#staphylococcus aureus treatment
Text
IN A STITCH, IN A PINCH | J. TODD
SUMMARY: you’ve developed something of a friendship with the Outlaws, but you’re not quite sure about what the irascible Red Hood thinks of you.
WARNINGS: graphic description of burn injury, oblique reference to canonical parental drug dependency, reader is a meta.
NOTES: bringing back an old work! Re: the burns treatment depicted here - my area of study was clinical microbiology, not emergency medicine; everything I know about burns is relegated to opportunistic Staphylococcus aureus infection and how Gram negative skin flora influence wound healing. Take none of what you see in this fic as medical advice; if you do have a severe burn, call 999 and get your arse to an A&E ASAP.

After an extraterrestrial incident in your city that ended with something to the tune of 5 and a half million dollars worth of property damage and you knitting Arsenal's torn-open back together in a moment of adrenaline-fuelled insanity, you've developed something of a friendship with the Outlaws.
What that really means is that you periodically come off your shift at the hospital to find 2 mercenaries and an alien princess divesting your fridge of it's contents, and get wheedled into using your meta abilities to heal wounds that would otherwise take them out of play for a good few months.
You're under no illusions. You're aware that a healer is a useful contact to have, that should the situation necessitate it they'll take the few scant inches you can give and run a mile with them.
However, you're also aware that being a meta is a risk and that it pays to be liked and valued by dangerous people.
It's a friendship of convenience, but a friendship nonetheless.
Kori picks you up bodily and spins you in a tight circle until you're giggly and dizzy when confess her favourite shirts of yours are always freshly washed, just in case.
Roy gives you a vulgar wink when you order his shirt off to take a look at where his back scarred over, but faithfully applies the Vitamin E cream you give him for the scarring, trusting you to ease his discomfort, and sneaks bottles of your favourite elderflower cordial and the tins of Zambuk you can never find in the US for you to find when he leaves.
The only one you can't quite puzzle out your relationship with is Jason. He's taciturn, stands watch faithfully as Roy and Kori pull you into friendly hugs and dizzy spins, pepper playful kisses on your cheek and rub their knuckles into your hair. He rolls his eyes at his teammates' antics, huffs through his nose at your fussing.
Sometimes though, he'll call you sweetheart in a low rasp as he bumps you away from the sink to take over doing the dishes.
Sometimes, you think you catch him watching you with something unnameable and warm in his eyes.

You're not expecting your front door to fly open and damn near off the hinges late on Saturday evening — just as you're fresh out of the shower and only just into your pyjama shirt & shorts, might you add — but your alarm and annoyance die on your tongue when you see Roy and Kori's grim faces and the way that Jason sways despite both of their considerable strength holding him up.
You smell the odd, sour-smoke char of burned flesh as they pass you to ease Jason down oh so gently onto your sofa, and your gut goes cold with fear. The burn, once you get his shirt cut open, is not as extensive as you'd feared, but it's still something from a horror scene.
It's a third degree burn, skin mulberry-red, weeping and blistered in a long arc that curls up from his right hip to just under his right pectoral.
"Bloody hell." You breathe, horrified.
You run to your room, digging out your first aid kit, and drop to your knees by the couch as you tear it open.
Roy snorts, bitter as cyanide. "Yeah, that's a fairly accurate summary of the situation, sweets. The only reason he's still alive is because he dodged and got a glancing blow from the energy beam instead of a direct hit."
You look up from Jason's side.
"I'll need you and Kori to get some things." You say, hands shaking at the prospect of the task in front of you. "I can reduce the severity of the burn to a first degree, maybe, but it–"
"What do you need?" Kori snaps, terse. You reel off a list - topical antiseptic, light bandages, a banana bag & an IV kit, amoxicillin - and then look to Roy.
"I need you to get him to take some co-codamol. It'll kick in in about 10 minutes given his enhanced metabolism, but I can't do anything until he's got painkillers in him."
Roy's brows tighten further.
"Jason doesn't do opiates."
"Roy, if this was anybody else he'd be hooked up to IV morphine! If I start working on him without him having painkillers, he'll go into shock which could kill him." You exclaim.
You make low, soothing sounds when Jason tenses at the shouting, only to groan at the fresh wave of agony in his side.
The sound of Jason's pain seems to be decisive enough for Roy, who moves round the couch and grabs the box of effervescent tablets, dissolving two in water and coaxing Jason into drinking it down.
When the glass is empty, Roy is back to his feet, quick as lightning. He strides to the door, shepherding Kori out of your apartment.
"We'll be back with everything you need in half an hour, tops. Please, help him."

Jason comes out of the shrieking adrenaline of agony to the sound of your voice, and a slight cotton fuzz in his head.
Narcotics, then, but a fairly low dose for him to still retain this degree of alertness. Feeling the encroaching spectre of that terrible pain just barely held at bay, finds he's grateful for the medication.
He goes to prop himself up on his elbows, only to strike a line of phosphorus-white flare of pain down his side that has him hissing breath through gritted teeth.
Above him, you make a startled sound, press a hand to his sternum to keep him down. His eyes catch yours, and he sees the relieved sag of your spine and shoulders at the alertness in his eyes.
"Thank fuck you didn't go into shock." You sigh. "Stay still, I've just about got this down to a second degree burn. I've just got your hip."
You snap off your nitrile gloves and lean forward, cupping his face in your hands. "Don't make a habit of this. You'll kill us off with stress if you keep on nearly-dying."
As if on cue, the front door opens and Roy and Kori come into the living room, pharmacy bags clutched tightly in their grips and fragile hope in their eyes.
When they see Jason's alert eyes, the slow knit of skin and sub-dermal tissue and hear his sheepish grumbling in, response to you, their smiles are like sunlight.

Healing the burn is slow going, taking a full five evenings after your shifts.
Roy and Kori are intent on Jason staying the full course of treatment — settled by a, literally, on account of Kori, flaming row when he asks for his helmet and body armour —and though your entreaties are quieter, they're no less insistent.
It serves him right, probably, but it's driving him to distraction.
Specifically, the feeling of your hands over his skin is driving him to distraction.
He's not sure whether it's mercy or the sweetest of torture when you approach him, eyes darting down his body in a way that's half-assessing, half appraising before the heat-shock of your touch makes contact, pieces his skin back together.
(The thing is, Jason's attuned to everything about you, has been ever since you pulled Roy's flayed skin back shut whilst the city was still smoking behind you, totally unafraid in scrub trousers and a hoodie.
He's got it bad, and it's not exactly subtle.
Roy and Kori haven't missed that, or the way he reacts to you, judging by the raised eyebrows and teasing smirks as they lean up against the wall and watch you work.
He hopes the glare he levels at them over the top of your head communicates exactly what he'll do to them if they open their mouths.
