#fever after covid-19 vaccine
Explore tagged Tumblr posts
Text
Hey! You there!
Get vaccinated against the current Covid and Flu strains! Tis the Season! To Immunize Yourself!
#seriously#I got Covid recently#still have it tbh#the past couple days have been ok#but that first day I felt like my brain was being pressure cooked#spent the day in bed with a fever and aching all over#had some crazy fever dreams where I was the king of an alien civilization?#that were stressful and scary but weirdly gender-affirming?#woke up after my fever broke covered in gross Covid sweat#-100/10 would not recommend#get vaccinated#also got anosmia again which I hate#every time I’m scared it’s gonna be permanent this time#it’s not a complete loss of smell unlike the other times but it still makes me feel out of sorts#like I can’t smell any of my citrus perfumes but I can smell my basil dish soap ok-ish#vent post#personal#covid 19#influenza#flu shot#covid shot
6 notes
·
View notes
Text
UPDATE: NOVAVAX NOW AVAILABLE!!!
Hi everyone, it's been about a year since I posted about updated COVID vaccines and it's time for another update if you are in the US:
THE BRIDGE ACCESS PROGRAM IS ENDING!!!!
If you are uninsured or your insurance does not cover covid boosters, please schedule a new booster appointment before the end of August because the Bridge Access Program (the way the government will still pay for your booster) ends in September. The updated mRNA boosters from Moderna and Pfizer are available now. Go Go GO!!!
Shitty, I know! If you can call your congressional reps, the FDA, the CDC, whomever to tell them you want this program to continue/be reinstated, that would be great. Also, while you're at it, call the FDA to tell them to expedite the approval for the updated Novavax booster (3017962640).
The new Novavax vaccine is designed for the JN.1 strain which is one of the most recent mutations of the virus going around. If you have insurance and can afford to wait, I highly recommend getting the Novavax booster when it becomes available.
We are currently in the largest Covid summer surge since 2021
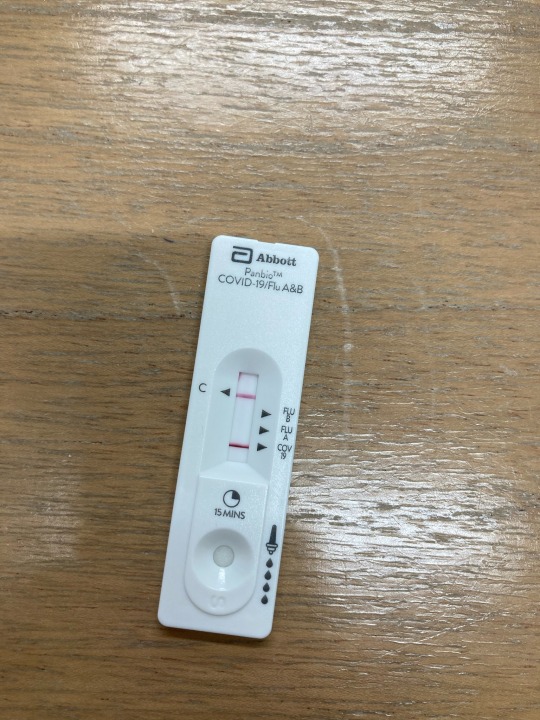
If you haven't had a booster in the past six months you are essentially unvaccinated. New strains with different spike proteins keep evolving faster than vaccine development and distribution can keep up. All that said, getting Covid is not a moral failing. If you do feel sick, take a rapid test! If it's negative, test again a day or two later. It is better to know than not to know. Here's a refresh on how to take a rapid test correctly:
If you do get Covid, it is worth getting on antiretrovirals within the first week of symptoms to reduce the overall viral load your body has to fight. If your insurance doesn't cover Paxlovid or Remdesivir, here are other low/no-cost ways to access it:
If you get sick, rest radically even after you stop testing positive on rapid tests. Avoid exercising for at least eight weeks after the fact to reduce the risk of developing long covid.
Regardless of your vaccination status, masking with a KN95 or N95 respirator (or equivalent standards in your country i.e. FFP2/3 in the EU) is the most reliable way to protect yourself and others. If Covid protections are a financial burden, there is likely an active Mask Bloc near you doing free distribution of respirators and tests that would be happy to help you. Here's a global map of them from covidactionmap.org
Some quick tips: if you're wearing a bi-fold mask, flatten the nose-bridge wire completely, then mold it to your nose on your face for a better fit. The best mask is the one that you will actually wear regularly to protect yourself. I really like the selection of styles, sizes and colors from WellBefore:
As school is starting, getting you and your family boosted is one of the best things you can do to protect yourselves. Masking is perhaps even more important. If you can advocate for updating and regularly changing the HVAC filters at your local schools to MERV-13 or higher to keep the indoor air cleaner, that can also make a big difference. Better indoor air quality in schools helps protect kids from illness, allergies, wildfire smoke, and more per the EPA's website.
These are steps you can take to improve air quality at home as well. Corsi-Rosenthal boxes are low-cost and highly effective for cleaning the air indoors.
Here's a map of clean air lending libraries for getting access to air purifiers for events from cleanairclub.org
#covid#covid 19#signal boost#boost#long covid#vaccine#wear a respirator#indoor air quality#covid testing
2K notes
·
View notes
Text
Also preserved on our archive (Daily updates!)
An older (published in January 2024) but interesting and comprehensive look at long Covid's effect on Latino families and communities in the US.
By Lygia Navarro and Johanna Bejarano
Editor’s note: This story first appeared on palabra, the digital news site by the National Association of Hispanic Journalists. It is part of a series produced in partnership between palabra and Northwest Public Broadcasting (NWPB) with the collaboration of reporters Lygia Navarro and Johanna Bejarano. *Some people interviewed for this article requested anonymity to discuss private health issues.
Victoria* is already exhausted, and her story hasn’t even begun. It’s late January 2021 in rural Sunnyside, Washington. The town of 16,000 people is a sleepy handful of blocks flecked with pickup trocas, churches on nearly every corner, and the twangs of Clint Black and Vicente Fernández. Geometric emerald chunks of farmland encircle the town.
Thirty-nine-year-old Victoria drags herself back and forth to her parents’ bedroom in a uniform of baggy burgundy sweatpants, scarf, knit hat and mask. Always a mask. As the eldest sibling, her unspoken job is to protect the family. But COVID-19 hits before they can get vaccinated.
When Victoria’s mamá got sick and quickly infected her papá, Victoria quarantined them. She shut them in their room, only cracking the door briefly to slide food in before retreating in a fog of Lysol.
Working in the health field, Victoria knows if they make it through the first 14 days without hospitalization, they will likely survive. Yet, caregiving drains her: Keeping track of fevers. Checking oxygen saturation. Making sure they’re drinking Pedialyte to stay hydrated. Worrying whether they will live or die.
Five days in, COVID comes for Victoria. Hard. Later, when she repeatedly scrutinizes these events, Victoria will wonder if it was the stress that caused it all — and changed her life forever.
At the pandemic’s onset, Victoria’s family’s work dynamics fit the standard in Sunnyside, where 86% of residents are Latino. “Keeping the members of your household safe — it was hard for a lot of families,” Victoria says. Living in multigenerational homes, many adult children, who’d grown up in the United States with access to education, had professional jobs, and switched to working from home. Their immigrant elders, who’d often only been able to finish fourth grade, braved the world to toil in fields, produce packing plants, supermarkets, or delivery trucks. As Leydy Rangel of the UFW Foundation puts it: “You can’t harvest food through Zoom.”
More than three decades ago, when 6-year-old Victoria’s family migrated from rural northern Mexico to this fertile slip of land cradling the zigzagging Yakima River, their futures promised only prosperity and opportunity.
According to oral histories of the Confederated Tribes and Bands of the Yakama Nation — who white colonizers forced out of the Yakima Valley in 1855 — the valley’s fecund lands have fed humans since time immemorial. Soon after the Yakamas’ removal to a nearby reservation, settler agriculture exploded.
By World War II, employers were frantic to hire contracted bracero laborers from Mexico — themselves descendants of Indigenous ancestors — to harvest the valley’s bounty of asparagus, pears, cherries and other cornucopia. This was how Victoria’s family arrived here: her abuelo and his brother had traveled back and forth to Washington as braceros decades before.
Victoria’s path took similar twists, in a 21st century, first-gen way. She moved all over the country for her education and jobs, then returned before the pandemic, bringing a newfound appreciation for the taste of apples freshly plucked from a tree that morning, and for the ambrosial scent of mint and grapes permeating the valley before harvest.
Today, agriculture is the largest industry fueling the Yakima Valley, the country’s twelfth-largest agriculture production area. Here, 77% of the nation’s hops (an essential ingredient in beer) and 70% of the nation’s apples are grown. Latinos, who constitute more than half of Yakima County’s population, power the agricultural industry.
