#list of open access medical journals
Explore tagged Tumblr posts
Text
Concept of Formae Speciales in Sclerotium rolfsii, a Collar Rot Pathogen of Crop Plants and its Use in Crop Diversification System

Concept of Formae Speciales in Sclerotium rolfsii, a Collar Rot Pathogen of Crop Plants and its Use in Crop Diversification System in Biomedical Journal of Scientific & Technical Research
Sclerotium rolfsii, a soil dwelling fungal plant pathogen causing seedling mortality/ collar rot disease in crop plants have a wider host range of cereals, millets, pulses, oilseeds, fibre crop, vegetables, fruit crops, medicinal, spices, flowering plants and forest trees to cause plant mortality and yield losses in fields and storages around the world. Sclerotium rolfsii, as a single pathogen infect all these crop species or there is variation among the isolates infecting these crop species and thereby presence of formae speciales in this pathogen, is not yet known. In our studies 13 isolates of Sclerotium rolfsii isolated from different crop species comprising cereal, pulses, oilseed, vegetables, medicinal plant, and flowering plant were test inoculated on 27 different crop species of above plants for their susceptibility to determine the host range of these individual/ particular isolate. On the basis of host-Pathogen interaction, leading to seedling mortality/collar rot disease at least 11 formae speciales of this pathogen viz. f.sp.ciceri, f.sp.glycinae, f.sp. betae, f.sp.gossypi, f.sp. plantago, f.sp. mangeferae, f.sp. lagenariae, arachis, polianthes, dahlia and lilium were established. Sclerotium rolfsii isolates from Chickpea, Wheat and Tomato had the same host range, and therefore inclusion of further different crops in host range studies will established the presence of formae speciales in the isolates from chickpea, wheat and tomato. Based on host range studies of these isolates/f. sp. a crop diversification system is proposed so as to avoid the infection in crop plants in the Sclerotium rolfsii infected fields. These results have a great significance in planning the crop cultivation in Sclerotium rolfsii sick soils.
For more articles in Journals on Biomedical Sciences click here bjstr
Follow on Twitter : https://twitter.com/Biomedres01 Follow on Blogger : https://biomedres01.blogspot.com/ Like Our Pins On : https://www.pinterest.com/biomedres/
#Journals on Biomedical Imaging#Medical and Medicinal Journal#List of Open Access Medical Journal#Journal of Biomedical Research and Review#journal of biomedical research and reviews impact factor
0 notes
Text
Researching as a Writer
Start Broad
begin with a list of more general topics and get specific as you go.
for example, research for a historical fantasy novel might follow a chain that looks like this:
life in the 1700s -> life in 1700s france -> 1700s french etiquette and lifestyle depending on class -> 1720s french fashion for middle and upper-middle class women.
starting with a general understanding of the topic you want to cover and narrowing down to specifics will make it easier to build on your knowledge as you go.
Think Critically
consider the source. if it doesn’t cite primary sources (for example, letters and photographs from a specific era and location), what sources does it cite? follow those sources if possible.
is the information reliable? is it provided by an educational institution or an expert on the subject?
who is the author? do they present any bias? what do they have to gain by promoting a specific mindset or conclusion? has any of their research been debunked?
Anecdotes
in general, anecdotal evidence is not sufficient for academic writing. luckily for you, this is a fiction writing page, and anecdotal evidence is usually fine!
work with a combination of scholarly sources and personal experience. if you’re trying to depict a specific health condition, you might consult medical sources about the technical details of the condition, as well as seeking firsthand accounts from people who have that condition.
remember that people are not monolithic! there are often forums online where people are more than happy to discuss their experiences; cross-consult these for common elements.
Lists
keep track of your sources!! if you ever need to consult something later on, it will be way easier to open a list of resources than go digging through your search history.
additionally, if you come across lists of sources compiled by other people, save those!! you are probably not the first person to research the specific topic you’re looking into, and there are entire websites dedicated to gathering research!
wordsnstuffblog.com/research has compilations of sources for everything from writing injuries to global period pieces by century.
Resources
if you can, check out your school or public library’s websites! they will often compile scholarly resources to access for free.
look for open access or open source sites like project gutenberg that archive and digitize historical documents and other works. scienceopen and the directory of open access journals are more of these. search using keywords!
keep an eye out for websites made specifically for educational purposes (those with .edu at the end of their addresses).
#🌿 writing#writing tips#writing advice#writing resources#i'm trying to compile some instagram posts on here for easier reference#writing research
915 notes
·
View notes
Text
things to do when u realize u feel shitty
so i have alexithymia (emotional blindness or challenges in recognizing, expressing, sourcing, and describing one's emotions) and i often dont realize why, whats causing me to feel that way, or even if its mental or physical shittiness. so here are things i try to do to reset.
so the first step is obviously realizing the feeling at first, is your brain making you feel bad about yourself? do you feel like theres no point in doing things? do you feel stuck? or has there been any drastic change in energy in a short time? these may look different for you, but learning to notice even something as small as do i feel Good or Bad, you dont need to get caught up in what specifically it is.
FIRST and foremost, medications. did you take your meds? vitamins? please do so if you can. if you've missed the time window that you are meant to or cant for another reason, no guilt please, its ok we all forget.
move! change locations. even if its just where you are sitting in bed from one side to the other and sit up if you can. i try to move to my desk chair. sometimes just sitting up can change the way you feel drastically.
this could also mean move as in take a walk around your room, stand up on your phone instead of laying down.
do a Task, or Activity. copy a journal spread from pinterst even if it takes like 3 hours. write some lists, make a bracelet, play a game. focus on something you like. very cliche advice i know but its great to allow yourself to do something you like.
get a snack/water. unfortunately hydration is important even tho its annoying. make it super cold, put some lemon or mint in there if you want. its all about making it a) more fun and b) different sensory experiences. if you are hungry go down a mental list of most to least effort meal and find what you can do (cook from sratch, add stuff to ramen, eat it plain, get a handful of nuts or fruits, etc)
open the curtains/blinds, let the outside in a bit. even if its dark out open them and look around and close again.
face feels gross? do some level of skincare, exfoliate your lips and put on some vasesline, brush and floss your teeth (love floss picks). if you have bangs wash them in the sink.
if weather + mental permits, go outside. even for 2 seconds to look at it
shower=full reset and rebirth. not a bath, a shower. let the water hit you and soak your hair. do as full of a shower as you can. use so much moisturizer (if you can) with a scent you love. sensory goodness is very helpful. this usually works for me to pull me out. often the reason why i feel shitty is actually just me not realizing my hair is dirty, or i need alone time, etc which is acheived by showering.
aligned with that, put on new clothes, either comfortable and lounge clothes that are good sensory, or you need a new fun outfit because you have been wearing the current one for too long and its irritating you in a way you dont notice.
clean something, same as the food go from most to least effort and find out what you can do. organize 1 drawer or your whole house. my go to is usually rearraging my bedside table top and drawer. because for me thats where i keep things like my journal, headphones, letters from friends, body butter, etc its a chance for me to help future me access this little self care station.
make your bed so you have a clean cozy place to lay and sit, unfortunately a made bed is more comfortable
in general, treat yourself like a littel guy, talk to yourself like a toddler even if it feels silly, the part of you that feels bad is basically a toddler throwing a tantrum tbh. silliness is often a precursor to feeling Good. these things feel so so hard but each time you do them despite feeling bad it will get easier i promise you, you will get good at what you practice so practice trying.
if all of these things seem too hard, or you cant do them, the main thing is thats ok too. and if you dont feel 100% better after doing these things, that is also ok. the truth is some days things will be hard and that is your body telling you to relax, or sleep, or that it just wants to have an off day. no day is wasted if you are still here to see it.
