#they also may lose bowel &/or bladder control
Explore tagged Tumblr posts
Text
Thank you so much @yandere-paramour for commissioning me.
Commission description: I got in a freak accident where in hs where I was in theatre rehearsal and basically a 4x4 fell directly onto my head and I was severely concussed for the Next month. Can you write this happening to Reader and Yves cannot prevent it in time? and he's very upset and angry at himself and Reader is just absolutely fucked up and nearly helpless.
tw: injury, yandere themes
(2632 words)
He oversaw your entire hospital residency. Yves didn't trust the doctors and nurses that were there, he would be the one to administer any treatment. Yves would also be the one to give you bed baths and clean any messes you may have made due to losing some control over your bladder or bowels. Yves had seen all of you.
All he needed to do was talk to a few people, pull some strings, forge a few signatures, and erase a handful of records.
You were in deep throbbing pain, only made manageable by the painkillers you were made to eat. But you couldn't think straight either, everything is just too hazy and foggy. The slightest bit of light bothers you to no end, luckily you were vaguely aware Yves was around to be with you. He knew what to do, he always knew what to do.
You could make out your boyfriend's hushed voice as he spoke through the phone. Squinting your eyes, you could discern a blurry image of Yves holding his smartphone in one hand, and the other typing away on his laptop. You had always found his voice soothing, but it sounded like he was upset, it didn't help that you were barely registering the words he was saying.
Noticing that your drugs are slowly wearing off, Yves quickly ended the call and walked over to you in large strides. You closed your eyes and he didn't say anything, only the shuffling and rustling of what you think came from the medical equipment reached your ears. Occasionally, you open your eyes only to close them again, catching glimpses of Yves toggling with your cannula and a filled syringe.
You were too concussed to question why Yves is doing the nurses' or doctors' job, or if he was even qualified to do so. You were just glad that he was by your side.
Soon, you felt the relief and newfound wooziness from the freshly administered IV painkillers and something else. You were sent to your own world when Yves pulled himself away to clean up and put everything back in place.
You felt him caress your cheek and kiss you on the forehead. After that, you felt the mattress of your hospital bed dip as Yves got on, he tucked himself under your blanket and spooned you from behind.
It was baffling how that wooden plank dislodged itself from somewhere and hit you. Just you, out of all the people present there. He does routine checks on the places where you frequent, the theatre didn't appear to be dilapidated, nor did his numerous tests yield any conclusions that could help him predict this outcome. That damned building passed all his safety checks, likewise, your coworkers weren't a threat to your life.
He buried his head in the crook of your neck, closing his eyes as he breathed in your scent. Yves was deep in thought while he tenderly rubbed the palm of your hands, it's not foul play. If it was, he already knew from the footage from a few dozen cameras he hid around the theatre. Moreover, he did his research on every single one you knew or knew you. The idea of someone trying to end your life is possible, but not plausible.
Yves had replayed that one video over and over again to try and discern the cause of the wooden plank falling from the top. It seemingly... isn't caused by anything. No matter how he digitally enhanced it, no matter how many times he watched it until it was positively seared into his brain, Yves found nothing of note. It just detached from the ceiling and fell. He frowned each time he had to remember the instant it slammed right into your head.
He even paid the theatre a visit just to investigate the site of impact itself. Bewilderingly, he could discern advanced signs of weakness in the surrounding areas that weren't there a day before but would have taken a few months to form through natural means. He swabbed everything and all his tests came out nothing. Yves was undetected by the owners of that building or the authorities because he broke in during the dead of night and scaled the beams quietly and skillfully. He balanced himself on a taut rope while he snapped pictures of the sites.
He called up people who he thought could give him advice and more information about the matter, but to no avail. It's almost like this was caused by something paranormal, there were no conceivable reasons as to how or why this happened. Even if there was, it defied the laws of physics in this reality.
Regardless of how strange and unexpected this event was, Yves was upset that he didn't think of a failsafe for this. He thought of everything but not this, because it was just so implausible.
You groan in discomfort, nothing feels right and you want your mind back now. However, there really isn't anything Yves could do and all the other relatively instantaneous healing methods he knew of would cause more significant harm than good. So, for now, you're stuck like this.
He sighed, murmuring that he was here to assure you. Well, at least this has given him a new set of data that he otherwise wouldn't go out of his way to induce and collect; there is at least that silver lining.
Yves frowned as he parted away from you, despising the cold nipping at him without you as his soft heater. But he has a lot to do, he has to maintain the life that you built for yourself while you're out of commission for at least a month.
He pressed a kiss on your forehead once more, ensuring that you were completely passed out from the drugs before taking out his phone again to make a few more important calls.
-
He transferred you to his humble abode a few days later, after determining that you were stable enough for him to resume your care outside of the hospital. You could barely walk, talk, or open your eyes, you were entirely helpless. Mumbling semi-incoherent words to try and communicate your needs and wants. Luckily for you, Yves clearly knew what you wanted just by your body language alone, so you were never too angry or frustrated that he couldn't understand you.
Unfortunately for your friends and family who would visit you from time to time, you were babbling in a language from another planet. They're either too loud, too panicky, or too pungent-smelling to be around with. It's as if the air was ruined by their presence. Your poor, concussed mind thought everyone else was just idiots and Yves is the only intelligent lifeform there.
Such an attentive man, he is. Yves would politely shoo them out of your shared bedroom when they got too much, he would then spend a few more minutes entertaining them with small talk downstairs before ultimately making them leave the property. The ones who truly care about you are glad you are under Yves's supervision.
However, if you were just lucid enough, you would question how Yves knew that you wanted a blanket from your heavy slurring, how he knew that you wanted to be hugged at that very moment by just watching you blink, how he knew what hurts by an incomprehensible grumble.
A few times, you did catch yourself realizing that you may have been completely unintelligible in verbalizing your wants. Still, he gave you exactly what you needed before you could correct yourself.
You always look forward to meal times, as he would never fail to whip up something delicious yet nutritious enough; packed chock full of vitamins, and minerals to your healing process. The best part was that he would spoon-feed you while sitting on his lap, it's ridiculously comfortable and you felt like absolute royalty. Strangely and fortunately for you, it never once felt degrading or patronizing. At most, you felt heavily nostalgic and had a strong sense of sadness that you couldn't conjure up an idea as to why. But it would all ebb away with every spoonful Yves fed you or every kiss he gave to show his appreciation for your cooperation.
Yves wouldn't allow you to use your phone or watch the television, he wouldn't allow anything in his house to emit too bright of a light. Which you were grateful for since it reduces the pain dramatically, and he would keep you fully engaged by reading stories from his library. They're always so exhilarating to hear as the protagonists always possess a wonderful personality that closely matches yours, allowing you to immerse yourself in whatever whimsical and fantastical world of his storybook. His smooth, baritone voice lulled you to sleep more times than you can count, letting you continue the story in your dreams.
Sometimes, you want to experience that particular story again, so you would pick up the book Yves read from. Only to find that its' pages are seemingly filled with illegible graphite chicken scratch. Asking him about it will lead him to tell you he wrote each and every single one of those pieces, they're all based on your proudest achievements and your life journey.
When Yves promised that he would take care of you to the fullest, he meant it. He wouldn't allow you to shower on your own, nor did he let you stand too long. He prepared a stool for you to sit on as streams of warm water washed over your nude body, Yves would roll his sleeves up and clean you up while you merely remained there in a daze; you didn't have to do anything, Yves would work up a lather on your hair and massage your scalp, he would gently scrub your skin with his smooth hands and apply an impossibly long list of skincare products that leaves your skin happy and glowing.
Yves is rarely apart away from you when you're this needy. And he enjoys it, savoring every second he spends with you. Yves would take his time styling your hair, stroking it, and collecting any strands you may have shed for data. Applying hair oil and caring for your body, he wouldn't have had the chance to do this when you're perfectly healthy, as you would either get too uncomfortable, bored, or too busy for him to do this for you.
In many ways, this accident was a blessing in disguise. For you to make up for all the missed bonding times with him; it's not that Yves is elated with you being severely concussed, but he isn't too upset over it either.
"Is this the color you want for your base?" He asked, ensuring his voice wasn't above the volume threshold. Yves brought up a bottle of nail polish in your favorite color.
You gave him a thumbs up, as nodding can cause you pain.
"What design would you like?" Yves continued asking, putting the polish away so he could begin to prep your fingernails. He had your hand limply resting on a towel draped over his thigh.
You opened your mouth to speak, but it was gibberish and garbled. But you were so used to talking like this and your brain is still healing from the damage, that you couldn't tell something was wrong.
Yves merely hummed in response while he skillfully pushed your cuticles in, they were softened by some cuticle oil he applied earlier. He needed no extra enlightenment even though you spoke in a tongue that no human could ever comprehend easily, Yves already knew what you wanted. He only asked that to give you an illusion of control.
You relaxed to the soothing music playing in the background while Yves continued with his manicure on you, skillfully using his tools to create intricate works of art on your nails. It's amazing how he could do that with laser precision in dim light.
Perhaps you tried holding a conversation with him, and you did. Albeit one-sided, Yves seemingly responds to your words normally as if he truly understood. But he was actually doing some very complex "guesswork" that was apparently accurate all the time. However, if there is one thing for certain, he memorizes all the sounds that left your mouth and movements you made no matter how random or unnecessary.
If thinks that you're getting too under-stimulated, he will recite one of the many stories he wrote for you to listen to and immerse yourself in. Yet, he wouldn't get distracted, continuing his work with elegance and expertise.
You were mesmerized by how he would hold his brush, how he would administer a graceful stroke, and how he would do the details of such an impossibly beautiful masterpiece.
