#outbreak of diarrhea
Explore tagged Tumblr posts
Text
बालोद: स्वास्थ्य अधिकारी ने ग्रामीण से मांगी माफी, शिविर में की थी मजाकिया टिप्पणी। Health officer apologizes in Balod
Health officer apologizes in Balod: बालोद। छत्तीसगढ़ के ग्राम तरौद में उल्टी-दस्त से फैली बीमारी के कारण एक युवक की मौत हो गई है, जबकि 30 से ज्यादा लोग बीमार हैं। शुक्रवार को 40 वर्षीय मोहित निषाद की हालत बिगड़ने से मौत हो गई और चार लोग गंभीर हालत में हैं। गांव में लगाया गया स्वास्थ्य शिविर बीमारी फैलने के बाद गांव में स्वास्थ्य शिविर लगाया गया। इलाज के दौरान कुछ ऐसा हुआ जिससे ग्रामीणों का…
#Balod health camp controversy#CMHO Mahesh Suryavanshi comment#Diarrhea outbreak in Chhattisgarh#Health officer apologizes#Health officer apologizes in Balod#Villager death due to diarrhea
0 notes
Text
Stuff like this is why I get so pissed off at accusations of genocide and apartheid.
Why would a genocidal country pause a war to vaccinate at least 90% of Gaza kids against polio as soon as the first case of a two year old paralyzed by type 2 poliovirus is confirmed? If they wanted gazans wiped off the earth they would keep the war going and vaccinate Israeli kids and citizens. If they wanted them dead they would never vaccinate “the enemy.” Russia wouldn’t do that.
I see you dickheads in the comments, “it’s for optics! Plus they must be worried about Jews getting it from them! That’s the only reason they want to vaccinate anyone. Plus vaccines are poison even checked by the WHO! They probably have autism in them!”
If it’s an apartheid why would Palestinians have access to the same places and bodies of water as Israelis? And if they don’t why would Israel vaccinate. The Regan administration didn’t respond to the HIV outbreak in the 80s because they hated gays and drug users and wanted them sick, spreading it, and most importantly dead. During peace time to their own citizens.
All Israel would have to do is ignore the outbreak.
Vaccines work. Polio is one of the most devastating diseases a kid can get. There’s no medication that can stop the damage once you get the virus. Lil kids die from diarrhea, are paralyzed for life and if they’re immune system doesn’t stop the paralysis at their legs it climbs up their bodies and once it hits their diaphragm (the muscle that lets you breath right under your rip cage) kids as young as a few months old to their teens will die from lack of air. Both are the absolute worst and most painful ways a person can die. Waking nightmare delusions from dehydration and low oxygen on top of the physical pain.
Nazis infected Jews with this shit intentionally to study how polio affects children. Israel is stopping in the middle of a war to end the polio outbreak when they are still trying to rescue kids so young they have spent the majority of their lives on earth in Hamas captivity. And after only one kid was confirmed with polio type 2, the one that causes paralysis.
How can it be a genocide or an apartheid when they are literally helping safeguard Palestines next generation of kids?
#genocide#israeli#israeli apartheid#israeli genocide#israel treat their “enemy” better than the american gov treats it's own citizens#jumblr#antisemitism#leftist antisemitism#hamas#palestine#gaza#if you think preventing kids from getting mortal illness is ever wrong than you are a monster
463 notes
·
View notes
Text
Good Omens Historical Trivia That's Haunting Me Today...
So we all know A.Z. Fell & Co is located on the fictitious Whickber Street in Soho and was established in 1800.

Aziraphale has run the shop ever since then and was in contact with Crowley at least until the 1820's when they took their little jaunt to Edinburgh and Crowley got sucked down the tube slide to Hell. They meet up again no later than the 1860's, when Crowley asks for Holy Water.
Stands to reason that between the 1820's and 1860's Aziraphale was in Soho doing Aziraphale things. Running his bookshop. Eating tiny cakes
Yeah... you know what else was going on in Soho during that time?
The worst cholera epidemic in London history.
If you don't know, cholera is a deadly bacterial infection caused by drinking contaminated water. Prior to the 1850's humans weren't really sure what caused cholera, but they knew it was terrifying and also that it was absolutely epidemic in big cities.
TW: this is gross - The main symptoms of cholera are agonizing stomach pain and non-stop watery diarrhea, eventually leading to the skin turning blue due to the thickening of blood from severe dehydration. Patients can lose more than 20% of their body weight in hours as they quite literally evacuate every drop of water in their bodies until they die of heart failure. - OK gross part over
Cholera symptoms show up as short as 5 hours after infection and could kill within as little as 12 hours. Cholera was especially terrifying because of how quickly and painfully it killed you, and because the patient maintained mental clarity up until the point of death. More than half of the people who contracted cholera died within a few days after consuming the bacteria-contaminated water.
And guess what water had cholera bacteria in it?
The public water pump on Broad Street in Soho in August of 1854

And this wasn't one of those epidemics that starts slowly and drags on. It hit like a bomb. It killed 600 Soho residents in ten days.
That's roughly 60 people a day in a 3-4 block area. Most of them died at home because the disease struck too quickly for them to to make it to a hospital. Survivors described hearses stacked with coffins 4-5 high going down the street nonstop all day long during the outbreak. Entire families were wiped out overnight.
What does that have to do with Good Omens?
Aziraphale's book shop was right in the epicenter of this outbreak.
Neil Gaiman has been pretty free about the fact that Whickber Street is a thinly veiled expy of the real Berwick Street in Soho.
This is a famous map showing the 1854 Soho Cholera epidemic. I highlighted Berwick Street and the public water pump that was the center of the contagion. The black bars (I circled a few in blue) on the map designate deaths. The thicker the black bar, the more people died in that particular house.
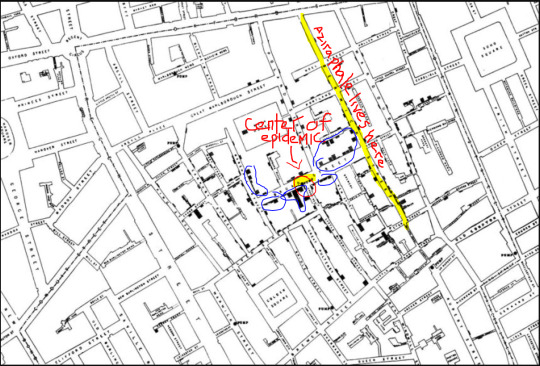
51 people died the week of the cholera outbreak on Aziraphale's Street alone.
Cholera was one of those diseases that provoked a lot of panic, not just because of how fast and painful it was, but because of the way it didn't follow common conventions about class or age. Children died while the elderly survived (often because the elderly had no one to gather water for them). Lower class houses were spared while their middle class landlords died. Churches were packed that week, because people in Soho had no idea who would get sick next. The epidemic pretty much burned itself out in a week and a half, since by that point everyone who drank the water had already died. I have to wonder what our resident Angel was up to during that time. Obviously cholera can't hurt him, but that's his neighborhood. There's no way hundreds of people, including entire families with children, are dying painfully in his neighborhood and Aziraphale doesn't notice. That means that in between this scene:

And this one:

Aziraphale would have watched one of the worst disease outbreaks in London history play out right outside his front door. I feel like there's great potential for a good story there if anyone better than me wants to write it.
#good omens meta#cholera#how often do those two tags go together#aziraphale#good omens history facts
539 notes
·
View notes
Text
McDonald's Quarter Pounders Linked to Multistate E.coli outbreak
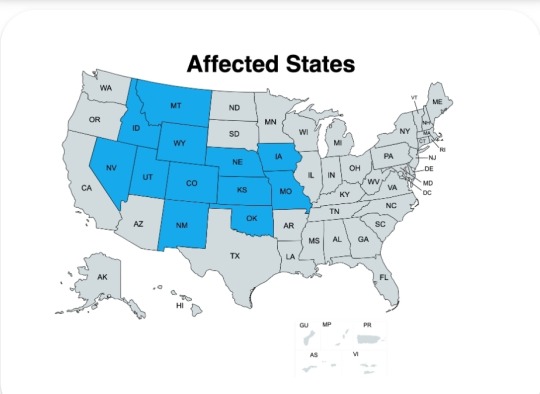
October 22, 2024
49 Sick, 1 dead
E.coli symptoms: Severe stomach cramps, diarrhea, fever, nausea, and/or vomiting.
The preliminary traceback indicates that the source of contamination was likely from the slivered onions.
