#the scientific method. if not germ theory
Explore tagged Tumblr posts
Text
Also preserved on our archive
SARS-CoV-2 is now circulating out of control worldwide. The only major limitation on transmission is the immune environment the virus faces. The disease it causes, COVID-19, is now a risk faced by most people as part of daily life.
While some are better than others, no national or regional government is making serious efforts towards infection prevention and control, and it seems likely this laissez-faire policy will continue for the foreseeable future. The social, political, and economic movements that worked to achieve this mass infection environment can rejoice at their success.
Those schooled in public health, immunology or working on the front line of healthcare provision know we face an uncertain future, and are aware the implications of recent events stretch far beyond SARS-CoV-2. The shifts that have taken place in attitudes and public health policy will likely damage a key pillar that forms the basis of modern civilized society, one that was built over the last two centuries; the expectation of a largely uninterrupted upwards trajectory of ever-improving health and quality of life, largely driven by the reduction and elimination of infectious diseases that plagued humankind for thousands of years. In the last three years, that trajectory has reversed.
The upward trajectory of public health in the last two centuries Control of infectious disease has historically been a priority for all societies. Quarantine has been in common use since at least the Bronze Age and has been the key method for preventing the spread of infectious diseases ever since. The word “quarantine” itself derives from the 40-day isolation period for ships and crews that was implemented in Europe during the late Middle Ages to prevent the introduction of bubonic plague epidemics into cities.
Modern public health traces its roots to the middle of the 19th century thanks to converging scientific developments in early industrial societies:
The germ theory of diseases was firmly established in the mid-19th century, in particular after Louis Pasteur disproved the spontaneous generation hypothesis. If diseases spread through transmission chains between individual humans or from the environment/animals to humans, then it follows that those transmission chains can be interrupted, and the spread stopped. The science of epidemiology appeared, its birth usually associated with the 1854 Broad Street cholera outbreak in London during which the British physician John Snow identified contaminated water as the source of cholera, pointing to improved sanitation as the way to stop cholera epidemics. Vaccination technology began to develop, initially against smallpox, and the first mandatory smallpox vaccination campaigns began, starting in England in the 1850s.
The early industrial era generated horrendous workplace and living conditions for working class populations living in large industrial cities, dramatically reducing life expectancy and quality of life (life expectancy at birth in key industrial cities in the middle of the 19th century was often in the low 30s or even lower). This in turn resulted in a recognition that such environmental factors affect human health and life spans. The long and bitter struggle for workers’ rights in subsequent decades resulted in much improved working conditions, workplace safety regulations, and general sanitation, and brought sharp increases in life expectancy and quality of life, which in turn had positive impacts on productivity and wealth.
Florence Nightingale reemphasized the role of ventilation in healing and preventing illness, ‘The very first canon of nursing… : keep the air he breathes as pure as the external air, without chilling him,’ a maxim that influenced building design at the time.
These trends continued in the 20th century, greatly helped by further technological and scientific advances. Many diseases – diphtheria, pertussis, hepatitis B, polio, measles, mumps, rubella, etc. – became things of the past thanks to near-universal highly effective vaccinations, while others that used to be common are no longer of such concern for highly developed countries in temperate climates – malaria, typhus, typhoid, leprosy, cholera, tuberculosis, and many others – primarily thanks to improvements in hygiene and the implementation of non-pharmaceutical measures for their containment.
Furthermore, the idea that infectious diseases should not just be reduced, but permanently eliminated altogether began to be put into practice in the second half of the 20th century on a global level, and much earlier locally. These programs were based on the obvious consideration that if an infectious agent is driven to extinction, the incalculable damage to people’s health and the overall economy by a persisting and indefinite disease burden will also be eliminated.
The ambition of local elimination grew into one of global eradication for smallpox, which was successfully eliminated from the human population in the 1970s (this had already been achieved locally in the late 19th century by some countries), after a heroic effort to find and contain the last remaining infectious individuals. The other complete success was rinderpest in cattle9,10, globally eradicated in the early 21st century.
When the COVID-19 pandemic started, global eradication programs were very close to succeeding for two other diseases – polio and dracunculiasis. Eradication is also globally pursued for other diseases, such as yaws, and regionally for many others, e.g. lymphatic filariasis, onchocerciasis, measles and rubella. The most challenging diseases are those that have an external reservoir outside the human population, especially if they are insect borne, and in particular those carried by mosquitos. Malaria is the primary example, but despite these difficulties, eradication of malaria has been a long-standing global public health goal and elimination has been achieved in temperate regions of the globe, even though it involved the ecologically destructive widespread application of polluting chemical pesticides to reduce the populations of the vectors. Elimination is also a public goal for other insect borne diseases such as trypanosomiasis.
In parallel with pursuing maximal reduction and eventual eradication of the burden of existing endemic infectious diseases, humanity has also had to battle novel infectious diseases40, which have been appearing at an increased rate over recent decades. Most of these diseases are of zoonotic origin, and the rate at which they are making the jump from wildlife to humans is accelerating, because of the increased encroachment on wildlife due to expanding human populations and physical infrastructure associated with human activity, the continued destruction of wild ecosystems that forces wild animals towards closer human contact, the booming wildlife trade, and other such trends.
Because it is much easier to stop an outbreak when it is still in its early stages of spreading through the population than to eradicate an endemic pathogen, the governing principle has been that no emerging infectious disease should be allowed to become endemic. This goal has been pursued reasonably successfully and without controversy for many decades.
The most famous newly emerging pathogens were the filoviruses (Ebola, Marburg), the SARS and MERS coronaviruses, and paramyxoviruses like Nipah. These gained fame because of their high lethality and potential for human-to-human spread, but they were merely the most notable of many examples.
Such epidemics were almost always aggressively suppressed. Usually, these were small outbreaks, and because highly pathogenic viruses such as Ebola cause very serious sickness in practically all infected people, finding and isolating the contagious individuals is a manageable task. The largest such epidemic was the 2013-16 Ebola outbreak in West Africa, when a filovirus spread widely in major urban centers for the first time. Containment required a wartime-level mobilization, but that was nevertheless achieved, even though there were nearly 30,000 infections and more than 11,000 deaths.
SARS was also contained and eradicated from the human population back in 2003-04, and the same happened every time MERS made the jump from camels to humans, as well as when there were Nipah outbreaks in Asia.
The major counterexample of a successful establishment in the human population of a novel highly pathogenic virus is HIV. HIV is a retrovirus, and as such it integrates into the host genome and is thus nearly impossible to eliminate from the body and to eradicate from the population (unless all infected individuals are identified and prevented from infecting others for the rest of their lives). However, HIV is not an example of the containment principle being voluntarily abandoned as the virus had made its zoonotic jump and established itself many decades before its eventual discovery and recognition, and long before the molecular tools that could have detected and potentially fully contained it existed.
Still, despite all these containment success stories, the emergence of a new pathogen with pandemic potential was a well understood and frequently discussed threat, although influenza viruses rather than coronaviruses were often seen as the most likely culprit. The eventual appearance of SARS-CoV-2 should therefore not have been a huge surprise, and should have been met with a full mobilization of the technical tools and fundamental public health principles developed over the previous decades.
The ecological context One striking property of many emerging pathogens is how many of them come from bats. While the question of whether bats truly harbor more viruses than other mammals in proportion to their own species diversity (which is the second highest within mammals after rodents) is not fully settled yet, many novel viruses do indeed originate from bats, and the ecological and physiological characteristics of bats are highly relevant for understanding the situation that Homo sapiens finds itself in right now.
Another startling property of bats and their viruses is how highly pathogenic to humans (and other mammals) many bat viruses are, while bats themselves are not much affected (only rabies is well established to cause serious harm to bats). Why bats seem to carry so many such pathogens, and how they have adapted so well to coexisting with them, has been a long-standing puzzle and although we do not have a definitive answer, some general trends have become clear.
Bats are the only truly flying mammals and have been so for many millions of years. Flying has resulted in a number of specific adaptations, one of them being the tolerance towards a very high body temperature (often on the order of 42-43ºC). Bats often live in huge colonies, literally touching each other, and, again, have lived in conditions of very high density for millions of years. Such densities are rare among mammals and are certainly not the native condition of humans (human civilization and our large dense cities are a very recent phenomenon on evolutionary time scales). Bats are also quite long-lived for such small mammals – some fruit bats can live more than 35 years and even small cave dwelling species can live about a decade.
These are characteristics that might have on one hand facilitated the evolution of a considerable set of viruses associated with bat populations. In order for a non-latent respiratory virus to maintain itself, a minimal population size is necessary. For example, it is hypothesized that measles requires a minimum population size of 250-300,000 individuals. And bats have existed in a state of high population densities for a very long time, which might explain the high diversity of viruses that they carry. In addition, the long lifespan of many bat species means that their viruses may have to evolve strategies to overcome adaptive immunity and frequently reinfect previously infected individuals as opposed to the situation in short-lived species in which populations turn over quickly (with immunologically naive individuals replacing the ones that die out).
On the other hand, the selective pressure that these viruses have exerted on bats may have resulted in the evolution of various resistance and/or tolerance mechanisms in bats themselves, which in turn have driven the evolution of counter strategies in their viruses, leading them to be highly virulent for other species. Bats certainly appear to be physiologically more tolerant towards viruses that are otherwise highly virulent to other mammals. Several explanations for this adaptation have been proposed, chief among them a much more powerful innate immunity and a tolerance towards infections that does not lead to the development of the kind of hyperinflammatory reactions observed in humans, the high body temperature of bats in flight, and others.
The notable strength of bat innate immunity is often explained by the constitutively active interferon response that has been reported for some bat species. It is possible that this is not a universal characteristic of all bats – only a few species have been studied – but it provides a very attractive mechanism for explaining both how bats prevent the development of severe systemic viral infections in their bodies and how their viruses in turn would have evolved powerful mechanisms to silence the interferon response, making them highly pathogenic for other mammals.
The tolerance towards infection is possibly rooted in the absence of some components of the signaling cascades leading to hyperinflammatory reactions and the dampened activity of others.
An obvious ecological parallel can be drawn between bats and humans – just as bats live in dense colonies, so now do modern humans. And we may now be at a critical point in the history of our species, in which our ever-increasing ecological footprint has brought us in close contact with bats in a way that was much rarer in the past. Our population is connected in ways that were previously unimaginable. A novel virus can make the zoonotic jump somewhere in Southeast Asia and a carrier of it can then be on the other side of the globe a mere 24-hours later, having encountered thousands of people in airports and other mass transit systems. As a result, bat pathogens are now being transferred from bat populations to the human population in what might prove to be the second major zoonotic spillover event after the one associated with domestication of livestock and pets a few thousand years ago.
Unfortunately for us, our physiology is not suited to tolerate these new viruses. Bats have adapted to live with them over many millions of years. Humans have not undergone the same kind of adaptation and cannot do so on any timescale that will be of use to those living now, nor to our immediate descendants.
Simply put, humans are not bats, and the continuous existence and improvement of what we now call “civilization” depends on the same basic public health and infectious disease control that saw life expectancy in high-income countries more than double to 85 years. This is a challenge that will only increase in the coming years, because the trends that are accelerating the rate of zoonotic transfer of pathogens are certain to persist.
Given this context, it is as important now to maintain the public health principle that no new dangerous pathogens should be allowed to become endemic and that all novel infectious disease outbreaks must be suppressed as it ever was.
The death of public health and the end of epidemiological comfort It is also in this context that the real gravity of what has happened in the last three years emerges.
After HIV, SARS-CoV-2 is now the second most dangerous infectious disease agent that is 'endemic' to the human population on a global scale. And yet not only was it allowed to become endemic, but mass infection was outright encouraged, including by official public health bodies in numerous countries.
The implications of what has just happened have been missed by most, so let’s spell them out explicitly.
We need to be clear why containment of SARS-CoV-2 was actively sabotaged and eventually abandoned. It has absolutely nothing to do with the “impossibility” of achieving it. In fact, the technical problem of containing even a stealthily spreading virus such as SARS-CoV-2 is fully solved, and that solution was successfully applied in practice for years during the pandemic.
The list of countries that completely snuffed out outbreaks, often multiple times, includes Australia, New Zealand, Singapore, Taiwan, Vietnam, Thailand, Bhutan, Cuba, China, and a few others, with China having successfully contained hundreds of separate outbreaks, before finally giving up in late 2022.