You smiled and cheered when you saw your nails, all that there was left for you to do was wait for the polish to dry. The corners of his lips were also pulled up into a pleased grin, feeling absolutely delighted to see you beaming like that. He couldn't resist pecking you on the apples of your cheeks, as he might accidentally squeeze you out of his cuteness aggression if he didn't at least expel some of it.
He cleaned up after himself and put the items away. You were still giddy over your nails and he was in joy too. Yves then sat right next to you, resting his head on your shoulder and letting his silky, jet-black hair tickle you in the nose.
Yves closed his eyes and relaxed at the sound of your heavenly giggles, nuzzling his head further into the side of your neck to keep the playfulness alive. He would occasionally litter your shoulder with kisses too.
Eventually, the atmosphere calms back down to a gentle lull, where you would be lying on his lap as Yves runs his fingers through your hair. A soft smile graced his face as he watched you stare at his artwork, feeling flattered and honored that you liked it.
Yves always knew the potential of himself enjoying the aftermath of such a tragedy happening to you was there. But he didn't anticipate that he loved it this much. As bad as it sounds, Yves is unwilling to think about the time when you will inevitably heal and leave him alone all over again to live your life.
His smile faltered a bit thinking how you're most likely going to go back to that theatre to work again, cutting the time that he's used to have with you short by a drastic amount. He is going to miss tender moments like these so awfully...
Yves paused when he noticed that you drifted into slumberland, softly breathing as your lips were slightly parted and drool running down the sides of your mouth. Yves chuckled a bit as he wiped them away with his thumb.
He blinked as he thought about the situation at hand even more.
You are such a strong, resilient person, who endured far worse than a measly headache. And it seems like your recovery process isn't too agonizing for you to bear, you're fine.
And, you would definitely be fine if Yves extended that duration for a few more weeks; he needs to make sure that you're fully healed before allowing you to go back into the real world. You would also be fine to consume a bit more sugar than usual, he knows you better than yourself.
Yves brought your hands and grazed his fingertips against your nails to see if it was fully dried. They were, and he gave them each a kiss.
The next few hours were spent with Yves watching you sleep, his green eyes were unblinkingly trained on you.
#oc yves#yandere concept#tw yandere#yandere oc x reader#yandere x you#yandere male#yandere x reader#male yandere oc x reader#yandere oc#yandere#thank you so much for your commission#male yandere#yandere x y/n#male yandere x reader#tw yandere content#cw yandere
81 notes
·
View notes
Text
am have to late autism regression that began late adolescence, but am don’t have “regressive autism.”
regressive autism is where child look develop normally, but at usually 15-30 months old, lose social skills, language & speech, and sometimes other skills, like motor skills and adaptive skills. this where before, child vocalizing babbling talking and interacting, and suddenly or slowly, stop talking stop responding to people (so no, it not “evil ableist parents ignore autism symptom🙃”). we no know why yet. also, child with regressive autism typically more severe symptom than child with non-regressive autism. [source]
even though many people here on tumblr seem have autism regression in teenage or early adult, “autistic regression” actually more common refer to this before-age-3 regression. other names include developmental regression. —which why when talk about own regression, typically on purpose add “late” autism regression. late autism regression is actually considered rare (whether because rarely studied rarely diagnosed, or actually rare in number, don’t know).
whether have late regression or not, need all be mindful that regressive autism & autism regression before 3 exist and not ignore or drown out it. need remember those with regressive autism, most won’t be able be here on tumblr talk about it, because well, they 3, it happen at 3. even if they older now, their severity of symptom mean many not able communicate about it or use social media. because of this, many people talk about this going to be parents of child with regressive autism.
.
ICD-11 recognize both regression before 3 (what am talk about here with regressive autism) and after 3. ICD-11 diagnosis of autism have modifiers (DSM also do but a little different modifiers): comorbid disorder of intellectual development (aka intellectual disability), degree of functional language impairment, and “loss of previously acquired skills,” aka regression.
A small proportion of individuals with Autism Spectrum Disorder may present with a loss of previously acquired skills. This regression typically occurs during the second year of life and most often involves language use and social responsiveness. Loss of previously acquired skills is rarely observed after 3 years of age. If it occurs after age 3, it is more likely to involve loss of cognitive and adaptive skills (e.g., loss of bowel and bladder control, impaired sleep), regression of language and social abilities, as well as increasing emotional and behavioural disturbances.
.
with either regression before 3 or after 3, include late adolescents regression, important to rule out all other causes. because other reasons that make look regression may be life threatening disorders.
regression also see in child disintegrative disorder (CDD), rett syndrome, and some others. they all a little different, timing, symptoms, etc.
.
do not debate “severity” of autism language here. do not use this to self diagnose. do not use this to talk about parental trauma or debate autism parents & parents of autistics.
#believe or not have seen late/no dx LSN autistic say regressive autism no exist because it just parents ignore autism symptoms 🥰#actually autistic#actuallyautistic#autism#autistic#loaf screm
203 notes
·
View notes
Text
What Do Dogs Usually Do Before They Die? What Are the Signs?

As pet owners, it's crucial to understand the signs and behaviors that indicate a dog might be nearing the end of its life. This knowledge helps us provide the best possible care and make informed decisions during these difficult times. Below, we explore the common signs that a dog is dying, focusing on physical, behavioral, and emotional changes.
1. Changes in Appetite and Thirst
A noticeable decline in a dog’s appetite and water intake is one of the most common signs that they are nearing the end of their life. Dogs may refuse food and water altogether or eat and drink in significantly reduced amounts. This change is often due to a lack of energy and a decline in the body’s ability to process food and fluids.
2. Decreased Mobility and Weakness
As dogs age or become seriously ill, they often experience a marked decrease in mobility. They might have difficulty standing up, walking, or climbing stairs. Muscle weakness and a lack of coordination can make even the simplest tasks challenging. This reduction in mobility is usually due to pain, discomfort, or severe fatigue.
3. Incontinence
Incontinence is a common sign of a dog nearing the end of life. Dogs may lose control of their bladder and bowels due to weakness or a lack of awareness. This can be distressing for both the pet and the owner but is often an unavoidable part of the process.
4. Breathing Difficulties
Changes in breathing patterns are also common in dying dogs. You might notice labored breathing, shallow breaths, or irregularities such as rapid or very slow breathing. These changes are often due to organ failure, which can affect the respiratory system.
5. Behavioral Changes
Behavioral changes can indicate that a dog is nearing the end of its life. Some dogs may become unusually clingy and seek constant companionship, while others may become withdrawn and isolate themselves. These behaviors are often a reflection of discomfort, confusion, or the need for reassurance.
6. Disinterest in Surroundings
A dog nearing the end of its life may show little to no interest in their surroundings or activities they once enjoyed. They may ignore toys, other pets, or people and might not respond to their name or favorite treats. This lack of interest is often due to physical discomfort or mental exhaustion.
7. Extreme Fatigue and Lethargy
Lethargy is a common symptom in dogs that are close to death. They may sleep much more than usual and have little to no energy for physical activities. This extreme fatigue can be attributed to the body shutting down and conserving energy.
8. Pain and Discomfort
Many dogs experience pain and discomfort as they near the end of life. Signs of pain include whining, whimpering, restlessness, and changes in posture. They might also exhibit defensive behavior when touched or handled. Pain management is crucial to ensure a dog’s comfort during this time.
9. Changes in Gum Color
Pale or bluish gums can indicate a lack of oxygen in the blood, which is a sign of severe health issues such as organ failure. Checking a dog’s gums can provide insight into their overall health status.
10. Weight Loss
Significant weight loss is common in dying dogs, often due to a combination of decreased appetite, muscle wasting, and the body’s declining ability to absorb nutrients. This weight loss can be rapid and pronounced.
11. Vomiting and Diarrhea
Frequent vomiting and diarrhea can occur in dogs that are nearing death. These symptoms may be a result of digestive system failure or the body’s inability to process food and liquids properly.
12. Seeking Solitude
Some dogs instinctively seek solitude when they are dying. This behavior is thought to be an instinctual response to protect themselves from potential threats during their vulnerable state. A dog may hide under furniture, in closets, or seek out quiet, isolated spots.
Conclusion
Understanding these signs can help pet owners recognize when their beloved dog is nearing the end of its life. It is essential to consult with a veterinarian to provide the best care and make informed decisions. Providing comfort, managing pain, and offering love and companionship are crucial during this difficult time. Recognizing and acknowledging these signs allows for a more compassionate and prepared approach to saying goodbye to our loyal companions.
Remember, every dog is unique, and the signs may vary. Pay close attention to your dog's behavior and consult with your veterinarian to ensure you are providing the best care possible in their final days.
#cat#dog#pet#my pets#pets#cute animals#puppy#doggo#animal#bd/sm pet#dogs of tumblr#bungou stray dogs#dog news#dogday#dogblr#cats
19 notes
·
View notes
Note
Hi there! My character screwed up and her boss punishes her by paralyzing her muscles so that she can’t move. She’s stuck like this for a few months, and every once in a while her boss would tend to her (feed her, let her use e bathroom, etc)
I was wondering what would happen to her body during this. How long could she go without food? How long can she go without her boss tending to her? And what would the side affects be after being freed?
So cool thing about this ask is that this situation is extremely well studied, and we know a lot about what happens to a person when they can't move for extended periods of time.
For the purposes of this ask, I'm assuming you mean some kind of magic paralysis of only skeletal muscle. Skeletal muscle is the muscle we can consciously control, like the muscles in our arms, legs, back, abdomen, etc... Other muscles, like the heart, diaphragm, muscles in our digestive tract, and muscles that control the diameter of our blood vessels would pretty instantly cause death if they stopped working.
Not to say that paralysis of skeletal muscle wouldn't cause problems of it's own, just that those problems are on a longer timescale.
