#ventricular pressure
Explore tagged Tumblr posts
Text
Ventricular Ejection
-- follows isovolumetric ventricular contraction
-- both ventricles continue to contract
-- the ventricular pressures exceed aortic and pulmonary arterial pressure
-- the aortic valve and pulmonary valve open
-- blood is ejected into aorta and pulmonary artery
#studyblr#notes#medblr#medical notes#med notes#ventricular ejection#ventricular contraction#ventricles#ventricular pressure#pulmonary valve#aortic valve#aorta#pulmonary artery#arterial pressure#aortic arterial pressure#pulmonary arterial pressure#cardiology#cardio#cardio notes#cardiology notes#cardiovascular system#cardiovascular notes#cardiovascular system notes
5 notes
·
View notes
Text
Danny's medical tests
Vitals and thresholds:
Age: 16
Pulse: 20 bpm resting, 54 bpm active (54 atrial, 30 ventricular), grayout at 80/35, blackout at 90/35. (Can stop heart for up to three minutes without repercussions; becomes painful after two)
Respiration: 6 breaths per minute resting, up to 30 active, no more than 15 resting. (Can slow to 1 breath per minute for up to half an hour; strain sets in after twenty)
Blood pressure: 90/40 (blood reaches his brain with Magic)
Temperature: between 50° and 80° (human) or 0° and 32° (ghost) Cold tolerance is no lower than 3° in human form, heat tolerance no higher than 90°
Height: 5’3’’
Weight: 101 lbs (3/5 what his weight should be by build)
Ectoplasmic purity: between 80% and 90% (low, normal for halfas)
Core pitch: 29 kilohertz (low, normal for halfas)
Power level: 214 (out of 300)
Aura brightness: 154 (low, lack of obsession fulfillment)
List of tests, results, and consults:
ECG shows a third degree AV block with a ventricular escape rhythm.
Echocardiogram shows no physical abnormalities.
Event monitor shows mild strain (palpitations, discomfort) with normal exercise and stress, moderate strain (chest pain, shortness of breath, dizziness) with high activity and stress.
(“No, this is pretty much what I remember exercise feeling like.”)
Blood reacts violently to all potential donors
Blood tests:
>Complete blood count:
>>White blood cells: slightly elevated, also weird (green, have faces)
>>Red blood cells: low (thinner blood)
>>Hemoglobin: high (red blood cells carry more oxygen)
>>Hematocrit (percentage red blood cells): 29%
>>Mean corpuscular volume: slightly low (smaller red blood cells)
>>Mean corpuscular hemoglobin: high
>>Mean corpuscular hemoglobin concentration: high
>>Red cell distribution width: low
>>Platelet count: low and also they are all green
>Comprehensive metabolic panel:
>>Glucose: 50 mg/dl (low)
>>Blood urea nitrogen: low (good kidney function)
>>Creatinine: low (good kidney function + can indicate low muscle) (this is not because of low muscle this is because of Ghost)
>>Estimated glomerular filtration rate: high (good kidney function)
>>BUN/Creatinine ratio: 12:1 (normal)
>>Sodium: high (electrolyte)
>>Potassium: very high (ectoplasm component) (electrolyte)
>>Chloride: very high (ectoplasm component) (electrolyte)
>>Carbon dioxide: low (waste product)
>>Calcium: high (electrolyte)
>>Protein, total: normal (plasma)
>>Albumin: slightly low (should be normal) (sign of malnutrition)
>>Globulin, total: high (high immune function)
>>Bilirubin, total: normal
>>Alkaline phosphotase: low (slow metabolism)
>>Aspartate aminotransferase: low (no liver damage)
>>Alanine transaminase: low (no liver damage)
>Lipid panel:
>>Cholesterol: normal
>>Triglycerides: low (dietary)
>>HDL Cholesterol: slightly low
>>VLDL Cholesterol Cal: normal
>>LDL, calculated: normal
>>Chol/HDL ratio: normal
>Thyroid tests:
>>Thyroid-stimulating hormone: low
>>Thyroxine: low
>>Triiodothyronine: low
DNA test: Takes an extremely long time to fully process, but early results show that Danny’s DNA is covered in a thin layer of ectoplasm, making the underlying structure difficult to decipher. Programming a machine to recognize it could be difficult.
Urine tests: normal
Pulmonary function tests: normal
Allergy panel shows no reactions.
Hypermobility test shows hypermobility in spine, elbows, and knees. No other signs of EDS, tentatively ascribed to his abilities.
Dietitian consult: nothing concrete yet. They discuss Danny’s eating habits, deal frankly with the fact that they don’t know what his exact dietary needs are, and talk about intuitive eating. Danny gets a list of signs to look out for and things to try.
Endocrinologist consult: they discuss Danny’s concerns and assess his current stage of puberty. Danny states (visibly mortified) that he has grown two inches since his accident, no vocal deepening, no facial or body hair, no reproductive function benchmarks. They discuss various possible causes of delayed puberty (excessive exercise, psychosocial problems, physical trauma, irradiation) as well as treatment options. Danny asks what circumstances would normally have them recommend inducing puberty (bullying, ostracization, distress) and they finally decide to go ahead and induce it.
Semen analysis: Danny is producing normally but the sperm die before exiting.
Slit-lamp exam shows tapetum lucidum in human form and odd eye structure in ghost form.
Autonomic nervous system tests:
>Gag reflex: Sensitive in human form, inactive in ghost form
>Motor reflexes (jaw jerk, biceps, triceps, brachioradialis, finger jerk, knee jerk, ankle jerk, superficial abdominal): hyperactive, forceful, but controlled. Identical in both forms.
>Pathologic reflexes: None present
>Cardiovagal function:
>>Heart rate variability: [not applicable because of heart condition]
>>HR response to deep breathing: exaggerated. This is how he stops his heart.
>>Valsalva: perfect adaptation. (blood pressure self-regulates rapidly)
>Vasomotor adrenergic function:
>>BP response to standing: perfect adaptation.
>>Tilt table testing: perfect adaptation. (blood pressure self-regulates rapidly)
>Sudomotor function:
>>QSART: Exaggerated in human form, not present in ghost form. (sweat response)
>>Silastic sweat test: Exaggerated in human form, not present in ghost form.
>Salivation: Normal in human form. No response in ghost form.
>Pupillography: rapid in human form, not present in ghost form.
>Cold pressor test: done with salted ice water. Reduced response. (sympathetic nervous system test)
Human CT scan was normal.
Ghost CT scan was semitransparent but otherwise normal.
Vaccine test shows good immune system function.
Human fNIRS, EEG, and MEG brain scans were used primarily for mapping. Showed normal activity for motor function and sensory activity, slightly reduced activity for memory exercises and problem solving, and substantially reduced activity for emotional responses.
Ghost EEG and MEG brain scans were used primarily for mapping. Showed no activity for motor function, mild activity for sensory and memory functions, and moderate activity for problem solving and emotional responses. No brain stem activity. (fNIRS not performed because it monitors blood oxygen activity in the brain and his ghost form doesn't have that)
Human MRI scan is largely normal, but shows darkened nerves on the left hand.
Ghost MRI scan indicated that his insides are abnormally malleable but highly coherent. Nerve damage is much less apparent owing to minimal function.
Human EMF reading showed increased activity corresponding to reduced brain activity.
Ghost EMF reading showed moderate activity for everything except emotional responses, which indicated strong activity.
Nerve conduction study shows severe nerve damage in ulnar and median nerves in human form, no nerve response in ghost form.
Electromyography shows that very few electrical signals are being transmitted in his left hand, Danny moves his hand with Magic. Otherwise normal readings in human form, ghost form shows no readings at all.
