#or abnormal morphology
Explore tagged Tumblr posts
Text
Which is the best IVF center in Pune?
Determining the "best" IVF center in Pune can depend on various factors, including success rates, expertise of the medical team, patient care, facilities, and individual preferences. While I can't definitively label one center as the absolute best, I can suggest a few renowned IVF centers in Pune:
Nova IVI Fertility:
Embrio IVF Centre:
Silverberries IVF Clinic:
Cloudnine Fertility:
Oasis IVF Centre:
Before choosing an IVF center, it's crucial to research each option thoroughly, consider factors such as success rates and patient reviews, and schedule consultations to discuss your specific needs and concerns with the medical team.
#poor motility#or abnormal morphology#EmbrioIVF#ParenthoodJourney#ivfsupport#fertilitycare#FamilyPlanning#fertilityjourney#joyofpossibility#infertilitysupport#ivftreatment#fertilitycommunity#ivfsuccess#BabyDreams#ParentingGoals#fertilityclinic#ParentingJourney#fertilitysolutions#ivfbaby#malefertility#malefertilityawarness
0 notes
Text
What Causes Male Infertility? 10 Common Reasons Explained

When it comes to infertility, the focus often falls on women, but male infertility is just as significant and affects millions of men worldwide. In fact, about one in every five couples struggling with infertility may have a male factor contributing to the challenge. Let’s dive into the 10 most common causes of male infertility. Whether you’re seeking answers for yourself or someone close to you, understanding these causes is the first step toward finding solutions.
1. Low Sperm Count (Oligospermia)
A low sperm count is one of the most common causes of male infertility. Normal sperm count ranges from 15 million sperm per milliliter to over 200 million. If a man has fewer than 15 million sperm per milliliter, the chances of conception decrease significantly. Low sperm count can be caused by hormonal imbalances, genetic factors, or environmental exposures.
2. Poor Sperm Motility (Asthenozoospermia)
Sperm motility refers to the ability of sperm to swim efficiently toward an egg. Poor sperm motility is another leading cause of male infertility. If the sperm cannot swim effectively, they may struggle to reach and fertilize the egg, reducing the chances of conception. This can result from lifestyle choices, infections, or structural issues in the reproductive organs.
3. Abnormal Sperm Morphology (Teratozoospermia)
Sperm morphology is the study of the size and shape of sperm. Sperm with abnormal morphology (irregular shape or size) can have difficulty reaching and penetrating an egg. This condition may be linked to genetic factors, environmental toxins, or certain health conditions such as diabetes.
4. Varicocele
A varicocele is the enlargement of veins within the scrotum, similar to varicose veins that occur in the legs. It can interfere with the temperature regulation of the testicles, causing sperm production to decrease. Varicoceles are found in about 15% of the general male population but can be responsible for up to 40% of cases of male infertility.
5. Erectile Dysfunction (ED)
Erectile dysfunction, the inability to achieve or maintain an erection sufficient for sexual intercourse, can significantly impact fertility. While ED does not directly affect sperm quality, it hinders the physical ability to ejaculate during intercourse. Causes of ED include psychological factors, health conditions (e.g., diabetes), or side effects from medications.
6. Testicular Ailments (Infections or Injury)
Infections such as epididymitis, orchitis, and sexually transmitted infections (STIs) can impact sperm production and function. Testicular injuries or surgeries can also damage sperm-producing cells, leading to infertility. Conditions like mumps, if contracted after puberty, can also affect the testicles and lead to permanent infertility.
7. Hormonal Imbalances
Hormones play a crucial role in sperm production. An imbalance in hormones like testosterone, thyroid hormone, or prolactin can disrupt the production of sperm. Conditions such as hypogonadism (low testosterone levels), obesity, or pituitary gland problems can lead to hormonal imbalances that affect male fertility.
8. Genetic Factors
Genetics can significantly influence male fertility. Conditions such as Klinefelter syndrome (an extra X chromosome), Y-chromosome microdeletions, or cystic fibrosis can lead to infertility. In some cases, genetic abnormalities affect the production or function of sperm, while in others, they affect the structure of the reproductive organs.
9. Lifestyle Factors
Smoking, excessive alcohol consumption, recreational drug use, and poor diet can all decrease sperm quality. Regular physical activity is essential for maintaining overall health, but excessive exercise or heat exposure (such as frequent use of saunas or hot tubs) may negatively impact sperm production.
10. Environmental and Occupational Factors
Exposure to environmental toxins and chemicals, such as pesticides, heavy metals, or industrial chemicals, can impair sperm production. Men working in occupations involving exposure to toxic substances, such as welding or chemical manufacturing, may have a higher risk of infertility. Similarly, radiation and prolonged exposure to high temperatures can also decrease sperm count and quality.
Early intervention, lifestyle changes, and medical treatments are often effective in overcoming male infertility. For those looking for expert care, Prashanth IVF offers the best treatment options for male fertility, with a team of specialists dedicated to providing personalized, cutting-edge solutions.
#Male infertility#causes of male infertility#male infertility solutions#low sperm count#poor sperm motility#abnormal sperm morphology#erectile dysfunction and infertility#testicular ailments and infertility#hormonal imbalances in men#genetic causes of male infertility#lifestyle and infertility in men#environmental factors and male infertility#male fertility treatments#oligospermia treatment#asthenozoospermia causes#teratozoospermia solutions#varicocele and male infertility#infertility due to ED#hormonal therapy for men#male infertility diagnosis#fertility specialists near me#how to improve sperm count#overcome male infertility#sperm health tips#infertility in men vs women#common fertility issues in men#varicoceles treatment options#sperm morphology improvement#impact of smoking on fertility#heat exposure and sperm count
0 notes
Text


Autopsy Report
Case Number: 2024-1125-01 Decedent Name: Chad Evanston Age: 19 Sex: Male Height: 5’11” Weight: 154 lbs (estimated lean build) Race/Ethnicity: Caucasian Date of Death: November 24, 2024 Time of Autopsy: November 25, 2024, 9:00 AM Pathologist: Dr. Robert Linfield
I. External Examination
General Appearance: The decedent is a well-developed, lean, and athletic-appearing 19-year-old male, weighing approximately 154 pounds. He has brown hair, approximately 3 inches in length, and brown eyes. Skin is pale but otherwise unremarkable, with no evidence of external trauma or defensive injuries. Fingernails are clean and well-trimmed.
