#polycystic ovarian syndrome acne treatment
Explore tagged Tumblr posts
Text
5 Reasons To Start PCOS Treatment In Homeopathy
It is ideal to consult a homeopathy doctor for PCOS treatment.
Some of the major reasons start PCOS treatment in homeopathy are: -
Get medicines free from side effects
Get remedies which are natural and suitable to your bodily needs
A holistic approach to treat irregular periods
Good treatment for hormone problems and cysts in ovaries with PCOD
Effective treatment for skin and hair problems like acne and hairfall
Consult Dr. Chintan Mehta in Mumbai, India to start treatment for polycystic ovarian syndrome.
Whatsapp +91 9869021226 to book appointment with Dr. Mehta in India.
Get the best homeopathy doctor for PCOS treatment in Mumbai India.
#pcod treatment#pcodawareness#pcos treatment#pcossupport#pcosawareness#homeopathy#ayushmanbharat#homeopathic doctor#homeopathy treatment#homeopathic clinic near me#homeopathy doctor#health & fitness#healthcare#acne treatment#polycystic ovarian syndrome#ovarian cysts
0 notes
Note
Hello sex witch,
I’ve got a period that’s normally pretty late, but right now it’s in the 40 day range. My mom told me it was because I weigh too much and that’s making my period irregular. Does weight have anything to do with periods? I’ve only seen things about being underweight leading to skipped periods, not overweight, and I can’t tell what’s the medical establishment being against fat people as a concept vs an actual thing that doctors have studied.
hi anon,
okay, so: I want to start by saying that if your mom is telling you that you weight too much your mom is being an asshole, full stop. there is no such thing as weighing too much; you weigh what you weigh.
the main thing we might want to be on the lookout for is polycystic ovarian syndrome (PCOS), which is the most common cause of long period cycles. people with PCOS are often also fat, because PCOS is caused by high levels of androgens and that can also cause people to gain weight. I want to be so clear that this is not a case of fatness causing irregular periods; this is a case of fatness and irregular periods both being caused by the same thing. blaming fatness for something it doesn't cause is fatphobic and unhelpful.
having said that! being fat + having an irregular period does not automatically mean PCOS is afoot, and if your periods are otherwise fine - no excess bleeding or debilitating pain, that kind of thing - then straight up, I wouldn't be concerned. if you're not in pain, then a 40 day cycle is fine. if you do have any difficulty with pain management around your periods, or if you're just curious to learn more, I'd recommend looking into some common PCOS symptoms to see if anything there resonates with you. this is a good place to start:
87 notes
·
View notes
Text
Understanding Hirsutism: How PCOS Affects Hair Growth
Hello again, and welcome back to Shining Through PCOS! Today we’re continuing a topic that resonates deeply with many of us living with Polycystic Ovarian Syndrome (PCOS)—hirsutism—and how our hormone imbalances contribute to this challenging symptom.
The Hormonal Connection to Hirsutism
Hirsutism, the growth of coarse, dark hair in areas where men typically grow hair, is one of the most distressing symptoms of PCOS. While it’s not uncommon for women to experience unwanted hair growth at some point, for those of us with PCOS, it often feels like a relentless battle against our own bodies. Understanding the underlying hormonal imbalances can help us navigate this challenge with more compassion for ourselves.
Previously, we discussed how some of the conditions we deal with as a result of PCOS overlap. At the heart of hirsutism in women with PCOS are elevated levels of androgens, often referred to as “male hormones.” While everyone has these hormones to some degree, women with PCOS typically have higher-than-normal levels (Rizvi et al., 2023). This hormonal imbalance is primarily due to something called insulin resistance, a condition where the body’s cells become less responsive to insulin, leading to higher levels within the bloodstream (Barber et al., 2019). Elevated insulin can stimulate the ovaries to produce more androgens, which in turn contributes to symptoms like hirsutism, acne, and irregularities in ovulation (Rosenfield & Ehrmann, 2016).
Understanding the Role of Androgens
Androgens play a crucial role in hair growth, but not in the way we might hope. In women with PCOS, the overproduction of hormones like testosterone can lead to the development of male-pattern hair growth (Mihailidis et al., 2015). Common areas for hirsutism include the face, chest, and back, making it a source of significant emotional distress for many of us (Mihailidis et al., 2015).
I remember grappling with so much embarrassment over the abundance of body hair I dealt with as a child. I felt perpetually frustrated and humiliated in my own skin. It’s a tough battle to handle feelings of inadequacy, especially at a young age when you’re not only worried about your self-perception but also how others perceive you. Many people may tell you it’s “just body hair,” but they underestimate the toll it can take. It affects how you perceive yourself, deprives you of your femininity, and impacts your ability to relate to others and feel a sense of normalcy and autonomy. It’s so much more than just hair.
For many women, including myself, it goes beyond mere appearance; it’s about how we feel in our skin. The pressure to meet certain beauty ideals can lead to feelings of shame and isolation, particularly in visible areas where hair growth can’t be ignored. It's vital to remember that these feelings are valid, and seeking support—whether through friends, family, or professional help—can be an important step in managing the emotional toll of PCOS.
Finding Hope in Treatment Options
While hirsutism can be a challenging aspect of living with PCOS, the good news is that effective treatment options are available. Laser-Based Hair Reduction (LBHR) has emerged as a popular choice for many women looking to manage excess hair growth. However, it’s essential to remember that LBHR targets the symptoms, not the underlying hormonal imbalance. Combining this treatment with lifestyle changes and, in some cases, medications like anti-androgens can create a more comprehensive approach to managing hirsutism (Narang et al., 2018).
As a student dermal clinician, I believe it is crucial for service providers to be as transparent as possible. While LBHR is an excellent treatment for addressing the rate of hair growth, length, and density, it is not a simple fix. It becomes even more complex with how LBHR is marketed as “permanent removal” when it is, in fact, “permanent reduction.” This requires a multidisciplinary approach, which can be a lengthy process. Providers must understand when a client needs this comprehensive approach and when to refer patients for aspects of a condition that may be outside our scope of practice.
Unfortunately, patients are often taken in without understanding the complexity of their condition and are not encouraged to seek medical advice regarding their hormonal levels. It’s essential for providers to discuss all aspects of PCOS instead of offering LBHR as a mere band-aid solution.
In future posts, we’ll delve deeper into these treatment options, discussing their benefits and limitations while emphasising the importance of a tailored approach for each individual.
L ᥫ᭡
References
Mihailidis, J., Dermesropian, R., Taxel, P., Luthra, P., & Grant-Kels, J. M. (2015). Endocrine evaluation of hirsutism. International Journal of Women's Dermatology, 1(2), 90-94. https://doi.org/10.1016/j.ijwd.2015.04.003
Narang, G. S., Jasleen, J., Kaur, J., & Kaur, T. (2018). Cutis vertices gyrate: A case report. International Journal of Contemporary Pediatrics, 5(4), 1693. https://doi.org/10.18203/2349-3291.ijcp20182592
Rizvi, M., Islam, M. A., Aftab, M. T., Naqvi, A. A., Jahangir, A., Ishaqui, A. A., Iqbal, M. Z., & Iqbal, M. S. (2023). Knowledge, attitude, and perceptions about polycystic ovarian syndrome, and its determinants among Pakistani undergraduate students. PLOS ONE, 18(5), e0285284. https://doi.org/10.1371/journal.pone.0285284
Rosenfield, R. L., & Ehrmann, D. A. (2016). The pathogenesis of polycystic ovary syndrome (PCOS): The hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocrine Reviews, 37(5), 467-520. https://doi.org/10.1210/er.2015-1104
7 notes
·
View notes
Note
A beautician is following me for laser hair removal (I am 16 years old and I started about a year ago). My beautician’s boss once checked my hair situation, and she was surprised I still had so many. So you told me I might have PCOS. Then I got scared because I didn’t know anything about it, and I talked to my mom about it. She told me that in fact, especially before, I was "a monkey", although, while I felt uncomfortable with my hair, I never realized I had so much out of the ordinary. We’ll go deeper to see if the beautician was right, but in the meantime, I wanted to talk to someone about it, see if you know anything about PCOS, like how it affects menstruation or anything else.
Having a notable amount of body hair that's above the "norm" is called hirsutism, which is a symptom of hyperandrogenism, and both of those are symptoms of PCOS.