(a lot of these tasks can be made easier by doing prep when you are feeling Good, which is part of the reason why i made this list, but i might do another post on prep stuff. )
#long post#depression tips#anxiety tips#mental health#mental wellness#self care#AS#i dont normally make posts like this#or at all#but i want to#being in a good place after being in such a bad one for so long is something i always feel the urge to share#or even being in a bad place but feeling like thats not the end
35 notes
·
View notes
Text
Free tactical medicine learning resources
If you want to learn first aid, emergency care or tactical medical care for real, you will need to practice these skills. A lot. Regularly. There’s no way to learn them just from books. But if you’re looking to supplement your training, can’t access hands on training, are a layperson doing research for your writing or otherwise just curious, here are some free resources (some may need a free account to access them).
TCCC
The current gold standard in the field is Tactical Combat Casualty Care (TCCC), developed by the US army but used by militaries around the world. There is also a civilian version of the system called Tactical Emergency Casualty Care (TECC). Training materials, Standards of Care, instructional videos, etc. can be accessed at deployedmedicine.com. You’ll need a free account. This should be your first and possibly only stop.
There’s also an app and a podcast if those are more your thing, although I haven’t personally tried them.
More TCCC (video) resources
STOP THE BLEED® Interactive Course
TCCC-MP Guidelines and Curriculum presentations and training videos
EURMED’s Medical Beginner's Resource List has suggested list of video materials (disclaimer: I haven’t watched the playlists, but I have been trained by nearly all of the linked systems/organisations and can vouch for them)
Tactical Medical Solutions training resource page (requires registration; some of the courses are free)
North American Rescue video downloads
Emergency medicine
WHO-ICRC Basic Emergency Care: approach to the acutely ill and injured — an open-access course workbook for basic emergency care with limited resources
Global Health Emergency Medicine — open-access, evidence-based, peer-reviewed emergency medicine modules designed for teachers and learners in low-resource health setting
AFEM Resources — curricula, lecture bank, reviews, etc.
Global Emergency Medicine Academy Resources (links to more resources)
OpenStax Anatomy and Physiology textbook
Open-access anatomy and physiology learning resources
OpenStax Pharmacology for nurses textbook
Principles of Pharmacology – Study Guide
Multiple Casualty Incidents
Management of Multiple Casualty Incidents lecture
Bombings: Injury Patterns and Care blast injuries course (scroll down on the page)
Borden Institute has medical textbooks about biological, chemical and nuclear threats
Psychological first aid: Guide for field workers
Prolonged field care
When the evac isn’t coming anytime soon.
Prolonged Field Care Basics lecture (requires registration)
Aerie 14th Edition Wilderness Medicine Manual (textbook)
Austere Emergency Medical Support (AEMS) Field Guide (textbook)
Prolonged Casualty Care (PCC) Guidelines
Wilderness Medical Society Clinical Practice Guidelines
Austere Medicine Resources: Practice Guidelines — a great resource of WMS, PFC, TCCC, etc. clinical practice guidelines in one place
The Wilderness and Environmental Medicine Journal (you can read past issues without a membership)
Prolonged Field Care Collective: Resources
National Park Services Emergency Medical Services Resources
Guerilla Medicine: An Introduction to the Concepts of Austere Medicine in Asymmetric Conflicts (article)
Mental health & PTSD
National Center for PTSD
Psychological first aid: Guide for field workers
Combat and Operational Behavioral Health (medical textbook)
Resources for doctors and medical students
Or you know, other curious people who aren’t afraid of medical jargon.
Borden Institute Military Medical Textbooks and Resources — suggestions: start with Fundamentals of Military Medicine; mechanism of injury of conventional weapons; these two volumes on medical aspects of operating in extreme environments; psychosocial aspects of military medicine; or Combat Anesthesia
Emergency War Surgery textbook and lectures
Disaster Health Core Curriculum — online course for health professionals
Médecins Sans Frontières Clinical guidelines
Pocket book of hospital care for children: Second edition — guidelines for the management of common childhood illnesses in low resource settings
Grey’s Quick Reference: Basic Protocols in Paediatrics and Internal Medicine For Resource Limited Settings
The Department of Defense Center of Excellence for Trauma: Trauma Care Resources (links to more resources)
#feel free to share and add more#tactical medicine#tactical combat casualty care#prolonged field care#austere medicine#military medicine#tccc#tecc#disaster medicine#wilderness medicine#emergency medicine#emergency medical services#learning resources#writing resources#mandalorian medics#paramedicine#medicine
34 notes
·
View notes
Text
I get very irritated by transphobic politicians pretending to care about "evidence" because I've yet to find one who actually does.
Look at this horseshit:
The Florida Department of Health wants to clarify evidence recently cited on a fact sheet released by the US Department of Health and Human Services and provide guidance on treating gender dysphoria for children and adolescents... Due to the lack of conclusive evidence, and the potential for long-term, irreversible effects, the Department's guidelines are as follows:
Social gender transition should not be a treatment option for children or adolescents.
The... The long term "irreversible" effects of being referred to by a different name or pronoun and possibly wearing different clothes than people might expect?
I mean I feel like you could reverse the effects by just... not doing that stuff anymore.
Anyway, they link, as evidence for their opposition to social transition, to this paper:
Title:
Not social transition status, but peer relations and family functioning predict psychological functioning in a German clinical sample of children with Gender Dysphoria
Literal first line of the abstract:
Research provides inconclusive results on whether a social gender transition (e.g. name, pronoun, and clothing changes) benefits transgender children or children with a Gender Dysphoria (GD) diagnosis.
Right in the introduction:
prepubescent children are not advised to receive any medical treatment before the onset of puberty (Tanner stage 2; Coleman et al., 2012). However, they often transition socially from one gender to another during childhood (Coleman et al., 2012). This reversible nonmedical step towards a life in the identified gender may include changing one’s name or pronoun, being introduced as the experienced gender in public, as well as gender typical appearance in terms of e.g., hair length and clothing (Steensma et al., 2013; Wong et al., 2019).
(Bolding mine)
Hey, big important Florida Surgeon General guy who wears a tie and influences the lives of millions of people:
I had to read your evidence for less than five fucking minutes before it openly contradicted what you say in your guidance.
People like this complain all the time about how evidence in trans medicine is hard to come by and uses small sample sizes, but then they link to a paper that has a sample size of 54 German kids.
Oh, and a paper which explicitly says,
Caution is also warranted in generalizing the results to all children with a GD because of the small and relative unique sample. All 54 children in the analysis sample were referred to the clinic for their GD, most of them came from families with a medium or high socio-economic background and the family support of the children’s gender identity was generally high. Due to the health care situation in Germany for children and adolescents with a GD diagnosis, some families go to considerable length to get access to treatment which they probably would not do if they did not generally support their child’s personal situation. At the same time, the clinical guidelines of the Hamburg GIS are quite liberal and allow for individual treatment pathways. Thus, these findings might not apply to a more diverse sample of transgender children who are not supported in their gender identity or expression by parents or clinicians, or children who identify themselves on a broader gender spectrum.
These people really, really fucking hope you don't actually read the evidence on this stuff.
I want to be clear: This isn't, like, one paper in a huge list of evidence against social transition, this is literally the only thing the Florida Surgeon General cites in opposing social transition.
30 notes
·
View notes
Note
List 5 things that make you happy, then put this in the askbox for the last 10 people who reblogged something from you! get to know your mutuals and followers 💜 (also no pressure of course)
Hi, Thanks for sending this in; I rarely divulge any info about myself, so I'm genuinely excited to answer this 🙂.
