#nonsteroidal treatment
Text
FDA Approval of Nonsteroidal Treatment for Duchenne Muscular Dystrophy
Breaking news in the medical world! The U.S. Food and Drug Administration has just approved Duvyzat (givinostat), an oral medication for the treatment of Duchenne Muscular Dystrophy (DMD) in patients six years of age and older. Duvyzat is making history as the first nonsteroidal drug approved to treat patients with all genetic variants of DMD. This is a significant milestone in the treatment of…

View On WordPress
0 notes
Text
On the one hand, I'm sad because I've been dealing with another one of my icky rashes for nearly three weeks now.
On the other hand? I think I really like my new PCP. I think she's actually doing better at treating my allergies than my allergist. She considers it a priority to get things controlled to the point that they aren't impairing my quality of life, while he seems to think that if my breathing numbers are OK, things must be good enough.
Two days ago she started me on a new ointment, one of those nonsteroidal immune suppressants, and I have to say, I've never seen an ointment work like this. Steroid ointments and high dose antihistamines sometimes work on a rash in the first few hours, but if they don't, or I miss that treatment window, I'm just fucked. And of course, I never know when I'm going to develop an allergy TO the treatment, even if I've used it for years.
This is actually taking the swelling out of spots that have been there for days. I had no idea a treatment that could do such a thing existed.
She also started me on another asthma treatment in the spring, which helped a lot. And she's talking about the possibility of an injected biologic. There'd be a lot of paperwork and phone calls and drama, but it might be possible.
11 notes
·
View notes
Text
Rheumatoid Arthritis:
Refer to rheumatologist.
●Nonpharmacologic measures – Nonpharmacologic measures, such as patient education, psychosocial interventions, and physical and occupational therapy, should be used in addition to drug therapy. Other medical interventions that are important in the comprehensive management of RA in all stages of disease include cardiovascular risk reduction and immunizations to decrease the risk of complications of drug therapies.
●Initiation of DMARD therapy soon after RA diagnosis – We suggest that all patients diagnosed with RA be started on disease-modifying antirheumatic drug (DMARD) therapy as soon as possible following diagnosis, rather than using antiinflammatory drugs alone, such as nonsteroidal antiinflammatory drugs (NSAIDs) and glucocorticoids (Grade 2C). Better outcomes are achieved by early compared with delayed intervention with DMARDs.
●Tight control of disease activity – Tight control treatment strategies to "treat to target" are associated with improved radiographic and functional outcomes compared with less aggressive approaches. Such strategies involve reassessment of disease activity on a regularly planned basis with the use of quantitative composite measures and adjustment of treatment regimens to quickly achieve and maintain control of disease activity if targeted treatment goals (remission or low disease activity) have not been achieved. (
●Pretreatment evaluation – Laboratory testing prior to therapy should include a complete blood count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), aminotransferases, blood urea nitrogen, and creatinine. Patients receiving hydroxychloroquine (HCQ) should have a baseline ophthalmologic examination, and most patients who will receive a biologic agent or Janus kinase (JAK) inhibitor should be tested for latent tuberculosis (TB) infection. Screening for hepatitis B and C should be performed in all patients. Some patients may require antiviral treatment prior to initiating DMARD or immunosuppressive therapy, depending upon their level of risk for hepatitis B virus (HBV) reactivation.
●Adjunctive use of antiinflammatory agents – We use antiinflammatory drugs, including NSAIDs and glucocorticoids, as bridging therapies to rapidly achieve control of inflammation until DMARDs are sufficiently effective. Some patients may benefit from longer-term therapy with low doses of glucocorticoids.
●Drug therapy for flares – RA has natural exacerbations (also known as flares) and reductions of continuing disease activity. The severity of the flare and background drug therapy influence the choice of therapies. Patients who require multiple treatment courses with glucocorticoids for recurrent disease flares and whose medication doses have been increased to the maximally tolerated or acceptable level should be treated as patients with sustained disease activity. Such patients require modifications of their baseline drug therapies.
●Monitoring – The monitoring that we perform on a regular basis includes testing that is specific to evaluation of the safety of the drugs being; periodic assessments of disease activity with composite measures; monitoring for extraarticular manifestations of RA, other disease complications, and joint injury; and functional assessment.
●Other factors affecting target and choice of therapy – Other factors in RA management that may influence the target or choice of therapy include the disabilities or functional limitations important to a given patient, progressive joint injury, comorbidities, and the presence of adverse prognostic factors.
Osteoarthritis
General principles – General principles of osteoarthritis (OA) management include providing continuous care that is tailored to the patient according to individual needs, goals, and values and should be patient-centered. Treatment can be optimized by OA and self-management education, establishing treatment goals, and periodic monitoring.
●Monitoring and assessment – The management of OA should include a holistic assessment which considers the global needs of the patient. Patient preferences for certain types of therapies should also be assessed, as compliance and outcomes can be compromised if the care plan does not meet the patient's preferences and beliefs.
●Overview of management – The goals of OA management are to minimize pain, optimize function, and beneficially modify the process of joint damage. The primary aim of clinicians should include targeting modifiable risk factors. Due to the modest effects of the individual treatment options, a combination of therapeutic approaches is commonly used in practice and should prioritize therapies that are safer.
●Nonpharmacologic therapy – Nonpharmacologic interventions are the mainstay of OA management and should be tried first, followed by or in concert with medications to relieve pain when necessary. Nonpharmacologic therapies including weight management and exercises, braces and foot orthoses for patients suitable to these interventions, education, and use of assistive devices when required.
●Pharmacologic therapy – The main medications used in the pharmacologic management of OA include oral and topical nonsteroidal antiinflammatory drugs (NSAIDs). Other options include topical capsaicin, duloxetine, and intraarticular glucocorticoids. Our general approach to pharmacotherapy is described below.
•In patients with one or a few joints affected, especially knee and/or hand OA, we initiate pharmacotherapy with topical NSAIDs due to their similar efficacy compared with oral NSAIDs and their better safety profile.
•We use oral NSAIDs in patients with inadequate symptom relief with topical NSAIDs, patients with symptomatic OA in multiple joints, and/or patients with hip OA. We use the lowest dose required to control the patient's symptoms on an as-needed basis.
•We use duloxetine for patients with OA in multiple joints and concomitant comorbidities that may contraindicate oral NSAIDs and for patients with knee OA who have not responded satisfactorily to other interventions.
•Topical capsaicin is an option when one or a few joints are involved and other interventions are ineffective or contraindicated; however, its use may be limited by common local side effects.
•We do not routinely use intraarticular glucocorticoid injections due to the short duration of its effects (ie, approximately four weeks).
•We avoid prescribing opioids due to their overall small effects on pain over placebo and potential side effects (eg, nausea, dizziness, drowsiness), especially for long-term use and in the older adult population.
•We do not routinely recommend nutritional supplements such as glucosamine, chondroitin, vitamin D, diacerein, avocado soybean unsaponifiables (ASU), and fish oil due to a lack of clear evidence demonstrating a clinically important benefit from these supplements. Other nutritional supplements of interest that may have small effects on symptoms include curcumin (active ingredient of turmeric) and/or Boswellia serrata, but the data are limited.
●Role of surgery – Surgical treatment is dominated by total joint replacement, which is highly effective in patients with advanced knee and hip OA when conservative therapies have failed to provide adequate pain relief.
●Factors affecting response to therapy – The discordance of radiographic findings to pain supports the notion that the mechanisms of pain are complex and likely multifactorial. The placebo effect is also known to impact response to therapy.
●Prognosis – Although there is great variability among individuals and among different phenotypes of OA, courses of pain and physical functioning have been found to be predominantly stable, without substantial improvement or deterioration of symptoms over time.
4 notes
·
View notes
Text
Can inflammation cause depression?
There’s evidence to suggest that inflammation can contribute to the development of depression in many people, particularly among individuals with preexisting inflammatory conditions or chronic illnesses.