Clothing: The decedent was found dressed in athletic attire, including a blue baseball cap, black athletic shorts, a running watch on the left wrist, and well-worn running shoes. The clothing was damp due to environmental exposure but showed no tears or stains of significance beyond expected post-mortem findings.
Identifying Marks: A faint scar measuring 2 cm is present on the left knee, consistent with prior minor trauma or surgery. No tattoos or other distinguishing marks.
II. Internal Examination
Cardiovascular System: The heart is notably abnormal upon inspection. Weighing 390 grams (upper end of normal for the decedent's size and build), the heart exhibits significant thickening of the left ventricle (left ventricular hypertrophy). The mitral valve shows marked structural abnormalities, including:
Fibrotic thickening of the leaflets.
Mild calcification at the annulus.
Evidence of prolapse of the posterior leaflet, causing incomplete coaptation during closure. This structural defect resulted in significant mitral regurgitation, which would have led to reduced cardiac efficiency during exertion.
Examination of the coronary arteries reveals no signs of atherosclerosis or narrowing. However, microscopic examination identifies mild interstitial fibrosis in the ventricular myocardium, particularly in the left ventricle. These findings are consistent with chronic strain and early-stage cardiomyopathy, likely exacerbated by prolonged high-intensity physical activity.The conduction system shows mild scarring near the sinoatrial node, likely the origin of the arrhythmias detected on the decedent's running watch.
Lungs: The lungs weigh 520 grams (right) and 480 grams (left), with mild congestion. Examination shows no emboli or aspirated material.
Abdominal Organs: All abdominal organs, including the liver, spleen, kidneys, and gastrointestinal tract, appear normal in size and morphology.
Brain: Examination of the brain reveals no hemorrhages, infarcts, or structural abnormalities.
III. Microscopic Findings
Heart Tissue: Histological examination of the heart confirms chronic myocardial fibrosis and focal areas of myocyte disarray. These findings are indicative of longstanding structural abnormalities and stress-induced cardiac remodeling.
Lung Tissue: Pulmonary alveoli appear congested but otherwise unremarkable.
Valvular Tissue: Fibrosis and calcification of the mitral valve tissue are evident, along with cellular degeneration, consistent with a congenital or acquired valvular defect exacerbated over time.
IV. Toxicology Report
Testing for substances, including recreational drugs, alcohol, and common stimulants, returned negative results.
V. Cause of Death
Sudden cardiac arrest secondary to severe mitral valve dysfunction and associated arrhythmia.
Detailed Analysis of Cardiac Findings
The decedent's heart exhibited chronic and progressive mitral valve disease. The fibrotic and calcified changes in the mitral valve likely originated from an undiagnosed congenital defect, aggravated over time by physical exertion. The incomplete closure of the mitral valve resulted in backflow of blood (regurgitation) during systole, progressively overloading the left atrium and left ventricle. Over time, this stress led to the observed hypertrophy and scarring of the myocardium.
The combination of myocardial fibrosis and conduction system scarring predisposed the decedent to severe arrhythmias. The running watch data corroborates this, showing prolonged arrhythmic episodes throughout the decedent's final run.
The sustained stress of a nine-mile run caused the decedent’s heart to become electrically unstable, leading to ventricular fibrillation—a fatal arrhythmia resulting in sudden cardiac arrest. The autopsy findings, supported by wearable device data, confirm that this event was precipitated by his preexisting cardiac abnormalities.
Despite being otherwise healthy and athletic, the decedent’s heart was structurally compromised, making high-intensity exercise particularly dangerous. The mitral valve's dysfunction was significant enough that even mild to moderate exertion may have posed a risk over time.
Conclusion: Chad Evanston’s death was due to undiagnosed and progressive cardiac pathology exacerbated by prolonged physical exertion. This case highlights the critical need for screening individuals engaging in high-intensity activities for underlying heart conditions.
Final Manner of Death: Natural
22 notes
·
View notes
Text
I am extremely picky about anime because my patience for anime bullshit is incredibly low, so I've only ever watched a handful of them and I've only ever watched one all the way through (Soul Eater) but I have zoology degree and work at a zoo so I obviously have watched the Furry Anime(tm) (Beastars).
I love the animation style and music, but I definitely have some issues with the writing. But I'm not here to talk about that. I'm here to complain about exactly one big nitpick I have because I'm a nerd about animal morphology.
So throughout the anime I feel like some of the herbivore species are portrayed as inherently really weak compared to carnivorous species, which is kind of bs if you think about it. Like I get it, a sheep and a bunny aren't going to stand up to something like a lion or a grizzly bear, and there are also examples of herbivores being able to stand up to predators (herbivores in the police force, the crime fighting horse that kills lions, etc.). My point is that a lot of herbivorous species could absolutely kick a carnivore's ass, no guns required.
My biggest issue, however, is with Louis, canonically a red deer, being portrayed as a skinny little twink compared to a grey wolf. I get it, it's part of the conflict he's dealing with, but also red deer are fucking HUGE.

Look at this fucking thing. It's a deer the size of an elk. Males can weigh up to 530 pounds while male grey wolves are around 180 at the absolute largest. A single grey wolf isn't gonna take one of these guys down without getting seriously hurt by those antlers and hooves. Wolves can take down adult moose, but only in a relatively large pack. They're also close to twice the height of an adult male grey wolf (around 51 in at the shoulder). Louis should be towering over Legosi, even with him being abnormally tall for a wolf. If they wanted a smaller, weaker deer I'd say make Louis a whitetail deer or fallow deer, not one of the largest deer species in the world.
Anyway yeah Louis should not be portrayed as a twink imo and he could kick the gay wolf's ass like 9 times out of ten. The guy should look like a gym bro or something.