My Cat- Photo of my cat inserted below; fun fact: she loves Cheesestrings!

2. My voluntary work—Okay, so for extra info, once a week, I help out at a drop-in community art group by making hot drinks, filling in the register, providing 1:1 support for our participants, and helping out at some events. I've been there for a long time and made friends with the group, and I feel distraught whenever I can't attend! I'm not going to get too specific because I don't want to dox myself, lol!
3. Whenever I meet up with my friends
4. I managed to bag tickets to a gig for one of my favourite bands called Litany after worrying all week that they wouldn't give me accessible seating. Also extra happy I didn't have to prove my medical problems + accessibility info 🥳
5. My writing (specifically my poetry and articles) —I wasn't going to put this down initially, but I realised
A) I don't talk about my writing at all, and
B) It makes me happy and immensely proud (sometimes). I've had a poem published and a bunch of articles as well (digitally), and that makes me really happy! But also, I've got a finished poem that I'm the proudest of because it took me a year to write, and it's one of my best (so far). Atm I'm trying to find a home for it. I'm just waiting for submissions to be open and for the right journal/magazine, it would fit with!
#asks#you asked for a list and I ended up rambling 😂#if anyone is genuinely interested in the 'professionally' published stuff then I'll happily give links#it doesn't feel right sharing my proper work on tumblr though lol#oh and if anyone wants more info on Litany#i.e. where to start on the discography (not that they have a big catalogue) I'll happily divulge 🙂#finally got around to answering this- had trouble deciding if I was rambling to much etc
4 notes
·
View notes
Text
In Hindsight, A Deafening Diagnosis by Ecler Jaqua in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
Dizziness is a common presentation to the outpatient, primary care physician. Its persistence, associated with hearing changes, should prompt further evaluation for more rare diagnoses such as an acoustic neuroma. Although not malignant, timely management of an acoustic neuroma is essential to prevent chronic facial paresthesia, pain, or taste disturbance, and more rarely death.
CASE PRESENTATION
This is a sample text. You can click on it to edit it inline or open the element options to access additional options for this element.
A 34-year-old female presents to the primary care physician with a 2-week history of fatigue, generalized headache, intermittent right-sided tinnitus, and dizziness that started abruptly after a dental procedure. Tinnitus is high-pitched and most often noted in the morning. The dizziness occurs mainly when changing from a supine to seated position. She has no pertinent medical history, engages in regular cardiovascular exercise but is plagued with an addiction to coffee, approximately 3 cups a day. She denies taking any medications or over-the-counter supplements.
Physical exam, including vital signs and orthostatic blood pressure measurement, is unremarkable. Differential diagnoses included benign positional vertigo and caffeine-induced headache. Plan was to obtain an audiogram, keep a headache diary, decrease caffeine consumption, and improve hydration on days of exercise.
While awaiting the audiogram, the patient presented again to her primary care physician for worsening fatigue and self-diagnosed anxiety, in addition to her stable dizziness, tinnitus, and headache. Physical exam was, once again, unremarkable. Differential diagnoses were expanded to include anemia, thyroid disorder, and vestibular migraine. Plan was to trial sumatriptan and begin laboratory evaluation for her fatigue and hair loss. Labs were unremarkable for anemia, electrolyte or vitamin imbalance, and thyroid disorder.
Almost one year later, the patient returns with persistent symptoms of fatigue, anxiety, tinnitus, dizziness, and intermittent headaches. She reports that her symptoms were overwhelming and affected all aspects of her life, not relieved with the sumatriptan. Physical exam, once again, was unremarkable. Differential diagnoses were again expanded to include Meniere’s disease, intracranial mass, and somatization disorder. Plan was to obtain the previously ordered audiogram, non-urgent magnetic resonance imaging (MRI) of her brain, and consultations with Psychology for coping techniques and Otolaryngology for her tinnitus and dizziness.
THE DIAGNOSIS
The audiogram was notable for asymmetric hearing loss (Fig 1) and subsequent imaging with MRI Brain confirmed the diagnoses of a 5mm intracanalicular tumor, suggestive of acoustic neuroma (Fig 2). The patient was offered proton therapy but elected for definitive, surgical intervention with Neurosurgery. She underwent translabyrinthine resection of the intracanalicular acoustic neuroma. Her postoperative course was complicated by facial weakness but resolved after one year. Follow-up imaging confirmed complete tumor resection and she continues to do well two years after surgery, without recurrence of the acoustic neuroma.
THE DISCUSSION
Headaches, dizziness, and tinnitus are challenging concerns because the differential diagnoses are quite broad. In this case, since the patient presents often, the symptoms were more likely to be acute and the more common diagnoses of benign paroxysmal positional vertigo, vestibular migraine, and caffeine-induced headache were considered. As the symptoms became more persistent, the clinician correctly broadened the differential diagnoses list and requested the appropriate imaging and specialty follow-up.
This patient’s diagnosis, a right-sided acoustic neuroma, was delayed by poor follow-up and procrastination in obtaining the audiogram. Fortunately, the acoustic neuroma is a slow-growing, benign tumor that develops from schwannoma cells along the branches of cranial nerve VIII, the vestibulocochlear nerve.1 Acoustic neuroma is also known as vestibular neuroma or schwannoma, most commonly affecting individuals between 65 and 74 years old with a prevalence of 1 in 100,000.2,3,4 The most common risk factor is having a history of neurofibromatosis type 2 or exposure to high-dose radiation.5 Increased prevalence, over the last several years, has been attributed to advanced imaging technology.3 Although it is a slow-growing tumor, its growth can compresses the facial and trigeminal nerves causing facial paresthesia, pain, and taste disturbance.6 Rarely, the tumor can compress the brainstem and cause death.6,7 It can be monitored for growth or treated with radiation and/or surgery.
THE TAKEAWAY
Unfortunately, the etiology of patients’ concerns cannot always be determined. But, it should be the responsibility of the primary care physician to evaluate potentially life-threatening conditions for persistent symptoms. This case demonstrates balancing the common with the uncommon differential diagnoses and illustrates the patient’s role in adherence to the treatment plan. Although headaches, dizziness, and tinnitus are non-specific symptoms, the persistence of them should warrant further investigation with more advanced imaging and specialty consultation.
#dizziness#JCRMHS#vitamin imbalance#Hindsight#tinnitus#Headaches#A Deafening Diagnosis#thyroid disorder#Free PubMed indexed case report journals
3 notes
·
View notes
Text





By: SEGM
Published: Aug 17, 2023
A major medical journal Ugeskrift for Læger, the Journal of the Danish Medical Association, confirmed that there has been a marked shift in the country’s approach to caring for youth with gender dysphoria. Most youth referred to the centralized gender clinic no longer get a prescription for puberty blockers, hormones or surgery—instead they receive therapeutic counseling and support.
In the course of less than a decade, like every other Western country, Denmark experienced an exponential increase in the number of young people presenting with gender dysphoria. In 2014, there were only 4 documented pediatric cases who requested gender reassignment. By 2022, the number of referrals grew by 8700% to 352, similar to the several-thousand-percent increase in less than a decade witnessed by a number of Western countries. As the number of young people wishing to undergo gender reassignment increased, so did the rates at which Danish gender clinicians transitioned them. By 2018, Denmark's centralized gender service was medically transitioning 65% of referred youth. This was similar to the proportion of referred children who got transitioned reported by other pediatric gender clinics. For purposes of comparison, the Netherland’s Amsterdam gender clinic reports transitioning 73% of late-onset referrals and 85% of early-onset referrals and in the US, researchers analyzing data from Seattle Children’s Hospital gender clinic reported that over 60% of the referrals underwent medical transition with puberty blockers or cross-sex hormones within one year of intake.