227 notes
·
View notes
Text
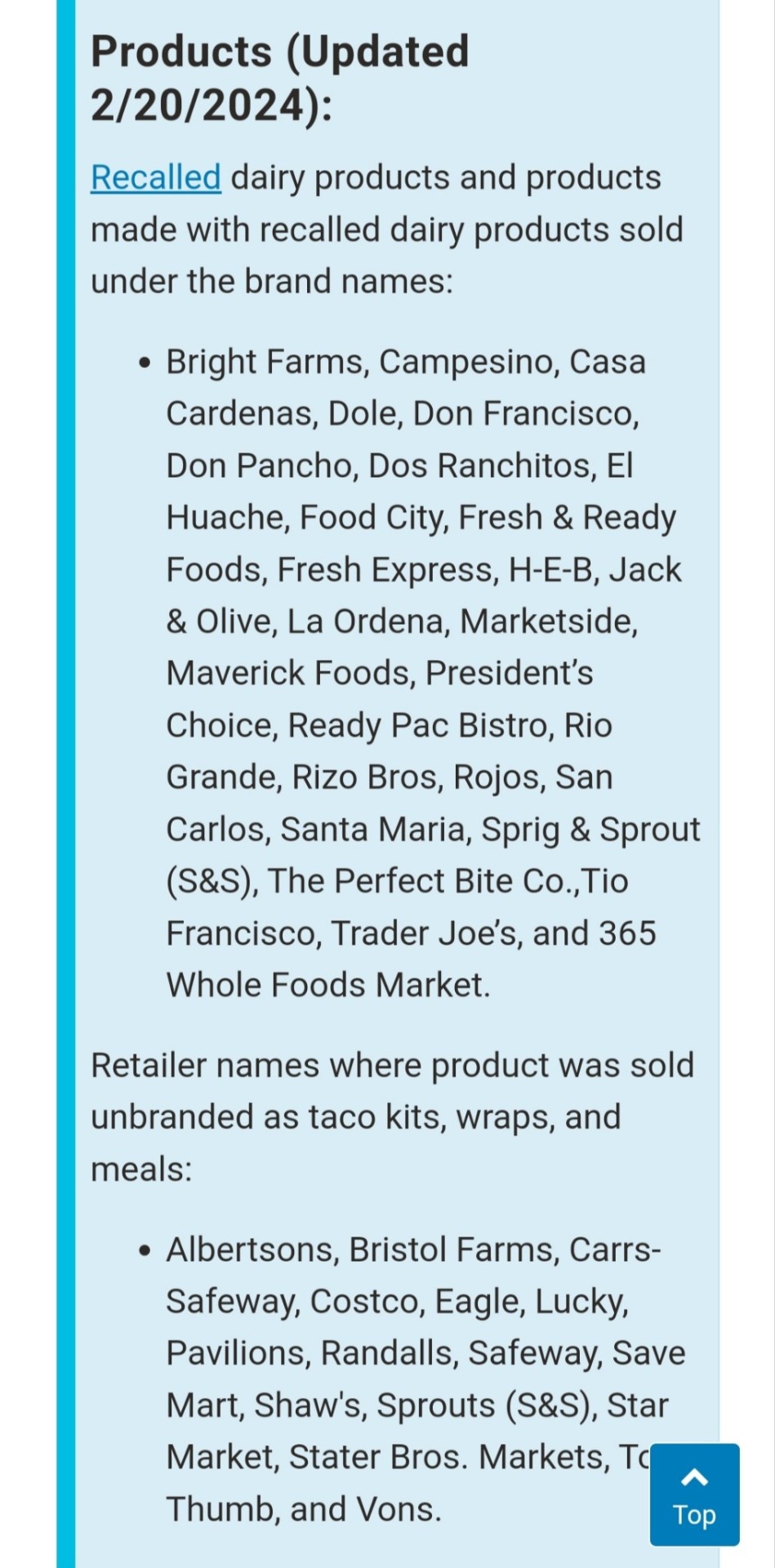
FreshRealm is recalling chicken fettuccine alfredo products due to potential Listeria monocytogenes contamination. The affected products were distributed to Kroger and Walmart locations nationwide in the United States. The issue was identified during an investigation into a Listeria outbreak affecting 17 people in 13 states. The recall was initiated on June 17, 2025. The investigation is ongoing to determine the contamination source. Product Details: - Brand: Marketside - Product: Grilled Chicken Alfredo with Fettuccine - Size: 32.8 oz. - Item Number: EST. P-50784 / EST. P-47770 / EST. P-47718 - Use By Dates: 06/27/2025 or prior - Brand: Marketside - Product: Grilled Chicken Alfredo with Fettuccine and Broccoli - Size: 12.3 oz. - Item Number: EST. P-50784 / EST. P-47770 / EST. P-47718 - Use By Dates: 06/26/2025 or prior - Brand: Home Chef - Product: Heat & Eat Chicken Fettuccine Alfredo - Size: 12.5 oz. - Item Number: EST. P-50784 / EST. P-47770 / EST. P-47718 - Use By Dates: 06/19/2025 or prior In case you are experiencing Listeria monocytogenes symptoms such as high fever, severe headache, stiffness, nausea, abdominal pain, and diarrhea, it is important to report it. It can help to detect & resolve outbreaks early and prevent others from being harmed, and it enables better surveillance. If symptoms persist, seek medical care.
24 notes
·
View notes
Photo

Plague in the Ancient & Medieval World
The word 'plague', in defining a lethal epidemic, was coined by the physician Galen (l. 130-210 CE) who lived through the Antonine Plague (165 - c. 180/190 CE) but the disease was recorded long before in relating the affliction of the Plague of Athens (429-426 BCE) which killed many of the city's inhabitants, including the statesman Pericles (l. 495-429 BCE). This epidemic, and some of the others that followed, may or may not have been actual plague as it was later defined; ancient writers tended to use the term plague for any widespread outbreak of pestilence.
Plagues certainly may have existed prior to the Athenian outbreak – and almost certainly did – but most studies of the epidemic begin with Athens as it is the first recorded by an eyewitness and survivor, the historian Thucydides (l. 460/455 - 399/398 BCE). Plagues are routinely named either for the person who reported them, the monarch at the time of the outbreak, the region afflicted, or by an epithet as in the case of the Black Death.
The major recorded plagues of the ancient and medieval world are:
Plague of Athens
Antonine Plague
Plague of Cyprian
Plague of Justinian
Roman Plague
Near East Plagues
Black Death
Columbian Exchange Epidemics
Of these, the Columbian Exchange Epidemics are not considered plague as they were a sweeping contagion of smallpox and other diseases but were just as lethal to the indigenous people of the Americas as plague was elsewhere. Other epidemics not considered plagues but which still ravaged populations were leprosy – especially during the 11th century CE in Europe – and the Japanese smallpox epidemic of 735-737 CE. Epidemics and pandemics continued into the modern era and, among the deadliest, were the 1918-1919 CE Spanish Flu epidemic and the HIV/AIDS epidemic (1981-present) though there were many others. At the time of this writing, the Covid-19/coronavirus is proving itself the latest addition to the list of most lethal pandemics in world history.
Nature & Types of Plague
The cause of the plague was unknown until the 19th century CE when the bacterium Yersinia pestis was isolated and identified in 1894 CE. Prior to that time, plague was thought to be supernatural in origin, a punishment from the gods or God, and/or the result of a population's sin. The actual cause was Yersinia pestis which was carried in the fleas of rodents, most often rats, which transmitted the bacterium to humans through bites. Other animals could catch the plague by eating rats – or other rodents – which were infected and this would lead to an epizootic outbreak which then spread to human beings. People die of the plague because of the toxic nature of Yersinia pestis which compromises one's immune system while, at the same time, multiplying in the body. Since the compromised immune system can no longer fight against the toxins, the person dies.
Plague is always described as beginning with symptoms resembling the flu, which appear, usually, 3-7 days after one has become infected. The symptoms at first are chills, body aches, fever, and overall weakness, which then progresses to vomiting, diarrhea, dehydration, respiratory failure (in some cases), and death. The three types of plague are:
Bubonic: caused by the bite of a carrier flea. This plague attacks the lymph nodes, inflaming them, and the swollen nodes are then called buboes, hence the name.
Septicemic: caused by either an infected flea or contact with an infected animal. It attacks by entering the bloodstream and multiplying.
Pneumonic: caused by contact with an infected animal and spreads person-to-person through coughing. It attacks the lungs, rapidly multiplying, which triggers an immuno-response eventually shutting the lungs down and leaving the person to die of respiratory failure.
Of the following, the first three may or may not have been plague. Descriptions of them by eyewitnesses suggest they may have been typhus or smallpox outbreaks but could have been plague.
Continue reading...
36 notes
·
View notes
Text
💎 I love my team, I love my crew (Part 3/7)
Title from Super (SEVENTEEN)
ILMTILMC Part I ILMTILMC Part II
Summary: Priority is to get the sick members comfortable.
