#my dermatologist is having me ask my doctor if she can put me on topical antiandrogens
Explore tagged Tumblr posts
Text
they should invent a testosterone that doesn't acne
#i am suffering#my dermatologist is having me ask my doctor if she can put me on topical antiandrogens#to leave the rest of me testosteroned but make my face untestosteroned#so maybe we will invent this 👍#transgender#transmasc#andy original
2 notes
·
View notes
Note
Hello!! I'd just like to say I love your blog, thank you for existing, it has brought me so much joy you have no idea!! 💕 Your comedy posts about the NXX team are some of my favourite things to exist on the internet, just aaaahhhh I love seeing them just exisiting and being cracky idiots together!! The best kind of shenanigans are team shenanigans <3 Thank you for bringing so much laughter into my life!!
Whille on the topic of team shenanigans though, I've always wondered where the NXX team members would fall on the scale between "i have a 10 step skincare routine that I follow religiously" to "facial soap?? Why do I need special soap for my face??"
I initally pegged Luke as type number 2, but Luke has spent a good chunk of his life living with MC, and she seems like the type that would insist on him actually using proper products because omg Luke that soap is meant for your body it's not the same you can't use that for everything!! So now he just keeps using the routine she recommended when they were younger because it just lowkey reminds him of her 🥺 I'm curious where the rest of the NXX boys would fall on this scale though!! You totally don't have to respond to this, I just thought it was an interesting idea! Bye for now!! 💕
awww, this ask is so sweet! thank you for your kind words, anon, im happy to make other people in this fandom happy :DDD now onto your ask bc THIS IS THE BEST THING EVER.
i dont take care of my skin at all but in the past ive chatted with a bunch of medical doctors/dermatologists (n if u take anything from this post, let it be this: all u need is wash face w/ water and sunscreen everyday even if ur indoors. thats it) so like. IT IS TIME FOR ME TO RAMBLE FOR A KILOMETRIC AMOUNT OF WORDS ABOUT SKINS OF THEMIS!!!!
nxx boys' skin......care routines
wc: 1.6k words about skin
vyn richter: supple and enraging, his skin is great and im suing him for it
vyn is fancy, vyn is prissy, vyn knows how to make MACARONS, so like obviously his skincare routine is high end as all fuckin hells. but like?? he doesnt even NEED IT TO BE!!! because his skin is naturally amazing
see, i may not know about vyn's diet (i assume it's delicious and balanced) or vyn's general physical health (he seems like a general physician's dream come true) but i do know one thing vyn richter gets a lot of: SLEEP.
sleep is like the best thing u can do for ur skin, passively. lets ur skin repair damage and thus reduces wrinkles or age spots. as marius loves to remind us every single second, vyn wakes up at 9am. prev canon content tells us that vyn sleeps at around 11pm, giving vyn's skin (skin richter...) 10 wholeass hours to take care of itself. recommended sleep hours for a person of his age is 7-9 hours. vyn adds on another hour. for the INDULGENCE OF IT ALL.
but yes, his skincare routine is the following in this order: gentle facial cleanser, toner, moisturizing lotion, sunscreen. pretty simple tbh, still on the scale of "chill" skincare routine but definitely near the line of "10 steps i will follow to my grave." important to note tho that all the products he uses are stupid fancy.
i think maybe sometimes, like after a busy or stressful day, he'll do a face mask. still fancy, but he doesnt rlly go after the ones that do too much, he likes the aromatic ones. fragrant face mask on, his antique gramophone crooning Rainy Days and Mondays by The Carpenters, and vyn is living the life.
luke pearce: skin thankfully was saved by mc, but before that it was TERRIBLE
i ONE HUNDO PERCENT agree with ur headcanon!!! it's SO SWEET HHHHH. i can imagine that once mc's skincare routine is drilled into his mind and heart (and she rlly made sure he remembered it!!! it's quite basic, not truly bare minimum, but on the chill scale of daily skincare: a gentle facial cleanser, moisturizer, and sunscreen. "that's it!!! that's all, luke!!! LUKE, STOP DODGING ME, IM JUST PUTTING ON THE DAMN SUNSCREEN!!!" these two together in the bathroom during their teen years was frigging world war 3) he really sticks to it!! and he uses the exact same products mc had used before EXACTLY for the emo reason u brought up.
luke pearce during his 8 year disappearance be like: shes watching over my......skin.....
aaron: when you say it like that, it's INCREDIBLY CREEPY
luke: SHUT UP, YOU KNOW WHAT I MEAN!!!!
and thats luke's skincare routine for basically the rest of his life. so since thats all been set up, i do wanna talk about Before The Salvation Of Luke's Skin---
---because LMAOOOO YEAAAA. bros, he was using not just normal body soap for his face. that was him on a good day. canon suggests that luke was a messy person, in his childhood. his room a mess yet he finds what he needs. that kind of philosophy is something i see bleeding into a lot of what he does. aka hes like "i mean my face doesnt get dirty, and it's still doing what a face is sposed to do, so i just wash it with just water in the shower."
mc, horrified: not even. soap?
luke: why would i need soap?
mc: "WHY WOULD YOU NEED SOAP"??????????
(im projecting on luke here lol. listen, just water is fine. ur not gonna win any awards with it but it's fine. and like, luke pearce sure as hell doesnt need more to help for him look GODDAMN BEAUTIFUL!!!!)
marius von hagen: skin so good it's infuriating, we have to steal it, IT'S TOO GOOD FOR HIM
now this is a mf knows skincare stuff from front to back. PAX has cosmetics branches but thats not why he knows imo, he knows because hes a fruity guy. and a vain one, sometimes. the point here is that he's KNOWLEDGEABLE. you cant scam this dude with subpar or overhyped skincare products. snail cream face mask? yeah ofc he knows about that [marius_von_scoffing.mp3] but youre saying this snail cream mask is the be-all-end-all of skincare? oh he KNOWSSSS UR WRONG, BUDDY!!!!!
that being said, since hes quite knowledgable he also knows skin differs from person to person. he did his research to figure out his skin type and what routine fits it best and makes him look sexy pretty hottest.
marius' skincare routine changes sometimes (theres one he does daily and one he does every 2 or 3 weeks, gotta exfoliate, duhhhh)
but his daily one is the following (after a shower): micellar water, toner, moisturizing lotion, sunscreen.
honestly, marius' biggest trouble is eyebags. he sleeps much too little and i am always gonna be stressed about that. hes stressed about it too bc he cant LOOK like hes having a hard time bc thatd mean ppl would be sincerely worried about him and marius is allergic to positive sincerity. hes got some products to protect against noticeable eyebags but hes not above using some concealer if it's a Bad Fuckin Week
additionally, marius often wears makeup for fun (gender feels) or for profit (business gatherings where theres a bunch of bright lights) so he always makes sure to prep his face for makeup and clean it all off after. regular makeup without the correct protection and aftercare is a death sentence for ur skin...
artem wing: it aint much but it's honest (skin) work (but forreal, artie, do a face mask sometime...)
artem is a guy who strikes me as a "does what has to be done" type of person with an added dash of "me? indulging? is that not what will send me to hell?" artem's idea of indulging is buying high quality whetstone to sharpen his kitchen knives with. he orders it online in advanced for his birthday and is pleased when the deliveryperson drops off the LITERAL BLOCK at artem's apartment. brick brick brick, it's fun! (whatever floats ur boat, artem)
anyway, he doesnt do anything about skincare until hes 20 years old or something in law school and good ol' mentor neil hume is like "artem, if you keep frowning and furrowing your brows like that, you're going to get wrinkles at 25" and artem is like "i dont care about...wrinkles" and neil is like jsdbfsdjkgjsd of course. but the conversation Does make artem curious enough to research about wrinkles, then about face skin, then about skincare and then hes like. IM DOING FACE SKIN THINGS ALL WRONG (I.E. I HAVE NOT BEEN DOING ANYTHING)
after that, artem does the following daily skincare routine: gentle facial cleanser particularly for dry skin (artem realizes his skin is dry, and that uh. HES DRY IN GENERAL. like have u seen how much coffee this dude drinks??? drink some water, sir??? hes toeing the line of dehydration, i know it, and his body is having trouble creating most liquids. dry skin. dry skin for artem wing), soft cream, sunscreen.
he does not enjoy...Strong Fragrances. or Intense Face Sensations. or just anything that feels like his face is going through something chemical, in the bad way. gentle products all the way, artem wing must be placed in a swaddles of softness ONLY...
bonus: nxx investigation team skincare bonding
marius and luke are the ones most open and game and HAPPY to have chill face mask friday night funtime with mc. granted, luke is gonna be like "THIS FEELS WEIRD AND COLD AND SLIMY" once mc slaps the mask onto his face. but he gets used to it pretty quickly. esp after marius teases him like "super spy can handle everything but aloe vera, huh?" and then after that marius has to dodge luke's tackle attack. friday night funtime with the boyz!!!
vyn and artem are invited to friday night funtime but theyre both hesitant. vyn because hes like "i dont look handsome when theres a face mask on my face" and artem because hes like "what if i get a bad grade at having fun on a friday night with friends. this is something both normal to fear and possible to achieve"
but i think mc has some great puppy eyes (she grew up with luke, of course she'd have great puppy eyes, im sure he TAUGHT HER) and so vyn and artem eventually get over themselves bc theyre both whipped as hell
once that happens, it's a lovely bonding disaster. marius is trying to ramble BETTER about the science of skincare vs. luke who did research because goddamnit, he's not going to let marius win so easily. artem prepared a relaxing spotify playlist and vyn takes potshots at him when a spotify ad plays and hes like "dont have premium? shame." and artem holds back on pelting the phone at vyn's clear skinned face. mc is just happy all her friends are here being dumb and having fun
all in all the nxx skinvestigation team is doing GREAT in terms of face skin. im sure random stellis citizens look at them walking around like "...he doesnt deserve his skin...i....deserve his skin..."
199 notes
·
View notes
Text
My Life with Hurley Story
My Hidradenitis Suppurativa Story
l believe the best way to start is with a description of the disease - and this is my description of the disease, based mostly on my experiences, but also drawing from the hundreds of medical articles, forums, and discussions I've had the pleasure of reading over the past decade in my attempts to understand and manage my disease better. Hidradenitis Suppurativa (HS) is a chronic skin disease, in which pus and blood-filled abscesses form under the skin in the groin area, inner thighs, armpits and under the breasts. These abscesses can range from the size of a pea to as large as baseballs. They grow in size until they are close enough to the surface of the skin, and may break open. When they do, they either do not heal at all, or take a very long time to heal... I'm talking years. As open wounds, they constantly leak blood and pus. There is nothing more horrid than the smell of an HS wound, trust me. They are extremely painful, if you can imagine. Large abscesses can often restrict your ability to move your arms, if they are located in the armpit, or restrict your ability to walk and make it vert uncomfortable to sit, if they are in the groin or inner thigh area. With all that being said, you can imagine the shame and embarrassment such a condition can bring to a person. An individual with this disease can be extremely self-conscious and depression is very likely as well. There are some points I'd like to stress before I move on to my personal experience with the disease.
HS is NOT contagious. It is NOT the individuals fault. No one knows why this happens. HS has NOTHING to do with a person's hygiene. HS has NO cure!
IN THE BEGINNING...
My HS started out as small pus-filled bumps on my groin when I was around 15 years old. These were easily popped open and were not painful. They would come and go. They were a nuisance, but were not totally alarming. I did not know I had a "disease" at this time. I did not seek medical care. I was about 20 when bumps started appearing around my breasts. These were larger and had to grow a few days before I was physically able to squeeze them out. The pus was generally very dry, like something that would come out of a pimple on your face. It would quickly shoot out and splatter onto the mirror or whatever I was in front of. I mention this only to illustrate the change in consistency of the pus over time. They would heal, but always come back. Same spot, same size. Seeking help was difficult. I didn't want anyone to see. I can remember going to a walk-in doctor who prescribed a topical cream to rub on them. That didn't help. Eventually, the pain was too much to bare and I was forced to go to the emergency room. I went in the middle of the night. I had an abscess about the size of a quarter on my chest, between my breasts. It was so painful, I couldn't sleep. I had my first I&D (incision & drainage) that night with a very nice doctor. After he had cut it, he told me a nurse would come in to "pack" the wound and that I would be set up with home care. I didn't know what "packing" meant at that time, so when the nurse came in and simply covered the wound with gauze and tape, I thought I was good to go. That specific wound came and went over the years but it would easily break open after a week or so, and the pus and blood would pour out, like syrup, messing up my bra and clothes.
I went to a walk-in maybe a year or so later who I could tell really sympathized with me, but truly didn't know what to do. She referred me to a dermatologist. I waited months to see her. When I finally did, she was cold towards me. I didn't feel like she cared as she told me there was no point in treating this externally (I was hoping she would cut one or two open to give me some relief). She told me the only way to get rid of this was to do it from the inside. She prescribed me some pills (probably an antibiotic). I asked her if it had worked for others, and she nodded yes and she scooted me out. The pills she prescribed did wonders for the acne on my face but absolutely nothing for my HS. I was told to come back and see her in three months, but I never did. She didn't care enough.
For a long time, I just waited for the lesions to grow large and break open on their own. There's one that I actually tried opening with a needle (DO NOT DO THIS), and of course I just made it worse and probably make it stick around a lot longer than it would have had I just gone to a doctor. I had started working full time when I began getting abscesses on my upper leg, extremely close to my groin and bottom. This was extremely painful. I had to find creative ways to sit on my chair without drawing too much attention to myself. There were many days I wouldn't even sit. I would just do type on the computer standing up, pretending like I was only checking something out on the computer and would have to leave in a second to do something else. The days in which I did sit, I learned I needed to sit on my jacket or sweater, in order to not stain the chair with the drainage coming out of my open wounds, seeping through my pants and onto the furniture. I often walked funny, trying to avoid feeling the wounds rubbing against my pants. If anyone asked why, I just told them I had a problem in my leg.
It was a Sunday night when I decided I needed to see a doctor to drain one lesion on my inner buttocks. My mother took me to the emergency room. When the doctor had seen how large the abscess was, and the others that surrounded it, he called for a surgeon to come and take a look. The surgeon told me that I needed surgery, but because I had eaten dinner that night, and she and her team had already had a long day, I agreed to come back in on Wednesday for surgery. On that day, while the surgeon was briefing me on the surgery, I asked her if she didn't mind also draining a lesion under my arm. When I showed it to her, she couldn't refuse. When I awoke from surgery, she mentioned that she had arranged for a Infectious Disease doctor in the morning and also told me that I may want to consider plastic surgery, a suggestion I wish I had taken at that time. I was released from the hospital the following day and set up with home health care.
The Infectious Disease doctor examined me and prescribed me two antibiotics to take over a period of three months. Whether theses helped my case or not, I'm not sure. It's possible I could have been worse off if I hadn't taken them, but I wasn't getting better. I went on living my life just waiting for my abscesses to open and draining them myself - or going to the emergency room if I thought it was getting too large with no signs that it was going to resolve on its own. Going to the ER always meant that I was going to be set up with home health care, or what they call CCAC (Community Care Access Centre). Nurses could either come to your home to change your dressings and check on the progress of your wound, or, as they preferred, you could go into a near-by clinic every day or every other day for the same service. This may be common knowledge, but there are great nurses, and there are terrible nurses. I could write a book about my bad experiences with CCAC, but I won't elaborate. The point is, more often than not, CCAC nurses made my life more difficult than pleasant.