However, following systematic reviews of evidence conducted in Europe and the subsequent reversal of the “gender-affirmation” paradigm in favor of a cautious, developmentally-informed approach that prioritizes psychosocial support and noninvasive resolution of gender distress in Sweden and Finland, Denmark appears to have made a quiet but resolute shift to treat most youth presenting with gender dysphoria with supportive counseling rather than puberty blockers, hormones, or surgery. In 2022, only 6% of those referred to Denmark’s centralized gender clinic were prescribed endocrine interventions (puberty blockers and/or cross-sex hormones).*
The rationale for this shift was explained in a recent publication in Ugeskrift for Læger (“Weekly Journal for Physicians”), the Journal of the Danish Medical Association. This Danish-language article provides one of the most sober discussions to date of the inherent medical and ethical uncertainties of providing minors with profound, life-altering interventions in the context of very limited understanding of the epidemiological shift in the population presenting for care, the growing rates of detransition, and the profound uncertainty about long-term outcomes.
The authors can hardly be accused of being “armchair critics.” They are the very clinicians responsible for assessing youth and approving them for gender transitions in Denmark. Realizing that their well-meaning intentions were based on insufficient evidence, and seeing the growing evidence of harm, they sharply reversed course. Today, only 6% of the referrals are approved for hormonal transition, and no minors are allowed to transition surgically.
The article is open-access, and only available in Danish. Below, we provide a synopsis.
The Danish centralized pediatric gender service was launched in 2016. Denmark opened a centralized gender transition service for minors in 2016, using a multidisciplinary approach that encompasses intake, evaluation, consultation, and referrals for puberty blockers and cross-sex hormones.
The rationale for launching the pediatric gender transition service was the Dutch studies’ reported success. The Danish youth gender transition service was launched based on the experience of the Amsterdam gender clinic and reports of its positive outcomes “suggesting that early hormone therapy resulted in better psychological and physical outcomes and less need for surgery in adulthood” as well as “body satisfaction, low rates of regret, and few side effects.” The two studies supporting this premise were the Dutch protocol as described by the Dutch clinicians in 2012, and the famous 2014 “Dutch study.”
A key assumption, now in question, was the permanence of transgender identity in youth with longstanding gender dysphoria that intensified in puberty. According to the authors, the Dutch “trials” of gender transition were justified insofar as it was believed that a cross-sex identity in adolescents with longstanding gender dysphoria that intensified in adolescence would be permanent, or “stable.” However, the authors now concede that there are significant questions brought about the growing rate of detransition, and concerns “about the generalizability of these studies,” especially their applicability to the young people referred to gender clinics today.
The significant “underexplained” increase in referrals of adolescents over age 11 “mainly made up of birth-assigned girls” became a major red flag. The authors describe a profound change in the epidemiology of gender dysphoria in youth following the launch of the centralized pediatric gender clinic service. “In Denmark, the number of referred persons has increased from 97 in 2016 to 352 in 2022, of which birth-assigned girls aged 11-18 make up 70%”. Noting the “excess of birth-assigned girls” among gender dysphoric youth, the authors express concern that “the background for the change is underexplained.”
Another red flag is the high rate of psychiatric comorbidities in currently-presenting cases. The authors note that unlike the Netherlands, where gender dysphoric youth reportedly have a relatively low rate of psychiatric comorbidities (33%), in Denmark and other countries there is a much greater proportion of gender dysphoric youth with comorbid mental illness (e.g., 75% in Finland). These conditions include depression, anxiety, suicidal thoughts/self-harm, autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD).
The authors raise a new concern: gender dysphoric youth have a younger age of pubertal onset. They reference a Danish study that found earlier puberty in youth with gender dysphoria compared to the general population of adolescents. They do not elaborate on the implications of this finding, but note that overall the pubertal age has been declining.
The authors call out more generally the growing rates of gender nonconformity in youth, and especially females, independent of the youths’ wish to medicalize. The study authors cite the results of the Danish Project SEXUS study which found a sharp increase in gender nonconformity (21.2% of females and 15.7% of males ages 15–24 years). The authors note a generally “higher incidence of non-gender-normative behavior among girls” and “low tolerance for non-gender-normative behavior in boys.”
The authors explicitly identify “social influence” as a contributor to the concerning epidemiological shift in gender dysphoria presentation. The idea that teens are products of their social environments and can adopt transgender identities following social influence does not appear to be controversial in Denmark. The authors openly discuss the possibility of social influence as directly contributing to the rapid rise of post-pubertal onset of gender dysphoria in youth. They also opine that the availability of treatment itself may have contributed to rapid rise of trans-identification in youth.
The Danish clinicians are concerned by growing rates of detransition among those who initiated transition in youth and a lack of research into the detransition phenomenon. “In recent years, there have been reports of reversal of hormone-induced permanent changes to the body that began in youth. There are no systematic estimates of the frequency or reasons why hormone treatment is discontinued.”
The Danish clinicians are now concerned that the basis for gender-transition of large numbers of minors with diverse presentations of gender dysphoria is a single short-term Dutch study based in a different population and which has failed replication outside the Netherlands. Throughout the article, the Danish clinicians describe their initially positive view of the Dutch research, and their now growing concern about the lack of applicability of the Dutch experience from years past to the current clinical realities in the rest of the Western world. They appear to be signaling a widening gap between the positive trends that the Dutch clinicians continue to report (youth with low rates of mental illness, low rates of detransition, and positive short-term transition outcomes), and the problems emerging in the rest of the Western world (much higher rates of comorbid mental illness, an inability to show robust and reliable improvements in mental health, and growing rates of detransition).
International changes, and especially those in the Nordic European countries, appear to have directly influenced Demarks’ move to a more cautious approach. In Finland and Sweden, youth with post-puberal onset of gender dysphoria are not typically considered to be candidates for medical transition in adolescence. Denmark’s gender clinicians quoted these changes in their new move to base treatment eligibility in part on the “duration” of gender dysphoria.
As a result of the above-mentioned concerns and international changes, Denmark has sharply restricted eligibility for hormone interventions for youth. The authors state that Denmark has “adopted a more cautious approach to hormone therapy until more evidence of its beneficial effects is available.” While the article does not provide year-over-year referral-to-treated ratios, another source confirms that in 2018, two-thirds (65%) of referred youth were transitioned and by 2022 this percentage fell to 6% (22/352).
The authors conclude with a call for more research and international collaboration:
"Several countries, including Denmark, have adopted a more cautious approach to hormone therapy until more evidence of its beneficial effects is available [2, 17]. In particular, there is a lack of knowledge about the increasing proportion of young people with onset of gender-related discomfort after puberty [2, 17, 23] and the presumably increasing proportion with mental disorders, as new studies suggest that the positive effects are not replicated in this group [22, 29]. There is a need for healthcare services that can be flexibly adapted in the future and systematic international cooperation in research and exchange of experience."
The current Danish treatment guidelines were published in 2018 and are due to be updated later this year. While the specifics of the changes have not yet been made public, the new approach described in the article foreshadows the likely principles and practices that will be included in the updated guidelines, specifically:
Thorough psychological assessments are required to determine whether gender dysphoria is related to a mental health disorder such as ASD, or psychosis. All young people are to be thoroughly assessed using broad and lengthy diagnostic interviews with multiple reporters including schools and parents as well as cognitive testing. The assessment aims to determine whether gender discomfort may be an aspect of a psychiatric disorder or mental illness.