The algorithm for containment is well established – passively break transmission chains through the implementation of nonpharmaceutical interventions (NPIs) such as limiting human contacts, high quality respirator masks, indoor air filtration and ventilation, and others, while aggressively hunting down active remaining transmission chains through traditional contact tracing and isolation methods combined with the powerful new tool of population-scale testing.
Understanding of airborne transmission and institution of mitigation measures, which have heretofore not been utilized in any country, will facilitate elimination, even with the newer, more transmissible variants. Any country that has the necessary resources (or is provided with them) can achieve full containment within a few months. In fact, currently this would be easier than ever before because of the accumulated widespread multiple recent exposures to the virus in the population suppressing the effective reproduction number (Re). For the last 18 months or so we have been seeing a constant high plateau of cases with undulating waves, but not the major explosions of infections with Re reaching 3-4 that were associated with the original introduction of the virus in 2020 and with the appearance of the first Omicron variants in late 2021.
It would be much easier to use NPIs to drive Re to much below 1 and keep it there until elimination when starting from Re around 1.2-1.3 than when it was over 3, and this moment should be used, before another radically new serotype appears and takes us back to those even more unpleasant situations. This is not a technical problem, but one of political and social will. As long as leadership misunderstands or pretends to misunderstand the link between increased mortality, morbidity and poorer economic performance and the free transmission of SARS-CoV-2, the impetus will be lacking to take the necessary steps to contain this damaging virus.
Political will is in short supply because powerful economic and corporate interests have been pushing policymakers to let the virus spread largely unchecked through the population since the very beginning of the pandemic. The reasons are simple. First, NPIs hurt general economic activity, even if only in the short term, resulting in losses on balance sheets. Second, large-scale containment efforts of the kind we only saw briefly in the first few months of the pandemic require substantial governmental support for all the people who need to pause their economic activity for the duration of effort. Such an effort also requires large-scale financial investment in, for example, contact tracing and mass testing infrastructure and providing high-quality masks. In an era dominated by laissez-faire economic dogma, this level of state investment and organization would have set too many unacceptable precedents, so in many jurisdictions it was fiercely resisted, regardless of the consequences for humanity and the economy.
None of these social and economic predicaments have been resolved. The unofficial alliance between big business and dangerous pathogens that was forged in early 2020 has emerged victorious and greatly strengthened from its battle against public health, and is poised to steamroll whatever meager opposition remains for the remainder of this, and future pandemics.
The long-established principles governing how we respond to new infectious diseases have now completely changed – the precedent has been established that dangerous emerging pathogens will no longer be contained, but instead permitted to ‘ease’ into widespread circulation. The intent to “let it rip” in the future is now being openly communicated. With this change in policy comes uncertainty about acceptable lethality. Just how bad will an infectious disease have to be to convince any government to mobilize a meaningful global public health response?
We have some clues regarding that issue from what happened during the initial appearance of the Omicron “variant” (which was really a new serotype) of SARS-CoV-2. Despite some experts warning that a vaccine-only approach would be doomed to fail, governments gambled everything on it. They were then faced with the brute fact of viral evolution destroying their strategy when a new serotype emerged against which existing vaccines had little effect in terms of blocking transmission. The reaction was not to bring back NPIs but to give up, seemingly regardless of the consequences.
Critically, those consequences were unknown when the policy of no intervention was adopted within days of the appearance of Omicron. All previous new SARS-CoV-2 variants had been deadlier than the original Wuhan strain, with the eventually globally dominant Delta variant perhaps as much as 4× as deadly. Omicron turned out to be the exception, but again, that was not known with any certainty when it was allowed to run wild through populations. What would have happened if it had followed the same pattern as Delta?
In the USA, for example, the worst COVID-19 wave was the one in the winter of 2020-21, at the peak of which at least 3,500 people were dying daily (the real number was certainly higher because of undercounting due to lack of testing and improper reporting). The first Omicron BA.1 wave saw the second-highest death tolls, with at least 2,800 dying per day at its peak. Had Omicron been as intrinsically lethal as Delta, we could have easily seen a 4-5× higher peak than January 2021, i.e. as many as 12–15,000 people dying a day. Given that we only had real data on Omicron’s intrinsic lethality after the gigantic wave of infections was unleashed onto the population, we have to conclude that 12–15,000 dead a day is now a threshold that will not force the implementation of serious NPIs for the next problematic COVID-19 serotype.
Logically, it follows that it is also a threshold that will not result in the implementation of NPIs for any other emerging pathogens either. Because why should SARS-CoV-2 be special?
We can only hope that we will never see the day when such an epidemic hits us but experience tells us such optimism is unfounded. The current level of suffering caused by COVID-19 has been completely normalized even though such a thing was unthinkable back in 2019. Populations are largely unaware of the long-term harms the virus is causing to those infected, of the burden on healthcare, increased disability, mortality and reduced life expectancy. Once a few even deadlier outbreaks have been shrugged off by governments worldwide, the baseline of what is considered “acceptable” will just gradually move up and even more unimaginable losses will eventually enter the “acceptable” category. There can be no doubt, from a public health perspective, we are regressing.
We had a second, even more worrying real-life example of what the future holds with the global spread of the MPX virus (formerly known as “monkeypox” and now called “Mpox”) in 2022. MPX is a close relative to the smallpox VARV virus and is endemic to Central and Western Africa, where its natural hosts are mostly various rodent species, but on occasions it infects humans too, with the rate of zoonotic transfer increasing over recent decades. It has usually been characterized by fairly high mortality – the CFR (Case Fatality Rate) has been ∼3.6% for the strain that circulates in Nigeria and ∼10% for the one in the Congo region, i.e. much worse than SARS-CoV-2. In 2022, an unexpected global MPX outbreak developed, with tens of thousands of confirmed cases in dozens of countries. Normally, this would be a huge cause for alarm, for several reasons.
First, MPX itself is a very dangerous disease. Second, universal smallpox vaccination ended many decades ago with the success of the eradication program, leaving the population born after that completely unprotected. Third, lethality in orthopoxviruses is, in fact, highly variable – VARV itself had a variola major strain, with as much as ∼30% CFR, and a less deadly variola minor variety with CFR ∼1%, and there was considerable variation within variola major too. It also appears that high pathogenicity often evolves from less pathogenic strains through reductive evolution - the loss of certain genes something that can happen fairly easily, may well have happened repeatedly in the past, and may happen again in the future, a scenario that has been repeatedly warned about for decades. For these reasons, it was unthinkable that anyone would just shrug off a massive MPX outbreak – it is already bad enough as it is, but allowing it to become endemic means it can one day evolve towards something functionally equivalent to smallpox in its impact.
And yet that is exactly what happened in 2022 – barely any measures were taken to contain the outbreak, and countries simply reclassified MPX out of the “high consequence infectious disease” category in order to push the problem away, out of sight and out of mind. By chance, it turned out that this particular outbreak did not spark a global pandemic, and it was also characterized, for poorly understood reasons, by an unusually low CFR, with very few people dying. But again, that is not the information that was available at the start of the outbreak, when in a previous, interventionist age of public health, resources would have been mobilized to stamp it out in its infancy, but, in the age of laissez-faire, were not. MPX is now circulating around the world and represents a future threat of uncontrolled transmission resulting in viral adaptation to highly efficient human-to-human spread combined with much greater disease severity.
While some are better than others, no national or regional government is making serious efforts towards infection prevention and control, and it seems likely this laissez-faire policy will continue for the foreseeable future. The social, political, and economic movements that worked to achieve this mass infection environment can rejoice at their success.
Those schooled in public health, immunology or working on the front line of healthcare provision know we face an uncertain future, and are aware the implications of recent events stretch far beyond SARS-CoV-2. The shifts that have taken place in attitudes and public health policy will likely damage a key pillar that forms the basis of modern civilized society, one that was built over the last two centuries; the expectation of a largely uninterrupted upwards trajectory of ever-improving health and quality of life, largely driven by the reduction and elimination of infectious diseases that plagued humankind for thousands of years. In the last three years, that trajectory has reversed.
The upward trajectory of public health in the last two centuries Control of infectious disease has historically been a priority for all societies. Quarantine has been in common use since at least the Bronze Age and has been the key method for preventing the spread of infectious diseases ever since. The word “quarantine” itself derives from the 40-day isolation period for ships and crews that was implemented in Europe during the late Middle Ages to prevent the introduction of bubonic plague epidemics into cities1.
Rat climbing a ship's rigging. Modern public health traces its roots to the middle of the 19th century thanks to converging scientific developments in early industrial societies:
The germ theory of diseases was firmly established in the mid-19th century, in particular after Louis Pasteur disproved the spontaneous generation hypothesis. If diseases spread through transmission chains between individual humans or from the environment/animals to humans, then it follows that those transmission chains can be interrupted, and the spread stopped. The science of epidemiology appeared, its birth usually associated with the 1854 Broad Street cholera outbreak in London during which the British physician John Snow identified contaminated water as the source of cholera, pointing to improved sanitation as the way to stop cholera epidemics. Vaccination technology began to develop, initially against smallpox, and the first mandatory smallpox vaccination campaigns began, starting in England in the 1850s. The early industrial era generated horrendous workplace and living conditions for working class populations living in large industrial cities, dramatically reducing life expectancy and quality of life (life expectancy at birth in key industrial cities in the middle of the 19th century was often in the low 30s or even lower2). This in turn resulted in a recognition that such environmental factors affect human health and life spans. The long and bitter struggle for workers’ rights in subsequent decades resulted in much improved working conditions, workplace safety regulations, and general sanitation, and brought sharp increases in life expectancy and quality of life, which in turn had positive impacts on productivity and wealth. Florence Nightingale reemphasized the role of ventilation in healing and preventing illness, ‘The very first canon of nursing… : keep the air he breathes as pure as the external air, without chilling him,’ a maxim that influenced building design at the time. These trends continued in the 20th century, greatly helped by further technological and scientific advances. Many diseases – diphtheria, pertussis, hepatitis B, polio, measles, mumps, rubella, etc. – became things of the past thanks to near-universal highly effective vaccinations, while others that used to be common are no longer of such concern for highly developed countries in temperate climates – malaria, typhus, typhoid, leprosy, cholera, tuberculosis, and many others – primarily thanks to improvements in hygiene and the implementation of non-pharmaceutical measures for their containment.
Furthermore, the idea that infectious diseases should not just be reduced, but permanently eliminated altogether began to be put into practice in the second half of the 20th century3-5 on a global level, and much earlier locally. These programs were based on the obvious consideration that if an infectious agent is driven to extinction, the incalculable damage to people’s health and the overall economy by a persisting and indefinite disease burden will also be eliminated.
The ambition of local elimination grew into one of global eradication for smallpox, which was successfully eliminated from the human population in the 1970s6 (this had already been achieved locally in the late 19th century by some countries), after a heroic effort to find and contain the last remaining infectious individuals7,8. The other complete success was rinderpest in cattle9,10, globally eradicated in the early 21st century.
When the COVID-19 pandemic started, global eradication programs were very close to succeeding for two other diseases – polio11,12 and dracunculiasis13. Eradication is also globally pursued for other diseases, such as yaws14,15, and regionally for many others, e.g. lymphatic filariasis16,17, onchocerciasis18,19, measles and rubella20-30. The most challenging diseases are those that have an external reservoir outside the human population, especially if they are insect borne, and in particular those carried by mosquitos. Malaria is the primary example, but despite these difficulties, eradication of malaria has been a long-standing global public health goal31-33 and elimination has been achieved in temperate regions of the globe34,35, even though it involved the ecologically destructive widespread application of polluting chemical pesticides36,37 to reduce the populations of the vectors. Elimination is also a public goal for other insect borne diseases such as trypanosomiasis38,39.
In parallel with pursuing maximal reduction and eventual eradication of the burden of existing endemic infectious diseases, humanity has also had to battle novel infectious diseases40, which have been appearing at an increased rate over recent decades41-43. Most of these diseases are of zoonotic origin, and the rate at which they are making the jump from wildlife to humans is accelerating, because of the increased encroachment on wildlife due to expanding human populations and physical infrastructure associated with human activity, the continued destruction of wild ecosystems that forces wild animals towards closer human contact, the booming wildlife trade, and other such trends.
Because it is much easier to stop an outbreak when it is still in its early stages of spreading through the population than to eradicate an endemic pathogen, the governing principle has been that no emerging infectious disease should be allowed to become endemic. This goal has been pursued reasonably successfully and without controversy for many decades.
