#how is pleurisy diagnosed
Explore tagged Tumblr posts
Text
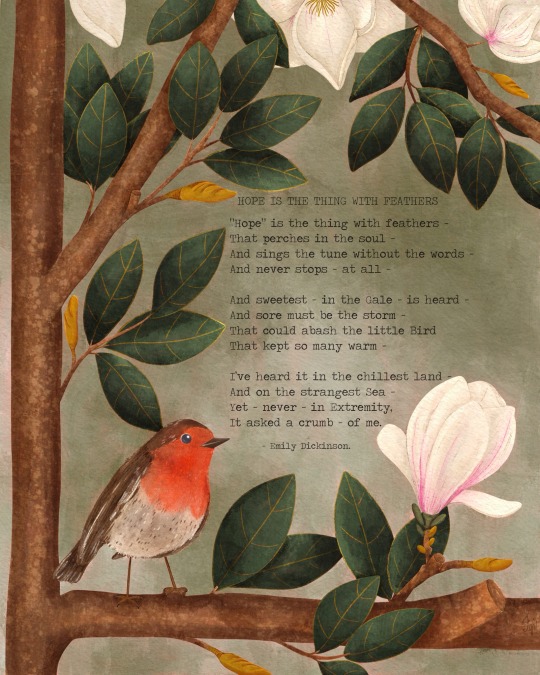
It (only) took me three weeks to finish this painting. I was supposed to paint it in May for LAM Awareness Month, but life got in my way and after getting pneumonia in April, I'm still recovering and have been on 24/7 supplemental oxygen and mandatory rest, making it hard to create.
June is Worldwide LAM Awareness Month, and this August marks 20 years since my diagnosis. Lymphangioleiomyomatosis (LAM) is a rare progressive lung disease affecting primarily women. It involves abnormal growth of smooth muscle cells and can cause symptoms like fatigue, chest pain (pleurisy), chronic cough, benign kidney tumours (angiomyolipomas), lung collapse (pneumothorax), shortness of breath (dyspnea), accumulation of fluid called chyle, in the chest cavity or abdomen (pleural effusion or chylothorax and angioleiomyomas). LAM Awareness Month aims to educate about the disease, raise funds to support patients, and inspire advancements in therapies.
In my 20 years with LAM, I’ve faced many challenges, I tire easily when walking and often need to take breaks to catch my breath. Climbing stairs, hills, and ramps is particularly challenging. My shortness of breath worsens in extreme cold and hot weather, and carrying heavy objects can leave me breathless. Even bending over and showering can trigger shortness of breath. I’ve experienced chylothorax, which led to my diagnosis, and have had four pneumothoraxes, five chest tubes inserted, two paracenteses, two thoracenteses, a pleurodesis, and a biopsy of cysts in the retroperitoneum (which was how I was ultimately diagnosed).
I hope that by sharing a bit of my experience, I can help you understand this disease better. For more information on LAM, please visit www.thelamfoundation.org and consider sharing this post to raise awareness for Worldwide LAM Awareness Month. @thelamfoundation.
Me llevó (solo) tres semanas terminar esta pintura. Debía pintarla en mayo para el Mes de Concientización sobre la Linfangioleiomiomatosis (LAM), pero la vida se interpuso y, tras contraer neumonía en abril, sigo recuperándome y he estado con oxígeno suplementario las 24 horas del día, los 7 días de la semana, y en reposo obligatorio, lo que me ha dificultado la creación.
Junio es el Mes Mundial de Concientización sobre la Linfangioleiomiomatosis (LAM), y este agosto se cumplen 20 años de mi diagnóstico. La linfangioleiomiomatosis (LAM) es una enfermedad pulmonar progresiva rara que afecta principalmente a mujeres. Implica el crecimiento anormal de las células musculares lisas y puede causar síntomas como fatiga, dolor torácico (pleuresía), tos crónica, tumores renales benignos (angiomiolipomas), colapso pulmonar (neumotórax), dificultad para respirar (disnea) y acumulación de líquido llamado linfa en la cavidad torácica o el abdomen (derrame pleural o quilotórax y angioleiomiomas). El Mes de Concientización sobre la LAM tiene como objetivo educar sobre la enfermedad, recaudar fondos para apoyar a pacientes e inspirar avances en las terapias.
En mis 20 años con LAM, he enfrentado muchos desafíos. Me canso fácilmente al caminar y a menudo necesito descansar para recuperar el aliento. Subir escaleras, cuestas y rampas es particularmente difícil. Mi dificultad para respirar empeora con el frío y el calor extremos, y cargar objetos pesados puede dejarme sin aliento. Incluso agacharme y ducharme pueden provocar dificultad para respirar. Sufrí un quilotórax, lo que condujo a mi diagnóstico, y me han realizado cuatro neumotórax, cinco tubos de drenaje torácico, dos paracentesis, dos toracocentesis, una pleurodesis y una biopsia de quistes en el retroperitoneo (que fue como finalmente me diagnosticaron).
Espero que al compartir un poco de mi experiencia, pueda ayudarte a comprender mejor esta enfermedad. Para obtener más información sobre LAM, visita www.thelamfoundation.org y considera compartir esta publicación para crear conciencia sobre el Mes Mundial de Concientización sobre LAM.
#WWLAM#WWLAM2025#rare disease#pulmonary disease#The LAM Foundation#LAM awareness month#frenchygv#frenchygvart#painting#botanical illustration#botanical art#digital painting#digital art#hope#lam#magnolia#magnolia tree#flowers#birds#poem#poetry#emily dickinson#hope is the thing with feathers#robin#robin bird#symbolism#symbolic#symbols#hope symbols
4 notes
·
View notes
Text
Can disability side of tumblr help me out? Particularly physical and autoimmune-related disabilities.
I got hit with a bunch of symptoms a little over a month ago that none of my care team can figure out. I'm going to list then below, and if you have any ideas for what I could suggest my care team look into, I'd really appreciate it! Disclaimer: I'm not asking to be diagnosed. I'm working closely with my doctors. Please don't reply/reblog with something like "no one here can tell you what this is, you need to see a medical professional." I am. I just want suggestions.
Anyway, list of new symptoms:
Chest tightness/pain (triggered by: standing, bending, walking "too fast," climbing/descending a short flight of stairs)
Shortness of breath (same triggers as above)
More fatigued than usual
Brain fog
Dizziness
Dry cough
Heart palpitations
Anxiety, not triggered by outside situations
Trouble focusing or staying present (even when my adhd meds are at what is typically their most effective time of the day)
This all began after I'd gotten the covid booster. Because of the timing, my doctored looked into, and ruled out, myocarditis and pericarditis, pleurisy, and general lung issues. Doc has now put me on an acid reflux medication for two weeks. I've been on it almost a week and nothing has changed (big surprise, I know). I did some digging, and I want to throw out the possibility of POTS to my doctor. That being said, is there anything else folks think would be a good idea to look into? Again, not asking to be diagnosed, but yall know how doctors are.
Even if you don't have suggestions, pretty please reblog this! Whatever this is has made it very difficult for me to do...well, most physical things. I could really use some suggestions!
#disability#disabled community#disabled#pots syndrome#pots#chronic illness#autoimmune disease#my posts
42 notes
·
View notes
Text
Apologies for this mental health rant but this is the only social site where my family don’t follow me and I feel like I could burst into flames I’m so angry so I need to get it out somewhere. I guess TW mental health, angry at parents, health stuff. Take care loves and scroll if you need to.