Minors whose gender dysphoria differs from the classic “Dutch” definition (i.e., early onset of gender dysphoria that worsens after puberty, no significant mental health comorbidities) will only be offered psychosocial, supportive treatment. The centralized team will assess for the appropriateness of medical transition. Most presenting cases are rejected from consideration for medical transition and instead are referred to “support or advisory conversations.” Of note, while the authors reference the longstanding duration of gender-related distress that worsens in puberty they do not explicitly require early childhood onset of gender dysphoria. It remains to be seen how explicit this requirement is in the updated guidelines.
Not every otherwise eligible minor will be considered able to consent. The authors explain that“…the level of functioning, stability and how any psychopathology, cognitive level and psychosocial conditions affect identity development and the ability to reflect on and make decisions about gender reassignment treatment.”
Teens ages 15 and older retain the right to consent to treatment without parental agreement or consent, but the treatments offered will prioritize counseling. According to the current 2018 Danish treatment guidelines, when a 15-year-old minor and their parents disagree about gender transition, the minor can proceed without parental consent. This is because Denmark’s laws consider 15-year-olds competent to make medical decisions. While these laws will not change, the authors recognize the important role of parents in this unusual situation, and underscore that the treatments offered to the teens will be “psychosocial support for the young person” and they further assert that “ideally all decisions are made in consultation with the parents.”
For the remaining few cases that will qualify for transition, significant uncertainties are explicitly identified. Irreversible changes are called out, along with the health risks: “…both types of sex hormones cause reduced fertility, however the degree and reversibility of this remains unknown. Contraindications to hormone therapy are abuse, suicidal ideation/self-harm, severe psychological distress and worrisome somatic conditions (eg cancer, thromboembolic disease).” It is acknowledged that hormone treatment will be lifelong.
Surgical interventions in minors, already rare, will likely be removed as an option. The current treatment guidelines do not allow genital surgeries for those under 18, but it appears that mastectomies for some older teens are still an option (although perhaps an option on paper only). Recent comments by the Danish Minister of Health suggest that mastectomies may be officially disallowed in the updated guidelines.
“I can also inform you that the National Board of Health [“Sundhedsstyrelsen”] issued a new guideline for gender reassignment surgery on March 28 this year at the latest, which is now in consultation. In the new referral guidelines, it is no longer possible to offer surgical treatment to children under the age of 18... An option that, by the way, has never been used in Denmark.” **
SEGM Take-Away
In the last several weeks, health journalists have reported that change may be afoot in Denmark. The article in Denmark’s Medical Association journal Ugeskrift for Læger leaves very little doubt that Denmark too has made a course correction in youth gender transitions, restricting this option to very few cases, while prioritizing counseling for the vast majority of the currently presenting youths. The article is an excellent summary of the rise-and-fall-of the “gender affirmation” model of care in Denmark. It describes how in 2016, following the influence of other northern European countries, Denmark chose to offer “a treatment approach with few barriers to hormone treatment for children and young people with gender dysphoria.” The treatment was justified by the foundational Dutch studies, “which indicated better well-being and body satisfaction after hormone treatment, a low degree of regret and few side effects.” However, the increasing number of referrals, changes in the presentation in gender dysphoria, and growing reports of regret—combined with a lack of long-term outcomes of the one and only sample of youth (n=55) on which the entire practice of gender transition rests—led the Danish clinicians to reverse course.
This change is notable. In 2014, Denmark became the first European country to pass a “self-id” law for adults whereby adults did not need a diagnosis of gender dysphoria to register a legal sex change. Denmark continued to be a leader in destigmatizing transgender identities and in 2017, becoming the first country in the world to remove “Gender Identity Disorder” (DF64) from the its public health authority's list of mental illnesses. To provide treatment, healthcare practitioners were instructed to use a “Z” code, “contact due to gender identity” (DX78X)." The barrier-free transition of minors, launched in 2016, was the logical next step.
To fully appreciate the scope of the changes underway in the treatment approaches for minors, it is helpful to review Denmark’s 2018 official practice guidance, Health professional help with gender identity issues (English-language version here). The guidance does not preclude any presentation of gender dysphoria from eligibility for transition; there is no minimum age for transition; and at age 15 minors who are considered able to understand the consequences of treatment for gender dysphoria may obtain medical transition services without parental consent.
Recently, Danish Minister of Health Sophie Løhde acknowledged that country’s national pediatric center for gender dysphoria in Copenhagen has grown “reluctant to offer hormone treatment compared to before,” particularly to youth with post-pubertal onset of gender dysphoria. The Danish Health Minister praised this change in practice, noting that “it is a positive thing that there is a response to research and experience... both in Denmark, but also abroad, which we must follow closely. And this knowledge and experience lead to adjustments in the current treatment options.”
While countries in Europe are increasingly leaning on one another’s experience and collective knowledge to devise an approach to intake, screening, and support of gender-dysphoric youth in order to safeguard them from inappropriate, non-evidence-based gender reassignment practices, the American medical establishment continues to double-down and “do it alone.” Earlier this month, the American Academy of Pediatrics (AAP) finally conceded to conduct an independent review of the evidence and update its guidance. This decision has come several years too late: the first call for these actions came from AAP members in 2019 and has been repeated every year since.
However, at the same time, at its 2023 Annual Leadership Forum earlier this month, AAP paradoxically reaffirmed its current “transition for all those who want it” affirmative care approach, refusing to acknowledge or consider the problems that have been documented by the recent European systematic reviews and react in real time. Rather than working collaboratively, as the Danish clinicians have suggested in their article, the CEO of the AAP has described a decidedly American-exceptionalism approach: “they engaged in their process, we’re engaging in our process.” And just earlier this week, the official AAP website platformed another article promoting gender transition of minors by two gender clinicians who reassured America’s pediatricians that "affirmation" is beneficial while caution is harmful: “When pediatricians lack knowledge about the needs of transgender and gender-diverse youth, they may default to the “watch and wait” approach. This method is outdated and harmful….” (The article does carry a footnote, "The views expressed in this article are those of the author, and not necessarily those of the American Academy of Pediatrics.)
America was fast to import and accelerate the European approach to treating minors, putting it “on steroids” and adding the scalpel. However, when it comes to reversing course, it intends to take its time. Why AAP staunchly refuses to accept the conclusions of multiple systematic reviews of evidence that found the practice of youth gender transition to either not be clearly beneficial, or net-harmful is unclear. Although the AAP has finally agreed to commission its own systematic review, it has already presaged the review's conclusion, which is that it will support the current pro-affirmation AAP position. In the meantime, thousands of American children and parents continue to be misinformed that science and evidence support the practice of gender transitions for youth who desire them, and that those raising concerns are merely science-deniers spreading “scientific misinformation” at best, and likely ill-intentioned. Therefore, it is not surprising that in America, the debate will continue to be politicized, and may ultimately be adjudicated in the court of law rather than due to the diligence and responsible actions and course corrections of the medical community itself, as is currently underway in Europe.
Intakes vs Approvals for Endocrine Interventions for Minors by Year, Denmark*:

Footnotes:
* The referrals and treated numbers for the Danish national gender clinic service are available at the Danish Rainbow Council website. While SEGM cannot independently verify the accuracy, we have no reason to doubt these statistics. Specifically, the number of referrals for 2017 (n=97) and 2022 (n=352) matches the data reported in this source and the numbers quoted in the referenced official Dutch medical journal.
** The speech by the Danish Minister of Health, Sophie Løhde, is available at this link. The English language transcript is available at this link.