The most famous newly emerging pathogens were the filoviruses (Ebola44-46, Marburg47,48), the SARS and MERS coronaviruses, and paramyxoviruses like Nipah49,50. These gained fame because of their high lethality and potential for human-to-human spread, but they were merely the most notable of many examples.
Pigs in close proximity to humans. Such epidemics were almost always aggressively suppressed. Usually, these were small outbreaks, and because highly pathogenic viruses such as Ebola cause very serious sickness in practically all infected people, finding and isolating the contagious individuals is a manageable task. The largest such epidemic was the 2013-16 Ebola outbreak in West Africa, when a filovirus spread widely in major urban centers for the first time. Containment required a wartime-level mobilization, but that was nevertheless achieved, even though there were nearly 30,000 infections and more than 11,000 deaths51.
SARS was also contained and eradicated from the human population back in 2003-04, and the same happened every time MERS made the jump from camels to humans, as well as when there were Nipah outbreaks in Asia.
The major counterexample of a successful establishment in the human population of a novel highly pathogenic virus is HIV. HIV is a retrovirus, and as such it integrates into the host genome and is thus nearly impossible to eliminate from the body and to eradicate from the population52 (unless all infected individuals are identified and prevented from infecting others for the rest of their lives). However, HIV is not an example of the containment principle being voluntarily abandoned as the virus had made its zoonotic jump and established itself many decades before its eventual discovery53 and recognition54-56, and long before the molecular tools that could have detected and potentially fully contained it existed.
Still, despite all these containment success stories, the emergence of a new pathogen with pandemic potential was a well understood and frequently discussed threat57-60, although influenza viruses rather than coronaviruses were often seen as the most likely culprit61-65. The eventual appearance of SARS-CoV-2 should therefore not have been a huge surprise, and should have been met with a full mobilization of the technical tools and fundamental public health principles developed over the previous decades.
The ecological context One striking property of many emerging pathogens is how many of them come from bats. While the question of whether bats truly harbor more viruses than other mammals in proportion to their own species diversity (which is the second highest within mammals after rodents) is not fully settled yet66-69, many novel viruses do indeed originate from bats, and the ecological and physiological characteristics of bats are highly relevant for understanding the situation that Homo sapiens finds itself in right now.
Group of bats roosting in a cave. Another startling property of bats and their viruses is how highly pathogenic to humans (and other mammals) many bat viruses are, while bats themselves are not much affected (only rabies is well established to cause serious harm to bats68). Why bats seem to carry so many such pathogens, and how they have adapted so well to coexisting with them, has been a long-standing puzzle and although we do not have a definitive answer, some general trends have become clear.
Bats are the only truly flying mammals and have been so for many millions of years. Flying has resulted in a number of specific adaptations, one of them being the tolerance towards a very high body temperature (often on the order of 42-43ºC). Bats often live in huge colonies, literally touching each other, and, again, have lived in conditions of very high density for millions of years. Such densities are rare among mammals and are certainly not the native condition of humans (human civilization and our large dense cities are a very recent phenomenon on evolutionary time scales). Bats are also quite long-lived for such small mammals70-71 – some fruit bats can live more than 35 years and even small cave dwelling species can live about a decade. These are characteristics that might have on one hand facilitated the evolution of a considerable set of viruses associated with bat populations. In order for a non-latent respiratory virus to maintain itself, a minimal population size is necessary. For example, it is hypothesized that measles requires a minimum population size of 250-300,000 individuals72. And bats have existed in a state of high population densities for a very long time, which might explain the high diversity of viruses that they carry. In addition, the long lifespan of many bat species means that their viruses may have to evolve strategies to overcome adaptive immunity and frequently reinfect previously infected individuals as opposed to the situation in short-lived species in which populations turn over quickly (with immunologically naive individuals replacing the ones that die out).
On the other hand, the selective pressure that these viruses have exerted on bats may have resulted in the evolution of various resistance and/or tolerance mechanisms in bats themselves, which in turn have driven the evolution of counter strategies in their viruses, leading them to be highly virulent for other species. Bats certainly appear to be physiologically more tolerant towards viruses that are otherwise highly virulent to other mammals. Several explanations for this adaptation have been proposed, chief among them a much more powerful innate immunity and a tolerance towards infections that does not lead to the development of the kind of hyperinflammatory reactions observed in humans73-75, the high body temperature of bats in flight, and others.
The notable strength of bat innate immunity is often explained by the constitutively active interferon response that has been reported for some bat species76-78. It is possible that this is not a universal characteristic of all bats79 – only a few species have been studied – but it provides a very attractive mechanism for explaining both how bats prevent the development of severe systemic viral infections in their bodies and how their viruses in turn would have evolved powerful mechanisms to silence the interferon response, making them highly pathogenic for other mammals.
The tolerance towards infection is possibly rooted in the absence of some components of the signaling cascades leading to hyperinflammatory reactions and the dampened activity of others80.
Map of scheduled airline traffic around the world, circa June 2009 Map of scheduled airline traffic around the world. Credit: Jpatokal An obvious ecological parallel can be drawn between bats and humans – just as bats live in dense colonies, so now do modern humans. And we may now be at a critical point in the history of our species, in which our ever-increasing ecological footprint has brought us in close contact with bats in a way that was much rarer in the past. Our population is connected in ways that were previously unimaginable. A novel virus can make the zoonotic jump somewhere in Southeast Asia and a carrier of it can then be on the other side of the globe a mere 24-hours later, having encountered thousands of people in airports and other mass transit systems. As a result, bat pathogens are now being transferred from bat populations to the human population in what might prove to be the second major zoonotic spillover event after the one associated with domestication of livestock and pets a few thousand years ago.
Unfortunately for us, our physiology is not suited to tolerate these new viruses. Bats have adapted to live with them over many millions of years. Humans have not undergone the same kind of adaptation and cannot do so on any timescale that will be of use to those living now, nor to our immediate descendants.
Simply put, humans are not bats, and the continuous existence and improvement of what we now call “civilization” depends on the same basic public health and infectious disease control that saw life expectancy in high-income countries more than double to 85 years. This is a challenge that will only increase in the coming years, because the trends that are accelerating the rate of zoonotic transfer of pathogens are certain to persist.
Given this context, it is as important now to maintain the public health principle that no new dangerous pathogens should be allowed to become endemic and that all novel infectious disease outbreaks must be suppressed as it ever was.
The death of public health and the end of epidemiological comfort It is also in this context that the real gravity of what has happened in the last three years emerges.
After HIV, SARS-CoV-2 is now the second most dangerous infectious disease agent that is 'endemic' to the human population on a global scale. And yet not only was it allowed to become endemic, but mass infection was outright encouraged, including by official public health bodies in numerous countries81-83.
The implications of what has just happened have been missed by most, so let’s spell them out explicitly.
We need to be clear why containment of SARS-CoV-2 was actively sabotaged and eventually abandoned. It has absolutely nothing to do with the “impossibility” of achieving it. In fact, the technical problem of containing even a stealthily spreading virus such as SARS-CoV-2 is fully solved, and that solution was successfully applied in practice for years during the pandemic.
The list of countries that completely snuffed out outbreaks, often multiple times, includes Australia, New Zealand, Singapore, Taiwan, Vietnam, Thailand, Bhutan, Cuba, China, and a few others, with China having successfully contained hundreds of separate outbreaks, before finally giving up in late 2022.
The algorithm for containment is well established – passively break transmission chains through the implementation of nonpharmaceutical interventions (NPIs) such as limiting human contacts, high quality respirator masks, indoor air filtration and ventilation, and others, while aggressively hunting down active remaining transmission chains through traditional contact tracing and isolation methods combined with the powerful new tool of population-scale testing.
Oklahoma’s Strategic National Stockpile. Credit: DVIDS Understanding of airborne transmission and institution of mitigation measures, which have heretofore not been utilized in any country, will facilitate elimination, even with the newer, more transmissible variants. Any country that has the necessary resources (or is provided with them) can achieve full containment within a few months. In fact, currently this would be easier than ever before because of the accumulated widespread multiple recent exposures to the virus in the population suppressing the effective reproduction number (Re). For the last 18 months or so we have been seeing a constant high plateau of cases with undulating waves, but not the major explosions of infections with Re reaching 3-4 that were associated with the original introduction of the virus in 2020 and with the appearance of the first Omicron variants in late 2021.
It would be much easier to use NPIs to drive Re to much below 1 and keep it there until elimination when starting from Re around 1.2-1.3 than when it was over 3, and this moment should be used, before another radically new serotype appears and takes us back to those even more unpleasant situations. This is not a technical problem, but one of political and social will. As long as leadership misunderstands or pretends to misunderstand the link between increased mortality, morbidity and poorer economic performance and the free transmission of SARS-CoV-2, the impetus will be lacking to take the necessary steps to contain this damaging virus.
Political will is in short supply because powerful economic and corporate interests have been pushing policymakers to let the virus spread largely unchecked through the population since the very beginning of the pandemic. The reasons are simple. First, NPIs hurt general economic activity, even if only in the short term, resulting in losses on balance sheets. Second, large-scale containment efforts of the kind we only saw briefly in the first few months of the pandemic require substantial governmental support for all the people who need to pause their economic activity for the duration of effort. Such an effort also requires large-scale financial investment in, for example, contact tracing and mass testing infrastructure and providing high-quality masks. In an era dominated by laissez-faire economic dogma, this level of state investment and organization would have set too many unacceptable precedents, so in many jurisdictions it was fiercely resisted, regardless of the consequences for humanity and the economy.
None of these social and economic predicaments have been resolved. The unofficial alliance between big business and dangerous pathogens that was forged in early 2020 has emerged victorious and greatly strengthened from its battle against public health, and is poised to steamroll whatever meager opposition remains for the remainder of this, and future pandemics.
The long-established principles governing how we respond to new infectious diseases have now completely changed – the precedent has been established that dangerous emerging pathogens will no longer be contained, but instead permitted to ‘ease’ into widespread circulation. The intent to “let it rip” in the future is now being openly communicated84. With this change in policy comes uncertainty about acceptable lethality. Just how bad will an infectious disease have to be to convince any government to mobilize a meaningful global public health response?
We have some clues regarding that issue from what happened during the initial appearance of the Omicron “variant” (which was really a new serotype85,86) of SARS-CoV-2. Despite some experts warning that a vaccine-only approach would be doomed to fail, governments gambled everything on it. They were then faced with the brute fact of viral evolution destroying their strategy when a new serotype emerged against which existing vaccines had little effect in terms of blocking transmission. The reaction was not to bring back NPIs but to give up, seemingly regardless of the consequences.
Critically, those consequences were unknown when the policy of no intervention was adopted within days of the appearance of Omicron. All previous new SARS-CoV-2 variants had been deadlier than the original Wuhan strain, with the eventually globally dominant Delta variant perhaps as much as 4× as deadly87. Omicron turned out to be the exception, but again, that was not known with any certainty when it was allowed to run wild through populations. What would have happened if it had followed the same pattern as Delta?
In the USA, for example, the worst COVID-19 wave was the one in the winter of 2020-21, at the peak of which at least 3,500 people were dying daily (the real number was certainly higher because of undercounting due to lack of testing and improper reporting). The first Omicron BA.1 wave saw the second-highest death tolls, with at least 2,800 dying per day at its peak. Had Omicron been as intrinsically lethal as Delta, we could have easily seen a 4-5× higher peak than January 2021, i.e. as many as 12–15,000 people dying a day. Given that we only had real data on Omicron’s intrinsic lethality after the gigantic wave of infections was unleashed onto the population, we have to conclude that 12–15,000 dead a day is now a threshold that will not force the implementation of serious NPIs for the next problematic COVID-19 serotype.
UK National Covid Memorial Wall. Credit: Dominic Alves Logically, it follows that it is also a threshold that will not result in the implementation of NPIs for any other emerging pathogens either. Because why should SARS-CoV-2 be special?
We can only hope that we will never see the day when such an epidemic hits us but experience tells us such optimism is unfounded. The current level of suffering caused by COVID-19 has been completely normalized even though such a thing was unthinkable back in 2019. Populations are largely unaware of the long-term harms the virus is causing to those infected, of the burden on healthcare, increased disability, mortality and reduced life expectancy. Once a few even deadlier outbreaks have been shrugged off by governments worldwide, the baseline of what is considered “acceptable” will just gradually move up and even more unimaginable losses will eventually enter the “acceptable” category. There can be no doubt, from a public health perspective, we are regressing.
