#on a sprained ankle and recently dislocated knee
Explore tagged Tumblr posts
Text
Sometimes. Having a high pain tolerance. Is bad. 😓
#sd.txt#I have been stupidly moving around my room sans cane#on a sprained ankle and recently dislocated knee#because packing has to get done!#I have just sat down and now that I’m no longer distracted#the ouchies have come to feast upon my hubris#this is… not fine#but it is the entirely predictable consequences of my actions
6 notes
·
View notes
Text
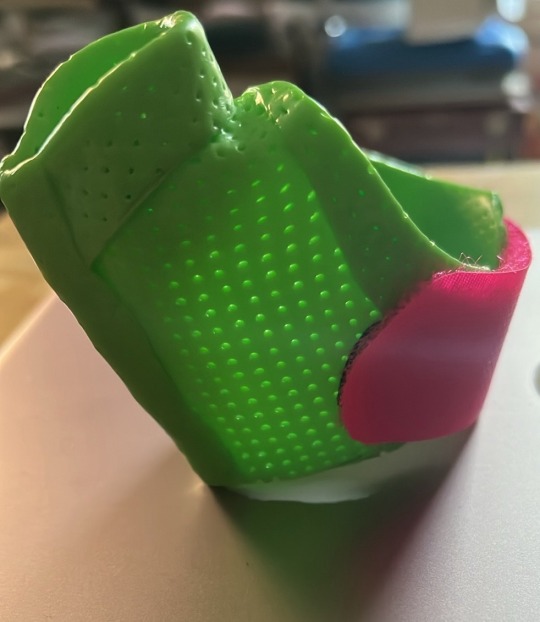
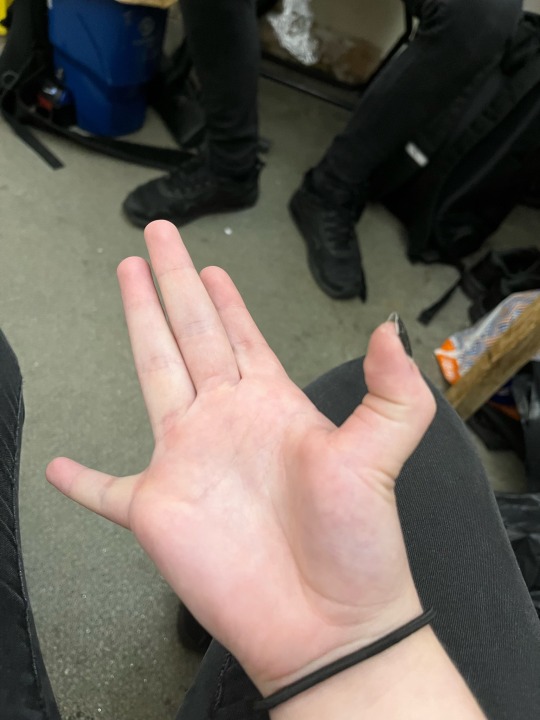
As most of you know I have been struggling with my health recently. This is my experience of HSD. Each person with the condition is affected differently and no two people are exactly the same with it. Just as a pre-warning I will be attaching photos at the end of injuries I have had but there is no blood. They are just dislocations and subluxations I’ve had. I also talk about some of the injuries as well. I am not writing this for sympathy but more as an explanation as to why I sort of disappear every so often.
Hypermobility Spectrum Disorders or HSD is a range of conditions that affect joint hypermobility. Often people are referred to as ‘bendy’, ‘flexible’ or ‘double jointed’. It is fairly common in children and young people but only 20% of people never lose the flexibility in their joints. More information about this condition is on The Ehlers-Danlos Society website.
This is my personal experience with the condition. Some people with HSD will experience these problems and others won’t.
When I was nine I had my first dislocation when my brother accidentally stood on my hand. I was taken to hospital by my parents and they sorted it pretty quickly with no alarms raised. However, when I was fourteen it got progressively worse. I kept having subluxations in my pinky finger on my right hand. A subluxation is an incomplete or partial dislocation of a joint. When I kept going to hospital they told me that it was a result of the injury when I was nine and they taught me how to manipulate it back into place. This happened almost everyday for two years at least.
The next year I dislocated my right thumb. Due to a medical error they missed the dislocation and the fracture on the x-ray and left it a week before noticing their mistake. I went back in to have it relocated a week after the injury. This is when I found out that I am immune to local anaesthetics so I had no pain relief when they did this. Due to a very observant doctor after my thumb dislocated inside of a plaster cast I was diagnosed with Joint Hypermobility Syndrome (the previous name for HSD).
After this I started having more subluxations and dislocations including in my ankle, both knees, my hip, my shoulder and my first and middle finger on my right hand.
Earlier this year I went to A&E with a swollen finger and they suspected rheumatoid arthritis. However, when I went to rheumatology I found that I was dislocating my finger in my sleep. That’s when my diagnosis name was changed to HSD. I scored a 6/9 on the Beighton Score. It is a system to measure joint flexibility. 0-3 is normal and 4-9 is when there is potentially a problem. I can hyperextend most of my joints and often I don’t notice when I am doing so.
I have now been receiving occupational therapy and I am on the waiting list for hypermobile physiotherapy.
My main symptoms include:
Fatigue but unable to sleep
Pain and stiffness in joints
Frequent strains and sprains
Frequent dislocations and subluxations
Poor balance
Bladder and bowel problems
I also suffer from scoliosis which I have had no treatment for and cluster headaches.
HSD is incurable and the only things I can do to help is have pain relief, hot baths, hot water bottles and hand warmers and use heat rub creams.
This condition affects my life quite severely. I haven’t got the worst symptoms someone can have but I am struggling to do daily tasks and even get out of bed some mornings. I use multiple types of joint supports as well as pen grips and back supports in my chair.
I am open to talking about this and will answer any questions about it.







20 notes
·
View notes
Text
I can't wait for the day when we can get our leg amputated. It'll make our life so much easier, in regards to dressing more masculinity or androgynously, in regards to pain levels, and so much more.
For context, our left leg is extremely screwed up (as in permanent damage-wise). Our knee is our biggest issue, constantly in pain, frequently swelling, subluxating and dislocating, giving out and being unsteady, and more—and we don't even have a diagnosis about what's wrong because we can't see all of the damage on MRIs or x-rays! Our ankle is also an issue, with being weak and hypermobile from constantly spraining, straining, and rolling it in elementary school. And last but not least, tendinitis. In not one, but more recently TWO tendons in our lower leg. (There's three tendons in lower legs.)
Our left leg is literally a piece of crap.
Someone take it away, please. I beg you. ToT
- Max / Kenneth
Front: Evan (xe/they)
#transgender#trans#transmasc nonbinary#transmasc#non-binary#non binary#osdd#osdd system#plural system#permanent damage#physically disabled#physical disabilty#disabled#cripple#cripple shit#someone please take away our fucking knee this is agony
4 notes
·
View notes
Text
random question time! has hanazaki ever focused on his tics too much and gotten stuck in a loop with his condition? has hanazaki ever suffered any injuries from his condition?


He has! Though it’s mostly from a recognition effect.
Hanazaki knows he has tics, he grew up with them from a young age, however, it only happens worse when it’s [ POINTED OUT ] either by - crowding, staring, vocal drops and mirrors. Hanazaki’s fell into several loops in the past, as a kid moreso than adult, from the lack of understanding of his own body and brain issues.
When a 10-year-old is smacking himself and humming extremely loud, it turns heads. It makes people stop and stare, it makes them film, point, gossip and laugh - mimicking him which is horrifying to a child. His first triggers tic-loop was in a supermarket, where his body just didn’t remember it was human and not a pretzel. His mother screamed, in fear of what was happening which in turn caused more and more attention to be put onto him and in turn made Hanazaki cry, scream and hum in several volumes of alarm - just not knowing what the actual heck was happening to his body.
Hanazaki was sedated by nurses from a called ambulance. After wetting himself, biting his tongue and spraining his shoulder from flailing so hard and bruising his eye from a mishap smack. He felt like a freak and broke down even more with his solitude in what he was and what he caused his Mother to go through.
It was a terrifying feeling for the whole family in all honesty and Hanazaki still has nightmares about it, enough to wake him each time, sometimes even wetting the bed from reliving that loss of full control. Thankfully now, when they are triggered it’s because he is constantly thinking about that time in the supermarket, it’s a one-track loop that makes him go, and then he is gone. But it took him around 12 years or so to get pass that loop with his own loop. Singing to himself really makes his head split in two in a sense. One side of his demented obsession makes him try and recite the lyrics perfectly, the other relapsing into his memory.
Over-all, it’s a hard gamble on which side wins, but over the recent years, he feels like he has mastered that coping mechanism to get himself out of a bad situation. Otherwise, he hopes that people are kind enough to call an ambulance once he is on the ground from his body just quitting in functioning normally for him.

He has indeed, injuries have bounced between;
Bruising upon his forehead from hitting himself too hard.
Sprained his ankle and wrist from over self-adjusting.
Neck-ache / whiplash from head twisting.
Bite a chunk of his tongue off from sneezing, grinding teeth and coughing all in one motion.
Dislocated two fingers from drumming his car door at a sharp angle.
Burned / Scolded his hand on hot items from ritual OCD fuelled touching. EG; moms hair straighteners, the iron on the ironing board, a boiling saucepan side.
Tripped himself up plenty of times from missing a step. Plenty of scrapped knees and hands.
Hanazaki is accident-prone, but it’s commonly due to his habit of just not registering what he is doing around himself. Touching things he knows are hot and painful, are just pushed aside, because if he doesn’t touch the saucepan’s hot-ass fuck handle for the second, third, fourth time to adjust it on the stove. He is going to have a fucking meltdown.
Over time Hanazaki’s got better at controlling the urges via moving onto another thing to get distracted, even if he still comes back to that thing, but he’ll do his best to divert his attention. It’s just constantly on his mind and his Mom often helps him regulate his breathing, thoughts and helps him in any way possible. ( EG; turning off the flame so he can touch, adjust and readjust the saucepan before moving on. )
2 notes
·
View notes
Text
Understanding Joint Pain and Swelling in Minors: Causes, Diagnosis, and Treatment

Introduction
Joint pain and swelling in minors are concerning symptoms that can significantly impact a child's daily activities and overall quality of life. While joint issues are often associated with adults, children and adolescents can also experience these problems. This article aims to provide a comprehensive overview of the causes, diagnosis, and treatment of joint pain and swelling in minors, helping parents and caregivers better understand and manage these conditions.
