinal surgery used to reduce pressure surrounding the spinal canal and nerve structures due to its compression against the wall of spinal cord. It is a minimally invasive procedure. Spinal laminoplasty tends to create extra space in the spinal canal by opening made in the vertebral lamina region for easy movement of the spinal cord. Increasing prevalence of spinal disorder such as spinal stenosis, spina bifida, spinal tumours, spondylotic, rheumatoid arthritis, and catastrophic kyphosis in the geriatric population are the major factors driving the growth of the market. Moreover, growing technological advancement in spine surgery coupled with rising adoption of minimally invasive spine surgeries further enhance the overall market demand for Spinal Laminoplasty during the aforesaid period.
Spinal Laminoplasty Market Segment Analysis - By Technology
Based on the Technology, Spinal Laminoplasty Market is segmented into Spine fusion, Spine Biologics, Decompression, and Motion Preservation. The spinal fusion segment is estimated to dominate the market during the period 2021-2026. This is attributed to rising number of spinal fusion surgeries worldwide coupled with rising advancement in spinal fusion techniques. The motion preservation segment is forecast to be the fastest-growing segment and is projected to grow at a CAGR of 3.8% during the period 2021-2026. This is mainly owing to its shorter recovery and rehabilitation process coupled with better spine movement and flexibility traction.
Request for Sample Report @ https://www.industryarc.com/pdfdownload.php?id=17293
Report Price: $ 4500 (Single User License)
Spinal Laminoplasty Market Segment Analysis - By Vertebral Position
Based on the Vertebral Position, Spinal Laminoplasty Market is segmented into Cervical Laminoplasty, Thoracic Laminoplasty, Lumbar Laminoplasty, Sacral Laminoplasty. In 2020, Cervical Laminoplasty is estimated to hold major share in the market. This is mainly owing to laminoplasty usage. Moreover, rising cases of spine disorder such as cervical spondylotic myelopathy, and catastrophic kyphosis resulting in neck, or arm pain are also contributing to the dominance of this segment. Also, Lumbar laminoplasty is projected to grow with a CAGR of 4.1% over the period 2021-2026. This is owing to its effectiveness and increasing adoption.
Spinal Laminoplasty Market Segment Analysis - By Geography
North America dominated the Spinal Laminoplasty market share accounting for 40% of the market in 2020. This is mainly owing to rising incidence of spine stenosis among the people across the countries such as U.S., Canada and others which contributes to increase in adoption of spinal laminoplasty. According to, North American Spine Society, spine stenosis is most commonly disorder in the U.S. However, the Asia-Pacific region is projected to be the fastest-growing over the period 2021-2026. This is owing to improving healthcare infrastructure coupled with rising advancement in spine surgery technology.
Spinal Laminoplasty Market Drivers
Increasing Prevalence of Spine Disorder
Increasing prevalence of spine disorder such as spine stenosis, spondylotic, rheumatoid arthritis in the geriatric population is driving the growth of Spinal Laminoplasty market. According to Australian Bureau of statistics 2017-18 National Health, approximately 16% of the population are suffering from back pain problem which accounts for 4 million people in Australia. Moreover, rising number of spine surgeries in outpatient settings is also leading to the market growth.
Rising Technological Advancement
Increase in research and development of advanced technology for spine surgery is also driving the market. Advanced technologies such as computer-assisted image-guided technology offer improved spinal surgery and are much more effective. Also, the increasing adoption of minimally invasive technology for spine surgery is also set to the growth of Spinal Laminoplasty Market.
Download Sample Report @ https://www.industryarc.com/pdfdownload.php?id=17293
Spinal Laminoplasty Market Challenges
High capital expenditure required for these procedure owing to usage of advance technology for improved spine surgery is challenging the market. Along with this, the uncertainties of reimbursement are also further challenging the growth of the market.