We had a second, even more worrying real-life example of what the future holds with the global spread of the MPX virus (formerly known as “monkeypox” and now called “Mpox”) in 2022. MPX is a close relative to the smallpox VARV virus and is endemic to Central and Western Africa, where its natural hosts are mostly various rodent species, but on occasions it infects humans too, with the rate of zoonotic transfer increasing over recent decades88. It has usually been characterized by fairly high mortality – the CFR (Case Fatality Rate) has been ∼3.6% for the strain that circulates in Nigeria and ∼10% for the one in the Congo region, i.e. much worse than SARS-CoV-2. In 2022, an unexpected global MPX outbreak developed, with tens of thousands of confirmed cases in dozens of countries89,90. Normally, this would be a huge cause for alarm, for several reasons.
First, MPX itself is a very dangerous disease. Second, universal smallpox vaccination ended many decades ago with the success of the eradication program, leaving the population born after that completely unprotected. Third, lethality in orthopoxviruses is, in fact, highly variable – VARV itself had a variola major strain, with as much as ∼30% CFR, and a less deadly variola minor variety with CFR ∼1%, and there was considerable variation within variola major too. It also appears that high pathogenicity often evolves from less pathogenic strains through reductive evolution - the loss of certain genes something that can happen fairly easily, may well have happened repeatedly in the past, and may happen again in the future, a scenario that has been repeatedly warned about for decades91,92. For these reasons, it was unthinkable that anyone would just shrug off a massive MPX outbreak – it is already bad enough as it is, but allowing it to become endemic means it can one day evolve towards something functionally equivalent to smallpox in its impact.
Colorized transmission electron micrograph of Mpox virus particles. Credit: NIAID And yet that is exactly what happened in 2022 – barely any measures were taken to contain the outbreak, and countries simply reclassified MPX out of the “high consequence infectious disease” category93 in order to push the problem away, out of sight and out of mind. By chance, it turned out that this particular outbreak did not spark a global pandemic, and it was also characterized, for poorly understood reasons, by an unusually low CFR, with very few people dying94,95. But again, that is not the information that was available at the start of the outbreak, when in a previous, interventionist age of public health, resources would have been mobilized to stamp it out in its infancy, but, in the age of laissez-faire, were not. MPX is now circulating around the world and represents a future threat of uncontrolled transmission resulting in viral adaptation to highly efficient human-to-human spread combined with much greater disease severity.
This is the previously unthinkable future we will live in from now on in terms of our approach to infectious disease.
What may be controlled instead is information. Another lesson of the pandemic is that if there is no testing and reporting of cases and deaths, a huge amount of real human suffering can be very successfully swept under the rug. Early in 2020, such practices – blatant denial that there was any virus in certain territories, outright faking of COVID-19 statistics, and even resorting to NPIs out of sheer desperation but under false pretense that it is not because of COVID-19 – were the domain of failed states and less developed dictatorships. But in 2023 most of the world has adopted such practices – testing is limited, reporting is infrequent, or even abandoned altogether – and there is no reason to expect this to change. Information control has replaced infection control.
After a while it will not even be possible to assess the impact of what is happening by evaluating excess mortality, which has been the one true measure not susceptible to various data manipulation tricks. As we get increasingly removed from the pre-COVID-19 baselines and the initial pandemic years are subsumed into the baseline for calculating excess mortality, excess deaths will simply disappear by the power of statistical magic. Interestingly, countries such as the UK, which has already incorporated two pandemic years in its five-year average, are still seeing excess deaths, which suggests the virus is an ongoing and growing problem.
It should also be stressed that this radical shift in our approach to emerging infectious diseases is probably only the beginning of wiping out the hard-fought public health gains of the last 150+ years. This should be gravely concerning to any individuals and institutions concerned with workers and citizens rights.
This shift is likely to impact existing eradication and elimination efforts. Will the final pushes be made to complete the various global eradication campaigns listed above? That may necessitate some serious effort involving NPIs and active public health measures, but how much appetite is there for such things after they have been now taken out of the toolkit for SARS-CoV-2?
We can also expect previously forgotten diseases to return where they have successfully been locally eradicated. We have to always remember that the diseases that we now control with universal childhood vaccinations have not been globally eradicated – they have disappeared from our lives because vaccination rates are high enough to maintain society as a whole above the disease elimination threshold, but were vaccination rates to slip, those diseases, such as measles, will return with a vengeance.
The anti-vaccine movement was already a serious problem prior to COVID-19, but it was given a gigantic boost with the ill-advised vaccine-only COVID-19 strategy. Governments and their nominal expert advisers oversold the effectiveness of imperfect first generation COVID-vaccines, and simultaneously minimized the harms of SARS-CoV-2, creating a reality gap which gave anti-vaccine rhetoric space to thrive. This is a huge topic to be explored separately. Here it will suffice to say that while anti-vaxxers were a fringe movement prior to the pandemic, “vaccination” in general is now a toxic idea in the minds of truly significant portions of the population. A logical consequence of that shift has been a significant decrease in vaccination coverage for other diseases as well as for COVID-19.
This is even more likely given the shift in attitudes towards children. Child labour, lack of education and large families were the hallmarks of earlier eras of poor public health, which were characterized by high birth-rates and high infant mortality. Attitudes changed dramatically over the course of the 20th century and wherever health and wealth increased, child mortality fell, and the transition was made to small families. Rarity increased perceived value and children’s wellbeing became a central concern for parents and carers. The arrival of COVID-19 changed that, with some governments, advisers, advocacy groups and parents insisting that children should be exposed freely to a Severe Acute Respiratory Syndrome virus to ‘train’ their immune systems.
Infection, rather than vaccination, was the preferred route for many in public health in 2020, and still is in 2023, despite all that is known about this virus’s propensity to cause damage to all internal organs, the immune system, and the brain, and the unknowns of postinfectious sequelae. This is especially egregious in infants, whose naive immune status may be one of the reasons they have a relatively high hospitalization rate. Some commentators seek to justify the lack of protection for the elderly and vulnerable on a cost basis. We wonder what rationale can justify a lack of protection for newborns and infants, particularly in a healthcare setting, when experience of other viruses tells us children have better outcomes the later they are exposed to disease? If we are not prepared to protect children against a highly virulent SARS virus, why should we protect against others? We should expect a shift in public health attitudes, since ‘endemicity’ means there is no reason to see SARS-CoV-2 as something unique and exceptional.
We can also expect a general degradation of workplace safety protocols and standards, again reversing many decades of hard-fought gains. During COVID-19, aside from a few privileged groups who worked from home, people were herded back into their workplaces without minimal safety precautions such as providing respirators, and improving ventilation and indoor air quality, when a dangerous airborne pathogen was spreading.
Can we realistically expect existing safety precautions and regulations to survive after that precedent has been set? Can we expect public health bodies and regulatory agencies, whose job it is to enforce these standards, to fight for workplace safety given what they did during the pandemic? It is highly doubtful. After all, they stubbornly refused to admit that SARS-CoV-2 is airborne (even to this very day in fact – the World Health Organization’s infamous “FACT: #COVID19 is NOT airborne” Tweet from March 28 2020 is still up in its original form), and it is not hard to see why – implementing airborne precautions in workplaces, schools, and other public spaces would have resulted in a cost to employers and governments; a cost they could avoid if they simply denied they needed to take such precautions. But short-term thinking has resulted in long-term costs to those same organizations, through the staffing crisis, and the still-rising disability tsunami. The same principle applies to all other existing safety measures.
Worse, we have now entered the phase of abandoning respiratory precautions even in hospitals. The natural consequence of unmasked staff and patients, even those known to be SARS-CoV-2 positive, freely mixing in overcrowded hospitals is the rampant spread of hospital-acquired infections, often among some of the most vulnerable demographics. This was previously thought to be a bad thing. And what of the future? If nobody is taking any measures to stop one particular highly dangerous nosocomial infection, why would anyone care about all the others, which are often no easier to prevent? And if standards of care have slipped to such a low point with respect to COVID-19, why would anyone bother providing the best care possible for other conditions? This is a one-way feed-forward healthcare system degradation that will only continue.
Finally, the very intellectual foundations of the achievements of the last century and a half are eroding. Chief among these is the germ theory of infectious disease, by which transmission chains can be isolated and broken. The alternative theory, of spontaneous generation of pathogens, means there are no chains to be broken. Today, we are told that it is impossible to contain SARS-CoV-2 and we have to "just live with it,” as if germ theory no longer holds. The argument that the spread of SARS-CoV-2 to wildlife means that containment is impossible illustrates these contradictions further – SARS-CoV-2 came from wildlife, as did all other zoonotic infections, so how does the virus spilling back to wildlife change anything in terms of public health protocol? But if one has decided that from here on there will be no effort to break transmission chains because it is too costly for the privileged few in society, then excuses for that laissez-faire attitude will always be found.
And that does not bode well for the near- and medium-term future of the human species on planet Earth.
(Follow the link for more than 100 references and sources)
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator
153 notes
·
View notes
Text
writing fictional Wikipedia articles as outlines for my historical fiction characters and having so much fun. dude look at this:
Daniel Ivey Clairville (3 May 1856 - 5 December 1941) was a prominent figure in the field of animal husbandry, early adopter of germ theory, animal behaviorist, cattle drover, diarist and Quaker theologian. Born in Philadelphia, Clairville apprenticed as a farrier until the death of his father in 1871 caused him to relocate to Texas to seek employment along the Chisholm Trail. Clairville was known for his ability to slow and halt the spread of disease among cattle using sanitation methods he pioneered, reducing cattle loss by up to 60% in herds under his care.
After retiring from the cattle industry in the late 1890s, he attended Cornell University, becoming an adjunct professor at Elgin Polytechnic Institute and publishing several texts on bovine husbandry and behavior.
Clairville was a relatively obscure scientific figure before his private writings about his sexuality, faith and experiences in the waning days of the Wild West were published posthumously.
^ Personal life
Clairville was gay and in a committed relationship with Joseph “Shortie” Alcott (14 November 1860 - 17 July 1906) until the latter’s mysterious death in Texas. Alcott was a train robber, outlaw, gambler, duelist and suspected serial killer. The couple met in the mid-1880s after Alcott was released from Utah Territorial Penitentiary and joined a trail drive lead by Clairville. Their relationship was described as inseparable but contentious by John Matthew Robertson-Clairville, Clairville’s adopted son, who often wrote about the couple’s relationship in his trail diary.
Having worked side by side for over a decade, Alcott initially followed Clairville east when he retired from the cattle industry in the 1890s but became embroiled in legal trouble in Pennsylvania and returned to Texas where he embarked on a crime spree that ended in a fatal two day shootout with a number of Texas rangers.
The details of Clairville’s private life and his connection to notorious criminal Shortie Alcott were largely forgotten until the 1970s when a box of personal letters and diaries was discovered in the attic of his former residence. The diaries of Clairville and Robertson-Clairville along with the correspondence between Clairville and Alcott in the latter’s final months form the basis of the book published by his great granddaughter in 1996.
Analysis of his writings and first hand accounts of his behavior suggest he had autism and OCD.
127 notes
·
View notes
Text
I often wonder what the actual state of medicine as a field is in dragonfable. We see that Magus Neron has a microscope, petri dishes, and hypodermic syringes. We know that the existence of cells is a known thing. Clearly we're not living in a pre-germ theory equivalent. But we also don't really see doctors around- alchemists like Alina seem to be the pick. Sir Junn is the only example I can really think of, and he also seems to be oriented towards alchemical solutions like the royal honey and corruption-cleansing potions, though we do have mentions of him using IVs in an ICU in his field hospital.
Healing potions would certainly be good for physical injuries, but I wonder at how well they treat illnesses and diseases. Are they a cure-all that's become so heavily relied on that, in the rare cases they don't work, nobody knows what else to do? Riadne's arachnomancy healing, delivering potions directly into the bloodstream, is treated as revolutionary, so I assume that pills or IV drips and infusions have not been popularized enough to be commonly used. Is that because potions as they currently exist are good enough for most applications, or because most people don't know how to use them, or because they're difficult to create or get ahold of? There are incredible technologies out there, as evidenced by the magisterium's drones and the gnomes'... everything. But whether or not these advances have ever been applied to medical applications has also never really been shown.
We've seen many examples of healing magic in lore, but the capabilities and limitations of it, as well as the actual process, are never really explored. Is it an actual active process of changing the body, or is it just empowering the natural healing process? We know that fleshweaving is a thing, but forbidden as an art due to its potential for abuse (and the fact that it apparently requires consuming elemental spirits), and Jaania's soulweaving-based healing of Brittany was a method she apparently invented through experimentation. So we can conclude that soul/fleshweaving are not being employed as a tool for medicine, and any commonly used healing magic probably doesn't modify the body in such a way.
