#hbot
Explore tagged Tumblr posts
Text
Also preserved on our archive
Some interesting science analyzed
BY BROOKS LEITNER
Imagine lying back in an enclosed chamber where you bask for 90 minutes in a sea of pure oxygen at pressures two to three times that felt at sea level. This is the world of hyperbaric oxygen therapy (HBOT), a technology that’s been around for decades and is now being explored as a possible treatment for Long COVID.
"The silence on the inside is deafening at first,” says John M.,* who has undergone dozens of HBOT treatments for his persistent Long COVID symptoms. Fortunately, there is a television outside the chamber in view, and it is easy to communicate with the provider if needed. While the potential protocol is still being refined, patients may undergo up to 40 HBOT sessions to address some of the most problematic, lingering symptoms of this complex condition.
HBOT is a therapeutic process that has been widely used to treat such conditions as decompression sickness in scuba divers, carbon monoxide poisoning, and diabetic foot ulcers. In HBOT, the body is exposed to 100% oxygen, a significant increase from the 21% oxygen concentration we typically breathe. The therapy takes place in an enclosed chamber where the air pressure is elevated above normal levels. The combination of high-pressure and high-oxygen conditions enhances the amount of oxygen that can reach the body's tissues. The hope is that this therapy can provide the same relief and healing to people with Long COVID that it does for those with other conditions.
According to John M., HBOT was the first treatment that helped with his sleep and reduced his heart palpitations. “At one point after hospitalization, my Long COVID symptoms were so bad that I could barely walk or talk. HBOT was a great tool that really assisted with my recovery,” he said. John added that he hopes the medical community will achieve a better understanding of how HBOT can help relieve suffering for patients with Long COVID and that more research will increase access to this innovative therapy.
Does HBOT improve Long COVID symptoms? One key observation from the work of Inderjit Singh, MBChB, an assistant professor at Yale School of Medicine (YSM) specializing in pulmonary, critical care, and sleep medicine, is that Long COVID patients often experience debilitating fatigue. Based on Dr. Singh’s previous Long COVID research, the exhaustion is thought to be linked to the muscles’ inability to efficiently extract and utilize oxygen.
To picture how HBOT might work, you can think of your muscles as engines sputtering, struggling to get the fuel they need. If oxygen is the gas that fuels the muscles, it’s as if you are trying to complete your daily routine while the gas tank is running on “empty.” By aiming to directly address this oxygen utilization impairment, HBOT may be a potential solution.
A systematic review by researchers at the China Medical University Hospital noted that HBOT could tackle another major factor in the Long COVID puzzle: oxidative stress. This relates to the body's struggle to maintain balance when harmful molecules, known as free radicals, run amok, causing chronic inflammation.
Research co-authored by Sandra K. Wainwright, MD, medical director of the Center for Hyperbaric Medicine and Wound Healing at Greenwich Hospital in Connecticut, suggests that HBOT, with its high-oxygen environment, might dampen this chronic inflammation by improving mitochondrial activity and decreasing production of harmful molecules. Other potential benefits of HBOT in the treatment of Long COVID may include restoration of oxygen to oxygen-starved tissues, reduced production of inflammatory cytokines, and increased mobilization of hematopoietic stem cells—primary cells that transform into red blood cells, white blood cells, and platelets.
HBOT for Long COVID: Current and ongoing research Several small-scale reports have indicated that HBOT is safe for patients with Long COVID.
To address this question, a trial that followed the gold standard of modern medical research—a randomized, placebo-controlled, double-blind design—assigned 73 Long COVID patients to either receive 40 sessions of HBOT or a placebo of only 21% oxygen. The study observed positive changes in attention, sleep quality, pain symptoms, and energy levels among participants receiving HBOT. In a longitudinal follow-up study published in Scientific Reports, the authors at the Tel Aviv University found that clinical improvements persisted even one year after the last HBOT session was concluded. In a second study, the same authors focused on heart function, measured by an echocardiogram, and found a significant reduction in heart strain, known as global longitudinal strain, in patients who received HBOT.
In another study, 10 patients with Long COVID underwent 10 HBOT treatments over 12 consecutive days. Testing showed statistically significant improvement in fatigue and cognitive function. Meanwhile, an ongoing trial at the Karolinska Institute in Sweden has reported interim safety results wherein almost half of the Long COVID patients in the trial reported cough or chest discomfort during treatment. However, it was unclear whether HBOT exacerbated this symptom or if this adverse effect was due to the effort of participation by patients suffering from more severe Long COVID symptoms.
Is HBOT currently available as a treatment for Long COVID? For HBOT to become a mainstream treatment option for Long COVID, several critical priorities must be addressed. First, there is currently no established method for tailoring HBOT dosages to individual patients, so researchers must learn more about the specific features or symptoms that indicate potential benefits from HBOT. At the same time, we need to identify factors that may be associated with any adverse outcomes of HBOT. And finally, it’s important to determine how long these potentially beneficial effects last in a larger cohort. Will just a few HBOT trials be enough to restore patients to their baseline health, or will HBOT become a recurring component of their annual treatment regimen?
For now, HBOT remains an experimental therapy—and as such is not covered by insurance. This is a huge issue for patients because the therapy is expensive. According to Dr. Wainwright, a six-week course of therapy can run around $60,000. That’s a lot to pay for a therapy that’s still being studied. In the current completed studies, different treatment frequencies and intensities have been used, but it’s unclear how the treatment conditions affect the patient’s outcome.
“I have had some patients notice improvements after only 10 or 15 treatments, whereas some others need up to 45 treatments before they notice a difference,” notes Dr. Wainwright. “I think that HBOT is offering some promising results in many patients, but it is probably a strong adjunctive treatment to the other spectrum of things Long COVID patients should be doing, like participating in an exercise, rehab, and nutritional program.”
Dr. Singh notes that “a major challenge for research is the heterogeneity of Long COVID. It is hard to determine which symptoms to treat and enroll patients into trials based on them.”
Perhaps treatments that target multiple issues caused by Long COVID, like HBOT, may help overcome this challenge.
*Not his real name.
Brooks Leitner is an MD/PhD candidate at Yale School of Medicine.
The last word from Lisa Sanders, MD: Hyperbaric oxygen therapy (HBOT) is just one of the many existing treatments that are being looked at to treat Long COVID. We see this with many new diseases—trying to use a treatment that is effective in one set of diseases to treat another. And there is reason for optimism: We know that HBOT can deliver high levels of oxygen to tissues in need of oxygen. That’s why it’s used to treat soft tissue wounds. If reduced oxygen uptake is the cause of the devastating fatigue caused by Long COVID, as is suggested by many studies, then perhaps a better delivery system will help at least some patients.
Studies referenced:
bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-023-08002-8
www.ncbi.nlm.nih.gov/pmc/articles/PMC8806311/
www.nature.com/articles/s41598-024-53091-3
www.nature.com/articles/s41598-022-15565-0
www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1354088/full
www.ncbi.nlm.nih.gov/pmc/articles/PMC11051078/#:~:text=Proposed%20Mechanism%20of%20HBOT%20o
#long covid#hbottherapy#HBOT#hyperbaric oxygen therapy#mask up#covid#pandemic#wear a mask#public health#covid 19#still coviding#wear a respirator#coronavirus#sars cov 2
37 notes
·
View notes
Text
Good News From Israel
In the 12th Jan 25 edition of Israel’s good news, the highlights include:
Massive increase in Israel’s PR budget.
Life-saving Israeli treatments for the brain, heart, and traumatic stress.
Golan Druze rush to become Israeli citizens.
Two innovative Israeli laser systems perform valuable non-military functions.
Israeli sustainable device for keeping farm produce fresh is so cool.
A dozen Israeli companies doubled their US market value in 2024.
Light one candle for Peter Yarrow of Peter, Paul & Mary, who “Puffed” magic songs.
Read More: Good News From Israel