PCOS stands for polycystic ovary syndrome. Despite the name, you do not have to actually have ovarian cysts to have it, although it's likely.
Three main signs of PCOS are:
Hyperandrogenism (which can manifest things such as "excess" body hair, deeper voice, facial hair, clitoromegaly, acne, hair loss in certain areas such as the head--although, everyone's body processes androgens ("male" sex hormones) differently, so not everyone will present with as strong signs of androgenization, even if they have a high level of androgens in their body)
Irregular periods. This can mean a variety of things. Periods can be far longer than other's, such as over a week. They might happen less often in a year, happening in a time frame over than ~28 days for each. Some people might have much lighter periods than most people or even shorter periods, only a few days. Some people might have large blood clots or extreme pain. Endometriosis can occur with PCOS, which often causes extremely painful periods. Pain is not necessary for irregular periods, though. This can also affect your ovulation cycle as well as your fertility.
Polycystic ovaries. Ovaries can become enlarged or inflamed and have multiple fluid filled sacs that often cause pain (although they might not).
Hyperandrogenism, hirsutism, and PCOS often go hand in hand. It can be hard to tell if someone has hyperandrogenism or PCOS, in some cases, especially since hyperandrogenism is a symptom of PCOS and cysts aren't necessary to be diagnosed with it. Some people might have hyperandrogenism for no "real" reason, whereas for others it is believed their hyperandrogenism and PCOS have a medical link. There are definitely cases where these variations in bodies aren't inherently indistinguishable from the other. A medical diagnosis is often useful because it allows for treatment if the patient desires it.
So, to be clear, based on what you describe, it's incredibly likely you have hirsutism, in which cause you may have hyperandrogenism (which, in turn, is a symptom of PCOS).
It's completely okay to be scared. Unknown things are scary, as is learning new things about our body. PCOS may sound like a scary syndrome, but it is incredibly common. Many women and people live with it. Many intersex people view it as an inherently intersex variation, as do they with hyperandrogenism and hirsutism.
While it's important to note that there are gatekeepers who do not, and these people are frowned upon by the vast majority of the intersex community and are often perisex (non-intersex) people.
Some other effects hyperandrogenism/PCOS might have include:
Oily skin
Predisposition to being fat
Smaller breasts
Insulin resistance
Increased libido
Increased muscle mass
Visible Adam's apple
More ambiguous genitalia (ties in with clitoromegaly)
If you have any other questions, feel free to send them! You are not alone. I wish you much luck on your intersex journey. And this is just some unwarranted advice, but do your best to be confident in yourself and your body. Don't let people try to influence you to do things to it or change it, especially with permanent procedures, unless it's something you've truly examined that you want, and not because others have pressured you, told you it's necessary when it isn't, or because you've been overall socially pressured to.
And I relate to that monkey comment, lol. My mom has always called me her little monkey because I've always been super hairy (although in my case, I've always taken great pride in being called that). It's part of why I chose a Pokémon based on a monkey for my new icon!
34 notes
·
View notes
Text
The Role of Yoga and Ayurveda in Women’s Reproductive Health

Women’s reproductive health is a crucial aspect of overall well-being, influencing not just fertility but also hormonal balance, menstrual health, and emotional stability. With modern lifestyles becoming increasingly stressful and sedentary, reproductive health issues are on the rise. From irregular periods and hormonal imbalances to polycystic ovarian syndrome (PCOS) and infertility, many women face challenges that affect their quality of life.
While modern medicine offers various treatments, many women seek holistic approaches that support long-term wellness without side effects. Yoga and Ayurveda, two ancient Indian sciences, provide natural and effective solutions to improve reproductive health. Ayurveda focuses on restoring balance through diet, lifestyle, and herbal remedies, while yoga enhances physical, mental, and emotional health through movement and breathwork.
Yoga and Ayurveda play a vital role in enhancing women’s reproductive health, offering practical strategies to integrate these ancient wisdom practices into daily life for better well-being.
Understanding Women's Reproductive Health Issues
Women experience a wide range of reproductive health challenges, often influenced by lifestyle, diet, stress levels, and genetic factors. Some of the most common reproductive health concerns include:
1. Menstrual Irregularities:
Irregular periods, painful cramps (dysmenorrhea), and heavy bleeding (menorrhagia) can indicate underlying hormonal imbalances. Factors such as stress, poor diet, and lack of physical activity contribute to menstrual disorders.
2. Polycystic Ovarian Syndrome (PCOS):
PCOS affects millions of women worldwide and is characterized by irregular periods, excessive hair growth, acne, and weight gain. It is often linked to insulin resistance and inflammation.
3. Endometriosis:
This condition occurs when tissue similar to the uterine lining grows outside the uterus, leading to severe pain, heavy periods, and fertility issues.
4. Infertility and Hormonal Imbalances:
Conditions like thyroid disorders, high prolactin levels, and premature ovarian failure can impact fertility, making it difficult for women to conceive.
5. Menopause and Perimenopause Symptoms:
As women age, hormonal fluctuations cause symptoms like hot flashes, mood swings, insomnia, and reduced bone density.
The good news is that yoga and Ayurveda offer natural ways to manage and improve these conditions by restoring hormonal balance, reducing stress, and promoting overall reproductive health.
Ayurveda: A Holistic Approach to Women's Reproductive Health
Ayurveda, the ancient science of life, believes that reproductive health is deeply connected to the balance of the three doshas: Vata, Pitta, and Kapha. When these doshas are in harmony, the body functions optimally, but any imbalance can lead to reproductive issues.
1. Ayurvedic Diet for Reproductive Health:
• Vata Imbalance: Causes irregular cycles and infertility. Eat warm, nourishing foods like ghee, milk, and cooked vegetables.
• Pitta Imbalance: Leads to heavy bleeding and inflammation. Consume cooling foods like cucumbers, coconut, and aloe vera juice.
• Kapha Imbalance: Can cause PCOS and weight gain. Eat light, dry foods like lentils, bitter greens, and turmeric.
2. Herbal Remedies:
• Ashwagandha: Helps manage stress and balance hormones.
• Shatavari: Supports fertility and regulates menstrual cycles.
• Turmeric: Reduces inflammation and improves digestion.
• Triphala: Detoxifies the system and enhances gut health.
3. Panchakarma Therapy:
This Ayurvedic detoxification process helps remove toxins, balance hormones, and rejuvenate reproductive organs.
Ayurveda teaches that by following a proper diet, using natural remedies, and adopting a balanced lifestyle, women can significantly enhance their reproductive health.
The Power of Yoga in Supporting Women's Reproductive Health
Yoga plays a vital role in enhancing reproductive health by improving blood circulation, reducing stress, and balancing hormones. Certain yoga postures are specifically designed to strengthen the reproductive organs and promote fertility.
1. Best Yoga Poses for Reproductive Health:
• Baddha Konasana (Butterfly Pose): Improves blood flow to the pelvic region and regulates menstrual cycles.
• Bhujangasana (Cobra Pose): Stimulates the ovaries and enhances hormonal balance.
• Setu Bandhasana (Bridge Pose): Strengthens the pelvic muscles and relieves menstrual discomfort.
• Supta Baddha Konasana (Reclining Bound Angle Pose): Relaxes the reproductive organs and reduces stress.
2. Breathing Techniques (Pranayama):
• Anulom Vilom (Alternate Nostril Breathing): Balances hormones and calms the nervous system.
• Bhramari (Bee Breath): Reduces anxiety and promotes relaxation.
3. Meditation and Relaxation:
Stress is a major factor in reproductive health issues. Practicing mindfulness and guided meditation can significantly lower cortisol levels, improving overall well-being.
Practical Tips to Integrate Yoga and Ayurveda into Your Daily Life for Better Reproductive Health Results
1. Start Your Day with Warm Water and Lemon: Helps detoxify and improve digestion.
2. Practice Yoga Daily: Even 15-20 minutes can bring noticeable improvements.
3. Eat Seasonal and Wholesome Foods: Prioritize fresh, home-cooked meals over processed foods.
4. Use Herbal Supplements Mindfully: Consult an Ayurvedic practitioner before taking herbs like Ashwagandha and Shatavari.