Now where was I - oh yeah -

It’s amazing how much one “well meaning” phone call from a parent can derail your day.
Apparently I’m “low” and “flat” and “I know you and when you’re focusing constantly on your health and staying in bed for weeks that means you’re depressed.”
Um no. Fuck right off. That was me 10 years ago when you were telling me exactly the same shit and it turned out I was genuinely chronically ill and in SEVERE and REAL pain, but you and others gaslit me into thinking it was in my head and made my life a fucking misery. Cheers for that.
So clearly, it won’t occur to you this time, that perhaps my mental health is, yes, a little down BECAUSE I’M SICK. That I spent over 2 weeks in bed not by choice and not because of my mental health but because I AM SICK. NOT THE OTHER WAY AROUND.

I was just coming out of this horrendous virus, JUST starting to piece my head back together from the cabin fever trauma horror of being so ill I was basically bedbound with the exhaustion of coughing and surviving and am still not quite well and have actual diagnosed-by-a-doctor pleurisy - like the lining of my ribs is INFLAMED WHAT MORE DO YOU WANT FROM ME?? Would you believe I was genuinely sick if I’d gone to hospital and wasted their resources just to prove how sick I was??? Is that what you want??
And the sad answer is even then it wouldn’t have been enough. I would’ve been being dramatic and overreacting and it would’ve still “clearly” been stress and depression caused, not literal actual illness.
Fucking parents man. You can be in your 30s and they still see you as the anxious gaslit 17 year old who died a long time ago.

3 notes
·
View notes
Text
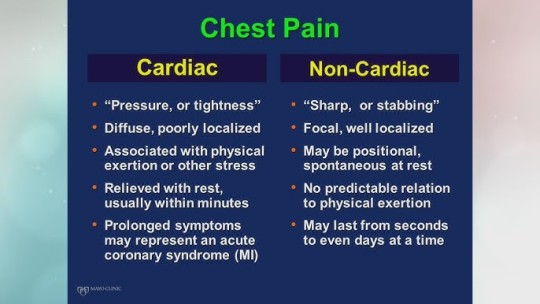
4 Key Differences Between Heart-Related Chest Pain and Other Conditions: Advice from a Chest Specialist in Raipur
Chest pain is a symptom that demands immediate attention, as it can indicate a range of underlying health issues—from benign conditions to life-threatening emergencies. One of the biggest challenges in medical diagnosis is distinguishing between heart-related chest pain and chest pain caused by other conditions. This distinction is vital because it directly impacts the course of treatment, urgency, and overall patient outcomes.
For patients of Raipur, a consultation with a Chest Specialist in Raipur guarantees proper diagnosis and treatment of chest pain. In this article, we present the 4 most significant differences between heart-related chest pain and others based on the Best Chest Doctor in Raipur's expert opinions. We further look at how the Best Doctors for Chest Pain in the city diagnose and treat chest pain to achieve effective and timely interventions.
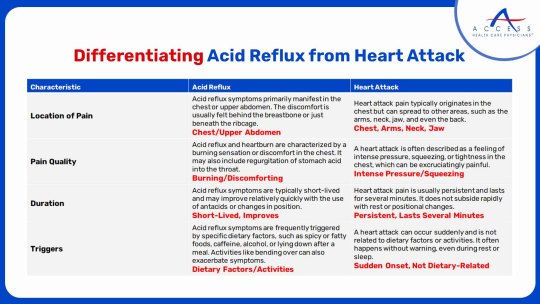
1. Location and Nature of the Pain
Heart-Related Chest Pain:
Chest pain of cardiovascular origin, commonly known as angina or the pain associated with a heart attack, is usually characterized as pressure, tightness, or squeezing in the middle or left side of the chest. It may extend to the shoulders, arms, neck, jaw, or back. This type of pain can persist for many minutes and could be precipitated or exacerbated by exertion, emotional stress, or large meals.
The pain is typically reported as a weight on the chest that cannot be ignored. It is usually accompanied by other signs like sweating, shortness of breath, nausea, or dizziness.
Non-Heart-Related Chest Pain:
Chest pain from other causes is typically different. For instance, pain from acid reflux or gastroesophageal reflux disease (GERD) is usually a burning kind of discomfort that develops after eating or when one lies down. Pain from musculoskeletal origins like costochondritis is stabbing and pinpoint, frequently exacerbated by specific movements or pressure on the chest.
A Chest Specialist in Raipur carefully evaluates the nature and location of pain to differentiate between these types. This differentiation helps in choosing the appropriate diagnostic tests and treatment.
2. Triggering Factors and Duration
Heart-Related Chest Pain:
Heart pain often is brought on by physical exertion or stress. As a result, climbing stairs or running can cause angina pain, which then remits with rest or medication such as nitroglycerin. Pain may be several minutes in duration and occasionally longer during a heart attack.
Non-Heart-Related Chest Pain
Contrary to this, anxiety or panic attack-induced chest pain tends to be sudden and not associated with physical exercise, accompanied by symptoms such as tachycardia, sweating, and fear of losing control. Chest pain induced by respiratory infections or pleurisy would tend to worsen with deep breaths or coughing.
Knowing these triggers is an important part of diagnosis by a Best Chest Doctor in Raipur. Knowing when and why the pain happens helps doctors limit the potential causes and determine the need for prompt intervention.
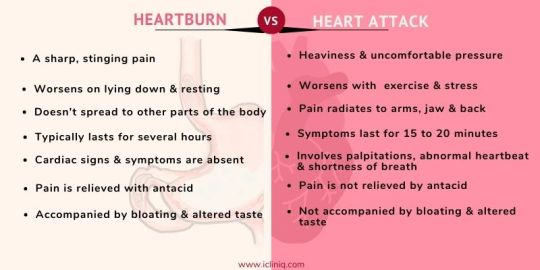
3. Associated Symptoms
Heart-Related Chest Pain:
Heart-related chest pain tends to be accompanied by symptoms including:
Shortness of breath
Excessive sweating
Nausea or vomiting
Lightheadedness or dizziness
Palpitations
These associated symptoms indicate that the heart is under strain or that blood supply might be impaired, necessitating urgent medical assessment.
Non-Heart-Related Chest Pain:
Pain of other origin within the chest can be associated with:
Symptoms of acid reflux such as sour taste or burning throat
Fever and cough in lung infections
Point tenderness or swelling at the chest wall for musculoskeletal pain
Symptoms of anxiety or panic such as shaking and sweating
A Raipur Chest Specialist performs a complete clinical assessment, considering these accompanying symptoms to effectively differentiate causes of chest pain.
4. Diagnostic Process and Treatment
Chest Pain Relating to the Heart:
Diagnostic measures for heart-related chest pain are:
Electrocardiogram (ECG): To identify irregularities in heart rhythm or evidence of a heart attack.
Blood Tests: To test for cardiac enzymes that confirm heart muscle damage.
Stress Testing: To assess the functioning of the heart under pressure.
Angiography: To see blockages in the coronary arteries.
Treatment can include drugs like nitrates, beta-blockers, or anticoagulants, and in selected cases, procedures like angioplasty or bypass surgery.
Non-Heart-Related Chest Pain:
For non-cardiac chest pain, the diagnosis can include:
Chest X-rays or CT scans: To detect lung infections, pulmonary embolism, or musculoskeletal disorders.