Covid-19 Impact
Moreover, the outbreak of COVID-19 around the world has impacted all industries including healthcare industry. Covid- 19 affects the spinal laminoplasty market including drastic reduction in emergency surgical procedures and also overall admission to the Emergency department (ED). Also owing to widespread of coronavirus, it affects workforce and staffing issues, procedural prioritisation as well as impact of spine laminoplasty. This affects Spinal Laminoplasty market by cancellation of scheduled surgery and shift of surgeons to the other area.
Spinal Laminoplasty Industry Outlook
Product launches, Merger & Acquisitions, joint ventures and R&D activities are key strategies adopted by players in the Spinal Laminoplasty Market. Spinal Laminoplasty top 10 companies are DePuy Synthes, Zimmer Spine, Medtronic, Pioneer Surgical Technologies, Cryo Life, Synthes Spine, Replication Medical, Arthro Kinetics, NuVasive and Pioneer Surgical Technologies
Acquisitions/Product Launches:
In January 2020, Medtronic acquired Illinois based company Stimgenics, LLC, that has pioneered a novel spinal cord stimulation (SCS) waveform known as Differential Target Multiplexed (DTM) Spinal Cord Stimulation. This acquisition will help Medtronic to enhance customer experience.
In November 2019, NuVasive, Inc., launched its new C360 cervical spine portfolio, as well as Anterior Cervical Plating (ACP) system. These products are designed to improve the quality of care for spine area.
Key Takeaways
In 2020, North America dominates the Spinal Laminoplasty Market owing to rising awareness about spinal laminoplasty among patients.
Increasing developments in healthcare infrastructure across the globe is driving the market growth of Spinal Laminoplasty.
Detailed analysis of the Strength, Weakness, and opportunities of the prominent players operating in the market will be provided in the Spinal Laminoplasty Market report.
High cost of spinal surgery and uncertainties surrounding reimbursement are challenging the growth of the market.
Related Reports :
A. Spinal Implants And Surgical Devices Market
https://www.industryarc.com/Research/Spinal-Implants-And-Surgical-Devices-Market-Research-501256
B. Spinal Fusion Devices Market
https://www.industryarc.com/Research/Spinal-Fusion-Devices-Market-Research-501943
For more Lifesciences and Healthcare Market reports, Please click here
About IndustryARC: IndustryARC primarily focuses on Cutting Edge Technologies and Newer Applications market research. Our Custom Research Services are designed to provide insights on the constant flux in the global supply-demand gap of markets. Our strong team of analysts enables us to meet the client research needs at a rapid speed, with a variety of options for your business. Any other custom requirements can be discussed with our team, drop an e-mail to [email protected] to discuss more about our consulting services.
1 note
·
View note
Text
Anterior Cervical Interbody Fusion System-Best way to recover for spine deceases
Anterior cervical discectomy and fusion are considered to be the gold standard for the treatment of indicative degenerative round disease. Dissimilar interbody combination techniques have been proposed in order to reinstate the physiological altitude of the intervertebral space and lordosis of the cervical backbone after taking away the offending disc and osteophyte. The autograft is the most normally used fusion material.
Anterior Cervical Interbody Fusion System:
Interbody fusion cages have been urbanized to avoid the complications related to bone harvesting from the giver site while rising instant stability of the cervical spine after decompression and promoting skinny fusion. Various authors suggested the use of frontal cervical fusion with a cage containing bone substitutes. Pleasing results were obtained regarding the fusion rates even though fusion was delayed as compared with that in a cage containing autograft.
The present learning was undertaken to appraise prospectively the efficiency of implanting Anterior Cervical Interbody Fusion System containing β-tricalcium phosphate for the healing of cervical radiculopathy and/or myelopathy. An additional reason for this study was to assess the fusion rates and outcomes in patients with or without aimlessly assigned plate fixation.