#SEGM#Society for Evidence Based Gender Medicine#medical scandal#medical transition#gender ideology#genderwang#queer theory#puberty blockers#sex trait modification#religion is a mental illness
8 notes
·
View notes
Text
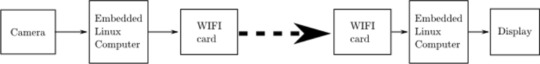
Cutting to the "shopping list" section:
We focused on using “off the shelf” components and open-source software to develop the wireless endoscope. This significantly lowered the cost with the goal to make the device accessible for resource-constrained environments. While the technology described is applicable to a variety of rigid lens applications, we attempted to replicate the 4 mm cystoscope lens and separately a clip-on universal endoscope camera.
2.1 Hardware systems
A miniature single-board computer (SBC) module the Raspberry Pi Zero W (Raspberry Pi Foundation, Caldecote, UK) was used because of its size, its low cost (US$10) and its ability to handle high-definition (720p) video.
A 3.7-mm tube camera (model: 1001LG, Shenzhen Eastern International Corporation Limited, Shenzhen, China) was used. It delivers 1280 × 720 high-definition video using a 1/7″ colour CMOS sensor. Lens construction allows a wide (115 degree) field of view and an extended depth of field allowing object in the range of 5 to 50 mm to be in focus. Connectivity is via a USB 2.0 interface with the SBC. The camera is certified IP67 waterproof and the manufacturer is ISO 13485:2016 certified for the design and manufacturer of medical endoscope cameras.
Illumination is via 6 high luminous 0603 white colour LEDs incorporated into the tube camera. The system was powered by a 1200mAh lithium polymer battery and incorporated into a fireproof acrylonitrile butadiene styrene enclosure.
For the clip-on wireless camera module, an 18–35 mm optical zoom coupler (Ouman Medical, Jiangsu Ouman Electronic Equipment Co., ltd, Jiangsu, China) and an 8-megapixel camera module (model: IMX219, Arducam) were used.
2.2 Software systems
Open-source Linux software was used on the SBC as follows:
1. The SBC runs on the Raspbian Pi operating system Lite, a minimal image of Debian Buster [9]. 2. The SBC Wi-Fi module is placed in monitor mode (“hotspot”) using RaspAP [10]. This makes wireless video transmission possible. 3. The video signal is streamed via the UV4L module of “Video 4 Linux 2” [11].
4. Lastly, the wireless video signal is viewed on a standard computer via any internet browser. Figure 2 illustrates the entire software setup.
Fig. 2:
7 notes
·
View notes
Text
“Ella Roe” (USA 2009–2010)
A paper in the Obstetrics & Gynecology medical journal in 2013 reported the death of a woman who died after taking the abortion pill because of Planned Parenthood’s negligence.
“Ella Roe” legally bought the abortion pill from a Planned Parenthood facility in 2009 or 2010. Planned Parenthood apparently failed to competently examine her in advance and most likely did not bother to give her an ultrasound. If they had, it would have been easy to diagnose Ella’s ectopic pregnancy.
Unaware that her life was in danger, Ella took the RU-486 pill. She trusted her health to an abortion facility and paid the price for their malpractice.
Ella died from the ruptured ectopic pregnancy. The condition could have and should have been diagnosed with a simple ultrasound, but Planned Parenthood didn’t care enough to examine her before selling her the pill.
The publication does admit to severe side effects, but claims that their work “reinforces the safety” of the abortion pill. However, there are severe limitations and conflicts of interest that most likely prevented significant amounts of data from being included.
First, the data used was obtained mostly from Planned Parenthood, with the corporation even listed as one of the authors. They have been known to lie about statistics relating to abortion and would directly benefit from withholding data that made them look bad. Second, nobody is legally required to report abortion pill deaths or complications to authorities, meaning that it would be very easy to simply not report a case. One of the authors of the study was also noted to “receive compensation” from Danco Laboratories (the manufacturer of the abortion pill) in exchange for “providing third-party telephone consults to clinicians who call for expert advice on mifepristone.”
Other studies on the abortion pill have observed a high level of danger. Even one pro-abortion source showed that as many as 1 in 12.5 abortion pill clients had to go to the ER. Still, even this statistic could easily be underestimated because it’s hard to get accurate data on complications form American abortions because of the grossly deficient and flawed reporting system full of discrepancies. The chemical abortion pill can cause excessive bleeding, sepsis, gas gangrene, hypovolemia, uterine inversion, cryptogenic stroke, tachycardia, leukocytosis, edema, hypotension, metabolic acidosis, necrosis, immunological weakening, cardiac arrest and excruciating pain.
In addition, Planned Parenthood’s own data report showed that they missed ectopic pregnancies in 16 clients during the study period and gave them abortion pills. All they would have had to do to diagnose any of them was a basic exam and ultrasound. Every one of those women could have died the way Ella did. There is no excuse for this level of negligence.
As surprising as it is for something including Planned Parenthood’s input to admit to a client death, the publication alone is by no means proof that the abortion pill is safe.
#tw abortion#pro life#unsafe yet legal#tw murder#tw ab*rtion#abortion#abortion debate#death from legal abortion#unidentified victim#planned parenthood#tw negligence#tw malpractice#the abortion pill kills#kill pill#this is chemical abortion#abortion pill
6 notes
·
View notes
Text
Cloning, Eukaryotic Expression Vector Construction and Tissue Expression Analysis of Mir-133b in Pigs

Cloning, Eukaryotic Expression Vector Construction and Tissue Expression Analysis of Mir-133b in Pigs in Biomedical Journal of Scientific & Technical Research
This experiment aims to construct the eukaryotic expression vector of pig pEGFP-N1- miR-133b and detect its expression in pig tissues. Using DLY (Duroc×Landrace×Yorkshire) growing-finishing pig genomic DNA as a template, the miR-133b precursor and part of its flanking sequence were cloned by PCR technology and inserted into a eukaryotic expression vector using conventional molecular cloning technology to obtain pEGFPN1-miR-133b. The recombinant plasmid was transfected into 3T3-L1 cells by liposome method and observed the fluorescence. Real-time qPCR was used to detect the expression of miR-133b in heart, liver, spleen, lung, longissimus dorsi, subcutaneous fat, and abdominal fat of pigs. The results showed that miR-133b was successfully amplified. 3T3-L1 cells were transfected with pEGFP-N1-miR-133b eukaryotic expression vector and pEGFP-N1 empty plasmid respectively for 48 hours, and the cells had green under a fluorescent inverted microscope. Fluorescence expression proves that the recombinant plasmid can be expressed in 3T3 cells. Using qPCR technology to detect the expression of miR-133b in 3T3 cells, the relative expression of the pEGFP-N1-miR-133b eukaryotic expression vector transfection group was extremely significantly higher than that of the empty group. The qPCR results showed that miR-133b was expressed highest in the longissimus dorsi muscle, followed by the heart, and the lowest expression in fat. In this study, the eukaryotic expression vector of pig miR-133b was successfully constructed, which provided a reference for studying the mechanism of miR-133b on pig muscle development.
For more articles in Journals on Biomedical Sciences click here bjstr
Follow on Twitter : https://twitter.com/Biomedres01 Follow on Blogger : https://biomedres01.blogspot.com/ Like Our Pins On : https://www.pinterest.com/biomedres/
#Biomedical Open Access Journals#List of Open Access Medical Journal#Journals on Biomedical Engineering#Biomedical Science and Research Journal#journal of biomedical research and reviews impact factor
0 notes
Text
A personal reminder is a tool, app, or system designed

A personal reminder is a tool, app, or system designed to help individuals stay organized by keeping track of important tasks, events, or deadlines. Here's a comprehensive guide to setting up and using a personal reminder effectively:
1. Why Use Personal Reminders?
Stay organized with tasks and deadlines.
Avoid forgetting important events (e.g., birthdays, meetings, bill payments).