#beastars#complaints#not really a complaint but i'm putting it in there#i have so many problems with this anime but also the worldbuilding lore is fascinating and perplexing from a zoology standpoint
23 notes
·
View notes
Text
Elleana's Hallaren form, known as the Hallaren by keepers or mistaken by the people as a Hanal'ghilan, is morphologically different than modern halla. While modern halla are much more likely to be of the Cervidae (deer) family, Elleana's halla form is much more like a Camelidae (camel) family, sans her antlers. She embodies likely an ancient species offshoot of halla (something in the Artiodactyla Order) that died out/evolved into the modern halla seen in Thedas. She has soft padded feet with long claw like toes that grow from her feet. These toes usually do not make contact with the ground and are abnormally sharp for a 'prey' creature. Her body form could be compared to a vicuña's, fairly small and compact, with short wool over most of her body. Her face is longer than a vicuña's and more forward set eyes; less like a prey creature and more like a predator. She has both upper and bottom teeth, with sharper wolf teeth, and consumes both vegetation and meat. Her antlers are slow growing and shed only 3-5 years, usually in late spring time, later than most halla. She will begin to regrow her antlers the following fall and will go into felting season in winter; making her seem horrific to the ignorant due to her blood stained hide. Her antlers grow out a deep golden hue and can be carved like other halla antlers. If polished the antlers will glow like gold due to the magickal energy stored in them. Her halla form's antler shed usually triggers when she will move on from a clan, leaving her shed antlers with them as a gift. In her elvhen form she wears a headdress with a set of her shed antlers that dates back shortly after the fall of Arlathan. They were carved for the intent of war and are wicked and sharp; a crown of gold points.
11 notes
·
View notes
Text
DR. MARTHE GAUTIER // RESEARCHER
“She was a French medical doctor and researcher, best known for her role in discovering the link of diseases to chromosome abnormalities. She worked at Trousseau Hospital in Raymond Turpin’s team. Turpin's research was focused on polymalformative syndromes, of which the most common is trisomy, characterized by intellectual disability and morphological abnormalities. At the time, Turpin favored the hypothesis of a chromosomal origin of trisomy but there was no laboratory for cell culture in France and the number of human chromosomes was estimated at 48, but without any certainty. She entrusted her research to Jérôme Lejeune, who offered to take pictures in another laboratory better equipt, however he did not return the slides of research, but instead reported the discovery as his own.”

5 notes
·
View notes
Text
Holding Space for the Unknown: Humanities, Identity, and Healing in Healthcare
As a healthcare worker and future medical professional, I’m learning to accept that sometimes, we just don’t know. And I hate that. The anxiety of the unknown—Are these benign? Did I cause this? Am I stuck with this forever?—can be just as debilitating as the physical symptoms. Living with uncertainty, especially in a body shaped by both chronic illness and gender-affirming hormone therapy, has forced me to grapple with more than medical unknowns. It’s a confrontation of what it means to live in a body that defies neat clinical categories.
What I (might) have—PCOS, or technically just a polycystic ovarian morphology—isn’t deadly. But that doesn’t mean it’s painless. It’s a chronic condition that fluctuates day to day. Some days, it’s manageable. Other days, I’m doubled over in pain, for no good reason. The unpredictability keeps me in a state of constant stress. And it can be exhausting.
My experience on testosterone has added some serious complexity. While it’s been lifesaving for my mental health and gender affirmation, it introduced new and unexplained symptoms. Severe abdominal pain (among other things) has led me from doctor to specialist and back again, with no clear answers. PCOS is a possibility—it tends to manifest in early adulthood, and I’m twenty—but the overlap with hormone therapy makes it harder to understand “why.” Stopping testosterone is not an option for me. It’s integral to my wellbeing. Yet, I think the healthcare system often lacks the tools—or the will—to hold space for bodies like mine.
I remember the ultrasound appointment vividly. The procedure was invasive and incredibly dysphoric. I asked the tech if she could interpret the images. She shook her head. Legally, she couldn’t tell me anything unless it was definitively normal. Her silence was so loud in my head, I knew she saw something abnormal. But hey, I kind of already knew something wasn’t right.
When I finally circled back to my primary care provider, she was able to interpret the ultrasound results. I had a 4.3 cm benign cyst on my left ovary, along with more than 40 total follicles in both ovaries, when the “normal” max is around 24 total. Even more alarming, my left ovarian volume measured 59cc—an incredibly enlarged size, considering the average volume sits around 7cc. The pain I’d been feeling for the past eighteen months wasn’t mysterious anymore; it was the result of these cysts constantly swelling, obstructing, and occasionally rupturing against my internal organs. The ruptures brought a wave of intense, sharp pain that often triggered debilitating migraines, the kind that none of my over-the-counter remedy would touch. The constant pressure in my abdomen also wreaked havoc on my gastrointestinal and genitourinary systems. It’s not something that can be fixed—it’s something I have to ride out. And I think that’s the hardest part for me. It’s frustrating and demoralizing, since the common treatment is estrogen!
Getting diagnosed with polycystic ovaries while on testosterone wasn’t just confusing—it kind of felt like a betrayal. I had done everything I thought was “right”: maintained a healthy routine, took my meds, stayed informed, you name it. But the pain did not care. Neither did the healthcare system, which didn’t quite know what to do with someone like me. It felt like medicine shoves bodies in boxes, and mine didn’t fit.
The diagnosis wasn’t only a medical label. It was an identity shock. PCOS is usually framed around cisgender women’s health—periods, fertility, “feminine” hormone imbalances. And while I find women’s health incredibly important, none of that aligned with how I experience my body. And still, the diagnosis was mine. It forced me to sit with the discomfort of a body that defies expectations both medically and socially. And that dissonance was almost funny in a tragic way: a trans man with ovaries producing too many androgens. How poetic!
Before spring break, I attended the art therapy session. I went in skeptical, I won’t lie. I’ve always been more of a science-and-structure kind of person, even though I knew how beneficial therapy can be. But the experience was surprisingly cathartic. The instructor emphasized that art could communicate when words fail. The pain I feel is often hard to localize. But I can draw it, I can map it, and I can give form to something otherwise formless. These drawings aren’t diagnostic tools; they’re emotional compasses. Sometimes they tell me I need ibuprofen. Other times, they remind me I need rest, or quiet, or leafy greens. In translating pain into something tangible, I reclaim some control.
I’ve worked at [a hospital] long enough to know its rhythms. I’ve transported patients, handled specimens, navigated sterile hallways. But nothing prepared me for the shift when I became the patient. Suddenly, the same art-filled corridors that I passed without thought became anchors. A landscape painting calmed my spiraling thoughts. The stained glass donor wall in the atrium gave me pause.
Judy Rollins, in Purpose-Built: Art in Hospitals: Art with Intent, highlights that the integration of art into healthcare spaces is not merely aesthetic—it’s deeply intentional. She argues that when art is thoughtfully selected and situated, it has the potential to provide a healing environment that can offer comfort, distraction, and “sense of agency” to patients and families (Rollins, 2021). I experienced this firsthand. In my most vulnerable moments, it wasn’t just clinical care I needed. It was humanity. And while I know my condition isn’t critical, I can only imagine how much more vital these visual moments of peace must be for families in critical care, or for patients facing terminal diagnoses. Art doesn't erase fear—but it can definitely help soften its edges.