Endoscopy: For acid reflux or esophageal problems.
Psychiatric Evaluation: For anxiety-induced chest pain.
Treatment accordingly—antacids for acid reflux, antibiotics for infections, or counseling and medication for anxiety.
The Best Doctors in Raipur for Chest Pain adopt a holistic diagnostic strategy so that each patient gets a personalized treatment plan that treats the cause of the chest pain.
Importance of Consulting a Raipur Chest Specialist
Chest pain may indicate an array of various health issues, from benign to severe. Misdiagnosis may result in inappropriate therapy, prolonged healing, or even worse. Seeing a Chest Specialist in Raipur guarantees:
Precise diagnosis using state-of-the-art diagnostic equipment.
Effective and timely treatment customized to the patient's individual condition.
Holistic care, including follow-up and lifestyle guidance to avoid recurrence.
Conclusion
It is complicated to differentiate the chest pain related to the heart and other ailments but crucial for proper treatment. The skill of a Chest Specialist in Raipur is priceless in diagnosing the specific cause and delivering proper care. Whether it is cardiac, gastrointestinal, respiratory, or psychological pain, precise assessment and treatment are provided by the Best Chest Doctor in Raipur.
For professional Chest Pain Treatment in Raipur, Vidya Hospital is the best Pulmonologist in Chhattisgarh, providing end-to-end and empathetic care to chest pain patients to achieve improved health outcomes and comfort.
0 notes
Text
Pneumonia Specialist in Hyderabad: Expert Care for Your Respiratory Health

Pneumonia is a serious respiratory condition that affects the lungs, causing inflammation and fluid buildup. It can be caused by various factors, including bacterial, viral, or fungal infections. Symptoms such as cough, fever, chest pain, and difficulty breathing may indicate pneumonia, and timely intervention by a pneumonia specialist in Hyderabad is crucial for effective treatment and recovery.
At TX Hospitals, we connect you with the best pneumonia specialists in Hyderabad who are dedicated to diagnosing, treating, and managing pneumonia. If you or a loved one is experiencing symptoms or needs expert care, don't hesitate to call us at 9089489089 to book an appointment or get more information.
Why You Need a Pneumonia Specialist
Pneumonia is a potentially life-threatening condition that requires professional evaluation and treatment. A pneumonia specialist is a medical expert with specialized training in managing respiratory conditions, particularly pneumonia. Here’s why consulting a pneumonia specialist is essential:
Accurate Diagnosis: Pneumonia can have similar symptoms to other respiratory diseases, such as the flu or bronchitis. A pneumonia specialist uses advanced diagnostic tools, including chest X-rays, blood tests, and sputum cultures, to determine the type and severity of pneumonia.
Customized Treatment Plans: The treatment for pneumonia depends on its cause, whether bacterial, viral, or fungal. A pneumonia specialist will create a personalized treatment plan that includes antibiotics, antivirals, or antifungal medications, along with supportive care to help you recover faster.
Management of Complications: Pneumonia can sometimes lead to complications, such as pleurisy (inflammation of the lining around the lungs), lung abscesses, or respiratory failure. A specialist is well-equipped to manage these complications and prevent them from worsening.
Preventive Care: Pneumonia specialists also focus on preventive care, helping patients understand how to reduce their risk of pneumonia. This includes vaccinations, smoking cessation programs, and lifestyle changes to strengthen the immune system.
Leading Pneumonia Specialists in Hyderabad
Hyderabad is home to several renowned pneumonia specialists who provide top-notch care for individuals suffering from pneumonia and other lung diseases. Here are some of the best experts in the city:
Dr. B Vijay Bhaskar – Best Pulmonologist for Pneumonia Dr. B Vijay Bhaskar is a highly experienced pulmonologist specializing in Pulmonary Medicine. With an MBBS, MD in General Medicine, and DM in Pulmonary Medicine, he is one of the leading specialists in Hyderabad for treating pneumonia. His expertise in diagnosing and managing complex respiratory conditions makes him a trusted name for pneumonia treatment.
Dr. Naresh Dude – Experienced Pneumonia Specialist Dr. Naresh Dude, with qualifications such as MBBS, DNB, and FCCM, is a skilled pneumonia specialist in Hyderabad. He has extensive experience in managing both bacterial and viral pneumonia and offers personalized care plans for his patients. Dr. Dude’s thorough approach and compassionate care ensure the best outcomes for those battling pneumonia.
Dr. Rohith Reddy – Lungs Specialist Dr. Rohith Reddy is a highly skilled MD in Pulmonary Medicine who specializes in treating a variety of respiratory diseases, including pneumonia. His expertise in diagnosing and managing pneumonia, combined with his patient-centered approach, makes him one of the best pneumonia specialists in Hyderabad.
Dr. Sathish Pogula – Chest and Pneumonia Specialist Dr. Sathish Pogula, with an MBBS, MD, and IDCCM, is an expert in managing chest conditions and pneumonia. He is dedicated to providing effective treatments for respiratory infections, ensuring that patients with pneumonia receive timely and appropriate care.
Dr. M.V. Sree Keerthi – Leading Pneumonia Specialist Dr. M.V. Sree Keerthi, with her MBBS, DNB, and DTCD in Pulmonary Medicine, is a well-known specialist for treating pneumonia. Her experience in pulmonary medicine and dedication to patient care make her one of the top choices for individuals seeking treatment for pneumonia in Hyderabad.
Dr. M. Sai Sashank – Pulmonary and Pneumonia Specialist Dr. M. Sai Sashank is an experienced pulmonary specialist with an MBBS and MD. He provides expert care for pneumonia patients and ensures they receive the right treatment based on their condition’s severity and underlying causes.
Symptoms of Pneumonia
Recognizing the symptoms of pneumonia early can lead to quicker diagnosis and treatment. Some common symptoms include:
Persistent cough (with or without mucus)
Fever and chills
Chest pain, especially while breathing or coughing
Shortness of breath
Fatigue and weakness
Confusion (especially in older adults)
If you or a loved one is experiencing any of these symptoms, it’s important to seek medical attention promptly. A pneumonia specialist can help determine the cause and begin treatment to prevent further complications.
Book an Appointment with a Pneumonia Specialist in Hyderabad
At TX Hospitals, we work with the best pneumonia specialists in Hyderabad who are committed to providing you with the highest level of care. Our doctors specialize in diagnosing and treating pneumonia, ensuring that each patient receives personalized attention and the most effective treatment.
Don’t wait if you suspect pneumonia. Call 9089 48 9089 today to book an appointment with one of our expert pneumonia specialists in Hyderabad. Let us help you breathe easy and recover quickly.
Your health is our priority—trust TX Hospitals for the best care for pneumonia and other respiratory conditions.
#pneumonia specialist in hyderabad#best pulmonologist in hyderabad#pulmonologist hyderabad#pulmonologist doctor in hyderabad
0 notes
Text
Tietze syndrome: mild chest pain...
Tietze syndrome is a condition characterised by sharp, localised pain in the cartilage of the ribs, where they meet at the sternum. Although the exact causes are still somewhat mysterious, this condition is generally benign and heals spontaneously.

What are the symptoms?
The main symptoms of Tietze syndrome are :
- Pain: A sharp, localised pain in one or more chondrocostal joints (junction between the cartilage of a rib and the sternum). This pain may be aggravated by movement, coughing or deep breathing.
