#neuroimaging techniques
Explore tagged Tumblr posts
Text

I. Symptoms of Parkinson's Disease:
Symptoms associated with Parkinson's Disease encompass a broad array of motor and non-motor manifestations that can significantly affect an individual's well-being. Motor symptoms include tremors, characterized by rhythmic shaking in various body parts, bradykinesia, which results in slowed movement initiation and execution, rigidity causing stiffness in limbs and trunk, and postural instability leading to balance and coordination difficulties, increasing the risk of falls. Non-motor symptoms span cognitive impairment, mood disturbances like depression and anxiety, sleep disturbances, autonomic dysfunction impacting functions such as blood pressure regulation and digestion, as well as sensory abnormalities.
II. Causes of Parkinson's Disease:
The causes of Parkinson's Disease remain largely unclear, thought to arise from a combination of genetic predisposition and environmental factors. While most cases are sporadic, approximately 5-10% are familial, linked to mutations in genes like SNCA, LRRK2, PARKIN, and PINK1. Environmental factors such as exposure to pesticides, herbicides, heavy metals, certain industrial chemicals, traumatic brain injury, and viral infections are also implicated.
III. Parkinson's Disease Diagnosis:
Diagnosing Parkinson's Disease relies primarily on clinical evaluation, including a detailed medical history, comprehensive physical examination, and assessment of both motor and non-motor symptoms. A diagnosis typically requires the presence of cardinal motor features along with a positive response to dopaminergic therapy. Neuroimaging techniques like MRI and PET scans may assist in excluding alternative diagnoses and monitoring disease progression.
IV. Treatment for Parkinson's Disease:
While Parkinson's Disease remains incurable, various treatment options aim to alleviate symptoms and improve quality of life. Pharmacotherapy, including levodopa, dopamine agonists, MAO-B inhibitors, and COMT inhibitors, is central to management, aiming to restore dopamine levels, manage motor fluctuations, and alleviate non-motor symptoms. In advanced cases resistant to medication, surgical interventions like deep brain stimulation (DBS) may be considered, involving the implantation of electrodes to modulate abnormal neuronal activity and alleviate symptoms.
Early detection and intervention in Parkinson's disease can help in managing the condition better. This can be achieved by undergoing regular health checkups. You can opt for a regular full body health checkup at Jaslok Hospital Mumbai, which is one of India's finest hospitals for the management of neurological conditions like Parkinson's disease.
#parkinson's disease#full body health checkup#regular health checkups#instability#risk of falls#bradykinesia#anxiety#sleep disturbances#neuroimaging techniques#neuroimaging#MRI scans#PET scans
0 notes
Text
TRANSABLEISM.

What is transableism ?
Transableism is characterized by the desire for a non-disabled individual to acquire a specific disability such as the loss of a sense or a limb (amputation, paralysis, blindness, deafness, etc.), thus placing them in a situation of disability.
The opposite of transabled is cisabled wich describes a person who does have that disability bodily.
Transableism is a new thing ?
No, ''transabled'' is a sociological and political term coined by Sean O'connor in 2004 in attempts to demedicalize disability desires and views them as healthy person's challenge to the stigma of disability as created by social norms. Researchers and transabled people use a variety of terms to describe it. some people refer to "apotemnophilia" a term that have been used the first time in a 1977 article by psychologists Gregg Furth and John Money. We do not recomand this term.
Then, In 2004 Michael First published the first clinical research in which he surveyed fifty-two people with the condition, a quarter of whom had undergone an amputation. Based on that work, First coined the term "body integrity identity disorder" (BIID) to express what he saw as more of an identity disorder than a paraphilia.
The newest term, ''xenomelia'' was established to acknowledge the neurologic component of the condition after neuroimaging studies showed structural changes to the right parietal lobe in individuals who desired amputation of their left lower limb, thus linking the part of the brain that processes sensory input from the affected limb. (McGeoch and others 2011).
Friendly reminder that a transabled person do not necessary experience body integrity identity dysphoria (BIID). People with BIID (dysphorics transableds) experience a suffering with a part of their body, such as a limb, and feel that removing or disabling that part of their body will relieve the discomfort. People with the condition may have intense feelings of envy toward amputees. They may pretend to be an amputee, both publicly and privately. Patients who experience the above symptoms consider them strange and abnormal.
Confusions.
Body dysmorphic disorder is sometimes confounded with disability desires. The two conditions may share a preoccupation with a specific part of one's body, but body dysmorphic disorder is typically concerned with the visual aspects of that part, which is never the case in disability desires. Also, the concerns in body dysmorphic disorders usually focus on facial parts, not on major limbs or sense.
WHY ?
A study conducted by Michael B. First on 52 aspiring or volunteer amputees shows that the main reason given is to regain their true identity, to correct an anatomical anomaly. It is difficult to establish precisely why this need manifests itself in transabled people, even if there are neurological and biological leads. The only difference between a transabled person and a transgender person would be the level of social acceptance of each phenomenon. As transgender people, the transition to the desired body in transabled people is associated with greater general well-being, and a significative decrease in suicidal and depressive thoughts.
It's a choice ?
No, feel the desire to acquire a physical deficit isn't a choice but start a process in order to acquire a disability is a choice. Just as for trans people, they do not choose to be trans but they choose (often the pressure of gender dysphoria) to transition.
When someone realize they are transabled ?
The disabled- desires comes very early in their life. Their first experiecs of such desires are felt in their childhood, around the age of 7 this study found.
Psychological therapy, psychopharmacological drugs and relaxation techniques had little effect and sometimes increased desire. They can reduces symptoms like depression, but not disability desires per se.
This study shows that the amputation of the healthy body part appears to result in remission of BIID and an impressive improvement of quality of life. 100% of transabled who had recived a surgical amputation confirm that it was helpful. With medication 73% pretended that this treatement for BIID was unhelpful and 60% confirm that therapy was unhelpful. Betweet those who recieved and didn't recieve an ambutation, those who didn't recievent it said that BIID had an extreme negative impact in their personal happinnes (17,2 in the Y-BOCS scale) in comparison, those who recieve an amputation affirmate that BIID had a extreme low effect in their personal life (3,2 on the Y-BOCS scale).
Psychotherapy was often supportive, but did not help diminishing BIID symptoms.
Those who didn't recieve an ambutation confirmate that BIID had severely disrupt their work counter a very neglectical effect (3,2 ON Y-BOCS scale) for those who recieve an amputation.
Several others studies: (1) (2) (3) shows that all transabled people who have successfully made the transition say they are very satisfied and happy.
In all cases quality of life was rated to be substantially increased, and no new disability desire emerged post-surgery. There is considerable support for the view that elective amputations can be ethically justified , even if long-term effects of the intervention still need to be assesse
Dangers for not letting a person acquire the desired handicap.
Amputations seem to be the only effective solution. Denying these people the only treatment that can cure their dysphoria will only prolong their suffering and many trans-capacitated individuals will therefore opt for dangerous solutions, such as turning to the black market, attempting to perform their own surgery, or injuring themselves severely enough that a doctor has no choice but to proceed with the amputation of an unwanted limb. It's like denying to a dysphoric transgender person the right to transition.
Why is not different from transgender people ?
Like transgender people, transabled people feel an internal identity that they seek to match with their body. The only difference between the two is the level of social acceptance, unlike transgender people, transabled people in addition to being even more stigmatized and marginalized by the ableist and cisableist society than transgender people, do not benefit from surgical intervention allowing them to obtain the desired body.
Anti-choice arguments.
Anti-choice authors in relation to transbled- surgical operations argue that these people are not autonomous, 'irrational', alienated by their conditionality and cannot make an informed choice. Elliott (2009, p. 159) summarizes the authors' position well (without adhering to it): "These objections focus on the nature of the 'wannabe's' belief that they should have a limb amputated, suggesting that because it is bizarre, irrational, and obsessive, they are unable to properly 'weigh' the information relevant to the decision, that these desires are not autonomous, and are not to be respected or followed. On the one hand, in light of previous data, this position is not scientifically supported and is based on prejudice and impression. Authors who support transabled-surgery argue that refusing it would be violating the first ethical principle of autonomy; if these people are rational and do not make their decision under coercion, their autonomy must be respected. On the other hand, this question of autonomy and rational choice rests on double standards. The very requirement of an explanation and a rational to justify this need obscures the fact that for many very important decisions in our lives, these explanations rationality are not required; for example, playing dangerous sports, having children, going on a humanitarian mission to a war-torn country, or simply choosing to live are not subject to the same questioning and the same requirement of rationality. As Gheen (2009, p. 99) argues, most of the choices we make do not have "rationality" and cannot be explained; we have needs and desires, we realize them, and no one demands evidence of rationality from these actions that sometimes have considerable impacts on our lives and the lives of others. Gheen argues that if this need of the transabled is considered irrational and illegitimate, it is because it goes outside the dominant norms.
Important barriers.
In addition to society's ableism and cisableism, the Hippocratic Oath, by which physicians pledge to "do no harm" to their patients, is the main barrier between a transabled person and his or her disability; practitioners cannot help individuals acquire an impairment that is presumed to have a "detrimental" effect on their lives (Johnston and Elliot, 2002). But an ethical question arises and a paradox emerges. Should we leave transabled dysphoric people in a state of severe suffering, causing them depressive symptoms and even suicidal ideas with the belief that amputation will have a "negative" impact on their lives, when we know that this is not true as datas we have seen previously, rather than allowing them to acquire the desired disability thus allowing their body dyphoria to remit and increasing their general well-being? If doctors commit themselves not to harm their patients isn't it paradoxical to refuse the only possible treatment, i.e. the medical acquisition of a handicap via a surgical intervention to someone, keeping them consequently in a state harmful to his mental health? In other words, the doctor refusing health care to someone who needs it is the equivalent of a health care professional refusing to allow a dysphoric transgender person to undergo a medical transition: it is bad from a moral point of view as well as from the point of view of the person's mental health and exposes them to the risk that she voluntarily injures themself or that they performs their own surgery with all the potential dangers on their life and their health that such a decision implies and opposes the fundamental freedom hard won by social movements to do what we want with our body.