For instance, research suggests that the link between inflammation and depression is commonly seen in conditions like autoimmune diseases (e.g., multiple sclerosis) and infections (e.g., sepsis) where the immune system plays a significant role.
How does inflammation affect your mental health?
When your immune system is activated, it affects not only the body but also the central nervous system, which includes the brain. Chronic inflammation is linked to changes in the brain’s chemistry and structure, which can increase the risk of depression.
Inflammation can impact mental health in several ways:
Neurotransmitter imbalance: ResearchTrusted Source suggests that inflammation may disrupt brain chemicals (neurotransmitters) like serotonin and dopamine, leading to mood imbalances.
Hormonal disruption: Inflammation can affect stress and sex hormone levels (e.g., cortisol, estrogen), impacting mood and cognition.
Neuroinflammation: EvidenceTrusted Source suggests that inflammation within the brain itself can cause cognitive and mood problems.
Reduced neuroplasticity: Chronic inflammation may hinder the brain’s ability to adapt and learn.
Oxidative stress: Inflammation may increase oxidative stress, damaging brain cells.
In many adults, depression and inflammation appear to be separate issues. One studyTrusted Source found that clinical depression in older individuals isn’t typically linked to increased inflammation unless they have preexisting inflammatory conditions like arthritis.
How do you know if your depression is caused by inflammation?
Determining if your depression is caused by inflammation typically involves specialized medical tests and assessments. This may involve blood tests to measure inflammatory markers or discussions with your doctor about your medical history and symptoms.
However, here are some signs that suggest inflammation may be contributing to your depression:
You have other inflammatory conditions (e.g., autoimmune disorders, chronic infections, or inflammatory bowel disease).
Your depression had a sudden onset (especially in response to an infection or injury).
Your depression doesn’t respond to antidepressants.
You have physical symptoms (e.g., fatigue, joint pain, or fever)
You have high stress levels (chronic stress can trigger inflammation).
You have a family history of both depression and inflammatory conditions.
You have elevated markers of inflammation, like CRP or cytokines, in specialized blood tests.
Treatment options for inflammation-related depression
Treatment options for inflammation-related depression typically aim to target both the underlying inflammation and the depressive symptoms. Here are some common approaches:
Anti-inflammatory medications: Some evidenceTrusted Source suggests that nonsteroidal anti-inflammatory drugs (NSAIDs) or anti-inflammatory agents like corticosteroids may be prescribed to reduce inflammation.
Healthy diet: A comprehensive reviewTrusted Source of 41 studies revealed that maintaining a consistently healthy diet, especially one in line with the traditional Mediterranean diet, or simply avoiding diets that promote inflammation, may protect against depression.
Psychotherapy: Cognitive-behavioral therapy (CBT) and mindfulness-based therapies may help manage depression symptoms.
Medications: Some evidenceTrusted Source suggests that certain antidepressants, like selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), can reduce inflammation in the brain, which may contribute to their effectiveness.
Light therapy: A 2017 study found that combining bright light therapy with antidepressants for nonseasonal depression could be effective. Participants also showed significant changes in immune-related lymphocyte counts.
Omega-3 fatty acids: Omega-3 supplements, found in fish oil, have anti-inflammatory properties and may help with depression symptoms.
Mind-body practices: Practices like yoga and meditation can help manage stress and potentially reduce inflammation.
Probiotics: Some research suggests that probiotics may have a positive impact on gut health and inflammation, which could indirectly affect mood.
Anti-inflammatory foods:
Here are some of the most anti-inflammatory foods on the planet, backed by research:
Fatty Fish: Fatty fish like salmon, tuna, mackerel, and sardines are rich in omega-3 fatty acids, which have potent anti-inflammatory effects.
Turmeric: Curcumin, a compound found in turmeric, has been shown to reduce inflammation and oxidative stress in the body.
Ginger: Ginger has anti-inflammatory compounds like gingerol and shogaol, which have been shown to reduce inflammation and pain.
Berries: Berries such as blueberries, raspberries, strawberries, and pomegranates are rich in antioxidants and polyphenols, which have anti-inflammatory effects.
Green Tea: Green tea contains epigallocatechin gallate (EGCG), which has been shown to reduce inflammation and improve symptoms of arthritis.
Dark Chocolate: Dark chocolate contains flavonoids, which have anti-inflammatory and antioxidant properties.
Olive Oil: Olive oil is rich in oleocanthal, a compound that has been shown to reduce inflammation and oxidative stress.
Cruciferous Vegetables: Vegetables like broccoli, cauliflower, and kale contain sulforaphane, which has anti-inflammatory and antioxidant properties.
Fatty Nuts and Seeds: Nuts and seeds like walnuts, chia seeds, and flaxseeds are rich in omega-3 fatty acids and antioxidants.
Leafy Greens: Leafy greens like spinach, kale, and collard greens are rich in antioxidants and polyphenols, which have anti-inflammatory effects.
Garlic: Garlic contains compounds like allicin, which have been shown to reduce inflammation and improve cardiovascular health.
Apples: Apples contain quercetin, a flavonoid that has anti-inflammatory properties.
Pineapple: Pineapple contains an enzyme called bromelain, which has anti-inflammatory properties.
Sweet Potatoes: Sweet potatoes are rich in beta-carotene, an antioxidant that has anti-inflammatory effects.
Mushrooms: Certain mushrooms like reishi, chaga, and cordyceps have been shown to have anti-inflammatory properties.

+ anti-inflammatory oils >here<
+ If you are into extracts or diet supplements, you can find products similar to >this<.
#depression#inflammation#mental health#health#mental illness#chronic illness#inspiration#consciousness#self care#self help#diet#food#food supplements#anti inflammatory#anxiety#ptsd#nervous system#immune system#autoimmune disease#autoimmune disorder
3 notes
·
View notes
Text
🌟 Essential Tips and Techniques to Alleviate Joint Pain 🌿
Joint pain can significantly impact daily life, making even simple tasks challenging and uncomfortable. Whether caused by arthritis, injury, or other factors, managing joint pain is crucial for maintaining quality of life and mobility.
This article explores various strategies, from lifestyle adjustments to therapeutic techniques, aimed at alleviating joint pain effectively.

Understanding Joint Pain
Joint pain can arise from various conditions, including:
Osteoarthritis: Degenerative joint disease due to wear and tear.
Rheumatoid arthritis: An autoimmune disorder affecting joints.
Injury: Sprains, strains, or fractures impacting joint function.
Other conditions: Such as gout, lupus, or fibromyalgia.
Each condition may require specific management approaches, but many general strategies can help mitigate joint pain and improve joint health overall.
Lifestyle Modifications
1. Maintain a Healthy Weight:
Excess weight puts additional stress on joints, particularly weight-bearing ones like knees and hips.
Aim for a balanced diet rich in fruits, vegetables, lean proteins, and whole grains.
2. Regular Exercise:
Low-impact exercises like swimming, biking, or walking can strengthen muscles around joints and improve flexibility.
Avoid high-impact activities that may exacerbate joint pain.
3. Joint-Friendly Activities:
Yoga and tai chi improve flexibility and reduce stiffness.
Physical therapy can provide tailored exercises to strengthen specific joints.
4. Proper Posture and Body Mechanics 💪🏻:
Maintain good posture to reduce stress on joints, especially the spine and neck.
Lift heavy objects properly using your legs and avoiding twisting motions.
5. Ergonomic Adjustments:
Use ergonomic chairs and desks to support joints during work.
Adjust your environment to minimize repetitive movements that strain joints.
Dietary Considerations
1. Omega-3 Fatty Acids:
Found in fish like salmon and mackerel, these can help reduce inflammation.
Consider supplements if dietary intake is insufficient.
2. Antioxidants:
Vitamins C and E, found in fruits and vegetables, may protect joints from oxidative stress.