DERMATOLOGY
My sister had told me about a dermatologist that would see patients without a referral. This sounded great to me because having to explain to doctor after doctor (or anyone, for that matter) about your disease and the things you've already tried to manage it is exhausting. I called and made myself an appointment for a few months later. When I met with Dr. A, I felt like he sympathized me and I had hope. He knew my disease. He had patients with my disease. He had touched my wounds and wiped away pus. He sampled the pus for testing. These are things the first dermatologist I had seen never did. He had a son who worked in clinical trials and had just finished a study on my disease with an expensive treatment called Humira. He called his son right there in the patient room to ask him if he knew of any upcoming studies so that I could possibly get medication for free, but unfortunately the answer was no. He had also treated patients with HS with Accutane, but this too was expensive. With the knowledge that I didn't have any drug coverage, Dr. A prescribed me two strong antibiotics to take over a course of three months. Those antibiotics did help some. When I revisited Dr. A after the three months had passed, he prescribed me another run of the antibiotics.
HS controls my life in every way. There's not a moment I'm not thinking about it. There's not a minute I am not uncomfortable or not in pain. There is not a decision I make without considering my disease. I have to think about my HS before doing the smallest tasks. There are times I put off going to the bathroom just because getting up, changing positions, can cause so much pain and discomfort, and I'm literally mentally preparing myself for what I'm about to experience. Needless to say, there are many activities I just cannot participate in. Simply getting into the car can be difficult. I dread going shopping - too much walking, which means wounds rubbing against my clothes. I'm often caught off guard when someone asks me why I'm walking funny, or holding my arm awkwardly, because I think I'm hiding it so well. HS also controls what I can wear. As much as I love form-fitting clothes, its just not comfortable to be in them. I don't wear anything white - my wounds will stain it. I don't wear anything sleeveless - my underarms are full of wounds I don't want anyone to see, not to mention the drainage that will have no place to hide. I try to wear my clothing as loosely as possible, but I'm fighting to keep my pride, despite this disease and I hate to look shabby. Depression is all over my face. I try to act happy as best I can, to not bring any attention to myself. I look back at old pictures, and miss how happy I was and how beautiful it was to not be in pain; to just feel nothing. I cry all the time. The tears often start because of the physical pain - but they quickly grow into a bawl just thinking about everything I've already been through, how much the disease controls my life, and how I don't have any idea how to make this better. HS affects my sleep, because it's not easy to fall asleep while you're in pain or you're too busy scratching or squeezing a nuisance of a wound. It's frustrating just knowing that I can't just tell someone, 'I have HS' and have them just know what it is and have a small idea what I'm going through - as I could have if I had something like arthritis or psoriasis. No one knows what this is. No one has heard of it. No one can ever understand - and so I don't try to explain it. I've tried before, and it only leads to individuals thinking they know how to take care of it. I've been told just to scrub it, just to take the pain and squeeze it out and it'll go away and never come back. I've been told to just use natural soaps; that my skin just can't handle the harsh chemicals. I've even been told that it's because I don't pray hard enough. Everybody thinks know, but nobody really knows. It hurts to know that people don't believe me when I say this is an actual disease! It cannot be healed by something as simple as washing it away. If it were that easy, I would have rid myself of this a long time ago, believe me. Would you tell a cancer patient to just wash it off? I didn't think so. My loved ones, who know my condition still don't know what I truly live with because I try so hard to be normal, act like it doesn't bother me, around them. Firstly, because I don't want their ideas on how to 'easily fix' the problem, and secondly, because I don't want to be pitied. I just want to be free.
After two three-month courses of antibiotics, I was over it. I was over putting these pills into my body just to get little to no results. I stopped seeing Dr. A and went back to just dealing with it - drug free. This meant frequent visits to the emergency room and urgent care centres, and of course just waiting for some to burst on their own. I remember crying to a doctor at an urgent care, telling her how tired I was and asking her to I&D an abscess under my armpit. She told me there was no way to cure this and I was just going to have to live with it. How rude! I mean, so far I haven't found what she said to be untrue, but she could have been a little more comforting and optimistic. Can you believe she didn't even cut the abscess? She told me to take some antibiotics and wait for it to break open on its own. With this disease, I've learned that you're going to have to kiss many frogs to find your prince - kisses being doctor appointments, frogs being doctors, and the prince being a doctor who doesn't necessarily have all the answers, but just cares enough to try, and then try again. That night, I was in so much pain and a doctor refused to help me. Physically and mentally, I was fed up. I actually quit my job that next morning and applied for Employment Insurance. Getting up and ready in the morning was too hard and my supervisor was beginning to give me a hard time for the times I showed up a few minutes late after giving too much attention to a wound in the morning. I was physically and emotionally tired, and I truly just needed a break. So I quit.
I must have had enough of 'just dealing with it on my own' again, because I decided to go see a doctor one more time. I went to see a family doctor, who prescribed me some antibiotics but also referred me to a lovely dermatologist, Dr. Nisha Mistry. Oh, Dr. Mistry, what can I say about you? On my first visit, she presented me with print-outs and spoke to me on what HS is, what the different causes might be and different treatments. Now, I had already read most of this online while doing my own research, but it truly meant a lot to me that she had taken the time out to read up on my disease prior to my visit. After I told her I had already tried antibiotics - maybe too many times, she told me about Humira. Humira defined by www.drugs.com: "Humira (adalimumab) reduces the effects of a substance in the body that can cause inflammation. Humira is used to treat rheumatoid arthritis, juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, plaque psoriasis, and and a chronic skin condition called hidradenitis suppurativa." Don't you just love how HS is the only disease they had to briefly define? She explained that she would only recommend this in extremely severe cases, because of the possible side effects. She had me change into a gown, and after taking a look at my wounds, she agreed I had a severe case. Unfortunately, like Dr. A had told me over a year prior, Humira is very expensive, and I didn't not have any drug coverage. She too, like Dr. A, knew of some clinical trials in which I could get the drug for free, but the trials had just ended before my meeting with her. That's when she told me about a program called compassionate care - where the Canadian government actually pays for your medicine because your doctor feels so terribly for you. That's my definition of compassionate care, anyway. She didn't make me any promises at that time, but told me she would put in an application for me. I was approved! There were a few tests and things I needed to do before I could officially start, but I eventually began my Humira treatment a few months later. I also started working again around the start of my Humira treatment, about four months after I had quit my last job.
I have to believe Humira helped me. It did not cure me, but I feel like my case got better. It's hard to say for sure because every time I would meet with Dr. Mistry for a check up, she would say it didn't look any better. But I felt better. My range of motion improved and I feel I was able to do more things a little more comfortably. I was still making visits to the emergency room, however. After one particular visit where I ended up staying the night, the hospital notified Dr. Mistry. She called me in a panic about a week later demanding that I come and see her right away. The hospital had totally exaggerated my symptoms. Apparently I had a fever when I was admitted, but they told her I came in shivering! They even told her I had been there for 3 days when it had really just been one night. I explained to her that it wasn't as serious as they made it seem, but she was still very concerned. She suggested I stop taking Humira immediately. At that time, I begged her to let me continue, but she pointed out that after eight months of treatment, I was not seeing sufficient results, and with the side effects of Humira, it may have been causing more harm than good. I agreed to stop, and after discussing with her some of the symptoms I was experiencing, she referred me to a gastroenterologist to check for Chron's disease, an internal medicine specialist, to just check me in general, and a general surgeon to actually operate on the HS manifestations.
SURGERY
Dr. Mistry had suggested I see the gastroenterologist for of some of the symptoms I was experiencing. I had a consult with the gastroenterologist to explain my medical history and my recent symptoms. At that time, he said if it was Chron's, the Humira should have helped with that - but he proceeded to schedule me for a colonoscopy anyway. I was cleared for Chron's - which I was happy about - but that doctor never really addressed the reasons I may have been experiencing the symptoms Dr. Mistry was worried about. Sigh. Doctors. Dr. Mistry had wanted me to see an internal medicine doctor because I was experiencing many fevers and she just wanted to make sure my body chemistry was alright. Somehow that appointment never happened. I was, however, scheduled to meet with general surgeon Dr. K for a consultation, rather quickly, I might add. She was lovely. Before examining me, she explained that she was only a general surgeon, and if my case would require something called a 'flap', then she would have to refer me to a plastic surgeon. A quick glance at my skin would confirm that I, of course, was more of a plastic surgery candidate. My heart sank. Luckily, she knew of an excellent plastic surgeon, she said, and would be able to get me an appointment with him a lot sooner than it would typically take. She was very sympathetic and encouraging and I really wished she could be my surgeon. At that time, I had recently been to the hospital for an I&D and was visiting the CCAC nurses every night. Getting the wound packed was very painful because the incision had been made so small. Dr. K was nice enough to widen it for me. As her nurse was dressing the wound, she assured me that the plastic surgeon I was being referred to was very good, told me I was very brave and that she was impressed with how high my spirits were. If only she knew I was fighting back the tears that would burst out of me as soon as I entered my car.
It felt like forever before I got a chance to see the plastic surgeon, Dr. T. If Dr. K had in fact expedited my appointment, I feel really sorry for those who don't have that privilege. My parents came with me to this appointment. After I had told them about what happened at my appointment with Dr. K, my dad told me to let him know of any future appointments. It means a lot to me that he didn't want me going alone. I'm guessing Dr. T had just finished reading a Wikipedia page or something on HS when he walked into my room because he was basically telling me all the things I would have read had I quickly did a google search on the disease. He basically told me at that time that surgery was not a good idea because of complications and scarring. This was before he even looked at my skin. After examining me, he tells me that he would prefer I go and see Dr. S, an expert in HS, and he would only perform the surgery if Dr. S recommended it. He told me that he would put in the referral, but not to worry because his office scheduled appointments quickly. In the mean time, he told me to focus on losing weight because HS was often made worse by heaviness. I am not a skinny girl, but I am not huge either. Weight may be a factor in other peoples HS, but not mine. I know this because I had actually lost quite a bit due to stress (of the disease) and my symptoms did not change. I didn't take it personally though. I knew he was just spewing out whatever he had just read on the internet. I was devastated, still. I had really high hopes about him because Dr. K and her nurse had praised him so much. I had even warned a supervisor at work that I may have to take time off shorty in order to recover from surgery. So of course, my heart was crushed. Another appointment that had caused me to go home and cry.
At this point, I'm waiting for an appointment from Dr. S, but not really, because for one, I had already seen a GREAT dermatologist in Dr. Mistry, and she had already recommended surgery, and two, I no longer trusted Dr. T. It didn't seem like he was eager to help me, and so I didn't want him to. I went back to 'just dealing with it', until I got a call from Dr. Mistry's office asking me to come in to talk about renewing my Humira prescription. I thought this was odd, seeing that I had stopped taking Humira, and Dr. Mistry knew of this. I went in to see her, anyway. I told her about my experiences with Dr. Kapala and Dr. T. She told me that she actually worked for Dr. Sibbald (who still hadn't called me for an appointment, by the way), on his team in his office on Fridays, and she knew for sure he would recommend surgery. This made me even more upset at Dr. T. She offered to refer me to another surgeon. I explained to her how frustrated and exhausted I was at all the appointments and disappointments - and that I needed a break from it. She understood completely, and let me know I could call her whenever I was ready to try again.
I got another odd call from Dr. Mistry's office a couple months later telling me that Dr. Mistry wanted me to call her to discuss my test results. It was odd because I hadn't taken any tests. I called anyway. She explained that she had been in contact with a Humira spokesperson who had asked her about my Humira experience. After she had told him that I didn't really benefit from it, he told her of a plastic surgeon who would love to help, as a 'special favor'. She said she knows I had opted to take a break from surgery consultations, but she didn't want to let the opportunity pass without offering it to me. I accepted. I wanted to at least talk to this surgeon. I was still in pain, and maybe this was my luck finally turning around.
I met with Dr. CT on Monday, November 21st, 2016. She asked about my Humira experience and about the surgeons I had seen before her. After I told her that Dr. T had basically told me he didn't want to do it, she told me that nobody wants to do it. She explained it was an extremely messy surgery that would require a skin graft and two separate surgery weeks apart, and after all of that, my body may reject it. When briefly describing what surgery on my lower body would be like, she mentioned that I would have to urinate in a bag temporarily. As you can imagine, this is where the tears starting filling my eyes. As she was working really hard to turn me off this surgery, I'm sitting there wondering why I was even invited to this appointment. I was told that there was a surgeon who wanted to help me as a special favor and when I met her, I felt like I was just being kicked in the gut. I told Dr. Mistry I needed a break from the heartbreak of surgeons telling me they can't help me, and she sent me to a surgeon that would reject me again. The surgery did sound awful, I have to admit. Her goal was clearly to make me change my mind about desperately wanting the surgery, and she did so well that I even forgave Dr. T for rejecting me. After seeing the tears run down my face and the disappointment in my eyes, Dr. CT offered to refer me to a plastic surgeon at St. Mikes Hospital who had done more complicated HS surgeries. I declined. I was so over it. Instead of surgery, Dr. CT suggested that I should go back on Humira. She stressed that it is a very new drug and it will get better and work. Whatever. I was on Humira for eight months and it barely helped me. I'm convinced I was just injecting cancer into myself and not seeing any immediate benefits with my HS. I refuse to go back on Humira. Something has got to give.
Dr. CT called me herself the next evening at 7:00PM to tell me she had spoken to the Humira representative, and he was doing to be in touch with Dr. Mistry in recommending some other dermatologists that have a little more experience with HS. She also said that she would contact Dr. Melinda Musgrave, the plastics surgeon at St. Mikes, and ask about any new approaches she has come across and can suggest. She explained St. Mikes is trying to develop a clinic of some sort where they can talk to HS patients about lifestyle changes, such as diet, that may minimize the effects of HS. She stressed that even though she didn't think surgery was a solution to HS, she didn't want me to believe that there was no hope, and that there were hopefully a couple things we could try before taking that route. The call meant everything for me. It lifted my spirits. It just felt like there was another doctor out there, in addition to Dr. Mistry, who was in my corner - who saw my pain and truly wanted to help.
NATUROPATHY
I had reached out to a naturopath, Dr. S. The appointment was booked for a few days after I got the call from Dr. Mistry about Dr. CT, and I almost cancelled it thinking that I wouldn't need him anymore because Dr. Mistry found me someone that would help, but I didn't. During my first appointment with him, I just spent the hour telling him about my disease and how it affected me daily. He asked questions, I would answer them. He ended the appointment by telling me that he "really, really, really wanted to help" me, and gave me a few of his ideas. He prescribed me Effer C, a supplement to help me go to the bathroom more often and Vitamin D, and we booked an appointment for about 3 weeks later. By the next appointment, he had a very detailed plan written up that predicted to have me pretty much healed in six months. The plan included a couple supplements, something called colonics, and a strict diet of no dairy, sugar, gluten or wheat. As you can imagine, sticking to that diet proved to be difficult, but I did try. I saw little to no results, but to be fair - I was not completely committed. I went to a few subsequent appointments, but naturooathy is not covered by OHIP, and although my work insurance covered a lot of the cost, it was becoming expensive to keep seeing him, and during the appointments, he was mostly just making other suggestions of changes I could make to my diet. I felt like I could handle that on my own.
What's it like to feel nothing? I miss feeling nothing. No discomfort, no pain, no sting. I used to take feeling nothing for granted, and now I know how precious it is. I miss being able to sit down on a chair, a bed, the floor, without feeling anything. I miss being able to get into a car without feeling anything. I miss being able to drive without feeling anything. I miss walking and feeling nothing. Oh, I miss going up and down stairs without feeling anything! I miss putting on my panties, my pants, my bra, my shirt, my coat, without feeling anything. What's it like to get in and out of bed without feeling anything? To take a shower and feel nothing?
SURGERY PT. 2
After that meeting in November 2016 with Dr. CT, I hadn't really been to any doctors, with the exception of the few additional visits with the naturopath. I gained a little relief by changing my diet - but no major improvements. In April 2018, the drainage coming from my arms was uncontrollable. My shirts were soaking wet within a few minutes of changing into them. I didn't know what else to do except to plea with a surgeon to operate on me. I chose Dr. CT. I met with her on June 6th 2018. Again, she illustrated a nasty surgery that might not even be successful. I told her I didn't care, I needed to do something. She offered to send me down to St. Michael's Hopsital to see plastic surgeon Dr. Melinda Musgrave or her colleague Dr. Karen Cross, who do a lot more work with HS. I agreed to a referral, just because I could tell how badly she did not want to operate on me. If you'll recall, she had mentioned referring me to these doctors before, but nothing ever came of it.