While the area’s agricultural enterprises paid out $1.1 billion in wages in 2020, 59% of the low-wage agriculture jobs are held by undocumented folks and contracted foreign seasonal laborers doing work many Americans spurn. Latinos here live on median incomes that are less than half of white residents’, with 16% of Latinos living in poverty. Also in 2020: as they watched co-workers fall ill and die, Latino farmworkers repeatedly went on strike protesting employers’ refusals to provide paid sick leave, hazard pay and basic COVID protections like social distancing, gloves and masks.
“Every aspect of health care is lacking in the valley,” Yakima Herald-Republic health reporter Santiago Ochoa tells me.
In interview after interview, Yakima Valley residents and health care workers sketch in the details of a dire landscape:
The state’s busiest emergency room. Abrupt shutdowns of hospital facilities. Impoverished people without transportation or internet access for telehealth. Eight-month waits for primary care appointments. Nearly one in five Latinos uninsured. More than half of residents receive Medicaid. Resident physicians cycling in and out, never getting to know their patients. Not enough specialists, resulting in day-long trips for specialized care in bigger cities. With its Latino essential workforce risking their lives to feed their families — and the country — by summer 2020, COVID blazed through Yakima County, which quickly became Washington’s most scorching of hot spots. Not only did Yakima County tally the highest per-capita case rate of all West Coast counties (with Latinos making up 67% versus, 26% for white people), it also saw more cases than the entire state of Oregon. Ask Latinos here about 2020, and they shiver and avert their gazes, the trauma and death still too near.
Their positive tests marked just the beginning of terrifying new journeys as COVID slammed Victoria and many other Yakima Valley Latinos. Mix in scanty rural health care, systemic racism and a complicated emerging illness, and what do you get? Chaos: a population hardest hit by long COVID, but massively untreated, underdiagnosed, and undercounted by the government and medicine itself.
It won’t go away The cough was the first clue something wasn’t right. When Victoria had COVID, she’d coughed a bit. But then, three months later, she started and couldn’t stop.
The Yakima Valley is so starved for physicians that it took five months to see a primary care doctor, who attributed Victoria’s incessant cough to allergies. Victoria tried every antihistamine and decongestant available; some brought relief for three, maybe four weeks, and then returned spasms of the dry, gasping bark. A few minutes apart, all day long. The worst was waking up coughing, at least hourly.
Victoria had chest x-rays. An ear, nose and throat specialist offered surgery on her nose’s deviated septum. As months passed, the black hair framing Victoria’s heart-shaped face started aging rapidly, until it was grayer than her mother’s.
Over a year after the cough began, an allergist prescribed allergy drops, and Victoria made a chilling discovery. Once the drops stopped the cough for a month, then two, Victoria realized that the extreme fatigue she’d thought was sleep deprivation from coughing all night persisted.
“The exhaustion comes from within your soul, it overpowers you,” she says. “It’s intolerable.”
And her mind was foggy. When interrupted at work every 10 minutes by a coughing jag, Victoria hadn’t realized COVID had substantially altered her brain. “There are things in my brain that I should have access to, like words, definitions, memories,” she says. “I know that they’re there but I can’t access them. It’s like a filing cabinet, but I can’t open it.”
Before long, the cough resurfaced. Sometime in 2021, reading COVID news for work, Victoria learned of long COVID: new or lingering health issues persisting at least three months after COVID infection.
How to get help if you think you might have long COVID Talk to your doctor, and if your doctor doesn’t listen to your concerns, bring a loved one to advocate for you at your next appointment. Bring this article (or other materials on long COVID) to show your doctor. Ask your doctor about seeing specialists for long COVID symptoms, such as a cardiologist (for dysautonomia symptoms like dizziness, heart palpitations and shortness of breath), a gastroenterologist (for digestive problems), or a neurologist (for chronic nerve pain). Ask to be referred to a long COVID clinic (if there is one in your area). Now four years into the pandemic, there is still no treatment or cure for long COVID. COVID long-haulers (as they call themselves) have reported over 200 varied symptoms, with fatigue, dizziness, heart palpitations, post-exertion exhaustion, gastrointestinal issues, and brain dysfunction among the most common.
Long COVID is far from a mysterious illness, as it’s often called by the medical establishment and some media. There are precedents: for at least a century, historical documentation has shown that, while most recover, some people remain sick after viral or other illnesses. Yet funds for research have been severely limited, and sufferers ignored. Myalgic Encephalomyelitis – sometimes called Chronic Fatigue Syndrome, or ME/CFS — is a prime example. Like ME/CFS, long COVID afflicts many more women (and people assigned female at birth) than men, with women comprising as many as 80% of COVID long-haulers. Most long-haulers are in their 30s, 40s and 50s — the busiest years for women with children, who often put their own needs last.
What should have been instantly clear, given how disproportionately Black and Brown communities were hit by COVID, was that long COVID would wallop Americans of color. Yet, the U.S. government waited until June 2022 to begin tracking long COVID. Even now, with 18 months of data showing Latinos are the population most impacted by long COVID, palabra is among the very few media outlets to report this fact. Are the nation and the medical community willfully ignoring Latino long-haulers — after sending them into clouds of coronavirus to keep society’s privileged safe?
Fighting for a diagnosis When Victoria mentioned long COVID, her doctor didn’t exactly ignore her: she listened, said “OK,” but never engaged on the topic. Same with Victoria’s allergist and the ear, nose and throat specialist. All they could do, the doctors said, was treat her symptoms.
“I’m highly educated and I know that you have to be your own advocate. But I kept asking, kept going on that line of thought, and they had nothing to say to me. Absolutely nothing,” she laments.
Victoria understood science on long COVID was limited, but still expected more. “All of the treatments we tried, it was as if COVID hadn’t existed. They should at least say that we need to investigate more, not continue acting like it wasn’t a factor. That was what was most frustrating.”
Just as Victoria fought to have her illness validated by doctors, 30 miles away in the northern Yakima Valley town of Moxee, 52-year-old María* waged a parallel battle. Both felt utterly alone.
When the pandemic began, María became the protector of her husband and children, all asthmatics. When she fell ill New Year’s Day 2021, she locked herself in her room, emerging weeks later to find her life unrecognizable.
Recounting her struggles, María reads deliberately from notes, holding back tears, then pushes her reading glasses atop her head. (María moved here from northern Mexico as an adult, and feels most comfortable in Spanish.) Her dyed brown hair, gold necklace and lightly made-up face project convivial warmth, but something intangible behind her expression belies a depth of grief María refuses to let escape. When I tell her I also have long COVID, and fell ill the exact same month, she breathes out some of her anxiety.
María’s long COVID includes chronic, full-body pain; memory lapses so severe she sometimes can’t remember if she’s eaten breakfast; such low energy that she’s constantly like a battery out of juice; unending shortness of breath; joint inflammation; and blood flow issues that leave her hands a deep purple. (The only time María ventured to the hospital, for her purple hands, she says staff attempted to clean them, thinking it was paint.) Like Victoria, María used to enjoy exercise and hiking in the valley’s foothills, but can do neither anymore.
María has no insurance, and receives care at the Yakima Valley Farm Workers Clinic, created in 1978 out of the farmworkers’ movement. The clinic’s multiple locations are the valley’s main providers of care irrespective of patients’ ability to pay.
Whereas Victoria’s doctors expressed indifference to the idea of COVID causing her health complaints, María’s doctors not only discounted this connection, but made serious errors of misdiagnosis.
“Every week I went to see my doctor. She got so stressed out (at not knowing what was wrong with me) that she stressed me out,” María says. “My doctor told me, ‘You know what? I think you have multiple sclerosis.’” María saw specialists, and afterwards, even without confirmation, María says her doctor still insisted she had MS. “I told her, ‘No. No, I don’t have multiple sclerosis. It’s COVID. This happened after COVID.’ I was really, really, really, really, really, really insistent on telling them that all of this was after COVID.”
Latinos uncovering the connections between their ill health and COVID is rare, partially due to the plummet in COVID coverage on Spanish-language news, says Monica Verduzco-Gutierrez, a long-hauler and head of the University of Texas Health Science Center San Antonio long COVID clinic. There has been no national public education on long COVID, in any language.
“It’s hard for people to understand what the real impact of long COVID is now and in the future,” says Lilián Bravo, Yakima Health District director of public health partnerships and the face of COVID updates on Yakima Valley television early in the pandemic. “We’re looking at a huge deficit in terms of people’s quality of life and ‘productivity.’”