5. Maintain a Regular Sleep Cycle: Proper rest is essential for hormonal balance.
6. Manage Stress with Meditation and Breathing Exercises: Reducing stress is key to a healthy reproductive system.
7. Stay Active but Avoid Overexertion: Moderate physical activity like walking or gentle yoga helps maintain balance.
Conclusion
Women’s reproductive health is deeply connected to their overall lifestyle, mental well-being, and daily habits. While modern medicine provides effective treatments, integrating yoga and Ayurveda into daily life can offer long-term benefits without side effects. By focusing on balanced nutrition, stress management, and mindful movement, women can naturally improve their reproductive health and overall vitality.
Whether dealing with PCOS, menstrual irregularities, or fertility concerns, these holistic practices offer a natural path to healing. With consistency and awareness, every woman can harness the power of Ayurveda and yoga to achieve better reproductive health and a higher quality of life.
4 notes
·
View notes
Text
PCOS: Understanding Polycystic Ovary Syndrome
Introduction
PCOS, or polycystic ovary syndrome, is a common hormonal disorder that affects millions of women worldwide. It is characterized by the presence of multiple cysts on the ovaries, as well as a range of symptoms that can have a significant impact on a woman's quality of life. In this article, we will explore the causes, symptoms, and treatment options for PCOS, providing you with a comprehensive understanding of this condition.
What is PCOS?
PCOS is a condition that affects the female reproductive system. It occurs when the ovaries produce excess androgens, which are male hormones typically found in smaller amounts in women. This hormonal imbalance can disrupt the normal menstrual cycle and lead to the growth of small cysts on the ovaries.
Causes of PCOS
The exact cause of PCOS is unknown, but several factors may contribute to its development. These include:
Genetics: PCOS tends to run in families, suggesting a genetic link.
Insulin Resistance: Insulin is a hormone that helps regulate blood sugar levels. Insulin resistance occurs when the body's cells become less responsive to the effects of insulin, leading to an overproduction of the hormone and an increase in androgen levels.
Hormonal Imbalance: Women with PCOS produce higher levels of androgens and lower levels of estrogen, which can disrupt the normal menstrual cycle.
Symptoms of PCOS
PCOS can manifest differently in each individual, but some common symptoms include:
Irregular or Absent Menstrual Periods: Hormonal imbalances can cause irregular or infrequent menstruation.
Excess Hair Growth: Increased androgen levels can stimulate the growth of excess facial and body hair.
Acne: PCOS-related hormonal imbalances can lead to the development of acne on the face, chest, and upper back.
Weight Gain: Many women with PCOS struggle with weight gain and find it difficult to lose weight.
Fertility Issues: PCOS is one of the leading causes of infertility in women due to the disruption of the ovarian function.
Diagnosis and Treatment
If you suspect you may have PCOS, it is important to consult with a healthcare professional. A doctor will typically perform a physical examination, review your medical history, and may order further tests, such as blood tests or ultrasound, to confirm a diagnosis.Treatment options for PCOS focus on managing symptoms and reducing the risk of long-term complications. These may include:
Lifestyle Changes: Maintaining a healthy weight through diet and exercise can help regulate hormone levels and improve symptoms.
Medications: Birth control pills, anti-androgen medications, and insulin-sensitizing drugs are commonly prescribed to manage PCOS symptoms.
Fertility Treatments: For women struggling with infertility, fertility treatments such as ovulation induction or in vitro fertilization (IVF) may be recommended.
Conclusion
PCOS is a complex condition that can have wide-ranging effects on a woman's health and well-being. By understanding the causes, symptoms, and treatment options for PCOS, individuals can take control of their health and work with healthcare professionals to manage their condition effectively. If you suspect you may have PCOS, it is essential to seek medical guidance for a proper diagnosis and personalized treatment plan to improve your quality of life. Remember, early intervention and ongoing management are key to living well with PCOS.
#pcos#pcosawareness#pcosweightloss#pcosjourney#pcossupport#american healthcare#disability#joint pain#hormones#endometriosis
14 notes
·
View notes
Note
What's pcos
PCOS stands for PolyCystic Ovarian Syndrome. This is a hormonal disorder that wrecks havoc on the body causing symptoms such as menstrual irregularity, infertility, enlarged ovaries (inflammation/pain), weight gain, insulin resistance, excess hair, acne, and of course as the name says, cysts on the ovaries.
There is no known cause, just that androgens are elevated for some reason. It is likely a genetic disorder. PCOS is common in people with ovaries, and it is often a chronic condition. There is no cure. The medical treatment is hormone therapy aka birth control, which can sometimes worsen symptoms instead of helping them. If there are cysts, they can be removed via laparoscopy.
In my own journey, I discovered I had PCOS when I was in college. I have always had irregular, painful, extremely bloody periods since I was 12. I thought it was normal. In my younger twenties, I was having extreme pain so horrible I went to the OBGYN and that is when I found out via ultrasound that I had a cyst on my ovary. I was confirmed to have PCOS. This cyst burst and it was terrible pain and swelling for days. I got on birth control and it was heaven; most of my symptoms disappeared. Eventually I stopped taking it when I left college and switched insurances and doctors, planning to get back on it eventually. The cysts formed before I did. There were two this time, and while we were monitoring them waiting for them to shrink, one of them torsed (twisted) and cut off the blood supply to my ovary. This was the worst pain I have ever felt in my life. I had emergency surgery and lost my ovary. (Side note, that surgery is when my OB discovered I also had endometriosis.) I am going to remain on hormone therapy to protect my lone ovary so that I might one day be able to get pregnant. Birth control has saved my life.
#pcos#chronic illness#chronic pain#invisible illness#pcos awareness#polycystic ovarian syndrome#pcos symptoms#my PCOS journey#asks open
15 notes
·
View notes
Text
Difference Between PCOD and PCOS
You may be aware of PCOS and PCOD, although these two conditions have different names, individuals sometimes refer to them as such. Despite having similar symptoms, their causes are distinct.
Before moving on to the differences section, let’s clarify what PCOS and PCOD are. What actually takes place in these conditions? and the advantages of Ayurvedic treatment for PCOD/PCOS.
PCOD (Polycystic Ovarian Disorder): In a normal cycle of menstruation, both ovaries release eggs alternatively. This is known as polycystic ovarian disorder, or PCOD. The ovaries of females with PCOD will either release eggs that are partially or fully immature. Cysts, which are small cavities full of water, form as a result of this.
PCOS (Polycystic Ovarian Syndrome): The endocrine system is involved in PCOS, which results in the production of excess androgens. This further leads to eggs turning into cysts. However, the eggs aren’t released in this case and they are built up in the ovaries.PCOS is much more serious than PCOD because the former is a disorder of the endocrine system.
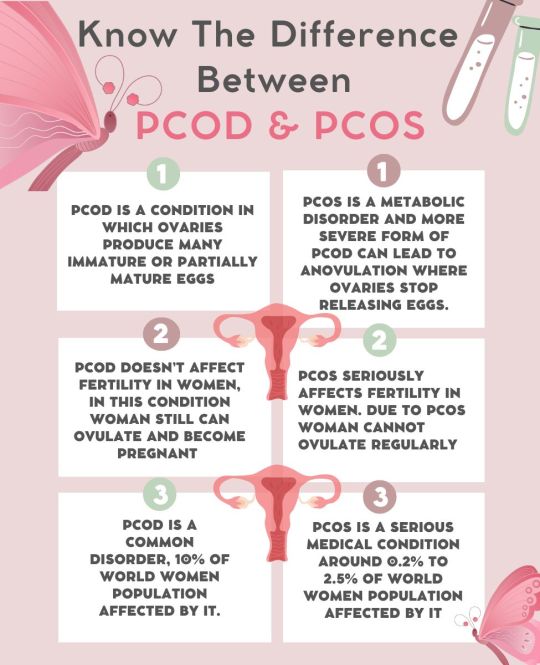
Both disorders have almost the same symptoms and causes which are listed below:
Symptoms of PCOS/PCOD
Irregular periods
Enlarged ovaries
Presence of cysts
Hirsutism
Weight gain
Acne
Male pattern baldness
Causes of PCOS/PCOD
Diet
Lifestyle
Insulin resistance
Obesity
Hormonal imbalance
There are no negative consequences from homoeopathic and ayurvedic medicine. On the other hand, Ayurveda is a natural medicine that uses a variety of herbs that are found in the natural world. Thus, I think the greatest and most efficient form of treatment is Ayurveda. It has been believed that using an ayurvedic medication is the best way to manage PCOD-PCOS. It is a natural approach that promises immediate relief and removes the disease completely. Numerous patients have found relief from various ailments with the aid of Ayurveda. You can also speak with our professionals at Dr. Sharada Ayurveda for further information.