CW: emeto, diarrhea in the context of illness, nightmares
Sickies: Woozi/Jihoon + Joshua + Seungkwan + Minghao + S.Coups/Seungcheol Caretakers: Hoshi/Soonyoung + Wonwoo + DK/Seokmin + Vernon + Jun + Jeonghan + Mingyu + Dino/Chan
💎🐯
“Shh, he just fell asleep”, Wonwoo whispered, holding his index finger to his lips to indicate quiet. Soonyoung nodded in agreement and walked over to them as silently as possible. It was cute, really. Jihoon was sprawled all over Wonwoo’s lap, effectively trapping the rapper under him. His hair was braided back in a french braid - the dancer hadn’t even known Wonwoo knew how to do that - and he was wearing his pajamas. In sleep, the producer looked so young and peaceful, if not for the paleness and the flush on his cheeks.
And the fact that they were still in the bathroom with the smell of sickness heavy in the air.
“How is he?”, Soonyoung asked quietly and knelt down next to Wonwoo, watching Jihoon breathe deeply. He was sound asleep - hopefully he would stay that way. From what Soonyoung had heard the producer had really gone through it during the afternoon.
“Hasn’t thrown up in about maybe thirty minutes, I’d reckon. I managed to get him into clean clothes and take some fever reducers and the antiemetic he normally takes for his migraines. He basically passed out on me after that”, Wonwoo explained and sighed. “He’s really not feeling good. Anyways, what was that meeting about?”
“Shua-hyung, Cheollie-hyung and Minghao-yah are also sick”, Soonyoung explained, watching as Wonwoo frowned in concern, “it’s likely a very contagious stomach flu. We split into teams to take care of the sick members … as long as we still can.”
Soonyoung was well aware that his voice was trembling. If he was honest, he was terrified. An outbreak of illness had not been on his mind when they had left the harbor two days ago. Even more so, they had been happily playing table tennis without a care in the world only hours ago.
Now it was evening and nearly one-third of the members were down.
“It’s going to work out, Soonyoung-ah”, Wonwoo comforted him, though Soonyoung knew him well enough that there was doubt in his voice.
“Why don’t we lay Jihoonie down on a bed? You both can’t be comfortable like this”, Soonyoung suggested. He itched to do something to help.
Wonwoo nodded and sheepishly added: “I think I lost feeling in my ass about twenty minutes ago.”
It was a bit awkward to lift Jihoon, even with his small frame and low weight - even lower now after he had been throwing up for hours - in the cramped bathroom but they managed. Wonwoo nearly fell when standing up, even his legs seemingly asleep.
“Let’s put him on Dino’s bed”, Wonwoo whispered, gesturing with one hand to the stuffed otter that was decorating one of the two lower bunk. Soonyoung, who had lifted Jihoon to his chest, raised his eyebrows. The other lower bunk was clearly Jihoon’s, the only bed completely empty of stuffed animals or multiple pillows. “He said he threw up on his bedding. I don’t think any of us even had time to take care of that.”
Soonyoung grimaced and nodded, waiting for Wonwoo to pull back the covers so the dance leader could lay down his precious burden. Jihoon stirred a bit when he came in contact with the mattress and both older members held their breath in hopes he’d fall back asleep. Jihoon sighed in his sleep, pulled the stuffed otter to his chest and curled up. It was adorable really.
They covered him back up and Soonyoung couldn’t resist snapping a quick picture and sending it to the group chat. When he was better Woozi would likely kill him but for now Soonyoung thought the rest of the members might need a pick-me-up and Jihoon was very cute. Like a kitten. There was a reason why Carats called the 96-liners the cat-line.
“He will not like that”, Wonwoo commented but Soonyoung saw him save the picture to his gallery anyways. So he just shrugged. “Let’s get the bedsheets clean, I guess?”
Wonwoo nodded and then said: “Why don’t you stay with Jihoonie? I have been cooped up in the bathroom for some time, I need to walk around a bit.”
“Yeah, sure, if you don’t mind”, Soonyoung agreed easily. He didn’t really want to leave Jihoon’s side anyways.
“Nah, it’s fine.”
💎⚔️
“Oh, it’s you”, Seungkwan whispered, a bit dejectedly, when Seokmin entered the sleeping cabin he shared with Joshua, Mingyu and Wonwoo.
“Thank you. That doesn’t hurt at all”, Seokmin said, only slightly offended and closed the door. The room was now only illuminated by the light coming in even through the curtains. It took a few seconds for Seokmin’s eyes to adjust to the relative darkness but then he spotted Joshua laying down on his bed, eyes closed and breathing deeply, seemingly asleep. There was a bucket by his head.
As Seokmin looked around he nearly missed the dark silhouette sitting on the floor, leaning back against the bed across from Joshua’s. Seungkwan had his head bowed, knees pulled to his chest. Something was off.
“Sorry. I didn’t mean it like that, hyung”, the youngest vocalist whispered, “I just hoped for Jeonghannie-hyung or Cheollie-hyung. I … I don’t feel good.”
Dread electrified Seokmin’s whole body. No, this was going wrong too quickly. Did they have to add Seungkwan to the list of sick members this shortly after Seungcheol-hyung? Seokmin didn’t like to admit it but he was terrified. He didn’t have a problem with helping sick members even if they were throwing up, which wasn’t what everybody could stomach, but caring for two sick members on his own? No, that would not work. There was a reason why they had decided on teams of two after all.
Seokmin shook himself. He didn’t have time to worry about that. He had a dongsaeng to cuddle. Careful to not stub his toes in the dark, Seokmin made his way to Seungkwan and knelt down beside him, pulling the youngest BSS member against his side. Immediately Seungkwan curled into his arms, sighing constantly.
“What’s wrong, Kwan-ah?”, Seokmin asked worriedly, inconspicuously feeling the younger’s forehead. Seungkwan was warm, maybe a bit warmer than usual, but Seokmin couldn’t tell if it was a fever. He hoped they had a thermometer somewhere because even if it wasn’t a fever yet it would turn into one for sure.
“I feel nauseous”, Seungkwan mumbled, “I mean I saw Woozi-hyung and Joshua-hyung throw up but I don’t think this is just sympathy.”
Seokmin hummed, pressing a kiss to the top of his head. “Do you want to go up to the deck, see if some fresh air helps?”
Seungkwan sighed but nodded. Seokmin stood up and then pulled the younger to his feet. Seungkwan swayed for a moment but gained his balance before Seokmin got too worried.
But now that Seungkwan was standing, clutching the back of Seokmin’s shirt did the older vocalist realize he would have to split himself in two if he wanted to help Seungkwan up to the deck and keep an eye on Joshua at the same time. Well, Joshua was asleep. Maybe he could get a manager to keep an eye on him while he was with Seungkwan. Decision made, Seokmin took Seungkwan’s hand in his and gently led him out of the room.
“What about hyung?”, Seungkwan asked worriedly, swallowing after.
“He’s asleep. I’m sure we’ll find somebody who can look after him soon.”
They had barely taken a few steps into the direction of the stairs that would lead them up to the living room hallway and then consequently out on deck when they ran into Vernon.
“Hey”, the rapper greeted them, carrying a stack of clothes in his arms. Seokmin winced, understanding instantly what had happened.
“Nonie”, Seungkwan whispered and rushed to his best friend, basically throwing himself into his arms. Vernon nearly dropped the items he was carrying but managed to hold onto them and wrap Seungkwan into his arms at the last second. Worriedly, he looked over Seungkwan’s shoulder at Seokmin.
Before the older vocalist had a chance to explain, Seungkwan whimpered: “Don’t feel good, Nonie.”
Understanding bloomed on Vernon’s face, closely followed by worry. “Have you been sick?”, he asked, pulling away to muster his other half. Seungkwan shook his head.
“Feel like I might though”, he mumbled. Vernon sighed and rubbed his arm. He was surprisingly unfazed by the sickly member considering his squeamishness but then again Vernon could push past his distaste for vomit when Seungkwan was involved.
“I was about to take him up to the deck and see if that helps”, Seokmin explained, “but uh, actually, could you do that? We left Shua-hyung alone…”
“Yeah, let’s go”, Vernon replied, sneaking his arm around Seungkwan’s waist to support him on the short walk, “we just need to stop by Jun and Minghao.”
“Thanks, Nonie”, Seokmin said. “Feel better, Kwan-ah.”
The two left quickly and Seokmin turned around to go check on Joshua, feverishly hoping that his absence had not been noticed.
When he pushed the door open, guilt washed over him. Joshua was awake, sitting on the bed with his head in his hands. He truly had chosen the moment nobody was there for him to wake up. Hearing the door, Joshua turned to look at Seokmin. Even with the low light spilling inside, he winced and squeezed his eyes shut but not before Seokmin was able to see the tears in his eyes.
“Hyung”, he breathed and rushed over, “how are you feeling?”
“My head”, Joshua whispered, “it hurts so badly, Min-ah.”
“Do you want to try medication?”, Seokmin offered, feeling a bit helpless. Sure, he had seen the older members take care of Joshua and Woozi when they were in the grasp of a migraine but he felt seriously out of his depth now.
“I don’t know if I can keep them down”, Joshua admitted, “where are Hannie or Cheollie?”