Pt: If you dont like us, just block! Feel free to ask for more information about the label.

Pt: DNI: Truscum, heavy religius, dahlia/winter, antiradqueer, anti transids, anti paras, anti muds, anti mspec, anti endos, anti profic, hypoharmful, non-good faith, anti cosang, anti therian, otherkin (etc), terfs, anti xenogenders or xenoids, pro-harrasment of any type, anti kink, anti agere/petre.
#radqueer#pro rq 🌈🍓#radqueer 🌈🍓#rq 🌈🍓#rqc🌈🍓#🌈🍓 safe#🌈🍓 coining#🌈🍓 please interact#pro transid#transid#transid defender#transid please interact#transid safe
43 notes
·
View notes
Text
https://neurosciencenews.com/neuroimaging-asd-markers-27593/ this is dumb bc the autistic subjects were recruited solely from people already known to have genetic markers they didn't describe any step that actually suggests that these techniques would identify the majority of people with clinically defined autism
5 notes
·
View notes
Text
You receive an invitation, emblazoned with a question: “A bouncing little ‘he’ or a pretty little ‘she’?” The question is your teaser for the “gender reveal party” to which you are being invited by an expectant mother who, at more than 20 weeks into her pregnancy, knows what you don’t: the sex of her child. After you arrive, explains cognitive neuroscientist Gina Rippon in her riveting new book, The Gendered Brain, the big reveal will be hidden within some novelty item, such as a white iced cake, and will be colour-coded. Cut the cake and you’ll see either blue or pink filling. If it is blue, it is a…
Yes, you’ve guessed it. Whatever its sex, this baby’s future is predetermined by the entrenched belief that males and females do all kinds of things differently, better or worse, because they have different brains.
“Hang on a minute!” chuckles Rippon, who has been interested in the human brain since childhood, “the science has moved on. We’re in the 21st century now!” Her measured delivery is at odds with the image created by her detractors, who decry her as a “neuronazi” and a “grumpy old harridan” with an “equality fetish”. For my part, I was braced for an encounter with an egghead, who would talk at me and over me. Rippon is patient, though there is an urgency in her voice as she explains how vital it is, how life-changing, that we finally unpack – and discard – the sexist stereotypes and binary coding that limit and harm us.
For Rippon, a twin, the effects of stereotyping kicked in early. Her “under-achieving” brother was sent to a boys’ academic Catholic boarding school, aged 11. “It’s difficult to say this. I was clearly academically bright. I was top in the country for the 11+.” This gave her a scholarship to a grammar school. Her parents sent her to a girls’ non-academic Catholic convent instead. The school did not teach science. Pupils were brought up to be nuns or a diplomatic wife or mother. “Psychology,” she points out, “was the nearest I could get to studying the brain. I didn’t have the A levels to do medicine. I had wanted to be a doctor.”
A PhD in physiological psychology and a focus on brain processes and schizophrenia followed. Today, the Essex-born scientist is a professor emeritus of cognitive neuroimaging at Aston University, Birmingham. Her brother is an artist. When she is not in the lab using state-of-the-art brain imaging techniques to study developmental disorders such as autism, she is out in the world, debunking the “pernicious” sex differences myth: the idea that you can “sex” a brain or that there is such a thing as a male brain and a female brain. It is a scientific argument that has gathered momentum, unchallenged, since the 18th century “when people were happy to spout off about what men and women’s brains were like – before you could even look at them. They came up with these nice ideas and metaphors that fitted the status quo and society, and gave rise to different education for men and women.”
Rippon has analysed the data on sex differences in the brain. She admits that she, like many others, initially sought out these differences. But she couldn’t find any beyond the negligible, and other research was also starting to question the very existence of such differences. For example, once any differences in brain size were accounted for, “well-known” sex differences in key structures disappeared. Which is when the penny dropped: perhaps it was time to abandon the age-old search for the differences between brains from men and brains from women. Are there any significant differences based on sex alone? The answer, she says, is no. To suggest otherwise is “neurofoolishness”.
“The idea of the male brain and the female brain suggests that each is a characteristically homogenous thing and that whoever has got a male brain, say, will have the same kind of aptitudes, preferences and personalities as everyone else with that ‘type’ of brain. We now know that is not the case. We are at the point where we need to say, ‘Forget the male and female brain; it’s a distraction, it’s inaccurate.’ It’s possibly harmful, too, because it’s used as a hook to say, well, there’s no point girls doing science because they haven’t got a science brain, or boys shouldn’t be emotional or should want to lead.”
The next question was, what then is driving the differences in behaviour between girls and boys, men and women? Our “gendered world”, she says, shapes everything, from educational policy and social hierarchies to relationships, self-identity, wellbeing and mental health. If that sounds like a familiar 20th-century social conditioning argument, it is – except that it is now coupled with knowledge of the brain’s plasticity, which we have only been aware of in the past 30 years.
“It is now a scientific given,” says Rippon, “that the brain is moulded from birth onwards and continues to be moulded through to the ‘cognitive cliff’ in old age when our grey cells start disappearing. So out goes the old ‘biology is destiny’ argument: effectively, that you get the brain you are born with – yes, it gets a bit bigger and better connected but you’ve got your developmental endpoint, determined by a biological blueprint unfolding along the way. With brain plasticity, the brain is much more a function of experiences. If you learn a skill your brain will change, and it will carry on changing.” This is shown to be the case in studies of black cab drivers learning the Knowledge, for example. “The brain is waxing and waning much more than we ever realised. So if you haven’t had particular experiences – if as a girl you weren’t given Lego, you don’t have the same spatial training that other people in the world have.
If, on the other hand, you were given those spatial tasks again and again, you would get better at them. “The neural paths change; they become automatic pathways. The task really does become easier.”
Neural plasticity throws the nature/nurture polarity out of the lab window. “Nature is entangled with nature,” says Rippon. Added to this, “being part of a social cooperative group is one of the prime drives of our brain.” The brain is also predictive and forward-thinking in a way we had never previously realised. Like a satnav, it follows rules, is hungry for them. “The brain is a rule scavenger,” explains Rippon, “and it picks up its rules from the outside world. The rules will change how the brain works and how someone behaves.” The upshot of gendered rules? “The ‘gender gap’ becomes a self-fulfilling prophecy.”
Rippon regularly talks in schools. She wants girls to have leading scientists as role models, and she wants all children to know that their identity, abilities, achievements and behaviour are not prescribed by their biological sex. “Gender bombardment” makes us think otherwise. Male babies dressed in blue romper suits, female ones in pink is a binary coding that belies a status quo that resists the scientific evidence. “Pinkification”, as Rippon calls it, has to go. Parents don’t always like what they hear.
“They say, ‘I have a son and a daughter, and they are different.’ And I say, ‘I have two daughters, and they are very different.’ When you talk about male and female identity, people are very wedded to the idea that men and women are different. People like me are not sex-difference deniers,” continues Rippon. “Of course there are sex differences. Anatomically, men and women are different. The brain is a biological organ. Sex is a biological factor. But it is not the sole factor; it intersects with so many variables.”
I ask her for a comparable watershed moment in the history of scientific understanding, in order to gauge the significance of her own. “The idea of the Earth circling around the sun,” she bats back.
Letting go of age-old certainties is frightening, concedes Rippon, who is both optimistic about the future, and fearful for it. “I am concerned about what the 21st century is doing, the way it’s making gender more relevant. We need to look at what we are plunging our children’s brains into.”
Ours may be the age of the self-image, yet we aren’t ready to let the individual self emerge, unfettered by cultural expectations of one’s biological sex. That disconnect, says Rippon, is writ large, for example, in men. “It suggests there is something wrong in their self-image.” The social brain wants to fit in. The satnav recalibrates, according to expectations. “If they are being driven down a route that leads to self-harm or even suicide or violence, what is taking them there?”
On the plus side, our plastic brains are good learners. All we need to do is change the life lessons.
How gender stereotypes led brain science
Research so far has failed to challenge deep prejudice, says Gina Rippon
Several things went wrong in the early days of sex differences and brain imaging research. With respect to sex differences, there was a frustrating backward focus on historical beliefs in stereotypes (termed “neurosexism” by psychologist Cordelia Fine). Studies were designed based on the go-to list of the “robust” differences between females and males, generated over the centuries, or the data were interpreted in terms of stereotypical female/male characteristics which may not have even been measured in the scanner. If a difference was found, it was much more likely to be published than a finding of no difference, and it would also breathlessly be hailed as an “at last the truth” moment by an enthusiastic media. Finally the evidence that women are hard-wired to be rubbish at map reading and that men can’t multi-task! So the advent of brain imaging at the end of the 20th century did not do much to advance our understanding of alleged links between sex and the brain. Here in the 21st century, are we doing any better?
One major breakthrough in recent years has been the realisation that, even in adulthood, our brains are continually being changed, not just by the education we receive, but also by the jobs we do, the hobbies we have, the sports we play. The brain of a working London taxi driver will be different from that of a trainee and from that of a retired taxi driver; we can track differences among people who play videogames or are learning origami or to play the violin. Supposing these brain-changing experiences are different for different people, or groups of people? If, for example, being male means that you have much greater experience of constructing things or manipulating complex 3D representations (such as playing with Lego), it is very likely that this will be shown in your brain. Brains reflect the lives they have lived, not just the sex of their owners.
Seeing the life-long impressions made on our plastic brains by the experiences and attitudes they encounter makes us realise that we need to take a really close look at what is going on outside our heads as well as inside. We can no longer cast the sex differences debate as nature versus nurture – we need to acknowledge that the relationship between a brain and its world is not a one-way street, but a constant two-way flow of traffic.