2 notes
·
View notes
Text
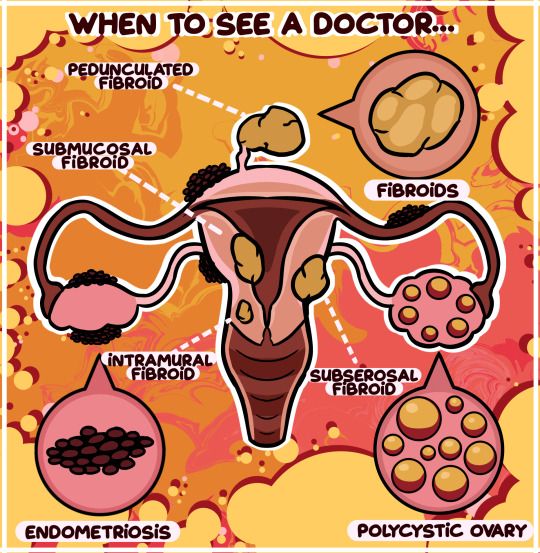
When To See A Doctor... | Comic Week 24 - created on Corel Painter.
The uterus is an important organ that holds many functions in a girl’s body. However, it can also be prone to contracting different medical issues and conditions that can alter the way someone lives their life. Last week, we explored the various abnormalities that may come about with menstruation. Today, let’s discuss three prominent medical conditions that cannot be ignored and need to be addressed by a doctor.
Polycystic ovarian syndrome (PCOS) is a condition caused by an imbalance of reproductive hormones in a woman’s body. This imbalance affects the ovaries, resulting in little fluid filled sacs called cysts forming in the ovaries, making it difficult for the ovaries to form a fully developed egg every month, or even develop an egg at all. Symptoms associated with PCOS are irregular or missed periods, excessive androgen production – a male hormone that may cause excess facial and body hair and acne – and sudden weight gain along with the inability to lose that weight easily. 10% of all women have PCOS, so it is not an uncommon condition, and it can present itself at any time after puberty. Because PCOS makes it difficult for the ovaries to produce eggs, fertility problems are common among young women with the condition who are looking to have children. It is important that, if you experience these symptoms, you ask a trusted adult to accompany you to a gynaecological visit. A gynaecologist – a specialist that deals with the health of female reproductive organs – will be able to assess you, and thankfully, PCOS is a condition treatable with medication, fertility treatment and life-style changes.
Many women – if not most women – will experience something called fibroids over the course of their life. Usually occurring in women between their 30s and 50s, fibroids are noncancerous growths that form on the uterus. These growths can range from being incredibly small in size to being large enough to distort the shape of the uterus; some women only have one, whereas other women may have many. Fibroids come in four types: intramural – appearing in the uterine muscle wall; subserosal – appearing on the outside; pedunculated – appearing on the end of a small stem; and submucosal – appearing in the middle muscle layer of the uterus. Many women may go their entire lives not realising they have fibroids because often times they present no symptoms. But when they do, menstruation with heavy and long bleeding, pelvic discomfort and bladder problems may be just a few symptoms that a woman may experience. While the growths themselves are relatively harmless, the pressure they put on the uterus and the bladder can cause serious pain, especially around menstruation. Seeing a gynaecologist when experiencing these symptoms is integral to getting the help needed to alleviate your discomfort. Thankfully, much like PCOS, fibroids are treatable with medication, non-invasive procedures and surgery – minimal and traditional.
The last condition is arguably more severe than the two above. Endometriosis is a painful disorder in which tissue much like the tissue that grows on the inside of your uterus – the endometrium – grows outside of the uterus. This tissue behaves in the same way endometrial tissue does, thickening, disintegrating and bleeding with every menstrual cycle. However, because this deteriorated tissue cannot leave the body through the uterus and down the vagina, it gets trapped and causes possible cysts on the ovaries while irritating the surrounding tissue. This irritated tissue can become scarred and develop adhesions that can make organs stick to one another! Endometriosis can affect any woman past puberty and is relatively as common as PCOS. Symptoms may include painful menstruation, pain with bowel movements, pain during sexual intercourse and infertility issues. If these symptoms plague you, then seeing a gynaecologist is certainly not optional as women with endometriosis are at a higher risk of ovarian cancer later on in life. Once again, thanks to the wonder of medicine, treatments such as hormone therapy, pain medication and, if necessary, surgery are all available to those with the condition.
The causes of these three common reproductive health issues are still relatively unclear to doctors, as many factors such as genetics and even lifestyle may contribute to their existence within a woman’s body. It is also important to keep in mind that they are not the only disorders that can affect you, so paying attention to your health and well-being at this pivotal time in your life is a habit that you should get into.
While these conditions can seem a little frightening, you are not alone if you develop one of them. Many women go about their days in a perfectly normal manner while living with them, making sure to seek medical assistance when they feel they need to. Ultimately, it is your duty to yourself to watch out for your own health and never hesitate to go to the doctor when you need to!
Illustrated and written for the IAMFORHER Foundation's educational program on puberty and menstruation for children and adolescents.
2 notes
·
View notes
Note
Hello! I have two questions if that’s okay. I was wondering if it’s normal to not be able to use a tampon? I tried several times for years but I psychically cannot :( I also wanted to know does having a very small chest indicative of less estrogen production? I’ve also started growing facial hair. My mom hasn’t ever experienced this and had an average puberty. Along with some other factors, I’m beginning to think I may have PCOS but I’m not sure because the only thing that doesn’t match up is my periods. But also my cousin has had periods that lasted weeks and left her bedridden a lot so I think it’s in my family
Hi Anon!
Sure, why not two questions? I'll answer them in two posts, tho, for easier referencing.
DOES CHEST SIZE CORRELATE TO ESTROGEN PRODUCTION?
Beyond initiation of thelarche (the beginning of breast development during puberty), and the development of breasts to prepare for lactation during pregnancy, estrogen does not affect overall breast size! That is to say - estrogen is required to develop breasts and prepare breasts for lactation, but there is no documented correlation between estrogen levels and general breast size. This is because how our bodies react to hormones is complicated and very individualized! People with larger breasts do not have more estrogen in their bodies than people with smaller breasts, and this has been proven in studies to be true of both AFAB people with endogenous (native) estrogen and trans women on estrogen hormone therapy.
(Source: Christel J M de Blok, et al. Sustained Breast Development and Breast Anthropometric Changes in 3 Years of Gender-Affirming Hormone Treatment, The Journal of Clinical Endocrinology & Metabolism, Volume 106, Issue 2, February 2021, Pages e782–e790, https://doi.org/10.1210/clinem/dgaa841)
---
QUICK PHYSIOLOGY LESSON - PCOS
Polycystic ovarian syndrome (PCOS) is a disorder marked by higher levels of androgens ("male" hormones). It's complicated, but the gist is that these higher levels of androgens lead to things like hirsutism ("excess" body hair on a person with a female hormonal profile) and acne, but also prevent ovulation from happening.
If you remember from the menstrual cycle post, the body needs estrogen to ovulate. Ovulation happens when the "cyst" around a developed egg pops. What happens if ovulation doesn't happen? You keep that cyst. . . and you don't get your period. So people with PCOS develop multiple cysts (which may be painful) from having anovulatory cycles, and have irregular, heavy periods. This can cause issues with fertility. Overweight and other endocrine issues are also common in people with PCOS.

Regarding your concerns about PCOS - this is a good concern to bring up to your doctor. The presentation of PCOS can vary wildly - not everyone has every symptom, and it does tend to run in families. Although hirsutism can be a symptom of PCOS, it can also just be a normal variant. If you're a teen, don't be surprised if your doctor takes a "wait and watch" approach, but they can probably get some bloodwork to get a baseline on your hormone levels.
Good luck!