Polysomnography shows several signs associated with hibernation, making Danny’s sleep deeper, but his brain waves still indicate REM sleep in a normal pattern.
All biopsies normal except the inclusion of ectoplasm.
Microneurography was for mapping only.
The doctors manage to create an external device that can monitor the EMF activity of Danny’s core in milligauss, as well as his core pitch. It outputs it as a graph. Danny’s core EMF is 3,210, and his resting surface EMF in ghost form is around 2,000, with a total range of 200 feet. In human form, this is significantly reduced to 800 mG at the surface, and a range of 80 feet. (GIW sensors only detect as low as 900 mG, while the Fentons’ goes as low as 750.)
Core EMF level varies from ghost to ghost, measured on a scale that goes from 1 to 300. This is found to be equivalent to 15 to 4500 milligauss. All but around 2/3 of radiation is naturally contained, but the amount rises rapidly with power use.
#sorry when i saw today's dannymay theme i had to lmao#these notes are for 'more like home' but it's still just danny's baseline biology so#also i know this is SO dry but i thought some people might be interested anyway#dannymay2025#danny phantom#danny fenton#halfa biology
183 notes
·
View notes
Text
The Difference Between Heart Attack, Heart Failure, and Cardiac Arrest
I think fiction has done us a huge disservice when they conflate the above, but even my nursing students were kind of on the edge of not understanding this, so we're gonna talk about it here.
Heart Attack: A blockage in the coronary arteries
A heart attack, also called a myocardial infarction, is when one of the arteries that supplies the actual muscle of the heart gets blocked by a blood clot. When this happens, the muscle the artery was supplying starts to die. The more muscle impacted, or the longer the heart attack goes untreated, the worse the outcome for the patient.

Symptoms of this are different between men and women:

Treatment for a heart attack usually involves inserting a small tube into the wrist or groin, snaking it up to the blocked artery, and stenting open the blockage, thus returning blood flow to the heart muscle.
Heart Failure: A problem with the heart's ability to pump
Heart failure occurs when the heart is not beating hart enough or well enough to adequately get blood out to the body. This can occur for several reasons. It can be because of damage from a heart attack, because a valve in the heart isn't working right, from poorly functioning electrical system, or from long term exposure to untreated high blood pressure.
The symptoms of heart failure come both from blood collecting "in front" of the heart waiting to get pumped (swelling, shortness of breath, weight gain), and not enough blood getting pumped out to the body (dizziness, fatigue).

Heart failure is treated with medications that make the heart beat more normally and get rid of excess fluid to take workload off the heart. It can also be treated with surgery if the problem is with a valve, or with a pacemaker if the heart is beating too slowly.
Cardiac Arrest: A problem with the heart's electrical system
The heart beats in a synchronized way because it is made of muscle cells that are responsive to electricity. Special cells called pacemaker cells generate small electrical currents, which wash over the heart. When the cells are stimulated with that current, they contract, creating a beat.
Cardiac arrest occurs when that normally organized current becomes disorganized, and lots of cells, not just the pacemaker cells, start making their own currents. This can happen because of a lack of oxygen, too much or too little of particular electrolytes like potassium, an electrical shock, or damage to the muscle from a heart attack.
See below for a comparison between the normal electrical activity of the heart (top) and the disorganized rhythm of ventricular fibrillation:

When the electrical rhythm is disorganized, the heart isn't beating, just quivering, and no blood gets out to the body. This is treated with CPR to keep some blood flowing to vital organs, medications that can stabilize the heart's electrical system, and defibrillation. Defibrillation works by stopping the heart with an overwhelming amount of electricity and letting it restart (hopefully) in a normal rhythm.
If someone has no electrical activity in their heart (known as asystole), defibrillation won't work, but sometimes medication will.
198 notes
·
View notes
Text
Writing Notes: Caffeine

Caffeine - A mild alkaloid stimulant made by some plants.
Found in coffee beans, tea leaves, and cocoa beans; added to soft drinks, energy drinks, and energy bars; and sold in capsules and tablets as a dietary supplement.
A mild stimulant. It is used to temporarily relieve fatigue and increase mental alertness. Caffeine is added to some antihistamine drugs to help counteract the sleepiness they may cause. It is also added to over-the-counter headache remedies (e.g., Excedrin) and migraine headache drugs to enhance their painkilling effects. Under medical supervision, citrated caffeine (a prescription drug) is used to treat breathing problems in premature infants.
From the Italian word cafée, meaning "coffee", is naturally made by about 60 plants. The most familiar of these are coffee leaves and beans, tea leaves, kola nuts, yerba mate, guarana berries, and cacao (the source of chocolate). In plants, caffeine is a pesticide. Insects eating plants that contain caffeine become disabled or die.
It has no nutritional value. But there seem to be some benefits to regular caffeine consumption, despite conflicting research.
Effects on the Body
Increases heart rate
Temporarily increases blood pressure
Relaxes smooth muscle cells in the airways
Releases fatty acids and glycerol in the body for energy use
Easily crosses the blood-brain barrier and changes the level of neurotransmitters in the brain
Passes into breast milk
Caffeine is absorbed in the stomach.
Its effects are noticeable in about 15 minutes and usually last several hours.
However, there is a huge variation among people both in their sensitivity to caffeine and in how long it stays in their bodies.
Although the average time it takes half a dose of caffeine to be eliminated from the body is 3-4 hours, this time may extend to 6 hours in women taking oral contraceptives; much longer in pregnant women and in people with liver damage.
Many well-designed, well-documented studies show that caffeine makes people more alert, improves short-term memory, enhances the ability to concentrate, increases the individual’s capacity for physical work, and speeds up reaction time.
In habitual caffeine drinkers, caffeine achieves this by preventing the detrimental effects of withdrawal.
It does not boost functioning to above normal levels.
All of these effects are temporary.
Caffeine does not replace the need for rest or sleep.
Caffeine Withdrawal
Discontinuing caffeine among regular users can cause withdrawal symptoms. These can include:
Headaches (very common)
Irritability
Nausea
Fatigue
Sleepiness
Inability to concentrate
Mild depression
Caffeine withdrawal symptoms begin 12–24 hours after caffeine is stopped.
Withdrawal symptoms peak at around 48 hours, and can last up to 5 days.
Tapering caffeine use, for example cutting down on caffeine by the equivalent of half a cup of coffee (about 50 mg) a day, minimizes or eliminates withdrawal symptoms.
Caffeinism
People who consume more than 500 mg of caffeine a day—equivalent to about five cups of coffee—may develop a condition called caffeinism, though the threshold varies among individuals.
Produces unpleasant sensations, some of which are similar to withdrawal symptoms. Symptoms of Caffeine Overuse include:
Restlessness
Irritability
Nervousness
Anxiety
Muscle twitching
Headaches
Inability to fall asleep
A racing heart
Related Disorders
Severe overuse of caffeine can cause a number of related disorders, including:
Caffeine Intoxication—usually the result of taking caffeine pills (e.g., NoDoz), this condition causes mental changes, rambling thoughts and speech, irregular heartbeat, and other symptoms associated with overuse. In severe cases death can result from ventricular fibrillation (unsynchronized contractions of the ventricle of the heart).
Caffeine-Induced Anxiety Disorder—severe anxiety that interferes with daily social interactions and occurs after caffeine intoxication or heavy long-term use of caffeine.
Caffeine-Induced Sleep Disorder—an inability to sleep that is so great it requires medical/psychiatric attention and occurs after prolonged caffeine consumption.
Non-Specific Caffeine-Induced Disorder—disorders not listed that are attributable to either acute or long-term caffeine consumption.