Eventually, María’s doctor sent her to another specialist, who said that if she didn’t improve within a month, he’d operate on her hip. María’s never had hip problems. “He said, ‘Well, I don’t know what you’re going to do,’” and then put her on a strong steroid medication that made her vomit horribly, María says. She hasn’t tallied what she’s spent on medical bills, but after paying $1,548 for a single test, it must be many thousands of dollars.
Meanwhile, María’s family and friends kept insisting her maladies were psychological. “I never accepted that. I told them: ‘It’s not in my head. It’s in my body.’” It wasn’t until more than a year after becoming ill that María finally saw a rheumatologist who diagnosed her with long COVID and other immune dysfunctions. “I told her, ‘Yes, I knew that my body wasn’t working. I knew that something was wrong.’ I felt like I could relax. Finally someone is telling me that it’s not all in my head.” Once María was diagnosed, her extended family switched to asking how she was feeling and sympathizing with her.
Victoria, on the other hand, has never received a long COVID diagnosis. At Victoria’s request, her doctor referred her to the state’s only long COVID clinic, at the University of Washington in Seattle, but Victoria’s insurance, Kaiser Permanente, refused to pre-approve the visit — and the clinic wouldn’t accept cash from her. At present, the clinic isn’t even accepting patients from the Yakima Valley or any other part of Washington — they are only accepting patients in King County, which includes Seattle.
Victoria’s family hasn’t accepted her health struggles either. “I’d say, ‘I know that you think I’m crazy,’” Victoria says, chuckling, as she often does to lighten her discomfort. “My mom would fight with me: ‘You forgot to do this! Why are you so spacey?’ ‘Mami, it’s not that I forgot. In reality, I completely lost track of it.’” If Victoria is fatigued, her family asks how that’s possible after a full night’s sleep. “I’ve found that I have to defend myself. When I try to explain to people, they hear it as excuses from a lazy person — especially being Latinos.”
Karla Monterroso, a 42-year-old California Latina long-hauler since March 2020 who spent her first year bedbound, says, “(With long COVID), we have to rest in a way that, in our culture, is very difficult to achieve. We really judge exhaustion.” In fact, pushing physically or mentally for work can make long-haulers much sicker. Karla says Latino ethics of hard work like those of Victoria’s parents “aren’t the principles that are going to serve us with this illness.”
Long COVID diagnoses in Latinos are still too rare, due to untrained family medicine physicians and medical stereotypes, says Verduzco-Gutierrez. (Doctors might see blood sugar changes, for example, and assume that’s just because of Latinos’ high rates of diabetes, rather than long COVID.) She says “misinformation on long COVID” is rampant, with physicians claiming long COVID is a fad, or misdiagnosing the bone-deep exhaustion as depression. When Verduzco-Gutierrez’s own doctor invited her to speak to their practice, the assembled physicians weren’t aware of basic research, including that the drugs Paxlovid and Metformin can help prevent long COVID if taken at infection. In Washington, physicians must complete training on suicide, which takes 1,200 to 1,300 lives in the state yearly, but there’s no state-wide training on long COVID, which currently affects at least 498,290 Washingtonians.
Cultural skepticism about medicine — and entrenched stigmas about illness and disability — mean Sunnyside conversations about aftereffects don’t mention COVID itself. Victoria’s relatives push traditional herbal remedios, assuming that anyone still sick isn’t doing enough to recover. “(People suffering) feel like they’re complaining too much if they try to talk about it,” Victoria says. Meanwhile, her parents and others in her community avoid doctors out of stubbornness and mistrust, she says, “until they’re bleeding, when they’re super in pain…, when it’s gotten to the worst that they can handle.”
“People in this community use their bodies for work,” Victoria says. “If you’re Latino, you’re a hard worker. Period,” says Bravo. “What’s the opposite of that, if you’re not a hard worker? What are you? People don’t want to say, ‘I came to this country to work and all of a sudden I can’t anymore.’”
Victoria sees this with her parents, who’ve worked since the age of 10. Both have health issues inhibiting their lives since having COVID — her dad can’t take his daily hour-long walks anymore because of heart palpitations and shortness of breath, and her mom began getting headaches and saw her arthritis worsen dramatically — yet neither will admit they have long COVID. Nor will their friends and family. “If they noticed the patterns of what they themselves are saying and what their friends of the same age are suffering after COVID,” Victoria says of her community, “they’d hear that almost everyone is suffering some type of long COVID.”
Long COVID’s deep impact on Latinos The “back to normal” ethos is most obvious in the absence of long COVID messaging while as many as 41 million adults now have — or have recovered from — long COVID nationwide. “The way that we’re talking about the pandemic is delegitimizing some of (long COVID’s) real impacts,” says Bravo of the Yakima Health District.
Even with limited demographic data, statistics show a nationwide reality similar to Victoria’s Sunnyside. Through a recurring survey, the Census Bureau estimates that 36% of Latinos nationally have had long COVID — likely a vast underestimate, given that the survey takes 20 minutes to complete online (Latinos have lower rates of broadband internet), and reaches only a sliver of the U.S. population. Experts like Verduzo-Gutierrez believe that true rates of long COVID in Latinos are higher than any reported statistic. California long-hauler Karla Monterroso agrees: “We are underdiagnosed by a severe amount. I do not believe the numbers.”
This fall, a UC Berkeley study reported that 62% of a group of infected California farmworkers developed long COVID. Weeks later, a survey from the University of Washington’s Latino Center for Health found that, of a sample group of 1,546 Washington Latinos, 41% of those infected became long-haulers. The Washington results may also be an undercount: many long-haulers wouldn’t have the energy or brain clarity to complete the 12-page survey, which was mailed to patients who’d seen their doctor within the prior six months. Meanwhile, many long-haulers stop seeing doctors after tiring of the effort and cost with no answers.
“Our community has not bounced back,” says Angie Hinojos, executive director of Centro Cultural Mexicano, which has distributed $29 million in rent assistance in Washington and hasn’t seen need wane. “That is going to affect our earning potential for generations.” The United Farm Workers’ philanthropic sister organization, the UFW Foundation, says union organizers hear about long COVID, and how it’s keeping people out of work, frequently.
Cultural and linguistic disconnects abound between doctors and Latinos on long COVID symptoms, some of which, like brain fog and fatigue, are nebulous. If doctors lack patient rapport — or don’t speak their language — they’ll miss what patients aren’t sharing about how long COVID changed their lives, work and relationships. That’s if Latinos actually go to the doctor.
“If you’re working in the orchards and your muscles are always sore, it’s just part of the day-to-day reality,” says Jesús Hernández, chief executive officer of Family Health Centers in north-central Washington. “If you’re constantly being exposed to dust and even chemicals in the work environment, it’s easy to just say, ‘Well, that’s just because of this or that,’ and not necessarily be readily willing to consider that this is something as unique as long COVID.”
Even Victoria says if not for the cough, she wouldn’t have sought medical advice for her fatigue. “There are a lot of people out there that are really tired, in a lot of pain and have no idea why. None,” says Karla, who was a nonprofit CEO when she became sick. “I have heard in the last three-and-a-half years the most racist and fatphobic things I have ever heard in my life. Like, ‘Oh, sometimes you got to lay off the beans and rice.’ I have a college education. I’m an executive. I am in the top 10% of wage earners in my community. If this is my experience, what is happening to the rest of my people?”
Conspiracy theories and misinformation As Yakima Valley’s Latino vaccination rates continue dropping, I hear all the COVID conspiracy theories: the vaccine has a chip that’ll track you; the vaccine makes you and your children infertile; COVID tests are rigged to all be positive; that hospitals get paid more for COVID patients. Victoria laughs at the most absurd one she’s heard. Her mom’s explanation for her health problems nearly three years after COVID: the vaccine.
Across the Latino United States, social media algorithms and WhatsApp threads promoting COVID disinformation proliferate. Last summer, Latino Center for Health co-director Dr. Leo Morales did a long COVID community presentation just south of Yakima Valley. The audience’s first question: Are vaccines safe? “This is where we’re still at,” Morales says. “That’ll be a big stumbling block for people…in terms of getting to talking about long COVID.”
One morning in early November, Morales and his team gather in Toppenish at Heritage University, where 69% of students are Latino, to present their survey data. Neither presenters nor attendees wear masks, an essential tool for preventing COVID transmission and long COVID. “The only conversation that I’m having about COVID is in this room,” says María Sigüenza, executive director of the Washington State Commission on Hispanic Affairs.
Yakima Valley health institutions are also ignoring long COVID. Of the two main hospital systems, Astria Health declines interview requests and MultiCare reports that of 325,491 patients seen between January and November 2023, 112 — or 0.03% — were diagnosed with long COVID. The Yakima Valley Farmworkers Clinic, where María’s doctor works, refuses to let me speak to anyone about long COVID, despite providing patient information for the Latino Center for Health’s survey. Their doctors simply aren’t seeing long COVID, the clinic claims. Same with the other main community provider, Yakima Neighborhood Health Services, whose media officer responds to my interview requests with: “It’s not going to happen.”