6 notes
·
View notes
Text
PCOD / PCOS
PCOS, or Polycystic Ovarian Syndrome, has become increasingly common among women of reproductive age in recent years. Women who have this condition may have irregular or altered menstrual cycles. The ovaries may also grow a lot of fluid-filled sacks that are incapable of releasing eggs. An endocrine disorder called PCOS/PCOD is a major contributor to infertility. Subfertility is a term used to describe a condition where a person is trying to get pregnant but is having a difficult time.
Best Ayurveda treatment for PCOD and PCOS
SYMPTOMS OF PCOS/PCOD
These are some of the typical PCOS/PCOD symptoms.
Period irregularities: Women may experience irregular menstrual cycles.
Missed Periods: Missed periods may occasionally last a long time. This may continue for several months.
Severe bleeding: This is caused by a thicker than usual uterine lining. Females can have prolonged periods of heavy bleeding.
Hair growth: The back, belly, chest, and face may all experience excessive hair growth. This ailment, also known as hirsutism, can be an annoying PCOS symptom.
Acne: Areas like the face, chest, and back are more likely to experience breakouts.
Obesity: Studies have shown that managing one’s weight can significantly lessen the symptoms of PCOS in up to 80% of females who have the condition.
Hair thinning and loss: Women with PCOS/PCOD may experience hair thinning and loss. The body’s overabundance of androgens is the cause of this.
Skin darkening: The nose, groin, under the breasts, and other places may develop dark skin pigmentation or patchy skin growth.
Headaches: A hormonal imbalance known as PCOS or PCOD can occasionally result in headaches.
Pelvic pain and fatigue: Women with PCOS may experience feelings of discomfort, such as pain in the pelvic area, along with fatigue.
REASONS BEHIND PCOS
High levels of androgen
A woman’s body contains a small amount of male hormones known as androgens. However, in PCOS, the amount of male hormones increases, which can prevent the ovaries from producing eggs during the monthly menstrual cycle. This can cause acne and excessive hair growth in women, which is one of the main symptoms of PCOS.
High levels of insulin
The insulin hormone is in charge of regulating the body’s glucose levels. PCOS is a condition in which many women have insulin resistance, which means that the glucose in the blood is not being used properly by their cells. Women are more likely than men to have a family history of Type 2 Diabetes. To avoid Type 2 Diabetes in the future, lifestyle changes are advised.Obesity and unhealthy lifestyle leads to PCOS
AYURVEDIC APPROACH TO PCOD/PCOS / Best Ayurveda treatment for PCOD and PCOS
According to the ancient texts of Ayurveda, it is referred to as “Granthi” in some cases, which refers to the development of abnormalities such as cysts, ulcers, lumps, or tumors. According to Ayurveda, PCOS is caused by imbalance of Rasa and Rakta Dhatus, as well as an imbalance in the three Doshas of the body (Vata, Pitta, and Kapha). These Rasa-Rakta Dhatus are weakened as a result of Dosha imbalance and Ama (toxins) buildup in the body. This can result in cyst formation and other PCOS symptoms.
Normally, the Vata Dosha dominates the reproductive system, and the female reproductive organs are made of “Artava Dhatu,” which nourishes the ovum. Vata Dosha is in charge of the follicle and ovum movement into the uterine fallopian tubes. The sub-dosha “Apana Vayu” is in charge of the downward flow or menstrual flow. Pitta Dosha is important for hormone production and balance in the body. The Kapha Dosha is in charge of nourishing and promoting follicle, uterine, and ovum tissue growth. As a result, a harmonious balance of the three Doshas is essential for producing healthy hormones and maintaining the health of the female reproductive system.
Best Ayurveda treatment for PCOD and PCOS
Ayurveda, as a holistic system of treatment, provides an all-encompassing treatment approach that addresses the underlying cause of this condition. This treatment can be tailored to an individual’s needs, and it is always best to consult an Ayurvedic expert before beginning any treatment or therapy. The goal of Ayurveda Treatment for PCOD is to-
Ayurvedic detoxification of the body to remove accumulated toxins
The female reproductive system should be strengthened, revitalized, and nourished.
Maintaining the body’s hormonal balance
Weight loss and insulin resistance correction
AYURVEDA DIET FOR MANAGING PCOS/PCOD SYMPTOMS:
The goal of following this Ayurvedic diet is to nourish the Aartava Dhatu in females.
Organic fruits and vegetables, such as raisins, pears, plums, dates, and figs, should be consumed by PCOS women. Fruits and berries in season should be included in the diet.
To boost the Agni (Digestive fire), avoid spicy foods, fermented foods, dairy products, buttermilk, and so on.
Consume Ragi (nachini, Eleusine coracana) grains.
Avoid taking added sugar or sugary foods, as well as artificial sweeteners.
AYURVEDA TREATMENT FOR PCOD INVOLVES-
Herbs like Ashwagandha, Turmeric, Shatavari, Varuna, Haritaki, Pippali, Bilva, Agnimantha, Punarvana, Guduchi, Chitraka, Shunthi, Dashmool, Shatapushpa, and others are very effective for balancing the tridoshas and Dhatus.
Panchakarma, ayurvedic therapies, Yoga and breathing exercises (Pranayama) . Dietary changes include increasing the consumption of fruits, vegetables, and whole grains while decreasing the consumption of saturated fats, salt, refined sugar, and refined carbs.
Varunadi Kashaya, Chitrakadi Vati, Triphala Guggulu, Punarvadi Kashaya, Shatavari Gulam, and other Ayurvedic formulations are effective.
PANCHAKARMA TREATMENT FOR PCOS/PCOD / Best Ayurveda treatment for PCOD and PCOS
Panchakarma Treatment is recommended to treat the underlying cause by removing toxins from the reproductive system and empowering the various organs such as the uterus, ovaries and Fallopian tubes. This Panchakarma Treatment also aids in the maintenance of the body’s hormonal balance.
Vamana
This is a cleansing technique used primarily to expel vitiated ‘Kapha.’ In PCOS, Vamana (therapeutic emesis or therapeutic vomiting) process helps to balance the vitiated kapha dosha.
Virechana
This therapy aids in the restoration of the vitiated Pitta Dosha. It involves cleansing the small intestine and improves Dosha elimination via the rectal route. It restores the female body’s hormonal balance.
Basti (Vastu)
This panchakarma therapy, which uses various types of herbal oils, Ghruta, milk, and other decoctions, is extremely effective in balancing the vitiated Vata Dosha. When specific oils are used for Basti, it aids in the regularisation of ovulation. So, Basti can help with infertility treatment, hormone balancing, PCOS treatment, fallopian tube blockage removal, and so on.
Uttarbasti (Vasti)
Uttarbasti (Vasti) is a highly effective treatment for gynecological conditions. In the case of PCOS, Uttarbasti aids in the dissolution of ovarian cysts, the flushing of the Aartava Vaha Srotas, the pacification of the vitiated Apana Vayu, and the increase of follicular maturity.
Fertility Massage
This is a gentle massage of the lower abdomen performed in a specific pattern to improve the natural functioning of the uterus. It also improves blood circulation in the lower pelvic region.
2 notes
·
View notes
Text
PCOS Belly Look Like: Causes, Risks, and Treatments

PCOS Belly Look Like: Causes, Symptoms, and Treatments
What is PCOS?
Polycystic ovarian syndrome (PCOS) is a common hormonal disorder affecting women of reproductive age. It is characterized by irregular periods, excessive hair growth (hirsutism), acne, weight gain, and insulin resistance. PCOS can also lead to fertility issues and increase the risk of metabolic conditions like type 2 diabetes and heart disease.
What Does a PCOS Belly Look Like?
A PCOS belly is typically characterized by an apple-shaped body, where fat accumulates around the midsection. Unlike regular belly fat, PCOS belly fat is primarily visceral, meaning it surrounds internal organs and often feels firm rather than soft. This type of fat is more challenging to lose and can contribute to long-term health risks.
Causes of PCOS Belly
PCOS belly fat is mainly caused by insulin resistance and hormonal imbalances:
Insulin Resistance: Higher insulin levels trigger the ovaries to produce more androgens (male hormones), which lead to abdominal fat storage.
Hormonal Imbalance: Elevated androgen levels contribute to weight gain, particularly around the waistline.
Chronic Inflammation: PCOS is associated with increased inflammation, which can exacerbate weight gain and metabolic dysfunction.
Genetics: Some women may be genetically predisposed to storing fat in the abdominal region.