With Israel fighting a war on at least seven fronts, Israelis have to focus on priorities.
This newsletter contains articles about those Israelis whose priority is defending the nation's citizens, rebuilding homes, rehabilitating the wounded, volunteering, advocating, integrating into society, or continuing the successful path they were on before Oct 7th 2023.
Then there are the many Israelis who are focused on activities to benefit humanity - developing life-saving medical devices; researching cures for critical diseases; saving endangered species or searching for the "elixir" for longer life.
Israeli scientists have developed focused lasers for communicating or protecting crops; coating to stop fires spreading; a device to keep fruit & veg fresh; AI systems to restore speech to the mute, or radically shorten the time to build new products. And foreign investors and multinationals are certainly focused on joining in with Israel's success.
The photo from one of the posters at Ben Gurion airport shows the focused attention that young Israelis are giving to their hi-tech training. Israel is focused on giving the next generation the skills to become the central focus of the future success of the Jewish State.
#aneurysm#anti-bacteria#Artificial Intelligence#Down syndrome#Druze#Eilat#Expo#Gaza#good news#HBOT#Houthi#IDF#Israel#Jerusalem#Jewish#lasers#Nvidia#Peter Yarrow#PTSD#Wix.com
24 notes
·
View notes
Text
Suicide Statistics and Brain Wound Insights: PART 2

