#emdr therapy and bipolar disorder
Explore tagged Tumblr posts
Text

Expert Trauma Counseling with EMDR in San Antonio
If you are looking for expert trauma? choose Jim Toombs, MA, LMFT, EMDR. Improve you with expert trauma counseling in San Antonio using EMDR therapy. Our experienced therapists offer personalized care to help you navigate and overcome past traumas. Take the first step towards emotional wellness today. Visit here: - https://jimtoombs.com/what-i-treat
#emdr therapy san antonio#emdr san antonio tx#emdr for stress#emdr counselling#emdr therapy and bipolar disorder#EMDR and Ketamine assisted psychotherapy KAP#PTSD EMDR
0 notes
Text
Welcome to McLeod Counseling, PLLC in Rochester, New York
McLeod Counseling, PLLC is a mental health and Christian counseling service in Rochester, NY. We specialize in helping couples in their marriages, those struggling with depression and anxiety, bipolar disorder, or helping those with grief, loss, PTSD or traumatic events. With over 20 years practicing and hundreds of clients, we are compassionate and understanding of all life experiences. We actively listen to your situation and concerns, and guide you through varying types of therapy to improve your mental health and and overall well-being. We also perform DWI and DOT/SAP assessments. Schedule a one-on-one counseling session or assessment today by calling us 585-967-9700 or requesting an appointment on our website.
McLeod Counseling, PLLC
3045 E Henrietta Rd, Henrietta, New York 14467
585-967-9700
#counseling#marriage counseling#family counseling#mental health#mental health counseling#grief counseling#trauma counseling#PTSD counseling#emdr therapy#Bipolar Disorder therapy#DOT SAP assessments#OASAS assessments#drug and alcohol counseling
1 note
·
View note
Text
cw for mentions of abuse, violence, self harm, suicide, substance abuse, etc (none of it goes into detail at all)
Text in images and resources under cut
Dissociative Identity Disorder
Hazy System / Fallen Collective
What is DID?
Dissociative Identity Disorder is a mental disorder where one has two or more identity states. These different parts, or alters, may have different names, genders, ages, mannerisms, behaviours, memories, and opinions. There is also amnesia, or more often, dissociative amnesia, along with struggling or being unable to function in day to day life.
(A picture of a fragmented person with smaller humanoid figures is in the bottom right corner)
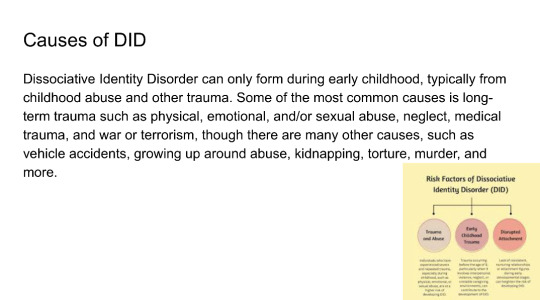
Causes of DID
Dissociative Identity Disorder can only form during early childhood, typically from childhood abuse and other trauma. Some of the most common causes is long-term trauma such as physical, emotional, and/or sexual abuse, neglect, medical trauma, and war or terrorism, though there are many other causes, such as vehicle accidents, growing up around abuse, kidnapping, torture, murder, and more.
(A picture that provides a graph titled: Risk Factors of Dissociative
Identity Disorder (DID) then a circle that says: Trauma and Abuse, below it says: Individuals who have experienced severe and repeated trauma, especially during childhood, such as physical, emotional, or sexual abuse, are at a higher risk of developing DID. A second circle says: Early Childhood Trauma, below it says: Trauma occurring before the age of 9, particularly when it involves interpersonal violence, neglect, or unstable caregiving environments, can contribute to the development of DID. A third circle says: Disrupted Attachment, below it says: Lack of consistent, nurturing relationships or attachment figures during early developmental stages can heighten the risk of developing DID.
Symptoms of DID
Symptoms required for a diagnosis are:
A disruption of identity by two or more distinct personality states. The disruption in identity involves marked discontinuity in sense of self and sense of agency, accompanied by other changes in affect, behaviour, consciousness, memory, perception, cognition, and/or sensory-motor functioning.
Recurrent gaps in the recall of everyday events, important personal information, and/or traumatic events that are inconsistent with regular forgetting.
The symptoms cause clinically significant distress or impairment in social, occupational, or important areas of functioning
The disturbance is not a normal part of a broadly accepted cultural or religious practice
The symptoms are not attributable to the psychological
effecte of cubstances.or other medical conditions
An image in the bottom right corner is titled: Dissociative identity disorder
(DID)
The symptoms of DID include: Having at least two identities. Gaps in memory. Daily functioning and socializing challenges.
And then at the bottom it gives the resource name, Cleveland Clinic
Prevalence of DID
Most current studies show dissociative identity disorder is diagnosed to 0.1% to 2% of the global population, though a few give estimates to as high as 3%-5%.
DID is often seen as a very rare disorder, but that's not entirely true. If a prevalence rate of 1.5% is accepted for DID, it is comparable to chronic major depressive disorder (1.5%), bulimia nervosa in women (0.46%-1.5%), and obsessive compulsive disorder (1.1%-1.8%); it is more common than intellectual disability (1%), autism spectrum disorder (1%-2% in the United States but 0.62% globally), schizophrenia (0.3%-0.7%), and persistent depressive disorder (dysthymia) (0.5%); and it is only slightly less common than panic disorder (1.7%-3%), adult ADHD (2.5%), and bipolar 1, bipolar 2, and bipolar disorder not otherwise specified combined (1.8%-2.7%)
Treatment
Common types of treatments are eye movement desensitization and reprocessing (EMDR) therapy, prolonged exposure (PE) therapy, and cognitive behavioral therapy (CBT).
There are two types of goals one may have for recovery and treatment. One may be integration (final fusion), or partial integration (resolution or functional multiplicity).
Integration is when all parts work together to get over the trauma, lower the dissociative amnesia between parts, and take ownership for all thoughts, feelings, memories, urges, skills, and other traits. This is so that the different alters can eventually fuse into one.
Partial Integration is when parts work together to get over the trauma and lower the dissociative amnesia between alters, but they remain separated as different parts for whatever reasons they may have. The end goal for them is really just to work through trauma and learning how to function in day to day life.
Inter-identity amnesia in dissociative identity disorder resolved: A behavioral and neurobiological study - by Lora Dimitrova, Andrew Lawrence, Eline Vissia, Sima Chalavi, Andreana Kakouris, Dick Veltman, and Antje Reinders
DID has subjectively reported inter-identity amnesia, reflecting compromised information transfer between dissociated parts. There have been many conflicting studies regarding memory transfer between parts. Inter-identity amnesia was investigated in people with DID using self-relevant, subject specific stimuli, and behavioral and neural measures. Data included 14 individuals with DID in a trauma-avoidant state, 16 trauma-avoiding DID stimulators, and 16 healthy controls. Reaction times and neural activation patterns were documented with three types of subject specific words: non-self-relevant trauma-related words (NSt), self-relevant trauma-related words from a trauma-avoidant identity state (St), and trauma-related words from a trauma-related identity state (St).
There were no differences in reactions times between XSt and St words, but faster reaction times of XSt over NSt words. Reaction times of the diagnosed DID group were longest, with increased brain activity to XSt words found in the frontal and parietal regions, while decreased brain activity in the anterior cingulate cortex in the diagnosed DID group. This finding of increased cognitive control over self-relevant trauma-related knowledge processing calls for the redirection of "inter-identity amnesia" to "inter-identity avoidance."