- Sensitivity: The affected area is very sensitive to touch.
- Swelling: Occasionally, slight swelling may occur in the affected joint.
What causes TMS?
The exact causes of Tietze syndrome are not yet fully understood. However, several factors may be involved:
- Repetitive strain injury: Repetitive movements or intense physical effort can irritate the chondrocostal joints.
- Viral infections: Certain viral infections may be the cause of cartilage inflammation.
- Immune disorders: Immune disorders may play a role in the development of the syndrome.
How is it diagnosed?
Tietze syndrome is generally diagnosed by a general practitioner or rheumatologist. It is based on a clinical examination and the exclusion of other causes of chest pain, such as a heart attack or pleurisy. Additional tests, such as an X-ray or CT scan, may be carried out to rule out other pathologies.
What is the treatment?
Tietze syndrome is generally a benign condition that heals spontaneously in a few weeks or months. The main aim of treatment is to relieve pain and inflammation. It may include :
- Medication: Non-steroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce pain and inflammation.
- Rest: It is important to rest and avoid activities that aggravate pain.
- Heat or cold: Localised application of heat or cold can bring relief.
- Physiotherapy: Breathing exercises and stretching can help improve thoracic mobility.
In short, Tietze syndrome is a benign condition that manifests itself as severe chest pain. Although the exact causes remain to be elucidated, treatment is generally symptomatic and provides rapid relief of symptoms.
If you are experiencing chest pain, it is important to consult a doctor for an accurate diagnosis and appropriate treatment.
Go further and contact
0 notes
Text
What Are The Common Signs Or Reasons For Pleurisy?
Have you ever experienced scary chest pain that occurs with every breath? This could be a sign of pleurisy, a condition that affects the thin lining of the chest and lungs called the pleura.
Although pleurisy is often misdiagnosed and misunderstood, it is a common condition. If you seek a high-quality physician, consider contacting Bansal Hospital in Bhopal. Check out our blog to learn more about pleurisy.
What Is Pleurisy?
The pain felt in the thin tissue of the chest wall (pleurisy pain location) that joins both lungs after breathing is referred to as pleurisy. Sharp chest pain that worsens with breathing is the result.
What Are Pleurisy Causes?
Pleurisy, or a lung infection resulting in inflammation and chest pain, is brought on by bacteria or viruses. Pneumonia can be caused by
Trauma or surgery
Rheumatoid arthritis
Blood clots in the lungs
Lung cancer
Sickle cell disease
Lupus
Pneumonia
Mediterranean fever
Tuberculosis
Fungal infections
What Are Pleurisy Symptoms?
Individuals with pleurisy experience distinct pleurisy symptoms. Some of them are:
Fever
Cough
Sneezing
Coughing
Heavy breathing
Some significant symptoms of Pleurisy are:
1. Pleural Effusion
Pleural effusion is the medical term for the accumulation of fluid in the lung tissue and a relatively narrow area. The tissue swells when there is a buildup of fluid, but when there is significantly less fluid, there is no swelling. Thus, there is no friction, which causes considerably less pain.
2. Atelectasis
Excess fluid accumulation can cause lung collapse because it puts more strain on the lungs and makes breathing complex and laborious. As the pulmonary pressure rises, the coughing gets worse.
3. Erythema
Empyema is a disorder where pus forms in the lungs as a result of an excessive buildup of fluid and feverish symptoms.
How Is Pleurisy Diagnosed?
The significant methods to diagnose pleurisy are:
1. Thoracoscopy
A tiny tube with a camera on it is inserted into the body during a thoracoscopy to examine the condition of the lungs and determine the best course of treatment.
2. Echocardiogram
The ECG is performed by applying electrode patches to the body to examine the heart's condition and determine that the seat should not be the source of chest pain.
3. Blood Test
The blood test is carried out to determine the parameters and examine any blood infections or signs of autoimmune illnesses.
4. The Fluid Is Tested
A tiny needle extracts the accumulated fluid from the lungs, after which the fluid is examined for signs of infection or pleurisy.
5. Imaging Test
The lungs and heart are examined using an MRI and CT scan to prevent severe repercussions.
How Is Pleurisy Treated?
The pleurisy treatment involves taking over-the-counter medications, such as aspirin, ibuprofen, or anti-inflammatory pharmaceuticals, for momentary relief. The majority of the time, pleurisy symptoms subside on their own with time, but severe cases necessitate medical attention and medication.
Your doctor might advise pleurisy medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids for your pain. The symptoms and illness of pleurisy can be treated with antifungal and antibiotic drugs.
What Are The Natural Treatments For Pleurisy?
Some primary treatments for Pleurisy are:
1. Tobacco Seeds
The anti-inflammatory effects of caraway seeds lessen the pleurisy symptoms. The natural analgesic properties of caraway assist in alleviating the cold and cough symptoms of pleurisy.
2. Ginger Tea
Ginger tea has anti-inflammatory properties and can limit the release of prostaglandin, a powerful anti-inflammatory spice.
3. Using Basal Leaves
Basal leaves or Tulsi treat the symptoms of coughing and fever. It is an excellent home remedy for pleurisy.
4. Turmeric Milk
Because of its potent antibacterial and antifungal qualities, turmeric helps to relieve pleurisy and chest congestion by reducing the likelihood of infection in the lungs and throughout the body.
5. Garlic
The anti-inflammatory properties of garlic can help to alleviate the symptoms of pleurisy. In sabji or any other recipe, incorporate 1-2 garlic cloves.
5. Say No To Smoking
Smoking should be put to an end because it can make lung infections worse and make breathing difficult. Smokers need to be aware of the harmful effects of heavy smoking.
When Should You See A Doctor?
It is recommended that you schedule a consultation with your doctor to discuss your symptoms and obtain an accurate diagnosis. However, certain symptoms may require urgent attention. This could indicate a more serious condition, and receiving prompt medical care is crucial to prevent any potential long-term effects on your well-being.
The Final Say
Understanding the usual pleurisy symptoms and causes is essential for early diagnosis and effective management of this ailment. Regular signs of pleurisy include a severe chest ache that worsens when breathing, coughing, or sneezing. Other symptoms, such as a fever, cough, and shortness of breath, might be used to detect it.
You can also contact the pulmonary department at the Bansal Hospital in Bhopal for any medical advice or care.
About Bansal Hospital
Bansal Hospital is a multispeciality hospital and is one of the leading, reputable and reliable healthcare providers trusted by patients and their families across the region. It has all the major departments, including cardiology, neurology, oncology, orthopaedics, gastroenterology, urology, liver transplant, bone marrow transplantation, nephrology, gynaecology and more. The hospital is equipped with state-of-the-art facilities and technology. It has a team of highly qualified and experienced doctors and medical staff who provide round-the-clock care to the patient.
Visit Our Website
0 notes
Note
hey i hope its ok to ask but i saw your post about lupus and i had some questions. 2 years ago i found out i was super anemic and i also got a positive ANA test but i didn't have enough symptoms for it to be concerning at the time..but now i'm experiencing more and more lupus symptoms but mildly. maybe im overthinking but was wondering how your stuff started? was it immediately kind of evident or very very slow? thanks and good luck with all. i hope you are able to get the care you need💛
(Omg I typed a whole-ass long story and then my phone died, AAAAAA! Here’s attempt 2...)