Source ⚜ More: Writing Notes & References ⚜ Describing Food ⚜ Cocktails
#caffeine#writing notes#writeblr#dark academia#spilled ink#writers on tumblr#writing reference#literature#writing prompt#poets on tumblr#poetry#writing inspiration#writing ideas#coffee#tea#creative writing#fiction#giuseppe de nittis#writing resources
156 notes
·
View notes
Text
Olivia’s Unfinished Story
*Happy Friday, everyone! I wanted to try something a little different this time around. I hope you enjoy!*
Her name was Olivia.
She was the kind of woman you might overlook in a crowd- slim, fair skinned, with straight, light brown hair that she kept neat and cut to her shoulders. Her bangs sat just above a pair of green eyes that always seemed to be watching, not out of shyness, but observation. At 5'8, the twenty-eight year old carried herself with quiet poise, a strange mix of bookish awkwardness, and buttoned-up grace. Her wardrobe was sensible- cardigans and slacks, modest blouses, neutral tones. It wasn’t that she lacked style; she simply didn’t think anyone was looking closely enough to warrant the effort.
By day, Olivia worked a corporate job in a beige office on the twelfth floor of a building with too much glass and not enough personality. Her cubicle was tidy. Her emails were prompt. She was the type who remembered birthdays, who always signed her messages with "Best," and who brought her lunch from home in reusable containers labeled with masking tape. Her coworkers liked her well enough, though they never really knew her. She existed on the periphery- reliable, polite, self-contained.
But at night, in a small apartment with a flickering desk lamp and chipped mugs of tea, Olivia became someone else. She wrote under the name "S.R. Quinn," a pseudonym she guarded like a secret lover. Her stories- twisting, cerebral mysteries filled with unreliable narrators and haunted minds, had attracted a quiet, devoted following online. Some of her readers speculated about the author's identity, but she never gave herself away. Olivia preferred it that way. Her characters said all the things she couldn’t. They unraveled in ways she never allowed herself to. Writing, for her, was a kind of release- a hidden doorway she stepped through every night.
She lived alone, but it never really felt lonely. Her walls were lined with shelves full of books, and her laptop bore the fingerprints of a thousand edits.
She had routines: the same route to work, the same booth at the quiet café near her apartment, the same brand of peppermint gum always tucked into her bag. Sometimes, on the subway, she would look at the people around her and wonder who among them led secret lives, too. It comforted her to think she wasn’t the only one pretending.
There were things she still wanted to do. A novel half-finished. A mystery not yet solved. A character she hadn’t quite figured out.
She had no idea she would be the latest patient in our emergency department. Last night, that’s exactly what happened to Olivia.
The trauma bay lights cast a sterile glow across her pale skin, and her chest bucked beneath gloved hands performing deep, violent chest compressions. The monitor beside her beeped incessantly in arrhythmic protest, displaying a jagged line of ventricular fibrillation. Beneath it, a stack of empty syringe caps and torn vials spilled from the tray, scattered among crumpled wrappers and used IV bags.
She lay supine on the table, stripped barefoot and topless, her bare chest glistening with conductive gel under the harsh overhead lights. Her green eyes were wide open- glassy, unblinking, eerily serene. The endotracheal tube jutted from her mouth, hugging her pale lips, secured tightly with tape, and the soft hiss of the ambu bag filled her lungs with each squeeze. Her pants remained on, the dark fabric in contrast to the table. There were no bruises, no blood, no visible trauma. Just a stillness that didn’t belong in a room like this.
The rhythm of chest compressions played like a grim metronome, gloved hands stacked over her sternum, pushing deep and fast. Each thrust drove Olivia’s chest down in sharp, unnatural motions, her ribs caving beneath the pressure. With every compression, her chest recoiled slightly, the skin pulling tight before collapsing inward again. The force rippled outward through her torso, making her belly tremble faintly.
The defib paddles were pressed against her bare chest. “CLEAR!” Dr Lindsay called out.
Her back arched as the jolt surged through her, then fell limp again. No change. Someone stepped up to resume CPR. The rhythmic thud of gloved hands on her sternum resumed, tilting her motionless face slightly with each thrust.
After that unsuccessful cycle of CPR, the paddles pressed back down against her bare chest, gel smearing beneath them. “CLEAR” Lindsay called once again. A sudden jolt of electricity surged through the writer’s body. Olivia’s back arched sharply, her spine lifting off the table in a stiff, unnatural bend. Her legs jerk in response- one foot kicking upward involuntarily, the other twisting inward, toes curling hard. For a split second, both feet hover awkwardly in the air before crashing ungracefully back down to the table. Her soles, flushed pale from poor perfusion, land heel-first, the deep, wide, soft wrinkles of her size 10 soles visible before her body goes slack again, motionless except for the rhythmic force of compressions that resumed after.
Another shock was delivered. A gasp escaped Olivia’s lips, though it was more of a reflex than a sign of life. Another cycle CPR ensued. A dose of epinephrine. Gloved hands moved with rehearsed precision, voices sharp, clipped, and clinical.
“Still in v-fib, Linds.” Nurse Nancy informs, shaking her head. “No pulse.” Dr Jen the resident chimes in.
“I’m shocking again. Re-charging the paddles to 360. CLEAR.” Lindsay responded, Heather halting CPR and stepping away from the table.
KA-THUNK! Olivia’s body jumped. The flat, lifeless gaze remained on her face. Her expression was untouched by fear or pain, frozen somewhere just before the end.
The next shock came and went. Her body jerked with unnatural stiffness, like a puppet pulled by unseen strings. For a breathless second, she froze midair- fingers curled, toes flexed, then collapsed on the table once more, as if gravity remembered her all at once.
Chest compressions resumed, but not for long. For a moment, the room stilled- hands hovered, eyes glanced to the monitor. A flatline stared back at everyone, unbroken and absolute.
“No cardiac activity on the monitors.” Jen the resident informed, calm and even, like they’re noting the time of day.
Nancy leaned in, shining a penlight across both of Olivia’s eyes. Nothing. No flicker, no constriction, no reaction whatsoever- just the blank, glassy look of fixed and dilated pupils.
A quiet pause passed.
“She’s been down forty minutes.” Lindsay speaks, voice low but certain. “Let’s go ahead and call it. Time of death, 1:11am.”
The ambu bag was detached from the ET tube and set beside Olivia’s head on the table. Chest compressions stopped for good. Heather shut off the monitor, muting the flatline. The paddles were placed back on the crash cart, the ECG leads peeled away, electrodes discarded in silence.
Olivia had written dozens of stories. None of us knew that, of course. Not Heather peeling off her EKG leads, not Dr Lindsay logging her time of death, not Dr Jen placing the sheet over her body. In life, she had been anonymous. In death, she remained so.
But somewhere, tucked into online archives and under a username no one could now trace, there were worlds Olivia had built. Complex characters. Tangled mysteries. Paragraphs people had read and re-read and bookmarked to revisit. She had more to tell. But last night, her story ended right here in our emergency department.
#resus writing#resus community#resus#cpr resus#cpr#cpr female#dark cardiophilia#medfet#defib#defibs#defibrillator#chest compressions#intubation
56 notes
·
View notes
Text

Paramedic Incident Report
Incident Number: 2024-19245 Date: December 6, 2024 Time of Call: 15:23
Incident Location: ClimbX Indoor Gym, 345 Summit Street, Boulder, CO
Patient Information:
Name: Daniel Carson
Age: 20
Gender: Male
Height: 5'11"
Weight: 165 lbs
Physical Description: Lean and muscular build with well-defined arms and torso typical of an experienced climber. Short dark brown hair, light complexion.
Description of Incident: At 15:23, dispatch received a 911 call reporting a young male climber had collapsed while bouldering at an indoor climbing facility. The patient was reportedly scaling a mid-level climb when witnesses described him suddenly clutching his chest, losing his grip, and falling to the mat below. He was unresponsive upon initial assessment by gym staff.