There's lots of potential for medical technology and practice to improve, so one has to wonder what factors are at play to ensure they don't. Is it just reliance on the magic that already exists, leaving the people with rare cases to be untreated? I wonder if, to a degree, there's a perception of standard alchemy being "good enough" that medicine doesn't need to be improved. Perhaps that's compounded with some cultural taboos around "messing with" or manipulating the body, which may extend beyond magical practice into the scientific sphere. It could even be an acceptance of a flawed paradigm surrounding healing magic, just like how most mages accepted the leyline model of mana as absolute, when soulthreads demonstrate that it's flawed?
Or maybe the devs intended it all to remain in the mcguffin realm, where healing magic does everything you want when it's convenient and is limited only when necessary. But that's less fun to think about.
#I <3 watsonian analysis of lore gaps and plot holes#late nights with ali#ali plays ae#dragonfable#also when researching lore abt this I was reading the Study of Forbidden Magicks from Azaveyr and#it's so funny to me how some of them are just. Jaania. Chamber of Elbaba is just what she did to Theano. Fool's Sacrifice was her Big Plan.#jaania reading it in the spark of the soul like 'oh jeez that's me'#long post
35 notes
·
View notes
Text
nosferatu posting about dr sievers because i like medical history. will probably revisit this when its not 2:30 am and make it make more sense and sound better.
in the 1830s, the medical field was undergoing a period of transition, still grounded in early modern practices while slowly incorporating more empirical, scientific methods. many old medical concepts and treatments, like humoral theory, continued to dominate. bloodletting, leeches, and herbal remedies were still widely used, and physicians operated with a limited understanding of disease transmission and pathology.
during this time, new scientific theories, such as germ theory and advances in anatomy and physiology, began to reshape medical practice. however, the shift toward a more empirical, evidence-based approach was gradual and met with resistance. this tension between old and new was particularly evident in the treatment of mental and physical health, where the lingering belief in supernatural or irrational causes of illness clashed with emerging medical theories.
dr. sievers, as a character, can be seen as a representation of this "modern" approach to medicine. his practices reflect the struggle between the scientific advancements of the time and the deeply entrenched superstitions about disease and health. his treatment of patients, particularly herr knock, highlights the evolving philosophy of 19th-century medicine. in contrast to traditional, authoritative methods, sievers' calm demeanor and use of reassuring language when dealing with knock demonstrate his belief in the power of bedside manner—a concept that was gaining prominence in the medical community. this shift in treatment philosophy, which emphasized compassion and psychological care, signaled an early move away from brute force and authoritarianism in medicine.
however, despite sievers' attempts to modernize, his approach to ellen’s treatment reveals the limitations of his progressive outlook, particularly in relation to patriarchal views of women. while medical knowledge was advancing, social and cultural norms about gender remained firmly entrenched in patriarchal structures. women's medical care was often shaped by deeply gendered assumptions that framed their emotional or mental distress as a result of inherent weakness or instability. sievers, despite his rational and scientific approach in other areas, remains influenced by these traditional, paternalistic attitudes toward women.
sievers' suggestion to "tie ellen to the bed" reveals his reliance on outdated and oppressive methods for dealing with a woman's emotional or psychological distress. this recommendation isn’t based on a genuine understanding of ellen’s situation but rather reflects a dismissive, paternalistic attitude that undermines her autonomy. this kind of physical restraint was all too common in 19th-century medical practice, particularly for women. in a time when women’s mental health was frequently misunderstood and dismissed, restraint was often used as a simple, albeit cruel, solution to their problems. unfortunately, this practice still persists today in certain mental health care settings, where forced restraint continues to be used as a method of control.
despite his scientific mindset, sievers does not challenge the patriarchal frameworks that dominate his view of women’s health. his suggestion to physically restrain ellen reflects the pervasive belief that women’s bodies, emotions, and decisions were something to be controlled rather than understood. his solution to her distress diminishes her agency and objectifies her, reinforcing the idea that women’s autonomy can be disregarded for the sake of medical authority. in sievers' mind, this is a rational approach, yet it is informed by the same gendered power structures.
furthermore, sievers' failure to understand the violation of ellen’s body and spirit—particularly in her relationship with orlok—reveals his ignorance of the more insidious forms of harm women often face, especially within the domestic sphere. freud’s later work, despite its controversial aspects, shed light on the prevalence of domestic violence in middle-class households, a reality that was met with disbelief by much of the medical community at the time. sievers' rational scientific approach allows him to address physical and psychological symptoms, but he is blind to the deeper trauma that women, particularly those trapped in patriarchal structures, endure. he fails to recognize how exploitation and gendered violence impact ellen’s well-being, as he cannot connect her suffering to larger societal issues of oppression.
this dynamic makes me think of michel foucault's analysis of power and discipline in Discipline and Punish (1975), where he discusses how medical and institutional systems serve to regulate bodies, especially those of women, through mechanisms of control and surveillance. sievers' treatment of ellen fits within this framework—his suggestion of physical restraint is not just a medical intervention, but an act of control, one that reflects the larger societal impulse to regulate and discipline women’s bodies and minds under the guise of care and healing. it also brings to mind helen longino's work Science as Social Knowledge which emphasizes how scientific practices, including medicine, are shaped by social and cultural assumptions, like those regarding gender. sievers' treatment of ellen reflects these assumptions, as his scientific approach remains entangled with patriarchal beliefs that undermine women's autonomy and dismiss their personal experiences.
in this sense, dr. sievers embodies the tension between the progressive ideals of the medical profession and the limitations of those ideals when it comes to gender. while he strives to apply reason and empathy in his medical practice, his treatment of ellen exposes how even in an era of medical advancement, the treatment of women—both in the domestic sphere and within the realm of mental health—was still heavily influenced by outdated and oppressive gender norms. these patriarchal assumptions ultimately undermine sievers' otherwise progressive approach, highlighting the deep-seated gender inequalities that continued to shape medicine well into the 19th century.
3 notes
·
View notes
Text
▪️The history of fasting spans hundreds of thousands of years, and it is deeply intertwined with the story of life on Earth. A closer look into fasting’s expansive timeline clearly shows that it was, and remains, a powerful tool for the survival, health, and wellness of our species.
The origins of fasting.
Fasting is an ability shared by virtually all animals; the animal kingdom is full of prolific fasters, including reptiles, penguins, bears, and seals, who can abstain from food for months at a time. Bears, for example, perform remarkable feats during hibernation, like achieving a heart-rate reduction of around 80% and a metabolic-rate reduction of 67% from the fed state. Additionally, alternate-day fasting and time-restricted feeding protocols have been shown to improve lifespan and metabolic-health markers in a variety of organisms, including yeast, worms, mice, rats, and, of course, humans.
Fasting physiology is built into the survival of our species. Prior to the agricultural revolution around 10,000 BC, food was not readily available, and even dangerous to procure. As such, early humans had to adapt to long stretches of time without eating — a sort of involuntary, but essential, form of fasting. Each individual hominid that made it to adulthood probably experienced involuntary fasts for days or weeks with some regularity.
Evidence suggests that, when there were much more distinct feeding-fasting cycles and greater physical activity levels, that people survived, and perhaps even thrived. Reliable, constant access to food is an incredibly new development if you consider the scope and timeline throughout all of human history. According to the thrifty-gene hypothesis, round-the-clock access to food may be contributing to contemporary obesity and metabolic-health challenges.
Ancient and religious fasting.
People of nearly every culture have participated in purposeful fasting for spiritual or health reasons. Nearly every major religion developed their own fasting rituals to support the spiritual development of their members. Ancient fasting practices first emerged around 1,500 BC with the Vedic, Hindu, and Jainism religions. Fasting on designated holy days was a common practice to reduce the burden and harm that harvesting and eating caused for both animals and plants.
The founder of Buddhism, Siddhartha Gautama, also fasted in an effort to achieve enlightenment, or nirvana. Fasting for religious reasons was also prevalent in other parts of the ancient world, including India, China, the Middle East, and Greece.
Fasting and early medicine.
There is a rich history of leveraging fasting as a natural and easily accessible tool to combat illness and disease. Prior to the advent of the scientific method and germ theory, early medicine was usually more detrimental than the illness or ailment it was trying to treat.
One notable example of this can be found in the records of George Washington’s treatment for what began as an acute sore throat one evening and progressed to shortness of breath by morning. While some controversy remains around his death, the physicians that were called to treat the first U.S. president attempted bloodletting and drained 82 ounces of his blood, or around 50% of his total blood volume.
In contrast, fasting as a form of early medicine was non-invasive and had far fewer adverse effects. It was also a surprisingly effective treatment for an array of conditions, ranging from acute infection to allergies, as well as many diseases known to be resistant to treatment.
Fasting in the 19th and 20th centuries.
By the 19th and 20th centuries, the science of fasting had been confirmed and duplicated as a treatment for many different maladies. Based on historical record and research data, fasting was used to help treat arthritis, asthma, chronic fatigue, high-blood pressure, lupus, Crohn’s disease, irritable bowel, paralysis, and many other conditions.
Historically, fasting was the primary treatment, and often the cure, for both diabetes and epilepsy. We now know that for diabetes patients, fasting helps regulate blood-glucose and insulin levels. In epilepsy, hyperactive neurons that are easily stimulated can be calmed in part by ketones, which are elevated during fasting. Once it was discovered that the ketogenic diet could mimic the ketone production of fasting without the need for calorie avoidance, many people started to embrace ketogenic-diet therapy in place of fasting.
Similarly, once medications that did not require fasting or dietary restriction became widely available, they started to supplant dietary treatments for many diseases, including diabetes and epilepsy. There are many documented stories of practitioners operating clinics relying on natural remedies, such as fasting, that were burdened by fines and imprisonment. Up until recently, there was hostility towards people who used fasting clinically to treat disease, but thanks to an increasing body of scientific research, intermittent fasting is being recognized more and more as a viable therapeutic and health-maintenance strategy.
A variety of short and extended duration fasting strategies are still used today for general health and healing benefits. Despite the popularity of intermittent fasting and time-restricted feeding for goals like weight loss, fasting continues to produce some controversy. There are only a few fasting-focused clinics that exist today, which supervise therapeutic water-only fasts as well as modified fasts with low calorie intake.
No drugs or pharmacies in my life.
Heal thyself!
2 notes
·
View notes
Text
How to change history with one simple concept
A common fun thought experiment is "If you went back in time, what could you invent or do to change the world?" I think there's a fairly simple one that can save millions of lives, but only became mainstream in the late 1800s: Germ theory.
Germ theory ("theory" is a kind of loose word, we are pretty certain at this point disease is not caused by miasma) is the idea that tiny organisms cause disease. Viruses, fungi, bacteria, etc. This extends into the logic that by protecting yourself against these, you are protecting yourself from disease. This can be as simple as washing your hands to stay clean.
Germ theory has been bandied about since the 1500s, but was thought ridiculous when 'miasma' was the common line of thinking. Miasma (Greek for 'pollution') would be a toxic mist associated with foul smells. It's why your plague doctor mask had the beak, it's stuff with strong-smelling herbs to keep out the bad disease-causing smells.
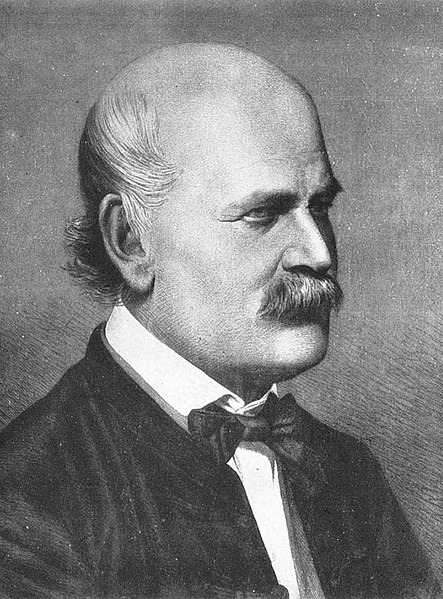
Lots of people got close to germ theory, but I want to focus on the strangest story of Ignaz Semmelweis, who really should be more of a household name for what he started. In 1846, Semmelweis was an Austrian obstetrician who noticed that out of the two clinics of his Viennese hospital, the one staffed by doctors instead of midwives had a 10x higher mortality rate.