Other Information
Quite a few people believe that DID can make someone violent, but that's not entirely true. Horror movies, and most media overall, that feature characters with DID have contributed to this myth and may even be responsible for it. DID is a controversial diagnosis partially because of the fear of criminals avoiding punishment if it is claimed that another alter did the crime; this is also not something that can happen, because if one part commits a crime, the individual as a whole will face punishment. A 2017 study shows that among 173 individuals with DID in treatment had low involvement with criminal justice system. The myth that people with DID are dangerous only further stigmatizes the disorder.
Other Information
The most probable first documentation of DID was in 1584, by Jeanne Fery.
Though convinced it was possession at the time, her recording of her symptoms match up with those with DID today. She had multiple alters, each with their own name, identity, and identifying features. The parts she documented would today be described as an internal self helper (ISH), persecutory protectors, and child alters. Her alters actions ranged from helping her heal to self harm to disordered eating, could be hear in her head, and could take control of her body, and had changes in knowledge and skills. The alters resulted in childhood physical and possible sexual abuse.
Resources: https://my.clevelandclinic.org/health/diseases/9792-dissociative-identity-disorder-multiple-personality-disorder
#long post#did#dissociative identity disorder#dissociative disorder#cdd#complex dissociative disorder#did info#did information#dissociative identity disorder info#endos dni
9 notes
·
View notes
Text
I’ve spent my 20’s trying to get better. Early on I had hope so so much hope. I tried each new medication and as each one didn’t work my hope dwindled but I tried to remain as positive as I could because it takes time and finding the right treatment isn’t easy it can take years. But I’m approaching 30 and the medication I thought was working actually wasn’t and it was just my ‘natural cycle’ for my Bipolar and now the Bipolar mania and depression has come back. The worst part is that I have run out of medications. They can try a combination of meds to add to my Lamotrogine but if they can’t find a combo and if the increase in my Lamotrogine doesn’t help with my bipolar depression then my only and last option is Lithium. I asked and he said I have literally run through everything there is. And sure it often requires more than one medication like Lamotrigine doesn’t help mania but should help my depression and he’s given me the name of a med I can try for my mania it doesn’t prevent it but helps reduce the symptoms of my manic episodes hopefully to something more manageable and less destructive. But the thing is it doesn’t stop there because that still leaves my BPD, CPTSD, Panic Disorder and GAD. I just started therapy earlier this year to do EMDR which should help the CPTSD and BPD idk about the rest. He said usually they treat the anxiety with anti depressants but I cannot go on those due to my Bipolar. I’ve spent my 20’s trying to find something to help managed my Bipolar and it feels like at this point I could spend my entire life just trying to not feel the pain the depression of my illnesses. Who wants to spend their entire life trying to fix the pain and never getting to the point where they have, where they’ve got to a point that it no longer hurts so much that I can live my life where it’s just a background noise that I have the skills and medication to manage it. What is the point in living if it’s just going to be a battle with myself that I never really win?
#er#erin talks#prsnl#depression#bipolar#bpd#cptsd#panic disorder#anxiety#mentally ill#what if it never gets better
8 notes
·
View notes
Text
the thing is
ocd is manageable with exposure response
Bipolar is treated with mood stabilizers and antipsychotics work well with psychosis
ptsd responds well to EMDR
BPD is manageable with DBT
diabetes with insulin
celiac with a gluten free diet
chronic pain with physical therapy
addiction with certain meds or treatment.
heart attacks with lifestyle changes
a lot of health issues can be managed with something doable. but is it affordable, and attainable and what if you have like three other conditions?
I’m over here like: every one of my mental disorders and physical conditions can be dealt with but my dudes I grow weary of juggling appointments and meds and it’s like a full time job to take care of myself, as a disabled person
Idk if that makes sense. I’m tired of how much work it is to stay healthy or even almost okay
0 notes
Text
I have a lot of different feelings about the psych abolition movement. On one hand, if that's your thing I support you wholeheartedly because I've seen it, I've lived it, I KNOW it's that grim and abusive and destructive most of the time.
Most of the time! And that is not in any way okay!
I don't mean "I know" as in "I believe you." I mean I know it better than most people do because I've been contending with it for decades. If I'm an expert in anything it's in dealing with the mental health system in the U.S. both as a 'client' and as a family member of loved ones who are.
On the other hand, honestly I'm mostly just heartbroken because I'm old enough to remember when it wasn't.
I'm gen X. I remember the culture of psych treatment as it was in the nineties and early 2000s. Back then I felt confident in suggesting to someone that they should get help. Nowadays when someone says they haven't found anyone worth trusting I'm like, IKR?
Back then, aside from the few people who obviously didn't belong in the profession, you just plain never ran across a therapist who didn't eventually spontaneously comment that their client is the expert and they're just following their client's lead. They would comment that they had learned far more from their clients than they ever did in school. Their entire thing was validation and unconditional positive regard and meeting someone where they were.
And then CBT happened. And then DBT happened. And then ACT happened. CBT started in the seventies but these have become more and more prominent and now they're nearly the only things out there.
I'm not knocking these things in their entirety. They're brilliant for what they do but they are all first aid. They will stop you from bleeding out long enough for you to start doing the real work.
They have forgotten the second part. There is no sense that you put someone through a cognitive therapy to start with and then you move them over to a humanistic or insight-oriented type of therapy. Just try calling any large practice that has a dozen or more therapists on staff and asking them if they have someone whose style of therapy isn't primarily cognitive. Just try telling them that you've already done CBT, DBT, and ACT and you're looking for someone who can offer a type of therapy other than that.
Eventually, maybe you'll find someone who does IFS or EMDR. Maybe. Good luck finding any of the other varieties of therapy that were the most common ones available in the nineties.
This isn't okay. This is what needs to change.
All might be fine if you're distressed over a circumstance but you're not actually mentally ill. CBT or ACT might be more than enough to get you through it and back on your feet. For something more internal, though? For CPTSD or one of the personality disorders or to deal with the pain and despair that comes with bipolar I or schizospec or any of the other deeply stigmatized diagnoses or living with racism, a chronic illness or disability, or another marginalized experience? The cognitive therapies are completely inadequate. They eventually amount to victim blaming and they completely miss the fact that our pain is reasonable and to be expected given what we're living with.
What is much, much worse than the lack of availability of other therapies are the attitudes of those CBT, DBT, and ACT therapists who wholeheartedly believe that their therapies are all that anyone should need. They believe that once you learn their skills and start to approach things from the right mindset, all will be fine.
If CBT, DBT, and ACT didn't do the trick why are you still complaining? You must be a failure. You must not have tried hard enough to do the work.
Wrong. If those didn't work it's because they were the wrong approach for what the person was struggling with. These therapists need to face up to the fact that the cognitive therapies are inadequate for in-depth treatment. Providing only cognitive therapy is neglectful at best. It is willfully neglegent because we know there are other tried-and-true therapies that work much better for people who aren't simply struggling with a temporary issue.
I'm not angry so much as I'm heartbroken because I know for a fact that this isn't how it has to be - because this isn't how it was.
#mental illness#mental health#actually mentally ill#psych abolition#cognitive therapy#cbt therapy#dbt therapy#act therapy#CPTSD#bpd safe#cluster b safe#personality disorders#marginalized groups
0 notes
Text
Beverly Hills Inpatient Mental Health Services
At Bridges to Recovery, we provide premier inpatient mental health services in Beverly Hills, offering a safe, private, and supportive environment where individuals can focus entirely on their recovery. We specialize in treating complex mental health disorders through individualized care plans that integrate evidence-based therapies and holistic treatments. Our goal is to help each client achieve lasting recovery and emotional well-being by addressing both the symptoms and underlying causes of their mental health challenges.