"In the past 18 months, three experienced Super Hornet pilots have died by suicide. According to their families, all had symptoms consistent with brain injuries." NYT Dave Philipps PRESS SUMMARY ON SUICIDES Dave Philipps of the New York Times continues his reporting on brain wounds inflicted on US service members using their own technology, in this case Top Gun pilots. Previously, he has looked at artillery and mortar crews, grenade instructors and Navy SEALs. In this case, Top-Gun Navy Pilots Fly at the Extremes. Their Brains May Suffer, he reports on Project Odin's Eye, which extends a study already underway with SEALs to assess the impact of Operator Syndrome. Operator Syndrome is a unique pattern of interrelated medical and behavioral health-care needs, typically experienced by Special Operations warriors, to include pilots flying high-G fighters. The symptoms closely parallel polytrauma, including "traumatic brain injury effects; endocrine dysfunction; sleep disturbance; obstructive sleep apnea; chronic joint/back pain, orthopedic problems, and headaches; substance abuse; depression and suicide; anger; worry, rumination, and stress reactivity; marital, family, and community dysfunction; problems with sexual health and intimacy; being "on guard" or hypervigilant; memory, concentration, and cognitive impairments; vestibular and vision impairments; challenges of the transition from military to civilian life; and common existential issues." Readers of this space know that many of the above symptoms can be addressed using Hyperbaric Oxygen Therapy (HBOT) for alleviation and healing of many of those brain and other bodily wounds, including behavioral and cognitive damage. Military Medicine published a piece, Cumulative Blast Impulse Is Predictive for Changes in Chronic Neurobehavioral Symptoms Following Low Level Blast Exposure during Military Training looking for predictors of long term brain health. The research looked at peak blast overpressure, impulse, total number of blasts, Time in Low-Level Blast Occupation, and Time in Service all showed strong evidence of influence on Neurobehavioral System Inventory (NSI) scores after blast exposure. In simple terms, repeated blast exposure correlates with negative brain health outcomes. Reinforcing the negative consequences of thousands of high-G-force insults to the brain, Special Warfare Combat Crewmen (SWCC) boat Veteran Anthony Smith writes in the Havok Journal: "At 65 mph, the boat slams into a wave about once every second. 3,600 impacts happen in an hour. The impacts can be as hard and severe as 125 rotational g-forces on the head and neck, producing severe whiplash and sub-concussive impact. Often, it’s only about 35 or 40 g. Pretty typical." Increasing numbers of SWCC boat operators are coming to TreatNOW for help with Allostatic Overload (Operator) Syndrome. Smith's survey of 1000 led to 314 responses. 299 of the 314 were verified SWCC operators, representing 3,584 years of SWCC experience. Of the fifteen (15) who were not SWCC, two (2) were SEALs, two (2) were fleet officers who had served in the Special Boat Teams, one (1) was a USCG Warrant Officer, and nine (9) were NSW combat service support personnel. The median age was fifty (50), and median number of years served as SWCC was eleven (11), while most completed five (5) deployments. 100% of respondents had service time on SWCC fast boats and are now living with long-term effects of traumatic brain injury (TBI), whiplash-associated disorders (WAD), and musculoskeletal disorders (MSD), including cognitive impairment, neuroendocrine dysfunction, sleep disorders, chronic pain, and psychological disorders. To summarise: A constellation of symptoms related to insults to the brain from a variety of forces in various service categories leads to brain wounding that can be addressed with Hyperbaric Oxygenation. HBOT is used safely, effectively and infrequently across the DoD. Donations and volunteers are helping the brain wounded, without national government funding, get into HBOT treatment across the US. Ten states know better and have collectively appropriated over $32 Million to treat TBI/PTSD using HBOT. The USG has to wake up and pay for HBOT treatments. The suicide epidemic needs ACTION to heal brain wounds, not only more research and public service announcements, call centers, cooperative agreements, and "lethal means safety." The continuing diagnosis and treatments aimed at "mental health" have to be expanded -- perhaps even expanded -- into "healing brain wounds." Final Note: A deep-dive into HBOT for COVID and PTSD is in the The Empowering Neurologist Podcast, Dec 09, 2024. Dr. Amir Hadanny is interviewed by Dr. David Perlmutter in "Hyperbaric Medicine Revolution." The discussion focuses on enhancing the oxygen availability to the brain for mitochondrial dysfunction, a powerful therapeutic tool across a wide variety of neurological issues like head injury/TBI/PTSD, concussion, Operator Syndrome, dementia, stroke and even long COVID. As Congressman Greg Murphy, MD (R-NC) recently put it to CBS NEWS, ” I believe it is medical malpractice not to offer this to our Veterans.” Heal Brains. Stop Suicides. Restore Lives. TreatNOW ****************************** The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, get patients off most of their drugs, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma from AHI and Burn Pits. Diabetic Foot Ulcers have become a major emphasis. www.treatnow.org Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made. Read the full article
#braininjury#brainwound#HBOT#HBOTTreatment#HealingwithHyperbarics#hyperbaricchamber#HyperbaricOxygentherapy#suicide#SuicideStatistics#VeteranSuicide#VeteranSuicidePrevention
3 notes
·
View notes
Text
Bon et bien cette fois c’est vraiment la fin de l’oxygénothérapie hyperbare.. Ma 100ème séances dont j’étais si fière était donc la dernière. Pour rappel j’en faisais gratuitement dans un centre depuis plus d’un an. C’était donc prévisible qu’à tout moment cela allait s’arrêter car il s’agit d’une thérapie extrêmement coûteuse et les propriétaires m’en faisait juste de bon coeur. À plusieurs reprises je pensais que c’était la fin car il y eut des périodes où je ne pouvais plus en faire (je vous en ai parlé à chaque fois). Sauf que cette fois les caissons quittent définitivement l’endroit où j’en faisais et donc ne me sont plus du tout accessible. Je suis reconnaissante d’avoir pu en bénéficier pendant tout ce temps, c’était digne d’un miracle, et tout le monde n’a pas cette chance. Cela va être violent pour mon corps de passer de minimum une séance par semaine à plus jamais. Mais au moins j’ai l’oxygène à la maison, malheureusement ce n’est pas autant efficace que l’hyperbare mais ça fait l’affaire pour calmer les douleurs sur le moment. D’ailleurs j’avais pris rendez-vous avec le spécialiste durant le mois où je pensais que l’oxygène hyperbare était définitivement terminé. C’est en lui parlant de ma situation avec l’oxygène qu’il avait de lui même décidé de m’en mettre à domicile. J’ai ensuite eu la nouvelle que je pouvais à nouveau faire de l’hyperbare mais je savais que c’était bientôt la fin, je vous avais d’ailleurs partagé que je ne savais pas pour combien de temps, mais au final ce n’était que pour très peu.. C’est donc très bien que j’ai pu anticipé la fin de l’oxygène en allant voir ce spécialiste et ainsi avoir une alternative pour l’oxygène. À voir ce que ça donnera sur mes symptômes de n’avoir que de l’oxygène normobare.

