#Angina pectoris
Explore tagged Tumblr posts
Text
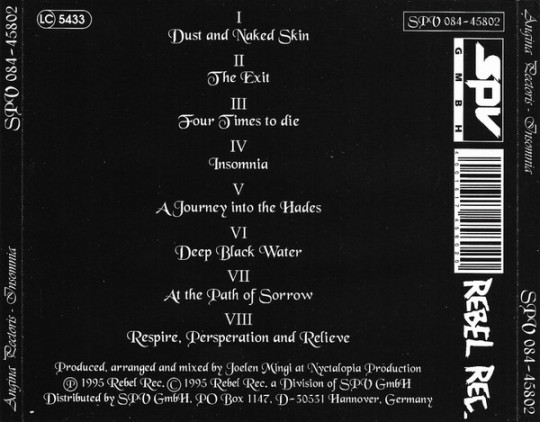
Angina Pectoris – Insomnia
Ahí va la primera banda. La primera en la frente. Chicos/chicas hay que salir un poco de los clásicos. Alguno/a me dira : Tío esos que subes son clásicos a reventar.
Claro! Y tú eres un pureta como yo. Con más años que las ruinas de Göbekli Tepe.
'Insomnia' Label: Rebel Rec. Germany - 1995
youtube

0 notes
Text
“Angina pectoris” di Nazim Hikmet: il cuore di un poeta tra oppressione e libertà. Recensione di Alessandria today
Un inno alla sofferenza universale e alla speranza senza confini
Un inno alla sofferenza universale e alla speranza senza confini Biografia dell’autore.Nazim Hikmet (1902-1963) è universalmente riconosciuto come uno dei maggiori poeti turchi del XX secolo. Nato a Salonicco, allora parte dell’Impero Ottomano, Hikmet ha vissuto una vita segnata dall’impegno politico e dalle lotte per la libertà. Le sue idee comuniste lo portarono spesso in conflitto con il…
#Alessandria today#amore per il popolo#Angina pectoris#battito del cuore.#Cina#cultura turca#cuore diviso#cuore e anima#denuncia sociale#Emozioni#Google News#Grecia#Hikmet poesia#impegno politico#introspezione#Introspezione poetica#Istanbul#italianewsmedia.com#LETTERATURA CONTEMPORANEA#letteratura mondiale#Libertà#Lirica#mela rossa#messaggio universale#Metafora#NAZIM HIKMET#oppressione#Pier Carlo Lava#Poesia#poesia di denuncia
0 notes
Video
youtube
Šta su pravi uzročnici infarkta i šloga?
#youtube#heart attack#myocardial infarction#stroke#atherosclerosis#omega 3#statins#arrhythmia#angina pectoris#cholesterol#ldl cholesterol#hdl#insulin#diabetes#coronary artery disease#bypass#blood vessels
0 notes
Text
Bekam untuk Angin Duduk
22 Juni 2024 membekam pak Herman (37 tahun) dengan keluhan kepala pusing, bahu dan leher kaku dan sakit, serta masuk angin. Kata orang dulu ini adalah Angin Duduk. Kata dokter, Angina Pectoris. Gejala serangan jantung. Gejala tambahan betis dan telapak kaki kebas. Continue reading Bekam untuk Angin Duduk

View On WordPress
0 notes
Text
what do you MEAN nitroglycerine was invented for heart problems????
0 notes
Text
What's Causing My Chest Pain?
Chest pain can be caused by several things, from a heart attack to acid reflux. However, in most cases, chest pain is not caused by a serious problem and can be treated with home remedies.
#chest pain#heart problems#lung problems#muscle pain#artery disease (CAD)#angina pectoris#aortic aneurysm#pulmonary embolism
0 notes
Text
Drugs Used In Angina Pectoris and Myocardial Infarction Short And Long Essay Question And Answers
#Pharmacology#PharmaceuticalIndustry#ClinicalPharmacology#DrugsandResearch#Drugs Used In Angina Pectoris and Myocardial Infarction Short And Long Essay Question And Answers
0 notes
Text
Angina Pectoris is a medical condition characterized by chest pain or discomfort caused by reduced blood flow to the heart muscle. It's a symptom of underlying heart disease and can be a warning sign of a heart attack. If your loved one is experiencing symptoms of Angina Pectoris, seeking timely and appropriate medical care is important. Here is a guide to visiting an Angina Pectoris Treatment Hospital in Noida to help you navigate the process more effectively.
0 notes
Text
I remember being with my friend William one time several years ago. We had driven like 40 minutes to the closest sex shop so we could buy poppers. Then we went to Walmart and drove around on the scooters while doing the poppers. He kept yelling out, "I need this for my angina pectoris!"