This time, I got a surgery consultation with plastics surgeon Dr. Karen Cross, scheduled originally for November 2018, but moved up to September 2018. It was simply and honestly the best consult I've ever had. She specializes in HS surgeries and really can't imagine why I hadn't been referred to her before. She told me I was an excellent candidate for surgery, but she agreed that my disease was so active that it probably wouldn't be effective. She requested that I see a dermatologist of her choice, follow their suggested treatment for about three months, and after the disease had calmed down, she would operate. I loved speaking with her because she just got it. She knew exactly how I was feeling as a person living with HS without me having to tell her. She knew and answered all my questions before I even had a chance to ask. It was obvious she had spent real time with other HS patients because she truly just got it. She was so hopeful and encouraging. She let me know that it would be a long journey to recovery, but that we would be on that journey together - and that I should always let her know where my head is at and how I'm truly feeling not only physically, but emotionally. I had never met a surgeon like her and even if I don't end up getting a surgery, I'm so glad that my path lead me to her - just to know doctors like her exist.
CLINICAL TRIALS
Dr. Cross referred me to dermatologist Dr. Afsaneh Alavi, also specializing in HS. She enrolled me into a clinical research study for a potential new "antibody therapy". Without going into much detail, I was required to go into a clinic every two weeks for intravenous infusion and complete a small questionnaire on a phone-like device nightly. I officially began getting dosed in October of 2018. A lot like my experience with Humira, I couldn't see any changes in the way the disease physically presented itself, but I can say the day to day pain dropped considerably and my quality of life increased. However, in mid-December, I developed a large abscess on my upper thigh. It had been growing in size and pain for about a week before my next scheduled infusion and meeting with Dr. Alavi. After examining the abscess, she decided immediately to take me off the study and arranged for me to have it drained that morning. She prescribed Ertapenem, an antibiotic infused intravenously daily, for four weeks.
ERTAPENEM
Ertapenem is an antibiotic administered intravenously. I was taught how to run the IV on my own at home. It took about 30-45 minutes and then I would wrap up the IV site with gauze until I was ready to do it again the next day. While showering, I used a arm cast protector I found in a home health care store. It's basically a long plastic glove-bag that spans the entire arm, the way a cast would, and tightly seals before the shoulder. I couldn't use that arm to clean myself with, but the IV site was protected from the water. My IV site would have to be changed every 3-5 days. I would go to a CCAC clinic to have a nurse set up a basic IV line in my arm or hand. I have very difficult veins, and so nurses often had a hard time starting my IV. On every visit, I was poked multiple times before one was successful. There was a night when the nurses were not able to find a good vein, and I was sent to the emergency room for one of the nurses there to try. I waited four hours that night just to get an IV started. Initially, the plan was for me to have a procedure done to get a 'picc line', which is more secure than the regular IV and could remain in my arm for weeks without having to be moved, but that wasn't scheduled until week three of my four week course of the drug and it just didn't make sense at that point. All this to say, the treatment of Ertapenem caused some minor inconveniences, but overall I was pleased with the results.
Ertapenem was the best treatment I've received so far. I felt virtually no pain during the 4 weeks I was on the medication. My wounds pretty much dried up. Although you could still see them, there was no drainage coming from any of my wounds. My clothes remained dry throughout the day and through the night and I never worried about staining my seat. Proving this, my laundry loads we significantly smaller and my jeans/pants were clean enough to re-wear before washing.
CLINICAL TRIAL DRUG: IFX-1
Although an effective treatment for me, I could not remain on Ertapenem for very long. Antibiotics are not meant to be taken long-term. I was on the drug for about five weeks. With permission from the sponsors and executives of the clinical trial, Dr. Alavi allowed me to continue treatment with the clinical drug, IFX-1. During the first phase of the trial, I was either being given the active drug, or a placebo. Dr. Alavi wanted to give me a chance to enter the second phase of the trial, which guaranteed active drug administration.
Since beginning the second phase, I can confidently say I feel better. I have not experienced any large new abscesses, and the ones I already had are smaller and draining less. The most improved symptom is my ability to move; my range of motion. I am able to move my arms and legs in ways I wasn't able to do before. This alone has improved my mood and my quality of life. Dr. Alavi agrees, I will still need surgery to remove the skin that the HS has completely destroyed over the years, but if this drug makes it to the market, I believe it could help many of us keep the disease under control.
December 30th, 2019 Dr. Cross performed a 'left axilla extraction with flap' surgery on October 31st, 2019. She removed all of the affected skin from my armpit and pulled skin from my back to replace the missing skin. It was a day surgery that took about 3 hours. The wound was cared for by near by clinic nurses. It took a little over a month to fully close. The surgery went extremely well and I am please with the results. I will meet with Dr. Cross again in a few months to talk about my right arm. Dr. Alavi thinks I should return to Humira in the mean time, but at this point, I don't think I want to take that route. I know it's only been a couple months, but I believe surgery is the solution for me.
November 22nd, 2020 Dr. Cross performed the same surgery, this time on my right axilla on August 20th, 2020. Again, the surgery went well and I am pleased with the results. Now, I don’t have any inflammation or affected skin in my armpits and it’s truly changed my life. I can wear sleeveless tops and I don’t have to worry about drainage messing up tops with sleeves. I can finally wear white if I choose to. I do still have some HS on my lower body, but nothing that warrants the surgeries I needed for my arms. I will try to treat what’s left with diet changes - specifically the keto diet and will keep you updated.
The rest is still unwritten...
#hidradenitis#hidradenitissuppurativa#chronicillness#skindisease#skincondition#mylifewithhurley#myhsstory
9 notes
·
View notes
Note
I dread taking showers. I know gross, but I have cholinerginc urticaria basically fancy word for hives, they make me itch, and make my skin feel like it’s on fire, 2 years ago when I didnt know I had it I would take a shower, sob for hours scratching my skin and just wanting to make it stop I would scream for my parents to make it stop I would take 4 Benadryl you’re only supposed to take 2 still didn’t work I would scream and cry at my mom for making me take a shower pt 1 tag as 🏐☀️
Pt2🏐☀️I was terrified to take a shower I still kinda am I feel like I may have developed ptsd over it I also have eczema which when I got allergy tested the first time the doctor told me that I wasn’t allergic to anything which I am allergic to a couple things that I only have eczema and just to put on lotion that was it no help whatsoever flash forward to a year later still sob after the shower and take too many Benadryl we went to see a dermatologist and she did a simple test and told me
Pt3🏐☀️ I have hives and then we went to the allergist next, I had 50 needles in my back for the allergy test turns out I was allergic to lots of stuff and i have super bad hives during all of this my entire body was red and I was in so much pain my experience with hives have been traumatizing, and I think I may have developed ptsd I know you can’t diagnose me but do you think I could have it or anything related to it? Thank you for taking your time to answer this love you all so much.
Hello there,
I'm sorry that you've been struggling so much. Physical illness like this can be very stressful. I personally suffer from hives as well, and it can be absolutely unbearable at times, almost feeling like torture, so I truly understand.
Have you been able to form a treatment plan with your specialist? I think that's an important step to take, so that you know what you can do to help these episodes. As for the Benadryl (antihistamine), the thing with taking more is that it won't help calm the itch down more. I am on a higher dose than the recommended, but it's best to ask your specialist how to take them - more often than not, they will recommend taking the regular dose, then taking another regular dose a few hours later. They will be able to advise you on what is better for your situation, and trial other methods to help calm the hives down. I also want to share about the only thing that helps me control it when I am in a flare - lidocaine cream and ice. Lidocaine cream is an over the counter cream, usually sold in the section for topical bug bite creams. Take a look at the ingredients of them, and buy ones that have that ingredient. As soon as you get an itch, put the cream on all of the affected areas, and grab an ice pack. Hold the ice pack/s on the worst affected areas. The lidocaine helps to numb the itch a little bit, and the ice helps to stop the swelling of the hives, which also works on reducing the itchiness. It's the only thing that lets me sleep when I am having a flare up.
As for post-traumatic stress disorder, you are right in that we cannot diagnose you. Only a professional can do that. So I'd suggest speaking to your doctor about the impact this has had on your mental health, so you can get some support. We have a page on Getting Help here that may have some useful information. That being said, post-traumatic stress is only diagnosed after experiencing an event that threatened the life of the person, or witnessing an event that threatened the life of another. It involves flashbacks to the event, feelings of hopelessness and terror, dissociation and nightmares. Whilst what you are describing definitely sounds like it brings on traumatic feelings, I am not sure that it fits the criteria for PTSD as it has not had a life-threatening impact on you.
However, that doesn't make the effects any less severe. I would say that any events relating to showering or the hives are incredibly triggering for you. Even non-life-threatening events can severely impact the way that we function, especially when they develop into triggers that set off intense emotional reactions like fear, panic, depression or helplessness. These emotions in themselves indicate that there is something going on with your mental health, and I think seeing a professional to look at diagnosis and treatment would be a great idea. They can narrow down the exact symptoms, look at how this has effected you, and give you a solid diagnosis. There are many medications and therapies that can be used to treat extreme emotional reactions to events like this, and they are listed in the getting help link above. Your doctor may want to try you on some of these to get some control over your symptoms.
We have a page on Recovery Tools here that I think may be useful for you. It has a few different tools, and I think the calming anxiety, grounding techniques, mindfulness and distraction tools in particular may be helpful for you. We also have a page here on DBT Skills, which are the skills taught in Dialectical Behaviour Therapy. These can help with panic, anxiety and extreme emotions, and really helped me to manage the panic associated with negative events from my past. The ones in the mindfulness section were the ones that particularly helped me. Lastly, we have a list of Helplines and Web Counsellors here, and I encourage you to reach out to them if you ever feel like you need some support in calming down the anxiety related to the showers and hives.
I hope that you can see your specialist and your doctor and both get a plan in place for treating the hives, and looking into mental health diagnosis and treatment. You deserve support through this. You are certainly not a gross person for being scared of being in the shower; I think your feelings are completely understandable, and it is a place that causes intense fear for you. I'm hoping with help from your doctors, this can become easier in time and they can help you find alternative ways to either shower or get clean without causing a flare up of the hives.
Positive thoughts your way,Alexandria.
#🏐☀️#hives#ptsd#post traumatic stress disorder#chronic illness#physical health#allergies#dermatitis#cholinerginc urticaria#anonymous#mhaalexandria#advice#advice blog#mental health advice
1 note
·
View note
Text
New story in Politics from Time: Tech Companies Are Transforming People’s Bedrooms Into ‘Virtual Hospitals.’ Will It Last Post-COVID?
When Curtis Carlson started having back pain this spring, he tried to put off seeing a doctor. The COVID-19 pandemic was raging, his job at a transitional housing organization in Ukiah, Calif. was busier than ever amid the economic collapse, and a hospital seemed like the last place he wanted to be.
But when he finally took himself to the emergency room and he was diagnosed with a kidney infection, Carlson figured he would have no choice but to stay. Instead, his doctors told him about a new program that would allow him to finish the rest of his hospital care at home, with a medical team monitoring him virtually around the clock and making in-person visits multiple times each day.
“I was blown away,” says Carlson, 49. When it became clear that staff would set up the equipment, which all fit on a TV tray, in Carlson’s home, and that he’d be able to communicate with his medical team via iPad, he was on board. “It was easy enough that I could use it, which was awesome,” says Carlson, who describes himself as “terrible” at technology.
Carlson’s experience was revolutionary, he says. After one night in the hospital, he was back at home with his wife and their four sons. “The biggest part for me was when I got home, seeing the look of relief on my seven-year-old’s face,” Carlson recalls. “While they were putting in the electrical wizardry, I asked him, ‘Were you worried about me?’ You could see him just crumble a little bit. He was definitely very happy Dad was home.”
Hospital administrators at Adventist Health, the system that runs the Ukiah hospital where Carlson went for care, had been looking for ways to reach rural patients outside their hospitals for years. But when the COVID-19 pandemic came to California this spring, administrators felt the timeline collapse. After finding the right technology in April, they began offering the service to patients like Carlson within 29 days. By May, Adventist Health had the infrastructure ready to care for 200 patients in their own homes.
Adventist is not alone in its warp-speed embrace of new technology during COVID-19. In recent months, hospitals around the country, looking for ways to free up beds for coronavirus patients, began expanding their virtual offerings, launching video doctors’ visits and virtual therapy sessions, and rolling out programs to remotely monitor vulnerable patients, like those in nursing homes. As doctors and patients embraced these new, online methods of care, Medicare, Medicaid and many private insurers temporarily changed their payment rules to accommodate them. But many of these changes are only guaranteed through October, and plenty of regulatory hurdles remain.
Now that it’s clear the pandemic is not going away anytime soon, medical providers and hospital administrators say they need more substantial reforms to ensure their investments in telehealth can continue. Whether innovations like remote hospital recovery beds will be available in the long term depends primarily on whether public and private insurers will continue to pay for them. In other words, in the topsy-turvy health care economy of the United States, it’s payment models—not technological ability or patient benefit—that will now determine the future of virtual care.
Hospital care at home
Prior to COVID-19, Medicare only covered telehealth services from certain providers. It also generally required telehealth patients to be located in a rural area and at a medical facility. Many Medicaid plans and most private insurers had similar restrictions. But after the coronavirus outbreak this spring forced nearly all doctors to stop seeing patients in-person, the Centers for Medicare and Medicaid Services (CMS) issued a number of waivers relaxing these rules, and private insurers followed suit.
Once CMS led the way, private insurers temporarily changed their rules too, and telehealth usage exploded. Between April 2019 and April 2020, telehealth claims increased 8,336%, according to FAIR Health, a nonprofit that analyzes private health insurance claims. More than nine million Medicare beneficiaries used telehealth services during the first three months of the crisis. And at University of Virginia’s network, which already had a more robust telehealth program than many others, virtual visits increased 9,000% between February and May.
“COVID-19 changed everything when it comes to telemedicine services,” says Dr. Karen Rheuban, director of the University of Virginia Center for Telehealth. “The genie’s not going back in the bottle.”
The Trump Administration is now pushing for more telehealth access. On Aug. 3, the President signed an executive order calling on CMS to permanently expand the kinds of telehealth services that Medicare covers, and the agency’s administrator Seema Verma has also said she believes access to telehealth should continue beyond the public health emergency. Broader expansions would need to come from Congress, where dozens of bills on telehealth have been introduced in recent months, but lawmakers have not yet seriously considered the topic.

Courtesy of Adventist HealthCurtis Carlson and his family at their home in Ukiah, California.
Telehealth advocates say now is the time to act. A range of virtual offerings could be revolutionary for patients who are seriously sick, need long-term care, or live in rural areas, where hospital closings have left millions of Americans without easy access to treatment. “The environment in a hospital, although it’s very conducive to high intensity care, is not that conducive to being able to engage in normal activities of daily living that might be actually important for recovery,” says Dr. Michael Apkon, president and CEO of Tufts Medical Center.
In March, when Apkon watched Italian hospitals overflow with coronavirus patients, he sped up Tuft’s long-simmering telehealth plans. Apkon called Raphael Rakowski, the CEO of the tech startup Medically Home, and by April, the two organizations had launched a program that would provide hospital-level care in patients’ homes. Rakowski says he’s spent years telling hospitals they could reduce overhead costs and improve the patient experience by embracing care at home. “Sadly, it took a pandemic to amplify the patient’s role in their own care,” he says.