A diversity of bone graft replacements, interbody cages, and frontal plates have been used in cervical interbody fusion, but no inhibited study was conducted on the clinical presentation of β-tricalcium phosphate and the result of supplemented anterior plate fixation Occipital Certical Fixation System Exporters.
The purpose of this potential, a randomized scientific study was to assess the efficiency of implanting Anterior Cervical Interbody Fusion System cage containing β-TCP for the action of cervical radiculopathy and/or myelopathy, and the fusion rates and outcomes in patients with or without aimlessly assigned plate obsession. Sixty-two patients with cervical radiculopathy and/or myelopathy due to yielding disc herniation or spondylosis were treated with one- or two-level discectomy and fusion with interbody cages containing β-TCP. They were arbitrarily assigned to receive supplemented frontal plates. The patients were followed up for 2 years postoperatively.

The radiological and scientific outcomes were assessed during a 2-year follow-up. The grades showed that the fusion rate after surgery in patients treated without anterior cervical plating was considerably lower than that with plate fixation, but victorious bone fusion was achieved in all patients of both groups at a 6-month follow-up appraisal. Patients treated without anterior plate obsession had cage subsidence at last follow-up. No difference was found concerning improvement in spinal curving as well as neck and arm pain, and revival rate of JOA score at all time intervals between the two groups.
Based on the findings of this learning, Anterior Cervical Interbody Fusion System cage containing β-TCP following one- or two-level discectomy proved to be a successful treatment for cervical spondylotic radiculopathy. Supplemented anterior plate fixation can encourage interbody fusion and avoid cage subsidence but do not recover the 2-year outcome when compared with those treated without anterior plate fixation.
Worldwide Market study Report offers up-to-date information and chronological data on the Cervical Interbody Fusion Cages market.
It gives a key investigation on the market position of the Cervical Interbody Fusion Cages manufacturers with the most excellent facts and figures, significance, meaning, SWOT study, expert opinions, and the latest developments across the sphere. The Report also works out the market size, Cervical Interbody Fusion Cages Sales, Price, proceeds, Gross periphery and Market Share, cost arrangement, and growth rate. The statement considers the profits generated from the sales of This Report and technologies by a range of application segments.
The investigation covers the existing Anterior Cervical Interbody Fusion System Cages market size of the market and its expansion rates based on 6-year records with company sketch of Key players/manufacturers.
Short explanation:
Anterior interbody cages are titanium cylinders that are located in the disc gap. The cages are absorbent and allow the bone graft to cultivate from the vertebral body through the cage and into the subsequently vertebral body.
The cages proffer outstanding fixation, so most patients do not require extra instrumentation or post-operative back braces for support.
Cervical Interbody Fusion Cage is extensively used in the healing of Spinal Diseases, manage Spinal Deformity Development, Guard of Spinal Nerves, and Others. The most quantity of Cervical Interbody Fusion Cage is for the action of Spinal Diseases.
If you want a healthy body and keep yourselves fit, kindly Visit us for more information at MJ Surgical.
0 notes
Text
Lupine Pubishers| Cervical Spinal Cord Injury During Coronary Artery Bypass Graft Surgery in An Elderly: A Case Report
Lupine Publishers | Journal of Surgery & Case Studies

Case Report
Intraoperative spinal cord injury (SCI) is uncommon and the pathology has not cleared. We report cervical cord injury without vertebral fracture during a coronary artery bypass operation. Cervical cord compression (CCC) is compression of the cervical spinal cord that occurs during the normal course of aging and may progress into cervical spondylotic myelopathy (CSM), which can cause neurologic dysfunction. Many people with cervical cord compression are asymptomatic. However, patients with CCC are at higher risk of SCI following minor injury. An 85-year-old woman with asymptomatic cervical cord compression underwent a coronary artery bypass graft surgery. After the surgery, he developed tetraplegia. MRI revealed severe spinal cord compression from C3 to C7 and C5/6 signal change of spinal cord (Figure 1). The radiograph and CT showed diffuse idiopathic skeletal hyperostosis and thoracic kyphosis of 55 degree (Figure 2). Cervical SCI after was diagnosed. After the diagnosis, we underwent laminoplasty (Figure 3). And he almost completely recovered after surgery.