Initial Assessment Upon Arrival (15:30):
Level of Consciousness: Unresponsive
Pulse: Absent
Respiratory Effort: None
Skin Condition: Pale, cool, and clammy
Pupils: Fixed and dilated
Bystanders reported that staff initiated CPR immediately after the collapse and delivered one shock using the facility's automated external defibrillator (AED).
Treatment at Scene (15:30-15:45):
CPR: High-quality chest compressions continued upon paramedics’ arrival.
Airway Management: Airway secured with a bag-valve mask; oxygen at 15 L/min.
AED Analysis: AED advised one additional shock, which was administered at 15:35. Return of spontaneous circulation (ROSC) achieved at 15:37.
Vital Signs Post-ROSC:
Pulse: Weak and irregular at 45 bpm
Blood Pressure: 80/50 mmHg
Respiration: Shallow and labored at 10 breaths/min
Oxygen Saturation: 78%
Transport Summary (15:45-16:00): Patient was loaded into the ambulance for transport to St. Anthony's Hospital. During transport, the patient exhibited further signs of cardiac distress. At 15:50, he experienced ventricular fibrillation (VF).
Intervention: CPR resumed, epinephrine 1 mg administered IV, and defibrillation attempted twice.
Outcome: No ROSC achieved after second cardiac arrest.
Time of Death: 16:00
Remarks: The patient suffered two cardiac arrests within a 30-minute period, likely indicative of a severe underlying cardiac condition. Efforts to stabilize were unsuccessful due to continued arrhythmias and compromised circulation.
Autopsy Report
Case Number: 2024-AU-1245 Date of Examination: December 7, 2024 Time of Examination: 09:00
Name: Daniel Carson Age: 20 Height: 5'11" Weight: 165 lbs Sex: Male Race: Caucasian
External Examination:
General Appearance: Well-developed and muscular young male. No evidence of external trauma except for mild abrasions on the back of hands and forearms, consistent with climbing activities. Skin pale with slight cyanosis around the lips and nail beds.
Scars/Marks: None significant.
Tattoos: None noted.
Clothing: Patient arrived wearing climbing shorts and a tank top.
Internal Examination:
Cardiovascular System:
Heart: Enlarged, weighing 420 grams (average for age/weight: 300-350 grams).
Valves: Mitral valve revealed significant calcification and fibrosis, indicative of a congenital defect. The defective valve exhibited stenosis, which restricted blood flow and created turbulent circulation.
Coronary Arteries: Severe occlusion (95%) of the left anterior descending (LAD) artery due to atherosclerotic plaque.
Myocardium: Evidence of acute ischemic changes and scarring, suggesting prior silent infarctions. The ventricular walls were thickened (hypertrophic cardiomyopathy).
Aorta: Normal caliber and appearance.
Respiratory System:
Lungs congested, with frothy fluid in the trachea and bronchi.
Right lung: 450 grams; Left lung: 430 grams.
Gastrointestinal System:
Stomach contained approximately 200 mL of partially digested food.
No abnormalities in the esophagus, stomach, or intestines.
Central Nervous System:
Brain weight: 1,450 grams. No gross abnormalities.
Other Organs:
Liver: Enlarged (1,600 grams), possibly due to mild congestion.
Kidneys: Unremarkable.
Spleen: Normal size.
Microscopic Examination:
Heart Tissue: Acute myocardial infarction visible in sections of the left ventricle.
Coronary Arteries: Advanced plaque buildup with rupture and thrombus formation.
Mitral Valve: Fibrotic thickening and calcification evident.
Toxicology:
No evidence of drugs or alcohol.
Summary and Cause of Death: Daniel Carson, a 20-year-old male, died from complications of a congenital mitral valve defect and severe coronary artery disease. The primary event was a massive myocardial infarction triggered by the blockage of the LAD artery. A second cardiac arrest during transport proved fatal.
Final Diagnosis:
Acute myocardial infarction secondary to LAD artery occlusion.
Congenital mitral valve stenosis and calcification.
Hypertrophic cardiomyopathy contributing to cardiac instability.
Cause of Death: Cardiac arrest due to a defective valve and blocked artery.
Manner of Death: Natural.
Signed by: Dr. Margaret Li, MD Pathologist
29 notes
·
View notes
Text
My ideas on how pressure works
* Warning: I am not a professional, this is just a speculation based on info found online *
While looking up about commotio cordis, I learned that mechanical stress on cardiac muscle causes it to discharge an electrical signal, disrupting the electrical activity of the heart.
I thought that since pressure is causing mechanical stress on the heart, the reason why pressure causes irregular heartbeats follows a similar principle.
Irregular beats can be divided into two categories, and I will speculate why pressure causes each type of irregular beat.
1. Atrial ectopic beat
These are caused by abnormal electrical signals from the atrium. Pressure disrupts blood flow in the heart. And I think because the walls of the atria are thin, disruptions in blood flow can cause abnormal stretching of the atria walls, causing them to release abnormal electrical signals. These cause atrial ectopic beats, such as PACs, and if you’re lucky, SVT.
2. Ventricular ectopic beat
These are caused by abnormal electrical signals coming from the ventricles. Normally I don’t get much of these with light pressure, so I think that you need heavy pressure to create the sufficient mechanical stress to make the ventricles misfire. This causes PVCs and VT.
I also think that by controlling the amount and location of pressure, you can control what kind of irregular heartbeat you get. With light pressure near the base of the heart, to screw with blood flow, you get PACs and SVT. With heavy pressure on the ventricles(near the apex), you get PVCs and VT.
These are just my thoughts on how pressure works. This may be totally wrong, so don’t take it too seriously.
36 notes
·
View notes
Note
Hope it's okay to ask two questions in one ask! One: Tension pneumothorax. I know this can be deadly because it puts pressure on the heart and other lung, but can the patient feel the pressure building before it gets to a critical stage? How deep does the decompression needle go (and can anything be substituted if they don't have one handy?) Are there any other ways to get one than a sucking chest wound? Two: People always say jarring a hypothermic patient can result in lethal arrhythmia, but they never really say what kind. Would they generally be shockable rhythms? "They're not dead until they're warm and dead" would be in full force!! Thank you! (And sorry if this duplicated!)
Of course you can ask two questions!
Patients can certainly feel chest pain and pressure before a pneumothorax becomes critical. The decompression needle has to penetrate the skin, subcutaneous tissue, muscle, and pleural sac, so it is about 5 to 8 centimeters long and will penetrate that deep. The length may vary depending on the size of the patient. A makeshift needle would need to be something long, thin, and sharp. I'm not sure what would work of the top of my head. Aside from sucking chest wounds, a tension pneumothorax can also be caused by blunt force trauma, rib fractures, decompression sickness that affects the lungs, pre-existing lung disease, and invasive procedures involving the lungs, chest, and ribs. Spontaneous pneumothoraxes can also sometimes occur in athletic young men and teenage boys.
Jostling a hypothermic patient can indeed cause arrhythmias such as sinus bradycardia, atrial fibrillation (A-fib), junctional rhythms, AV block, and ventricular fibrillation (V-fib). V-fib is the only shockable rhythm among these, however it may not be responsive to defibrillation in cases of hypothermia. The other rhythms are treated with medications and pacemakers.
Happy whumping!
3 notes
·
View notes
Text
Redacted Audio Shifter OC RP blog
Ronan Bowey
30, 5'8
Trans man
All photos not reblogged are from pintrest

So what had happened was, I was an Olympic Track Hopeful. Unfortunately during trials I took a bad fall and had to get medical attention. Turns out I developed a Ventricular Arrythmia. Sayonara Olympic dreams.