Common Causes of Joint Pain and Swelling in Minors
Joint pain and swelling in children can arise from various conditions, ranging from minor injuries to serious medical disorders. Some of the most common causes include:
1. Juvenile Idiopathic Arthritis (JIA)
Juvenile Idiopathic Arthritis (JIA) is one of the most common chronic rheumatic diseases in children. It is an autoimmune condition where the body's immune system mistakenly attacks the joints, leading to inflammation, pain, and swelling. JIA can present in several forms, including oligoarticular, polyarticular, and systemic JIA, each with distinct characteristics and patterns of joint involvement.
2. Infectious Arthritis
Infectious arthritis, also known as septic arthritis, occurs when a joint becomes infected with bacteria, viruses, or fungi. This condition can result from infections elsewhere in the body spreading to the joint or from direct injury to the joint. Infectious arthritis typically causes severe pain, redness, swelling, and fever, requiring prompt medical attention.
3. Injury or Trauma
Injuries such as sprains, strains, fractures, and dislocations are common causes of joint pain and swelling in children. These injuries can occur during sports activities, play, or accidents. In such cases, the pain is usually localized to the affected joint and is accompanied by swelling, bruising, and difficulty in movement.
4. Growing Pains
Growing pains are a common, benign cause of joint pain in children, typically affecting the legs. These pains usually occur at night and do not cause swelling or long-term damage. Growing pains are believed to be related to the rapid growth and development of bones and muscles.
5. Osteochondritis Dissecans
Osteochondritis Dissecans (OCD) is a condition in which a fragment of bone and cartilage separates from the joint surface, leading to pain, swelling, and limited joint movement. OCD commonly affects the knees, elbows, and ankles and can result from repetitive stress or trauma to the joint.
6. Reactive Arthritis
Reactive arthritis is a condition that develops in response to an infection elsewhere in the body, often in the gastrointestinal or urinary tract. This type of arthritis can cause joint pain and swelling, typically affecting the knees, ankles, and feet. It may also be accompanied by other symptoms, such as eye inflammation and skin rashes.
Diagnostic Approaches
Accurate diagnosis of joint pain and swelling in minors is essential for effective treatment. The diagnostic process typically involves a combination of medical history, physical examination, laboratory tests, and imaging studies.
1. Medical History
A detailed medical history helps identify potential causes of joint pain and swelling. The physician will ask about the onset, duration, and pattern of symptoms, as well as any recent injuries, infections, or family history of joint disorders.
2. Physical Examination
During a physical examination, the physician will assess the affected joint(s) for signs of inflammation, tenderness, warmth, and range of motion. They will also check for systemic symptoms such as fever, rash, and lymphadenopathy that may indicate an underlying condition.
3. Laboratory Tests
Laboratory tests can provide valuable information about the underlying cause of joint pain and swelling. Common tests include:
Complete Blood Count (CBC): To check for signs of infection or inflammation.
Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): To measure the level of inflammation in the body.
Rheumatoid Factor (RF) and Antinuclear Antibodies (ANA): To screen for autoimmune conditions such as JIA.
Joint Fluid Analysis: To detect infection or crystal deposits in the joint fluid.
4. Imaging Studies
Imaging studies help visualize the affected joint and surrounding structures, aiding in the diagnosis of joint conditions. Common imaging techniques include:
X-rays: To detect fractures, dislocations, and signs of arthritis.
Ultrasound: To assess soft tissue structures and detect fluid accumulation in the joint.
Magnetic Resonance Imaging (MRI): To provide detailed images of bones, cartilage, and soft tissues, useful for diagnosing conditions like OCD and soft tissue injuries.
Treatment Options
The treatment of joint pain and swelling in minors depends on the underlying cause, severity of symptoms, and the child's overall health. A multidisciplinary approach involving pediatricians, rheumatologists, orthopedic surgeons, and physical therapists is often necessary for optimal management.
1. Medications
Medications play a crucial role in managing joint pain and swelling in children. Commonly used medications include:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): To reduce pain and inflammation.
Corticosteroids: To control severe inflammation in conditions like JIA and infectious arthritis.
Disease-Modifying Antirheumatic Drugs (DMARDs): To slow disease progression in autoimmune conditions like JIA.
Antibiotics or Antiviral Medications: To treat underlying infections in cases of infectious arthritis or reactive arthritis.
2. Physical Therapy
Physical therapy is essential for maintaining joint function, improving range of motion, and strengthening muscles around the affected joint. A physical therapist will design a personalized exercise program tailored to the child's needs, focusing on pain relief, flexibility, and strength.
3. Orthopedic Interventions
Orthopedic interventions may be necessary for certain conditions, such as fractures, dislocations, and severe cases of osteochondritis dissecans. These interventions can include:
Casting or Splinting: To immobilize the affected joint and promote healing.
Joint Aspiration: To remove excess fluid from the joint and relieve pressure.
Surgical Procedures: To repair damaged structures, realign bones, or remove loose fragments in the joint.
4. Lifestyle Modifications
Lifestyle modifications can help manage joint pain and swelling in children. These may include:
Adequate Rest: To allow the affected joint to heal and reduce inflammation.
Balanced Diet: To support overall health and reduce the risk of obesity, which can strain the joints.
Appropriate Footwear: To provide proper support and cushioning for the joints during physical activities.
Weight Management: To minimize stress on weight-bearing joints and improve mobility.
Preventive Measures
While not all cases of joint pain and swelling in minors can be prevented, certain measures can reduce the risk of developing joint issues. These include:
1. Promoting Safe Physical Activity
Encouraging children to participate in safe physical activities with proper techniques and protective gear can help prevent injuries. Parents and caregivers should educate children about the importance of warming up, stretching, and following safety guidelines during sports and play.
2. Early Detection and Management
Early detection and prompt management of underlying conditions, such as infections and autoimmune disorders, can prevent complications and minimize joint damage. Regular medical check-ups and monitoring of symptoms are essential for timely intervention.
3. Maintaining a Healthy Lifestyle
Promoting a healthy lifestyle with a balanced diet, regular physical activity, and adequate rest can support joint health and overall well-being. Educating children about the importance of maintaining a healthy weight and avoiding overuse injuries is also crucial.
Conclusion
Joint pain and swelling in minors can significantly impact their daily lives and development. Understanding the common causes, diagnostic approaches, and treatment options is essential for effective management and improved outcomes. By promoting early detection, safe physical activity, and a healthy lifestyle, parents and caregivers can help minimize the risk of joint issues and support their child's overall health and well-being. If a child experiences persistent joint pain or swelling, it is important to seek medical attention promptly to identify the underlying cause and initiate appropriate treatment.
0 notes
Text
Tarik Crumpton Georgia’s Injury Prevention and Rehabilitation Strategies

In the fast-paced world of basketball, injuries are an unfortunate reality that can sideline even the most talented athletes. In this comprehensive guide, we delve into the essential principles of injury prevention and rehabilitation strategies tailored specifically for basketball players, drawing insights from the expertise of Tarik Crumpton, a renowned sports medicine specialist based in Georgia. With a focus on safeguarding athletes' health and optimizing performance, this resource offers invaluable knowledge for players, coaches, and medical professionals alike.
Understanding Common Basketball Injuries
Basketball places unique physical demands on athletes, leading to a variety of injuries ranging from sprained ankles to knee ligament tears. In this section, we explore the most prevalent injuries encountered by basketball players, including their causes, symptoms, and risk factors. Drawing from Tarik Crumpton Georgia's expertise, we highlight the importance of injury awareness and early intervention in minimizing the impact of these injuries on players' careers.
Injury Prevention Strategies on and off the Court
Prevention is the cornerstone of maintaining peak performance and longevity in basketball. Here, we discuss proactive measures that players can take both during training and in everyday life to reduce the likelihood of injuries. From proper warm-up routines and conditioning exercises to nutrition and sleep hygiene, He emphasizes the holistic approach required to keep athletes injury-free and performing at their best.
Rehabilitation Protocols for Basketball-Specific Injuries
When injuries do occur, an effective rehabilitation program is essential for facilitating recovery and preventing future setbacks. This section outlines evidence-based rehabilitation protocols tailored to common basketball injuries, such as ACL tears and shoulder dislocations. Drawing upon Tarik Crumpton Georgia's expertise in sports medicine, we delve into the stages of rehabilitation, key exercises, and progression milestones to guide athletes through the recovery process.
Integrating Technology and Sports Science in Injury Management
In recent years, advancements in technology and sports science have revolutionized injury management strategies for basketball athletes. From wearable devices for monitoring workload and biomechanics to sophisticated imaging techniques for injury diagnosis, He explores the cutting-edge tools and methodologies available to support athletes' health and performance goals. We also discuss the role of data analytics in identifying injury trends and optimizing training programs to mitigate injury risk.
Mental and Emotional Rehabilitation Support
Injuries not only take a physical toll but can also impact athletes' mental and emotional well-being. In this final section, we examine the psychological aspects of injury rehabilitation and the importance of providing athletes with comprehensive support beyond physical therapy. Drawing upon Tarik Crumpton's holistic approach to sports medicine, we discuss strategies for maintaining motivation, managing stress, and fostering resilience throughout the recovery journey, ultimately empowering athletes to bounce back stronger than ever.
0 notes
Note
🌅 = Early Bird or Night Owl?
📺 = Favorite Childhood TV Show(s)?
💈= Current Hair Color?
✨ = If You Could Be Any Supernatural Creature, What Would You Be?
📏 = How Tall Are You?
🥑 = Favorite Food(s)?
📍 = What’s The Furthest You’ve Travelled?
💀 = Have You Ever Broken A Bone?
🌅 Early bird or night owl?
EARLY BIRD. 4 am club over here!
📺Favorite childhood TV show(s)?
The Wiggles! And the Backyardigans
💈Current hair color?
Brunette. It always has been
✨If you can be any supernatural creature, what would it be?
Ghost, honestly. Cause I’m a paranormal fanatic
📏How tall are you?
5’ 2 and will be for the rest my life *cries*
🥑Favorite foods?
Netuella! I could just sit there and eat a whole jar of that if I could
📍What’s the furthest you’ve traveled?