It all comes to a head on Monday evening, when you come home from your OR shift, duck into the shower and then come into the living room in a too-large grey t-shirt and deliciously short sleep pants.
Jason's heart stops for a second. He lets his eyes flit despairingly over to Roy and Kori as you prep your kit, watches their unrepentant grins with a burning resentment towards them.
Having you this close to him, worry-soft and lit like a Rembrant from the lamp on the side table without being able to touch you is the closest thing to hell there is. You're close enough that he can smell the overlapping, inoffensive fragrances of your facial skincare products, see the faint pearlescent sheen of the residue of some serum on the apples of your cheeks, the tip of your nose, the soft line of your jaw.
Your nitrile-gloved hand settles gently on the raw new skin just above his hip and he jumps, his own broad hand flying up defensively to catch your wrist and still your movement. It's a mistake he regrets immediately.
The skin of your wrist is still tacky-soft with still-settling moisturiser, hair curling damp where the spray of your shower caught it. Jason's mind spins an unbidden reel of your hands, smoothing lotion over the plush expanse of your thighs, the line of your neck and the gentle swell of your décolletage, the curve of your hip.
He presses his eyes shut tightly.
He feels feral, the hungry bones of him blown open and exposed like the hull of a shipwreck. He wants to worry marks the shape of his mouth into your thighs, your neck, across your collarbones. He wants your knees bracketing his hips, the weight of you on top of him.
God, he wants–
"Are you okay? You're not in too much pain, are you?" He hears you ask.
He knows he's in far too deep when the thought of tasting the way the words roll off your tongue flits across his mind.
"Sorry." He croaks, releasing your hand. "Instinct."
(Roy turns to Kori with a snort, murmuring low so you can't hear.
"He's been watching like he wants to eat them alive since the first time we met and it's a miracle he's got enough blood north of his waistband to be capable of speech, but sure. Instinct.")
#marley.txt#jason todd x reader#red hood x gn!reader#red hood x reader#red hood x you#jason todd x gn!reader#jason todd x you#jason todd fic#jason todd#jason todd fluff#dc x reader#I am a humble path lab dude if the medicine is wrong that’s not my problem 😭👍🏽#do not get your medical advice from fic abeg#if you’re getting poly vibes…. you may be on to something…. 🤭#part 2 might come along depending on the response to this#(guess this is where we see if folks read the tags of my fics LMFAOAOAOAOA)#zambuk ref!!!! spot the sub Saharan 😭😭😭
596 notes
·
View notes
Text
"An international research team has found almost a million potential sources of antibiotics in the natural world.
Research published in the journal Cell by a team including Queensland University of Technology (QUT) computational biologist Associate Professor Luis Pedro Coelho has used machine learning to identify 863,498 promising antimicrobial peptides -- small molecules that can kill or inhibit the growth of infectious microbes.
The findings of the study come with a renewed global focus on combatting antimicrobial resistance (AMR) as humanity contends with the growing number of superbugs resistant to current drugs.
"There is an urgent need for new methods for antibiotic discovery," Professor Coelho, a researcher at the QUT Centre for Microbiome Research, said. The centre studies the structure and function of microbial communities from around the globe.
"It is one of the top public health threats, killing 1.27 million people each year." ...
"Using artificial intelligence to understand and harness the power of the global microbiome will hopefully drive innovative research for better public health outcomes," he said.
The team verified the machine predictions by testing 100 laboratory-made peptides against clinically significant pathogens. They found 79 disrupted bacterial membranes and 63 specifically targeted antibiotic-resistant bacteria such as Staphylococcus aureus and Escherichia coli.
"Moreover, some peptides helped to eliminate infections in mice; two in particular reduced bacteria by up to four orders of magnitude," Professor Coelho said.
In a preclinical model, tested on infected mice, treatment with these peptides produced results similar to the effects of polymyxin B -- a commercially available antibiotic which is used to treat meningitis, pneumonia, sepsis and urinary tract infections.
More than 60,000 metagenomes (a collection of genomes within a specific environment), which together contained the genetic makeup of over one million organisms, were analysed to get these results. They came from sources across the globe including marine and soil environments, and human and animal guts.
The resulting AMPSphere -- a comprehensive database comprising these novel peptides -- has been published as a publicly available, open-access resource for new antibiotic discovery.
[Note: !!! Love it. Open access research databases my beloved.]"
-via Science Daily, June 5, 2024
#superbugs#bacteria#viruses#microbiology#antibiotics#medicines#public health#peptides#medical news#antibiotic resistance#good news#hope#ai#artificial intelligence#pro ai#machine learning
178 notes
·
View notes
Text
The unbearable itch that accompanies the chronic inflammatory skin condition eczema has a new culprit.
Scientists have discovered that a familiar bacteria, Staphylococcus aureus, ignites persistent itches by directly triggering sensory neurons in the skin, a finding that could help researchers devise new treatments.
Eczema, which is also known as atopic dermatitis, is common in children and teenagers but also affects one in ten adults.
Up until now, immune cells and the inflammatory molecules they secrete were thought to be the main drivers of the insufferable itch that occurs with eczema. That itch so often drives a vicious urge to scratch which only damages the skin further, leaving it red, raw, swollen, and cracked.
Years ago, researchers figured out that people lacking a skin protein called filaggrin were more likely to develop eczema; but what specifically caused the itch that enflames eczema still bugged them.
Continue Reading.
365 notes
·
View notes
Text
I Just need 5 minutes to read this maybe you can save our children👇😥💔
Impetigo is a highly contagious bacterial skin infection that primarily affects young children but can occur in people of all ages. It is characterized by red sores or blisters that can ooze, crust over, and become itchy or painful. In environments such as displaced camps, where living conditions may be crowded and hygiene facilities limited, impetigo can spread rapidly among individuals.💔😥👇
In a displaced camp, where people are often living in close quarters within tents, the transmission of impetigo can be facilitated by several factors.
1. Close Contact: People in such settings frequently come into close contact with each other, which can easily transmit the bacteria that cause impetigo, namely Staphylococcus aureus or Streptococcus pyogenes.
2: Shared Facilities: Shared resources like washing facilities, bedding, and clothing can become contaminated with bacteria and contribute to the spread of the infection.
3. Hygiene Challenges: Limited access to clean water and soap makes it difficult to maintain good personal hygiene, increasing the risk of infection and its spread.
4. Crowded Conditions: Overcrowding in tents can exacerbate the spread of impetigo, as the bacteria can be passed from person to person through skin-to-skin contact or through contaminated surfaces.
Preventing the spread of impetigo in such environments involves improving sanitation, educating residents about hygiene practices, and ensuring access to medical care for early diagnosis and treatment. Implementing effective infection control measures, such as regular cleaning of shared spaces and prompt treatment of affected individuals, is crucial in managing outbreaks and protecting the health of displaced populations.