Why Choose Our Mental Health Treatment Facility
Choosing the right mental health treatment facility is critical for achieving sustainable recovery. At Bridges to Recovery, we pride ourselves on offering personalized, one-on-one care in a peaceful, home-like setting. With only six clients per residence, we ensure that every individual receives the focused attention they need from our team of experienced clinicians. Our Beverly Hills facility fosters a sense of comfort and security, allowing clients to fully engage in their healing journey.
We take a holistic approach to mental health care, combining traditional therapies like cognitive behavioral therapy (CBT) with holistic practices such as yoga, meditation, and physical fitness. This comprehensive approach supports the mental, emotional, and physical health of our clients, allowing them to heal on all levels and build a foundation for long-term recovery.
Therapies Provided for Behavioral Health Treatment
Bridges to Recovery offers a wide range of therapeutic modalities to address the diverse needs of our clients. These therapies include:
Cognitive Behavioral Therapy (CBT): Helps clients identify and challenge negative thought patterns and behaviors.
Dialectical Behavior Therapy (DBT): Focuses on emotional regulation, mindfulness, and improving interpersonal relationships.
Psychodynamic Therapy: Encourages exploration of unconscious thoughts and emotions to better understand their impact on behavior.
EMDR (Eye Movement Desensitization and Reprocessing): A trauma-focused therapy that helps clients process distressing memories and heal from traumatic experiences.
Holistic Therapies: Incorporating yoga, meditation, acupuncture, and physical fitness to promote overall well-being.
Inpatient Treatment Programs in Beverly Hills, CA
At Bridges to Recovery, we offer a variety of specialized inpatient treatment programs designed to provide intensive care in a nurturing, supportive environment. Each program is tailored to meet the unique needs of our clients and promote long-term recovery.
Anxiety Treatment
Our anxiety treatment program helps individuals manage generalized anxiety, social anxiety, and panic disorders. Through therapy, mindfulness practices, and holistic treatments, we help clients reduce anxiety symptoms and regain control over their lives.
Depression Treatment
Our depression treatment program is designed to address both the emotional and physical symptoms of depression. We combine therapy, holistic care, and medication management to help clients achieve emotional stability and rediscover joy and purpose in their lives.
Bipolar Disorder Treatment
Our bipolar disorder treatment program helps clients manage both manic and depressive episodes. Through individualized therapy and psychiatric care, we provide the tools needed for mood stabilization and long-term emotional balance.
ADHD Treatment
Our ADHD treatment program focuses on helping clients develop strategies to manage symptoms such as impulsivity, inattention, and hyperactivity. We provide therapy and behavioral interventions that improve focus, organization, and emotional regulation.
OCD Treatment
For individuals living with obsessive-compulsive disorder (OCD), we offer exposure and response prevention (ERP) therapy. Our program helps clients reduce compulsive behaviors, manage intrusive thoughts, and regain control over their daily lives.
PTSD Treatment
Our PTSD treatment program provides trauma-focused care for individuals suffering from post-traumatic stress disorder. We use evidence-based therapies like EMDR and somatic experiencing to help clients process and heal from traumatic experiences, promoting emotional stability and recovery.
Trauma Therapy
Our trauma therapy program is designed to help individuals heal from past traumatic events. We integrate various therapeutic approaches to help clients process trauma, develop healthier coping mechanisms, and achieve long-term recovery.
Panic Disorder Treatment
Our panic disorder treatment program helps individuals understand and manage panic attacks. Through therapy and relaxation techniques, we provide tools to reduce the frequency and intensity of panic episodes, allowing clients to regain control of their lives.
Antisocial Personality Disorder Treatment
We offer specialized care for antisocial personality disorder, focusing on helping clients develop healthier behaviors, increase empathy, and build stronger relationships. Our therapy programs support emotional and social growth, fostering positive change.
Borderline Personality Disorder Treatment
We specialize in treating borderline personality disorder (BPD) through dialectical behavior therapy (DBT). Our program helps clients manage emotional instability, reduce impulsive behaviors, and build healthier, more fulfilling relationships.
Dependent Personality Disorder Treatment
Our dependent personality disorder treatment program helps clients develop independence and self-confidence. We offer individualized therapy to help clients reduce reliance on others and build a stronger sense of self.
Narcissistic Disorder Treatment
Our narcissistic personality disorder treatment program helps clients address underlying emotional vulnerabilities and develop healthier interpersonal relationships. We provide compassionate care that promotes self-awareness and personal growth.
Complicated Grief Treatment
For individuals living with unresolved or prolonged grief, our complicated grief treatment program offers emotional support and therapeutic care. We help clients process their loss in a safe, compassionate environment and move toward healing and closure.
Dissociative Disorder Treatment
Our dissociative disorder treatment program helps clients reconnect with their sense of self and manage dissociative symptoms. We provide trauma-informed care that promotes emotional integration and long-term healing.
Childhood Trauma Treatment
Our childhood trauma treatment program helps individuals heal from early life experiences that have left a lasting impact on their mental health. We use trauma-focused therapies to address the psychological effects of childhood trauma, fostering long-term recovery.
Schizophrenia Treatment
Our schizophrenia treatment program offers comprehensive care for individuals experiencing symptoms such as hallucinations, delusions, and disorganized thinking. We provide therapy and medication management to help clients stabilize and improve their daily functioning.
Schizoaffective Disorder Treatment
Our schizoaffective disorder treatment program addresses both mood and psychotic symptoms, helping clients achieve emotional stability and improved mental health. We offer personalized therapy and psychiatric support to guide clients toward recovery.
Reach Out to Our Mental Health Clinic in Beverly Hills
If you or a loved one is living with mental health challenges, Bridges to Recovery in Beverly Hills is here to help. Our inpatient treatment programs provide the care and support necessary for lasting recovery in a peaceful, nurturing environment. Contact us today to learn more about how we can guide you on your path to healing and well-being.
1 note
·
View note
Text
Top Arizona Psychologist: Dr. Karen Hawk Specializing in Therapy and Counseling
When it comes to mental health, finding the right psychologist can make all the difference. Whether you're dealing with stress, anxiety, depression, relationship challenges, or trauma, a skilled psychologist can provide the support, tools, and guidance needed to help you navigate life's difficulties and achieve greater emotional wellness. In Arizona, Dr. Karen Hawk stands out as one of the leading psychologists, known for her compassionate approach, expertise, and dedication to her clients’ well-being.
In this blog post, we’ll explore why Dr Karen Hawk Psychologist Arizona is considered one of the top psychologists in Arizona and how she specializes in therapy and counseling to support individuals, couples, and families.
Dr. Karen Hawk: An Experienced and Compassionate Psychologist
Dr. Karen Hawk is a licensed psychologist in Arizona with extensive training and experience in a wide range of therapeutic techniques. With a deep commitment to helping individuals achieve mental wellness, Dr. Hawk provides compassionate, client-centered care. Whether you are dealing with specific mental health conditions or just need a supportive space to talk, Dr. Hawk’s approach to therapy is rooted in empathy, respect, and professionalism.
Her therapeutic approach emphasizes collaboration and trust, where clients are encouraged to actively participate in their healing process. Dr. Hawk works closely with her clients to understand their unique experiences, perspectives, and goals, and tailors each treatment plan to address their individual needs. This personalized approach ensures that clients receive the most effective care for their specific concerns.