4 notes
·
View notes
Text
Steps you can take now to start taming inflammation:
1. Prioritize anti-inflammatory foods:
•Heathy fats (omega-3s) - Olive oil, avocado, coconut, nuts & seeds
•Fruits high in vitamin C - citrus fruits
•Antioxidants - berries, green tea
•Vegetables -leafy greens
•Lean protein & legumes
•Herbs & spices - turmeric (curcumin), ginger, garlic, cinnamon
•Fermented foods (probiotics)
2. Juice alkaline, antioxidant, & chlorophyll-rich vegetables & fruits. Especially those that are green (kale, spinach, broccoli, spirulina, chlorella, basil, cilantro…).
Chlorophyll is alkalizing, high in antioxidants, & detoxifying. All of which help improve oxygen delivery throughout the body by promoting red blood cell production. Oxygen is like water on the inflammation fire.
3. Anti-inflammatory therapies:
•Hyperbaric oxygen therapy
•Cryotherapy or cold plunges
•Red light therapy
If you’re local, you can visit my friends @upgradelabsriverton and try these therapies.
#antiinflammatory #antioxidants #health #healthylifestyle #healthyfats #nutrition #wellness #guthealth #healthyfood #antioxidant #cbd #organic #antiinflammatorydiet #inflammation #detox #turmeric #chlorophyll #longevity #healthy #healthyliving #holistichealth #painrelief #natural #immunesupport #antiinflammatoryfood #immunesystem #omega #juice #juicing #foodismedicine
#antiinflammatory#Inflammation#diet#Nutrition#food#health#Healthy#healthy foods#healthyeating#chlorophyll#juicing#oxygen#HBOT#cellhealth#disease#disease prevention#autoimmune#autoimmune disease
4 notes
·
View notes
Text
Hyperbaric Medicine (HBO)
I'm sorry, what is that?

I have a side hustle as a hyperbaric medicine provider and I am here to give you the down and dirty!
Sometimes referred to as HBO (hyperbaric oxygen), hyperbaric or dive medicine is a specialty that utilizes oxygen at high pressure to treat a variety of conditions, primarily things involving wounds. We place a patient in a chamber, deliver 100% oxygen to them, pressurize the chamber, and keep them in there for about 120 minutes. Since oxygen is the number one thing you need to heal a wound, we use a lot of it to try and speed up the process.
The Basics
Wait - what? HOW? Try not to have PTSD from your days in chemistry, but remember these?

The treatment physiology of hyperbarics relies on gas laws. Recall that it takes a lot of pressure to dissolve a gas into a liquid.
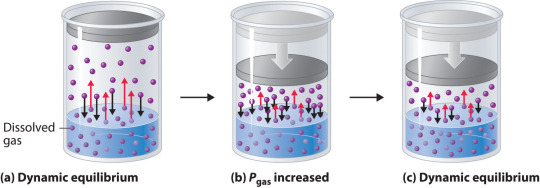
We use pressure to force oxygen into the blood stream at high rates to facilitate wound healing. For reference, most of your oxygen content is bound to hemoglobin (~98%). You do have dissolved oxygen in your blood, represented by your PaO2/PvO2 in a blood gas. However, this makes up a fraction of O2 content (~2%: if you want a clinical soap box, you should hear me talk about blood gases to students lol). A normal ABG would have a PaO2 of 65-100. An ABG acquired during hyperbaric treatment would be well over 2,000.
As an aside, recall that ambient air is 21% oxygen. Also, as a reminder, we exist at 1.0 ATA of pressure (one atmosphere).
How is it done?
Delivering oxygen this way requires delivery of a lot of pressure. We utilize dive chambers for this purpose. There are two types of chambers:
Monoplace: literally looks like a class coffin. Holds one patient and delivers oxygen at pressure through the entire chamber. These are very popular at wound centers.

Multiplace: literally looks like a submarine. Holds 2+ patients and delivers oxygen at pressure to individual patients hooked up to hoods or masks. These are found at tertiary care/academic medical centers.

Literally, the multiplace hoods make you look like a silly space person.