Once we acknowledge that our brains are plastic and mouldable, then the power of gender stereotypes becomes evident. If we could follow the brain journey of a baby girl or a baby boy, we could see that right from the moment of birth, or even before, these brains may be set on different roads. Toys, clothes, books, parents, families, teachers, schools, universities, employers, social and cultural norms – and, of course, gender stereotypes – all can signpost different directions for different brains.
Resolving arguments about differences in the brain really matters. Understanding where such differences come from is important for everyone who has a brain and everyone who has a sex or a gender of some kind. Beliefs about sex differences (even if ill-founded) inform stereotypes, which commonly provide just two labels – girl or boy, female or male – which, in turn, historically carry with them huge amounts of “contents assured” information and save us having to judge each individual on their own merits or idiosyncrasies.
With input from exciting breakthroughs in neuroscience, the neat, binary distinctiveness of these labels is being challenged – we are coming to realise that nature is inextricably entangled with nurture. What used to be thought fixed and inevitable is being shown to be plastic and flexible; the powerful biology-changing effects of our physical and our social worlds are being revealed.
The 21st century is not just challenging the old answers – it is challenging the question itself.
3 notes
·
View notes
Photo
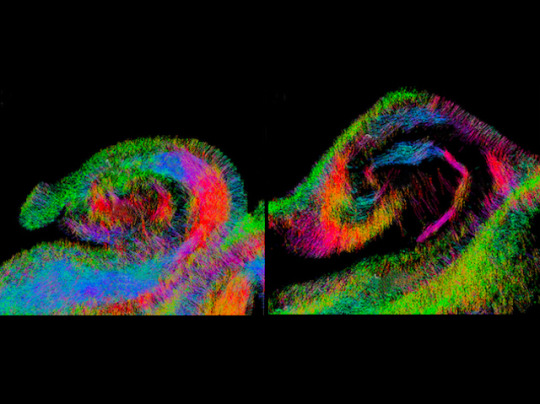
Diving to Depths
The dentate gyrus is a part of the brain that contributes to the formation of memories. In individuals with Alzheimer’s disease, this is the first site known to undergo degenerative changes even before symptoms start to show. This sounds promising for detecting Alzheimer’s earlier, but this structure is only a few millimetres thick and hidden deep within the brain. To exploit this knowledge, we would need really powerful imaging techniques to detect microscopic changes. Here, researchers used a 16.4 Tesla MRI scanner – a much stronger magnetic field than currently used for human body imaging – to measure changes for example in neuron density and abnormal protein accumulation within the dentate gyrus from postmortem brains of cognitively normal individuals (left) and those with Alzheimer’s (right). Colours highlight neuron fibres in subregions, revealing differences. While this technology is far from ready for a clinical setting, it is a step in the right direction.
Written by Sophie Arthur
Image from work by Nien-Chu Shih and colleagues
USC Stevens Neuroimaging and Informatics Institute, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in NeuroImage: Clinical, January 2023
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#neuroscience#alzheimers#Alzheimer's disease#dentate gyrus#mri scan#neurons#body imaging
15 notes
·
View notes
Photo

Editorial: Is autism overdiagnosed? (Eric Fombonne, The Journal of Child Psychology and Psychiatry, 2023)
“That at least some of these community diagnoses are false positives was illustrated in one of our studies where, of 232 school-age children and adolescents with a pre-existing community diagnosis of ASD referred to our academic center for a neuroimaging study, only 47% met research criteria for ASD after an extensive diagnostic re-evaluation process (Duvall et al.,2022).
Yet, many were deemed to have been ‘meeting DSM criteria’ or ‘above the ADOS cut-off’ in prior records.
Overdiagnosis can result from shortcomings at either the diagnostic instrument or the diagnostic process levels.
With regard to diagnostic instrument, ADOS training workshops provide testers with a road map for organizing structured activities and social interactions designed to elicit diagnostically informative behaviors.
Techniques of test administration are straightforward to learn. However, scoring instructions are complex and necessitate a careful analysis and interpretation of the behaviors observed.
Even though the coding conventions are rigorously operationalized, a good deal of clinical judgment and experience remains necessary for the tester to accurately map observed behaviors to underlying autistic disturbances.
For example, children may talk repetitively about dinosaurs they saw during a recent museum visit which may be age-appropriate in young children; however, for this intense interest to be considered as excessive or ‘circumscribed’ requires that other features are demonstrated (odd quality, interference with demands, etc...).
Likewise, abnormal eye gaze is not specific to ASD and is observed across a number of other clinical conditions.
To count toward an ASD diagnosis, eye contact does not simply need to be absent or decreased but evidence of poor modulation in the dynamic context of a social interaction must be brought.
The issue is that many atypical behaviors that are linked to ASD are not specific to ASD.
Counting abnormal behaviors without establishing their specific autistic quality or nature is a source of overdiagnosis. (…)
For example, turn-taking in a conversation can be impaired in both ASD (Failure of normal back-and-forth conversation) and Attention Deficit Hyperactivity Disorder (ADHD) (Often talks excessively, Blurts out answers).
Ascribing a symptom to either disorder requires a clinical analysis and judgment about the mechanism underlying conversation difficulty (pragmatic deficit? orimpulsivity?) that comes with experience in general psychopathology.
Overdiagnosing may also occur due to deficiencies in the overall diagnostic process and formulation.
As Bishop & Lord articulated, the diagnostic decision process must transcend the results of any particular tool, even if the administration of that test is considered to be a gold standard.
Combination of findings from different observations across contexts, informants, and data collection procedures (direct observation, caregiver report, school evaluations, medical records,...) must be performed.
Discrepancies between test results are common; there is no simple algorithmic solution to resolve them and expert clinical judgment is necessary to that end. (…)
Many would argue that the priority is to provide access to services for children presenting with neurodevelopmental disorders and that the consequences of underdiagnosis are far more deleterious than those due to overdiagnosis.
It may be so but that does not mean that erroneously diagnosing a child with ASD is harmless.
At the individual level, carrying an ASD diagnosis may unduly constrain one individual’s range of social and educational experiences and have long-lasting effects on his/her/their identity formation.
At a population level, the unjustified use of intensive services raises concerns about equity and fairness in services access for children who have neurodevelopmental disorders other than autism and struggle to access support services that they need as much as their peers with ASD.”
14 notes
·
View notes
Text

Mapping human brain function is a longstanding goal of neuroscience that promises to inform the development of new treatments for brain disorders. Early maps of human brain function were based on locations of brain damage or brain stimulation that caused a change in function. Over time, this approach was largely replaced by technologies such as functional neuroimaging, which identify brain regions correlated with behaviors or symptoms. Despite their advantages, these technologies reveal correlation, not causation. This creates challenges for interpreting the data generated from these tools and using them to develop treatments for brain disorders. A return to causal mapping of human brain function based on brain lesions and brain stimulation is underway. New approaches can combine these causal sources of information with modern neuroimaging and electrophysiology techniques to gain new insights into the functions of specific brain areas. In this Review, we provide a definition of causality for translational research, propose a continuum along which to assess the relative strength of causal information from human brain mapping studies, and discuss recent advances in causal brain mapping and their relevance for developing treatments.
6 notes
·
View notes
Text
Alzheimer's Disease: biomarkers and neuroimaging markers cheatsheet for research articles
As Alzheimer's Disease (AD) research skews toward understanding the brain than the pathogenic proteins, studies exploring biomarkers and neuroimaging are hopeful toward developing a method for successful prevention of AD. A biomarker is a molecule, whose presence indicates abnormality or disease, and thus, is crucial in diagnostic procedures. Levels of certain molecules is notably altered in cerebrospinal fluid and in blood plasma, which helps in diagnosing the occurrence of AD. Neuroimaging involves the use of techniques such as magnetic resonance imaging and computed tomography to observe neuronal activity in the brain. This is good news, especially for AD, as the asymptomatic stage of the disease can be identified early enough.
Although the exact function and involvement in clinical practice is not profuse, altered concentrations of these biomarkers in plasma or cerebrospinal fluid encourage further research:
Amyloid and tau serve as the unsurprising biomarkers of AD pathology.
Neurofilament-light chain (NF-L) and visinin-like protein-1 (VILIP-1) are the most promising biomarkers of neuronal injury.
Post-synaptic protein neurogranin (Ng) and pre-synaptic proteins synaptosome-associated protein-25 (SNAP-25) and synaptotagmin-1 (Syt-1) are considered major biomarkers of synaptic injury.
Brain and CSF levels of tumor necrosis factor alpha (TNF-α) and increased levels of interleukin group of proteins (ILs) indicate intensified microglial response to neuroinflammation.
TREM2 receptor and YKL-40 glycoprotein are also reliable indicators of inflammation and impaired clearance of amyloid beta.
Heart-type fatty acid-binding protein (hFABP) could be a marker for pathology in blood vessels supplying the brain. Some vascular markers also show potential as markers of vascular injury in AD: von Willebrand factor (vWF) and monokine induced by γ-interferon (MIG, also known as CXCL-9).
Concentrations of TAR-DNA binding protein (TDP-43) in the brain and plasma and serum indicate, even contribute to, inflammation, mitochondrial dysfunction, and neuronal/synaptic injury in AD.
Neuroimaging techniques reveal structural, functional, and diffusion-related activities of the neurons. To identify them, markers are tracked in images obtained. Each marker is determined with the activity and biochemistry of the group of/individual neurons being studied.
Structural MRI will show location and severity of atrophy which can be identified in grey scale images by applying programs that create analogous color grading.
Functional MRI relies on blood oxygenation level dependent (BOLD) signal which reflects changes in blood oxygenation levels in response to neural activity.
Diffusion weighted imaging (DWI) focuses on diffusion of water molecules. A tensor model is applied to images obtained from DWI. The diffusion tensor imaging (DTI) metrics thus obtained help in studying connectivity through structural integrity of white matter tracts.
Tractography involves 3-D reconstruction of white matter as observed in DWI, which provides a more detailed look into a patient’s neural networks.