De-conditioning. Muscle is metabolically expensive to maintain, so if you don't use it, you lose it. Even a few days of bed rest can cause a decrease muscle mass. A few weeks or months of paralysis and the person wouldn't be able to walk on their own. They would need likely weeks or months of physical therapy to bring the person back to baseline.
Contractures. A contracture is a shortening and stiffening of muscles and other types of soft tissue around a joint, essentially freezing it in place. This commonly happens during paralysis when a joint doesn't move for long periods of time. Contractures can be prevented if someone moves all the joints for the paralyzed person at least daily- something called range of motion exercises. Once contractures occur, though, they often need to be treated with long term physical therapy and/or surgery.
Pressure injuries. Pressure injuries (sometimes called bed sores) are sores that occur when a piece of tissue (skin, fat, muscle) is sandwiched between a surface (like a bed or piece of medical equipment) and a bone for an extended period of time. Often these occur on bony prominences, like the sacrum, hips, shoulders, and heels. To prevent these in someone who is paralyzed, the person must be turned and placed in a new position at least every 2 hours to keep pressure off of any one spot. Once they occur, they are difficult to treat and often scar badly.
Incontinence. If a person can't move, they also generally can't control their bowel or bladder. This means they're probably going to go in the bed. This can contribute to skin breakdown if not cleaned quickly and thoroughly each time (think pressure injuries combined with diaper rash and those wrinkles you get from being in a pool too long). Urine may dribble out continuously, so a lot of times its difficult to keep the person dry enough to prevent skin breakdown without some kind of diaper cream.
Aspiration. If someone can't move, they can't eat without the risk of choking. If they end up breathing food in, this can result in something called aspiration pneumonia, which is when food irritates the lining of the lungs. This can be fatal. This can be prevented by feeding the person through a tube that goes from their nose into their stomach, or for longer term situations, through their abdominal wall into their stomach (placed surgically). Formula is sold for this purpose, but well-blended whole food also works.
Clots. Staying in the same position for long periods (or even short ones, say following surgery), causes blood to pool in the legs. When blood pools, it tends to clot, and those clots can travel into the lungs, brain, and heart. A clot in the lungs is called a pulmonary embolism, one in the brain is called a stroke, and one in the heart is a heart attack. All of them are essentially the same process- blood being blocked from getting where it needs to go in a vital organ- and they can all be very deadly. These can be prevented with range of motion exercises, sequential compression devices, and blood thinning medications.
Someone who is completely paralyzed needs round the clock nursing care. Between ROM exercises, every-2-hour turns, cleaning up urine and stool probably at least as often, preparing formula, bolus feeding, and cleaning up, it would probably take about 6-8 hours of direct care spread evenly over a 24 hour period to prevent the outcomes described above.
Ross @macgyvermedical
52 notes
·
View notes
Text
Since I was telling you guys about The Silent Alpha (listening to it on DreameFM), i figured I might share a little on the first book in the series, The Ivory Queen? I actually think both stories are quality and was mostly juat gossiping on all the juicy drama parts haha
The Ivory Queen is about a Mexican-American girl named Aurora Montenegro who's father Emiliano is killed by rogue wolves on her 13th birthday, and when her pack finds her with the body they immediately blame her. Since your 13th birthday is your first shift, they automatically assume she went feral and killed her father, and the entire pack, the Lluvia Blanca pack, spends the next 5 years absolutely torturing her, even by her mother and siblings. She's beaten up, kept in a basement, denied proper food, forced to work as a slave, and denied ever being able to shift which makes her incredibly weak on top of already being malnourished. This isnt even to touch on stuff like, "oh her brother Chava once locked her in a closet and used his illusion powers to make her see rogues like the ones who killed her father and left her like that for hours and then he dragged her out covered in her own piss and shit because she'd literally been losing control of her bladder and bowels in terror after being in there so long and he dragged her in front of other people and then everyone mocked her during this extremely traumatizing experience and after the fact some of them literally threw diapers at her, for MONTHS". Like. jesus fucking christ dude. Kill all of them maybe? Like Im starting to adore the idea of a Reader who was horrifically abused and just goes "fuck this high horse bullshit, hey new mate, you're a powerful wolf and you love me? Kill these bitches to prove it. Make them suffer"
When Aurora finally meets her mate, Alpha Olivier of River Moon Pack, he rejects her because he recognizes her and has heard all the awful rumors, but soon, he actually regrets his decision and vows that he wants to see who she really is and they team up to not only get her away from her abusive pack and family, solve the mystery of her father's death, but also discover an even deeper plot of a looming war, a prophecy, and the truth surrounding her heritage
The story is not only well written and well voice acted but also contains decent amounts of representation (like Olivier is French, and he has his pack cook traditional Mexican food for Aurora when she first arrives which literally makes her sob with gratitude because she hasn't had home cooked Mexican food since before her father died) and also naturally covers subjects like women's rights and things are written in a mature and realistic tone (like another conversation with a Luna named Kehlani opening up that she felt like her breasts were too low and far apart after giving birth, and it's like God that is such an actual realistic female struggle. a lot of these other authors just kind of, idk, some of these stories are like comparing potato chips to a full course meal kwim? Emotional journeys vs popcorn literature YA novels)
Oh. I will say though. One of the horrible things to happens to Aurora is that she is and had been sexually assaulted by another member of this pack and this does happen in written detail so, if that is triggering for you you may need to skip any interactions with that character (who's name i can't remember but you'll be able to tell because he's openly creepy and before the assault happens Aurora already let's the reader know, he's a guy who "does unspeakable things to me I can't talk about")
Like it is very dark. She gets knocked out and wakes up with her attacker already on top of her, already in the midst of it while she was blacked out, and interestingly, this is a story where the mate bond also transfers pain, so, Olivier experiences the pain of, well, being an assaulted woman, and that deepens his love, respect, and sympathy for Aurora and her strength to survive. But I also don't like that Aurora also had to lowkey provide comfort to Olivier for something that happened to her after the fact, like it isn't like forced upon her ,she wants to comfort him, but it's like... that happened to HER, idk, Olivier getting attention for the issue makes me feel kinda weird
Either way it's a cute story about finding love and acceptance when you feel like you have nowhere you belong and feel like everyone hates you and sees you as nothing. A nice read and a nice story, albeit a little long ^^;
4 notes
·
View notes
Text
Skip to main content

Home
Conditions
Back
Conditions
View All
ADD/ADHD
Allergies
Arthritis
Atrial fibrillation
Breast Cancer
Cancer
Crohn's Disease
Depression
Diabetes
DVT
Eczema
Eye Health
Heart Disease
HIV & AIDS
Lung Disease
Lupus
Mental Health
Multiple Sclerosis
Migraine
Pain Management
Psoriasis
Psoriatic Arthritis
Rheumatoid Arthritis
Sexual Conditions
Skin Problems
Sleep Disorders
Ulcerative Colitis
Drugs & Supplements
Back
Drugs & Supplements
Drugs
Supplements
Pill Identifier
Interaction Checker
Well-Being
Back
Well-Being
Aging Well
Baby
Birth Control
Children's Health
Diet & Weight Management
Fitness & Exercise
Food & Recipes
Health & Balance
Healthy Beauty
Men's Health
Parenting
Pet Health
Pregnancy
Sex & Relationships
Teen Health
Women's Health
Symptom Checker
Find a Doctor
More
Back
More
News
Blogs
Podcasts
Webinars
Newsletters
WebMD Magazine
Best Hospitals
Support Groups
Privacy & More
Subscribe
Log In
Search
Subscribe
Epilepsy
Epilepsy Guide
Help When Epilepsy Treatment Doesn't Work
Medically Reviewed by Christopher Melinosky, MD on May 12, 2023
Written by Katherine Kam
7 min read
What Is Refractory Epilepsy?
If your doctor says you have refractory epilepsy, it means that medicine isn't bringing your seizures under control. You might hear the condition called by some other names, such as uncontrolled, intractable, or drug-resistant epilepsy.
Your doctor can try certain things to help keep your seizures under better control. For instance, they might try different combinations of drugs or a special diet.
Your doctor may also put a device under your skin that sends electrical signals to one of your nerves, called the vagus nerve. This may cut the number of seizures you get. A Neuropace device is a reactive neurostimulator that detects seizures and shocks the brain to stop them.
Surgery that removes a part of the brain that causes your seizures may also be an option. With any of these treatments, you may still need to take epilepsy medicine throughout your life.
It's natural to feel anxious when the doctor tells you your epilepsy isn't getting better with the medicine you're taking. You don't have to go through it alone, though. It's important to reach out to family and friends to get the emotional support you need. You might also want to join a support group, so you can talk with other people who are going through the same things you are.
Featured
Tests and a Diagnosis for Epilepsy
Common Types of Seizures
Types of Epilepsy
Causes
Doctors don’t know why some people have refractory epilepsy and others don't. You can have refractory epilepsy as an adult, or your child might have it. About 1 in 3 people with epilepsy will develop it.
Symptoms
The symptoms of refractory epilepsy are seizures despite taking anti-seizure medication. Your seizures could take different forms and last from a few seconds to a few minutes.
You may have convulsions, which means you can't stop your body from shaking.
When you have a seizure, you may also:
Black out
Lose control of your bowels or bladder
Stare into space
Fall down suddenly
Get stiff muscles
Bite your tongue
Getting a Diagnosis
Your doctor has several ways to diagnose refractory epilepsy. They may ask you questions such as:
How often do you have seizures?
Do you ever skip doses of your medicine?
Does epilepsy run in your family?
Do you still have seizures after taking medicine?
Your doctor may also give you a test called an electroencephalogram. To do this, they'll place metal discs called electrodes on your scalp that measure brain activity.
Other tests might include a CT scan of your brain. It's a powerful X-ray that makes detailed pictures of the inside of your body.
You might also need to get an MRI of your brain. It uses magnets and radio waves to make pictures of your brain.