Lourivelle, Kentucky. That was like a 10 hour drive or maybe 12 hour.
💀Ever broken a bone?
Yep. I dislocated my knee while dancing a couple years back and recently sprained my ankle from dancing as well
4 notes
·
View notes
Text
Silent Treatment

gif is not mine
word count: 3.1k
author: Allie
warnings: angst, some gore, talk about death. There aren’t really any, just a lot of feelings.
a/n: phew, okay, first post. Don’t be nervous, Allie, you can do it. Ah! Hi! I’m new to this! Please enjoy!
“Why do I always seem to find you in the infirmary?” You ask a dishevled Obi Wan with a knowing hand on your hip. His gaze flies from the expansive transparisteel to your eyes, a broad grin stretching his face.
“Where else would you find me?”
“I don’t know, elsewhere in the Temple.” You respond, checking your data pad then scanning his body for any injuries. “Or the senate building, perhaps. I don’t spend all of my time here, you know.” He lets out a chuckle.
“I know. But as a Jedi, I nearly always have an excuse to visit the med bay, more so than the senate building.” He remarks, his grin never faltering.
“It seems you live quite an opposite life from me, then.” You gather first-aid materials from the cabinets. “Senator Organa has been piling on the work. It seems the only time I’m not at the senate building is when I’m volunteering here-“
“Is when you’re spending time with me?” He grins playfully. You roll your eyes, but you can’t help the smile tugging at you lips.
“Patching you up, more like.”
“How is the Senator, by the way?”
“He is well.“
“Good.”
“Kind of you to ask about my mentor, Master Kenobi.” You smile as you prep a swab with antiseptic ointment.
“Well, his status tends to reflect onto you. I just want to make sure you’re well enough to fix me properly.”
You toss him another eye roll. His grin remains plastered.
“Now. What is your excuse for visiting me this time?”
“Well,” He began, “Anakin and I were assigned to guard Senator Amidala - there were recent threats on her life, my Padawan and I were the only ones available, you know how it goes. Anakin kept insisting that we investigate the matter, and I had to constantly remind him that we were there to protect, not interrogate. He was still difficult. Although, I’ve come to realize that when it comes to the senator, Anakin gets a little too carried away.”
“Doesn’t Anakin have a habit of getting too carried away?”
“Why, yes,” He chuckles, “However, I fear he has grown rather attached to her…” Obi Wan’s expression morphs, his grin faltering as he gazes at you. But it doesn’t remain long enough for you to decipher it. He shakes his head.
“Anyway, last night an assassin released a pair of Kouhun’s into the senator’s bedroom. Anakin sensed them just before I did. He ran in and killed the bugs just as I jumped out the window to-“
“You jumped out a window?!”
Obi Wan’s shit-eating grin returned.
“I’m alright, darling. I’m alive, aren’t I?” His assuring tone sends butterflies to your stomach. You shake your head and chuckle.
“How many times do I have to tell you to stop unnecessarily putting your life at risk?”
“How many times have I visited the infirmary?”
“Obi Wan…” Your tone is stern yet compassionate, and he senses your concern.
“I’m sorry.” He says genuinely as he holds your eyes. You feel the butterflies flit around your insides again.
“Just don’t let me catch you back in here again anytime soon.” You finish patching up his face you don’t say anything about how he needn’t come to the infirmary for a scratch and he nods.
“I promise.”
“If you’ll wait just a moment, the doctor will be in shortly-“
“I think I’m alright,” He hops up from the bed and turns to you. “I only came to see you, anyway.” His eye drops in a wink and he jogs out the infirmary door.
*******
You should be paying attention, Representative Binks just moved to give the chancellor emergency power, but your mind keeps drifting back to what Obi Wan said to you in the infirmary: “I only came to see you, anyway.” You always knew that his injuries weren’t the only reason he visited the medical wing, but he never admitted it out loud before. And the fact that it was accompanied by a wink, well, the butterflies hadn’t stopped dancing since. You think about Obi Wan every day and every night, for that matter the whole week, and your mind is still spinning with thoughts of the suave Jedi. You wonder what he’s been up to, what missions he’s completed, what planet he’s on. And secretly hope he might dislocate his shoulder or sprain his ankle so he might remain in the infirmary for a few days when he gets back…
“Well, this is a terrifying turn of events.” Senator Organa’s words drag you out of your thoughts. You involuntarily hum at his exclamation. The senator turns to you.
“Have you been listening at all?” He asks, you wince.
“Not entirely, Senator.” He only sighs in response
“Will you be volunteering in the med bay this evening?”
“Only tomorrow.” You shake your head.
“Good. We have our work cut out for us. I need to send a message to Padme…” His voice trails as your mind returns to Obi Wan, your mind relishing in the sparkle of his eyes and the joy of his smile and how good his ass looks in those trousers. In all your years of knowing him, you only recently started noticing how handsome he truly is. Sure, he was attractive as a padawan, but it was more his humor and his nature that made you want to be his friend. However, as soon as he cut the braid and grew out his hair, he began to make you weak in the knees.
You would never admit it, though, at least not out loud, and especially not to his face. He is a good Jedi, dedicated to the council and the code. You are not convinced he would break it for an aspiring politician like you. So, you keep your pining to yourself, and cherish the brief moments you share in the medical wing.
*******
Two weeks after Obi Wan’s last visit, you get word of a devastating battle on Geonosis. Hundreds of Jedi dead, and the few survivors are to return in mere hours. Your mind instantly pictures your Jedi, the one you’ve foolishly grown so fond of. Had he been there? Did he make it out? Is he alive?
You tune your ears into the whispers buzzing through Senate. “Master Yoda came in with a clone army.” “Count Dooku is apparently a Sith Lord.” “Senator Amidala along with Master Kenobi and his padawan were captured and sentenced to be executed-“
Executed?! Your mind races against your heart, a neck and neck battle for the finish line. You bolt to the elevator, bouncing your knee and tugging the pendant around your neck, anxiously urging the machine to move faster. It reaches ground level. You don’t even bother looking for a speeder, the notorious Coruscant traffic will only hinder your mission. You run. No, sprint. With your shoes in your hand and the concrete hard on your feet, all you can think about is getting to the Jedi Temple as fast as possible, confirm that your Obi Wan isn’t dead.
The thought makes your heart shrivel inside your chest, and you aren’t sure if it’s the sting of the wind or your pain that pricks tears into your eyes. Obi Wan was permanent for you, a constant in your life. You wouldn’t know what to do if he were taken from you. Who else would brighten your day with only a smile? Who else would bring you such unconditional joy?
You don’t know how long it takes for you to arrive at the temple, but as soon as you do, you B-line for the docking bay, heaving and aching. You immediately spot Padme and Anakin being helped onto stretchers. You get closer and notice Padme has a gash slicing her back and Anakin missing an arm, but no sign of his Master.
“Where is he?” You pant when you reach them. Anakin looks at you, reassuring yet unsurprised.
“He’s already at the infirmary. He’s in better shape than I am.” He winces and your heart rate slows.
“Oh, thank the Maker.” You exhale and express your gratitude before darting up to the medical wing.
“Miss (Y/L/N), I thought you didn’t have a shift today-“
“I’m here to see Master Kenobi.”
“Oh!” The receptionist’s eyebrows raised. “He’s just inside. He’s been asking for you.”
Asking for you. You barrel into the infirmary and scan the now-filled beds for the familiar strawberry blonde hair. You pan the room, eyes frantic until-
There he is, tucked into the bed furthest on the left, as disheveled as ever. Your shoulders drop in relief and his eyes meet yours. His grin splits his face as you approach him, like your presence is the only treatment he needs. All you can see of his injuries are a few scratches on his face and his arm in a sling. You are sure that isn’t the extent of them, but he’s breathing, and that’s all that matters. But it doesn’t ease the constricting under your ribs. You can tell he senses your concern and his brow creases.
“I’m fine, darling,” His voice is hoarse. “I’m going to be fine. The doc said they’re just flesh wounds.” Wounds. There’s more than one. “A few days in a bacta tube and I’ll be back to normal.”
“I heard you were to be executed.” Your lip unwillingly trembles. “I thought you…died,” You whimper. “I…I thought I lost you.” Your knees buckle. Obi’s smile falters and he reaches for your hand.
“You could never loose me, little one,” He brings your hand to his lips. “Never.”
You tear slips down your cheek and you stare at the hand that so gingerly grasps yours. Seeing him alive and intact should be enough to relieve you, yet you can’t help the nagging, tugging at your heart. What if you really had lost him? What if he was reckless? Or outnumbered? Or worse, what if he decided to play the hero and sacrifice himself? What would have been left of you then? Would he have even thought of you before drawing his final breath? Would he be as broken if the roles were reversed…?
You gently drop your hand from his grasp and you watch as his brow furrows. Without another word, you back away and slowly make your way out of the infirmary.
*******
It’s been days, no, weeks, you lost count since you last saw Obi Wan. This time, however, it’s on purpose that you don’t see him. On the day of his so near brush with death you vow to limit your interactions with your favorite Jedi. It would be easier to forget him that way. You cancel your shifts in the infirmary and dive head first into your senate work. And it’s not like you have to try very hard to do so: Senator Organa is swamped with messages and whatnot since the start of the Clone Wars, and can’t go through it all alone.
On day 15 17 18 locked in the senator’s office, you get a call from a rather frantic receptionist at the med bay.
“Please, Miss (Y/L/N)- there’s an empty bed in wing 5 -we are so short staffed and- the saline packets are already prepped -we could really use your help.”
“I’m sorry, but Senator Organa and I are overloaded with work-“
“If they need you, (Y/N), you can go.” The senator interrupts. Your eyes beg him to provide you with an excuse - you know if the infirmary is overwhelmed, then Obi Wan Kenobi is surely among the patients.
“But Senator, there’s still so much to-“
“Go.” He smiles knowingly. “I’ll be fine.” You fight the urge to roll your eyes. You know the receptionist on the other side of the hologram could hear the exchange with your mentor, so there was no way to wiggle yourself out of this one.
“I’m on my way.”
This time on your way to the temple, you’ll take a speeder.
When you arrive, it’s chaos. 50 clones are packed into the first wing of the infirmary, and you can imagine how many more congest the others. You grab the nearest datapad and quickly start assessing soldiers, determining who can be cleared and who needs to stay over night. You’re just finishing up with your 39th? patient when a familiar voice materializes behind you.