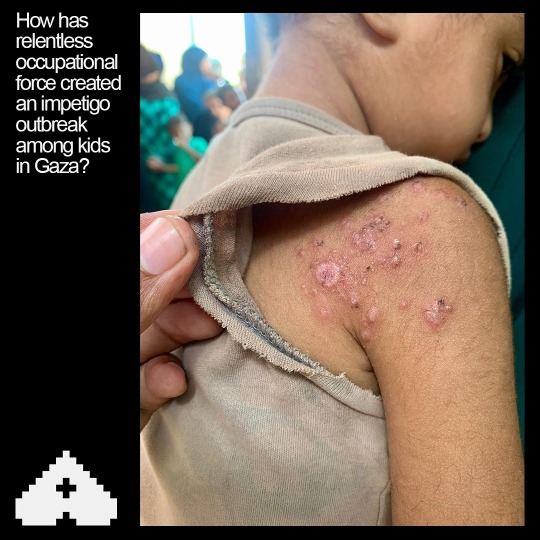

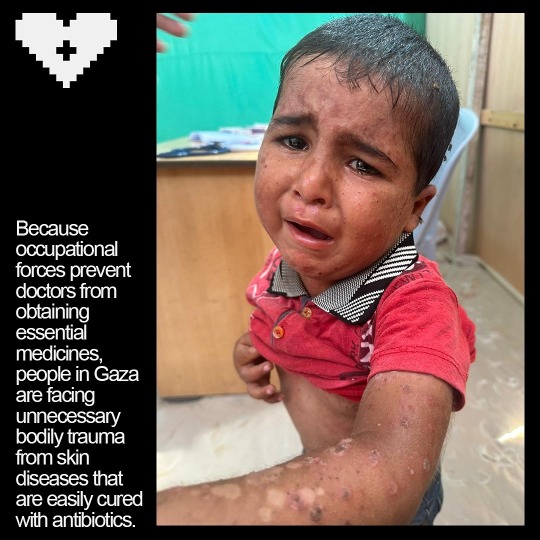
Save our children from this war. Link for donation 👇🔗🍉
Verified by OOB master list line 395 👍
Sending you lots of love and hugs for standing with us🇵🇸🍉🙏
@fairuzfan @sayruq @longlivepalestina @nabulsi @self-hating-zionist @thenewgothictwice @el-shab-hussein @risoria @palipunk @palestine @intersectionalpraxis @fallahifag @sealuai @malcriada @mangocheesecakes @youdontknowwhotfiamm @farcillesbian @stil-lindigo @apsswan @star-and-space-ace @rainbowywitch @marscodes @oursapphirestar @annoyingloudmicrowavecultist @boyvandal-blog @the-bastard-king @13ag21k @agentfascinateur
#palestine#free gaza#gaza#gaza genocide#gaza strip#fuck israel#rafah#education#north gaza#film#art#advertising#architecture#animals#black and white#nail art#artists on tumblr#my art#digital art#artwork#he#self help#human rights#humanization#humanity#history#children
19 notes
·
View notes
Note
Hi! I just found your blog and noticed you have some posts where you explain how to write certain medical conditions, and I was wondering - could you perhaps do a post on blood poisoning, please? I am struggling with it a little lol.
I have a character that got stabbed, and I don't know what are the odds they could get blood poisoning and if yes, how fast and generally how it progresses.
If you don’t have time or something, don't sweat it, it's just a silly idea I got lol :D
Episode 4 of SciFiMedic Explains: How do I write sepsis?
Hi Anon!
So, your character got themselves stabbed, huh? Before we get to the nuts and bolts of how this is going to progress, we have to clear up a little choice of words here.
The term blood poisoning is not the medically correct term for an infection inside the blood- we call it sepsis. Unless you meant literal poison from the weapon (which I can do a follow-up post on, if that’s the case) I’m going to guess that we’re talking about a severe, system-wide infection of the blood.
Let’s walk through a few options:
Scenario 1:
Your character is stabbed in an area with lots of big blood vessels (highlighted red in diagram), and while everyone does all they can, the poor guy quickly dies of blood loss. There’s no time for infection to set in.
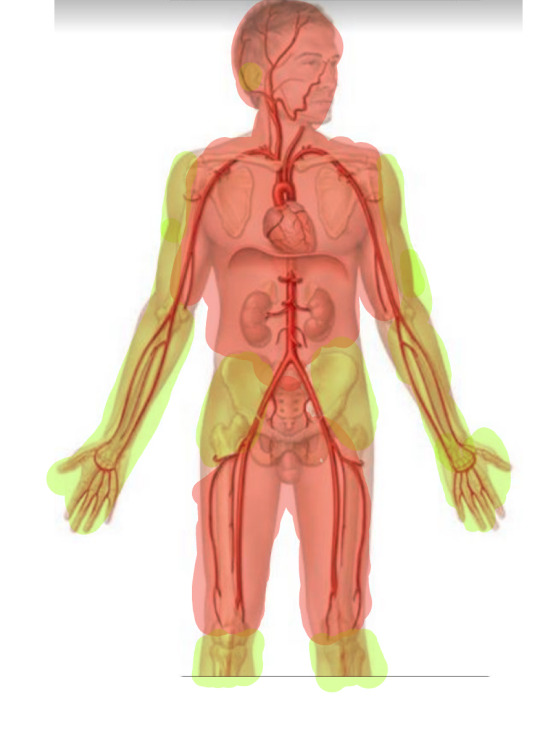
Scenario 2:
Your character is stabbed in a non-lethal area, like the arms, legs, or shallowly on the gut (highlighted green in diagram) They’re able to bandage themselves up, or maybe someone helps them out and they manage to get the bleeding stopped.
Unfortunately, 12 hours later, they notice red streaking coming from around the wound. They also:
Feel freezing cold, but have a high temperature
Are dizzy
Are shivering
Can’t quite catch their breath and feel the need to pant
Throw up
Look pale
These are all signs of the injury going septic, which is when the infection spreads away from the site of the wound and into the bloodstream. It happens fast. From the onset of these symptoms, they can be dead within only 12 hours.
Here’s what needs to happen for them to survive:
1: Hospital. No buts, no delay. If you want them to survive, they need advanced medical treatment, detailed below. (I will allow for a field hospital, or a makeshift hospital with a trained professional and plenty of supplies.)
2: Blood and wound cultures. This means taking a small tube of blood from the arm, rubbing a cotton swab in the wound, and then sending both samples to the lab for study. They will smear the sample on a slide, put it in a warm, wet environment, and wait for it to grow out. Then, they’ll pop it under a microscope and run chemical tests on it to find out what the infection is. This process can take up to 4 days. The good news? The more pathogens that’s in the sample, the faster it will grow out. If you have blood that is severely infected, it could take as little as 12 hours to see results. (I know this from personal experience.)