Berries, spinach, and nuts are rich sources.
3. Spices and Herbs 🌿:
Turmeric and ginger have anti-inflammatory properties.
Incorporate these into cooking or take as supplements.
4. Hydration:
Drink plenty of water to maintain joint lubrication and overall hydration.
Limit sugary drinks and alcohol, which can exacerbate inflammation.
Pain Management Strategies
1. Over-the-Counter Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can reduce pain and inflammation.
Acetaminophen is an alternative for pain relief.
2. Topical Treatments:
Creams and gels containing capsaicin or menthol can provide localized pain relief.
Consider patches for convenience and prolonged relief.
3. Hot and Cold Therapy:
Heat packs or warm baths can relax muscles and improve circulation.
Cold packs or ice packs reduce inflammation and numb pain.
4. Acupuncture and Massage:
Acupuncture may help alleviate pain by stimulating specific points.
Massage therapy can reduce muscle tension and improve joint mobility.
Medical Interventions
1. Prescription Medications:
Disease-modifying antirheumatic drugs (DMARDs) for autoimmune conditions.
Corticosteroid injections for severe inflammation.
2. Joint Support Devices:
Braces, splints, or orthotics can provide stability and reduce joint strain.
Custom orthotics may correct alignment issues contributing to pain.
3. Surgical Options:
Joint replacement surgery by Dr. Siram helps alleviate joint pain by replacing damaged or deteriorated joints with prosthetic implants, restoring mobility and reducing discomfort significantly.
Arthroscopic surgery to repair or remove damaged tissue in the joint.
Psychological and Emotional Support
1. Coping Strategies:
Practice mindfulness or meditation to manage stress and pain perception.
Join support groups to connect with others facing similar challenges.
2. Cognitive Behavioral Therapy (CBT):
Helps develop coping skills and change negative thought patterns related to pain.
May complement medical treatments for better pain management.
Conclusion
Managing joint pain requires a multifaceted approach that combines lifestyle modifications, dietary adjustments, pain management strategies, and sometimes medical interventions.
By incorporating these tips and techniques into daily life, individuals can alleviate pain, improve joint function, and enhance overall quality of life.
Consult with healthcare professionals to develop a personalized plan that addresses specific needs and conditions, ensuring long-term joint health and well-being. 🩺💼
2 notes
·
View notes
Text
Treatment for Psoriatic Arthritis
Psoriatic arthritis is a chronic inflammatory condition that affects individuals with psoriasis, a skin disorder characterized by red, scaly patches. Treatment for psoriatic arthritis aims to alleviate symptoms, reduce inflammation, and prevent joint damage. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen may be prescribed to manage pain and inflammation. Disease-modifying antirheumatic drugs (DMARDs) like methotrexate or sulfasalazine are often used to slow down the progression of joint damage. In cases of more severe disease, biologic medications, such as tumor necrosis factor (TNF) inhibitors like adalimumab or etanercept, may be recommended to target specific components of the immune system responsible for inflammation. Additionally, lifestyle modifications, including regular exercise, a balanced diet, and stress management, can contribute to overall well-being and help manage symptoms of psoriatic arthritis.
2 notes
·
View notes
Text
Medical Abbreviations on Pharmacy Prescriptions
Here are some common medical abbreviations you may see on pharmacy prescriptions:
qd - once a day
bid - twice a day
tid - three times a day
qid - four times a day
qh - every hour
prn - as needed
pc - after meals
ac - before meals
hs - at bedtime
po - by mouth
IV - intravenous
IM - intramuscular
subQ - subcutaneous
mL - milliliter
mg - milligram
g - gram
mcg - microgram
stat - immediately, right away
NPO - nothing by mouth
cap - capsule
tab - tablet
susp - suspension
sol - solution
amp - ampule
inj - injection
Rx - prescription
C - Celsius
F - Fahrenheit
BP - blood pressure
HR - heart rate
RR - respiratory rate
WBC - white blood cell
RBC - red blood cell
Hgb - hemoglobin
Hct - hematocrit
PT - prothrombin time
INR - international normalized ratio
BUN - blood urea nitrogen
Cr - creatinine
Ca - calcium
K - potassium
Na - sodium
Cl - chloride
Mg - magnesium
PO2 - partial pressure of oxygen
PCO2 - partial pressure of carbon dioxide
ABG - arterial blood gas
CBC - complete blood count
BMP - basic metabolic panel
CMP - comprehensive metabolic panel.
ECG - electrocardiogram
EEG - electroencephalogram
MRI - magnetic resonance imaging
CT - computed tomography
PET - positron emission tomography
CXR - chest x-ray
CTX - chemotherapy
NSAID - nonsteroidal anti-inflammatory drug
DMARD - disease-modifying antirheumatic drug
ACE - angiotensin-converting enzyme
ARB - angiotensin receptor blocker
SSRI - selective serotonin reuptake inhibitor
TCA - tricyclic antidepressant
ADHD - attention deficit hyperactivity disorder
COPD - chronic obstructive pulmonary disease
CAD - coronary artery disease
CHF - congestive heart failure
DVT - deep vein thrombosis
GI - gastrointestinal
UTI - urinary tract infection
OTC - over-the-counter
Rx - prescription
OD - right eye
OS - left eye
OU - both eyes.
TID - thrombosis in dementia
TDS - ter die sumendum (three times a day)
BOM - bilaterally otitis media (infection in both ears)
BT - body temperature
C&S - culture and sensitivity
D/C - discontinue or discharge
D/W - dextrose in water
ETOH - ethyl alcohol
FUO - fever of unknown origin
H&P - history and physical examination
I&D - incision and drainage
I&O - intake and output
KVO - keep vein open
N&V - nausea and vomiting
PERRLA - pupils equal, round, reactive to light and accommodation
PR - per rectum
QAM - every morning
QHS - every bedtime
QOD - every other day
S/P - status post (after)
TPN - total parenteral nutrition
UA - urinalysis
URI - upper respiratory infection
UTI - urinary tract infection
VO - verbal order.
XRT - radiation therapy
YOB - year of birth
BRBPR - bright red blood per rectum
CX - cervix
DVT - deep vein thrombosis
GB - gallbladder
GU - genitourinary
HCV - hepatitis C virus
HPI - history of present illness
ICP - intracranial pressure
IVP - intravenous pyelogram
LMP - last menstrual period
MRSA - methicillin-resistant Staphylococcus aureus
MVA - motor vehicle accident
NKA - no known allergies
PEG - percutaneous endoscopic gastrostomy
PRN - pro re nata (as needed)
ROS - review of systems
SOB - shortness of breath
TAH - total abdominal hysterectomy.
TIA - transient ischemic attack
Tx - treatment
UC - ulcerative colitis
URI - upper respiratory infection
VSD - ventricular septal defect
VTE - venous thromboembolism
XR - x-ray
w/c - wheelchair
XRT - radiation therapy
ASD - atrial septal defect
Bx - biopsy
CAD - coronary artery disease
CKD - chronic kidney disease
CPAP - continuous positive airway pressure
DKA - diabetic ketoacidosis
DNR - do not resuscitate
ED - emergency department
ESRD - end-stage renal disease
FFP - fresh frozen plasma
FSH - follicle-stimulating hormone.
GCS - Glasgow Coma Scale
Hct - hematocrit
Hgb - hemoglobin
ICU - intensive care unit
IV - intravenous
JVD - jugular venous distension
K - potassium
L - liter
MCH - mean corpuscular hemoglobin
MI - myocardial infarction
Na - sodium
NGT - nasogastric tube
NPO - nothing by mouth
OR - operating room
PCN - penicillin
PRBC - packed red blood cells
PTT - partial thromboplastin time
RBC - red blood cells
RT - respiratory therapy
SOA - short of air.