I moved out to Cali to chill out. And it was great. My blood pressure's never BEEN more stable. But my Arrythmia was still concerning my doc and I was bedrotting. So I needed something to get me out of the house. Enter Eden, my service dog.

Anyway, I figure delivery'll be really fulfillin, give me purpose again.
4 notes
·
View notes
Text
Read first the Disclaimer in the pinned entry of the blog.
------------------------------------------------------------------------------
Glycyrrhiza glabra
"Lethal Arrhythmia Induced by Licorice Glycyrrhetinic acid, an active metabolite of licorice, can cause mineralocorticoid overload by inhibiting the enzyme 11-ß-hydroxysteroid dehydrogenase enzyme type 2. Mineralocorticoid reaction results in pseudoaldosteronism characterized by hypertension, metabolic acidosis, sodium elevation and potassium reduction. A daily consumption of glycyrrhetinic acid of 95 mg or more may cause an increase in blood pressure. In the present case, long-term use of licorice may induce pseudoaldosteronism with intractable hypokalemia, resulting in lethal polymorphic ventricular arrhythmias." ->Source<-
10 notes
·
View notes
Text
If you write anything that features characters dying in fights and want to spice things up a bit then incorporate more commotio/contusio cordis, please it’s so cool. It’s where someone is hit in the chest at a very specific point during the cardiac cycle and the energy released by the impact disrupts the cycle and causes the person to go into ventricular fibrillation. (The thing defibs treat)
And if you don’t necessarily want to kill them there is a very slim chance (<5%) that their body will sort out the heart’s electrical fuckup and get things back online; OR, if you write supernaturally powerful characters/non-human characters who wouldn’t necessarily be killed by having their heart stopped, this can be a fun way to knock them out for a moment by stopping their heart, rapidly dropping their blood pressure, and making them pass out. This is especially applicable with supernaturally powerful characters imo since they would be more likely to have the reaction time needed to hit that very precise window to trigger this.
My favorite part is how you don’t even technically need to cause physical trauma to the heart to do it, that’s what commotio cordis is vs contusio cordis. Contusio cordis is when the heart shows signs of physical trauma after the incident, bruising and such, whereas commotio cordis is where the heart actually looks perfectly fine upon physical exam. You don’t even need to be struck hard enough to cause physical trauma to the heart in order to fatally disrupt the heart’s ability to beat which is so cool imo.
But of course for those worried about it irl now don’t be, it’s super fucking rare and especially not in adults who have thicker chest walls due to puberty which protects the heart. It has to be struck in a very specific location and at a very specific time in the cardiac cycle, a window of 40 milliseconds max per heart beat, in order for it to happen, not to mention that you need to be struck with a pretty large amount of force for it to happen since it has to be enough energy to go through all those tissues and still be enough to fuck up the heart. It mostly happens in baseball and mostly boy’s baseball since again, less developed chest wall, and that’s where you’re most likely to find small objects accidentally hitting very specific parts of the chest with a large amount of force. So tl;dr don’t be worried about it irl (unless you’re a young boy playing baseball ig lol), but if you want something to spice up your writing you should totally incorporate it because it’s pretty fucking cool lbr.
4 notes
·
View notes
Text
The pathophysiology of hypertension
Introduction
Hypertension, or high blood pressure, is a complex medical condition affecting a significant proportion of the global population. Despite its prevalence, there remains uncertainty regarding its pathophysiology, with essential hypertension constituting a substantial portion where no single identifiable cause is found. This comprehensive discussion aims to delve into the physiological mechanisms involved in the development of hypertension, exploring factors such as cardiac output, peripheral resistance, the renin-angiotensin-aldosterone system, the autonomic nervous system, endothelial dysfunction, genetic factors, and intrauterine influences.
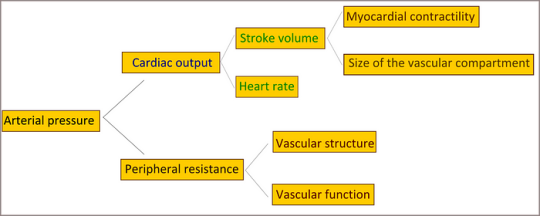
Cardiac Output and Peripheral Resistance
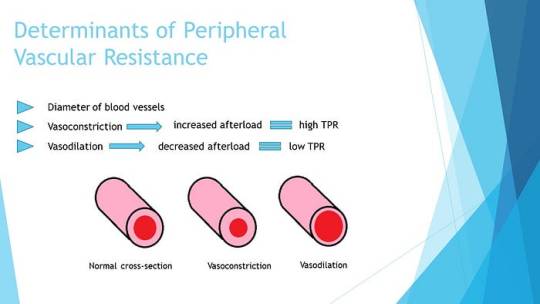
Maintaining normal blood pressure relies on the delicate balance between cardiac output and peripheral vascular resistance. Essential hypertension often involves a normal cardiac output but elevated peripheral resistance, primarily determined by small arterioles. The role of smooth muscle cells, calcium concentration, and structural changes in arteriolar vessel walls contribute to the irreversible rise in peripheral resistance.
Renin-Angiotensin System
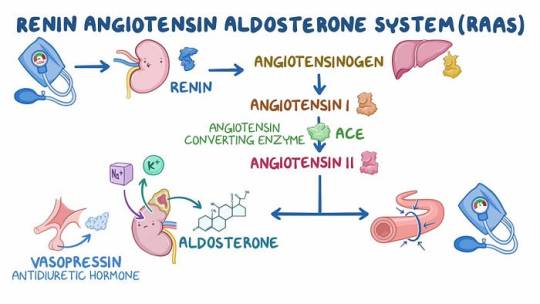
The renin-angiotensin system plays a crucial role in blood pressure regulation. Renin, released in response to various stimuli, initiates the conversion of angiotensinogen to angiotensin I, which is then converted to the vasoconstrictor angiotensin II. This system also stimulates aldosterone release, promoting sodium and water retention. While the circulating system may not be directly responsible for essential hypertension, local renin-angiotensin systems in organs like the kidney, heart, and arterial tree gain significance in regulating regional blood flow.
Autonomic Nervous System

Sympathetic nervous system stimulation affects arteriolar constriction and dilation, playing a pivotal role in maintaining normal blood pressure. Although the exact role of epinephrine and norepinephrine in hypertension etiology remains unclear, drugs blocking the sympathetic nervous system demonstrate therapeutic efficacy.
Endothelial Dysfunction
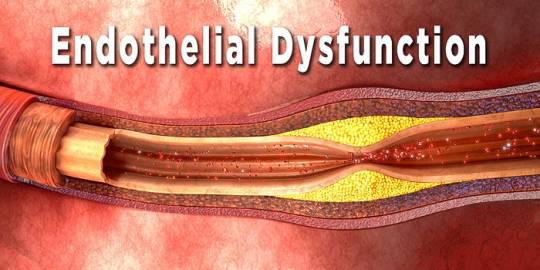
Vascular endothelial cells, producing vasoactive agents like nitric oxide and endothelin, play a key role in cardiovascular regulation. Endothelial dysfunction, implicated in essential hypertension, involves impaired production of nitric oxide. This dysfunction, once established, becomes irreversible, highlighting its primary nature in hypertension.
Vasoactive Substances
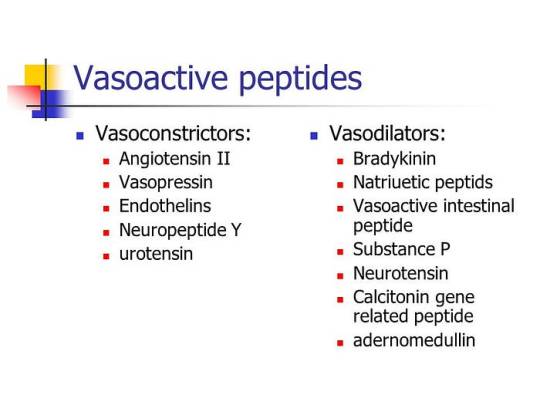
Various vasoactive substances, such as bradykinin, endothelin, atrial natriuretic peptide, and ouabain, influence sodium transport and vascular tone. These substances contribute to the delicate balance in maintaining normal blood pressure.