Manage daily routines efficiently.
Reduce stress by relying on a system instead of memory.
2. Types of Personal Reminders
Digital Reminders (Apps and Tools)
Reminder Apps:
Google Keep
Microsoft To-Do
Apple Reminders
Any.do
Yaad Rakho (specific to your needs)
Calendar Apps:
Google Calendar
Outlook Calendar
iCalendar (Apple devices)
Personal Assistant Devices:
Amazon Alexa
Google Assistant
Siri
Manual Reminders
Sticky Notes: Place them in visible areas like desks or refrigerators.
Planners/Diaries: Write daily tasks and mark deadlines.
Bullet Journals: Track habits, tasks, and goals.
3. Setting Up Personal Reminders
Using an App
Download and Install: Choose an app that suits your needs (e.g., Yaad Rakho for tailored reminders).
Create a Task:
Input the task name (e.g., "Pay electricity bill").
Set the date and time.
Add additional details (e.g., location, notes, or attachments).
Set Notifications:
Opt for push notifications, SMS, or email alerts.
Customize the alert frequency (e.g., daily, weekly, or a one-time alert).
Using a Calendar
Open your calendar app.
Add an event or task with:
Title
Date & Time
Recurrence (if applicable)
Enable reminders or alarms.
Manual Systems
Write tasks in your planner every morning.
Use color-coded sticky notes for categorization (e.g., red for urgent tasks, green for routine).
4. Common Uses of Personal Reminders
Daily Tasks: Exercise, grocery shopping, medication.
Work Deadlines: Project submissions, meetings, client follow-ups.
Bill Payments: Credit card, utilities, subscriptions.
Special Occasions: Birthdays, anniversaries, events.
Self-Improvement: Habit tracking, learning goals.
5. Best Practices for Using Personal Reminders
Prioritize Tasks: Use categories like "High Priority," "Medium Priority," and "Low Priority."
Avoid Overloading: Set reminders only for key tasks to prevent notification fatigue.
Review Regularly: Check completed tasks and update the list frequently.
Synchronize Across Devices: Use apps that sync with your phone, tablet, and computer.
Back-Up Data: In case of app or device failure, ensure your reminders are saved online (e.g., Google Cloud).
6. Benefits of Using Personal Reminder Services Like Yaad Rakho
Fully customized reminders based on your needs.
Email and SMS alerts for critical tasks.
Multi-device support to ensure accessibility anytime, anywhere.
Specialized features like recurring reminders and event tracking
0 notes
Text

MRCS After MBBS: A Strategic Pathway to a Successful Surgical Career
For MBBS graduates with permanent registration from the Indian Medical Council, pursuing MRCS After MBBS is a highly valuable alternative to traditional postgraduate courses, especially for those looking to bypass the NEET PG exam.
With the growing demand for skilled surgeons in India, the MRCS exam opens up new career avenues, providing a globally recognized qualification and an opportunity to specialize in General Surgery.
Comprehensive MRCS Training: Equipping You for Success
At TAU, our MRCS training adheres to the Royal College of Surgeons standards, offering structured, high-quality preparation for the MRCS exam. The training spans three years, during which trainees gain hands-on experience in various surgical departments.
Supervised by expert consultants and Royal College-certified program consultants, students are guided in acquiring advanced surgical skills.
Key Features of the Training Program:
Hospital-based teaching in major Indian hospitals
Clinical rotations following Royal College standards
Access to weekly lectures, mock exams, and question banks for exam preparation
Review of contemporary surgical articles to stay updated with the latest in the field
This rigorous training methodology ensures that students are fully prepared for the MRCS exam, enabling them to enhance their surgical career.
List of Associated Hospitals
Trainees benefit from practical experience in some of the top hospitals across India, including:
St Theresa Hospital, Hyderabad
Fortis Hospital, Mumbai
Aakash Hospital, Delhi
Ruby Hall Clinic, Pune
Saifee Hospital, Mumbai
Queen’s NRI Hospital, Vizag
These facilities provide a comprehensive learning environment, with exposure to a variety of surgical cases and procedures.

Why Choose TAU for MRCS Training?
Our MRCS training in India is designed to meet international standards, making it an ideal choice for those pursuing a career in General Surgery.
Structured 3-Year Training: Equivalent to UK-based Royal College programs, offering comprehensive surgical skills.
Supervised Training: Each trainee is mentored by experienced consultants to ensure personalized learning and development.
Practical Experience: Gain hands-on experience at some of India’s leading hospitals.
Continuous Assessments: Weekly lectures, mock exams, and a question bank prepare students thoroughly for the MRCS exam.
Career Enhancement: The MRCS qualification significantly enhances your job prospects in both national and international medical settings.
Faculty, Support, and Online Resources
TAU is proud of its international faculty, who are dedicated to providing timely guidance throughout your training. Our experienced mentors and academic advisors ensure that all academic requirements are completed on time.
Additionally, we offer access to a wealth of online resources, including e-journals, LIRN, and Springer Publishing materials, to keep you up-to-date with the latest developments in General Surgery.
Ready to Take the Next Step?
Don't miss out on this exciting opportunity to advance your surgical career with the MRCS After MBBS program. Enroll today and embark on a transformative journey that will open doors to a successful and fulfilling career in General Surgery!
Apply now and shape your future as a world-class surgeon!
0 notes
Text
Ginekologia,
Ginekologia,
women's reproductive health. To write an article for a gynecology-focused publication, it is essential to consider the target audience, the purpose of the article, and the specific topic you wish to address.
Sample Article Outline for "Ginekologia" Title: Advances in Minimally Invasive Gynecological Surgery
Introduction: Minimally invasive surgery (MIS) has revolutionized the field of gynecology over the past few decades, offering women less painful, safer, and faster recovery options compared to traditional open surgeries. This article explores the latest advancements in minimally invasive gynecological procedures, including laparoscopic and robotic-assisted surgeries, and their implications for patient care.
Body:
Overview of Minimally Invasive Surgery in Gynecology:
Definition and history of MIS in gynecology. Comparison with traditional open surgery. Commonly performed minimally invasive procedures (e.g., hysterectomy, myomectomy, endometriosis treatment). Laparoscopic Surgery:
Explanation of laparoscopic techniques. Benefits: smaller incisions, reduced pain, quicker recovery. Recent advancements in laparoscopic technology and techniques. Robotic-Assisted Surgery:
Introduction to robotic-assisted surgery (e.g., the da Vinci Surgical System). Advantages over conventional laparoscopic surgery. The role of robotics in complex gynecological surgeries. Emerging Technologies and Techniques:
Innovations in imaging and navigation technologies. The future of single-incision laparoscopic surgery (SILS). Use of artificial intelligence and machine learning in gynecological surgery. Patient Outcomes and Considerations:
Discussion on patient selection for MIS. Comparative outcomes: recovery time, complications, and patient satisfaction. Cost-effectiveness and accessibility of minimally invasive procedures. Challenges and Ethical Considerations:
Training and proficiency in minimally invasive techniques. Ethical implications of robotic surgery and the cost burden on patients. Addressing disparities in access to advanced gynecological care. Conclusion: Minimally invasive gynecological surgery has transformed patient care, offering women safer and more efficient options for various conditions. As technology continues to advance, the potential for further improvements in surgical outcomes and patient satisfaction is vast. However, ensuring equitable access and addressing the ethical challenges of these technologies remain critical to the field’s future.
References: A list of references from recent journals, articles, and textbooks in gynecology should be included to support the article's content.