In order to be eligible for the Tufts-Medically Home partnership program, patients must typically have a similar profile to Curtis Carlson: they must have relatively stable health, be suffering from common conditions such as heart failure, diabetes, pneumonia, or kidney infections, and they must have a safe, stable place to live. If a patient meets that criteria, Medically Home provides all the equipment, including communications devices, monitors, backup internet, cell signals and power sources. (Some locations are admitting patients such as those with cancer, COVID-19 or who need longer-term care, and over time those will grow, says Rakowski.)
In Boston, where Medically Home is based, the tech company itself employs nurses, paramedics and other staffers who visit the Tufts patients in person several times each day to administer IVs, do blood tests or provide other care, and the patient checks in with their doctors via video. In California, where Carlson was treated, and in other locations, Medically Home’s partner hospitals provide the staff. Teams of nurses and physicians also monitor each patient 24 hours a day from a “command center,” and can be reached immediately if any questions or complications arise.
Even accounting for the time and cost of staff traveling to visit patients at their homes, Rakowski says at-home hospitalization costs about 20 to 25% less on average than care in a traditional hospital setting. In California, where Carlson was one of Adventist Health’s first patients to use the Medically Home model, Adventist Health President Bill Wing sees significant savings in the future. Maintaining hospital facilities and building new infrastructure is very expensive, he notes, so if Adventist Health can care for more patients remotely, it could potentially avoid hundreds of millions in construction costs.
“I believe that longer term we’ll see at least 20 percent less utilization inside the four walls,” Wing says. Adventist Health had been considering building a couple new hospitals, but may no longer pursue those plans, he says.
Keeping patients healthy
Telehealth can also play an important role in helping patients before they reach the point of needing hospital care. When non-urgent procedures were canceled during the early months of the pandemic, many Americans turned to virtual visits to keep up with routine treatment and ask for guidance from health care providers before venturing into offices.
While some doctors have returned to in-person visits, telehealth remains an important component of many practices, says Dr. Joseph Kvedar, a dermatologist in Massachusetts and president of the American Telemedicine Association. Physicians in his office have all added a half day of telehealth onto their in-person schedules so that they can keep the number of patients in the waiting room low and minimize their exposure to the coronavirus.
Even emergency rooms, which typically serve the purpose of receiving unexpected in-person visits, have turned to telehealth. This spring, the University of Virginia started a virtual urgent care service to address smaller problems without requiring patients to come to the hospital. UVA also expanded its remote monitoring program to keep tabs on patients quarantined at home with COVID-19.
And as nursing homes and other congregate care settings saw massive outbreaks of the virus, University of Virginia doctors developed a telemedicine strategy that allowed them to partner with long-term care facilities, rapidly deploy technology, coordinate care with on-site nursing staff and reduce hospitalizations.
These kinds of programs do require large investments in technology and training, UVA’s Rheuban says, but in the long-term, she has seen that telemedicine “diminishes the need for in person visits and improves clinical outcomes.”
Paying for the care
For these innovations to continue, doctors and health systems need to convince insurers—or lawmakers—that virtual services go beyond convenience and are important for treating a broad range of conditions. Already, commercial insurers are raising questions. “Since we’ve had this explosive growth, we don’t necessarily know what the impact on patient outcomes has been,” says Kate Berry, senior vice president of clinical affairs and strategic partnerships at America’s Health Insurance Plans (AHIP), the industry’s main lobbying group.
During the pandemic, many major insurers have reimbursed telehealth at the same rates as in-person visits. Some have said they will continue these rates until the end of the year, while others have not made decisions past September or October. AHIP says it wants patients to have access to telehealth, but is opposed to laws that would mandate coverage or require insurers to reimburse telehealth at specific rates.
Nancy Foster, vice president of quality and patient safety policy at the American Hospital Association, says that some of her organization’s members have already heard from insurers that don’t plan to cover telehealth beyond the emergency, or that only want to cover it at reduced rates. “They seem to be taking some steps back, which is unfortunate,” she says. “It may be yet another thing that creates a greater opportunity for the wealthy than for those who are unable to afford the additional cost of paying for it themselves.”
The AHA supports the changes that CMS has made and is advocating for Congress to pass legislation that would allow more permanent flexibility in where patients could be and what technologies they use to access telehealth.
But cost is still a central concern for lawmakers and insurers. “There have been a bunch of barriers to telehealth,” says Glenn Melnick, a health care economist at the University of Southern California who studies hospital systems. “If you take those out of the equation, utilization is going to go up.”
In the current system where each visit means a separate fee, this could add up quickly. Physicians typically argue that telehealth should be paid the same as in-person care because the work is equally complex and time-consuming, but insurers will want to find savings. “It’s sort of a balancing act,” says Josh Seidman, managing director at consulting firm Avalere Health. “There are going to be a lot of changes over the next six to 12 months that will last long term in terms of how care is delivered and paid for.”
In the meantime, Medically Home and its hospital partners are working to secure more commitments from private and government insurers to cover their care. Both Adventist Health and Tufts are excited with the results of the program so far, but their leaders say the program’s ability to scale remains to be seen.
Carlson, the patient in California, had his stay covered by his state Medicaid plan, and says he would choose the at-home model again if he needs care in the future. After four days of treatment at home, his doctors determined he was ready to be discharged. But before the Adventist team moved forward, they helped Carlson find a primary care physician, transitioned his records and relevant information, and made sure he scheduled a follow up appointment. The tech team arrived to pick up the equipment and Carlson remained in place. “No complaints,” he says.
from Blogger https://ift.tt/3ktuZ62 via IFTTT
0 notes
Text
Life in the healthcare environment By Hector Shan

Reflection
Guided from Scott Christ’s article “7 Powerful Questions To Find Out What You Want To Do With Your Life,” I was able to put into perspective my aspirations. My greatest passions in life involve soccer and biology. I have played soccer since I was 5 years old. In Panama, soccer was the main source of entertainment for kids in our neighborhood. The reason biology is also my passion is because I believe it is interesting to understand how life works. Biology has always been a subject in which I excelled in since middle school which inclined me to pursue it in college.
I am currently a pre-med major and I aspire to become a physician hopefully specialized in dermatology. I want to specialize in dermatology because ever since I started going through puberty I have dealt with acne. During that time, I used to stress over how to get rid of it and ventured in the field of skincare looking for answers. As I ventured, I realized that I found a deep interest in deep interest in understanding how the skin functions and its properties. Therefore, I began to look into what it takes to become a dermatologist and discovered it was a highly competitive field to attempt to get into, but that it also was one of the less grueling fields to specialize in due to its high paying salary and its usual 8 hour job shifts. The high paying salary is an important factor for me because I am trying to lead a steady lifestyle in which I can live comfortably and take care of other of my family members as well. I understand that in order to achieve my dreams I will have to stay focused and work as hard and smart as I can to realize them. For more information on the physician career path, I utilized the Occupational Outlook Handbook.
Physician Career Path
According to the Occupational Outlook Handbook entry “Physicians and Surgeons,” the occupation of physicians is to diagnose and treat diseases. There are two types of physicians: M.D. (Medical Doctors) or D.O. (Doctor of Osteopathic Medicine). Both involve similar methods, but D.O.s tend to concentrate on whole-person patient care rather than specializing in a specific field. Therefore, D.O.s are most likely to become primary care physicians. They typically work in hospitals or for the government. Some even own their own private practices. Solo practitioners tend to have more freedom than employed physicians due to abiding to public hospital rules and schedules. Surgeons and anesthesiologists have the most grueling job in which they have to work for longer periods of time and be called in case of emergencies.
The path to becoming a physician is not an easy one. They require a bachelor’s degree and a medical school degree which take 4 years each to obtain. They have one of the highest paying wages in the United States with an average wage of $208,000 per year. The employment rate for physicians is expected to grow 7 percent from 2018 to 2028. The rate of growth is the fastest compared to other occupations because of the growing and aging population. A great way to understand this topic thoroughly is by interviewing someone working in the healthcare field.
Life in healthcare

To find out more about the healthcare career environment, I interviewed my mother’s friend named Betzaida Feliz who is a nurse/caregiver. Betzaida used to work in a hospital as a registered nurse, but then decided to work at a nursing home as a caregiver due to her leaving the country for a few years and not renovating her license. In her early childhood, she used to play with her neighborhood friends and one of the favorite games they would play would be “Hospital.” They would act as if someone was sick and use a stethoscope to give fake diagnosis to each other. She said ever since then she realized she had a strong passion for helping others and interest in healthcare.
She did her undergraduate in Panama and jokingly told me that the first year of college she did not take it seriously at all because she was constantly partying. During that time of her life, her grades were suffering greatly and she realized if she wanted to realize her dream she had to commit. After that, she would find herself constantly in the library studying and ignoring her couple of friends that still insisted on partying. As she told me her story, I realized my first year of college was similar even though I am not really the partying type, but I also slacked on certain things which I could have done way better. She proceeded to tell me that once she graduated, she shortly left to live in the United States to start a family. When she got her first job as a nurse, it was slightly hard for her to adapt to a fast paced environment in which she was not used to the language yet, but with time she grew accustomed. I asked her what are the qualities needed for a person to work in healthcare and Betzaida said, “You need to be kind, patient, smart and compassionate.”
She emphasized patience because she says many patients in a hospital setting can be rude and stubborn. She mentioned how a couple of times older patients did not want to get attended by her because of her racial background, but she did not let this get to her head and stop her from doing her job. She mentioned that sometimes patients families would tell the doctors that they did not want her attending their family members because she was not doing her job correctly, but she believes they were all lies to cover up their racial motives. what infuriated her the most is that the hospital would sometimes abide to the bidding just to avoid more conflict, even though they knew she was doing her job correctly.
During her time working at the hospital, she worked 12 hours shifts 3 days a week. She said she was constantly exhausted because the 12 hour shifts were grueling and felt a great relief once she got to her house to see her family. As a caregiver, she now deals with a slower-paced work environment with less stress, but the than is less than a nurse working in the hospital setting. Therefore, she mentioned that even though working as a nurse was more stressful the pay made her overcome her issues with the job. Even though she is getting paid less as a caregiver, she is still comfortable with the job as it still covers most of her major expenses. Overall, I learned from her stories and they gave me a basis to guide myself on for my life journey. To have better insight into what becoming a physician involves, I used a current event article from the New York Times.
Current event affecting the healthcare environment
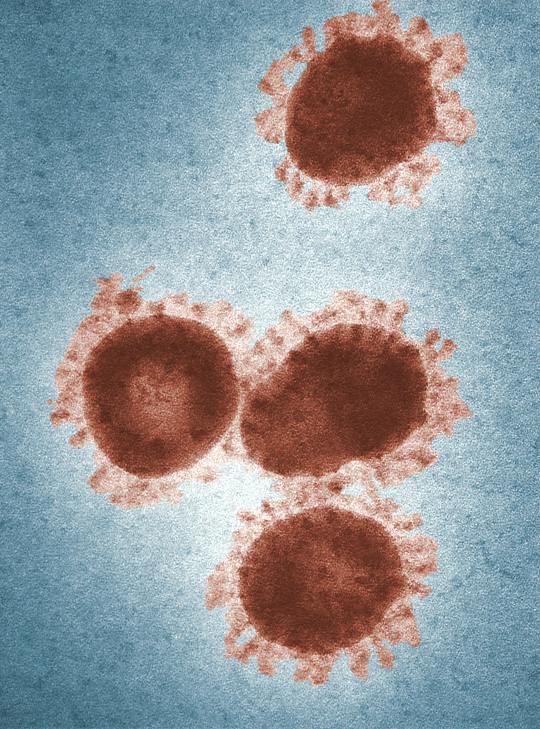
According to the New York Times article “How to Prepare for the Coronavirus, ” Gina Kolata states that the Coronavirus is a virus which is named due to the crown-looking structures on its surface. The virus believed to have originated from Wuhan,China and has affected around 80,000 people in 33 countries. The virus has also shown to be moderately infectious close to the SARS and is most likely conveyed through coughs, sneezes and contaminated objects. The World Health Organization has been working with Chinese officials to contain the virus, but cases have recently spiked on two continents and experts believe the world is not ready for a major outbreak.
According to Gina Kolata, american health officials warned on February 25th that the Coronavirus is predisposed to affect communities in the United States and advised the people to get their families prepared. Infectious disease experts recommend people to not havoc and use common sense. The Coronavirus expert Dr. Stanley Perlman said “if you see someone on a bus who is coughing, move away.” Americans tend to ignore diseases and continue on with their daily lifestyles until the sickness worsens. The article recommends Americans to not care about hurting someone else's feelings and to actually set a distance between them and a sick person. A distance of at least six feet would be helpful in the avoiding transmission of an infection. It also recommends people to constantly watch their hands especially whenever it is possible they have sullied them with bacteria or viruses. The reason I chose this article is because it is currently a major issue which has affected today's society unexpectedly and countries all over the world are trying to deal with the outbreak.
The topic is also of high importance because much is not known of the Coronavirus and it is essential to educate others on what is known in order to prevent further spread of the disease. The article relates to my career which involves becoming a physician because doctors, nurse, and scientists are the ones that directly dealing with the infected of the Coronavirus and are currently finding ways to control the disease. I have learned from this article that people in general should now be mindful if sick and not expose others with any contagious diseases as much as possible. The career connections project allowed me to organize my ideas on what I want to do with my life. I learned a lot from researching my career path and discovering new aspects from it.
0 notes
Text
No Filter - Dealing with Rosacea
In February 2019, I noticed a small, red patch on the left side of my face. I didn’t think much of it.

I figured I had a pimple or skin irritation that would soon go away. I put concealer on it and tried to forget about it. Little did I know that this small red patch would end up covering my entire face and cause months of doctor appointments, tons of money, and even a trip to the emergency room. The redness on my face turned out to be a type of Rosacea. Rosacea is a condition that causes redness and sometimes small acne-like bumps on the face and is common in middle-aged women.
Initially, I saw my primary doctor who thought I may have had a bacterial rash that I could have caught while on vacation at Universal Studios Orlando. We rode several water rides and I had picked the area thinking it was a pimple. She cultured the area and put me on antibiotics. The area did not improve, so she sent me to a dermatologist. The dermatologist suggested it was a type of contact dermatitis. He asked me several questions about what products I was using and what types of things I come into contact with. Nothing was out of the ordinary but he gave me a topical hydrocortisone and told me to be mindful of what I was using. Soon after that, the rash that had been isolated to the left side of my face spread to the right side and became more painful.

In frustration I returned to the dermatologist who then told me that “a lot of people have problems we can’t figure out.” He made me feel awful. I felt embarrassed about how my skin looked, and was in a lot of pain. It was swollen and felt like a horrible sunburn that I couldn’t get rid of. I became more and more depressed.
I returned to my primary doctor and she prescribed a low-level dosage of doxycycline, which seemed to help a little. She also ran blood panels and they revealed a positive ANA, which meant antinuclear bodies were found in my blood. This prompted my doctor to send me to a rheumatologist. Often, a positive ANA can indicate Lupus.
Even with this potential prognosis, I wasn’t about to miss out on riding roller coasters. Tim and I made our first trip to Cedar Point in mid-May. We had Fast Lane Plus and rode as many rides as we could, a large portion of them being on Steel Vengeance. By the end of that day, my face was killing me. By Sunday night of that same weekend my face was so swollen and red that we went to the emergency room. I became worried when I noticed the swelling had progressed down to my neck. The ER did nothing and told me to follow through with the rheumatologist, as it was probably Lupus.



I went to the rheumatologist the next day, which required me to miss work. My face was bright red and very sore. They did x-rays and numerous blood tests. She told me that she doubted I had Lupus, but we would see what the tests revealed. After I described my first visit to the dermatologist, she suggested I find another doctor.


The test results were returned and, thankfully, negative for Lupus.