For some reason, they kicked us out. Idk, I guess they have a problem with people with heart conditions? Pretty fucked up. I questioned Walmart corporate about it one time but they never responded. Typical ableist shit, you know how Walmart is.
11 notes
·
View notes
Note
pill bitch
Oooh the creativity of anons is unmatched these days :) yeah such a whore for the medication that kept me alive tbh. Btw guys my heart and pacemaker are back at it and i'm without heart medication for a while now. So far the risk of heart attacks / angina pectoris is declining. Thats so cool.
16 notes
·
View notes
Text

These stupid fucking ads give me angina pectoris
3 notes
·
View notes
Text
Angor animi (also referred to as angina animi,[1][2] Gairdner's disease[2] and also angina pectoris sine dolore[2]), in medicine, is a symptom defined as a patient's perception that they are in fact dying. Most cases of angor animi are found in patients with acute coronary syndrome (cardiac-related chest pain) such as myocardial infarction.
If you are having a heart attack and think you might be dying aren’t you just like. Accurately assessing the situation?
26 notes
·
View notes
Text
Let Me Tell Ya Something: Artists and Writers of the Aestheticism Movement
(Note: I've gone bonkers at the end of it)
The art movement called ‘Aestheticism” is both interesting and weird.
The movement originally started back in 1860 and ended in 1900 (At least according to articles and Youtube videos).
There are two sections or categories that Aestheticism is found in (or at least I'm interested in). Art and Literature. But first…
What Is Aestheticism?
Aestheticism is basically the embodiment of “Art for the sake of art”
As Aestheticism was uninspired by the natural world, and instead only showed the shallow beauty of things. As the article that I read wrote; Beauty escapism. Or something along those lines. The movement chose beauty over sharing political and/or social ideas. Aestheticism showcased the beauty of manly or female beauty and created a new fashion trend as it influenced public consciousness. Aestheticism was also associated with the Decadent movement. Aestheticism looks back to the art of the past, similar to the Renaissance, but with no substance other than being food for the eyes. (You can correct me if I'm wrong)
Aestheticism is also a philosophy. The study and nature of beauty.
Artists During The Aestheticism Movement
(Note that information about these artists and writers in this blog may be insufficient, and I will shorten the description of each individual as much as possible)
- Dante Gabriel Rossetti (I am unsure how his surname is spelled, as it kept changing between sources)
- Lord Leighton
Dante Gabriel Rossetti
Born in London, England on May 12, 1828. He was the most celebrated member of the Rossetti family. Rossetti was an English artist and poet. He helped found the Pre-raphaelites Brotherhood, painters who were just haters of Raphael��s and Michelangelo’s works to put it simply and lightly. But, by the 1860s, he moved on from the pre-raphaelites and was searching for something new to paint.
Rossetti was known for painting his muse (and wife, which is cute) Elizabeth Siddal, who had pale skin and bright red hair. A trait considered to be ‘undesirable’ back then (and also they associate them with witches if I’m correct?) But, because Rossetti continued to paint Elizabeth, the beauty standard between people with red hair began to change, he made red hair socially acceptable.
He eventually died in 1882 on Easter Sunday. His health withered due to Chloral, while his wife died due to Laudanum (a drug made of 10% opium). Rossetti died of Bright’s disease, which he was suffering from for quite some time now.
This is unfortunately the only information that I wrote down about him. I do not have the time to do further research about him. For I have a group activity to do ;-;
Lord Fredric Leighton
Born in Scarborough, United Kingdom on December 3, 1830.
Now, let me tell you this. HE IS RICH AF. His dad paid his allowance for his whole life. Like, are you fr????
Anyways. Based on my notes he:
Became the President of the Royal Academy in 1878 and lasted until he died in 1896.
He was the most famous artist of his day and won many honours and national awards. He also worked on a house till his death, he lived inside that house for 30 years and worked on it around the mid-1860s. The house had multiple styles (And looks rad af). The sources came from Italian Renaissance and the architecture from the near east. The house is often described to as a “Private palace of art”
Leighton would travel around Europe and often come back to Florence and Rome until his death. And, up to this day, it is debated whether he had an illegitimate child with one of his models, or if he was a homosexual. (tbh, I think he’s the latter)
Lord Leighton died on January 25, 1896. Due to Angina Pectoris. A symptom of heart disease, but could be a sign of a heart attack.