Seokmin winced. Should he tell Joshua or not? Worry wouldn’t help the American but then again, keeping him in the dark was also not realistic. “We’re having a bit of a problem”, Seokin started to explain, wincing as he realized his first sentence was a big understatement. “A lot of members are sick at the moment. The medic said it’s likely norovirus. Next to you, Woozi-hyung, Minghao and Seungcheol-hyung are sick. Seungkwan might be too.”
“Oh.” Joshua looked stunned.
“Yeah.”
They were silent for a few seconds until Joshua was seemingly hit with another bout of pain. He closed his eyes and pressed his palms against his forehead, groaning. Seokmin internally panicked but knew he couldn’t really afford to. He spotted the ice pack that must have fallen off of Joshua when he woke up and grabbed it. It was still mostly cold. Relieved, he lifted it and took Joshua’s hands into his own to free his forehead. The hold Joshua had on his hand was painfully tight but it lessened a bit when the ice came into contact with his burning skin. They sat there, at the edge of the bed, for a few minutes with Joshua just breathing. Seokmin didn’t know what to do but be silent support.
Finally Joshua took one last deep breath in before asking: “Painkillers? They are with my bag, I think.”
Seokmin scrambled to his feet, happy to have something to help. He spotted the blister and within a minute he had gotten Joshua to drink a bit of water along with the pills.
“Do you want to lie back down?”, he asked then.
“No”, Joshua choked out, “I think I feel better sitting up. Even my head. Min-ah, I’m sorry, but can you hand me the bucket just in case?”
Worriedly Seokmin bent down and lifted it up into his hyung’s lap. Joshua mumbled a small “thanks” and bent over it, one arm coming to rest on the rim and his head laying down on it. Seokmin, not sure how else to comfort him, just ran his hand up and down his back.
Watching his hyung nauseously bent over a bucket, occasionally swallowing down gags was not subject to his entertainment tax. Seokmin looked away, staring into the mostly dark room not that the sun had apparently started to set. He wondered how Seungkwan was faring. How Seungcheol and Woozi and Minghao were doing. Had any of the other members started to feel the effects of sickness already? Did he himself? He hadn’t paused yet to actually check in with his body on how he was doing.
Seokmin took a deep breath himself, trying not to freak himself out. But as he closed his eyes and focused on his head and stomach, he felt fine. There was no upset, nothing bothering his body except for maybe a tiny sunburn on his shoulders.
The vocalist was torn out of his thoughts by the sound of a nearly silent gag. He opened his eyes just in time to see a watery mouthful of vomit rush out of Joshua’s mouth into the bucket. There went the medication.
Joshua heaved a few times, Seokmin able to feel his back ripple under his hand but he brought nothing else up. It caused the vocalist to wonder if Joshua was empty and had nothing else to throw up in his system or if he had managed to keep himself from vomiting up more.
Then Joshua was whimpering, silent tears streaming down his face.
Now Seokmin couldn’t contain the panic anymore. “Hyung?”, he asked, rushing to put the bucket down and wrap the older in his arms. Joshua just shook, face buried in Seokmin’s shoulder. “What’s happening?”
“It hurts so much, Min-ah”, Joshua sobbed.
💎😸
“Xiao Ba, please let me in”, Jun begged, knocking on the bathroom door for the umpteenth time. Minghao hadn’t exactly … made it to the bathroom before his stomach had rebelled for the third time that day. The younger was terribly embarrassed and Jun got it, he really did. He’d feel humiliated too if he had soiled himself in front of another member even in the throes of illness. But it had caused Minghao to lock himself in the bathroom, sobbing so loudly and violently that Jun feared he would pass out due to dehydration before Jun managed to coax him out. Vernon appearing to help out had been as much of a curse as a blessing. Getting him to grab new clothes made everything just a tiny bit easier for Jun.
Yet, he was becoming terribly sick - pun not intended - of staring at the door for minutes on end, without being able to help his dongsaeng. He was just glad that a kind manager had cleaned the bathroom earlier and had even thought of putting a trash can inside. Plus, he had informed Jun of what he had done which had reassured the dancer a lot.
“Eissa, I know you are embarrassed”, Jun said defeatedly in Chinese - so very grateful for the bit of privacy it granted them - and let his head thunk against the wood, “but I promise you gege isn’t judging you or is angry or whatever you are thinking. You’re sick. It happens. Please, let me help you, baby.”
The lock firmly stayed in the occupied position.
Jun sank down to his knees and sat down awkwardly on the ground. It promised to be a long wait.
A minute passed. Two. Five. Ten.
Just as Jun was about to knock on the door again Vernon appeared, his arm slung around a pale looking Seungkwan. Jun scrambled to get to his feet, his hand immediately coming up to feel Seungkwan’s clammy cheek. He didn’t seem overly warm. But the paleness and especially the quietude made it obvious that Seungkwan was not feeling well.
“Oh, love, you too?”, Jun cooed.
“Haven't thrown up yet”, Seungkwan muttered. He looked like he would any moment now. Jun kept that thought to himself.
“We wanted to go outside, see if it helps a bit”, Vernon explained. Jun nodded in agreement. At least it couldn’t hurt.
“Go, go”, he said, ushering them to the door leading them outside, taking the change of clothes from Vernon in the same movement. He watched them trudge outside, Vernon never letting go of his best friend.
The ship was built with the hallway having a row of windows showing the deck outside, with the living room separated by a wall and the door outside and the bathroom on opposite short ends, with a tiny alcove with the stairs down to the sleep level. So Jun was able to watch them stand by the railing a bit longer, his only pastime. It was cute really, how Vernon was fussing over the vocalist.
A manager approached the two maknaes and conversed with Vernon for a moment, looking worried. Both of them started when suddenly Seungkwan leaned forward and presumably threw up over the railing. Jun couldn’t see but if it wasn’t obvious from the way Seungkwan was bent forward, his back moving with the retches, it was by Vernon brushing his fringe back and looking at the manager with panic.
Jun was brought out of his worries when Jeonghan and the medic emerged from the living room, both looking unhappy.
“How is Cheollie-hyung?”
“How is Minghao-yah?”
Jeonghan and Jun asked the questions nearly simultaneously, both chuckling a bit at the situation despite it not actually not being that funny. It was the small things helping them keep their sanity.
“Chan-ah and Mingyu got him”, Jeonghan replied. “He fell asleep on the couch, his fever is pretty high. Hyukjae-ssi…” - he gestured at the medic - “...is going to check out what medications we have available and the managers are trying to figure out a way to sail back. Apparently one of the managers with a sailing license is sick too, so we are not sure how to proceed. I wanted to go check on Shua and Jihoonie after this.”
“And Seungkwan, I guess”, Jun said, nodding his head in the direction of the sick member now sitting down with his back to the railing and Vernon and the manager kneeling beside him. Jeonghan sighed.
“And Seungkwan.”
“Minghao is … well, he’s pretty embarrassed”, Jun said, slightly awkward. He didn’t want to tattle on his dongsaeng but he knew Minghao needed help soon. And Jun, despite his closeness to him, was slowly doubting he’d get Minghao out of the bathroom any time sooner.
“Poor him”, Jeonghan sighed. They all stopped when the sound of coughing took up. Minghao was throwing up again.
“He’s throwing up and having diarrhea, right?”, the medic asked. Jun nodded.
“Fever?”
“Maybe a slight one.”
“He’s going to be dehydrated soon, if he isn’t already. Can you try to get him out? I have at least a few IV’s and he will likely need one if he can’t keep any fluids inside”, the medic said.
Jun nodded. “I’ll try.”
💎🐕
Mingyu wished himself back in time. Arguing with Seokmin over a lost table tennis match was so much better than seeing their members succumb to the sickness one by one. He most certainly wasn’t a big fan of puking and watching over Seungcheol after said leader had just spewed his stomach onto the floor and had fallen asleep clutching the plastic bag in his hands … Mingyu had to admit he wished he was somewhere far away.
Dino had curled up with a gloom look on his face by the leader’s head and was absently running his hands through Seungcheol’s hair. Mingyu himself had sat down on a chair further away, burying his head in his hands. He wanted to help but he’d also rather stay far far away.
“Hyung?”, Dino asked, sounding a bit concerned. He probably knew how Mingyu was feeling. The rapper had never hid the fact that vomit grossed him out. He just felt bad for burdening the maknae.
“Hm?”, he asked, lifting his head.
“Can you go get an ice pack from the kitchen? Cheollie-hyung is burning up”, Dino requested and then added with a wink: “And while you’re there, why don’t you check if we have ingredients for juk or galbitang? I’m sure the members will appreciate some light meals soon.”
It was a beautiful out. They truly had the best maknae. Minguy nodded and nearly stumbled into the doorway on his way to the kitchen. Inside he met a stylist noona, boiling water on the stove.
“Hello Mingyu-ssi”, she greeted with a smile, “I thought I could prepare some tea for the sick ones.”