In positron emission tomography (PET), markers are identified and labelled so their features or functions can be traced during this procedure to obtain a resulting PET scan. The imaging procedure is named according to its marker: amyloid-PET, tau-PET, FDG-PET, inflammation-PET, receptor-PET.
FDA approved drugs Galantamine, Rivastigmine, and Donepezil alleviate symptoms such as memory loss and confusion in mild to moderate AD, although their effects seem to be negligible. They also cause nausea and vomiting as side effects and are not suitable for every patient. Recently approved drugs, Aducanumab and Lecanemab focus on removing accumulated amyloid. Their effectiveness is still doubted on the basis of studies finding that targeting amyloid has little to do with curbing the actual progression of the disease.
bibliography -
Tarawneh R. Biomarkers: our path towards a cure for Alzheimer disease. Biomarker insights. 2020 Nov;15:1177271920976367.
Cavedo E, Lista S, Khachaturian Z, Aisen P, Amouyel P, Herholz K, Jack Jr CR, Sperling R, Cummings J, Blennow K, O’Bryant S. The road ahead to cure Alzheimer’s disease: development of biological markers and neuroimaging methods for prevention trials across all stages and target populations. The journal of prevention of Alzheimer's disease. 2014 Dec;1(3):181.
Medications for Alzheimer's Disease Stanford Healthcare. Accessed 21-04-2023.
#aging#alzheimers#dementia#neuroscience#clinical medicine#diagnostics#diagnosis#brain injuries#neurological conditions#neurodegenerative disorders#neurodegeneration#neurons#neurology#brain research#neurological disease#neurological disorders and injuries#chronic illness#neuroinflammation#neuroimaging#science#science side of tumblr#research paper#academic writing
7 notes
·
View notes
Text
Role of dementia screening – We do not routinely screen asymptomatic older adults for cognitive impairment. However, cognitive difficulty observed in a patient encounter, and family or patient concerns for memory and cognition, require thorough evaluation. (See 'Screening for dementia' above.)
●History – Family members or other informants who know the patient well are invaluable resources for providing an adequate history of cognitive and behavioral changes. A drug history is particularly important, as many medications may impact cognition in older patients. (See 'History' above.)
●Cognitive and neurologic examination – Adequate time should be arranged for a full assessment of cognitive function, followed by a complete physical examination, including neurologic examination.
A brief screening assessment such as the Mini-Mental State Examination (MMSE) or Montreal Cognitive Assessment (MoCA) is useful and may be sufficient cognitive assessment in some patients. (See 'Cognitive testing' above and 'Physical examination' above.)
●Depression screening – Depression is a common treatable comorbidity that may also masquerade as dementia. (See 'Screening for depression' above and 'Dementia mimics' above.)
●Laboratory testing – Screening for B12 deficiency and hypothyroidism is recommended for patients being evaluated for dementia. Other laboratory testing is performed selectively. (See 'Laboratory testing' above.)
Genetic testing for the apolipoprotein E epsilon 4 allele is not currently recommended, nor is genetic testing for other potential causes of dementia. (See 'Genetic testing' above.)
●Neuroimaging – A noncontrast MRI or head CT should be considered in the initial evaluation of all patients with dementia.
The purposes of structural imaging are to detect treatable causes of dementia and to differentiate among various dementia subtypes. (See 'Neuroimaging' above.)
●Diagnosis and ongoing assessment – History and examination along with limited laboratory testing and a neuroimaging study are usually sufficient to make a diagnosis of dementia and in most cases to identify a presumptive cause.
As most causes of dementia are progressive, a follow-up visit after several months can often confirm the original diagnosis, can offer ongoing treatment and monitoring, and, in some cases, may cause a clinician to reconsider the original diagnosis if the progression does not occur or is atypical. (See 'Criteria for dementia' above and 'Dementia syndromes' above.)
●Role of specialized testing – Other tests (neuropsychological assessment, advanced neuroimaging techniques, lumbar puncture [LP], and, rarely, brain biopsy) are performed in selected patients (such as those who are younger or have a rapidly progressive course) and when the presentation is otherwise atypical. (See "Early-onset dementia in adults" and 'Specialized testing in selected patients' above and "Creutzfeldt-Jakob disease", section on 'Differential diagnosis'.)
2 notes
·
View notes
Note
hi, I saw on a post (the one discussing gender) that you said you’re a neuroscientist. if you don’t mind me asking, what do you do as one? i’m interested in the field.
thank you!!!
@colombianlitproject absolutely, no problem!!
I studied visual neuroscience and did a bunch of work on how human brains process visual information, which is more widely applicable than you think; whilst I was doing all the theoretical research around mechanisms and neural patterns, the lab I was in very succesfully turned that research into a new method for detecting cancer from bodyscans. I followed those projects up with a bit of work into early detection of Alzheimers. All of my projects involved a mix of neuroimaging techniques (fMRI, EEG, and TMS, the latter of which is wild -- "hey, you, let's give you temporary brain lesions for science") and behavioural experiments. I particularly recommend "The Man Who Mistook His Wife For A Hat" by Oliver Sacks as a good all-purpose intro to vision neuroscience
7 notes
·
View notes
Text
The creative process of painting can be a complex interplay of various brain regions and cognitive functions. While the exact brain activity can vary from artist to artist, here are some general insights into what happens in the brain when artists paint:
1. Frontal Cortex Engagement: The frontal cortex, particularly the prefrontal cortex, is involved in planning, decision-making, and creativity. Artists use this part of the brain to conceptualize their artwork, plan the composition, and make creative choices.
2. Motor Skills and Coordination: Painting involves precise motor skills and hand-eye coordination. The brain's motor cortex and cerebellum are active as artists control their brushstrokes, apply paint, and manipulate tools.
3. Visual Processing: The occipital lobe, responsible for visual processing, is highly active when artists observe their subject matter or visualize their artistic vision. This region helps them perceive shapes, colors, and details.
4. Emotional and Expressive Elements: The limbic system, associated with emotions, can be engaged during the creative process. Artists often draw upon their emotions to infuse their work with feeling and expression.
5. Memory and Association: The brain's memory centers, such as the hippocampus, can be involved when artists recall references, past experiences, or techniques they've learned.
6. Reward System Activation: Creating art can activate the brain's reward system, including the release of dopamine, which can lead to feelings of satisfaction and pleasure when artists achieve their creative goals.
7. Flow State: Many artists experience a "flow state" when deeply engrossed in their work. This state is associated with increased activity in the prefrontal cortex and reduced activity in the part of the brain responsible for self-criticism, leading to a sense of timelessness and immersion in the creative process.
8. Problem-Solving: Artists often encounter challenges during painting, such as how to depict a particular texture or achieve a desired effect. This engages areas of the brain involved in problem-solving and creativity.
It's important to note that the brain's activity during painting can vary widely depending on the artist's style, subject matter, and personal approach to the creative process. Additionally, neuroimaging studies on artists are ongoing, and our understanding of the neural processes involved in art creation continues to evolve.
1 note
·
View note
Text
Neurology Treatment in India
Neurology Treatment
What is Neurology?
Neurology is a branch of medicine that deals with studying and treating disorders of the nervous system. It is a complex, sophisticated system of cells and fibers that controls every function of the human body. With a deep-rooted foundation in both science and clinical practice, neurology plays a significant role in decoding the nervous system and addressing multiple conditions that afflict it.
The nervous system is broadly divided into:
Central Nervous System (CNS):It comprises the brain and spinal cord.
Peripheral Nervous System (PNS):It comprises the nerves that extend throughout the body. It also includes eyes, ears, skin, and other sensory receptors.
Specialists in Neurology
Various specialists are trained to diagnose, treat, and manage nervous system disorders. The key specialists in the field of neurology include:
Neurologists:Neurologists diagnose and treat disorders of the nervous system. They undergo specialized training in neurology, including residency programs focusing on evaluating and managing various neurological disorders.
Neurosurgeons:Neurosurgeons specialize in the surgical treatment of conditions of the nervous system. They perform surgeries for conditions such as brain tumors, traumatic brain injuries, spinal cord injuries, and movement disorders.
Neurointensivists:Neurointensivists are physicians who provide emergency care for patients admitted to the neurology ICU for life-threatening neurological conditions.
Neuropsychologists:Neuropsychologists assess and treat cognitive, emotional, and behavioral disorders associated with neurological conditions. They evaluate memory, language, and other elements of brain function and help develop individualized treatment modules.
Neuroscientists:Neuroscientists study the structure, function, and development of the nervous system and investigate the mechanisms of neurological disorders. They use research techniques like neuroimaging, electrophysiology, and genetic studies to develop new treatments for neurological conditions.
Neurology Technologists:Neurology technologists are trained professionals who perform diagnostic procedures to evaluate the function of the nervous system. They specialize in neurodiagnostic testing, such as electroencephalography (EEG), nerve conduction studies (NCS), electromyography (EMG), and evoked potentials (EP), to help diagnose and monitor neurological conditions.
What Conditions Do Neurologists Treat?
Neurologists help treat a diverse array of neurological conditions, each presenting its unique challenges and manifestations.
These conditions include:
Stroke:Neurologists treat stroke, a condition when the blood flow to the brain is disrupted, through evaluation of symptoms and clot-bursting medication.
Epilepsy:Treatment of epilepsy (a neurological disorder characterized by seizures) includes antiepileptic medications, lifestyle changes, and surgical interventions.
Headaches:Neurologists specialize in headache disorders, such as migraines and cluster headaches. The treatment includes clinical evaluation and customized treatment.
Movement Disorders:Neurologists treat movement disorders such as Parkinson’s disease, essential tremor, dystonia, and Huntington’s disease. The treatment includes medications, physical therapy, or surgical interventions.
Multiple Sclerosis (MS):Neurologists treat multiple sclerosis, an autoimmune disorder, by prescribing therapies to reduce disease activity and progression and manage symptoms.
Alzheimer’s Disease and Dementia:Neurologists treat neurodegenerative disorders, such as Alzheimer’s disease, vascular dementia, and frontotemporal dementia, with medicines and collaboration with other healthcare providers.