The reason oxygen is delivered this way in a multiplace chamber is to reduce the risk of fire. Oxygen at pressure can go boom. Having an entire chamber full of O2 is a big risk. So, we deliver the gas individually to each patient.
How did it start?
Dinking around with gases at pressure has been a thing for 400 years. However, it didn't become a more focused endeavor until the first dive suits started to be a thing in the 1870s. The specialty itself is relatively new, developed in the 1930s due to advent of decompression illness with divers. Things really progressed in the 1950s.
One pivotal study was "Life without Blood" in 1959. Dr. Boerema proved that he could keep a pig alive with HBO alone. The ethics of this experiment are questionable but he exsanguinated a pig under hyperbaric conditions (3.0 ATA, 100% FiO2). Plasma was left behind. By doing this, he proved that, at pressure, an organism does not need hemoglobin to live. Kind of a radical thing to prove! Don't worry, the pigs did get their blood back and recovered without issue.
What is treated with HBOT? (hyperbaric oxygen therapy)
Anything related to wound healing can be treated with HBOT. We also treat carbon monoxide poisoning, air gas embolism, and decompression sickness with HBOT. I'll start with those since they are (imo), the most clinically interesting. ;-D
Carbon monoxide poisoning: The physiology of using HBOT to treat CO poisoning is based on the binding affinity of CO to hemoglobin. CO has 200 x the binding affinity for hemoglobin than O2 or CO2 does. Because the binding sites are taken up by CO, hemoglobin cannot pick up O2. It also can't offload whatever O2 is already bound. The goal with HBOT is to bombard the blood with massive amounts of O2 to force CO off.