“I think they’re not asking, they’re not looking,” Verduzco-Gutierrez says. “Do the doctors just…look at your diabetes or your blood pressure, but not ask you, ‘Did your diabetes get worse when you had COVID? Did your blood pressure get worse? Did you not have blood pressure problems before? And now do you get dizzy? Do you get headaches? Do you have pains?’” She believes that many, if not most, Latinos with long COVID aren’t getting care, whom she calls “the ones that we’re missing.”
An uncertain future The outlook for Latinos with long COVID is grim. Cultural stigma and ableism cause now-disabled long-haulers to feel shame. (Ableism is societal prejudice and discrimination against disabled people.) Disability benefits are nearly impossible to get. Long-haulers are losing their homes, jobs and insurance. Latinos’ overrepresentation in sectors that don’t offer sick pay and are heavily physical — cleaning, service, agriculture, construction, manufacturing, homecare and healthcare among them — may automatically put them at higher long COVID risk, given ample anecdotal evidence that pushing through a COVID infection instead of resting can lead to long COVID. Latino care providers will become ill in greater numbers, imperiling the healthcare industry.
But Latinos may not be clear on these factors, says long-hauler Karla Monterroso. “My tío had said…'We must be defective because we get sick more than the white people.’ And I’m like ‘No, tío. We are exposed to the illness more. There’s nothing defective about our bodies.’ I’m afraid for us. It’s just going to be disability after disability after disability. We have to start in our small communities building caring infrastructure so that we can help each other. I am clear: No one is coming to save us. We’ve got to save us.”
Disability justice advocates worry about systems unable to cope with inevitable disabling waves of COVID in the future. “(Latinos) aren’t taking it as serious as they should,” says Mayra Colazo, executive director of Central Washington Disability Resources. “They’re not protecting each other. They’re not protecting themselves.” Karla sees the psychology behind this denial: “I have thought a lot about how much it takes to put yourself in danger every single day. (You have) to say ‘Oh, it’s fine. People are exaggerating,’ or you get that you’re in existential hell all of the time.”
Reinfection brings additional risk of long COVID, research shows, and Verduzco-Gutierrez says, “We still don’t know the impact of what is going to happen with all these reinfections. Is it going to cause more autoimmune disease? Is it going to be causing more dementia? Is it going to be causing more cancer?” She believes that every medical chart should include a COVID history, to guide doctors to look for the right clues.
“If we were to be lucky enough to capture everybody who has long COVID, we would overwhelm our (health) system and not be able to do anything for them,” Victoria says. “What’s the motivation for the medical field, for practitioners to find all those people?” For now, Victoria sees none. “And until that changes, I don’t think we will (properly count Latino long-haulers),” she adds.
Flashes of hope do exist. In September 2023, the federal government granted $5 million each to multiple long COVID clinics, including three with Latino-specific projects. In New York City, Mt. Sinai Hospital will soon open a new long COVID clinic near largely-Latino East Harlem, embedded in a primary care clinic with staff from the community to reach Latino long-haulers. Verduzco-Gutierrez’s San Antonio clinic will teach primary care providers across largely rural, Latino South Texas to conduct 15-minute low-tech long COVID examinations (the protocol for which is still being devised), and will deploy community tools to educate Latinos on long COVID.
Meanwhile, at the University of Washington long COVID clinic, staff are preparing a patient handbook, which will be adapted for Latinos and then translated into Spanish. They will also train primary care physicians to be local long COVID experts, and will return to treating patients from the whole state rather than just the county containing Seattle. After palabra’s inquiry, the UFW Foundation now has plans to survey United Farm Workers members to gauge long COVID pervasiveness, so the Foundation can lobby legislators and other decision makers to improve Latino long-hauler care.
Back at the Yakima Valley survey presentation, attendees brainstorm new care models: Adding long COVID screening to pediatric checkups, given that long COVID most impacts child-bearing-age women, so moms can bring information to their families and community. Using accessible language for long COVID messaging, or, as Heritage University nursing faculty member Genevieve Aguilar puts it: “How would I talk to my tía, how would I talk to my abuelita? If they can understand me, we’re good to go. If they can’t, olvídate. We have to reframe.”
More than anything, personal narratives will be the key to open people’s minds about long COVID — although that path may be challenging. In Los Angeles, Karla has dealt with a lack of full family and community support, in part, she believes, because her body represents COVID. “I am living, breathing proof of a pandemic no one wants to admit is still happening, and that there is no cure for what I have. That is a really scary possibility.”
While Karla does identify as disabled, Victoria and María don’t. Victoria has learned to live and move within her physical limits. At work, she sometimes feels inhibited by her cognitive issues. “I tell my boss all the time, ‘Oh man, you guys hired such a smart person. But what you got was after COVID, so it’s not the same.’” At times, she worries about the trajectory of her career, about how her work’s intense problem-solving wears out her brain. Will she be able to pursue larger challenges in work in the future? Or will long COVID ultimately make her fail?
Victoria tells me she “remains hopeful that there is a solution.” In a surprising twist, her cough completely disappeared eight months ago — when she became pregnant. (Other long-haulers have seen their symptoms improve with pregnancy, as well, likely due to immune system changes allowing a pregnant person’s body to not reject their baby’s growing cells). Victoria is optimistic that her other symptoms might disappear after she gives birth. And that, maybe someday, her parents will admit they have long COVID, too.
#long covid#covid 19#mask up#covid#pandemic#public health#wear a mask#still coviding#wear a respirator#coronavirus#sars cov 2#covid conscious#covid is airborne#covidー19#covid isn't over#covid pandemic#covid19
171 notes
·
View notes
Note
hi there! I wonder if you do hc request cus this thought came to my mind
how would the eltingville boys react to the covid 19 pandemic and what do they do during the lock down?
OOOOO I love this!!
Headcanons for Covid 19 lockdown!
(I’ll be doing pre epilogue for context!!)

Bill
He’d be ecstatic to know that school was out for two weeks. That meant he’d be free to spend time gathering stuff for his collection. Then was royally butt hurt over the fact everything was closed.
Refused to wear a mask. Claimed it was “hard to breathe” and “useless.”
Went outside once out of spite. Immediately caught Covid. I like to think he has a weak immune system
Very clingy when sick and strangely kind. Enjoyed being around his brother and sister when he could be.
By strangely kind— just didn’t cuss at his siblings often, begrudgingly joined games of their, and often times was happy to have someone else to talk to.
I know for sure he tried to argue he wasn’t sick while looking like death. Then became a clingy mess when his mom got him into bed.
Chicken noodle soup enjoyer. Specifically his mom’s. Hates literally any other kind of cooking, but especially loves his mothers when he’s sick.
You have to hold him down to get him to drink water. Say it hurts his throat.
kitten sneeze. No I will not argue. He hates it.
Spent most of his day on the internet, banned from Reddit more times than he can count.
Didn’t know how to shave so he got scruff early.
Would attempt to sneak out to see his friends or make a club meeting. Always failed since he sucked at sneaking out and being quiet.
Closest person to actually ever attend a club meeting was Josh since they live so close.
Was mostly bored during Covid.
Almost cried over when the ban was lifted and immediately tried to hold a meeting.
Everyone got Covid after said meeting.
Once during a fever, ripped open a limited edition figurine and played with it. When his fever broke he threw a hissy fit at his actions.
Would lay around most days doing nothing because he couldn’t do much.
Yknow Rodrick from DOAWK. Yeah he momentarily became him during Covid before turning back into his regular jerk self to his siblings.
He would beg to walk the dog just to see the outdoors.

Josh
Calls his friends often. The reason why his parents phone bill was so high.
Ended up mailing them for awhile.
He surprisingly took care of his hair more during the lockdown.
Shocked his friends when they saw his curls. A week later they were hidden by his greasy locks.
Was kicked out of a mall because he threw a hissy fit over wearing a mask.
Wears them begrudgingly so he doesn’t get his mom sick.
Was the first member of the group to get Covid. Let them know through his mother through the landline.
Becomes a vegetable when sick. Doesn’t argue, doesn’t move much, sleeps, eats, etc.
Spoiled beyond belief while sick. He wants a popsicle, done. Another box of tissues, you got it. Random video game, sure and here’s some controllers.
Probably got hospitalized at some point because his fever just wouldn’t break.
He was fine thought.
Became a bit of an hypochondriac. Got the vaccine immediately.
Wouldn’t eat after most people. Always got food first. He’d hog most of it because he wouldn’t know if this was his last meal or not.