Peripheral Neuropathy:Neurologists evaluate and treat peripheral neuropathy, a condition where peripheral nerves are damaged through nerve conduction studies and electromyography, medications, and lifestyle modifications.
Neuromuscular Disorders:Neurologists treat neuromuscular disorders, such as muscular dystrophy, myasthenia gravis, and amyotrophic lateral sclerosis (ALS), with medications, physical therapy, and coordination with specialists.
Neurological Infections and Inflammatory Disorders:Infections of the nervous system, such as meningitis and encephalitis, and inflammatory conditions, like multiple sclerosis and Guillain-Barré syndrome, are treated through medicines.
Neurogenetic Disorders:Neurologists treat genetic neurological disorders, such as Huntington’s disease, muscular dystrophy, and hereditary neuropathies, via genetic counseling, genetic testing, and personalized treatment.
Diagnostic Modalities in Neurology
Neurologists begin the diagnostic process by recording a detailed medical and family history, evaluation of symptoms, and a physical examination, which includes:
Coordination, balance, reflexes, and gait
Muscle strength
Vision, hearing, and speech
Sense of touch
Common neurologic tests include:
Neuroimaging:Neuroimaging techniques visualize the structures of the brain and spinal cord and help detect abnormalities. These techniques include:
Magnetic Resonance Imaging (MRI): MRI uses magnetic fields and radio waves to produce detailed images of the brain and spinal cord.
Computed Tomography (CT) Scan: CT scans use X-rays to create cross-sectional images of the brain and spinal cord.
Positron Emission Tomography (PET) Scan: PET scans use radioactive tracers to measure brain activity and metabolism.
Single Photon Emission Computed Tomography (SPECT) Scan: SPECT scans also use radioactive tracers to measure brain blood flow and activity.
Electroencephalography (EEG):EEG measures electrical activity in the brain via electrodes placed on the scalp.
Nerve Conduction Studies (NCS) and Electromyography (EMG):NCS and EMG are tests used to evaluate the function of peripheral nerves and muscles.
Cerebrospinal Fluid (CSF) Analysis: CSF analysis involves obtaining a sample of cerebrospinal fluid to analyze it for abnormalities.
Neuropsychological Testing:Neuropsychological testing involves assessing cognitive function, memory, language, and other aspects of brain function.
Genetic Testing:Genetic testing is used in certain neurological disorders with a known genetic component to identify specific genetic mutations.
Evoked Potentials:These tests measure how fast electrical signals in the brain respond to sensory stimuli.
Angiography:Angiography detects if blood vessels in the brain, head, or neck are blocked or damaged. It is also used to detect blood clots.
Myelography:This test helps diagnose spinal cord tumors, herniated disks, and fractures.
Thermography:This test monitors changes in the temperature of your body or a particular organ. It helps examine peripheral nerve disorders, nerve root compression, and pain syndromes.
Polysomnogram:This test records the activities of the brain and the body during sleep. It diagnoses several sleep disorders. https://health-gates.com/neurology-treatment-in-india/
0 notes
Text
Tracking the Recovery of a Mild Traumatic Brain Injury Patient utilizing a 60-s Combined Functional Near-Infrared Spectroscopy and Psychomotor Testing Approach: A Case Study by Dr. Cory M. Smith in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
Identifying and tracking the recovery of patients with mild traumatic brain injuries (mTBI) has remained elusive due to the lack of non-invasive, objective neuroimaging techniques. The purpose of this case study was to provide a proof of concept for performing a combined functional near-infrared spectroscopy (fNIRS) and 60-s psychomotor vigilance testing (60-s PVT) that can identify and track the recovery of a patient with a mTBI. The patient was a 19-year-old female acrobatics and tumbling athlete who was kicked in the left temple by a teammate. Video footage of the injury was utilized to determine the region of impact and weekly fNIRS and 60-s PVT assessments were performed throughout the 10 weeks of recovery. The patient was cleared for activity based upon symptoms at week 7; however, the patient reported increased symptomology during weeks 7 and 8 following exercise. Our fNIRS neuroimaging technique was able to detect the systemic physiological responses associated with mitochondrial dysregulation and oxygen extraction fraction at weeks 1 to 8. Based on our findings, the patient remained injured at week 8, and that the physical activity performed at weeks 7 and 8 may have regressed recovery and induced additional dysfunction resulting in increased recovery time. In conclusion, we were able to identify and track the recovery of our patient with a mTBI using our non-invasive combined fNIRS and 60-s PVT approach. Results provided real time physiological responses associated with the injury throughout the recovery process.
Introduction: Identifying and tracking the recovery of patients with mild traumatic brain injuries (mTBI) has remained elusive due to the lack of non-invasive, objective neuroimaging techniques and that each injury may be unique in its severity, signs and symptoms.1 This present case provides an overview of a novel utilization of functional near-infrared spectroscopy (fNIRS) combined with a 60-s psychomotor vigilance test (60-s PVT) for the monitoring of a patient with a severe mTBI. fNIRS examines the hemodynamic responses in brain tissue by using specific wavelength light absorbance rates to quantify the oxygenated (O2Hb), deoxygenated (HHb), and total hemoglobin (tHb) within a targeted region of the brain.2–4 mTBI’s with associated cerebral damage (e.g., cerebral hemorrhage), require increased nutrient exchange to heal causing greater blood flow to the damaged region when under load.5–8 Furthermore, following a mTBI, moderate to severe cognitive tasks are often contraindicated as they induce a worsening of symptoms.9–11 As a result, complex screening tools may induce greater severity scores immediately following a mTBI or place the patient at increased risk of adverse events such as headaches, nausea, or malaise.12,13 The 60-s PVT utilized in this case study mildly stimulates the major regions of the brain through visual, motor, and cognitive stimuli to induce a hemodynamic shift over the damaged region which would otherwise be undetectable.14,15 To our knowledge this is the longest published tracking of the recovery of a patient with an mTBI using fNIRS following injury onset.16–18 In addition, the present case is novel in that neuroimaging began within 72-hr from the onset of injury, weekly tracking was performed, and the exact time and location of injury was established through video footage of the injury’s occurrence which allowed for precise neuroimaging and tracking of the patient during their recovery.
Our fNIRS technique is ideal for real-world monitoring as it is not as impacted by movement or environmental conditions as the traditionally used electroencephalograms (EEG). In addition, fNIRS is more portable than functional magnetic resonance imagining (fMRI) techniques which are costly and cannot be performed on the field during sporting events.5,19 The fNIRS technology has been shown to have greater spatial resolution than EEG, similar to that of fMRI.2,4,20,21 In addition, fNIRS has slightly lower temporal resolution than EEG, but much greater than that of fMRI. Thus, the portability and unique blend of spatial and temporal neuroimaging resolution makes the use of fNIRS ideal for identifying and tracking mTBI in real-world environments.2,4,20,21 However, previous studies using fNIRS have shown mixed results in its ability to identify mTBI’s.17,18,22–24 We hypothesized that these conflicting results were the result of methodological approaches that included unoptimized post-processing neuroimaging data fusion and mTBI-specific analysis algorithms for regional injury determinations.17,25,26 Furthermore, other fNIRS studies have utilized O2Hb hemoglobin measures in their statistical analyses. However, many studies have reported HHb and tHb as more robust in detecting alterations in cognitive load and neuroplastic changes.3,18,27,28 Therefore, the purpose of this case study was to provide a proof of concept for performing weekly fNIRS (O2Hb, HHb, and tHb) and 60-s PVT monitoring of a unique mTBI patient suffering from severe symptoms.
Methods
Patient: The patient was a 19-year-old female acrobatics and tumbling athlete. Prior to enrollment in college, the patient had a history of concussions with prolonged recovery periods. During a synchronized tumbling pass the patient was kicked in the left temple by a teammate, followed by hitting her forehead on the mat during landing. Immediately following the impact, the patient presented with signs and symptoms (e.g., headache, altered mental status) warranting a referral to an emergency department (ED) for further evaluation. At the ED a head computerized tomography (CT) scan revealed that the patient was suffering from a severe mTBI. However, results of the CT scan did not identify a skull fracture or hemorrhaging. An assessment completed by the school’s medical staff after being released from the hospital found the patient was suffering from headaches, visual disturbances, and disorientation. Further, neurocognitive testing revealed substantial deficits in processing speed, reaction time, and executive functioning. The patient was then re-evaluated the day after the initial injury where she reported headaches, disorientation, and fatigue.
In total, the patient was symptomatic for 10 weeks following injury. Video footage of the injury was utilized to determine the region of impact and weekly neuroimaging assessments were performed throughout the 10 weeks. Recovery from the mTBI during this time was marked by a slow and steady decrease in symptoms (e.g., headaches, difficulty sleeping, sensitivity to light/noise, vision issues, dysphasia, emotional disturbances). The patient did not return to any physical activity until seven weeks after the initial injury. However, her activity was early threshold aerobic exercise primarily consisting of cycling while being monitored for increases in reported mTBI signs and symptoms. Due to the prolonged recovery and previous concussion history, the medical team and patient decided that further participation in the sport was not feasible. Thus, the patient medically disqualified from further participation. This project was approved by the institutions IRB (Approval ID#: 2012044), is aligned with the Declaration of Helsinki, and the patient’s consent was provided to publish the data within this case study. This study.29
Functional Near-Infrared Spectroscopy Signal Analysis:
The overall fNIRS-derived hemodynamic responses were monitored each week for 10 weeks of the patient’s recovery beginning after the onset of the injury. The location of placement for the fNIRS sensors were determined based on video footage of the injury and athletic trainers present at the time of injury. fNIRS hemodynamic monitoring were collected over left (Injured) and right (Control) superior temporal region of the patients’ head using a 4x1 optode to receiver layout which was secured to the head with a full head neoprene cap, chin strap, and pressure relief system to maintain sensor placement (OxyMon MKII, Artinis Medical Systems, Einstinweg, Netherlands). The centerpoint of the 4x1 sensor grid was the location of impact and the identical location on the opposing side of the head. Each of the 4 optodes on each region of the head were sampled at 10 Hz for each of the 762 and 848 nm wavelengths utilized to monitor the hemodynamic responses. Each wavelength penetrates through the skull and into the cerebral cortex at a distance of ~2.5 cm. The thickness of the skull was estimated based on the patients age and utilized to calculate a correction factor for the differential pathlength factor (DPF) caused by the refraction of the skull fNIRS signals were performed by filtering for Mayer waves, respiration, and heart pulsation by examining the power density spectrum prior to the continuous wavelet (CWT) analysis. A Morlet Wavelet was utilized for the CWT transform using time-step coefficients without any overlap was then performed. The Wavelet coefficients were determined from the culmination of all the CWT data over each weeks 60-s PVT test and was used to further analyze the CWT Multiscale Peak Detection to quantify the amplitude of each CWT. This analysis allowed for the calculation of fNIRSamp values for O2Hbamp, HHbamp, and tHbamp. Together, these metrics provide the regional cerebral blood flow (tHbamp), metabolic stress (HHbamp), and available oxygen (O2Hbamp) in the Control and Injured regions of the brain. Each hemisphere’s 4 optode grid channels were then summated to provide an individual activation level for each locations site of interest during each week’s 60-s PVT.