For reference, it would take about 6 hours for CO to offload on its own from hemoglobin on room air. It would take half as long at 100% FiO2 delivered at standard air pressure (1.0 ATA). CO is rapidly forced off within 30 minutes with HBOT. With very severe CO poisoning, particularly in cases of LOC, this is vital for limitation of hypoxia and neurological sequelae of exposure. Treatment is 1-3 "dives" depending on clinical context. The patient is treated at 2.8 ATA (60 feet of sea water) for about 120 minutes.
Air gas embolism: This occurs when gas is accidentally introduced into circulation. It can either be venous or arterial. The venous system has much more flexibility in tolerance for air bubbles. 15 cc or less of gas introduction is probably not going to result in symptoms. Higher volumes go to the lungs and can result in local lung infarction.
The real danger with this is air introduced into arterial circulation. Depending on where it is introduced, it can go directly to the heart causing an MI, or to the brain causing a stroke. Any volume of air introduced into arterial circulation is bad news bears. Treatment is usually 1 "dive" but could be more based on the context. The patient is treated at 2.8 ATA for 30 minutes and then the ascent is extremely slow. The whole dive takes about 5 hours. Why so long? If we ascend too quickly, the air bubble will reform.
Decompression sickness: This occurs primary with scuba divers who ascended too quickly. Scuba divers generally breath mixed gas, most commonly air (21% O2, ~79% N2) or nitrox (35% O2, ~65% N2). As someone is diving, the nitrogen they breath is also dissolved into their blood since they are at a pressure greater than 1.0 ATA. If a diver ascends too quickly, the nitrogen dissolved in the blood will rapidly reform air bubbles in the blood. We just mentioned how that is problematic.
Since air bubbles can go everywhere in circulation, the symptoms are variable ranging from headache, vertigo, nausea, joint pain, chest pain, stroke symptoms, loss of bowel/bladder function, etc. The treatment for this is to recompress the patient and very slowly ascend in the HBO chamber. Treatment is usually 1 dive but could be more based on the context. The patient is treated at 2.8 ATA for 30 minutes and then the ascent is extremely slow. The whole dive takes about 5 hours. Why so long? Again, if we ascend too quickly, the air bubble will reform.
Wound related conditions: there are roughly 15 approved diagnoses for HBO by Medicare in the USA. This is important to mention because if a condition is not covered, paying out of pocket is extremely cost-prohibitive. Insurance is billed $6,000 per treatment! Some of the most common conditions treated are osteoradionecrosis, soft-tissue radionecrosis, irradiation cystitis with hematuria, and refractory chronic osteomyelitis. Wounds created from radiation exposure have the best evidence to support the use of HBOT. These are considered outpatient conditions so patients come to be treated Monday-Friday. We dive to 2.4 ATA for 120 minutes. At minimum, patients are prescribed 20 dives but most treatment protocols for radiation induced injuries is at least 40 dives.
As you can see, this is a HUGE commitment for the patient. One dive is not enough for these wound related conditions. As a hyperbaric provider, I can say that we have patients with such significant symptom relief from HBO. For example, irradiation cystitis with hematuria is extremely debilitating. Patients are fatigued from chronic blood loss, deal with painful bladder spams and pelvic pain, pain with urination, and increased frequency. The blood can clot and obstruct their urethra or foley catheter. Symptoms like this limit quality of life. HBOT makes a huge difference for them.
Benefits
Anyone who has barriers to wound healing can benefit from HBO. Barriers include vascular disease, CKD, COPD, DM, heart failure, and immunocompromised status. The goal is symptom resolution/improvement or healing of the wound. Some patients get approved for far more treatments than we typically do. Usually the maximum insurance will cover is 60. However, in some situations, the clinical benefit of continued treatments is recognized by insurance and treatment is extended.
As a provider, I get to know these patients pretty well. They show up every day that I am staffing in HBO and it is rewarding to see them improve. Compared to my critical care role, this is a nice change of pace.
Adverse Reactions and Risks
There are risks and side effects to HBO. The most common are barotrauma, pneumothorax, seizure, temporary worsening of cataracts/vision, and abdominal distention.
Barotrauma of the ears and sinuses is by the most common issue we face in HBOT. If patients are not able to clear their ears as they descend ("pop" their ears), they can rupture their ear drums. Patients that cannot descend without extreme pain may need myringotomy tubes (ear tubes) to assist with equalizing pressure.
Seizure is a risk of HBOT and that primarily comes from oxygen reducing the seizure threshold. We mitigate this with "air breaks". These are 5 minutes intervals of the treatment where the patient is receiving air rather than 100% O2. Example, we treat at 100% for 30 minutes, have a 5 minute air break, repeat x 2. Obviously the people at highest risk are those with epilepsy or taking seizure threshold reducing medications.
HBOT can worsen cataracts and vision temporarily. The mechanism of this is poorly understood but we know it is reversible. Distance vision is affected the most.
Contraindications
The only absolute contraindication to HBOT is an untreated pneumothorax. There are many relative contraindications that require a risk benefit analysis. An example of this is pregnancy. HBOT has not been thoroughly studied in pregnancy and is not recommended EXCEPT in cases of CO poisoning where we know that the CO concentration is higher in fetal circulation than maternal. Always treat a pregnant person with CO poisoning.
Other potential contraindications include use of certain chemotherapy agents, COPD with blebs/bullae, severe heart failure, epilepsy, sinus/HEENT disease, claustrophobia, certain implanted devices, or active infection.
With certain chemo agents, they can lower the seizure threshold putting patients at higher risk of seizure in the chamber. People with COPD and blebs are at risk of those blebs popping under pressure and causing acute respiratory distress. People with heart failure can experience flash pulmonary edema after an HBO treatment. If people are claustrophobic, obviously spending time in a monoplace chamber can trigger panic attacks. At my center, we sometimes have people referred to our multiplace chamber for exactly that reason.
Most implanted medical devices are HBOT compliant. Generally, pacers and other devices are tested at 4.0 ATA of pressure. We double check with the manufacturer that the device is compliant. If it isn't, we cannot safely treat and have to deny the consult.
Obviously, if someone is sick, we don't want them in the chamber. Particularly colds, severe allergies, fever, or anything that is affecting HEENT. People with acute sinus infection are unable to clear sufficiently to dive. Even if they can clear, they feel miserable. No need to go through that.
Safety Issues
I mentioned that high O2 environments are at risk for explosion. Safety is the number one concern with any chamber. The goal is to reduce risk of fire by removing fabrics that create static (anything synthetic), removing electronic devices that are not HBOT approved, and going through multiple levels of safety checks for patients and for chamber preparation.
At our chamber, only 100% cotton is allowed in the chamber. All patients have special scrubs that they wear during treatment. No electronic devices can be brought in the chamber which includes phones, tablets, laptops, e-readers, watches, pagers, etc. We do have HBOT approved IV pumps and radio headsets that we use. These have been tested at 4.0 ATA. The radio headsets are for the attendant (staff member) who is in the chamber and this is also for safety purposes. Since we have a mulitplace chamber, a staff member is always in the chamber with the patient(s).
One thing I do want to address is that some people are concerned about putting a patient with active cancer into the chamber. There is concern that the high O2 environment will "feed" the cancer. There is simply not data to support this. Active cancer is not a contraindication to HBOT.
And there you have it! The down and dirty of HBOT! Hopefully you learned something cool. If you think you have a patient who would benefit, find your local HBOT provider. We are always happy to talk with you about the process. If you care about a soapbox of how insurance companies suck, see below. :-D
Soapbox: I will say, I have definitely been frustrated with insurance companies. They are the gatekeepers of this treatment. You can have several providers supporting the use of treatment and an insurance company can still say "no". Very frustrating.
A prime example of this are patients who have avascular necrosis that is steroid or chemotherapy induced. These are often younger patients (late teens, early 20s) who have/had leukemia of some kind. They end up having necrosis at a joint, usually the femoral head, that will likely result in complete joint replacement at a young age. No orthopedic surgeon wants to replace joints on a young person. It comes will all kind of problems and always needs revision later in life.
Insurance companies will say "we only cover radiation induced necrosis" because that is what the literature supports. Yes, they are correct that the vast majority of studies support HBOT for radiation induced injury. However, the pathophysiology of the tissue destruction, while a little different, ends up with the SAME problem. There are studies that support HBOT use in these situation but not nearly as many as radiation induced injury. The result is that patients suffer, get a joint replacement they could have avoided (or postponed until they are fully developed), and generally are shafted.
*end soapbox*
#pablr#medblr#nurblr#pharmblr#physician assistant#physician associate#doctor#physician#hyperbaric medicine#hbot#hbo#medicine#oxygen therapy
6 notes
·
View notes
Text



Renessence, Amsterdam
3 notes
·
View notes
Text
Leading Multispeciality Hospital in Bangalore | Nano Hospitals
Nano Hospitals is one of the best multi-specialty chain in JP Nagar Bangalore, providing affordable world-class HBOT healthcare services and treatments.