Symptoms of PCOS Belly
Women with a PCOS belly may experience:
A higher waist-to-hip ratio, often exceeding 0.87
Difficulty losing weight despite exercise and dieting
A firm, bloated midsection
Increased risk of insulin resistance, type 2 diabetes, and cardiovascular diseases
How to Manage PCOS Belly
1. Consult a Doctor
A healthcare provider can assess your symptoms and recommend a personalized treatment plan. This may include medications like metformin to improve insulin sensitivity.
2. Adopt a Healthy Diet
A well-balanced diet can significantly impact weight management and hormone balance:
High-Fiber Foods: Whole grains, vegetables, and legumes help regulate blood sugar levels.
Lean Proteins: Include chicken, fish, eggs, and plant-based proteins to support muscle mass and metabolism.
Healthy Fats: Avocados, nuts, seeds, and olive oil provide essential nutrients without spiking insulin levels.
Avoid Processed Foods & Sugar: Refined carbs and sugary drinks can worsen insulin resistance and promote belly fat storage.
3. Follow an Anti-Inflammatory Diet
Since PCOS is linked to inflammation, incorporating anti-inflammatory foods can help manage symptoms:
Eat More: Berries, leafy greens, fatty fish (salmon, mackerel), nuts, and green tea.
Limit: Processed foods, trans fats, and excessive dairy consumption.
4. Try a Low Glycemic Index (GI) Diet
A low-GI diet can help control insulin levels and support weight loss:
Include: Whole grains, non-starchy vegetables, nuts, seeds, and lean proteins.
Avoid: White rice, white bread, sugary cereals, and refined snacks.
5. Exercise Regularly
Regular physical activity improves insulin sensitivity and helps reduce visceral fat:
Cardio Workouts: Walking, swimming, and cycling can help burn calories and improve heart health.
Strength Training: Lifting weights or bodyweight exercises can increase muscle mass and boost metabolism.
Consistency Matters: Aim for at least 150 minutes of moderate-intensity weekly exercise.
6. Reduce Stress & Improve Sleep
Stress Management: High-stress levels can increase cortisol, leading to more belly fat. Try yoga, meditation, or deep breathing exercises.
Quality Sleep: Poor sleep can disrupt hormones and lead to weight gain. Aim for 6-8 hours of restful sleep each night.
Final Thoughts
Managing a PCOS belly requires a holistic approach, including a balanced diet, regular exercise, stress reduction, and proper medical guidance. While it can be challenging, small, consistent changes can lead to significant improvements. Consult a gynecologist for a personalized plan to effectively manage PCOS and support long-term health.
For more information, Please visit
https://www.saispecialitycenter.com/blog/what-does-pcos-belly-look-like/
0 notes
Text
Understanding PCOS: Causes, Symptoms, and Treatment

Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder affecting women of reproductive age. It can cause a range of symptoms, including irregular menstrual cycles, excessive hair growth, acne, and fertility issues. At Hiremath Hospital, Dr. Bharti Hiremath provides expert care for women dealing with PCOS, offering personalized treatment plans to help manage symptoms effectively.
What is PCOS?
PCOS is a condition where the ovaries produce excessive androgens (male hormones), leading to hormonal imbalances. This can result in multiple small cysts forming on the ovaries, though not every woman with PCOS develops these cysts. The exact cause of PCOS is unknown, but genetic and environmental factors play a role.
Common Symptoms of PCOS
Irregular Periods: Infrequent, prolonged, or missed menstrual cycles.
Excessive Hair Growth: Known as hirsutism, affecting areas such as the face, chest, and back.
Acne and Oily Skin: Due to increased androgen levels.
Weight Gain: Difficulty in managing weight, often linked to insulin resistance.
Hair Thinning: Male-pattern baldness or hair loss.
Infertility: Due to irregular ovulation or anovulation (lack of ovulation).
Causes and Risk Factors
The exact cause of PCOS is not fully understood, but several factors contribute to its development:
Genetics: Family history increases the likelihood of developing PCOS.
Insulin Resistance: High insulin levels can lead to increased androgen production.
Inflammation: Chronic low-grade inflammation may contribute to PCOS symptoms.
Diagnosis and Treatment at Hiremath Hospital
Dr. Bharti Hiremath at Hiremath Hospital specializes in diagnosing and managing PCOS with a comprehensive approach, including:
Medical History & Physical Exam
Blood Tests to Assess Hormone Levels
Ultrasound to Check Ovarian Health
Treatment Options
Lifestyle Modifications: A balanced diet and regular exercise help manage weight and improve insulin sensitivity.
Medications: Birth control pills, anti-androgen medications, and insulin-sensitizing drugs like Metformin.
Fertility Treatments: Ovulation induction medications for women trying to conceive.
Hair and Skin Treatments: To manage excessive hair growth and acne.
Why Choose Hiremath Hospital for PCOS Treatment?
Dr. Bharti Hiremath and her team at Hiremath Hospital provide patient-centric, compassionate care tailored to each woman’s unique needs. With advanced diagnostic tools and holistic treatment approaches, they ensure the best outcomes for managing PCOS effectively.
If you are experiencing symptoms of PCOS and need expert guidance, book a consultation with Dr. Bharti Hiremath at Hiremath Hospital today. Early diagnosis and appropriate management can help improve your quality of life and reproductive health.
#caesarean section specialist in pcmc#gynecologist in pcmc#normal delivery in pcmc#painless devlivery in pcmc#pcos treatment in pcmc
0 notes
Text
Understanding PCOS: Unravelling the Complexity of a Common Hormonal Disorder
Hello and welcome back to Shining Through PCOS! Today, we’re diving deeper into what PCOS really is, how it’s diagnosed, and the unique ways it affects women.
What is PCOS?
Polycystic Ovarian Syndrome (PCOS) is more than just a hormonal imbalance; it's a multifaceted condition that affects approximately 1 in 10 women of reproductive age around the globe (Singh et al., 2023). The symptoms can vary significantly, from irregular menstrual cycles to the presence of polycystic ovaries and elevated levels of androgens—often referred to as male hormones (Singh et al., 2023). One of the most challenging symptoms is hirsutism, characterised by the growth of coarse, dark hair in areas typically associated with male hair patterns, such as the face, chest, and back (Spritzer et al., 2022).
For many women, including myself, the emotional toll of excess hair growth is profound. It can feel like a constant battle against your own body, leading to feelings of frustration and embarrassment, especially when it’s in visible areas. I remember feeling overwhelmed by societal expectations of beauty while grappling with my own unwanted hair growth, leading me to seek out various treatments such as depilatory creams and shaving that only exacerbated my issue.
Diagnosing PCOS: The Complexity of Symptoms
Diagnosing PCOS is not always a straightforward process. This can be quite difficult because it can manifest so differently from woman to woman. In an attempt to help doctors better identify the condition, the Rotterdam criteria were introduced (Smet & McLennan, 2018). This diagnostic tool provides a standardised way to assess whether someone has PCOS by looking at three key factors:
Irregular or absent periods – This signals potential ovulatory dysfunction.
Signs of hyperandrogenism (excess androgens) – Such as excess hair growth, acne, or thinning hair on the scalp.
Polycystic ovaries on an ultrasound – Where the ovaries show multiple, small cysts.
To meet the diagnosis of PCOS, two out of these three criteria must be present. What’s important to note is that you don’t need to meet all three, which can lead to different manifestations of PCOS depending on the patient (Smet & McLennan, 2018). However, the absence of a universal diagnostic test can lead to delays in receiving proper care.
Many women find themselves navigating a confusing landscape where symptoms overlap with other conditions, making it crucial for us to advocate for our health. Often, healthcare providers may overlook the complexity of PCOS, attributing symptoms solely to lifestyle factors or weight issues, rather than considering the broader hormonal picture (Dewani et al., 2023).
The Hormonal Landscape and Its Impact on Women
The hormonal imbalance at the heart of PCOS doesn’t just affect our reproductive health; it also has significant implications for our metabolic and emotional well-being. Women with PCOS are at a higher risk of developing insulin resistance, which can lead to weight gain and complicate our ability to manage our symptoms (Barber et al., 2019). This can create a vicious cycle, where weight gain exacerbates hirsutism, making it even more challenging to feel a sense of autonomy over our bodies (Barber et al., 2019).