“You’ve been avoiding me, little one.”
You pause, blink slowly and let out an exasperated sigh. You discharge the clone, he was in better shape then most of his comrades, and muster all of the courage you can to face your Obi Wan. He’s banged up, but not nearly as busted as the last time he visited. However his most disturbing injury is that his usually sparkling eyes are shrouded in confusion.
“I haven’t-“
“Don’t lie to me,” He’s stern, “I can sense it.” Hurt flashes in his eyes before fading into selfless concern. He can see you’re struggling, but he doesn’t know why.
“Master Kenobi-“
“Darling, you can talking to me. Whatever is troubling you, please-“
“Master Kenobi, this is hardly the time or place-“
“I’ll come to your apartment tonight, then.” He tries to calm the panic in your voice and smiles warmly. “For a cup of tea.”
You can hardly focus the rest of the day. He looked so small, his usual confidence eluding him. You dare, for just a moment, to entertain the thought that he might be just as terrified to loose you as you are to loose him. But an incorrect stitch on a soldier’s wound immediately shakes it from your mind. As the amount of patients in the infirmary dwindle, the chief medic approaches you.
“Your assistance is no longer necessary, Miss.” He shakes your hand “Thank you for coming on such short notice.”
“I’m happy to help.”
You make your way back to your apartment just as the sky starts to darken. You realize that Obi Wan never told you what time he would arrive. Of course didn’t, even without a schedule, his timing is always impeccable. You ponder what you might say to him. There’s no way to explain your recent behavior without confessing your feelings to him. But his eyes keep flashing in your mind; desperate, hurt, and confused. Is it at all possible he feels the same way?
You continue with your nighttime routine as if he weren’t coming at all. It’s better than just sitting and waiting at your kitchen table. You allow your body to take over and your mind to relax. The conversation you’re about to have is inevitable, there is no use fretting about it. You’ve been distancing yourself from him this whole time to lesson the pain of loosing him. Whether you lost him to his own mortality or to unrequited love, you are prepared nonetheless. At least, that’s what you tell yourself.
You almost don’t hear the soft knock on your chamber door. You’d been staring into space for longer than you care to admit, lost in the beating of your heart in your throat. Your eyes flick to the door and you swallow the lump you notice forming.
“It’s unlocked.” You announce meekly. The door creaks, and a just as timid Obi Wan steps through.
“You really shouldn’t leave your door unlocked, you know.” He closes it with a soft thud. On any other day, you would have come up with an equally witty remark, but in this moment, all you can do is nod.
“Have you started the kettle?” He asks, already knowing the answer. He meets you in the kitchen and goes straight to the cabinet where the tea kettle lived. He’s been to your place countless times before. But this time, it feels like a stranger is in your flat. You’re silent as he prepares the pot.
“Tell me what’s on your mind, darling.”
“Obi…” You mumble. “I don’t know where to start.” Obi wan pulls two mugs from a top shelf.
“That day, after I came back from Geonosis, I’ve never seen you so upset.” He explains.
“I was.” You revel in how patient he’s being with you. You can feel how desperate he is for answers, but he isn’t pushing you. It’s in this moment you realize how much you’ve missed him, how wrong you’ve been this entire time.
“I was so afraid of loosing you, Obi Wan.” You begin, and your voice cracks. Obi Wan stops prepping the tea. You take a shaky breath. “I understood that the threat was always there, but being so close to actually loosing you…it terrified me. I thought that by limiting my contact with you, that fear would subside, I wouldn’t be so attached to you anymore.” You find his eyes. “I realize now how wrong I was.”
“What do you mean?”
“I realize that I would rather have you in my life and risk loosing you, than not have you at all. I’d rather risk my heart breaking everyday because I know you don’t love me the way I love you-“
You gasp. Your hands fly to cover your mouth. You’ve never said it aloud before. You swore you’d never say it to him. You watch his eyes widen and panic seeps into your veins.
“Oh, Obi Wan, please forgive me. I don’t want-“
In two long strides, his lips are on yours, his calloused hands gently, desperately pulling your face against his. You’re caught completely off guard, worried words muffled by his gesture. You would have fallen if it weren’t for his sturdy grasp.
But despite your whirring thoughts, your body melts into him, and you allow yourself to be held…kissed. Soon, your mind follows suit, and Obi Wan senses your relaxation. He relinquishes your lips, slow but sure, and eventually opens his eyes to meet yours, wide and searching. You bring your hands to hover above his chest. You’re trying to form words, but they escape you. All you can think about is Obi Wan stroking your hair behind your ear. You accept defeat, unable to express all that you are currently feeling, and place your hands on his chest.
“I am sorry to have been breaking your heart for so long,” He whipsers, “But it baffles me that you think I do not love you.” He rests his forehead against yours. “How could I not?”
“But the code-“
“Code be dammed.”
“But it’s illegal, Obi. You’ll be expelled.”
“Shhh, darling. That’s a conversation for the morning. For now, just promise you’ll never ignore me again. I couldn’t bare it.”
Relief, true relief, relaxes your shoulders and exhales from your mouth. You slide your fingertips along the linen of his tunic to his now shorter hair, pressing yourself closer to him.
“I promise.” You vow against his lips, this kiss gentler and sweeter than the last, lost in the bliss and the warmth that is your Obi Wan.
#obi wan kenobi#obi wan#obi wan imagine#obi wan x reader#obi wan x y/n#obi wan fanfiction#star wars#star wars fanfiction
155 notes
·
View notes
Text
Survivor (Prologue) - Part 1
Zaurac Al-Saiph did not expect to die on such a fine autumn day, but he stood steadfast, determined to give his last stand against the enemy.
The Redguard stood before three more undead, his sword gripped in both hands as the midday sun reflected off its deadly edge. Behind him lay the corpse of his horse; the poor beast had been skewered by a skeleton’s errant spear.
Beyond that, the battle still raged, with Zaurac’s comrades being cut down. They had escorted caravans near the coast for weeks, watching for any pirates or Aldmeri sea raiders attempting to make landfall near the borders joining Bangkorai and Hammerfell. During their most recent journey back to Sentinel, they had been ambushed by a horde of undead; the necromancers who controlled them had likely waited weeks to attack.
A zombie shuffled towards him, its rust-splotched blade raised high for Zaurac’s head. Zaurac tightened the grip on his sword hilt and twisted, the blade rebounding off his weapon and throwing the reanimated corpse off-balance. Before the husk could recover, Zaurac brought his blade in a horizontal slash across its neck, beheadinh im. The next zombie advanced, attempting to grab the Redguard in a vice grip. Zaurac brought his boot up and kicked it to the ground, plunging his sword downwards into its chest as it lay supine.
The final undead, a skeleton of immense size, charged at Zaurac, bringing its axe in a downward sweep. Zaurac noticed the tusks in its jaw and the moldering cuirass it wore and cursed; orcs were already hard enough to fight while they were alive. Attempting to block the blow with his sword would have dislocated his arms, so Zaurac pivoted out of the way, the axe missing him by mere inches. The Redguard slashed his sword at the skeleton orc with little success - even in poor condition, orcish armor was sturdy, and the blade rebounded from the cuirass. The skeleton redoubled its assault, blue witchfire burning in its empty eye sockets, and swung again. The blow only clipped Zaurac in one of his pauldrons, but the force behind the strike sent him sprawling to the ground. Stars exploded in his vision as the impact with the earth hit him; Zaurac blinked several times to clear his vision, only to see the axe coming down for his face.
Zaurac rolled out of the way a mere second before the axe came crashing down. Rising to his feet, Zaurac unsheathed the mace he carried on his belt. Most Redguards preferred to fight with swords, a tradition that was carried all the way back to their Yokudan ancestors, but Zaurac realized the necessity of blunt weapons.
Especially at a time like this.
Fortune seemed to smile on Zaurac for a brief moment, because the skeleton had struck with such force that the axe was momentarily lodged in the terrain. Before the foe could fully recover itself, Zaurac swung his mace, his muscles and shoulders carrying the weighted weapon forward, striking the skeleton’s left leg. The limb exploded in a burst of bone shards, causing the skeleton to topple to the ground. Bringing the weapon up again, Zaurac brought it downwards, striking the skeleton’s skull repeatedly until it no longer moved.
Zaurac straightened himself, beards of sweat rolling down his forehead. Before he could even spare a moment to survey the battlefield, he was forced to duck under a shard of ice aimed for his head by a necromancer. Zaurac glanced up to see the wizard stalking towards him, her hands motioning to strike again. The Redguard snarled in frustration; there was no way he could close the gap to her in time, and his bow lay by his horse’s saddle behind him.
Zaurac dropped his mace and gripped his sword in both hands once more.
Only one chance to pull this off.
The necromancer, despite showing magical aptitude, appeared young and inexperienced with combat, as indicated by the lack of markings on her black robes. Zaurac waited for the moment she was about to cast again, raised his sword over his head and flung it with every ounce of strength he had. The weapon was not weighted to be thrown, but it soared end over end, tearing into the necromancer’s robe.
The sword tore into her robes; she shrieked and flung her arms towards Zaurac, the ice shards hurtling towards him in a lopsided manner. Zaurac dodged the first one, but the second one struck his hip, and he used the momentum of the blow to trip himself over his horse and land near his bow and quiver. Zaurac gritted his teeth in agony; had the necromancer completely finished the spell, the shard would have likely skewered him. Zaurac nocked an arrow into his bow, holding it downward near his groin as he lay there. He could hear the necromancer walking closer.
The second Zaurac could see her come into his view, his hands moved in a blur, raising the bow to fire.
The necromancer’s smug, self-assured look of triumph drained and gave way to shock as the arrow lodged itself into her throat. She collapsed to her knees and fell to her side as the last essence of life ebbed from her desiccated body.
Zaurac sat up, his attempts to stand coming to a halt when he shouted in pain. He had sprained his ankle, his shoulder burned with pain, and it felt like he had broken two of his ribs in the fighting. His lungs felt like they were burning as his chest rose and fell. He placed his left hand on the ground and positioned himself to survey the field.
Everyone had perished. He was the last one alive.
He was miles away from the nearest outpost. With his wounds and with no horse, there was no way he could possibly drag himself to safety. Zaurac lay on his back and consigned himself to his death. He hoped that Tu’whacca would show favor on him for avenging the deaths of his fellow Redguards.