“Thank you, noona. It’s very nice of you. I’m going to bring an ice pack to Cheollie-hyung and then maybe we can cook together?” Anything to get his mind of the sickness spreading and the noona was nice.
Mingyu returned to the living room just in time to find Dino trying to soothe an agitated Seungcheol. The leader was deeply asleep, it seemed, but trapped in a nightmare. He was tossing and turning, sweat pouring out of every pore and he seemed to be crying.
It tore at Mingyu’s heart strings to see their mat-hyung like that. Normally Seungcheol was emotionally so strong and while he had cried in their presence before - how could he have not in all the time they’ve known each other? - it hadn’t been this desperate for a long time, not since his anxiety was at its worst.
It had been years and years ago when Seungcheol had admitted to Mingyu during a sleepless night in a shared hotel room that part of the reason for his insomnia was the fear of nightmares. Mingyu had woken up to a crying and kicking leader, completely lost in the scenarios his brain came up with. Even with Seventeen famous and successful, Seungcheol had never been able to shake the fear of disbandment, the fear of losing his members like they had lost Doyoon, MingMing, Dongjin and Samuel before debut.
“Hyungie”, Mingyu whispered and within seconds he was on his knees in front of the couch, stroking back Seungcheol’s hair and trying to reduce his subconscious fears.
“I don’t know what happened”, Dino said, eyes blown wide, “he just started crying in his sleep.”
It was no wonder that Dino was so scared. He had likely never seen Seungcheol like this. It had been terrifying for Mingyu back then too, not knowing what to do when his friend wouldn’t wake up from his terror. Now Mingyu knew to gently rub his arms and talk to him, so that Seungcheol woke up feeling comforted not trapped when held down (which had been a mistake Mingyu had only made once).
“Nightmare. He’s had them since forever”, Mingyu explained. He felt bad that Seungcheol was going through this but he was also glad he could finally help. “Hold the ice pack to his forehead. Here. I’m gonna try to wake him up.”
Dino nodded and took the ice pack from Mingyu, nearly dropping it with his shaking hands.
“Don’t be scared, Chan-ah. I know it looks scary but Cheollie-hyung is gonna be fine, you’ll see.”
It took a few minutes of soothingly rubbing Seungcheol’s arm to stimulate him and whispered reassurances and comforting words before the general leader slowly calmed down and his eyes blinked open. Tears were still leaking out the corners of his eyes and he looked to be in pain but he was awake. The terror was gone, still his hands came up to clutch at Mingyu’s shirt.
“Ming’?”, Seungcheol whispered, his raspy voice swallowing down the last part of his name. He sounded so exhausted and his eyes, while open, were glazed over. Mingyu cupped the leader’s face and brushed a falling tear away with his thumb. Seungcheol’s skin was burning.
“I’m here, hyung. You’re okay. It was just a nightmare.”
“Nightmare?”, Seungcheol repeated, sounding young and lost. “I don’t … ‘gyu, I feel sick.”
Mingyu had no idea why the situation didn’t make him want to run away. If anything he wanted to stay closer to his hyung and comfort him, even if he threw up. There was so much vulnerability in his voice and such child-like innocence.
“It’s okay, we got you, hold on a sec if you can”, Mingyu promised even when Dino threw him a confused and concerned look.
The younger rapper helped Seungcheol move his feet off the couch and lifted the leader’s upper body into his embrace, so that Seungcheol was basically slumped against his chest. Dino quickly provided them with the plastic bag that Seungcheol nearly immediately lifted to his lips. The leader seemed exhausted and all his energy seemed to be going towards staying awake. His hands were shaking and Dino had to help him keep holding the bag open.
It took only a few seconds until Seungcheol started expelling more of his stomach contents, the bag quickly growing full. Mingyu held Seungcheol tightly, fearing the leader would fall over if he didn’t. One of his hands came down to press softly against Seungcheol’s stomach, hoping that it would help the leader’s pain.
Watching Seungcheol throw up was disgusting, the sight, sound and smell, everything a bit too much, but Mingyu couldn’t put his own comforts over his sick leader’s. And if he got sick, he got sick. He probably would get infected in the near future anyway. There was no way out.
It took a painful few minutes until Seungcheol stopped vomiting and by then he was so weak that he just fell back against Mingyu, curling up in his lap and softly crying again. Dino took the bag from his hands, tied it off and set it to the side.
“Hyungie?”, he asked, brushing back Seungcheol’s fringe. “Do you want to rinse out your mouth?”
Seungcheol shook his head. “Tired”, he whispered, more tears leaking from his eyes. “My head hurts. I just want to sleep. I don’t even know why I’m crying.” The last sentence was accented by an adorable pout that would have sent Mingyu squealing in any other situation.
“I think it’s the fever”, Mingyu mumbled, leaning down to press his lips to hot skin. “We need to get you cooled down.”
“I’ll get more ice packs”, Dino suggested and scurried off. Mingyu just continued rubbing his stomach, it seemed to comfort the leader at least a bit.
ILMTILMC Part IV
Masterlist links: Fairy's Masterlist 2024 Fairy's Masterlist 2025 Fairy's Masterlist - SEVENTEEN
#Kpop#Kpop blog#Kpop sick#Kpop sickfic#Sickfic#Emeto#🧚🏻♀️#Title from Super (SEVENTEEN)#Part 3/7#Seventeen#Seventeen sick#Sick seventeen#Seventeen sickfic#💎#🍒#😇#🦌#😸#🐯#🐈⬛#🍚#🐕#⚔️#🐸#🍊#🐢#🦖#Sick Woozi/Jihoon#Sick Joshua#Sick Minghao
43 notes
·
View notes
Text

Scavengers like turkey vultures remove millions of tons of waste each year by consuming carrion. U.S. Fish and Wildlife Service
Excerpt from this story from Smithsonian Magazine:
Scavengers are in trouble—and their decline could be harmful to human health.
With many of these creatures that feast on dead animals struggling to survive, scientists say their downfall could lead to a rise in infectious diseases among humans, according to a paper published Monday in Proceedings of the National Academy of Sciences.
For the study, researchers looked at 1,376 vertebrate species known to eat some amount of carrion, ranging from tiger sharks and spotted hyenas to cane toads and common shrews. When they investigated each animal’s status on the International Union for Conservation of Nature (IUCN) Red List, they found that 36 percent are threatened or decreasing in number.
When the team dug even deeper into the data, a more nuanced picture emerged. Large species and those that rely on carrion for survival tend to be imperiled, while smaller species and those that scavenge occasionally are thriving.
Obligate scavengers, or those that only consume carrion, are especially vulnerable. Half of the 17 obligate scavenger species included in the study are considered “vulnerable” or “critically endangered” by the IUCN.
That’s a bad dynamic, because in the wake of their disappearance, some smaller, occasional scavengers—known as mesoscavengers—are proliferating. These creatures, such as rodents and feral dogs, have a tendency to transmit diseases to humans. For example, places where mice and rats are the most abundant scavengers are more vulnerable to outbreaks of illnesses like the bacterial disease leptospirosis and the diarrhea-causing cryptosporidiosis.
In addition, mesoscavengers cannot adequately fill the roles left vacant as their larger counterparts disappear. Smaller scavengers often need to follow larger ones to find rotting carcasses on the landscape. And once they arrive, they typically must wait for the bigger creatures to rip open the decaying remains before they can dig in.
“As we went through the literature, it was a reoccurring pattern that mesoscavengers cannot functionally replace the carrion consumption,” lead author Chinmay Sonawane, a biologist at Stanford University, tells Science News’ Bethany Brookshire.
Why are some species proliferating while others are struggling? Some are just better at adapting to humans, the researchers write. Apex scavengers are disproportionately affected by activities like intensive livestock production, land use changes and the wildlife trade.
Hunters, for example, are more likely to target large animals for consumption and trade, according to the study. Beyond that, apex scavengers are sometimes killed accidentally—hyenas and lions can get caught in wire snares meant for herbivores in Africa. And when hunters kill too many prey animals, there’s often not enough left for scavengers to eat.
Apex scavengers may also accidentally consume toxic substances, such as poison intended for predators threatening livestock, or veterinary drugs found in livestock carcasses.
11 notes
·
View notes
Text
Yesterday, health officials in Louisiana announced that a patient who was hospitalized with severe bird flu in December has died. The individual contracted bird flu after exposure to a backyard flock and wild birds. It is the first death recorded in the United States attributed to H5N1, or avian influenza.
The person was over the age of 65 and reportedly had underlying medical conditions. The Louisiana Health Department has not released any more details about the patient.
A total of 66 people in the US tested positive for bird flu in 2024, according to the Centers for Disease Control and Prevention. In all of the other cases, people developed mild symptoms and made a full recovery. But the Louisiana case is a stark reminder that avian flu can be dangerous. And as the number of human infections rises, health experts worry about more cases of severe illness—and potentially more deaths.