This is the start of the scientific method: Make an observation, form a hypothesis (Another idea that seems obvious today but would be groundbreaking in ye olde times). Semmelweis found that the doctors' clinic had a morgue, and often doctors would go straight from an autopsy to delivering a child without washing their hands.
Semmelweis instituted a policy of hand-washing before examining a patient, and mortality dropped 90%! For this earth-shattering success, Semmelweis was essentially ostracized by the medical community, Doctors were gentlemen whose hands are clean because they are doctors, of course. You could also read into the rejection of hand-washing as a refusal by doctors to accept guilt for how many deaths they had unwittingly caused.
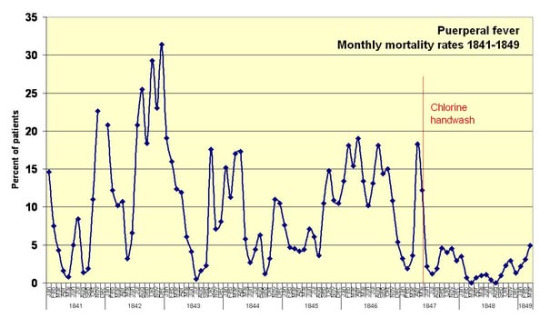
Semmelweis continued to campaign for hand washing, and was forced to leave Vienna. His family had him sent to an insane asylum to fix his single-minded obsession with medical sanitation. There, he was beaten by guards and died of an infection. At this point I'd like to write something about the importance of bravery and doing the right thing, but man. What a downer ending. Louis Pasteur and others picked up on Semmelweis's advances decades later, and now we better understand how infections happen.
1 note
·
View note
Text
The History and Evolution of Disinfection Sprays
The idea of disinfecting is thousands of years old. In old times, Egyptians utilised palm wine and vinegar for cleansing wounds and keeping bodies intact. But, the spray form of disinfection as we understand it now appeared very later for sure. Early human societies noticed that some materials could stop rotting and sickness, but they did not have the scientific knowledge to make specific mixes for these purposes.

The Scientific Revolution
During the 19th century, there was a significant change because of Louis Pasteur's germ theory and Joseph Lister's antiseptic methods. These findings created the base for creating modern Disinfection Sprays. By 1900, they were using phenol (carbolic acid) solutions, which were sprayed by hand in hospitals and houses to fight against diseases. These early versions were far from the convenient products we use today.
The Birth of Commercial Products
At the beginning of the 20th century, it was when commercial disinfection spray products started to be sold. Lysol is an example of a product like this - first introduced in 1889 to help stop a cholera pandemic. It was promoted as an everyday cleaner for homes and also for personal cleanliness purposes. When we reached the period of the 1950s, there were big changes due to aerosol technology, which changed how these disinfectants are delivered, making them easier for normal customers to use and buy.
Modern Formulations
From the 1960s to the 1990s, there was significant progress in the chemistry of disinfection sprays. The makers found substitutes that are not as poisonous as strong phenols and formaldehyde. They used quaternary ammonium compounds or "quats". These were liked because they worked well against many types of disease-causing agents, but did no big harm to surfaces and skin.
Environmental and Health Considerations
In the last few years, people have started to use disinfectant sprays that are good for the environment. Issues like volatile organic compounds (VOCS), problems with breathing and damage to ecology lead us towards innovations. Disinfectants made from plants, hydrogen peroxide formulas, and hypochlorous acid came forward as strong substitutes for old chemical disinfectants.
The Pandemic Effect
The COVID-19 pandemic drastically raised the awareness and need among consumers for efficient disinfection products. In response, producers have created new spray formulas of disinfection tested particularly against enveloped viruses. This time also experienced an uncommon amount of study into methods of disinfection, which resulted in products being more effective, easier to use and safer.
Future Directions
The study we are doing today is on the creation of intelligent disinfection spray methods that give protection for a longer time. New ideas involve surfaces which can disinfect themselves, targeted removal of harmful bacteria without damaging useful ones, and eco-friendly packaging solutions that decrease plastic waste but still keep product effectiveness.
#electric water blaster#karcher#carpet cleaning machine#across the spiderverse#Disinfection Spray#Steam Cleaners#truck wash machine
0 notes
Text
The Snow Globe:
Unmasking the World of Microorganisms (Part 2)
By Arjuwan Lakkdawala
Ink in the Internet
To have a proper understanding of microorganisms we must also understand their vectors, one of the scariest is the air. A disease is most horrifying when it is thought to be airborne. As an emergency resort humans have often turned to masks for immediate protection from danger in the air. So in this article I’m going to explore the scope of the air we breathe, and our defenses against contaminated air.
Usually after a rainfall that beautiful fresh earthy fragrance that spreads in the air. Ever wonder what it is? It’s mainly ozone that comes down to earth with droplets of rain from the stratosphere, which is the second layer of the earth’s atmosphere.
The official term for the fragrance is Petrichor, coined in 1964 by Australian scientists.
Ozone is a molecule that consists of three oxygen atoms.
Some other compounds that contribute to the fragrance are geosmin and plant oils.
The envelope of atmosphere that surrounds earth comprises five layers.
The entire coat of atmosphere around earth weighs about 5.5 quadrillion tons.
1. Troposphere, this is the first and it starts from the surface of earth.
2. Stratosphere
3. Mesosphere
4. Thermosphere
5. Exosphere, this is the last and where satellites orbit earth.
To give it a poetic description we are in a global snow globe. We must care for the purity and cleanliness of the atmosphere because it is the air everyone on earth breathes.

Daily we inhale 12,000 liters of air and exhale carbon dioxide.
What’s in this air has great affect on our overall health. From microorganisms to industrial pollutants like particulate matter (MP) the air circulating the globe carries everything in it all round the planet.
The composition of the air in our atmosphere in its essential form is 78% nitrogen and 21% oxygen, the remaining 1% is trace gases and water vapour.
In our understanding of protection against microorganisms most of us grew up knowing hygiene and disinfectants was the way to go. Masks were things we mainly saw in hospitals worn by surgeons. That was the general idea. It wasn’t until the Covid-19 pandemic that masks were propelled into public scientific debate; about their use in the prevention of the virus spreading. Eventually it became mandatory to wear masks in public.
Before science progressed enough for us to understand how air can get contaminated with industrial pollution or airborne diseases, or before we knew the germ theory. Past civilizations could detect the symptoms when a disease was airborne.
In the 17th century when the Bubonic Plague was wiping out Europe, it was evident that the disease was somehow spreading through the air breathed by the infected.
Side note: What is the Bubonic Plague? It is a disease caused by the bacterium Yersinia pestis. It was spread by the fleas on rodents that got into Europe on ships. If left untreated all three types of the plague caused by the bacterium can be fatal.
1. Bubonic Plague, which causes swelling as large as eggs in the neck, armpits, groin, and blackened skin due to gangrene.
2. Septicemic Plague, in this the infection spreads in the entire body.
3. Pneumonic Plague, when the lungs get infected.
The plague doctor had a costume believed to purify air. The costume was the “personal protection equipment.” It was a robe with a mask that had a long beak, which would be filled with herbs thought to filter the air from the disease; as it passed through the long nozzle, before it was breathed in by the wearer.
Unfortunately it didn’t work.
However, as the dawn of science came upon us. Scientists realized that air could be a very dangerous vector for diseases as there was no way to virtually contain it. So they studied various methods of air purification including wearing masks to filter air.
Masks became notoriously famous during the Covid-19 pandemic. Especially since it took scientists so long to determine if the virus was transmitted through the air.
Making the perfect mask is not easy. It’s complicated.
How effective is the common surgical mask at filtering contaminated air?
If you have a disease which can spread through the air by aerosol respiratory droplets, then masks offer significant reduction in the disease going viral. With a mask on when you cough, talk, or sneeze, most of the respiratory droplets will stay in the mask. The other matter is if you don’t have any disease, how good is the common surgical mask at offering protection? The harsh reality is not much. Because droplets or aerosols in the air can penetrate easily through the gaps in the mask, caused by the asymmetry of the mask’s fitting due to facial geometry.
Research on masks showed that multi-layered masks that had fabric like cotton, instead of straight threads was better at preventing penetration of pollutants, some masks are even designed to use static repulsion to catch pollutants. However, too many layers can make it difficult to breathe. Even the N95 masks offers limited protection.
There are several types of masks that have varying degrees of protection against particulate matter (MP) and germs in the air. But no mask is 100% foolproof.
It isn’t only outdoors air that is of concern. Indoors air could be even more consequential to our health. It is said that most humans spend 90% of their time indoors. There are ongoing studies about how air quality affects cognition during the course of life. The studies suggest that there is cognitive impairment with long term exposure to air pollution. This subject still needs further research.
While not living with germs is not really an option, we can reduce their percentage to prevent the emergence of pathogens. The term for germs found indoors is: ‘Indoors Microbiome.’ Studies have shown that they are mostly from endogenous sources from the human or animal occupants.
Air conditioning and ventilation could contribute to the indoor microbiome. There are different types of air filters that can keep the air indoors clean, and some plants can also contribute to purifying the air from pollutants and volatile organic substances (VOS).
If you have pets avoids plants that are toxic. Always research the plants you would like to keep indoors or outdoors.
The vapor of essential oils from certain herbs has also been studied for it’s effect of disinfecting the indoors air.
“Ability of Essential Oils Vapour to Reduce Numbers of Culturable Aerolised Coronavirus, Bacteria and Fungi." In this study it says essential oils of certain herbs have compounds that can destroy the structure of some types of microorganisms, so that they are ineffective.

The air is denser nearer to the earth’s surface, the atmosphere gets thinner with altitudes. But can germs be found high up in the air? The answer is that some scientists got samples of air from 1,000 meters above the surface of the earth, and found microorganisms in abundance, including pathogens that are a hazard to human health.
Can microorganisms travel the globe on air?
“The journal PNAS published the results of a study showing that hundreds of microorganisms, some of which cause human disease, can survive atmospheric travel of over 2,000 kilometers (1,242 miles).” - El Paìs
Arjuwan Lakkdawala is an author and independent science resesrcher
X/Twitter/Instagram: Spellrainia
Email: [email protected]
Copyright ©️ Arjuwan Lakkdawala 2025
Sources:
El Paìs - Pathogenic microbes can travel thousands of miles through the atmosphere, daniel mediavilla
National Library of Medicine - Ability of Essential Oil Vapours to Reduce Numbers of Culturable Aerosolised Coronavirus, Bacteria and Fungi, Parthasarathi Kalaiselvan 1, Muhammad Yasir 1, Rajesh Kuppusamy 1, Mark Willcox 1,*, Ajay Kumar Vijay 1
Editors: Carla Sabia1, Ramona Iseppi1
Author information
Article notes
Copyright and License information
PMCID: PMC8944824 PMID: 35326856
Royal Society of Chemistry - Effectiveness of wearing face masks against traffic particles on the streets of Ho Chi Minh City, Vietnam†
Erik Velasco *a, Hoang Hieu Ha b, Anh Duc Pham c and Soheil Rastan
National Library of Medicine - Air pollution and respiratory infections: the past, present, and future
Alexys Monoson 1, Evangeline Schott 2, Kerry Ard 3, Brita Kilburg-Basnyat 4, Robert M Tighe 5, Sonal Pannu 6, Kymberly M Gowdy 7,✉
Author information
Article notes
Copyright and License information
PMCID: PMC10025881 PMID: 36622042
EPA - Indoor Air Quality - What are biological pollutants, how do they affect indoor air quality?
Teqoya - What's in the Air We Breathe? Exploring the Overlooked 1% of Air Composition
NOAA - Layers of the Atmosphere
Phys Org - Researchers find live fungi, bacteria and viruses high in the Earth's atmosphere
by Bob Yirka , Phys.org
Sanalife - The Impact of Indoor Air Quality on Cognitive Function
ACS.org - Petrichor - The Smell of Rain
EPA - Basic Ozone Layer Science
National Geographic - Ozone Layer
Cleveland Clinic - Bubonic Plague
Nesw Medical - Does air pollution reduce cognitive function over time?, by Dr. Liji Thomas, MD, reviewed by benedette cuffari, m,sc,
EPA - Particulate Matter (PM) Basics
National Library of Medicine - Int J Environ Res Public Health
. 2022 Jan 27;19(3):1405. doi: 10.3390/ijerph19031405
Air Pollution and Cognitive Impairment across the Life Course in Humans: A Systematic Review with Specific Focus on Income Level of Study Area
Mina Chandra 1,*, Chandra Bhushan Rai 1, Neelam Kumari 1, Vipindeep Kaur Sandhu 1, Kalpana Chandra 2, Murali Krishna 3, Sri Harsha Kota 4, Kuljeet Singh Anand 5, Anna Oudin 6,7
Editors: Palestini Paola, Paul B Tchounwou
Author information
Article notes
Copyright and License information
PMCID: PMC8835599 PMID: 35162428
Britannica - How Much Does Earth’s Atmosphere Weigh?