I was able to schedule an appointment with a PA at another local dermatologist’s office. At this point, I was an emotional wreck. My husband went with me and I broke into tears as I waited for her to see me. I had all my records sent over and explained everything I had gone through for the last four months. She was so kind and understanding as she listened to my story. She then proceeded to tell me she thought I had an unusual type of Rosacea. She prescribed me a higher dose of Doxycycline and daily antibiotic cream. She said to see how I respond and we could go from there. This appointment was June 3rd and by my brothers wedding on the 15th, I was feeling and looking like myself again.




The PA I saw told me some important things I would need to change in order to manage my Rosacea. One of the most important things is protecting my skin from the sun by wearing a non-irritating lotion with no lower than a 30 SPF rating. While researching, I discovered that there are both physical and chemical sunscreens. Physical sunscreens tend to be less irritating to people with sensitive skin as it does not absorb into the skin like chemical sunscreens. In addition to daily sunscreen, careful use of facial products is also necessary. People with Rosacea tend to be sensitive to products containing fragrance and alcohol.


She also suggested the importance of wearing a hat while outside. Some of my Cedar Point pictures and videos after May, you will notice I was wearing a hat. I’m not quite ready for the wide-brimmed hats as she suggested! I tried some on in the store for a laugh but a ball cap is much more my style.



Stress is also a huge trigger. It’s difficult not to get upset when something is happening to you that you really can’t control. I’ve been working on going to yoga and exercising more as a way to release some tension.

I’m glad I found a doctor to finally help me discover what was going on. I have improved, but I still have bad days and flares. As a result I’ve made some life changes. It’s embarrassing to share some of these photos of my skin at its worst but I’m happy to share this story in the hope that it can help someone else. I have found some other great blogs and posts online of people sharing their experience with Rosacea. This blogger shares some great info on her page: https://talontedlex.co.uk/
If you have any questions or suggestions, please feel free to contact me. I’d love to hear from you.
0 notes
Note
Hey! So this is kind of a weird question, but you commented on some other post about skin care/acne that you have had good results with Adapalene gel. Im someone who has pretty bad skin so I was twice a day and moisturize and stuff and a year or so ago my doctor prescribed an antibiotic and the gel. I'm off the antibiotic now, but I'm haven't see a whole lot of results with the gel. I'm thinking maybe I'm using it wrong or something? What was your routine with it? Thanks!
Hi! Not a problem at all, I’d love to help!
I actually used a topical antibiotic last year for 2 months (I was prescribed 1 month, but it just made my skin worse, so I kept using it hoping it would improve...it didn’t) and definitely understand the frustration. If you don’t mind my asking, how long have you been using Adapalene gel? For me, it got worse before it got better (for the first 4-5 weeks, I broke out so much more/in places i normally didn’t usually get pimples). However, around weeks 6-8 new pimples gradually stopped appearing and the existing ones started to disappear. Just keep that in mind, because it does take a while to see results, but at week 18ish where I am now, I think it was definitely worth it!
Sorry for the lengthy preamble, but I’m going to finally answer your question now haha. So my routine is pretty simple since I also realized I’d been harming my skin with harsh scrubs and spot treatments (cough cough salicylic acid and benzoyl peroxide). Also the water in my college dorm was really bad, so I switched to micellar water.
Morning:
1) Cleanse with Micellar Water - I wet a cotton pad with micellar water (I recommend the Simple brand. I started out with Garnier, but like Simple better) and thoroughly wipe my face and neck.
2) Wash Hands - and wait for my face to air dry (sometimes I fan my face with my hands lol).
3) Moisturize and Sunscreen* - once dry, I apply moisturizer and then sunscreen. I used to use Olay complete moisturizer/sunscreen so it went on at the same time, but now I use Lush Vanishing Cream and Aveeno sunscreen.
*Optional: Primer/Makeup in Between - If I wear makeup, I would wait about 5 minutes after moisturizing to put on primer (and let that sink in for about 2 minutes) before using concealer/BB cream/both depending on the day.
Basically just make sure your hands/brushes/sponges are clean whenever touching your face!
Night:
1) Remove Makeup (if you have any on) - I use Simple Cleansing face wipes (I know people frown on not actually using cleanser and water on your face, but again my dorm water is gross and I usually don’t wear much make-up. Just be really thorough!
2) Cleanse with Micellar Water - pretty much the same as the morning, but I’ll occasionally use an extra pad or two depending on how dirty my face has gotten/how much makeup is left.
3) Adapalene Gel - I squeeze out a pea-sized drop onto my left index finger (having washed my hands before!) and kind of dab it with my right index finger to pick up like 1/4 of it and make dots on my forehead and nose. I rub that in gently, then get another 1/4 each to dot each cheek, and use the last 1/4 on my chin/neck area.
4) Turn off the lights! - I believe light deactivates some of the chemicals in the gel and makes it less effective, so I don’t put it on until I’m ready to go to bed.
Notes:-I don’t moisturize my skin at night because I feel like my Adapalene gel is hydrating and does a good enough job, but if you have dry skin, then I would recommend using it after step two.-I know micellar water sounds like a big jump and if you’re more comfortable washing your face in a sink, that’s totally understandable! If you’re concerned at all about your tap water, a friend’s dermatologist told her she uses bottled water to wash her face so you could try that.-If you want to continue using a topical antibiotic, I’ve heard that you can do it in the morning, right after you wash off the Adapalene gel.
Sorry again for the super lengthy response, but I hope this helps; just be patient and stick with it--hopefully you’ll see results soon! Feel free to ask if you have more questions, or just let me know how it’s going :)
1 note
·
View note
Text
Mystery Health Issue?
So on June 3rd I broke out between my legs. They were little circular itchy splotches between my legs. They itched like crazy. I thought - since I’ve gotten them before and I’m a thicker girl - it was heat hives. Which are a thing.
I went home, took two Benadryl’s and put topical ointment on my legs and went to sleep. I woke up about five hours later with my face swollen and my body still itchy. I had to call into work and I went to Urgent care. Urgent care couldn’t do anything for me. They told me everything I had done was all they would suggest and with my face swollen up, it was an ER job now. So I went to ER
I’m the ER they gave me a shot, gave me three pills, two of which were Benadryl, and then I was sent home. One of the pills they issued me was Prednisone. Which is a steroid. And they had me get Benadryl topical ointment. Anyway I took it, went to bed, then the next day I’m feeling fine. I’m not itching anymore, the swelling went down. It’s June 4th by this point. And I went to a swap meet and walked around a bit before coming home
When I got home I was swelling up again and itching everywhere. I had to call into work. Once again I went to the ER. They gave me two shots, and more Benadryl and another allergy pill. Me and my mom were in the room for awhile. The itching wouldn’t stop even with two shots and the Benadryl. So then they gave me an antihistamine. That somewhat helped but not really. I was still fairly swollen. And still fairly itchy. But they simply sent me home. With more Prednisone. Woopie.
Saturday rolls around and I’m again at an ER. This time a different one since the other place wasn’t helping. They check me over but because I can breath there’s not much they can do. They give me - surprise - more steroid shots, an antihistamine shot, and an epi pen shot. I’m given more medication- more Prednisone and a few other drugs - before they’re sending me home again with my mother.
Sunday rolls around - June 6th at this point - and I had gone to sleep with no clothes on. Hoping I could sleep - after I hadn’t actually gotten much sleep due to my itching - and not itch as much. It sort of worked and I got a marginal amount of sleep. It’s noon when I try to get out of bed… And realize that I can’t move. As in my entire body has locked up and I have no way of walking. If you’ve ever felt your legs fall asleep then tried to stand up and walk on them, then it was somewhat like that. But while also wearing exercise weights. Like the ones Goku trains in… I couldn’t sit up. I had to literally grab the bed and pull. My body was dead weight. I sat up - with difficulty because my body tried to fold in on itself as I sat in bed - and grabbed a towel on the end of my bed to wrap around my naked self.
I Waite until I could somewhat feel my feet before trying to walk… Bad idea. I stumbled side to side while trying to hold the towel around my body. I fell out of my bedroom like a drunk, crying but laughing because I was so scared of what was happening. I fell in front of mom and stumbled to the bathroom - which is diagonal from my room - unable to lift my legs and my arms up, clutching my towel and scared. My mom - later - would say that with my face being so puffy on one side and me falling to one side more that the other - that she thought I was having a stroke. Or a TIA. Either way it scared her. She had me try to sit down. I say “try” because I couldn’t. I could not get my body to sit on the toilet. Instead I fell over when I tried and was trying to hold myself up on my left side because that’s the side I fell on and where all my weight was trying to go. And instead I fell forward off the toilet. Sliding on my arm rather comically as my younger brother walked by, oblivious to me falling in the bathroom.
I laid on the floor until slowly I got strength in my body to move. Well crawl. I crawled - clutching a towel around me still - until my mom got me one of dads sleep shirts and a pair of boy shorts to put on - with difficulty. Now mind you, the whole time I was bumbling from my bedroom, I could not talk. My words were slurred and I sounded drunk. And when these episodes happen - because that’s right friends, they keep happening- I can’t speak properly. I legitimately sound drunk and I can’t form full coherent thoughts. I struggle to talk and think when these happen.
Obviously spooked, mom and dad rush me to the second ER I had gone to on the 5th. They get me in quickly and assess me. The doctor that sees me is a nice young guy, but immediately he’s thinking I’m having a stroke and/or a TIA. I can not explain what I had happen very well. It took five times of me trying to explain what I felt and what happened to the man. Again I can’t form coherent thoughts and when I try to talk, it’s all garbled or I repeat myself a lot. But eventually he understood what I was saying. He believed the. That it wasn’t a stroke. That I was being pumped full of enough steroids to take out five people and my body was freaking out. So they said no more steroids, take these different meds instead. So I did that. Once again they wouldn’t admit me because I could still breath and wasn’t having a stroke at all. So I was sent home again… Yeah
Monday the 7th rolls around. Grandma comes to pick me up for a visit with a dermatologist. By this point I’m still broken out in hives and itching. But the new meds they gave me - the antihistamine- are helping the hives and itching go down. Well the dermatologist takes a look and is startled by the hives I got. She admits she’s never seen this many hives on a single person. I ask if I could’ve rolled around in something. She explains that you don’t get hives from contact on the skin you get them from ingesting something or they’re idiopathic. Which means I was or had ingested something that triggered these hives and my swelling or they’re chronic and I may never know what caused them. As for my muscles shutting down - which was still happening- she had no idea.
Well after my dermatologist visit, I went to get food with grandma… But then the locking up thing happened… And I couldn’t move. So grandma got upset and took me to the ER. This time to the one I 1st went to when everything started. They got me into the back quick, gave me meds, and I talked with a rather essentric but caring doctor who I told everything to. And he fully assessed “you are not having a stroke, I’ve had enough stroke victims to recognize the signs”. He assessed that my body was panicking from all the meds I’d been pumped with and was dealing with and it was trying to protect me so it started shutting me down basically. So he said “no more prednisone”. Which I wasn’t taking because it wasn’t helping anyway. And two just take the antihistamines until they’re finished.
Now by the 11th I was no longer covered in hives. I still felt off - weak and a bit disoriented and I got sick if I got hot or went outside for too long - but I was feeling better. I didn’t have any limb locking at all… Fast forward to tonight. Embarrassingly I had to call the county EMS to come check on me. My limbs had locked up on my left side. First my whole body felt heavy and stiff. I got a little dizzy and then my left side locked up. For a solid 5 minutes I sat locked up. Before I had to call EMS. And then came the guys I work with. They’re all concerned and looking at me confused as EMS checks my blood pressure and heart and I’m anxious and annoyed and it makes me cry. Which is extra embarrassing. Who wants to cry in front of coworkers? Not me.
Anyway I had to sign paperwork that I didn’t want them taking me to the damn ER. Because I couldn’t stand the very idea of going to the ER again when they’ll - again - tell me they can’t do anything and then send me on my way. But now I gotta get a doctor’s note saying I can be at work. So I gotta go to the doctor anyway 😭
I have no clue what’s going on with me. I’m annoyed and mildly scared and confused…
Last week during all this was supposed to be my vacation… Fuck me sideways 😓
16 notes
·
View notes
Link
Kenyon Strother loves almost every aspect of his job as a hospitality professional at Chick-fil-A. He works in the kitchen of a South Carolina franchise of the fast-food chain, cooking meats and vegetables, and says the company has “great benefits and good wages.”
There’s just one problem: The employee dress code requires him to be clean-shaven. That’s a challenge for Strother because, like many black men, frequent shaving causes him to develop razor bumps, which can lead to dark marks, scar tissue, and even infection.
In addition to painting a very narrow image of what constitutes professionalism, bans on facial hair pose medical risks for men who suffer from razor bumps and can alienate men who wear beards for religious reasons.
Restrictions on beards pose more barriers to employment for men of color, particularly black men and Indian Americans who practice Sikhism, one of the world’s largest religions. Men from both groups have sued over beard bans, but a corporate sector that has historically normalized whiteness and “othered” minorities continues to prohibit facial hair.
Sikh men have filed multiple lawsuits related to the discrimination they face because of facial hair. Westend61/Getty Images
Razor bumps, known medically as pseudofolliculitis barbae, are an inflammatory skin condition. They mostly affect people with coarse, curly hair who remove it by shaving or plucking. When tightly coiled hair is shaved closely, it may retract below the skin’s surface and break through the follicle wall. The razor bumps that result can lead to dark marks, scar tissue, and even infection.
The best treatment for the problem is to stop shaving altogether, but many men work for companies that bar facial hair. Workers in food service, the military, and public service jobs commonly run into such bans. And men who run Fortune 500 companies typically don’t have facial hair either, but that trend may be changing. Younger executives, such as Google’s Sundar Pichai and Sergey Brin, wear beards, as did Steve Jobs later in his career.
Just having facial hair can make men targets of employment discrimination. Practicing Sikhs, who wear beards for religious reasons, have filed lawsuits against companies that have denied them jobs because of their appearance. Medical groups, convenience stores, and even the US Army have been sued for discriminating against Sikhs because of their beards.
Kenyon Strother first raised concerns about his Chick-fil-A’s facial hair ban during his employee orientation four months ago. He recalled a human resources officer telling him that perhaps he’d be the one to change the company’s policy. Although Strother put a petition on Coworker.org to lift the beard ban that has garnered 1,600 signatures, spoken to his managers, and even presented them with a doctor’s note about his medical condition, he said Chick-fil-A has not budged on its policy or exempted him from the clean-shaven rule. (Chick-fil-A did not respond to a request for comment about their grooming policies.)
“My wife is a nurse, and she said, ‘You’re going to have scar tissue,’” Strother said. “I’m literally shaving over the razor bumps. I’ve tried clippers. I’ve tried one-blade straight razors. I spent money on steroid creams for my neck. I’m almost in tears when I shave because I start bleeding. I have to take Tylenol it’s so bad.”
Dr. Carlos Charles, a New York City dermatologist who specializes in treating patients of color, said that he’s seen a number of men struggle with razor bumps while working for organizations that prohibit facial hair. At his New York City practice, Derma di Colore, he’s treated city workers, like policemen and firefighters, with the condition, and he calls pseudofolliculitis barbae “a huge issue.”
“It’s really challenging for any man irrespective of work environment,” Charles said. “We try to give them some advice along the line of shaving correctly, shaving with the grain of the hair, using a sharp blade. We’ll also prescribe different topical creams, some retinoids, topical antibiotics.”
Entrepreneur and NBA star LeBron James with a beard. Many black men wear facial hair to avoid razor bumps. Michael N. Todaro/FilmMagic
Laser hair removal is one of the most effective ways to remove unwanted hair for those with condition, but it is also among the most expensive treatments. Charles says each treatment can cost about $200 per session, and monthly rounds are typically needed as well as maintenance visits afterward, which may be unaffordable to some people. Charles said that he’s helped plenty of patients without going this route, but for men whose skin has been resistant to other kinds of treatment, laser hair removal may prove helpful.