Genetic Factors
Genetic predisposition significantly contributes to hypertension, with specific mutations linked to disorders like Liddle’s syndrome, glucocorticoid-remediable aldosteronism, and others. The intricate interplay of multiple genes makes it challenging to pinpoint individual contributions.
Intrauterine Influences
Fetal influences, particularly birth weight, emerge as determinants of adult blood pressure. The Barker hypothesis suggests a link between low birth weight, metabolic abnormalities, and hypertension in later life. However, the role of genetic factors in this relationship requires further exploration.
Diastolic Dysfunction

Hypertensive left ventricular hypertrophy leads to impaired diastolic relaxation, affecting ventricular input during exercise. This dysfunction contributes to increased atrial pressure, pulmonary congestion, atrial fibrillation, and potential complications like pulmonary edema.
Conclusion
In conclusion, understanding the pathophysiology of hypertension involves a multifaceted exploration of various physiological mechanisms. While essential hypertension remains a complex and often multifactorial condition, advancements in research shed light on factors such as cardiac output, peripheral resistance, the renin-angiotensin system, the autonomic nervous system, endothelial dysfunction, genetic influences, and intrauterine factors. A comprehensive understanding of these elements is crucial for developing effective therapeutic strategies and preventive measures against the global burden of hypertension.
We hope this helps in improving our comprehension of the Hypertension condition. All the best in your journey in the medical field.
Incase of any challenges' and in need of professional guidance, contact;
Expert Academic Assignment Help at;
#fullmetal alchemist#healthcare#medical students#assignment help#aesthetic#puppies#kittens#ratblr#fourteenth doctor#tenth doctor#doctor who#14th doctor#medicine#medicare#medication#nursing school#nursing student#nurses#nurse#pharmercy#pets#health tips#health and wellness#online pharmacy#pharmacy student#pharmacy technician#pharmacy colleges#phar
5 notes
·
View notes
Text
Understanding Heart Disease: What is Heart Disease
What is Heart Disease?
Heart disease, also known as cardiovascular disease (CVD), encompasses a range of conditions affecting the heart and blood vessels. It is the leading cause of death worldwide, causing significant morbidity and mortality. The term "heart disease" is often used interchangeably with "cardiovascular disease," although technically, cardiovascular disease includes all diseases of the heart and blood vessels, while heart disease specifically refers to conditions affecting the heart itself.
Types of Heart Disease
Coronary Artery Disease (CAD): CAD is the most common type of heart disease and occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to plaque buildup (atherosclerosis). This can lead to chest pain (angina), heart attacks, and other complications.
Heart Failure: Heart failure, or congestive heart failure, happens when the heart muscle is unable to pump blood efficiently, leading to a buildup of fluid in the lungs and other tissues. Causes include CAD, hypertension, and cardiomyopathy.
Arrhythmias: These are disorders of the heart's rhythm, which can be too fast (tachycardia), too slow (bradycardia), or irregular. Common arrhythmias include atrial fibrillation and ventricular fibrillation, which can significantly impact heart function.
Heart Valve Disease: Heart valve disease involves damage to one or more of the heart's valves, affecting blood flow within the heart. Conditions include stenosis (narrowing of the valve), regurgitation (leakage of the valve), and prolapse (improper closure of the valve).
Congenital Heart Defects: These are heart abnormalities present at birth, ranging from simple defects like a hole in the heart's walls (septal defects) to more complex malformations. They can affect how blood flows through the heart and to the rest of the body.
Cardiomyopathy: Cardiomyopathy refers to diseases of the heart muscle. The heart muscle becomes enlarged, thickened, or rigid, which can lead to heart failure or arrhythmias. Types include dilated, hypertrophic, and restrictive cardiomyopathy.
Pericarditis: Pericarditis is inflammation of the pericardium, the thin sac surrounding the heart. It can cause chest pain and fluid buildup around the heart, affecting its function.
Causes and Risk Factors
Heart disease is influenced by a combination of genetic, environmental, and lifestyle factors. Major risk factors include:
High Blood Pressure (Hypertension): Hypertension forces the heart to work harder to pump blood, leading to the thickening of the heart muscle and potential heart failure.
High Cholesterol: Elevated levels of cholesterol, particularly low-density lipoprotein (LDL), contribute to the formation of plaque in the arteries, leading to atherosclerosis.
Smoking: Smoking damages the lining of blood vessels, increases blood pressure, reduces oxygen to the heart, and raises the risk of heart disease.
Diabetes: Diabetes significantly increases the risk of heart disease. High blood sugar levels can damage blood vessels and the nerves that control the heart.
Obesity: Excess body weight strains the heart, raises blood pressure, and increases the likelihood of diabetes and cholesterol problems.
Physical Inactivity: A sedentary lifestyle contributes to obesity, hypertension, and other heart disease risk factors.
Unhealthy Diet: Diets high in saturated fats, trans fats, cholesterol, sodium, and sugar can lead to heart disease by raising cholesterol levels, blood pressure, and weight.
Family History: A family history of heart disease increases one's risk, suggesting a genetic predisposition.
Age and Gender: Risk increases with age, and men are generally at higher risk earlier in life than women, although women's risk increases and can surpass men's post-menopause.
Symptoms
Symptoms of heart disease vary by condition but may include:
Chest pain or discomfort (angina)
Shortness of breath
Pain, numbness, or coldness in the legs or arms
Fatigue
Lightheadedness or dizziness
Palpitations (irregular heartbeats)
Swelling in the legs, ankles, and feet
Diagnosis and Treatment
Diagnosing heart disease often involves a combination of medical history review, physical examination, and diagnostic tests such as:
Electrocardiogram (ECG or EKG)
Echocardiogram
Stress tests
Blood tests
Cardiac catheterization
CT or MRI scans
Treatment strategies vary based on the specific type of heart disease and its severity and may include:
Lifestyle Modifications: Healthy diet, regular exercise, smoking cessation, and weight management are crucial for preventing and managing heart disease.
Medications: Medications can control risk factors such as hypertension, high cholesterol, and diabetes, or treat specific heart conditions like arrhythmias and heart failure.
Procedures and Surgeries: Angioplasty, stent placement, bypass surgery, valve repair or replacement, and implantable devices like pacemakers or defibrillators may be necessary for severe cases.
Prevention
Preventing heart disease involves managing risk factors through:
Maintaining a healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats
Regular physical activity
Avoiding tobacco use
Controlling blood pressure, cholesterol, and blood sugar levels
Regular health screenings
Stress management techniques
Understanding and addressing heart disease through lifestyle changes, medical management, and preventive measures is crucial in reducing its impact and improving overall heart health.
2 notes
·
View notes
Text
Kiana’s Cardioversion
Kiana was a 25 year old black girl who worked as a personal trainer. She stood at 5’3 with a slim, but fit and toned build. Kiana had dark, medium length, curly, natural hair with a side part. Her eyes were a darker shade of brown, and she had a nose ring and bellybutton ring.
Earlier today, Kiana found herself in our emergency department after developing an array of worrisome symptoms completely out of the blue. She experienced a severe tearing pain in her chest, heart palpitations, and shortness of breath. As a result, she was sitting in the upright position on one of our trauma room tables. She was barefoot, and stripped down to only her sports bra and matching underwear. There were EKG electrodes stuck onto Kiana’s chest, and there were IVs set up in both arms. She was visibly uncomfortable, writhing in pain, squirming around a bit.