SCD - sequential compression device
SIRS - systemic inflammatory response syndrome
STAT - immediately
T - temperature
TPN - total parenteral nutrition
WBC - white blood cells
ABG - arterial blood gas
A fib - atrial fibrillation
BPH - benign prostatic hypertrophy
CBC - complete blood count
CO2 - carbon dioxide
COPD - chronic obstructive pulmonary disease
CPR - cardiopulmonary resuscitation
CT - computed tomography
CXR - chest x-ray
D5W - dextrose 5% in water
Dx - diagnosis
ECG or EKG - electrocardiogram
EEG - electroencephalogram
ETO - early termination of pregnancy.
FHR - fetal heart rate
GSW - gunshot wound
H&P - history and physical exam
HCG - human chorionic gonadotropin
I&D - incision and drainage
IBS - irritable bowel syndrome
ICP - intracranial pressure
IM - intramuscular
INR - international normalized ratio
IOP - intraocular pressure
LFT - liver function test
LOC - level of consciousness
LP - lumbar puncture
NG - nasogastric
OA - osteoarthritis
OCD - obsessive-compulsive disorder
OTC - over-the-counter
P - pulse
PCA - patient-controlled analgesia
PERRLA - pupils equal, round, reactive to light and accommodation.
PFT - pulmonary function test
PICC - peripherally inserted central catheter
PO - by mouth
PRN - as needed
PT - physical therapy
PT - prothrombin time
PTSD - post-traumatic stress disorder
PVC - premature ventricular contraction
QD - once a day
QID - four times a day
RA - rheumatoid arthritis
RICE - rest, ice, compression, elevation
RSI - rapid sequence intubation
RSV - respiratory syncytial virus
SBP - systolic blood pressure
SLE - systemic lupus erythematosus
SSRI - selective serotonin reuptake inhibitor
STAT - immediately
TB - tuberculosis
TIA - transient ischemic attack.
TID - three times a day
TKO - to keep open
TNTC - too numerous to count
TPN - total parenteral nutrition
URI - upper respiratory infection
UTI - urinary tract infection
V-fib - ventricular fibrillation
V-tach - ventricular tachycardia
VA - visual acuity
WNL - within normal limits
AED - automated external defibrillator
ARDS - acute respiratory distress syndrome
BID - twice a day
BP - blood pressure
BUN - blood urea nitrogen
CAD - coronary artery disease
CHF - congestive heart failure
CVA - cerebrovascular accident
D/C - discontinue
DKA - diabetic ketoacidosis.
DM - diabetes mellitus
DVT - deep vein thrombosis
EGD - esophagogastroduodenoscopy
ER - emergency room
F - Fahrenheit
Fx - fracture
GI - gastrointestinal
GTT - glucose tolerance test
HCT - hematocrit
Hgb - hemoglobin
HRT - hormone replacement therapy
ICP - intracranial pressure
IDDM - insulin-dependent diabetes mellitus
IBS - irritable bowel syndrome
IM - intramuscular
IV - intravenous
K - potassium
KVO - keep vein open
L&D - labor and delivery
LASIK - laser-assisted in situ keratomileusis.
ROM - range of motion
RT - radiation therapy
Rx - prescription
SCD - sequential compression device
SOB - shortness of breath
STD - sexually transmitted disease
TENS - transcutaneous electrical nerve stimulation
TIA - transient ischemic attack
TSH - thyroid-stimulating hormone
UA - urinalysis
US - ultrasound
UTI - urinary tract infection
VD - venereal disease
VF - ventricular fibrillation
VT - ventricular tachycardia
WBC - white blood cell
XRT - radiation therapy
XR - x-ray
Zn - zinc
Z-pak - azithromycin (antibiotic).
AAA - abdominal aortic aneurysm
ABG - arterial blood gas
ACS - acute coronary syndrome
ADL - activities of daily living
AED - automated external defibrillator
AIDS - acquired immunodeficiency syndrome
ALS - amyotrophic lateral sclerosis
AMA - against medical advice
AML - acute myeloid leukemia
APAP - acetaminophen
ARDS - acute respiratory distress syndrome
ASCVD - atherosclerotic cardiovascular disease
BPH - benign prostatic hyperplasia
BUN - blood urea nitrogen
CABG - coronary artery bypass graft
CBC - complete blood count
CHF - congestive heart failure
COPD - chronic obstructive pulmonary disease
CPAP - continuous positive airway pressure
CRF - chronic renal failure.
CT - computed tomography
CVA - cerebrovascular accident
D&C - dilation and curettage
DVT - deep vein thrombosis
ECG/EKG - electrocardiogram
EEG - electroencephalogram
ESRD - end-stage renal disease
FSH - follicle-stimulating hormone
GERD - gastroesophageal reflux disease
GFR - glomerular filtration rate
HbA1c - glycated hemoglobin
Hct - hematocrit
HIV - human immunodeficiency virus
HPV - human papillomavirus
HTN - hypertension
IBD - inflammatory bowel disease
IBS - irritable bowel syndrome
ICU - intensive care unit
IDDM - insulin-dependent diabetes mellitus
IM - intramuscular.
IV - intravenous
LFT - liver function test
MI - myocardial infarction
MRI - magnetic resonance imaging
MS - multiple sclerosis
NPO - nothing by mouth
NS - normal saline
OCD - obsessive-compulsive disorder
OSA - obstructive sleep apnea
PCOS - polycystic ovary syndrome
PMS - premenstrual syndrome
PPD - purified protein derivative
PSA - prostate-specific antigen
PT - prothrombin time
PTT - partial thromboplastin time
RA - rheumatoid arthritis
RBC - red blood cell
RSV - respiratory syncytial virus
SLE - systemic lupus erythematosus
TB - tuberculosis.
It is important to remember that medical abbreviations can vary based on location and specialty.
Healthcare professionals should use medical abbreviations with caution and only when they are familiar with their meanings.
Patients should always communicate any questions or concerns they have about their medications or medical care to their healthcare provider or pharmacist to ensure they receive safe and accurate medical care.

9 notes
·
View notes
Text
Physical Therapy Clinic in New York City
Ehlers-Danlos Syndrome (EDS) is a group of rare genetic connective tissue disorders that affect the body's ability to produce collagen, a key protein that provides strength and elasticity to various tissues. People with EDS often experience a range of symptoms, including hypermobility of joints, skin that is easily bruised and hyper-elastic, and various complications related to weak connective tissues.
Pain management for individuals with Ehlers-Danlos Syndrome can be complex and require a multidisciplinary approach involving medical professionals such as rheumatologists, geneticists, pain specialists, physical therapists, and more. Here are some strategies that might be considered:
Medications: Depending on the type and severity of pain, various medications might be prescribed. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help manage joint and muscle pain. For more severe pain, opioid medications might be considered, though their use should be carefully monitored due to the risk of addiction.
Physical Therapy: Physical therapy can be extremely beneficial for individuals with EDS. A physical therapist can provide exercises to improve joint stability, strengthen muscles, and enhance overall body mechanics. Aquatic therapy might be particularly useful due to the buoyancy of water reducing stress on joints.
Bracing and Assistive Devices: Depending on the specific type of EDS and its impact on joints, bracing or assistive devices might be recommended to provide support and reduce strain on joints.
Pain Management Techniques: Techniques such as heat or cold therapy, massage, and acupuncture might provide some relief for certain individuals.
Lifestyle Modifications: Adopting a healthy lifestyle can help manage pain. Maintaining a healthy weight can reduce stress on joints, and staying active within the limits of what your body can handle can also be beneficial.
Counseling and Psychological Support: Chronic pain can have a significant psychological impact. Counseling, mindfulness, and relaxation techniques can help individuals cope with the emotional aspects of managing pain.
Nutrition and Supplements: A balanced diet rich in nutrients that support collagen production, such as vitamin C, might be helpful. Consultation with a medical professional or registered dietitian is recommended before making significant dietary changes or starting supplements.
Pain Management Specialists: Depending on the severity of pain, a pain management specialist might be consulted. They can provide more advanced interventions like nerve blocks, epidural injections, or other specialized treatments.