Entrepreneurs have also cultivated products that target the problem, such as Tristan Walker of Walker and Co. Brands, whose Bevel shave system and trimmer was developed with men of color in mind.
The shaving system uses a straight razor that helps users remove hair at skin level rather than beneath the skin’s surface, Walker explained. Fifty years ago men of all ethnic backgrounds shaved with such razors, which eliminated pulling and tugging, he said. But multi-blade commercial razors grew in popularity, leaving black men vulnerable to razor bumps.
“Large companies have not tried to solve the problem,” Walker said of razor bumps. “A lot of the mass market razors are multi-blade and pull hair from beneath the surface, and then it’s going to grow into your skin [causing razor bumps].” Because many of the shaving products on the market are alcohol-based, which dries out the skin and exacerbates irritation, he’s also developed products that aim to moisturize.
“I really wanted to solve my own problem,” Walker said.
Like Charles, Walker said he routinely hears from black men who must shave for work.
“In the military, there are men of color who have to shave every single day,” he said. “They have to fill out forms to get permission not to shave every day.”
Years ago when he worked on Wall Street as an intern for an investment bank, Walker said he was criticized for showing up on the trading floor with facial hair, an incident he found unsettling. “No one has shown me that I perform better at work with a clean-shaven face,” he said.
While some men have medical or religious reasons for wearing beards, others simply have trouble making the time to shave regularly. Count Brandon Wesley among them. He started working at the Publix grocery store chain in Florida about five years ago as a high school student. But once he entered college, balancing work and school stretched his time thin; after class, he had to race home to shave before starting his Publix shift.
Three years ago, he started a petition asking the company to change its grooming policy. After the petition garnered more than 21,000 signatures, Publix recently announced that September 28 would be the last day of its beard ban. (Publix did not respond to a request for comment.)
“It was pretty awesome,” said Wesley of the news. “I’m glad everyone kept [the petition] going. I am super excited. I didn’t once doubt that the [new policy] was going to pass; I just knew it wasn’t going to take time. It’s truly an issue within the company. ”
Wesley, who has worked as a bagger, cashier, and shelf stocker for Publix, said that he never received a clear reason for why the company implemented the beard ban. He suspects the company viewed clean-shaven workers as more professional-looking.
Strother said that he’s not clear on why Chick-fil-A has a beard ban either. Because he cooks, managers have raised concerns that his facial hair could get into food, but a beard net would lessen that possibility. He hopes the new Publix policy will influence Chick-fil-A to change its grooming requirements.
“This rule was put into place decades ago, when mostly white people worked for the company,” Strother said. “I have no problem following rules. I just like following rules that make sense.”
Original Source -> Why workplace bans on facial hair marginalize men of color
via The Conservative Brief
0 notes
Link
When Curtis Carlson started having back pain this spring, he tried to put off seeing a doctor. The COVID-19 pandemic was raging, his job at a transitional housing organization in Ukiah, Calif. was busier than ever amid the economic collapse, and a hospital seemed like the last place he wanted to be.
But when he finally took himself to the emergency room and he was diagnosed with a kidney infection, Carlson figured he would have no choice but to stay. Instead, his doctors told him about a new program that would allow him to finish the rest of his hospital care at home, with a medical team monitoring him virtually around the clock and making in-person visits multiple times each day.
“I was blown away,” says Carlson, 49. When it became clear that staff would set up the equipment, which all fit on a TV tray, in Carlson’s home, and that he’d be able to communicate with his medical team via iPad, he was on board. “It was easy enough that I could use it, which was awesome,” says Carlson, who describes himself as “terrible” at technology.
Carlson’s experience was revolutionary, he says. After one night in the hospital, he was back at home with his wife and their four sons. “The biggest part for me was when I got home, seeing the look of relief on my seven-year-old’s face,” Carlson recalls. “While they were putting in the electrical wizardry, I asked him, ‘Were you worried about me?’ You could see him just crumble a little bit. He was definitely very happy Dad was home.”
Hospital administrators at Adventist Health, the system that runs the Ukiah hospital where Carlson went for care, had been looking for ways to reach rural patients outside their hospitals for years. But when the COVID-19 pandemic came to California this spring, administrators felt the timeline collapse. After finding the right technology in April, they began offering the service to patients like Carlson within 29 days. By May, Adventist Health had the infrastructure ready to care for 200 patients in their own homes.
Adventist is not alone in its warp-speed embrace of new technology during COVID-19. In recent months, hospitals around the country, looking for ways to free up beds for coronavirus patients, began expanding their virtual offerings, launching video doctors’ visits and virtual therapy sessions, and rolling out programs to remotely monitor vulnerable patients, like those in nursing homes. As doctors and patients embraced these new, online methods of care, Medicare, Medicaid and many private insurers temporarily changed their payment rules to accommodate them. But many of these changes are only guaranteed through October, and plenty of regulatory hurdles remain.
Now that it’s clear the pandemic is not going away anytime soon, medical providers and hospital administrators say they need more substantial reforms to ensure their investments in telehealth can continue. Whether innovations like remote hospital recovery beds will be available in the long term depends primarily on whether public and private insurers will continue to pay for them. In other words, in the topsy-turvy health care economy of the United States, it’s payment models—not technological ability or patient benefit—that will now determine the future of virtual care.
Hospital care at home
Prior to COVID-19, Medicare only covered telehealth services from certain providers. It also generally required telehealth patients to be located in a rural area and at a medical facility. Many Medicaid plans and most private insurers had similar restrictions. But after the coronavirus outbreak this spring forced nearly all doctors to stop seeing patients in-person, the Centers for Medicare and Medicaid Services (CMS) issued a number of waivers relaxing these rules, and private insurers followed suit.
Once CMS led the way, private insurers temporarily changed their rules too, and telehealth usage exploded. Between April 2019 and April 2020, telehealth claims increased 8,336%, according to FAIR Health, a nonprofit that analyzes private health insurance claims. More than nine million Medicare beneficiaries used telehealth services during the first three months of the crisis. And at University of Virginia’s network, which already had a more robust telehealth program than many others, virtual visits increased 9,000% between February and May.
“COVID-19 changed everything when it comes to telemedicine services,” says Dr. Karen Rheuban, director of the University of Virginia Center for Telehealth. “The genie’s not going back in the bottle.”
The Trump Administration is now pushing for more telehealth access. On Aug. 3, the President signed an executive order calling on CMS to permanently expand the kinds of telehealth services that Medicare covers, and the agency’s administrator Seema Verma has also said she believes access to telehealth should continue beyond the public health emergency. Broader expansions would need to come from Congress, where dozens of bills on telehealth have been introduced in recent months, but lawmakers have not yet seriously considered the topic.

Courtesy of Adventist HealthCurtis Carlson and his family at their home in Ukiah, California.
Telehealth advocates say now is the time to act. A range of virtual offerings could be revolutionary for patients who are seriously sick, need long-term care, or live in rural areas, where hospital closings have left millions of Americans without easy access to treatment. “The environment in a hospital, although it’s very conducive to high intensity care, is not that conducive to being able to engage in normal activities of daily living that might be actually important for recovery,” says Dr. Michael Apkon, president and CEO of Tufts Medical Center.
In March, when Apkon watched Italian hospitals overflow with coronavirus patients, he sped up Tuft’s long-simmering telehealth plans. Apkon called Raphael Rakowski, the CEO of the tech startup Medically Home, and by April, the two organizations had launched a program that would provide hospital-level care in patients’ homes. Rakowski says he’s spent years telling hospitals they could reduce overhead costs and improve the patient experience by embracing care at home. “Sadly, it took a pandemic to amplify the patient’s role in their own care,” he says.
In order to be eligible for the Tufts-Medically Home partnership program, patients must typically have a similar profile to Curtis Carlson: they must have relatively stable health, be suffering from common conditions such as heart failure, diabetes, pneumonia, or kidney infections, and they must have a safe, stable place to live. If a patient meets that criteria, Medically Home provides all the equipment, including communications devices, monitors, backup internet, cell signals and power sources. (Some locations are admitting patients such as those with cancer, COVID-19 or who need longer-term care, and over time those will grow, says Rakowski.)
In Boston, where Medically Home is based, the tech company itself employs nurses, paramedics and other staffers who visit the Tufts patients in person several times each day to administer IVs, do blood tests or provide other care, and the patient checks in with their doctors via video. In California, where Carlson was treated, and in other locations, Medically Home’s partner hospitals provide the staff. Teams of nurses and physicians also monitor each patient 24 hours a day from a “command center,” and can be reached immediately if any questions or complications arise.
Even accounting for the time and cost of staff traveling to visit patients at their homes, Rakowski says at-home hospitalization costs about 20 to 25% less on average than care in a traditional hospital setting. In California, where Carlson was one of Adventist Health’s first patients to use the Medically Home model, Adventist Health President Bill Wing sees significant savings in the future. Maintaining hospital facilities and building new infrastructure is very expensive, he notes, so if Adventist Health can care for more patients remotely, it could potentially avoid hundreds of millions in construction costs.
“I believe that longer term we’ll see at least 20 percent less utilization inside the four walls,” Wing says. Adventist Health had been considering building a couple new hospitals, but may no longer pursue those plans, he says.
Keeping patients healthy
Telehealth can also play an important role in helping patients before they reach the point of needing hospital care. When non-urgent procedures were canceled during the early months of the pandemic, many Americans turned to virtual visits to keep up with routine treatment and ask for guidance from health care providers before venturing into offices.
While some doctors have returned to in-person visits, telehealth remains an important component of many practices, says Dr. Joseph Kvedar, a dermatologist in Massachusetts and president of the American Telemedicine Association. Physicians in his office have all added a half day of telehealth onto their in-person schedules so that they can keep the number of patients in the waiting room low and minimize their exposure to the coronavirus.
Even emergency rooms, which typically serve the purpose of receiving unexpected in-person visits, have turned to telehealth. This spring, the University of Virginia started a virtual urgent care service to address smaller problems without requiring patients to come to the hospital. UVA also expanded its remote monitoring program to keep tabs on patients quarantined at home with COVID-19.
And as nursing homes and other congregate care settings saw massive outbreaks of the virus, University of Virginia doctors developed a telemedicine strategy that allowed them to partner with long-term care facilities, rapidly deploy technology, coordinate care with on-site nursing staff and reduce hospitalizations.
These kinds of programs do require large investments in technology and training, UVA’s Rheuban says, but in the long-term, she has seen that telemedicine “diminishes the need for in person visits and improves clinical outcomes.”
Paying for the care
For these innovations to continue, doctors and health systems need to convince insurers—or lawmakers—that virtual services go beyond convenience and are important for treating a broad range of conditions. Already, commercial insurers are raising questions. “Since we’ve had this explosive growth, we don’t necessarily know what the impact on patient outcomes has been,” says Kate Berry, senior vice president of clinical affairs and strategic partnerships at America’s Health Insurance Plans (AHIP), the industry’s main lobbying group.
During the pandemic, many major insurers have reimbursed telehealth at the same rates as in-person visits. Some have said they will continue these rates until the end of the year, while others have not made decisions past September or October. AHIP says it wants patients to have access to telehealth, but is opposed to laws that would mandate coverage or require insurers to reimburse telehealth at specific rates.
Nancy Foster, vice president of quality and patient safety policy at the American Hospital Association, says that some of her organization’s members have already heard from insurers that don’t plan to cover telehealth beyond the emergency, or that only want to cover it at reduced rates. “They seem to be taking some steps back, which is unfortunate,” she says. “It may be yet another thing that creates a greater opportunity for the wealthy than for those who are unable to afford the additional cost of paying for it themselves.”
The AHA supports the changes that CMS has made and is advocating for Congress to pass legislation that would allow more permanent flexibility in where patients could be and what technologies they use to access telehealth.
But cost is still a central concern for lawmakers and insurers. “There have been a bunch of barriers to telehealth,” says Glenn Melnick, a health care economist at the University of Southern California who studies hospital systems. “If you take those out of the equation, utilization is going to go up.”
In the current system where each visit means a separate fee, this could add up quickly. Physicians typically argue that telehealth should be paid the same as in-person care because the work is equally complex and time-consuming, but insurers will want to find savings. “It’s sort of a balancing act,” says Josh Seidman, managing director at consulting firm Avalere Health. “There are going to be a lot of changes over the next six to 12 months that will last long term in terms of how care is delivered and paid for.”
In the meantime, Medically Home and its hospital partners are working to secure more commitments from private and government insurers to cover their care. Both Adventist Health and Tufts are excited with the results of the program so far, but their leaders say the program’s ability to scale remains to be seen.
Carlson, the patient in California, had his stay covered by his state Medicaid plan, and says he would choose the at-home model again if he needs care in the future. After four days of treatment at home, his doctors determined he was ready to be discharged. But before the Adventist team moved forward, they helped Carlson find a primary care physician, transitioned his records and relevant information, and made sure he scheduled a follow up appointment. The tech team arrived to pick up the equipment and Carlson remained in place. “No complaints,” he says.
0 notes
Text
Meet The Essential Oil That Could Stop Cancer In Its Tracks!
Nowadays, also science verifies that particular kinds of important oils properly quit the growth of cancer, as they cause affected cells to close themselves down.
The power of necessary oils to deal with cancer cells, as well as countless various other illness, is not doubted.
The frequency of a totally healthy body varies from 62 to 78 MHz, as well as the incidence of diseases begins at 58Hz. One test of frequency showed that holding a mug of coffee in only 3 secs reduced the frequency from 66 Hz to 58 MHz, as well as it took 3 days to return to typical. In addition, researchers have actually discovered that the regularity is reduced as a result of unfavorable thoughts, while positive ones boost it by 10 MHz.
The research study carried out on one of the most prominent vital oils, like ginger, mint, lavender, lemon, grapefruit, rose, jasmine, chamomile, cinnamon, and also thyme, revealed that they have the potential to cure cancer. Scientist examined antibacterial potency as well as vitro toxicology against human cancer cell lines.
The discovery of Bruce Tanio, of Tainio Innovation as well as head of the Department of Farming at Eastern Washington College, was called Calibrated Regularity Display (CFM), and it is meant to estimate the frequencies of essential oils as well as their impact on the frequencies of people, after their application.
One such monitor is made use of in the Vital Oils lab, while the other is at Johns Hopkins University, where experts utilize it to take a look at frequencies and also their connect to various diseases.
The immunologist Mahmoud Suhail mentions that " Cancer begins when the DNA code within the cell's center becomes damaged". Consequently, necessary oils have the ability to tell the appropriate DNA code to cells.
There many kinds of essential oils, but a few of them are of bad high quality, as they have actually been incorporated with ingredients as well as alcohol throughout the artificial process of production. You must constantly utilize 100% pure therapeutic grade quality crucial oils, in order to get the desired effects.
The writer of the book The Body Electric, Robert O. Becker, M.D., validates the electric frequency of the human body, as well as its power to impact the wellness of the person.
Even Nikola Tesla stated that the removal of outdoors frequencies that conflicted in the human body will make it resistant to diseases. Likewise, Dr. Otto Warburg was a two-time Nobel Laureate as well as won the Nobel Prize for cancer research, due to his searchings for that our cells have an electric voltage.
There is no question that particular regularities could safeguard the body from illness, while others may make it prone to ailments. Furthermore, higher frequencies ruin the lower ones.
The Therapeutic grade of Vital Oils begins at 52, and mosts likely to 320 MHz, offering the complying with values: Pepper mint 78 MHz, Helichrysum 181 MHz, Lavender 118 MHz, Sandalwood 96 MHz, Ravensara 134 MHz, Incense 105 MHz, Angelica 85 MHz, Rose 320 MHz, Incense 147 MHz, German Camomile 105 MHz, Juniper 98 MHz.
All of these crucial oils have actually been discovered to provide miraculous wellness advantages, and to possess the required recovery residential properties to deal with and also prevent various health problems as well as diseases.