If you’re in a field hospital, unfortunately this is a luxury you don’t have. See next step.
3: IV antibiotics immediately. Since you don’t know the bacteria causing the sepsis, you don’t know which antibiotic to give. Good news, people a lot smarter than I have created a plan for this.
3a: According to this study done by the National Library of Medicine, 67.9% of people presenting outside a hospital setting had their wounds infected with either Staphylococcus aureus or Pseudomonas aeruginosa.
3b. Thankfully, we have two very strong antibiotics- Vancomycin and Ciprofloxacin- that can each treat these pathogens. Unfortunately, each antibiotic is effective against only one of these pathogens, and nearly useless (or has developed resistance) against the other one!
3c. Good news, these antibiotics can be safely run together. Boom, you’ve just slammed (and it’s a slam- these drugs are horrible for you long term) 67.9% of patients with the right antibiotics to start treating their sepsis.
3d. What about the other 32.1% you may be asking? Good news, they’re not doomed. Just because a given antibiotic isn’t the best choice against a certain pathogen, it doesn't mean it will be completely ineffective. You may be buying them more time for the cultures to come back. You can also take your next best guess, and switch the antibiotics after a few hours if they aren’t having any effect.
4. Fluids. IV time! The biggest tell that someone has sepsis is that their blood pressure plummets to dangerous levels (which is what will eventually kill them, but we’ll get to that.) In order to prevent that drop, we need to raise the blood pressure by adding more volume to the blood through fluids. They might also need a blood transfusion, depending on how much blood they lost from the initial stab wound.
It’s important to note that it may not be possible to gain IV access, because when the blood pressure is that low, the veins tend to shrivel up and disappear (not literally.) In that case, your next best option is an IO, which is a needle drilled into the center of the upper arm bone, or lower leg bone. Yes, it hurts.
5. Vasopressors. Fancy name for medications that force the blood pressure to come up. There are four main pressors:
Norepinephrine
Epinephrine
Phenylephrine
Vasopressin
They should be added in that order, although this article admits there isn’t too much hard evidence to back this up.
It’s important to note that this is ICU level care, and unless we’re in the middle of the woods, we will have transferred there.
How do you know if it’s time to add another pressor? You’re not getting the results you need- AKA the blood pressure is continuing to stay or fall too low. In the ICU, we use a different measure of blood pressure that most people aren’t as familiar with, called a MAP score. It’s easy, I promise.
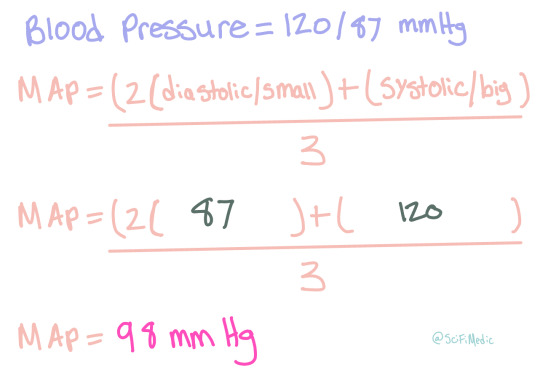
We use this method because it’s more representative of the amount of blood actually getting to the organs- though that is debated quite a bit in various circles. In America however, that’s the way most ICUs do it.
The ultimate goal for a sepsis case is to have a MAP above 65 mmHg. You can use this calculator to play around with the numbers and see if the blood pressure you’re thinking is within those parameters. If it’s not, time for another pressor.
At this point, your character is passed out most of the time. They’ve got a high fever, rapid heart beat, and are covered in sweat. They might also have a seizure from the fever and general stress on their body- at the very least they’ll be shaking from the chills. Their skin will be very, very pale, and might look kinda blue or gray in places- kinda like spots.
6. Hold your breath. No, not literally. But at this point, you’ve done all you can and you have to wait for them to either get better, or get worse.
If they get better, they’ll slowly start to maintain their own blood pressure, the fever will come down, and they’ll be able to string a coherent sentence together again. Recovery from sepsis can take a long, long time- as many as two to four months in the hospital. It totally depends on the person and how strong they are. The fittest, luckiest patient I’ve seen recover from sepsis was with us in the ICU for three weeks, then spent another month in a step down unit doing various therapies to regain strength.
However… if we’re looking at failure… well, then it’s time to move onto scenario 3.
Scenario 3:
After completing all of the above steps, they end up getting worse. Don’t worry, it’s not your fault- sepsis is fickle and kills fast. At this point, their kidneys are starting to fail from the inadequate blood pressure- you’ll need dialysis for that. They might stop breathing, or be unable to oxygenate their blood properly, then they’ll need a ventilator. At this point, they’re not stable enough to go into surgery anymore, so there’s no hope there. Eventually, the high fever will cause seizures, which will lead very quickly to brain death. As little as 12 hours after the initial dizziness and red streaks, their heart stops and they’re pronounced dead.
Summary:
The odds of your character developing sepsis from a non-fatal stab wound without immediate medical care are high- 90%
If they’re rushed to a hospital, their odds are better- 50%
If they do develop sepsis inside a hospital, they’re likley to survive- only 10.55% of people die of this kind of wound infection.
If they develop sepsis outside a hospital, then it’s almost certain they will die- 99%
Disclaimer: Although I’m in school to become a medical professional, I’m not one yet. All mistakes are mine, and I’m always open to discussion.
Anon, this was a fun prompt! If this isn’t quite what you were looking for, feel free to submit another ask with more follow up questions!
Everyone else, also feel free to send me an ask, or reblog this (or any SciFiMedicExplains Episode) with a scene you’d like me to help you write!
#whump#whump writing#medically accurate#writing help#sepsis#fever#hospital whump#infection#accurate whump#stabbing#injury#SciFiMedicExplains#medical whump
23 notes
·
View notes
Text



Staphylococcus Aureus : This is the most dangerous of all of the many common staphylococcal bacteria. This bacteria often causes skin infections but can cause pneumonia, heart valve infections and bone infections.
# These bacteria are spread by having direct contact with an infected person
# skin infections are common but the bacteria can spread through the bloodstream and infect distant organs ; blisters, abscesses, and redness and swelling in the infected area.
Treatment: Antibiotics
Surgical removal of infected bone and or foreign material
…. Health is wealth …
12 notes
·
View notes
Text

Tartarian Aster
Did you know: This species has been used for at least 2,000 years in traditional Chinese medicine. The root contains triterpenes and triterpene saponins, and is a stimulant expectorant herb for the bronchial system, helping to clear infections. It is antibacterial, antifungal, antitussive, expectorant and stimulant. It has an antibacterial action, inhibiting the growth of Staphylococcus aureus, E. coli, Bacillus dysenteriae, B. typhi, Pseudomonas and Vibrio Proteus. The root is taken internally in the treatment of chronic bronchitis and tuberculosis and is often used raw with honey in order to increase the expectorant effect. The root is harvested in the autumn and can be dried for later use. The plant contains the triterpene epifriedelinol, which has shown anticancer activity, and is used as a folk cure for cancer.