All failed because he wound up sick because of Bill’s meeting.
Likes to be around people when he’s sick because he doesn’t like being quarantined alone.
Had his “first” panic attack over his dad getting Covid. He was fine. Josh was grateful.
Organized and re-organized his collection. Got bored very quickly.
Tried to pick up new hobbies but was limited because of the lack of the objects in his home and he couldn’t exactly order them.
Became more social because his parents were his only physical company. He ended up picking up some cooking skills from his mom.
Made breakfast for them one day, tried to act aloof but was very happy when they enjoyed it.

Pete
Whole family got sick, including Pete.
Was pretty helpful because he didn’t think he was too “sick,” was actually the worst one of them all.
Fell asleep in awkward places, his siblings only knew where he was by his wheezy breathing.
Once everyone was done being “sick” they assumed it was just a one off thing.
They got sick many MANY more times.
Surprisingly Josh and Pete called the most. Second was Pete and Jerry.
Usually would call one of the two so they can watch a new movie of some sorts together and make commentary over it.
His dad was not happy about the phone bill.
Pete’s immune system is pretty strong because of where he grew up. Just gets hit with symptoms hard.
His little sister definitely covered him in her stuffed animals so he’d get better. It helped him a lot— mentally.
Fight me, Pete’s a cuddler. He likes to hug something while he’s sick. Won’t remember it but his family does.
They tease him over it.
Freaked out when his hair was growing too long. Doesn’t like it when it touches his neck. So he cut it himself instead of letting his dad do it like usual.
He ended up having to get it all buzzed off. But Pete didn’t care, just happy it wasn’t touching his neck.
Didn’t wear a mask throughout Covid.
He didn’t believe it was real (even though he caught it many times), thought masks wouldn’t help (he wore them wrong), and just would decline them.
Him and his siblings resorted to any social interaction with one another. Leading to a lot of game and movie nights.
Uno, Sorry, Monopoly, and even gold fish are banned. 3 holes in the wall are the reason, plus a broken table.
It was never a boring day during Covid since they’d argue over anything.
Everyone caught cabin fever.

Jerry
Last person to get Covid. First caught it through his mom.
His parents forced him to wear a mask, wash his hands, and were on top of his hygiene.
Mostly because they didn’t want to lose already limited work days because of Covid.
Jerry took care of his mom through her sickness, she definitely felt upset over this but grateful. Scolded him when he caught it from her.
They have a specific routine for every sickness Jerry gets: specific pajamas, soups, drinks, etc. His mom believes this order will always cure him in a week flat.
Always succeeds.
Called Bill once to ask him about his day. Bill understood nothing since Jerry’s voice was so raspy.
Buried himself under blankets because he’s always so cold.
Watches movies over and over since he falls asleep through them. Wore out his “Dark Crystal” tape.
Eh he hallucinates during his fevers. Nothing scary just thinking he’s in some fantasy adventure.
His mom caught him on the bed babbling about some dungeon mission. To his stuffed animals that were: Josh, Bill and Pete.
She walked out immediately.
When she came back. He was asleep in bed and curled up around the stuffed animals that were his “friends.”
After his Covid meeting, he definitely became more aware of how easy it is to catch.
Was a bit iffy on seeing the guys after the lift on quarantine.
Regretted immediately when he caught it again.
Convinced his parents to play D&D. Actually went pretty well. They had a campaign going for a few months.
Art skills improved DRASTICALLY.
Would take any social interaction as win, outside of his parents.
Probably taught himself something silly. Like juggling or balloon art.
Sorry if this isn’t what you meant 0.o but I tried to make it sound like them.
#eltingville#bill dickey#josh levy#jerry stokes#pete dinunzio#welcome to eltingville#eltingville epilogue#freye ramble#the eltingville club
89 notes
·
View notes
Text
castle of... quarantine — senku i.
brief summary: castle of sand!reader and senku during quarentine (if petrification never happened)
what to expect: covid lmao, spoilers for castle of sand up to chapter like 12, references to suicide attempt
your sword's note: this came to mind when i heard the tokyo (nya ichi ni san nya arigato) song (i miss quarentine so much), plus i am sick rn, more on my mistresslist

This never even happened, fiction within fiction am I right? What I am seeing through my crystal ball is this though: after very obviously surviving the attempt, you fixed your living situation, NOT coming back to live with your mom, so you were living now on your own, which was okay.
Better believe Senku found out about what happened, that broke him, he started acting strange. You knew he knew, he knew you knew he knew. He kept trying to approach the situation and you would dodge it all the time, but eventually he had to be direct and that was a whole crying session. He became more tender with you.
You spent new years with Senku and Byakuya, once he came back from space. Byakuya started dating Lillian, I will avoid making accommodations for that complicated situation since she is a whole star and they live in completely different countries and what not, but she was there too.
The new year started alright! You were getting used to your new house, since it was close to the school it was also close to Senku's apartment, so he would be there all the time.
Then, people started getting sick. You also better believe that Senku went out to hunt corona-virus 19 to analyze it. He got sick before quarantine even went global 💀. Nonetheless he kept it around —in a Petri dish or something, I do not know about how these things work—, and would spend all his time analyzing it. (This comes from him going to Africa to study ebola💀, he can only be so lucky to not get fucking ebola so he got covid, I say that is a gift from god).
Classes became virtual, and the world shut off. Still, as a pretend adult, you had to go out at times to get groceries and a pile of toilet paper like everyone else, and during those times he would see you. "You should come over, I will show you how the virus looks under the microscope." He would walk around you in the supermarket trying to convince you to see his damn covid. That was a no. So instead he went to your house, under the excuse that he would help you with the groceries (he carried the milk, you carried the rest). Sometimes it would get late and he would stay over, he had to call his dad to make sure he would keep an eye on his covid so it would stay alive.
You started making videos, wether it was on YouTube or TikTok or whatever platform, about philosophy, and got a decent number of followers, something like 5k, and one day you lost a bet to Senku and he made you wear cat ears and dance, congratulations you went viral! Yoohoo. Downside is that people would look at your philosophy videos and instead request more dancing, but it balanced out quickly.
At some point, his covid decided it wanted to take a journey to the outside world, and mysteriously you got sick.
"Your temperature is ten billion degrees. You probably got it." Senku shook his head looking at the thermometer. It was something rare to hear you curse, but you cursed at him right there and then. He resolved that he would stay with you and take care of you since it was his fault you got sick (Facade for treating you like his first patient). He would cook for you and spoon-feed you, give you medicine, put cold compresses on your forehead when you got fever. At the middle of the night he got an insane idea, so he rushed home after checking you were not going to start hallucinating Aristotle speaking to you, and went home for his covid pet, then, he started working on a vaccine.
"If you let me try vaccine number one on you, I will grant you one wish." Senku almost begged but it was a hard no. He ended up sending it to some real medical corporation and they actually used that for the real vaccine.
People would do crazy things during covid, personally I would always see people getting buzzcuts... yes this is going there. After seeing so many videos of people deciding to go bald, you took some scissors laying around and cut your hair until it was a mess, and then passed the electric razor. "Senku come over right now, I have what could be the best surprise I can give you in life." At your call he ran, he was imagining anything but that, when he rang the bell and you opened the door, bald as hell, he almost cried. You were shocked at his clearly in pain expression. But well you were now bald. As expected, it was not about the hair and more about the friends we made on the way (He still found you attractive like that).
His vaccines were actually working, first amongst his many science feats.
#senku x reader#ishigami senku#senku#senku ishigami#dr stone senku#dcst#dr stone#drst#x reader#dcst senku#senku x y/n#dr stone x reader#dr stone season 4
46 notes
·
View notes
Text
A new study has found that people who received mRNA “vaccines” are more likely to be hospitalized due to a COVID-19 infection.
The study revealed that Covid “vaccines” do nothing to lessen the severity of the virus.
In fact, the researchers found that the mRNA injections make COVID-19 symptoms far more severe.
The study, led by Dr. Aditi Bhargava of the University of California San Francisco, confirmed that mRNA “vaccines” increased hospitalization rates for COVID-19.
This may come as a surprise to many, as health officials around the world told the public to get their shots to reduce their risk of hospitalization.
The results of the study were just published in the journal Nature Portfolio.
In the “Abstract” section of the study’s paper, the researchers wrote:
“In an online global survey of 7,541 individuals from 95 countries, high grade fever (> 102˚F)/ hospitalization after a first SARS-CoV-2 infection were more likely to be reported by vaccinated males than unvaccinated males (13.64% vs. 8.34%; p = 0.0483; HR = 1.63 [95% CI: 1.008, 2.65]).
“Vaccine-associated hospitalization was reported by 6.24% SARS-CoV-2 naïve respondents versus 1.06% of unvaccinated after 1st SARS-CoV-2 infection.”