What ultimately helped me begin to accept the uncertainty of my condition wasn’t just seeing specialists—it was turning to narrative medicine and the humanities. In Graphic Medicine Manifesto, Charon et al. emphasize that narrative medicine offers tools to articulate experiences that resist straightforward diagnosis. My pain doesn’t always show up on scans. But in words and images, it becomes visible and valid.
I’ve started journaling again, sketching when the pain comes, writing down what I notice in my body. These aren’t necessarily clinical, but they’re honest and they help me hold the parts of my story that medicine can’t really fix. Living with health uncertainty is not something I’ve mastered. Some days, I still spiral. But I’ve learned that not knowing doesn’t mean I’m broken. It means I’m alive—complicated, shifting, and human. Experiences like art therapy, music therapy, and readings like Purpose-Built and Graphic Medicine Manifesto, have helped me see illness not just as a problem to solve but as a narrative to honor. Healing, I’ve come to understand, isn’t always clinical. It’s multifaceted. Sometimes it’s creative, sometimes it’s just showing up, and sometimes, it’s learning to live fully in the in-between.
#essay#long post#pcos#pcosawareness#ftm#transgender#trans rights#trans healthcare#health humanities#journal entry#if someone could help me figure out how to deal with pain#that would be great#hipaa#who is she#modern healthcare#womens health#hipaa who???#airing out my dirty laundry#polycystic ovaries
5 notes
·
View notes
Text
So you heard how countryhumans were made… mythologically
Now to hear what science has to say.
Countryhumans' scientific name is Homo terra, under the genus Homo. All Homo terra have a form of defensive form, used to protect themselves and their people and triggered by danger. Mythologically, their primary diety Pangaea had the foresight to know that Her children would need such a thing, so She granted them such power. Science, however, begs to differ. Defensive forms, in fact, are what was used to trace the origins of Homo terra.
—
Once they were manifestations of the raw cooperative energy created by humans working together in large, meta-familial groups. They were nebulous in morphology, taking on whatever form was most appealing to the group they represented. They co-existed, and eventually co-evolved with Homosapiens, growing to depend on them more for continued survival. How human social energy became sentient and sapient is still unexplained.
—
Eventually, these manifestations began to take on Homosapien forms, but not because they decided to willingly take on a permanent, anthropomorphic embodiment. Their ancestors began to intermingle more with humans, including reproductively. Once again, it remains unknown how Homo terra ancestors reproduced successfully with Homo sapien. They eventually fell under the genus Homo, with their original energy form being unknown. Now, Homo terra are visually nearly indistinguishable from other humans, with the exception of features like wings, horns, or tails, as well as abnormal sizes and adaptive internal organs.
—
Each Homo terra is equipped with a defensive form that is mostly controlled by fear and danger responses. This was an evolutionary advantage from their ancestors that remained after their merge with homosapien. Another evolutionary advantage from their ancestors is their extreme durability, regenerative ability, and incredibly long lifespans. Homo terra genes are being used to regenerate limbs and organs of humans, with mixed results.
--
This theory is also proposed to explain why some Homo terra are “born” from social necessity or by chance, but evolutionary biologists still have yet to explain why they would not be more alike their ancestors in morphology. While it has not been discovered how the infamous "blood and earth" method works to reproduce, biologists suspect it has something to do with special properties of their blood, linked to Homo terra's regenerative abilities.
--
Belief in Pangaea remains prolific as an explanation to the scientifically unexplained, a God-of-the-Gaps.
#countryhumans#original character#original characters#country humans#statehumans#flaghumans#countryhumans origins
5 notes
·
View notes
Text
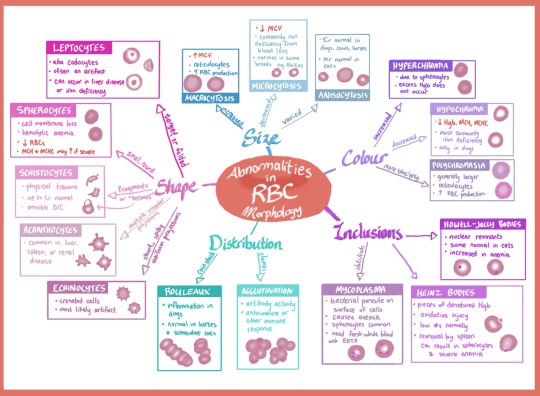
Abnormalities in RBC Morphology
9 notes
·
View notes
Text
Unraveling the Enigma: Exploring the Causes of Infertility in Men and Women

Infertility, a condition that affects millions of couples worldwide, can be a source of immense emotional distress and frustration. While there are numerous factors that can contribute to infertility, understanding its underlying causes is essential for effective diagnosis and treatment. In this article, we delve into the multifaceted causes of infertility in both men and women, shedding light on the complex interplay of biological, environmental, and lifestyle factors.
Causes of Infertility in Women
Ovulation Disorders: Irregular or absent ovulation can hinder conception. Conditions such as polycystic ovary syndrome (PCOS), thyroid disorders, and premature ovarian insufficiency (POI) can disrupt the ovulation process.
Fallopian Tube Damage: Blockages or damage to the fallopian tubes can prevent the egg from reaching the uterus for fertilization. Previous pelvic infections, endometriosis, or surgery may contribute to fallopian tube issues.
Uterine Abnormalities: Structural abnormalities in the uterus, such as fibroids or polyps, can interfere with embryo implantation and development, leading to infertility.
Age-related Factors: As women age, the quantity and quality of their eggs decline, making conception more challenging. Advanced maternal age is a significant risk factor for infertility.
Causes of Infertility in Men
Low Sperm Count or Quality: Issues with sperm production, motility, or morphology can impair fertility. Factors such as hormonal imbalances, genetic conditions, and lifestyle choices (e.g., smoking, excessive alcohol consumption) can affect sperm health.
Varicocele: A varicocele, an enlargement of the veins within the scrotum, can lead to decreased sperm production and quality. It is a common reversible cause of male infertility.
Testicular Factors: Conditions such as undescended testicles, testicular trauma, or infections can impact sperm production and function, contributing to infertility.
Ejaculatory Disorders: Disorders affecting the ejaculation process, such as retrograde ejaculation or erectile dysfunction, can hinder the delivery of sperm during intercourse.