He knew not how long he lay there, waiting for death to take him, but he heard shouting from the coast. Zaurac opened his eyes, his vision blurred, and thought he saw the sails of Aldmeri ships.
No. Not Aldmeri. Worse.
Pirates.
The last thing Zaurac saw before blacking out were the brigands walking towards him with chains.
#The Elder Scrolls#the elder scrolls online#My writing#writing#heralds of nerevar#hammerfell#redguard#zaurac al-saiph
7 notes
·
View notes
Text
#TripAndFall #PersonalInjury #WinningMatters TRIP AND FALL
Trip and fall accidents can result in serious injuries and long-term consequences. Fixed objects, uneven surfaces like broken sidewalks, or objects impeding a pathway can initiate a stumble which can often result in a fall. Some of the most common types of injuries resulting from a Trip and Fall are hip, wrist, and ankle fractures and elderly people are more likely to break a bone as a result of a fall. Other types of injuries can include sprains, dislocated shoulders, knee damage, spine and nerve damage, and traumatic brain injury.
It is important to have a report of the incident. If possible, gather evidence such as:
Take photographs of the scene of the accident;
If someone witnesses your fall, gather their information;
If your trip and fall occurs in a store, such as a department or grocery store, make sure you file an accident report. You can do this by asking for the manager and they will then document your version of the accident. This will prove to be valuable in representing you for your injuries. If possible, make sure to obtain an accident report prior to leaving the store.
If you or your loved one have suffered serious injuries from a trip and fall, let us fight for you to get the compensation you deserve. Call us today to set up your free consultation at 718-502-9112 and be sure to visit our website for more information: https://www.karasiklawyers.com/. At Karasik Law Group, Winning Matters! Our office recently settled a trip and fall case prior to trial for $70,000.00. We speak for the injured; our results speak for themselves.
source https://karasiklawyers.com/tripandfall-personalinjury-winningmatters-trip-and-fall/ source https://kristynam.tumblr.com/post/188812360150
1 note
·
View note
Text
medical issues dump
Every medical issue i can think of at the moment. This is mostly a vent post.
~~~~~~~~
I have hypermobility in my joints that causes pain mostly in my knees, hips, wrists, and to a lesser degree, my ankles, elbows, and shoulders (not really much back pain, thank god).
With my knees and hips, it can make it painful to walk. Most of the time I'm in no pain at all and I can walk/run/whatever perfectly fine. But when it hurts, I have to walk with a bit of a limp. There was only one occasion, though, where it was so bad I was scared to walk at all and I kinda limp-hopped around the house for a few days until it got better. I've considered getting a cane, but really I don't think I'm in enough pain that often to warrant one.
The issue with my wrists upsets me more, though. For background: I've dreamed of doing gymnastics/cheer since I was a kid but it was too expensive. It is one of my few life goals to do a back handspring. Finally in college, I joined the cheer team. And only a couple months in, I learned the hard way that hypermobility lends to easier sprains. I sprained both my wrists practicing (spotted) back handsprings. It takes a longer time to heal with hypermobile joints too. Even a year after that happened, I still felt the effects when I put too much strain on my wrists. This specifically really destroys me inside. But it's whatever. I don't care if I break both arms doing it, I'm gonna do a back handspring at some point.
The wrist pain is easier to play off in everyday life. The knee/hip pain though is a bit embarrassing. I try to limp discreetly cause I can't stand the idea of people seeing me limp. And what am I supposed to tell friends/acquaintances? "I have hip pain" What am I a fucking grandma?? It makes me cringe.
And that is why I've turned to whump to romanticize my pain. Whump makes me feel better about myself because it takes something I can't stand (haha literally) about myself, and spins it into something enjoyable. Also, seeing how people enjoy whump, it gives me this sense of hope that what I see as cringy and embarrassing for myself, at least some people won't see it that way. And I know this is probably not the best coping mechanism but it makes me feel a bit better about myself.
~~~~~~~~
About my other issues/ symptoms:
This is one of the most pressing issues right now. Recently I've had issues with getting too dizzy when I stand up. Sometimes I just feel a little dizzy, sometimes I'm very dizzy and find myself on the ground without losing consciousness, and sometimes I actually pass out for just a second. And sometimes I'm perfectly fine. It's weird and I don't know why it's happening. This is also something that makes me cringe imagining anyone seeing me like that. That would be so embarrassing, between the hip pain and the fainting, you'd think I'm 90 years old. But that hasn't happened yet, I can hide it pretty well by pretending to look at my phone and leaning against the chair.
I get really really heavy periods. Like, "Putting on a Maxi Extra Heavy Overnight pad and bleeding through my pants in 20 minutes", heavy. It's been so bad that sometimes I don't even bother going to class, because I know I'll either be in and out of the bathroom or bleed through my pants into the seat. And I'm lucky I only get normal cramps now, I used to get the worst cramps when I was younger. I've felt pain before. I've sprained both my wrists simultaneously. I've slammed head first into the ground from 8 ft in the air. My shoulders will sometimes partially dislocate. When I say period cramps are the worst pain I've ever felt, I mean it 100%. I remember being 13, in so much pain I was literally begging and praying for death. Not a fun time.
Around the same time that I started getting joint pain (abt 12 y/o), my hair started falling out a lot. Not in big clumps that make bald spots, but enough that my hair is very visibly thinning. I cut my hair to a short, almost bowl cut so I don't have to deal with as much mental distress combing out long hair and watching it all fall out.
I have Keratosis Pilaris, an overproduction of keratin that creates little bumps on my legs. I dont think i will ever experience having smooth legs and i know thats the least of my problems but really upsets me for some reason. also- possibly related to the hair thing?
I have Rumination Syndrome and have had it since I was young. Basically, it's hard sometimes for me to keep food down. Sometimes I regurgitate food back up. cool right :/
uhh what else
I have diagnosed ADHD
I have had bad anxiety since I was a kid, and still now, but am not diagnosed. Still bitter towards my parents seeing me struggle like that as a little kid and doing nothing.
Probably relating to anxiety, I have developed some sort of nervous tic that forcefully jerks my head to the side whenever I think of something embarrassing, stressful, or anxiety-inducing, which is pretty frequent. It feels like my brain is punching me in the face. It gives me headaches :(
0 notes
Text
Asia-Pacific Trauma Fixation Market Manufacturers, Regions, Type and Application, Forecast To 2027
Market Analysis and Insights: Asia-Pacific Trauma Fixation Market
Asia-Pacific Trauma Fixation Market, By Type (Internal Fixators, External Fixators and Other Trauma Products), Material (Stainless Steel, Titanium and Others), Surgical Site (Lower Extremities and Upper Extremities), End User (Hospitals, Trauma Centers, Ambulatory Surgery Centers and Others), Distribution Channel (Direct Tender and Retail), Country (Japan, China, India, South Korea, Australia, Singapore, Malaysia, Thailand, Indonesia, Philippines, Rest of Asia-Pacific) Industry Trends and Forecast to 2027
Download Exclusive Sample PDF at: https://www.databridgemarketresearch.com/request-a-sample/?dbmr=asia-pacific-anti-nuclear-antibody-test-market
Trauma fixation market is expected to gain market growth in the forecast period of 2020 to 2027. Data Bridge Market Research analyses the market to growing at a CAGR of 6.69% in the above-mentioned forecast period.
Growing incidence of trauma cases such as burns, fractures, dislocations, sprains, and strains and rising geriatric population are major factor driving market growth whereas high risk for osteoporosis will increase demand for market, favourable reimbursement policies and rising awareness about latest technological development in trauma fixation devices will boost market growth. In addition technological advancement and innovation of new devices will create lucrative opportunities for market in coming years. However, the high cost of devices and issues like side effects from usage of these devices are the restraining factors for the market whereas the availability of alternatives will be the challenging factor for the market.
This Asia-pacific trauma fixation market report provides details of new recent developments, trade regulations, import export analysis, production analysis, value chain optimization, market share, impact of domestic and localised market players, analyses opportunities in terms of emerging revenue pockets, changes in market regulations, strategic market growth analysis, market size, category market growths, application niches and dominance, product approvals, product launches, geographic expansions, technological innovations in the market. To gain more info on Data Bridge Market Research trauma fixation market contact us for an Analyst Brief, our team will help you take an informed market decision to achieve market growth.
Have Any Query? Ask Our Expert @ https://www.databridgemarketresearch.com/inquire-before-buying/?dbmr=asia-pacific-trauma-fixation-market
Trauma Fixation Market Scope and Market Size
Trauma fixation market is segmented on the basis of type, surgical site, material, distribution channel and end-use. The growth amongst these segments will help you analyse meagre growth segments in the industries, and provide the users with valuable market overview and market insights to help them in making strategic decisions for identification of core market applications.
Based on type, the trauma fixation market is segmented into internal fixators, external fixators and other trauma products. Internal fixators are further segmented into plates, screws, nails, and others whereas external fixators unilateral & bilateral external fixators, circular fixators, and hybrid fixators.
Based on surgical site, the trauma fixation market is segmented into lower extremities and upper extremities. Lower extremities segment is further segmented into hip & pelvic, foot & ankle, knee, and others. The upper extremities segment is further segmented into hand & wrist, shoulder, spine, and others.
On the basis of distribution channel, the trauma fixation market is segmented into stainless steel, titanium and others.
On the basis of distribution channel, the trauma fixation market is segmented into direct tender and retail.
Trauma fixation market has also been segmented based on the end use into hospitals, trauma centers, ambulatory surgery centers and others.
Trauma Fixation Market Country Level Analysis
Trauma fixation market is analysed and market size insights and trends are provided by country, type, surgical site, material, distribution channel and end-use as referenced above.
The countries covered in the trauma fixation market report are the China, Japan, India, South Korea, Singapore, Malaysia, Australia, Thailand, Indonesia, Philippines, Rest of Asia-Pacific (APAC) in the Asia-Pacific (APAC).
India, Japan and China are expected to register significant market growth rate due to rising awareness about growing incidence of trauma cases and increasing geriatric population whereas rising government initiative to improve healthcare infrastructure and technological advancement will fuel region market growth.