17 notes
·
View notes
Text
Another mysterious infectious fatal disease has emerged outside the US.
At least 79 people have died from an unknown disease that is causing flu-like symptoms in south-western Democratic Republic of Congo, the health ministry says. The health ministry says the majority of people who have died are between the ages of 15 and 18. More than 300 people have been infected with patients exhibiting symptoms like fever, headaches, runny noses and coughs, breathing difficulties and anaemia.
If you do the math, this infection has a death rate of over 25%. It also targets young people like the deadly "Spanish Flu" pandemic of 1918-1919. Being "flu-like" means it may be difficult to distinguish from typical seasonal influenza. That also implies that it could easily be transmitted like the flu.
Response teams have been sent to Kwango Province, specifically the Panzi health zone, where the disease is most common, to manage cases and investigate the nature of the disease. Cephorien Manzanza, a civil society leader, told Reuters news agency the situation was worrying as the number of infected people continues to rise. "Panzi is a rural health zone, so there is a problem with the supply of medicines," he said. A World Health Organisation (WHO) Africa region official told the BBC they have "dispatched a team to the remote area to collect samples for lab investigations". Authorities have urged the population to remain calm and vigilant.
Kwango Province is adjacent to the region where the capital Kinshasa (pop. 17 million) is located.

If the Kwango infection spreads to the US after Trump's inauguration, we would be in even worse shape than when COVID-19 came to the US. Instead of Dr. Anthony Fauci, we'd have anti-vaxxing quacks like RFK Jr. and other clowns running American public health.
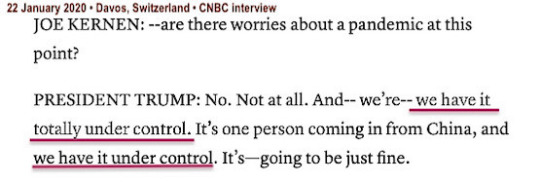
Trump himself would try to underplay a new pandemic the way he did in 2020. In case you've forgotten, this was his reaction to the first case of COVID in the US...
Trump waited until March 13th to declare a state of emergency. COVID had already spread to most of the US during the 50 days he hoped the infection would just go away on its own.
Urge your US senator to reject any Trump public health nominee who does not accept standard scientific and medical thinking related to infectious diseases.
In the meantime, it's a good idea to catch up on related vaccinations such as seasonal flu, COVID boosters, and RSV before the December holidays.
#infectious diseases#democratic republic of congo#kwango#panzi#world health organization#flu-like symptoms#high fatality rate#donald trump#unqualified nominees#public health#rfk jr.#anti-vaxxers#quacks#covid-19#pandemic#trump botched the response to covid-19#vaccines
25 notes
·
View notes
Text
So, school has started once more, so my wife and I went yesterday for our flu and Covid boosters- we got the new booster that just came out, and if you were waiting to get it because of possible side effects, I wanted to record my experience.
1) pain at time of injection- present, but mild compared to previous years. There was a flash of deeper pain about an hour later, but that faded too.
2) sore arm- It’s now been almost 19 hours and it feels like a bruise rather where the bandaid is rather than the full on hurt myself at the gym soreness from previous years.
3) headache- none
4) chills- none
5) fever- none
6) gastric distress- none
7) sore neck- could be? But I often have stiff and sore neck muscles because of how I sit at my craft table. So, I don’t k own if it’s related.
They say side effects, if any, appear 8-12 hours after injection and last for maybe 48 hours. Like I said, it’s been about 19. I’m a little sore and a little tired, but otherwise I’m fine. Get vaccinated.
43 notes
·
View notes
Text

Welcome to another Work in Progress Wednesday! So, if we're getting technical, this story is completed, but I want a chance to give it at least one or two read-throughs because one day, I was writing with a fever because I reacted very strongly to the COVID-19 vaccine [get your shots!] This fic is a little over 7k at the moment, but I'm not sure what the final word count will be once we get the edits in. This fic serves as a pretty decent follow-up to events that take place in both Sleeping Wake/Waking Sleep and The Hour of Separation, but I do try to make sure to give enough details so you can understand more or less what happened. On The Brink Of Hell should be posted in the next day or two and I'm about to start outlining another one-shot in this verse.
"I was wondering when you were going to turn up," Johanna said, and she was not going to call attention to the fact that her voice cracked; she absolutely refused, even if she knew Dream would never judge her for showing weakness.
"The memory and nightmare do not happen every night, and since you have asked me not to interfere with them, this is what I can do for you," Dream replied. He moved across her room almost silently, but Johanna could very much feel his presence as he sat down next to her on the couch. Not long ago, she would have shied away from taking comfort like this, but she leaned into Dream and let him hold her for a moment. "Something else is troubling you."
"Sometimes I think I shouldn't have shown you my tells," Johanna replied, but there wasn't any humor behind it. She sat up and looked at the notebook in her hands. "Edwin, when I first met him and Charles, I said I wouldn't work for free, so I asked for something. You could see it as much as I could, the scars that hell left on his soul, and he told me that he found his own way out." Dream seemed to go very still at her side. "It wasn't a portal or anything we need to worry about; it was a door that was closed after he went through it, so no worries there. He was sent back, and Charles used his notes and map as a guide to go down and pull Edwin out again. So, I asked for his map out of hell for payment."
#dead boy detectives#the sandman#payneland#johanna constantine#edwin payne#charles rowland#dream of the endless#my writing#work in progress wednesday
20 notes
·
View notes
Text
ASAN is deeply troubled by reports made by The Washington Post this Tuesday that the CDC is planning to change its COVID-19 isolation guidelines. ASAN condemns the potential new guidelines, which would remove the five-day isolation period currently recommended after a positive test for COVID-19. Instead, people with a positive test result would not need to isolate if they have been fever-free for at least 24 hours without the aid of medication.
ASAN has spoken repeatedly on the failures of the US government to respond adequately to COVID-19. Despite the ongoing pandemic, the end of the public health emergency and subsequent Medicaid unwinding have been devastating to the disability community and other marginalized communities. Efforts to encourage adherence to masking guidance and improve indoor air quality have been underwhelming. Through their actions, the CDC and US Government as a whole have indicated the strategy to combat COVID-19 is seemingly a vaccine-only response, but, with adult uptake of the latest bivalent booster being only 21.9%, even these efforts are beyond inadequate.
This change is particularly alarming given who is likely to be among the most impacted. Changing the isolation window disproportionately exposes and affects vulnerable populations such as disabled and immunocompromised people, older adults, and other high-risk groups. These guidelines would increase COVID-19 exposure and make people at high risk of poor outcomes from COVID-19 less safe in a range of public and private spaces.
Asymptomatic spread remains a serious concern with the latest variants. Reduced access to at-home and PCR testing since the end of the public health emergency contributes to transmission. Removing the isolation window adds increased pressure to return to school and work while potentially infectious. This will disproportionately affect individuals with hourly jobs that must be performed in person and families with children that are lower-income and families of color, as many communities aggressively enforce truancy laws against these households. Counting on the availability of treatments like Paxlovid as a mitigation strategy is highly inequitable as racial and ethnic disparities in outpatient treatment of COVID-19 remain prevalent. An approach to COVID-19 that accepts widespread and repeated infection leaves the most vulnerable among us unprotected. As we have seen throughout the pandemic, it has also led to the emergence of new variants, putting our communities at additional risk. Each repeated infection increases an individual’s likelihood of developing Long COVID, a potentially lifelong disability with limited treatment options.
The CDC has continually failed to take into account disabled people when making COVID-19 policies and regulations. The CDC is moving in the wrong direction by reducing COVID-19 isolation periods. Instead, it should release improved guidelines to promote masking and increase availability, accessibility, and understanding of vaccines, testing, and treatment. States and the federal government also must address the continued effects of the pandemic and the end of the public health emergency on health care access and home and community based services, make investments in improving indoor air quality and preventing and treating Long COVID, and address the economic and human impacts of this crisis. ASAN condemns the possible shortening of isolation guidelines and will continue to hold the federal government accountable for protecting the public from the ongoing risk of COVID-19.
73 notes
·
View notes
Text
May 2025 Covid Update 🦠
There are 2 concerning new variants competing to be the dominant strain: NB.1.8.1 (Nimbus) - Omicron subvariant XFG - Omicron subvariant
Both were spreading at similar rates in different parts of the world but are now being detected globally and could lead to higher waves.
NB.1.8.1: has a high rate of transmission as it bonds to cells efficiently. Symptoms: sore throat, fatigue, fever, mild cough, muscle aches, nasal congestion, gastrointestinal symptoms - nausea, loss of appetite, stomach discomfort, and diarrhea. Some surges in hospitalization in some areas (China, Hong Kong, India).