It’s absolutely fine to ask! I’m not too sure if my symptoms progressed slowly or fast, since originally my health declined at 13. Back then I suffered from fatigue, joint pains and depression. I got better at dealing with it through the years, and I honestly don’t know if it could have been early onset Lupus, or just depression.
Either way, my ‘severe’ symptoms started about 9 months ago, after I had probably caught a virus. It started with the frequent swelling of my lymph nodes, vague joints pains, and extreme fatigue. Those symptoms spanned several months, then disappeared. I also started noticing the skin in my face looked weird, and I remember fearing I’d developed rosacea like my dad, or that I was perhaps just getting old and ugly.
When the symptoms returned after a while, they were much more frequent and more severe. I couldn’t use the affected joints, and there were usually multiple affected at a time. Then the breathing issues started. I had pain breathing in, as well as pain all across my chest. I had heart palpitations, my heartbeat was always elevated, and I started having fevers every single day. My inflammations markers were over a 100, and it was then I got referred to an internist.
I tested positive for ANA, and after several examinations it was determined I have inflammatory fluid in both my lungs and heart. I have pleurisy, as well as pericarditis and myocarditis. I urinated blood, and I felt pain in my lower back. I have frequent headaches, brain fog, as well as difficulty concentrating and separating dreams from reality. I often feel dizzy, with a strange static within my skull. I also have frequent sores in my mouth and nose. I was then diagnosed with Lupus by a rheumatologist.
If the disease started at 13, then its development has been very slow. I did have really bad hair loss several years ago, and I have urinated blood without a bladder infection before. If it started at 27, then it’s been an absolute wrecking ball and it has developed very fast in my case. All in all, it’s very serious, and if you recognise any of these symptoms I think it’d be a good thing to try and get a diagnosis. The faster you get one, the better. I already have organ damage, and it’d be great if you could prevent that. I wish you all the best, and I really hope this helped. 💜
1 note
·
View note
Text
New Post has been published on Medical Reference. All of the diseases and ailments of the human body. How to recover from various diseases
New Post has been published on http://bit.ly/2FyCBQ2
Back pain emphysema - the world health org
#how is pleurisy diagnosed#how to relieve pleurisy#pleurisy caused by stress#pleurisy how long does it take to recover#what antibiotics treat pleurisy
0 notes
Text
SELF DIAGNOSIS
You can’t diagnose yourself.
I know it’s really cool right now to see self-diagnosis as a very empowering way to kick against the pricks in government who are stopping you from getting access to an affordable and reasonable psychiatrist, but you can’t diagnose yourself. You have a cough? You can’t diagnose yourself with emphysema, or pulmonary fibrosis, or metastasising cancer of the lungs, or pleurisy, or upper respiratory tract infection, or heart failure, or consumption, or whatever lung related complaint belongs to a fictional character you admire.
It is impossible to be objective about the self, this much we know. We can think we know ourselves and to some extent we do -- we can largely predict our reactions to things, our relationships to people, our feelings about events, and though there will be moments of outlying behaviour, thoughts and feelings, we can usually understand ourselves enough to know why we did or said something that we did or said. But we can’t know everything, because of COGNITIVE BIASES. This is when our interpretation of something becomes distorted owing to our long-held beliefs that have been formed over our lives because of our unique life experiences and social factors and biological factors that all come together in an idiosyncratic whole, and that whole is you, the person, who nobody else is like. But there are parts of yourself you have no idea about, and that’s totally normal. There’s no sociopath out there who knows everything about themselves and whilst we have a tendency to introspection and self-analysis, doesn’t mean we’re also highly trained psychologists, or that we even have the impossible ability to dissociate to such an intellectual degree that we can sit opposite ourselves, understand ourselves from the outside, apply that knowledge to ourselves, and give ourselves a diagnosis. You can read all the online literature and you can even feel a sense of recognition and identification with the thing you are reading, and once in a blue moon you may even be correct about yourself, but the chances are, you’ll miss some things.
And psychologists miss things too! That’s why there are self-report scales designed to work out what your intentions are without asking directly, because you may have a bias that confirms how you want to be seen, or how you want to feel about yourself (quick hint: when a psychologist asks you if you get more headaches than the average person, they don’t really care at all about your headaches). Malingering scales exist not to catch people out or humiliate people, but to see if someone’s perception of themselves matches up with what they tell to psychiatrists and psychologists. Personality measuring scales can be anything from a 250 question yes or no self-report, but then that progresses onto a structured clinical interview, a whole history of who you are and what made you, what illnesses are in your family, what formative experiences did or didn’t you have, what age were you when these things happened, who else was in your life, what were your friends like, what did normal look like to you and what does it look like to you now? And psychologists may not even agree. They most likely won’t. Your doctor will ask colleagues, higher-ups, may even write to the person who devised the test for more information. It takes years of schooling to even begin to diagnose a personality disorder, and even then, nobody can really fully agree what a typical personality disorder looks like. There’s no unique formula for sociopathy, you could have two twins raised in the exact same environment, doesn’t mean both or either or neither could become sociopaths. Because it’s hard to diagnose, and you cannot diagnose yourself.
And you may be friends with antisocials, you may identify with antisocials in your life, you may have a diagnosis already that you don’t agree with, but then what you may find you’re doing is altering the aspects of who you really are to fit into the bias you’ve created with an aspirational diagnosis. If you find yourself vehemently justifying behaviours you feel are not concomitant with ASPD so that they become excusable within the framework of ASPD, then you probably don’t have it. If your attachments in relationships and friendships and otherwise don’t stack up with antisocial attachment styles, then you maybe don’t have it. Yes, even if your manipulative behaviours are manipulative because of reasons that don’t apply to ASPD, then there’s a chance you don’t have it. Because you can’t diagnose yourself. You can’t sit with us. And honestly, why on earth would you want to?
35 notes
·
View notes
Text
THIS FUCKING SUCKS.
I had to go to the ER a couple of years ago because I had difficulty breathing and horribly painful coughs and they diagnosed me with pleurisy (it's line an infection of the lining of your lungs), gave me some pills and sent me home, telling me to follow up with my doctor. So a week later I went to my doctor to follow up on my infected lung, and I was told to lose weight. For a lung infection.
Just so you know how fucked this is, I AM A SMOKER. My doctor never suggested I stop smoking because of the lung infection. She, instead suggested that I lose weight.
On a separate occasion, my gf went to the dermatologist because of a scar she hates, and she was told to lose weight.
I CAN'T EVEN.

doctoring while fat
64K notes
·
View notes
Text
10 Questions You Should Ask Your Chest Specialist in Raipur About Chest Pain
Chest pain is a frequent but life-threatening symptom that has numerous potential causes, some of which require immediate medical care. Whether sharp and stabbing or dull and aching, chest pain can be caused by a multitude of causes, from cardiovascular disease to gastrointestinal disorders, musculoskeletal disorders, or anxiety. If you have chest pain, visiting a Chest Specialist in Raipur is necessary to determine the cause of it and to get proper treatment.
To assist you in making the best out of your visit, below are 10 important questions you must ask your Chest Specialist in Raipur about your chest pain. These questions will help you better understand your condition and what must be done to address and treat it properly.

1. What Are the Possible Causes of My Chest Pain?
One of the first questions that you need to ask your Chest Specialist in Raipur is about the potential reasons for your chest pain. Your chest pain may be caused by a number of conditions, some heart-related and others not. Some of the potential reasons are:
Heart disease: Angina, heart attack, or pericarditis.