Three exploratory t-tests were performed on the mean Control and Injured tHbamp, HHbamp, and O2Hbamp measures, collapsed across the 10 weeks for sufficient data points, to determine the gross differences in hemodynamics throughout the 60-s PVT.
Psychomotor Vigilance Test:
A 60-s PVT was performed each week while wearing the fNIRS neuroimaging sensor on the injured and control regions of the patient’s brain. The 60-s PVT test was performed on a touch screen tablet (iPad 10.2in 9th generation, Apple, Cupertino, CA) using the Research Buddies software (Research Buddies Version 1.53). During to quantify injury severity as it has been suggested that a PVT has difficultly determining differences in patient injury severity scores.14 In a previous study31 that examined healthy, military non-TBI patients suffering from extreme hypoxemia and physical fatigue reported an average 60-s PVT time ranging from 380-450-ms. Taken together, the findings of these previous studies suggest that a 60-s PVT can help to identify deficits and potentially severity, but the 60-s PVT alone is unable determine if an mTBI occurred and its injury severity. However, the addition of our fNIRS neuroimaging technique coupled with the 60-s PVT results may allow for a methodology of tracking the occurrence and severity of mTBI patients.
Functional Near-Infrared Spectroscopy: Neuroimaging:
Neuroimaging the contralateral side of the brain as a Control was effective for identifying the hemodynamic and metabolic differences from the Injured region of the brain in our patient as a pre-injury image was unavailable. The relatively consistent tHbamp, HHbamp, and O2Hbamp metrics across the 10 weeks for the Control compared to the Injured side reflects a low neurophysiological load placed on the Control region of the brain typical of a non-mTBI patient during the 60-s PVT (Figure 4).2,26 Furthermore, Figure 5 illustrates the similarities in the neurophysiological load placed on the Control and Injured regions of the brain at the initial 0 to 10-s of the 60-s PVT, however, after 30-s of load a greater hemodynamic and metabolic responses occurred in the Injured but not the Control region of the brain. Thus, the 60-s PVT load placed on the brain was minimal enough to not impact the Control region of the brain while sufficient at stimulating a response from the Injured region of the brain. Therefore, the utilization of a Control region was effective and allowed us to develop a target recovery threshold for the Injured region of the brain to match the tHbamp, HHbamp, and O2Hbamp of the Control region. The combined tHbamp, HHbamp, and O2Hbamp pattern of responses throughout the 10 weeks of recovery indicated maintenance of the patients Oxygen Extraction Fraction (OEF) in the Injured region of the brain. 32 The HHbamp and O2Hbamp ratio remained relatively constant in the Injured region of the brain with a concomitant increase in tHbamp which suggested that greater oxygenation utilization was required in the Injured region of the brain compared to the Control (Figure 4). The overall increased blood flow to the Injured region and increased metabolic demand, as indicated by the greater HHbamp, likely aimed to offset the mTBI associated Ca2+ overload within the patient. Increasing of the patients overall regional blood flow (tHbamp) to the Injured region may reflect a protective mechanism to avoid the catabolic effects of a Ca2+-induced intracellular dysregulation that has been shown to result in the overproduction of free radicals, activation of cell death signaling pathways and stimulation of inflammatory responses.33–35 That is, the fNIRS responses captured throughout the recovery of this patient tracked with the expected systemic physiological responses associated with the maintenance of OEF. Furthermore, it has been well established that mTBI’s result in mitochondrial dysregulation which result in a greater hemodynamic shift to the injured region of the brain to provide sufficient oxygen, dilution, and clearance rates for the metabolic byproducts.33,34 It is hypothesized that the combined mitochondrial dysregulation induced hemodynamic shift was likely the driving factor for the increased metabolic stress (HHbamp) while OEF further stimulated a greater hemodynamic flow to the Injured region of the brain to avoid further injury associated with a buildup of metabolic byproducts. The combined regional cerebral blood flow regulation pattern (tHbamp) and increased metabolic demand captured in this patient indicated that the damage to the patient’s brain was detectable using our fNIRS approach. Furthermore, the combined utilization of our CWT tHbamp, HHbamp, and O2Hbamp methodology allowed for identification of the hemodynamic shifts associated with the injury and increased load induced by the 60-s PVT.
In our patient, all fNIRS metrics that were elevated from weeks 1 to 8 improved to within Control values at week 9 and remained at the Control levels at week 10 (Figure 4). The tracked improvements in all fNIRS measures suggest that this patient’s recovery became physiologically improved at week 9, however, the patient reported minimal symptomology at rest at week 7 which cleared the patient to begin light physical activity. During weeks 7 and 8 the patient reported increased symptomology when exercising which was her rate limiter to perform physical activity. Considering the onset of the symptomology due to exercise and the fNIRS detected hemodynamic shifts associated with mitochondrial dysregulation coupled with OEF, the patient may have been less symptomatic if exercise was resumed at week 9.32,34 Specifically, the improved fNIRS and 60-s PVT metrics at week 9 were closely aligned with the Control and expected reaction time values, respectively, suggesting that our fNIRS approach could track the physiological recovery in this patient (Figure 4). Early physical activity in patients with mTBI’s has been linked to increase metabolic byproduct accumulation, greater hemodynamic shifts, potential reduced recovery rates, and increased symptomology.32,34,36,37 Thus, the elevated tHbamp, HHbamp, and OxyHbamp values at week 8 suggest that the physical activity performed at weeks 7 and 8 may have regressed recovery and induced additional dysfunction, lengthening recovery time. Therefore, further development of this non-invasive neuroimaging approach will provide clinicians with a useful assessment tool to make more informed decisions on the rate of recovery and activity a patient may be prescribed.
Limitations: This was an exploratory case study performed on a single patient to examine the clinical feasibility of the fNIRS and 60-s PVT analysis approach which will need greater refinement and development prior to clinical adoption. We acknowledge that greater data from a larger population should be studied to make this technology useable when real-time accounts or video footage of the injury site is unavailable. Thus, data from this study should not be applied to a broader patient pool until further studies focusing on the refinement and application of this approach is completed. The data from this case study does provide the foundational information needed to replicate the study methodology and highlights the relevance to the clinical community aiming to develop non-invasive mTBI monitoring devices.
Conclusion: In conclusion, the 60-s PVT was capable of detecting deficits in our patient, however, the 60-s PVT alone was unable to determine injury severity. The addition of our fNIRS neuroimaging technique was able to detect the systemic physiological responses over the injured region of the brain that align with mitochondrial dysregulation induced hemodynamic shifts and increased metabolic stress (HHbamp). In addition, tHbamp and HHbamp identified OEF which further stimulated a greater hemodynamic flow to the Injured region of the brain to avoid a buildup of metabolic byproducts. The neuroimaging from the contralateral side of the brain was effective as a Control in our patient as a preinjury image was unavailable. Using the Injured and Control region neuroimaging, we determined the elevated tHbamp, HHbamp, and OxyHbamp values at week 8 suggest that the physical activity performed at weeks 7 and 8 may have regressed recovery and induced additional dysfunction, lengthening recovery time. Therefore, this case study showed that a combined 60-s fNIRS neuroimaging and PVT technique was capable of detecting the patients mTBI and tracked her recovery better than subjective assessments. Furthermore, the physiological data obtained through our non-invasive neuroimaging approach was able to identify the patient’s physiological response including potential mitochondrial dysregulation and OEF. Therefore, the physiological responses and recovery state capture in our patient indicates that the weekly assessments of a combined 60-s fNIRS and PVT approach could provide clinically relevant data on the recovery status and injury severity. Future research should focus on the development of fNIRS threshold values that can be utilized to better identify the severity of a mTBI and its associated physiological responses in a large sample of mTBI patients.
Acknowledgements: We would like to thank the patient for their time and willingness to volunteer for this study. In addition, we would like to thank Baylor Athletics Executive Senior Associate Athletic Director Kenny Boyd, Associate Athletic Director Carrie Rubertino Shearer, and all the athletic trainers who assisted in this project.
#Mild Traumatic Brain Injury#Near-Infrared Spectroscopy#Psychomotor Testing Approach#Journal of Clinical Case Reports Medical Images and Health Sciences#JCRMHS#Journal of Clinical Case Reports Medical Images and Health Sciences (JCRMHS)| ISSN: 2832-1286
0 notes
Text
Best Neurology Doctor in Hyderabad – Expert Care at TX Hospitals

When it comes to your neurological health, choosing the right doctor is crucial. Neurological disorders can affect the brain, spinal cord, and nerves, requiring expert attention and precision care. At TX Hospitals, we are proud to have a team of the best neurology doctors in Hyderabad who specialize in diagnosing and treating a wide range of neurological conditions with compassion and advanced medical techniques.