Figure 1: Magnetic resonance imaging (MRI) of the cervical spine.
Figure 2: MRI showed multilevel spinal cord compression.
Figure 3: The radiograph and CT showed diffuse idiopathic skeletal hyperostosis and thoracic kyphosis Radiograph after laminoplasty for cervical spinal cord injury.
Iatrogenic cervical SCI after non spinal surgeries that requires neck hyperextension is rarely reported, probably due to underdiagnosis and underreport. In the current aging society, the prevalence of patients with CCC is expected to increase. In our population-based magnetic resonance imaging (MRI) study, the prevalence rate of CCC was 24.4%, and it was higher with increasing age in both men and women [1]. Among the 15 cases (including ours) published in the literature [2], most patients had cervical cord compression and were old men. Eight patients had undergone coronary artery bypass surgery that requires prolonged operative time. Only 3 patients had almost complete recovery. Two patients required tracheostomy for long-term ventilator support. Two patients died. These cases reiterate the potential risk of iatrogenic SCI in people with predisposing conditions such as cervical spondylosis and CCC. Moreover, in this case, the patient had diffuse idiopathic skeletal hyperostosis and thoracic kyphosis of 55 degree, which can lead inflexibility of spine. The inflexibility of thoracic spine might cause hyperextension of cervical spine during the surgery. Surgeries requiring prolonged neck hyperextension put patients with cervical spondylosis and CCC at risk for SCI. It is essential to recognize the potential occurrence of iatrogenic SCI might endanger patients’ lives.
For more Lupine Publishers Open Access Journals Please visit our website:
http://www.lupinepublishers.us/
For more Surgery Journal articles Please Click Here:
https://lupinepublishers.com/surgery-case-studies-journal/
To Know More About Open Access Publishers Please Click on Lupine Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers Follow on Twitter : https://twitter.com/lupine_online
#Lupinepublishers#Lupine publishers#Lupine Publishers Group#Journal of Surgery#Journal of Case Studies
0 notes
Text
How to Find Best Brain Tumor Treatment Hospital in India ?
Treatment for a brain tumor differs depending on several factors such as a person's age, general health, and the size, location, and type of tumor. Treatment of brain cancer is usually complex. Most treatment plans involve several consulting doctors. Surgery to remove the tumor is typically the first option once a brain tumor has been diagnosed. The purpose of surgery is to confirm that the abnormality seen during testing is indeed a tumor and to remove the tumor. If the tumor cannot be removed, a sample of the tumor will be taken to identify its type. Radiation and chemotherapy are other modalities may also be used. Spine and Brain India directed by Dr. Arun Saroha offers one of the best brain tumor treatment in India.
Delhi is a hub for medical tourists flocking in from all corners of the world to receive superlative treatment from the best in the field. Dr. Arun Saroha is a noted neurosurgeon available in Delhi and Gurgaon with over 20 years of experience treating a wide variety of neurological conditions varying from acute pain to the most complex spinal deformity in both adult and pediatric patients. He has successfully performed over 7000 procedures with patients from different parts of the world. He is one of the best brain tumor doctor in Delhi who has the highest expertise in treating different types of brain tumor in adults as well as pediatric patients. He is well known for recommending the most effective and safest treatment options, delivering expert care tailored to the needs of the individual patients.
Dr. Arun Saroha is the Director of Neurosurgery at Max Hospital, Saket New Delhi and Gurgaon. Max Hospital is one of the top hospital in India offering the best brain and spine treatment using the latest technologies that increases the precision of the surgeon’s work and thereby improving the outcome of the treatment. In addition to the advanced technologies being utilized, correct diagnosis is the key to effective treatment. Doctors in India are known for their accurate diagnosis and best treatment at affordable rates as compared to Western countries.