“This is an ongoing game of Russian roulette,” says physician Nahid Bhadelia, founding director of the Center on Emerging Infectious Diseases at Boston University. “The more virus there is in our environment, the more chances there are for it to come into contact with humans.” It was only a matter of time before bird flu turned deadly, she says.
The US is in the middle of an H5N1 outbreak that shows no signs of stopping. The virus has infected more than 130 million birds, including commercial poultry, since January 2022. In April 2024 it spilled into dairy cows for the first time. Though not fatal for cows, the virus has sickened more than 900 dairy herds in 16 states.
Most people who come down with bird flu are farm workers or others who have direct contact with sick animals. Of the 66 confirmed infections in the US last year, 40 had exposure to dairy cows, while 23 had exposure to poultry and culling operations. In the three other cases, the exact source of exposure is unknown.
Since 2003, more than 850 human cases of H5N1 bird flu have been reported outside the United States, and about half of those have resulted in death. In a statement released Monday, the CDC said a death from H5N1 bird flu “is not unexpected because of the known potential for infection with these viruses to cause severe illness and death.” Federal health officials say the risk of getting bird flu remains low for the general public, and there is no evidence that the virus is spreading from person to person anywhere in the country.
One of the puzzling aspects of the current US outbreak is why all the human infections until now have resulted in mild illness. “It could be that they're young, healthy people,” says Jennifer Nuzzo, director of the Pandemic Center and a professor of epidemiology at Brown University. “It could be that the way they're being exposed is different from how we've historically seen people get infected. There are a number of hypotheses, but at this point they're all just guesses.”
Nuzzo says it’s very possible that the Louisiana patient’s preexisting health conditions contributed to the severity of their illness, but also points to the case of a teenager in Canada who was hospitalized with bird flu in November.
The 13-year-old girl was initially seen at an emergency department in British Columbia for a fever and conjunctivitis in both eyes. She was discharged home without treatment and later developed a cough, vomiting, and diarrhea. She wound up back in the emergency department in respiratory distress a few days later. She was admitted to the pediatric intensive care unit and went into respiratory failure but eventually recovered after treatment. According to a case report published in the New England Journal of Medicine, the girl had a history of mild asthma and an elevated body-mass index. It’s unknown how she caught the virus.
“What that tells us is that we have no idea who is going to develop mild illness and who is going to develop severe illness, and because of that we have to take these infections very seriously,” Nuzzo says. “We should not assume that all future infections will be mild.”
There’s another clue that could explain the severity of the Louisiana and British Columbia cases. Virus samples from both patients showed some similarities. For one, both were infected with the same subtype of H5N1 called D1.1, which is the same kind of virus found in wild birds and poultry. It’s different from the B3.13 subtype, which is dominant in dairy cows.
“Right now, the question is, is this a more severe strain than the dairy cattle strain?” says Benjamin Anderson, assistant professor of environmental and global health at the University of Florida. So far, scientists don’t have enough data to know for sure. A handful of poultry farm workers in Washington have tested positive for the D1.1 subtype, but those individuals had mild symptoms and did not require hospitalization.
“In the case of the Louisiana infection, we know that person had comorbidities. We know that person was an older individual. These are factors that contribute to more severe outcomes already when it comes to respiratory infections,” Anderson says.
In the Louisiana and British Columbia cases, there’s evidence that the virus may have evolved in both patients to produce more severe illness.
A CDC report from late December found genetic mutations in the virus taken from the Louisiana patient that may have allowed it to enhance its ability to infect the upper airways of humans. The report says the changes observed were likely generated by replication of the virus throughout the patient’s illness rather than transmitted at the time of infection, meaning that the mutations weren’t present in the birds the person was exposed to.
Writing in the New England Journal of Medicine, the team that cared for the Canadian teen also described “worrisome” mutations found in her viral samples. These changes could have allowed the virus to more easily bind to and enter cells in the human respiratory tract.
In the past, bird flu has rarely been transmitted from person to person, but scientists worry about a scenario where the virus would acquire mutations that would make human transmission more likely.
For now, people who work with birds, poultry, or cows, or have recreational exposure to them, are at higher risk of getting bird flu. To prevent illness, health officials recommend avoiding direct contact with wild birds and other animals infected with or suspected to be infected with bird flu viruses.
24 notes
·
View notes
Text
I love all of the small but important bonding moments we get in the show. We get multiple significant bonding moments every episode—I got you baby girl, it wasn’t time that did it, you deserve a choice, diarrhea is hereditary, etc.—but also so many tiny little things that make me so 😭❤️
Ellie asking Joel if they’re gonna be okay. Joel answering her questions about the outbreak. Joking together about music. Helping Ellie up when she falls. Ellie laying on him on the horse and in the basement. Joel asking for puns because he knows it makes Ellie happy. Letting her get some rest in the car. Telling her he knows it’s scary on the wooden plank. Chef Boyardee. So, so many more.
It’s one of those things that makes TLOU so good, and something that is missing in so many other shows. The fact that we have multiple times an episode where we slow down and get to see our characters talk and bond and grow just a bit closer. The show would work without it, but it adds so much to their relationship and makes us fall in love with the characters in a really rare and special way.
#PaigeGoneAnalysis#the last of us#the last of us hbo#tlou#tlou hbo#ellie williams#joel miller#bella ramsey#pedro pascal#the last of us analysis#tlou analysis#ellie and joel#joel and ellie