Written and fact-checked by the editors of Encyclopaedia Britannica
#arjuwan lakkdawala#science#ink in the internet#biology#nature#viruses#bioengineering#atmosphere#stratosphere#masks#microorganisms
1 note
·
View note
Text
A jeremiad is a literary form named for the prophet Jeremiah and the text, attributed to him, which appears both in the Torah and in most Christian Old Testaments. In its lower-case form in English the word means "a list of gripes or complaints" but more correctly means "a list of society's woes, esp. as just punishment for today's moral failings."
The book's authorship is pinned down by historians as about 2,500 years ago. The form is named because, throughout those intervening 2,500 years, authors since Jeremiah have used the template. The author is typically older than the average member of society, and given prominence for his age and wisdom, which is why jeremiads are published widely, taken seriously, and preserved in the historical record. They all take basically the same form: "Society is collapsing! Kids these days don't respect their elders! Shameful habits are ruining the youths."
Nonetheless, the intervening 2,500 years -- where the drumbeat of each jeremiad has been basically "the whole world is going to hell, it's almost certain this is the last generation that will amount to anything, etc." -- the intervening 2,500 years have produced a string of remarkably lucky breaks from the pattern, including, in no particular order:
The scientific method
Surfing
Movable type & nearly worldwide literacy
The republic and electoral democracy
The concept of individual liberty
Lace-topped thigh high stockings
Indoor plumbing
Microbiology
Jazz
Anime
Computers
The internet
Blue jeans
Lasagna
Stable currency markets
Germ theory, vaccines
Heavier-than-air flight (incl. crewed rocketry and spaceflight)
Electricity (incl. generation by steam, solar, nuclear, etc.)
So, broadly speaking, if you have to bet money for or against a given jeremiad... I'm not saying the author is wrong, but I am saying that if their perspective is accurate, they'd be more or less the first one in 2,500 years to be correct.
W.K. Haselden in the Daily Mirror, October 3, 1935
17K notes
·
View notes
Text
¶ … deaths in childbirth were a major problem for the medical community (Ey). The most significant cause for the large number of women dying during this process was the occurrence of puerperal sepsis which was more commonly known as childbed fever. A variety of theories were offered to explain this phenomena but some dated theories surrounding the causes of diseases such as malaria and typhoid made progress toward reaching a cure for childbed fever more difficult. The prevailing thought was that both diseases were caused through contact with water and this fact, added to the lack of indoor plumbing, caused doubt to be raised when Hungarian born Ignaz Phillip Semmelweis first suggested his germ theory and its relationship to childbed fever. Semmelweis, before Lister introduced his germ killing theory, began insisting that the failure to properly wash one's hands between procedures was the cause of infections and, therefore, the reason why childbed fever was such a prominent problem among maternity wards throughout Europe. Semmelweis developed his initial theory by observing the differences between how physicians in the hospitals administered to pregnant mothers and how midwifes were caring for their patients. The difference, Semmelweis theorized was in the hand washing- physicians did not include it as part of their procedure while midwifes did. Subsequently, Semmelweis insisted upon proper hand washing between procedures in the hospitals where he was the supervisor and he began to test his theories. He publishes his findings in 1861 but his publication is not well received. It is not until Lister eventually publishes the results of his own work in 1870, A Method of Antiseptic Treatment Applicable to Wounded Soldiers in the Present War, that germ theory began to be widely accepted. Lister, however, gives credit to Semmelweis for providing the inspiration for his work. The beauty of Semmelweis' theory was it simplicity. Today the procedures that he was recommending are considered a routine part of any medical procedure but in his generation the suggestion that physicians could be the source of spreading infection was looked upon with disdain (Biddle). As a result, Semmelweis' theory was largely ignored and criticized. Nevertheless, in the institutions where Semmelweis practiced his hand and instrument washing procedures were followed religiously and resulted in significantly fewer cases of childbed fever. Interestingly, despite the remarkable success of his methods, Semmelweis continued to be subject to criticism and, unfortunately, he did not react well to such criticism. He eventually fell into a deep depression and died in an asylum at the early age of 47. The controversy surrounding germ theory and the considerable problem brought about by childbed fever demonstrates how difficult it often is to bring about change in institutions like the practice of medicine. Although the mechanism for examining the relationship between germs and infection had been available for several hundred years since the invention of the compound microscope, physicians in the 19th century refused to believe that their procedures could have any relationship to the fact that women were dying in childbirth. It was only through the isolated efforts of physicians such as Oliver Wendell Holmes in the United States and Semmelweis in Austria and Hungary, and the scientific work of Joseph Lister and Louis Pasteur that the medical community as a whole began to recognize that the germ -- streptococcus -- was the cause of such widespread problems (Cork). It took even longer for physicians to recognize that the problem could be eradicated through the adoption of a simple procedure such as hand washing. The universal acceptance of germ theory did not occur until the early years of the 20th century but its acceptance had a remarkable effect on the incidences of childbed fever throughout Europe and the United States. Instead of double digit percentages of women dying from childbirth, the numbers began to fall to percentages in the range of 2-3% as hand washing and instrument sterilization became a routine part of all deliveries. The efforts and observation skills of Semmelweis contributed significantly to stemming a serious problem. His simple insistence that physicians and other personnel assisting in the birth procedure in one Vienna Hospital follow his hand washing procedure stemmed an epidemic. The use of his procedure reduced the cases of fatal childbed fever from 18% of all births to 3% (Raju). Remarkably, this reduction occurred almost instantly, yet, the acceptance of his methods was still not accepted by the medical community. Semmelweis' contributions to the study of medicine in general and to the practice of obstetrics, in particular, have been largely minimized but his procedures and theory, nevertheless, curtailed a major epidemic (Carter). Although childbed fever was a significant problem throughout most of Europe in the mid-19th century, Semmelweis' efforts brought the problem under control. Semmelweis' efforts demonstrate the importance of simple observation and the importance of being willing to put aside prior prejudices and beliefs. Despite the success of Semmelweis' procedures and their simplistic application, they were not met with acceptance outside his small sphere of influence and, as a result, childbed fever continued to be a serious problem for many years after Semmelweis' introduction of his theory and protocols. In the end, Semmelweis' efforts and the criticism that he received despite his successes demonstrate that mainstream acceptance does not equate with clinical correctness. The procedures suggested by Semmelweis were introduced nearly fifty years prior to their universal acceptance and, as a result, thousands of women died needlessly as the medical community refused to put aside its archaic beliefs for Semmelweis' enlightened and well-studied approach. Works Cited Biddle, C. "Semmelweis revisited: hand hygiene and nosocomial disease transmission in the anesthesia workstation." AANA Journal (2009): 229-237. https://www.paperdue.com/customer/paper/childbed-fever-45284#:~:text=Logout-,ChildbedFever,-Length3pages Carter, K. Codell. Childbed Fever: A Scientific Biography of Igna Semmelweis (Revised Edition). Piscataway, NJ: Transaction Publishers, 2005. Cork, D.P. "Remembering Semmelweis: hand hygiene and its importance on today's clinical practice." American Surgeon (2011): 123-125. Ey, Bridson. "Iatrogenic epidemics of puerperal fever in the 18th and 19th centuries." British Journal of Biomedical Science (1996): 134-139. Raju, T.N. "Ignac Semmelweis and the etiology of fetal and neonatal sepsis." Journal of Perinatology (1999): 307-310. Childbed Fever Read the full article
0 notes
Text
Am I Old Yet?
At what precise point in this inexorable march toward the proverbial hilltop—nay, over it—should I commence my descent into the quagmire of sanctimonious moral posturing, sycophantic obeisance to unbridled capitalist avarice, and enthusiastic endorsement of reactionary xenophobic demagogues? Is there a designated age at which one must willfully abandon reason and embrace the comforting embrace of supernatural absurdities, reject the rigor of the scientific method, and conveniently erase from memory the inconvenient truths of causality, germ theory, and, indeed, the entire sordid chronicle of human history? Or is this transformation into a caricature of cognitive dissonance something that arrives unbidden, like a creeping malaise, suffused with the rank odor of intellectual decay?
Exhaustion scarcely begins to describe my growing disdain for the perpetually senile and inexcusably obtuse Homo alopecius stultus—and by that, I mean humans, bald greater primates who insult the evolutionary marvel that brought them here. Yes, primates—not monkeys, not chimps, nor orangutans, but humans, like you and I, who might as well be as uncivilized and primitive as their evolutionary brethren. Though I say this with the full expectation that most among them will fail to grasp even the meaning of their own Latinate epithet, let alone the depths of the condescension it conveys.

#am i a boomer yet#the elderly be like#midlife resurgence#tired of this shit#pedantry#condescending#sardonic#cynical#rant#funny rant#im old now#over 45#gen x#the critical skeptic#atheism#scientific method#dont forget history#sarcasm
0 notes
Text
Bloodletting Through the Ages: Unveiling the Fascinating History of Phlebotomy
# Bloodletting Through the Ages: Unveiling the Fascinating History of Phlebotomy
Throughout history, phlebotomy, commonly known as bloodletting, has been a widely practiced medical procedure that has both fascinated and horrified people. From ancient civilizations to modern times, the practice of extracting blood from the body for therapeutic purposes has evolved significantly. In this article, we will delve into the intriguing history of bloodletting, exploring its origins, methods, beliefs, and impact on medicine over the centuries.
## Origins of Bloodletting
The roots of bloodletting can be traced back to ancient civilizations such as Egypt, Greece, and Rome, where it was believed that the body’s health was governed by the balance of bodily fluids or “humors.” The theory of the four humors – blood, phlegm, yellow bile, and black bile – was prominent in ancient medical practices, and an imbalance of these fluids was thought to cause illness.
Bloodletting was seen as a way to restore this balance by removing excess or “bad” blood from the body. The procedure was performed using various tools, including knives, lancets, and leeches, and was often accompanied by rituals or incantations to enhance its healing effects.
## Evolution of Bloodletting Techniques
As medical knowledge advanced, so did the techniques and tools used for bloodletting. In the Middle Ages, barber-surgeons were commonly tasked with performing bloodletting alongside their hair-cutting duties. These practitioners developed specialized tools like fleams and scarificators to make the process more efficient and less painful for patients.
During the Renaissance, bloodletting reached its peak in popularity, with renowned physicians such as Galen and Paracelsus advocating for its therapeutic benefits. However, as the scientific revolution unfolded, the practice of bloodletting came under scrutiny, with critics questioning its effectiveness and safety.
## Decline and Resurgence of Bloodletting
By the 19th century, bloodletting fell out of favor in mainstream medicine, as new discoveries and technologies revolutionized healthcare practices. The development of germ theory and the understanding of the circulatory system debunked many of the traditional beliefs surrounding bloodletting, leading to its gradual decline.
However, bloodletting continued to be practiced in certain cultures and communities, often rooted in ancient traditions or alternative medicine philosophies. In recent years, there has been a resurgence of interest in bloodletting as a complementary therapy for certain conditions, such as hemochromatosis or polycythemia.
## Benefits and Practical Tips
While bloodletting is no longer a common medical practice, it still holds a place in history as a significant aspect of traditional healing methods. Some potential benefits of bloodletting include:
– Reducing excess iron levels in patients with hemochromatosis – Treating high blood pressure in select cases – Improving blood circulation and detoxification
If you are considering bloodletting as a therapeutic option, it is essential to consult with a qualified healthcare professional who can provide guidance and ensure the procedure is conducted safely and effectively.
## Case Studies
One notable case of bloodletting in history is that of George Washington, the first President of the United States. In 1799, Washington fell ill with a throat infection, and his doctors performed bloodletting as a treatment. Unfortunately, the excessive blood loss likely contributed to his untimely death, underscoring the dangers of indiscriminate bloodletting practices.
## Conclusion
The history of bloodletting is a fascinating journey through the evolution of medical practices and beliefs. While modern medicine has largely moved away from this ancient therapy, the legacy of bloodletting lives on in our understanding of the human body and the enduring quest for healing and wellness.