Genetic Counseling: Since EDS is a genetic disorder, individuals and families might benefit from genetic counseling to better understand the condition, its inheritance pattern, and potential implications for family planning.
It's important to note that each individual's experience with EDS and their pain management needs can vary widely. A personalized approach that takes into account the specific type of EDS, its symptoms, and the person's overall health is crucial. Always consult with qualified medical professionals who are experienced in dealing with Ehlers-Danlos Syndrome for proper guidance and treatment.
Types of EDS
The Ehlers-Danlos syndromes are a group of genetic connective tissue disorders that are currently classified into a system of thirteen types. Despite this grouping and their common name, each type is a distinct condition caused by a different gene mutation. This means that a child cannot inherit a different type of EDS from the one their parent has. It also means that one type cannot later turn into another, and there is no increased risk of having another type just because you have one – they are simply not connected. It is also extremely unlikely that one person would have more than one type, given the rarity of most of these illnesses.
Recently some of the criteria used to diagnose the Ehlers-Danlos syndrome and some of the terminology describing them changed, in order to reflect scientific research from the past twenty years. The 2017 EDS International Classification recognizes thirteen types of EDS and defines for the first time some related conditions, hypermobility spectrum disorders (HSD) which have similar symptoms to hypermobile EDS (hEDS). The term joint hypermobility syndrome (JHS) is no longer used.
The most common type of EDS is thought to be the hypermobile type (formerly known as the hypermobility type or type 3) although the exact prevalence of this condition is not currently known. The medical literature states that it affects 1 in 5,000 people however this statistic is based on research that is out-of-date and hEDS/HSD frequently go undiagnosed or are misdiagnosed as other conditions. HSD and possibly hEDS are likely to be common. The classical and vascular types are rare, with other types being rarer still. It is probable that all the types are underdiagnosed to some degree.
#physical health#physical therapy#ehlers danlos syndrome#ehlers danlos syndrome physical therapy#hypermobile ehlers danlos#ehlers danlos syndrome threatment#physical therapy for ehlers danlos syndro
2 notes
·
View notes
Text
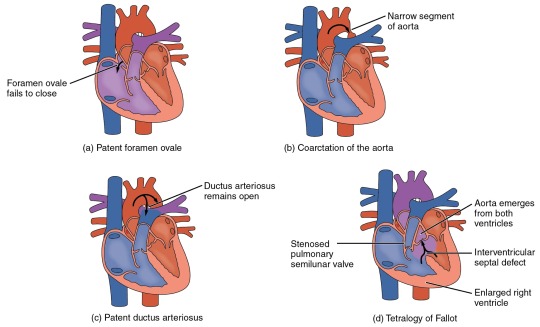
Heart Defects
Heart Defects
One very common form of interatrial septum pathology is patent foramen ovale, which occurs when the septum primum does not close at birth, and the fossa ovalis is unable to fuse. The word patent is from the Latin root patens for “open.” It may be benign or asymptomatic, perhaps never being diagnosed, or in extreme cases, it may require surgical repair to close the opening permanently. As much as 20–25 percent of the general population may have a patent foramen ovale, but fortunately, most have the benign, asymptomatic version. Patent foramen ovale is normally detected by auscultation of a heart murmur (an abnormal heart sound) and confirmed by imaging with an echocardiogram. Despite its prevalence in the general population, the causes of patent ovale are unknown, and there are no known risk factors. In nonlife-threatening cases, it is better to monitor the condition than to risk heart surgery to repair and seal the opening.
Coarctation of the aorta is a congenital abnormal narrowing of the aorta that is normally located at the insertion of the ligamentum arteriosum, the remnant of the fetal shunt called the ductus arteriosus. If severe, this condition drastically restricts blood flow through the primary systemic artery, which is life threatening. In some individuals, the condition may be fairly benign and not detected until later in life. Detectable symptoms in an infant include difficulty breathing, poor appetite, trouble feeding, or failure to thrive. In older individuals, symptoms include dizziness, fainting, shortness of breath, chest pain, fatigue, headache, and nosebleeds. Treatment involves surgery to resect (remove) the affected region or angioplasty to open the abnormally narrow passageway. Studies have shown that the earlier the surgery is performed, the better the chance of survival.
A patent ductus arteriosus is a congenital condition in which the ductus arteriosus fails to close. The condition may range from severe to benign. Failure of the ductus arteriosus to close results in blood flowing from the higher pressure aorta into the lower pressure pulmonary trunk. This additional fluid moving toward the lungs increases pulmonary pressure and makes respiration difficult. Symptoms include shortness of breath (dyspnea), tachycardia, enlarged heart, a widened pulse pressure, and poor weight gain in infants. Treatments include surgical closure (ligation), manual closure using platinum coils or specialized mesh inserted via the femoral artery or vein, or nonsteroidal anti-inflammatory drugs to block the synthesis of prostaglandin E2, which maintains the vessel in an open position. If untreated, the condition can result in congestive heart failure.
Septal defects are not uncommon in individuals and may be congenital or caused by various disease processes. Tetralogy of Fallot is a congenital condition that may also occur from exposure to unknown environmental factors; it occurs when there is an opening in the interventricular septum caused by blockage of the pulmonary trunk, normally at the pulmonary semilunar valve. This allows blood that is relatively low in oxygen from the right ventricle to flow into the left ventricle and mix with the blood that is relatively high in oxygen. Symptoms include a distinct heart murmur, low blood oxygen percent saturation, dyspnea or difficulty in breathing, polycythemia, broadening (clubbing) of the fingers and toes, and in children, difficulty in feeding or failure to grow and develop. It is the most common cause of cyanosis following birth. The term “tetralogy” is derived from the four components of the condition, although only three may be present in an individual patient: pulmonary infundibular stenosis (rigidity of the pulmonary valve), overriding aorta (the aorta is shifted above both ventricles), ventricular septal defect (opening), and right ventricular hypertrophy (enlargement of the right ventricle). Other heart defects may also accompany this condition, which is typically confirmed by echocardiography imaging. Tetralogy of Fallot occurs in approximately 400 out of one million live births. Normal treatment involves extensive surgical repair, including the use of stents to redirect blood flow and replacement of valves and patches to repair the septal defect, but the condition has a relatively high mortality. Survival rates are currently 75 percent during the first year of life; 60 percent by 4 years of age; 30 percent by 10 years; and 5 percent by 40 years.
In the case of severe septal defects, including both tetralogy of Fallot and patent foramen ovale, failure of the heart to develop properly can lead to a condition commonly known as a “blue baby.” Regardless of normal skin pigmentation, individuals with this condition have an insufficient supply of oxygenated blood, which leads to cyanosis, a blue or purple coloration of the skin, especially when active.
Septal defects are commonly first detected through auscultation, listening to the chest using a stethoscope. In this case, instead of hearing normal heart sounds attributed to the flow of blood and closing of heart valves, unusual heart sounds may be detected. This is often followed by medical imaging to confirm or rule out a diagnosis. In many cases, treatment may not be needed.
#atomic heart#science#biology#college#education#school#student#medicine#doctors#health#healthcare#nursing#physiology#pathology
3 notes
·
View notes
Text
Magical Remedy for Breast Cancer in Women - Anastrozole
One of the most frequent cancers in women is breast cancer. Although it can happen at any age, breast cancer is most frequently discovered in adults over the age of 50. Overall, compared to women of all other races or ethnicities, non-Hispanic white women have a somewhat increased risk of acquiring breast cancer. Breast cancer develops when cells in your breast multiply and expand out of control, resulting in a mass of tissue known as a tumor. Breast cancer symptoms might include feeling a lump, noticing a change in breast size, and noticing changes to the skin around your breasts.