29 notes
·
View notes
Text
18 April 2024
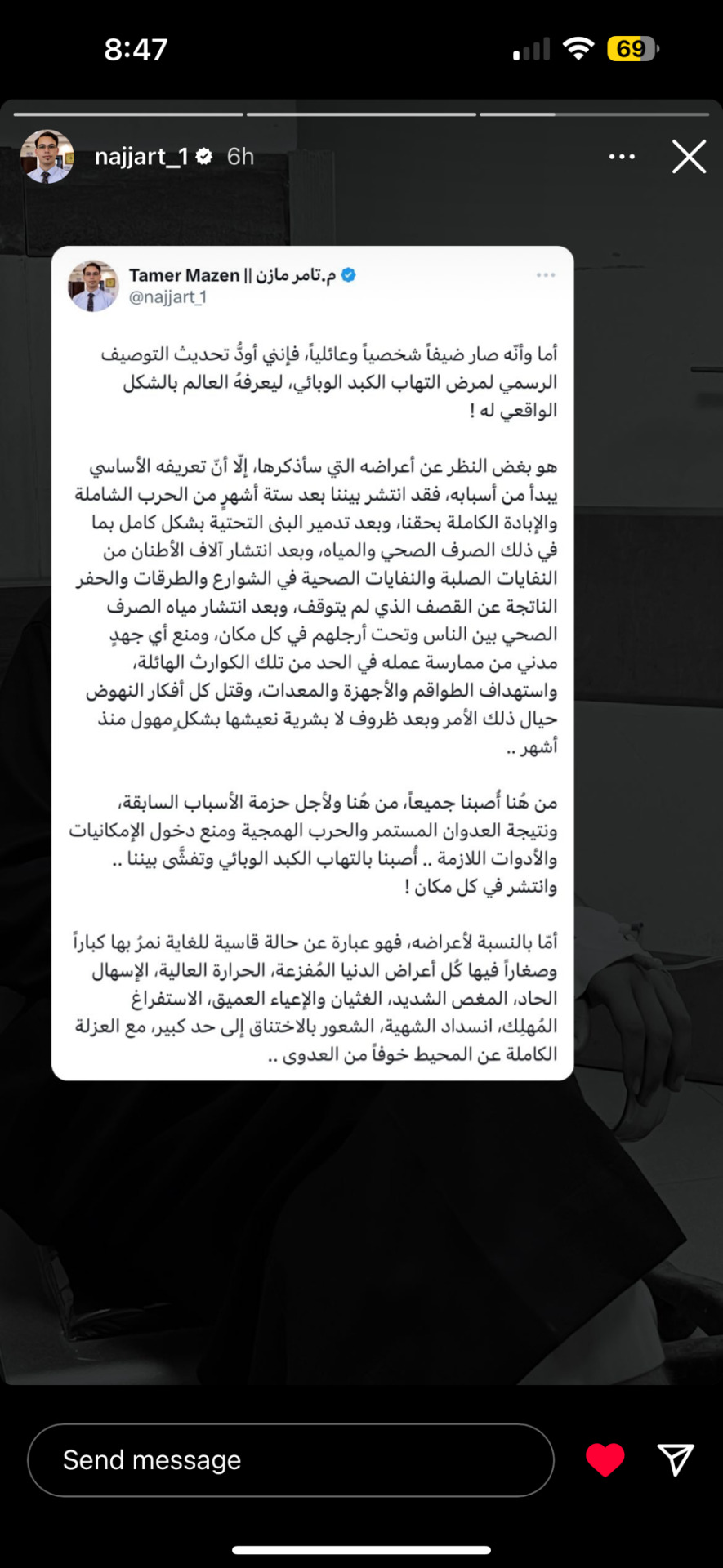
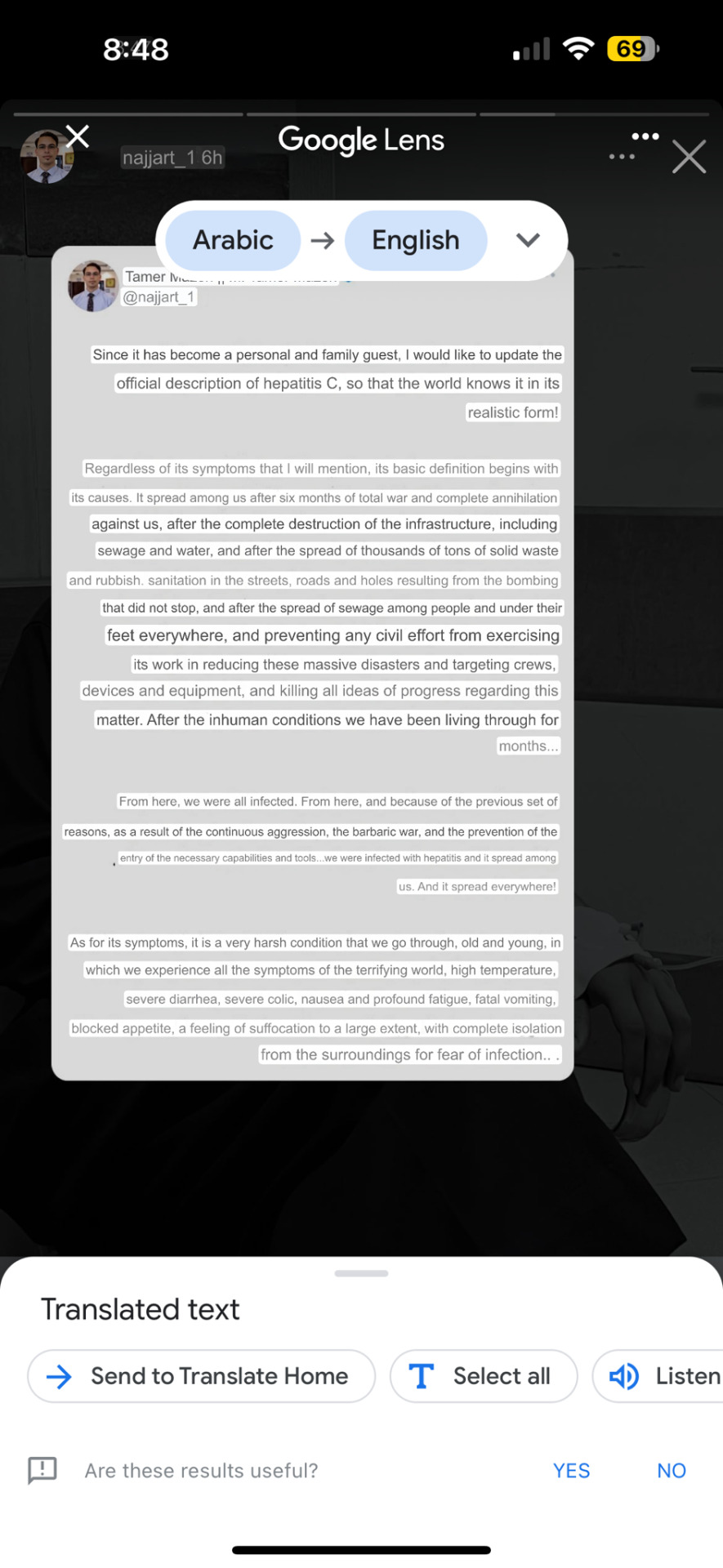
Environmental engineer Dr. Tamer Al-Najjar describes the Hepatitis C outbreak in north Gaza, with which he himself and his family are afflicted. The following was entered into a machine translation software and as such is bound to have some flaws, but the main ideas are still clear. Dr. Al-Najjar’s condition continues to worsen, and he has asked for prayers for his recovery.
He writes,
Since it has become a personal and family guest, I would like to update the official description of hepatitis C, so that the world knows it in its realistic form!
Regardless of its symptoms that I will mention, its basic definition begins with its causes. It spread among us after six months of total war and complete annihilation against us, after the complete destruction of the infrastructure, including sewage and water, and after the spread of thousands of tons of solid waste and rubbish. sanitation in the streets, roads and holes resulting from the bombing that did not stop, and after the spread of sewage among people and under their feet everywhere, and preventing any civil effort from exercising its work in reducing these massive disasters and targeting crews, devices and equipment, and killing all ideas of progress regarding this matter. After the inhuman conditions we have been living through for months...
From here, we were all infected. From here, and because of the previous set of reasons, as a result of the continuous aggression, the barbaric war, and the prevention of the entry of the necessary capabilities and tools...we were infected with hepatitis and it spread among us. And it spread everywhere!
As for its symptoms, it is a very harsh condition that we go through, old and young, in which we experience all the symptoms of the terrifying world, high temperature, severe diarrhea, severe colic, nausea and profound fatigue, fatal vomiting, blocked appetite, a feeling of suffocation to a large extent, with complete isolation from the surroundings for fear of infection.. .
#gaza#gaza genocide#gaza strip#north gaza#gaza under attack#free gaza#from the river to the sea palestine will be free#palestinian genocide#gaza journalists#stop genocide#gaza under bombardment#gaza update#gaza under fire#gaza under siege#gaza under genocide#stop gaza genocide#stop the genocide#stop israel#end israel's genocide#save north gaza#gazan genocide#18 April 2024#tamer al najjar#israeli war crimes#israel is a terrorist state#israel is committing genocide#israeli terrorism#gaza news#gazaunderfire#gazaunderattack
86 notes
·
View notes
Text
The Plague in Romeo and Juliet
The Plague ruins everything in Romeo and Juliet. Like, it's always understated how important the Plague is to the plot. A BIT OF HISTORY Shakespeare was alive during the second wave of the Bubonic plague in England (in the mid 1590s). Theaters had to be closed so people didn't, you know, die and stuff, so it ended up impacting his livelihood quite significantly. Romeo and Juliet was written around the time of the Plague, so it is safe to say that it was on Shakespeare's mind. Plus, it's set in Italy in the mid 1300s, during (you guessed it!) the first wave of the Bubonic Plague. So if we're looking for historical accuracy, Romeo and Juliet is going to be set during the Plague.
FAIR VERONA The Montagues and Capulets hate each other's guts. That much is clear from the first scene. And a common criticism of the play is "why don't they just get out of Verona?" It seems like kind of a weird plot hole, until you take their current situation into account. The Montagues and the Capulets can't leave Verona. Not unless they want to have long and painful deaths. - Verona is a walled city (safe from the outside world) - It is surrounded by a river - The city outside (Mantua, and we'll get to it later) was a hotspot for the Plague Verona was highly insular, and that was its benefit. It was also its major flaw, because the two major families of the area hated each other's guts. The tensions caused by the Plague and not being able to leave only went to exacerbate this hatred.
"A PLAGUE ON BOTH YOUR HOUSES" RIP Mercutio. You would've loved drag brunch. Also vaccines, since the Plague (indirectly) is probably the reason he died. Yes, I realize he dies because Tybalt stabs him. But why did Tybalt stab him in the first place? Let's roll back the clock a little. - Tybalt killed Mercutio because he was aligned with the Montagues, who are the enemies of the Capulets - The Capulets and Montagues can't just avoid each other because they're stuck in the same city - They're stuck in the same city because of the Plague There's also something to be said for the desperation felt by the people in Verona. Either they can die from sores and diarrhea, or they can die in a fight. And I dunno about y'all, but one of those things sounds a lot cooler. With the Plague closing in, of course people are gonna start picking fights. It's the perfect storm of stressed and reckless. If we contextualize the quote "a plague on both your houses" with the era, it's not just Mercutio cursing everyone out because he's angry he's gonna die (though that's definitely part of it). It's a warning. The Plague is the great equalizer, and it's going after everyone, regardless of whether they're a Montague or a Capulet.
ROMEO'S BANISHMENT Another compelling bit of evidence for the Plague's importance in Romeo and Juliet is Romeo's reaction to being exiled. Romeo is a lovesick puddle of soup. He fell in love with a girl at a party and then died because he couldn't live without her. He's overdramatic. But his reaction to being banished from Verona is pretty dramatic, even for him. Like, come on, dude. But what if it wasn't the fact that he would be separated from Juliet that he was the most worried about? Remember when I said we'd circle back around to Mantua? We're circling back around. Because Mantua (right outside of Verona) was a playground for the Plague. A Plague-ground, if you will. It was a place where a lot of people came and went, and it was blocked off by bridges. So, if an outbreak happened, Mantua (and those in it) would be cut off from the world and left for dead. Suddenly, Romeo's complaints about leaving Verona don't sound quite so unreasonable. Juliet's worry about Romeo going away doesn't seem quite so silly. And the Nurse's advice to Juliet, saying "he's basically dead now, so don't worry about him anymore" actually seems pretty reasonable. In fact, the biggest reason why Romeo and Juliet don't survive in the end is because the correspondence Friar Lawrence meant to send didn't go through fast enough, because Friar Peter (the guy he gave the letter to) was being quarantined.