The heart monitors were beeping, chirping, and alarming rather loudly, creating a bit of tension and sensory overload in the exam room. The readings on the monitors were a bit concerning as well. Kiana’s heart was racing at 170 beats per minute, and her blood pressure was low at 75/40. The rhythm itself was a tachyarrhythmia of some sort. The EKG showed a narrow QRS complex and possible atrioventricular block. The symptoms and EKG readings pointed Dr Lindsay and in a few very different directions. One possibility was an NSTEMI heart attack, but how likely is that in a 25 year old personal trainer? Next was junctional ectopic tachycardia, which is an uncommon, but potentially deadly arrhythmia that tends to occur in infants or people who recently had open heart surgery. The other possibilities were an electrolyte imbalance, particularly potassium, or her symptoms could be attributed to stimulant use from substances such as cocaine, meth, or molly.
Since the possibilities were all very different, Dr Lindsay had to be thorough and order a whole bunch of tests. First off were blood samples. A CBC, a BMP, a toxicology screening, a cardiac enzyme test, an HCG, and a d-dimer were all drawn and sent off to the lab for stat analysis. Because Kiana was experiencing chest pain, Dr Lindsay decided to order a chest x-ray and an echocardiogram. Unfortunately, both tests didn’t help Lindsay narrow anything down. The chest x-ray came back completely normal, and the echocardiogram showed slight thickening of the ventricular septum, which is a sign of hypertrophic cardiomyopathy. But some of the other symptoms didn’t point in that direction. So what exactly was going on with Kiana? Dr Lindsay was certainly stumped. All she could do was treat Kiana’s symptoms, and hope the lab tests would come back soon and show something noteworthy.
Of course the lab was taking their sweet ass time with Kiana’s stat labs. And of course Kiana started to get worse. Her heart raced faster and faster, and the arrhythmia became more troublesome. Dr Lindsay wasted no time and started chemical cardioversion, urgently trying to calm Kiana’s heart and relieve her symptoms a bit. But as the next little while unfolded, Kiana’s condition didn’t improve, almost as if the antiarrhythmic medications did absolutely nothing. When chemical cardioversion doesn’t work, the next step is electrical cardioversion.
Dr Lindsay explained to Kiana that her heart was in a dangerous rhythm, and they had to give it a quick shock to make it beat normally again. Kiana was a bit nervous and hesitant, but nodded in response to Dr Lindsay, reluctantly agreeing. The defib pads were then stuck onto Kiana’s chest and charged to a lower setting of 125 joules. Lindsay told Kiana the defibs were ready, then pushed the shock button a few seconds later. “MMMM!” Kiana moaned loudly, squeezing her eyes shut, wincing in pain from the quick jolt of electricity. After the shock, Dr Lindsay studied the monitors for a few moments and listened to Kiana’s heart and lungs with a stethoscope. Lindsay discovered there was no change in the rhythm and informed Kiana she had to be shocked again. The defib pads were recharged to 150 joules, and the next shock was sent into Kiana’s racing heart. Her torso shivered, and she clenched her chest with one hand while her face had a distressed look.
Dr Lindsay repeated the same process as before, studying the heart monitors and listening to Kiana’s heart and lungs. Just like before, Dr Lindsay didn’t see any change whatsoever and needed to shock Kiana again at 175 joules. The pads were charged and readied, and Kiana received the next shock. Her chest propelled forwards, and she let out a grunt, reacting to the electricity racing through her while wide awake. This shock failed to correct the arrhythmia, and Lindsay informed Kiana she had to be shocked again. “NO MORE! NO MORE!” She protested, writhing around on the table, on the verge of tears. Despite Kiana’s protests, Lindsay shocked her again at 200 joules. “AHH!” Kiana yelped. After that shock, she started to breathe heavily and tears started to roll down her face. “PLEASE! NO MORE, NO MORE!” she cried, begging Dr Lindsay to stop. But the arrhythmia was still there, so unfortunately Lindsay was unable to stop the cardioversion. The defibs were recharged to 225, and the next shock was delivered. Kiana gasped and cried out reacting to the shock, but just like all the others, the arrhythmia was still there. “PLEASE… JUST STOP! NO MORE! I DON’T WANNA DIE!” Kiana cried out hysterically, squirming and writhing around on the table wanting the nightmare to end.
The defib pads were recharged to 250 joules- twice the strength of the very first shock, and the next shock was administered. Kiana’s body trembled, and she scrunched her toes at the far end of the table trying to fight the pain, showing off the white nail polish on her toes and the thick, soft, wide wrinkles throughout the soles of her size 6 feet. Immediately after that particular shock, Kiana’s breathing slowed a bit. Her head lolled to the side and her eyes rolled back. Kiana’s body went completely limp, and the heart monitors were practically shouting at Dr Lindsay and the rest of our team.
It didn’t take long to realize that Kiana had gone into v-fib, so the team had to change gears and start running a normal code. The bed was lowered, and Kiana’s sports bra was snipped off, allowing her perky, deceptively large breasts to spill out. CPR was immediately started, causing Kiana’s chest to cave in, and her belly to ripple out. At the head of the bed, her airway was the priority. A 7.0 ET tube was carefully but quickly navigated into her airway, being held in place by a blue tube holder once proper placement was confirmed. Post intubation, CPR was halted, and the team decided to try their luck with the defib paddles, rather than the pads. The paddles were gelled, charged to 250 joules, and pressed up against Kiana’s bare chest. KA-THUNK! Her small body was thrown around effortlessly on the table while her eyes remained half open, almost as if she was still watching the events unfold around her. V-fib was still on the monitors, so the paddles were readied once again, and Kiana received a 300 joule shock. Her chest shot up and her back arched. Her big, perky tits jiggled around while she crashed back down onto the table. Kiana remained in v-fib even after this shock, so she was defibbed again after a cycle of CPR and ambu bagging. Her shoulders shrugged forwards. Kiana’s hands made loose fists from the electric current that ran through her body. Unfortunately, the shock didn’t bring her back.
With a few unsuccessful shocks out of the way, the team decided to resume chest compressions and push meds into Kiana’s IV line. Kiana’s chest was pumped violently but rhythmically for several minutes, but the compressions and 2 doses of meds failed to restart her heart. The team decided to defib Kiana again. The paddles were gelled, charged to 360, and she was shocked again. Kiana’s body twitched sharply in response to the shock, but her heart didn’t start back up. “again! Everyone…CLEAR!” Lindsay shouted, immediately shocking Kiana again. KA-THUMP! Kiana jolted violently on the table while her eyes remained open, staring up above with an expressionless gaze. Kiana was shocked unsuccessfully another 3 times after that and given another dose of meds, but v-fib was the clear winner of the battle up to that point.
Dr Lindsay was reluctant to give up on the beautiful young lady. However, the code became redundant the longer it went on. Kiana would receive a few shocks, then it was back to a few minutes of CPR and meds, rinse and repeat. At the 30 minute mark of the code, it was noted that Kiana’s pupils were fixed and dilated. Dr Lindsay knew she exhausted all possible options in this particular case. At that point, resuscitation efforts were ceased, and Kiana’s time of death was called at 4:48pm. The ambu bag was detached and the chirping, flashing v-fib monitors were turned off. The EKG electrodes were disconnected, and the defib pads were peeled off. The defb gel was wiped off of Kiana’s bruised, battered chest. Her eyes were gently shut for the final time, and her body was covered up. Lastly, a toe tag was filled out and placed on the big toe of her left foot. The tag dangled against the wrinkled soles of Kiana’s feet, signifying a sudden and tragic end for the beautiful young lady.