The country section of the trauma fixation market report also provides individual market impacting factors and changes in regulation in the market domestically that impacts the current and future trends of the market. Data points such as consumption volumes, production sites and volumes, import export analysis, price trend analysis, cost of raw materials, down-stream and upstream value chain analysis are some of the major pointers used to forecast the market scenario for individual countries. Also, presence and availability of global brands and their challenges faced due to large or scarce competition from local and domestic brands, impact of domestic tariffs and trade routes are considered while providing forecast analysis of the country data.
Request for TOC @-https://www.databridgemarketresearch.com/toc/?dbmr=asia-pacific-trauma-fixation-market
Healthcare Infrastructure growth Installed base and New Technology Penetration
Trauma fixation market also provides you with detailed market analysis for every country growth in healthcare expenditure for capital equipment, installed base of different kind of products for trauma fixation market, impact of technology using life line curves and changes in healthcare regulatory scenarios and their impact on the trauma fixation market. The data is available for historic period 2010 to 2018.
Competitive Landscape and Trauma Fixation Market Share Analysis
Trauma fixation market competitive landscape provides details by competitor. Details included are company overview, company financials, revenue generated, market potential, investment in research and development, new market initiatives, global presence, production sites and facilities, production capacities, company strengths and weaknesses, product launch, product width and breadth, application dominance. The above data points provided are only related to the companies’ focus related to trauma fixation market.
The major players operating in the trauma fixation market report are Johnson & Johnson Services Inc., Smith & Nephew, Stryker, Zimmer Biometr, Integra Lifesciences Corporation, Medtronic, Bioretec Ltd., B.Braun Melsungen AG, Arthrex, Inc., Corin, Orthofix Medical Inc., Acumed LLC, Wright Medical Group N.V., NuVasive Inc., Advance Orthopaedic Solutions, Arthrosurface, and CONMED Corporation among other domestic and global players. Market share data is available for global, North America, Europe, Asia-Pacific (APAC), Middle East and Africa (MEA) and South America separately. DBMR analysts understand competitive strengths and provide competitive analysis for each competitor separately.
Customization Available
Data Bridge Market Research is a leader in advanced formative research. We take pride in servicing our existing and new customers with data and analysis that match and suits their goal. The report can be customised to include price trend analysis of target brands understanding the market for additional countries (ask for the list of countries), clinical trial results data, literature review, refurbished market and product base analysis. Market analysis of target competitors can be analysed from technology-based analysis to market portfolio strategies. We can add as many competitors that you require data about in the format and data style you are looking for. Our team of analysts can also provide you data in crude raw excel files pivot tables (Factbook) or can assist you in creating presentations from the data sets available in the report.
Browse more related report to know about market analysis
Asia-Pacific Flexible Digital Video Cystoscopes Market
Asia-Pacific Intraoperative Imaging Market
Asia-Pacific Skin Tightening Market
Dental Diagnostic & Surgical Equipment Market
Europe Cardiac Pacemakers Market
Data Bridge Market Research set forth itself as an unconventional and neoteric Market research and consulting firm with unparalleled level of resilience and integrated approaches. We are determined to unearth the best market opportunities and foster efficient information for your business to thrive in the market
Contact: Data Bridge Market Research
Tel: +1-888-387-2818
Email: [email protected]
0 notes
Text
Klaine Advent - “A Dancer Dies Twice” - (Rated PG)
After an unfortunate accident, Kurt, Principal Dancer for the New York City Ballet, is forced to retire.
But he's nowhere near ready. (1728 words)
Notes: Written for the Klaine Advent prompt Day 3 - collapse. The title and inspiration comes from an NPR segment I was listening to of the same name, but, as with other one-shots I've written recently, this one is also personal. Angst, emotional hurt/comfort, reference to injuries and bruises.
Read AO3.
“Hey, baby. Are you ready to go yet?”
Kurt doesn’t answer right away, sifting through the contents of a bag he’s packed and re-packed at least two dozen times in the past hour. Not that he had much to pick up to begin with. Aside from his favorite costumes (that the NYCB was being gracious enough to let him have), he’d forgotten a few dance belts, a pair of shoes, and a leotard, all of which he’ll probably end up tossing in the Goodwill bin anyway. He was really only back to shake some hands, say his obligatory good-byes, and fill out paperwork.
Finalize the details of his retirement.
But he needed this – to sit on the worn, wooden floor of the practice room one final time before it was all over. He had spent two decades here, having been accepted to the School of American Ballet before the end of high school. He’d learned here, taught here, performed here.
He’d also collapsed here – twisted his ankle on a landing three months ago and hit the floor so hard, he’d dislocated his shoulder. Ten years ago, it wouldn’t have been that big a deal. He’d pop it back in, finish his lesson, then go home and ice up – no real harm done … or so he’d thought. Apparently, those injuries he’d muscled through – the sprained ankles, the pulled muscles, the bruised knees, the wrenched shoulders - had all started to add up.
They were all strikes against him.
At the time, he could shrug it off. His ankle and his shoulder would look gross for a while, but that’s the price of being a dancer for the New York City Ballet. He wore those black-and-blues with pride, danced with his shirt off when he had them so that everyone could see, could marvel at his strength and perseverance.
His resilience.
But that was ten years ago. He’s not the same man he once was, even though, in his heart, he feels like nothing’s changed. He’s still that sixteen-year-old boy standing on the stage in his high school auditorium, being told again that he was too “effeminate” to convincingly play a leading man. That was a turning point in his life. He’d had to decide then and there – should he accept rejection with grace and plug along, knowing that there would probably be more, similar rejections ahead? Or should he take this thing about himself that everyone else saw as a deficit and turn it into the greatest positive of his life?
In the end, he chose the latter. He quit his school’s Glee club and theater program, and enrolled in ballet. Ballet had been his first real passion from back when he was six and life had yet to bombard him with its grim and inescapable realities - with death, and bullying, and heartbreak. He’d always been told that he had a natural, easy grace, and a fluidity of movement that couldn’t be taught. It was simply innate. So he’d go to a place where those things were considered an asset.
He’d started with a simple recreation center class, something to get his feet wet, until a chance encounter with a guest director sling-shotted him to stardom – a private audition, followed by an offer of early enrollment and a scholarship. Before he knew it, mere weeks after he’d made up his mind to re-set his course in life, he was testing out of McKinley, taking the first plane out of Ohio, and moving to the city of his dreams.
New York.
It had seemed like a fairy tale. He couldn’t believe that he, Kurt Hummel, who had a reputation for getting universal shit on, was getting everything he ever wanted. He finally felt like the person he saw when he looked in the mirror – a leading man.
But he’d had so many stars in his eyes clogging up his vision and cluttering up his brain that he forgot – not all fairy tales have happy endings.
His doesn’t … save one.
He looks up at his husband with glistening eyes and a weak smile, and says: “No. No, I’m not ready.” He sniffs, wipes a tear from his eyes. “You know, I’ve seen so many dancers retire during my time here, so many walk through those doors and never come back, and I knew, eventually, I would be one of them. But now that I’m doing it …” He shakes his head, fighting back tears he swore he wouldn’t shed. “It’s too soon.”
“I’m so sorry,” Blaine says. He’s said it a hundred times already, and here he is, still saying it. In fact, I’m sorry is the first thing he ever said to Kurt when they met at Callbacks many, many years ago. Blaine was the bar’s in-house pianist at the time, his part time job while he put himself through school. Kurt was passing him by, heading to the bar for a refill on his Diet Coke, but Blaine thought he was coming up to talk to him.
Hoping, more like, since, from the direction of his eyes and the intensity of his gaze, it was obvious Kurt was going to blow right by him. But Blaine thought now or never, right? He stood up, pushed his bench out a little too far, and before he could say a word of warning, Kurt hit the corner and tripped, head over heels, onto the floor.
(Every time Blaine recounts the story of the way they met, he always jokes that Kurt ‘fell head over heels’ for him. Kurt has yet to find it funny.)
Kurt landed on his palms, leaving them bloody. The corner of the bench tore through his pants and cut his knee. On top of that, he’d spilt the drink he was refilling down the front of his designer silk shirt. It was a disaster all around. Through numerous repetitions of “I’m sorry! I’m so, so sorry!” Blaine offered Kurt a Band-Aid and some antibacterial ointment, but Kurt turned him down. He called Blaine a ‘talentless, classless swine’, and left.
Blaine never thought he’d see him again.
Until the next night, when Kurt returned with a single red rose, looked deep into his eyes, and said, “It’s my turn to say I’m sorry.”
Blaine wants to stop saying sorry and offer his husband more in the way of comfort and wisdom, but he doesn’t know what else to say. He can’t fix this, can’t change it. A Band-Aid and a tube of Neosporin won’t make this wound go away.
“Becoming a ballet dancer … it was a way to cope, a way to overcome. I knew I could do it, but I was also so used to be being pushed down despite my talent that I never thought it would actually happen. I didn’t think it would become my life, that I would be lucky enough. Becoming Principal Dancer so quickly … it was a dream come true.”
“And you deserved it.” Blaine gets down on one knee in front of his husband. “Every minute of it.”
Kurt nods. He’s not being condescending. He worked hard for it, for everything he has. He did deserve it.
He doesn’t deserve this.
“You know, they say a dancer dies twice.” Kurt sniffs again. Blaine reaches into his pocket, pulls out a handkerchief, and passes it to his husband. “That used to terrify me.”
“How does it feel now?”
Kurt chuckles hollowly, patting his eyes dry. “Painless.”
“But … isn’t painless a good thing?”
“No. Because when I leave here, I don’t want it to be on my own two feet. I want you to wheel me out of here, crippled, unable to stand or walk. But I can stand …” He rises to his feet. “I can walk.” He struts around his husband with regal posture, toes pointed as he follows the ghosts of his own steps around the room. “I can even arabesque.” He considers trying it, but he decides not to, because what if he’s wrong? What if he can’t do it? He’s already lost so much of his technique, watched it slip through his fingers in a frighteningly short amount of time. It would shatter his heart to know how much more he’s losing by the day. “But beyond that, I’m finished. And I’m not ready to be.”
“I know it seems like everything’s over …” Blaine stands. He crosses the floor, and takes his husband’s hands in his “… but this isn’t an ending, Kurt. Your life isn’t done. In many ways, it’s a beginning. Think of all the traveling we can do now! The long vacations we can take! Don’t think of this as retirement. Think of it as re-birth.”