Breast cancer is classified into multiple types, such as:
Infiltrating ductal carcinoma
Ductal carcinoma in situ
Infiltrating lobular carcinoma
Lobular carcinoma in situ
Triple-negative breast cancer
Inflammatory breast cancer
Several treatment options are available for breast cancer, including surgery, chemotherapy, radiation therapy, hormone therapy, immunotherapy, and targeted medication therapy. It depends on many factors, such as the tumor's size and the spot, the results of your lab tests, and whether the cancer has spread to other parts of your body.
Some medicines can specifically target the cancer-causing features of certain cell types. If your breast cancer has spread to other parts of your body, your doctor may advise you to take specific medication therapy. The most popular medicines used to treat breast cancer are Anastrozole Tablets.
Anastrozole tablet is used to treat early hormone receptor-positive breast cancer. It contains 1mg dosage. It is used in conjunction with other treatments, such as surgery or radiation, to treat early breast cancer in women who have reached menopause, or the end of their monthly menstrual cycles. Anastrozole 1mg tablet is also used as a first therapy for breast cancer that has spread within the breast or to other regions of the body in women who have gone through menopause.

Anastrozole 1mg tablet belongs to the class of drugs known as nonsteroidal aromatase inhibitors. It functions by reducing the body's production of estrogen. Many forms of breast cancer cells that require estrogen to grow can be slowed or stopped by Anastrozole tablets.
Along with the treatment of Anastrozole might have to undergo some lifestyle changes such as maintaining a healthy weight, exercising, and quitting alcohol. Anastrozole comes as a tablet to take by mouth. It is usually taken once a day with or without food. Take this medication at around the same time every day. You may need to take anastrozole for several years or longer. Continue to take anastrozole even if you feel well. Do not stop taking anastrozole without talking to your doctor.
2 notes
·
View notes
Video
youtube
Using Acupuncture For Natural Joint Pain Relief
Numerous individuals feel pain around their joints because of multiple factors. A fundamental, ongoing condition, like rheumatoid joint pain or osteoarthritis, can cause joint pain. Other likely purposes behind joint pain incorporate wounds and strain from overexertion, which numerous competitors are susceptible to. Regardless, some individuals could feel frustrated with traditional treatment techniques, including a medical procedure, drug, and, surprisingly, customary injections for relief. Fortunately, there is a natural choice for joint pain relief as acupuncture. Peruse more to see if this elective treatment is something you can pursue joint pain relief.
Figuring out Pain
Nearly everybody has encountered joint pain at some point in their lives. For some's purposes, a rare event simply means overuse or overexertion from actual work or physical work. Notwithstanding, many individuals have joint pain daily and have figured out how to adapt to it as a component of their daily lives.
For what reason Would it be advisable for you to Think about Acupuncture?
In many occasions, the most broadly used form of relief for pain is nonsteroidal calming drugs (NSAIDs). For serious pain, a specialist might try and endorse a more grounded drug for relief. Nonetheless, traditional forms of clinical treatment probably won't be just about as compelling as some individuals would like. Those with persistent pain might wish to seek out different choices for pain relief. Another explanation individuals could seek out acupuncture for pain relief is because of the intricacies and results of traditional clinical treatment, which you might see with calming meds and steroid injections.
How Does Acupuncture Function For Joint Pain?
Acupuncture is a customary piece of traditional Chinese medication that has existed for a long time. Acupuncture treatment includes an authorized acupuncture practitioner who uses meager needles embedded through the skin to assist with invigorating explicit focuses around the body. According to the Public Community for Reciprocal and Elective Medication (NCCAM), the traditional Chinese medication hypothesis is that acupuncture can help control "qi." Qi is an individual's essential energy that streams along pathways all through the body, known as meridians. A Public Wellbeing Interview Review discovered that back pain was the most generally detailed use for acupuncture, trailed by joint pain.
Is Acupuncture Safe?
According to NCCAM, acupuncture is safe assuming it is performed by an accomplished practitioner using sterile needles. Less antagonistic aftereffects are related with acupuncture than most standard medication treatments normally used to alleviate pain. While infections and penetrated organs are potential dangers while using acupuncture for natural joint pain relief, these events are incredibly rare.
6 notes
·
View notes
Text
Why Is Bunion Treatment Without Surgery A Great Option?
If you're struggling with the pain and discomfort that comes with bunions, it will be a good idea to consider bunion treatment without surgery. This is a safe and cost-effective option that often offers significant benefits over traditional surgery. Here are four reasons why bunion treatment without surgery is a great choice:
1) Bunion treatment without surgery is a safe and affordable option. Surgery is often expensive, and it can lead to long-term pain and discomfort. Bunion treatment without surgery typically involves wearing special shoes or inserts for a period of time, which helps to minimize the chances of developing bunions in the future.
2) There is no need for significant recovery time, with little to no pain. Unlike traditional surgery, which can require weeks or months of rest, most people who undergo bunion treatment without surgery experience minimal pain and minimal recovery time. In some cases, people can resume their normal activities immediately after the treatment.
3) It can improve strength, flexibility, and range of motion. Bunions often cause restriction in these areas, but bunion treatment without surgery can help to restore lost range of motion and improve overall physical function.
4) The main goal of bunion care without surgery is the preservation of the original joint architecture. Surgery aims to correct or fix flaws in the joint surface – but this approach often leads to cosmetic deformity as well as long-term instability or pain in the joint area. By preserving the original joint architecture through bunion care without surgery, patients are able to achieve better results that look more natural overall.
What Non-Surgical Methods Are Used For Treating Bunions?
Bunion treatment is a common issue, and there are several ways that can be used to bring pain relief to the bunion. Some of these methods include shoe modifications, orthotic devices, medications, and surgery.
Many people find that, wearing shoes can reduce pressure on the bunion area and it helps to relieve pain and inflammation. This can be done by switching to shoes with a higher arch or by wearing shoes with a more flexible insole.
Orthotic devices can also be used to help reduce the pressure on the foot in numerous ways. These devices include inserts that fit into your existing shoes or custom-made orthotics that you wear inside your sneakers or boots.
If Bunions are severe enough, surgery is necessary to correct them. However, not all bunions require surgical correction – sometimes, simple shoe modifications will do the trick! If you're still considering surgery, it's important to speak with your doctor about your specific case so that they can provide you with accurate information and advice.
In addition to footwear and orthotics, medications can also be prescribed to relieve bunion pain and inflammation. NSAIDs (nonsteroidal anti-inflammatory drugs) like ibuprofen are effective at reducing inflammation and pain caused by bunion syndrome. At the same time, over-the-counter remedies like aspirin can also provide relief when taken as prescribed.
To Wrap Up
Bunions can be a painful condition, but they don't need to mean the end of your active lifestyle. Non-surgical bunion treatment is a great option for many, as it offers relief from pain and discomfort without the risks associated with surgery. By taking these steps to find relief from bunion pain and discomfort, you can get back on track with your daily activities and enjoy life again!
Contact us: https://www.thefootworkclinic.com.au/
3 notes
·
View notes
Text
What are the Best Options for Pain Medication for Fibromyalgia Patients?
Fibromyalgia is a syndrome that causes chronic pain all over the body, often accompanied by fatigue and sleep problems. While there is no cure for fibromyalgia, there are several treatments that can help relieve symptoms. In this article, we'll discuss some of the best options for pain medication for fibromyalgia.

What are the Types of Pain Medications for Fibromyalgia?
There are a number of types of pain medications for fibromyalgia, but the best options for treating fibromyalgia depend on the specific symptoms being treated and the individual's tolerances. Common pain medications used to treat fibromyalgia include antidepressants, muscle relaxants, and anti-inflammatory medications. Many patients find relief from these treatments, but it is important to discuss the potential side effects with a doctor before starting any new medication.
How do Fibromyalgia Patients Respond to Pain Medications?