If you need surgery to treat refractory epilepsy, these tests can help doctors find out where your seizures are starting.
Your doctor will most likely want you to report your symptoms regularly. They may try several drugs at different doses.
Questions for Your Doctor
What might be causing my seizures?
Which tests are needed to diagnose refractory epilepsy?
Should I see an epilepsy specialist?
What treatments are available for refractory epilepsy?
What precautions should I take to avoid getting injured during a seizure?
Are there any limits on my activities?
Treatment
Medications. Your doctor may take a second look at the drugs you're taking. They may suggest another medicine, either alone or combined with other drugs, to see if it helps you have fewer seizures.
Many drugs can treat epilepsy, including:
Brivaracetam (Briviact)
Cannabidiol (Epidiolex)
Carbamazepine (Carbatrol, Tegretol)
Cenobamate (Xcopri)
Clobazam (Sympazan)
Divalproex (Depakote)
Dilantin (Phenytek)
Eslicarbazepine (Aptiom)
Felbamate (Felbatol)
Gabapentin (Neurontin)
Lamotrigine (Lamictal)
Levetiracetam (Keppra)
Oxcarbazepine (Trileptal)
Perampanel (Fycompa)
Potiga (Ezogabine)
Primidone (Mysoline)
Rufinamide (Banzel)
Tiagabine (Gabitril)
Topiramate (Topamax)
Vigabatrin (Sabril)
Zonisamide (Zonegram)
Surgery. If you still have seizures after trying two or three anti-epilepsy drugs, your doctor might recommend brain surgery.
It can help a lot if your epilepsy only affects one side of your brain. Doctors call that refractory partial epilepsy.
A surgeon removes the area of your brain that's responsible for your seizures.
It's natural to worry about brain surgery and to wonder if it will affect the way you think or if you'll seem like a different person afterward. Talk with your doctor about what to expect if you choose the surgery or if you don't, so you can weigh the risks and benefits. A lot of people who have the surgery say that getting free of seizures -- or at least making them less common and less intense -- makes them feel much better.
The surgeon usually operates on an area of your head that's behind your hairline, so you won't have noticeable scars.
After it's done, you'll probably need to stay in an intensive care unit of the hospital for a few days. After that, you'll move to a regular hospital room, where you may need to stay for up to 2 weeks.
You should take it easy for a while after you get back home, but you'll probably be able to return to a normal routine in 1 to 3 months. Even with the surgery, you might need to take seizure medication for a few years. You might need to stay on the drugs for the rest of your life.
Talk to your doctor about any side effects you might have from the surgery. You can ask them to put you in touch with other people who've had the surgery, so you can better understand what to expect.
Diet. The ketogenic diet helps some people with epilepsy. It's a high-fat, low-protein, no carb diet. You have to start it in a specific way and follow it strictly, so you need a doctor's supervision.
Your doctor will watch closely to see whether or when you can lower any of your medication levels. Because the diet is so specific, you may need to take vitamin or mineral supplements.
Doctors aren't sure why the ketogenic diet works, but some studies show that children with epilepsy who stay on the diet have a better chance of reducing their seizures or their medications.
For some people, a modified Atkins diet may work, too. It's slightly different from the ketogenic diet. You don't have to restrict calories, protein, or fluids. Also, you don't weigh or measure foods. Instead, you track carbohydrates.
People with seizures that are hard to treat have also tried a low-glycemic-index diet. This diet focuses on the type of carbs, as well as the amount that someone eats.
Electrical stimulation, also known as neuromodulation. This technology works directly on your nerves. It changes or controls nerve activity by sending electrical signals or medicine to a specific area. Methods include:
Cortical stimulation. Temporary electrodes are placed on the surface of your brain. The doctor sends a signal through them at a level low enough that you won’t notice. If it helps, they can be replaced with permanent electrodes for continuous stimulation.
Closed-loop stimulation. The doctor implants a device under your scalp and within your skull. It’s connected to two electrodes placed either on the surface of your brain, in the brain, or both. The electrodes record your brain waves. When the neurostimulator detects seizure-like activity, it sends a small electrical current to your brain that can stop, shorten, or maybe prevent the seizure.
Deep brain stimulation. The doctor implants thin electrodes deep into certain areas of your brain and a pulse generator under your collarbone. Wires under your skin connect the two. The pulse generator sends signals to disrupt abnormal patterns of brain activity.
Vagus nerve stimulation (VNS). The doctor puts a device that looks like a heart pacemaker under your left collarbone. It connects to the vagus nerve in your neck through a wire that runs under your skin. The device sends a current to the nerve, which may cut down on the number of seizures you get or make them less intense.
Clinical trials. You may want to ask your doctor if you could take part in a clinical trial. These trials test new drugs to see if they're safe and if they work. They're often a way for people to try new medicine that isn't yet available to everyone.
Taking Care of Yourself
Stress can sometimes trigger seizures. Talking to a counselor is a great way to find solutions to manage your stress.
Try going to a support group, too. You can talk with people who know what you're going through and who give advice from their own experience.
What to Expect
Even though you have refractory epilepsy, it's still possible to get your seizures under control. It may be a matter of switching to a different treatment.
Your doctor may find a different drug combination that helps. Getting electrical stimulation of the vagus nerve means fewer seizures for about 40% of people who try it. And if a brain surgeon can remove the part of the brain that's causing seizures, the seizures may stop, or at least happen less often and become less intense.
Getting Support
As you are finding out what works best, you'll need a strong network of family and friends who can offer emotional support, especially if your seizures prove hard to control. Having a trusted person to listen to you can be a great comfort when you're going through something tough.
Ask your doctor for information on support groups in your area. You can also find out about support groups by going to the website of the Epilepsy Foundation.
SourcesUpdate History
Share
Print
Save
View privacy policy, copyright and trust info
More on Epilepsy

Understanding Epilepsy Basics
What Is Epilepsy Surgery?
Everyday Tips for a Child With Focal Onset Seizures
Recommended

FEATURED
Related Links
Epilepsy News
Epilepsy Reference
Epilepsy Slideshows
Epilepsy Videos
Epilepsy Medications
Find a Neurologist
Brain & Nervous System
Children's Health
Drug Interaction Checker
Juvenile Myoclonic Epilepsy
Lennox-Gastaut Syndrome
Sign up for our free Good Health Newsletter
Get wellness tips to help you live happier and healthier
Subscribe
By clicking Subscribe, I agree to the WebMD Terms & Conditions & Privacy Policy and understand that I may opt out of WebMD subscriptions at any time.
Follow WebMD on Social Media
Download WebMD App

Policies
About
For Advertisers
Privacy Policy
Cookie Policy
Editorial Policy
Advertising Policy
Correction Policy
Terms of Use



© 2005 - 2024 WebMD LLC, an Internet Brands company. All rights reserved. WebMD does not provide medical advice, diagnosis or treatment. See additional information.

0 notes
Text
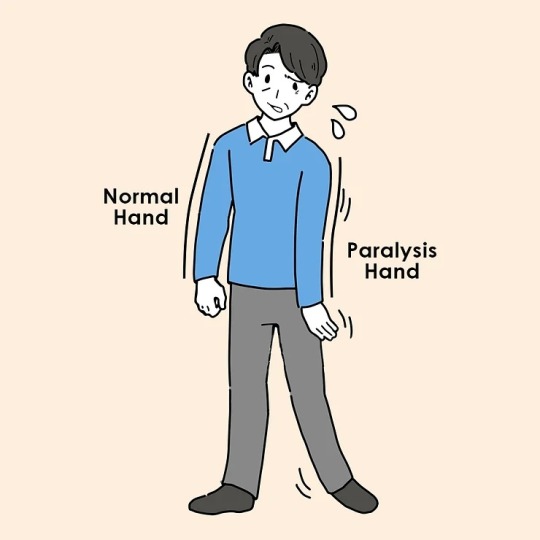
Understanding Paralysis: Debunking the Myths and Discovering Ayurvedic Remedies
Welcome to Vedicmed’s blog related to Paralysis. People have a lot of confusion and misconceptions about Paralysis. Many people suffering from paralysis are unfortunately hopeless without proper treatment due to a lack of proper knowledge and deep-seated superstitions. Through this blog, our aim is to clear the misconceptions about paralysis among people and create awareness about Ayurvedic treatment for paralysis. Before knowing everything about ayurvedic treatment in detail, let’s know about it one by one: what is Paralysis, what are its symptoms, and what are the causes of Paralysis.
Paralysis occurs when someone loses muscle function in one or more parts of their body. Paralysis can occur due to several reasons, and it affects different parts of the body in different ways. Sometimes, this leads to a partial loss of movement, but in other cases, it can lead to complete immobility. In this blog, we at Vedicmed will tell you the various Ayurvedic treatments for Paralysis in detail.
Here is the some key factors that can lead to paralysis:
Stroke: When a blood vessel in the brain becomes blocked or ruptures, it cuts off the supply of oxygen and nutrients to brain cells, often resulting in paralysis.
Spinal Cord Injury: Traumatic incidents, such as car accidents or falls, can cause significant damage to the spinal cord, leading to paralysis.
Traumatic Brain Injury: Severe head injuries can cause damage to the brain, which may result in paralysis depending on the area affected.
Neurological Disorders: Conditions like multiple sclerosis, cerebral palsy, and Guillain-Barré syndrome can lead to paralysis by damaging the nerves.
Infections: Certain infections, such as polio and meningitis, can attack the nervous system, damaging nerves and leading to paralysis.
Symtoms of Paralysis:
When most people think of paralysis, the first thing that comes to mind is the inability to move or control a part of the body. However, paralysis can come with other important symptoms. Here’s what to look out for:
Numbness or Loss of Sensation: Often, the paralyzed area may feel numb, making it difficult to detect touch or other sensations.