“That does sound nice,” Kurt says, though the tone of his voice tells Blaine that’s he’s humoring him. “But I’ve never exactly been an R&R type of guy. I think I’d go crazy after a while. I need to be on stage. I need to perform.”
“So, perform,” Blaine suggests, grasping for something that might make Kurt feel better, that will bring the smile back to his face – the one he lost in this room the day he fell to the floor. “Maybe your spotlight here has dimmed, but there’s always one somewhere. You used to talk about being on Broadway. We … we can start there! We’ll get you a vocal coach, whip your voice back in shape. I graduated from NYADA, Kurt! One of the premiere performing arts schools in the country! I’m sure with your resume and my recommendation, you’d have professors bending over backward to get you back on the stage.” Blaine pulls his husband to him, rests his forehead against his, desperate to make his heart whole again as quickly as possible. “You can do anything you set your mind to, Kurt! Anything!”
“Do you believe that?” Kurt whispers.
“I do, Kurt! I always have!”
A tear slides down Kurt’s cheek, but he chuckles all the same. It’s that same hollow laugh from before, but this time, more deeply gutted.
“Then you’re lying to yourself, love.”
Blaine jerks back a little, in hurt and disbelief. “How do you figure?”
“Because what I want to do is dance, Blaine. I want to spin, and leap, and soar. It’s all I want to do. And I never will again.”
49 notes
·
View notes
Text
Broken ankle or broken wrist// I don’t have any fun commentary for this one
Bruised ribs or a concussion// as someone who’s hurt their ribs before, it hurts like fuckin hell
CPR or the heimlich// BROKEN RIBS
falling off a cliff or almost drowning// this happened in a otome game I was playing and now I love it
shot or stabbed// shrugs
broken nose or broken fingers// there’s something abt characters with blood running down their face that I just vibe with yknow
physical pain or emotional// 👌
sickness or injuries//
romantic caretakers or platonic// f o u n d f a m i l y
appendicitis or pneumonia// I've read some good fics man
car accident or building collapse// aaAAA making me choose is cruel,,,, I’m falling back on how much I like the whump and emotional pain that follows
sprained ankle from hiking or tortured by a whumper// depends on the character
collapsing from exhaustion or collapsing from diabetes//
heart problems or Ruptured spleen // I don’t actually really like either of these fhdkfkfj, but in a game I played somewhat recently there was a character with heart problems and it was angsty and wonderful
broken collarbone or broken knee//
crutches or sling//
wheelchair or cane//
tonsillectomy or appendectomy// both are good for found family uwu
broken bones or dislocated limbs // honestly I don’t even have a reason
This or That (Whump edition)
I like doing those This or That games where you tag people, so I made this one up. Bold the ones that you prefer. I’ll go first!
Broken ankle or broken wrist// Bruised ribs or a concussion// CPR or the heimlich// falling off a cliff or almost drowning// shot or stabbed// broken nose or broken fingers// physical pain or emotional// sickness or injuries// romantic caretakers or platonic// appendicitis or pneumonia// car accident or building collapse// sprained ankle from hiking or tortured by a whumper// collapsing from exhaustion or collapsing from diabetes// heart problems or Ruptured spleen // broken collarbone or broken knee// crutches or sling// wheelchair or cane// tonsillectomy or appendectomy// broken bones or dislocated limbs
Even if I don’t tag you, go ahead and do it if you want to! Just as a reminder, please reblog this when you do it rather than make your own post so that I can see all your answers.Thanks!
I tag: @mypoorfaves @poor-sickies @bigwhumpus @whumpitgood @dontyoubleedoutonme @thoughtsonhurtandcomfort
411 notes
·
View notes
Text
A timeline of Tua Tagovailoa’s injury history

Photo by Wesley Hitt/Getty Images
Before getting drafted by Miami at No. 5 overall, Tua Tagovailoa was sidelined with various injuries at Alabama.
Tua Tagovailoa was drafted by the Miami Dolphins with the No. 5 overall pick in the first in round of the 2020 NFL Draft. The former Alabama quarterback had a historic run with the Tide. Over his three seasons, he set school records for career touchdown passes (87) and single-season passing yards (3,966). He also came off the bench to lead Alabama to a national championship as a freshman, followed by another title game appearance as a sophomore.
For most of his career, he was considered to be the top quarterback prospect whenever he decided to enter the NFL.
However, there have been concerns the QB’s health since he declared for the draft after his junior season. Most recently, and most importantly, Tagovailoa suffered a season-ending hip injury in 2019, but he’s been banged up quite a bit throughout his college career. Let’s run through a complete timeline of all his injury setbacks:
March 20, 2018: Tagovailoa breaks finger in spring practice
In Alabama’s first spring practice of 2018, Tagovailoa suffered an injury to his left throwing hand. According to AL.com, the injury occurred after he hit his hand on a lineman’s helmet. Tagovailoa’s father said it was a broken finger and his son underwent surgery.
He was able to return to practice a few days later, but was limited with what he could do.
.@AlabamaFTBL @Tuaamann_ back at #Bama practice two days after injuring thumb. Not much throwing but #Tua was back!@gohawaii @SECNetwork @SEC #RollTide pic.twitter.com/MVOVPDE3TV
— Rick Karle WVTM 13 (@RickKarle) March 22, 2018
In April, Alabama head coach Nick Saban said Tagovailoa had a “setback” with his injured hand. The quarterback missed the Tide’s spring game.
Oct. 6, 2018: Tagovailoa suffers sprained right knee
A few days after Alabama beat Arkansas, Saban told reporters Tagovailoa was dealing with a sprained knee. He sustained the injury in the 65-31 win and wore a knee brace at one point.
During the Missouri game on Oct. 13, the QB tweaked his knee after sliding on a play in the third quarter. Tagovailoa eventually came out of the tent, but with the game already decided, he did not play again.
Tua leaves the tent. pic.twitter.com/yraVHTnAj0
— Michael Casagrande (@ByCasagrande) October 14, 2018
A week later, Tagovailoa was slow to get up after throwing a touchdown in the third quarter against Tennessee:
*checks watch* yep, it's about time for another Alabama touchdown pic.twitter.com/D6kETH4TBJ
— SI College Football (@si_ncaafb) October 20, 2018
The quarterback’s day was over at that point, though Saban said after Bama’s 58-21 win that Tagovailoa could have returned if necessary.
He came up limping after a play against LSU a couple weeks later, but didn’t miss any time from the knee injury in that game or the rest of the season.
Nov. 10, 2018: Tagovailoa leaves game against Mississippi State with quad injury
In the third quarter against the Bulldogs, Tagovailoa left the game after taking a big hit that resulted in an injury to his left quad:
Tua limped off the field and into the injury tent after this hit. pic.twitter.com/KUEp5QUEdv
— Yahoo Sports College Football (@YahooSportsCFB) November 10, 2018
Bama rolled to a 24-0 victory, and Tagovailoa suited up in time the next week.
Dec. 1, 2018: Tagovailoa suffers high ankle sprain during SEC Championship vs. Georgia
Early in the fourth quarter, one of Tagovailoa’s offensive linemen stepped on his right ankle as he was attempting to make a throw:

Tagovailoa exited the game and the next morning he underwent what’s called a “TightRope” surgery to repair his ankle, which typically has a two-week recovery time. The relatively new surgery serves as an “orthopedic zip tie” for the injured ankle. Here’s more from the Southern California Orthopedic Institute:
It can be used to repair a high ankle sprain, which damages the soft tissue structures between the tibia and fibula and causes these bones to separate. It can also be used to stabilize a fracture of the fibula. The TightRope system anchors the ends of the tibia and fibula together with a braided cord, rather than with a rigid surgical screw, to restore the original position of the bones and to allow for proper healing.
Twelve days after he underwent surgery, Tagovailoa was back practicing ahead of Bama’s College Football Playoff semifinal game against Oklahoma:
.@AlabamaFTBL first day of bowl practice and Tua Tagovailoa is running around. @Tuaamann has been telling us all along he's taking advantage of every second possible to rehab from his ankle surgery- Video shot by CBS 42's @RonGSports pic.twitter.com/O90kxnJwLH
— Chris Breece (@ChrisBreece) December 14, 2018
Even though he told reporters his ankle was only about 85 percent, Tagovailoa went 24-of-27 passing for 318 yards and four touchdowns in Alabama’s win.
Oct. 20, 2019: Tagovailoa suffers high ankle sprain in opposite ankle
Less than a year later, Tagovailoa injured his other ankle when he took a sack against Tennessee just about midway through the second quarter.

He headed to the locker room and didn’t return to the game. The next day, he had a “TightRope” procedure to repair it — the same surgery he had the season prior. He missed Alabama’s game against Arkansas the next week. Since the Tide had a bye the week after that, Tagovailoa was back in time for Alabama’s Nov. 9 game against LSU.
Nov. 16, 2019: Tagovailoa dislocates right hip against Mississippi State
Just a week after making his return against LSU, Tagovailoa’s season was cut short due to a gruesome hip injury he suffered after being dragged down by a pair of Bulldogs tacklers. Visibly emotional and upset, Tagovailoa was carted off the field:
youtube
Tagovailoa underwent surgery on his right hip on Nov. 18 and did not play for Alabama again.
Jan. 6, 2020: Tagovailoa declares for the NFL Draft
The news wasn’t too much of a surprise, but he still had a year of eligibility left if he wanted to return.
Feb. 23-March 2, 2020: Tagovailoa attends the NFL Combine, but doesn’t participate in drills
The QB hadn’t been cleared for full drills just yet, but he still went through interviews and met with various teams.
“Mentally, it’s been a grind,” Tagovailoa said of his rehab process. “But it’s not something that’s new to me. I’ve dealt with my hand injury, my left ankle and my right ankle. I sort of know what to expect going through this process. But it’s definitely been a grind.”
Although he didn’t throw at the combine, he had plans to throw at Alabama’s pro day in March.
March 23, 2020: Tagovailoa posts video of his footwork after pro day cancellation
Bama’s pro day was initially supposed to take place on March 24, but it was cancelled weeks due to the Covid-19 virus. Tagovailoa was still able to show off what he could do, though:
Practicing social distancing with the long ball today. Feels good to spin it again. #Process pic.twitter.com/BZnBF7Sfdc
— Tua. T (@Tuaamann) March 24, 2020
March 31, 2020: Tagovailoa gets fully cleared by doctor to perform football-related activities
This news meant Tagovailoa could start training with any team that selected him, without restrictions.