Areas of Specialization
Dr Karen Hawk Psychologist practice covers a wide variety of mental health challenges, with a focus on helping individuals, couples, and families improve their emotional health and relationships. Some of the key areas she specializes in include:
1. Anxiety and Stress Management
Anxiety is one of the most common mental health challenges individuals face today, and it can manifest in many different ways—whether it's chronic worry, panic attacks, or constant stress. Dr. Hawk specializes in helping clients understand the root causes of their anxiety and provides them with effective strategies to manage their symptoms.
Using evidence-based techniques such as Cognitive Behavioral Therapy (CBT) and relaxation training, Dr. Hawk helps clients reframe negative thought patterns, develop coping skills, and regain control over their emotions. By teaching mindfulness and stress-reduction techniques, Dr. Hawk empowers clients to face anxiety-provoking situations with confidence and calm.
2. Depression and Mood Disorders
Depression can impact nearly every aspect of life, from daily activities to relationships and work. Dr. Hawk specializes in treating mood disorders, including major depressive disorder, dysthymia, and bipolar disorder. Through therapy, she helps clients identify underlying emotional triggers, challenge negative thought patterns, and develop healthy coping mechanisms to improve mood and outlook.
Her approach often involves Cognitive Behavioral Therapy (CBT) to challenge distorted thinking, combined with goal-setting techniques to help clients develop a sense of hope and purpose. Dr. Hawk also works with clients to improve self-care practices and create a balanced lifestyle that supports mental well-being.
3. Trauma and PTSD
Dr Karen Hawk Psychologist Arizona a strong background in trauma-informed therapy and specializes in helping individuals who have experienced trauma, whether recent or in the past. Whether the trauma is related to abuse, accidents, combat, or other life-altering events, Dr. Hawk works with clients to process and heal from these experiences.
Using specialized therapies like Eye Movement Desensitization and Reprocessing (EMDR) and trauma-focused Cognitive Behavioral Therapy (CBT), Dr. Hawk helps clients work through painful memories, reduce the emotional charge of traumatic events, and regain a sense of control over their lives. The goal is to help individuals heal from their trauma and rebuild their emotional resilience.
4. Relationship Counseling and Couples Therapy
Dr. Hawk understands that healthy relationships are key to overall emotional wellness. Whether you are dealing with communication issues, conflict, or intimacy problems, Dr. Hawk offers couples counseling to help partners strengthen their connection and resolve relationship challenges.
She employs evidence-based approaches to help couples understand each other’s needs, improve communication, and develop strategies for resolving conflict in a healthy and constructive way. Her goal is to help couples rebuild trust, improve emotional intimacy, and navigate the ups and downs of their relationship with mutual understanding and respect.
5. Family Therapy
Family dynamics can be complex, and when conflict arises, it can affect everyone involved. Dr. Hawk provides family therapy to help families improve communication, resolve conflicts, and strengthen their bonds. Whether the issue involves parent-child relationships, sibling rivalry, or blended family challenges, Dr. Hawk works with families to improve understanding and foster harmony.
In family therapy, Dr. Hawk helps each family member express their thoughts and feelings in a safe and non-judgmental space, fostering empathy and collaboration. The goal is to create healthier relationships and a more supportive family environment.
6. Personal Growth and Self-Esteem
Many individuals seek therapy not just to address specific mental health issues but to foster personal growth and improve self-esteem. Dr. Hawk specializes in helping clients increase self-awareness, develop a more positive self-image, and achieve their personal goals.
Through therapy, Dr. Hawk encourages clients to explore their strengths, challenge limiting beliefs, and work toward greater self-acceptance. Her approach is empowering, helping individuals realize their potential and pursue the life they want with confidence and resilience.
Dr. Hawk’s Therapeutic Approach
What sets Dr Karen Hawk Psychologist apart from other psychologists is her holistic and integrative approach to therapy. Rather than focusing solely on symptoms, Dr. Hawk works to address the root causes of mental health challenges, guiding clients through a comprehensive healing process.
1. Client-Centered Care
Dr. Hawk believes in a collaborative and client-centered approach to therapy. She sees each individual as the expert on their own life and works with them to create a treatment plan that fits their unique needs and goals. She takes the time to listen, understand, and respond to each client's concerns, fostering a sense of trust and partnership in the therapeutic relationship.
2. Evidence-Based Techniques
Dr. Hawk uses scientifically proven therapeutic techniques to ensure that her clients receive the most effective care. By integrating Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), mindfulness, and trauma-focused therapies, she provides clients with a toolkit of strategies to address their challenges and achieve emotional balance.
3. Holistic Focus
Dr. Hawk recognizes that mental health is closely intertwined with physical and emotional well-being. In addition to talk therapy, she encourages clients to consider other aspects of their life, such as physical health, lifestyle, and social connections, as part of their overall mental wellness. This holistic perspective allows for a more comprehensive approach to healing and personal growth.
4. Warm, Empathetic Environment
Dr. Hawk’s practice is built on creating a warm and empathetic environment where clients feel comfortable, understood, and supported. She recognizes that therapy can be a vulnerable experience, and she strives to create a space where clients can express themselves openly without fear of judgment. This supportive environment encourages trust and fosters a sense of safety, which is essential for effective therapy.
Why Choose Dr. Karen Hawk?
As one of Arizona's top psychologists, Dr. Hawk stands out for her expertise, compassionate care, and personalized approach to therapy. Clients choose Dr. Hawk because:
She tailors treatment to each individual: Dr. Hawk takes the time to understand each client’s unique needs and goals, creating a personalized therapy plan.
She offers a wide range of services: Whether you're an individual seeking therapy for anxiety or depression, a couple looking to strengthen your relationship, or a family in need of conflict resolution, Dr. Hawk provides services to meet a variety of needs.
She uses evidence-based practices: Dr. Hawk employs scientifically supported techniques to help clients achieve lasting change.
She fosters a supportive, non-judgmental environment: Clients feel safe and understood in Dr. Hawk’s practice, which is essential for effective healing.
Get Started with Dr. Karen Hawk Today
If you’re looking for an experienced psychologist in Arizona who specializes in therapy and counseling, Dr. Karen Hawk is here to help. With a commitment to your mental wellness and a compassionate, client-centered approach, Dr. Hawk can guide you through your challenges and help you achieve the emotional health and happiness you deserve. Reach out today to schedule a consultation and take the first step toward a better, more fulfilling life.
0 notes
Text
Understanding Mental Health: A Deep Dive Into the Most Common Conditions

Understanding mental health is crucial for everyone, as it impacts our daily lives, relationships, and overall well-being. This blog post will explore ten common types of mental health conditions, shedding light on their symptoms, causes, and potential treatments. By the end, you will have a better understanding of these conditions, which can help in nurturing empathy and providing support to those affected.
Anxiety Disorders
Anxiety disorders are characterized by excessive fear and worry. These feelings can interfere with daily activities like work and social interactions. Common forms include generalized anxiety disorder, panic disorder, and social anxiety disorder. Symptoms may involve restlessness, rapid heartbeat, and difficulty concentrating. Treatments often combine therapy and medication to help manage symptoms effectively.
Depression
Depression is more than just feeling sad. It’s a serious mental health condition that affects how one feels, thinks, and handles daily activities. Symptoms range from persistent sadness and loss of interest in activities to changes in appetite and sleep patterns. Treatment usually involves a mix of medications like antidepressants and psychotherapy, offering a holistic approach to recovery.