If you're searching for the best neurology doctor in Hyderabad, TX Hospitals offers the expertise and state-of-the-art facilities you need for accurate diagnosis and effective treatment.
Leading Neurology Experts at TX Hospitals
At TX Hospitals, we bring together some of the top neurology doctors in Hyderabad. Our specialists are highly experienced in managing complex neurological cases, ensuring the best outcomes for patients.
1. Dr. Naresh Kumar Gajjala – Leading Neurosurgery Specialist
Qualifications: MBBS, MS, MCh (Neurosurgery)
Dr. Naresh Kumar Gajjala is one of the most trusted neurosurgeons in Hyderabad. He specializes in treating brain and spinal disorders with advanced neurosurgical techniques.
2. Dr. B. Dinesh Kumar – Expert Neurologist
Qualifications: MBBS, MD (Paediatrics), DM (Neurology)
With extensive experience in treating neurological conditions in adults and children, Dr. B. Dinesh Kumar focuses on conditions such as epilepsy, migraines, and developmental disorders.
3. Dr. Srinivas Thankari – Renowned Neurosurgeon
Qualifications: MBBS, MS, MCh (Neurosurgery)
Dr. Srinivas Thankari is a leading expert in neurosurgery, known for his precision in performing complex surgeries for brain and spinal conditions.
4. Dr. Rakesh Reddy – Neuro Physician
Qualifications: MBBS, MD, DM (Neurology)
Dr. Rakesh Reddy specializes in treating chronic neurological disorders, including Parkinson’s disease, multiple sclerosis, and movement disorders.
5. Dr. Gouthami Priya Darshini – Neurology Specialist
Qualifications: MBBS, MD, DM, DNB (Neurology)
Dr. Gouthami Priya Darshini is skilled in diagnosing and managing conditions such as stroke, migraines, and neurodegenerative diseases.
Why Choose TX Hospitals for Neurological Care?
At TX Hospitals, we are committed to providing world-class neurological care. Here’s why we are the preferred choice for patients in Hyderabad:
Experienced Neurology Doctors: Our team includes the best neurology doctors in Hyderabad with years of experience in diagnosing and treating complex neurological conditions.
Comprehensive Neurological Services: From consultations and diagnostic evaluations to advanced treatments and surgeries, we offer holistic care for all neurological needs.
State-of-the-Art Technology: TX Hospitals is equipped with cutting-edge medical technology, including advanced neuroimaging and diagnostic tools for precise treatment.
Patient-Centric Approach: We believe in delivering compassionate care, ensuring our patients feel comfortable and informed throughout their treatment journey.
Affordable and Accessible Care: Quality healthcare doesn’t have to come with a high price tag. At TX Hospitals, we provide affordable treatment options without compromising on quality.
Neurological Conditions We Treat
Our expert neurology doctors at TX Hospitals specialize in treating a variety of conditions, including:
Stroke and transient ischemic attacks (TIA)
Epilepsy and seizure disorders
Migraines and chronic headaches
Parkinson’s disease and movement disorders
Multiple sclerosis and autoimmune neurological conditions
Neuropathies and nerve injuries
Brain and spinal cord tumors
Neurodegenerative diseases such as Alzheimer’s and dementia
Advanced Facilities for Neurological Care
At TX Hospitals, we leverage the latest advancements in medical science to deliver precise and effective treatments. Our facilities include:
MRI and CT Scans: For detailed imaging of the brain and spinal cord.
Neuro Electrophysiology Labs: To evaluate nerve and muscle function.
ICU for Neurological Emergencies: Round-the-clock critical care for strokes, traumatic brain injuries, and other emergencies.
Rehabilitation Programs: Post-treatment support to help patients regain functionality and improve their quality of life.
Book an Appointment with the Best Neurology Doctor in Hyderabad
If you or your loved one is experiencing neurological symptoms, don’t delay seeking expert care. At TX Hospitals, our neurology doctors are dedicated to providing the best treatment and support for a healthier future.
Call now: 9089 48 9089 to book your appointment with the best neurology doctor in Hyderabad. Take the first step toward recovery and experience world-class care at TX Hospitals.
Your health and well-being are our priorities at TX Hospitals. Trust us to provide you with the expertise, care, and compassion you deserve.
#best neurologist in hyderabad#neurologist in hyderabad#top neurologist in hyderabad#neurologist specialist in hyderabad#neurologist doctor in hyderabad
0 notes
Text
Top Hospital for Brain and Spine Surgery in India—Dr. Rao’s
Non-Invasive Treatments for Neurological Conditions at Dr. Rao’s Hospital When it comes to managing neurological disorders, many patients often seek non-invasive treatments before considering surgery. Non-invasive techniques are beneficial for patients who want to avoid the risks and recovery time associated with traditional surgery. At Dr. Rao’s Hospital, patients benefit from a variety of non-invasive and minimally invasive treatments designed to manage everything from spinal issues to brain disorders. These procedures include methods like stereotactic radiosurgery, advanced neuroimaging, and targeted therapy to treat tumors and other neurological conditions without the need for traditional open surgery. Dr. Rao, a famous neurosurgeon in India, is highly skilled in non-invasive and invasive techniques, ensuring each patient gets a customized treatment plan tailored to their unique needs.
Best Surgical Hospital in India: Dr. Rao’s Hospital, Guntur Recognized as one of the best surgical hospitals in India, Dr. Rao’s Hospital stands out due to its focus on cutting-edge technology and expert care. With state-of-the-art facilities, the hospital specializes in neurosurgery, spinal surgery, and endovascular treatments. What sets Dr. Rao’s Hospital apart is its comprehensive care, which spans from initial diagnosis to rehabilitation, all in one facility. Under the leadership of Dr. Mohana Rao Patibandla, the hospital has earned a reputation for delivering outstanding results, particularly in complex neurological surgeries. Patients from India and across the globe, including those seeking affordable medical tourism, come to Dr. Rao’s Hospital for world-class medical care at a fraction of the cost compared to other countries.
Surgeon Medical Doctor: Expertise in Neurological and Spine Surgery A surgeon medical doctor like Dr. Rao is more than just a medicine practitioner; he is a pioneer in neurosurgery and spine surgery. Trained in India and internationally, Dr. Rao brings years of expertise and a compassionate approach to each case. His extensive training allows him to offer patients various surgical and non-surgical solutions. Whether you need a specialist in scoliosis or treatment for a brain tumor, Dr. Rao’s approach is patient-centered, focusing on the least invasive yet most effective treatment options. He always aims to minimize complications and maximize recovery, ensuring patients have the best possible outcomes.
Pain After Operation: Managing Post-Surgery Recovery One of the main concerns for patients undergoing neurological surgery is pain after the operation. Dr. Rao’s Hospital is known for its excellent post-operative care, which includes advanced pain management strategies. Depending on the patient’s condition, these strategies range from medications to physical therapy and alternative treatments like acupuncture or chiropractic care. Minimally invasive surgery, which Dr. Rao often recommends, significantly reduces recovery times and post-surgical pain compared to traditional open surgery. This approach ensures that patients experience less discomfort and return to their daily lives faster.
Famous Neurosurgeon in India: Dr. Mohana Rao Patibandla Dr. Mohana Rao Patibandla is widely regarded as one of the most famous neurosurgeons in India. His extensive experience and cutting-edge surgical techniques make him the go-to expert for complex cases. Dr. Rao has performed thousands of successful surgeries, many of which involved high-risk conditions like brain tumors, spinal disorders, and aneurysms. His expertise has earned him numerous national and international accolades, and his commitment to patient care is unmatched. Whether treating international patients through medical tourism in India or handling difficult neurosurgical cases domestically, Dr. Rao consistently delivers excellent outcomes.
Best Hospital for Spine Surgery in India Regarding finding the best hospital for spine surgery, Dr. Rao’s Hospital leads the way in India. The hospital’s spine surgery department is renowned for its successful track record in treating complex spinal disorders, including scoliosis, herniated discs, and spinal stenosis. Whether the patient requires non-invasive surgery or a more involved procedure like a spinal fusion, the hospital offers a comprehensive approach that includes pre-operative assessments, advanced imaging, and post-operative rehabilitation. Dr. Rao’s team consists of some of the best spine specialists in the country, ensuring that patients receive world-class care.
Best Neurosurgery Hospitals: Dr. Rao’s Hospital, Guntur As one of the best neurosurgery hospitals in India, Dr. Rao’s Hospital is recognized for its innovative approach to treating brain and spinal conditions. With cutting-edge technology like neuronavigation systems, intraoperative MRIs, and the latest surgical instruments, the hospital can handle even the most complicated neurosurgical procedures. Dr. Rao’s Hospital is also a hub for research and education, consistently updating its techniques to reflect the latest advancements in neurosurgery.
Spine Neuro: Comprehensive Care for Spinal and Neurological Conditions Spine neuro refers to the intersection of spinal and neurological conditions, often requiring a multi-disciplinary approach for effective treatment. At Dr. Rao’s Hospital, the team of spine surgery and neurology experts work closely together to provide comprehensive care. Whether the patient needs surgery for a spinal tumor, a herniated disc, or degenerative spine disease, the hospital offers both surgical and non-surgical treatment options. Minimally invasive spine surgery, such as keyhole surgery, is a key offering that reduces recovery time and minimizes complications.
Neuro Surgery Procedures: Pioneering Techniques Dr. Rao’s Hospital is at the forefront of neuro surgery procedures, offering various innovative surgical treatments. From cervical discectomies to brain tumor resections and aneurysm repairs, the hospital is equipped to handle the most complex cases. The team’s expertise in minimally invasive techniques, including stereotactic radiosurgery, ensures that patients receive the most advanced care with the least downtime.
Specialist in Scoliosis Treatment As a specialist in scoliosis, Dr. Rao and his team at Dr. Rao’s Hospital offer a range of treatment options for patients suffering from this condition. Depending on the severity of the scoliosis, treatments may range from physical therapy and bracing to spinal fusion surgery. Dr. Rao’s expertise in spine surgery ensures that patients have access to the most effective and least invasive options.