Moreover, the psychological aspects of PCOS are often overlooked. Many women report feelings of anxiety and depression associated with their symptoms, which can be exacerbated by societal pressures and beauty standards (Almhmoud et al., 2024). When we look at the prevalence of conditions such as generalised anxiety and depressive disorders amongst diagnosed women with PCOS, the rate is between 28% and 39% for anxiety, and 11% to 25% for depression (Dewani et al., 2023). This makes it all the more essential to recognise that PCOS is not just a reproductive disorder but a condition that impacts many facets of our lives.
The Role of Laser-Based Hair Reduction (LBHR)
For women dealing with hirsutism, finding effective and long-lasting treatment options can feel like a constant battle. One treatment that has gained significant attention is Laser-Based Hair Reduction (LBHR), which offers a long-term solution for managing excessive hair growth (Hosseini et al., 2022). Although it's not a cure for PCOS, LBHR can help in controlling a key symptom: unwanted hair growth.
As someone who has experienced this issue firsthand, and as a dermal clinician who has seen numerous patients benefit from LBHR, I truly feel that this treatment can help empower women by giving them a sense of control over their bodies. I’ve seen women come into the clinic feeling closed off, hesitant, and unsure during their first consultation. But as their treatments progress, something amazing happens—their confidence begins to grow. Session after session, they become more comfortable in their own skin, seeing results and no longer feeling defined by their unwanted hair. It’s truly rewarding to witness that transformation, especially as this is something that hits very close to home.
In saying this, it's important to have a clear understanding of what LBHR can—and cannot—achieve. While LBHR significantly reduces the rate of hair regrowth, it does not address the underlying hormonal imbalances that cause hirsutism in PCOS. PCOS is a chronic hormonal condition, and excess androgens (male hormones) will continue to trigger hair growth even after several laser sessions (Kopera et al., 2010). What LBHR does is target the melanin within the hair follicle, slowing down the process by damaging these follicles, leading to thinner, finer hair that delays the growth process over time (Bhat et al., 2020).
It’s important to note that LBHR typically requires multiple sessions spaced out over several weeks to months, as hair grows in cycles, and laser treatments target hair follicles during their active growth phase (anagen phase). In my experience, patients usually see optimal results after 6 to 8 sessions, but individual responses vary based on factors like skin type, hair texture, and hormonal fluctuations (Bhat et al., 2020). This makes a personalised treatment plan crucial.
One thing I always emphasise to patients is that LBHR isn’t a quick fix, but rather a long-term management tool. Even after completing the initial series of treatments, most women with PCOS will need maintenance sessions to keep hair growth under control. While it can significantly improve quality of life by reducing the need for constant hair removal methods like shaving, waxing, and depilatory creams, LBHR should be viewed as part of a comprehensive approach to managing PCOS—not a stand-alone solution (Sheehan, 2004).
Combining LBHR with treatments that address hormonal imbalances, such as medication (like anti-androgens) or lifestyle changes, ensures the most effective, lasting results (Tan et al., 2024). Think of it as attacking an issue from every angle to ensure the best outcome. In this way, LBHR becomes a cornerstone in a broader PCOS management plan, helping to reduce the emotional and physical toll of hirsutism while maintaining realistic expectations for long-term hair control.
Finding the Right Treatment Path for You
Navigating PCOS requires a holistic approach. From my experiences, having a healthcare provider who understands both the medical and aesthetic aspects of treatment is essential. We spoke earlier about combination therapies, but a similar multidisciplinary approach, including endocrinologists, dermatologists, and even nutritionists, can help us manage our symptoms in the most effective way.
In my own journey, I learned that addressing the root causes of PCOS—rather than just its symptoms—is the key to achieving lasting relief. This isn’t a standalone task and involves lifestyle changes alongside medical treatments tailored to my needs.
In future posts, we’ll explore these topics in more depth, discussing the science behind PCOS, how it affects hair growth specifically, and how we can navigate the challenges many women face while managing this condition. My hope is that by sharing these insights, we can create a supportive community for all of us living with PCOS as a collective.
Thank you for joining me as we unravel the complexities of PCOS and its impact on our lives. Together, let’s empower ourselves and others to take control of our health and well-being.
Until next time, L ᥫ᭡
References
Almhmoud, H., Alatassi, L., Baddoura, M., Sandouk, J., Alkayali, M. Z., Najjar, H., & Zaino, B. (2024). Polycystic ovary syndrome and its multidimensional impacts on women’s mental health: A narrative review. Medicine, 103(25), e38647. https://doi.org/10.1097/md.0000000000038647
Barber, T. M., Hanson, P., Weickert, M. O., & Franks, S. (2019). Obesity and polycystic ovary syndrome: Implications for pathogenesis and novel management strategies. Clinical Medicine Insights: Reproductive Health, 13, 117955811987404. https://doi.org/10.1177/1179558119874042
Bhat, Y. J., Bashir, S., Nabi, N., & Hassan, I. (2020). Laser treatment in hirsutism: An update. Dermatology Practical & Conceptual, e2020048. https://doi.org/10.5826/dpc.1002a48
Dewani, D., Karwade, P., & Mahajan, K. S. (2023). The invisible struggle: The psychosocial aspects of polycystic ovary syndrome. Cureus. https://doi.org/10.7759/cureus.51321
Hosseini, M. H., Ehsani, A. H., Fakour Y., Aryanian Z., Elhamfar M., & Noormohammadpour P. (2022). Effect of Laser-Assisted Hair Removal (LAHR) on the Quality of Life and Depression in Hirsute Females: A Single-Arm Clinical Trial. J Lasers Med Sci, 13. https://doi.org/10.34172/jlms.2022.46
Kopera, D., Wehr, E., & Obermayer-Pietsch, B. (2010). Endocrinology of hirsutism. International Journal of Trichology, 2(1), 30. https://doi.org/10.4103/0974-7753.66910
Sheehan, M. T. (2004). Polycystic ovarian syndrome: Diagnosis and management. Clinical Medicine & Research, 2(1), 13-27. https://doi.org/10.3121/cmr.2.1.13
Singh, S., Pal, N., Shubham, S., Sarma, D. K., Verma, V., Marotta, F., & Kumar, M. (2023). Polycystic ovary syndrome: Etiology, current management, and future therapeutics. Journal of Clinical Medicine, 12(4), 1454. https://doi.org/10.3390/jcm12041454
Smet, M. E., & McLennan, A. (2018). Rotterdam criteria, the end. Australas J Ultrasound Med, 21(2), 59-60. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8409808/
Spritzer, P. M., Marchesan, L. B., Santos, B. R., & Fighera, T. M. (2022). Hirsutism, normal androgens and diagnosis of PCOS. Diagnostics, 12(8), 1922. https://doi.org/10.3390/diagnostics12081922
Tan, K., Coster, T., Mousa, A., Mar, A., Piltonen, T., Boyle, J. A., Teede, H., Joham, A., Romualdi, D., & Tay, C. T. (2024). Laser and light-based therapies for hirsutism management in women with polycystic ovarian syndrome. JAMA Dermatology, 160(7), 746. https://doi.org/10.1001/jamadermatol.2024.0623
7 notes
·
View notes
Text
PCOD/PCOS Treatment in Jagatpura Jaipur - Dr. Chandrakanta Sulaniya Gynae-Oncology Center
Polycystic Ovary Syndrome (PCOS) or Polycystic Ovary Disease (PCOD) is a common hormonal disorder that affects women of reproductive age. It leads to irregular menstrual cycles, excessive hair growth, acne, weight gain, and even fertility issues. If you're living in Jaipur, particularly in the Jagatpura area, and are struggling with PCOD/PCOS, there is good news! You don’t need to suffer in silence or go through a trial-and-error approach to find a solution. Dr. Chandrakanta Sulaniya Gynae-Oncology Center, located in Jaipur, offers personalized and expert PCOD/PCOS treatment options that can help you regain control over your health.
Understanding PCOD/PCOS
PCOD/PCOS is a condition where a woman's ovaries produce an abnormal amount of androgens (male hormones). This hormonal imbalance can disrupt the menstrual cycle and lead to the development of cysts in the ovaries. Symptoms can vary from woman to woman, but common signs include:
Irregular or missed periods
Difficulty in conceiving
Weight gain
Excessive hair growth on the face, chest, or abdomen
Thinning hair on the scalp
Acne and oily skin
Depression or anxiety
While PCOD and PCOS are often used interchangeably, PCOS is the more severe condition with long-term consequences if left untreated. It is crucial to consult a qualified gynecologist for a proper diagnosis and treatment plan.