This plant is also stunning, native, drought tolerant, and a great source of late season pollen.
39 notes
·
View notes
Text
Medical Abbreviations on Pharmacy Prescriptions
Here are some common medical abbreviations you may see on pharmacy prescriptions:
qd - once a day
bid - twice a day
tid - three times a day
qid - four times a day
qh - every hour
prn - as needed
pc - after meals
ac - before meals
hs - at bedtime
po - by mouth
IV - intravenous
IM - intramuscular
subQ - subcutaneous
mL - milliliter
mg - milligram
g - gram
mcg - microgram
stat - immediately, right away
NPO - nothing by mouth
cap - capsule
tab - tablet
susp - suspension
sol - solution
amp - ampule
inj - injection
Rx - prescription
C - Celsius
F - Fahrenheit
BP - blood pressure
HR - heart rate
RR - respiratory rate
WBC - white blood cell
RBC - red blood cell
Hgb - hemoglobin
Hct - hematocrit
PT - prothrombin time
INR - international normalized ratio
BUN - blood urea nitrogen
Cr - creatinine
Ca - calcium
K - potassium
Na - sodium
Cl - chloride
Mg - magnesium
PO2 - partial pressure of oxygen
PCO2 - partial pressure of carbon dioxide
ABG - arterial blood gas
CBC - complete blood count
BMP - basic metabolic panel
CMP - comprehensive metabolic panel.
ECG - electrocardiogram
EEG - electroencephalogram
MRI - magnetic resonance imaging
CT - computed tomography
PET - positron emission tomography
CXR - chest x-ray
CTX - chemotherapy
NSAID - nonsteroidal anti-inflammatory drug
DMARD - disease-modifying antirheumatic drug
ACE - angiotensin-converting enzyme
ARB - angiotensin receptor blocker
SSRI - selective serotonin reuptake inhibitor
TCA - tricyclic antidepressant
ADHD - attention deficit hyperactivity disorder
COPD - chronic obstructive pulmonary disease
CAD - coronary artery disease
CHF - congestive heart failure
DVT - deep vein thrombosis
GI - gastrointestinal
UTI - urinary tract infection
OTC - over-the-counter
Rx - prescription
OD - right eye
OS - left eye
OU - both eyes.
TID - thrombosis in dementia
TDS - ter die sumendum (three times a day)
BOM - bilaterally otitis media (infection in both ears)
BT - body temperature
C&S - culture and sensitivity
D/C - discontinue or discharge
D/W - dextrose in water
ETOH - ethyl alcohol
FUO - fever of unknown origin
H&P - history and physical examination
I&D - incision and drainage
I&O - intake and output
KVO - keep vein open
N&V - nausea and vomiting
PERRLA - pupils equal, round, reactive to light and accommodation
PR - per rectum
QAM - every morning
QHS - every bedtime
QOD - every other day
S/P - status post (after)
TPN - total parenteral nutrition
UA - urinalysis
URI - upper respiratory infection
UTI - urinary tract infection
VO - verbal order.
XRT - radiation therapy
YOB - year of birth
BRBPR - bright red blood per rectum
CX - cervix
DVT - deep vein thrombosis
GB - gallbladder
GU - genitourinary
HCV - hepatitis C virus
HPI - history of present illness
ICP - intracranial pressure
IVP - intravenous pyelogram
LMP - last menstrual period
MRSA - methicillin-resistant Staphylococcus aureus
MVA - motor vehicle accident
NKA - no known allergies
PEG - percutaneous endoscopic gastrostomy
PRN - pro re nata (as needed)
ROS - review of systems
SOB - shortness of breath
TAH - total abdominal hysterectomy.
TIA - transient ischemic attack
Tx - treatment
UC - ulcerative colitis
URI - upper respiratory infection
VSD - ventricular septal defect
VTE - venous thromboembolism
XR - x-ray
w/c - wheelchair
XRT - radiation therapy
ASD - atrial septal defect
Bx - biopsy
CAD - coronary artery disease
CKD - chronic kidney disease
CPAP - continuous positive airway pressure
DKA - diabetic ketoacidosis
DNR - do not resuscitate
ED - emergency department
ESRD - end-stage renal disease
FFP - fresh frozen plasma
FSH - follicle-stimulating hormone.
GCS - Glasgow Coma Scale
Hct - hematocrit
Hgb - hemoglobin
ICU - intensive care unit
IV - intravenous
JVD - jugular venous distension
K - potassium
L - liter
MCH - mean corpuscular hemoglobin
MI - myocardial infarction
Na - sodium
NGT - nasogastric tube
NPO - nothing by mouth
OR - operating room
PCN - penicillin
PRBC - packed red blood cells
PTT - partial thromboplastin time
RBC - red blood cells
RT - respiratory therapy
SOA - short of air.
SCD - sequential compression device
SIRS - systemic inflammatory response syndrome
STAT - immediately
T - temperature
TPN - total parenteral nutrition
WBC - white blood cells
ABG - arterial blood gas
A fib - atrial fibrillation
BPH - benign prostatic hypertrophy
CBC - complete blood count
CO2 - carbon dioxide
COPD - chronic obstructive pulmonary disease
CPR - cardiopulmonary resuscitation
CT - computed tomography
CXR - chest x-ray
D5W - dextrose 5% in water
Dx - diagnosis
ECG or EKG - electrocardiogram
EEG - electroencephalogram
ETO - early termination of pregnancy.
FHR - fetal heart rate
GSW - gunshot wound
H&P - history and physical exam
HCG - human chorionic gonadotropin
I&D - incision and drainage
IBS - irritable bowel syndrome
ICP - intracranial pressure
IM - intramuscular
INR - international normalized ratio
IOP - intraocular pressure
LFT - liver function test
LOC - level of consciousness
LP - lumbar puncture
NG - nasogastric
OA - osteoarthritis
OCD - obsessive-compulsive disorder
OTC - over-the-counter
P - pulse
PCA - patient-controlled analgesia
PERRLA - pupils equal, round, reactive to light and accommodation.
PFT - pulmonary function test
PICC - peripherally inserted central catheter
PO - by mouth
PRN - as needed
PT - physical therapy
PT - prothrombin time
PTSD - post-traumatic stress disorder
PVC - premature ventricular contraction
QD - once a day
QID - four times a day
RA - rheumatoid arthritis
RICE - rest, ice, compression, elevation
RSI - rapid sequence intubation
RSV - respiratory syncytial virus
SBP - systolic blood pressure
SLE - systemic lupus erythematosus
SSRI - selective serotonin reuptake inhibitor
STAT - immediately
TB - tuberculosis
TIA - transient ischemic attack.