The best brain surgeon in Delhi and Gurgaon, Dr. Arun Saroha, is also one of the very few in the country who treats pediatric neurosurgical conditions, including hydrocephalus, chiari I malformations, a rachnoid cysts, spine disorders including tethered cord, spinal tumors, vascular malformations, head and spine trauma. The particular types of brain conditions that arise in children differ in important ways from those found in adults. For children, particular risks and benefits correspond to particular treatments in ways that may be different than for adults.
Most of the hospitals in India are internationally accredited, thus enhancing customer’s access to better healthcare services and meeting their expectations. The accredited healthcare organization practices and delivers continuous quality services and functions in the best interests of all patients giving importance to access, affordability, efficiency and quality healthcare services.
Spine and Brain India headed by Dr. Arun Saroha, one of the best brain surgeon in Delhi and Gurgaon is dedicated in providing comprehensive diagnosis and treatment for all types of brain and spine conditions including Cervical, Thoracic and Lumbar Disorders, Disk Herniation, Spinal Stenosis, Spondylolisthesis, Spondylotic Myelopathy, Brain and Spine Trauma, Brain Tumors for both adult and pediatric patients.
youtube
#brain tumor surgery#SPINE AND BRAIN INDIA#best brain surgeon in Delhi and Gurgaon#best brain and spine treatment#Dr. Arun Saroha#best brain tumor doctor in Delhi#Brain Surgery in Gurgaon#Brain tumor doctor in Delhi NCR
0 notes
Link
Comprehensive Myelopathy Spinal Cord Surgery in India. Myelopathy describes any neurologic deficit related to the spinal cord. It can be cervical, thoracic or lumbar, the most common of which is cervical spondylotic myelopathy and is caused by arthritic changes the cervical spine. If your symptoms are mild, you may find relief with non-surgical treatments. These include pain medication, activity modification or physical therapy. Any treatment program should be under the guidance of a medical professional because with myelopathy the spinal cord is being overly compressed.
#Comprehensive Myelopathy Spinal Cord Surgery in India#Comprehensive Myelopathy Spinal Cord Surgery in Delhi#Best Hospital for Comprehensive Myelopathy Spinal Cord Surgery#Best Doctors for Comprehensive Myelopathy Spinal Cord Surgery
0 notes
Text
Microendoscopic laminotomy versus conventional laminoplasty for cervical spondylotic myelopathy: 5-year follow-up study
Microendoscopic laminotomy versus conventional laminoplasty for cervical spondylotic myelopathy: 5-year follow-up study
J Neurosurg Spine 27:403–409, 2017
The goal of this study was to characterize the long-term clinical and radiological results of articular segmental decompression surgery using endoscopy (cervical microendoscopic laminotomy [CMEL]) for cervical spondylotic myelopathy (CSM) and to compare outcomes to conventional expansive laminoplasty (ELAP).
METHODS Consecutive patients with CSM who required…
View On WordPress
#Cervical spine#cervical spondylotic myelopathy#Clinical outcome#endoscopic surgery#laminoplasty#Minimally invasive surgery#pincer mechanism
0 notes
Text
Microendoscopic laminotomy versus conventional laminoplasty for cervical spondylotic myelopathy: 5-year follow-up study
Microendoscopic laminotomy versus conventional laminoplasty for cervical spondylotic myelopathy: 5-year follow-up study
J Neurosurg Spine 27:403–409, 2017
The goal of this study was to characterize the long-term clinical and radiological results of articular segmental decompression surgery using endoscopy (cervical microendoscopic laminotomy [CMEL]) for cervical spondylotic myelopathy (CSM) and to compare outcomes to conventional expansive laminoplasty (ELAP).