Research has located that thyme, jasmine, cinnamon, and also chamomile oils treat cancer, with chamomile eliminating as much as 93% of afflicted cells artificial insemination. Thyme is much more reliable, ruining up to 97% of cancer cells when it comes to breast cancer.
The journal Industrial Crops and also Products released a research study which showed that chamomile oil has potent antioxidant properties, that is, Roman chamomile oil showed the highest antioxidant activity, when compared with 11 various other sort of crucial oils, including bitter and also sweet fennel, lavender, winter season mouthwatering, thyme, rosemary, sage, French tarragon, peppermint.
Frankincense Oil
Dr. Suhail states that “Frankincense divides the 'mind' of the cancerous cell - the center - from the 'body' - the cytoplasm, and also shuts down the nucleus to stop it recreating damaged DNA codes."
This oil has monoterpenes, which are compounds that are able to kill damaged cells on the beginning, along with their development phases, so it is perfect for the treatment of cancer, no matter the time of its discovery.
This oil might revolutionize the cancer treatment, as it eliminates just cancer cells, unlike chemotherapy, which likewise eradicates healthy and balanced body cells. Dr. Suhail also includes: " There are 17 active representatives in incense crucial oil."
At the Budwig center, numerous people inform their tales and also experiences with making use of vital oils as well as their favorable result from the resist cancer.
These are several of their tales:
Five- years of age kid with mind cancer
A little kid, at the age of five, was identified with mind cancer. His parents found out regarding the essential oils therapy and saved his life! This young boy had a decline of incense, alternated with a decrease of sandalwood put on the feet bottom, and some lavender oil to the wrist.
Bone Marrow Degeneration
A woman, called Ellen, has a bone marrow degeneration and also polyscithemiarubravera. She additionally tried the treatment with necessary oils, as well as these are her words: " After 3 months my blood examinations are revealing enormous improvements positioning most pens right into the regular range!
I have actually not had to do 2 of the last 3 phlebotomies that I was having every 2 weeks and are currently every month or longer! I am feeling like a million bucks as well as not resemble I am at fatality's door! Do these oils and also have faith that this will function. It does."
Breast Cancer
Another female utilized frankincense essential oil to treat breast growth, as well as after some period of time, her medical professionals can not find also a trace of cancer cells! Namely, after a surgical removal of her bust growths, she made use of lemongrass and also incense, applying it on the bust, on a regular basis. After half a year, she took place a check up, as well as her medical professional told her the good information- her cancer cells has disappeared!
Terminal liver cancer
The spouse of a lady in Long Coastline was diagnosed with liver cancer cells, yet doctors claimed it was so established, that a surgical treatment was not an option.
Yet, this lady has actually become aware of the therapy with 100% pure frankincense oil, as well as she suggested its usage. On a daily basis, she used this oil over the liver area, and also under the tongue of her husband.
After a long time, their examination showed that the growths have actually started to shrink, and also just a few months later on, the medical professionals recommended a surgical treatment. They removed cancer cells, along with 3/4 of his liver, and also today, this man enjoys his life and also lives a pleased as well as healthy and balanced life.
Cervical Cancer
" My friend just contacted us to tell me that she learnt that her sis's cervical cancer came back for the 2nd time. She was arranged today to have her womb removed. When she discovered, she sent her sis wintergreen as well as incense.
She advised her mommy to make certain she applied the wintergreen as well as incense under of feet every 3 to 4 hours for the pain in addition to using directly on her abdomen. A week ago, the unhealthy cells were still turning up in her blood work. Today [much less compared to a month after very first starting the oils] was her surgical procedure to eliminate her uterus removed as well as they could not discover any cancer cells."
Bladder Cancer
Jackie Hogan was additionally detected with a rare bladder cancer, and also physicians advised a surgical elimination of the bladder. Yet, she also found out about the amazing residential or commercial properties of frankincense oil, found by the scientists at the University of Oklahoma, especially when incorporated with sandalwood oil.
This blend aided her reward her condition and also enjoy her health and wellness once again. Specialists state that "Frankincense crucial oil might stand for a prospect on a growing checklist of all-natural substances selectively getting rid of cancer cells."
Lung Stage 4 - transition to bones, spine, ribs, hips, pelvis
The mom of Bebe had malignant growths in the lungs, and cancer has actually spread out to the ribs, shoulders, bones, spine, hips, and hips. Four months after a therapy with important oils, her cancer cells were quickly going away. She started operating in her garden as well as also intended her next getaway. and months after the diagnosis that she was to pass away really quickly, she was in superb health, and her cancer was completely gone.
Bebe informed the treatment: She took incense oil openly on every couple of hours, topically, on the affected body components, as well as used it on the feet bottom. For far better results, you can additionally drop a bit under the tongue.
Skin
" I opted for a routine eye examination in February 2013. The Dr informed me the growth over my eye is exactly what I had presumed a form of skin degeneration: basil cell cancer cells. Yikes! One year prior to that eye examination I was at the Dermatologist workplace to have a few suspicious places eliminated from my face, neck and back.
Having gone via that invasive experience lead me to ask is there a more secure method to remove this place (mind you this area is right above my eye). I did a bit of reading concerning vital oil use for skin cancer and it appeared much less invasive than dermatologist plus I did not need to miss time from job. I got a container of Incense and also used it as advised topically 3 times a day and also did 2 declines under my tongue morning as well as night.
The first week no actual substantial change simply a tingling feeling because area after using topically and taking it inside. The 2nd week I did discover it getting smaller. Throughout the third week, the area began to ooze a bit however it was getting smaller sized. The fourth week is when it appeared to IMPLODE on itself and oozed more but still it was getting smaller sized.
The fifth week it was much, much smaller sized and also developed a scab. Week 6 the scab fell off while washing my face as well as was the dimension of a small white head. In 6 weeks a big place was lowered to the size of a pin head all from using and ingesting a crucial oil - Frankincense. I was ASTOUNDED, AMAZED and THRILLED!!!! Important oils functioned for me !!!"
Throat
The good friend of a male had problem with throat deterioration, which was rapidly spreading to various other body areas. A year back, he learnt more about the incense oil as well as its power as well as started the treatment. Today, he has received the great information that he no more experienced the disease!
Basal cell
" My buddy's papa had Basic cell developments on his nose. It had actually experienced the density of his nostril as well as the oncologist wished to eliminate a big section of the nostril, to his upper lip and also over a finger size right into his cheek, by the time he contacted me.
I had not collaborated with cancer cells prior to with the oils and also wanted to aid as much as feasible. He also eliminated sugar from his diet plan, raised water consumption, consumed extra raw foods as well as believed he could beat this.
Within a pair weeks, it appeared closed, an additional week as well as the weeping quit completely as well as the inflammation around the area started lightening. After 6 weeks, that side of his nose looked much healthier than the various other untouched side !! That was 15 months ago and also he has had no signs of it returning."
Prostate
Another male had a buddy that was detected with prostate cancer. He started making use of important oils, and after 3-4 months, he went to see his physician, and also he informed him that his cancer cells has totally disappeared.
Pancreatic
Another guy told another fascinating tale concerning the potential of crucial oils: "A buddy had pancreatic deterioration and also was given 3-4 weeks. He did the following, 3 drops frankincense, 1 drop each lemongrass, lavender, peppermint, sandalwood and also all-natural remedies. He is now in fantastic health ... It's been 8 months currently."
Melanoma
" I applied frankincense early morning as well as evening as well as covered with a band-aid. In 3 days the mole had shrunk. Day 5 it hemorrhaged a little and fifty percent diminished. Day 7, gone! I had a little of pink skin and I worried it was a mark.
A few days later, entirely gone! My hubby had a stage 4 deadly melanoma eliminated in 2014 from his back ... one more cancer malignancy came up on his nose ... before we started utilizing vital oils we did radiation on that one. It has since expanded back ... and we have because become educated making use of essential oils. He began making use of lavender frankincense, as well as Immortelle on the melanoma and also it is SHRINKING!"
Leukemia
Another young boy, who experienced a second leukemia reoccurrence of leukemia, began integrating radiation treatment and essential oils. He went right into remission with an increased speed and also stayed clear of all the damaging effects of the treatment.
0 notes
Text
My Skin Journey...
My skin has been a delicate ecosystem my whole life. When I was a baby I had eczema all over my body. With the help of topical creams and washes, and of course with the loving care of my Mammy- my eczema was cured. My skin following this was perfect, and I always put that down to the treatment I received as a baby.
However this all changed in August/ September 2016. All the way through puberty I was relatively lucky with my skin- maybe only having 2 or 3 small spots on average. But I started getting large painful spots all over my face, especially in the cheek region. At first I didn't know how to feel about it but I just assumed that it was a phase and would pass, sadly it wasn't as temporary as I thought. It is only now (march 2018) that I can see an obvious improvement on my acne and it was a long and difficult journey getting here.
So as I said, my first reaction to the spots was acceptance because I was sure it would pass. At this time I had started a PLC course which meant I could wear more makeup than I usually did, during my Leaving Cert I didn't bother with makeup and my skin wasn't bad. So makeup was my first course of action in fighting my acne.
Makeup is a catch-22 for acne. Yes, your skin appears perfect and it gave me a lot more confidence, but long term it is probably doing more damage. During this time, the other big change in my life was that I had made the decision to start drinking alcohol. For a girl who was previously “anti-alcohol”, this was a shock to the system. So I just thought it was my body’s reaction to alcohol but the acne continued long after I stopped drinking.
As time went on, the worse my acne was getting and the more it was upsetting me. I was someone who was quite vain and superficial at this time, and for me to wake up and see my beautiful face covered in volcanoes- it was heart wrenching.
The following June, I went on a family trip to Toronto, Canada. I was there for 12 days and I think I wore make up for the majority of the time that I was there. I had brought my full makeup kit with me and each morning I would apply the face. Of course at this point I was used to being around my family bare-faced with my spots but it was the fact that there would be countless pictures that made me self-conscious of my skin. The day I went to Niagara Falls was a particularly painful day in relation to my acne. That day I had decided not to wear makeup for a variety of reasons- it was hot and I would have been getting wet at the falls which would ruin my makeup, we were up early and I was tired and also my skin had taken a turn for the worse from the traveling and different food so I thought it best to let my skin breathe for a day. It wasn't a conscious decision of mine but I was just avoiding mirrors that day and I wore a baseball cap to make my skin less noticeable. In the elevator my sister simply asked me “why I didn't put on makeup today of all days?” and although she didn't mean any harm, that comment really hurt me. In that moment, she was my mirror. I know she meant well as she herself had severe acne and she was aware of all the pictures that would be taken that day. After that I was put in a bad mood, I was angry. Why did I have to cover up? It wasn't fair.
During the summer, we went on many excursions and trips but there are barely any pictures of me, barefaced, online. I was always so conscious of it. And the world of snapchat and instagram didn’t help. A camera constantly on your face, when you’re not happy with you see is a dagger to heart every time. I remember one day during the summer my friends and I went to the beach, and the thought of being bare faced was too much so I put on my mask of makeup again and any pictures I uploaded I felt I had to blur out the lumps on my face.
It was the September of 2017 that I finally seeked medical help. I went to see a dermatologist and she diagnosed me with acne. She prescribed me with a drug called “Roaccutane”. This drug is famous for its breathtaking effect on acne. My sister had used it and the results were astounding. However, it wasn't that easy. Roaccutane contains an ingredient that made it impossible for me to take because of my nut allergy. The doctor assured us that there was a form without that ingredient, but after several hours of my Mammy ringing around to different pharmacies we discovered that it would cost over €1000 a month. Which really wasn’t a feasible option.
In the end I was prescribed Minocin (antibiotic) and Dianette (contraceptive used to treat acne). I took these for 3 months and then stopped because we didn't see any improvement whatsoever and I was experiencing some undesirable side effects. Following this I tried taking Dianette by itself for two months. There was some improvement but since stopping taking all medication in february I can see a greater improvement. I don't know how long this will last as I am scared that someday I'll wake up and have a face full of acne again but there are some things I have learned:
Don't be ashamed of your skin and don't let others make you feel that way. I think going away for college helped me with this. I think in total I wore make up 3 times in college so the people that seen me there were used to my skin (in my mind) as they had nothing to compare it too.
You’re not alone. I met people and seen people exactly like me which gave me some perspective. The first time I spoke to someone about my skin at college was to a friend who also had acne. For a person with acne there is nothing worse than someone with a miniscule pimple saying “how awful their skin is” or “how yours isn’t as bad as mine” etc. So to talk to someone who knows exactly what you’re feeling is reassuring.
It will eventually pass. I don't know how long it will take but like with everything in life- it will pass.
What works for someone else won’t necessarily work for you. I would spend hours looking online for “acne cures/hacks”- none of which worked. I only got more frustrated looking at pictures of models telling me to “just drink loads of water”. I actually tried going off dairy altogether, which with hindsight was a mistake. Being a college student and having a nut allergy made it pretty much impossible to go off dairy in a healthy way. I was replacing dairy products with a lot of refined sugar and my diet was very unhealthy. And it wasn’t worth it because it made no difference and I couldn’t eat my favourite foods which only worsened my mood.
Finally, have patience with those around you
I have an amazing family who are very supportive but sometimes if they made a comment or a suggestion I would get really defensive and annoyed. They were only trying to help but when you’re in that dark place you don't want to hear it. I used to wake up and look in the mirror and just cry, and someone saying something you already know just puts salt in the wound.
To end this i just want to say, YOU ARE BEAUTIFUL AND YOUR ACNE DOESN'T DEFINE YOU. Please remember it is just skin and even if you have to say it to yourself daily- it is just skin and your mental health is so much more important.
0 notes
Text
Black Women Are Using Vicks VapoRub On Their Edges And Hair To Make It Grow-Does It Work?
[brightcove:4874661127001 default]
This article originally appeared on Essence.com.
We've seen our fair share of wacky beauty trends and home remedies-from squiggle eyebrows to mayonnaise hair masks-proving we're willing to give almost anything a try in the name of beauty. So when we discovered a bevy of Black women reaching for Vicks VapoRub (target.com, $4.99) on wash day we were definitely intrigued.
A quick YouTube search of "natural hair Vicks VapoRub" and over 35k results instantaneously appear. The first video touting Vick's magical hair growth properties was posted back in March of 2016 by Atlanta-resident Jocquelyn Hill, who goes by Just Jocq on YouTube.
In a video titled "Awesome Tips & Tricks on How To Use Vicks Vapor Rub Part II," a follow-up to her original post nearly a year prior, Jocquelyn explains several unexpected uses for Vicks, including hair strengthening and growth.
"Some viewers say they place it on their scalp and do a scalp massage, and that Vicks VapoRub on their scalp stimulates the hair follicle," she shares. Jocquelyn goes on to explain exactly how one of her viewers does it.
"She mixes Vicks VapoRub, castor oil, and coconut oil and applies that to her scalp and hair. She says she's retained and received a lot of hair growth from mixing Vicks VapRub and those items," she says.
While it's unclear if Jocquelyn's tried it for herself, YouTube's Black hair community quickly headed her viewer's advice and began to use the unlikely hair growth solution for themselves. Videos by @MakeupMesha and @Kimera Yvonne have since received more than a million views combined in just under a year.
In her five-part-series Sonya uses Vicks, along with a few other products, on her teenage daughter's newly natural hair. In the video the mom is seen applying the cream directly to the scalp in small sections, pre-wash and condition.
What's most interesting is that Black women across hair type and textures, including both relaxed and natural, are singing Vicks' praises. In her video @MakeupMesha, who has a relaxer, hair growth is undeniable. In a four week update she proudly shows off inches of new growth which she directly attributes to Vicks.
"My hair has grown like it's been in full blown cornrows to the back. This is usually what I experience when my hair has been in a protective style for a while, this works pretty good," she excitedly shares.
The average time reported by Vicks advocates to see significant hair growth is around 30-60 days. Patience and consistency seem to be the two most important ingredients, after the rub itself, to see results.