Non-Invasive Surgery: The Future of Neurosurgical Care The rise of non-invasive surgery is transforming the field of neurosurgery, and Dr. Rao’s Hospital is at the forefront of this movement. Procedures like gamma knife radiosurgery, endovascular surgery, and stereotactic radiosurgery allow for the treatment of complex conditions like brain tumors and aneurysms without the need for traditional open surgery. These procedures significantly reduce the risk of complications and shorten recovery times, making them ideal for high-risk patients.
Best Brain Surgery Hospital: Dr. Rao’s Hospital, Guntur As the best brain surgery hospital in India, Dr. Rao’s Hospital has set a high standard for neurological care. The hospital offers state-of-the-art facilities and a team of specialists who are experts in treating brain tumors, aneurysms, and other neurological disorders. Whether you need a second opinion or are seeking complex neurosurgical care, Dr. Rao’s Hospital is the leading choice for patients looking for affordable medical tourism and high success rates.
Best Neurosurgeon Doctor in India: Dr. Mohana Rao Patibandla Dr. Rao’s credentials as the best neurosurgeon doctor in India are well-established. With numerous national and international awards, Dr. Rao’s expertise in traditional and minimally invasive surgery makes him a leader in the field. His domestic and international patients consistently report high satisfaction rates and excellent outcomes, particularly for brain and spine surgeries. Brain Hospital Chennai: Affordable and Effective Care For patients looking for the best neurological care in South India, Dr. Rao’s Hospital in Guntur rivals even the best brain hospital in Chennai. Offering similar, if not better, outcomes with more affordable treatment options, Dr. Rao’s Hospital is a preferred choice for both Indian and international patients. The hospital’s focus on minimally invasive neurosurgery and medical tourism in India makes it an excellent option for those looking for world-class care without the prohibitive costs often associated with neurosurgical treatments.
Dr. Rao’s Hospital: Your Destination for World-Class Neurosurgical Care Dr. Rao’s Hospital is the best option in India for patients seeking top-tier neurological and spinal care. With cutting-edge technology, a highly skilled medical team led by Dr. Mohana Rao Patibandla, and a focus on invasive and non-invasive treatments, this hospital offers comprehensive care tailored to each patient’s needs. Whether you’re dealing with a complex brain tumor, spinal disorder, or vascular condition, Dr. Rao’s Hospital has the expertise and technology to ensure the best possible outcome.
Conclusion: If you’re seeking affordable, high-quality neurological care, consider Dr. Rao’s Hospital in Guntur. Here, advanced technology and expert hands meet to offer the best brain and spine care. The hospital’s dedication to patient-centered care and Dr. Rao’s expertise ensure that you’re in the best hands possible. Whether you’re looking for non-invasive surgery, spine surgery, or advanced treatment for brain disorders, Dr. Rao’s Hospital stands as one of the best neurosurgery centers in India and globally. Dr. Rao’s Contact Information: Phone: 9010056444, 9010057444 Email: [email protected] Address: Old Bank St, GV Thota, beside AK Biryani Point, Guntur, Andhra Pradesh 522001 Website: Dr. Rao’s Hospital

1 note
·
View note
Text
What You Need to Know About Cerebral Aneurysm Surgery in Hyderabad

Cerebral aneurysms are a serious medical condition where a weakened blood vessel in the brain bulges, creating the risk of rupture and life-threatening complications such as haemorrhagic stroke. For individuals diagnosed with this condition, timely medical intervention is critical, and Cerebral Aneurysm Surgery in Hyderabad, offers a potentially life-saving solution. Hyderabad, with its advanced medical infrastructure and renowned neurosurgeons, has emerged as a leading destination for this specialized treatment.
Understanding Cerebral Aneurysms
A cerebral aneurysm occurs when a blood vessel wall in the brain weakens, forming a balloon-like bulge. These aneurysms may go unnoticed until they rupture, leading to severe symptoms such as:
Sudden, intense headaches.
Blurred or double vision.
Nausea and vomiting.
Loss of consciousness in severe cases.
Early detection through imaging techniques like CT scans, MRIs, or angiography can prevent severe outcomes and enable timely treatment.
Types of Cerebral Aneurysm Surgery
In Hyderabad, hospitals and neurosurgeons employ cutting-edge techniques to treat cerebral aneurysms. The two primary surgical approaches are:
Surgical Clipping
A procedure where the surgeon places a tiny metal clip at the base of the aneurysm to stop blood flow into it.
Performed through open brain surgery, it is effective for accessible aneurysms.
Endovascular Coiling
A minimally invasive procedure where a catheter is used to insert tiny coils into the aneurysm, promoting clotting and reducing rupture risk.
Suitable for aneurysms that are hard to access surgically.
Why Choose Hyderabad for Cerebral Aneurysm Surgery?
Hyderabad is home to some of India’s most reputed neurology and neurosurgery specialists. Here are key reasons why Hyderabad stands out for cerebral aneurysm treatment:
World-Class Hospitals: Facilities like Apollo Hospitals, Yashoda Hospitals, KIMS, and TX Hospitals are equipped with advanced neuroimaging and surgical tools.
Expert Neurosurgeons: Hyderabad boasts highly skilled neurosurgeons experienced in complex brain surgeries.
Affordable Care: Compared to global treatment costs, cerebral aneurysm surgery in Hyderabad offers excellent care at a fraction of the price.
Comprehensive Post-Operative Care: Patients receive holistic support, including neuro-rehabilitation and follow-up care.
Top Neurosurgeons for Cerebral Aneurysm Surgery in Hyderabad
Hyderabad is home to some of the most skilled and experienced neurosurgeons who specialize in treating cerebral aneurysms using advanced surgical techniques. Here's a list of top neurosurgeons and neurophysicians in Hyderabad renowned for their expertise in cerebral aneurysm surgery and treatment:
1. Dr. Naresh Kumar G
Qualifications: MBBS, MS, MCh (Neurosurgery)
Specialization: Neurosurgery with a focus on complex brain aneurysms and vascular neurosurgery.
Highlights: Known for his precision in surgical clipping and minimally invasive aneurysm procedures.
2. Dr. B. Dinesh Kumar
Qualifications: MBBS, MD (Paediatrics), DM (Neurology)
Specialization: Pediatric and adult neurology, with expertise in diagnosing and managing cerebral aneurysms.
Highlights: Offers comprehensive care for both ruptured and unruptured aneurysms.
3. Dr. Srinivas Thankari
Qualifications: MBBS, MS, MCh (Neurosurgery)
Specialization: Neurosurgery with significant experience in endovascular coiling and surgical clipping.
Highlights: Renowned for handling complex cases with high success rates.
4. Dr. Chandra Sekhar Tavisetty
Qualifications: MS (General Surgery), DNB, FNB, MCh (Neurosurgery)
Specialization: General and vascular neurosurgery, including advanced cerebral aneurysm treatments.
Highlights: Expertise in minimally invasive neurosurgical techniques.
5. Dr. Rakesh Reddy
Qualifications: MBBS, MD, DM (Neuro Physician)
Specialization: Neurophysiology and diagnostics, aiding in precise treatment planning for aneurysms.
Highlights: Focused on early diagnosis and non-surgical management of cerebral aneurysms.
6. Dr. Varun Kodam
Qualifications: MBBS, MD, DM (Neurology, NIMS)
Specialization: Neurology with a focus on cerebrovascular disorders, including aneurysms.
Highlights: Known for integrating modern imaging techniques to optimize surgical outcomes.
7. Dr. K. Amareshwar Rao
Qualifications: MBBS, MD, DM (Neurology)
Specialization: Neurology with an emphasis on post-operative care and long-term recovery from cerebral aneurysm surgeries.
Highlights: Expertise in rehabilitation and patient-centric care.
8. Dr. A. Goutami
Qualifications: MBBS, MD, DM, DNB (Neurology)
Specialization: Neurology with advanced training in managing vascular disorders like cerebral aneurysms.
Highlights: Provides personalized treatment plans tailored to patient needs.
Choosing the Right Specialist
Selecting a qualified neurosurgeon or neurologist is crucial for successful cerebral aneurysm surgery. Factors to consider include:
Experience in handling complex aneurysm cases.
Success rates with the chosen treatment method (clipping or coiling).
Availability of advanced facilities for diagnosis and surgery.
Preparing for Cerebral Aneurysm Surgery
Patients scheduled for cerebral aneurysm surgery must follow pre-operative guidelines to minimize risks. These include:
Avoiding blood-thinning medications as advised by your doctor.
Undergoing pre-surgical imaging tests for precise planning.
Discussing medical history and allergies with the surgeon.
What to Expect After Surgery
Recovery from cerebral aneurysm surgery depends on the procedure and the patient’s overall health. Here are general post-surgery guidelines:
Hospital stay of 3-10 days for observation and recovery.
Avoiding strenuous activities during the initial weeks.
Follow-up imaging to monitor the success of the surgery.
Rehabilitation therapies, including physiotherapy and speech therapy, may be recommended if neurological deficits occur.
Conclusion
Cerebral aneurysms require prompt medical attention, and surgery is often the best solution to prevent life-threatening complications. With its advanced healthcare infrastructure and top-notch specialists, Hyderabad is a trusted destination for Cerebral Aneurysm Surgery. Whether you’re a resident or considering traveling for treatment, Hyderabad offers a combination of expertise, technology, and compassionate care to ensure the best possible outcomes.
If you or a loved one are seeking expert care for a cerebral aneurysm, consult with Hyderabad’s leading neurosurgeons today to discuss the best treatment options.
Contact us at - 9089489089
Book an Appointment - https://txhospitals.in/book-an-appointment/
#"Cerebral Aneurysm Surgery in Hyderabad#Cerebral Aneurysm Treatment in Hyderabad#Best Hospitals for Cerebral Aneurysm Surgery in Hyderabad
0 notes