Gastrointestinal problems: Acid reflux (GERD), peptic ulcers, or esophageal spasms.
Musculoskeletal conditions: Muscle strain, rib injury, or inflammation of cartilage between ribs (costochondritis).
Respiratory diseases: Pneumonia, pleurisy, or pulmonary embolism.
Anxiety: Panic attacks can also cause chest tightness or pain.
Having knowledge of the possible causes will help you and your doctor determine what to do next in diagnosing and treating your condition.
2. What Tests Do I Need to Diagnose the Cause of My Chest Pain?
Once your Chest Specialist in Raipur has assessed your symptoms, they may recommend a variety of tests to determine the cause of your chest pain. Some of the most frequent tests are:
Electrocardiogram (ECG): To assess the heart's electrical activity and detect any abnormalities, such as arrhythmias or signs of a heart attack.
Blood tests: To detect signs of a heart attack, inflammation, or infection.
Chest X-ray: To evaluate the lungs, heart, and ribs for any abnormalities.
Echocardiogram: Ultrasound of the heart to evaluate the structure and function of the heart.
Stress test: To observe how your heart functions under stress.
Endoscopy: To search for acid reflux or other problems in the gastrointestinal tract.
CT scan or MRI: In certain cases, to observe more detail of the chest area.
Asking about the tests will allow you to understand how your condition will be diagnosed and what you can expect from the process.
3. What Are the Symptoms I Should Be Concerned About?
It is important to know the symptoms that indicate that your chest pain could be a serious illness, such as a heart attack or a pulmonary embolism. Some red flags that require urgent medical care are:
Sudden, severe chest pain or pressure, especially if it radiates to the arm, jaw, neck, or back.
Shortness of breath, dizziness, or lightheadedness.
Nausea, sweating, or feeling of impending doom.
Pain that lasts longer than a few minutes or comes back over and over.
Coughing up blood or fainting.
By discussing these symptoms with your Chest Specialist in Raipur, you'll get a better sense of when chest pain might be a symptom of a life-threatening condition.
4. How Bad Is My Chest Pain? Do I Need Emergency Care?
It is important to know how urgently you require medical care. Although not all chest pain is a heart attack or other life-threatening condition, there are some causes of chest pain that are considered emergencies. Your Raipur Chest Specialist can help you determine whether your chest pain requires emergency treatment or if you can be treated as an outpatient.
If your pain is severe or accompanied by other symptoms like dizziness, nausea, or shortness of breath, it’s crucial to seek immediate medical attention. Your doctor will provide guidance on the next steps and whether hospitalization is necessary.

5. What Treatment Options Are Available for My Chest Pain?
After your Chest Specialist in Raipur has diagnosed the cause of your chest pain, he or she will recommend treatment based on your condition. Treatment can be:
Medicines: To treat chest pain caused by heart problems, nitrates, aspirin, or beta-blockers may be prescribed. To treat digestive issues, antacids or proton pump inhibitors may be administered.
Lifestyle Modifications: Your doctor may recommend dietary changes, exercise, and stress reduction to improve heart health or address gastrointestinal issues.
Surgical Procedures: In severe heart disease, an angioplasty, stent placement, or bypass surgery may be necessary to restore blood flow.
Physical Therapy: If the chest pain has musculoskeletal causes, physical therapy may be prescribed to relieve muscle tension and improve posture.
You must understand your choices and what is at stake with each choice.
6. How Can I Avoid Having Chest Pain Again?
Avoiding future occurrences of chest pain will allow you to better your overall health. A Raipur Chest Specialist can give advice on how to lower the risk of recurrence. Some of the usual preventive measures are:
Eating a healthy diet for the heart: Full of fruits, vegetables, lean meat and fish, and whole grains, and low in salt, saturated fats, and processed meat.
Exercise: Exercise strengthens the heart and promotes better circulation.
Stress reduction: Yoga, meditation, or deep breathing can all ease stress, a common cause of chest pain.
Quitting smoking: Quitting smoking reduces the risk of heart disease and other serious health conditions.
Preventive care will be needed to manage underlying conditions and reduce the likelihood of returning chest pain.
7. Are There Any Side Effects or Risks of My Treatment?
It's worth asking your doctor prior to any treatment what risks or side effects may be involved in the treatment. For example, medications for conditions of the heart can cause dizziness or gastric issues, and surgery has the risk of infection or hemorrhage.
Knowing this allows you to make an informed decision about treatment and to anticipate any resulting side effects.
8. How Long Will It Take for Me to Recover from Chest Pain?
Recovery time depends on the reason for the chest pain and the treatment. If your chest pain is due to a heart attack, recovery will take a few weeks with a gradual return to physical activity. Recovery will be quicker if the pain is due to acid reflux or musculoskeletal issues.
Your Raipur Chest Specialist will provide you with an estimated recovery time depending on your condition and treatment plan.
9. Can I Continue My Regular Activities While Managing Chest Pain?
It's essential to understand how chest pain is impacting your daily life. Depending on the severity and etiology of your chest pain, your Chest Specialist in Raipur may recommend avoiding excessive exertion, specifically in the context of cardiac-related chest pain. If it's pain related to stress or anxiety, you may be able to return to your daily routine after resolving the root cause.
Always consult your physician prior to going back to usual activities, particularly exercise or work activities.

10. How Often Should I Follow Up with You for Chest Pain Management?
Follow-up visits are necessary to see that your treatment plan is functioning properly and you're recovering as planned. Your Best Chest Doctor in Raipur will guide the frequency of visits based on your condition. Follow-up visits on a regular basis can track progress, adjust drugs, and catch any potential issues early.
Conclusion
Chest pain can be due to a variety of causes, and the cause needs to be identified so that appropriate treatment can be availed. If you ask your Raipur Chest Specialist these 10 important questions, you will be able to understand your condition properly and do the right thing.
For expert care and Chest Pain Treatment in Raipur, Vidya Hospital offers thorough diagnostic and treatment solutions. With experienced cardiologists and high-end machines, Vidya Hospital guarantees the top standard of care for chest pain, with prompt and efficient solutions for the condition. Vidya Hospital excels at being the Best Doctors for Chest Pain, offering different options in treatment and help in patients' cardiovascular well-being.
0 notes
Text
order online Tramadol. Fast Shipping! Where To Buy Tramadol
What is Pleurisy and how to treat it with Tramadol Opioid?
Pleurisy is an inflammation layer that covers the lungs called the pleura.
Therefore, the most common symptom of pleurisy is chest pain while breathing deeply. Or sometimes the pain is also felt in the shoulder like someone is throwing a stone.

visit here: https://tramadolovernightus.com/product-category/buy-tramadol-online/
call us: +1(707) 510-0015
Also, Other symptoms can include shortness of breath and a dry cough.
What causes pleurisy?
Therefore, Such as pneumonia and viral infection as flu are the main causes of pleurisy.
Moreover, in rarer cases, pleurisy happens by conditions. Such as blocking the flow of blood into the lungs or lung cancer.
However, pleurisy can affect people of all ages. But people above 65 years are most at risk because they're more likely to develop a chest infection.
Besides, the pleura are two thin sheets of tissue that separate the lungs and ribcage. One is a link to the ribcage and the other is a link to the lungs.