Writers During The Aestheticism Movement
- Oscar Wilde
- Algernon Charles Swinburne (will forever remember such a badassatron surname)
- Ernest Dowson
Oscar Wilde
(As his surname implies, dude’s a wildin’)
The most famous artist and writer during the Aestheticism movement. Born on October 16, 1854, in Westland Row, Dublin, Ireland. Wilde was both a poet and a playwrite. Wilde attended Trinity College and Oxford University. His works were often flamboyant and witty. He won the Newdigate prize back in 1878. He was first inspired by aestheticism through what Walter Pater taught.
And just like a peacock, he LOVED attention, good or bad he would GOBBLE IT UP. He got married in 1884 and had two kids with his wife. And since a peacock is a bird and birds can be gay (not peacocks though, which ruins this analogy), Oscar Wilde was imprisoned due to his gayness, to say the least. He had a relationship with Lord Alfred Douglas, and he (Oscar Wilde) was accused to be a ‘Sodomite” aka; he likes hot butt sex. (iyyk)
When he was finally freed from prison, he went to France. But he went bankrupt and died broke. He died due to meningitis and a condition called “I’m Broke Bruh” (IBB) in Paris in 1900.
Algernon Charles Swinburne
Born in London, 5th of April 1837. Swinburne was a famous lyric poem of his time. Mostly a poet, but he also wrote novels, plays and critics. Swinburne contributed to the Encyclopedia Brittanica,
Swinburne’s works tackled subjects such as atheism and cannibalism, subjects not often read in books, poetry or of any kind. He went to Eton and Oxford University. There, he met Dante Gabriel Rossetti.
And according to my notes, he liked scaring people. His works that were often tackling sadomasochism shocked people, so much so their heads must’ve split open, an image I wish I didn’t imagined while writing this. One of his famous work was called “Poems and Ballads” a collection of… well.. poems and ballads.
Swinburne eventually died on April 10, 1909, due to flu. Bro had a badassatron name but died in a not do badassatron way (I'm not saying dying due to flu is boring, I just didn't expect him to die that way)
Ernest Dowson
Born in Kent, England back in 1867. He was a novelist and a poet (like me, but he was successful). He was considered a Decadent writer due to his age and reputation. He also followed the ideals of the Aestheticism movement. And his most famous work came to fruition because of an unrequited love. And just like most authors, he died broke. (That’s my future right there) He died of tuberculosis at the age of 32, on February 23, 1900.
Moral of the Story
If you're a writer, you're going to die broke, and maybe young.
If you're an artist, and have not been born in a wealthy family. You're going to die broke.
#writeblr#writing#writers and poets#art#artists on tumblr#aestheticism#aesthetic#Information may not be accurate#Let me tell ya something
3 notes
·
View notes
Text
When I was born, my maternal great grandmother gave me a generous gift of Pfizer stock. She had been impressed by Pfizer’s key role in discovering how to mass produce penicillin during World War II (in which her son was killed in action). Eighteen years later her gift paid for my university education. And then, in 1998, Pfizer received FDA approval to sell Viagra.
Pfizer initially developed the drug to treat high blood pressure and angina pectoris. However, as Pfizer’s researchers discovered in clinical trials, the drug was better at inducing erections than managing angina. And so, the company repurposed the drug for erectile dysfunction and launched a massive, global PR and marketing campaign—including seeking moral approval from Pope John Paul II and contracting the war hero and 1996 presidential candidate Bob Dole to be the brand’s poster gentleman—that succeeded in making Viagra a blockbuster.
So, I learned why pharmaceutical companies seek to develop blockbuster drugs with fanatical zeal. Formulating a safe and effective new medicine to address a large, unmet need is very difficult and expensive. Performing clinical trials and obtaining FDA-approval is an arduous process that normally takes several years. Thus, if an opportunity for a new blockbuster presents itself, a big drug company like Pfizer will go to extreme lengths to seize it.
Three years after the release of Viagra, I learned that Pfizer was not the respectable company my great grandmother had believed it to be. I arrived at this realization through my interest in British spy novels. In 2001 I lived in Vienna, around the corner from the Burgkino (Burg Cinema) which still played the 1949 film noir classic The Third Man on its big screen every weekend. I spent many a dreary winter Sunday afternoon watching the film. Based on the novella and screenplay by Graham Greene, The Third Man is a crime story about Harry Lime—an American running a medical charity in Vienna, who makes a killing selling penicillin on the bombed out, impoverished city’s black market. To increase his profits, he cuts the drug with other substances, thereby destroying its efficacy and causing the patients (including children) to die horribly from their infections.
2 notes
·
View notes
Text
Drugs Used In Angina Pectoris and Myocardial Infarction Short And Long Essay Question And Answers
#Pharmacology#PharmaceuticalIndustry#ClinicalPharmacology#DrugsandResearch#Drugs Used In Angina Pectoris and Myocardial Infarction Short And Long Essay Question And Answers
0 notes