Seeking Help from a Male Fertility Doctor
For couples struggling with infertility, consulting a male fertility doctor, also known as a reproductive urologist or andrologist, can provide valuable insights and guidance. These specialists are trained to evaluate and treat male infertility issues, offering diagnostic tests, fertility evaluations, and personalized treatment plans to address underlying causes and improve reproductive outcomes.
Conclusion
Infertility can stem from a myriad of factors affecting both men and women. By understanding the potential causes of infertility and seeking specialized care from a male fertility doctor specialist, couples can embark on a journey towards achieving their dream of parenthood. With advancements in reproductive medicine and personalized treatment approaches, there is hope for overcoming infertility challenges and building a family.
2 notes
·
View notes
Text
Tanza Mortal Races
Draki
Here
Humans
Humans are the defacto dominant species of Tanza, morphologically speakin they are exactly the same as real life humans, except they have long, mobile ears. Humans dont have natural bright colours (purple/blue stuff like that) unless they have Drakin ancestry, but human mages who spend a lot of time handling Neautra may come to experience abnormal coloration, usually the eyes, tip of the finguers and hair.
Speaking of Neautra, unlike Drakin that have a natural gift for it, pure blood humans are not able to naturally wield Neautra and must use conduits to cast magic, such as spellbooks (books with ready to use spells written out that simply need to be activated), Jewels made of Crystalized Neautra, or in some more radical cases tatooing spells on the body that allow for instant cast.
Humans form the Izeriath Empire, a very technologically advanced nation, (they have stuff like fantasy internet, magic phones, magic cars etc) as well culturally diverse given its immense size. It spend much of its history struggling to keep itself togheter, tought it has been pretty stable for the past century.
One of the most dark periods in Izerianthi history has been 500 years ago, when a Demon Lord managed to breach into the mortal realm right into the empire's capital, that demon lord started a 20 year reign of terror, mortals had never faced a demon this powerful before, and only thanks to an Izerianthi and Drakin alliance managed to finally slay him.
The Empire had a very closed relationship with the spirits, their archmages were able to communicate and learn their language to master powerful magics, The Imperial Family had a deal with a spirit and blessed by it, and the Gods had a honorary seat at the State Council. It was enjoying a very nice period of stability, until the god Shadlan was killed by a mortal, the spirits turned on them and demon attacks have become more and more common.
3 notes
·
View notes
Text
Series I, Part II
SCP-007 - Abdominal Planet
This one kinda scares the hell out of me, to be honest. Not the skip itself (dude with a planet where his abdomen should be, kinda weird, but otherwise fairly tame for an SCP entry). No, what scares me about this one is (and this will be a recurring theme) the way they’re just holding a dude hostage with no real oversight or recourse. Sure, the guy’s SSN comes up as invalid, but still. They’ve got this guy, they’re denying him access to the outside world, and…they’re just gonna get away with it.
As I said, this will be a recurring theme. In a lot of cases, I think the actual containment of things (usually people) is worse than the thing itself.
7/10
SCP-008 - Zombie Plague
This one does nothing for me. It’s exactly what it says on the tin, and while that’s fine, it just doesn’t appeal to me. All the same, I feel hesitant to give it a low rating because it is well written, it just isn’t my thing.
6/10
SCP-009 - Red Ice
This one’s kinda neat. It’s evil water (you can tell it’s evil because it’s red). It can contaminate normal water (including the water in people) and will kill them. It’s probably from another dimension. I don’t have much to say about this one. It’s just a fun concept.
7/10
SCP-010 - Collars of Control
I don’t like this one.
Not conceptually. Conceptually it’s great. Collars that allow whoever has the remote complete control over the wearer as long as they understand how to use the remote is a great concept. I love it. I also hate it, because one of the lines is “The most abnormal feature of the collars is the effect they have on the body morphology. They allow the user of the remote to reconfigure the shape of the victim to an extent that is apparently only limited by the knowledge of the programming language of the remote.” Nope. Hate it. I can take a lot of body horror, but like…something about that sets off all my Nope! Alarms.
9/10
SCP-011 - Sentient Civil War Memorial Statue
This one’s just kinda sweet? Again, it’s exactly what it says on the tin: A Civil War Memorial Statue in Vermont that just happens to be alive and sentient. It’s nice. I liked reading this one.
10/10
#jill rates scps#scp foundation#scp#scp 007#scp 008#scp 009#scp 010#scp 011#I will be really good at roman numerals by the time I've done all seven thousand something articles of this
6 notes
·
View notes
Text
Male Infertility Causes & Treatments in Madurai – Expert Guide by Sumathi Hospital
In the journey toward building a family, addressing Male infertility treatment Madurai is often the crucial first step.
Men facing challenges like low sperm count, poor motility, or abnormal morphology can find hope through targeted diagnostic assessments—semen analysis, hormone profiling, and advanced imaging—to uncover the root causes.
From lifestyle adjustments and nutritional supplementation to medications that optimize testosterone or treat varicoceles, modern male fertility care empowers many couples to progress toward success.
When these interventions alone aren’t enough, cutting-edge assisted reproductive technologies become essential.
Test tube baby treatment Madurai, better known as IVF (In‑Vitro Fertilization), and its specialized variant ICSI (Intracytoplasmic Sperm Injection), offer powerful options. ICSI is particularly effective for severe sperm disorders: a single sperm is directly injected into each egg under the microscope, dramatically improving fertilization chances .
At Sumathi Hospital, semen preparation techniques are combined with IUI (Intrauterine Insemination) and ICSI protocols tailored to each couple’s needs.
Holistic Infertility treatment Madurai involves personalized fertility planning: combining male and female evaluations to design protocols that may include hormone therapy, timing of insemination, or full IVF cycles.
The goal is maximizing success while minimizing unnecessary interventions. For some, lifestyle factors—like diet, exercise, quitting smoking, or reducing heat exposure—can be the game-changer.
For others, a coordinated series of techniques from IUI to IVF/ICSI leads to the long-awaited positive pregnancy test.
Over more than three decades, IVF hospitals in Madurai treatments have evolved.
At Sumathi Hospital, expert clinicians guide every step, from semen diagnostics and varicocele repair to advanced sperm retrieval and ICSI-based fertilization.
The centre pioneers Male infertility treatment Madurai, combining evidence-based protocols with compassionate care.