XFG: has a high rate of transmission and seems to be able to evade immune protection better. Symptoms: sore throat, fatigue, fever, mild cough, muscle aches, nasal congestion, gastrointestinal symptoms - nausea, loss of appetite, stomach discomfort, and diarrhea.
Note: loss of taste and smell is not commonly reported for either new variant.
Vaccine/Booster/Protection: Current Covid vaccines are for previous variants KP.2/JN.1 and should still protect against severe disease with these variants. Vaccine immunity is strongest in the first 2 months with gradually declining protection for up to 6 months. The immune response from getting Covid declines more quickly than vaccination. The wait time for a booster after having Covid is 3 months.
Vaccines to match the new dominant variant(s) may be updated in the fall.
Covid-19 is airborne so ventilation, air filtration, avoiding exposure, and N-95 masks are good variant proof protections.
4 notes
·
View notes
Text
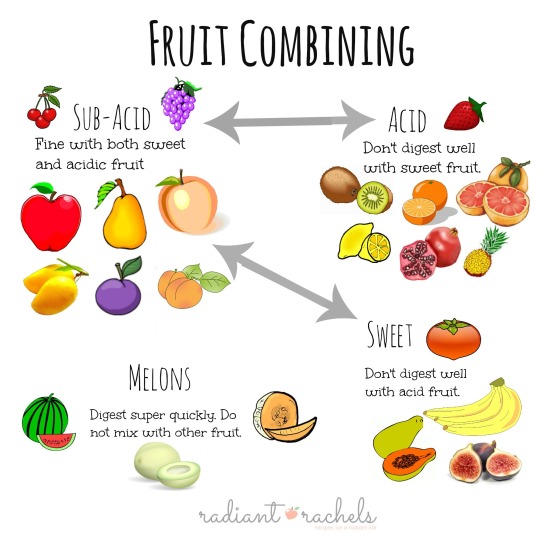
I like to re post this every now and again because it's good advice I frequently forget.
Also I post it in part because I'm laying in bed with Covid (for the first time) at the moment and eating as much fruit as I can to expedite recovery. I grabbed a banana and orange, ate the banana and asked myself if this was a good combo or not. Glad I checked, because it was not. The last thing I need is indigestion.
But because it's me, my main focus has been doubling down on nutrition and observing my own results. I was eating plant based before, but sometimes I went a little too hard on the peanut butter trail mix, breads, or other sweet treats.
My doctor said rest and hydrate, but I took it a step further and since testing positive have cut out wheat, sugar, and any kind of dairy or processed foods. I figure nothing that could make inflammation worse. I've been consuming tons of herbs like cinnamon, ginger, echinacea, and turmeric while eating fresh citrus fruits like lemon, orange, strawberry, and pineapple daily.
Now I did a bit of tooling about the internet to see if any studies had been done over the last four years regarding a plant based diet and it's effects on Covid. The results were hopeful.
I found one study that said,
"Merino et al revealed that healthy plant-based foods could decrease the risk and severity of COVID-19.21 In this large survey, it was shown that as the quality of the diet rises, the risk of disease COVID-19 (HR 0.91) and severe COVID-19 (HR 0.59) diminishes.
Which gave me hope so I kept digging.
Another one stated, "Compared with an omnivorous Western diet, plant-based diets containing mostly fruits, vegetables, grains, legumes, nuts and seeds, with restricted amounts of foods of animal origin, are associated with reduced risk and severity of COVID-19. "
And I can tell you that has been my experience thus far. I developed a fever that went away after 24 hours and didn't go over 100.4. My only other symptom has been a stuffy nose with sinus pressure. Im definitely tired and need to limit activity but I can still taste and smell, breathe through my nose a decent amount of the time, and I'm not coughing. I'm lucky in that I have time off from work and for that I am grateful, as rest is another key component.
And why would a plant based diet be so beneficial for mitigating Covid symptoms? Because, "plant-based dietary patterns are rich in antioxidants, phytosterols and polyphenols which positively affect several cell types implicated in immune function and exhibit direct antiviral properties."
The full study can be found if you pop this into Google::
Acosta-Navarro JC, Dias, LF, de Gouveia LAG et al. Vegetarian and plant based diets associated with lower incidence of COVID-19. BMJ Nutr Prev Health 2024:e000629. doi:10.1136/bmjnph-2023-000629
I was really scared at first and this information helped me feel more empowered in my health and recovery. It's not a substitute for any medical attention or prevention like vaccines, hand washing, and mask wearing- all things I was doing regularly prior to getting sick which may have also been variables in keeping my symptoms down. A little help goes a long way.
Has any other plant based person had a similar experience? Let me know.
#food#vegan#foodie#healthy#health#vegetarian#fitness#diet#nutrition#plant based#plant based diet covid#covid conscious#covid recovery#covid vegan#study#herbology#herbs#inflammation#fitblr#healthy lifestyle#long covid
43 notes
·
View notes
Text
Also preserved on our archive
By Pandora Dewan
Levels of the virus that causes COVID-19 remain high across the U.S. despite recent decreases in positive case reports across the country. However, viral activity varies significantly across different states, new data from the U.S. Centers for Disease Control and Prevention (CDC) shows.
As of September 21, the overall viral activity level in wastewater across the country has been demoted from "very high" to just "high," although "very high" levels are still being detected in 13 states. These are particularly concentrated in the Midwest. Twenty-one states now exhibit "high" levels of wastewater activity, and nine are classed as "moderate."
Meanwhile, "low" levels have been detected in six states, with "minimal" levels, the lowest classification, seen in New York.
After a surge in COVID-19 cases this summer, infection rates seem to be on the decline. Positive tests now account for 11.6 percent of all COVID tests (excluding at-home testing) in the U.S., down 1.8 percent from the previous week. Coronavirus levels do remain high in certain states, especially those in the Central U.S.
The map below shows which states have seen the highest detections in wastewater.
(Follow link for interactive map)
Viral levels in wastewater are a helpful indicator of disease prevalence within a population.
Recent spikes in COVID-19 cases have been largely driven by a new class of subvariants nicknamed FLiRT after the position of the mutations on the virus' spike proteins, the projections that allow them to enter our cells.
These proteins are also used as targets by immune systems and vaccinations, so changes in their structure can allow the virus to bypass the body's defenses more easily. However, existing vaccines are likely to provide at least some form of protection against more severe symptoms and long COVID.
As of September 28, the now dominant subvariant, KP.3.1.1, accounted for more than 59 percent of all U.S. COVID-19 cases over the previous two weeks, according to the CDC, with the FLiRT variants accounting for more than 80 percent of cases in total.
However, while the U.S. has seen a steady rise in infections over the summer, hospitalizations and deaths have remained relatively low. It appears that the new FLiRT variants, while more infectious, do not generally cause such severe symptoms.
The symptoms include the following, according to the CDC:
Fever or chills Cough Shortness of breath Fatigue Muscle or body aches Headache Loss of taste or smell Sore throat Runny nose Nausea or vomiting Diarrhea
More vulnerable individuals may still be at risk of severe illness, so it is important to self-isolate if you receive a positive COVID test.
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#wear a respirator#still coviding
204 notes
·
View notes
Text
Reed McMaster at MMFA:
So far in 2024, New York Jets Quarterback Aaron Rodgers has appeared on multiple right-wing podcasts where he has promoted conspiracy theories. What began publicly as a hesitancy to get vaccinated for COVID-19 appears to have devolved, with the athlete now spewing absurd conspiracy theories and bigoted misinformation on right-wing platforms.
Rodgers has been a repeat guest on ESPN’s The Pat McAfee Show for years. Rodgers has had a long-running deal with The Pat McAfee Show, making regular weekly appearances during the NFL season as part of “Aaron Rodgers Tuesdays.” According to The Pat McAfee Show’s YouTube channel, Rodgers has made at least 68 appearances since September 18, 2019. [YouTube, accessed on 5/20/24; Forbes, 10/12/23]
In 2021, Rodgers revealed on The Pat McAfee Show that he was unvaccinated for COVID-19 after claiming earlier in that year that he was “immunized.” Rodgers defended his decision not to get vaccinated and claimed he was not being dishonest by insisting he was “immunized” earlier that year. He also complained that a “woke mob” was trying to “cancel” him because he’s unvaccinated against COVID-19. [NBC, 11/5/21]
New York Jets QB and Pat McAfee Show regular Aaron Rodgers has become infamously known for spewing bonkers conspiracy theories in recent years.