In almost all of the videos menthol, eucalyptus and camphor, which are found in Vicks, are touted for the hair's growth and stimulation. Menthol is a compound known to clear pores of irritants so that hair can grow easily while eucalyptus and camphor are both essential oil that stimulate the hair follicles and improve circulation when applied topically.
However the petroleum in Vicks has some women weary of using it. "Because Vicks has petroleum in it, this is one product women don't want to put on their hair. Me personally I don't have a problem with petroleum, it's one ingredient I really don't have an issue with," vlogger Kimera Yvonne shares.
Asked if he'd heard of this hair growth remedy, Dr. Carlos Charles, a New York City-based dermatologist who specializes in working with people of color, told ESSENCE he had not.
"While Vicks VapoRub is generally safe, a brief look at the ingredients list several oils that could potentially cause allergic or irritant skin reactions as with any topically applied product," Dr. Charles warns.
So although rubbing Vicks on your scalp and hairline may work it's probably best to proceed with caution, as both the doctor and many of the women on YouTube suggest. "Don't leave it on for too long and make sure you don't have any open scabs," Sonya reminds.
While we have yet to try Vicks VapoRub on our scalp or hairline we can't help but marvel at the ingenuity of our fellow sisters.
Still intrigued?
Below are a few of the most viewed YouTube videos of Black women using Vicks VapoRub to grow their edges and natural hair for your viewing pleasure.
0 notes
Text
Hairkeeper
youtube
Hair Loss - Cause, Prevention and Treatment
An increasing number Haaruitval vitamine of Singaporean men are shedding their 'crowns of glory' and this pattern could also be getting earlier and earlier.On the streets in these current years, we could spot a comparatively number of young males who're bald or balding. Evaluate this phenomenon to say ten years ago when this phenomenon isn't commonly seen haaruitval mannen tegengaan.
This balding development amongst Singaporean men is sparking an growing proliferation of hair therapy centres. Hair therapy centres have practically sprung up everywhere in the island with the likes of Beijing 101, Yunnan, Svenson, Bossin, and many others. Causes of hair loss will be hereditary, or caused haaruitval vitamine d by stress, drug medicines, poor diets, oily scalp and so on and these causes manifest into the many kinds or forms of hair loss equivalent to male pattern baldness, telogen effluvium, alopecia areata, and so forth. A standard human loses about 50 to a hundred hairs per day and this loss isn't alarming.
However if more than this quantity is misplaced per day, one ought to seek a health care provider earlier than it's too late.Hair grows from follicles, and if one balds and takes no actions, the follicles will finally die and there will be no extra progress. It will be too late for any motion. Notice that after I say bald, normally a human will not go totally bald, the follicles on the sides of the human scalp, the components above the years are programmed for life, and hair grows for life at these particular areas. Balding follows a sample often called the Norwood chart. There are three phases of hair growth: anagen (the growing phase), catagen (the intermediate phase) and telogen (the shedding part). Hair loss happens when the hair grows and sheds fast.
The average life cycle of a hair is 2 to three years and every hair development to fall can final 25 cycles, balding happens when these cycles are accelerated and completed so quick that the cycles end, the follicles dies off and the hair can by no means develop again once more. I understand on this put up, there are a lot of jargons and technical phrases which are used. The web gives a rich array of resources for which one can research in depth and understand more about hair loss. On this publish, I will just roughly summarize what I perceive and experience about hair loss from my studies and very own personal experiences.In the past, I've very thick volumes of hair a lot in order that I complained about having to go to the barber usually as my hair grows so quick.
Showering, there would be no hair misplaced as my hair is so sturdy. Following a medical therapy some two years in the past from a supposedly respected clinic and consuming the drug nimigen, I notice hair loss, my hair shed within the dozens on the bed and at the bathtub sinks each day so much in order that I stopped taking this drug nimigen and cease the laser treatments.
Through the consumption of nimigen, my complexion becomes too dry as it's supposed to prevent facial oiliness however it overdoes. Until today, I still have no idea the true purpose for my hair loss although I consider it has to do significantly with the laser therapy and the consumption of nimigen. On hindsight, I shall not have carried out with the remedy and the consumption of the medicine and this doctor still asked his nurses to power me again to continue with the remaining therapies and on the similar time, refuting all my allegations squarely. I spent near $3K solely to lose even more.
Anyway that is the past already and nothing might be completed to turn again the clock. What I want to share with readers listed here are my experiences and what I've gone via to combat hair loss and hopefully it could possibly provide some useful glimpses or lessons to those who are presently affected by hair loss.Okay for the start, I first stopped all of the causes that I consider have contributed to my hair loss and that's to discontinue with the medical remedies and the nimigen consumption. However even with that, two months down the street, the hair loss doesn't subside, so it was time to take some actual actions.
From the internet, I got here to learnt of two medication referred to as Propecia, an oral treatment, costing about $ninety five dollars at that time for 28 tablets, to be taken one tablet a day; and a topical hair spray referred to as minoxidil (referred to as Regaine, Rogaine, Growell, etc available in the market) also at a $95 for one bottle that can final a month.I went to a doctor and was prescribed Propecia, taking one capsule a day for 3 months, after which I stopped.
Why do I cease? Firstly, there was no enchancment and secondly, I started to expertise what was talked about as the unwanted effects of this drug, i.e. I start to really feel less manly, though it was a minor side effect that the drug claimed and that it affect only a small share of customers. With these two elements, I ended utilizing this drug and the less- than- manly feeling, which was momentary finally subsided. I didn't use Minoxidil, as I additionally learnt of its uncomfortable side effects too. I want to listing down the doable uncomfortable side effects of these two medicine here:Propecia: Lack of 'manliness'Minoxidil: Increase scalp sensitivity, itchiness, dandruff, enhance sensitivity to the solar.
And crucial disadvantage of these two scientific proven drugs is that after you stop utilizing these two medication, whatever new hair that you've grow will fall again! Thus these two medicine are to be used for all shampoo tegen haaruitval kruidvat times! Think about the fee involved to take care of these newly formed hair: $a hundred (for each of those therapies per 30 days), this quantity interprets to $1200 and extra per 12 months, and so forth......
So after ending the use of the Propecia, I started to discover pure ways of treatment. One methodology that I thought of was using delicate shampoo like Johnson Child Shampoo, however its gentle focus was not sturdy sufficient to clear the oilness of my scalp. My hair loss could also be due to oiliness and dandruff as I did discover these symptoms like dandruff on my pillow.
So I decided to discover the assistance of execs and there was an unlimited array of selections from the dermatogists and hair therapy centres. I went to at least one such hair treatment centre for a free consultation and these 'professionals' scanned my hair, solely to disclose many patches of oil and these 'professionals' introduced me a package to clear my scalp greasiness.
The package value a bomb and I didn't just like the pushiness of those professional in introducing these packages to me. Additionally I've heard many stories of people having spent greater than $10,000 on these supposedly good cures only to lose even more hair or having no enchancment seen, in addition to losing their arduous-earned money! Thus, hair therapy centres scared me off at that point and I decided to seek the advice of a top hair dermatologist in Singapore instead. It was not low cost. First session alone cost $eighty. The dermatologist inspected my hair and stated there was nothing unsuitable. She prescribed me with two shampoo, Nizoral ($25) and a Light Shampoo ($21) to be rotated interchangeably day by day and a sebum regulator to be utilized on the scalp at night time after washing ($18).
Nevertheless, there was shampoo tegen haaruitval loreal still no enchancment.
In fact, the residue from the sebum regulator produced tiny sticky white residue on my hair once my hair dried to the extent that my colleagues thought my hair had dandruff. Anyway my hair was still very oily and coated with some dandruff too, despite applying the supposedly sturdy and helpful shampoos that the top dermatologist prescribed. I confirmed this https://www.hairkeeper.eu truth once I popped into one of many hair therapy centre at a buying centre for curiosity and did a free consultation with the centre. The 'scanner' that the centre operators used magnified my scalp glands many instances over, revealing the oily spots, it really look disgusting with such a hundred instances over magnification of the sebaceous scalp glands.
The operators stated my scalp glands have been choked with oil, and this may trigger hair loss; however I didn't need to take any likelihood with this centre and off I left. I went for a second session with the dermatologist read more on wikipedia here I saw previously. Again, the dermatologist stated there was nothing improper with my hair or with my scalp and the results from the 'hair-pull' take a look at she carried out on me revealed no extraordinary hair loss.
After listening to the story of the medical therapy I did and the drug nimigen I consumed, she suspected that it could be telogen effluvium attributable to the treatment, a condition which could only go away in times to come; although my oily scalp could also be a contributing issue too. She advised me that she couldn't Hair keeper do something besides to assist me diagnose the reason for my hair loss via a scalp biopsy ($589) and a blood test ($169); all price said with out GST. Hearing the costs, I hesitated but in an urge to seek out out the true cause, I made a decision to make the leap and carried out the scalp biopsy and the blood check.
I did the blood check first and the ache was nothing compared to the scalp biopsy I undergone later on. It was no joke, having a bit of your head scalp being removed surgically and the pain was terrible regardless of Hairkeeper Social Profile the applying of anaesthetics prior to the remedy. After both the exams, the nurse rubbed a Bactroban cream on the a part of my scalp which was operated on to kill the bacteria; after sewing this a part of the scalp.
There was still little pain that subsisted each time I shampoo the sewn a part of the scalp. I was informed to come back two weeks later to take away the stitch and to obtain the outcomes of the analysis. I was given the remaining of the Bactroban cream to visit the blog apply day by day on the affected scalp to ease the pain and kill the bacteria. Two weeks later, I returned to the same clinic to remove the stitch and the dermatologist handed me the consequence; and the outcome indicated that it was telogen effluvium.
The dermatologist mentioned it was good news as this situation which can be because of the medicine I took would lastly subside after some time. I would be ready for this to come quickly.But alas, days move and then months, it was futile. Seeing tons and tons of hair on the toilet sink and waking up on a regular basis to witness the a whole bunch of hair strewn across my mattress and on my bed room floor did nothing to assuage me that my illness would go away. The visits to the dermatologist have additionally drained me financially and in a desperate transfer, I made a decision to try out some off-the-counter hair loss products available at pharmacies.
I tried the Himalyan Hair Loss Cream (Natural) for about one month nevertheless it was ineffective so I went to see the dermatologist again for the fourth and fifth time (that was in April and Could final 12 months), haaruitval bij vrouwen vitaminen however once more the dermatologist assessed and mentioned there was nothing mistaken with my hair, no male pattern loss or no matter. But certainly, my hair was getting thinner and thinner by the day.
She prescribed me with stronger shampoos and sebum regulator which I used without seeing any improvements. It was at the moment that I lastly determined not to see the dermatologist again as there was simply no use in any respect! Hair continued to fall and fall. useful link From then on (Jun 07), I've 'roughly accepted my destiny' and accepted my hair loss fact. I attempted Kaminomoto Hair Development Accelerator and a good shampoo known as Melaleucca Shampoo recommended by my pal nevertheless it was really no use at all.
The telogen effluvium which I used to be identified with didn't appear to be the hair illness that struck me because it merely didn't cease within a short interval. It was over one year and my hair nonetheless continued to fall like rain. Over the entire of this hair loss ordeal, I carried out numerous researches shampoo tegen haaruitval on hair loss over the internet, which further geared up me with all information concerning hair loss. I tried all I could, from observing what I consumed (less oil), watching my food regimen, exercising commonly and even cutting down on some espresso and tea. But it surely did not assist in the loss.
I have also shared my findings with others on an internet discussion discussion board posting and the thread saw some 55,000 odd readers before it was finally eliminated by the administrator. With my information learnt from the web and my ordeal, I shared with a few of these forumers; some of them even emailed me to ask questions. For hair loss, there's actually nobody mounted miracle panacea: what works for one could not work for others. The hair loss did have an effect on my life a bit: waking up in the morning and after shampooing, I counted the variety of strands of hair that I lost and any fewer in depend would make me slightly happier.
I used to enjoy the wind however now I avoid being 'confronted' with a gust of wind for worry that the wind would blow off a few of my hair. It doesn't help that Singapore can get breezy at occasions! And definitely, my vanity would suffer a bit of loss and it did not assist that I am nonetheless without a girlfriend at my age! Hair loss will surely dealt me a serious drawback on this 'picture-acutely aware' society; though it might not be always true: I nonetheless do my fair share of admirers as some women will not be particular over seems.Getting into the MRT daily, I all the time observed young man at different stages of balding; typically I noticed friends who I have not seen for some years utterly bald!
0 notes
Text
The Problem with Your Skin is...
The problem with your skin is that you have cystic acne, more or less caused by genetic predisposition to it from your father; Your hormones aren’t on par so you should start taking birth control, and finally begin to spend all of your time ruining your stomach and liver with excessive amounts of oral antibiotics to pre-treat bacteria.
I have been struggling with acne for roughly 8 years. At this point I can’t remember when I started to officially have acne, I just always remember having it; but for the sake of this post, I will assume at least 8 years. Acne is my Voldemort. Our interaction began when I was a kid, followed me closely as I grew up, left a scar (realistically, scars) on my face, and has eaten away at me psychologically - leaving my self-confidence and self-acceptance in the dirt. I cannot run from it, nor have a found a successful way to get it out of my life.
Whenever I bring this aspect up when people ask me about my acne, or choose to nag about their lonely pimple that made a guest appearance on the day of their period, people never seem to comprehend the magnitude to which acne can affect the mentality of those it plagues. OR they never realized that it can affect people (especially female teens) in such a dramatic way. The link I will post below touches on the surface of the effect acne can have on ones emotional health.
https://www.aad.org/public/diseases/acne-and-rosacea/emotional-health-effects-of-acne
In touching on the topic labeled “Early treatment can prevent emotional distress, acne scars”:
I can believe what they are stating in this section, and where part of me believes that it is most likely a reasonable way to avoid long-lasting emotional distress I know from personal experience that early treatment doesn’t always eliminate the problem. I will tell you what I mean by this, I started my Accutane journey when I was a freshman in high school. This was after all of the doctors appointments, topical treatments, oral antibiotics, and dermatologist exams. My dermatologist recommended Accutane to see if this would be the end-all-be-all for my stubborn hormonal, genetic, cystic acne. One year later my face was dry as the Sahara desert and my mother was insanely concerned about my fluctuating emotions (the term “emotional rollercoaster” had nothing on 13 year-old me, I was a flippen hurricane).
But, the results were starting to become apparent. Although I had cracked lips my acne had become less than mild. So I took a 4 month breather from it, I finally felt like I could handle on my acne. Those 4 months were short-lived. My acne returned and so my dermatologist recommended I continued for another 5 or 6 months to see if it would help. It did, but after my sophomore year of dry skin and raging emotions (thank you puberty for coming at a time that you weren’t needed) I ended my second journey with Accutane and have not touched it since.
The reason I am explaining this is because I did the early intervention and treatment of my acne, and all it did was left me utterly confused and totally unpleasant to be around (if your mother can handle you while being a 13/14 year-old teen female who starts puberty and has crazy drugs like Accutane causing chaos in their body, she deserves a purple heart). But this is just my story, for some this worked and they were free from the evils of their Voldemort.
I am now 21 years old and I still suffer from acne breakouts. In looking back at all the experiences I've had in trying to treat my acne I have realized that I am at the perfect point in my life where I can finally understand how to better my skin. I find that diet, stress, and skin care are the way to go. Yea that to most sounds like a huge “umm DUH”, but I have come to a point where it all makes sense. This is mainly because I am starting to become more comfortable in who I am and really, what I look like. I have suffered through depression and anxiety; I know that I was young and took in to account too many peoples opinions of beauty and how far I felt I strayed from that description.
Well, here I am. My Voldemort still comes around to pick on me and put me down, but I will not let him get the best of me any longer.
0 notes