Their comprehensive suite—from initial male fertility workup to integration with IVF/ICSI—demonstrates why Sumathi Hospital is renowned for Male infertility treatment Madurai.
For more details:
Call: 73588 00889
Visit sumathihospital.com
Follow us on Instagram - https://www.instagram.com/sumathihospital/
#MaleInfertility#IVF#ICSI#IUI#FertilityMadurai#TestTubeBaby#FertilityTreatment#MaleFertility#InfertilitySupport#SumathiHospital
0 notes
Text
Male infertility treatment noida
The journey to parenthood is often envisioned as a beautiful, natural progression, a shared dream blossoming into reality. Yet, for many couples, this path can present unexpected and deeply personal challenges. While discussions around infertility often gravitate towards female factors, it's crucial to acknowledge that male infertility plays a significant, equally important role, contributing to a substantial portion of conception difficulties. Facing such a diagnosis can bring a unique set of emotional hurdles and questions for men and their partners. In the heart of Noida, navigating these complexities requires not just medical expertise, but also a compassionate understanding of the unique emotional landscape involved. When seeking effective male infertility treatment Noida residents need a specialist who offers both cutting-edge solutions and empathetic guidance.
male infertility treatment noida
In this vital pursuit of family building, one name stands out as a beacon of excellence and profound understanding: Dr. Parul Agrawal. With a distinguished career spanning over 23 years, Dr. Parul Agrawal has established herself as a formidable figure in Obstetrics and Gynecology, particularly renowned for her deep specialization in Reproductive Medicine. As the esteemed Director of Reproductive Medicine & IVF at Cloudnine Hospital, Noida, she brings an unparalleled fusion of rigorous scientific acumen, extensive practical experience, and a genuinely empathetic approach to every individual and couple she guides. Her remarkable professional journey, marked by pivotal roles at renowned hospitals and fertility centers, has allowed her to meticulously hone her skills across the vast and intricate spectrum of reproductive health. This extensive background positions her not only as a leading IVF Specialist in Noida but as the definitive expert for comprehensive male infertility treatment Noida couples can turn to with absolute confidence.
Beyond Stereotypes: Understanding Male Infertility
For too long, infertility has been a conversation predominantly centered around women. However, modern reproductive science has unequivocally demonstrated that male factors contribute to approximately 40-50% of all infertility cases, either solely or in combination with female factors. This crucial understanding reshapes the narrative, highlighting that conceiving a child is inherently a shared journey, where the reproductive health of both partners is equally vital.
Male infertility is not a singular condition but a broad term encompassing various issues that affect a man's ability to impregnate his partner. It can manifest as problems with:
Sperm Production: Low sperm count (oligozoospermia) or complete absence of sperm (azoospermia).
Sperm Function: Sperm that are abnormally shaped (morphology issues), have poor movement (motility issues), or are unable to properly fertilize an egg.
Sperm Delivery: Blockages or other issues that prevent sperm from being ejaculated effectively.
Hormonal Imbalances: Disruptions in the hormones that regulate sperm production.
Understanding these diverse facets is the first step towards effective intervention. This is why Dr. Parul Agrawal always emphasizes the importance of a comprehensive and unbiased approach to diagnosis for both partners right from the start, a process that begins with thorough fertility counselling and basic evaluation for couples. This foundational step ensures that every potential factor contributing to infertility is meticulously explored, paving the way for targeted and effective male infertility treatment Noida.
The Pillars of Effective Male Infertility Treatment in Noida
Successful male infertility treatment Noida hinges on a meticulous, multi-pronged approach that begins with accurate diagnosis and extends through highly personalized treatment strategies. Dr. Parul Agrawal's philosophy is rooted in this comprehensive model, ensuring every aspect of male reproductive health is thoroughly addressed.
1. Thorough Diagnostic Evaluation: The First Crucial Step
Before any treatment plan can be formulated, a precise understanding of the underlying cause of male infertility is paramount. Dr. Parul Agrawal ensures a meticulous diagnostic process, which typically includes:
Initial Consultation & Medical History: A detailed discussion about medical history, lifestyle, previous infections, surgeries, and any relevant family history.
Physical Examination: A thorough examination of the reproductive organs to identify any anatomical abnormalities or issues like varicocele.
Semen Analysis: This is the cornerstone of male fertility assessment. Multiple samples are typically analyzed over time to evaluate critical parameters such as:
Sperm Count: The concentration of sperm per milliliter of semen.
Motility: The percentage of sperm that are moving and their quality of movement.
Morphology: The percentage of sperm that have a normal shape and size.
Volume and pH: Other important characteristics of the semen fluid.
Hormone Profiling: Blood tests to measure levels of key hormones that regulate sperm production, including Testosterone, Follicle-Stimulating Hormone (FSH), Luteinizing Hormone (LH), and Prolactin. Imbalances in these can significantly impact fertility.
Genetic Testing: For cases of severe male factor infertility (e.g., very low sperm count or azoospermia), genetic tests like Karyotyping (to check for chromosomal abnormalities) and Y-chromosome microdeletion testing (to identify deletions on the Y chromosome affecting sperm production) are crucial.
Imaging Studies: A scrotal ultrasound can help detect conditions like varicocele (enlarged veins in the scrotum) or other testicular abnormalities. A transrectal ultrasound might be used to check for blockages in the ejaculatory ducts.
Post-Ejaculation Urinalysis: This test checks for the presence of sperm in urine, which can indicate retrograde ejaculation – where semen enters the bladder instead of exiting the penis during orgasm.
Testicular Biopsy: In specific cases of azoospermia (no sperm in the ejaculate), a small tissue sample is taken from the testicles. This helps determine whether the absence of sperm is due to a production issue or a blockage in the sperm transport system.
By meticulously conducting these diagnostic tests, Dr. Parul Agrawal’s clinic ensures a precise and accurate diagnosis, laying the groundwork for the best male infertility treatment in Noida tailored to each individual's needs.
2. Tailored Treatment Strategies for Diverse Male Factors
Based on the diagnostic findings, Dr. Parul Agrawal develops a highly personalized treatment plan, drawing from a wide array of advanced interventions available for male infertility treatment Noida. These strategies are often multi-faceted:
Lifestyle Modifications: Simple yet effective changes can significantly improve sperm health. This includes adopting a balanced, antioxidant-rich diet, engaging in regular exercise, maintaining a healthy weight, effectively managing stress, and strictly avoiding harmful substances like smoking, excessive alcohol, and recreational drugs.