Pain medications for fibromyalgia can be quite effective in reducing the level of pain a patient experiences. However, some patients may find that these medications cause side effects that make them less likely to stay adherent to their treatment plan. Additionally, there are different types of pain medications available that may be more or less effective for different types of fibromyalgia pain. Patients should discuss their individual needs with their doctor during prescription consultation. Some common options for pain medication for fibromyalgia include:
Opioids: Opioids are among the most commonly used types of pain medication for treating chronic pain. They work by binding to opioid receptors in the brain and spinal cord, which then block the transmission of signals that are causing the patient's pain. Opioids can be addictive and have side effects such as euphoria, drowsiness, constipation, and nausea. However, they are also very effective at relieving chronic pain and are considered one of the most effective forms of treatment for fibromyalgia.
Triptans: Triptans are a type of medication that functions as an agonist at serotonin receptors. This means that they stimulate the production of serotonin, which reduces feelings of fatigue and helps to improve moods. Commonly prescribed triptans include sumatriptan (Imitrex), zolmitriptan (Zomig), rizatriptan (Maxalt), and almotriptan (Axert). While triptans can be quite effective at reducing pain, they also have side effects such as dizziness, drowsiness, and headache. They should be taken with caution if a patient is also taking other medications that affect serotonin levels, such as SSRIs (selective serotonin reuptake inhibitors).
Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs are a type of medication that work by blocking the activity of various enzymes that are responsible for causing inflammation. This class of drugs includes ibuprofen (Advil, Motrin), naproxen (Aleve), celecoxib (Celebrex), and etodolac (Lodine). NSAIDs can be quite effective at relieving pain, but they also have some side effects, including gastrointestinal problems, liver damage, and kidney impairment. They should be used with caution if a patient is also taking other medications that can damage the kidneys or liver.
Acetaminophen: Acetaminophen is a type of medication that functions as an analgesic and antipyretic. It works by reducing the level of inflammation in the body and helping to relieve pain. Acetaminophen can be dangerous if taken in high doses or if it is taken with other medications that can increase the risk of liver damage. It is generally safe to take acetaminophen in low doses without any additional precautions.
Potential Side Effects of Pain Medications for Fibromyalgia
If you are experiencing chronic pain due to fibromyalgia, there are a number of medications that can help. However, all medications have potential side effects. It is important to speak with your doctor about the best option for you and to be aware of any potential side effects.
The following are some of the most common side effects associated with pain medications for fibromyalgia:
Drowsiness
Nausea and vomiting
Anxiety and irritability
Restlessness and insomnia
Conclusion
Fibromyalgia is a debilitating condition that affects the entire body, causing widespread pain and stiffness. If you are suffering from the same, Nerve Rescue is here to help you. It’s a scientifically proven and highly absorbable nerve rescue formula, Made with 100% pure R-Alpha Lipoic acid, this product helps to calm nerve pain and burning sensation. Premium Nerve Rescue is the ultimate choice for those dealing with pain medication for Fibromyalgia Patients. With its potent antioxidant content, it calms inflammation and supports healthy nerve function. Try Nerve Rescue today!
2 notes
·
View notes
Text
Mechanisms of injury – Rib fractures are common injuries that occur most often following direct blunt thoracic trauma but can also result from severe coughing, athletic activities (eg, rowing, swinging golf clubs), child abuse, and bone metastases.
●Clinical features – Patients with rib fractures typically describe a history of a minor to moderate chest wall injury. Frequently, they can localize the pain to one or two ribs. Examination reveals point tenderness on a specific rib or focal tenderness caused by compression of the ribcage distant from the site of pain. A deep breath typically elicits pain at the fracture site. Rib stress fractures present with a gradual onset of activity-related chest wall pain.
●Diagnosis and diagnostic imaging – Rib fractures in victims of blunt trauma are generally identified clinically or by chest radiograph (CXR). A definitive diagnosis of rib fractures is not always necessary. The presence of isolated rib fractures does not have to be radiologically confirmed in all patients once associated injury has been adequately excluded, typically with a CXR, which is obtained primarily to identify pneumothorax, hemothorax, and other signs of intrathoracic injury.
•In most cases when CXR is not sufficient for the identification of rib fractures, chest computed tomography (CT) should be performed. Chest CT demonstrates greater sensitivity and specificity for rib fractures compared with plain radiographs but should not be performed for the sole purpose of assessing potential rib fractures since the clinical significance of these additionally discovered fractures is generally minimal. When expertise and technology is available, emergency physician-performed bedside ultrasound is an emerging modality with test characteristics comparable to CT for identifying rib fractures. Rib radiographs have very limited utility when CT is available.
•In patients with concern for stress fracture in whom definitive diagnosis will change management, magnetic resonance imaging (MRI) has become the modality of choice. Both bone scintigraphy and MRI have traditionally had better sensitivity for fracture than CT but are limited by resource availability. Bone scintigraphy requires large doses of ionizing radiation and has poor specificity.
•A skeletal survey should be obtained in infants with rib fractures, especially multiple fractures in various stages of healing, since this raises suspicion for abuse.
●Fracture patterns associated with internal injuries – Liver or spleen lacerations, mediastinal injury, pneumothorax, hemothorax, flail chest, and pulmonary contusion may occur but are uncommon with isolated rib injuries. An increasing number of rib fractures correlates with serious intrathoracic and intra-abdominal injuries. Displaced fractures increase the risk of internal injury and delayed bleeding.
•First rib fractures are associated with greater overall injury severity and life-threatening internal injury (including injuries to the brain, spine, lungs, and pelvis).
•Fractures of superior ribs (numbers 1 to 3) reflect trauma involving significant force and the potential for injury to mediastinal structures, major blood vessels (eg, aorta), and lung parenchyma.
•Fractures of ribs 9 through 12 may be associated with intra-abdominal injury. Right lower rib fractures may be associated with hepatic injury and left lower rib fractures with splenic injury. Fractures of the posterior portion of the lower ribs can be associated with renal injury.
•Three or more adjacent ribs each fractured in two places (ie, flail chest) (figure 4) is often associated with significant morbidity from pulmonary contusion as well as injuries elsewhere.
●Management – Treatment of rib fractures should be focused on early and adequate pain relief to avoid complications (eg, pneumonia) from splinting and atelectasis. Analgesia for isolated rib fractures includes nonsteroidal antiinflammatory drugs (NSAIDs) with or without opioids. Encourage incentive spirometry to prevent atelectasis.
For more severe injuries, intercostal nerve blocks are an effective approach but typically require admission.
Rib stress fractures are treated similarly to other low-risk stress fractures. Treatment begins with restriction of the inciting activity for four to six weeks followed by a gradual return to the activity as tolerated.
●Disposition – We typically hospitalize patients with three or more rib fractures and use a more conservative threshold for admission in older or frail adults and those at increased risk for pulmonary complications. An algorithm to assist clinicians with the disposition of patients with isolated rib fractures is provided (algorithm 1).
●Follow-up care – A follow-up evaluation six to eight weeks after the injury is reasonable, especially if the patient has persistent pain or any questions regarding ability to return to sports or work. Virtually all rib fractures heal well within six weeks. Follow-up chest radiographs are unnecessary unless indicated by clinical symptoms (eg, new shortness of breath, new or severe pain). (See 'Follow-up care' above.)
●Return to sports and work – Some patients are able to return to work within a few days, depending on their occupation, while some patients may experience prolonged pain and disability. (See 'Return to sports and work' above.)
4 notes
·
View notes
Text
Understanding the Complexities of Endometriosis and Its Treatment

Endometriosis is a challenging and frequently misunderstood condition that impacts millions of women globally. Despite its prevalence, it remains a significant challenge for diagnosis and treatment. Understanding the intricacies of endometriosis and its management can empower individuals to seek the care they need and improve their quality of life.
This blog explores the symptoms of endometriosis and its treatment options.
What is Endometriosis?