METHODS Consecutive patients with CSM who required…
View On WordPress
#Cervical spine#cervical spondylotic myelopathy#Clinical outcome#endoscopic surgery#laminoplasty#Minimally invasive surgery#pincer mechanism
0 notes
Text
Outcomes Similar With Ventral vs Dorsal Approach to CSM Surgery
However, the randomized trial results also show significantly improved outcomes and about a 50% reduction in cost with laminoplasty for cervical spondylotic myelopathy (CSM) compared to fusion surgeries. Medscape Medical News from Medscape Medical News Headlines https://ift.tt/3iu9Tn0 via IFTTT
0 notes
Text
Looking for the best spine doctor in Delhi? Here’s our safe choice!
India is the most prominent destination due to highest quality of treatment provided at an affordable cost. Delhi is a hub for medical tourists to receive the best spine treatment in the country. Dr. Arun Saroha is one of the best spine doctor in Delhi. He is the Director of Neurosurgery at Max Hospital Saket, New Delhi and Gurgaon. He has successfully performed over 7000 spine and brain surgeries in over 20 years of experience and continues to offer life changing treatments to both pediatric and adult patients. He hones surgery of brain and spine including gliomas, meningiomas, pituitary tumors, skull base tumors, craniopharyngiomas, pineal tumors, epilepsy, back spinal cord tumors, pediatric neuro surgery, cervical, thoracic and lumbar disorders, disc herniation, spinal stenosis, spondylolisthesis, spondylotic myelopathy, traumatic and degenerative spinal instability and deformity. He is best known for his exceptionally low complications and high success rate for the most complex patients. There isn’t a condition that cannot be treated in India where the patient needs to go to the West for spine treatment.

Dr. Arun Saroha, one of the best spine doctor in Delhi is also one of the very few in the country who treats pediatric neuro and spine patients. The particular types of brain conditions that arise in children differ in important ways from those found in adults. For children, particular risks and benefits correspond to particular treatments in ways that may be different than for adults. Hence, it is of great importance to consult the right doctor. His surgical expertise also includes extensive experience with minimally invasive techniques as well. Minimally invasive spine surgeries involves smaller incisions, less muscle destruction and lesser blood loss. Dr. Arun Saroha’s reliable and high quality customized treatment makes him one of the top neurosurgeon in India prolonging lives and improving quality of life.
youtube
#best spine doctor in Delhi#Dr. Arun Saroha#Best spine surgeon in India#spine specialist in gurgaon#spine surgeon in gurgaon#Best spine hospital in india#Best spine surgery hospital in india
0 notes
Text
Complications After Cervical Spondylotic Myelopathy Surgery
http://dlvr.it/NBxJ3R
0 notes
Text
About Me:
Qualification
MBBS
MS
DNB (Orthopaedics)
Awards and Achievements
Kamarkar Gold Medal (1994) for highest in surgery at GS Medical College Mumbai & Second Rank in Surgery in Mumbai University.
Pandurangi Award (1996) for Best Resident in Orthopedics.
IOACON Appreciation Award 2005 for outstanding work in spine surgery.
Best Clinical Research Paper Award (Association of Spine Surgeons of India ) 2006.
ASSI Award for Maximum Peer reviewed publications 2006.
Surgical decision making in cervical spondylotic myelopathy – prospective analysis of 115 cases. MASSALLAWALA BEST PAPER AWARD SESSION, WIROC, Mumbai 2006 (Co-Author).
Pathogenesis and staging of craniovertebral tuberculosis. Travel Award. RSNA Chicago, November, 2010 (Co Author).
Recovery Patterns in late onset myelopathy. MASSALLAWALA BEST PAPER AWARD SESSION, WIROC, Mumbai 2010 (Co-Author).
SM Tuli Best Case paper award. Indian Orthopaedic Association Conference, Mumbai, 2012
ASSI-Ingalhalikar Gold Medal for Best Clinical Paper 2013.
MOA (Maharashtra Orthopedic association ) best paper award 2016.
0 notes