Bipolar Disorder
Bipolar disorder involves extreme mood swings ranging from manic highs to depressive lows. During manic phases, individuals may feel euphoric and full of energy, while depressive phases can lead to overwhelming sadness and fatigue. Medication and therapy are key components in managing this condition, helping stabilize mood swings and improve quality of life.
Schizophrenia
Schizophrenia is a severe mental health condition that affects a person’s ability to think clearly, manage emotions, and interact with others. Symptoms include hallucinations, delusions, and disorganized thinking. Antipsychotic medications and psychosocial treatments are essential in managing schizophrenia, aiming to reduce symptoms and support functional recovery.
Anger Management Disorder
Anger management disorder involves the inability to control one's anger responses, often leading to aggressive behavior and emotional distress. Individuals may experience heightened irritability, frequent outbursts, and difficulty calming down after being upset. This condition can negatively impact relationships and overall well-being. Effective treatment, like therapy or online adult anger management program, which often includes cognitive-behavioral therapy, which helps individuals identify triggers and develop healthier coping strategies to manage their anger constructively.
Obsessive-Compulsive Disorder (OCD)
OCD is characterized by unwanted, repetitive thoughts (obsessions) and behaviors (compulsions). These can interfere with daily functioning and cause significant distress. Common compulsions include excessive cleaning and checking. Treatment often involves cognitive-behavioral therapy (CBT) and medications, which help manage symptoms and improve coping mechanisms.
Post-Traumatic Stress Disorder (PTSD)
PTSD can develop after experiencing or witnessing a traumatic event. Symptoms can include flashbacks, nightmares, severe anxiety, and uncontrollable thoughts about the event. Therapy, such as exposure therapy and EMDR (Eye Movement Desensitization and Reprocessing), alongside medication, can significantly alleviate symptoms and support recovery.
Eating Disorders
Eating disorders, such as anorexia nervosa, bulimia nervosa, and binge-eating disorder, are serious conditions related to persistent eating behaviors negatively impacting health. These disorders often involve preoccupation with food, body weight, and shape, leading to dangerous eating habits. Treatment typically includes nutritional counseling, therapy, and medical monitoring.
Attention-Deficit/Hyperactivity Disorder (ADHD)
ADHD is commonly diagnosed in children but can persist into adulthood. It involves symptoms like inattentiveness, hyperactivity, and impulsivity. These can affect academic performance and social interactions. Treatment often includes stimulant medications and behavioral therapies, helping individuals improve focus and manage symptoms effectively.
Borderline Personality Disorder (BPD)
BPD is characterized by intense emotional instability, impulsive behavior, distorted self-image, and unstable relationships. Individuals with BPD may experience episodes of anger, depression, and anxiety lasting a few hours to days. Dialectical behavior therapy (DBT) has proven effective in treating BPD, helping individuals develop emotional regulation and interpersonal skills.
Understanding these common mental health conditions can foster empathy and support for those affected. Awareness is the first step towards breaking the stigma and encouraging individuals to seek help. If you or someone you know is struggling with mental health, consider reaching out to a healthcare professional for guidance and support. For further resources, visit our website and explore available support options.
0 notes
Text
Why Choose Luxury Rehab Center in Dehradun?

All rehabs are not created equal. At any licensed drug and alcohol addiction center, you can expect a treatment program to help you detox — but there is so much more to rehab than detox.
Luxury rehab offers addiction treatment programs of the highest quality, all in an idyllic setting. Though the cost of luxury rehab is typically higher than that of standard rehab, clients find the investment in their recovery worthwhile.
Take a look at the benefits of luxury rehab vs. standard rehab so you can choose the best option for your individual needs.
Personalized Care Plan
One of the key benefits of luxury rehab center over standard rehab is personalization. At a luxury rehab, you will not be assigned to a one-size-fits-all program. Rather, you will receive individualized care and a treatment plan that’s matched to your unique circumstances and diagnoses.
For example, luxury rehab centers typically offer dual diagnosis treatment to address co-occurring substance abuse and mental health issues, such as anxiety, depression, PTSD, and bipolar disorder. Custom treatment plans are a hallmark of luxury rehab, providing a deep level of personalization and accommodation of your individual needs.
One-on-One Attention
Such personalized care is possible because of the low client-to-staff ratio at private rehab centers. With a limited number of clients at any given time, luxury rehabs have a greater degree of freedom in structuring treatment plans to the client, rather than the other way around. As a result, you will receive the utmost attention and care. NuLifeLineCare Rehab, for instance, only serves 40 clients at a time to ensure the highest standards of addiction care. In luxury rehab, you are more than a number — you are a unique individual.
Holistic Treatment
While both luxury rehab and standard rehab provide detox and therapy from licensed addiction specialists, luxury rehab offers so much more. At a private rehab center, you can benefit from holistic treatment that addresses your physical, mental, emotional, and spiritual needs. Such treatments may include art therapy, music therapy, EMDR therapy, and others.
You can also enjoy access to holistic activities like yoga, meditation, and horseback riding, as well as massage and chiropractic treatment. These activities support your personal transformation and healthy lifestyle, with amenities that are simply not available in a standard rehab center.
Plenty of Privacy
Though there is no shame in seeking help for addiction, there is also no reason for others to know your private business. That’s where luxury rehab plays an essential role. With remote locations and strict security measures, you can rest easy knowing your privacy is being carefully safeguarded.
In luxury rehab, single-occupancy rooms and suites enable you to enjoy the privacy and anonymity you desire. While there are opportunities to interact with other clients, you can also retreat to the comfort of your own luxurious indoor space or a peaceful outdoor setting.
Minimal Distractions
Conquering addiction requires time and energy dedicated to rehab and recovery. At a luxury rehab, you won’t have to deal with the distractions of bad food, uncomfortable accommodations, or hard labor. Instead, staff members will take care of the cooking, cleaning, and other chores so you can concentrate on your treatment and recovery. Luxury rehab removes barriers to success so you can focus on why you’re there in the first place — to overcome addiction.
Serene Setting
If you’d like to seek treatment in a relaxing environment instead of hospital-like surroundings, luxury rehab has what you’re looking for. Luxury rehabs are typically found in tranquil locations such as tropical beach resorts or calming mountain retreat centers, providing an ideal backdrop for recovery.
NuLifeLineCare Rehab, for instance, offers an intimate setting on the beautiful mountains of Dehradun, Uttarakhand, campus with exclusive access to the lush natural landscape. Throughout your treatment, you’ll enjoy stunning views , sunny skies, and swaying trees.
Luxury rehab offers a high-quality, holistic approach to recovery in a beautiful location. The personal support and individualized programs can help you commit to the full course of treatment needed to start a new, addiction-free life.
Is luxury rehab right for you? Contact NuLifeLineCare Rehab’s trained admissions counselors at 8958305058 to discover the full suite of amenities at our private rehab center.
#drugsfreeindia#saynotodrugs#nashamuktbharat#nashamuktbharatabhiyaan#nmba#bestrehabcentre#rehabilitation#nashamuktikendra#bestrehabindehradun#uttarakhand#fightagainstdrugs#fightagainstaddiction#nomoredrugs#addictionawareness#addictionrecovery#recovery#nasha_ab_nahi#bandkaronasha#dehradun#addiction#bestnashamuktikendra#nulifelinecarerehab
0 notes
Text
Unlocking Healing Paths: The Transformative Power of EMDR for Stress Relief
In the realm of stress relief, EMDR stands as a beacon of hope, offering a unique and powerful approach to healing. Its ability to target the root causes of stress, reprocess traumatic memories, and promote adaptive responses positions it as a transformative therapy for individuals seeking relief from the burdens of modern life.