Medical Management:
Hormonal Therapy: For men with identified hormonal imbalances, specific medications can be prescribed to regulate hormone levels and stimulate sperm production.
Antibiotics: If an infection in the reproductive tract is detected, a course of antibiotics can often clear the infection, though it doesn't always guarantee immediate restoration of fertility.
Medications for Sexual Dysfunction: For issues like erectile dysfunction or premature ejaculation, appropriate medical or psychological interventions can improve the chances of natural conception.
Surgical Interventions:
Varicocelectomy: Surgical correction of a varicocele (enlarged veins in the scrotum) can often improve sperm quality and count, as varicoceles can lead to increased testicular temperature affecting sperm production.
Reconstructive Surgery: For blockages in the vas deferens or epididymis (tubes that transport sperm), surgical repair or vasectomy reversal can restore sperm flow.
Sperm Retrieval Techniques: For men with very low sperm count or azoospermia, where sperm are produced but not ejaculated (obstructive azoospermia) or produced in very low numbers directly from the testicles (non-obstructive azoospermia), advanced surgical sperm retrieval techniques are employed. These include:
TESA (Testicular Sperm Aspiration): Sperm are aspirated directly from the testis using a fine needle.
PESA (Percutaneous Epididymal Sperm Aspiration): Sperm are aspirated from the epididymis.
Micro-TESE (Microsurgical Testicular Sperm Extraction): A more advanced procedure performed under a microscope to precisely locate and extract sperm from testicular tissue, often used in cases of non-obstructive azoospermia. These vital procedures enable successful infertility treatment in noida for many couples.
Assisted Reproductive Technologies (ART): When natural or less invasive treatments are not sufficient, ART offers powerful solutions:
Intrauterine Insemination (IUI): In cases of mild male factor infertility, IUI involves placing a concentrated sample of healthy sperm directly into the woman's uterus around the time of ovulation.
IVF with ICSI (Intracytoplasmic Sperm Injection): This is a cornerstone of ivf treatment in noida for male factor infertility. A single, healthy sperm (obtained either through ejaculation or surgical retrieval) is directly injected into an egg in the laboratory. This technique dramatically increases the chances of fertilization even with very few or compromised sperm.
The seamless integration of these advanced techniques within a comprehensive fertility treatment noida plan underscores the expertise of an ivf doctor in noida like Dr. Parul Agrawal.
Dr. Parul Agrawal: A Beacon for Male Infertility Treatment in Noida
Dr. Parul Agrawal’s extensive experience and specialized focus in reproductive medicine make her an unparalleled expert in male infertility treatment Noida. With over 23 years dedicated to the field, she possesses the profound insight and refined skills necessary to address the most complex male fertility challenges. She is not merely an IVF Specialist doctor in Noida but a holistic fertility specialist doctor Noida who understands that successful outcomes are built on a deep understanding of both partners’ reproductive health.
Her practice is founded on a patient-centric approach, where clear communication and emotional support are as vital as medical precision. She meticulously explains every diagnostic step and treatment option, empowering couples with knowledge and reassurance. Her proficiency in advanced techniques like ICSI and various surgical sperm retrieval methods (TESA, Micro-TESE) ensures that even in cases of severe male factor infertility, there are viable pathways to parenthood. Operating as the Director of Reproductive Medicine & IVF at Cloudnine Hospital, she leads a facility that stands as the best ivf centre in noida. This ensures access to cutting-edge laboratory facilities, advanced equipment, and a highly skilled multidisciplinary team of embryologists and support staff, all working in unison to maximize the chances of success for every couple pursuing fertility treatment noida under her guidance. This commitment to excellence and compassionate care truly distinguishes her as the best ivf treatment doctor in noida.
Your Path Forward: Hope and Expertise in Noida
Facing male infertility can be a difficult diagnosis, but it is crucial to remember that it is a treatable condition. With the right expert guidance and advanced medical interventions available today, the dream of parenthood is more attainable than ever before. Taking the first step towards comprehensive evaluation and personalized care is the most empowering decision you can make.
If you are a couple in Noida navigating the complexities of male infertility and seeking expert, compassionate care, we warmly invite you to explore the comprehensive solutions offered by Dr. Parul Agrawal. Discover more about her approach and the advanced treatment options available by visiting her website. Your journey to welcoming a child into your life is one that Dr. Parul Agrawal is profoundly committed to helping you achieve.
ALSO SEE-
ivf treatment in noida
best ivf doctor in noida
IVF Specialist in noida
ivf treatment doctor noida
fertility treatment noida
fertility specialist doctor noida
0 notes
Text
Do You Want To Know Who Needs ICSI Treatment?

Infertility is an emotional and physical challenge faced by countless couples across the globe. In a country like India, where starting a family is often considered an important milestone in married life, infertility can be particularly distressing. Fortunately, medical advancements in the field of assisted reproductive technologies (ART) have opened up a new world of hope. Among the most effective and innovative treatments available today is ICSI treatment, or Intracytoplasmic Sperm Injection. For couples seeking trusted, expert care, ICSI Treatment for Infertility in Delhi at Shivam IVF provides a highly specialized solution that brings dreams of parenthood closer to reality.
Understanding ICSI Treatment
Intracytoplasmic Sperm Injection (ICSI) is a form of In Vitro Fertilization (IVF) that is specifically used to overcome severe male infertility issues. Unlike traditional IVF, where many sperm are placed with an egg in the hope that one will fertilize it, ICSI involves the direct injection of a single healthy sperm into a mature egg. This method significantly increases the chances of fertilization and is especially beneficial when sperm count is low, sperm motility is poor, or sperm morphology is abnormal.
Who Needs ICSI Treatment?
ICSI is typically recommended in the following cases:
Very low sperm count
Poor sperm motility or movement
Abnormally shaped sperm
Previous IVF failure due to poor fertilization
Obstruction in the male reproductive tract
Use of frozen sperm or sperm retrieved surgically
Unexplained infertility
For couples experiencing any of these issues, ICSI Treatment for Infertility in Delhi at Shivam IVF offers a targeted and effective approach.
Why Choose Shivam IVF for ICSI Treatment?