TID - three times a day
TKO - to keep open
TNTC - too numerous to count
TPN - total parenteral nutrition
URI - upper respiratory infection
UTI - urinary tract infection
V-fib - ventricular fibrillation
V-tach - ventricular tachycardia
VA - visual acuity
WNL - within normal limits
AED - automated external defibrillator
ARDS - acute respiratory distress syndrome
BID - twice a day
BP - blood pressure
BUN - blood urea nitrogen
CAD - coronary artery disease
CHF - congestive heart failure
CVA - cerebrovascular accident
D/C - discontinue
DKA - diabetic ketoacidosis.
DM - diabetes mellitus
DVT - deep vein thrombosis
EGD - esophagogastroduodenoscopy
ER - emergency room
F - Fahrenheit
Fx - fracture
GI - gastrointestinal
GTT - glucose tolerance test
HCT - hematocrit
Hgb - hemoglobin
HRT - hormone replacement therapy
ICP - intracranial pressure
IDDM - insulin-dependent diabetes mellitus
IBS - irritable bowel syndrome
IM - intramuscular
IV - intravenous
K - potassium
KVO - keep vein open
L&D - labor and delivery
LASIK - laser-assisted in situ keratomileusis.
ROM - range of motion
RT - radiation therapy
Rx - prescription
SCD - sequential compression device
SOB - shortness of breath
STD - sexually transmitted disease
TENS - transcutaneous electrical nerve stimulation
TIA - transient ischemic attack
TSH - thyroid-stimulating hormone
UA - urinalysis
US - ultrasound
UTI - urinary tract infection
VD - venereal disease
VF - ventricular fibrillation
VT - ventricular tachycardia
WBC - white blood cell
XRT - radiation therapy
XR - x-ray
Zn - zinc
Z-pak - azithromycin (antibiotic).
AAA - abdominal aortic aneurysm
ABG - arterial blood gas
ACS - acute coronary syndrome
ADL - activities of daily living
AED - automated external defibrillator
AIDS - acquired immunodeficiency syndrome
ALS - amyotrophic lateral sclerosis
AMA - against medical advice
AML - acute myeloid leukemia
APAP - acetaminophen
ARDS - acute respiratory distress syndrome
ASCVD - atherosclerotic cardiovascular disease
BPH - benign prostatic hyperplasia
BUN - blood urea nitrogen
CABG - coronary artery bypass graft
CBC - complete blood count
CHF - congestive heart failure
COPD - chronic obstructive pulmonary disease
CPAP - continuous positive airway pressure
CRF - chronic renal failure.
CT - computed tomography
CVA - cerebrovascular accident
D&C - dilation and curettage
DVT - deep vein thrombosis
ECG/EKG - electrocardiogram
EEG - electroencephalogram
ESRD - end-stage renal disease
FSH - follicle-stimulating hormone
GERD - gastroesophageal reflux disease
GFR - glomerular filtration rate
HbA1c - glycated hemoglobin
Hct - hematocrit
HIV - human immunodeficiency virus
HPV - human papillomavirus
HTN - hypertension
IBD - inflammatory bowel disease
IBS - irritable bowel syndrome
ICU - intensive care unit
IDDM - insulin-dependent diabetes mellitus
IM - intramuscular.
IV - intravenous
LFT - liver function test
MI - myocardial infarction
MRI - magnetic resonance imaging
MS - multiple sclerosis
NPO - nothing by mouth
NS - normal saline
OCD - obsessive-compulsive disorder
OSA - obstructive sleep apnea
PCOS - polycystic ovary syndrome
PMS - premenstrual syndrome
PPD - purified protein derivative
PSA - prostate-specific antigen
PT - prothrombin time
PTT - partial thromboplastin time
RA - rheumatoid arthritis
RBC - red blood cell
RSV - respiratory syncytial virus
SLE - systemic lupus erythematosus
TB - tuberculosis.
It is important to remember that medical abbreviations can vary based on location and specialty.
Healthcare professionals should use medical abbreviations with caution and only when they are familiar with their meanings.
Patients should always communicate any questions or concerns they have about their medications or medical care to their healthcare provider or pharmacist to ensure they receive safe and accurate medical care.

9 notes
·
View notes
Text
Understanding Conjunctivitis: Causes, Symptoms, and Treatment
Conjunctivitis, commonly referred to as pink eye, is an inflammation of the conjunctiva, the thin membrane that covers the white part of the eye and lines the inside of the eyelids. This condition can cause discomfort, redness, and in some cases, even vision problems. In this comprehensive guide, we will explore the various types of conjunctivitis, delve into their causes and symptoms, discuss effective treatment options, and emphasise the importance of seeking care at the best multispeciality hospital for optimal management.
Types of Conjunctivitis
Infectious Conjunctivitis: This type is caused by bacterial or viral infections. Common bacteria involved include Staphylococcus aureus and Streptococcus pneumoniae, while adenoviruses are a common viral culprit.
Allergic Conjunctivitis: Triggered by allergens like pollen, dust mites, and pet dander, this type results from an overactive immune response and often accompanies other allergies like hay fever.
Irritant Conjunctivitis: Exposure to irritants such as smoke, chemicals, and chlorine can lead to this type, causing temporary inflammation.
Giant Papillary Conjunctivitis (GPC): Typically linked to prolonged contact lens wear, GPC involves the formation of bumps on the inner eyelids.
Causes and Risk Factors
Infectious Conjunctivitis:
Bacterial: Highly contagious, it spreads through direct contact with contaminated items or personal contact.
Viral: Spread through respiratory droplets, it's common in crowded places and among those with compromised immune systems.
Allergic Conjunctivitis:
Allergens trigger an immune response, leading to symptoms.
Individuals with a history of allergies are more susceptible.
Irritant Conjunctivitis:
Environmental irritants lead to this type.
Common in people working in chemical-heavy industries or those exposed to smoke.
Giant Papillary Conjunctivitis (GPC):
Prolonged contact lens use and improper hygiene are common causes.
More prevalent among those who use rigid gas-permeable lenses.
Symptoms
Redness and Irritation: The eyes appear bloodshot and feel itchy or gritty.
Watery or Discharge: Excessive tearing or discharge can indicate infection.
Swelling and Sensitivity: Swollen eyelids and sensitivity to light may occur.
Blurry Vision: Vision might be impaired temporarily.
Giant Papillae Formation: GPC can lead to discomfort and blurred vision due to bumps on the inner eyelids.
Diagnosis and Treatment
Diagnosis:
Healthcare professionals conduct comprehensive eye exams.
Medical history and possible triggers are considered.
Samples of eye discharge may be collected for testing in infectious cases.