Alongside, Between the pleural sheets is a thin layer of liquid. That lube the pleura, helping to reduce friction when you breathe in and out.
Although, When there's inflammation. The surfaces of the two layers become rough.
This can cause the layers to rub together, the conclusion is pain and discomfort.
Furthermore, If you have an infection with a germ. Take painkillers regularly until the pain eases. Your doctor may prescribe stronger painkillers if the pain is serious.
What are the symptoms of pleurisy?
The most characteristic symptom of pleurisy is a sharp pain in the chest or shoulder. Hence, Some people report aching or burning pain.
The pain can get worse when the person is:
breathing deeply
coughing
sneezing
moving their chest or trunk
What is the Diagnosing of pleurisy?
Your doctor will discuss your symptoms with you. To examine your condition. Furthermore, Doctors use chest x-rays or CT scans to look at your pleura, lungs, and chest area.
just in case of any other conditions that have symptoms similar to pleurisy.
However, they may also do a blood test to check your white and red blood cell counts. indicating whether you have an infection.
Lastly, your doctor may remove some of the fluid from your pleura with a needle for testing.
What is the treatment of pleurisy?
However, the best treatment for treating pleurisy is taking a Tramadol opioid. However, we all are already aware of that, Tramadol is a strong painkiller.
Thus, which helps to reduce your pain. Also, manage your physical and mental health to handle this pain.
Alongside, this medicine you can manage your pleurisy chest pain. Thus, this medicine tramadol can help you reduce your chest pain.
Also, and make you assure that you would not get any problem while coughing.
Moreover, this opioid is a pain management opioid. It makes you feel relief from your pain.
And, this medicine also helps you to distract your mind that can move you to feel from messages.
Conclusion:
Besides, Pleuritis is caused by viral or bacterial infections. The coronavirus is a viral infection of the lungs. That can cause pneumonia and another bacterial infection in your lungs.
Moreover, It's important to get medical care if you think you have pleurisy. Making sure the cause is a viral infection, and get treatment from a doctor. Moreover, untreated pleurisy can lead to serious complications
References:
https://www.nhsinform.scot/illnesses-and-conditions/lungs-and-airways/pleurisy#causes-of-pleurisy
https://www.nhsinform.scot/illnesses-and-conditions/lungs-and-airways/pleurisy#:~:text=Pleurisy%20is%20inflammation%20of%20the,chest%20pain%20when%20breathing%20deeply
https://www.medicalnewstoday.com/articles/158813#symptoms
https://www.medicinenet.com/is_covid-19_one_of_the_causes_of_pleurisy/article.htm
https://www.aafp.org/afp/2017/0901/p306.html#:~:text=after%20initial%20treatment.-,Pleuritic%20chest%20pain%20is%20characterized%20by%20sudden%20and%20intense%20sharp,to%20the%20neck%20or%20shoulder.
0 notes
Photo
My thusband had pleurisy from mold exposure at their old job. We didn’t know that’s what it was...all we knew was that they were having chest pains and trouble breathing. So obviously I rushed them to the ER. We were there for 12 hours. After 6 hours they told us that they were perfectly fine. They didn’t see anything that could be causing the pain at all. 6 more hours just waiting to be discharged...with no prescriptions or anything it just took them that long to disconnect the equipment and tell us we could leave.
They didn’t have insurance back then so the bill was $7,500. $7,000 was just for sitting in the hospital. $500 for the actual tests billed separately. For them to literally do nothing.
How did we know they actually did have pleurisy? We went to their E.N.T for unrelated reasons but mentioned it anyway because, surprise surprise the symptoms hadn’t magically gone away, and he was able to make the actual diagnoses. He was a hearing loss specialist and he could figure out without fancy equipment that they had pleurisy.
Fuck the American health care system.

9K notes
·
View notes
Text
Fucking ignore this
When I was about fourteen, I began having these incidents. Where I would be laying in bed, scrolling through the internet and my heart would suddenly start going nuts. My chest would hurt, I couldn’t breathe, my skin would get clammy and I’d get sweaty. The incident would last about ten minutes, and things would calm down...
After the first few, I told my mother, who took me to the doctor. A new pediatrician took over my file from my old and immediately declared the incidents were panic attacks. My mother suggested it might be related to the asthma I had been diagnosed with as a baby, and the doctor announced that no, it absolutely was NOT asthma, it was PANIC ATTACKS and she had EXACTLY the medicine for that. Where I would have developed asthma she had no idea. All those doctors from years past had no idea what a PANIC ATTACK looked like and she knew. I didn’t have words to ask if it was my heart. I was 14, I had been getting my period, I was scared of the world, I hated everything and I couldn’t breathe right or play because I was allergic to pretty much everything in the world. Why would I know how to ask someone to look at my heart? She demanded we go to a therapist and be diagnosed for my OBVIOUS anxiety and panic attacks, and she refused, outright to look for any other solution. So we went ot hte therapist I had been going to since I was 8... and he wrote a not-so-kind letter back to the doctor requesting she kindly not diagnose his long time patients with conditions they did not have, and to look for a PHYSICAL reason as she was NOT a psychology doctor she was a physical doctor and to kindly stay in her lane in the future and take a look for a medical reason for these incidents.
The incidents continued, after being told off by the psychologist, she reluctantly admitted the incidents COULD possibly be asthma, and I just needed to take my asthma medication when they happened.
Except, I had been. the medication made them worse, and I would end up shakey, disorientated, and uncomfortable because my heart would thud in my ears.
Side effects of the asthma medication, you’re having asthma attacks. You have asthma, so it’s nothing but that.
I learned to hate my asthma medication. It made my chest hurt worse, I could breathe, but my head would pound I felt like the world was caving in around me, I was paranoid (I didn’t know the word) and jittery...
The incidents continued. Every doctor would take a look at my medical history and announce it was asthma.
Not one ever looked at my heart.
The incidents get worse under stress, physical or mental. Most times I won’t be doing anything though. I’ll get excited, and happy... and it’ll happen. I’ll be mostly calm and see something that makes me superbly happy... it happens. When I get stressed my heart feels like it’ll jump from my chest, like it’s beating against my ribs and I feel choked. My lungs tighten up, my blood rushes and pounds in my ears, and my body goes clammy and cold and then I begin coughing and choking because there isn’t enough air. I black out sometimes, because there’s no air. It turns into an asthma attack. I take my inhaler. I can breathe, but the thudding heart remains, the headaches change, but stay, my skin doesn’t get warm, and I shake.
Every medical professional declared the same thing. It’s just your asthma. You don’t have anything else wrong with you. It’s allergies and asthma. When I got older, I got overweight. Now the diagnosis is that I’m too fat. I need to lose weight, and everything else is nothing but asthma. You have asthma, so that must be it.
I learned control. When the incidents begin, I stop, I control my breathing, I close my eyes. I force my breathing to go a certain way so the muscles push against my heart and force it to stop beating so hard. I breathe, I take deep breathes and concentrate on which parts of my lungs to inflate most, to squeeze my heart for seconds at a time, to make it stop feeling as if it’ll burst out of my chest. I flex my pec muscles to squeeze everything down, I rotate my shoulders to align my ribs so I can push against my own chest and stop my flighty organs from going haywire.