“I am extremely pleased,” Dr. Lyle Cain said via Yahoo Sports. “If you told me four, almost five, months ago now that he’d be where he is now, I think I would have been very happy. I think he’s done extremely well for where he started out.”
April 10, 2020: Tagovailoa performs virtual pro day
Tagovailoa sent video of his virtual pro day to teams, and he also explained on Instagram Live why teams shouldn’t worry about his durability.
“I’m not playing badminton. I’m not on the swim team,” Tagovailoa told Mike Locksley, his former offensive coordinator, as transcribed by ESPN. “[Football] is a physical sport. You’re gonna get hurt. That just comes with it. And it was just very unfortunate that I got hurt every season.
“It’s a part of the game. It’s a contact sport. I can only control what I can control. I can’t control that.”
April 23, 2020: Tagovailoa drafted by the Dolphins
Tua will join quarterbacks Josh Rosen and Ryan Fitzpatrick in Miami, but he will be the likely starter from the three. We’ll see what his NFL career holds with the Dolphins, and more importantly, if he can stay healthy.
0 notes
Text
Sacroiliac Joint Sprain and Dysfunction
There are two Sacroiliac (SI) joints. They connect both sides of the sacrum to the iliac part of the pelvic bones, forming the ring of the pelvis. The sacrum is usually formed by five vertebrae fused together (though it can be four or six). The SI joints are big and very strong and are synovial (fluid filled) joints. They are held together by thick and strong ligaments. They are subjected to a small rocking movement in opposite directions to each other when walking. They are subjected to twisting forces when the spine twists. They are under compressive forces when standing or walking, and extreme forces when landing after a jump. The SI joints are ‘shock absorbers’, and transfer forces from the axial skeleton to the legs, and from the legs to the axial skeleton. In women, a large movement of the SI joints are needed to facilitate childbirth. No single muscle crosses the joints and moves the joints as a ‘prime mover’; instead, the joints are moved as a result of complex musculoskeletal movements such as walking.
What is Sacroiliac Joint Pain?
Sacroiliac pain is often described as pain that is focused in the lower portion of the back and the buttocks. It may radiate out to one hip. In some cases it may travel around to the front on one side, in the groin area. Some males may feel pain in the testicles as well. Pain may radiate down the back of one leg, to either the knee or the ankle, but will rarely be felt in the foot. The pain may be similar to sciatica. The pain may increase by walking or weight bearing on the affected side. Sneezing, coughing, rolling over in bed and bending may increase the pain. Stiffness in the lower back may be experienced as well. The sacroiliac joint can become strained and inflamed, with or without a subluxation (this is a partial dislocation). The bones are slightly displaced, which stretches the ligaments that hold it together and causes them to become inflamed. Subluxation of an SI joint may be caused by bending and lifting to one side, or landing heavily on one leg. Pain can come from the joint surfaces or from the synovial membrane or fibrous capsule of the joint or from the ligaments that hold the joint together. These are rich in nerve endings, and therefore any inflammation or injury to this area results in pain. A subluxed SI joint may give the appearance of a short or long leg on that side, depending on the direction that the SI joint is subluxed. The resultant tilt of the base of the sacrum them puts a twist and side-bending into the lower lumbar spine, and can cause dysfunction and symptoms in this region and sometimes above. A feeling that the leg, or hip, is rotated may accompany this condition, and the toes of one foot may turn out more than the other. One hip bone may appear higher than the other, and there may be asymmetry in the waist.
SI joint sprain may be accompanied by piriformis syndrome, though piriformis syndrome may occur without a SI sprain and be misdiagnosed as a SI sprain. Pain may radiate into one leg, either because there is pressure on some of the nerves to that leg, as some of them passes through the piriformis muscle (which crosses the SI joints); or because of a stretch of the hamstring or adductor muscles due to a shift of their origins caused by the ischial and pubic bones having moved by a subluxation of the SI joint. The hormones of pregnancy soften the sacroiliac ligaments to allow extra movement of the sacrum, to enable the baby to pass through the pelvis at childbirth. Unfortunately this also means that pregnant women are more susceptible to sacroiliac joint strains. Also it is possible for one or both joints to become subluxed and ‘jammed’, which can lead to an obstructed delivery and an emergency caesarean if it is not corrected. Fortunately strained sacroiliac joints in pregnancy are easily treated, though it is important to see an osteopath who specializes in pregnancy, as not all osteopathic colleges train their students in the most suitable techniques. Unfortunately many pregnant women with sacroiliac joint strains are told that it is ‘normal’ and they have to live with it. Sacroiliac Joint Pain may be the result of inflammatory disease processes such as ankylosing spondylitis, which can eventually lead to fusion of the SI joints. Fractures can be caused by acute trauma, such as a car accident, causing severe pain.
Conventional treatments include injections and surgery. Manipulation is best from an osteopath, who will make a complete bio-mechanical analysis of the joints and muscles of the spine and pelvic girdle; and treat where appropriate using both manipulation of the relevant joints and soft tissue work on the muscles.Osteopaths have always believed the sacroiliac joints move and can become strained, and have always treated sacroiliac joint strains and dysfunction. Until recently, medical doctors and physiotherapists didn’t believe that sacroiliac joints could move, let alone become strained. This is because of the teachings of a famous British orthopaedic surgeon called James Cyriax, who died in 1985 at the age of 80. He always maintained that SI joints couldn’t move or become strained, and that osteopaths were fraudulent for claiming that they could, which delayed the recognition of osteopaths. He taught crude and rough manipulation techniques to doctors and physiotherapists, ignoring underlying causes. Since his passing, it has become widely accepted that sacroiliac joints can move and become strained, and osteopaths are now widely recognized and regulated by statute. Unfortunately his methods are still widely practiced by doctors and physiotherapists.
Exercises
If you are looking to do exercises for sacroiliac joint pain then your first focus should be to stabilize the pelvis including the sacrum in proper alignment. DO NOT do SI joint exercises in poor pelvic alignment, you will only stabilize the faulty alignment and cause more problems! See your osteopath first!
1) Learn neutral spine:Neutral Spine is the healthiest and most stable position for the spine and pelvis taking in to account the natural curvature of the spine.
Standing: Back up against a wall with your buttocks and shoulder blades leaning into the wall. Notice whether your lower back is against the wall or if there is an excessive arch there. The latter is more common.To achieve neutral keep the buttocks and shoulders against the wall and then draw the middle part of your back into the wall. You should feel the abdominal muscles engage and/or the ribs drawing in.
Lying: Lying on a mat with your knees bent and feet hip width apart, arms at your side. Begin by releasing your tailbone down creating an arc in the lower back, move up into the mid back and draw it down without flattening the spine. The shoulder blades are down and heavy and the back of the neck is long, do this by drawing your chin down towards your chest leaving the size of a fist space there.
Sitting: When sitting in a chair press your bottom right up against the back of the chair then stack the rest of the spine over it. Your collarbone is over your hip bones and your breastbone is right above the pubic bone. Navel drawn in gently.Proper posture is the best way to reduce tension from sitting at work all day, on computers, driving, etc.
2) Pelvic Stabilization Exercises for Sacroiliac Joint Pain:
Wall squats Position: Standing in neutral against the wall with your feet the length of your thighs away from the wall.Action: Bend your knees no lower than a 90 degree angle keeping your weight in the heels evenly for both feet. Kneecaps should line up with the second toe in each foot. Repeat for 8-12 repetitions. Do 2-3 sets every other day. Cues: Place hands on hip bones and make sure they stay level as you bend and lift, also keep the buttocks, shoulder blades, and mid part of the back against the wall throughout the exercise.
Pelvic clocks Position: Lying on the floor with neutral spine and knees bent.Action: Imagine your pelvis as a clock. 12 o'clock is at your navel, 6 is at your pubic or tailbone, 3 and 9 are the hip bones. Now imagine there is water in that clock or bowl and you are going to empty from 12 o'clock around clockwise and then counterclockwise feeling each number on the clock working. Cues: Keep the knees still you are just mobilizing the pelvis.
Diaphragmatic Breathing Position: Lying in neutral spine. Action: Without changing the position of your spine inhale deeply through the nose filling up or expanding into the ribs and upper back, then exhale through your mouth expelling the air again without changing the spine. On the exhale feel all the air leave your body feeling the muscles tighten around the waist as your abdomen flattens.
3) Strengthening Exercises for Sacroiliac Joint Pain: Once you have a stable and aligned pelvis you can begin mobilizing exercises to continue strengthening.
Leg Circles. Position: Lying on the floor with one leg extended along the mat and the other at a 90 degree angle to the floor and a neutral spine.Action: Keeping the pelvis still circle the thigh (leg) in the hip socket 6 times each direction. Switch legs. Cues: Focus on keeping the torso and leg on the mat very still as you freely circle the leg in the air.
Bridges. Position: Lying in neutral with knees bent arms at your side.Action: Inhale to prepare and exhale as you press into your heels lifting the pelvis up in neutral until weight is between shoulder blades not in the neck. Inhale hold then exhale to bring the tailbone and ribs down all at one time. Cues: Focus on the navel drawn in to lift the pubic bone up to the ceiling. Weight even in the feet. Rotation and side bending exercises can be added as you are symptom free in neutral spine.
4) Stretching Exercises for Sacroiliac Joint Dysfunction.
The main objective of exercises for sciatic pain from sacroiliac joint dysfunction is to restore the range of motion in this joint which can be limited if the joint is inflamed. Performing range of motion exercises directed at the SI joint can often restore normal movement and alleviate the irritation of the sciatic nerve. Three helpful exercises are:
Single knee to chest stretch. Pull one knee up to the chest at a time, gently pumping the knee three to four times at the top of the range of motion. Do 10 repetitions for each leg.
Press-up. From the prone position, press up on the hands while the pelvis remains in contact with the floor. Keep the lower back and buttocks relaxed for a gentle stretch. Hold the press- up position initially for five seconds, and gradually work up to 30 seconds per repetition. Aim to complete 10 repetitions.
Lumbar rotation—non-weight bearing. Starting by lying on the back with both knees bent, keep the feet flat on the floor while rocking the knees from side to side. The thighs should rub together and the knees will not move very far. The lower spine should remain fairly still. Rock the knees for 30 seconds.
0 notes