Muscle Stiffness or Spasticity: The affected muscles may become stiff or rigid, making everyday movements challenging and uncomfortable.
Muscle Atrophy: Over time, muscles that aren’t being used may start to waste away, leading to a noticeable loss of strength and function.
Loss of Bladder and Bowel Control: In some cases, paralysis can lead to difficulties in controlling bladder and bowel functions, complicating daily routines.
Difficulty Breathing: In more severe cases, especially when higher-level spinal cord injuries are involved, paralysis can impact the ability to breathe properly, requiring urgent medical attention.
Ayurvedic treatment for Paralysis at Vedicmed :
Ayurveda offers a range of holistic treatments to help manage and improve paralysis. These therapies work together to address various aspects of the condition, aiming to restore balance, improve mobility, and enhance overall quality of life. Let’s explore some of the Ayurvedic treatments we used at Vedicmed:
Oral Medication: Vedicmed’s experts are prescribe Herbal formulations to enhance circulation, reduce inflammation, and support the nervous system. These medicines aim to restore balance and promote healing from within.
Virechana (Purgative Therapy): This specialized treatment, known as ‘Pakshaghata Virechanam', helps to balance doshas, especially pitta and vata, believed to play a role in paralysis. It removes toxins and promotes overall well-being.
Abhyanga (Oil Massage): This therapeutic massage uses medicated oils to increase blood flow, strengthen muscles, and correct vata imbalances. It can improve mobility and enhance muscle function.
Swedana (Steam Therapy): Localized steam therapy improves circulation, reduces vata, and increases mobility. It also aids in detoxification, contributing to overall wellness.
Pizhichil : Warm medicated oils are poured over the body while massaging, strengthening nerves, reducing vata, and alleviating pain and swelling.
Pinda Sweda: This therapy uses medicinal boluses to reduce infection, lower inflammation, and improve muscle strength.
Basti (Enema Therapy): Medicated enemas reduce vata dosha, alleviate pain, and improve digestion.
Shiro Pichu: A medicated oil-soaked cloth is placed on the forehead to improve concentration, reduce slurred speech, enhance memory, and manage stress and blood pressure.
Shiro Dhara: Warm medicated oil is poured over the forehead, controlling blood pressure, managing stress, and addressing insomnia.
Nasya (Nasal Therapy): Medicated oils or herbal powders stimulate the pituitary gland, balance hormones, and improve sleep patterns.
#Paralysis#paralysis treatment#Paralysis ayurvedic treatment#vedicmed#health and wellness#ayurvedictreatment#healthcare#health tips#ayurvedic products
0 notes
Text
Dissociative Seizures
Educational post. Trigger warnings: Medical equipment and description of seizure.
Written by Tom and Blade.
Why will we cover this?
Although dissociative seizures are not exclusive for those with dissociative disorders. Some people with dissociative disorders will have seizures.
A dissociative seizure is named differently in different parts of the world.
I will be referring to them as dissociative seizures or Non-epileptic attack disorder (NEAD).
However, may also be seen as a one of the many symptoms/types of Functional neurological disorders (FND) its matching term in the ICD-11 is Dissociative neurological symptom disorder. And this post will focus specifically on only the non epileptic seizures.
It is also known as Psychogenic non-epileptic seizures (PNES), Non-epileptic seizures, and Psychogenic seizures.
If you have known these as "pseudo seizures", it is asked that this is no longer a term that should be used because the name suggests that the seizures are not real or faked by the individual having them or cannot have an ever lasting impact.
What causes a dissociative seizure?
Unlike epileptic seizures they are not caused by abnormal electrical activity in the brain.
A person can get triggered by sensations, thoughts, emotions and difficult situations. Memories of painful events can suddenly come into thoughts or awareness or a build up of stress can happen in a moment. The dissociative seizure can happen as a way to cut off stress or bad memories so that they are not relieved. This can cause a person to start to dissociate. This is when they will feel disconnected from the world around them or make it seem like the world is not real. The brain will "shut down" to protect itself from overwhelming stress. The seizure then happens because the emotional reaction of the person becomes physical. It is known that extreme emotional distress can cause illnesses and disorders such as non epileptic seizures.
Some people who have dissociative seizures have them caused by traumatic events. For some they may happen after the event or for others they could start years later. They may start to happen suddenly with no apparent reason at the moment. However, in some people they can be caused by the build up of stress overtime.
When seizures start they can be triggered by stressful or frightening events, even the worry of having a seizure can trigger one. They could also occur spontaneously in non stressful events. Patients may not be able to understand why seizures happen as for some it is hard to recognise the level of stress they are feeling.
What do dissociative seizures look like?
Dissociative seizures can look different from person to person.
You could have episodes of uncontrolled movements, sensations or behaviour. Some dissociative seizures may look more like epileptic seizures or may look more like fainting. Someone may have palpitations, sweat, hyperventilate and have a dry mouth. Someone may fall on the ground or have jerking and shaking movements either on one side or the whole body. A person may lose control of their bladder or bowels and may also bite their tongue. Some people may go unresponsive to people around them and may stare and go blank.
Having seizures caused by a delayed response to a traumatic event may be a part of Post Traumatic Stress Disorder (PTSD). In these seizures a person may have flashbacks, scream or cry and they may not remember the seizure afterwards.
Diagnosis of dissociative seizures.
A specialist will have many ways to tell whether the seizures are epileptic or not. The doctor may be able to tell from detailed descriptions of the seizures or a video of one happening. However, a doctor may ask someone to have an electroencephalogram (EEG) to determine whether electrical changes occur within the person's brain during a seizure. It may also be suggested for a person to have a video-telemetry. This could be done as an inpatient in a hospital or at home. A person will wear EEG equipment for a few days and is linked to a camera. This means that during a seizure the EEG and a video of it happening can be taken at the same time.
Brain scans such as Magnetic resonance imaging (MRI) or Computed Tomography Scan (CT) scans may also be done to rule out any neurological cause for these seizures.
Treatment for dissociative seizures.
Patients may also be asked to see a psychiatrist or psychologist. They can offer Treatment such as psychotherapy, stress-reduction (such as relaxation and biofeedback training), and personal support to help you cope with their seizures.
Talking therapy is useful to understand if there are triggers for the seizures and ways to manage these triggers in daily life. Cognitive behavioural therapy (CBT) is often recommended.
Medication will not help treat non epileptic seizures so they will only be suggested if the patient also has epileptic seizures. Taking medication for non epileptic seizures can cause side effects and do not benefit the person.
It is recommended to keep a normal daily routine. And to make sure that their family and friends are aware and understand. This will mean they will likely be able to help the person in a seizure and prevent harm.
First aid for dissociative seizures (Outsider's perspective):
DO:
- Make sure the person is safe. This can include moving objects away from them. If the person is lying on the floor, put a cushion/something soft under their head.
- Speak Calmly and in a reassuring way to the person
- Non epileptic seizures do not cause damage to the brain no matter how long it happens BUT if you are not sure if it is a dissociative seizure and lasts more than 5 minutes an ambulance must be called. If it is epileptic then a seizure longer than 5 minutes can damage the brain. (Again important to note this is advice given by the NHS of the UK)
- Stay with the person until they have recovered
DO NOT:
- Do not restrain the person. This can cause injury and make the seizure worse.
- Do not put anything in the person's mouth
- Do not attempt to give medication
Self-help tips:
- Write down how you are feeling
- Continue to live normally and not become over cautious. This can help to speed up recovery. It is important to talk to your employer about these seizures and make clear your colleagues know what to do as well.
- Eat and Sleep well
- Build up self confidence
- Green exercise is a great way to boost your mood by being outside even if it is for a short while. Going for a walk outside.
- Fitness programmes can be found online and most can be done from your home
- Remaining positive
The sources we have used for this information also have more information on disability rights and benefits for those with dissociative seizures. And on driving regulations. However, these are only applicable to the UK.

Epilepsy Society, O’Sullivan S. Non-epileptic Seizures and Dissociative Seizures | Epilepsy Society. epilepsysociety.org.uk. Published August 2023.
British Epilepsy Association. Dissociative (non-epileptic) Seizures. Epilepsy Action. Published August 2022.
NHS. What to Do If Someone Has a Seizure (fit). nhs.uk. Published April 9, 2018.
Further information:
People's experiences:
Documentary film: Photosensitive Epilepsy Trigger Warning at (9:14 - 9:30 ) and at (45:25 - 46:18)
Websites for more information:
NeuroKid: - This is a website for children and young people with dissociative seizures but also has information for parents of these children. The website is also available in French at https://www.neurokid.co.uk/fr/.
Non-Epileptic Attacks: A page written by professionals. They have more resources and go into more detail about the self help we have addressed.
FNH Hope UK: Has fundraising challenges across the UK. They also have online classes such as dance, painting, mindful meditation and yoga.
Charities:
FND Action: They can provide ID cards for those in the UK struggling with dissociative seizures.
Brain Charity: Provides Emotional support and social support for those in the UK and has a helpline.
Trigger warnings: Medical equipment and description of seizure. Educational post.
#dissociative identity disorder#dissociative system#dissociation#actually dissociative#non epileptic seizures#functional neurological disorder#dissociative disorder#disability#psychogenic non epileptic seizures#did system#actually did#endos dni#complex dissociative disorder#ossdid#other specified dissociative disorder#partial dissociative identity disorder#partial did#did osdd#osdd#fnd#fnd awareness#actually system
52 notes
·
View notes
Text
Causes and Treatment of Sciatica, Neurosurgeon in Dwarka, Delhi

Sciatica is a common spine condition that causes severe pain or tingling sensations in the back or legs. The pain, numbness, and tingling caused, radiate along the sciatic nerve, This condition negatively impacts one’s efficiency while doing normal activities in daily life. In this comprehensive article, Dr. Nagesh Chandra, one of the top neurosurgeon in Dwarka, Delhi explains symptoms and treatment options for sciatica in India.