Located in the heart of Delhi, Shivam IVF Centre has become a beacon of hope for thousands of couples struggling with infertility. It is recognized not just for its world-class infrastructure and modern medical technology but also for its compassionate and patient-centric approach. Here’s why Shivam IVF stands out as a top destination for ICSI Treatment for Infertility in Delhi:
Step-by-Step ICSI Process at Shivam IVF
Here’s a detailed look at how ICSI Treatment for Infertility in Delhi is performed at Shivam IVF:
1. Initial Consultation and Testing
The journey begins with a comprehensive evaluation of both partners. Blood tests, ultrasound scans, semen analysis, and hormonal evaluations are performed to assess reproductive health.
2. Ovarian Stimulation
The female partner is given fertility medications to stimulate the ovaries to produce multiple mature eggs. This stage is carefully monitored through regular ultrasounds and blood tests.
3. Egg Retrieval
Once the eggs are mature, a minor surgical procedure is performed under sedation to retrieve the eggs from the ovaries.
4. Sperm Collection and Preparation
On the same day, a sperm sample is collected from the male partner or retrieved surgically if necessary. The healthiest sperm are selected for injection.
5. ICSI Procedure
A single, high-quality sperm is carefully injected into each mature egg using a microneedle under a high-powered microscope. Experienced embryologists perform this delicate process in a sterile lab environment.
6. Embryo Culture
Fertilized eggs (embryos) are monitored for 3-5 days in the lab. The healthiest embryos are selected for transfer.
7. Embryo Transfer
The selected embryo(s) are transferred into the woman’s uterus using a thin catheter. This is a painless procedure that is performed without anesthesia.
8. Pregnancy Test
Approximately two weeks after the embryo transfer, a blood test is conducted to confirm pregnancy.
Conclusion
Infertility no longer needs to be a roadblock in your journey to parenthood. With advanced medical treatments like ICSI and expert care from top fertility specialists, the dream of becoming parents is now more achievable than ever. For couples dealing with male-factor infertility or unexplained fertility issues, ICSI Treatment for Infertility in Delhi at Shivam IVF offers the hope and help they need.
Whether you’re just starting your fertility journey or exploring advanced treatment options after multiple failures, Shivam IVF is here to guide and support you every step of the way. Book your consultation today and take the first step toward building your family with confidence and care.
Contact Shivam IVF Today
30, Shanti Vihar, Karkardooma, Delhi – 110092
9810740459 | [email protected]
0 notes
Text
6 IVF Options Every Couple Should Explore
With the latest fertility science advancements, IVF(In-Vitro Fertilisation) brings hope for many couples dreaming of a family. IVF isn’t just one treatment, its a spectrum of possibilities. It gives you wide range of options to choose based on your body, medical history and personal preferences.Whether you’re just starting on this journey or have been on this for a while, understanding your IVF choices helps you to make informed decisions. Let’s explore six IVF options in this blog that every couple should know about on their journey to parenthood.
1. Conventional IVF: The Classic Route
This is the most common and well-known form of IVF which is widely tried and tested by many. It involves stimulating the ovaries with hormone injections to produce multiple eggs. These eggs are retrieved and fertilised in the lab using the partner’s sperm. After fertilisation, one or more of the healthiest embryos get transferred into the uterus.
Best suited for:
Couples with unexplained infertility
Women under 35 with good ovarian reserve
Cases where both partners are using their own eggs and sperm
This method is tried and tested but success can heavily depend on age factor and egg quality.
2. Mini IVF or Natural Cycle IVF: Gentler Approaches
For some reasons, some women prefer a less intensive yet successful option is they’re sensitive to medications or they want to avoid high hormonal doses. This method is called Mini IVF or Natural Cycle IVF, the former uses low dose stimulation and the later one is done without medications. In this method, fewer eggsa re retrieved but may produce higher quality embryos in select cases.
Best suited for:
Women with low ovarian reserve
Those wanting a more natural or body-friendly approach
Women prone to side effects or at risk for OHSS
Since fewer eggs are collected, this path may find physically and emotionally easier for the patients.
3. ICSI (Intracytoplasmic Sperm Injection): Targeted for Male Factor Infertility
For couples facing fertility issues due to the male partner, ICSI can be a game changer. In this method, healthy sperm is injected directly into an egg by an embryologist.
Best suited for:
Men with low sperm count, poor motility, or abnormal morphology
Couples with previous IVF fertilisation failures
Cases using frozen or surgically retrieved sperm
This method has significant success rates for many couples where the sperm needed a little help to get into the egg.
4. Frozen Embryo Transfer (FET): Timed for Success
In this method embryos created in the previous IVF cycle are kept frozen and are transferred in the future cycle. It gives the woman’s body time to recover from ovarial stimulation and maintains a optimal hormonal environment.
Best suited for:
Women who experienced OHSS
Couples delaying pregnancy for health or personal reasons
Those using PGT (genetic testing) before embryo transfer
This method has increased success rates and some research suggests frozen transfers can lead to healthier pregnancies in certain cases.
5. Donor IVF: When Your Own Gametes Aren’t Viable
When the either of the partners can’t use their egg or sperm due to medical , genetic conditions or due to age related reasons, this method is a powerful alternative. They can experience the joy of pregnancy and childbirth using donor eggs, sperm or embryos.
Best suited for:
Women with poor egg quality or early menopause
Men with non-retrievable sperm
Same-sex couples or single parents by choice
Mentally choosing donor IVF can be complex but it opens the door for parenthood.
6. Surrogacy: When Carrying the Pregnancy Isn’t Possible
Due to some reasons, some may not be medically fit or physically healthy to carry a pregnancy. In such cases, gestational surrogacy is done where another healthier woman carries the pregnancy using the couple’s embryo.
Best suited for:
Women with uterine abnormalities or past surgeries
Those with medical conditions that make pregnancy risky
Same-sex male couples
This method involves legal, financial and emotional considerations.
Choosing the Right Path for You
Each IVF procedures comes with its own set of considerations which should align medically, emotionally,financially and ethically with the couples who opt for and for the hospitals to perform this procedures. Its crucial to sit with a fertility specialist and analyse your case and understand your unique story. Choose the option which not only provides the medical solution but that one that aligns with your heart.
IVF is Not Just a Procedure—It’s a Possibility
Infertility can make you feel isolated but with modern IVF treatments it can open doors to numeros possibilities. Its about choosing the right choice according to your preferences. With the scientific advancements, hope comes in many forms. At Velammal Hospital’s Fertility Centre in Madurai, we walk this path with you, guide you and support you with compassionate care and personalised treatment plans in that way we help the couples turn their parenting dreams into reality. Book a consultation with our fertility experts today click here because the path to parenthood is different for everyone.
0 notes