Customizing the Article Target Audience: Adjust the technical depth based on whether the article is for healthcare professionals, medical students, or the general public. Topic: Focus on specific areas like fertility, cancer treatment, or postpartum care if that aligns better with the publication's needs. Regional Focus: Consider adding local data or studies if the article is aimed at a specific geographic audience. Let me know if you'd like a more detailed write-up or any specific modifications!
0 notes
Text
“I hear a voice sometimes, but it’s not generally distressing these days. I feel like I can keep myself safe and make sound decisions these days, but I want support before I live independently in subsidized housing, which is a daydream of mine for the future....when? I'm open to whenever I'm ready, whether that day comes or not. A group environment may be ideal for me long-term. The entity in my body/mind is not as agitating as it used to be. I’ve gotten a lot better in this phenomenal hospital, particularly with my medication regimen, and the voice has become more therapeutic albeit still sometimes bothersome but when it’s like that, I fight back against it by speaking up now. Part of why I'm going to an ALF and not a shelter is that I don't feel able to live entirely independently at this time, but I also don't think I need to continue being in a locked facility. I'm ready to start living my day-to-day wellness plan and building up stable time where I'm sober from drugs other than my prescription medications (I say that because they're drugs too, but they're drugs I need to be sane and functional and healthy and content.) I’ll continue to speak up if the entity in my mind/body is an issue, and am going into an ALF so as to maximize my chances of staying recovered while in the real world as I prepare for the transition to independent living in the future if that day ever comes. I'm really interested in the "Hearing Voices" movement, and learning more about shamans - religion is a big part of my life and identity. I have been working with my treatment team to develop a relapse prevention and wellness plan, as well as a list of coping strategies and activities to make life worth living. I don’t want to spend my life in a hospital when all I need is residential treatment, continuous/ongoing sobriety, psychiatry, and the absence of abuse/ongoing trauma in order to be happy, healthy, and well. I’ve gotten so much better here. For the first time in years I’m not suicidal and I'm speaking up to some people's faces about what my reality is like, and I’m eager to live the simple life I want of running, going to farmer's markets, studying, window shopping, and visiting libraries and museums on top of a daily run. (Those are the things I can't access here - my daily life has and will have other parts.) I’m not from Baltimore, but it seems like a really cool city. I’m excited to check out the aquarium, the capital Jewish museum, and maybe attend a concert someday. I also love creative writing and fashion, and am so excited to spend the money I already have on some little things to enrich my life like clothes I love #minimalistchicwardrobe #ipad #makeup #skincare #planner #artmarkers #journal #notebooks. I know I may not have much of a disposable income while in an ALF, but with my basic material needs met and any generosity I am gifted with, I am confident I will be 100% content with my financial situation assuming we can work out the food situation. I'm a vegetarian for ethical reasons, and sustainable eating has been important to me since my foray into veganism into middle school, which was fueled by my concern for the environment and the animals victimized by factory farming. I pray for a safe and happy future and what DBT taught me to call a life worth living."
0 notes
Text
NEET College Predictor 2024: Your Guide to Finding the proper Medical College

The National Eligibility cum Entrance Test (NEET) may be a pivotal exam for aspiring medical students in India. Securing a great rank in NEET opens the entryways to a few of the finest medical colleges in the nation. In any case, with over 80,000 MBBS seats available across India, it can be challenging to decide which colleges you're likely to get into based on your NEET score. This can be where a NEET college predictor tool comes in handy. In this web journal, we are going to discuss what a NEET college predictor is, how it works, and how you'll be able to utilise it to create educated choices approximately your medical education in 2024.
What is a NEET College Predictor?
A NEET college predictor is a web apparatus outlined to assist NEET aspirants anticipate which restorative colleges they can get confirmation to based on their NEET rank or score. The device employs authentic information, such as past years cut-offs, and other components to supply an gauge of the colleges where a student might secure a situate. It considers different parameters, counting the candidates category (Common, OBC, SC, ST), domestic state, and favoured courses.
How Does a NEET College Predictor Work?
The NEET College predictor 2024 employs a calculation that analyses numerous information focuses to supply accurate expectations. Here's a step-by-step overview of how it works:
Input NEET Subtle elements: The student inputs their NEET score, rank, and other pertinent subtle elements such as category, state of house, and favoured course (MBBS, BDS, etc.).
Authentic Data Analysis: The tool gets to a database of verifiable information, counting past years cut-offs for various medical colleges and courses.
Calculation Processing: Utilising this information, the calculation calculates the likelihood of securing a situation in completely different colleges. It takes into consideration patterns, changes in cut-offs, and situational accessibility.
Comes about Show: The predictor gives a list of colleges where the understudy features a high, direct, or low chance of getting admission.
Benefits of Using a NEET College Predictor
Educated Decision-Making
One of the foremost noteworthy points of interest of employing a NEET college indicator is that it makes a difference when students make educated choices. Rather than depending on mystery, students can utilise the predictor to urge a reasonable thought of their admission prospects.
Time-Saving
The admission process can be time-consuming and unpleasant. A college indicator streamlines this process by rapidly narrowing down the list of potential colleges, saving students a part of time and exertion.
Planning Ahead
By knowing their chances of getting into different colleges, students can arrange their other steps more viably. They can prioritise their choices, plan for counselling sessions, and guarantee they have all fundamental reports ready.
Financial Planning
Understanding which colleges are within reach moreover makes a difference students and their families arrange fiscally. They can research the fee structures of the anticipated colleges and make vital budgetary arrangements.
How to Utilise a NEET College Predictor for 2024
Using a NEET college predictor is straightforward. Here a step-by-step guide:
Assemble Your Information
Before utilising the predictor, make beyond any doubt you've got all the fundamental data prepared, including:
Your NEET 2024 score or rank
Category (Common, OBC, SC, ST, etc.)
State of domicile
Favoured course (MBBS, BDS, etc.)
Choose a Solid Predictor Instrument
Several websites and educational stages offer NEET college predictor devices. Select a reliable and trustworthy one, such as those given by coaching institutes like Aakash, Allen, or platforms like Shiksha and Careers360.
Input Your Points of interest
Enter your points of interest precisely into the predictor tool. Double-check the data to guarantee it is rectified.
Analyse the Results
Once you yield your details, the predictor will give a list of colleges categorised by your chances of admission (high, moderate, low). Audit this list carefully.
Research the Colleges
Take a little time to research the colleges recommended by the predictor. See into their framework, staff, situation records, charge structures, and any other variables that are important to you.
Get ready for Counselling
Utilise the expectations to get ready for the counselling process. Keep your archives prepared, make a list of preferred colleges, and be prepared to form speedy choices amid the counselling sessions.
Tips for Maximising Your NEET College Predictor Results
Stay Updated with Cut-offs
Cut-offs can alter each year based on different components such as the difficulty level of the exam, number of candidates, and situate accessibility. Remain upgraded with the latest cut-off patterns to guarantee the predictors that come about are significant.
Consider All Factors
Whereas the predictor gives you a list of plausible colleges, consider other components such as location, college notoriety, campus offices, and individual inclinations some time recently making a final decision.
Utilise Multiple Predictors
To induce a comprehensive see, use different NEET college predictor devices. Diverse apparatuses might utilise distinctive calculations and information sets, giving a broader run of choices.
Counsel with Experts
Counselling with teachers, career counsellors, and current medical understudies can give extra experiences and assist you make a well-rounded choice.
Conclusion
A NEET College Predictor 2024 may be an important device for students aspiring to pursue medical education in India. By giving a realistic appraisal of the colleges you'll get into based on your NEET score, it makes a difference streamline the admission process, spares time, and decreases stretch. As you get ready for NEET 2024, make beyond any doubt to leverage this instrument to upgrade your decision-making and secure a situate in a college that best fits your academic and career objectives.
0 notes