ADULTS OF VERONA The Plague helps explain the actions of the adults, too. Juliet's parents are trying to get her to marry, even though she's really young (even by the standards of the era). This can be interpreted in a couple different ways. Either they want Juliet to hurry on with her life and get out of their hair, or they know that something might happen to them (or Juliet, for that matter) and they want to do their best to put Juliet in a good situation. The choice of Paris is, given what Juliet is facing, a pretty good one. He's good-looking, generally depicted as being close enough to Juliet's age, courteous, filthy rich, and not affiliated with either the Montagues or the Capulets. Juliet might not be in love with him, but she would at least be taken care of. Was Lord Capulet a perfect man? No. But can his actions be boiled down into just a desire for control? Not if you account for the Plague, at which point he (and his fellow adults) become much more nuanced and much more reasonable.
Romeo and Juliet, on its own, is plausible. It is possible to accept the story of the star-crossed lovers (I mean, the adaptations speak for themselves). But the introduction of the Plague creates a perfect storm of storytelling, cementing it as a tragedy. Not only could it happen, but this was the way it was always going to happen.
#classic literature#shakespeare#william shakespeare#dramaturgy#theatre history#the plague#romeo and juliet#stuff they didn't teach you in English class#here's a cutesy little sleep-deprived rant about theatre history#unnecessary and kind of tasteless puns#literary analysis#literature#the Plague ruins everything#But seriously: Mercutio would've LOVED drag brunch#wash your hands#renaissance
7 notes
·
View notes
Text
Can I offer you a nice egg in this trying time?
The politics of poultry and eggflation
Boil 'em, crack 'em, stick 'em in a soup. Eggs are an American staple. Despite back and forth about cholesterol and animal ethics, demand for eggs hasn’t going anywhere. At a few cents each, eggs have historically been one of the most affordable nutritious foods; now, they're nearly $1 apiece and rising -- if you can find them at all. How did we get here? And more importantly, how do we get back?
H.P.A.I. Four accursed letters that haunt every veterinarian and I would dare say most Americans. Avian Influenza (AI), or bird flu, causes issues ranging from respiratory disease and diarrhea to decreased egg production. Within AI, there are high and low pathogenic strains; of primary concern is the highly pathogenic avian influenza (HPAI) H5N1 strain, a form that spreads quickly, causing more severe illness and more deaths. Despite having disease nationwide, HPAI is still considered a "Foreign Animal Disease," a government designation of a carefully monitored disease not regularly in the USA (ignoring backyard flocks).
In addition to killing birds and marine mammals as it has been doing for years, the recent concern with HPAI has been the new species affected: humans, cattle, and cats. People are becoming ill or even dying. Dairy cows have been miscarrying, dying, and losing milk production. Seemingly healthy cats are dropping dead.
Another epidemic making eggs expensive, it's 2020 all over again! Except unlike COVID, we already have answers. And this time, we’ve got our eyes on Big Egg. HPAI has been a problem for years. We have the tools to deal with it. Yet, we refuse to use them. As a Foreign Animal Disease, the federal government controls how HPAI outbreaks are handled, specifically the United States Department of Agriculture (USDA).
The USDA dictates that commercial flocks (more than 1,000 birds) that test positive for HPAI are culled. Culled. Depopulated. Notably, different from euthanasia. Every bird in the infected flock must be killed. Commonly using carbon dioxide foam or gas, suffocating the birds. While unsavory, mass depopulation has its place to protect other animals from contagious disease, especially when the infected animals have little chance of surviving.
Except that current knowledge suggests that mass depopulation may increase spread. Production is delayed by an overzealous requirement that houses remain vacant for 14 days despite virus no longer being contagious within 96 hours. HPAI causes death – but not 100% death. In fact, in healthy unvaccinated populations, as much as 25% the flock could survive, building immunity which culling prevents.
Unvaccinated populations, like every poultry flock in the entire country. Unvaccinated implies availability of a vaccine though. And there is! Just… not here. In much of Asia, HPAI is commonplace, as it is becoming in the USA. As such, some countries such as China vaccinate all commercial birds. And it works, bringing HPAI-related death as low as 3% and speeding recovery with up to 97% survival. What about us? The vaccine is not available for use within the United States. Chickens are food animals under the USDA, heavily restricting vaccine use. Understandably so! Not all vaccines are good – some are dangerous, some just don’t work. Except other countries have been using this vaccine for years, so we know it’s safe and effective.
The USDA has yet to approve it for two reasons: trade and surveillance. In allowing chickens to die, the USDA maintains trade partners – certain countries would ban import of American poultry products should HPAI vaccination be permitted. Additionally, the USDA claims that the high mortality allows more effective surveillance so we can stamp out disease quickly. A strategy based in culling, an inefficient method of control rife with animal welfare concerns, human stressors, and economic impact. Even with vaccination, death rates are at least 2x that of a flock without HPAI (3% versus 0.5-1.5% normal mortality). Of course, cows with HPAI are not mass depopulated, further calling into question poultry use of this “stamping out” strategy.
The current outbreak, even just in dairy cows, has been a problem for a year now, the first case reported in late March 2024. Everything thus far has been bipartisan, absent of administration-specific criticism. These are ongoing issues, present through several presidential administrations, all failing to successfully address HPAI. Which is not to say I lack administration specific criticisms regarding ongoing epidemic(s) – HPAI … tuberculosis, measles, Listeria... Prior to mass layoffs and NIH funding freezes, research in both cows and chickens were underway to reassess the vaccine and its place in our production systems. Despite the destruction DOGE wreaks in the name of deregulation to “streamline our government,” we have yet to see changes benefiting Americans. Reassessment of HPAI vaccine and mass depopulation protocols ought to be a priority. An effective human HPAI vaccine would minimize hospitalizations and death; instead, we are left wondering if we will even have a flu vaccine next season. As an administration entrenched in a “bread and circuses” mindset, the clowns are excelling at circuses in the form of human rights violations but have yet to make groceries more affordable, ostensibly the reason many Americans voted for them
#HPAI#actually science related#fucked up i know how dare i#science#veterinary#my writing#science writing#it got rejected by a publisher as an opinion piece#prob because i called trump a clown#alas i couldn't help myself#politics#us politics#this is my special interest btw#the intersect of social values politics public health and medicine#like we live in a nightmare time but objectively interesting#chickens#eggs#highly recommend keeping quails btw#it is expensive and not super rewarding and time consuming#but they're my little guys#avian influenza#highly pathogenic avian influenza
11 notes
·
View notes
Text
Symptoms of Listeriosis (Listeria Infection)
Symptoms usually start within two weeks after eating food contaminated with Listeria but may start as early as the same day or as late as 10 weeks after. Mild symptoms may include a fever, muscle aches, nausea, tiredness, vomiting, and diarrhea. If the more severe form of listeriosis develops, symptoms may include headache, stiff neck, confusion, loss of balance, and convulsions.
#We usually get the Costco chicken street taco kit for easy meals#We were unfortunately affected.#listeria#outbreak
28 notes
·
View notes
Text
In addition to a generally miserable illness, measles can cause complications: 1 in 5 unvaccinated people with measles in the US end up hospitalized. About 1 in 10 develop ear infections and/or diarrhea, and 1 in 20 develop pneumonia. Between 1 to 3 in 1,000 die of the infection. In rare cases, it can cause a fatal disease of the central nervous system called Subacute sclerosing panencephalitis, which typically develops 7 to 10 years after an infection. Measles can also devastate immune responses to other infections (immune amnesia), making people who recover from the illness vulnerable to other infectious diseases.
5 notes
·
View notes
Text
Brazil's Vale do Javari Faces Indigenous Child Deaths, Water Shortages, and Flu Outbreak
Health Ministry claims to follow protocols to prevent disease spread in the Amazon

Children dying from preventable causes, a pharmacy comparable to a chicken coop, tables used as stretchers, lack of potable water and medicine, flu and diarrhea outbreaks, and symptomatic patients disregarding quarantine and moving freely through villages.
According to a series of documents accessed by Folha, this is the current situation in Vale do Javari, in the Amazon, the territory with the highest number of isolated Indigenous peoples in the world.
The records cover the past 13 months and various Indigenous groups living in the region, including communities that require special protection due to their extreme immunological vulnerability to diseases like the flu, which can be fatal in these cases.
Continue reading.
#brazil#brazilian politics#politics#environmentalism#indigenous rights#amazon rainforest#image description in alt#mod nise da silveira
6 notes
·
View notes