Treatment:
Infectious Conjunctivitis:
Bacterial: Antibiotics in the form of eye drops or ointments are used.
Viral: Usually self-limiting; lubricating eye drops offer relief.
Allergic Conjunctivitis:
Antihistamine Eye Drops: Over-the-counter or prescription drops alleviate symptoms.
Avoidance: Identifying and avoiding allergens is crucial.
Irritant Conjunctivitis:
Artificial Tears: Lubricating eye drops flush irritants.
Avoidance: Prevent further exposure to irritants.
GPC:
Lens Management: Temporarily halt lens wear and maintain proper hygiene.
Medication: Eye drops with anti-inflammatory properties may be prescribed.
Finding Care at the Best Multispeciality Hospital
Conjunctivitis, though common, requires timely and accurate care for optimal recovery. When seeking treatment, consider the following aspects of the best multispeciality hospital:
Expertise: Look for hospitals with experienced ophthalmologists specializing in various types of conjunctivitis.
Comprehensive Care: Opt for a hospital offering a wide range of diagnostic services, treatments, and follow-up care.
Advanced Technology: The hospital should be equipped with state-of-the-art equipment for accurate diagnoses and effective treatments.
Patient-Centric Approach: Choose a hospital that prioritizes patient comfort, education, and individualized treatment plans.
Hygiene and Safety: Given the contagious nature of certain conjunctivitis types, ensure the hospital maintains strict hygiene protocols.
Reputation: Seek recommendations and read reviews to gauge the hospital's reputation and quality of care.
Prevention
Preventing conjunctivitis involves hygiene, allergen avoidance, and careful lens use:
Hand Hygiene: Regular handwashing minimizes the risk of spreading infectious conjunctivitis.
Lens Hygiene: Proper contact lens care reduces the risk of GPC and other complications.
Allergen Awareness: Stay informed about allergen levels and take precautions during peak allergy seasons.
ConclusionConjunctivitis is a common eye condition that can be caused by infections, allergies, irritants, or contact lens misuse. Understanding its types, causes, symptoms, and treatment options is crucial for effective management. Seeking care at the best multispeciality hospital ensures access to experienced professionals, advanced technology, and comprehensive treatment plans, ultimately promoting faster recovery and better eye health. Remember to prioritize hygiene and follow preventive measures to minimize the risk of conjunctivitis and its complications.
2 notes
·
View notes
Text
Necrotising fasciitis, also known as flesh-eating disease, is a rare but serious bacterial infection that can rapidly destroy skin, fat, and muscle tissue. It's important to be aware of the signs and symptoms of this condition to seek prompt medical attention.
The initial symptoms of necrotising fasciitis may include redness, swelling, and severe pain in the affected area, as well as fever, nausea, and vomiting. As the infection progresses, skin may turn purple or black, and blisters may form. The bacteria can enter the body through a cut, scrape, or other type of wound.
Necrotising fasciitis can be caused by a variety of bacteria, including group A streptococcus and methicillin-resistant Staphylococcus
aureus (MRSA). The condition can progress rapidly and become life-threatening if not treated promptly.
Treatment typically involves antibiotics and surgery to remove dead tissue. Early detection and treatment are crucial for a successful recovery. If you suspect an infection, seek medical attention immediately.
Preventing necrotising fasciitis starts with good wound care. Keep all wounds clean and covered until they are healed. If you have a cut or scrape that shows signs of infection, such as redness, swelling, or discharge, seek medical attention right away.
It's also important to be aware of the signs and symptoms of necrotising fasciitis. Knowing what to look for can help you seek medical attention promptly and receive the care you need to recover.
On a personal note, after having seen a case go extremely wrong, I’m always in a state of panic and anxiety every time I see any swelling or redness, ?cellulits……fuck no!! I must always rule out neck fasc even if the evidence does not point that way.
2 notes
·
View notes
Photo

VRE = Vancomycin-Resistant Enterococci. Enterocci are Gram-positive bugs that normally live in the human gut, so they don’t belong in the central nervous system (meningitis) or urinary tract (UTI). Treat with linezolid, daptomycin, tigecycline, and others.
VISA = Vancomycin-Intermediate Staphylococcus Aureus. Technically these bacteria have intermediate sensitivity to glycopeptide antibiotics, so the name should be "GISA."
VRSA = Vancomycin-Resistant Staphylococcus Aureus. Due to vanA gene. Because there have been so few cases of VISA/VRSA, there are no widespread treatment guidelines; ask your local ID specialist.
2 notes
·
View notes
Text
Dicloxacillin and cephalexin are the preferred first-line therapies for nonbullous impetigo. This infection is most commonly caused by β-hemolytic Streptococcus or Staphylococcus aureus, with only around 1% of cases being identified as methicillin-resistant S aureus (MRSA). The Infectious Diseases Society of America (IDSA) has clear recommendations on therapy, and multiple sources agree with use of topical mupirocin for limited infections and empiric treatment covering both Streptococcus and Staphylococcus species. If culture determines Streptococcus species as causing disease, then oral penicillin is a reasonable alternative. Because this patient has extensive skin involvement and culture has not been performed, oral dicloxacillin, an antistaphylococcal penicillin, is indicated for empiric treatment.
Impetigo is easily recognized by its characteristic honey-colored crust. Diagnosis is often clinical, and empiric therapy should cover both Staphylococcus and Streptococcus species. If methicillin-resistant Staphylococcus aureus is identified, doxycycline, clindamycin, and sulfamethoxazole-trimethoprim are recommended for first-line treatment
5 notes
·
View notes
Photo
REXITIN, DIZOLVE & BUILDREX HERB CAPS.* *SOME TREATMENT PROCEDURES USING REXITIN, DIZOLVE & BUILDREX HERB CAPS.* *1. ULCER:* Cases of Ulcer usually take between 1-2 months of Treatment. This might require 1-2 Months Treatment depending on the Type of Ulcer and the Patients Body System. *2. FIBROID :* Cases of Fibroid requires 3 months of Treatment. *3. INFERTILITY ISSUES :* Cases of Infertility and Low Sperm Count require 2-3 months of Treatment. *4. DIABETES :* Severe cases of Diabetes might requires 3 months of Intensive Treatment to help stabilize Blood Sugar. *5. HIGH BLOOD PRESSURE :* Cases of H. B. P require 2 months of Treatment to help ensure the Blood Pressure rates of Patients are very much stable. *6. CANCER:* Cancer cases requires 6 months of Treatment at least to help kill the Cancer cells and stop it's growth. *7. HEPATITIS B* A serious liver infection caused by the hepatitis B virus that's easily preventable by a vaccine. It requires 3 months treatment. *8. ARTHRITIS* Arthritis is the swelling and tenderness of one or more of your joints. The main symptoms of arthritis are joint pain and stiffness, which typically worsen with age. The most common types of arthritis are osteoarthritis and rheumatoid arthritis. Includes Diseases: Osteoarthritis; Rheumatoid arthritis;... Cases of Arthritis requires 4 months of intensive treatment which is 2-3 caps morning and night. *STAPHYLOCOCCUS AUREUS* (3 months treatment) *PARALYSIS/STROKE* Take the normal dosage. 2-3 caps first thing in the morning before meal and 2- 3 caps in the evening before meal . Drink water always ( *Compulsory* ) *3 months treatment* *Note: DO NOT SKIP YOUR DOSAGE WHEN* *UNDERGOING ANY TREATMENT*🙅🏻♀️🙅🏽♂️* 08055391718/08060629005 https://www.instagram.com/p/Cofz8gmIfRt/?igshid=NGJjMDIxMWI=
2 notes
·
View notes
Text
Understanding Bovine Mastitis: Causes, Symptoms, and Impact on Dairy Production
Bovine mastitis is a significant issue in dairy farming, characterized by the inflammation of the mammary gland and udder tissue in cows. This condition not only affects the health of the animal but also has a considerable impact on dairy production. Understanding the causes, symptoms, and effects of mastitis is crucial for dairy farmers seeking to maintain herd health and optimize milk yield.