Whether viewed as a relic of the past or a potential treatment modality, bloodletting continues to intrigue and captivate those interested in the intersection of tradition and modern science. As we gain new insights and technologies in the field of healthcare, the practice of phlebotomy remains a testament to the enduring legacy of ancient healing arts.
youtube
https://phlebotomytechnicianschools.org/bloodletting-through-the-ages-unveiling-the-fascinating-history-of-phlebotomy/
0 notes
Text
ON EMPIRICISM: THE VIENNA CIRCLE
Habitual exposure makes things invisible. Fish are unaware of the water they move through, just as we humans typically fail to notice the air around us, unless there is a breeze.
For as long as most of us have been alive, our modern culture’s methods for exploring reality have prioritized mathematical logic and empirical science as the exclusive means to uncover truths about existence. Even spiritual intuitions or faith in a received religion is almost always framed in reference (and sometimes in opposition) to the standards of science. Scientific standards are like the air around us or the water in which fish swim.
Of course, this was not always so. In European culture, it took several centuries of struggle for empirical science and mathematics to push back against received religious “wisdom” about how the universe works. Scientists were often threatened with excommunication or death for promulgating empirical findings that contradicted church teachings (see: Copernicus). Even as empirical science rose in its powers of persuasion and credibility, social fissures developed and violence ensued (see: Darwin).
The cultural shift toward science as the arbiter of truth was not a constant march but rather a fitful, sporadic, and haphazard journey. During the centuries-long transition, it was not uncommon to find people with one foot solidly in each camp. Most notable among them, perhaps, was Sir Isaac Newton himself, discoverer of the laws of gravity and codiscoverer of calculus, who nonetheless produced far more written pages on alchemy than he ever did on mathematics or science.
At some point, though, the balance of power did shift. Science gained ground throughout the nineteenth century, with the advent of the Industrial Revolution. Scientific successes such as germ theory and the electric light bulb were vivid and immediate indicators of its reliability. And with the collapse of the old social orders in the violent chaos and destruction of World War I, momentum picked up speed.
The war had demolished the Austro-Hungarian Empire and reordered political power throughout Europe. Medieval hierarchies (the church and the aristocracy) were giving way to capitalism, communism, socialism, and fascism. Meanwhile, modern art, music, and writing were flourishing. Eventually, a movement coalesced in Vienna, one that would ultimately solidify what was to become our modern perspective.
From his office at Berggasse, Freud paved the way for a radical new understanding of human behavior. Not far away, Gustav Klimt and Egon Schiele were painting, Gustav Mahler and Arnold Schoenberg were composing, and Robert Musil and Stefan Zweig were writing.
Within this emergent hotbed of cultural activity, a diverse group of idealistic thinkers came together to concretize the view that empirical science and mathematical logic, exclusively, should guide our understanding of the world. These philosophers, scientists, mathematicians, logicians, and political and social theorists would later come to be known as the Vienna Circle.
They sought to banish nonscientific insights from what they considered reasonable, modern discourse and to purge philosophy of the more fanciful speculations of prior centuries. They didn’t aspire to perform science themselves but sought to catapult philosophy into the twentieth century; with the aid of modern logic, their aim was to make philosophy as scientific as possible.
The Vienna Circle was first gathered in 1924 by the philosopher Moritz Schlick, the social reformer Otto Neurath, and the mathematician Hans Hahn. Meeting regularly on Thursday evenings in a small lecture hall at the University of Vienna, the group referred to themselves as “logical positivists” and immediately entered into a decade of heated, though largely collegial, debate. What mattered most to them was how to characterize scientific knowledge and how to understand the nature of mathematics. Their fervent mission was to prevent philosophical confusion rooted in unclear language and unverifiable claims. They wished instead to convert philosophy into something “scientific” and set mathematics on complete and consistent foundations. As a corollary to all this, they also sought to banish metaphysics from modern thought.
Metaphysics is a field of philosophical inquiry concerned with questions that cannot be answered through an examination of material existence. Any attempts to understand the nature of life after death or the existence of a soul, for instance, would be a metaphysical speculation, as would efforts to comprehend the nature of gods and goddesses, or of a singular creator God.
Until the modern era, statements about consciousness fell exclusively within the realm of metaphysics. Church doctrines derived from ancient texts or spiritual insights—the only attempts to grapple with consciousness available at the time—were all metaphysical.
To a member of the Vienna Circle struggling to push past medieval modes of thought, anything with the whiff of metaphysics was to be summarily dismissed. If something could not be ascertained by empirical science or mathematical formal logic, it was deemed worthless. Indeed, among this crowd, declaring some statement to be “metaphysics” was to suggest not merely that it was wrong but that it was devoid of any meaning or significance. When debates within the circle grew heated, a declaration of “metaphysics!” by an opposing thinker was the ultimate smackdown.
The Vienna Circle led the way for our modern culture to award science and mathematics exclusive ownership over the truth. And the many successes of empirical science—from the development of antibiotics and vaccines to the exploration of other planets—fully demonstrated the power and importance of scientific methods.
As it turned out, though, while the philosophical vision of the Vienna Circle was idealistic and well-intentioned, it was also naive and destined to fall short.
0 notes
Text
Turning history of science into a comic adventure
New Post has been published on https://thedigitalinsider.com/turning-history-of-science-into-a-comic-adventure/
Turning history of science into a comic adventure


The Covid-19 pandemic taught us how complex the science and management of infectious disease can be, as the public grappled with rapidly evolving science, shifting and contentious policies, and mixed public health messages.
The purpose of scientific communication is to make the complexity of such topics engaging and accessible while also making sure the information conveyed is scientifically accurate. With that goal in mind, one MIT team recently transformed themselves into time-traveling comic book characters, in an effort to convey the fascinating history of infectious disease science.
The multimedia project, “A Paradigm Shift in Infectious Diseases,” follows its creators — and the story’s protagonists — on a journey through scientific history. MIT Associate Professor Lydia Bourouiba and cancer-researcher-turned-graphic-artist Argha Manna travel across the world, leaping from one century to the next to learn about paradigm shifts in science from philosophers of science and to meet scientific luminaries and other scholars as they changed the understanding of infectious diseases and their transmission.
“Our goal with this project was to communicate effectively about the scientific method,” says Bourouiba, director of MIT’s Fluid Dynamics of Disease Transmission Laboratory, part of the Fluids and Health Network; a core faculty member of the Institute for Medical Engineering and Science (IMES); and an associate professor in the departments of Civil and Environmental Engineering and of Mechanical Engineering. “During crises like the Covid-19 pandemic, we saw a lot of confusion and misunderstanding from the public that stemmed, in part, from a lack of knowledge about how science actually evolves.”
The project was exhibited in MIT’s Rotch Library Gallery last month and was the subject of an event at the Hayden Library that explored broader questions about the scientific method and scientific literacy. The authors are currently in talks with publishers to create a comic book from the story, and Bourouiba is teaching a related class, HST.537/1.063/2.25 (Fluids and Diseases), this spring.
The exciting history of infectious disease research
Bourouiba pitched the idea for the exhibit to the MIT Center for Art, Science and Technology (CAST) in 2021 during the Covid-19 pandemic. CAST agreed to fund the project, which also received support from the Department of Civil and Environmental Engineering, IMES, and the MIT Libraries.
“We wanted to use visual art in the form of comics, which allows us to convey multilayered messages, with the two protagonists traveling through time and locations to try to understand the processes that led to the different understandings of infectious diseases and how they are transmitted,” Bourouiba explains.
Like all good science communication, the project tells a story. The comic starts with Bourouiba and Manna discussing how infectious diseases spread. They read about experiments by William F. Wells in the 1930s, focusing on the size of exhaled droplets and how it determines how fast they evaporate. And they learn about the origins of germ theory, which after much pushback and debate, was eventually established by Louis Pasteur and Robert Koch toward the end of the 19th century. Soon, Bourouiba and Manna are transported back in time to come face to face with the subjects of their study. The adventure brings them to ancient Greece, Egypt, Italy, and eventually back to MIT — but in the 1940s — where Harold “Doc” Edgerton conducted pioneering work on stroboscopic photography, which could capture images of moving droplets in previously unprecedented detail.
“Through the adventure of the protagonists in this comics, one learns that the evolution of ideas on infectious diseases is far from solely a school of medicine effort,” Bourouiba says. “Instead, it involved, from its start, physicists, ecologists, engineers, and modelers, in addition to those managing public good, eventually establishing public health structures.”
Through it all, the audience learns about various “paradigm shifts” in science that mark progress and put in perspective contemporary shifts in our understanding of infectious disease.
The power of science communication
A panel at the Hayden Library served to launch the exhibit and included Professor Joel Gill, associate professor of art and chair of the Department of Visual Narrative at Boston University; Edward Nardell, professor of global health and social medicine at Harvard Medical School; Carl Zimmer, New York Times journalist and author; John Durant, then-director of the MIT Museum and adjunct professor in the MIT Program in Science, Technology, and Society (STS); and Robin Scheffler, associate professor in MIT STS.
The panel discussed shifts in ideas about science and how we communicate them using media like videos, books, and comics.
“We need to think about our audience, we need to know the audience we’re talking to, and we need to be prepared to listen as well as to speak to the audience,” Durant said. “We also need to find ways of moving outside of the circle of people who think the way we do.”
In Scheffler’s talk, he showed examples throughout history of scientists using art and artists using science.
“By thinking about the slippery-ness between [art and science] and having a greater sense that there isn’t a hard and fast line to draw in terms of paradigm shifts in science, I think we can all have a more empathetic and practical approach in how we communicate and talk about the nature of changing science and changing understandings of disease,” Scheffler said.
Ultimately, the comic exemplifies an idea by one of its central characters, Doc Edgerton. The famed educator once said, “The trick to education is to teach people in such a way that they don’t realize they’re learning until it’s too late.”
#approach#Art#artists#Arts#Bacteria#book#Books#Cancer#Capture#Center for Art#Science and Technology#Civil and environmental engineering#communication#complexity#covid#covid 19#creators#Discoveries#Disease#Diseases#droplets#dynamics#Edgerton#education#Egypt#engineering#engineers#Environmental#Evolution#Faculty
0 notes
Text
"..I can imagine that to be rather frustrating." She sometimes feels like she can barely keep up with things as it is - she can't imagine what it must be like for someone who's 300 years old.
"I will..try to keep that in mind." And not consider herself to be the problem in not being able to understand what she's saying - easier said than done.
Gina could probably tell you what my problems are- She won't relay that sentiment though: she doesn't have to go into their frustrated relationship any further.
"Well..I think I understand the concept? Broadly? That our understanding of the world is limited, so there is so much stuff out there to bring in - sorry, that we should expand our world out into the unknown-" her need to self-correct might already portray a separate struggle: needing to get the whole thing right.
"..But I cannot get myself to believe that basically everything didn't exist- well, they did exist, but not really - until humans conjured them from the ether.
That dinosaur bones are only in the dirt because we believe they'll be there, or that miasma theory was true until someone decided that germs are a thing, and suddenly there they were- that cold didn't kill people until they assumed that it would!
It feels like dream logic! And she says it is similar to the observation paradox, but we only see that in subatomic particles, and they didn't behave the way we believed them to when observed, they just changed behaviours!
Not to mention that the whole scientific method is based on the fact that hypothesis can be wrong! So if everyone that stands in a room believes that an experiment will go one way, but then it goes another, does that not disprove the whole concept entirely?"

"Of course we're still inventing things. Many of us simply spend more time to ourselves than spend time around others. The world changes but we don't, and many are uncomfortable with feeling out of place like that. We're smart, yes, but we're people."
"And you shouldn't be so down on yourself or comparing yourself to her. Few people can be compared to her in any way, and that's how she prefers it. Sometimes I think she likes to do things to make herself even more outlandish. Covers up her insecurities."
"But know that she has problems because she has expectations and doesn't understand how to convey things to you. Granted, she's probably not the right mouthpiece."
"So, tell me this: what exactly are you struggling with in terms of trying to follow her teachings?"
45 notes
·
View notes
Text
The Guy Who Predicted Germ Theory And Went Insane
[…] Science is a slow, methodical process of testing hypotheses and forming conclusions, but every once in a while, a mind comes along that leapfrogs the entire scientific community. And even though they are right, it might take years, decades, even centuries for their ideas to be accepted. Here’s 10 examples of scientists the world just wasn’t ready for. […]
View On WordPress
0 notes