The sciatic nerve is the thickest and longest nerve in the human body, that comes from the lower back and extends down the side of each leg and buttock. It consists of multiple nerve roots flowing from the lumbar and sacral spine.
What are the causes of Sciatica?
Sciatica is mainly caused when the sciatic nerve is pinched. The following are the causes of sciatica:
Herniated Discs: One of the main causes of sciatica is a herniated disc. When the soft inner material of a disc protrudes and compresses the adjacent nerve roots, it results in sciatic nerve pinching and pain.
Spinal Stenosis: Narrowing of the spinal canal, a condition known as spinal stenosis, can also lead to sciatica. This narrowing put pressure on the nerves, causing pain and discomfort.
Piriformis Syndrome: The sciatic nerve can be irritated by the piriformis muscle, a condition referred to as piriformis syndrome. This occurs when the muscle spasms or tightens, compressing the sciatic nerve.
Degenerative Spine Disease: As the discs in the spine age, they lose their cushioning ability. This degeneration causes sciatica, especially in older individuals after 50 years of age.
What are the Symptoms of Sciatica
Sciatica causes following symptoms:
Pain: The primary symptom of sciatica is pain radiating from the lower back down the leg. The pain ca be a mild ache or even a sharp, burning sensation.
Numbness and Tingling: Individuals with sciatica experience numbness and tingling along the path of the sciatic nerve. This can go from the lower back to the toes.
Weakness: Sciatica causes weakness in the affected leg, sometimes it makes difficult to to stand, walk, or perform daily activities.
How a spine specialist diagnose Sciatica?
A qualified spine doctor would undergo following tests to confirm sciatica including:
Physical Examination: A physical examination to assess reflexes, muscle strength, and sensory function.
Lab tests: X-rays, MRI, and CT scans to get the detailed images of the spine, helping identify the root cause of sciatica.
Electromyography Test for sciatica (EMG): This test measures the electrical activity in muscles, to diagnose nerve damage.
When to see a spine doctor?
Experiencing sciatica is very painful at times and hence knowing when to consult doctor can save you from severe spine conditions. Here are the following conditions when you should immediately visit a spine specialist:
Persistent Pain: If you’re experiencing persistent and severe pain that doesn’t improve with pain relievers, consult the doctor now.
Symptoms Worsening: If your symptoms are getting worse, including increased pain, numbness, or weakness.
Numbness or Weakness: The numbness or weakness in the leg or foot, particularly if it is affecting your ability to walk or perform daily activities, is a concerning symptom that needs immediate medical diagnosis.
Bowel or Bladder Dysfunction: Difficulty controlling bowel or bladder function, such as incontinence or retention, may indicate a more severe nerve compression and requires immediate medical attention.
Injury: If your sciatica is the result of a recent injury or trauma, it’s essential to see a doctor
Fever or Infection Signs: If you experience symptoms such as fever, chills, or signs of infection (redness, warmth, swelling) around the lower back or buttocks,
No Improvement with traditional treatment: When you’ve tried home remedies, rest, and medicines for a reasonable period without relief, it’s time to consult specialist.
What is the Treatment for Sciatica available in India?
Dr. Nagesh explains the available treatment options for sciatica adopted by spine doctor in Dwarka, Delhi including:
Traditional Sciatica Treatment without surgery options:
Physical therapy can be used for relieving sciatica symptoms. Experts design specific exercises plans to strengthen the muscles surrounding the sciatic nerve, it can be a long-term treatment but can help in long run too.
Applying heat or cold packs also offer relief.
Medicines for sciatica treatment
Nonsteroidal anti-inflammatory drugs (NSAIDs) help reduce inflammation and alleviate pain.
Muscle relaxants: Prescribed to alleviate muscle spasms.
Oral corticosteroids: In some cases, steroids are also prescribed to reduce inflammation around the affected nerve. But it should only be taken if prescribed as these can have side-effects.
Epidural Steroid Injections: In severe cases, a neurosurgeon administer corticosteroids directly into the epidural space around the affected nerve root, providing targeted relief.
Sciatica Surgery in Delhi
Neurosurgeons can suggest following types of surgeries if the above treatments don’t give positive results:
A microdiscectomy is a minimally invasive surgery for removing a small portion of the herniated disc that is pressing on the sciatic nerve. This surgery relieve pressure on the nerve and reduce associated symptoms.
Laminectomy involves the removal of the lamina (a portion of the vertebra) to create more space around the nerve roots. This spine surgery is recommended for cases of spinal stenosis that are causing sciatica.
Lumbar decompression surgery is a term that encompasses surgeries aimed at relieving pressure on the spinal nerves. This includes laminectomy, foraminotomy, or other techniques depending on the underlying cause of sciatica.
Spinal fusion is recommended in cases where instability of the spine is leading to the sciatica. In this surgery, fusing two or more vertebrae together is done to provide stability and reduce nerve irritation.
Why choose Dr. Nagesh Chandra, for sciatica treatment in Delhi?
When it comes to addressing complex neurological issues such as sciatica, seek the expertise of a skilled neurosurgeon. Dr. Nagesh Chandra, a renowned neurosurgeon in Delhi who is offering treatment at his clinic called Center for Brain and Spine. He has performed more than 800 neuro surgeries and is experienced in treating sciatica and other neurosurgical conditions from last 25 years.
Dr. Chandra’s expertise and experience as a neuro specialist helps patients to get personalized treatment and recovery quickly.
If you or a loved one is grappling with the challenges of sciatica, consider consulting with Dr. Nagesh Chandra for assessment and treatment.
#SPINE DOCTOR IN DELHI#SPINE SURGERY IN DELHI#SCOLIOSIS TREATMENT IN DELHI#NEUROSURGEON IN DELHI#BEST NEUROSURGERY SPECIALIST IN DELHI
0 notes
Text
Continence Aids Australia - Funding For Bladder and Bowel Problems
Bladder and bowel problems can range from a small leak to losing control completely. They can be prevented or managed but some people need support and assistance. The Australian Government and state and territory governments operate a range of funding schemes with diverse eligibility criteria. Some products may be subsidised including pads, catheters and bedding protectors. Your continence nurse adviser can advise you on what is available.
Continence Aids Australia is the national peak body for continence, bladder and bowel health providing education, advocacy, awareness and support. It has representatives in each state and territory.
The Australian Government Department of Health provides support for continence products through the Continence Aids Payment Scheme (CAPS). CAPS enables eligible people who have permanent and severe incontinence to meet some of the cost of the continence products they need, through the supplier of their choice. You can find more information on the CAPS website.
Some states and territories also provide support for continence equipment and products through their individualised funding schemes. In New South Wales, for example, there is the Community Equipment Scheme (CES) operated by EnableNSW which offers continence products and supplies through a contracted supplier. The CES program requires you to have a completed assessment by an EnableNSW continence nurse or occupational therapist and hold a Pensioner Concession Card.
It is important to know that continence issues can be prevented by drinking plenty of fluids, eating a healthy diet and maintaining a normal weight. Regular exercise, avoiding smoking and not overdoing it can also help.
Many continence products can be found in supermarkets but you may need to visit a medical supply store to get more specialised items like dribble pouches for men or catheters for women. Some of these suppliers offer discounts for bulk purchases, and your continence nurse advisor can refer you to the best one in your area.
If you need help with continence, talk to your GP or a continence nurse specialist at your local hospital or private practice. Your local community health service can also help by offering referrals to specialists. If you are eligible for the NDIS or have a permanent and severe disability, your NDIS planner can arrange continence products and equipment through your plan. Your assessing health practitioner can provide you with a Continence Direct Order Form which allows you to purchase a maximum of three months of continence products at a time. The forms are valid for two years and must be renewed by your assessing health professional or nominated representative. If your needs change, your assessing health professional or nominated person should contact the current supplier to discuss changing orders as soon as possible. If you do not have an assessing health professional, contact the Continence Direct Order line on 1300 747 937. You can also access the Continence Library which is a resource of information and advice for different types of incontinence, including tips and product recommendations. It is accessible via the internet or by calling the free Continence Helpline on 1800 330 066 staffed by continence nurses.
Best HealthCare Products, where we prioritise your comfort and convenience. At our store, we focus on providing top-tier NDIS continence products to alleviate the challenges of incontinence. Our dedication lies in curating a selection of premium brands at the most competitive prices, ensuring that you not only save money but also receive unparalleled quality.
#continence aids australia#incontinence booster pads#continence aids meaning#incontinence pads australia
0 notes
Text
Assistance with Daily Living | melbourneeternity.com.au
ADL assessments are often the first step in identifying whether someone needs assistance with daily living. ADLs include everything from dressing and undressing to showering, eating and getting around.
Instrumental Activities of Daily Living (iADLs) are more complex self-care tasks and generally require a higher level of thinking and planning than ADLs. It’s common for people to lose iADL skills before ADL skills decline.
Meal Preparation
Meal preparation services are a vital component of assistance with daily living. They ensure seniors get proper nutrition and help them avoid dangers like tripping over food left on the floor or accidentally starting a fire when heating a frozen meal.
In addition, meal preparation helps them retain a sense of independence and selfreliance. Caregivers also help them maintain a healthy diet that includes vegetables, fruits, protein sources and more.
Some seniors require special dietary needs, so caregivers discuss their diet with them and nutritionists/doctors to make sure the meals are nutritionally sound. This can include dietary restrictions, including vegetarian, vegan and kosher diets. Similarly, meal planning can take into account other dietary considerations like fluid intake and medication-related restrictions.