90 notes
·
View notes
Text



Paramedic Report
Incident Number: 2024-07-08-DK-0562 Patient Name: Darren Kozlowski Age: 31 Sex: Male Height: 6’1” Weight: Approx. 185 lbs Date of Incident: July 8, 2024 Time of Call Received: 10:12 AM
Incident Description: Emergency services were dispatched to a trail located in Riverbend Park following an alert from the patient’s smartwatch, which detected a suspected cardiac event. Bystanders reported finding the patient collapsed approximately 1.3 miles into the trail. The patient was unresponsive and pulseless upon paramedic arrival at 10:22 AM.
Initial Assessment:
Airway: Clear
Breathing: Apneic
Circulation: No palpable pulse; asystole confirmed on ECG
Skin Condition: Cool, pale, diaphoretic
Interventions (On-Site):
CPR initiated: High-quality chest compressions performed immediately upon arrival.
Defibrillation: Delivered one shock (200J) following identification of ventricular fibrillation (VF) on ECG. VF converted to sinus rhythm; ROSC (Return of Spontaneous Circulation) achieved at 10:27 AM.
Medications Administered:
1 mg Epinephrine IV every 3–5 minutes during CPR (3 doses given).
300 mg Amiodarone IV push following initial shock.
Transport to Hospital:
Time En Route: 15 minutes
Condition During Transport: Patient deteriorated en route, suffering a second cardiac arrest at 10:33 AM. Aggressive CPR was resumed with defibrillation (2 shocks, 200J each) and ROSC achieved at 10:38 AM.
Vital Signs Pre-Hospital Arrival:
Heart Rate: 48 bpm (weak, irregular)
Blood Pressure: 72/50 mmHg
SpO2: 82% (on 100% O2 via BVM)
Hospital Arrival:
Time of Arrival: 10:44 AM
Patient presented with recurrent arrhythmia, hypotension, and altered mental status. Handoff provided to ER staff for advanced resuscitation.
Autopsy Report
Patient Name: Darren Kozlowski Case Number: ME-2024-894 Age: 31 Sex: Male Date of Death: July 8, 2024 Time of Death: 11:03 AM Performed By: Dr. Laura Mendelson, MD, Forensic Pathologist Location: County Medical Examiner’s Office
External Examination:
Height: 6’1”
Weight: 185 lbs
Build: Lean and fit; well-developed musculature.
Hair: Short blonde hair and beard.
Eyes: Blue.
Distinguishing Features: None noted.
External Trauma:
Rib fractures (bilateral, 3rd–6th ribs) consistent with CPR.
Bruising along the sternum.
Minor abrasions on knees and hands from collapse.
No other injuries identified.
Internal Examination:
Heart:
Weight: 375 grams (normal range: 280–340 grams).
Severe coronary artery disease identified:
95% occlusion of the left anterior descending artery (LAD).
80% occlusion of the right coronary artery (RCA).
Evidence of acute myocardial infarction (MI) involving 40% of the left ventricle, with microscopic examination confirming recent myocardial necrosis and hemorrhage.
Mild left ventricular hypertrophy noted (wall thickness: 1.5 cm).
Lungs:
Pulmonary congestion and edema (weight: 750 grams per lung).
No evidence of pulmonary embolism.
Other Organs:
Liver: Mild steatosis.
Kidneys: Acute tubular necrosis, likely secondary to hypoperfusion during cardiac arrest events.
Brain: Mild cerebral edema, no gross signs of anoxic injury.
Toxicology Results:
Negative for alcohol, illicit drugs, and prescribed medications.
Positive for mild caffeine levels consistent with normal consumption.
Cause of Death: Acute myocardial infarction due to severe coronary artery disease, complicated by multiple cardiac arrests.
Manner of Death: Natural.
Pathologist’s Summary: The decedent, a 31-year-old male, succumbed to complications from a severe heart attack while running. Advanced resuscitation efforts successfully restored circulation twice; however, irreversible cardiac damage and circulatory collapse led to his death. Contributing factors include undiagnosed atherosclerosis and left ventricular hypertrophy, suggesting a predisposition to cardiac events under physical exertion.
25 notes
·
View notes
Text

TYPES OF HEART DISEASE
Heart disease encompasses a wide range of cardiovascular problems. Various conditions fall under the heart disease umbrella, each affecting the heart or blood vessels in distinct ways. Understanding these types can help in recognizing symptoms early and seeking appropriate treatment. This article explores the primary types of heart disease, their causes, and potential treatments.
1. Coronary Artery Disease (CAD)
Overview:
Coronary Artery Disease is the most common type of heart disease. CAD occurs when the coronary arteries, responsible for supplying blood to the heart muscle, become hardened and narrowed due to the buildup of cholesterol and other materials, known as plaque, on their inner walls. This process is called atherosclerosis.
Symptoms:
Chest pain (angina)
Shortness of breath
Fatigue
Treatment:
Treatments include lifestyle changes, medication, and possibly procedures like angioplasty or coronary artery bypass grafting (CABG).
2. Heart Arrhythmias
Overview:
Arrhythmias are irregular heartbeats. The heart can beat too fast (tachycardia), too slow (bradycardia), or irregularly. This can be due to a fault in the heart’s electrical system.
Symptoms:
Palpitations
Dizziness
Fainting
Treatment:
Treatment might involve medications, lifestyle adjustments, and in some cases, implantable devices like pacemakers or procedures like catheter ablation.
3. Heart Valve Disease
Overview:
The heart contains four valves: the tricuspid, pulmonary, mitral, and aortic valves. These valves open and close to direct blood flow through the heart. Valve disease occurs when one or more of these valves do not function properly.
Symptoms:
Fatigue
Swollen ankles or feet
Shortness of breath
Treatment:
Treatment may include medication, surgical repair, or valve replacement depending on the severity and specific type of valve disease.
4. Congestive Heart Failure (CHF)
Overview:
Heart failure, sometimes known as congestive heart failure, occurs when the heart can’t pump blood as well as it should. This can result from any condition that damages the heart muscle, including CAD, high blood pressure, and heart valve disease.
Symptoms:
Shortness of breath
Persistent coughing or wheezing
Swelling in legs, ankles, and feet
Treatment:
Managing heart failure involves a combination of lifestyle changes, medications, and possibly surgery or devices like ventricular assist devices (VADs) or implantable cardioverter-defibrillators (ICDs).
5. Cardiomyopathy
Overview:
Cardiomyopathy refers to diseases of the heart muscle. These diseases enlarge or make the heart muscle rigid and more prone to arrhythmias.
Symptoms:
Breathlessness
Swelling of the legs
Fatigue
Treatment:
Treatment focuses on controlling symptoms and may include medications, lifestyle modifications, or devices to help the heart pump more effectively.
6. Congenital Heart Defects
Overview:
Congenital heart defects are structural problems with the heart present from birth. They can involve the walls of the heart, the valves of the heart, and the arteries and veins near the heart.
Symptoms:
Symptoms vary widely and can include cyanosis (a bluish tint to the skin, lips, and fingernails), breathing difficulties, and fatigue.
Treatment:
Treatment depends on the type and severity of the defect and may involve medication, catheter procedures, or surgery.
Conclusion
Heart disease is a broad term that covers various conditions affecting the heart’s structure and function. Recognizing the signs and symptoms of these different types can lead to early diagnosis and treatment, significantly improving quality of life and outcomes for those affected. Regular check-ups and conversations with healthcare providers about heart health can help individuals understand their risks and take proactive steps towards heart disease prevention.
#usascriphelpersofficial#heart failure#heart disease#heart disease prevention#heart disease risk#health care#medical care#public health
2 notes
·
View notes