#emdr for stress#emdr psychotherapy#emdr therapy and bipolar disorder#eye movement therapy for anxiety#eye movement therapy for depression#eye movement desensitization and reprocessing#Dissociative Identity Disorder
0 notes
Text
emdr for heff! part 1
By the way! I’m sorry that it took so long for me to get to this. I actually had it in my reminders app in my phone (I can’t live without the reminders app) so whenever I opened it I was like oh yeah ! I need to get in touch with you about EMDR! As I’ve said, there’s a lot going on for me this summer in general plus the Lampard holes in the brain, but I always remember eventually! So I figured I would slide into your DMs. And…here we go! Warning: long
I’m really happy to always share stuff about mental health, mental illness journey, etc. I’ve been through a lot and some of the problems I’ve had don’t ever get talked about on this website, even though Tumblr’s very pro…mental health and healing. In my situations, I’m often, and by often I mean always, completely alone. So, I don’t really believe in TMI, very little about my situation is TMI, and I have no problem just not sharing what I’m not comfortable with, so that’s fine.
So EMDR…I started it in April and the first few sessions you don’t really do the actual procedure. The first session was just a quick visit to see if we’d be a good fit. I do it virtually, which is great for my schedule. Then next session you do the “intake” and you go over your concerns, your family history, etc. For me, because I’m 1014194 years old and have had this problem basically my entire life, and I’ve been in therapy for so long that I’m very aware of all of the things, the intake took I believe 2 or 3 50-minute sessions. I also have bipolar disorder! (this is why I talk so much! It’s one of the most common and annoying symptoms lol), so I’ve had a crazy adult life full of crazy shit especially before I took medication, so there was a LOT to say. But it was good, because I actually felt comfortable telling her stuff I’ve never told anyone else other than my best friend maybe—not even comfortable enough to tell other therapists. So I guess it took over a month to really start going through the memories of my trauma.
I have childhood trauma—it’s complex trauma (CPTSD). Idk how much you know about this stuff, but with CPTSD you basically got retraumatized over and over. It’s usually just easier to say PTSD when you’re talking about it offline, but complex trauma is often even harder to deal with and has a very big impact on your life, especially with how you interact with the world socially. I genuinely have no idea who I am without it, which is trippy and a half. I got this diagnosis 12 years ago, and the doctor I work with on that is really amazing (GENERALLY—he’s also the fucker who’s told me I talk too much, AND I have to see him later today and I’ve got beef with him from him telling me I talk too much two weeks ago so…*cracks knuckles*). However, bipolar and CPTSD are a very difficult duo to manage.
(Bipolar is what I mean when I say that tumblr doesn’t talk about it…I don’t think I’ve ever known more than one other Internet Person who’s had it like…in all my years of being on the internet. It is known to be hard to diagnose, because people don’t go to therapy when they feel “good” (even though if the “good” is mania you often feel fucking awful in a unique way that I would definifely wish on my worst enemy), and if they tell a therapist they feel depressed, it’s easy for a therapist to just prescribe antidepressants and be done with it. The number of therapists and even psychiatrists who are clueless about bipolar disorder is higher than the number of men Franky’s fantasized about sleeping with! But uh, anyway.) I’m not truly alone because SO many people in my extended family have it (it’s CONTAGIOUS!) and we all take the same medication lol, but still, it’s like the hidden disorder that no one on tumblr ever talks about. So, I’m down to talk about anything, because these things have an extreme impact on how I behave and the energy I have to spend on myself, if that makes sense.
But yeah, it’s a very difficult combination because you’re very reactive. With bipolar, your brain reacts very inappropriately and dramatically to any kind of stimuli. That’s sort of the fundamental of it. So, something could set me off, and it can trigger the fight or flight of the trauma to kick in, and once the trauma kicks in it’s very hard to tone that down, even if you’re knowledgeable and aware, you take your medications, you’re much more stable, etc. It’s a physical reaction and it’s based on the kind of reaction you’re supposed to have to danger! My psychiatrist is always like, “if you were a caveman you’d be number 1 caveman, you’re hypervigilant, you always have 20 backup plans in your mind, you’d survive very well.” But of course we don’t live in that kind of world. It’s very difficult, very paralyzing, and has created a lot of trouble for me and I spend a lot of time dissociating. Which I enjoy. It’s kind of like an addiction to be honest. A lot of the time, I prefer to be in my own head than interact socially, which sigh. In offline life I pass for “normie” very well if I need to, but I just don’t have a lot of friends in person. I could, that’s the thing, I could, but I prefer to be in my own head, and I don’t always like that. Sometimes that gets me feeling lonely, frustrated, etc. but yeah…That’s kind of the introduction. Yikes.
My trauma is also very strange—and this is where I don’t totally want to share the details—because it’s just weird, it’s different than a lot of other people I know’s trauma, and what me and my mom think is that it’s something that started pre-memory, so the stuff that traumatized me is likely to have started happening when I was an actual baby. That’s harder to access of course, since…you can’t remember it! I had to check with my EMDR therapist to make sure she can work with pre-memory and early trauma. (By the time I was in school, so like four years old, I was pretty noticeably fucked up.)
Obviously, I’m not saying it’s “better” to have trauma from later on in life, but it’s easier to work with in that for the most part those memories are more accessible, or can become more accessible.
I don’t think EMDR changes things very quickly, but about a month ago I started feeling like I was able to make sense of some important things in my head—mostly, stuff about the very nonexistent or abusive (depending on the day) relationship between my mind and body. My mind hates and disrespects my body, which I feel makes a lot of sense for a trauma victim, and all of a sudden I’m making some positive changes to unite the two that have NEVER been possible in over 3 decades. I have serious issues that need help beyond that but this is giving me some hope. It’s definitely not a quick fix but I think even the process of doing EMDR gives you some of that hope.
I’m always telling my EMDR therapist, “This seems fake!” or that it seems like a really bad movie written about a crazy person by someone who’s never had mental health issues. Because the stuff that my head is just coming up with, and how correct/unsurprising it feels, is really remarkable. It truly is crazy, and I don’t know how this works. My mom is a therapist herself and she’s explained it to me but anything remotely sciencey is Not my thing so I can’t remember. It’s just sort of shaken up so much in my brain. My younger self has spoken to me, I’ve argued with myself, my younger self has made me cry and hurt my feelings because of how angry she is at me for not being able to “get her help”…it’s wild. I find it really incredible, but it’s not always easy. OKAY I’m going to get to your questions.
0 notes
Text
Welcome to Grace Health Care NP: Your Partner in Comprehensive Mental Health and Wellness
At Grace Health Care NP, we understand that mental health and overall well-being are crucial to leading a fulfilling life. Our dedicated team is here to support you through a range of services designed to address various mental health and wellness challenges. Whether you’re struggling with anxiety, dealing with sleep disorders, or seeking support for women’s health issues, we’re here to provide compassionate and professional care tailored to your unique needs. Explore our services below to learn how we can assist you on your path to better health.
ADHD (Attention-Deficit/Hyperactivity Disorder)
ADHD can impact various aspects of life, from work to relationships. At Grace Health Care NP, we offer personalized evaluations and treatment plans to help manage ADHD symptoms effectively. Our approach includes behavioral strategies, medication management, and support to enhance focus and organization, ultimately improving your quality of life.