Personal Hygiene
Maintaining good hygiene is essential to a senior’s health and wellbeing. Aside from promoting confidence and dignity, the skin acts as an armor that protects against bacteria (germs).
Hygiene services include bathing/showering, grooming (including brushing hair, washing teeth and oral care), and nail care. They can also provide assistance with continence, which refers to one’s ability to use the restroom and control bladder and bowel functions.
They can also help with transferring and ambulating, which involves moving in and out of bed and using a wheelchair or walker. Lastly, they can assist with feeding and nutrition by serving meals and providing snacks, as well as grocery shopping.
Housekeeping
Daily living services offer help with house cleaning and maintenance tasks, shopping errands, food prep, laundering clothing and bedding. Some services also help with more serious daily activities such as bathing and toileting.
The Lawton-Brody Instrumental Activities of Daily Living (IADLs) scale is a commonly used checklist to determine someone’s ability to perform IADLs independently. Generally, a score of 5 or more indicates that an individual is able to perform IADLs without assistance.
Our team of home health aides can assist with the following home support services in the area of daily living:
Transportation
Getting around and visiting friends and family can be difficult for older people with disabilities, especially those who don’t drive. This support covers the cost of transportation services to enable participants to access services outside their homes, such as shopping or attending appointments.
Typically, this type of support can be combined with domestic ndis assistance with daily living or personal care, but standalone options are available if that doesn’t suit a participant. For example, a ride-hailing service might cover transport while a cleaning service can take care of housekeeping duties.
It’s important to remember that a person’s ability to complete ADLs and IADLs declines gradually over time. This means that it may be hard for you to notice a change until your loved one needs more assistance than you can provide.
Medication Management
A medication management program (also known as medicine use review) ensures a participant’s prescriptions are being used correctly and at the right dosages. This is important because the physiology of each patient is different and some medications can have unexpected results.
A comprehensive medication management plan can also help participants avoid negative drug interactions and prescription-based side effects. This is especially useful when a participant sees multiple doctors who have no prior knowledge of each other’s prescribed medications.
NDIS funding for daily living support covers a range of services including:
0 notes
Text
When A Traumatic Brain Injury Alters Your Senses
Did you know that moderate to severe traumatic brain injury cases often worsen over time, with about 30% of TBI cases showing no improvement five years after the injury, as reported by the CDC?
Additionally, some TBI survivors may encounter another challenge: traumatic anosmia, the loss of their sense of smell. While TBIs typically result from head trauma, they can also occur due to penetrating brain injuries, such as gunshot wounds to the head.
As a result, TBIs can affect individuals in a multitude of ways, impacting them emotionally, cognitively, and sensorily, often leaving a lasting mark that may persist for a lifetime.
Physical Challenges Most TBIs are caused by falls, but they can also result from auto accidents or assaults. Physical repercussions may include:
– Sleep disturbances
– Persistent fatigue
– Changes in appetite
– Swallowing difficulties
– Paralysis
– Chronic pain
– Loss of bladder or bowel control
– Seizures
Cognitive Impairments Many TBI survivors grapple with headaches, concentration issues, memory deficits, and confusion. Some may also experience perseveration, the repetitive use of gestures or words.
Communication Hurdles TBIs can disrupt a person’s ability to communicate, leading to speech difficulties. For instance, aphasia may develop, causing problems with expressing ideas or understanding spoken language. This can be further categorized into receptive aphasia (trouble comprehending speech) and expressive aphasia (difficulty articulating thoughts).
Vision and Hearing Complications Some TBI victims may experience vision problems like double or blurred vision, involuntary eye movements (nystagmus), or heightened sensitivity to light (photophobia). Hearing issues, including ringing in the ears (tinnitus) and sound sensitivity, can also arise.
Emotional and Social Challenges TBIs can give rise to social-emotional difficulties, including mood swings, irritability, and even aggression.
Sensory Disruption When specific areas of the brain are affected by a TBI, sensory integration problems can arise, affecting sight, touch, hearing, taste, and smell.
Challenges of Traumatic Anosmia Anosmia, the diminished sense of smell, can result from a TBI when the olfactory nerve, responsible for transmitting scent information from the nose to the brain, is damaged. The prognosis for recovery depends on the extent of nerve damage.
Causes of Olfactory Nerve Trauma Trauma to the olfactory nerve often occurs when the ethmoid bone in the face, which separates the upper nasal cavity and the bottom of the eye sockets, is fractured. This can happen during:
– Vehicle accidents where the face hits the steering wheel or dashboard
– Slip and fall incidents
Seek Legal Counsel for TBI Cases Sadly, insurance companies sometimes underestimate the significance of losing one’s sense of smell. However, traumatic anosmia can be life-altering, as it may prevent you from detecting hazards like smoke or harmful chemicals, potentially endangering your health and safety.
Furthermore, the loss of smell can disrupt your sense of taste, leading to issues like malnutrition and unhealthy weight loss. Upon discovering your loss of smell, it’s crucial to consult a medical specialist in olfactory dysfunction promptly.
Insurance companies or defendants in TBI personal injury claims may downplay such injuries, prioritizing profits over your well-being. Nevertheless, the loss of smell, like other TBI conditions, should never be taken lightly.
Know Your Rights for Personal Injury Claims If you’ve suffered a loss of smell due to a traumatic brain injury or face any other injury-related condition, you need to act swiftly in California. The statute of limitations for personal injury claims related to TBI is two years from the injury date. If you discover the injury later, you have one year from the discovery date to file your claim.
Contact Belal Hamideh Law for Expert Guidance To learn more about your rights regarding personal injury claims related to TBI or traumatic anosmia, get in touch with Belal Hamideh Law for a consultation at (562) 526-1224 today.
0 notes
Text
Stay hearty and healthy during pregnancy by following these simple tips

Pregnancy marks the onset of parenthood. We often think that we only become a parent after the birth, but it really starts at conception. During the phase of pregnancy, everything we eat, drink, breathe, say, think… becomes relevant in a whole new way altogether.
You probably know some of the basics about taking care of yourself and the baby. Don’t smoke. Don’t drink. Get your rest. The list goes on and on…There are do’s and don’ts for everything. But, instead of following a set rulebook, and stressing yourself out even more, just keep in mind that staying healthy comprises of simple efforts carried out every day. Here are some handy tips, that can help ensure a safe and healthy pregnancy.
Take prenatal vitamins daily
Even when you’re still trying to conceive, it is the right time to start taking prenatal vitamins. Your baby’s neural cord, which becomes the brain and spinal cord, develops within the first month of pregnancy, so it’s important you get essential nutrients, like folic acid, calcium, and iron, from the very start. Plan an exercise chart
Staying active is a must for most moms to be. Regular exercise will help you control your weight, improve circulation, boost your mood, and help you sleep better. Pilates, yoga, swimming, and walking are all great activities for most pregnant women, but be sure to check with your doctor first before starting any exercise program. Aim for 30 minutes of exercise most days of the week. Listen to your body, though, and don’t overdo it.
Know about latest trends
Even if this is not your first child, attending a childbirth/prenatal class will help you feel more prepared for delivery. Not only will you have the chance to learn more about childbirth and infant care, but you can ask specific questions and voice any concerns. You’ll also become more acquainted with the facility and its staff. This is also a good time to brush up on your family’s medical history. Talk to your doctor about problems with past pregnancies, and report any family incidences of birth defects.
Practice Kegels
Kegels strengthen the pelvic floor muscles, which support your bladder, bowels, and uterus. When done correctly, this simple exercise can help make your delivery easier and prevent problems later with urinary incontinence. It is a very convenient and easy exercise and can be done daily.
Practice squeezing as though you’re stopping the flow of urine when you use the bathroom.
– Hold for three seconds, then relax for three.
– Repeat 10 times.
Track your weight gain
In pregnancy, the common notion is to eat for two people. But packing on too many extra kilos may make them hard to lose later. At the same time, not can gaining enough weight can put the baby at risk for a low-weight birth, a major cause of developmental problems.
Go shoe shopping
As your body grows, so may your feet. This happens due to natural weight gain throwing off your center of gravity, putting extra pressure on your feet. Over time this added pressure can cause painful over-pronation, or flatten out the feet. You may retain fluids, too, which can make your feet and ankles swell. To prevent these problems, wear comfortable shoes with good support.
Folate-rich foods are a must
Folic acid is crucial for the baby’s neurological development and vital for the creation of new red blood cells. It is a smart choice to start eating plenty of folate-rich foods like fortified cereals, asparagus, lentils, wheat germ, oranges, and orange juice.
Recharge with fruits
Most doctors recommend limiting caffeine during pregnancy since it can have harmful effects on you and the baby. Cutting down can be tough, though, especially when you’re used to your morning cup. For a quick boost up, try nibbling on some fruit. “The natural sugars in fruits like bananas and apples can help lift energy levels.
Fly smart
According to clinical experts, mid-pregnancy, around 14 to 28 weeks, is usually the best time to fly. By this time you’re probably over morning sickness, and the risk of miscarriage or early delivery is low. Still, check with your doctor about any travel plans, and make sure the airline has no restrictions for pregnant women. While on the plane, drink plenty of water to stay hydrated, and get up and walk around every half hour to reduce the risk of blood clots. An aisle seat will give you more room and make trips to the bathroom easier.