The primary causes of bovine mastitis are bacterial infections, although other pathogens such as viruses and fungi can also be involved. The most common bacteria associated with mastitis include Staphylococcus aureus, Streptococcus agalactiae, and Escherichia coli. These pathogens can enter the udder through the teat canal, leading to inflammation and infection.
Symptoms of mastitis can range from mild to severe. Early signs include swelling of the udder, redness, and increased warmth. Affected cows may exhibit discomfort and a reduced appetite. More severe cases can result in the production of abnormal milk, which may appear clotted or discolored, and a significant drop in milk yield. In chronic cases, mastitis can lead to permanent damage to the udder tissue.
The impact of mastitis on dairy production is substantial. Infected cows often produce less milk, and the quality of the milk can be compromised due to changes in its biochemical composition. This can lead to economic losses for farmers, as lower milk yields and reduced milk quality affect profitability. Additionally, mastitis can increase the cost of veterinary care and labor for managing and treating the condition.
Preventing and managing mastitis involves several strategies. Maintaining good hygiene practices, such as regularly cleaning milking equipment and ensuring proper teat sanitation, is essential. Providing adequate nutrition and managing cow comfort can also help reduce the risk of mastitis. Regular veterinary check-ups and prompt treatment of infections are crucial for minimizing the impact of this disease on dairy production.
understanding bovine mastitis involves recognizing its causes, symptoms, and effects on dairy production. Effective management and prevention strategies are vital for maintaining the health of dairy cattle and ensuring the quality and quantity of milk production.
For more information visit us:
0 notes
Text
Understanding the Role of Protein A in Antibody Purification

In the rapidly evolving field of biotechnology, Protein A Antibody Purification plays a pivotal role in isolating monoclonal antibodies (mAbs), which are essential in both therapeutic treatments and research applications. As demand for high-quality antibodies continues to rise, the efficiency of purification methods becomes increasingly important.
Among various purification techniques, Protein A chromatography is the gold standard for antibody purification, particularly for immunoglobulin G (IgG). This article explores how Protein A functions in the antibody purification process and why it remains so vital to the biopharmaceutical industry.
What is Protein A?
Protein A is a bacterial protein originally derived from Staphylococcus aureus. It has a high affinity for the Fc region of immunoglobulins, particularly IgG antibodies, making it a key tool for antibody purification. Due to its strong and specific binding ability, Protein A is immobilized onto chromatography resins and used in column-based purification systems. The selective nature of Protein A allows for the efficient capture of antibodies from complex mixtures, such as cell culture supernatants or serum.
The Role of Protein A in Antibody Purification
Protein A Antibody Purification is a process designed to isolate antibodies from a variety of sources. Antibodies are critical for therapies, diagnostics, and research, and their purity directly impacts their efficacy and safety in these applications. The specificity of Protein A for the Fc region of antibodies ensures that the purification process yields highly pure antibody products with minimal impurities.
High Specificity and Selectivity
The primary advantage of Protein A Antibody Purification lies in its high specificity. Protein A selectively binds to the Fc portion of IgG antibodies, leaving other proteins and impurities behind. This strong affinity for IgG is especially useful when purifying antibodies from complex biological mixtures. This high degree of selectivity reduces the need for additional purification steps, making the process more streamlined and cost-effective.
Efficiency and Yield
Protein A chromatography is renowned for its efficiency. The method allows for the rapid purification of large quantities of antibodies in a relatively short time. This is particularly important in industrial-scale antibody production, where time and yield are critical factors. Protein A Antibody Purification consistently produces high yields of pure antibodies, making it the preferred method in commercial biomanufacturing settings.
Scalability
Another major advantage of Protein A Antibody Purification is its scalability. Whether purifying milligrams of antibody for research or kilograms for therapeutic use, Protein A chromatography can be adapted to meet the scale required. The technique is well-established in both small-scale laboratory environments and large-scale commercial antibody production facilities.
Purity and Quality
One of the key metrics for any purification process is the purity of the final product. Protein A Antibody Purification consistently delivers highly pure antibodies, typically achieving purities of over 95%. This high level of purity is critical for therapeutic antibodies, where any impurities can impact the safety and efficacy of the drug. In addition to purity, Protein A purification provides high-quality antibodies with preserved structural integrity and biological activity, which is essential for their function in clinical settings.
Challenges and Considerations in Protein A Antibody Purification
While Protein A Antibody Purification is highly efficient and widely used, it is not without its challenges. One of the primary concerns is the cost of Protein A resins, which are relatively expensive compared to other chromatography methods. However, the cost is often justified by the high yield and purity of the antibodies obtained.
Another consideration is that Protein A has a strong affinity primarily for IgG antibodies. For antibodies that do not have an Fc region or for other types of immunoglobulins, alternative purification methods may be required. Despite these challenges, Protein A remains a versatile and indispensable tool in the purification of monoclonal antibodies.
Conclusion
Protein A Antibody Purification continues to be a cornerstone in the biopharmaceutical industry, particularly for the production of monoclonal antibodies. Its high specificity, scalability, and ability to produce high-purity antibodies make it the preferred choice for antibody purification in both research and therapeutic applications. Although there are challenges associated with its use, the benefits far outweigh the costs, making Protein A an essential component of modern antibody purification processes.
By understanding the critical role that Protein A plays in antibody purification, researchers and manufacturers can optimize their processes to achieve the highest quality antibody products. This, in turn, contributes to the development of more effective therapeutics and diagnostic tools, ultimately improving patient outcomes.
Original Source: https://lyticsolutions.blogspot.com/2024/09/understanding-role-of-protein-in.html
0 notes