I got electorcated at work, twice in the same day. My boss was forced by OSHA to take me to the hospital. He dropped me off at the ER door and drove away. The ER nurses declared I hadn’t been electorcated, because they couldn’t find K in my blood. By the time OSHA forced my boss to take me to the ER, it had been nearly an hour, my back was locked up, and I had felt the electricity go through my heart. The ER said my heart was fine, my lungs were clear. But I had asthma, so breathe this nebulizer. The chest pains were nothing but asthma.
My dad pushed a factory job on me, the stress of being on the assembly line caused it again, I passed out that time. I whited out. I was fine and looked away from the line, but everything wouldn’t stop moving and I couldn’t concentrate on my method for stopping it. My dad insisted it was dehydration and undernourished. The doctor said it was asthma. We paid 200$ for the doctor to ignore my pleas to check my heart. Something was -wrong- would they please just LOOK at my heart... something was WRONG. You have asthma, this was nothing but an asthma attack. You need to keep your inhaler on you and take it. That’s all.
I’ve had “walking pneumonia”, and I’ve had lower pneumonia. I’ve had pleurisy... I’ve had lots of respiratory illnesses over the years. My mother, father, grandparents, great grandparents, several uncles and aunts, and even great aunts and uncles have all had heart issues. My mother has 3/4 of a heart, one chamber doesn’t beat properly, particularly when she gets stressed.
My father’s had two bypass surgeries already.
I continue to have incidents. And I’ve been sick for over a year, never -really- getting better. Only a week or two of good days.
My lungs feel like when you try to blow a balloon up underwater, and when I do get air in them, it feels like there’s only half as much as there should be.
I saw a doctor about 6 weeks ago, he heard me coughing. It was bad, a hard barking cough that threatened to make me pass out again. I’ve had it on and off for a year. If I laugh too much now, I start coughing and then I have an incident.
I told him that. I told him I’ve been sick for a while, but can’t do anything about it, I told him my chest hurts, if I laugh or get stressed I start coughing, and I told him sometimes I’ll just get excited and my heart will start going weird and wild, then I start coughing.
“Have you been tested for asthma, that breathing problem sounds like asthma”
“I’ve had asthma since I was a baby.”
“Oh well there you go, it’s just asthma attacks.”
Now. Covid-19 is around, everyone is going off. “You should get that checked out, it sounds bad.”
“You should go to the doctor”
“You should get ot the hospital”
Why?
all they are ever going to tell me is that I have asthma. Because after 36 years of very distinctively different feelings when I have an asthma attack and ~an incident~ and now this sickness. I clearly don’t know what my own asthma attacks feel like. But every fucking doctor out there will know it in thirty seconds from looking at my health records.
I’m fat. I have asthma.
They will never check to see why asthma meds don’t help. They will never check my heart. They will never test me for a virus. They will never test me for pneumonia, or flu, or anything else.
I have to INSIST for a strep test when I get strep because:
“You have asthma”
“It’s just an asthma attack”
“Take your inhaler”
If I go to the doctor I pay for the privilege of being told, for the millionth time, that I have asthma.
Because if it was ever anything else, they would have to do actual work.
I have NEVER had a stress test, I have only ever had one EKG (when I was electrocuted) and since becoming an adult I haven’t had a single chest xray.
0 notes
Text
The Long Literary Haul
I suppose its time to vent about the subject that I probably keep the most closed off. I'm not afraid to discuss many things, from sexual health and gender identity all the way to masculinity and emotional barriers... and I pride myself in that. When it comes to my own illnesses, however, it becomes very uncomfortable for me.
I grew up in a single parent house. My mom busted her ass as a machinist, house cleaner, you name it all to keep us going. When she was diagnosed with Lupus, she kept working until she felt she couldn't anymore. (In her forties was her diagnosis timeframe) For my diagnosis, I had just returned to college that September. Had a relatively new job. Was cast in my first male role of any consequence. I had been having trouble breathing, had back pain and was generally just feeling sick. Eventually, I knew I had to at least go to the doctor. They sent me straight to the ER where I was immediately admitted. I had double lung pneumonia and pleurisy, quarantined to a room for 8 days. I wasn't getting better. I had huge red patches on my legs. My temperature was 104s. I didn't want to eat anything. I was quite literally dying. They finally gave me the diagnosis of Lupus, Rheumatoid Arthritis and Sjogrens. I was only 23. Being the person that I am, all I wanted to do was get back to rehearsals. So after I was discharged I went home, slept for 24 hours and went right back to college. That sets up the scene for how I am.
Flash forward to now, almost 10 years later. I'm on an injectable low dose chemo medicine called methotrexate, which isn't doing enough for me. The next step is infusion therapy. I've been putting it off for about 2 years for a variety of reasons.
I'm hurting.
The way we Lupies best describe our condition is to imagine you have the flu. That run down, exhausted, ache in your bones, feverish stuff we all know and loathe. Now picture being told that's a good day for the rest of your life. That's this autoimmune disorder. I consider myself lucky in that my RA is more active than my Lupus. I'm not currently showing organ damage, which is what tends to happen. (Kidneys are usually the first) But I feel like I'm 80 most days. There is always something bugging me. Tendonitis, stiffness, movement/flexibility pain... you name it. Its exhausting.
It compounds when I factor in having Raynaud's (which is a circulation problem in your extremities), IBS and panic disorder. I never know what I'm going to get on any given day. The panic is the newest and something that has mangled my life. I'm far better than I was when Celexa first brought on the start of my panic cycles (I had a very rare reaction to it that essentially brought on PD where I'd never had it before in my life) but I still deal with dizziness, shortness of breath, vision disturbances and disassociation at random.
I've gotten really...autobiography here, but I feel like it needs stated for backstory.
Where I'm at now with trying to heal mentally and make my life better is...I don't know how. I am overwhelmingly stuck. For the past 6 months or so, I feel myself getting worse. My lupus butterfly rash looks like a sunburn on my face constantly now. I'm having new symptoms I've never had before (like mouth ulcers) and just....generally feel myself slipping. I power through every day because I know its what I have to do. I cannot afford to live off what disability would offer. I help my mom pay for her house. But I'm tired. Its something that doesn't get better with sleep. (A fun fact of Lupus is that sleep is not restorative like in healthy people. I recharge probably 25% to someone else's 100%) I mentioned my mom in the first part because as loving and amazing as she is, she always compares my journey to hers. She uses her experience to tell me why I'm not doing enough. That its not enough. That I'm essentially letting her down. I've told her so many times that its hurtful and unfair. I can't get it to stick. I'm thankful her illness is not as severe as mine. She has enough other shit on her plate. But when I am entirely honest with myself about how I feel daily... I'm terrified to keep living. I don't want to be that old man gnarled over his walker in agony. To need to be in assisted living. I couldn't even afford that anyhow. I don't have kids or a partner. Who will look out for me? I'm already getting forgetful. I'm so behind on some medication plans because I simply cannot remember to take them. I forget to change laundry over when its in the same room as me. It is scary stuff that I just push out of my head and wall off. My anxiety makes me terrified to die and my body makes me not want to live. Its a vicious mingling in my soul. Maybe that's why my emotions have shut so far down. I live now to make sure my mom is taken care of in her golden years, because she did it so selflessly for my grandparents. What after? What purpose, to what end, for me?
I don't expect to feel healthy and "normal" again. I just want some hope. I'm just not sure where to find it. I'll keep looking for as long as I am able, though. Keep working until you cannot.

0 notes