Endometriosis is a long-term medical condition in which tissue resembling the uterine lining, called the endometrium, develops outside the uterus. This abnormal growth can occur on the ovaries, fallopian tubes, the outer surface of the uterus, and other organs within the pelvis. Each month, these endometrial-like tissues respond to the menstrual cycle hormones, thickening, breaking down, and bleeding. However, unlike the tissue inside the uterus, this blood has no way to exit the body, leading to inflammation, pain, and the formation of scar tissue.
Symptoms and Diagnosis
The symptoms of endometriosis vary widely among individuals, making diagnosis challenging. Common symptoms include:
Pelvic Pain: Often described as severe menstrual cramps, pelvic pain can occur throughout the menstrual cycle.
Pain During Intercourse: Pain during or after sexual activity is common.
Pain with Bowel Movements or Urination: Particularly noticeable during menstruation.
Infertility: Endometriosis can be discovered incidentally during investigations for infertility.
Other Symptoms: Fatigue, diarrhea, constipation, bloating, and nausea may also occur.
Diagnosing endometriosis often involves a combination of medical history, physical examinations, imaging tests (such as ultrasounds or MRIs), and laparoscopy, a minimally invasive surgical procedure that allows doctors to view and obtain a biopsy of the endometrial-like tissue.
Treatment Options
There is no one-size-fits-all approach to treating endometriosis. The treatment plan often depends on the severity of the condition, the symptoms, and the individual’s goals, such as pain management or fertility preservation.
Here are the main treatment options:
1. Pain Management: Over-the-counter pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help alleviate pain. However, pain relief strategies should be part of a broader treatment plan.
2. Hormonal Therapies: Hormonal treatments are designed to reduce or stop menstruation, which can help alleviate endometriosis symptoms. Managing these hormonal changes and their effects on overall well-being is essential. Common hormonal therapies include:
Birth Control Pills: Regulate or eliminate menstrual periods.
Progestins: Hormones that prevent menstruation.
GnRH Agonists and Antagonists: Medications that induce a temporary menopause-like state to reduce estrogen levels and endometriosis growth.
3. Surgical Options: For women who experience severe symptoms or do not respond to other treatments, surgery may be necessary. The goal of surgery is to remove or destroy endometrial growths while preserving the uterus and ovaries. In some cases, a hysterectomy (removal of the uterus) may be considered, particularly if other treatments are unsuccessful.
4. Lifestyle and Alternative Therapies: Complementary approaches such as dietary changes, physical therapy, acupuncture, and stress management techniques may help manage symptoms and improve overall well-being. However, these should be used in conjunction with conventional treatments rather than as replacements.
Managing Endometriosis: A Holistic Approach
Endometriosis management often requires a multidisciplinary approach. Working with a team of healthcare professionals, including gynecologists, pain specialists, and mental health professionals, can provide a comprehensive treatment plan. Additionally, support groups and counseling can offer emotional support and practical advice for navigating the challenges of living with endometriosis.
Conclusion
Ongoing research is focused on better understanding the causes of endometriosis, improving diagnostic methods, and developing more effective treatments. As awareness of the condition grows, there is hope for advancements that will enhance the quality of life for those affected.
Endometriosis is a complex condition that impacts various aspects of a person’s life. Although managing it can be difficult, a combination of medical care, lifestyle changes, and support can greatly improve the situation. If you suspect you have endometriosis or are dealing with its symptoms, consulting an experienced gynecologist in Mumbai is the first step toward relief and enhancing your quality of life.
0 notes
Text
A Guide to Chronic Knee Pain: Understanding, Managing, and Treating
Chronic knee pain can be a debilitating condition, affecting daily activities and overall quality of life. It often results from long-term conditions and injuries, requiring comprehensive management and treatment. In this guide, we will explore the causes, symptoms, and treatment options for chronic knee pain to help you better understand and manage this condition.
Understanding Chronic Knee Pain
Chronic knee pain is defined as pain that persists for more than three months. Unlike acute knee pain, which results from a sudden injury, chronic knee pain usually develops gradually and may be related to ongoing conditions.
Common Causes of Chronic Knee Pain
Osteoarthritis
Description: A degenerative joint disease where the cartilage in the knee joint wears down over time.
Symptoms: Pain, stiffness, and swelling, particularly after periods of inactivity or excessive use.
Rheumatoid Arthritis
Description: An autoimmune condition that causes inflammation of the knee joint lining.
Symptoms: Swelling, pain, and stiffness, often affecting both knees simultaneously.
Tendinitis
Description: Inflammation of the tendons around the knee, often due to overuse.
Symptoms: Pain during movement, tenderness, and swelling.
Bursitis
Description: Inflammation of the bursae, the small fluid-filled sacs that cushion the knee joint.
Symptoms: Swelling, warmth, and pain, especially with pressure on the knee.
Gout
Description: A type of arthritis caused by the buildup of uric acid crystals in the knee joint.
Symptoms: Intense pain, redness, and swelling, often occurring suddenly.
Patellofemoral Pain Syndrome
Description: Pain originating from the interaction between the patella (kneecap) and the femur (thighbone).
Symptoms: Pain around or behind the kneecap, worsening with activity or prolonged sitting.
Symptoms of Chronic Knee Pain
Persistent aching or sharp pain in the knee
Swelling and stiffness
Reduced range of motion
Difficulty bearing weight on the affected knee
Popping or crunching noises
Instability or weakness in the knee
Diagnosis of Chronic Knee Pain
To accurately diagnose the cause of chronic knee pain, a healthcare provider may:
Conduct a Physical Examination: Assess the knee’s range of motion, stability, and areas of tenderness.
Order Imaging Tests: X-rays, MRIs, or CT scans to view the internal structures of the knee.
Perform Lab Tests: Blood tests to check for signs of infection, inflammation, or autoimmune disorders.
Aspirate Joint Fluid: Extract fluid from the knee joint for analysis, particularly in cases of suspected gout or infection.
Treatment Options for Chronic Knee Pain
1. Lifestyle Modifications
Weight Management: Reducing body weight to decrease stress on the knee joints.
Low-Impact Exercise: Engaging in activities like swimming, cycling, or walking to strengthen muscles without overstressing the knee.
Proper Footwear: Wearing supportive shoes to improve knee alignment and reduce strain.
2. Physical Therapy
Strengthening Exercises: Targeting muscles around the knee to improve support and reduce pain.
Flexibility Training: Stretching exercises to maintain or improve range of motion.
Manual Therapy: Techniques like massage or joint mobilization performed by a physical therapist.
3. Medications
Pain Relievers: Over-the-counter options like acetaminophen or prescription medications.
Anti-Inflammatories: Nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and swelling.
Topical Analgesics: Creams or gels applied directly to the knee.
4. Injections
Corticosteroids: To reduce inflammation and pain.
Hyaluronic Acid: To lubricate the knee joint and improve mobility.
Platelet-Rich Plasma (PRP): To promote healing and reduce pain.
5. Surgical Options
Arthroscopy: A minimally invasive surgery to repair or remove damaged tissue.
Osteotomy: Realigning bones to reduce pressure on the knee joint.
Partial or Total Knee Replacement: Replacing damaged parts of the knee with artificial components.
Managing Chronic Knee Pain
Regular Monitoring: Keeping track of symptoms and flare-ups to inform treatment adjustments.
Pain Management Techniques: Using heat or cold therapy, practicing relaxation techniques, and maintaining a healthy diet.
Support Groups: Joining groups or online forums for people with chronic knee pain to share experiences and tips.
Conclusion
Chronic knee pain can be challenging, but understanding its causes, symptoms, and treatment options is the first step toward effective management. By working closely with healthcare providers like Dr. Vivekananda, the Best Knee Replacement Surgeon in Hyderabad, and incorporating lifestyle changes, physical therapy, medications, and, if necessary, surgical interventions, individuals can significantly improve their knee health and overall quality of life. If you experience persistent knee pain, consult a healthcare professional to develop a personalized treatment plan tailored to your needs.
0 notes