#Aaron Rodgers#Conspiracy Theories#Joe Rogan#NFL#New York Jets#ESPN#Pat McAfee#The Pat McAfee Show#Eddie Bravo#Tucker Carlson#The Joe Rogan Experience#The Tucker Carlson Show#Anti Vaxxer Extremism#Coronavirus#Sports Media
14 notes
·
View notes
Text
So I caught COVID-19 for the first time, and I just wanted to share how the symptoms have presented themselves with me, an overweight woman in her late twenties that has had four vaccinations
So, I’ve had a cough for several days, at least since Wednesday. But it wasn’t until Sunday that I had a fever, slight body aches, a heavier cough, nasal congestion, a runny nose. My fever reached 38.7°C (101.66°F) so I rested all day. The following day, my fever was gone and has not returned.
I went to work on Monday (I didn’t know it was covid, and my job expects people to only stay home if they have a fever). My cough was really bad. I was on the subway with this violent cough and itch in my throat. It was like my entire body was exerting itself, so when my coughs subsided, I would feel pain even in my pelvis, back, and arms. It wouldn’t last long, it felt the way your chest hurts and relaxes after coughing.
A few hours into work, I started to feel that my coughs were turning into retching. So, I ran to the restroom and vomited, and my nose bled at the same time.
For the next couple of hours, I needed to keep blowing my nose because it was so runny, and my voice was hoarse. I also felt fatigue. I left early from work and went to a clinic to take a rapid test. I tested positive.
Since then, I’ve been self-quarantining. As said previously, I haven’t had a fever since Sunday. However, when coughing up phlegm, and just recently vomiting, I’ve bled from my nose. I had pain within my left ear on Monday night, and it was painful to swallow at one point. My mucus has been thick, and I’ve had a stuffy nose.
Regarding the nosebleeds, I do want to share that I’m someone who gets random nosebleeds every once in a while, ever since I was a kid. However, I’ve never had nosebleeds while vomiting or coughing before. And this time around, I’ve been having so many nosebleeds that I’ve lost count. And the blood has come out of both nostrils.
I’ve never seen any mention about frequent nosebleeds as a symptom of Covid before, so I thought that piece in particular would be noteworthy.
3 notes
·
View notes
Text
It did not seem like a good thing when a precious consignment of human tumour samples on its way from Kampala, Uganda, to Heathrow was diverted to Manchester. When the samples finally arrived at the Middlesex hospital in London, they were swimming in murky fluid in their vials as though they had been infected with bacteria.
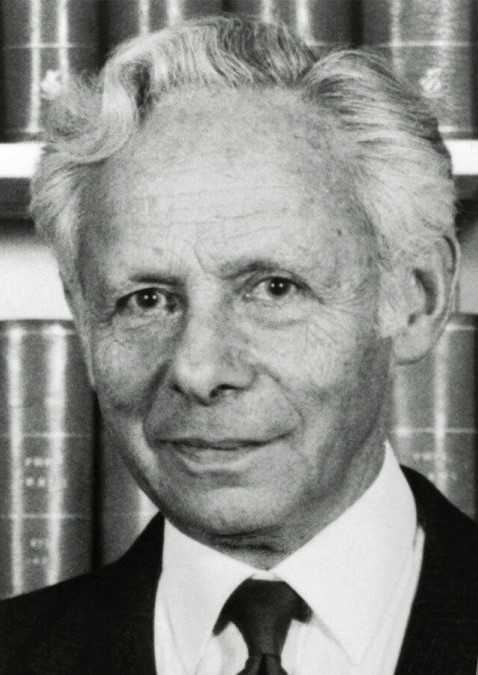
But when the pathologist Anthony Epstein looked at the fluid under the microscope he saw no bacteria, just individual cells that had been shaken loose from the tumours. And that was just what he needed in order to search for elusive virus particles and test his hunch that they were causing cancer.
In the early 1960s Epstein, who has died aged 102, had heard a lecture by Denis Burkitt, an Irish surgeon working in Kampala, that described strange tumours (now known as Burkitt lymphoma) growing around the jaws of children in equatorial Africa.
Intriguingly, the geographical distribution of the condition seemed to depend on temperature and rainfall, suggesting a biological cause. Epstein, who had been working with viruses that cause cancer in chickens, immediately suspected a virus might be involved, perhaps in association with another tropical disease such as malaria.
Epstein began to collaborate with Burkitt, who supplied him with tumours from children he had treated. But Epstein’s efforts to grow pieces of tumour in the laboratory and isolate a virus had all been unsuccessful until the dissociated cells arrived.
With his graduate student Yvonne Barr, he then decided to look at cultures of these cells in an electron microscope, a powerful instrument that had only recently become available in his lab.
The very first image showed a tell-tale outline that looked like one of the family of herpes viruses. It turned out to be a previously undescribed member of that family, and was given the name Epstein-Barr virus. In 1964, Epstein, Barr and Epstein’s research assistant, Bert Achong, published the first evidence that cancer in humans could be caused by a virus – to be greeted by widespread scepticism even though they went on to demonstrate that EB virus caused tumours in monkeys.
Thanks to samples supplied by Epstein, in 1970 Werner and Gertrude Henle at the Children’s hospital in Philadelphia discovered that EB virus also caused glandular fever. That made it possible to design a test for antibodies to the virus in order to confirm a diagnosis. EB virus turned out to be very common, infecting most children in early life, though it usually causes glandular fever only in older teenagers and young adults. As well as causing Burkitt lymphoma in endemic areas in Africa and Papua New Guinea, it is also associated with a cancer of the nose and throat that is the most common cancer of men in south China, as well as cancers in people whose immune systems have been compromised, such as those infected with HIV.
More recent research suggests that EB virus might also be involved in some cases of multiple sclerosis, and that people who have previously had glandular fever are more susceptible to severe Covid-19.
After the discovery, Epstein and others devoted time and effort to trying to find out under what circumstances EB virus causes cancer. The relationship between the virus, other diseases, human genetics and cancer is complex, and it took decades before the medical community could accept the EB virus as a cause with confidence.
Not until 1997 did the International Agency for Research on Cancer class it as a Group 1 carcinogen, formally acknowledging its role in a variety of cancers.
The discovery of EB virus opened up a whole new field of research into cancer-causing viruses. It also raised the exciting possibility of preventing cancers through vaccination, an advance that has now been achieved in the case of human papilloma virus, which causes cervical cancer, and hepatitis B virus, which causes liver cancer.
By the time of his retirement in 1985, Epstein’s research group at the University of Bristol had developed a candidate vaccine that protected monkeys infected with EB virus against tumours, but neither it nor any other candidate has yet been successfully developed for human use.
Epstein was born in London, one of three children of Olga (nee Oppenheimer) and Mortimer Epstein. Mortimer was a writer and translator who edited The Statesman’s Yearbook for Macmillan from 1924 until his death in 1946. Olga was involved with charitable work in the Jewish community. Anthony attended St Paul’s school in west London, where the biology teacher Sidney Pask encouraged boys to go far beyond the syllabus and whose pupils also included Robert Winston and Jonathan Miller.
Epstein won a place to study medicine at Trinity College, Cambridge. He moved to Middlesex hospital medical school in wartime London to complete his training, before doing his national service in India with the Royal Army Medical Corps. He returned to work at the Middlesex hospital as assistant pathologist, conducting his own research. Thinking electron microscopy might be useful in his studies of cancer-causing viruses in chickens, he spent some time learning the new technique at the Rockefeller Institute in New York (now Rockefeller University). Not long afterwards he attended Burkitt’s lecture and began the serendipitous route to his discovery.
In 1968 he was appointed professor and head of the department of pathology at the University of Bristol, where he remained until his retirement. He moved to Oxford as a fellow of Wolfson College in 1986, becoming an honorary fellow in 2001.
An exemplary scientific good citizen, he served as foreign secretary and vice-president of the Royal Society, and sat on boards and councils for numerous national and international research organisations, including as a special representative of the director general of Unesco; he was also a patron of Humanists UK. Among his many prizes and honorary degrees, he received the international Gairdner award for biomedical research in 1988. He was appointed CBE in 1985 and knighted in 1991.
“It was a series of accidents, really,” he said of his discovery in a conversation with Burkitt they recorded for Oxford Brookes University’s oral history archive in 1991. “Lucky quirks.” Burkitt immediately responded with Louis Pasteur’s aphorism: “Chance favours the prepared mind.”
Epstein was a deeply cultured man who retained a lively interest in many subjects – particularly oriental rugs, Tibet and amphibians – until the end of his life.
He is survived by his partner, Kate Ward, by his children Susan, Simon and Michael, from his marriage to Lisbeth Knight, from whom he was separated in 1965, and who died in 2015, and by two grandchildren and two great-grandchildren.
🔔Michael Anthony Epstein, pathologist, born 18 May 1921; died 6 February 2024
Daily inspiration. Discover more photos at Just for Books…?
13 notes
·
View notes