Anxiety Disorder
Anxiety can be overwhelming and interfere with daily functioning. Our team provides a range of treatments including cognitive-behavioral therapy (CBT), mindfulness techniques, and medication options. We work with you to identify triggers and develop coping strategies that help you regain control and reduce anxiety.
Behavioral Issues
Behavioral issues can manifest in many forms and affect various aspects of life. We offer comprehensive assessments and interventions tailored to individual needs. Our goal is to help you understand and manage behavioral patterns, improving your overall well-being and interpersonal relationships.
Bipolar Disorder
Bipolar disorder requires a nuanced approach to treatment. Our experienced practitioners offer a combination of medication management and psychotherapy to help stabilize mood swings and support long-term mental health. We work closely with you to develop a treatment plan that addresses both the symptoms and the underlying causes of bipolar disorder.
Coping Skills
Developing effective coping skills is essential for managing stress and overcoming challenges. At Grace Health Care NP, we provide resources and techniques to help you build resilience and handle life’s ups and downs with greater ease. From stress management workshops to one-on-one counseling, we’re here to equip you with practical tools for everyday life.
Depression
Depression can affect every aspect of life, making it difficult to find joy and motivation. Our approach to treating depression includes a combination of therapy and medication, tailored to your specific needs. We aim to help you navigate through depression, regain a sense of purpose, and improve your overall mental health.
ODD (Oppositional Defiant Disorder)
ODD can create challenges in relationships and daily functioning. Our team specializes in providing strategies and interventions to address oppositional and defiant behaviors. We work collaboratively with you to implement effective techniques that promote positive behavior changes and improve relationships.
PTSD (Post-Traumatic Stress Disorder)
PTSD can significantly impact your life following traumatic experiences. We offer trauma-informed care, including evidence-based therapies such as EMDR (Eye Movement Desensitization and Reprocessing) and trauma-focused CBT. Our goal is to help you process trauma, alleviate symptoms, and move towards healing and recovery.
Sleep Disorder
Sleep is vital for overall health and well-being. If you’re struggling with sleep disorders, our team can help diagnose and treat conditions such as insomnia, sleep apnea, and restless leg syndrome. We provide comprehensive assessments and personalized treatment plans to help you achieve restful and restorative sleep.
Women’s Health Issues
Women’s health encompasses a wide range of physical and mental health concerns. At Grace Health Care NP, we offer specialized care addressing issues such as hormonal imbalances, menstrual disorders, and menopause. Our goal is to provide holistic support to enhance your overall health and well-being.
Why Choose Grace Health Care NP?
At Grace Health Care NP, our mission is to provide high-quality, compassionate care to support your mental health and overall wellness. Our team of professionals is dedicated to understanding your unique needs and working with you to create a personalized care plan. We are here to offer support, guidance, and expertise every step of the way.
If you’re ready to take the next step towards improved health and well-being, contact us today to schedule a consultation. Let us be your partner in achieving a healthier, happier you.
0 notes
Text
Second Life Rehabilitation Centre: Leading Rehabilitation Centre in Delhi

Second Life Rehabilitation Centre stands as a premier rehabilitation centre in Delhi, renowned for its comprehensive and holistic approach to recovery. With a focus on addiction treatment, mental health services, and physical rehabilitation, Second Life offers tailored programs to meet the unique needs of each individual. This article highlights the key features and benefits of choosing Second Life Rehabilitation Centre for a path to recovery and wellness.
why choose second life rehabilitation centre?
Second Life Rehabilitation Centre In Delhi excels providing effective addiction treatment programs. Understanding that addiction is a multifaceted condition, the centre adopts a holistic approach to ensure long-term recovery. Key components of their addiction treatment include:
Detoxification: The initial phase involves medically supervised detox to safely manage withdrawal symptoms and prepare the patient for ongoing treatment.
Counseling and Therapy: Individual and group therapy sessions are central to the program. Techniques such as Cognitive Behavioral Therapy (CBT) and Motivational Interviewing help patients understand and overcome the underlying causes of their addiction.
Family Support: The centre emphasizes the importance of family involvement in the recovery process, offering counseling sessions to help rebuild trust and improve family dynamics.
Mental Health Services
As a leading rehabilitation centre in Delhi, Second Life Rehabilitation Centre provides specialized mental health services to address a variety of conditions. Their team of experienced psychiatrists, psychologists, and counselors work together to offer comprehensive care for:
Depression and Anxiety: Customized treatment plans that include therapy, medication, and lifestyle modifications to manage and alleviate symptoms.
Bipolar Disorder: Integrated care plans that encompass medication management, psychotherapy, and support groups to help stabilize mood and enhance quality of life.
Post-Traumatic Stress Disorder (PTSD): Utilizing evidence-based therapies such as Eye Movement Desensitization and Reprocessing (EMDR) and trauma-focused CBT to help patients process and recover from traumatic experiences.
Physical Rehabilitation Services
Second Life Rehabilitation Centre is also a leader in physical rehabilitation, offering tailored programs for individuals recovering from injuries, surgeries, or chronic conditions. The centre’s physical rehabilitation services include:
Physiotherapy: Personalized exercise and treatment plans designed to improve mobility, strength, and function.
Occupational Therapy: Helping patients regain the skills needed for daily living and work activities.
Pain Management: Comprehensive pain management strategies that include medication, physical therapy, and alternative therapies such as acupuncture.
Holistic Healing Approach
A distinguishing feature of Second Life Rehabilitation Centre is its holistic approach to healing. The centre integrates traditional medical treatments with complementary therapies to promote overall well-being. This approach includes:
Yoga and Meditation: Enhancing mental and physical health through practices that reduce stress and improve focus.
Nutritional Counseling: Developing healthy eating plans to support recovery and overall health.
Recreational Activities: Engaging patients in activities such as art therapy, music therapy, and sports to promote social interaction and physical fitness.

Plus points of choosing second life rehabilitation centre
Experienced and Compassionate Staff
The success of Second Life Rehabilitation Centre is largely due to its team of experienced and compassionate professionals. The staff includes doctors, nurses, therapists, and support personnel who are dedicated to providing personalized and empathetic care. Their expertise ensures that each patient receives the best possible treatment tailored to their specific needs.
State-of-the-Art Facilities
Second Life Rehabilitation Centre offers state-of-the-art facilities designed to provide a comfortable and conducive environment for recovery. The centre features modern medical equipment, comfortable accommodations, and serene outdoor spaces that enhance the healing process.
Commitment to Sustainability
In addition to focusing on high-quality care, Second Life Rehabilitation Centre in Delhi is committed to sustainability. The centre adopts eco-friendly practices in its operations and promotes environmental awareness among its staff and patients.

Get in Touch
SECOND LIFE
561/2 Village Dera Chhatarpur Behind Sunder Gym New Delhi 110074
+91-9810638232
1 note
·
View note
Text
Exploring the Expertise of Michele Green: A Compassionate Guide on the Path to Healing
Michele Green, a dedicated professional with a Master's Degree in Social Work from the University of Nevada, Las Vegas (2013), stands out as a beacon of support and understanding in the realm of mental health. As a licensed Clinical Director holding the designations of MSW (Master of Social Work) and LSW (Licensed Social Worker), Michele brings a wealth of knowledge and experience to her practice. Specializing in trauma, Michele is known for her compassionate approach in assisting individuals who have faced sexual, physical, and emotional trauma and abuse. Let's delve into the expertise and specialties that define Michele Green's therapeutic practice.