Dr. Chandrakanta Sulaniya - Expertise in Gynaecology and Gynae-Oncology
Dr. Chandrakanta Sulaniya is a highly experienced Gynaecologist in Jaipur with specialized knowledge in Gynae-Oncology. Her expertise in the management of PCOD/PCOS makes her a go-to specialist for women in Jagatpura and across Jaipur. With years of practice, Dr. Sulaniya is known for providing compassionate care and cutting-edge medical solutions tailored to each patient’s unique needs.
The Dr. Chandrakanta Sulaniya Gynae-Oncology Center has state-of-the-art facilities, ensuring that every patient receives the highest standard of care. Whether you’re looking for PCOD/PCOS treatment or need expert advice on managing gynecological health, the center is equipped to offer comprehensive care.
Treatment for PCOD/PCOS at Dr. Chandrakanta Sulaniya Gynae-Oncology Center
When it comes to treating PCOD/PCOS, a one-size-fits-all approach does not work. At Dr. Chandrakanta Sulaniya Gynae-Oncology Center, each patient’s treatment plan is personalized. Here’s what the center offers:
Comprehensive Diagnosis Dr. Sulaniya starts by conducting a thorough examination and lab tests to confirm whether you have PCOD/PCOS and determine the severity. The diagnosis includes blood tests, pelvic ultrasound, and hormone level assessments.
Medication Medication plays a significant role in managing the symptoms of PCOD/PCOS. Dr. Sulaniya may prescribe hormonal medications like birth control pills to regulate menstrual cycles or anti-androgen medications to control excess hair growth. For women trying to conceive, fertility treatments may also be recommended.
Lifestyle Modifications Adopting a healthy lifestyle is crucial for managing PCOD/PCOS. Dr. Sulaniya emphasizes a balanced diet and regular exercise. She works with patients to develop a sustainable nutrition plan and exercise routine that can help in managing weight, which is essential for reducing symptoms.
Surgical Intervention (If Necessary) In some cases, when other treatments don't show results, surgical interventions like laparoscopic ovarian drilling might be considered. This procedure can help stimulate ovulation and restore regular menstrual cycles.
Psychological Support PCOD/PCOS can often lead to emotional stress, anxiety, or depression. Dr. Sulaniya takes a holistic approach by offering emotional support, counseling, and stress-relieving techniques that can help women cope with the challenges of living with PCOD/PCOS.
Follow-up Care Continuous monitoring of the condition is essential for ensuring the effectiveness of the treatment. Dr. Sulaniya provides regular follow-up care to track the patient’s progress and make adjustments to the treatment plan if necessary.
Why Choose Dr. Chandrakanta Sulaniya Gynae-Oncology Center in Jagatpura, Jaipur?
Personalized Care: Dr. Sulaniya ensures every patient receives a customized treatment plan designed to meet their specific needs.
Experienced Gynaecologist: With years of experience in treating PCOD/PCOS and other gynecological issues, Dr. Sulaniya is well-known for her expertise and patient care.
Advanced Medical Facilities: The clinic is equipped with the latest technology for diagnosing and treating PCOD/PCOS, making your treatment journey smoother and more effective.
Holistic Approach: The center takes a holistic approach, addressing not just the physical symptoms but also the emotional and psychological well-being of patients.
Convenient Location: Located in Jagatpura, Jaipur, the clinic is easily accessible for residents in and around Jaipur.
Conclusion

PCOD/PCOS can be a challenging condition to manage, but with the right treatment, it is possible to lead a healthy and fulfilling life. If you're looking for PCOD/PCOS treatment in Jagatpura Jaipur, Dr. Chandrakanta Sulaniya Gynae-Oncology Center is your trusted destination for expert care. Consult Dr. Sulaniya today and take the first step toward a healthier tomorrow!
0 notes
Text
Best Doctor for PCOS in Hyderabad – Dr. Vindhya Gemaraju
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder affecting millions of women worldwide. It is a condition that requires expert medical attention to manage symptoms and improve overall health. In Hyderabad, one of the most renowned doctors for PCOS treatment is Dr. Vindhya Gemaraju. With her vast experience, patient-centric approach, and expertise in treating hormonal disorders, she has earned a strong reputation among women seeking effective management of PCOS.

Understanding PCOS
PCOS is a complex hormonal condition that affects the ovaries, leading to irregular menstrual cycles, excessive androgen levels, and the formation of small cysts on the ovaries. The common symptoms of PCOS include:
Irregular periods or no periods at all
Excessive hair growth (hirsutism)
Acne and oily skin
Weight gain and difficulty losing weight
Thinning hair or hair loss
Insulin resistance and risk of diabetes
Fertility issues
If left untreated, PCOS can lead to serious health complications such as type 2 diabetes, heart disease, and infertility. That is why consulting a specialist like Dr. Vindhya Gemaraju is crucial for early diagnosis and proper treatment.
Why Choose Dr. Vindhya Gemaraju for PCOS Treatment?
Dr. Vindhya Gemaraju is a highly skilled and experienced doctor specializing in the treatment of PCOS and other hormonal disorders. Here’s why she is considered the best doctor for PCOS in Hyderabad:
1. Extensive Experience and Expertise
Dr. Vindhya Gemaraju has years of experience in diagnosing and treating PCOS. Her deep understanding of hormonal imbalances and reproductive health makes her an excellent choice for women struggling with PCOS-related issues.
2. Holistic and Personalized Treatment Plans
Each patient’s condition is unique, and Dr. Vindhya Gemaraju follows a personalized approach to treatment. She designs customized treatment plans based on individual symptoms, medical history, and lifestyle factors. Her holistic approach includes:
Diet and lifestyle modifications
Medications to regulate hormones
Weight management strategies
Fertility treatments for those trying to conceive
3. Advanced Diagnostic Techniques
Dr. Vindhya uses state-of-the-art diagnostic methods to accurately assess and diagnose PCOS. Some of the tests she may recommend include:
Ultrasound scans to check ovarian cysts
Hormonal blood tests
Insulin resistance assessment
4. Comprehensive Care for Women’s Health
Beyond PCOS treatment, Dr. Vindhya Gemaraju also provides comprehensive women’s healthcare services, including:
Menstrual disorder management
Fertility treatments
Thyroid disorder management
Weight management programs
Patient Testimonials
Many patients have shared positive feedback about their experience with Dr. Vindhya Gemaraju. Here are a few testimonials:
“Dr. Vindhya Gemaraju is the best doctor for PCOS in Hyderabad. Her approach to treatment is very effective, and she genuinely cares for her patients.”
“I had been struggling with irregular periods and weight gain for years. After consulting Dr. Vindhya, I saw significant improvements in just a few months.”
“Her guidance and treatment helped me conceive after battling infertility due to PCOS.”
How to Book an Appointment with Dr. Vindhya Gemaraju
If you are looking for the best doctor for PCOS in Hyderabad, you can schedule a consultation with Dr. Vindhya Gemaraju. She practices at top medical facilities in Hyderabad and offers both in-person and online consultations for patient convenience.
Contact Details:
Phone Number: +91 8522 8692 78, 810 6688 026
Website: Laparoscopic Surgeon Hyderabad
Link: Best Doctor for PCOS in Hyderabad
Clinic Address: 8-1-284/OU, Plot No 541 Pokkalwada, OU Colony, Shaikpet, Hyderabad, Telangana 500008
Conclusion
PCOS is a challenging condition, but with the right medical guidance, it can be effectively managed. Dr. Vindhya Gemaraju is a leading expert in PCOS treatment in Hyderabad, known for her patient-focused approach, advanced treatment methods, and commitment to women’s health. If you are experiencing symptoms of PCOS, don’t wait—schedule an appointment with Dr. Vindhya Gemaraju today for expert care and comprehensive treatment.
#gynecologist in shaikpet#vnotes specialist in hyderabad#gynecologist in hyderabad#best doctor for pcos in hyderabad#top gynecologist in shaikpet#best gynecologist in hyderabad#best vnotes specialist in hyderabad#best gynecologist in shaikpet#top vnotes specialist in hyderabad
0 notes