2 notes
·
View notes
Text
Nano Hospitals - Bangalore
Multispecialty hospitals combine HBOT and medical specialties under one roof to provide patients with comprehensive care.

2 notes
·
View notes
Text
Hyperbaric Oxygen Therapy Hair Growth
Hyperbaric oxygen therapy (HBOT) is a clinical treatment that includes taking in 100 percent oxygen in a compressed chamber. This therapy has been viewed as successful in various circumstances, including wound mending, carbon monoxide harming, and even going hair loss.
In recent years, research has shown that HBOT can also be an effective treatment for hair growth. By increasing blood flow and oxygen supply to the scalp, HBOT can provide the hair follicles with the necessary nutrients and oxygen needed to promote hair growth. This increased blood flow can also help remove any toxins or waste products that may be hindering hair growth.
3 notes
·
View notes
Text
How HBOT Enhances Healing and Recovery
The human body relies on oxygen for cell regeneration, immune function, and tissue repair. Hyperbaric Oxygen Therapy (HBOT) takes this a step further by increasing oxygen delivery to every cell in the body.

0 notes
Text
Hyperbaric Oxygen Therapy
One of our most fundamental connections to life is the assimilation of oxygen from the air we breathe into every tissue in our bodies. Without oxygen, and its ability to spark our body’s life-giving process of creating cellular energy, we could not survive. For centuries physicians have used oxygen in a healing capacity, and at least as far back as the 1600s began experimenting with the effect of putting patients into a pressurized, or hyperbaric environment for the purpose of stimulating healing.
Many have heard of hyperbaric oxygen for the purpose of treating decompression sickness or “the bends”, for divers who have ascended too quickly. In these instances, hyperbaric oxygen is a lifesaving therapy that helps resolve excess nitrogen accumulated in body tissues. Over the last century however, the use of a hyperbaric oxygen chamber has expanded to treat a long list of health conditions, by the simple fact that increasing levels of oxygen in tissues can have a profound healing effect.
#Alzheimer#Brain Healing#HBOT#healing for TBI PTSD#hyperbaric oxygen therapy#Improving dementia#Joshua Phillips ND#stroke
1 note
·
View note
Text
Good News From Israel
In the 17th Nov 24 edition of Israel’s good news, the highlights include:
Volunteers at a Gaza border refreshment tent have served half a million IDF soldiers.
Israeli innovations combat cancer, heart disease, PTSD, brain diseases, and aging.
A Druze-Israeli spoke Arabic to save Israeli soccer fans in Amsterdam.
The war certainly doesn’t scare off visitors to Israel from the animal kingdom.
Israeli startups can save the planet from plastic pollution.
Israel’s economic indicators are increasingly healthy.
Israeli technology protects more American soldiers.
Two new Israeli Chief Rabbis have been inaugurated.
Read More: Good News From Israel

This week's newsletter sees Israel valiantly advancing in its war to topple Hamas, Hezbollah, Iran and its terror proxies. Meanwhile, Israel's citizens have been awarded top national and international honors including as "Lions of Zion", rocket scientists, sports champions, and religious leaders. These achievements are just some of the highlights of Israel's continuing efforts to produce top innovations that benefit humanity.
The photo is of a Netanya school awards ceremony, illuminated by solar powered lighting on top of the playground.
#Aliyah#Amsterdam#Arabic#cancer#Druze#El Al#Gaza#good news#Hamas#HBOT#Hezbollah#IDF#Israel#Jerusalem#Jewish#October 7th#plastic#PTSD#rockets#Weizmann
21 notes
·
View notes
Text
BRAIN WOUND UPDATE #10: AVIV Clinic Press Release: Review of Scientific Basis of HBOT for TBI

BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD ORLANDO, Fla., Aug. 01, 2023 (GLOBE NEWSWIRE) -- Aviv Clinics, one of the most advanced brain clinics in the world, shares the results of a new comprehensive literature review that shows hyperbaric oxygen therapy (HBOT) should be recommended as an effective therapy for patients suffering with chronic mild traumatic brain injury (TBI). Chronic mild traumatic brain injury occurs when symptoms from a mild traumatic brain injury are prolonged and last for more than six months. The literature review, The efficacy of hyperbaric oxygen therapy in traumatic brain injury patients: literature review and clinical guidelines, was conducted by the Sagol Center for Hyperbaric Medicine and Research at Shamir Medical Center, Tel Aviv University and University of Pittsburgh Medical Center’s neurosurgery department, and published in the official journal of the European Society of Medicine, Medical Research Archives. The literature review evaluated articles and human clinical trials data from 1969 to April 2023 that provided detailed information on the type of HBOT treatment and clinical outcomes. The articles were categorized into acute-subacute traumatic brain injury and chronic traumatic brain injury and evaluated by HBOT experts and esteemed research leaders Dr. Shai Efrati, director of the Sagol Center and co-founder of Aviv Scientific; Dr. Amir Hadanny, chief medical officer at Aviv Scientific and chief medical research officer at the Sagol Center; and Dr. Joseph Maroon, vice chairman of the Department of Neurological Surgery at the University of Pittsburgh Medical Center. The literature review concluded that HBOT should be recommended for chronic traumatic brain injury for a selected group of patients suffering from prolonged post-concussion syndrome (PPCS) who have clear evidence of metabolic dysfunctional brain regions and who have been properly evaluated by standardized cognitive tests and functional brain imaging. Evidence involved in the review, including seven randomized controlled trials and six prospective studies, suggested significant improvement in cognitive function, symptoms and quality of life in patients with chronic mild traumatic brain injury. For acute moderate-severe TBI, the review concluded that HBOT may be recommended as a treatment but explained that further studies are needed to both evaluate outcomes and determine the optimal treatment protocols. Evidence in the review, including nine randomized controlled trials, one meta-analysis and two prospective studies evaluating the clinical effects of hyperbaric oxygen therapy in patients suffering from acute and subacute traumatic brain injuries, showed mortality was significantly reduced but mixed results for favorable functional outcomes in survivors. “This literature review scoured an immense amount of data related to HBOT as a therapy for traumatic brain injury, and the evidence that HBOT is effective against chronic traumatic brain injury is clear,” said Dr. Amir Hadanny, Chief Medical Officer at Aviv Scientific and Chief Medical Research Officer at the Sagol Center. “When looking at the comprehensive data over a larger stretch of time, we’re seeing the quality of studies have improved, and it’s exciting to see HBOT research heading further in the right direction. Many people are dealing with symptoms of chronic traumatic brain injury, and the current rehabilitation methods are limited in their efficacy. The science behind how HBOT can be effective is evident, and there is hope for those who are suffering.” HBOT is a medical treatment in which 100% oxygen is administered at an increased environmental pressure. Aviv’s unique HBOT protocol, the hyperoxic-hypoxic paradox, fluctuates oxygen levels during treatment and is being used to repair and regenerate damaged brain tissue in several types of brain injuries including traumatic brain injury, stroke, PTSD, long COVID and age-related cognitive decline among others. Previous studies from the research team at the Sagol Center for Hyperbaric Medicine and Research have demonstrated the efficacy of HBOT as a treatment for persistent post-concussion syndrome (PPCS), suggesting that HBOT improves cognitive function, behavioral function and quality of life in both adult and pediatric patients suffering from PPCS at the chronic stage, even years after their injury. Aviv Clinics offers an advanced treatment program with a multidisciplinary team of medical experts providing patients with top-line care and the opportunity to improve their quality of life. The Aviv Medical Program includes an in-depth assessment of the patient’s physical and neurological condition to assess the fit for the program. For patients that meet the criteria, the Aviv team will then prepare a comprehensive treatment schedule combining HBOT with personal cognitive training, and physical and dietary coaching, for a holistic approach to patient health. The HBOT sessions are conducted in state-of-the-art multiplace chambers that are comfortable, safe and allow for medical staff to accompany patients during the treatment. The elevated pressure in the HBOT chamber creates an optimal oxygenation condition, ultimately encouraging damaged brain and body tissues to regenerate and heal. The full study is available here. For more on Aviv Clinics, visit aviv-clinics.com Aviv Clinics is the leader in the research and treatment of age-related cognitive and functional decline and novel applications of hyperbaric oxygen therapy (HBOT) to maximize human performance. Based on an exclusive partnership with the world’s largest hyperbaric medicine and research facility, the Sagol Center at Shamir Medical Center in Israel, Aviv is introducing a global network of clinics delivering the most effective evidence-based treatment of the aging related decline – the Aviv Medical Program. The three-month regimen, designed to improve the aging-related decline in healthy adults, was developed based on over a decade of research and thousands of patients treated worldwide under the scientific leadership of Shai Efrati, M.D., chair of Aviv Scientific’s Medical Advisory Board and director of the Sagol Center. Media Contact: Ellie Holt [email protected] ########## The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can help heal the symptoms and effects of acute concussion/TBI/PTSD by helping heal brain wounds. Heal Brains. Stop Suicides. Restore Lives. TreatNOW Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made. Read the full article
#acutemoderate-severeTBI#AvivClinics#brainhealth#braininjured#braininjury#brainwound#chronictraumaticbraininjury#concussion#concussionprotocol#ConcussionSymptoms#concussiontreatment#HBOT#HBOTTreatment#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#hyperoxic-hypoxicparadox#mildtraumaticbraininjury#stroke#TBI#TBItreatment#traumaticbraininjury
2 notes
·
View notes
Text
(Jeudi 8 août 2024) 💪🏼

5 notes
·
View notes
Text
Hyperbaric chambers have long been used in the medical world for treating a variety of conditions. From decompression sickness to chronic wounds, these pressurized environments help deliver oxygen to tissues in need of repair. Recent research highlights their potential in managing postoperative complications, particularly for individuals recovering from mastectomy surgeries. Mastectomy, a procedure often performed to treat breast cancer, comes with potential complications like skin flap ischemia. This condition, where blood flow to the skin is reduced, can delay healing and cause significant discomfort. Researchers have been exploring the use of hyperbaric chambers to address this issue, and the results are promising.

#HyperbaricChambers#HyperbaricOxygenTherapy#HyperbaricChambersForMastectomyRecovery#BenefitsOfHyperbaricChambers#HyperbaricTherapy#HBOT
1 note
·
View note