Specialties: Michele's professional expertise encompasses a wide array of mental health specialties, demonstrating her commitment to addressing diverse needs. Her areas of specialization include:
Anxiety: Offering support to individuals grappling with overwhelming anxiety.
Depression: Providing guidance and therapeutic interventions for those navigating the challenges of depression.
Grief: Assisting individuals in coping with the complexities of grief and loss.
PTSD: Supporting those dealing with post-traumatic stress disorder.
Addiction: Offering a compassionate approach to individuals struggling with addiction.
Bipolar Disorder: Providing guidance and strategies for managing bipolar disorder.
Coping Skills: Equipping individuals with effective coping mechanisms for life's challenges.
Gender Dysphoria and Gender Transitioning: Specialized support for individuals exploring their gender identity and transitioning.
Self-Harming: Assisting individuals in understanding and overcoming self-harming behaviors.
Substance Use: Supporting individuals dealing with substance use issues.
Suicidal Ideation: Offering a safe space for those navigating thoughts of self-harm or suicide.
Transgender: Providing affirming and understanding therapy for transgender individuals.
Trauma and PTSD: Specialized support for individuals who have experienced trauma and post-traumatic stress disorder.
Women's Issues: Addressing mental health concerns unique to women.
Dissociative Disorders (DID): Supporting individuals with dissociative disorders.
Mood Disorders: Providing guidance for individuals dealing with various mood disorders.
Client Focus: Michele's empathetic and inclusive approach is reflected in her diverse client focus, which includes:
Families
Individuals
Adults
Teens
Bisexual Allied
Gay Allied
Intersex Allied
Lesbian Allied
Non-Binary Allied
Open Relationships Non-Monogamy
Queer Allied
Sex Worker Allied
Sex-Positive, Kink Allied
Transgender Allied
Type of Therapy: Michele Green employs a versatile range of therapeutic approaches to meet the unique needs of her clients. These approaches include:
Clinical Supervision and Licensed Supervisors
Cognitive Behavioral Therapy (CBT)
Compassion Focused Therapy
Culturally Sensitive Therapy
Eclectic Therapy
Eye Movement Desensitization and Reprocessing (EMDR)
Emotionally Focused Therapy
Family Systems Therapy
Humanistic Therapy
Integrative Therapy
Internal Family Systems (IFS)
Motivational Interviewing
Somatic Therapy
Strength-Based Therapy
Trauma-Focused Therapy
Parts and Memory Therapy
Free Screening Assessment: To make mental health support more accessible, Michele Green and Insight Therapy Solutions offer a free short online screening test. This assessment covers various mental health concerns, including depression, anxiety, bipolar disorder, OCD, PTSD, panic disorder, postpartum depression, and social anxiety disorder. Individuals facing these challenges can initiate their mental health journey by taking this free screening assessment.
Conclusion: Michele Green, with her educational background, professional licenses, and diverse therapeutic expertise, stands as a beacon of support for individuals navigating the complexities of mental health. Her commitment to inclusivity, compassion, and evidence-based therapeutic approaches makes her a trusted guide on the path to healing. To schedule an appointment with Michele Green, individuals are encouraged to contact Insight Therapy Solutions at 888-409-8976. Embrace the opportunity to embark on a transformative journey towards improved mental well-being with Michele's expert guidance and support.
0 notes
Text
Unearthing the Buried Pain: The Devastating Effects of Untreated Childhood Trauma
Childhood is meant to be a time of innocence, laughter, and carefree moments. However, for many individuals, their formative years are marred by experiences of trauma that can leave lasting scars. The consequences can be profound and far-reaching when these wounds are left unattended. In this article, we will explore the harrowing journey of individuals who have experienced childhood trauma and the dire outcomes that can unfold when such trauma goes untreated.
The Prevalence of Childhood Trauma
Childhood trauma comes in various forms, including physical, emotional, and sexual abuse, neglect, witnessing domestic violence, and more. Sadly, it is more common than we might think. According to the Centers for Disease Control and Prevention (CDC), nearly two-thirds of adults in the United States have experienced at least one traumatic event during their childhood.
The Immediate Impact
Untreated childhood trauma can have immediate and lasting effects on a person's emotional, psychological, and physical well-being. During childhood, the immediate impact may manifest as behavioral problems, difficulties in school, anxiety, depression, or even post-traumatic stress disorder (PTSD). Children may struggle to form healthy relationships, experience trust issues, and have a distorted self-image.
The Long-Term Consequences
When childhood trauma remains unaddressed, the consequences can extend well into adulthood, affecting every aspect of a person's life.
Mental Health Issues
Untreated childhood trauma is a significant risk factor for the development of mental health disorders. Individuals may grapple with anxiety, depression, bipolar disorder, borderline personality disorder, and other conditions. These mental health issues can be crippling, making it challenging to hold down a job, maintain relationships, or find joy in life.
Substance Abuse and Addiction
Many individuals who have experienced untreated childhood trauma turn to drugs or alcohol as a means of coping with their emotional pain. Substance abuse becomes a dangerous escape from the memories and feelings associated with their traumatic past. This can lead to a vicious cycle of addiction, further compounding their struggles.
Physical Health Problems
Childhood trauma has been linked to a range of physical health problems in adulthood. High levels of stress hormones over an extended period can weaken the immune system, increase the risk of chronic diseases, and even reduce life expectancy. Individuals who have experienced untreated trauma may find themselves plagued by chronic pain, autoimmune disorders, or heart problems.
Self-Destructive Behaviors
In an attempt to numb the emotional pain or regain a sense of control, some survivors of childhood trauma engage in self-destructive behaviors. This can include self-harm, risky sexual behavior, or even suicidal tendencies. Without appropriate intervention, these behaviors can escalate and lead to tragic outcomes.
Difficulty Forming Healthy Relationships
One of the most profound impacts of untreated childhood trauma is the struggle to form and maintain healthy relationships. The scars left by early trauma can make it challenging to trust others, express emotions, or engage in open and honest communication. This can result in a pattern of failed relationships and social isolation.
Breaking the Cycle
While the consequences of untreated childhood trauma can be overwhelming, it is essential to recognize that healing is possible. Therapy, support groups, and other forms of treatment can help survivors address their trauma and work toward a brighter future.
Therapy and Counseling
Therapists and counselors with expertise in trauma can provide survivors with a safe and supportive environment to process their experiences. Techniques such as cognitive-behavioral therapy (CBT) and eye movement desensitization and reprocessing (EMDR) have been effective in helping individuals overcome the effects of childhood trauma.
Support Groups
Joining a support group for trauma survivors can provide a sense of community and understanding. Sharing experiences with others who have faced similar challenges can be incredibly validating and therapeutic.
Self-Care and Mindfulness
Practicing self-care and mindfulness techniques can help survivors manage their emotional responses and reduce stress. Meditation, yoga, and journaling can promote healing and resilience.
Building Healthy Relationships
Survivors can learn to build and sustain healthy relationships with therapy and support. This process may involve redefining trust, improving communication skills, and addressing any negative patterns learned in childhood.
Childhood trauma is a profoundly distressing experience that can cast a long shadow over an individual's life when left untreated. The consequences can encompass mental and physical health issues, addiction, self-destructive behaviors, and difficulties forming healthy relationships. However, it is crucial to recognize that recovery is possible. With the proper support and interventions, survivors can heal, break free from the cycle of trauma, and build fulfilling lives. Childhood trauma may leave scars, but it doesn't have to define one's future.
0 notes