Know when to call the doctor
Being pregnant can be confusing, especially if it is your first time. How do you know which twinge is normal and which one isn’t? According to the Centers for Disease Control and Prevention, you should call your doctor if you have any of these
symptoms:
– Pain of any kind
– Strong cramps
– Contractions at 20-minute intervals
– Vaginal bleeding or leaking of fluid
– Dizziness or fainting
– Shortness of breath
– Heart palpitations
– Constant nausea and vomiting
– Trouble walking, edema (swelling of joints)
– Decreased activity by the baby
Get regular prenatal care
Begin prenatal care as soon as your pregnancy test result is positive, when you decide you want to conceive or when you suspect you might be pregnant. You can start by seeing your regular doctor, but will likely want to transfer to a specialized prenatal care doctor as your pregnancy progresses. As long as you are undergoing a normal pregnancy (according to your doctor), your scheduled prenatal appointments should follow this timeline:
See your physician every four weeks until you are 28 weeks pregnant
See your physician every two weeks from the time you are 28 weeks to 36 weeks pregnant
See your physician once a week (or more often, as per your doctor’s instructions) after the 36th week of pregnancy
Indulge Yourself
You may think you’re busy now, but once the baby is born, you will have even fewer precious moments to yourself. Treating yourself to a pedicure/manicure, spending time with friends, or simply taking a quiet walk can help you relax and de-stress, and that’s good for both you and the baby.
0 notes
Text
What are the health benefits of green tea?

What are the health benefits of green tea? Green tea's health advantages have been touted for generations. Green tea may improve skin, weight reduction, and cardiovascular health, according to research.
Tea is the second most drank beverage after water, according to the International Institute of Sustainable Development.
All teas except herbal use dried Camellia sinensis leaves. Leaf oxidation determines tea type.
Green tea is unoxidized and little processed. It has the greatest antioxidants and polyphenols.
Here are defining health benefits of green tea.

Health benefits of green tea
By Thealthiest Web Desk: Traditional Chinese and Indian medicine utilized green tea to control bleeding, heal wounds, promote digestion, heart and brain health, and body temperature.
Green tea may aid weight reduction, liver health, type 2 diabetes, Alzheimer's disease, and more.
Scientists need more evidence to prove these potential health advantages.
Cancer prevention
Green tea lovers have decreased cancer rates. Human studies have not consistently proven that green tea decreases cancer risk.
2020 database reviewTrusted Source Empirical and experimental investigations in people showed contradictory findings and scant evidence that green tea reduces cancer risk. 142 studies with 1.1 million participants were examined.
However, topical green tea polyphenol extracts may protect skin from UVB exposure. Tea polyphenols may protect UVB-induced skin cancer, according to a 2018 review.
Animal and test-tube cell studiesTrusted Source suggests benefits for certain cancers:
breast
bladder
ovarian
colorectal (bowel)
esophageal (throat)
lung
prostate
skin
stomach
Overall findings from numerous human studies have yielded inconsistent results and limited evidence of the benefit of drinking green tea on the overall risk of cancer.
Weight loss
A analysis of multiple trials indicated that green tea catechins and caffeine may increase energy metabolism and weight reduction.
Another meta-analysisTrusted Source of multiple tea polyphenols-induced weight loss pathways showed that catechins and caffeine synergistically caused weight reduction.
Green tea may help you lose weight, but not clinically. Most studies showing minor metabolic alterations employed green tea extracts with exceptionally high catechin concentrations.
Inflammatory skin conditions
Anti-inflammatory green tea. Clinical trials reviewTrusted Source Both cellular and animal tests showed that green tea and its main component, epigallocatechin-3-gallate (EGCG), reduce inflammation.
2019 analysisTrusted cosmetic tea extract source backed this. When administered topically, tea extract solutions reduced inflammation. The damaged skin microcirculation improved.
Also read: Benefits of Planting Trees
Heart health
2006 studyTrusted Source indicated green tea drinking reduces cardiovascular disease mortality.
Since 1994, the research monitored 40,000 Japanese 40–79-year-olds. Green tea drinkers had a lower risk of cardiovascular disease death.
A 2016 meta-analysis validated similar findings. Nine trials with 259,267 participants were analyzed. The researchers found that green tea drinking reduced cardiovascular and ischemic disease risk.
Green tea polyphenols may lower blood pressure, inflammation, and epithelial function, which may lessen heart disease risk in obese persons, according to 2017 and 2019 studies.
0 notes
Text
盆底肌弱化会引发哪些健康问题?不容忽视的警示!
Did you know that having weak pelvic floor muscles can lead to various health problems? That's right! Pelvic floor muscles support our internal organs and play a crucial role in bladder and bowel control. However, many people tend to overlook the importance of these muscles until they experience serious health issues. Therefore, it's essential to understand how weak pelvic floor muscles can affect your health and take necessary measures to strengthen them. The Perils of Weak Pelvic Floor Muscles: What You Need to Know! First and foremost, weak pelvic floor muscles can cause urinary incontinence, a condition where you lose control over your bladder. This means you may leak urine when you cough, sneeze, or exercise. Unfortunately, urinary incontinence can significantly affect your quality of life, leading to social embarrassment, anxiety, and depression. Moreover, weak pelvic floor muscles can also cause fecal incontinence, which is an inability to control bowel movements, leading to involuntary stool leakage. Another potential risk of weak pelvic floor muscles is pelvic organ prolapse, where your pelvic organs, such as the uterus, bladder, or rectum, drop down from their normal position and push against the vaginal wall. This can cause discomfort, pain, and difficulties with urination or bowel movements. Women who have given birth vaginally, obese people, and those who frequently lift heavy weights are at risk of developing pelvic organ prolapse. Therefore, strengthening your pelvic floor muscles can help prevent this condition. Additionally, weak pelvic floor muscles can affect sexual health. Men with weak pelvic floor muscles may experience erectile dysfunction or premature ejaculation, while women may have difficulty achieving orgasm or experience pain during sexual intercourse. Strengthening your pelvic floor muscles can improve your sexual health and enhance sexual pleasure. Don't Ignore the Signs: How Weak Pelvic Floor Muscles Affect Your Health! If you experience any signs of weak pelvic floor muscles, such as urinary or fecal incontinence, pelvic pain, or discomfort during sexual activity, it's crucial to seek medical attention. Your doctor may recommend pelvic floor exercises or refer you to a physical therapist who specializes in pelvic floor rehabilitation. These exercises can help improve bladder and bowel control, reduce pelvic pain, and enhance sexual function. Moreover, making lifestyle changes can also help prevent weak pelvic floor muscles. Maintaining a healthy weight, avoiding constipation, and practicing good toilet habits, such as not straining during bowel movements, can reduce your risk of developing pelvic floor problems. Additionally, avoiding heavy lifting and high-impact exercises can also help prevent pelvic organ prolapse. In conclusion, weak pelvic floor muscles can lead to several health problems, including urinary and fecal incontinence, pelvic organ prolapse, and sexual dysfunction. However, with proper care, you can prevent these conditions and improve your quality of life. So, don't ignore the signs and take steps to strengthen your pelvic floor muscles today! Read the full article
0 notes
Text
DISC INJURY TREATMENT IN FORT WORTH

Top Chiropractic Care for Herniated Disc in Fort Worth
Disc injuries cause a great deal of pain and discomfort. If you are one of the many people who suffer from a herniated disc, it would be highly recommended to work with a Chiropractor. A Chiropractor is specially trained to treat these types of injuries and can help you get back to your life.
Chiropractors are experts in treating spinal injuries and can provide you with the care you need to reduce your pain and improve your quality of life.
What is a Herniated Disc?
A herniated disc is a condition that results when the outer layer of the spinal disc tears, allowing the inner layer to leak out. This can cause pain, numbness, and tingling in the back and neck. When this happens, the discs can put pressure on the spinal cord or nerves, leading to more serious problems. Herniated discs are a common cause of neck and back pain and can often be treated without surgery.
Causes of a Herniated Disc
A herniated disc can happen for a number of reasons, including:
lifting heavy objects
sudden movements or accidents
poor posture
age-related wear and tear
smoking
If you are experiencing pain as a result of a herniated disc, it is important to see a Chiropractor right away. A Chiropractor can help you determine the cause of your injury and provide you with the care you need to get relief.
Symptoms of a Herniated Disc
Most of the time, a herniated disc usually happens in the lower back area. However, they can occur in the neck as well. Common Symptoms of a herniated disc can include:
pain in the back or neck
tingling or numbness in the arms or legs
weakness in the arms or legs
loss of bladder or bowel control
If you are experiencing any of these symptoms, it is important to see a Chiropractor right away. Our chiropractic team in Fort Worth can help you determine the underlying cause and build a treatment plan to get you back on track to optimal health and pain-free life.
Degenerative Disc Disease
Degenerative disc disease (DDD) is different than a herniated disc. It is a condition that occurs when the discs between the vertebrae in the spine begin to break down and lose their cushioning effect. This can lead to pain, stiffness, and a loss of mobility in the spine. DDD is a common cause of back pain and can often be treated without surgery.
There are several factors that can contribute to DDD, including:
aging
smoking
excessive weight
trauma or injury
poor posture
If you are experiencing pain as a result of DDD, it is also important to see a Chiropractor in Fort Worth right away. A Chiropractor can help you determine the cause of your injury and provide you with the care you need.
Benefits of Chiropractic Care for Herniated Disc & Disc Pain
Chiropractic care is a non-invasive treatment to help restore your disc to proper alignment.
There are a few different Chiropractic techniques that can be used to treat a herniated disc. The most common technique is spinal manipulation, which is also known as chiropractic adjustment. This technique uses manual pressure to restore the alignment of the spine.
In some instances, it may include massage, electrical stimulation, and ultrasound. In many cases, Chiropractic care can help you avoid surgery.
Most people experience significant relief from their symptoms after chiropractic care. In some cases, however, there may be a small amount of discomfort as the disc heals. With time and patience, however, you should be able to return to your normal activities.
Get Chiropractic Care for Your Herniated Disc in Fort Worth
If you’re experiencing a herniated disc, degenerative disc disease, or other disc-related issues, we are here for you. Our chiropractic team specializes in spinal health and keeping your spine in alignment. You don’t have to live in pain.
Give our office a call to book an appointment today.
0 notes